Abstract
Objectives:
To assess the relationship between mean versus peak calcified plaque density, their impact on calculating coronary artery calcium (CAC) scores, and to compare the corresponding differential prediction of atherosclerotic cardiovascular disease (ASCVD) and coronary heart disease (CHD) mortality.
Background:
The Agatston CAC score is quantified per-lesion as the product of plaque area and a four-level categorical peak calcium density factor. However, mean calcium density may more accurately measure the heterogenous mixture of lipid-rich, fibrous, and calcified plaque reflective of ASCVD risk.
Methods:
We included 10,373 individuals from the CAC Consortium who had CAC >0 and per-vessel measurements of peak calcium density factor and mean calcium density. Area under the curve (AUC) and continuous net reclassification improvement (NRI) analyses were performed for CHD and ASCVD mortality to compare the predictive abilities of mean calcium density versus peak calcium density factor when calculating the Agatston CAC score.
Results:
Participants were on average 53.4 years old, 24.4% were women, and the median CAC score was 68 AU. The average values for mean calcium density and peak calcium density factor were 210 ± 50 HU and 3.1 ± 0.5, respectively. Individuals <50 years old and/or those with a total plaque area <100 mm2 had the largest differences between the peak and mean density measures. Among persons with CAC 1–99, the use of mean calcium density resulted in a larger improvement in ASCVD mortality reclassification (NRI=0.49, p<0.001 versus 0.18, p=0.08) and CHD mortality discrimination (ΔAUC=+0.169 versus +0.036, p<0.001) compared to peak calcium density factor. Neither peak nor mean calcium density improved mortality prediction at CAC scores >100.
Conclusion:
Mean and peak calcium density may differentially describe plaque composition early in the atherosclerotic process. Mean calcium density performs better than peak calcium density factor when combined with plaque area for ASCVD mortality prediction among persons with Agatston CAC 1–99.
Keywords: coronary artery calcium, calcium density, atherosclerotic plaque, vascular calcification, multidetector computed tomography, cardiovascular disease, risk, primary prevention
Introduction
The measurement of coronary artery calcium (CAC) via non-contrast computed tomography is a non-invasive imaging approach that improves atherosclerotic cardiovascular disease (ASCVD) risk stratification and is recommended by the 2019 American College of Cardiology/American Heart Association Prevention of Cardiovascular Disease Guidelines when there is uncertainty regarding risk(1). The Agatston method is currently the most widely used scoring algorithm for quantifying CAC, which is calculated as the product of plaque area and a quantized peak calcium density weighting factor for each lesion, which is then summed across all lesions to give a total CAC score(2). However, CAC density is heterogeneous across coronary plaques and an arbitrary maximum value to capture peak calcium density, as currently used in Agatston scoring, may result in ASCVD risk misclassification among persons with non-zero CAC scores(2–4). Likewise, the utilization of peak calcium density for an overall lowattenuation lesion may not be reflective of its underlying biology and true susceptibility for acute vascular events(5).
In modeling approaches that include measures of plaque area and volume, calcium density is independently and inversely associated with ASCVD and coronary heart disease (CHD), but only after adjustment for total plaque area(6,7). In particular, the presence of super calcified plaque (>1K Hounsfield units, HU) associates with a lower risk of acute coronary syndrome on a per-patient and per-lesion assessment, suggesting that progressively increasing plaque density and CAC scores in the same individual may paradoxically represent plaque stabilization(8). However, previous studies involving calcium density and ASCVD outcomes have been partially limited, as they have not separately considered mean versus peak calcium density. In contrast to peak calcium density, overall mean calcium density may be a more accurate representation of total lesion composition and broader ASCVD risk in such scenarios, comprehensively capturing the mixture of low attenuation lipid-rich and higher attenuation fibrous and calcified plaques across all lesions. Despite these differences, there have been no previous studies which have assessed the association of plaque morphology and ASCVD outcomes stratified by mean calcium density, peak calcium density, and total plaque area.
Therefore, among persons with CAC >0, we sought to assess 1) the relationships of mean versus peak calcium density with age and total plaque area, 2) the correlation between mean and peak calcium density as a function of CAC score and total plaque area, and 3) the predictive utilities of mean versus peak calcium density for ASCVD and coronary heart disease (CHD) mortality over a follow-up period of 11.3 years.
Methods
Study Population
The CAC Consortium is a multi-center cohort study involving four high-volume centers the United States, Cedars-Sinai Medical Center (Los Angeles, CA), PrevaHealth Wellness Diagnostic Center (Columbus, OH), Harbor-UCLA Medical Center (Torrance, CA), and Minneapolis Heart Institute (Minneapolis, MN). The rationale for the multicenter retrospective cohort study was to assess the association of CAC with long-term, disease-specific mortality, and the study design and methods have been previously described in detail elsewhere(9). In brief, investigators included individuals 18 years of age or older who were free of clinical ASCVD or cardiovascular symptoms at the time of CAC scanning. The major indication for CAC testing among participants included in the study pertained to uncertainty in risk assessment in the presence of underlying ASCVD risk factor(s). A majority of participants reported hyperlipidemia and/or family history of CHD as precipitants for undergoing CAC scanning. All study participants provided written informed consent at baseline, and study protocols were approved by the Johns Hopkins University School of Medicine.
Findings represented in the current analysis represent the baseline CAC Consortium data collection, occurring from 1991 to 2010. Previous studies have suggested comparability between baseline characteristics of the CAC Consortium to more recent cohorts, including the 2001–2002 National Health and Nutrition Examination Survey, Framingham Offspring Study, and the Multi-Ethnic Study of Atherosclerosis(9). After excluding participants with CAC=0 and those who did not have direct measurements of mean calcium density, there were 10,373 individuals included for the current analysis (Supplemental Figure 1).
Measurement of Calcium Density and CAC Scoring
Coronary artery calcium was quantified using non-contrast, cardiac-gated computed tomography (CT) at all participating medical centers according to a standard protocol using measured coronary plaque area (mm2) and peak calcium density (HU) on the per-lesion basis (9). A quantized calcium density weighting factor for the Agatston algorithm was used to assign a value of 1 through 4 based on the measured peak calcium density attenuation value of the lesion (1: 130–199 HU, 2: 200–299 HU, 3: 300–399 HU, 4: >400 HU). Calculated CAC scores were then categorized into CAC groups of 1–99, 100–399, and >400 Agatston units (AU). Both electron beam tomography (EBT) and multi-detector CT (MDCT) were used for imaging, and previous studies have shown no clinically significant differences in CAC measurement between these two scanning methods(10).
The mean per-lesion calcium density was directly measured from CT images for each participant that had calcified plaques (three contiguous voxels of at least 130 HU). Mean (composite) calcium density in HU across all lesions was then divided by 100 to create a mean calcium weight factor scale that matched the Agatston peak calcium density weighting factor scale. For example, a measured mean (composite) calcium density of 350 HU would yield a mean calcium weighting factor of 3.5.
Calculation of Peak Calcium Density and Total Plaque Area
Peak calcium density was measured and quantized for the calculation of Agatston CAC scores. Total plaque area (mm2) for each participant were calculated by dividing CAC volume scores by the slice thickness used for each respective CT imaging protocol. As previously described(6,7), the average peak calcium density was then back calculated as the quotient of the Agatston score and total plaque area for each participant (average peak calcium density = Agatston score/total plaque area). A comparison between mean versus peak calcium density and sample calculations are provided in Supplemental Figure 2.
Evaluation of ASCVD Risk Factors
Assessment of ASCVD risk factors occurred during the clinical visit that accompanied CAC testing. Diabetes and hypertension were defined by a previous clinical diagnosis or reported antihypertensive or glucose-lowering medication utilization. Hyperlipidemia (low-density lipoprotein-cholesterol >160 mg/dL), hypertriglyceridemia (triglycerides >150 mg/dL), and low high-density lipoprotein-cholesterol (<40 mg/dL in men, <50 mg/dL in women) were defined by a previous clinical diagnosis or utilization of lipid-lowering therapy. Information on smoking and family history of CHD (first-degree relative with history of CHD at any age) were obtained through self-report data.
ASCVD and CHD Mortality Ascertainment
Patient records were linked with the Social Security Administration Death Master File using a previously validated algorithm to ascertain mortality in the CAC consortium(11). Unique patient identifiers are used by the algorithm in a semiflexible hierarchical matching process. Death certificates were acquired from the National Death Index service and deaths were classified using the International Classification of Diseases, Ninth Revision and the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision(9). There was greater than 90% specificity and 72%–90% sensitivity for identifying known deaths.
Statistical Analysis
Study population characteristics were stratified according to mean calcium density and peak calcium density tertiles (Table 1 & Supplemental Table 1). Continuous variables were presented as means and standard deviations, while percentages are used for categorical variables for categorical variables. Due to a non-normal distribution of CAC, the median was used to represent the central tendency of CAC scores. The Student’s t-test and Wilcoxon signed-rank test were used to assess differences in normally and non-normally distributed continuous variables, respectively. Differences between categorical variables were evaluated through Pearson’s Chisquare test.
Table 1.
Characteristics of 10,373 individuals of the CAC Consortium with CAC >0, stratified by mean calcium density
| All 130–419 HU (n=10373) |
Tertile 1 130–185 HU (n=3524) |
Tertile 2 186–230 HU (n=3420) |
Tertile 3 231–419 HU (n=3429) |
P-Value* | |
|---|---|---|---|---|---|
| Age, mean ± SD, years | 56.7 ± 9.2 | 53.4 ± 8.7 | 56.8 ± 8.5 | 59.8 ± 9.0 | <0.001 |
| Women, % | 24.4 | 25.1 | 22.8 | 25.1 | 0.03 |
| Ethnicity, % | 0.97 | ||||
| White | 96.7 | 96.4 | 96.7 | 96.8 | |
| Asian | 0.7 | 0.8 | 0.7 | 0.7 | |
| Black | 0.4 | 0.4 | 0.4 | 0.4 | |
| Hispanic | 0.3 | 0.4 | 0.3 | 0.2 | |
| Other | 1.9 | 2.0 | 1.9 | 1.9 | |
| CAC, median (Q1, Q3), AU | 68 (16, 253) | 8 (2, 20) | 93 (41, 219) | 286 (113, 719) | <0.001 |
| CAC, AU, % | <0.001 | ||||
| 1–100 | 57.7 | 97.1 | 52.6 | 22.2 | |
| 100–400 | 25.0 | 2.7 | 35.7 | 37.2 | |
| >400 | 17.3 | 0.2 | 11.7 | 40.6 | |
| Mean Calcium Density, mean ± SD | 2.1 ± 0.5 | 1.6 ± 0.1 | 2.1 ± 0.1 | 2.7 ± 0.3 | <0.001 |
| Body Mass Index, mean ± SD, kg/m2 | 28.9 ± 5.5 | 29.5 ± 5.8 | 29.1 ± 5.5 | 28.1 ± 5.2 | <0.001 |
| Smoking, % | 11.8 | 10.6 | 11.1 | 13.8 | <0.001 |
| Hypertension, % | 28.0 | 24.3 | 28.9 | 31.1 | <0.001 |
| Hyperlipidemia, % | 63.1 | 61.4 | 65.1 | 62.9 | 0.007 |
| Diabetes, % | 6.0 | 4.7 | 7.0 | 6.5 | <0.001 |
| Family History of CHD, % | 51.5 | 52.4 | 51.0 | 51.2 | 0.46 |
| All-Cause Mortality, n (%) | 666 (6.4) | 161 (4.6) | 182 (5.3) | 323 (9.4) | <0.001 |
| CVD Mortality, n (%) | 197 (1.9) | 40 (1.1) | 56 (1.6) | 101 (3.0) | <0.001 |
| CHD Mortality, n (%) | 83 (0.8) | 18 (0.5) | 24 (0.7) | 41 (1.2) | 0.004 |
| Cancer Mortality, n (%) | 247 (2.4) | 61 (1.7) | 70 (2.1) | 116 (3.4) | <0.001 |
chi-square test
The relationship between mean versus peak calcium density across increasing age, CAC scores and total plaque area burden were evaluated graphically through local regression and the LOESS function. There were three CAC score groups of interest (CAC 1–99, CAC 100–399, CAC >400) and total plaque area burden was similarly categorized into tertiles (0.16–9.0 mm2, 9.0–52.1 mm2, 52.1–348.2 mm2) for graphical and statistical analyses.
The associations of mean and peak calcium density with ASCVD and CHD mortality were assessed through multivariable Cox proportional hazards regression. The proportional hazards assumption was satisfied and was tested by assessing the significance of time-dependent independent variables concurrently. The base model included total plaque area for ASCVD and CHD mortality prediction. Mean calcium density and peak calcium density were each individually added as continuous variables to the total plaque area model. The incremental predictive value of mean versus peak calcium density, beyond total plaque area, were evaluated using log-likelihood, area under the curve (AUC), and continuous net reclassification improvement (NRI) analyses(12,13). Incremental AUC values for mean and peak calcium density were calculated by comparing each respective model to the base model. The continuous NRI was calculated in the full multivariable Cox proportional hazards regression models. Differences in concordance and NRI statistics between models were assessed through approaches developed by Uno et al (14). All statistical analyses were conducted using STATA 13 (Stata Corp., College Station, Texas). Statistical significance was defined as a p-value <0.05 on a 2-tailed test.
Results
The mean age of participants was 56.7 years, 24.4% were women, and 3.3% of participants were of non-white ethnicity (Table 1). The median CAC score was 68 (16, 253) AU, and a majority of participants (57.7%) had CAC scores of 1–100. Participants were on average overweight (body mass index=28.9±5.5 kg/m2), while hyperlipidemia (63.1%) and a family history of CHD (51.5%) were the most prevalent traditional ASCVD risk factors. There was a total of 666 deaths (6.4%) over a mean follow-up period of 11.3 ± 2.1 years, of which 197/666 and 83/666 were attributed to ASCVD and CHD, respectively.
The average mean calcium density was 210 ± 50 HU and the average peak calcium density weighting factor was 3.1 ± 0.5, corresponding to a signal attenuation of 300–399 HU. All modifiable risk factors and ASCVD mortality significantly differed across mean calcium density tertiles. Contrastingly, there were no significant differences across peak calcium density tertiles for several risk factors, including smoking and diabetes, and for CHD mortality (Supplemental Table 1).
Fitted regression curves indicated that the largest magnitude differences between mean and peak calcium values were among persons <50 years old, though the two calcium measures converged with older age (Figures 1A–1C). Correspondingly, mean and peak calcium density differed most strongly among individuals with a total plaque area <100 mm2 but were more similar for those with a higher total plaque area burden on fitted regression (Figure 2). Compared to individuals with CAC 100–399 and/or CAC >400, individuals with CAC 1–99 had a larger magnitude difference, but stronger correlation between mean and peak calcium density values (Figure 3A). A similar pattern between mean and peak calcium density was observed across increasing total plaque area tertiles (Figure 3B).
Figure 1. Association of mean and peak calcium density with age among all participants (A), women (B), and men (C).
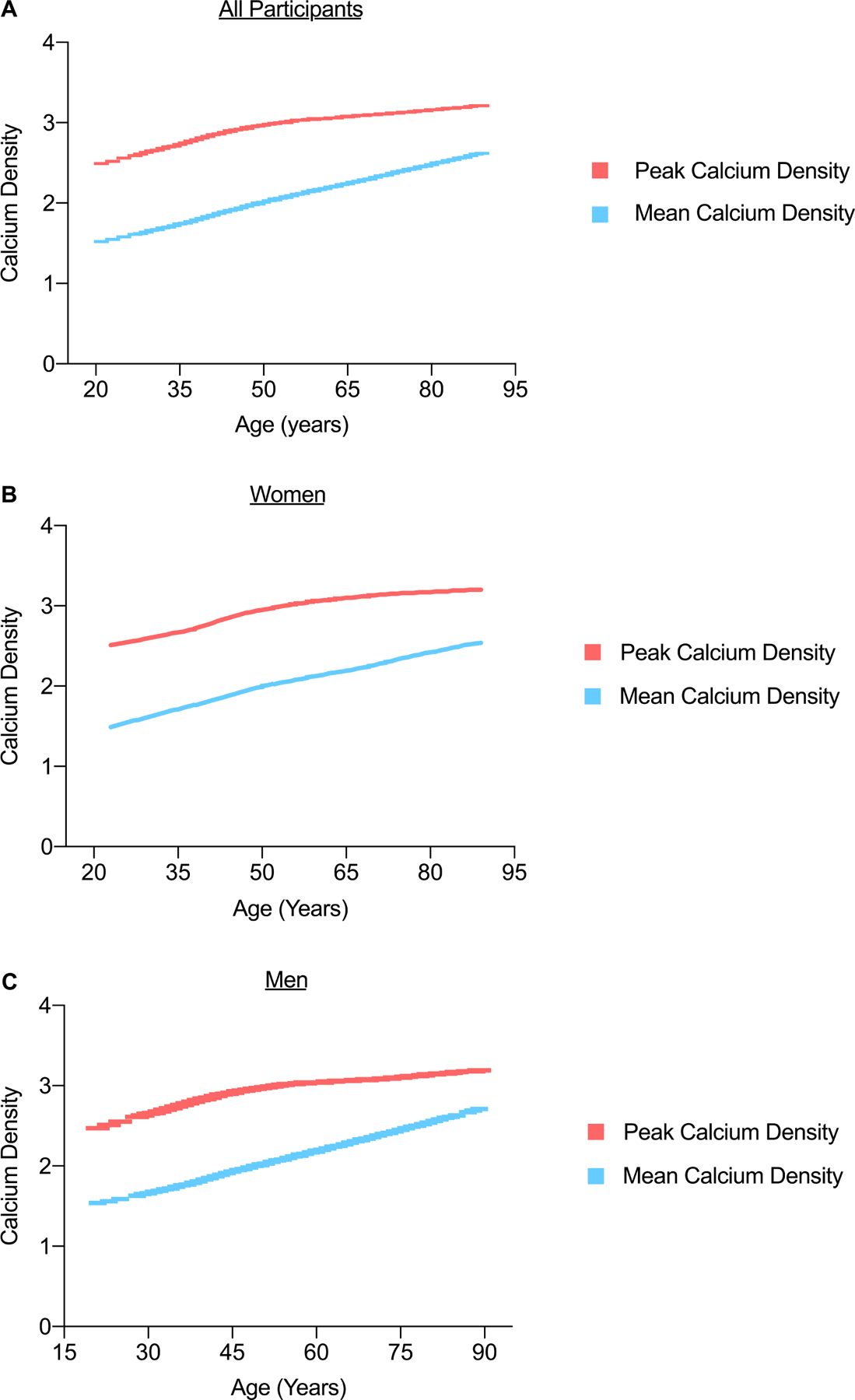
The largest differences between mean and peak calcium values were among persons <50 years old, though the two calcium measures converged with older age.
Figure 2. Association of mean and peak calcium density with total plaque area burden.
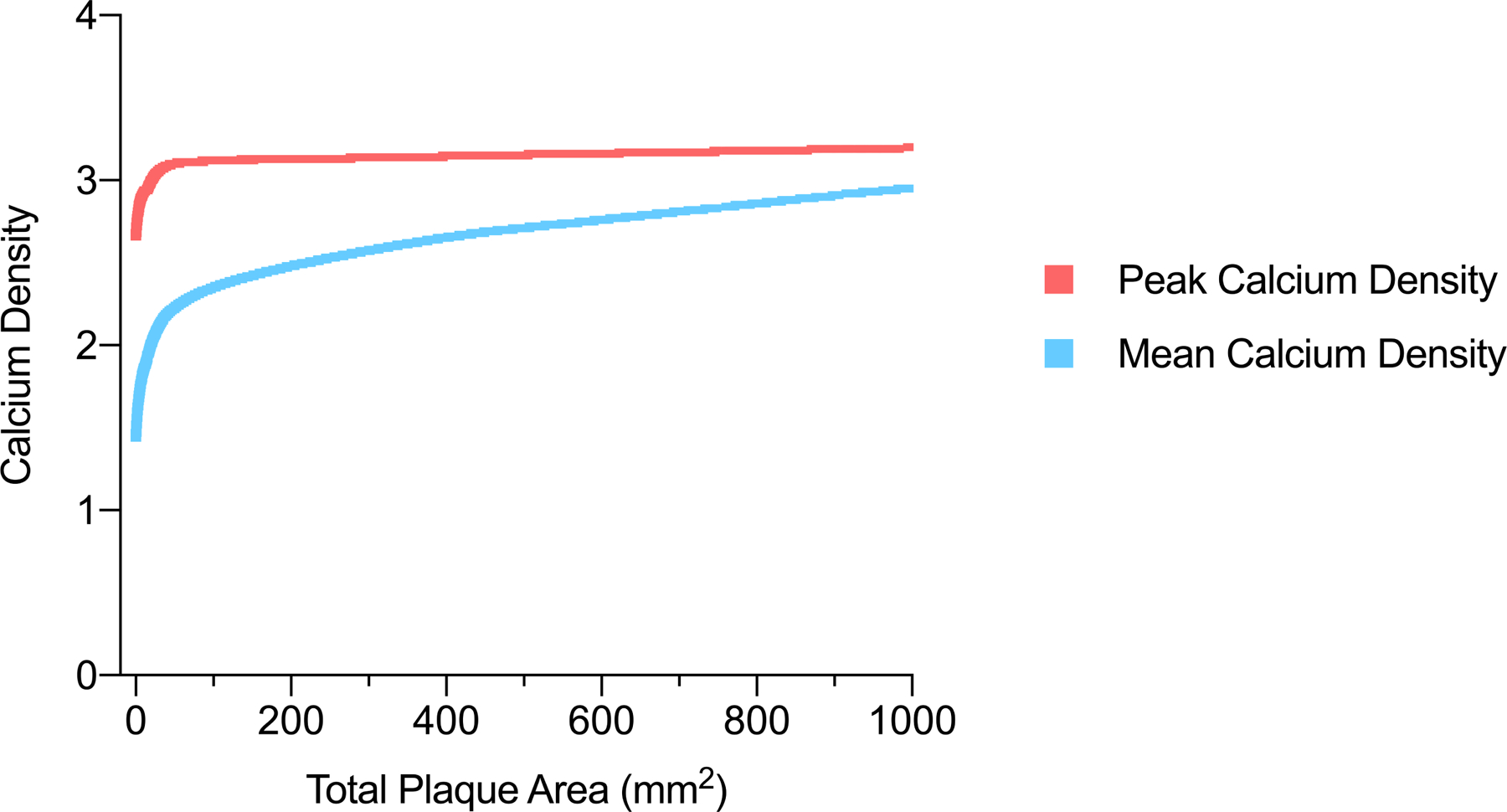
Mean and peak calcium density most strongly differed among individuals with a total plaque area <100 mm2 but were more similar for those with a higher total plaque area burden.
Figure 3. Correlation between mean and peak calcium density, stratified by CAC score (A) and total plaque area burden tertiles (B).
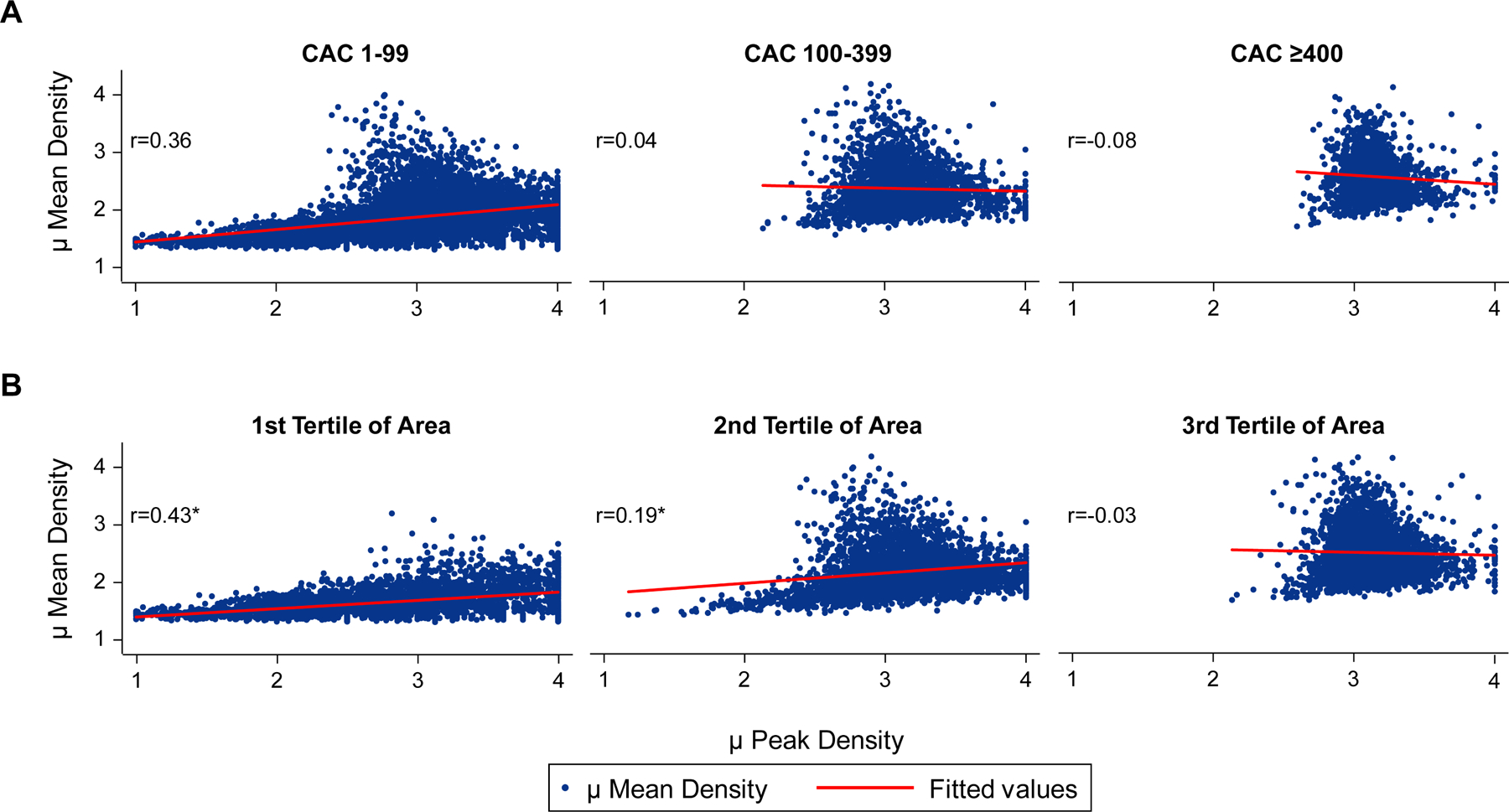
Compared to individuals with CAC 100–399 and/or CAC >400, individuals with CAC 1–99 had a larger magnitude difference, but stronger correlation between mean and peak calcium density values. A similar pattern between mean and peak calcium density was observed across increasing total plaque area tertiles.
There was considerable heterogeneity in the additive predictive abilities of mean and peak calcium density across CAC score groups for both ASCVD and CHD mortality (Table 2 and Table 3). Among individuals with CAC 1–99, the addition of mean calcium density to total coronary plaque area improved reclassification of ASCVD mortality, whereas adding peak calcium density resulted in a non-significant reclassification statistic (NRI=0.49, p<0.001 versus NRI=0.18, p=0.09). A larger magnitude NRI difference between mean and peak calcium density was observed for CHD mortality among persons with CAC 1–99 (NRI=0.77, p<0.001 versus NRI=0.13, p=0.27). Likewise, the addition of mean calcium density resulted in a greater improvement in CHD mortality discrimination compared to peak calcium density among persons with CAC 1–99 (ΔAUC=+0.169 versus +0.036, p<0.001). No significant improvements in the log-likelihood, AUC, and NRI were observed when adding mean or peak calcium density to the total plaque area burden for persons with CAC >100 or when considering all participants together. When compared to peak calcium density, mean calcium density correctly reclassified a larger proportion of persons with CAC 1–99 upward who had an ASCVD (50.9%, p=0.19 versus 73.7%, p=0.003) or CHD event (50.0%, p=0.54 versus 83.3%, p=0.002) (Supplemental Table 2 and Supplemental Table 3).
Table 2.
Mean versus peak calcium density for the prediction of ASCVD mortality, stratified by CAC score group
| ASCVD Mortality | |||||
|---|---|---|---|---|---|
| Log Likelihood Test | Area Under the Curve | Continuous NRI | |||
| P-value | C-Statistic | Contrast P-value* | NRI | P-value | |
| CAC 1–99 (n=5983) | |||||
| Total Plaque Area Alone | - | 0.522 | - | - | - |
| Total Plaque Area + Mean Calcium Density | <0.001 | 0.661 | - | 0.49 | <0.001 |
| Total Plaque Area + Peak Calcium Density | 0.004 | 0.602 | 0.08 | 0.18 | 0.09 |
| CAC 100–399 (n=2592) | |||||
| Total Plaque Area Alone | - | 0.553 | - | - | - |
| Total Plaque Area + Mean Calcium Density | 0.48 | 0.556 | - | 0.003 | 0.49 |
| Total Plaque Area + Peak Calcium Density | 0.86 | 0.554 | 0.95 | 0.07 | 0.33 |
| CAC >400 (n=1798) | |||||
| Total Plaque Area Alone | - | 0.607 | - | - | - |
| Total Plaque Area + Mean Calcium Density | 0.58 | 0.596 | - | −0.04 | 0.63 |
| Total Plaque Area + Peak Calcium Density | 0.92 | 0.601 | 0.39 | −0.05 | 0.67 |
NRI = net reclassification index
p-value comparing mean versus peak calcium density
Table 3.
Mean versus peak calcium density for the prediction of CHD mortality, stratified by CAC score group
| CHD Mortality | |||||
|---|---|---|---|---|---|
| Log Likelihood Test | Area Under the Curve | Continuous NRI | |||
| P-value | C-Statistic | Contrast P-value* | NRI | P-value | |
| CAC 1–99 (n=5983) | |||||
| Total Plaque Area Alone | - | 0.583 | - | - | - |
| Total Plaque Area + Mean Calcium Density | <0.001 | 0.752 | - | 0.77 | <0.001 |
| Total Plaque Area + Peak Calcium Density | 0.19 | 0.619 | <0.001 | 0.13 | 0.27 |
| CAC 100–399 (n=2592) | |||||
| Total Plaque Area Alone | - | 0.626 | - | - | - |
| Total Plaque Area + Mean Calcium Density | 0.83 | 0.627 | - | 0.15 | 0.26 |
| Total Plaque Area + Peak Calcium Density | 0.10 | 0.673 | 0.39 | 0.32 | 0.08 |
| CAC >400 (n=1798) | |||||
| Total Plaque Area Alone | - | 0.571 | - | - | - |
| Total Plaque Area + Mean Calcium Density | 0.27 | 0.617 | - | 0.20 | 0.10 |
| Total Plaque Area + Peak Calcium Density | 0.17 | 0.563 | 0.25 | 0.05 | 0.39 |
NRI = net reclassification index
p-value comparing mean versus peak calcium density
The associations of mean calcium density and peak calcium density with ASCVD and CHD mortality were different across total plaque area burden tertiles (Supplemental Table 4 and Supplemental Table 5). Mean calcium density (p=0.02) and peak calcium density (p=0.03) improved discrimination of ASCVD mortality when added to total plaque area for individuals in the lowest total plaque area tertile (<9.0 mm2). Among persons with a total plaque area <9.0 mm2, the addition of mean calcium density improved reclassification of ASCVD (NRI=0.33, p=0.03) and CHD mortality (NRI=0.48, p=0.04). On the contrary, adding peak calcium density to total plaque area did not result in a significant NRI for either ASCVD or CHD mortality among the second and third total plaque area tertile (>9.0 mm2). Among persons in the first tertile of total plaque area, mean calcium density correctly reclassified a larger proportion of individuals who had an ASCVD event (67.6%, p=0.05 versus 55.5%, p=0.14) upwards compared to peak calcium density (Supplemental Table 6 and Supplemental Table 7).
Mean calcium density had a positive association with ASCVD and CHD mortality when adjusting for age and sex (Supplemental Table 8 and Supplemental Table 9). However, after adjusting for total plaque area, each one-unit increase in mean calcium density was significantly associated with a 39% and 41% lower risk of ASCVD (HR=0.61, 95% CI: 0.39, 0.95, p=0.03) and CHD (HR=0.39, 95% CI: 0.18, 0.81, p=0.01), respectively. In contrast, peak calcium density had a modest inverse but non-significant association with ASCVD and CHD mortality upon adjusting for age and sex (Supplemental Table 8 and Supplemental Table 9). After sequentially adjusting for total plaque area, a significant and stronger magnitude inverse association for peak calcium density with ASCVD mortality was observed (HR=0.52, 95% CI: 0.35, 0.76, p=0.001).
When added to a base model including the 10-year Pooled Cohort Equations ASCVD risk score, CAC scores calculated using peak calcium density (Agatston score) and mean calcium density (modified score) performed similarly and reclassified a larger proportion of individuals downwards regardless of the presence/absence of an actual event (Supplemental Table 10). Both the recalculated CAC score and traditional Agatston CAC score were significantly associated with ASCVD (OR=1.26 per 1 unit change of ln(CAC), 95% CI: 1.15, 1.37, p<0.001 and OR=1.27, 95% CI: 1.15, 1.39, p<0.001) and CHD mortality (OR=1.34, 95% CI: 1.17, 1.53, p<0.001 and OR=1.37, 95% CI: 1.18, 1.58, p<0.001) after adjusting for age and sex. The relative strength of association for the CAC scores using mean calcium density and peak calcium density with ASCVD and CHD mortality was similar across age strata (Supplemental Table 11 and Supplemental Table 12).
Recalculating CAC using mean calcium density instead of the peak density weighting factor resulted in a larger proportion of individuals with lower CAC scores (Figure 4). A total of 600 (23.1%) individuals with Agatston CAC 100–399 were reclassified downwards into the CAC 1–99 group. Similarly, 349 (19.4%) persons with Agatston CAC >400 were shifted to a CAC score of 100–399 when calculations were performed using mean calcium density instead peak calcium density.
Figure 4. Calculation of coronary artery calcium scores with mean versus peak calcium density.
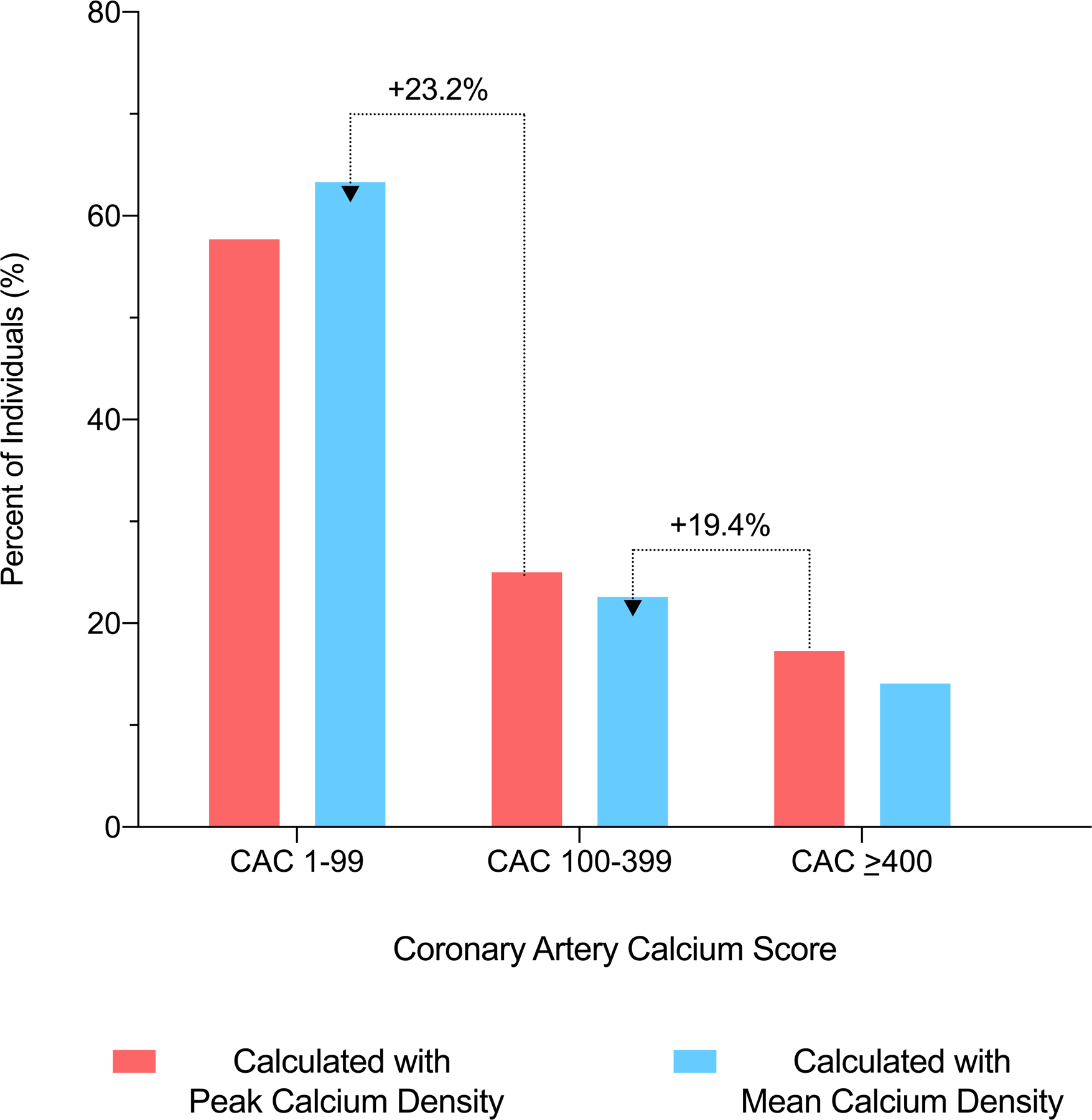
Recalculating CAC using mean calcium density resulted in a larger proportion of individuals with lower CAC scores.
Discussion
Among more than 10,000 individuals with prevalent CAC, we found that mean calcium density values were considerably lower in magnitude compared to peak calcium density values in the early stages of atherosclerotic CHD, with the largest differences present among individuals aged <50 years and those with a total plaque area <100 mm2. Among persons with CAC 1–99, mean calcium density performed better than peak calcium density for the prediction of ASCVD and CHD mortality when added to total coronary plaque area burden. Furthermore, recalculation of CAC using mean calcium density resulted in approximately 25% of individuals with an Agatston CAC score of 100–399 being downwardly reclassified into a CAC score group of 1–99 (Central Illustration). These results overall suggest that mean and peak calcium density reflect may unique atherosclerotic processes and that CAC quantification using mean calcium density could potentially improve long-term risk assessment for persons with early subclinical coronary atherosclerosis (Figure 5).
Central Illustration. Mean versus peak calcium density in CAC scoring and mortality risk prediction.
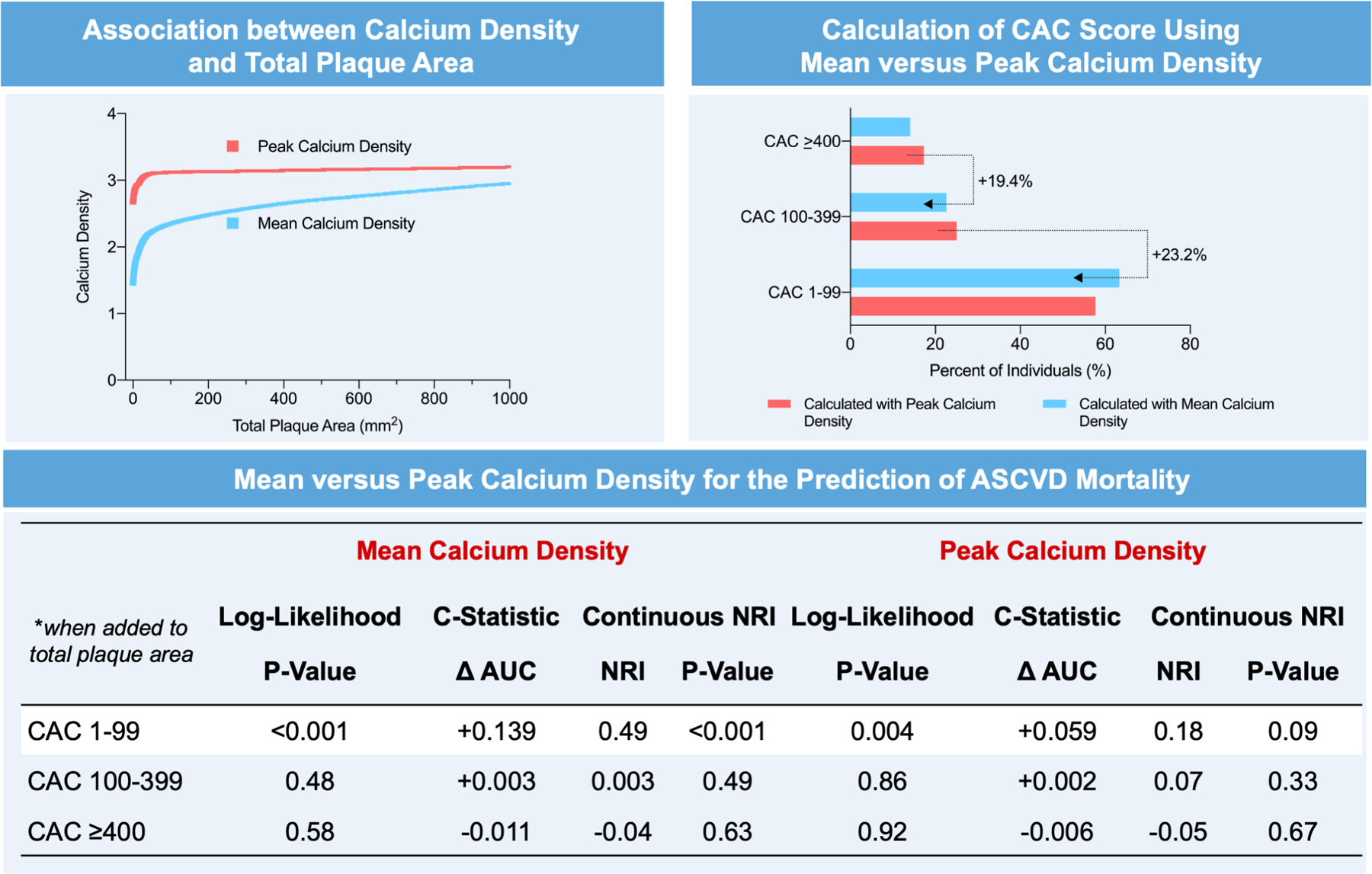
Mean and peak calcium density are most strongly dissimilar among individuals with a total plaque area <100 mm2, and approximately 25% of individuals with an Agatston CAC score of 100–399 are downwardly reclassified into a CAC score group of 1–99 when scoring occurs with mean instead of peak calcium density. Mean calcium density performs better than peak calcium density for the prediction of ASCVD mortality for individuals with CAC 1–99.
Figure 5. Summary of differences and potential applications of mean versus peak calcium density.
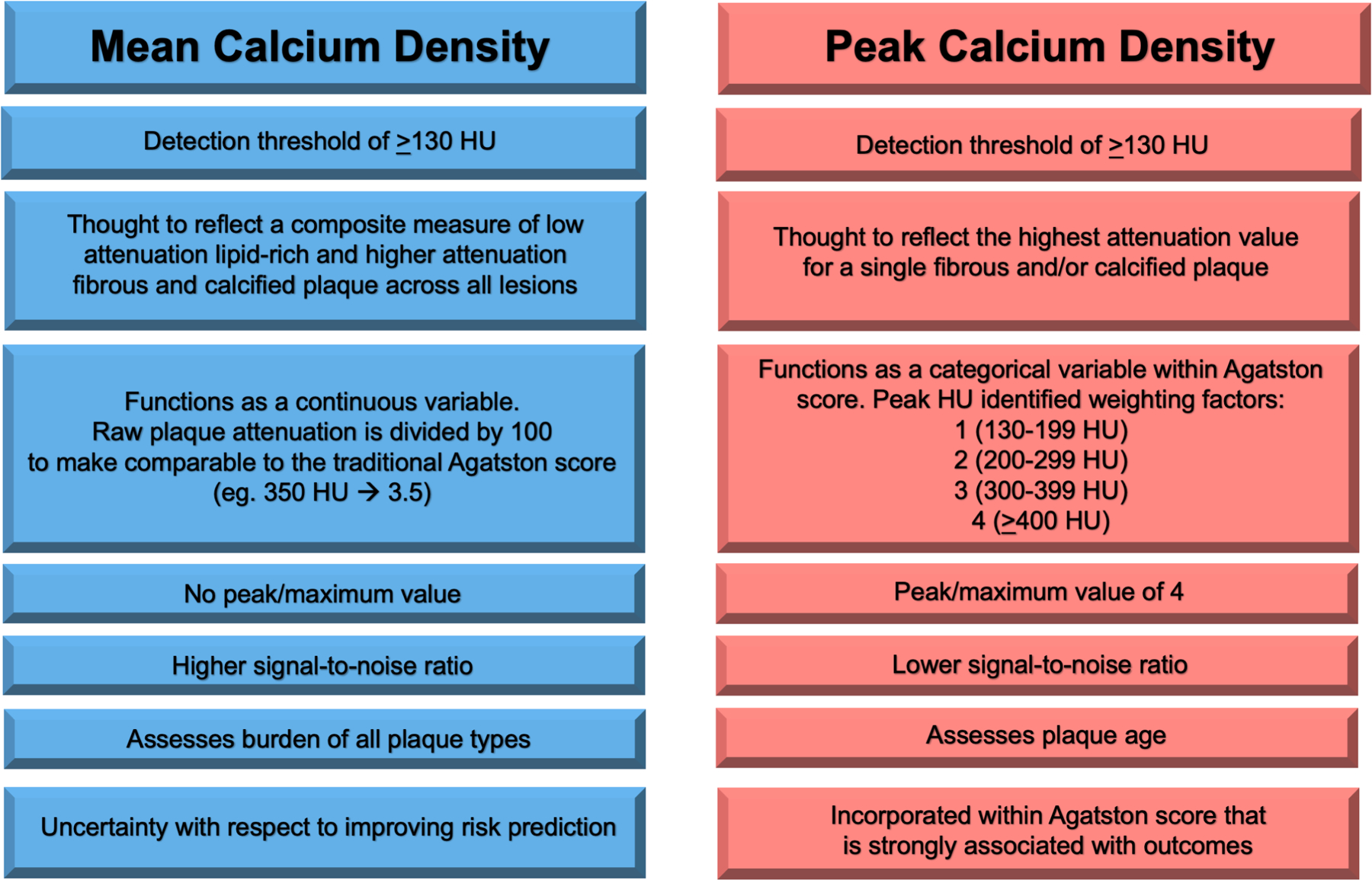
Mean calcium density versus peak calcium density.
Mean and peak calcium density differed by approximately one full density category/unit for young adults and those with a modest total coronary plaque area burden, though heterogeneity between the two density values was reduced among older age groups and those with more advanced CHD. These findings demonstrate that mean and peak calcium density have large differences during the early development of atherosclerosis and that mean calcium density may more precisely reflect plaque biology and vulnerability during this initial stage. Coronary plaques with low calcium density are susceptible to vascular events due their extensive lipid cores and positive remodeling, while fibrocalcific plaques have higher calcium density reflecting overall stability(15–17). However, calcium density varies across coronary lesions and within individual plaques themselves(5). For example, intravascular ultrasound studies demonstrate that more than 50% of coronary plaques have at least two different remodeling patterns along distinct locations of individual lesions(18). Utilization of the average peak calcium density of all coronary plaques may thus lead to an overestimation of CAC and risk for persons with a low total plaque area burden. Inferring the density of plaques from the location of maximum attenuation may be an imprecise approach that may mischaracterize plaque susceptibility, especially during the initial atherosclerosis process. On the other hand, mean calcium density, at both the individual lesion and overall composite levels, has the opportunity be a more reliable measure that is less prone to signal noise for comprehensively assessing susceptibility for vascular events and quantifying CAC scores for risk stratification among persons who have early/asymptomatic CHD.
There was an overall weak correlation between mean and peak calcium density, which considerably decreased across higher CAC scores and total coronary plaque area burden. The calcium density integer scale involved in Agatston scoring is a probable explanation for a very low correlation between mean and peak calcium density among individuals with CAC 100–400 (r=0.04) and CAC >400 (r=0.08). The Agatston calcium density weighting factor categorizes all plaques with an attenuation >400 HU as the same numerically(2), thus the very weak correlation between mean calcium and peak calcium density at higher CAC score ranges can likely be attributed to the limited variance of calcium density values among such individuals. For example, the current Agatston scoring algorithm categorizes peak calcium density values of 400 HU and 1000 HU in the same quantized density factor level. Likewise, mean and peak calcium density became further uncorrelated as total plaque area burden increased, which could be due to the ceiling threshold of the density weighting factor.
One major clinical implication of our findings may be the reclassification and shift towards lower CAC score groups when quantifying CAC with mean calcium density rather than peak calcium density. Using this approach, approximately 25% of participants with a traditional Agatston CAC score 100–399 were reclassified with CAC 1–99, and nearly 20% moved from Agatston CAC >400 to a new CAC between 100–399. These results are important because a majority of ASCVD risk stratification occurs among individuals with lower CAC scores(4,19), as CAC >100 has demonstrated to be an important discriminatory threshold for primary versus secondary prevention risk(20). For example, individuals with CAC >100 appear to derive net benefit from aspirin therapy, whereas the risk for bleeding events is larger in magnitude than the reduction in primary ASCVD events for individuals with prevalent CAC below 100 (21,22).
When added to models including total coronary plaque area, mean calcium density performed better than peak calcium density for long-term ASCVD mortality prediction among persons with CAC 1–99. Specifically, the addition of mean calcium density strongly improved ASCVD mortality reclassification among individuals with CAC 1–99 and for individuals in the lowest total plaque area tertile, while no significant NRI statistics were observed for models including peak calcium density among the two latter subgroups. These observations were further followed by a larger improvement in CHD mortality discrimination for the addition of mean versus peak calcium density among those with CAC 1–99. Previous studies have shown that calcium density is inversely associated with incident ASCVD and that supplementing coronary plaque area and/or CAC volume measures with calcium density improves risk prediction for ASCVD events, particular among persons with an intermediate risk(6,7).
Here, we show that calcium density is positively associated with ASCVD and CHD mortality when adjusting for age and sex alone. However, we subsequently show that calcium density is negatively associated with ASCVD and CHD mortality after additionally accounting for total plaque area. These results may be explained by the concept that calcium density is strongly correlated with age (and likely atherosclerotic plaque age). We also further build on previous findings and demonstrate that the predictive utility of calcium density for ASCVD mortality is most valuable among persons with CAC <100 and is more effectively leveraged using mean rather than peak calcium density measures. Overall, our results raise the question as to whether a new CAC score which incorporates different imaging metrics, such as mean calcium density, the number of affected vessels, and/or the location of calcified plaque, would help to improve ASCVD risk assessment.
Observations in the current study may have important cardiovascular imaging implications, which may help to further refine CAC scores in the future. In particular, there may be a utility to remeasuring CAC data from raw Digital Imaging and Communications in Medicine (DICOM) data in specific intermediate-high risk patient groups, such as those with hypercholesterolemia, diabetes, and/or a family history of CHD. Directly remeasuring mean calcium density per-vessel, lesion size, vessel diffusivity index, and the geographic location/distribution of calcific plaques may provide further insight into the imaging-based diagnosis and risk assessment of CHD. Furthermore, linking these new imaging metrics to ASCVD outcomes and event data would be able to inform the generation of more comprehensive CAC scores for risk assessment. For example, current CAC scoring systems distribute equal weight for a given calcium density and plaque area without considering the location of such atherosclerotic lesions, even though left main CAC is more strongly associated with ASCVD and all-cause mortality compared to non-left main CAC (23).
The main strengths of our study include a novel and relevant study design for assessing the imaging and prognostic implications between mean versus peak coronary calcium density among over 10,000 individuals. To our knowledge, we are among the first studies to compare the predictive value of mean versus peak calcium density on ASCVD mortality outcomes. Our data suggest that there may be several different prognostic components within the calcium density metric itself, and that further studies are required before broadly concluding that higher calcium density is universally protective. As the methodology of CAC scoring continues to evolve, our study findings are likely to be helpful for ASCVD risk stratification among persons with early/asymptomatic disease, which will be especially important for primary prevention purposes.
Our study findings should be interpreted in the setting of certain limitations. Due to limitations in obtaining raw CT images for each study participant, we compared measured composite mean calcium density to calculated average peak calcium density values for all lesions rather than on a per-lesion basis. This may have introduced a certain degree of misclassification bias for peak calcium density, as only direct measurement of peak calcium density from the raw images would have enabled modeling of peak density across the entire range of Hounsfield Units; however, it should be noted that conventional Agatston scoring also does not consider peak density as a continuous variable. Likewise, total plaque area was also back calculated from individual Agatston scores for each participant. Future studies that can prospectively and directly measure both mean and peak calcium density per-lesion in the setting of ASCVD event and mortality data will be beneficial to build on our findings and further enhance CAC scores for risk assessment among patients. Furthermore, the Agatston CAC score incorporates peak calcium density but not mean calcium density, which confers complexity to our interpretation of results when assessing the ASCVD and CHD predictive utility of mean and peak calcium density when stratifying by CAC burden. However, mean calcium density also generally performed better than peak calcium density when similarly stratifying by total plaque area, suggesting consistency in our results. Although the interpretation of the highly correlated mean and peak calcium density measures will undoubtedly continue to be challenging, assessment of their differences in risk prediction is very important to potentially help refine CAC scoring for ASCVD risk assessment and advance our knowledge of plaque biology. Additionally, minority populations including African Americans, Asians and Hispanics were underrepresented in the current study and subsequent studies evaluating the roles of mean versus peak calcium density in ASCVD risk prediction among diverse populations should be pursued.
In conclusion, mean and peak calcium density have dissimilar values most notably among individuals with prevalent CAC <100, which suggests that the two calcium density components may uniquely describe plaque composition, particularly early in the atherosclerotic process. When added to total coronary plaque area, mean calcium density performs better than peak calcium density for the prediction of ASCVD mortality among persons with CAC 1–99, suggesting that CAC quantification using mean calcium density for persons with early subclinical coronary atherosclerosis may help to inform new CAC score development for ASCVD risk assessment.
Supplementary Material
Clinical Perspectives.
Competency in Medical Knowledge:
Mean and peak calcium density may reflect unique atherosclerotic processes and have strongly dissimilar values during the early development of CHD, such that approximately 25% of individuals with an Agatston CAC score of 100–399 are downwardly reclassified into a CAC score group of 1–99 when scoring occurs with mean instead of peak calcium density. Mean calcium density performs better than peak calcium density for the prediction of ASCVD mortality for individuals with CAC 1–99, suggesting that CAC quantification using mean calcium density may more accurately assess risk and guide preventive care for persons with early subclinical coronary atherosclerosis.
Translational Outlook:
Additional studies are required to confirm the prognostic advantage of mean versus peak calcium density on a per-lesion basis for CAC scoring and ASCVD mortality risk prediction among persons with early subclinical coronary atherosclerosis.
Acknowledgements:
The authors thank the other investigators, the staff, and the participants of the CAC Consortium for their valuable contributions.
Sources of Funding:
This project was supported in part by a research grant from the National Institutes of Health (NIH)-National Heart, Lung, and Blood Institute (NHLBI) [L30 HL110027].
Disclosures:
Michael Blaha reports grants from the National Institutes of Health, US Food and Drug Administration, American Heart Association, and Aetna Foundation; grants and personal fees from Amgen; and personal fees from Sanofi, Regeneron, Novartis, Bayer, and Novo Nordisk outside the submitted work. No other disclosure for the other authors are reported. None of the other authors have any conflict of interest.
Abbreviations:
- AU
Agatston units
- AUC
area under the curve
- ASCVD
atherosclerotic cardiovascular disease
- CAC
coronary artery calcification
- CHD
coronary heart disease
- HU
Hounsfield units
- NRI
net reclassification index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. J Am Coll Cardiol. 2019;74(10):e177–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990. Mar 15;15(4):827–32. [DOI] [PubMed] [Google Scholar]
- 3.Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the Vulnerable Plaque. Journal of the American College of Cardiology. 2006. [DOI] [PubMed] [Google Scholar]
- 4.Blaha MJ, Mortensen MB, Kianoush S, Tota-Maharaj R, Cainzos-Achirica M. Coronary Artery Calcium Scoring: Is It Time for a Change in Methodology? JACC: Cardiovascular Imaging. 2017. [DOI] [PubMed] [Google Scholar]
- 5.Zaromytidou M, Antoniadis AP, Siasos G, Coskun AU, Andreou I, Papafaklis MI, et al. Heterogeneity of Coronary Plaque Morphology and Natural History: Current Understanding and Clinical Significance. Current Atherosclerosis Reports. 2016. [DOI] [PubMed] [Google Scholar]
- 6.Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA - J Am Med Assoc. 2014; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Criqui MH, Knox JB, Denenberg JO, Forbang NI, McClelland RL, Novotny TE, et al. Coronary Artery Calcium Volume and Density: Potential Interactions and Overall Predictive Value: The Multi-Ethnic Study of Atherosclerosis. JACC Cardiovasc Imaging. 2017;10(8):845–54. [DOI] [PubMed] [Google Scholar]
- 8.Van Rosendael AR, Narula J, Lin FY, Van Den Hoogen IJ, Gianni U, Al Hussein Alawamlh O, et al. Association of High-Density Calcified 1K Plaque with Risk of Acute Coronary Syndrome. JAMA Cardiol. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blaha MJ, Whelton SP, Al Rifai M, Dardari ZA, Shaw LJ, Al-Mallah MH, et al. Rationale and design of the coronary artery calcium consortium: A multicenter cohort study. J Cardiovasc Comput Tomogr. 2017;11(1):54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mao SS, Pal RS, McKay CR, Gao YG, Gopal A, Ahmadi N, et al. Comparison of coronary artery calcium scores between electron beam computed tomography and 64-multidetector computed tomographic scanner. J Comput Assist Tomogr. 2009; [DOI] [PubMed] [Google Scholar]
- 11.Al-Mallah MH, Keteyian SJ, Brawner CA, Whelton S, Blaha MJ. Rationale and design of the henry ford exercise testing project (the FIT project). Clin Cardiol. 2014; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leening MJG, Vedder MM, Witteman JCM, Pencina MJ, Steyerberg EW. Net reclassification improvement: Computation, interpretation, and controversies: A literature review and clinician’s guide. Annals of Internal Medicine. 2014. [DOI] [PubMed] [Google Scholar]
- 13.Cook NR. Quantifying the added value of new biomarkers: how and how not. Diagnostic Progn Res. 2018; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uno H, Cai T, Pencina MJ, D’Agostino RB, Wei LJ. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med. 2011; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shemesh J, Apter S, Itzchak Y, Motro M. Coronary calcification compared in patients with acute versus in those with chronic coronary events by using dual-sector spiral CT. Radiology. 2003; [DOI] [PubMed] [Google Scholar]
- 16.Hou ZH, Lu B, Gao Y, Jiang SL, Wang Y, Li W, et al. Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc Imaging. 2012; [DOI] [PubMed] [Google Scholar]
- 17.Motoyama S, Kondo T, Sarai M, Sugiura A, Harigaya H, Sato T, et al. Multislice Computed Tomographic Characteristics of Coronary Lesions in Acute Coronary Syndromes. J Am Coll Cardiol. 2007; [DOI] [PubMed] [Google Scholar]
- 18.Stone PH, Saito S, Takahashi S, Makita Y, Nakamura S, Kawasaki T, et al. Prediction of progression of coronary artery disease and clinical outcomes using vascular profiling of endothelial shear stress and arterial plaque characteristics: The PREDICTION study. Circulation. 2012; [DOI] [PubMed] [Google Scholar]
- 19.Blaha MJ. Predicting the Age of Conversion to CAC >0: A Role for Polygenic Risk Scores? J Am Coll Cardiol. 2021;S1936–878X(20):31092–5. [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N, Blumenthal RS, et al. Coronary Calcium Predicts Events Better With Absolute Calcium Scores Than Age-Sex-Race/Ethnicity Percentiles. MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2009;53(4):345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ajufo E, Ayers CR, Vigen R, Joshi PH, Rohatgi A, De Lemos JA, et al. Value of Coronary Artery Calcium Scanning in Association with the Net Benefit of Aspirin in Primary Prevention of Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: Estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lahti SJ, Feldman DI, Dardari Z, Mirbolouk M, Orimoloye OA, Osei AD, et al. The association between left main coronary artery calcium and cardiovascular-specific and total mortality: The Coronary Artery Calcium Consortium. Atherosclerosis. 2019; [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


