Abstract
In this study, we aimed to assess the current scientific evidence concerning the effectiveness of combining two acceleration techniques or repeating an acceleration procedure in comparison with the single application in terms of the speed of the orthodontic tooth movement (OTM).
We performed a comprehensive electronic search to retrieve relevant studies on 10 databases. Randomized controlled trials (RCTs) on fixed orthodontic treatment patients who received multiple types of acceleration techniques or underwent a repeated acceleration procedure compared to a single application were included. Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) was used for assessing the risk of bias of retrieved studies.
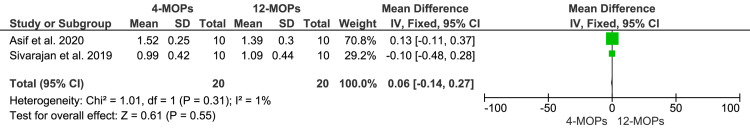
A total of six RCTs were included in this review. Regarding multiple acceleration methods, it seems that the combination of low-level laser therapy (LLLT) with a surgical technique outperforms the single application of each technique separately. Additionally, the combination of two surgical interventions may have a synergistic effect leading to reduced treatment time compared to the application of a single intervention. Regarding acceleration method repetition, it seems that the re-application of surgical procedures twice is more efficient than the single application. The meta-analysis showed a non-significant difference in the canine retraction rate between the four-weekly micro-osteoperforations (MOPs) (three times of applications) and both the eight-weekly MOPs (two times of applications) [mean difference (MD) = 0.24; 95% CI: -0.2-0.77; p = 0.36], as well as 12-weekly MOPs (two times of applications) (MD = 0.06; 95% CI: -0.14-0.27; p = 0.55).
Based on very low evidence, combining two acceleration techniques is superior over a single application in accelerating tooth movement. Again, very low evidence suggests that the efficacy of repetition of surgical procedures twice and three times is similar. Further high-quality RCTs are required to assess the benefit of repeating an acceleration procedure or combining two different methods. In addition, more insight is needed into the possible side effects associated with the repetition or multiplicity of procedures.
Keywords: low-level laser therapy, mops, multiple osteoperforation, corticotomy, non-surgical acceleration, surgical acceleration, repeated application, combined application, acceleration, arthodontic tooth moevement
Introduction and background
Comprehensive orthodontic treatment for moderate to severe cases of malocclusion usually lasts for more than 18 months, taking into account several factors that lead to a significant difference [1]. Elongating orthodontic treatment may lead to white spots formation, dental caries, apical root resorption, periodontal disease, pain, and discomfort [2,3]. Moreover, many adult patients wish to finish orthodontic treatment faster for aesthetic or social reasons [4]. Hence, many attempts have been made to shorten orthodontic duration: local or systemic administration of pharmacological substances, mechanical or physical stimulation, and surgical interventions [5].
Pharmacological interventions depend on the injection of local substances, which is related to the biological response occurring during tooth movement. The efficacy of pharmacological molecules has been investigated in many human and animal studies [6]. Many of these substances have proven their effectiveness, e.g., prostaglandins, which are inflammatory mediators that increase the number of osteoclasts leading to stimulating bone resorption and acceleration of the orthodontic tooth movement (OTM). Prostaglandin injection has been proven to be associated with pain and dose-dependent root resorption [7]. Also, pharmacological molecules that have proven effective in accelerating OTM include vitamin D [8] and hormones such as the parathyroid hormone (PTH) [9]. On the other hand, relaxin, which is considered to be a hormone, has many roles as it helps during childbirth as well as impacts some physiologic functions such as collagen turnover, angiogenesis, and antifibrosis, in addition to its role in soft tissue remodeling [10]. It affects the OTM by increasing the collagen in the tension site and decreasing it in the compression site. The mechanism of relaxin's effect on acceleration OTM remains unclear. However, one of the studies that investigated the effect of relaxin in humans showed that its injection was not effective in accelerating OTM [10].
The physical methods rely on using device-assisted therapy and include direct electric currents, pulsed electromagnetic field, vibration [11], and low-level laser, which has been widely investigated in many research projects [12] and has proven to be effective in its stimulating efficacy in alveolar bone resorption and formation processes by increasing osteoclast and osteoblast numbers, leading to the acceleration of OTM [13].
The surgical procedures are considered the most clinically effective methods, and they have been rigorously tested several times in terms of the possibility of significantly decreasing treatment duration [3]. However, the surgical intervention includes various procedures such as conventional corticotomy [5,14], dentoalveolar distraction [15], periodontal distraction [16], interseptal alveolar surgery [17], accelerated osteogenic orthodontics [18], piezocision [2,19], corticision [20], and micro-osteoperforations (MOPs) [21]. All these procedures depend on the same principle, "regional acceleratory phenomenon" (RAP), which was first described by Forest and is based on the principle that the occurrence of surgical injury to the alveolar bone may temporarily speed up OTM [22]. The RAP was described as a transient stage of localized soft and hard tissue remodeling that resulted in the rebuilding of the injured sites to a normal state through recruitment of osteoclasts and osteoblasts by way of local intercellular mediator mechanisms involving precursors [22]. This mechanism does not involve any secondary healing by fibrous tissue formation.
The focus of several recently published systematic reviews (SRs) has been on evaluating the effectiveness of different individual interventions for orthodontic acceleration, both surgical [23-25] and non-surgical [26,27]. Mohaghegh et al. [28], in their recent SR, discussed the effect of single and multiple MOPs on the rate of OTM. However, this SR was oriented only toward the MOPs procedure although repetition can be performed for other acceleration procedures such as traditional corticotomy, flapless corticision, flapless piezocision corticotomy, and high-intensity laser therapy-assisted corticotomy. In addition, no SR has evaluated the effect of combining different procedures, such as combining surgery with low-level laser therapy (LLLT) or surgery with vibrational devices. Hence, we performed this SR to address the following focused review question: Does the repetition of an acceleration procedure or the combination of different procedures outweigh a single application in patients undergoing fixed orthodontic treatment? In light of this objective, we aimed to critically appraise the available evidence regarding the effectiveness of multiplicity or repetition of acceleration procedures in comparison with the single application for speeding up orthodontic treatment.
Review
Materials and methods
Initially, a PubMed® scoping search was carried out to verify the existence of similar SRs and to check out potentially eligible trials before writing the final SR protocol. The search results indicated the presence of one potentially eligible study and the absence of any similar SRs about the same topic. Registration of this review with PROSPERO was performed (https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42021274314; 2021: CRD42021274314). This SR was prepared in accordance with the Cochrane Handbook for Systematic Reviews of Interventions [29], and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [30,31].
Eligibility criteria
Criteria of Exclusion and Inclusion Were Applied According to the PICOS (Patient/Population, Intervention, Comparison, and Outcomes) Framework as Follows:
Participants: healthy patients of both genders (regardless of age, malocclusion type, and racial group) undergoing fixed orthodontic treatment (either extraction- or non-extraction-based treatments).
Type of interventions: first theme: multiple methods of acceleration [two or more different methods of acceleration even they fell within the same category of acceleration (e.g., corticision followed by MOPs, both being surgical interventions)]. Second theme: repeated acceleration using a single method of acceleration at different time intervals (in the interventional group) compared to a single application of this method (or less frequent applications) in the control group.
Comparisons: first theme: only a single method of acceleration from any category. Second theme: only one application of the acceleration procedure without repetition (or with less frequent applications compared to what was applied in the control group).
Outcomes: primary outcomes were the rate of tooth movement (RTM), the time of tooth movement (TTM), or any equivalent measurement. Secondary outcomes: a complication reported by patients (e.g., pain, discomfort, and other related experiences), or gingival and periodontal problems including periodontal index (PI), gingival index (GI), attachment loss (AT), gingival recession (GR), and periodontal depth (PD), or undesired tooth movement (tipping, torquing, rotation), or anchorage loss, or bone/root changes including bone density (BD), bone resorption (BR), root resorption (RR), or long-term treatment stability.
Study design: we took into account all randomized controlled trials (RCTs) without any restrictions regarding the publication year or the language used.
Exclusion criteria: retrospective studies, non‑English language trials, in vitro studies, animal studies, reviews and technique description papers, editorials, personal opinions, case reports or case series reports, and finite element analysis articles were excluded.
Search strategy
An electronic search of databases [The Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE®, Scopus®, PubMed®, Web of Science™, Google™ Scholar, Trip, OpenGrey (to determine the grey literature), and PQDT OPEN from pro-Quest® (to determine dissertations and theses)] was carried out in August 2021 in the English language only with no time limitation. Scrutiny of selected trials reference lists' was done to investigate if any scientific paper was inadvertently missed during electronic research. Also, manual searching was conducted in the same period; the American Journal of Orthodontics and Dentofacial Orthopedics, the European Journal of Orthodontics, and the Angle Orthodontist. ClinicalTrials.gov and World Health Organization International Clinical Trials Registry Platform Search Portal (ICTRP) were also screened electronically to recover any unpublished studies or recently completed research work. More details about the electronic search strategy are provided in Table 1.
Table 1. Electronic search strategy.
| Database | Search strategy |
| CENTRAL (The Cochrane Library) | #1 orthodontic* OR orthodontic tooth movement" OR "orthodontic Treatment" OR "orthodontic Therapy" #2 accelerat* OR rapid* OR short* OR speed* OR fast #3 (surgical OR invasive OR minimally invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #4 (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #5 #1 AND #2 #6 #3 AND #5 #7 #4 AND #5 |
| EMBASE | #1 orthodontic* OR orthodontic tooth movement" OR "orthodontic Treatment" OR "orthodontic Therapy" #2 accelerat* OR rapid* OR short* OR speed* OR fast #3 (surgical OR invasive OR minimally invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #4 (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #5 #1 AND #2 #6 #3 AND #5 #7 #4 AND #5 |
| PubMed | #1 orthodontic* OR orthodontic tooth movement" OR "orthodontic Treatment" OR "orthodontic Therapy" #2 accelerat* OR rapid* OR short* OR speed* OR fast #3 (surgical OR invasive OR minimally invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #4 (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #5 #1 AND #2 #6 #3 AND #5 #7 #4 AND #5 |
| Scopus | #1 TITLE-ABS-KEY (orthodontic* OR "orthodontic tooth movement” OR "orthodontic Treatment" OR "orthodontic Therapy"). #2 TITLE-ABS-KEY (accelerat* OR rapid* OR short* OR speed* OR fast) #3TITLE-ABS-KEY (“surgical” OR “invasive” OR “minimally invasive”) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #4 TITLE-ABS-KEY (“non-surgical” OR “non-invasive”) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #5 #1 AND #2 #6 #3 AND #5 #7 #4 AND #5 |
| Web of Science | #1TS = (orthodontic OR "orthodontic tooth movement” OR "orthodontic Treatment" OR "orthodontic Therapy"). #2TS = (accelerat* OR rapid* OR short* OR speed* OR fast) #3TS = (surgical OR invasive OR minimally invasive) AND TS = (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #4TS = (non-surgical OR non-invasive AND TS = (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) #5 #1 AND #2 #6 #3 AND #5 #7 #4 AND #5 |
| Google Scholar | #1 (orthodontic OR "orthodontic tooth movement” OR "orthodontic Treatment" OR "orthodontic Therapy") AND (accelerat* OR rapid* OR short* OR speed* OR fast) AND (surgical OR invasive OR minimally invasive ) AND (combine* OR join* OR associate*) #2 (orthodontic OR "orthodontic tooth movement” OR "orthodontic Treatment" OR "orthodontic Therapy") AND (accelerat* OR rapid* OR short* OR speed* OR fast) AND (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicat*) |
| Trip | (orthodontic* OR "orthodontic tooth movement” OR "orthodontic Treatment" OR "orthodontic Therapy") AND (accelerate* OR rapid* OR short* OR speed* OR fast) AND (surgical OR invasive OR minimally invasive) AND (combine* OR join* OR associate*) OR (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicate*) |
| OpenGrey (http://www.opengrey.eu/) | #1 acceleration AND tooth movement #2 orthodontic AND acceleration #3 (surgical OR invasive OR minimally invasive ) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicate*) #4 (non-surgical OR non-invasive) AND (combine* OR join* OR associate*) AND (multiple or repeat* or duplicate*) |
| PQDT OPEN (from proQuest) | #1 acceleration AND tooth movement #2 orthodontic AND acceleration |
| World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) Search Portal | (orthodontic OR ‘tooth movement’ OR ‘orthodontic tooth movement’) AND (accelerate* OR rapid* OR short* OR speed* OR fast) |
| ClinicalTrials.gov | (orthodontic OR ‘tooth movement’ OR ‘orthodontic tooth movement’) AND (accelerate* OR rapid* OR short* OR speed* OR fast) |
Study selection and data extraction
Two reviewers (DTA and MYH) separately evaluated the studies' eligibility, and in instances of disagreement, a third author (OJ) helped in resolving this. At first, only titles and abstracts were checked. Subsequently, the full text of trials that appeared to be pertinent was evaluated and selected for inclusion, as well as titles or abstracts that were unclear to aid in decision-making. Failure to achieve one or more of the inclusion norms would have meant that the article was disqualified. In case of a need for more clarification or extra data, the specific author was e-mailed. Data extraction was independently achieved by the same two authors (DTA and MYH). A third author (OJ) was consulted to reach a solution when the two authors had disagreements. The data summary tables included the following items: general information (the name of authors, the year of publication, and study setting); methods (study design, treatment comparison); participants (sample size, age, and gender); intervention (the type of interventions, intervention site, and technical aspects of interventions); orthodontic aspects (malocclusion characteristics, type of movement, frequency of orthodontic adjustments, and follow-up time), and outcomes (primary and secondary outcomes mentioned, methods of outcome measurements, the statistical significance of reported differences in patients vs. controls).
Assessment of risk of bias in included studies and strength of evidence
The quality of the selected articles was estimated by two reviewers (DTA and MYH) using Version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) as the included studies were randomized trials [32]. Any conflict was resolved by discussion between the two reviewers. The following domains were evaluated as low, high risk, or some concern of bias for randomized trials: bias arising from the randomization process, bias due to deviations from intended interventions (effect of assignment to intervention; effect of adhering to intervention), bias due to missing outcome data, bias in the measurement of the outcome, and bias in the selection of the reported result. The overall risk-of-bias judgment of the included trials was assessed according to the following: "low risk of bias" if all fields were estimated as "at low risk of bias"; "some concerns" if at least one domain was assessed as "some concerns" but not to be at "high risk of bias" for any domain; "high risk of bias" if at least one or more fields were estimated as "at high risk of bias" or if there were some concerns for multiple domains in a way that substantially lowered confidence in the result. Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to obtain a supplemental summary of the reliability of the conclusions and strength of the evidence [33] as follows: high, moderate, low, or very low.
Data synthesis and statistical analysis
The details of the electronic search strategy are presented in Table 1.
Treatment intervention, trial protocol, patients, methodology, and outcome measures were taken into account when evaluating the included studies' heterogeneity. At first, heterogeneity was assessed visually and then mathematically. For conducting a meta-analysis, the RTM following the canine retraction in one month was considered. The meta‑analysis was carried out using Review Manager Version 5.4.1 (The Nordic Cochrane Centre, the Cochrane Collaboration, Copenhagen, Denmark). Mean difference (MD) with a confidence interval of 95% was estimated as the included articles used the same scale for outcome measurements [29]. If I2 was greater than 40%, the heterogeneity was considered as high, and the random effect model was used for meta-analysis [29].
Results
Study Selection and Inclusion in the Review
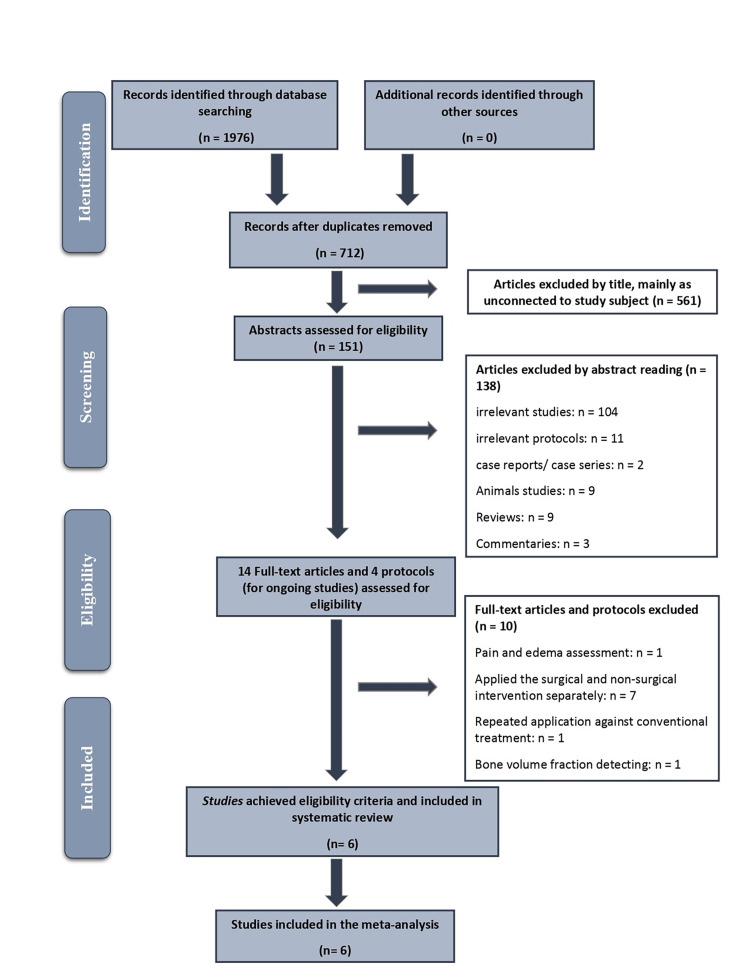
A flow chart of study selection for this review is presented in Figure 1. A total of 1,967 articles were identified from the electronic databases. After taking off duplicates and reviewing titles and abstracts, full texts of 14 potentially relevant papers were evaluated in-depth. Ten completed studies and two of the ongoing studies did not meet the inclusion criteria. A summary of the excluded articles after full-text assessment with reasons for exclusion is illustrated in Table 2. Subsequently, six RCT trials were included in the SR.
Table 2. Excluded studies and the reasons for exclusion.
| Study | Reason for exclusion |
| Rajasekaran UB, Krishna Nayak US (2014). Effect of prostaglandin E1 versus corticotomy on orthodontic tooth movement: an in vivo study. Indian Journal of Dental Research: official publication of the Indian Society for Dental Research. 25(6):717-21 | The study did not apply surgical and non-surgical acceleration methods together, but they were applied separately in the same group of patients |
| Muñoz F, Jiménez C, Espinoza D, Vervelle A, Beugnet J, Haidar Z (2016). Use of leukocyte and platelet-rich fibrin (L-PRF) in periodontally accelerated osteogenic orthodontics (PAOO): Clinical effects on edema and pain. Journal of Clinical and Experimental Dentistry, 8(2), | A cohort observational study; did not detect the tooth movement acceleration; it used leukocyte and platelet-rich fibrin (L-PRF) in periodontally accelerated osteogenic orthodontics (PAOO) to detect edema and pain |
| El-Ashmawi N, Abd El-Ghafour M, Nasr S, Fayed M, El-Beialy A, Nasef E (2018). Effect of surgical corticotomy versus low-level laser therapy (LLLT) on the rate of canine retraction in orthodontic patients. Orthodontic Practice US. 9:1-11 | The study did not apply surgical and non-surgical acceleration methods together, but they were applied separately in the same group of patients |
| Haliloglu-Ozkan T, Arici N, Arici S (2018). In-vivo effects of flapless osteopuncture-facilitated tooth movement in the maxilla and the mandible. Journal of Clinical and Experimental Dentistry, 10(8), e761 | The study compared the repeated application of osteopuncture against conventional orthodontic treatment |
| Sedky Y, Refaat W, Gutknecht N, ElKadi A (2019). Comparison between the effect of low-level laser therapy and corticotomy-facilitated orthodontics on RANKL release during orthodontic tooth movement: a randomized controlled trial. Lasers in Dental Science. 3(2):99-109 | The study did not apply surgical and non-surgical acceleration methods together, but they were applied separately in the same group of patients |
| Abdarazik MA, Ibrahim SA, Hartsfield JK, AlAhmady HH (2020). The effect of using full-thickness mucoperiosteal flap versus low-level laser application on orthodontic tooth movement acceleration. Al-Azhar Dental Journal for Girls. 7(2 April-Pediatric dentistry and orthodontics issue (Pediatric Dentistry, Orthodontics)):285-93 | The study did not apply surgical and non-surgical acceleration methods together, but they were applied separately in the same group of patients |
| Teh NHK, Sivarajan S, Asif MK, Ibrahim N, Wey MC (2020). Distribution of mandibular trabeculae bone volume fraction in relation to different MOP intervals for accelerating orthodontic tooth movement: A randomized controlled trial. The Angle Orthodontist, 90(6), 774-782 | The study aimed to investigate the effect of different intervals of micro-osteoperforation on the horizontal and vertical distribution of mandibular trabecular bone volume fraction |
| Türker G, Yavuz İ, Gönen ZB (2020). Which method is more effective for accelerating canine distalization short term, low-level laser therapy or piezocision? A split-mouth study. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie. :1-9 | The study did not apply surgical and non-surgical acceleration methods together, but they were applied separately in the same group of patients |
| CTRI/2018/05/014328: Comparison of micro-osteoperforation and low-level laser therapy on the rate of retraction-an in vivo study | Ongoing trial (protocol): the study is not applying surgical and non-surgical acceleration methods together, but they are applied separately in the same group of patients |
| NCT03308851: Evaluation of the effects of osteoperforation and piezocorticision on canine retraction | Ongoing trial (protocol): the study is not applying surgical and non-surgical acceleration methods together, but they are applied separately in the same group of patients |
Figure 1. The PRISMA flow diagram of the retrieved studies.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Characteristics of studies
The characteristics of the six included trials [16,34-38] are illustrated in Table 3 and Table 4. Only two trial protocols were found; more information about those ongoing research projects is given in Table 5 and Table 6.
Table 3. Characteristics of the included studies: PICOS, follow-up period, and main findings.
PICOS: patient/population, intervention, comparison, and outcomes; RCT: randomized controlled trial; NAC: non-accelerated control; compound design: consisting of both parallel and split-mouth; MOPs: micro-osteoperforations; LLLT: low-level laser therapy; Exp: experimental; M: male; F: female; RTM: rate of tooth movement; TTM: time of tooth movement
| Authors (year, country) | Methods | Participants | Type of Malocclusion | Interventions | Outcomes | |||
| Study design | Treatment comparison | Patients (M/F); age (years) | Type and site of intervention/technical aspects of interventions | Application frequency | Follow-up time | Primary and secondary outcomes | ||
| Multiple methods of acceleration (two or more different methods of acceleration) | ||||||||
| Abdelhameed and Refai, 2018, Minya, Egypt [34] | RCT (compound design) | MOPs/NAC vs. LLLT/NAC vs. MOPs + LLLT/NAC | Patients (M/F): 30 (NR/NR). Control: 30. Exp: 30. Age (years): 15-25 | Patients who need to extract maxillary 1st premolars and maxillary canine retraction | MOPs: 12 MOPs (with a depth of 6 mm) were applied by miniscrews (six MOPS were done buccally and six palatally). LLLT: a soft laser (wavelength: 810 ± 10 nm) was used from buccal and palatal surfaces along the root of the U3 | MOPs: the technique was repeated every two weeks. LLLT: the application of laser was at the beginning of a canine retraction, after three days, one week, two weeks, then every two weeks for three months | 3 months | Primary outcome: RTM (mm/week) |
| Farid et al., 2019, Cairo, Egypt [36] | RCT (split-mouth design) | Corticotomy + LLLT vs. corticotomy | Patients (M/F): 16 (0/16). Control: 16. Exp: 16. Age (years): 17-25 | Class I or Class II (Angles’ classification) malocclusion cases needed to extract 1st premolars | Corticotomy: after an elevated full-thickness flap, 10-15 corticotomy perforations with a depth of 1-2 mm were done from the distal surface of the 2nd premolar to the mesial surface of the U3, using a round bur. LLLT: InGaAs diode laser (wavelength: 940 ± 10 nm) was applied at the middle point of the U3 root on buccal and palatal surfaces for 240 seconds | LLLT: the application of laser was on the 1stday of retraction, after one, two, and three weeks, then every two weeks. The application of LLLT started on the same day of surgery | 4 months | Primary outcome: RTM (mm/month). Secondary outcomes: molar anchorage loss |
| Yousif et al., 2019, Tanta, Egypt [16] | RCT (compound design) | Multiple osteoperforation/NAC vs. multiple osteoperforation + corticotomy/NAC | Patients (M/F): 30 (NR/NR). Control: 30. Exp: 30. Age (years): 15-18 | Patients who need to extract 1st premolars and maxillary canine retraction | Multiple osteoperforation: after an elevated flap, 3 MOPs (2-mm wide, 2-mm deep, and 2 mm apart from each other) were done along the mesial and distal side of the U3 root, using round surgical bur. Corticotomy: after an elevated flap, a corticotomy cut along the distal side of the U3 root was carried out | Until the completion of the canine retraction | Primary outcome: TTM (days). Secondary outcomes: pain and discomfort., canine angulation | |
| Repetition of an acceleration method | ||||||||
| Sivarajan et al., 2019, Kuala Lumpur, Malaysia [38] | RCT (compound design) | MOP 4-weekly maxilla/8-weekly mandible/NAC vs. MOP 8-weekly maxilla/12-weekly mandible/NAC vs. MOP 12-weekly maxilla/4-weekly mandible/NAC | Patients (M/F): 30 (7/23). Control: 30. Exp: 30. Age (years): 18 years and above | Patients who need to extract four first premolars and canine retraction | MOPs: 3 MOPs (with a depth of 3 mm and 2 mm apart from each other vertically) were applied using an Orlus screw (through the buccal mucosa adjacent to the extraction site) | MOPs: the technique was repeated every 4 weeks in Group 1 (4 sessions of MOPs), 8 weeks in Group 2 (2 sessions of MOPs), and 12 weeks in Group 3 (2 sessions of MOPs) | 4 months | Primary outcome: RTM (mm/month). Secondary outcomes: pain and its impact on daily function |
| Asif et al., 2020, Kuala Lumpur, Malaysia [35] | RCT (compound design) | MOP 4-weeks/NAC vs. MOP 8-weeks/NAC vs. MOP 12-weeks/NAC | Patients (M/F): 30 (NR/NR). Control: 30. Exp: 30. Age (years): 18 years and above | Patients who need to extract four first premolars and canine retraction | MOPs: 3 MOPs (with a depth of 3 mm and 2 mm apart from each other vertically) were applied using an Orlus screw (through the buccal mucosa of the extraction site) | MOPs: the technique was repeated every 4 weeks in Group 1 (4 sessions of MOPs), 8 weeks in Group 2 (2 sessions of MOPs), and 12 weeks in Group 3 (2 sessions of MOPs) | 3 months | Primary outcome: RTM (mm/month) |
| Jaiswal et al., 2021, New Delhi, India [37] | RCT (split-mouth design) | One-time MOP vs. two-time MOP | Patients (M/F): 16 (4/13). Control: 16. Exp: 16. Age (years): 15-25 | Patients who need to extract 1st premolars and maxillary canine retraction | MOPs: 3 MOPs (with a depth of 7 mm) were applied using Propel (through the buccal mucosa of the extraction site) | MOPs: the technique was repeated one month after the first MOP in the Exp Group | 6 months or until the completion of the canine retraction | Primary outcome: RTM (mm/month), molar anchorage loss, canine angulation |
Table 4. (Continuation of Table 3): Additional Characteristics of the included studies (appliance and anchorage used, orthodontic adjustments, statistical outcomes, and methods of primary outcome measurements).
TADs: temporary anchorage devices; SS: stainless steel; U3: upper canines; L3: lower canines; TPA: trans-palatal arch: RTM; rate of tooth movement; TTM: time of tooth movement; MOPs: micro-osteoperforations; LLLT: low-level laser therapy; 5-PLS: 5-point Likert scale; VAS: visual analog scale; IOPA: intraoral periapical radiographs
| Authors (Year, Country) | Appliance characteristics | Anchorage used | Orthodontic adjustments | Statistical significance of reported outcomes | Methods of primary outcome measurements |
| Primary and secondary outcomes | |||||
| Multiple methods of acceleration (two or more different methods of acceleration) | |||||
| Abdelhameed and Refai, 2018, Minya, Egypt [34] | MBT prescription brackets + NiTi closed-coil springs (150 g) for retraction U3 | TADs between 5 and 6 | Every two weeks | RTM (mm/week): 2nd, 4th, and 6th week: (MOPs) p-value = 0.000 8th, 10th, 12th week: (MOPs) p-value = 0.001 2nd, 4th, 6th, 8th, 10th, 12th week: (LLLT) p-value = 0.001 2nd, 4th, 6th, 8th, 10th, 12th week: (MOPs and LLLT) p-value = 0.000 2nd week: MOPs: 1.3 ± 0.12/LLLT: 0.98 ± 0.27/MOPs and LLLT: 1.82 ± 0.19 4th week: MOPs: 2.16 ± 0.27/LLLT: 1.81 ± 0.39/MOPs and LLLT: 2.83 ± 0.12 6th week: MOPs: 2.92 ± 0.73/LLLT: 2.38 ± 0.27/MOPs and LLLT: 3.46 ± 0.64 8th week: MOPs: 3.43 ± 0.66/LLLT: 2.63 ± 0.87/MOPs and LLLT: 3.86 ± 0.27 10th week: MOPs: 3.92 ± 0.88/LLLT: 3.26 ± 0.89/MOPs and LLLT: 4.39 ± 0.73 12th week: MOPs: 4.33 ± 0.64/LLLT: 3.72 ± 0.71/MOPs and LLLT: 4.87 ± 0.88 | Direct intraoral measurements using a digital intraoral caliper |
| Farid et al., 2019, Cairo, Egypt [36] | Roth prescription brackets + 0.017 x 0.025-inch SS + NiTi closed-coil springs (150 g) for retraction U3 | Soldered TPA | Every two weeks | RTM (mm/week): 1stmonth: p-value = 0.019 Corticotomy + LLLT: 0.81 ± 0.58, Corticotomy: 1.16± 0.67 2nd month: p-value = 0.064 Corticotomy + LLLT: 1.04 ± 0.61, Corticotomy: 0.82 ± 0.36 3rdmonth: p-value = 0.968 corticotomy + LLLT: 1.83 ± 1.00, Corticotomy: 2.01 ± 1.37 4thmonth: p-value = 0.033 Corticotomy + LLLT: 1.43 ± 1.18, Corticotomy: 0.83± 1.03 | Measurements were done using 3D-scanned study models |
| Yousif et al., 2019, Tanta, Egypt [16] | Roth prescription brackets + 0.016 x 0.022-inch SS + elastomeric chain for retraction U3, giving force (150 g) that was replaced every three days | Soldered TPA | Every week | TTM (days): p-value = 0.001 MOPs: 11.0 ± 2.36 Corticotomy + MOPs: 15.2 ± 1.62 Control: 8.1 ± 1.90 Canine angular changes: p-value = 0.001 Multiple osteoperforations: 11.0 ± 2.36 corticotomy + multiple osteoperforations: 67.7 ± 3.09 Control: 110.5 ± 4.84 Acceleration rate: multiple osteoperforations, corticotomy + multiple osteoperforations accelerated the canine retraction by 22%, 38.5%, respectively | Direct intraoral measurements using a digital intra-oral caliper. Canine angulation was assessed by panoramic radiography |
| Repetition of an acceleration method | |||||
| Sivarajan et al., 2019, Kuala Lumpur, Malaysia [38] | MBT prescription brackets (0.022x 0.028-inch slot) + 0.018 x 0.025-inch SS + elastomeric chain (140-200 g) for retraction U3 and L3 | TADs between 5 and 6 | Every month | RTM (mm/4 months): p-value = 0.004 MOP-4: 3.96 ± 1.71 MOP-8: 4.15 ± 1.71 MOP-12: 4.39 ± 1.78 Control: 3.06 ± 1.64 Pain and its impact on daily function: MOP-4: 3.96 ± 1.71 moderate (score 2/5), 60% of patients severe (score 3/5), 15% of patients MOP-8: 1.35 ± 0.59 mild (score 1/5), 70% of patients MOP-12: 1.3 0± 0.57 mild (score 1/5), 75% of patients | Direct intraoral measurements using a digital intraoral caliper. Pain intensity was assessed by 5-PLS, whereas VAS was used to assess its impact |
| Asif et al., 2020, Kuala Lumpur, Malaysia [35] | MBT prescription brackets (0.022 x 0.028-inch slot) + 0.018 x 0.025-inch SS + elastomeric chain (140-200 g) for retraction L3 | TADs between 5 and 6 | Every month | RTM (mm/3 months): p-value:<0.001 MOP: 4.03 ± 0.79, Control: 2.77 ± 0.79 p-value = 0.001 MOP-4: 4.57 ± 0.77, Control: 3.08 ± 0.77 p-value = 0.006 MOP-8: 3.06 ± 0.60, Control: 1.94 ± 0.60 p-value = 0.004 MOP-12: 4.17 ± 0.92, Control: 3.03 ± 0.92 | Direct intraoral measurements using a digital intraoral caliper |
| Jaiswal et al., 2021, New Delhi, India [37] | Roth prescription brackets (0.022 slot) + 0.019 x 0.025-inch SS + NiTi closed-coil springs (150g) for retraction U3 | TADs between 5 and 6 | Every month | RTM (mm/month): 1stmonth: p-value = 0.840 One-time MOP: 1.37 ± 0.43, Two-time MOP: 1.41 ± 0.43 2nd month: p-value<0.001 One-time MOP: 2.40 ± 0.52, Two-time MOP: 3.20 ± 0.64 3rdmonth: p-value<0.001 One-time MOP: 3.31 ± 0.87, Two-time MOP: 4.68 ± 1.01 6th month: p-value<0.001 One-time MOP: 4.57 ± 0.54, Two-time MOP: 6.12 ± 0.76 Canine angular changes: p-value = 0.001 1st month: p-value = 0.907 One-time MOP: 97.13 ± 9.2, Two-time MOP: 97.13 ± 8.7 2ndmonth: p-value = 0.889 One-time MOP: 96.31 ± 9.09, Two-time MOP: 95.88 ± 8.56 3rdmonth: p-value = 0.727 One-time MOP: 95.13 ± 8.90, Two-time MOP: 94.06 ± 8.11 Molar anchorage loss: p-value = 0.657 One-time MOP: 0.31 ± 0.24, Two-time MOP: 0.30 ± 0.39 | Measurements were done using 3D scanned study models. Canine angulation was assessed by IOPA |
Table 5. Protocols of the ongoing studies registered at the WHO ICTRP.
WHO ICTRP: World Health Organization International Clinical Trials Registry Platform; RCT: Randomized controlled trial, U3: upper canine, NR: not reported; TTM: time of tooth movement; RTM: rate of tooth movement
| Study ID | Trial name or title | Study design | Intervention + treatment comparison | Sample size/age/gender | Outcomes |
| CTRI/2018/07/015109 | Effectiveness of combined piezocision and low-level laser therapy in reducing orthodontic treatment duration and patient discomfort: A randomized controlled trial | RCT | Piezocision and low-level laser therapy versus conventional orthodontic treatment | 17/NR/NR | Primary outcomes: TTM. Secondary outcomes: the analgesic effect of low-level laser therapy following piezocision |
| CTRI/2020/04/024453 | Effectiveness of piezocision-assisted corticotomy and low-level laser therapy in enhancing rapid maxillary canine retraction: A randomized controlled trial | RCT | Piezocision-assisted corticotomy versus low-level Laser therapy (LLLT) versus LLLT and piezocision versus control | 40/NR/NR | Primary outcomes: RTM. Secondary outcomes: molar anchorage loss, the periodontal index for the U3, and canine vitality and root resorption |
Table 6. Additional characteristics of the protocols of ongoing studies.
NR: not reported; U3: upper canine, LLLT: low-level laser therapy
| Study ID | Setting | Orthodontic aspects | Technical aspects of interventions | Notes |
| CTRI/2018/07/015109 | Department of Orthodontics and Dentofacial Orthopaedics, Manipal College of Dental Sciences, India | Baseline Characteristics: subjects requiring maxillary canine retraction following 1st premolar extraction as a part of their treatment plan. Subjects with permanent dentition. No prior H/o orthodontic treatment | Piezocision: two vertical cuts mesial and distal of the U3, 5-8 mm long, 3mm deep, and sutured if necessary. LLLT: a semiconductor (GaAs) diode with a wavelength of 980 nm, and total energy of 2.5 J, for the 10 points along the root of the maxillary canine | This study is currently in Phase 3. Starting date: 01-08-2018. Completion date: NR |
| CTRI/2020/04/024453 | Department of Orthodontics and Dentofacial Orthopedics, Teerthankar Mahaveer, Moradabad, India | Baseline Characteristics: patients requiring first upper premolars extraction and two-step retraction technique. Complete permanent dentition (except third molars). No previous orthodontic treatment. Healthy patients without systemic diseases that can affect bone and tooth movement. Good oral hygiene and healthy periodontium, which will be evaluated clinically | NR | This study is not yet recruiting. Starting date: 15-04-2020. Completion date: NR |
Six completed RCTs [16,34-38], with a total of 152 patients, with ages ranging from 15 to 25 years, were included in this SR. One study included only female patients [36], three studies did not give information about sex distribution [16,34,35], while the other two studies included both genders, with a predominance of females [37,38]. Four of the involved studies were of a compound design (COMP) [a parallel-group design with a split-mouth design (SMD) in each group] [16,34,35,38], and the others were of SMD [36,37]. Three studies touched on the multiplicity of acceleration methods. Two of them combined LLLT and surgical interventions (MOPs, corticotomy) [34,36]. In one paper, the authors evaluated LLLT + MOPs versus each of these techniques separately [34], whereas, in the other study, only the comparison between LLLT + corticotomy versus corticotomy was performed [36]. Moreover, the third study combined multiple osteoperforation with a corticotomy procedure against multiple osteoperforation only [16]. On the other hand, the other three studies [35,37,38] discussed the efficacy of repeating the acceleration procedures. All three papers dealt with the repetition of MOPs at different time intervals. The surgical interventions in the retrieved studies ranged from invasive (traditional corticotomy [16,36], multiple osteoperforation with flap elevation [16]) to minimally invasive (MOPs [34,35,37,38]).
All the included studies [16,34-38] involved extraction‑based treatments and were primarily about accelerating canine retraction. Four papers studied the upper canines retraction [16,34,36,37], one studied the distalization of both upper and lower canines [38], and one trial assessed the retraction of lower canines [35]. The retraction was performed on canines after the first premolar extraction, which was performed before the beginning of orthodontic treatment in two papers [34,37], and after the completion of leveling and alignment in two trials [16,36], while this information was not mentioned in the other studies [35,38].
Measurement of tooth movement was expressed as RTM in five papers [34-38], and as TTM in one paper [16]. Four studies depended on temporary anchorage devices (TADs) [34,35,37 38], whereas the other studies used soldered trans-palatal arch for anchorage [16,36]. Concerning the method used to measure the speed of tooth movement, there were differences between the trials. Four of the included studies used digital intraoral caliper [16,34,35,38], whereas the others conducted the measurements using 3D-scanned study models [36,37]. Follow-ups varied between three months [34,35], to four months [36,38], and till the completion of canine retraction [16,37].
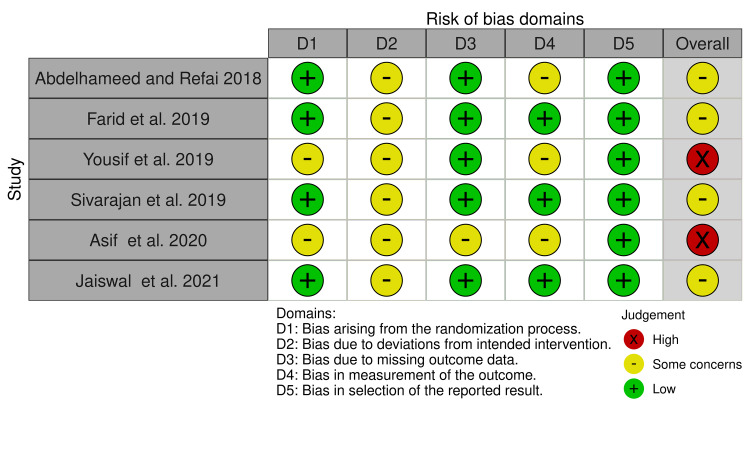
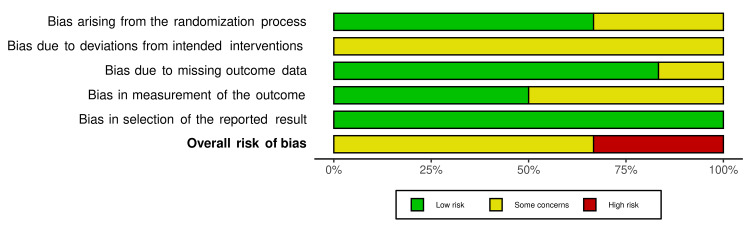
Risk of bias of the included studies
The risk of bias of the included trials is demonstrated in Figure 2, while Figure 3 shows the overall risk of bias for each field. More details about the assessment of the bias risk with supporting reasons for every assessment can be found in Table 7. Four of the included studies [34,36-38] were assessed as "some concern of bias", but the other two trials [16,35] were at 'high risk of bias". Bias due to deviations from intended interventions (effect of assignment to intervention or effect of adhering to intervention) and bias in the measurement of the outcomes were the most questionable domains (100% of some concern of bias in all studies, and 50% in three studies, respectively).
Table 7. Risk of bias assessment according to RoB 2 tool.
RoB 2: Cochrane risk-of-bias tool for randomized trials
| Study | Bias arising from the randomization process | Bias due to deviations from intended interventions | Bias due to missing outcome data | Bias in measurement of the outcome | Bias in selection of the reported results | |
| Effect of assignment to interventions | Effect of adhering to interventions | |||||
| Abdelhameed and Refai, 2018 [34] | Low risk: "assignment of patients and the sides of interventions were performed as follows: computer-generated random numbers were done using Microsoft Office Excel 2013 sheet". (Page 2181) | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "no information" on whether the important non-protocol interventions were balanced across intervention groups | Low risk: "during the study, there was one dropout patient in Group C. Also, there were some missing appointments which were all recorded as follows: Group (A), two missing patient appointments at the 4th, and 10th weeks. Group (B), one missing patient appointment in the 10th week. Group (C), no missing patient appointments but there was one dropout patient as mentioned previously". (Page 2182). "Nearly all" the outcome data is available. | Some concerns: the method of measuring the outcome is appropriate but the outcome assessor was not blind for the assignment of each intervention. "Data for the evaluation of each intervention were collected by direct intraoral measurements using a digital intraoral caliper". (Page 2182) | Low risk: the numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
| Farid et al., 2019 [36] | Low risk: "random numbers were generated on a computer using Microsoft Office Excel 2007 sheet by a person who was not involved in the clinical trial (MA). The concealed allocation was performed by using a set of random numbers placed in sealed opaque envelopes. Each patient picked up a number that would represent the intervention side (laser + corticotomy) performed either on the RT side or the LT side and thus the opposing number would be the comparator side (corticotomy only). By calling FS who was accessible to the random table, the intervention which will be performed either on the LT or the RT side was revealed. At the time of intervention, the subject was allowed to choose one of the envelopes to detect her number in the randomization sequence and thus detect which was the intervention side". (Page 276) | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "no information" on whether the important non-protocol interventions were balanced across intervention groups | Low risk: "all patients had successfully completed the four months duration of the study except for 3 dropout patients who did not continue the follow-up visits at the beginning of leveling and alignment phase of the orthodontic treatment that was substituted by another 3 patients who were fulfilling the same inclusion criteria of the study." "During the course of the study, there were no losses in the pre-intervention or in the final records derived from the dental models. No dropout visits were recorded regarding the monthly impression visits. As for laser visits, nine patients missed their appointments in the third and fourth months that was recorded by date and was replaced by another consecutive visit." (Page 279) | Low risk: the method of measuring the outcome is appropriate and the outcome assessor was blind for the assignment of each intervention. "Three-dimensional digital models were obtained by scanning the sequential stone models using a surface laser scanner. The incremental rate of canine retraction was then measured using a 3-shape program". (Page 278). "Landmark identification was done through two blinded assessors (NA and AN) and an average of their measurements was considered for the statistical analysis". (Page 279) | Low risk: The numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
| Yousif et al., 2019 [16] | Some concerns: the method used for randomization was not reported. “A randomized split-mouth clinical multi-operator study was performed on 30 orthodontic patients". "Subjects were randomized equally into three canine retraction groups" | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "no information" on whether the important non-protocol interventions were balanced across intervention groups | Low risk: "no information" on whether the outcome available for all, or nearly all, participants, and probably the result was not biased by missing outcome data. "Study was carried out to overcome attrition bias (patient dropout) due to poor oral hygiene or bad patient compliances" (Page 3223) | Some concerns: the method of measuring the outcome is appropriate but the outcome assessor was not blind for the assignment of each intervention. "The distance between the distal surface of the canine and the mesial surface of the second premolar was recorded directly in patient’s mouth every week using a caliper with 0.01-mm scale". (Page 3226) | Low risk: the numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
| Sivarajan et al., 2019 [38] | Low risk: "randomized block sampling was carried out using RANDOM.ORG online software to allocate participants into three intervention groups on a 1:1:1 basis". (Page 185) | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "No information" on whether the important non-protocol interventions were balanced across intervention groups | Low risk: "thirty subjects were enrolled into the study between September 2014 and March 2016 with data collection complete by March 2017 and no dropouts". (Page 186). "All" the outcome data is available | Low risk: "the distance from the central point of the canine bracket to the superior margin of the mini implant (maxilla) and the inferior margin of the mini implant (mandible) and the distance from the canine cusp tip to the mesiobuccal groove of the first molar was clinically measured using electric digital calipers (accurate to 0.01 mm)". (Page 185). "The outcome measurements were also blinded". (Page 185). The method of measuring the outcome is appropriate and the outcome assessor was blind for the assignment of intervention | Low risk: the numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
| Asif et al., 2020 [35] | Some concerns: the method used for randomization was not reported. "This study was a single-center, single-blind, prospective randomized split-mouth clinical trial". (Page 580) | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "No information" on whether the important non-protocol interventions were balanced across intervention groups | Some concerns: 6 patients (2 from MOP 4-weeks Group and 4 from MOP 8-weeks Group) were dropouts. The reasons are illustrated in Figure 4 (consort flow diagram). (Page 583) | Some concerns: "the distance of canine movement was recorded every 4 weeks with digital calipers accurate to 0.01 mm, for 12 weeks". (Page 581). “Two observers (orthodontic postgraduate students) were blinded to the frequency of MOP while analyzing the BV/TV ratio using CT analyzer software as CBCT files were labeled by random numbers". (Page 581). The method of measuring the outcome is appropriate, but there is "no information" on whether the outcome assessor was blind to the assignment of each intervention | Low risk: the numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
| Jaiswal et al., 2021 [37] | Low risk: "random numbers were generated in the permuted random block size of 2 using the Research Randomizer software (Research Randomizer, Version 4, Urbaniak GC and Plous S) by the investigator AJ. The numbers were concealed in opaque envelopes and kept in a box. Each patient was then asked to pick a sealed envelope to assign the second MOP to either the right or left side, executed separately without any role of primary clinical investigators, shuffled every time before picking". (Page 417) | Some concerns: blinding cannot be performed. There is "no information" on whether any deviations arose because of the trial context | Some concerns: blinding cannot be performed. And "No information" on whether the important non-protocol interventions were balanced across intervention groups | Low risk: "one patient was excluded after intervention owing to miniscrew implant failure". (Page 418). "Nearly all" outcome data is available | Low risk: “the models were scanned with Maestro 3D scanner (MDS 400, AGE solutions S.r.l., Pisa, Italy) with an accuracy of 0.01 mm to obtain digital models. These digital models were imported in Dolphin 3D software (Version 11.9, Patterson Inc., Chatsworth, CA) and the baseline (T0) model was superimposed on T30, T60, T90, and T180 day models with medial 2/3rd of third rugae as the reference point". (Page 417). “However, the extracted data was coded during collection and analysis to ensure blinding". (Page 417). The method of measuring the outcome is appropriate and the outcome assessor was blind to the assignment of each intervention | Low risk: the numerical result being assessed has not probably been selected, based on the results, from multiple eligible outcome measurements within the outcome domain and analyses of the data. The eligible reported results for the outcome corresponded to the intended outcome measurements |
Figure 2. Risk of bias summary of RCTs.
+ sign: low risk of bias; - sign: some concern of bias; X sign: high risk of bias
RCTs: randomized controlled trials
Figure 3. The overall risk of bias score for each field of RCTs.
RCTs: randomized controlled trials
Effects of interventions
Primary outcomes: first theme: multiple methods of acceleration
Combining LLLT With a Surgical Intervention Against the Application of Each Technique Separately
Abdelhameed and Refai [34] estimated the impact of combined LLLT + MOPs versus the impact of the application of each technique separately on the RTM in a three-arm compound-design RCT. When comparing the accelerated sides with the non-accelerated sides, MOPs and LLLT, as well as MOPs + LLLT interventions, showed an increased rate of upper canine retraction. Statistically significant differences were found at all assessment times (p<0.05). On the other hand, the combination of ' MOPs + LLLT was found to be superior to the single application of MOPs or LLLT separately. According to GRADE, the overall quality of evidence supporting this outcome is low (Table 8). The mean rate of canine retraction in the MOPs + LLLT side was the highest in the first, second, and third months (x ®= 2.83 ± 0.12 mm, x ®= 3.86 ± 0.27 mm, x ®= 4.87 ± 0.88 mm, respectively). Moreover, In the first, second, and third months, the mean rate of canine movement in MOPs side (x ®= 2.16 ± 0.27 mm, x ®= 3.43 ± 0.66 mm, x ®= 4.33 ± 0.64 mm, respectively) was significantly greater than the LLLT side (x ®= 1.81 ± 0.39 mm, x ®= 2.63 ± 0.87 mm, x ®= 3.72 ± 0.71 mm, respectively). The MOPs technique accelerated the canine retraction rate by 1.6 fold whereas LLLT achieved this by 1.3 fold compared with the non-accelerated sides. Nevertheless, the combination of MOPs + LLLT gained priority by increasing the canine retraction rate by 1.8 fold compared with the non-accelerated side.
Table 8. Summary of findings according to the GRADE guidelines for the included trials.
High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate
CI: confidence interval; SP: split-mouth design; COMP: compound design; LLLT: low-level laser therapy MOPs: micro-osteoperforations
a, bDecline in one level for risk of bias (bias due to deviations from intended interventions [35,38], bias arising from the randomization process, bias in the measurement of the outcome, and bias in the measurement of the outcome [35]), one level for indirectness**, and one level for imprecision***
c, h, jDecline in one level for risk of bias (bias due to deviations from intended interventions), one level for imprecision*** [37]
dDecline in one level for risk of bias (bias due to deviations from intended interventions, bias in the measurement of the outcome), one level for indirectness**, and one level for imprecision*** [35]
e, gDecline in one level for risk of bias (bias due to deviations from intended interventions), one level for imprecision*** [36]
f, gDecline in one level for risk of bias (bias arising from the randomization process, bias due to deviations from intended interventions, bias in the measurement of the outcome), one level for indirectness**, and one level for imprecision [16]
*Differences in results; **Outcome is not directly related; ***Limited number of trials
| Quality assessment criteria | Summary of findings | Comments | ||||||||
| Number of studies | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Number of patients | Effects | Certainty | ||
| Absolute (95% CI) | Relative (95% CI) | |||||||||
| Rate of canine retraction accelerated by multiple MOPs (every 4 weeks versus every 8 weeks) | ||||||||||
| 2 RCTs (COMP) | Serious | Not serious | Serious | Serious | None | 34 | - | Relative effect (95% CI): MD 0.24 (-0.28-0.77) | Very low ⊕⊖⊖⊖a | |
| Rate of canine retraction accelerated by multiple MOPs (every 4 weeks versus every 12 weeks) | ||||||||||
| 2 RCTs (COMP) | Serious | Not serious | Serious | Serious | None | 40 | - | Relative effect (95% CI): MD 0.06 (-0.14-0.27) | Very low ⊕⊖⊖⊖b | |
| Rate of canine retraction accelerated by multiple MOPs (2 times versus 1 time) | ||||||||||
| 1 RCT (SP) | Serious | Not serious | Not serious | Serious | None | 16 | - | Relative effect (95% CI): not estimable | Low ⊕⊕⊖⊖c | Application two-time MOP was more efficient than the one-time MOP (p<0.001) |
| Rate of upper canine retraction accelerated by combined techniques and a single application of technique | ||||||||||
| 1 RCT (COMP) | Serious | Not serious | Serious | Serious | None | 30 | - | Relative effect (95% CI): not estimable | Very low ⊕⊖⊖⊖d | The combination of MOPs + LLLT is superior to the application of each technique separately |
| 1 RCT (SP) | Serious | Not serious | Not serious | Serious | None | 16 | - | Relative effect (95% CI): not estimable | Low ⊕⊕⊖⊖e | The combination of corticotomy + LLLT was not more efficient than the application of corticotomy only |
| Time of upper canine retraction accelerated by combined techniques and a single application of technique | ||||||||||
| 1 RCT (COMP) | Serious | Not serious | Serious | Serious | None | 30 | - | Relative effect (95% CI): not estimable | Very low ⊕⊖⊖⊖f | Canine retraction took more time in multiple osteoperforations side than multiple osteoperforations + corticotomy side |
| Adverse effects: anchorage loss | ||||||||||
| 1 RCT (SP) | Serious | Not serious | Not serious | Serious | None | 16 | - | Relative effect (95% CI): not estimable | Low ⊕⊕⊖⊖g | Anchorage loss was greater on the corticotomy side than on the LLLT + corticotomy side |
| 1 RCT (SP) | Serious | Not serious | Not serious | Serious | None | 16 | - | Relative effect (95% CI): not estimable | Low ⊕⊕⊖⊖h | There was an insignificant difference in loss of anchorage between the one-time MOP side and the side of the two-time MOP (p<0.05) |
| Adverse effects: canine angulation | ||||||||||
| 1 RCT (COMP) | Serious | Not serious | Serious | Serious | None | 30 | - | Relative effect (95% CI): not estimable | Very low ⊕⊖⊖⊖i | Distal tipping and buccal inclination of canine were greater in the multiple osteoperforation + corticotomy side than the multiple osteoperforation side |
| 1 RCT (SP) | Serious | Not serious | Not serious | Serious | None | 16 | - | Relative effect (95% CI): not estimable | Low ⊕⊕⊖⊖j | There was an insignificant difference in canine tipping between the one-time MOP side and the side of the two-time MOP (p<0.05) |
Combining LLLT With a Surgical intervention Against a Single Application of the Latter
Farid et al. [36] evaluated the combined effect of LLLT + corticotomy versus corticotomy only on the RTM in a split-mouth RCT. In the first month of upper canine retraction, the results were opposite of what was expected. The mean rate of canine movement was greater in corticotomy only side (x ®= 1.16± 0.67 mm) compared with the LLLT + corticotomy side (x ®= 0.81± 0.58 mm) with a statistically significant difference (p = 0.019). Conversely, the mean rate of canine movement in the fourth month was greater in the LLLT + corticotomy side (x ®= 1.43± 1.18 mm) than corticotomy only side (x ®= 0.83± 1.03 mm) with a statistically significant difference (p = 0.033). However, there was no statistically significant difference between the sides of LLLT + corticotomy and corticotomy only regarding the rate of upper canine retraction in the second and third months (p = 0.064, p = 0.968), respectively. The high heterogeneity between the previous studies [34,36] did not allow for conduct quantitative synthesis of the findings.
Combining Two Different Surgical Interventions Against a Single Application of One of Them
The clinical trial by Yousif et al. [16] evaluated the effect of the combined multiple osteoperforation + corticotomy procedure against multiple osteoperforation on TTM in a three-arm compound-design RCT. The multiple osteoperforation side required less than three months (x ®= 85.1 ± 3.03 days) for the completion of canine retraction, whereas the multiple osteoperforation + corticotomy side took about two months only (x ®= 67.7 ± 3.09 days) to complete this procedure, with a statistically significant difference between the two sides (p = 0.001). According to GRADE, the overall quality of evidence supporting this outcome is low (Table 8). The canine retraction was accelerated by 22% for the multiple osteoperforation side and 38.5% for the multiple osteoperforation + corticotomy side. Due to the use of a different outcome variable between this study and the previous, the meta-analyses were not performed.
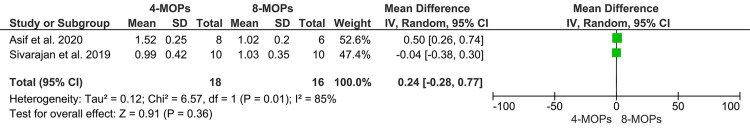
Second theme: repetition of an acceleration method
Three of the included studies assessed the repetition of acceleration procedures. Moreover, all of these studies focused on the reapplication of MOPs [35,37,38]. Sivarajan et al. [38] and Asif et al. [35] in a three-arm compound-design RCT evaluated the effect of multiple intervals of MOPs (every four, eight, or 12 weeks in groups 1, 2, and 3 respectively) on the RTM. The pooled estimate showed that there was no statistically significant difference between the four-week MOPs group (three times of application) and the eight-week MOPs group (two times of application) in the rate of canine retraction in one month (MD = 0.24; 95% CI: -0.28-0.77; p = 0.36, Figure 4). Heterogeneity between the two studies was high (χ2 = 6.57; p = 0.01; I2 = 85%). Also, the MD of 0.06 was found (95% CI: -0.14-0.27; p = 0.55, Figure 5) between the four-week MOPs group and the 12-week MOPs group, which was not statistically significant, with low heterogeneity (χ2 = 1.01; p = 0.31; I2 = 1%). According to GRADE, the overall quality of the evidence supporting this outcome is very low (Table 8).
Jaiswal et al. [37] compared the efficacy of two-time MOPs versus one-time application on the RTM in an SMD RCT. In the first month of canine retraction, no significant differences were found between the two sides of the mouth (x ®= 1.37 ± 0.0.43 mm and x ®= 1.41 ± 0.43 mm, respectively; p = 0.840). On the contrary, the overall canine retraction rate was statistically greater in the two-time MOPs side than the one-time side (x ®= 6.12±0.76 mm and x ®= 4.57 ± 0.54 mm, respectively; p<0.001). According to GRADE, the overall quality of the evidence supporting this outcome is low (Table 8). The difference in the repetition intervals between this study and the other two studies prevented its inclusion in the meta-analysis.
Figure 4. Forest plot of the comparison between the four-weekly MOPs and eight-weekly MOPs of canine retraction in one month.
MOP: micro-osteoperforation; CI: confidence interval
Figure 5. Forest plot of the comparison between the four-weekly MOPs and 12-weekly MOPs of canine retraction in one month.
MOP: micro-osteoperforation; CI: confidence interval
Secondary outcomes
The overall quality of evidence according to GRADE for secondary outcomes is illustrated in Table 8.
Secondary Outcomes Associated With Multiple Methods of Acceleration (Two or More Different Methods of Acceleration)
Two of the included papers in this hub [16,36] evaluated secondary outcomes. Farid et al. [36] assessed molar anchorage loss between the groups of corticotomy + LLLT and corticotomy only. The MD of anchorage loss was greater in the corticotomy only side than the corticotomy + LLLT side (MD: 0.46 ± 2.81 mm). However, this difference was statistically insignificant. Yousif et al. [16] evaluated pain and discomfort between the combined multiple osteoperforation + corticotomy side against the multiple osteoperforation side. No pain and discomfort were reported in both groups. Yousif et al. [16] also assessed canine angulation and inclination. They found that the mean canine angulation changes were greater in the multiple osteoperforation + corticotomy side (x ®= 15.2° ± 1.65°) compared to the multiple osteoperforation side (x ®= 11.0° ± 2.36°) with a statistically significant difference (p = 0.001). Moreover, the distal inclination of the canine was also greater in the multiple osteoperforation + corticotomy side compared to the multiple osteoperforation side with a statistically significant difference (p = 0.001). We could not pool the results of the secondary outcomes to quantitative synthesis due to the use of a different outcome variable between trials.
Secondary Outcomes Associated With Repetition of an Acceleration Method
Two studies in this hub [37,38] discussed the associated secondary outcomes. Sivarajan et al. [38] evaluated the pain and its impact on daily function between the multiple intervals of MOPs (every four, eight, and 12 weeks). Pain associated with MOP was reported in all groups. However, 60% of the MOP-4 patients' group reported moderate pain, with the highest mean pain score (x ®= 1.75 ± 0.72). Moreover, 70% of the MOP-8 patients' group and 75% of the MOP-12 patients' group reported only mild pain with a similar mean pain score (x ®= 1.35 ± 0.59 and x ®= 1.30 ± 0.57, respectively). The impact of this reported pain on daily function centered on speech and chewing; without any statistically significant effect on general activities, like mood and social interaction (p>0.05). Jaiswal et al. [37] estimated molar anchorage loss as well as canine angulation between one-time MOP and two-time MOP sides. Regarding the molar anchorage loss, a statistically insignificant difference (p = 0.657) was found between the one-time MOP side (0.31 ± 0.24 mm) and the side of the two-time MOP (0.30 ± 0.39 mm). Moreover, the canine tipping also demonstrated a statistically insignificant difference in the overall canine retraction intervals (p>0.05), which was 2° in the one-time MOP side and 3° in the two-time MOP. We could not pool the results of the secondary outcomes to quantitative synthesis due to the use of a different outcome variable between trials.
The Strength of the Evidence According to the GRADE Guidelines for the Included Trials
As per the GRADE recommendations, the evidence strength regarding the rate of orthodontics tooth movement as well as the adverse effects ranged from very low to low, as shown in Table 8. The decline in the evidence strength happened because of the risk of bias [16,34-38], indirectness [16,34,35,38], and imprecision [16,34-38].
Discussion
Acceleration of OTM has become a trend in the orthodontic field in recent decades. In the beginning, the trend was to assess the effectiveness of the methods used for OTM acceleration. Subsequently, some clinical trials have been conducted to evaluate the effectiveness of combining two methods or more or repeating a specific method to accelerate the OTM. This approach has not been widely accepted among orthodontic practitioners, and the effectiveness of this combination or repetition is still not known with any certainty.
First theme: multiple methods of acceleration
Unfortunately, the results of the two studies [34,36], which focused on the combination of LLLT with surgical intervention versus a single application of one of them, were contradictory. Abdelhameed and Refai [34] concluded that a combination of MOPs + LLLT achieved a synergistic effect with superior accelerated tooth movement compared to the sole application of each technique. On the contrary, Farid et al. [36] found that the combination of corticotomy + LLLT was not more efficient than the single application of corticotomy only in accelerating canine retraction. The dissimilarity in the findings could be attributed to the fact that the interventions were applied using different protocols. Abdelhameed and Refai [34] applied LLLT from the buccal and palatal surfaces along the root of the canines in addition to the application of MOPs six times over a period of three months, whereas in Farid et al.'s trial [36], the LLLT was applied at the middle point of the canine root on buccal and palatal surfaces, and the corticotomy procedure was performed only once. As mentioned before, the high heterogeneity between the previous studies [34, 6] did not allow for quantitative synthesis of the findings.
However, Yousif et al. [16], who compared the combination of two different surgical interventions against a single application of one of them, reported that the combination outperformed the single surgical technique group as the mean TTM was less in the combination group (67.7 ± 3.09 days) compared to the single-procedure group (85.1 ± 3.03 days). One possible explanation could be the synergistic effect of two surgical techniques with an increased RAP, i.e., increased cortical bone porosity with increased osteoclastic activity following the surgical healing of the cortical bone [39]. On the other hand, the combination of two surgical interventions (corticotomy + MOPs) reduced the treatment duration by 42.8%. This is superior to the acceleration of canine retraction with the MOPs only, which reduced the treatment duration by 25.4% when compared to conventional retraction. This is somewhat consistent with a previous trial, which suggested a possible reduction in the treatment duration of up to 30% [38]. Although surgical methods have been proven to be effective in accelerating OTM [24], different acceleration rates have been published in the literature. A study evaluating traditional corticotomy (with flap elevation) reported that canine retraction increased by two to four times when compared to the non-accelerated group [5], whereas a laser-assisted flapless corticotomy accelerated the canine retraction by 2.5 times when compared to the conventional retraction [40]. On the other hand, flapless piezocision-based corticotomy accelerated canine retraction by 1.5-2 times when compared to the non-accelerated group [2], whereas the application of MOPs produced OTM that was 2.3 times faster than the conventional retraction [41].
Second theme: repetition of an acceleration method
The results of the meta-analysis indicated that the rate of OTM was almost the same after repeated application of MOPs by three times (every four weeks) and two times (every eight or 12 weeks), as shown in Figures 4, 5. However, Jaiswal et al. [37] found the RTM was statistically greater in the two-time MOP side when compared with the one-time MOP side. The previous results could be explained by understanding the mechanism of RAP and the purpose of repeating the acceleration procedures. RAP is a transient phenomenon, beginning a few days after surgery, reaching its highest point at one to two months, and then declining over time [42]. Here is where the role of the repetition of intervention to ensure a continuous activation of the RAP biological response becomes important [43]. Since the purpose of the repetition is the same, which is to re-evoke the RAP and maintain the accelerated OTM, this could be the reason why there is no difference between repetition by two or three times.
The associated secondary outcomes
Considering the associated side effects, the anchorage loss was assessed in two trials, which concluded the same result. Farid et al. [36] found a statistically insignificant difference between the single acceleration method side (corticotomy) and the combined methods side (LLLT + corticotomy). Additionally, Jaiswal et al. [37] demonstrated that anchorage loss did not differ statistically between the sides of one-time MOP and two-time MOP. This could be attributed to the fact that the accelerating interventions were applied topically, leading to localized alveolar response without affecting the posterior segments, and hence anchorage loss did not differ between the two sides of the intervention.
Canine angulation was investigated in two studies. Yousif et al. [16] reported that more distal tipping and more buccal inclination of the canine were shown in the combined acceleration method side (multiple osteoperforation + corticotomy) than the single-method side (multiple osteoperforation). This result can be explained by understanding the biomechanical mechanism. It is known that in sliding techniques, an initial crown tipping is induced first, followed by root uprighting later [44]. The faster the OTM is done, the more tipping of the crown will occur. On the contrary, Jaiswal et al. [37] indicated that the canine tipping was minimal, with non-significant differences between the two sides of one-time MOP and two-time MOP. This can be attributed to the use of a rigid 0.019 x 0.025 stainless steel wire with a closed-coil spring for canine retraction. It is known that rectangular archwire provides good control for tipping during canine sliding; however, the looseness of the archwire fits in the bracket slot and causes a certain degree of tipping [45,46]. Although no important side effects were found in the included three studies, data on periodontal complications, postoperative infection, root resorption, tooth vitality loss, and possible morbidity are not available in the retrieved studies and further research is required.
Limitations of the current review
Only six RCTs (three studies in each theme), which fulfilled the eligibility criteria, were found and included in this SR; four of them were assessed to have some concern of bias, whereas the other two trials were at high risk of bias. The strength of evidence ranged from very low to low. Therefore, there is a need for high-quality RCTs to assess the value of multiplicity or repetition in orthodontic acceleration. Canine retraction following premolar extraction was carried out in all included studies. We could not find trials evaluating acceleration in different treatment strategies such as decrowding of upper and lower teeth, incisors’ retraction or intrusion, and en-masse retraction of anterior teeth. The high heterogeneity and the use of different outcome measures as well as treatment protocols prevented the inclusion of all of the retrieved studies in a meta-analysis and the results of only two studies were pooled. Not all included studies evaluated the side effects associated with the acceleration techniques. Moreover, the studied side effects reported were limited. Therefore, it was difficult to arrive at clear conclusions regarding the accompanying negative effects.
Conclusions
The combination of LLLT with a surgical technique seemed to outperform the application of each technique separately when accelerating tooth movement. The combination of two surgical interventions may produce a synergistic effect leading to a reduced treatment time compared to the application of a single surgical intervention. The quality of evidence of previous conclusions was very low. The double application of surgical procedures appears to be more effective than the single application but the quality of evidence in this aspect is low. As the strength of evidence of the reported results ranged from low to very low, we confirm the need for more well‑conducted RCTs evaluating the benefits of combining several acceleration techniques throughout the treatment procedure or repeating specific methods in comparison with the single application. Future research should also consider the broad spectrum of possible side effects accompanying multiple or repeated applications.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Effectiveness of minimally invasive surgical procedures in the acceleration of tooth movement: a systematic review and meta-analysis. Alfawal AM, Hajeer MY, Ajaj MA, Hamadah O, Brad B. Prog Orthod. 2016;17:33. doi: 10.1186/s40510-016-0146-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evaluation of piezocision and laser-assisted flapless corticotomy in the acceleration of canine retraction: a randomized controlled trial. Alfawal AM, Hajeer MY, Ajaj MA, Hamadah O, Brad B. Head Face Med. 2018;14:4. doi: 10.1186/s13005-018-0161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evaluation of the effectiveness of piezocision-assisted flapless corticotomy in the retraction of four upper incisors: a randomized controlled clinical trial. Al-Imam GM, Ajaj MA, Hajeer MY, Al-Mdalal Y, Almashaal E. Dent Med Probl. 2019;56:385–394. doi: 10.17219/dmp/110432. [DOI] [PubMed] [Google Scholar]
- 4.Attractiveness, acceptability, and value of orthodontic appliances. Rosvall MD, Fields HW, Ziuchkovski J, Rosenstiel SF, Johnston WM. Am J Orthod Dentofacial Orthop. 2009;135:276–212. doi: 10.1016/j.ajodo.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? A split-mouth design randomized controlled trial. Al-Naoum F, Hajeer MY, Al-Jundi A. J Oral Maxillofac Surg. 2014;72:1880–1889. doi: 10.1016/j.joms.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Efficacy of surgical and non-surgical interventions on accelerating orthodontic tooth movement: a systematic review. Kalemaj Z, DebernardI CL, Buti J. http://www.quintpub.com/journals/ejoi/full_txt_pdf_alert.php?article_id=15230&ref=/journals/ejoi/journal_contents.php?iss_id=12944ZZ5journal_name=EJOI4ZZ5vol_year=20154ZZ5vol_num=8. Eur J Oral Implantol. 2015;8:9–24. [PubMed] [Google Scholar]
- 7.The clinical application of prostaglandin E1 on orthodontic tooth movement - a clinical trial. Patil AK, Keluskar K, Gaitonde S. J Indian Orthod Soc. 2005;39:91–98. [Google Scholar]
- 8.Evaluation of the influence of local administration of vitamin D on the rate of orthodontic tooth movement. Iosub Ciur MD, Zetu IN, Haba D, Viennot S, Bourgeois D, Andrian S. https://pubmed.ncbi.nlm.nih.gov/30148332/ Rev Med Chir Soc Med Nat Iasi. 2016;120:694–699. [PubMed] [Google Scholar]
- 9.Local and chronic application of PTH accelerates tooth movement in rats. Soma S, Matsumoto S, Higuchi Y, Takano-Yamamoto T, Yamashita K, Kurisu K, Iwamoto M. J Dent Res. 2000;79:1717–1724. doi: 10.1177/00220345000790091301. [DOI] [PubMed] [Google Scholar]
- 10.A randomized, placebo-controlled clinical trial on the effects of recombinant human relaxin on tooth movement and short-term stability. McGorray SP, Dolce C, Kramer S, Stewart D, Wheeler TT. Am J Orthod Dentofacial Orthop. 2012;141:196–203. doi: 10.1016/j.ajodo.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 11.Acceleration of tooth movement during orthodontic treatment--a frontier in orthodontics. Nimeri G, Kau CH, Abou-Kheir NS, Corona R. Prog Orthod. 2013;14:42. doi: 10.1186/2196-1042-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Effectiveness of low-level laser therapy in reducing orthodontic pain: a systematic review and meta-analysis. Deana NF, Zaror C, Sandoval P, Alves N. Pain Res Manag. 2017;2017:8560652. doi: 10.1155/2017/8560652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: a randomized controlled clinical trial. AlSayed Hasan MM, Sultan K, Hamadah O. Angle Orthod. 2017;87:499–504. doi: 10.2319/062716-503.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The effectiveness of traditional corticotomy vs flapless corticotomy in miniscrew-supported en-masse retraction of maxillary anterior teeth in patients with Class II Division 1 malocclusion: a single-centered, randomized controlled clinical trial. Khlef HN, Hajeer MY, Ajaj MA, Heshmeh O, Youssef N, Mahaini L. Am J Orthod Dentofacial Orthop. 2020;158:0–20. doi: 10.1016/j.ajodo.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 15.The effect of using a modified dentoalveolar distractor on canine angulation following rapid canine retraction: a split-mouth design randomized controlled trial. Al-Ainawi KI, Al-Mdalal Y, Hajeer MY. J Contemp Dent Pract. 2016;17:49–57. doi: 10.5005/jp-journals-10024-1802. [DOI] [PubMed] [Google Scholar]
- 16.Accelerated canine retraction by corticotomy assisted or periodontal distraction. Yousif AAA, Abo-Taha NF, Essa EF. Egypt Dent J. 2019;65:3221–3231. [Google Scholar]
- 17.Interseptal bone reduction on the rate of maxillary canine retraction. Leethanakul C, Kanokkulchai S, Pongpanich S, Leepong N, Charoemratrote C. Angle Orthod. 2014;84:839–845. doi: 10.2319/100613-737.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Periodontally accelerated osteogenic non-extraction orthodontics versus conventional extraction-based orthodontics in dental decrowding: a randomized controlled trial. Al-Naoum F, Alsabbagh R, Aljundi A. https://journals.usj.edu.lb/iajd/article/view/197 Int Arab J Dent. 2015;6:9–19. [Google Scholar]
- 19.Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: a randomized controlled trial. Gibreal O, Hajeer MY, Brad B. Eur J Orthod. 2019;41:188–195. doi: 10.1093/ejo/cjy042. [DOI] [PubMed] [Google Scholar]
- 20.Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding-a randomized clinical trial. Uribe F, Davoody L, Mehr R, et al. Eur J Orthod. 2017;39:595–600. doi: 10.1093/ejo/cjw091. [DOI] [PubMed] [Google Scholar]
- 21.Effect of micro-osteoperforation on the rate of canine retraction: a split-mouth randomized controlled trial. Aboalnaga AA, Salah Fayed MM, El-Ashmawi NA, Soliman SA. Prog Orthod. 2019;20:21. doi: 10.1186/s40510-019-0274-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The regional acceleratory phenomenon: a review. Frost HM. https://scholarlycommons.henryford.com/hfhmedjournal/vol31/iss1/2/ Henry Ford Hosp Med J. 1983;31:3–9. [PubMed] [Google Scholar]
- 23.Efficacy and safety of different interventions to accelerate maxillary canine retraction following premolar extraction: a systematic review and network meta-analysis. MacDonald L, Zanjir M, Laghapour Lighvan N, da Costa BR, Suri S, Azarpazhooh A. Orthod Craniofac Res. 2021;24:17–38. doi: 10.1111/ocr.12409. [DOI] [PubMed] [Google Scholar]
- 24.The effectiveness of surgical adjunctive procedures in the acceleration of orthodontic tooth movement: a systematic review of systematic reviews and meta-analysis. Mheissen S, Khan H, Alsafadi AS, Almuzian M. J Orthod. 2021;48:156–171. doi: 10.1177/1465312520988735. [DOI] [PubMed] [Google Scholar]
- 25.Effect of micro-osteoperforation on the rate of orthodontic tooth movement-a systematic review and a meta-analysis. Shahabee M, Shafaee H, Abtahi M, Rangrazi A, Bardideh E. Eur J Orthod. 2020;42:211–221. doi: 10.1093/ejo/cjz049. [DOI] [PubMed] [Google Scholar]
- 26.The effect of low-level laser therapy on the acceleration of orthodontic tooth movement. Baghizadeh Fini M, Olyaee P, Homayouni A. J Lasers Med Sci. 2020;11:204–211. doi: 10.34172/jlms.2020.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The effectiveness of locally injected platelet-rich plasma on orthodontic tooth movement acceleration. Li Z, Zhou J, Chen S. Angle Orthod. 2021;91:391–398. doi: 10.2319/061320-544.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The effect of single/multiple micro-osteoperforation on the rate of orthodontic tooth movement and its possible complications: a systematic review and meta-analysis. Mohaghegh S, Soleimani M, Kouhestani F, Motamedian SR. Int Orthod. 2021;19:183–196. doi: 10.1016/j.ortho.2021.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Cochrane Database Syst Rev. 2019;10:0. doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Liberati A, Altman DG, Tetzlaff J, et al. BMJ. 2009;339:0. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Moher D, Liberati A, Tetzlaff J, Altman DG. Ann Intern Med. 2009;151:264–269. [PMC free article] [PubMed] [Google Scholar]
- 32.RoB 2: a revised tool for assessing risk of bias in randomised trials. Sterne JA, Savović J, Page MJ, et al. BMJ. 2019;366:0. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 33.GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. Guyatt GH, Thorlund K, Oxman AD, et al. J Clin Epidemiol. 2013;66:173–183. doi: 10.1016/j.jclinepi.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 34.Evaluation of the effect of combined low energy laser application and micro-osteoperforations versus the effect of application of each technique separately on the rate of orthodontic tooth movement. Abdelhameed AN, Refai WM. Open Access Maced J Med Sci. 2018;6:2180–2185. doi: 10.3889/oamjms.2018.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osseous evidence behind micro-osteoperforation technique in accelerating orthodontic tooth movement: a 3-month study. Asif MK, Ibrahim N, Sivarajan S, Heng Khiang Teh N, Chek Wey M. Am J Orthod Dentofacial Orthop. 2020;158:579–586. doi: 10.1016/j.ajodo.2019.09.022. [DOI] [PubMed] [Google Scholar]
- 36.The effect of combined corticotomy and low level laser therapy on the rate of orthodontic tooth movement: split mouth randomized clinical trial. Farid KA, Eid AA, Kaddah MA, Elsharaby FA. Laser Ther. 2019;28:275–283. doi: 10.5978/islsm.19-OR-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Comparison of the efficacy of two-time versus one-time micro-osteoperforation on maxillary canine retraction in orthodontic patients: a split-mouth randomized controlled clinical trial. Jaiswal AA, Siddiqui HP, Samrit VD, Duggal R, Kharbanda OP, Rajeswari MR. Int Orthod. 2021;19:415–424. doi: 10.1016/j.ortho.2021.06.003. [DOI] [PubMed] [Google Scholar]
- 38.Mini-implant supported canine retraction with micro-osteoperforation: a split-mouth randomized clinical trial. Sivarajan S, Doss JG, Papageorgiou SN, Cobourne MT, Wey MC. Angle Orthod. 2019;89:183–189. doi: 10.2319/011518-47.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Wilcko WM, Wilcko MT, Bouquot J, Ferguson DJ. http://www.quintpub.com/userhome/prd/prd_21_1_wilcko1.pdf. Int J Periodontics Restorative Dent. 2001;21:9–20. [PubMed] [Google Scholar]
- 40.Evaluation of the efficacy of laser-assisted flapless corticotomy in accelerating canine retraction: a split-mouth randomized controlled clinical trial. Jaber ST, Al-Sabbagh R, Hajeer MY. Oral Maxillofac Surg. 2022;26:81–89. doi: 10.1007/s10006-021-00963-x. [DOI] [PubMed] [Google Scholar]
- 41.Effect of micro-osteoperforations on the rate of tooth movement. Alikhani M, Raptis M, Zoldan B, et al. Am J Orthod Dentofacial Orthop. 2013;144:639–648. doi: 10.1016/j.ajodo.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 42.Periodontal accelerated osteogenic orthodontics: a description of the surgical technique. Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ. J Oral Maxillofac Surg. 2009;67:2160–2166. doi: 10.1016/j.joms.2009.04.124. [DOI] [PubMed] [Google Scholar]
- 43.Piezocision-assisted orthodontic treatment using CAD/CAM customized orthodontic appliances: a randomized controlled trial in adults. Charavet C, Lecloux G, Jackers N, Albert A, Lambert F. Eur J Orthod. 2019;41:495–501. doi: 10.1093/ejo/cjy082. [DOI] [PubMed] [Google Scholar]
- 44.Nanda R, Ghosh J. Biomechanics in Clinical Orthodontics. Vol. 1. Philadelphia, PA: Saunders; 1997. Biomechanical considerations in sliding mechanics; pp. 188–217. [Google Scholar]
- 45.Ireland AJ, McDonald F. The orthodontic patient: treatment and biomechanics: Oxford University Press. Vol. 181. Oxford, UK: Oxford University Press; 2003. The Orthodontic Patient: Treatment and Biomechanics; p. 182. [Google Scholar]
- 46.The effects of friction and flexural rigidity of the archwire on canine movement in sliding mechanics: a numerical simulation with a 3-dimensional finite element method. Kojima Y, Fukui H, Miyajima K. Am J Orthod Dentofacial Orthop. 2006;130:275. doi: 10.1016/j.ajodo.2006.02.030. [DOI] [PubMed] [Google Scholar]