Abstract
Objective:
The social and economic burden of eating disorders is significant and often financially devastating. Medicare is the largest public insurer in the United States and provides coverage for older adults and some disabled individuals. This study explores prevalence, sociodemographic and clinical characteristics, and health care spending for Medicare enrollees with eating disorders.
Method:
A cross-sectional study was conducted with the nationally representative 20% sample of 2016 Medicare inpatient, outpatient, carrier, and home health fee-for-service claims and Medicare Advantage encounter records. Sociodemographic characteristics and comorbid somatic conditions were compared between individuals with versus without an eating disorder diagnosis. Mean spending was compared overall and separately for inpatient, outpatient, home health, and pharmacy claims.
Results:
The sample included 11,962,287 Medicare enrollees of whom 0.15% had an eating disorder diagnosis. Compared to those without a 2016 eating disorder diagnosis, a greater proportion of individuals with an eating disorder were female (73.8% vs. 54.3%), under age 65 (41.6% vs. 15.5%), and dually eligible for Medicaid due to disability or low-income qualification (48.0% vs. 19.6%). Individuals with eating disorders had higher rates of comorbid conditions, with the greatest differences in cardiac arrythmias (35.3% vs. 19.9%), arthritis (40.1% vs. 26.6%), and thyroid conditions (32.2% vs. 19.4%). Spending was higher for enrollees with eating disorders compared to those without overall ($29,456 vs. $7,418) and across settings.
Discussion:
The findings establish that eating disorders occur in the Medicare population, and that enrollees with these illnesses have risk factors associated with significant healthcare spending and adverse health outcomes.
Keywords: anorexia nervosa, binge-eating disorder, bulimia nervosa, eating disorders, healthcare costs, health expenditures, health insurance, health policy, Medicare
1 |. INTRODUCTION
Eating disorders are serious psychiatric illnesses with significant morbidity and mortality (Halmi, 2018; Mehler, 2018; Mitchell, 2016). Among the somatic comorbidities of these conditions are cardiac complications including sudden cardiac death, impaired gastrointestinal and liver function, and reduced bone density (Mehler, 2018). Psychiatric comorbidities include affective disorders, anxiety disorders, and substance use disorders (Halmi, 2018). The social and economic burden associated with eating disorders is significant and can be financially devastating to individuals and families.
Research on the cost of eating disorders includes both cost-of-illness studies and those limited to healthcare expenditures. A systematic review by Stuhldreher et al. (2012) and subsequent studies across the globe (Bellows et al., 2015; de Oliveira, Colton, Cheng, Olmsted, & Kurdyak, 2017; Gatt et al., 2014; Lee, Hong, Park, Kang, & Oh, 2021; Samnaliev, Noh, Sonneville, & Austin, 2014; Streatfeild et al., 2021; Tseng, Tu, & Chang, 2021; Watson et al., 2018) found that the costs related to eating disorders are substantial, burdensome, and likely underestimated. In the United States, Streatfeild et al. (2021)’s cost-of-illness study conservatively estimated the annual cost of eating disorders at $64.7 billion—approximately $11,800 per affected individual. This cost was calculated from a societal perspective, incorporating both direct costs such as healthcare spending, and indirect costs such as lost productivity and lost well-being. Although cost-of-illness studies estimate mean costs per affected individual, in the U.S. prices for healthcare services are negotiated between providers and insurers resulting in different costs for the same services depending on the payer. In addition, across payers there are differences in how much of the cost is borne by enrollees due to different copayment and coinsurance amounts.
American health insurance includes commercial plans and government-funded coverage. The two largest government programs are Medicaid and Medicare. Medicaid provides insurance primarily for low-income individuals. Medicare is a federal insurance program that covers adults aged 65 and older and provides coverage for qualifying individuals of any age with disabilities and those with end-stage renal disease. Approximately 85% of Medicare enrollees qualify based on age, and 15% based on disability status (Kaiser Family Foundation, 2021). When enrolling in Medicare, individuals either select traditional fee-for-service Medicare coverage administered by the federal government, or a Medicare Advantage (MA) plan managed by private insurance companies (Kaiser Family Foundation, 2019). There are also individuals enrolled in Medicare who qualify for Medicaid referred to as “dually eligible.” Individuals may become dually eligible either by qualifying for Medicare first and then Medicaid, or vice versa. Approximately 18% of all Medicare enrollees are dually eligible for Medicaid (Medicare-Medicaid Coordination Office, 2020a).
To date, U.S.-based health services research examining direct healthcare spending for people with eating disorders has been primarily conducted in commercially insured populations (Dickerson et al., 2011; Huskamp et al., 2018; Mitchell et al., 2009; Striegel-Moore et al., 2005; Striegel-Moore, Leslie, Petrill, Garvin, & Rosenheck, 2000). Findings from those data include sustained increased healthcare costs for people with eating disorders following diagnosis compared to those without (Mitchell et al., 2009), and increased outpatient service utilization following a change in federal mental health policy that went into effect in 2010 (Huskamp et al., 2018). As a result of prior research focusing on the commercially insured, individuals aged 65 and older, low-income individuals, and those with significant disability are typically excluded. Prior research has established that increasing age is associated with increasing numbers of comorbid conditions as well as healthcare utilization and spending. In addition, in a 2011 study of Medicare enrollees, Joynt et al. found that a greater percentage of high-cost individuals (those in the highest 10% of spending) were originally eligible for Medicare due to receipt of disability insurance benefits (instead of age) than nonhigh-cost enrollees (33.7% vs. 24.2%). The median number of chronic conditions was also higher among high-cost enrollees (11.0 vs. 6.0) (Joynt et al., 2016). Understanding total spending (combined spending by the government and by enrollees) for those insured through Medicare is especially critical as their age or disability status may make them high-cost, high-need enrollees and increase the extent to which they experience the morbidity and financial effects of eating disorders.
Three clinical profiles of eating disorders have been noted in the older adult population—early-onset, chronic course without previous recovery; relapse after a period of remission; and late onset without a prior eating disorder diagnosis (Baker & Runfola, 2016). In a review of the literature on eating disorders in middle-age and older adults, Mangweth-Matzek and Hoek (2017) found that while eating disorders occur among older adults, there are few studies that capture incidence and prevalence. In addition, there is a dearth of research on the potential compounding effects of eating disorders and the aging process on morbidity and mortality.
To explore the occurrence of eating disorders within the Medicare population we identified three primary research questions; (a) What is the prevalence of eating disorder diagnoses among Medicare enrollees? (b) How do the sociodemographic and clinical characteristics compare between Medicare enrollees with and without an eating disorder diagnosis? (c) How does healthcare spending for individuals with eating disorders compare to those without eating disorders across the inpatient, outpatient, home health, and pharmacy settings?
2 |. METHODS
To address our research questions, we performed an exploratory, descriptive cross-sectional study with the nationally representative 20% sample of 2016 Medicare inpatient, outpatient, carrier, pharmacy and home health fee-for-service claims and MA encounter records.
2.1 |. Data
The data used in this study include individuals enrolled in fee-for-service Medicare and MA plans from 2016 obtained through the Research Data Assistance Center. The Medicare fee-for-service data is comprised of a 20% nationally representative sample of individuals that includes claims for covered services in inpatient, outpatient, carrier, and home health, settings. These files contain patient demographic information including Medicaid dual eligibility status, diagnosis and procedure codes, dates of service, charged dollar amounts, amounts paid, and provider information such as National Provider Identification numbers. Providers submit this information directly to the Centers for Medicare and Medicaid Services (CMS).
The MA data is from encounter records that also include inpatient, outpatient, carrier and home health settings. These data include similar information to the fee-for-service data, but do not include payment information. The information in these records is submitted by the MA Organizations (who sponsor the privately managed plans) rather than by providers. For both fee-for-service Medicare and MA enrollees with Part D prescription drug coverage, the data also include pharmacy claims.
2.2 |. Sample
The total sample included 11,962,287 individuals, 8,028,870 enrolled in fee-for-service Medicare and 3,933,417 enrolled in MA plans. Individuals with eating disorders were identified as those with one or more claims or encounters with a diagnosis of anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), other specified feeding or eating disorder (OSFED), and other unspecified feeding or eating disorder (OUSFED). Diagnoses were identified in the data using ICD-10 codes, F50.0x for AN, F50.2x for BN, F50.81 for BED, F50.8x for OSFED (excluding F50.81), and F50.9 for OUSFED. We considered diagnosis codes in any position on the outpatient, inpatient, carrier, and home health claims and encounter records.
2.3 |. Analysis
We compared sociodemographic characteristics and comorbid somatic conditions for individuals with versus without an eating disorder diagnosis. Sociodemographic characteristics examined include sex, age category (<40 years, 40–54 years, 55–65 years, 65–74 years and 75+ years), race, enrollment in MA, and dual eligibility for Medicaid. The presence of comorbid conditions was summarized using the Elixhauser Comorbidity Index (Elixhauser, Steiner, Harris, & Coffey, 1998). The current version of this measure includes 31 categories of comorbid conditions that are dichotomously indicated as present or not present. Higher scores on this index indicate a greater number of comorbid conditions.
We also examined the presence of specific comorbid gastrointestinal, cardiovascular, musculoskeletal, and endocrine conditions, comparing those with an eating disorder to those without, and by eating disorder diagnosis. A list of diagnosis codes can be found in Appendix A. We then stratified the results by age category to assess differences in the number and type of comorbid conditions within age categories among those with and without eating disorders.
To compare total spending between individuals with and without an eating disorder diagnosis, we calculated mean total spending, as well as mean inpatient, outpatient, home health, and pharmacy spending. Since we required some contact with the medical system to identify individuals with an eating disorder diagnosis, we also compared spending for individuals with an eating disorder diagnosis to spending for the subset of individuals without an eating disorder diagnosis with at least one medical or pharmacy claim. These calculations were conducted only for Medicare fee-for-service enrollees, as the MA encounter records do not contain payment information.
We used Pearson χ2 tests to compare proportions of categorical variables and two-sided t-tests to compare means. We considered differences to be statistically significant if p values were below .05. This study was approved by the Johns Hopkins Bloomberg School of Public Health IRB (approval #11318). Data were extracted using SAS 9.4 and all analyses were conducted in Stata 16.
3 |. RESULTS
Of the total 2016 sample, 0.15% had an eating disorder diagnosis. Compared to those without an eating disorder, a greater proportion of individuals with an eating disorder diagnosis were female (73.8% vs. 54.3%, p < .01), under age 65 (41.6% vs. 15.5%, p < .01), and dually eligible for Medicaid due to disability or low-income qualification (48.0% vs. 19.6%, p < .01) (Table 1). Of those with an eating disorder, demographic characteristics varied across diagnoses. People with BN were the youngest, with 73.9% under age 65, and 22.9% under age 40. This was followed by BED with 60.9% under age 65. Individuals with OSFED were the oldest with 36.5% over age 75 closely followed by those with AN with 35.4%. Dual eligibility for Medicaid was highest among people with BN (58.4%) and AN (50.4%).
TABLE 1.
Demographic characteristics of individuals with and without eating disorder diagnoses in the 2016 20% sample of fee-for-service Medicare claims and Medicare Advantage encounter data
| By eating disorder diagnosis |
|||||||
|---|---|---|---|---|---|---|---|
| No ED N = 11,944,313 |
Any ED N = 17,974 |
AN N = 3,223 |
BN N = 1,650 |
BED N = 793 |
OSFED N = 7,510 |
OUSFED N = 6,959 |
|
| Enrolled in Medicare Advantage (%) | 32.9% | 31.1%** | 30.2% | 30.4% | 30.8% | 29.6% | 31.7% |
| Female (%) | 54.3% | 73.8%** | 79.8% | 86.6% | 81.1% | 71.0% | 73.7% |
| Age (%) | |||||||
| <40 years | 2.2% | 9.6%** | 11.4% | 22.9% | 12.9% | 7.3% | 11.4% |
| 40–54 years | 5.2% | 17.3%** | 17.4% | 33.7% | 26.2% | 14.4% | 19.2% |
| 55–64 years | 8.2% | 14.7%** | 13.9% | 17.3% | 21.8% | 14.1% | 15.8% |
| 65–74 years | 48.3% | 26.9%** | 21.9% | 19.0% | 32.0% | 27.8% | 28.3% |
| 75+ years | 36.2% | 31.6%** | 35.4% | 7.1% | 7.1% | 36.5% | 25.4% |
| Dual eligible (%) | 19.6% | 48.0%** | 50.4% | 58.4% | 44.5% | 46.3% | 48.7% |
| Race (%) | |||||||
| White | 74.6% | 73.9%* | 77.2% | 80.7% | 82.9% | 72.1% | 74.6% |
| Black | 10.4% | 13.1%** | 8.9% | 7.8% | 7.9% | 15.0% | 12.9% |
| Hispanic | 9.0% | 8.7% | 8.9% | 6.8% | 5.7% | 8.8% | 8.2% |
| Other/unknown | 5.9% | 4.3%** | 5.0% | 4.7% | 3.5% | 4.2% | 4.3% |
Note: This table reports the percent of individuals for each column that meet the row demographic or clinical characteristic. For example, 32.9% of individuals without an eating disorder diagnosis were enrolled in Medicare Advantage.
p ≤ .05
p ≤ .01 statistically significant difference within row for individuals with any eating disorder diagnosis compared to individuals without. We used Pearson χ2 tests to compare proportions.
Abbreviations: AN, anorexia nervosa; BN, bulimia nervosa; BED, binge-eating disorder; OSFED, other specified feeding or eating disorder; OUSFED, other unspecified feeding or eating disorder.
3.1 |. Comorbid conditions
A greater proportion of individuals with an eating disorder diagnosis had a high (six or greater) Elixhauser Comorbidity Index score compared to individuals without an eating disorder diagnosis (54.3% vs. 21.7%, p < .01) (Table 2). More than 50% of individuals with OSFED (56.3%), OUSFED (55.4%), and AN (52.5%) had high scores on the Elixhauser Comorbidity Index. A larger proportion of individuals with eating disorders, compared to those without, had each of the specifically examined conditions during 2016. The greatest percentage point differences between people with eating disorders and those without were in cardiac arrythmias (35.3% vs. 19.9%, p < .05), arthritis (40.1% vs. 26.6%, p < .05) and thyroid conditions (32.2% vs. 19.4%, p < .05). Approximately twice the number of people with eating disorders had heart attacks compared to those without (3.7% vs. 1.9%, p < .01), and 3.2 times as many had irritable bowel syndrome (6.7% vs. 2.1%, p < .01) (Table 2).
TABLE 2.
Comorbid somatic conditions of individuals with and without eating disorders
| By eating disorder diagnosis |
|||||||
|---|---|---|---|---|---|---|---|
| No ED N = 11,944,313 |
Any ED N = 17,974 |
AN N = 3,223 |
BN N = 1,650 |
BED N = 793 |
OSFED N = 7,510 |
OUSFED N = 6,959 |
|
| Mean Elixhauser Comorbidity Index score (SD) | 1.7 (0.8) | 2.4 (0.7)** | 2.4 (0.8) | 2.2 (0.8) | 2.2 (0.7) | 2.4 (0.7) | 2.4 (0.7) |
| Elixhauser Comorbidity Index score (%) | |||||||
| Low (0–2) | 48.4% | 14.8%** | 16.8% | 22.8% | 20.4% | 13.1% | 13.6% |
| Medium (3–5) | 29.9% | 30.9%** | 30.7% | 38.4% | 40.7% | 30.6% | 31.0% |
| High (6+) | 21.7% | 54.3%** | 52.5% | 38.8% | 38.8% | 56.3% | 55.4% |
| Gastrointestinal | |||||||
| Irritable bowel syndrome | 2.1% | 6.7%** | 9.3% | 11.7% | 7.4% | 5.7% | 6.9% |
| Celiac disease | <1% | <1% | <1% | 1.1% | 1.3% | <1% | <1% |
| Gluten sensitivity | <1% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% | 0.0% |
| Barrett’s esophagus | <1% | <1% | <1% | 0.2% | 0.0% | <1% | <1% |
| Ulcerative colitis | <1% | 1.2%** | 1.5% | 1.1% | 0.9% | 1.3% | 1.1% |
| Cardiovascular | |||||||
| Heart arrythmia | 19.9% | 35.3%* | 37.1% | 23.6% | 18.0% | 36.3% | 35.8% |
| High cholesterol | 57.0% | 61.1%* | 51.9% | 47.3% | 61.8% | 64.5% | 61.3% |
| Heart attack | 1.9% | 3.7%** | 3.8% | 1.7% | <1% | 3.9% | 3.7% |
| Musculoskeletal | |||||||
| Arthritis | 26.6% | 40.1%* | 35.5% | 28.1% | 40.2% | 41.7% | 41.0% |
| Osteopenia | 5.0% | 6.1%** | 7.1% | 6.9% | 5.8% | 6.2% | 5.5% |
| Osteoporosis | 10.0% | 16.3%* | 24.4% | 13.5% | 9.6% | 15.9% | 14.1% |
| Hip fracture | <1% | <1% | <1% | 0.4% | 0.0% | <1% | <1% |
| Endocrine | |||||||
| Thyroid disease | 19.4% | 32.2%* | 33.0% | 29.8% | 31.9% | 32.7% | 31.4% |
| Diabetes | 27.6% | 38.1%* | 26.5% | 25.2% | 41.4% | 41.5% | 39.8% |
Note: This table reports the percent of individuals for each column that have a diagnosis of the row somatic condition. For example, 2.1% of individuals without an eating disorder diagnosis had a diagnosis of irritable bowel syndrome. We calculated Elixhauser Comorbidity Index scores based on outpatient, inpatient, and carrier/encounter records.
p ≤ .05
p ≤ .01 statistically significant difference within row for individuals with any eating disorder diagnosis compared to individuals without. We used Pearson χ2 tests to compare proportions and two-sided t-tests to compare means. We do not report statistically significant differences for rows where the prevalence of the condition is below 1% both for individuals with any eating disorder diagnosis and individuals without.
Abbreviations: AN, anorexia nervosa; BN, bulimia nervosa; BED, binge-eating disorder; OSFED, other specified feeding or eating disorder; OUSFED, other unspecified feeding or eating disorder.
When stratified by age group, a higher proportion of individuals with eating disorders had irritable bowel syndrome, heart arrythmias, high cholesterol, arthritis, osteoporosis, thyroid disease, and diabetes across all ages (Table 3). There was no difference in occurrence of heart attacks between individuals with and without eating disorders in those under age 40 and between ages 40 and 54, but approximately 2.3 times as many people over 75 with eating disorders had heart attacks than those without eating disorders (6.4% vs. 2.8%, p < .01).
TABLE 3.
Comparison of comorbid somatic conditions of individuals with and without eating disorders by age group
| <40 years |
40–54 years |
55–64 years |
65–74 years |
75+ years |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No ED | Any ED | No ED | Any ED | No ED | Any ED | No ED | Any ED | No ED | Any ED | |
| n = 257,943 | n = 1,720 | n = 619,823 | n = 3,104 | n = 974,837 | n = 2,646 | n = 5,772,442 | n = 4,833 | n = 4,319,268 | n = 5,671 | |
| Gastrointestinal | ||||||||||
| Irritable bowel syndrome | 2.0% | 10.5%** | 2.7% | 9.7%** | 2.5% | 8.5%** | 1.9% | 5.6%** | 2.1% | 3.9%** |
| Celiac disease | <1% | <1% | <1% | 0.7%** | <1% | <1% | <1% | <1% | <1% | <1% |
| Gluten sensitivity | <1% | 0% | <1% | 0% | <1% | 0% | <1% | 0% | <1% | 0% |
| Barrett’s esophagus | <1% | <1% | <1% | <1% | <1% | 0% | <1% | <1% | <1% | <1% |
| Ulcerative colitis | <1% | 1.4%** | <1% | <1% | <1% | 1.1%** | <1% | 1.3%** | <1% | 1.3%** |
| Cardiovascular | ||||||||||
| Heart arrythmia | 8.8% | 24.1%** | 11.9% | 22.5%** | 15.4% | 27.3%** | 13.9% | 31.8%** | 30.9% | 52.5%** |
| High cholesterol | 17.8% | 26.6%** | 39.7% | 47.8%** | 52.4% | 63.1%** | 54.8% | 70.3%** | 65.7% | 70.1%** |
| Heart attack | <1% | <1% | 1.3% | 1.3% | 2.1% | 2.7%* | 1.4% | 3.8%** | 2.8% | 6.4%** |
| Musculoskeletal | ||||||||||
| Arthritis | 5.8% | 12.7%** | 18.8% | 30.1%** | 27.5% | 45.4%** | 22.7% | 44.2%** | 33.9% | 47.9%** |
| Osteopenia | <1% | 2.9%** | 1.3% | 3.3%** | 2.8% | 6.3%** | 5.4% | 8.9%** | 5.8% | 6.1% |
| Osteoporosis | 1.1% | 4.6%** | 2.9% | 7.8%** | 6.1% | 15.2%** | 8.1% | 18.6%** | 14.9% | 22.9%** |
| Hip fracture | <1% | <1% | <1% | <1% | <1% | <1% | <1% | <1% | <1% | <1% |
| Endocrine | ||||||||||
| Thyroid disease | 8.9% | 20.1%** | 14.4% | 28.6%** | 17.1% | 33.8%** | 16.5% | 33.3%** | 25.3% | 36.0%** |
| Diabetes | 11.2% | 21.1%** | 25.3% | 31.6%** | 33.6% | 41.4%** | 25.2% | 42.3%** | 30.6% | 41.7%** |
Note: We used Pearson χ2 tests to compare proportions. We do not report statistically significant differences for rows where the prevalence of the condition is below 1% both for individuals with any eating disorder diagnosis and individuals without.
p ≤ .05
p ≤ .01 statistically significant difference by age group within row for individuals with any eating disorder diagnosis compared to individuals without.
3.2 |. Spending
Overall, when combining inpatient, outpatient, home health, and pharmacy expenditures, mean spending for Medicare fee-for-service enrollees with eating disorders ($29,456) was approximately four times greater than for those without eating disorders ($7,418, p < .01) and three times greater than for those without an eating disorder and at least one medical or pharmacy claim ($9,834, p < .01) (Figure 1). For inpatient spending, mean spending for eating disorders was significantly higher than for people without an eating disorder ($12,843 vs. $3,046, p < .01) and for individuals without an eating disorder who had at least one medical or pharmacy claim ($12,843 vs. $4,046, p < .01). Individuals with eating disorders also had higher spending in the outpatient ($9,686), home health ($1,295), and pharmacy claims ($5,638) compared with all other enrollees without an eating disorder ($1,635, $439, and $2,265, all p < .01) and those without an eating disorder who had at least one medical or pharmacy claim ($2,165, $581, and $3,002, all p < .01).
FIGURE 1.
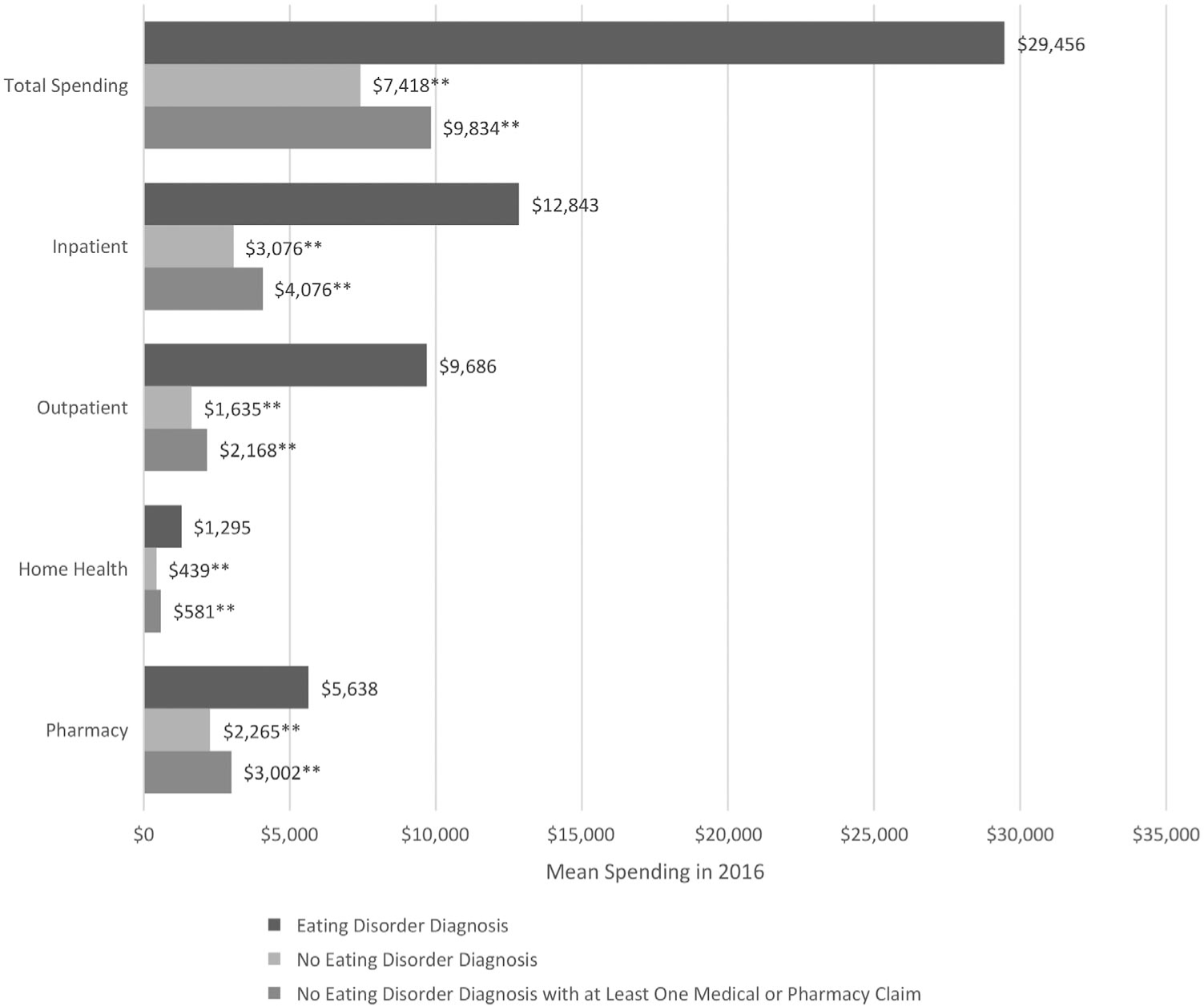
Healthcare spending for fee-for-service Medicare enrollees with an eating disorder diagnosis compared to those without. *p ≤ .05; **p ≤ .01. Statistically significant difference comparing mean spending for individuals with an eating disorder diagnosis (reference group) to those without and to those without who have at least one medical or pharmacy claim
4 |. DISCUSSION
In the United States, Medicare is the largest payer of healthcare services, providing coverage to more than 60 million adults. Historically, eating disorders research has concentrated on adolescents and young adults, such that the occurrence of these conditions is understudied in the Medicare program. This study of the presence and cost of eating disorders within Medicare enrollees finds prevalence similar to commercially-insured populations and higher costs than for those without eating disorders (Striegel-Moore et al., 2000). However, the prevalence is lower than has been found in U.S. population samples (Hudson, Hiripi, Pope, & Kessler, 2007; Udo & Grilo, 2018). Underdiagnosis of eating disorders has been shown to occur among individuals with higher weight status, non-Whites, and males (Sonneville & Lipson, 2018; Strother, Lemberg, Stanford, & Turberville, 2012); population rates may be underestimated in this sample. In addition, while individuals under age 65 comprise roughly 16% of all Medicare enrollees, they represent approximately 42% of enrollees with any eating disorder diagnosis, a reflection of the extent to which many individuals with eating disorders are qualifying for Medicare due to disability status.
Among Medicare enrollees, individuals with eating disorders are medically complex. More than half have greater than six comorbid conditions. Prior research has shown that higher numbers of comorbidities adversely impact survival and increase spending in Medicare enrollees (Fillenbaum, Pieper, Cohen, Cornoni-Huntley, & Guralnik, 2000; Keeney et al., 2020; Kriegsman, Deeg, & Stalman, 2004). Furthermore, eating disorders are associated with elevated mortality. One study of characteristics and survival of individuals with eating disorders found that the leading causes of death were diseases of the respiratory system; followed by injury, poisoning, and certain other consequences of external causes; and diseases of the digestive system (Demmler, Brophy, Marchant, John, & Tan, 2020). Understanding the prevalence of eating disorders in the Medicare population and commonly co-occurring conditions will allow for better identification of high-need cases and care management both by individual clinicians and across specialties.
Compared to enrollees without eating disorders, approximately 2.4 times as many enrollees with eating disorders are dually eligible for Medicare and Medicaid. Generally, dually eligible individuals experience higher rates of chronic illness and many have significant social risk factors for adverse health outcomes (Medicare-Medicaid Coordination Office, 2020b). They also account for a disproportionately high degree of spending. This population also faces bureaucratic challenges with the need to coordinate across the federal Medicare program and state-run Medicaid programs. It is likely that care coordination between Medicare and Medicaid benefits for individuals with eating disorders will be challenging.
Medicare beneficiaries with an eating disorder diagnosis had more than $20,000 higher average healthcare expenditures than their counterparts without an eating disorder diagnosis in 2016. The spending for Medicare enrollees with eating disorders impacts the federal budget and has direct implications for individuals. Out-of-pocket costs for enrollees vary but are typically comprised of premiums, deductibles and subsequent cost-sharing (copayments and coinsurance). Individuals with multiple chronic conditions, at least one inpatient hospitalization, and poorer self-reported health had higher out-of-pocket spending. Cubanski, Koma, Damico, and Neuman (2019) note that for enrollees with five or more chronic conditions 14% of their income was spent on out-of-pocket healthcare costs compared to only 8% among those with no chronic conditions. The increased spending across settings for people with eating disorders, and the higher proportion with greater than six comorbid conditions, suggests high out-of-pocket spending for individuals with eating disorders. While some Medicare enrollees may have supplemental insurance (private insurance plans that cover certain costs not paid by Medicare such as copayments, coinsurance, and deductibles), these costsmay be a significant burden to the individual or family.
The proportion of individuals with most conditions increased with age in those with and without an eating disorder diagnosis. Individuals with eating disorders had higher rates for most conditions across age groups. Momen et al. (2021) found bidirectional risk between eating disorders and 12 categories of general medical conditions including neurological, infectious, immune, respiratory, gastrointestinal, skin, musculoskeletal, genitourinary, circulatory, endocrine, congenital, and injury. Other studies have found associations between eating disorders and gastrointestinal disorders (Santonicola et al., 2019), autoimmune disorders (Raevuori et al., 2014; Zerwas et al., 2017), and cardiovascular disease (Sardar et al., 2015; Tith et al., 2019). Understanding the relationships between somatic conditions and eating disorders could help identify individuals with complex medical and psychiatric needs.
The findings in this study establish that people with eating disorders covered through Medicare are high-cost and medically complex. From a policy perspective, consideration should be given to the ways that Medicare benefit design and coverage do or do not promote access to specialty eating disorder treatment. For example, as of November 2021, Medicare only provides coverage for nutrition services to individuals with diabetes or kidney disease and those who have had a kidney transplant in the previous 36 months (Centers for Medicare & Medicaid Services, 2021b). If an individual with an eating disorder is covered by Medicare, they currently cannot access these services unless they can afford to pay the full cost out of pocket or have additional insurance that covers the cost.
In addition, CMS has explored options for ways to increase quality of care and decrease costs for medically complex, high-cost enrollees. One approach CMS has implemented is care coordination—including accountable care organizations and patient-centered medical homes (Agency for Healthcare Research and Quality, 2021; Centers for Medicare & Medicaid Services, 2021a). Neither model has been specifically tested in an eating disorder population, but both provide mechanisms for clinicians to bill for typically uncompensated care coordination which could improve health outcomes.
There are several strengths of this research. This is one of few studies of eating disorders utilizing healthcare claims data, allowing comparison of expenditures between people with eating disorders and those without. The use of Medicare data provides insight into adults aged 65 and older and those who qualify through disability status, a population that is often excluded from other research. The 20% sample of Medicare data provides a nationally representative sample of Medicare enrollees, and the inclusion of MA encounter data allows us to examine demographics and comorbid conditions of a wider sample that includes those who choose privately managed plans.
The findings need to be considered in light of several limitations. These data came from a single year (2016); prevalence and treatment patterns for people with eating disorders may differ in different years. Furthermore, the data in this study reflect Medicare claims and encounters for services rendered, thus only representing utilization and spending patterns for individuals with at least one claim or encounter with an eating disorder diagnosis. The ICD-10 code for BED is a subcode of OSFED. A relatively large number of individuals received only the main OSFED code, potentially underestimating the occurrence of BED. In order to compare the clinical and sociodemographic profiles of individuals with and without eating disorders we conducted a series of statistical tests. As the number of statistical comparisons increases, so does the possibility of statistically significant results due to chance. However, we addressed this potential limitation by also calculating sharpened false discovery rates and, after applying this false discovery rate correction, found that each of the results reported as statistically significant based on the p value remained statistically significant (Anderson, 2008). Finally, this is one of the first years of MA encounter data released to researchers and it may have missing records.
The findings in this study establish that eating disorders occur in the Medicare population, and that enrollees with these illnesses have risk factors associated with higher spending and adverse health outcomes. Future research should look at patterns of healthcare utilization and spending in individuals with eating disorders across multiple years to better understand the relationship between eating disorders and comorbid somatic conditions. Another important area for future research is access to treatment or this population, including research on acceptance of Medicare by eating disorder specialists across the country, the settings (inpatient hospital, residential, outpatient, etc.) in which patients are receiving care for their eating disorders, the capacity of eating disorder specialists and facilities to accept new patients, and the out-of-pocket costs incurred by patients. Understanding where individuals with eating disorders are obtaining treatment and how insurance coverage impacts their treatment options is crucial to ensuring that they can access appropriate care and minimize adverse health outcomes.
Public significance statement: The present study found that, in 2016, eating disorders occurred in 0.15% of U.S. Medicare enrollees, similar to rates found in commercially-insured populations. These enrollees had more somatic comorbidities and greater spending than enrollees without eating disorders. Further research is needed to assess this population’s access to specialty eating disorder treatment and the trajectory of morbidity and mortality over time.
ACKNOWLEDGMENTS
Dr. Kelly E. Anderson has full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Kelly E. Anderson gratefully acknowledges support from the Agency for Healthcare Research and Quality (T32HS000029). Dr. Rachel Presskreischer gratefully acknowledges support from the National Institute of Mental Health (T32MH109436).
Funding information
National Institute of Mental Health, Grant/Award Number: T32MH109436; Agency for Healthcare Research and Quality, Grant/Award Number: T32HS000029
APPENDIX A: INCLUDED ICD-10 DIAGNOSIS CODES
| Condition | ICD-10 codes |
|---|---|
| Arthritis | M15.x, M16.x, M17.x, M18.x, M19.x |
| Osteopenia | M85.80 |
| Osteoporosis | M80.0x, M80.8x, M81.0, M81.6, M81.8 |
| Hip fracture | M84.459x, M84.359x |
| Irritable bowel syndrome | K58.x |
| Celiac disease | K90.0 |
| Nonceliac gluten sensitivity | K90.41 |
| Barrett’s esophagus | K27.7x |
| Ulcerative colitis/Crohn’s disease | K51.x |
| Heart arrythmia | I44.1–I44.3, I45.6, I45.9, I47.x –I49.x, R00.0, R00.1, R00.8, T82.1, Z45.0, Z95.0 |
| High cholesterol | E78.x |
| Heart attack (MI) | I21.x |
| Thyroid disease | E00.x–E03.x, E89.0 |
| Diabetes mellitus | E10.x, E11.x, E13.x |
Footnotes
CONFLICT OF INTERESTS
Dr. Joanna E. Steinglass receives royalties from UpToDate. Other authors declare no conflict of interests.
Action Editor: Ruth Striegel Weissman
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from ResDAC. Restrictions apply to the availability of these data, which were used under license for this study.
REFERENCES
- Agency for Healthcare Research and Quality. (2021). Defining the PCMH. Retrieved from https://pcmh.ahrq.gov [DOI] [PubMed] [Google Scholar]
- Anderson ML (2008). Multiple inference and gender differences in the effects of early intervention: A reevaluation of the abecedarian, Perry preschool, and early training projects. Journal of the American Statistical Association, 103(484), 1481–1495 [Google Scholar]
- Baker JH, & Runfola CD (2016). Eating disorders in midlife women: A perimenopausal eating disorder? Maturitas, 85, 112–116. 10.1016/j.maturitas.2015.12.017 [DOI] [PubMed] [Google Scholar]
- Bellows BK, DuVall SL, Kamauu AW, Supina D, Babcock T, & LaFleur J (2015). Healthcare costs and resource utilization of patients with binge-eating disorder and eating disorder not otherwise specified in the Department of Veterans Affairs. International Journal of Eating Disorders, 48(8), 1082–1091. 10.1002/eat.22427 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2021a). Accountable Care Organizations (ACOs): General Information. Retrieved from https://innovation.cms.gov/innovation-models/aco
- Centers for Medicare & Medicaid Services. (2021b). Nutrtion therapy services. Retrieved from https://www.medicare.gov/coverage/nutrition-therapy-services
- Cubanski J, Koma W, Damico A, & Neuman T (2019). How much do medicare beneficiaries spend out of pocket on health care? Retrieved from https://www.kff.org/medicare/issue-brief/how-much-do-medicare-beneficiaries-spend-out-of-pocket-on-health-care/
- de Oliveira C, Colton P, Cheng J, Olmsted M, & Kurdyak P (2017). The direct health care costs of eating disorders among hospitalized patients: A population-based study. International Journal of Eating Disorders, 50(12), 1385–1393. 10.1002/eat.22797 [DOI] [PubMed] [Google Scholar]
- Demmler JC, Brophy ST, Marchant A, John A, & Tan JOA (2020). Shining the light on eating disorders, incidence, prognosis and profiling of patients in primary and secondary care: National data linkage study. British Journal of Psychiatry, 216(2), 105–112. 10.1192/bjp.2019.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson JF, DeBar L, Perrin NA, Lynch F, Wilson GT, Rosselli F, … Striegel-Moore RH (2011). Health-service use in women with binge eating disorders. The International Journal of Eating Disorders, 44(6), 524–530. 10.1002/eat.20842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, & Coffey RM (1998). Comorbidity measures for use with administrative data. Medical Care, 36(1), 8–27. 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG, Pieper CF, Cohen HJ, Cornoni-Huntley JC, & Guralnik JM (2000). Comorbidity of five chronic health conditions in elderly community residents: Determinants and impact on mortality. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 55(2), M84–M89. 10.1093/gerona/55.2.m84 [DOI] [PubMed] [Google Scholar]
- Gatt L, Jan S, Mondraty N, Horsfield S, Hart S, Russell J, … Essue B (2014). The household economic burden of eating disorders and adherence to treatment in Australia. BMC Psychiatry, 14(1), 338. 10.1186/s12888-014-0338-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halmi KA (2018). Psychological comorbidities of eating disorders. In Agras WS & Robinson A (Eds.), The Oxford handbook of eating disorders (2nd ed., pp. 229–243). New York, NY: Oxford University Press. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348–358. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huskamp HA, Samples H, Hadland SE, McGinty EE, Gibson TB, Goldman HH, … Barry CL (2018). Mental health spending and intensity of service use among individuals with diagnoses of eating disorders following Federal Parity. Psychiatric Services, 69(2), 217–223. 10.1176/appi.ps.201600516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joynt KE, Figueroa JF, Beaulieu N, Wild RC, Orav EJ, & Jha AK (2016). Segmenting high-cost Medicare patients into potentially actionable cohorts. Healthcare, 5(1–2), 62–67. 10.1016/j.hjdsi.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (2019). Medicare Advantage. Retrieved from https://www.kff.org/medicare/fact-sheet/medicare-advantage/
- Kaiser Family Foundation. (2021). Distribution of Medicare beneficiaries by eligibility category. Retrieved from https://www.kff.org/medicare/state-indicator/distribution-of-medicare-beneficiaries-by-eligibility-category-2
- Keeney T, Belanger E, Jones RN, Joyce NR, Meyers DJ, & Mor V (2020). High-need phenotypes in Medicare beneficiaries: Drivers of variation in utilization and outcomes. Journal of the American Geriatric Society, 68(1), 70–77. 10.1111/jgs.16146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kriegsman DM, Deeg DJ, & Stalman WA (2004). Comorbidity of somatic chronic diseases and decline in physical functioning:; the longitudinal aging study Amsterdam. Journal of Clinical Epidemiology, 57(1), 55–65. 10.1016/S0895-4356(03)00258-0 [DOI] [PubMed] [Google Scholar]
- Lee SM, Hong M, Park S, Kang WS, & Oh I-H (2021). Economic burden of eating disorders in South Korea. Journal of Eating Disorders, 9(1), 30. 10.1186/s40337-021-00385-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangweth-Matzek B, & Hoek HW (2017). Epidemiology and treatment of eating disorders in men and women of middle and older age. Current Opinion in Psychiatry, 30(6), 446–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare-Medicaid Coordination Office. (2020a). Data analysis brief: Medicare-Medicaid dual enrollment 2006 through 2019. Centers for Medicare & Medicaid Services. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/ [Google Scholar]
- Medicare-Medicaid Coordination Office. (2020b). People dually eligible for Medicare and Medicaid. Centers for Medciare & Medicaid Services. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/ [Google Scholar]
- Mehler PS (2018). Medical complications of anorexia nervosa and bulimia nervosa. In Agras WS & Robinson A (Eds.), The Oxford handbook of eating disorders (2nd ed.). New York, NY: Oxford University Press. [Google Scholar]
- Mitchell JE (2016). Medical comorbidity and medical complications associated with binge-eating disorder. The International Journal of Eating Disorders, 49(3), 319–323. 10.1002/eat.22452 [DOI] [PubMed] [Google Scholar]
- Mitchell JE, Myers T, Crosby R, O’Neill G, Carlisle J, & Gerlach S (2009). Health care utilization in patients with eating disorders. The International Journal of Eating Disorders, 42(6), 571–574. 10.1002/eat.20651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Momen NC, Plana-Ripoll O, Bulik CM, McGrath JJ, Thornton LM, Yilmaz Z, & Peterson LV (2021). Comorbidity between types of eating disorder and general medical conditions. The British Journal of Psychiatry, 1–8. 10.1192/bjp.2021.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raevuori A, Haukka J, Vaarala O, Suvisaari JM, Gissler M, Grainger M, … Suokas JT (2014). The increased risk for autoimmune diseases in patients with eating disorders. PLoS One, 9(8), e104845. 10.1371/journal.pone.0104845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samnaliev M, Noh HL, Sonneville KR, & Austin SB (2014). The economic burden of eating disorders and related mental health comorbidities: An exploratory analysis using the U.S. Medical Expenditures Panel Survey. Preventive Medicine Reports, 2, 32–34. 10.1016/j.pmedr.2014.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santonicola A, Gagliardi M, Guarino MPL, Siniscalchi M, Ciacci C, & Iovino P (2019). Eating disorders and gastrointestinal diseases. Nutrients, 11(12), 3038. 10.3390/nu11123038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardar MR, Greway A, DeAngelis M, Tysko EO, Lehmann S, Wohlstetter M, & Patel R (2015). Cardiovascular impact of eating disorders in adults: A single center experience and literature review. Heart Views, 16(3), 88–92. 10.4103/1995-705X.164463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, & Lipson SK (2018). Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. The International Journal of Eating Disorders, 51(6), 518–526. 10.1002/eat.22846 [DOI] [PubMed] [Google Scholar]
- Streatfeild J, Hickson J, Austin SB, Hutcheson R, Kandel JS, Lampert JG, … Pezzullo L (2021). Social and economic cost of eating disorders in the United States: Evidence to inform policy action. The International Journal of Eating Disorders, 54(5), 851–868. 10.1002/eat.23486 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm F-A, Kraemer HC, Schreiber GB, Crawford PB, & Daniels SR (2005). Health services use in women with a history of bulimia nervosa or binge eating disorder. The International Journal of Eating Disorders, 37(1), 11–18. 10.1002/eat.20090 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, & Rosenheck RA (2000). One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: Evidence from a national database of health insurance claims. The International Journal of Eating Disorders, 27(4), 381–389. [DOI] [PubMed] [Google Scholar]
- Strother E, Lemberg R, Stanford SC, & Turberville D (2012). Eating disorders in men: Underdiagnosed, undertreated, and misunderstood. Eating Disorders, 20(5), 346–355. 10.1080/10640266.2012.715512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuhldreher N, Konnopka A, Wild B, Herzog W, Zipfel S, Löwe B, & König HH (2012). Cost-of-illness studies and cost-effectiveness analyses in eating disorders: A systematic review. The International Journal of Eating Disorders, 45(4), 476–491. 10.1002/eat.20977 [DOI] [PubMed] [Google Scholar]
- Tith RM, Paradis G, Potter B, Low N, Healy-Profitos J, He S, & Auger N (2019). Association of bulimia nervosa with long-term risk of cardiovascular disease and mortality among women. JAMA Psychiatry, 77(1), 44–51. 10.1001/jamapsychiatry.2019.2914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseng MM, Tu CY, & Chang YT (2021). Healthcare use and costs of adults with anorexia nervosa and bulimia nervosa in Taiwan. The International Journal of Eating Disorders, 54(1), 69–80. 10.1002/eat.23419 [DOI] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biological Psychiatry, 84(5), 345–354. 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson HJ, Jangmo A, Smith T, Thornton LM, von Hausswolff-Juhlin Y, Madhoo M, … Bulik CM (2018). A register-based case-control study of health care utilization and costs in binge-eating disorder. Journal of Psychosomatic Research, 108, 47–53. 10.1016/j.jpsychores.2018.02.011 [DOI] [PubMed] [Google Scholar]
- Zerwas S, Larsen JT, Petersen L, Thornton LM, Quaranta M, Koch SV, … Bulik CM (2017). Eating disorders, autoimmune, and autoinflammatory disease. Pediatrics, 140(6), e20162089. 10.1542/peds.2016-2089 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from ResDAC. Restrictions apply to the availability of these data, which were used under license for this study.


