Summary
Background
The COVID-19 pandemic has disproportionately impacted the most vulnerable and widened the health disparity gap in both physical and mental well-being. Consequentially, it is vital to understand how to best support elderly individuals, particularly Black Americans and people of low socioeconomic status, in navigating stressful situations during the COVID-19 pandemic and beyond. The aim of this study was to investigate perceived levels of stress, posttraumatic growth, coping strategies, socioeconomic status, and mental health between Black and non-Hispanic, White older adults, the majority over the age of 70. Additionally, we investigated which variables, if any, were associated with posttraumatic growth in these populations.
Methods
One hundred seventy-six community dwelling older adults (mean age = 76.30 ±8.94), part of two observational studies (The Harvard Aging Brain Study and Instrumental Activities of Daily Living Study) in Massachusetts, US, were included in this cross-sectional study. The survey, conducted from March 23, 2021 to May 13, 2021, measured perceived stress, behavioral coping strategies, posttraumatic growth, and mental health during the COVID-19 pandemic. We investigated associations with post-traumatic growth in a multiple linear regression model and examined their differences by race with t-tests, Wilcoxon rank-sum tests, and Fisher's exact tests. A second multiple linear regression model was used to examine which coping strategies were associated with posttraumatic growth.
Findings
Our results indicated no significant difference between the groups in terms of mental health or stress. However, Black participants showed significantly greater posttraumatic growth compared to non-Hispanic, White participants. Additionally, the coping strategies of religion and positive reframing were found to be significantly associated with posttraumatic growth. Furthermore, even with the effects of stress and coping strategies controlled for, race remained significantly associated with posttraumatic growth.
Interpretation
The COVID-19 pandemic has differentially impacted Black and non-Hispanic White older adults. These results may help encourage further analysis on geriatric psychiatry as well as understanding how cultural values and adaptations impact posttraumatic growth and mental health in diverse populations.
Funding
The Harvard Aging Brain Study (HABS) has been funded by NIH-NIA P01 AG036694 (PI: Reisa Sperling). The IADL study is funded by the National Institute on Aging (R01 AG053184, PI: Gad A. Marshall).
Keywords: Aging, Posttraumatic growth, Pandemic, Geriatrics, COVID-19, Coping strategies, Socioeconomic status, Race, Stress, Religion, Mental health
Abbreviations: PTG, Post-Traumatic Growth; SES, Socioeconomic Status; PSS, Percieved Stress Scale; BCI, Brief Cope Inventory; PROMIS, Patient-Reported Outcomes Measurement Information System
Research In Context.
Evidence before this study
Prior to the COVID-19 pandemic, multiple studies examined posttraumatic growth and the relationship between race, socioeconomic status, and coping mechanisms. We searched PubMed using the terms “COVID posttraumatic growth”, “race posttraumatic growth”, “disparities in posttraumatic growth”, “coping strategies posttraumatic growth”, “stress posttraumatic growth”, and “older adults posttraumatic growth”. However, there is a paucity of studies on elderly populations as well as posttraumatic growth during the pandemic, and no study examines these variables during the COVID-19 pandemic in a cohort largely consistent of older adults over the age of 70.
Added value of this study
To our knowledge, this is the first study to evaluate differences in perceived stress, coping strategies, posttraumatic growth, socioeconomic status, and mental health during the COVID-19 pandemic between Black and non-Hispanic, White older adults, largely over 70. In particular, this study found that race and certain coping strategies are independently associated with posttraumatic growth.
Implications of all the available evidence
Our findings provide insight on a rarely studied age group that is particularly vulnerable to the SARS-CoV-2 infection. The findings suggest that race and the use of religion and positive reframing are independently associated with posttraumatic growth in older adults. Understanding the variables that contribute to posttraumatic growth may provide insight for therapeutic approaches that emphasize the impact of race, socioeconomic status, and systemic oppression for mental health professionals.
Alt-text: Unlabelled box
Introduction
The coronavirus (COVID-19) pandemic is a global public health crisis that has inflicted major stress, particularly on the elderly, communities of color, and people of low-income status. In the USA, there have been over 36 million COVID-19 cases and more than 620,000 deaths, of which nearly 80% were among people over the age of 65.1 According to the Center for Disease Control and Prevention (CDC), the pandemic has had devastating effects on Black persons as they are nearly 3 times more likely to be hospitalized and 2 times more likely to die from COVID-19 compared to non-Hispanic, White persons.2 Additionally, Black and low-income patients were twice as likely to test positive for COVID-19 compared to non-Hispanic, White, and High-income patients.3 These vulnerable groups are placed at higher risk of developing severe complications due to their older age, comorbidities, substandard housing, accessibility to healthcare, financial inequities, and racial and systemic discrimination.
The COVID-19 pandemic represents for many, an ongoing set of stressful circumstances such as contracting the virus, sensationalism by mass media, witnessing death or suffering, social isolation, financial difficulties, and food insecurities. Thus, one might consider that the pandemic period itself has comprised a heterogeneous set of experiences that may contribute to the incidence and severity of stress-related disorders.4 Interestingly, Bridgland and colleagues5 reported that the pandemic can be understood as a traumatic stressor event capable of eliciting posttraumatic stress disorder-like responses. Importantly there is also evidence suggesting that some individuals can experience positive change from trauma, termed as posttraumatic growth,6 further defined as a “positive psychological change experienced as a result of the struggle with highly challenging life circumstances”.7 Previous research has shown that the experience of positive growth in the face of adversity usually manifests in a variety of ways, including an increased appreciation for life, more meaningful interpersonal relationships, and a heightened sense of personal strength and spirituality.7 Posttraumatic growth has also been found in many cultures and religions,6, 7, 8, 9 and has been shown to be related to coping skills and social support,10,11 as well as sociodemographic variables.12, 13, 14 In the context of the COVID-19 pandemic, a recent study found that age had a significant effect on posttraumatic growth, such that younger age was related to greater growth.15 These results are similar to previous studies that have shown that younger people experience more posttraumatic growth compared to older people,6 although it should be noted that studies on groups with average ages over 70 are rare.6,12 Given that older individuals have a greater vulnerability to COVID-19, the findings by Celdran and colleagues suggest that older adults may have perceived the event as more fearful than the younger individuals, thereby reducing the appearance of posttraumatic growth during this period.15 However, more studies in the oldest generation are needed to understand more deeply the mechanisms that might generate posttraumatic growth in older adults.
In line with that, previous studies have implicated that race and socioeconomic status may be associated with posttraumatic growth. For instance, in a study by Helgeson and colleagues, the authors reported that underrepresented groups were more likely to experience positive effects following trauma.14 Moreover, in a previous study investigating low-income mothers who survived Hurricane Katrina, researchers found that Black mothers reported significantly higher levels of both posttraumatic stress and posttraumatic growth compared to non-Hispanic, White mothers.16 Both studies hypothesized that this could be due to the greater adversity systematically oppressed groups face. Furthermore, in a study on posttraumatic growth and sociodemographic factors in Chinese breast cancer survivors, high education levels and household incomes were both shown to positively influence posttraumatic growth.17 Wang and Lu similarly reported an association between household income with posttraumatic growth in Chinese American breast cancer survivors.18 These studies highlight the importance of considering race and socioeconomic status when evaluating posttraumatic growth.
Although positive outcomes on mental health with posttraumatic growth have shown varied results,9,11 the COVID-19 pandemic has increased the incidence of mental illnesses.19 Furthermore, vulnerable groups such as the elderly, people of low income, and historically oppressed racial groups have been disproportionately affected as the health disparity gap was further exacerbated. Ettman and colleagues found that individuals with lower social economic resources, lower social resources, and greater exposure to stressors such as job loss experienced more depressive symptoms.20 Prior to the pandemic, in the US, studies have shown that Black Americans tend to report higher levels of psychological distress than non-Hispanic, White Americans.21 Additionally, despite having similar rates of mental illness to non-Hispanic, White Americans, Black Americans receive less mental health treatment, are more likely to be incorrectly diagnosed, and when they do seek treatment, it is usually because of severe mental illness requiring hospitalization.21,22
Consequentially, understanding stress, mental health, coping strategies, and posttraumatic growth in the context of the COVID-19 pandemic may be critical to understanding how to best support individuals navigating stressful situations. These strategies must take into consideration vulnerable groups and social determinants of health to ensure optimal healthcare intervention. Therefore, this study aimed to investigate perceived levels of stress, behavioral coping strategies, posttraumatic growth, socioeconomic status, and mental health between Black and non-Hispanic, White persons, with a majority over the age of 70 during the pandemic. Additionally, we investigated variables associated with posttraumatic growth. Finally, we examined what coping strategies, if any, were associated with posttraumatic growth in these populations.
Methods
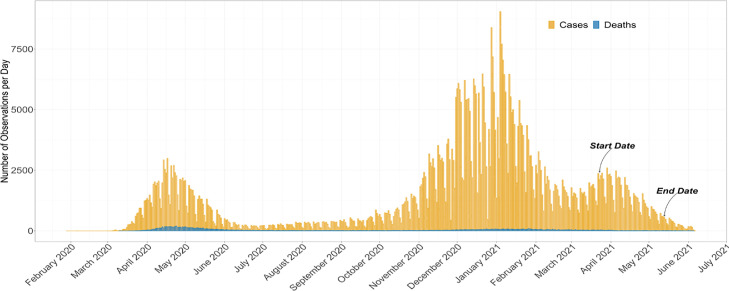
This cross-sectional study is based on data collected from a survey that ran from March 23, 2021 until May 13, 2021. This is the second survey of a series of sub-studies in study participants who were actively enrolled in 2 longitudinal observational research studies of older adults in Massachusetts, US; the Harvard Aging Brain Study (HABS, P01 AG036694, PI: Sperling and Johnson) or the Instrumental Activities of Daily Living Study (IADL, R01 AG053184, PI: Marshall). The time window of the survey and its relationship to observed cases and deaths in Massachusetts are illustrated in Figure 1. HABS is comprised of approximately 300 participants, of which 254 were actively enrolled at the time of the study. The participants in HABS were all cognitively normal at baseline and have been evaluated longitudinally with multi-modal neuroimaging and extensive clinical evaluations. IADL is a natural history, non-interventional imaging 3-year study of older adult individuals who were either cognitively normal or had a diagnosis of amnestic mild cognitive impairment at the time of enrollment. The study is actively enrolling participants and at the time of this study it was comprised of 45 individuals. To assess clinical diagnosis, a group of 6–7 experienced clinicians holds recurrent consensus meetings to evaluate whether a participant is cognitively normal or meets criteria for either mild cognitive impairment or Alzheimer's Disease dementia (using similar criteria to those of the Alzheimer's Disease Neuroimaging Initiative (ADNI)). All actively enrolled participants were eligible for the survey. However, study invitation was only sent to participants with a listed email address and those who had not previously opted out of consideration for sub-studies. The main outcome of the first survey including details of the study design and recruitment procedures has been published previously.23
Figure 1.
The time window of the survey start date (March 23, 2021) and end date (May 26, 2021) as well as its relationship to observed cases and reported deaths per day in Massachusetts between February 2020 and July 2021. Data source: https://www.mass.gov.
In brief, participants were sent an invitation to participate via electronic mail (e-mail), which provided them with the study context, a link to access the online consent form, and the subsequent survey via Research Electronic Data Capture (REDCap).24, 25, 26 REDCap is a web-based software platform designed to securely build, manage, and support data capture for research studies both offline and online. REDCap provides 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages, and 4) procedures for data integration and interoperability with external sources. Survey completion was voluntary, and participants were instructed that they could skip questions or stop at any time. A total of 193 out of 277 invited participants consented to the survey, of which 10 non-Black, non-White individuals were excluded, and 7 persons were excluded due to incomplete data. Of the remaining 176, 16 individuals were Black and 160 were non-Hispanic white. Socioeconomic status (SES) was determined using the 2-factor Hollingshead, which measures education and occupation status.27 The Hollingshead score ranges from 11-77, with higher values indicating lower SES. The participants’ demographics are summarized in Table 1. We found no significant differences in demographics between our sample and the total cohort of invited participants. However, when comparing respondents to non-respondents, we found a significantly higher proportion of Black individuals among non-respondents (see Supplemental Table 1).
Table 1.
Mean/SD/Median of Demographics, PTG Domains, Perceived Stress Scale, and 14 Brief Cope Inventory Strategies
| All |
Black |
White NH |
Welch T-Test |
Wilcoxon Rank Sum Test |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | Mean | SD | Median | Mean | SD | Median | Mean | SD | df | t | p | p (adj) | W | p | p (adj) | |
| Age | 76.75 | 76.3 | 8.94 | 75.5 | 73.12 | 9.26 | 76.88 | 76.62 | 8.87 | 17.87 | -1.45 | .17 | .28 | 1005.5 | .16 | .28 |
| Years of Education | 16.5 | 16.43 | 2.58 | 16 | 14.81 | 3.02 | 17.5 | 16.59 | 2.49 | 17.1 | -2.29 | .04* | .08 | 864 | .03* | .07 |
| Hollingshead Score | 18 | 24.02 | 13.09 | 23.5 | 32.56 | 17.87 | 18 | 23.16 | 12.27 | 16.44 | 2.06 | .06 | .11 | 1702.5 | .03* | .07 |
| PROMIS Mental Health | 50.8 | 51.17 | 8.68 | 50.8 | 49.55 | 9.74 | 50.8 | 51.33 | 8.59 | 17.41 | -0.7 | .49 | .61 | 1185 | .63 | .71 |
| PTG Total | 46 | 47.95 | 24.48 | 70 | 69.75 | 20.2 | 45 | 45.77 | 23.84 | 19.43 | 4.45 | <.001*** | .003** | 1989 | <.001*** | .003** |
| PTG Relating to Others | 2.43 | 2.45 | 1.23 | 3.5 | 3.33 | 0.99 | 2.29 | 2.36 | 1.22 | 19.89 | 3.64 | .002** | .008** | 1864.5 | .003** | .011* |
| PTG New Possibilities | 1.8 | 2 | 1.24 | 3 | 3.04 | 1.13 | 1.7 | 1.9 | 1.2 | 18.54 | 3.82 | .001** | .008** | 1934 | <.001*** | .007** |
| PTG Personal Strength | 2.5 | 2.48 | 1.34 | 3.88 | 3.52 | 1.22 | 2.38 | 2.37 | 1.31 | 18.6 | 3.54 | .002** | .01** | 1890.5 | .002** | .008** |
| PTG Spiritual Change | 1 | 1.55 | 1.67 | 4 | 3.5 | 1.63 | 0.5 | 1.36 | 1.55 | 17.8 | 5.03 | <.001*** | .002** | 2104 | <.001*** | <.001*** |
| PTG Appreciation of Life | 2.67 | 2.59 | 1.28 | 3.33 | 3.4 | 0.9 | 2.67 | 2.51 | 1.29 | 21.79 | 3.6 | .002** | .008** | 1770 | .01* | .04* |
| PSS | 14 | 14.9 | 8.49 | 13.5 | 14.02 | 9.69 | 14 | 14.99 | 8.39 | 17.32 | -0.38 | .71 | .73 | 1204 | .70 | .73 |
| BCI Self Distraction | 1.5 | 1.44 | 0.82 | 1 | 1.03 | 0.74 | 1.5 | 1.48 | 0.82 | 18.86 | -2.29 | .03* | .08 | 880 | .04* | .08 |
| BCI Active Coping | 2 | 1.72 | 0.83 | 1.5 | 1.5 | 0.89 | 2 | 1.74 | 0.82 | 17.6 | -1.03 | .32 | .43 | 1098 | .34 | .46 |
| BCI Denial | 0 | 0.22 | 0.43 | 0 | 0.38 | 0.59 | 0 | 0.21 | 0.41 | 16.5 | 1.09 | .29 | .41 | 1455.5 | .25 | .36 |
| BCI Substance Use | 0 | 0.22 | 0.51 | 0 | 0.09 | 0.38 | 0 | 0.24 | 0.53 | 21.4 | -1.4 | .18 | .28 | 1093 | .17 | .28 |
| BCI Emotional Support | 1.5 | 1.5 | 0.89 | 0.75 | 0.91 | 0.95 | 1.5 | 1.56 | 0.87 | 17.59 | -2.64 | .02* | .05 | 770 | .008** | .03* |
| BCI Instrumental Support | 1 | 1.04 | 0.77 | 0.5 | 0.81 | 0.75 | 1 | 1.06 | 0.77 | 18.32 | -1.25 | .23 | .34 | 1026 | .18 | .28 |
| BCI Behavioral Disengagement | 0 | 0.23 | 0.45 | 0 | 0.22 | 0.45 | 0 | 0.23 | 0.45 | 18.21 | -0.06 | .95 | .95 | 1257 | .88 | .90 |
| BCI Venting | 1 | 0.9 | 0.66 | 1 | 1.03 | 0.88 | 1 | 0.88 | 0.64 | 16.61 | 0.65 | .53 | .63 | 1369 | .64 | .71 |
| BCI Positive Reframing | 1.5 | 1.41 | 0.88 | 1.25 | 1.22 | 0.84 | 1.5 | 1.43 | 0.88 | 18.51 | -0.95 | .35 | .46 | 1120.5 | .41 | .52 |
| BCI Planning | 1.5 | 1.46 | 0.94 | 0.75 | 0.94 | 0.93 | 1.5 | 1.51 | 0.92 | 18.1 | -2.36 | .03* | .07 | 860 | .03* | .07 |
| BCI Humor | 2 | 1.8 | 0.81 | 1.5 | 1.44 | 0.87 | 2 | 1.83 | 0.8 | 17.63 | -1.75 | .10 | .18 | 937 | .07 | .14 |
| BCI Acceptance | 2.5 | 2.11 | 0.89 | 1.75 | 1.53 | 1.02 | 2.5 | 2.17 | 0.86 | 17.18 | -2.39 | .03* | .07 | 806 | .01* | .04* |
| BCI Religion | 0.5 | 1 | 1.05 | 2 | 1.84 | 0.93 | 0.5 | 0.91 | 1.03 | 18.92 | 3.79 | .001** | .008** | 1920 | <.001*** | .007** |
| BCI Self-Blame | 0.5 | 0.6 | 0.7 | 0.5 | 0.53 | 0.74 | 0.5 | 0.61 | 0.7 | 17.79 | -0.39 | .70 | .73 | 1186 | .61 | .71 |
| All | Black | White NH | Fisher's Exact Test | |||||||||||||
| N | % | N | % | N | % | p | p (adj) | |||||||||
| Sex | .06 | .12 | ||||||||||||||
| F | 102 | 58% | 13 | 81% | 89 | 56% | ||||||||||
| M | 74 | 42% | 3 | 19% | 71 | 44% | ||||||||||
| Knew Someone Diagnosed with COVID | .53 | .63 | ||||||||||||||
| False | 39 | 22% | 2 | 12% | 37 | 23% | ||||||||||
| True | 135 | 77% | 14 | 88% | 121 | 76% | ||||||||||
| No Response | 2 | 1% | 0 | 0% | 2 | 1% | ||||||||||
| Race | ||||||||||||||||
| Black | 16 | 9% | ||||||||||||||
| Non-Hispanic White | 160 | 91% | ||||||||||||||
The reporting of this study conforms to the STROBE statement.
Ethical Considerations
The study was approved by the Massachusetts General Brigham Human Research Review Board. All participants provided informed consent to the study.
Survey components
The survey consisted of several questionnaires which are presented in detail below.
Questions estimating the level of perceived stress
Perceived stress was measured using the Perceived Stress Scale (PSS-14); which consists of a 14-item questionnaire that assesses the degree to which situations in a person's life are appraised as stressful.28 The questions are framed to ask about feelings and thoughts during the last month, such as “in the last month, have you felt that you were unable to control the important things in your life.” Participants select a response for each statement on a 5-point Likert scale, ranging from 0 (never) to 4 (very often). The perceived stress scale (PSS) is computed as the sum of all PSS questions with the appropriate questions' scale reversed. A total score ranging from 0 to 56 was used to measure participants’ level of stress with higher scores indicating increased perceived stress. This tool is classically used to measure perceived stress and has shown validity and good psychometric properties in elderly adults.29 The Cronbach's Alpha value for this scale was α = .92, indicating excellent internal consistency.
Posttraumatic Growth Inventory
Posttraumatic growth (PTG) was assessed with the Posttraumatic Growth Inventory,6 which is a 21-item instrument that measures positive outcomes reported by persons who have experienced traumatic events. Participants were asked to rate the degree to which they experienced the change described by each item. Each question uses a 6-point scale, ranging from 0 (not at all) to 5 (to a very great degree). A total PTG score, computed as the sum of all PTG questions (ranging from 0 – 105) was used in this study. The PTG measure has shown good internal validity and acceptable test-retest reliability.6,30 The 5 subscales consisted of Relating to Others (consisting of 7 items with Cronbach's Alpha value α = .92), New Possibilities (5 items, α = .87), Personal Strength (4 items, α = .87), Spiritual Change (2 items, α = .89), and Appreciation of Life (3 items, α = .76). Cronbach's Alpha for the total PTG score was α = .96.
Mental Health
Mental health was assessed using the Mental Health subscore from the 10-item version of the Patient-Reported Outcomes Measurement Information System (PROMIS).31,32 The PROMIS is an open-access global health questionnaire exploring multiple domains of global health. Previous studies demonstrated good construct validity for this tool, and it has been applied in multiple contexts and pathologies since its development.33 Different dimensions can be extracted, including a mental health sub-score summarizing 4 different items exploring quality of life, mood and thinking ability, social activities, and emotions (e.g., anxiety, depression, irritability). Raw scores are then transformed into standardized T-scores so that the normal average score would be at 50 with a 10-point standard deviation.32 Possible mental health T-scores range from 21.2 to 67.6, where a higher score indicates better mental health. The Cronbach's Alpha value for the mental health subscale was α = .82, indicating good internal consistency.
Coping
The Brief COPE inventory (BCI)34 was administered to measure the use of coping strategies. This measure has shown good reliability and validity.35,36 The scale assesses 14 different coping strategies; active coping, planning, positive reframing, humor, use of emotional support, use of instrumental support, acceptance, religion, self-distraction, denial, substance use, behavioral disengagement, venting, and self-blame; using 2 questions for each strategy for a total of 28 questions. Participants were asked to appraise how often they have used each strategy as it applies to them in this current situation using a 4-point Likert scale. Scores were averaged over each pair of questions for the 14 coping strategies, with a higher score indicating more frequent use of that coping strategy. Cronbach's Alpha ranged between 0.4 to 0.5 for Self-Distraction, Denial, and Venting; between 0.5 and 0.6 for Behavioral Disengagement; between 0.6 and 0.7 for Instrumental Support, Humor, and Self Blame, between 0.7 and 0.8 for Active Coping, Emotional Support, Positive Reframing, and Acceptance; and between 0.8 and 0.9 for Substance Use, Planning, and Religion.
Missing Items
For each of the PSS, BCI, and PTG measures, a threshold of 30% missing values was used as criteria for exclusion. Thus, participants who answered at least 70% of each measure's questions had missing values filled with the survey average for the given question. Following PROMIS scoring guidelines, participants who did not answer all PROMIS mental health questions were excluded. In total, 7 individuals were excluded for insufficient data. Of those, 5 were missing PTG, 1 was missing PSS, 5 were missing PROMIS, and 1 was missing SES information. In addition to substituting missing values, we also ran a complete case analysis which resulted in the same findings. Finally, to examine whether data was missing at random, logistical regression models for each demographic variable of SES, race, age, and sex were run on each questionnaire item to predict whether it was missing or not. We found no differences by SES, age, or sex, but Black respondents had a higher prevalence of missing values for all survey items.
Statistical methods
All statistical analyses were performed using R 4.1.1 (https://www.R-project.org/). We compared participant demographic and psychological measures in the Black versus non-Hispanic, White group using Welch t-tests and non-parametric Wilcoxon Rank-Sum tests for continuous measures and Fisher's exact tests for categorical measures. P-values were adjusted for multiple comparisons using the FDR method. In order to examine the factors contributing to PTG, a hierarchical multiple linear regression model was computed with PTG as the outcome variable and with age, sex, socioeconomic status, race, perceived stress, and coping mechanisms as the predictors. The level 1 model included only the demographic effects of age, sex, race, and SES, while the level 2 model added the psychological factors of perceived stress and coping mechanisms. In both linear models, continuous variables were standardized (z-score transformation) before inclusion, and the conditions of linearity, homoscedasticity of errors, normal distribution of residuals, lack of outliers, and lack of multicollinearity were all confirmed to be met. In addition, a confirmatory matched analysis between the Black and non-Hispanic, White group was performed using a sample matched on age, gender, and SES in predicting PTG.
Role of funding sources
The funding sources had no involvement in the study design, data collection, analysis, or interpretation.
Results
The final sample for this analysis consisted of 176 participants (102 women, 74 men), with a mean age of 76.30 (±8.94) and an average of years of education of 16.43 (±2.59). Of the 176 in total, 147 participants came from the HABS and 29 from the IADL study. Only participants that identified as Black or non-Hispanic, White were used for this analysis, specifically 16 Black and 160 non-Hispanic, White persons.
To better understand the sample characteristics of the participants of the survey we compared the demographic characteristics, that is age, SES, years of education, PSS, PTG, PROMIS, and coping strategies between Black and non-Hispanic, White participants (Table 1). On average, the group of White, non-Hispanic participants was slightly older, more educated, had a higher socioeconomic status, and was comprised of more men than the group of Black participants. However, none of these differences were significant after adjustment for multiple comparisons.
Levels of perceived stress
The mean perceived stress score of the whole cohort as assessed with the PSS-14 questionnaire was 14.9, with S.D. = 8.49, corresponding to low to moderate stress. No statistically significant difference was found for stress between Black respondents and non-Hispanic, White participants (see Table 1).
Coping strategies
The means, medians, and differences between the groups for the 14 coping strategies from the Brief Cope Inventory are presented in Table 1. As these variables are ordinal and not normally distributed, the results from the non-parametric Wilcoxon rank-sum tests are also reported. The most endorsed coping strategy across the whole sample was acceptance (mean = 2.11, median = 2.5). This was the most-endorsed strategy among non-Hispanic, White persons (mean = 2.17, median = 2.5) and the second-most endorsed strategy among Black persons (mean = 1.53, median = 1.75). The difference between groups was statistically significant (p = .04) such that non-Hispanic, White persons endorsed acceptance more than Black persons. For Black persons, religion was the most endorsed coping strategy (mean = 1.84, median = 2) and was significantly different (p < .001) compared to non-Hispanic, White persons (mean = 0.91, median = 0.5). The least endorsed coping strategy among the Black respondents was substance use (mean = 0.09, median = 0), and among the non-Hispanic, White persons, denial (mean = 0.21, median = 0). There was also a significant difference in use of emotional support (p = .03), with non-Hispanic White, persons (mean = 1.56, median = 1.5) endorsing this strategy more than Black persons (mean = 0.91, median = 0.75). Although there was a significant unadjusted difference in self-distraction and planning, with White respondents reporting higher use of each of those strategies, the difference did not survive adjustment for multiple comparisons.
Posttraumatic Growth
Out of a total score of 105, the mean total PTG for the full sample was 47.95 (±24.48). Black respondents had significantly higher total PTG on average (t(19.43) = 4.45, p = .003) with a mean of 69.75 (±20.20) compared to non-Hispanic, White persons with a mean PTG of 45.77 (±23.84). Notably, Black respondents reported significantly higher PTG across each of the 5 subcategories (see Table 1).
Mental Health
PROMIS mental health T-scores ranged between 25.1 and 67.6 in the full cohort, with a mean of 51.2 and a standard deviation of 8.68. There was no statistically significant difference in mental health scores between Black and non-Hispanic, White respondents.
Investigating associations with posttraumatic growth in Black and non-Hispanic, White responders
A hierarchical multiple regression analysis was performed to measure associations with posttraumatic growth and is presented in Table 2. In step 1, age, sex, race, and socioeconomic status were entered as main effects. We found that race was associated with PTG such that Black respondents had significantly higher PTG compared to non-Hispanic, White respondents (β = 0.87, t(171) = 3.34, p = .001). In addition, a confirmatory matched analysis was run. A sample matched on age, sex, and SES was generated using propensity score matching. A simple linear regression model was run with PTG as the outcome variable and race as the only independent variable. Similar to the previous model, this analysis explained a significant proportion of the variance in PTG; R2 = 0.14, F(1, 30) = 5.00, p = 0.03. Race was significantly associated with PTG, β = 0.74, t (30) = 2.24, p = 0.03.
Table 2.
Hierarchical multiple linear regression model predicting posttraumatic growth as a function of perceived stress, race, socioeconomic status, and brief cope inventory.
| Level 1 | |||||
|---|---|---|---|---|---|
| β | t | p | Proportion of Variance | R² | |
| 0.1*** | |||||
| Age | -0.1257 | -1.67 | .096 | 0.029 | |
| Sex (M) | -0.1283 | -0.84 | .401 | 0.009 | |
| Race (Black) | 0.86736 | 3.34 | .001** | 0.065 | |
| Hollingshead Score | 0.04232 | 0.57 | .568 | 0.002 | |
| Level 2 | |||||
| 0.3*** | |||||
| Age | -0.0296 | -0.39 | .694 | 0.029 | |
| Sex (M) | 0.18785 | 1.21 | .229 | 0.009 | |
| Race (Black) | 0.73928 | 2.73 | .007** | 0.065 | |
| Hollingshead Score | 0.0114 | 0.16 | .876 | 0.002 | |
| PSS | -0.0564 | -0.61 | .543 | 0.000 | |
| BCI Self Distraction | 0.08292 | 1.05 | .294 | 0.019 | |
| BCI Active Coping | 0.04068 | 0.41 | .679 | 0.013 | |
| BCI Denial | -0.0304 | -0.39 | .7 | 0.001 | |
| BCI Substance Use | -0.0832 | -1.18 | .24 | 0.013 | |
| BCI Emotional Support | 0.04017 | 0.4 | .689 | 0.005 | |
| BCI Instrumental Support | 0.15512 | 1.57 | .117 | 0.024 | |
| BCI Behavioral Disengagement | 0.01144 | 0.13 | .893 | 0.007 | |
| BCI Venting | -0.0265 | -0.31 | .758 | 0.002 | |
| BCI Positive Reframing | 0.3663 | 3.59 | <.001*** | 0.033 | |
| BCI Planning | -0.143 | -1.32 | .189 | 0.008 | |
| BCI Humor | -0.0704 | -0.75 | .455 | 0.001 | |
| BCI Acceptance | -0.1629 | -1.81 | .073 | 0.023 | |
| BCI Religion | 0.26167 | 3.14 | .002** | 0.045 | |
| BCI Self-Blame | -0.1086 | -1.25 | .212 | 0.007 | |
In step 2, perceived stress and the 14 BCI strategies were added. Race remained significant (β = 0.74, t(156) = 2.73, p = .007) and use of the coping mechanisms of positive reframing (β = 0.37, t(156) = 3.59, p < .001) and religion (β = 0.26, t(156) = 3.14, p = .002) demonstrated significant contribution to higher PTG. The level 1 and level 2 models each explained a significant proportion of the variance in PTG; R2 = 0.11, F(4, 171) = 5.01, p < 0.001, and R2 = 0.30, F(19, 156) = 3.59, p < 0.01, respectively. Due to the sample size, we could not run a confirmatory matched analysis on this step.
Discussion
This study examined differences in perceived levels of stress, stress coping, posttraumatic growth, socioeconomic status, and mental health during the COVID-19 pandemic in a sample of Black and non-Hispanic, White community dwelling older adults living in Massachusetts and neighboring states (U.S.). Additionally, the effects of perceived stress, race, socioeconomic status, and coping strategies on posttraumatic growth were evaluated.
No significant differences for demographic measures were found between the Black respondents and non-Hispanic, White respondents. Perceived stress levels for all participants were low to moderate on average and no statistically significant difference was found between Black and non-Hispanic, White persons. These results are in contrast with the Zaheed and colleagues' study, which analyzed older adults pre-COVID-19 in the Washington Heights-Inwood Colombia Aging project and reported significantly higher levels of perceived stress in Black persons compared to non-Hispanic, White persons.37 Although similar low to moderate stress levels have been reported in studies conducted early in the pandemic, our findings could be interpreted as the pandemic being experienced as a similar stressor for all included in this cohort, despite ethnic and socioeconomic backgrounds.23,38,39 Additionally, the timing of the survey could explain the absence of stress differences as participants were examined more than 1 year following the beginning of the pandemic, vaccine rollouts, and after the 2 waves of peaked cases in Massachusetts. Thus, we can hypothesize that, at the time of the survey, our participants may have had a sufficient amount of time to adjust to the pandemic.
On the PROMIS scale, we observed a mean level of mental health of 51.2 in our participants, slightly above the US population average. We did not find any significant difference between the groups, indicating that mental health was the same across the Black and non-Hispanic, White persons. When analyzing coping strategies, overall, non-Hispanic, White persons significantly endorsed the use of acceptance and emotional support compared to Black persons. However, Black respondents reported the use of religion significantly more than non-Hispanic, White persons. These results were similar to those from the Bautista and colleagues’ study who found that religion was significantly endorsed by Black persons compared to non-Hispanic, White persons.40 However, in that study, for the acceptance strategy, both groups reported similar endorsement and for emotional support and planning strategies, Black persons reported significantly higher usage. The use of acceptance and religion as a coping strategy has been associated with better health-related quality of life.41,42 Denial was the least endorsed coping strategy for non-Hispanic, White persons and substance use was the least endorsed coping strategy for Black respondents. These findings are in line with a previous study investigating stress during the pandemic.43 Additionally, these findings are also similar to our previous publication measuring coping behaviors at the beginning of the pandemic, and some of the participants are overlapping with the current study.23
The mean level of posttraumatic growth for the total cohort was 47.95, with a range between 0 and 105. We found that Black respondents reported significantly higher PTG, both for the total score and the individual subcategories, compared to non-Hispanic, White persons which is similar to other studies comparing Black and White participants during major events.16,44 The highest subdomain reported in the total sample was appreciation of life. However, it is important to acknowledge that t-tests cannot adjust for potential confounding, and thus, these results should be interpreted with caution. In the Calderon and colleagues study on posttraumatic growth in older adults during the pandemic, researchers found that social resources predicted posttraumatic growth.15 However, their study's cohort, study timeline, and research methods were slightly different. Specifically, the average age was younger (mean age 65.99), the study was conducted in May 2020 immediately after the forced lockdown in Spain, and researchers used a short form version of the posttraumatic growth index. In contrast, when assessing posttraumatic growth associations amongst sex, age, and socioeconomic status in our study, race was the only significant independent predictor of posttraumatic growth. When perceived stress and coping strategies were included as additional independent variables, race remained significant, and the coping strategies of positive reframing and religion became significant. These results are similar to other studies where positive reframing and religion were associated with greater posttraumatic growth.45,46 Thus, praying, meditating, and trying to view things in a different and positive manner may be a way to cultivate posttraumatic growth. Moreover, SES was not associated with PTG in our models. These findings are in contrast with the study by Wang and colleagues who found an association between education and household income, and posttraumatic growth in Chinese American breast cancer survivors.18 However, it should be noted that even though we have a wide SES range (range: 11-73, where a higher value indicates lower SES) in our sample, the mean SES was relatively high (mean of 24.02) and might not be representative of the wider population. Thus, future studies are needed to investigate this more in detail.
We acknowledge that there are limitations to our study. First, all the measures were self-reported as this is a self-administered survey, and thus could be influenced by recent events and emotional state. We also did not examine other mental health conditions such as posttraumatic stress disorder, depression, or anxiety. However, in the future, we will be assessing more data on mental health in this cohort as we are continuing to collect these data as part of participants’ regular assessments in our studies. We also acknowledge that the small sample size of our Black respondents, which corresponds to approximately 9% of the study cohort is a limitation, though this is in line with the population demographics of the overall HABS and IADL study cohorts (approximately 14% Black participants, see Supplemental Table 1). Additionally, there was a higher prevalence of missing data among the Black respondents. These factors limit the power of our analysis and the generalizability of our findings. Therefore, we realize these results must be replicated in larger samples. However, of note, in the current study, any missing responses were substituted with the mean across all participants. Thus, any missing responses in the Black participants would have resulted in more resemblance to the White participants, which potentially could make it harder to see a difference between the groups. Despite this, our findings of a significant difference by race strengthen our results and interpretations. In addition, although this study cohort was small, the results were consistent with previous studies, where Black participants reported significantly higher posttraumatic growth.16,44 Furthermore, we acknowledge that this study was a targeted comparison between Black and White research study participants, and as such cannot be extended to other underrepresented populations. Future work should therefore also include data from other underrepresented groups. Given that the participants are all recruited from the same geographic region (Massachusetts and neighboring states), we acknowledge that our findings should be extended into other geographic regions. Lastly, our cross-sectional design makes it difficult to infer causal relationships between the variables examined.
This exploratory study can encourage future research, inform study designs on posttraumatic growth, mental health, and the proposed conceptual framework that focuses on mass group-level posttraumatic growth in the context of historical trauma.47 Historical trauma refers to populations that have been historically subjected to long-term, mass trauma over a life span and across generations. Historical trauma is shared by a group of people, is intergenerational, and has been associated with adverse mental and physical health outcomes.47, 48, 49, 50 Additionally, previous studies have shown that historical trauma connects the history of mass group experienced trauma to present day experiences and health.49 Our study may contribute to this framework as it illustrates the importance of race, which may guide researchers with understanding why underrepresented groups experience more posttraumatic growth.
In conclusion, our findings are consistent with other studies that have shown increased posttraumatic growth in Black Americans compared to non-Hispanic, White Americans. Previous studies have suggested that the findings of increased posttraumatic growth could be due to the greater adversity systematically oppressed groups face. Our findings warrant future research to further investigate social and cultural factors that may relate to posttraumatic growth. It must also be acknowledged that elderly Black persons were able to experience both posttraumatic growth and similar mental health status despite their social inequities, higher risk of poor outcomes from COVID-19, and their minority status, which exposes them to greater vulnerability to discrimination and racism. However, more quantitative research must be done to ensure generalizability, especially in age groups over 70 as well as underrepresented groups. Moreover, the pandemic may have made it tougher for people to utilize various coping outlets. Overall, our findings indicate that religion and positive reframing were 2 coping strategies associated with posttraumatic growth in the context of the COVID-19 pandemic. Thus, more research should be done to determine how these strategies can be implemented in existing community resources. However, our findings should not overshadow the importance of investing in an equitable allocation of mental health resources that integrates and prioritizes race, culture, systemic oppression, and economic disparity.
Contributors
Brea Willey: Data interpretation, manuscript writing and editing, and accessed the raw data.
Kayden Mimmack: performed analytic computations, manuscript writing and editing, and accessed the raw data.
Geoffroy Gagliardi: Data interpretation, manuscript writing and editing, and accessed the raw data.
Michelle L. Dossett: design of the study, reviewing and editing of ms
Sharon Wang: Data curation, involved in collection and quality checking of data, design of the study, reviewing and editing of ms
Onyinye J Udeogu: Data curation, involved in collection and quality checking of data, design of the study, reviewing and editing of ms
Nancy J. Donovan: design of the study, reviewing and editing of ms
Jennifer R. Gatchel: design of the study, reviewing and editing of ms
Yakeel T. Quiroz: design of the study, reviewing and editing of ms
Rebecca Amariglio: design of the study, reviewing and editing of ms
Cindy H. Liu: reviewing and editing of ms
Sunah Hyun: reviewing and editing of ms
Abdelrahman ElTohamy: reviewing and editing of ms
Dorene Rentz: design of the study, reviewing and editing of ms
Reisa A. Sperling: design of the study, reviewing and editing of ms
Gad A. Marshall: design of the study, reviewing and editing of ms
Patrizia Vannini: Supervision, formal analysis, data curation, manuscript writing and editing, accessed the raw data.
All authors approved the final version of the article and had final responsibility for the decision to submit for publication.
Declaration of interests
Dr. Dossett reports personal fees from UpToDate, personal fees from Harvard Health Publishing, and grants from NCCIH, outside the submitted work.
Dr. Quiroz reports grants from US National Institute on Aging, grants from Alzheimer's Association, and consulting fees from Biogen, outside the submitted work.
Dr. Rentz reports consulting from Digital Cognition Technologies, consulting from Biogen Idec, and is on the Scientific Advisory Board for Neurotrack, outside the submitted work.
Dr. Sperling reports grants or contracts from Eli Lilly and Co. and Eisai and Co., and consulting fees from AC Immune, Janssen, Ionis, NervGen, Oligomerix, and Genentech, outside the submitted work.
Dr. Marshall has received research salary support from Eisai Inc., Eli Lilly and Company, Janssen Alzheimer Immunotherapy, Novartis, and Genentech, and consulting fees from Grifols Shared Services North America, Inc., and Eisai Inc, outside the submitted work.
All other authors have nothing to declare.
Acknowledgments
Data Sharing Statement
The dataset analyzed for this paper is not publicly available. However, it may be available from the corresponding author on reasonable request: patrizia@bwh.harvard.edu. Brea Willey, Kayden Mimmack, Geoffroy Gagliardi, and Patrizia Vannini accessed and were responsible for the raw data involved in the study.
Acknowledgments
The US National Institute of Health (NIH) supported Patrizia Vannini (R21AG064348, R01AG061083), Reisa Sperling (P01AG036694), Gad Marshall (R01 AG053184), Michelle Dossett (K23AT009218), Jennifer R Gatchel (K23 AG058805), and Yakeel Quiroz (R01 AG054671).
Reisa Sperling was also funded with additional support from several philanthropic organizations. Jennifer R Gatchel was also supported by the Alzheimer's Association Clinical Fellowship (AACF-16-440965), and Yakeel Quiroz by Massachusetts General Hospital ECOR.
We would also like to thank the faculty of the Harvard Visiting Research Internship Program, Dr. LM Nadler, Dr. JY Reede, Dr. MF Lopez, and Ms. J St. Louis for the opportunity for Brea Willey to conduct this study in the context of the program. The authors thank all participants for contributing their valuable time and effort, without which this study would not have been possible.
Funding
The Harvard Aging Brain Study (HABS) has been funded by NIH-NIA P01 AG036694 (PI: Reisa Sperling). The IADL study is funded by the National Institute on Aging (R01 AG053184, PI: Gad A. Marshall).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101343.
Appendix. Supplementary materials
References
- 1.CDC COVID Data Tracker [Internet]. [cited 2021 Jul 9]. Available from: https://covid.cdc.gov/covid-data-tracker/#datatracker-home
- 2.CDC. Cases, data, and surveillance [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2021 Aug 8]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- 3.Wasfy J.H., Hidrue M.K., Rockett H., Cafiero-Fonseca E.T., Ferris T.G., del Carmen M.G. Socioeconomic and demographic characteristics of both inpatients and outpatients with positive testing for SARS-CoV-2. J Gen Intern Med. 2021;36(8):2522–2524. doi: 10.1007/s11606-021-06919-x. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vinkers C.H., van Amelsvoort T., Bisson J.I., et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol. 2020;35:12–16. doi: 10.1016/j.euroneuro.2020.05.003. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bridgland V.M.E., Moeck E.K., Green D.M., et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0240146. Sar V, editor. Jan 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tedeschi R.G., Calhoun L.G. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–471. doi: 10.1007/BF02103658. Jul. [DOI] [PubMed] [Google Scholar]
- 7.Tedeschi R.G., Calhoun L.G. Target article: “posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq. 2004;15(1):1–18. Jan. [Google Scholar]
- 8.Calhoun L.G., Tedeschi R.G. Lawrence Erlbaum Associates; Mahwah, N.J: 2006. Handbook of Posttraumatic Growth: Research and Practice; p. 387. editors. [Google Scholar]
- 9.Tedeschi R., Calhoun L. SAGE Publications, Inc.; 1995. Trauma & Transformation: Growing in the Aftermath of Suffering.http://sk.sagepub.com/books/trauma-and-transformation [Internet]2455 Teller Road, Thousand Oaks California 91320 United States:[cited 2022 Jan 12]. Available from: [Google Scholar]
- 10.Dong X., Li G., Liu C., et al. The mediating role of resilience in the relationship between social support and posttraumatic growth among colorectal cancer survivors with permanent intestinal ostomies: a structural equation model analysis. Eur J Oncol Nurs Off J Eur Oncol Nurs Soc. 2017;29:47–52. doi: 10.1016/j.ejon.2017.04.007. Aug. [DOI] [PubMed] [Google Scholar]
- 11.Teixeira R.J., Pereira M.G. Psychological morbidity, burden, and the mediating effect of social support in adult children caregivers of oncological patients undergoing chemotherapy. Psychooncology. 2013;22(7):1587–1593. doi: 10.1002/pon.3173. Jul. [DOI] [PubMed] [Google Scholar]
- 12.Wu X., Kaminga A.C., Dai W., et al. The prevalence of moderate-to-high posttraumatic growth: a systematic review and meta-analysis. J Affect Disord. 2019;243:408–415. doi: 10.1016/j.jad.2018.09.023. Jan. [DOI] [PubMed] [Google Scholar]
- 13.Jayawickreme E., Blackie L.E.R. Springer Science + Business Media; New York, NY, US: 2016. Exploring the Psychological Benefits of Hardship: a Critical Reassessment of Posttraumatic Growth. ix, 77 p. (Exploring the psychological benefits of hardship: A critical reassessment of posttraumatic growth) [Google Scholar]
- 14.Helgeson V.S., Reynolds K.A., Tomich P.L. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- 15.Celdrán M., Serrat R., Villar F. Post-traumatic growth among older people after the forced lockdown for the COVID–19 pandemic. Span J Psychol. 2021;24:e43. doi: 10.1017/SJP.2021.40. [DOI] [PubMed] [Google Scholar]
- 16.Lowe S.R., Manove E.E., Rhodes J.E. Posttraumatic stress and posttraumatic growth among low-income mothers who survived Hurricane Katrina. J Consult Clin Psychol. 2013;81(5):877–889. doi: 10.1037/a0033252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang M.L., Liu J.E., Wang H.Y., Chen J., Li Y.Y. Posttraumatic growth and associated socio-demographic and clinical factors in Chinese breast cancer survivors. Eur J Oncol Nurs Off J Eur Oncol Nurs Soc. 2014;18(5):478–483. doi: 10.1016/j.ejon.2014.04.012. Oct. [DOI] [PubMed] [Google Scholar]
- 18.Wang C., Lu Q. Poster Presentations - Proffered Abstracts. American Association for Cancer Research; 2020. Abstract A060: socioeconomic status and quality of life among Chinese American breast cancer survivors: the role of post-traumatic growth. [Internet][cited 2022 Jan 12]. p. A060–A060. Available from: http://cebp.aacrjournals.org/lookup/doi/ [DOI] [Google Scholar]
- 19.Hossain M.M., Tasnim S., Sultana A., et al. Epidemiology of mental health problems in COVID-19: a review. F1000Research. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. Sep 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sneed R.S., Key K., Bailey S., Johnson-Lawrence V. Social and psychological consequences of the COVID-19 pandemic in African-American communities: lessons from Michigan. Psychol Trauma Theory Res Pract Policy. 2020;12(5):446–448. doi: 10.1037/tra0000881. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Office of the Surgeon General (US) Substance Abuse and Mental Health Services Administration (US); Rockville (MD): 2001. Center For Mental Health Services (US), National Institute of Mental Health (US). Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General.http://www.ncbi.nlm.nih.gov/books/NBK44243/ [Internet][cited 2021 Sep 25]. (Publications and Reports of the Surgeon General). Available from: [PubMed] [Google Scholar]
- 23.Vannini P., Gagliardi G.P., Kuppe M., et al. Stress, resilience, and coping strategies in a sample of community-dwelling older adults during COVID-19. J Psychiatr Res. 2021;138:176–185. doi: 10.1016/j.jpsychires.2021.03.050. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.REDCap [Internet]. [cited 2021 Aug 9]. Available from: https://projectredcap.org/
- 25.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hollingshead A de B. Yale; New Haven, Connecticut: 1965. Two Factor Index of Social Position. [Google Scholar]
- 28.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 29.Ezzati A., Jiang J., Katz M.J., Sliwinski M.J., Zimmerman M.E., Lipton R.B. Validation of the perceived stress scale in a community sample of older adults. Int J Geriatr Psychiatry. 2014;29(6):645–652. doi: 10.1002/gps.4049. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shakespeare-Finch J., Martinek E., Tedeschi R.G., Calhoun L.G. A qualitative approach to assessing the validity of the posttraumatic growth inventory. J Loss Trauma. 2013;18(6):572–591. Nov. [Google Scholar]
- 31.Reeve B.B., Hays R.D., Bjorner J.B., et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the patient-reported outcomes measurement information system (PROMIS) Med Care. 2007;45(5):S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. May. [DOI] [PubMed] [Google Scholar]
- 32.Hays R.D., Bjorner J.B., Revicki D.A., Spritzer K.L., Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873–880. doi: 10.1007/s11136-009-9496-9. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cella D., Choi S.W., Condon D.M., et al. PROMIS® adult health profiles: efficient short-form measures of seven health domains. Value Health. 2019;22(5):537–544. doi: 10.1016/j.jval.2019.02.004. May. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carver C.S. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 35.García F.E., Barraza-Peña C.G., Wlodarczyk A., Alvear-Carrasco M., Reyes-Reyes A. Psychometric properties of the Brief-COPE for the evaluation of coping strategies in the Chilean population. Psicol Reflex E Crít. 2018;31(1):22. doi: 10.1186/s41155-018-0102-3. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yusoff N., Low W.Y., Yip C.H. Reliability and validity of the Brief COPE Scale (English version) among women with breast cancer undergoing treatment of adjuvant chemotherapy: a Malaysian study. Med J Malays. 2010;65(1):41–44. Mar. [PubMed] [Google Scholar]
- 37.Zaheed A.B., Sharifian N., Kraal A.Z., et al. Mediators and moderators of the association between perceived stress and episodic memory in diverse older adults. J Int Neuropsychol Soc. 2020:1–13. doi: 10.1017/S1355617720001253. Dec 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whitehead B.R. COVID-19 as a stressor: pandemic expectations, perceived stress, and negative affect in older adults. J Gerontol Ser B. 2021;76(2):e59–e64. doi: 10.1093/geronb/gbaa153. Neupert S, editor. Jan 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bautista R.E.D. Racial differences in coping strategies among individuals with epilepsy. Epilepsy Behav. 2013;29(1):67–71. doi: 10.1016/j.yebeh.2013.06.035. Oct. [DOI] [PubMed] [Google Scholar]
- 41.Elfström M., Rydén A., Kreuter M., Taft C., Sullivan M. Relations between coping strategies and health-related quality of life in patients with spinal cord lesion. J Rehabil Med. 2005;37(1):9–16. doi: 10.1080/16501970410034414. Jan 1. [DOI] [PubMed] [Google Scholar]
- 42.Abu H.O., McManus D.D., Lessard D.M., Kiefe C.I., Goldberg R.J. Religious practices and changes in health-related quality of life after hospital discharge for an acute coronary syndrome. Health Qual Life Outcomes. 2019;17(1):149. doi: 10.1186/s12955-019-1218-6. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Umucu E., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil Psychol. 2020;65(3):193–198. doi: 10.1037/rep0000328. Aug. [DOI] [PubMed] [Google Scholar]
- 44.Bellizzi K.M., Smith A.W., Reeve B.B., et al. Posttraumatic growth and health-related quality of life in a racially diverse cohort of breast cancer survivors. J Health Psychol. 2010;15(4):615–626. doi: 10.1177/1359105309356364. May. [DOI] [PubMed] [Google Scholar]
- 45.Bussell V.A., Naus M.J. A longitudinal investigation of coping and posttraumatic growth in breast cancer survivors. J Psychosoc Oncol. 2010;28(1):61–78. doi: 10.1080/07347330903438958. Jan 14. [DOI] [PubMed] [Google Scholar]
- 46.Pérez-San-Gregorio M.Á., Martín-Rodríguez A., Borda-Mas M., Avargues-Navarro M.L., Pérez-Bernal J., Gómez-Bravo M.Á. Family caregivers of liver transplant recipients: coping strategies associated with different levels of post-traumatic growth. Transplant Proc. 2018;50(2):646–649. doi: 10.1016/j.transproceed.2017.09.067. Mar. [DOI] [PubMed] [Google Scholar]
- 47.Ortega-Williams A., Beltrán R., Schultz K., Ru-Glo Henderson Z., Colón L., Teyra C. An integrated historical trauma and posttraumatic growth framework: a cross-cultural exploration. J Trauma Dissociation. 2021;22(2):220–240. doi: 10.1080/15299732.2020.1869106. Off J Int Soc Study Dissociation ISSDApr. [DOI] [PubMed] [Google Scholar]
- 48.Sotero M. A conceptual model of historical trauma: implications for public health practice and research. J Health Disparities Res Pract. 2006;1(1):93–108. Fall. [Google Scholar]
- 49.Mohatt N.V., Thompson A.B., Thai N.D., Tebes J.K. Historical trauma as public narrative: a conceptual review of how history impacts present-day health. Soc Sci Med. 2014;106:128–136. doi: 10.1016/j.socscimed.2014.01.043. Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams-Washington K.N., Mills C.P. African American historical trauma: creating an inclusive measure. J Multicult Couns Dev. 2018;46(4):246–263. Oct. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.