Abstract
The objective was to clarify occurrence, phenomenology, and risk factors for novel psychiatric disorder (NPD) in the first 3 months after mild traumatic brain injury (mTBI) and orthopedic injury (OI). Children aged 8-15 years with mTBI (n = 220) and with OI but no TBI (n = 110) from consecutive admissions to an emergency department were followed prospectively at baseline and 3 months post-injury with semi-structured psychiatric interviews to document the number of NPDs that developed in each participant. Pre-injury child variables (adaptive, cognitive, and academic function, and psychiatric disorder), pre-injury family variables (socioeconomic status, family psychiatric history, and family function), and injury severity were assessed and analyzed as potential confounders and predictors of NPD. NPD occurred at a significantly higher frequency in children with mTBI versus OI in analyses unadjusted (mean ratio [MR] 3.647, 95% confidence interval [CI95] (1.264, 15.405), p = 0.014) and adjusted (MR = 3.724, CI95 (1.264, 15.945), p = 0.015) for potential confounders. In multi-predictor analyses, the factors besides mTBI that were significantly associated with higher NPD frequency after adjustment for each other were pre-injury lifetime psychiatric disorder [MR = 2.284, CI95 (1.026, 5.305), p = 0.043]; high versus low family psychiatric history [MR = 2.748, CI95 (1.201, 6.839), p = 0.016], and worse socio-economic status [MR = 0.618 per additional unit, CI95 (0.383, 0.973), p = 0.037]. These findings demonstrate that mild injury to the brain compared with an OI had a significantly greater deleterious effect on psychiatric outcome in the first 3 months post-injury. This effect was present even after accounting for specific child and family variables, which were themselves independently related to the adverse psychiatric outcome.
Keywords: mild traumatic brain injury, pediatrics, prospective longitudinal controlled study, psychiatric disorders
Introduction
Mild traumatic brain injury (TBI) is a major public health problem in the United States.1 While it is established that children with severe TBI are at high risk for post-injury new-onset psychiatric disorder, termed novel psychiatric disorder (NPD),2–6 studies of children with mild TBI (mTBI) are plagued with methodological problems resulting in conflicting findings and fueling controversy. There is not a single psychiatric interview study of pediatric mTBI that is free of problems related to definition of mTBI, control group selection, outcome measurements, lack of longitudinal design, selection bias, sample size, or assessment of injury and psychosocial risk factors.7
The importance of this research is highlighted by findings of two large prospective studies of mTBI.8,9 The first involved a birth cohort,9 and the second involved surveillance of computerized medical information of children consecutively treated for mTBI.8 Both studies showed that children with mTBI had significantly more new-onset behavioral symptoms than controls. The major weaknesses of these studies include that the psychiatric outcome measure was not generated from standardized psychiatric interviews and there was an absence of injured control groups.10,11 Nevertheless, the results challenge authoritative reviews of relatively benign behavioral outcomes of mTBI in well-designed studies.12,13 The present study aims to clarify the controversy regarding behavioral outcomes in pediatric mTBI with a comprehensive psychiatric investigation to overcome the methodological problems of previous studies.
Our study is modeled after the study led by Yeates14–17 that focused on post-concussion symptoms (PCS) rather than the broader spectrum of psychiatric disorders. “Post-concussional disorder” was significantly higher in the mTBI versus the orthopedic injury (OI) control group 2 weeks after injury (51% vs. 30%), but not thereafter in the first year post-injury (19-27% versus 19-21%).18 Fay and colleagues found that mTBI was more likely to result in PCS relative to OI, among children of lower compared with higher cognitive ability.15
The literature regarding pre-injury child and family variables predictive of NPD in the context of mTBI is limited to studies of consecutively hospitalized children (i.e., samples of children who were more seriously injured than the current cohort). In these studies, NPD was associated with pre-injury lifetime psychiatric disorder in children with mild to moderate TBI.2,19,20 Other pre-injury predictors of NPD that followed mTBI included lower socioeconomic status, psychosocial adversity, adaptive function, estimated pre-injury academic function, and estimated pre-injury reading.21-23
The major objective of this study was to clarify the occurrence, phenomenology, and risk factors for NPD in the first 3 months after mTBI. The use of an OI group controlled for factors that predispose children to accidents, as well as control for the psychological trauma associated with an injury and its treatments. Our first hypothesis was that NPD in children will occur with significantly higher frequency in children with mTBI versus comparable OI controls. The second hypothesis was that frequency of NPD in children will be predicted by child variables (lower pre-injury child adaptive function, lower pre-injury cognitive function, lower pre-injury academic function, and presence of pre-injury lifetime psychiatric disorders), and pre-injury family variables (lower socio-economic status, lower pre-injury family function, more intense family psychiatric history) in children with mTBI and OI.
Methods
The study was approved by institutional review boards at all participating institutions. Written informed consent was obtained from parents, and youth provided written consent or assent depending on their age. The study used a prospective longitudinal design. We enrolled 220 children aged 8-15 years consecutively seen at an emergency department (ED) for mTBI and 110 children with mild orthopedic injury (OI) from consecutively treated patients seen at the same ED matched at the group-level by age and sex.
To ensure that children with “a bump on the head” but with no brain trauma were excluded, the mTBI group included children only if they suffered a closed-head injury that resulted in an observed loss of consciousness, a Glasgow Coma Scale (GCS)24 score of 13 or 14, or at least two symptoms of concussion as noted by the ED medical staff (i.e., persistent post-traumatic amnesia, transient neurological deficits, vomiting, nausea, headache, diplopia, dizziness). Hospitalization did not automatically exclude participation. However, children with delayed neurological deterioration (e.g., GCS <13) were excluded. Children were excluded if their loss of consciousness was greater than 30 min or had a GCS score of less than 13. The GCS was obtained from a review of the electronic medical record.
Other exclusion criteria for the mTBI group included the following: 1) associated injury that is severe documented with the Abbreviated Injury Scale (AIS)25 score greater than 3; 2) associated injury that is likely to interfere with cognitive testing (e.g., injury to dominant upper limb); 3) hypoxia, hypotension, or shock associated with the injury; 4) alcohol, drug ingestion, or child abuse involved with the injury; 5) documented history of previous TBI meeting the above criteria for at least mTBI; 6) pre-injury neurological disorder, schizophrenia, autism spectrum disorder, or intellectual deficiency; 7) any medical contraindication to magnetic resonance imaging; 8) any injury requiring neurosurgical intervention; or 9) illegal immigrant status.
Inclusion criteria for children with OI were the presence of upper or lower limb fractures associated with AIS scores of 3 or less. Exclusion criteria included: 1) injury to the head or TBI; and 2) exclusion criteria 1-9 listed for the mTBI group.
The children's pre-injury function was assessed at baseline (mean = 17.7 ± standard deviation [SD] = 5.8 days) and post-injury outcome was assessed at 3 months (mean = 103.1 days ± SD = 16.9) post-injury.
Assessment of pre-injury child function
Lifetime pre-injury psychiatric status
Lifetime pre-injury psychiatric disorder was measured with the Schedule for Affective Disorders and Schizophrenia for School Aged Children: Present and Lifetime Version (K-SADS-PL) interview.26 The KSADS-PL has high inter-rater reliability and validity.26 The Neuropsychiatric Rating Schedule (NPRS)27 interview was administered to detect the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) diagnosis, Personality change due to TBI.28 The NPRS reliably and validly identifies symptoms and subtypes of personality change due to TBI.6
The Teacher's Report Form (TRF)29 was used to aid the psychiatric interviewer to reach a “best-estimate” diagnosis.30 The interviewers discussed their diagnostic impressions by presenting every case to the first author, a board-certified child and adolescent psychiatrist, who was blind to group affiliation.
Pre-injury adaptive behavior function
The adaptive behavior composite was assessed using the Vineland Adaptive Behavior Scales (Vineland II) interview with the parent.31
Pre-injury intellectual and academic function
The Wechsler Abbreviated Scale of Intelligence (WASI-II)32 Vocabulary and Matrix Reasoning subtests were administered at baseline to obtain an estimate of pre-injury Full Scale IQ standard score. The Wide Range Achievement Test-Fourth Edition (WRAT-4)33 which assesses sentence comprehension, word recognition, spelling, and calculation skills, was administered at baseline. Standard scores of sentence comprehension and calculation skills were used in the analyses. Previous research has indicated that these measures of “crystalized ability” are relatively insensitive to the effects of mTBI when measured shortly after the injury.16,34
Assessment of pre-injury family status
Family function
The McMaster Structured Interview of Family Functioning (McSIFF)35 was conducted by trained research assistants with family household members at baseline to retrospectively assess pre-injury family function. The interview is a tool used to derive scores on a rating scale termed the Clinical Rating Scale (CRS).35 Using the McSIFF, pre-injury family function is a consistent predictor of novel psychiatric disorder after TBI.2 The global CRS score has been shown to be a valid and reliable method of family assessment.35,36 The General Functioning Scale of the McMaster Family Assessment Device (FAD),37 which was completed by the primary caretaker of the injured child at baseline, is a reliable and valid 12-item rating scale that provides an overall measure of pre-injury family functioning38 that was used in the analyses
Family psychiatric history
The Family History Research Diagnostic Criteria39 modified to DSM-IV Text Revision criteria is a semi-structured interview with the parent that screens for specific psychiatric diagnoses in first-degree family members. The analyses used the overall family psychiatric history ratings, which are summarized on a 4-point scale: 0 = no psychiatric disorder; 1 = at least one family member met criteria for a psychiatric disorder but no treatment was received; 2 = a family member met criteria for a psychiatric disorder and received outpatient treatment or was arrested for antisocial behavior; 3 = a family member met criteria for a psychiatric disorder and had inpatient psychiatric treatment or was incarcerated.2 Participants were categorized as having either low (scores of 0-1) or high (scores of 2-3) intensity family psychiatric history for the analyses
Socioeconomic status
Socioeconomic status (SES), expressed as a z-score, was assessed using a composite of maternal education and median income for the census tract of the family's residence. The composite was calculated by averaging the sample z-scores of the two variables. This composite score functions well as a measure of SES in TBI studies.40
Assessment of injury severity
The Injury Severity Score (ISS) from the Abbreviated Injury Scale (AIS) was recorded from electronic medical record data.25 The ISS is the sum of the squares of the highest AIS code in each of the three most severely injured ISS body regions.
Post-injury psychiatric outcome
The K-SADS-PL, NPRS, and TRF were repeated at 3 months. The interviewer generated “best-estimate” clinically significant psychiatric diagnoses by integrating the information from these instruments.30 As in previous work,2,5 an NPD diagnosis was given in two circumstances: First, this could occur in a participant with no pre-injury lifetime psychiatric disorder who then develops a psychiatric disorder. Second, this could occur in a participant with a pre-injury lifetime psychiatric disorder who develops a different psychiatric disorder (e.g., a participant with a pre-injury lifetime history of major depression who develops attention-deficit/hyperactivity disorder [ADHD] following the injury would receive the classification but would not if only a new episode of major depression occurred). Duration criteria for psychiatric disorders except for major depression and bipolar disorder were waived to examine the phenomenology of emerging post-injury disorders. Similarly, as in our previous work, the age of onset criterion for ADHD was waived to study the phenomenology of this particular NPD.2
The interviewers made every attempt to remain blind to group membership (mTBI vs. OI control), although at baseline, this was often impossible because of physical stigmata of TBI and OI. However, the baseline psychiatric assessment deals only with pre-injury psychiatric status and was not the outcome of interest. Therefore, the study design insured that the interviewer who conducted the baseline assessment for a particular participant did not conduct post-injury psychiatric assessments for that individual. This left the psychiatric interviewer who conducted the 3-month blind to injury group. The interviewers presented every case to the first author who was blind to group affiliation.
Inter-rater reliability for psychiatric diagnoses was conducted based on 12 video-recorded interviews (Supplementary Material). All research participants and their guardians were asked to consent for video recording of the psychiatric interview process. The “best-estimate” current and past ratings involved integration by the clinician of the parent's and child's video-recorded interview, teacher's input when available, and clinical judgment of the parent's and child's reliability and mental status. Agreement with respect to psychiatric diagnosis was perfect in 10/12 (83%) cases encompassing agreement for all specific current as well as past diagnoses or absence of a diagnosis in a participant. We conducted a Kappa analysis of inter-rater reliability for these categorical diagnoses. There was agreement between raters in 26/29 specific diagnostic data points and disagreement in 3/29 yielding a Kappa = 0.80 indicating substantial agreement.
Statistical analysis
The eligible patients with mTBI who presented to the ED but who did not enroll in the study (n = 741) were compared with the patients with mTBI who did enroll (n = 220) with respect to sex using Pearson's chi-square test, and with respect to age and GCS score using independent sample t-tests. Fisher's exact test was used instead of Pearson's test when the expected counts were ≤5 in any of the crosstabulation cells. Similarly, we used Pearson's or Fisher's test for categorical variables and independent sample t-test for continuous variables in comparisons of the enrolled mTBI versus OI groups, the participating mTBI versus OI groups at 3 months, and also the entire participating cohort at 3 months versus the enrolled but non-participating cohort at 3 months with respect to age, sex, SES, race (White vs. Minority), ethnicity, pre-injury lifetime psychiatric disorder, pre-injury current disorder, pre-injury adaptive function, family psychiatric history, pre-injury family function, IQ, sentence comprehension, calculation skills, Injury Severity Score, cause of injury, and sports-related injury status.
To determine the effect of mTBI on NPD in the first 3 months post-injury (hypothesis 1), the NPD count (total number of diagnoses) for each child was recorded at the 3-month visit and was compared between the mTBI and OI groups using a Poisson log-linear regression model. The potential confounders included demographics: age, sex, race; pre-injury child function: lifetime pre-injury psychiatric disorder, Vineland Adaptive Behavior composite, WASI-II Full Scale IQ, WRAT-4 Sentence Comprehension and Calculation Skills; pre-injury family status: SES, family psychiatric history, family function (CRS and FAD); and injury status (Injury Severity Score). Among these potential confounders, those which were significant at p < 0.15 in single-predictor Poisson regression models were included in the starting multi-predictor Poisson regression and subject to backward model selection with a p < 0.15 threshold (adjusted analysis). The statistical tests and 95% confidence intervals (CI95) were based on the likelihood ratio test. Backward model selection with a lax threshold of 0.15-0.20 is recommended in regression models for determining causal effects in the presence of confounding.41 An overdispersion check was based on the ratio of the residual deviance to the residual degrees of freedom, which was ≤2 in all cases (no overdispersion). The effects of predictors are reported in terms of mean ratio of NPD counts between any two groups under comparison, adjusted for the other predictors in the model.
To determine a multi-predictor model for the NPD count at 3 months (hypothesis 2), we similarly fit a multi-predictor Poisson model, where predictors with p < 0.15 in single-predictor analyses were included in the starting model and the model was reduced using backward model selection with p < 0.15 threshold. This is similar to the analysis determining the effect of mTBI, except that here mTBI exposure was also subject to model selection.41
Results
Representativeness of enrolled mTBI participants
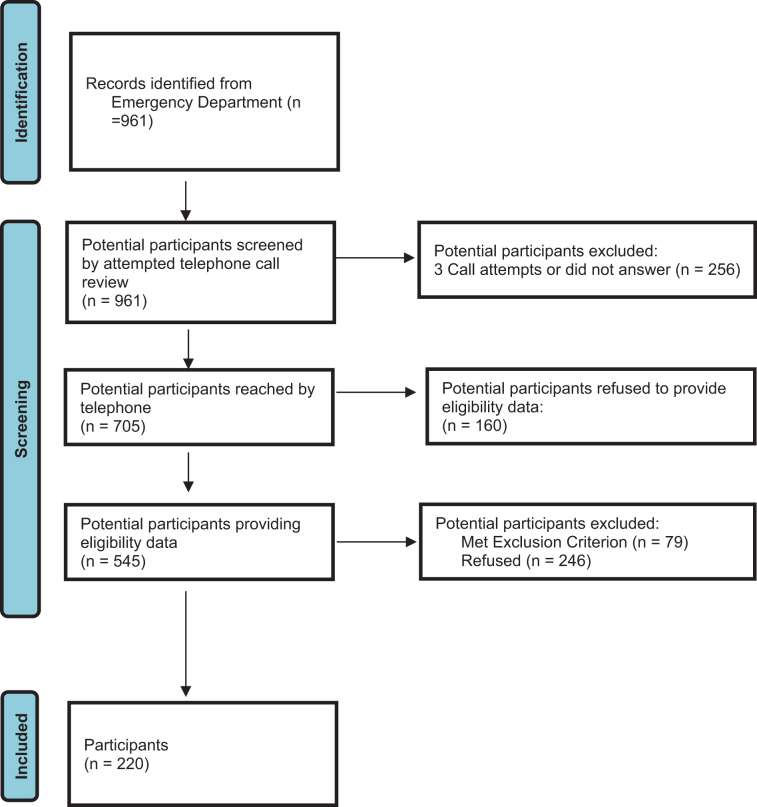
The enrolled cohort of children with mTBI (n = 220) was compared with the children with mTBI who did not enroll (n = 741; Fig. 1). The mean (SD) age of the enrolled group (12.3 ± 2.1 years) was significantly older than the non-enrolled group (11.7 ± 2.2 years; p = 0.0001). The enrolled mTBI and non-enrolled mTBI groups were not significantly different with respect to sex (145/220; 66.0% vs. 521/741; 70.3% males respectively; p = 0.21), nor with respect to injury severity measured by GCS scores (14.95 ± 0.21 vs. 14.97 ± 0.20 respectively; p = 0.44). The research design was to recruit an OI control group matched to the enrolled mTBI on age and sex, and not necessarily to be representative of the consecutive series of children with OI seen in the ED.
FIG. 1.
Identification of children with mild traumatic brain injury. Color image is available online.
Baseline characteristics
Table 1 shows that our efforts to match the OI group (n = 110) as a whole to the mTBI group (n = 220) by age and sex were successful. Further, there were no significant group differences in pre-injury child variables (ethnicity, adaptive function, lifetime and current psychiatric disorder, IQ, academic function) and pre-injury family variables (socioeconomic status, family psychiatric history, family function). Compared with the OI group, the mTBI group had a significantly lower percentage of White (65.0% vs. 79.1%) versus Minority (35.0% vs. 20.9%) race enrolled participants (Pearson's chi-squared test p = 0.011). The Injury Severity Score was significantly higher in the enrolled OI group versus the enrolled mTBI group (3.98 ± 1.00 vs. 2.70 ± 2.46 respectively; df = 328; p = 0.000). There was a significant difference in the cause of injury between the mTBI and OI enrolled groups (Fisher's exact test p = 0.000). Inspection of the data revealed that this was driven by falls accounting for 85% of OI cases versus 55% of mTBI cases, and more mTBI cases were injured by accidentally striking or being struck by an object, accidentally striking or being struck by a person, and having a transportation-related injury. The left half of Table 2 shows that the rates of specific pre-injury lifetime psychiatric disorders in the mTBI and OI groups were very similar. The rates of all the disorders are within the ranges of pediatric epidemiological studies except for a higher rate of ADHD. This exception is typical of populations of injured children.42 Teachers' input by means of the TRF was available for only 116/330 (35.2%) participants for reaching “best-estimate” psychiatric diagnoses at baseline.
Table 1.
Baseline Demographics, Psychiatric, Adaptive, Family, Intellectual, Academic Status, Injury Severity, and Cause of Injury
| |
Enrolled participants |
3-Month follow-up participants |
||
|---|---|---|---|---|
| Mild TBI (n = 220) | Orthopedic injury (n = 110) | Mild TBI (n = 189) | Orthopedic injury (n = 94) | |
| Age | 12.3 (2.1) | 12.2 (1.9) | 12.2 (2.15) | 12.2 (1.89) |
| Males (n; %) | 145 (65.9%) | 79 (71.8%) | 123 (65.1%) | 70 (74.5%) |
| Socioeconomic status | 0.063 (0.903) | -0.127 (1.164) | 0.062 (0.908) | -0.151 (1.21) |
| Race (n; %) | ||||
| White | 143 (65.0%)+ | 87 (79.1%)+ | 126 (66.7%) | 73 (77.7%) |
| Minority | 77 (35.0%)+ | 23 (20.9%)+ | 63 (33.3%) | 21 (22.3%) |
| Minority Composition | ||||
| African-American | 8 (3.6%) | 6 (5.5%) | 8 (4.2%) | 6 (6.4%) |
| Native American | 3 (1.4%) | 0 (0%) | 1 (0.5%) | 0 (0%) |
| Asian | 3 (1.4%) | 3 (2.7%) | 3 (1.6%) | 2 (2.1%) |
| Native Hawaiian or other Pacific Islander | 1 (0.5%) | 1 (0.9%) | 1 (0.5%) | 1 (1.1%) |
| More than 1 race | 49 (22.3%) | 7 (6.4%) | 39 (20.6%) | 6 (6.4%) |
| Other | 13 (5.9%) | 6 (5.5%) | 11 (5.8%) | 6 (6.4%) |
| Ethnicity | ||||
| Hispanic/Latino | 121 (55.0%) | 63 (57.3%) | 100 (52.9%) | 57 (60.6%) |
| Not Hispanic/Latino | 99 (45.0%) | 47 (42.7%) | 89 (47.1%) | 37 (39.4%) |
| Pre-injury lifetime psychiatric disorder (n; %) | 73 (33.2%) | 36 (32.7%) | 66 (34.9%) | 31 (33.0%) |
| Pre-injury current psychiatric disorder (n; %) | 57 (25.9%) | 30 (27.3%) | 50 (26.5%) | 25 (26.6%) |
| Pre-injury Vineland Adaptive Behavior Composite | 107.5 (13.0) | 104.8 (12.7) | 108.2 (13.0)* | 104.4 (12.5)* |
| Family Psychiatric History | 1.15 (1.20) n = 218 | 1.01 (1.19) n = 109 | 1.15 (1.20) n = 187 | 0.98 (1.18) n = 93 |
| McMaster Structured Interview of Family Function | 4.95 (1.16) n = 174 | 4.80 (1.16) n = 95 | 4.95 (1.17) n = 165 | 4.82 (1.18) n = 90 |
| Family Assessment Device (primary caretaker's report) | 1.63 (0.41) n = 217 | 1.68 (0.47) n = 109 | 1.62 (0.40) n = 187 | 1.69 (0.48) n = 93 |
| WASI-II Full-Scale IQ | 102.4 (14.7) n = 219 | 101.0 (12.5) n = 109 | 103.6 (14.8) n = 188 | 101.6 (12.8) n = 93 |
| WRAT-4 Sentence Comprehension | 106.1 (16.7) | 106.2 (16.4) n = 109 | 106.7 (17.1) | 106.2 (17.2) n = 93 |
| WRAT-4 Calculation Skills | 107.6 (15.9) | 107.1 (14.0) n = 109 | 107.8 (16.5) | 106.3 (14.4) n = 93 |
| Injury Severity Score | 2.70 (2.46)++ | 3.98 (1.00)++ | 2.62 (2.42)+++ | 3.93 (0.94)+++ |
| Cause of Injury (n; %) | ||||
| Fall | 120 (54.5%) | 93 (84.5%) | 105 (55.6%) | 82 (87.2%) |
| Struck (object) | 45 (20.5%) | 6 (5.5%) | 39 (20.6%) | 4 (4.3%) |
| Struck (person) | 41 (18.6%) | 9 (8.2%) | 33 (17.5%) | 6 (6.4%) |
| Transportation accident | 12 (5.5%) | 0 | 10 (5.3%) | 0 |
| Other | 2 (.9%) | 2 (1.8%) | 2 (1.1%) | 2 (2.1%) |
| Sports-related | 132 (60.0%) | 68 (61.8%) | 110 (58.2%) | 57 (60.6%) |
Values are expressed as means ± standard deviation unless otherwise specified.
Of all the group comparisons (mild TBI vs. orthopedic injury) of enrolled participants and those attending the 3-month assessment, only three were significant (p < 0.05).
+The distribution of race was significantly different in the mild TBI versus the OI group with regard to enrolled participants (Fisher's exact test p = 0.011).
There was a significant group difference (mild TBI vs. orthopedic injury) in pre-injury adaptive function in participants at the 3-month assessment (df = 281; p = 0.019).
++The Injury Severity Score was significantly higher in the enrolled OI group versus the enrolled mTBI group (df = 328; p = 0.000).
+++The ISS was significantly higher in the orthopedic injury group versus the mild TBI group in the participants at the 3-month assessment (df = 281; p = 0.000).
TBI, traumatic brain injury; ns, not significant; WASI-II, Wechsler Abbreviated Scale of Intelligence Second Edition; WRAT-4, Wide Range Achievement Test-4th Edition.
Table 2.
Specific Lifetime Pre-injury Psychiatric Disorders and Specific Novel Psychiatric Disorders in the First 3-Months Post-injury
| |
Pre-injury lifetime psychiatric disorders |
Novel psychiatric disorders in the first 3 post-injury months |
|||
|---|---|---|---|---|---|
| Mild TBI (n = 220) | Orthopedic injury (n = 110) | Mild TBI (n = 189) | Orthopedic injury (n = 94) | ||
| ADHD | 40 (18.2%) | 16 (14.6%) | 7/155 (4.5%) | 0/81 (0%) | |
| Oppositional defiant Disorder | 5 (2.3%) | 1 (0.9%) | 3/178 (1.7%) | 1/89 (1.1%) | |
| Other specified disruptive, impulse-control, and conduct disorder (OSDI-CCD) | 7 (3.2%) | 5 (4.6%) | 0/178 (0%) | 0/89 (0%) | |
| Externalizing disorder (ADHD/ODD/OSDI-CCD) | 44 (20.0%) | 19 (17.3%) | 9/185 (4.9%) | 1/93 (1.1%) | |
| Adjustment disorder | 6 (2.7%) | 5 (4.6%) | 4/183 (2.2%) | 1/89 (1.1%) | |
| GAD | 2 (0.9%) | 0 (0%) | 1/187 (0.5%) | 0/94 (0%) | |
| Specific phobia | 12 (5.5%) | 5 (4.6%) | 1/178 (0.6%) | 1/92 (1.1%) | |
| Separation anxiety Disorder | 3 (1.4%) | 4 (3.6%) | 1/186 (0.5%) | 0/91 (0%) | |
| Agoraphobia | 1 (0.5%) | 0 (0%) | 0/188 (0%) | 0/94 (0%) | |
| Social phobia | 1 (0.5%) | 0 (0%) | 0/188 (0%) | 0/94 (0%) | |
| Other specified anxiety disorder | 6 (2.7%) | 5 (4.6%) | 1/183 (0.6%) | 0/88 (0%) | |
| Post-traumatic stress disorder (PTSD) | 3 (1.4%) | 0 (0%) | 0/186 (0%) | 0/94 (0%) | |
| Any anxiety Disorder/PTSD | 26 (11.8%) | 14 (12.7%) | 4/189 (2.1%) | 1/94 (1.1%) | |
| Major Depression/other depressive disorder | 5 (2.3%) | 2 (1.8%) | 0/184 (0%) | 0/92 (0%) | |
| Internalizing disorder (depressive/anxiety disorder/PTSD) | 28 (12.7%) | 15 (13.6%) | 4/189 (2.1%) | 1/94 (1.1%) | |
| Personality change due to a general medical condition | 0 (0%) | 0 (0%) | 3/189 (1.6%) | 0 (0%) | |
| Tic disorder | 9 (4.1%) | 5 (4.6%) | 1/181 (0.6%) | 0/89 (0%) | |
| Encopresis | 1 (0.5%) | 3 (2.7%) | 0/188 (0%) | 0/91 (0%) | |
Bolded numbers indicate details of the specific novel psychiatric disorders that developed in each group.
There were no cases of the following pre-injury or novel psychiatric disorders: panic disorder, obsessive-compulsive disorder, cyclothymia, bipolar disorder, alcohol use disorder, and drug use disorder.
Denominators vary for novel psychiatric disorders in the first 3 months due to the ineligibility of certain individuals for a particular novel psychiatric disorder if they already manifested that disorder before the injury.
TBI, traumatic brain injury; ADHD, attention-deficit/hyperactivity disorder; GAD, generalized anxiety disorder.
Follow-up characteristics
The 3-month follow up analyses were based on 189/220 (85.9%) of the enrolled participants with mTBI and 94/110 (85.5%) of the enrolled participants with OI. The right two columns of Table 1 show a significant difference in the 3-month follow up cohort with regard to a higher pre-injury Adaptive Behavior Composite score in the mTBI versus OI group (108.2 ± 13.0 vs. 104.4 ± 12.5; df = 281; p = 0.019). The Injury Severity Score was significantly higher in the OI group versus the mTBI group in the participants at the 3-month assessment (3.93 ± 0.94 versus 2.62 ± 2.42 respectively df = 281; p = 0.000). There was a significant difference in cause of injury between the mTBI and OI groups participating at 3 months (Fisher's exact test p = 0.000). Inspection of the data revealed that this was driven by the falls accounting for 87% of OI cases versus 56% of mTBI cases, and more mTBI cases were injured by accidentally striking or being struck by an object, accidentally striking or being struck by a person, and having a transportation-related injury. When we compared the participants (n = 283) versus non-participants (n = 47) at the 3-month follow up, we found no differences in any of the variables (demographic, psychiatric, adaptive, family, academic, injury severity, and cause of injury) listed in Table 1, except that the participants had a significantly higher IQ than non-participants (103.0 ± 14.2; n = 281 vs. 95.8 ± 11.0; n = 47; p < 0.0005).
Post-injury recurrence of pre-injury psychiatric disorders
Post-injury recurrences of previously resolved pre-injury psychiatric disorders were noted in four participants, all of whom had mTBI, all of whom evidenced a single recurring disorder, and none of whom exhibited an accompanying novel psychiatric disorder. These events included recurrence of previously resolved ADHD, recurrence of an adjustment disorder (previously unspecified and currently depressed), recurrence of a specific phobia of needles, and recurrence of “other specified disruptive impulse control and conduct disorder” which was already in partial remission. A fifth participant with mTBI, also with no novel psychiatric disorder, had accrual of sufficient additional anxiety symptoms to shift category from “other specified anxiety disorder” to generalized anxiety disorder.
Novel psychiatric disorders
NPD during the 3-month post-injury follow up developed in 18 children with mTBI, including four children with mTBI who had two NPDs and 14 children with mTBI who developed one NPD. NPD occurred in three of the children with OI and each of these children had a single NPD. The specific NPDs and categories of NPD are shown in Table 2. Within the mTBI group, the NPDs were ADHD (n = 7); adjustment disorder (n = 4); anxiety disorder (n = 4) that included generalized anxiety disorder, specific phobia, separation anxiety disorder, and other specified anxiety disorder; oppositional defiant disorder (n = 3); personality change due to a general medical condition (n = 3); and a tic disorder (n = 1). The NPDs in the OI group consisted of oppositional defiant disorder, adjustment disorder, and specific phobia. Teachers' input by means of the TRF was available for only 100/283 (35.3%) participants for guiding “best-estimate” psychiatric diagnoses at the 3-month assessment.
Effect of mTBI on novel psychiatric disorders
In unadjusted analyses, the mTBI group was associated with a higher frequency of NPD than the OI group at 3 months [mean ratio (MR) 3.647, 95% confidence interval CI95 (1.264, 15.405), p = 0.014]. After adjustment for confounders (SES, pre-injury lifetime psychiatric disorder, and family psychiatric history, family function), the effect of mTBI was similar [MR = 3.724, CI95 (1.264, 15.945), p = 0.015; Table 3].
Table 3.
Predictors of Higher NPD Count, and Effect of Mild TBI on NPD Count at 3 Months: Unadjusted and Adjusted Poisson Log-Linear Regression Analysis
| |
|
Unadjusted analysis |
Adjusted analysis |
||
|---|---|---|---|---|---|
| N | Mean ratio (95% CI) | p Value | Mean ratio (95% CI) | p Value | |
| mTBI vs. OI | 283 | 3.647 (1.264, 15.405) | 0.014 | 3.724 (1.264, 15.945) | 0.015 |
| Age, per year | 283 | 1.006 (0.833, 1.222) | 0.951 | ||
| Female sex | 283 | 0.834 (0.324, 1.914) | 0.680 | ||
| Socioeconomic Status, per unit | 283 | 0.709 (0.473, 1.047) | 0.084 | 0.618 (0.383, 0.973) | 0.037 |
| Race (Minority vs. White | 283 | 0.592 (0.197, 1.462) | 0.271 | ||
| Pre-injury lifetime psychiatric disorder | 283 | 2.876 (1.306, 6.614) | 0.009 | 2.284 (1.026, 5.305) | 0.043 |
| Pre-injury Vineland Adaptive Behavior Composite, per unit | 283 | 0.993 (0.963, 1.023) | 0.647 | ||
| Family Psychiatric History, high vs. low | 280 | 2.833 (1.260, 6.944) | 0.011 | 2.748 (1.201, 6.839) | 0.016 |
| McMaster Structured Interview of Family Function Clinical Rating Scale (McSIFF CRS), per unit | 255 | 0.683 (0.498, 0.950) | 0.024 | ||
| Family Assessment Device (mother; FAD), per unit | 280 | 0.935 (0.358, 2.277) | 0.886 | ||
| WASI-II Full-Scale IQ, per unit | 281 | 0.982 (0.955, 1.010) | 0.161 | ||
| WRAT-4 Sentence Comprehension | 282 | 0.989 (0.966, 1.012) | 0.331 | ||
| WRAT-4 Calculation Skills | 282 | 0.996 (0.972, 1.021) | 0.733 | ||
| Injury Severity Score | 283 | 0.901 (0.717, 1.093) | 0.311 | ||
Bolded numbers represent variables with p < 0.15 values in single-predictor analyses, which were included in the starting model for multi-predictor analyses.
The results are reported as mean ratios and 95% confidence intervals, based on the likelihood ratio test.
NPD, novel psychiatric disorder; TBI, traumatic brain injury; CI, confidence interval; mTBI, mild traumatic brain injury; OI, orthopedic injury; WASI-II, Wechsler Abbreviated Scale of Intelligence Second Edition; WRAT-4, Wide Range Achievement Test-4th Edition.
Predictors of mTBI on novel psychiatric disorders
In single-predictor analyses, the following factors were significantly associated with higher NPD counts at 3 months: mTBI versus OI (see above), pre-injury lifetime psychiatric disorder [MR = 2.876, CI95 (1.306, 6.614), p = 0.009], high versus low family psychiatric history [MR = 2.833, CI95 (1.260, 6.944), p = 0.011], and worse family function [MR = 0.683 per unit on the McSIFF CRS, CI95 (0.498, 0.950), p = 0.024]. Worse socio-economic status showed a trend-level association [MR = 0.709 per additional unit, CI95 (0.473, 1.047), p = 0.084].
In multi-predictor analyses, the factors significantly associated with higher NPD mean counts after adjustment for each other were mTBI versus OI [MR = 3.724, CI95 (1.264, 15.945), p = 0.015]; pre-injury lifetime psychiatric disorder [MR = 2.284, CI95 (1.026, 5.305), p = 0.043]; high versus low family psychiatric history [MR = 2.748, CI95 (1.201, 6.839), p = 0.016]; and worse socio-economic status, [MR = 0.618 per additional unit, CI95 (0.383, 0.973), p = 0.037]. This statistical model coincided with the adjusted model for the effect of mTBI (Table 3).
Discussion
There were three main findings in the study that examined the number of NPDs that occurred in the first 3 months after mTBI versus OI. Our first hypothesis was supported in that NPD occurred at a significantly higher mean ratio in children with mTBI versus OI before and after adjusting for potential confounders including child variables (lower pre-injury child adaptive function, lower estimated pre-injury cognitive function, lower estimated pre-injury academic function, and the presence of pre-injury lifetime psychiatric disorders), and pre-injury family variables (lower socio-economic status, lower pre-injury family function, and more intense family psychiatric history). The second hypothesis was also supported by the finding that NPD was significantly predicted by child variables (pre-injury lifetime psychiatric disorders), and pre-injury family variables (lower socio-economic status, lower family function, and more intense family psychiatric history). Third, the most common NPD was ADHD, which occurred in 7/155 (4.5%) of children with NPD and in none of the 81 children with OI evaluated 3 months post-injury.
The finding that NPD is significantly more common in the first 3 months after mTBI versus OI (mean ratio 3.724) is consistent with behavioral studies with continuous and categorical measures of PCS.18,43 The adjusted analyses that controlled for known child and family psychosocial confounders underscored that indeed it was membership in the mTBI group that accounted for the observed differences in NPD. These findings suggest that there is at least a perturbation of brain function that is caused by mTBI that disrupts attention and behavior, affects mood regulation, and compromises coping with adversity resulting in elaboration of ADHD and ODD, anxiety disorders, and adjustment disorder respectively.
The study was the first to examine prediction of NPD outcome by child psychosocial measures in a controlled psychiatric interview study of mTBI. The results showing that NPD was significantly predicted by higher pre-injury psychiatric disorder is consistent with findings from both short-term (3-24 months)2 and even long-term (24-year follow up)44 prospective longitudinal uncontrolled psychiatric studies. This risk is noted even in the absence of mTBI and is a robust finding in natural history studies of childhood psychopathology.45 The results did not support lower presumed pre-injury intellectual function and academic function as risk factors for NPD. This finding diverges from those of a psychiatric study of consecutively hospitalized children with mTBI which found lower processing speed, lower IQ, and lower measures of expressive language function significantly related to NPD in the first 6 months post-injury.23 It is most likely that these discrepant findings are related to mTBI sample differences with regard to severity of injury—specifically children consecutively treated primarily in the ED versus those consecutively hospitalized. This suggests that in the context of the milder forms of mTBI, pre-injury psychiatric disturbance is a more important risk factor for post-injury psychiatric domain-convergent disturbance (NPD) than are pre-injury neurocognitive domain-divergent variables.
This study is also the first to examine prediction of NPD outcome with family psychosocial measures in a controlled psychiatric interview study of mTBI. The findings are similar to those of studies examining PCS outcomes.46 In univariable analyses, lower socio-economic status, lower family function, and more intense family psychiatric history were significantly related to NPD. The adjusted analyses found that lower socio-economic status, and more intense family psychiatric history in first-degree relatives, in addition to child variables (mTBI group and higher pre-injury lifetime psychiatric disorder) independently significantly predicted NPD. These findings underscore the point that both distal (lower socio-economic status) and proximal (more intense family psychiatric history) family variables, along with child variables, are informative in understanding NPD after mTBI.
The mechanisms by which these independent distal and proximal family measures operate are likely different. Children raised in lower versus higher socio-economic environments generally have less access to equivalent education, medical care, and recreational opportunities, and have higher rates of psychiatric disorder even in general population samples.47 The potential mechanism of more intense family psychiatric history in first-degree relatives may relate to both adverse environmental and genetic influences on the development of NPD.48,49 The environmental influence of family psychiatric illness may decrease the extent that the child's developmental needs are met by preoccupied and ill parents in particular. That family function was a significant variable predicting NPD in univariable analyses, but not in the adjusted analyses suggested that proximal family environment factors were relatively less critical in outcome in this sample of mTBI.
The study has several limitations. First, novel psychiatric disorders are relatively uncommon after mTBI and even more uncommon after OI in the first 3 months post-injury. Even though the sample was relatively large, an even larger sample may be useful to study this low frequency outcome in general and specific NPDs in particular. Second, the enrolled mTBI group had a significantly higher minority race representation compared with the OI group, yet this was not reflected in SES differences. However, the difference in the mTBI versus OI racial composition of the 3-month cohort, upon which our findings depend, was not statistically significant. Further, NPD was not significantly related to race. Third, attrition from baseline to 3 months was approximately 14%, and the group lost to follow up had a significantly lower baseline IQ. However, those who did not follow up were not significantly different in every other pre-injury variable measured including age, sex, SES, race, ethnicity, pre-injury psychiatric disorder, pre-injury adaptive function, family psychiatric history, family function, and academic function.
Fourth, we were successful in getting teachers' behavioral questionnaire reports in only approximately 35% of the participants. Fifth, the enrolled sample of children with mTBI was significantly older than the non-enrolled group. However, this difference was only 0.6 years and is unlikely to be clinically significant and age was not a significant predictor of NPD outcome. Sixth, there is an implicit risk of a “good old days bias” when pre-injury functioning is assessed retrospectively after the injury. This risk was mitigated by the proximity of the initial assessment to the injury (mean = 17.7 ± SD = 5.8 days). The finding in this study and other similarly designed studies that presence rather than absence of pre-injury lifetime psychiatric disorder predicts higher frequency of NPD suggests that this bias is small.2,3,19,20
Seventh, although diagnoses were made only in the context of significant impairment, the findings may nonetheless reflect transient psychiatric disturbance which may or may not develop into full-blown psychiatric disorders. This is a particularly important consideration given the overlap in symptomatology between symptoms commonly experienced after mTBI, which are expected to resolve in most cases, and psychiatric diagnoses that are lifelong and may require pharmacological intervention (e.g., ADHD). If in fact, novel disorders such as ADHD persist, there may be important implications in understanding the effect of mTBI on neurodevelopment. Such insights may be especially relevant given earlier research on a sample of more seriously injured children, i.e., consecutively hospitalized children with mild to severe TBI, that found neurocognitive profile differences in children diagnosed with new-onset ADHD versus developmental (pre-injury) ADHD.50
There were several notable strengths of the study. This was the first prospective controlled psychiatric interview study of a consecutive sample of children treated in the ED for mTBI. The sample size was relatively large and the injured control group matched the mTBI cohort very well, by design, with regard to age and sex. Further, the groups were not significantly different with respect to most of the predictive variables, including SES, pre-injury psychiatric diagnosis, family psychiatric history, pre-injury family function, IQ, and academic function. The study's primary outcomes—NPD counts—were generated from psychiatric assessments at 3 months post-injury conducted by interviewers who were blind to group affiliation. The diagnoses were made only in the context of significant impairment. There was excellent inter-rater reliability for psychiatric diagnoses with a second rater who was blind to group affiliation. The assessment tools were clinically relevant and included interviewer-rated, and not merely self-reported, data on psychiatric status, family psychiatric history, and a family assessment interview. The gold-standard interviewer's “best-estimate” psychiatric assessments relied on multiple informants including the primary care taker, the child, teacher (in 35% of cases), and mental status assessed by the interviewer. All assessments were reviewed by the first author, who is a board-certified child and adolescent psychiatrist and who was blind to group affiliation.
There were several clinical implications of the findings. First, a small but important minority of children treated primarily in the ED for mTBI or for OI present with NPDs in the first 3 months after injury. Second, the injured children who were more likely to develop NPDs were those with mTBI, pre-injury lifetime psychiatric disorder, lower SES, and more intense family psychiatric history. Third, the gathering of corresponding clinical data in the ED could identify children at highest risk for post-injury psychiatric sequelae and potentially lead to early intervention. Fourth, a public health debate should focus on the generation of a best-practice protocol whereby ED administrative personnel routinely seek the guardian's permission to share injury information with the child's primary care physician and school teacher or counselor who should be provided with continuing education regarding identification and surveillance of their patients/students who are at highest risk for psychiatric complications. Research participation by teachers could be enhanced through educational outreach efforts aimed at school students and faculty within catchment-area school districts.
In conclusion, children who suffered mTBI were significantly more likely than children who incurred extracranial injuries to exhibit more NPDs within the first 3 months post-injury. This finding was independent of child variables (pre-injury psychiatric disorder) and family variables (lower SES, higher family psychiatric history), which also significantly predicted adverse psychiatric outcomes.
Funding Information
This research was supported by a National Institute of Child Health and Development Grant HD088438 (Dr. Max: Principal Investigator; Drs. Wilde and Vaida).
Supplementary Material
Author Disclosure Statement
Dr. Max provides expert testimony in cases of traumatic brain injury on an ad hoc basis for plaintiffs and defendants on a more or less equal ratio. This activity constitutes approximately 5% of his professional activities.
Dr. Bigler is retired but still provides expert testimony in cases of traumatic brain injury.
For the other authors, no competing financial interests exist.
Supplementary Material
References
- 1. Langlois, J.A., Rutland-Brown, W., and Wald, M.M. (2006). The epidemiology and impact of traumatic brain injury: a brief overview. J. Head Trauma Rehabilitation 21, 375–378. [DOI] [PubMed] [Google Scholar]
- 2. Max, J.E., Robin, D.A., Lindgren, S.D., Smith, W.L.Jr., Sato, Y., Mattheis, P.J., Stierwalt, J.A., and Castillo, C.S. (1997). Traumatic brain injury in children and adolescents: psychiatric disorders at two years. J. Am. Acad. Child Adolesc. Psychiatry 36, 1278–1285. [DOI] [PubMed] [Google Scholar]
- 3. Brown, G., Chadwick, O., Shaffer, D., Rutter, M., and Traub, M. (1981). A prospective study of children with head injuries: III. Psychiatric sequelae. Psychol. Med.11, 63–78. [DOI] [PubMed] [Google Scholar]
- 4. Gerring, J.P., Brady, K.D., Chen, A., Vasa, R., Grados, M., Bandeen-Roche, K.J., Bryan, R.N., and Denckla, M.B. (1998). Premorbid prevalence of ADHD and development of secondary ADHD after closed head injury. J. Am. Acad. Child Adolesc. Psychiatry 37, 647–654. [DOI] [PubMed] [Google Scholar]
- 5. Max, J.E., Koele, S.L., Smith, W.L.Jr., Sato, Y., Lindgren, S.D., Robin, D.A., and Arndt, S. (1998). Psychiatric disorders in children and adolescents after severe traumatic brain injury: a controlled study. J. Am. Acad. Child Adolesc. Psychiatry 37, 832–840. [DOI] [PubMed] [Google Scholar]
- 6. Max, J.E., Robertson, B.A., and Lansing, A.E. (2001). The phenomenology of personality change due to traumatic brain injury in children and adolescents. J. Neuropsychiatry Clin. Neurosci. 13, 161–170. [DOI] [PubMed] [Google Scholar]
- 7. Emery, C.A., Barlow, K.M., Brooks, B.L., Max, J.E., Villavicencio-Requis, A., Gnanakumar, V., Robertson, H.L., Schneider, K., and Yeates, K.O. (2016). A systematic review of psychiatric, psychological, and behavioural outcomes following mild traumatic brain injury in children and adolescents. Can. J. Psychiatry 61, 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Massagli, T.L., Fann, J.R., Burington, B.E., Jaffe, K.M., Katon, W.J., and Thompson, R.S. (2004). Psychiatric illness after mild traumatic brain injury in children. Arch. Phys. Med. Rehabil. 85, 1428–1434. [DOI] [PubMed] [Google Scholar]
- 9. McKinlay, A., Dalrymple-Alford, J.C., Horwood, L.J., and Fergusson, D.M. (2002). Long term psychosocial outcomes after mild head injury in early childhood. J. Neurol. Neurosurg. Psychiatry 73, 281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mayer, A.R., Stephenson, D.D., Dodd, A.B., Robertson-Benta, C.R., Pabbathi Reddy, S., Shaff, N.A., Yeates, K.O., van der Horn, H.J., Wertz, C.J., Park, G., Oglesbee, S.J., Bedrick, E.J., Campbell, R.A., Phillips, J.P., and Quinn, D.K. (2020). Comparison of methods for classifying persistent post-concussive symptoms in children. J. Neurotrauma 37, 1504–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wassenberg, R., Max, J.E., Koele, S.L., and Firme, K. (2004). Classifying psychiatric disorders after traumatic brain injury and orthopaedic injury in children: adequacy of K-SADS versus CBCL. Brain Inj. 18, 377–390. [DOI] [PubMed] [Google Scholar]
- 12. Carroll, L.J., Cassidy, J.D., Holm, L., Kraus, J., and Coronado, V.G. (2004). Methodological issues and research recommendations for mild traumatic brain injury: the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J. Rehabil. Med. 113–125. [DOI] [PubMed] [Google Scholar]
- 13. Satz, P., Zaucha, K., McCleary, C., and Light, R. (1997). Mild head injury in children and adolescents: a review of studies (1970-1995). Psychol. Bull. 122, 107–131. [DOI] [PubMed] [Google Scholar]
- 14. Ayr, L.K., Yeates, K.O., Taylor, H.G., and Browne, M. (2009). Dimensions of postconcussive symptoms in children with mild traumatic brain injuries. J. Int. Neuropsychol. Soc. 15, 19–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fay, T.B., Yeates, K.O., Taylor, H.G., Bangert, B., Dietrich, A., Nuss, K.E., Rusin, J., and Wright, M. (2010). Cognitive reserve as a moderator of postconcussive symptoms in children with complicated and uncomplicated mild traumatic brain injury. J. Int. Neuropsychol. Soc. 16, 94–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Taylor, H.G., Dietrich, A., Nuss, K., Wright, M., Rusin, J., Bangert, B., Minich, N., and Yeates, K.O. (2010). Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychology 24, 148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yeates, K.O., Taylor, H.G., Rusin, J., Bangert, B., Dietrich, A., Nuss, K., Wright, M., Nagin, D.S., and Jones, B.L. (2009). Longitudinal trajectories of postconcussive symptoms in children with mild traumatic brain injuries and their relationship to acute clinical status. Pediatrics 123, 735–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hajek, C.A., Yeates, K.O., Gerry Taylor, H., Bangert, B., Dietrich, A., Nuss, K.E., Rusin, J., and Wright, M. (2010). Relationships among post-concussive symptoms and symptoms of PTSD in children following mild traumatic brain injury. Brain Inj. 24, 100–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Max, J.E., Smith, W.L.Jr., Sato, Y., Mattheis, P.J., Castillo, C.S., Lindgren, S.D., Robin, D.A., and Stierwalt, J.A. (1997). Traumatic brain injury in children and adolescents: psychiatric disorders in the first three months. J. Am. Acad. Child Adolesc. Psychiatry 36, 94–102. [DOI] [PubMed] [Google Scholar]
- 20. Max, J.E., Troyer, E.A., Arif, H., Vaida, F., Wilde, E.A., Bigler, E.D., Hesselink, J.R., Yang, T.T., Tymofiyeva, O., Wade, O., and Paulsen, J.S. (2021). Traumatic brain injury in children and adolescents: Psychiatric disorders 24 years later. J. Neuropsychiatry Clin. Neurosci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Max, J.E., Friedman, K., Wilde, E.A., Bigler, E.D., Hanten, G., Schachar, R.J., Saunders, A.E., Dennis, M., Ewing-Cobbs, L., Chapman, S.B., Yang, T.T., and Levin, H.S. (2015). Psychiatric disorders in children and adolescents 24 months after mild traumatic brain injury. J. Neuropsychiatry Clin. Neurosci. 27, 112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Max, J.E., Pardo, D., Hanten, G., Schachar, R.J., Saunders, A.E., Ewing-Cobbs, L., Chapman, S.B., Dennis, M., Wilde, E.A., Bigler, E.D., Thompson, W.K., Yang, T.T., and Levin, H.S. (2013). Psychiatric disorders in children and adolescents six-to-twelve months after mild traumatic brain injury. J. Neuropsychiatry Clin. Neurosci. 25, 272–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Max, J.E., Schachar, R.J., Landis, J., Bigler, E.D., Wilde, E.A., Saunders, A.E., Ewing-Cobbs, L., Chapman, S.B., Dennis, M., Hanten, G., and Levin, H.S. (2013). Psychiatric disorders in children and adolescents in the first six months after mild traumatic brain injury. J. Neuropsychiatry Clin. Neurosci. 25, 187–197. [DOI] [PubMed] [Google Scholar]
- 24. Teasdale, G., and Jennett, B. (1974). Assessment of coma and impaired consciousness. A practical scale. Lancet 2, 81–84. [DOI] [PubMed] [Google Scholar]
- 25. Association for the Advancement of Automotive Medicine (1990). Abbreviated Injury Scale, 1990 Revision. Association for the Advancement of Automotive Medicine: Des Plaines, IL. [Google Scholar]
- 26. Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., Williamson, D., and Ryan, N. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- 27. Max, J.E., Castillo, C.S., Lindgren, S.D., and Arndt, S. (1998). The Neuropsychiatric Rating Schedule: reliability and validity. J. Am. Acad. Child Adolesc. Psychiatry 37, 297–.304. [DOI] [PubMed] [Google Scholar]
- 28. American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Eisorders. 4th, TR ed. American Psychiatric Press: Washington, DC. [Google Scholar]
- 29. Achenbach, T.M. (2001). Child Behavior Checklist Teacher's Report Form for Ages 6-18, in: Manual for the ASEBA school-age forms & profiles: An Integrated System of Multi-Informant assessment. ASEBA (Achenbach System of Empirically Based Assessment). University of Vermont, Research Center for Children, Youth, and Families: Burlington, VT. [Google Scholar]
- 30. Leckman, J.F., Sholomskas, D., Thompson, W.D., Belanger, A., and Weissman, M.M. (1982). Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch. Gen. Psychiatry 39, 879–883. [DOI] [PubMed] [Google Scholar]
- 31. Sparrow, S.S., Cicchetti, D.V., and Balla, D.A. (2005). Vineland Adaptive Behavior Scales, Second Edition. American Guidance Services: Circle Pines, MN. [Google Scholar]
- 32. Wechsler, D. (2011). Weschler Abbreviated Scale of Intelligence Manual. The Psychological Corporation: San Antonio, TX. [Google Scholar]
- 33. Wilkinson, G.S., and Robertson, G.J. (2006). Wide Range Achievement Test: Professional Manual. Psychological Assessment Resources: Lutz, FL. [Google Scholar]
- 34. Yeates, K.O., and Taylor, H.G. (1997). Predicting premorbid neuropsychological functioning following pediatric traumatic brain injury. J. Clin. Exp. Neuropsychol. 19, 825–837. [DOI] [PubMed] [Google Scholar]
- 35. Miller, I.W., Kabacoff, R.I., Epstein, N.B., and Bishop, D.S. (1994). The development of a clinical rating scale for the McMaster Model of Family Functioning. Family Process 33, 53–69. [DOI] [PubMed] [Google Scholar]
- 36. Max, J.E., Castillo, C.S., Robin, D.A., Lindgren, S.D., Smith, W.L.Jr., Sato, Y., Mattheis, P.J., and Stierwalt, J.A. (1998). Predictors of family functioning after traumatic brain injury in children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry 37, 83–90. [DOI] [PubMed] [Google Scholar]
- 37. Miller, I.W., Epstein, N.B., Bishop, D.S., and Keitner, G.I. (1985). The McMaster Family Assessment Device: reliability and validity. J. Marital Fam. Ther. 11, 345–356. [Google Scholar]
- 38. Schwartz, L., Taylor, H.G., Drotar, D., Yeates, K.O., Wade, S.L., and Stancin, T. (2003). Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. J. Pediatr. Psychol. 28, 251–263. [DOI] [PubMed] [Google Scholar]
- 39. Andreasen, N.C., Rice, J., Endicott, J., Reich, T., and Coryell, W. (1994). The family history approach to diagnosis. In: Psychatric Epidemiology Assessment Concepts and Methods. Mezzich, J.E., Jorge, M.R., and Salloum, I.M. (eds). The John Hopkins University Press: Baltimore, MD, and London, UK, pps. 349–367. [Google Scholar]
- 40. Taylor, H.G., Yeates, K.O., Wade, S.L., Drotar, D., Stancin, T., and Minich, N. (2002). A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology 16, 15–27. [DOI] [PubMed] [Google Scholar]
- 41. Maldonado, G., and Greenland, S. (1993). Simulation study of confounder-selection strategies. Am. J. Epidemiol. 138, 923–936. [DOI] [PubMed] [Google Scholar]
- 42. Brunkhorst-Kanaan, N., Libutzki, B., Reif, A., Larsson, H., McNeill, R.V., and Kittel-Schneider, S. (2021). ADHD and accidents over the life span—a systematic review. Neurosci. Biobehav. Rev. 125, 582–591. [DOI] [PubMed] [Google Scholar]
- 43. Barlow, K.M., Crawford, S., Stevenson, A., Sandhu, S.S., Belanger, F., and Dewey, D. (2010). Epidemiology of postconcussion syndrome in pediatric mild traumatic brain injury. Pediatrics 126, e374–e381. [DOI] [PubMed] [Google Scholar]
- 44. Arif, H., Troyer, E.A., Paulsen, J.S., Vaida, F., Wilde, E.A., Bigler, E.D., Hesselink, J.R., Yang, T.T., Tymofiyeva, O., Wade, O., and Max, J.E. (2021). Long-term psychiatric outcomes in adults with history of pediatric traumatic brain injury. J. Neurotrauma 38, 1515–1525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Last, C.G., Perrin, S., Hersen, M., and Kazdin, A.E. (1996). A prospective study of childhood anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 35, 1502–1510. [DOI] [PubMed] [Google Scholar]
- 46. McNally, K.A., Bangert, B., Dietrich, A., Nuss, K., Rusin, J., Wright, M., Taylor, H.G., and Yeates, K.O. (2013). Injury versus noninjury factors as predictors of postconcussive symptoms following mild traumatic brain injury in children. Neuropsychology 27, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reiss, F., Meyrose, A.K., Otto, C., Lampert, T., Klasen, F., and Ravens-Sieberer, U. (2019). Socioeconomic status, stressful life situations and mental health problems in children and adolescents: results of the German BELLA cohort-study. PloS One 14, e0213700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Rutter, M., Macdonald, H., Le Couteur, A., Harrington, R., Bolton, P., and Bailey, A. (1990). Genetic factors in child psychiatric disorders—II. Empirical findings. J. Child Psychol. Psychiatry 31, 39–83. [DOI] [PubMed] [Google Scholar]
- 49. Polderman, T.J., Benyamin, B., de Leeuw, C.A., Sullivan, P.F., van Bochoven, A., Visscher, P.M., and Posthuma, D. (2015). Meta-analysis of the heritability of human traits based on fifty years of twin studies. Nat. Genet. 47, 702–709. [DOI] [PubMed] [Google Scholar]
- 50. Ornstein, T.J., Sagar, S., Schachar, R.J., Ewing-Cobbs, L., Chapman, S.B., Dennis, M., Saunders, A.E., Yang, T.T., Levin, H.S., and Max, J.E. (2014). Neuropsychological performance of youth with secondary attention-deficit/hyperactivity disorder 6- and 12-months after traumatic brain injury. J. Int. Neuropsychol. Soc. 20, 971–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.