Abstract
Background: Time to pregnancy (TTP) is a biomarker of fecundability and has been associated with behavioral and environmental characteristics; however, these associations have not been examined in a large population-based sample of application (app) users.
Materials and Methods: This observational study followed 5,376 women with an age range of 18 to 45 years who used an app to identify their fertile window. We included women who started trying to conceive between September 30, 2017 and August 31, 2018. TTP was calculated as the number of menstrual cycles from when the user switched to “Plan” mode up to and including the cycle in which they logged a positive pregnancy test. We examined associations with several characteristics, including age, gravidity, body mass index, cycle length and cycle length variation, frequency of sexual intercourse, and temperature measuring frequency. Discrete time fecundability models were used to estimate fecundability odds ratios.
Results: For the complete cohort the 6-cycle and 12-cycle cumulative pregnancy probabilities were found to be 61% (95% confidence interval [CI]: 59–62) and 74% (95% CI: 73–76), respectively. The median TTP was four cycles. The highest fecundability was associated with an age of less than 35 years, with cycle length variation <5 days and logging sexual intercourse on at least 20% of days added (the proportion of days in which intercourse was logged) (11.5% [n = 613] of entire sample). This group achieved a 6- and 12-cycle cumulative pregnancy probability of 88% (95% CI: 85–91) and 95% (95% CI: 94–97), respectively, and a TTP of 2 cycles.
Conclusions: Natural Cycles was an effective method of identifying the fertile window and a noninvasive educational option for women planning a pregnancy. Women under age 35 with regular cycles showed a high pregnancy rate.
Keywords: time to pregnancy, FABM, mobile application, fertility, conception
Introduction
Sexually active women who are attempting to become pregnant may be advised to use a fertility awareness based method (FABM) to identify her fertile window, especially if they are over 35 years old.1 The biological fertile window is defined as the 5 days before ovulation and the day of ovulation2 as this takes into account the time sperm can survive in the female genital tract and the 24 hours of egg viability. However, it is currently not possible to prospectively predict this with absolute certainty, and instead, various FABMs predict a larger fertile window in the hope that the biological 6 days time frame will be within the predicted. Dunson et al. (1999)3 found that the rate of conception was highest when intercourse occurred on the day before ovulation.
Methods for identifying the fertile window include the calendar method, measurement of basal body temperature (BBT), cervical mucus monitoring, and luteinizing hormone (LH) testing. Calendar based methods may be less accurate particularly for individuals with variable cycle lengths, especially given that few women have the textbook 28 day cycle with ovulation on day 14.4
The popularity of FABM mobile applications (apps) has grown considerably. There are more than 100 FABM mobile apps claiming to help women who are trying to conceive.5 Apps marketed as fertility apps mainly use menstrual cycle dates to estimate ovulation which do not rank as favorably as others that incorporate biometrics such as BBT/LH into the fertile window calculation. A previous study from our group found that Natural Cycles, a digital FABM of contraception, more accurately defined a shorter fertile window compared to the Rhythm and Standard Days methods.6
Natural Cycles provides personalized fertility predictions based on menstruation, BBT, and LH measurements.7 Menstruation and BBT logging are mandatory, while LH testing is optional. The primary use of the app is as a contraceptive in “Prevent” mode, but it can be used in “Plan” mode to identify the fertile window for those trying to conceive. Time to pregnancy (TTP) is shorter for women who used the app before trying to conceive versus those who had previously used hormonal contraception.8
In this study we aimed to investigate the time to conception for Natural Cycles users. We investigated factors associated with the probability of pregnancy, specifically age, gravidity, body mass index (BMI), menstrual cycle characteristics, and tracking of sexual intercourse.
Materials and Methods
Study population
Data were obtained from users of the fertility-awareness based mobile application Natural Cycles. The app uses a statistical algorithm that estimates the probability of conception on a given day.7 There are three modes in the app, “Prevent,” “Plan,” and “Follow (a pregnancy),” allowing users to choose the most suitable option for their current intentions. Most women start using the app in Prevent mode, that is, to prevent a pregnancy by avoiding unprotected intercourse during days which the app calculates to be fertile days. Users may subsequently change their intentions and are instructed to register this by switching to Plan mode in which the app serves as an aid to the timing of intercourse to achieve conception. The algorithm calculates the predicted fertile days in a similar way in both Prevent and Plan. The same colors are displayed (red for fertile and green for not fertile); however, in Prevent a day is either strictly red or green, whereas in Plan a color scale is used during the fertile window.
This observational cohort study included women aged 18 to 45 with the majority living in Sweden (31%), the United Kingdom (29%), and the United States (14%). Users provided the following information at registration, that is, when installing the Natural Cycles app and creating an account: country of residence, previous contraception type, date of birth, height, weight, and known medical conditions impacting fertility. Each day while using the app they could log BBT measurements, menstruation data, LH tests (if used), and sexual intercourse. Additional information, such as gravidity and level of education, was gathered through nonmandatory question-and-answer messages presented within the app a few weeks after registration. To have full access to the app functionalities, users were required to confirm that they had discontinued hormonal contraception before commencing app usage.
Consent to research
Only users who gave consent to utilization of their anonymized data for scientific research were included in the study (90% of new registrants consent). Consent was obtained separately to the questionnaire presented when registering with Natural Cycles. It was requested through a consent form sent within the app a few days after registration. The user had the options to consent or decline and could modify her decision at any time within the application. Users could also demand the erasure of their data according to data privacy regulations.
Time to pregnancy
Data were obtained from users who started using the Natural Cycles app on Prevent mode, used it for at least two full cycles without becoming pregnant, and then switched to Plan mode for at least one fertile window. This was required to ensure that we could identify with reasonable accuracy when the user started trying to conceive and being exposed to the Plan mode, minimize the residual effect of hormonal contraception in those women that had previously discontinued its use, and enable our users to become reasonably familiar with the daily app routine. The median time spent by users on Prevent before starting their attempt to conceive was six cycles.
The date of switching to Plan mode, and beginning of the exposure, was taken as the first day of the first cycle of the pregnancy attempt. A cycle is considered as the first Plan cycle if the couple switched to the Plan mode within the first 4 days of the cycle. The 4-day period was justified by the average length of menstruation among Natural Cycles users, and by the fact that, when very limited BBT data are available, the algorithm conservatively indicated all days after the end of menstruation as potentially fertile, encouraging the user to have sexual intercourse to increase her chances to conceive. If the couple switched later, then the following cycle was considered as the first Plan cycle. This was necessary to ensure that the couple was indeed seeking pregnancy during the fertile window of this first cycle.
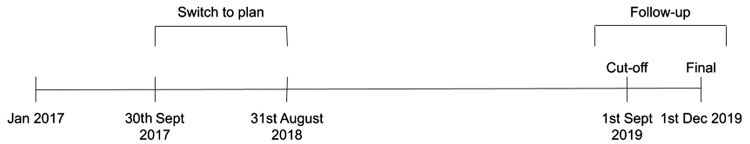
The switch to Plan had to happen between September 30, 2017 and August 31, 2018 to allow at least 12 months of potential usage up to the cutoff date of September 1, 2019. Version 3 of the Natural Cycles algorithm was released on September 1, 2017 so all users were using this version while on Plan. The date constraints were applied to ensure that all users included in the study were exposed to the same version of the app. Three months of follow-up time were given up to the study end date of December 1, 2019 so that users who were still active after the cutoff date could complete their final cycle and to give time to answer follow-up e-mails.
All users registered to use the app between January 2017 and December 31, 2017 (Fig. 1). To be included in this analysis users must have completed at least 20 daily data entries (not consecutively) in total during their Plan participation.
FIG. 1.
Study timeline (time axis not to scale).
Pregnancies are directly reported by the user either by entering a positive pregnancy test in a daily data entry, by answering a follow-up message (if they discontinued use of the app), or by switching to follow a pregnancy mode of the app, which gives an estimated date of delivery and week-by-week status updates. Pregnancies can also be indirectly identified based on patterns in user data, that is, continued high temperature data following a detected ovulation.9
Two censoring events were defined. First, women who stopped actively logging data in the app were censored on the last day of the menstrual cycle on which their last data entry occurred, estimated based on their average cycle length. Second, if a woman switched back to Prevent mode, she was censored on the last day of the previous cycle. All users who discontinued active usage were sent a follow-up e-mail message to determine their pregnancy status before dropout. Two hundred seventy-three women were contacted by the follow-up e-mail, 102 women did not respond, 152 communicated that they had not achieved pregnancy, and 19 answered that they had indeed become pregnant while actively using the application. Their pregnancies were counted on their last active cycle. If a woman was not reached or did not respond, all her cycles on Plan were taken into account, including the censoring cycle.
Users who switched back to Prevent before the end of the first Plan cycle were excluded entirely from the study, regardless of whether they became pregnant.
The definitions of beginning and end of the pregnancy attempt given above were an attempt to establish the woman's intention toward planning or preventing a pregnancy as transparently and consistently as possible. The NC app offers different features and content to users on Prevent and Plan mode, and it is technically straightforward to switch between the two modes. It is therefore very common for women on Prevent who have the intention to start planning a pregnancy in the near future to change modes multiple times to access the content and explore the features available to Plan users. It is not common for a woman who is actively trying to get pregnant to switch back to Prevent mode to access the contraception content. Any switch back to Prevent is a good indicator of the intention to end the attempt to conceive. As it was not possible to directly inquire the woman about her intention at the beginning of each cycle, it had to be inferred from her activity in the app.
TTP was measured in terms of complete cycles. The total exposure to the Plan mode was calculated by counting all cycles from the first cycle on Plan until the conception cycle or the censoring cycle included, according to the definitions given above.
Data analysis
We report the 6- and 12-cycle cumulative pregnancy probabilities by the Kaplan–Meier method10 with 95% confidence intervals (CIs) by the Kalbfleisch and Prentice method.11
A discrete-time proportional odds regression is used to estimate the associations between a number of physiological and behavioral predictors and TTP.
Physiological characteristics examined were as follows: age at the beginning of the exposure to Plan mode (18–29, 30–34, 35–45), BMI (<18.5, 18.5–25, 25–30, >30), cycle regularity (cycle length standard deviation <5, ≥5 days) and average cycle length (within or without the normal 21–35 day range),12 and previous pregnancies (binary: 0 if none, 1 if the user had been pregnant before her registration). Averages and standard deviations of the cycle length were calculated over all cycles, regardless of whether they were Prevent or Plan cycles, to have a more reliable estimate. It has been observed in other studies that the age-related decline in fecundability is confounded by parity, that is, the number of previous pregnancies carried to delivery after 24 gestational weeks (Paul, 2016). As this information is not gathered through the app, gravidity, that is, the number of previous pregnancies regardless of their outcome, is used as a proxy and included as a confounder in the model. The question, “have you been pregnant before,” was asked to users through an in-app message. The answer did not define whether the pregnancy had continued past 24 gestational weeks and, therefore, parity could not be assumed, simply gravidity.
Behavioral factors while trying to conceive were also included: frequency of BBT logging during the exposure to Plan mode (0%–50%, 50%–70%, 70%–100% of days) and frequency of logging sexual intercourse (0%, 0.1%–10%, 10%–20%, 20%–100% of days where sexual intercourse took place and was logged, regardless of when with respect to the fertile window). A frequency of 70% and higher in logging temperature data corresponds to recommended use, that is, entering temperatures on 5 out of every 7 days on average throughout the cycle. The information of whether sexual intercourse had taken place or not on a given day is instead not required for the NC algorithm to assess the woman's fertility. Therefore, intercourse logging is considered optional, and no specific recommendation is given. Missing intercourse data constitute a limitation of this study.
Both temperature and intercourse logging frequency were considered as a measure of how dedicated the user is to using the app correctly. By including the temperature logging frequency, the intercourse tracking frequency is decoupled from how dedicated a user is to entering data. The main parameters used in fertility status calculations vary depending on what data the user logs, how frequently and when. The algorithm will respond to the data entered by giving weight to that data. LH testing results are incorporated into algorithm calculations to help predict ovulation.
After removing users who were missing data in any of the exposures there were 4,500 women included in the regression.
Satisfaction of the proportional odds assumption is verified for the above choices. Adjustment for educational level was not necessary as there was no significant effect on fecundability.
The effect of the selected predictors on the TTP is estimated in terms of fecundability odds ratio (FOR), that is, the odds of getting pregnant each cycle for a given exposure, conditional on not being pregnant in the previous cycle, relative to a baseline. The baseline cohort was defined as ages 18–29, BMI 18.5–25, cycle length standard deviation <5, average cycle length 21–35 days, no previous pregnancy, sexual intercourse logged on 0% of days (logging intercourse is not mandatory so although 0% was a criterion, it does not mean that intercourse was not taking place), and temperature logging frequency below 50%.
Data availability
The data that support the findings of this study are available from Natural Cycles USA Corp. but restrictions apply to the availability of these data, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Natural Cycles USA Corp.
Code availability
The code that constitutes the Natural Cycles mobile application (including the ovulation detection algorithm) is proprietary and not available for release. The code used to analyze the data was developed in-house and also incorporates the publicly available Lifelines Python package for survival analysis (https://lifelines.readthedocs.io/en/latest/). It may be made available upon reasonable request to the corresponding author and with permission of Natural Cycles USA Corp.
Ethical statement
The study protocol was reviewed and approved by the regional ethics committee (EPN, Stockholm, Serial No. 2016/2037-31; 2019-02377).
Results
Study population
Five thousand three hundred seventy-six women were included in the study with an average age at registration on Natural Cycles of 31.8 ± 4.0 years and BMI of 23.3 ± 5.2 kg/m2 (Table 1).
Table 1.
Study Population Description
| Characteristic | Percentage of cohort | Number of women |
|---|---|---|
| Age, years | ||
| 18–29 | 29.2 | 1,570 |
| 30–34 | 46.3 | 2,490 |
| 35–45 | 24.5 | 1,316 |
| BMI, kg/m2 | ||
| <18.5 | 3.3 | 177 |
| 18.5–24.9 | 68.9 | 3,644 |
| 25–29.9 | 19 | 1,005 |
| 30–34.9 | 6.3 | 333 |
| >35 | 2.4 | 128 |
| Maximum educational level | ||
| Primary school | 0.8 | 36 |
| Secondary school | 10.4 | 450 |
| University degree | 68.8 | 2,971 |
| Trade/technical/vocational training | 9.0 | 388 |
| PhD | 11.0 | 473 |
| Average cycle length, days | ||
| 21–35 | 88.0 | 4,713 |
| <21 or >35 | 12.0 | 641 |
| Cycle length variability, standard deviation, days | ||
| <5 | 79.0 | 4,232 |
| ≥5 | 21.0 | 1,122 |
| Temperature logging frequency, % of days | ||
| 0–50 | 48.5 | 2,605 |
| 50–70 | 16.6 | 892 |
| 70–100 | 34.9 | 1,875 |
| Sex logging frequency, % of days | ||
| 0 | 18.1 | 973 |
| 0.1–10 | 37 | 1,989 |
| 10–20 | 27.4 | 1,471 |
| 20–100 | 17.5 | 943 |
| Gravidity 1 or higher, % | 27.8 | 1,255 |
Not all questions were mandatory and therefore response rate varied.
BMI, body mass index.
Pregnancy probability and time to pregnancy
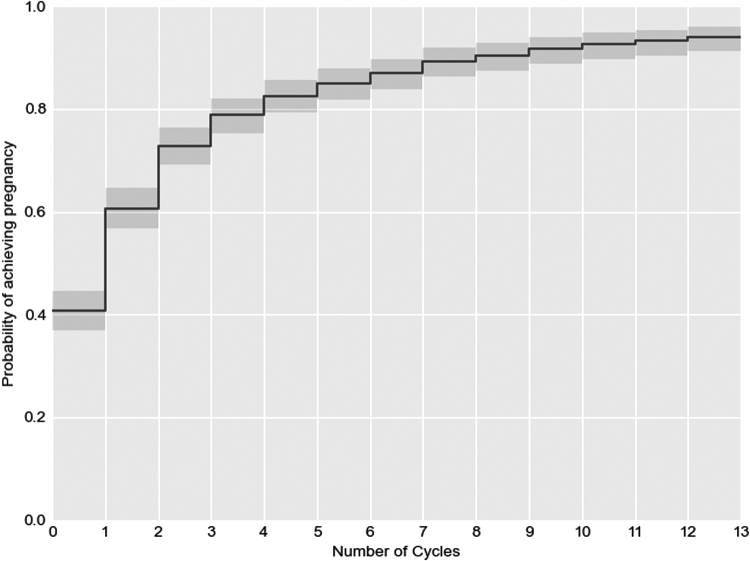
Of the women, 30.5% (1,640/5,376) dropped out, of which 24.5% (403/1,640) switched back to Prevent mode. From 3,736 remaining women, 84.7% (3,166/3,736) women achieved pregnancy within 13 cycles, while 15.3% (570/3,736) women were still trying to get pregnant at the end of the observation period. Figure 2 shows the Kaplan–Meier nonpregnancy probability over 13 cycles with 95% CI. These were found to be 61% (95% CI: 59–62) and 74% (95% CI: 73–76) for 6 and 12 cycles, respectively. The median TTP was 4 cycles, determined as the 50th percentile of the Kaplan–Meier curve.
FIG. 2.
Kaplan–Meier nonpregnancy probability of the entire study population with 95% CI. CI, confidence interval.
Both physiological and behavioral characteristics were found to affect the pregnancy probability. Figure 3 shows the Kaplan–Meier for users with higher fecundability (age less than 35 and with cycle length variation <5 days) which represented 58% (n = 3,096) of study participants. If the additional behavioral condition of logging sexual intercourse on at least 20% of days is added (11.5% [n = 613] of entire sample), this group achieves a 6-cycle and 12-cycle cumulative pregnancy probability of 88% (95% CI: 85–91) and 96% (95% CI: 94–97) and a median TTP of 2 cycles.
FIG. 3.
Kaplan–Meier probability of pregnancy per cycle of optimal cohort (age <35, cycle length variation <5 days, logged intercourse on at least 20% of cycle days) with 95% CI.
The worst performing group of users (>35 years, irregular cycles) consisted of 3.3% (n = 179) of the total sample. Analysis of this group was attempted however; due to the range of results and low sample size, nothing could be concluded.
The impact of age and cycle irregularity was also evaluated separately. Women of age >35 years achieve a 6 cycle and 12 cycle cumulative pregnancy probability of 54% (95% CI: 51–57) and 75% (95% CI: 73–78), respectively, while women with irregular cycles achieve a 6 cycle and 12 cycle cumulative pregnancy probability of 58% (95% CI: 55–62) and 79% (95% CI: 76–82).
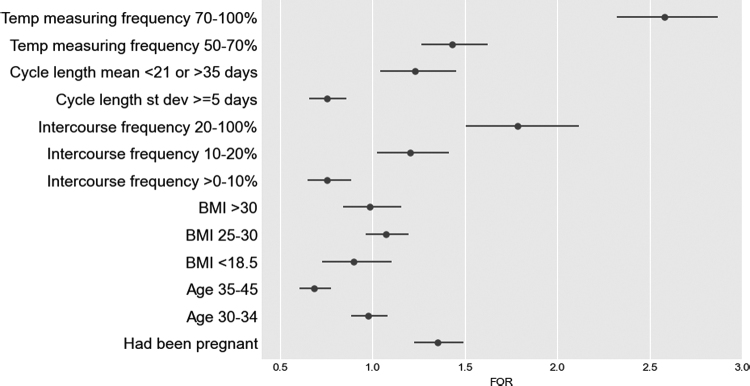
Fecundability odds ratios
Figure 4 shows the 95% CI relative to the baseline (dotted line) (for data see Table 2). Age over 35 years, BMI in the underweight range, irregular cycles, and sporadic sexual activity are related with FOR <1, indicating worse fecundability (Fig. 4 and Table 2).
FIG. 4.
FOR with 95% CI corresponding to the selected set of exposures, from a single discrete-time fecundability model. For the relative percentages in each cohort please refer to Table 1. Older age, BMI in the underweight range, irregular cycles, and sporadic sexual activity are related with FOR <1, indicating worse fecundability. BMI, body mass index; FOR, fecundability odds ratio.
Table 2.
Fecundability Odds Ratio for Different User Characteristics from a Single Discrete-Time Fecundability Model Fit to the Data
| Characteristic | Value | FOR (95% CI) |
|---|---|---|
| Intercourse frequency | 20–100% | 1.78 (1.50–2.12) |
| 10–20% | 1.20 (1.03–1.41) | |
| >0–10% | 0.76 (0.65–0.88) | |
| Not logging | 1.0 | |
| BMI | >30 | 0.98 (0.84–1.15) |
| 25–30 | 1.07 (0.96–1.20) | |
| 18.5–25 | 1.0 | |
| <18.5 | 0.90 (0.73–1.10) | |
| Age | 35–45 | 0.68 (0.60–0.77) |
| 30–34 | 0.98 (0.88–1.08) | |
| 18–29 | 1.0 | |
| Cycle length mean | <21 or >35 days | 1.23 (1.04–1.45) |
| 21–35 days | 1.0 | |
| Cycle length standard deviation | ≥5 days | 0.75 (0.66–0.86) |
| <5 days | 1.0 | |
| Previous pregnancies | Yes | 1.35 (1.23–1.49) |
| No | 1.0 | |
| BBT logging frequency | 70%–100% | 2.58 (2.32–2.87) |
| 50%–70% | 1.43 (1.26–1.62) | |
| <50% | 1.0 |
BBT, basal body temperature; CI, confidence interval; FOR, fecundability odds ratio.
Discussion
Our observational study on 5,376 women using the Natural Cycles mobile app to plan a pregnancy overall found a 6-cycle pregnancy probability of 61% (95% CI: 59–62) and a 12-cycle pregnancy probability of 74% (95% CI: 73–76). The population of users with no known characteristics of subfertility (i.e., under the age of 35 and with cycle length variation <5 days) represented 58% of the study participants, which is lower than what would be expected in the general population.1 If this group logged sex on at least 20% of cycle days (11.5% of entire cohort [n = 613]), excellent conception outcomes were achieved with 12 cycles and 6 cycles of cumulative pregnancy probability of 88% (95% CI: 85–91) and 96% (95% CI: 94–97) and a median TTP of 2 cycles.
A similar study investigating the pregnancy rate in a cohort of women (aged 20–43, mean age 29.2) using fertility awareness (using either electronic hormonal fertility monitoring or cervical mucus monitoring or both) found a 12 cycle rate of 83%,13 which is slightly higher but comparable to results in our study. The pregnancy rate after 12 months has been reported to be higher in other studies (∼80%) when individuals were counseled to have intercourse on the predicted day of ovulation.14 Sample size was 200 in the Zinaman et al. study, a fraction of the number of women included in our analysis. Another previous study also reported 12 month pregnancy rates of ∼80% from questionnaire data however; data were gathered retrospectively among pregnant women, excluding infertile couples, which could explain the difference between these results.15,16 Gnoth et al.17 investigated the TTP in women using Natural Family Planning methods in a cohort of 300 women (aged 20–44, mean age 29). The estimated cumulative probabilities of conception in this group were 81% at 6 months and 92% at 12 months for the entire cohort.
The median TTP of four cycles was slightly higher compared to a Dutch population based study, which reported a median TTP of 3 months.18
In this study women used the Natural Cycles app to support conception through tracking of BBT and identifying the fertile window. Successful identification of fertile days was possible due to tracking of physiological parameters beyond just menstruation together with automated analysis of these data using a highly sophisticated mathematical algorithm housed within the application. Tracking of multiple physiological parameters is necessary for identification and prediction of fertile days because there is significant variation in follicular phase, luteal phase lengths, and ovulation day across the general population.19 In these real-world studies less than 20% of women had cycles of 28 days in length, and there was significant intraindividual variation in menstrual cycle parameters. In our study of over 600,000 menstrual cycles, we found that only 65% of women had cycle lengths of 25–30 days and the mean day of ovulation varied from 10.4 to 26.8 over all women.4 In this study we observed that high cycle length variation (standard deviation of 5 days or more) was associated with lower fecundability. Cycle length variation cannot be accounted for with calendar-based apps, and this leads to poor quality of fertile window prediction.20
Only women who had used the app and logged data for at least two cycles on the Prevent mode before starting the attempt to conceive were included in this study. Although these two cycles were not included in the TTP estimate, these additional data are important for individualization of the prediction of the fertile period and, therefore, to maximize speed of conception. Temperature measuring frequency also had a significant effect on FOR suggesting that those users that logged more temperatures within the app achieved a pregnancy faster. This makes sense given that the more data the algorithm has regarding an individual's cycle, the more accurately it can predict ovulation and increase the chance of conception. Therefore, this information could be used to further motivate women using FABMs to regularly log data to increase their chances of conception. Increased logging of intercourse also improved FOR as expected; however, intercourse logging was not mandatory for users of the application.
Women using an FABM without an app may naturally find the calculations and process more labor intensive and thus time consuming and stressful. The benefits of using an app to support conception go beyond identification of the fertile days and the use of the algorithm to learn about an individual woman's cycle. In a recent qualitative study of 24 couples using the app to support conception the app was found to have impacted on a number of different areas of everyday life.21 Many women felt greater autonomy and responsibility for the process of conception and found that the app helped to facilitate conversations around fertility with partners and health care professionals. Users felt that the app became a trusted part of the conception process and was valuable in helping women to learn about their body. The importance of commitment to the method was highlighted, and many users found that morning BBT measurement became habitual. Many found that the app offered reassurance; however, there should be caution as use of an app may lead to increased anxiety in some women due to regular reminders about the desire to conceive. Women who are considering using the app to support conception should balance the benefits of the method against the potential risks.
As an increasing number of women use apps and Femtech Technologies to support conception, there is tremendous potential to offer fertility related education and medical support through these platforms. Preconception advice is often difficult to access22; yet, behavioral modification to improve health and well-being can have a significant impact on pregnancy outcomes. Apps can be excellent platforms to provide preconception education on topics such as the menstrual cycle, female fertility decline, the fertile window, nutrition, smoking cessation, environmental health, subfertility, and sexually transmitted infections. There is the potential to extend the functionality of the platform to offer online medical services to address serious challenges such as mental health problems, substance misuse, and interpersonal violence both in the preconception and postdelivery periods. In the future it is likely that intelligent algorithms will be used to analyze data input by the user to identify women who may be at risk of subfertility or other related medical conditions.
Conclusions
The Natural Cycles app can be used by women to support conception by providing an easy to use individualized daily fertility status. The study population was predominantly women with at least one feature of subfertility, suggesting that Natural Cycles was being used to support women who may be experiencing difficulty conceiving. Women who conceive naturally without the use of Natural Cycles are therefore underrepresented in this dataset. Median TTP is two cycles for the majority of sexually active women without features of subfertility (age <35, cycle length variation <5 days); however, this group made up 11.5% of the entire cohort. In this minority group, TTP compares favorably to published TTP figures without the app. Eighty-eight percent of these women successfully achieve pregnancy within 6 months. Fertility awareness apps have an important role in educating women and their partners about fertility and facilitating discussions around the topic. In the future smart algorithms may facilitate early identification of couples who may benefit from infertility assessment.
Limitations
Users of the app in this study had a higher educational level and lower BMI than would be expected in the general population. Close to 50% had characteristics associated with subfertility such as age >35 years, highly variable cycle length, or anovulatory cycles.
We chose to consider the cycle in which the woman changed to the Plan mode as part of the exposure only if the switch was performed within the first 4 days of this cycle. On one hand, this choice was considered to be the most reasonable for this study. It limited in fact the difficulties of assessing the intention in cases where the switch took place in the fertile window, and it is applicable to all NC users regardless of the quality of their data. On the other hand, it might shorten the estimate of the TTP for those women who, despite having started the pregnancy attempt, have switched later in the cycle.
Logging of sexual intercourse is encouraged but not strictly recommended, as the quality of intercourse data has no impact on the app's functioning. The average fraction of days in which intercourse took place and was logged was found to be around 11%, while about 18% of the women never logged intercourse in the whole pregnancy attempt. It is therefore quite likely that sexual intercourse was underreported in this study.
The dropout rates from this study were relatively high, with many users switching back to Prevent mode. We followed up with discontinuing users to find out if they had become pregnant, but it is possible that some pregnancies were not captured in this study.
Acknowledgments
Jonathan Bull and Federiko Barabas are thanked for their contributions to the design of this study and supervision of the data analysis. The corresponding author had full access to the data in this study and had final responsibility for the decision to submit for publication.
Authors' Contributions
C.F., J.T.P., and S.P.R. contributed to the study design, data interpretation, and article preparation. C.F. and A.M.J. contributed to the study design, data analysis, and interpretation. E.B.S. and R.S. contributed to the study design, data acquisition, and final approval. K.G.D. contributed to study design and article review. J.H. contributed to the study design, data interpretation, article preparation, and final approval.
Author Disclosure Statement
J.R.B., F.B., S.P.R., J.T.P., C.F., and M.C. are full time employees of Natural Cycles USA Corp. with shares in the company. E.B.S. and R.S. are the founders of Natural Cycles USA Corp. with shares in the company. J.C.H. has previously received honorarium for Natural Cycles presentations and media activities and is founder of the web based forum www.globalwomenconnected.com
Funding Information
The study was funded by Natural Cycles USA Corp. This research was also supported, in part, by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences under project number Z01ES103333.
References
- 1. Borght MV, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem 2018;62:2–10. [DOI] [PubMed] [Google Scholar]
- 2. Weinberg CR, Wilcox AJ. A model for estimating the potency and survival of human gametes in vivo. Biometrics 1995;51:405–412. [PubMed] [Google Scholar]
- 3. Dunson DB, Baird DD, Wilcox AJ, et al. Day specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod 1999;14:1839. [DOI] [PubMed] [Google Scholar]
- 4. Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med 2019;2:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ali R, Gürtin ZB, Harper JC. Do fertility tracking applications offer women useful information about their fertile window?. Reprodctive Biomed Online 2021;42:273–281. [DOI] [PubMed] [Google Scholar]
- 6. Kleinschmidt TK, Bull JR, Lavorini V, et al. Advantages of determining the fertile window with the individualised Natural Cycles algorithm over calendar-based methods. Eur J Contracept Reprod Health Care 2019;24:457–463. [DOI] [PubMed] [Google Scholar]
- 7. Berglund Scherwitzl E, Lindén Hirschberg A, Scherwitzl R. Identification and prediction of the fertile window using NaturalCycles. Eur J Contracept Reprod Health Care 2015;20:403–408. [DOI] [PubMed] [Google Scholar]
- 8. Scherwitzl EB, Lundberg O, Kopp Kallner H, et al. Short- and long-term effect of contraceptive methods on fecundity. Eur J Contracept Reprod Health Care 2019;24:260–265, . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buxton CL, Atkinson WB. Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. J Clin Endocrinol Metab 1948;8:585. [PubMed] [Google Scholar]
- 10. Bland JM, Altman DG. Statistics notes: Bayesians and frequentists. BMJ 1998;317:1151–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. In: Wiley Series in Probability and Statistics, New York, NY: Wiley, 2002. [Google Scholar]
- 12. Reed BG, Carr BR. The normal menstrual cycle and the control of ovulation. In:, Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext. SouthDartmouth, MA: MDText.com, Inc., 2018. [Google Scholar]
- 13. Bouchard TP, Fehring RJ, Schneider MM. Achieving pregnancy using primary care interventions to identify the fertile window. Front Med 2018;4:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zinaman MJ, Clegg ED, Brown CC, O'Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril 1996;65:503–509. [PubMed] [Google Scholar]
- 15. Juul S, Karmaus W, Olsen J. Regional differences in waiting time to pregnancy: Pregnancy-based surveys from Denmark, France, Germany, Italy and Sweden. The European Infertility and Subfecundity Study Group. Hum Reprod 1999;14:1250–1254. [DOI] [PubMed] [Google Scholar]
- 16. Jensen TK, Slama R, Ducot B, et al. Regional differences in waiting time to pregnancy among fertile couples from four European cities. Hum Reprod 2001;16;2697–2704. [DOI] [PubMed] [Google Scholar]
- 17. Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freund G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod 2003;18:1959–1966. [DOI] [PubMed] [Google Scholar]
- 18. Mutsaerts MAQ, Groen H, Huiting HG, et al. The influence of maternal and paternal factors on time to pregnancy—A Dutch population-based birth-cohort study: The GECKO Drenthe study. Hum Reprod 2012;27:583–593. [DOI] [PubMed] [Google Scholar]
- 19. Johnson S, Marriott L, Zinaman M. Can apps and calendar methods predict ovulation with accuracy?. Curr Med Res Opin 2018;34:1587–1594. [DOI] [PubMed] [Google Scholar]
- 20. Freis A, Freundl-Schütt T, Wallwiener L-M, et al. Plausibility of menstrual cycle apps claiming to support conception. Front Public Health 2018;6:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grenfell P, Tilouche N, Shawe J, French RS. Fertility and digital technology: Narratives of using smartphone app ‘Natural Cycles' while trying to conceive. Sociol Health Illn 2021;43:116–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tuomainen H, Cross-Bardell L, Bhoday M, Qureshi N, Kai J. Opportunities and challenges for enhancing preconception health in primary care: Qualitative study with women from ethnically diverse communities. BMJ Open 2013;3:e002977. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from Natural Cycles USA Corp. but restrictions apply to the availability of these data, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Natural Cycles USA Corp.