Abstract
Background:
We aimed to evaluate the influence of HF on clinical and economic outcomes among older adults ≥75 years of age during their AMI admission in large population-based study from the United States. We also evaluated the clinical characteristics associated with the presence of HF and the predictors of mortality, healthcare utilization, and cost among older adults with AMI.
Methods:
From January 1st, 2000, to December 31st, 2016, AMI admission was identified using the primary diagnosis and concomitant HF was identified using any non-primary diagnoses in the Premier Healthcare Database.
Results:
Of the 468,654 patients examined, 42,946 (9%) had concomitant HF during their AMI admission. These patients were older, more often female, and were more likely to be White. Patients with concomitant HF were more likely to be frail than non-HF patients (59% vs 15%, p<0.001). The mean (SD) Elixhauser comorbidity index was 2.6 (2.5) vs 0.4 (1.1), p <0.001 in the AMI with HF vs AMI only group. The use of PCI in those with AMI and HF was lower than those with AMI only (15% vs. 31%, p <0.001). The overall mortality rate for those with HF was 12%, the median [IQR] hospital length of stay was 5 [3,9] days, and only 25% of patients were discharged home. A higher proportion of patients were discharged to rehabilitation or hospice if they had AMI and HF (Rehabilitation: 33% vs 20%, p <0.001; Hospice: 5% vs. 3%, p <0.001). The mean unadjusted cost of an AMI hospitalization in patients with concomitant HF was lower ($12,411± $14,860) than in those without HF ($15,828 ± $19,330). After adjusting for age, gender, race, hypertension, frailty, revascularization strategy, and death, the average cost of hospitalization attributed to concomitant HF was +$1,075 (95% CI +876 to $1,274) when compared to AMI patients without HF.
Conclusion:
In patients ≥75 years of age, AMI with concomitant HF carries higher risk of death, but at ages ≥85 years, the risk difference diminishes due to other competing risks. HF was also associated with longer hospital length of stay and higher likelihood of referral to hospice and rehabilitation facilities when compared to older patients without HF. Care for these older adults is associated with increased hospitalization costs. Measures to identify HF in older adults during their AMI admission are necessary to optimize health outcomes care delivery and costs.
Keywords: Older Adults, Myocardial Infarction, Heart Failure, Coronary Disease
INTRODUCTION
In the United States, the older adult population is expanding rapidly. In 2012, adults aged 75 years or older represented 6.1% of the United States population (~19.2 million), but these estimates are projected to increase to 46 million individuals in 2050, representing 11.5% of the census.1 Older adults are disproportionately affected with acute myocardial infarction (AMI) when compared to younger patients.2 Significant challenges in the management of AMI in older patients exist because of the concomitant presence of geriatric syndromes such as frailty, sarcopenia, multimorbidity, polypharmacy, physical, and cognitive dysfunction.3 Acute cardiovascular care becomes even more complex when an older patient presents with AMI complicated by heart failure (HF).4 The clinical and economic impact of HF among a large population of older adults admitted with their AMI admission remains unknown. We aimed to evaluate the influence of HF on clinical and economic outcomes among older adults ≥75 years of age during their primary AMI admission in large population-based study from the United States. We also evaluated the clinical characteristics associated with the presence of HF and the predictors of mortality, healthcare utilization, and cost among older adults with AMI.
METHODS
Study Population
This study used data from the Premier Healthcare Database (Premier Inc., Charlotte, NC) that included 121 million inpatient encounters and more than 10 million encounter per year since 2012, accounting for approximately 20% of the total hospital admissions in the United States.5 The data contain patient-level information on demographic variables, comorbidities, procedures, healthcare utilization, and costs during hospital admission.5 Each patient is assigned a unique identifier that allows the individual to be tracked across inpatient and hospital-based outpatient settings within the same hospital system.
Study Population
The study population included patients ≥75 years of age who were admitted to the hospital with a principal diagnosis of AMI, defined as the individual’s primary AMI admission diagnosis recorded in the Premier Healthcare Database at a specific hospital between July 2000 and January 2016. AMI was identified using the International Classification of Diseases, Ninth and Tenth Revisions (ICD-9 and ICD-10) Clinical Modification codes (ICD-9: 410; ICD-I21)6. Patients who expired in the emergency department, transferred to another hospital, or those placed under observation status were excluded from the analysis. HF was identified using any non-primary diagnosis among older adults ≥75 years of age (ICD-9 codes 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 428.X; ICD10 code I50.X).
Study Outcomes
The primary outcome was in-hospital mortality defined as death occurring after index admission and before hospital discharge. Secondary outcomes were defined as disposition after discharge, mean length of hospital stay, inpatient hospital charges, and inflation-adjusted total costs. Hospital charges were defined as the amount the hospital billed for services and costs is defined as the actual expenses incurred for hospital services, such as wages, supplies, and utility costs.
Comorbidities and Procedures
Comorbid conditions were defined in accordance with the Elixhauser Comorbidity Index, which was part of the Healthcare Cost and Utilization Project by the Agency for Healthcare Research and Quality.7 For this analysis, readmissions after index AMI hospitalization were excluded from the study because Premier only tracked patients readmitted within the same hospital system. For each patient, only the first admission for AMI during the study period was included.
Statistical Analysis
We aggregated the Premier Healthcare Database from 2000–2016 and used descriptive statistics to describe the cohort’s baseline demographics, admission source and type, comorbidities, frailty, and use of cardiovascular procedures stratified by presence or absence of concomitant HF. Differences between the presence or absence of HF were compared between the two groups using t tests for continuous variables and χ2 test for dichotomous variables, as appropriate. We applied similar statistics to compare hospital outcomes (disposition after discharge, mortality, mean length of stay, charges, and costs) by presence or absence of concomitant HF.
Of the study population, the mean HF hospitalization and all-cause mortality were calculated for each year during the study period (Figure 1). To assess the influence of HF on hospital mortality during index AMI admission, we first applied a univariable logistic regression analysis to calculate a crude odds ratio for those with versus without HF. Then, several multivariable logistic regression models were fitted based on common confounding variables that may influence outcomes in patients with AMI. The multivariable models included age, female gender, race, hypertension, claims-based frailty index, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG) surgery, and year of admission. The mean all-cause-mortality rate was evaluated for patients with and without HF during each year of the study period by the age of the participant. We evaluated the influence of PCI on all-cause mortality among patients with HF and concomitant AMI using a logistic regression model adjusting for age, gender, ethnicity, hypertension, and frailty status. To assess for the influence of HF on inflation-adjusted costs of AMI hospitalization, we fitted a simple linear regression model for HF on inflation-adjusted cost. Then, a multivariable linear regression models were used to assess the association between HF diagnosis and inflation-adjusted cost during the study period. All statistical analyses were performed using STATA version 15 MP (Stata-Corp, College Station, TX). We considered a p value of <0.05 as significant and all tests were 2-sided.
Figure 1.
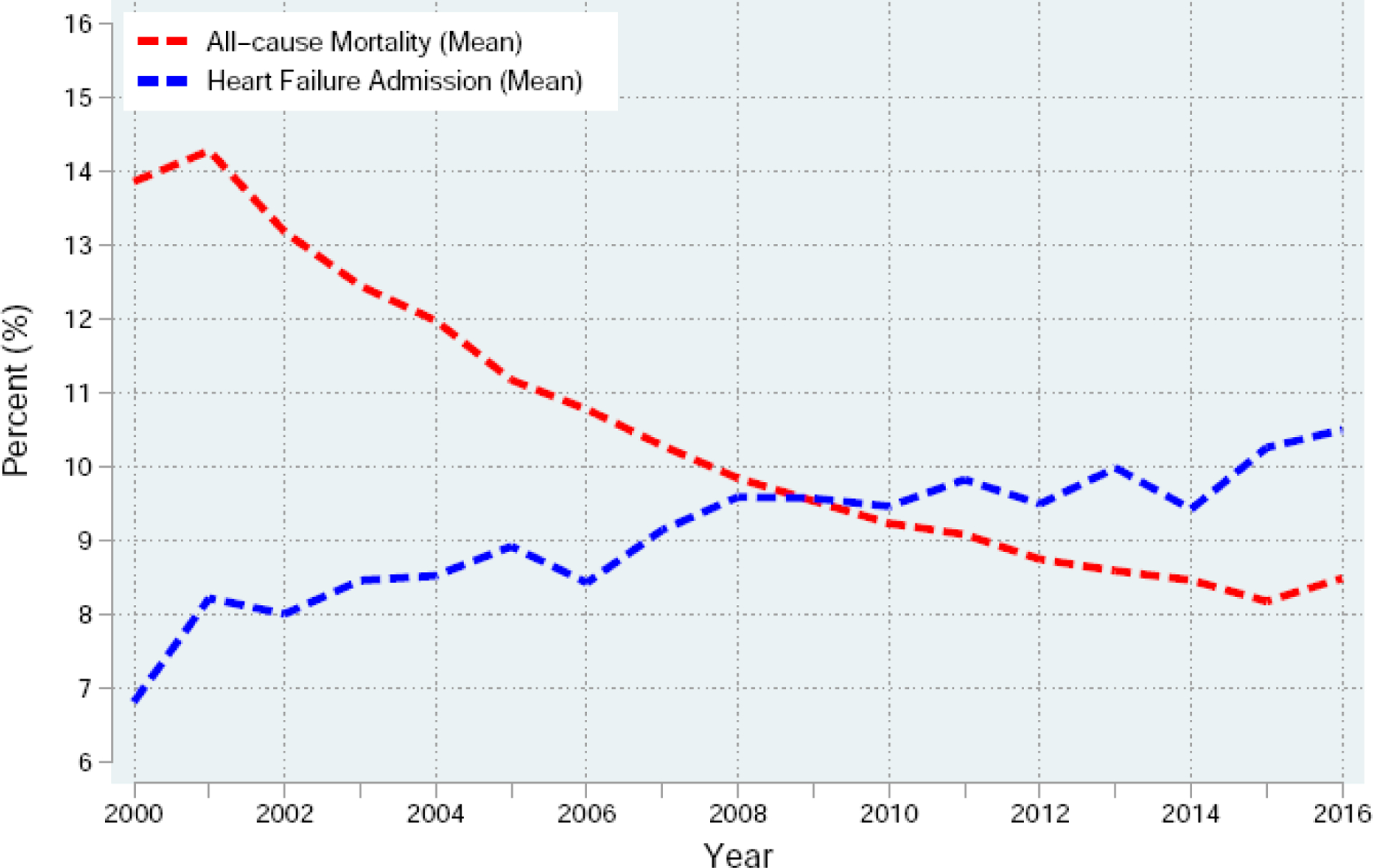
Heart failure admission (mean) and all-cause mortality (mean) in the United States among older adults ≥75 years during their first observed acute myocardial infarction in the Premier Healthcare Database from 2000 to 2016.
RESULTS
From 2000 to 2016, we identified 468,654 encounters for patients ≥75 years of age with a primary diagnosis of AMI. Of the total population, 42,946 (9%) had concomitant HF. The average age of the cohort was 82.3 years. Most patients were women, White, and 36% were older than 85 years. Patients with concomitant AMI and HF were older (83.2 vs 82.2 years, p <0.001), more likely to be White (76.1% vs 75.1%, p <0.001), and had higher comorbidity burden at the time of presentation. During index admission, patients with HF were less likely to have PCI or CABG and were more likely to present to the hospital urgently through the emergency department or from a non-healthcare facility (Table 1).
Table 1.
Demographic characteristics in older adults with acute myocardial infarction by whether they had concomitant heart failure during index admission in Premier Healthcare Database from 2000 to 2016.
| Variable Name | Total (n=468,654) | Heart Failure (n=42,946) | No Heart Failure (n=425,708) | P-Value |
|---|---|---|---|---|
| Age, mean (SD) | 82.3 (4.7) | 83.2 (4.7) | 82.2 (4.7) | <0.001 |
| Age>85, % | 36.0 | 43.8 | 35.2 | <0.001 |
| Male, % | 46.8 | 43.3 | 47.2 | <0.001 |
| White, % | 75.1 | 76.1 | 75.1 | <0.001 |
| Hispanic, % | 12.9 | 11.4 | 13.0 | <0.001 |
| Admission Source | ||||
| Emergency Department, % | 40.4 | 43.7 | 40.0 | <0.001 |
| Non-Healthcare Facility, % | 35.9 | 38.9 | 35.6 | <0.001 |
| Transfer, % | 14.5 | 6.2 | 15.4 | <0.001 |
| Admission Type | ||||
| Emergent, % | 72.2 | 79.8 | 71.4 | <0.001 |
| Urgent, % | 20.5 | 14.2 | 21.2 | <0.001 |
| Elective, % | 6.4 | 5.3 | 6.5 | <0.001 |
| Comorbidities | ||||
| Hypertension, % | 76.5 | 88.0 | 75.4 | <0.001 |
| Diabetes Mellitus, % | 30.7 | 43.3 | 29.5 | <0.001 |
| Diabetes Mellitus with Complications, % | 6.9 | 15.5 | 6.1 | <0.001 |
| Valvular Heart Disease, % | 4.0 | 23.5 | 2.0 | <0.001 |
| Pulmonary Circulation Disorder, % | 1.3 | 9.0 | 0.5 | <0.001 |
| Peripheral Vascular Disease, % | 17.5 | 27.9 | 16.5 | <0.001 |
| Paraplegia, % | 2.9 | 5.3 | 2.6 | <0.001 |
| Neurologic Disorder, % | 11.0 | 17.1 | 10.4 | <0.001 |
| Chronic Lung Disease, % | 25.4 | 43.6 | 23.6 | <0.001 |
| Hypothyroidism, % | 17.4 | 23.9 | 16.8 | <0.001 |
| Renal Failure, % | 23.9 | 44.2 | 21.9 | <0.001 |
| Coagulopathy, % | 6.6 | 11.7 | 6.1 | <0.001 |
| Obesity, % | 6.8 | 10.7 | 6.4 | <0.001 |
| Weight loss, % | 4.6 | 11.3 | 4.0 | <0.001 |
| Electrolyte disorder, % | 31.1 | 56.0 | 28.6 | <0.001 |
| Blood loss, % | 2.3 | 5.7 | 2.0 | <0.001 |
| Iron deficiency anemia, % | 27.2 | 51.3 | 24.7 | <0.001 |
| Psychiatric disorder, % | 2.4 | 4.6 | 2.1 | <0.001 |
| Depression, % | 8.7 | 17.0 | 7.8 | <0.001 |
| Claims-based Frailty Indexα, % | 19.1 | 59.3 | 15.1 | <0.001 |
| PCI, % | 29.8 | 14.9 | 31.4 | <0.001 |
| CABG Surgery, % | 7.3 | 4.6 | 7.6 | <0.001 |
Abbreviations: AIDS = acquired immune deficiency virus; PCI = Percutaneous coronary intervention; CABG = coronary artery bypass surgery.
Frailty was defined according to the claims-based frailty index derived from inpatient and outpatient data from 6 months prior to the acute myocardial infarction admission.
Among the study population, the overall cumulative hospital mortality was 10.3%, but it was higher in patients with concomitant HF (10.3% vs. 12%, p< 0.0001). Over the study period, the mean all-cause mortality rate in older patients with AMI declined, while the proportion of patients admitted with HF increased (Figure 1). Fewer patients with concomitant HF were discharged home and patients with HF were more likely to be discharged to hospice, rehabilitation, or long-term acute care facilities. Patients with concomitant HF had higher mean hospital length of stay and incurred more charges and costs than those without concomitant HF (Table 2). The mean HF admission and all-cause mortality rates increased with advancing age, with the highest rate observed among those ages 85 years or older (Figure 2). Over the 17-year study period, all-cause mortality remained higher in older patients with AMI and HF than patients with no HF diagnosis (Figure 3). Multivariable analysis showed an independent effect of HF on mortality in older patients with AMI. After adjustment for potential confounders, the presence of concomitant HF increased hospital mortality by 23.5% (OR 1.24, 95% CI 1.19–1.28) (Table 3). Among patients with concomitant HF and AMI, PCI reduced the risk of all-cause mortality after adjusting for age, gender, ethnicity, hypertension, and frailty status (Table 4).
Table 2.
Hospital outcomes in older adults with acute myocardial infarction by the presence or absence of concomitant heart failure during index admission in Premier Healthcare Database from 2000 to 2016.
| Variable Name | Total (n=468,654) | HF (n=42,946) | No HF (n=425,708) | P-value |
|---|---|---|---|---|
| Hospital Mortality, % | 10.3 | 11.6 | 10.2 | <0.001 |
| Discharge Status | <0.001 | |||
| Home, % | 42.0 | 25.0 | 43.7 | |
| Hospice, % | 3.0 | 5.0 | 2.8 | |
| Rehabilitation or LTC, % | 20.9 | 33.2 | 19.7 | |
| Other* | 34.1 | 36.8 | 34.5 | |
| Length of Stay, days, mean (SD) | 5.9 (6.3) | 7.6 (10) | 5.7 (5.7) | <0.001 |
| Charges ($), mean (SD) | 55,414 (69,859) | 60,660 (106,815) | 54,938 (64,972) | <0.001 |
| Cost ($), mean (SD) | 15,554 (19,033) | 17,585 (29,968) | 15,353 (17,515) | <0.001 |
Abbreviations: LTC = Long-term care facility.
Others include: discharged or transferred to SNF, discharged or transferred to ICF, discharged or transferred to cancer center, discharged to home health organization, left against medical advice, discharged to court of law enforcement, discharged to other locations.
Figure 2.
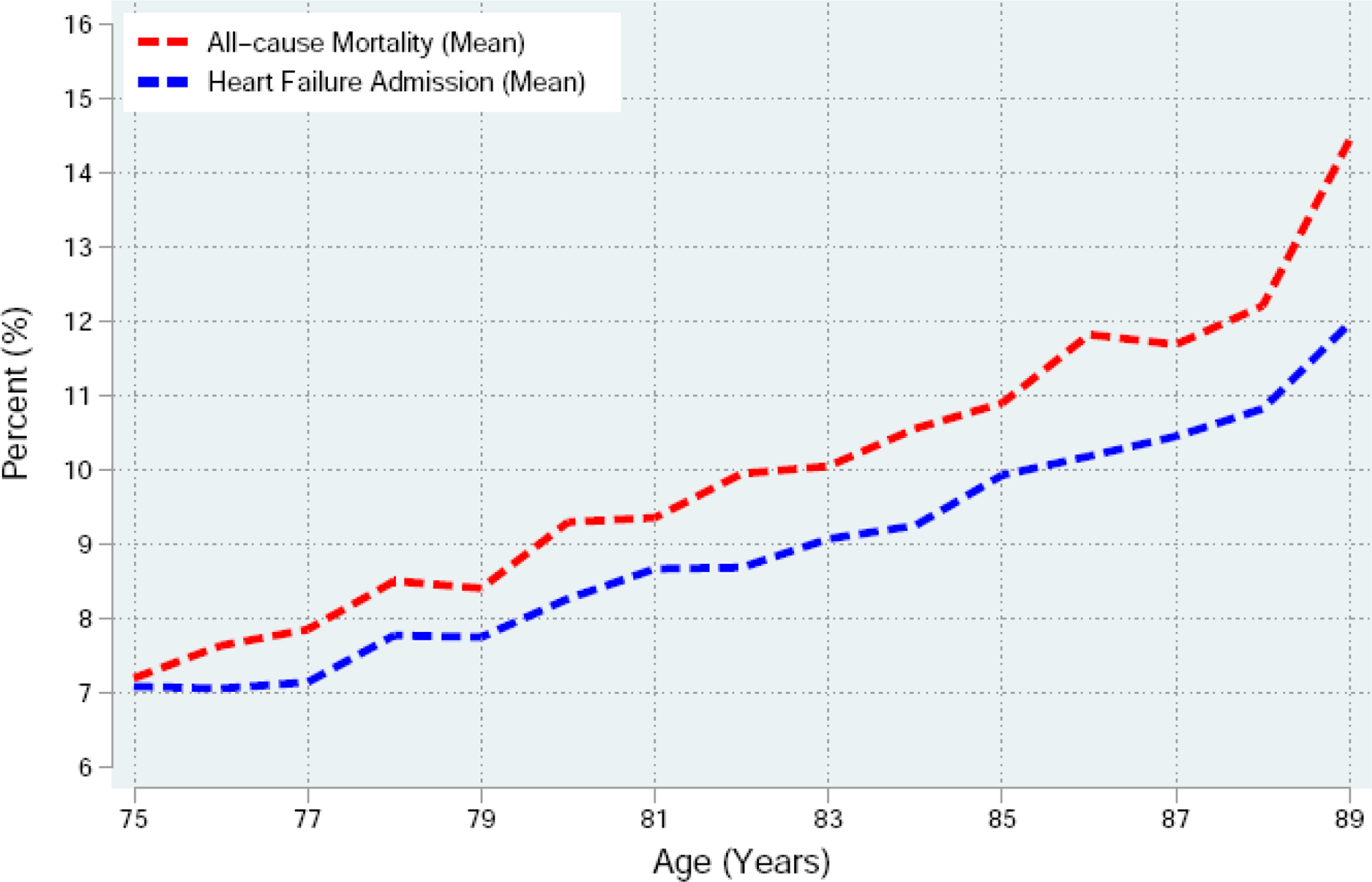
Heart failure admission and all-cause mortality in the United States by age among older adults ≥75 years during their first observed acute myocardial infarction in the Premier Healthcare Database from 2000 to 2016. The figure demonstrates that among adults aged 75 years or older, the risk of heart failure admission and the risk of all-cause mortality increase significantly with age. The mean HF admission represents the mean of number of HF and AMI admissions to total number of AMI admissions by age. The mean all-cause mortality represents the mean number of all-cause mortality to total number of AMI patients enrolled in this study by age.
Figure 3.
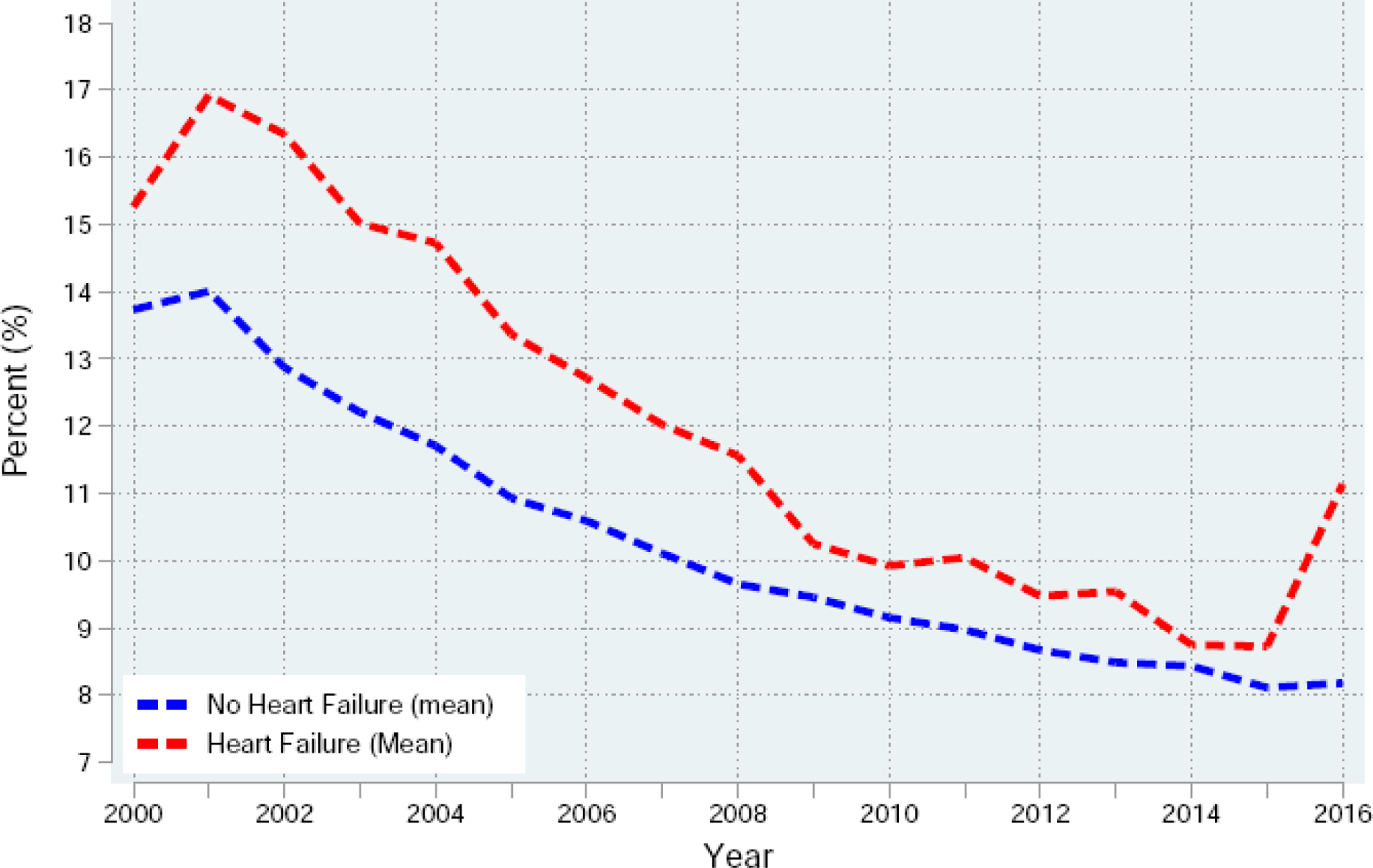
All-cause mortality by heart failure status during index admission among older adults with acute myocardial infarction between 2000 and 2016.
Table 3.
Multivariable logistic regression model examining the association between heart failure and hospital mortality among older adults with acute myocardial infarction during index admission in Premier Healthcare Database from 2000 to 2016.
| VARIABLES | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| Heart Failure | 1.321*** (0.0212) |
1.321*** (0.0212) |
1.333*** (0.0259) |
1.255*** (0.0244) |
1.235*** (0.0240) |
1.227*** (0.0239) |
| Age | 1.054*** (0.00111) |
1.054*** (0.00111) |
1.050*** (0.00122) |
1.041*** (0.00122) |
1.038*** (0.00123) |
1.040*** (0.00124) |
| Female Gender | 0.945*** (0.00921) |
0.944*** (0.00921) |
0.961*** (0.00947) |
0.948*** (0.00937) |
0.938*** (0.00928) |
0.927*** (0.00920) |
| White | 0.966*** (0.0107) |
1.000 (0.0124) |
1.000 (0.0124) |
0.999 (0.0124) |
1.013 (0.0126) |
|
| Hypertension | 0.594*** (0.00629) |
0.599*** (0.00637) |
0.600*** (0.00639) |
0.641*** (0.00695) |
||
| Frailty | 1.124*** (0.0179) |
1.086*** (0.0173) |
1.077*** (0.0171) |
1.090*** (0.0174) |
||
| PCI | 0.535*** (0.00673) |
0.518*** (0.00659) |
0.536*** (0.00684) |
|||
| CABG | 0.697*** (0.0151) |
0.694*** (0.0151) |
||||
| Year | 0.967*** (0.00105) |
|||||
| Constant | 0.00149*** (0.000130) |
0.00152*** (0.000132) |
0.00283*** (0.000268) |
0.00687*** (0.000657) |
0.00946*** (0.000919) |
2.349e+27*** (5.084e+27) |
| Observations | 469,827 | 469,401 | 468,217 | 468,217 | 468,217 | 468,217 |
Standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
Abbreviations: PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft.
Frailty was defined according to the claims-based frailty index derived from inpatient and outpatient data from 6 months prior to the acute myocardial infarction admission.
Table 4.
Multivariable logistic regression model examining the association between percutaneous coronary intervention and hospital mortality among older adults with acute myocardial infarction and heart failure in Premier Healthcare Database from 2000 to 2016.
| Variable | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| PCI | 0.53*** (0.027) |
0.52*** (0.027) |
0.53*** (0.028) |
0.56*** (0.029) |
| Age | 1.01*** (0.003) |
1.01*** (0.003) |
1.01*** (0.003) |
0.97*** (0.003) |
| Female Gender | 0.87*** (0.026) |
0.88*** (0.026) |
0.886 *** (0.027) |
0.80*** (0.025) |
| White | 1.04 (0.036) |
1.03 (0.037) |
1.21*** (0.45)*** |
|
| Hypertension | 0.61*** (0.025) |
0.55*** (0.023) |
||
| Frailty | 6.14*** (0.70) |
|||
| Constant | 0.057*** (0.015) |
0.056*** (0.015) |
0.096*** (0.026) |
0.73 (0.227) |
| Observations | 42,946 | 42,946 | 42,946 | 42,946 |
Standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
Abbreviations: PCI = percutaneous coronary intervention.
Frailty was defined according to the claims-based frailty index derived from inpatient and outpatient data from 6 months prior to the acute myocardial infarction admission.
The mean cost of AMI hospitalization in older patients with concomitant HF was lower ($15,353 ± $17,515) than in those without HF ($17,585 ± $29,968). Parallel with the higher mortality rate observed in patients with HF, a multivariable linear regression model adjusting for age and gender showed that the average inflation adjusted cost for hospitalization attributed to diagnosis of HF was $2,770 dollars lower than the average inflation adjusted cost for older AMI patients without HF (estimate: −2,770; 95% CI −2,969 to −2,573, dollars). However, after adjusting for common confounders that increase the risk of death during AMI admission including age, gender, race, hypertension, frailty, revascularization strategy, and death, the average cost of hospitalization attributed to HF was +$1,075 (95% CI +876 to $1,274) when compared to AMI patients without HF (Table 5).
Table 5.
Multivariable linear regression model examining the association between heart failure and inflation adjusted costs ($) per hospitalization among older adults with acute myocardial infarction during index admission in Premier Healthcare Database from 2000 to 2016.
| VARIABLES | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
| Heart Failure | −2,770*** (101.1) |
−2,771*** (101.0) |
−1,534*** (119.1) |
−961.2*** (118.5) |
1,146*** (101.6) |
1,075*** (101.4) |
| Age | −562.7*** (5.910) |
−558.0*** (5.912) |
−502.1*** (6.526) |
−426.5*** (6.549) |
−60.18*** (5.678) |
−71.61*** (5.672) |
| Female Gender | −1,981*** (55.45) |
−2,012*** (55.45) |
−1,923*** (55.71) |
−1,810*** (55.34) |
−575.4*** (47.49) |
−555.9*** (47.39) |
| White | −1,420*** (63.43) |
−1,960*** (68.62) |
−1,973*** (68.15) |
−1,907*** (58.36) |
−1,907*** (58.24) |
|
| Hypertension | 208.4*** (65.08) |
111.6* (64.64) |
−270.3*** (55.36) |
−99.24* (55.39) |
||
| Frailty | −1,900*** (94.35) |
−1,568*** (93.80) |
−510.0*** (80.36) |
−538.0*** (80.20) |
||
| PCI | 4,908*** (60.89) |
9,105*** (53.13) |
9,281*** (53.17) |
|||
| CABG | 38,238*** (92.67) |
38,341*** (92.51) |
||||
| Hospital Death | 3,370*** (77.12) |
|||||
| Constant | 63,154*** (483.8) |
63,852*** (484.7) |
59,719*** (526.7) |
51,938*** (531.9) |
16,942*** (463.3) |
17,345*** (462.5) |
| Observations | 469,827 | 469,401 | 468,217 | 468,217 | 468,217 | 468,217 |
Standard errors in parentheses
p<0.01,
p<0.05,
p<0.1
Abbreviations: HF = heart failure; PCI = percutaneous coronary intervention; CABG = coronary artery bypass graft.
Frailty was defined according to the claims-based frailty index derived from inpatient and outpatient data from 6 months prior to the acute myocardial infarction admission.
DISCUSSION
In Premier Healthcare Database, we examined the clinical and economic impact of HF among adults ≥75 years of age admitted with a primary diagnosis of AMI. The main findings of this study are: (1) The presence of HF during AMI hospitalization in older adults was 9%, but the prevalence of HF during the study period has been rising as older adults live into their older years; (2) While the overall mortality for AMI has decreased from 2000 to 2016, the presence of HF was associated with higher all-cause mortality, particularly among octogenarians; (3) After adjustment for confounders that increase the risk for hospital mortality during AMI admission, the inflation-adjusted cost attributed to HF was +$1,075, but remained lower than the cost attributed to other cardiovascular procedures.
The prevalence of HF among patients admitted with AMI varies widely in the published literature.8–11 Among 187,803 patients hospitalized for AMI in the ACTION registry, 12% had signs of HF on admission, while another 18.7% developed HF during their index hospitalization. Among patients above the age of 75 with ST-elevation myocardial infarction, the estimate for those showing signs of HF is even higher approaching 36%.11 Of 86,771 patients in the Cardiovascular Disease in Norway Project, 18.7% of patients with AMI presented with or developed HF after the admission.10 In that study, of the 33,447 patients ≥75 years of age, 25.6% of men and 27.1 % of women developed HF prior to or during index admission for AMI.10 In a large heterogenous population of older adults in the United States, we found that HF in patients with AMI ~9%. Despite our conservative definition for our study population, this lower estimate of HF may be due to the much larger denominator of AMI patients studied over 16-year period of the study. Cooper and colleagues found that the transition from ICD-9 to ICD-10 has improved the specificity of diagnosing HF in large administrative data, but refinement in the claims-based definition for heart failure is still needed.12
We found higher mortality in older adults admitted with AMI and concomitant HF than those without HF. Among 13,707 patients enrolled in the GRACE registry, patients with concomitant AMI and HF had higher in-hospital mortality rates (17.8% versus 12.0%), than those without HF and those ≥75 years of age had the highest mortality across all age groups.16 Among 187,803 patients hospitalized for AMI, the prevalence of HF was associated with higher in-hospital mortality (6.7% vs. 0.9%).11 A registry of French patients with AMI showed that patients with AMI and HF had a significantly increased risk of death during index hospitalization (12.2% vs. 3.0%) and during 1 year follow-up (26.6% vs. 5.2%) than those without concomitant HF.13 The presence of HF underscores the higher risk profile of older AMI patients with elevated filling pressures, impairment in systolic or diastolic function, and in severe cases, pump failure and cardiogenic shock. These characteristics likely explain the higher mortality rate observed in older patients during their AMI admission.
There are limited data on disposition and healthcare cost of older patients with AMI and HF after discharge and hospital related cost. Of 13,196,801 patients hospitalized with HF between 2002–2017, 65.7% were discharged home, 3.1% to short-term rehabilitation facility, and 25.4% to long term care facility. The rate of discharge to home and short-term rehabilitation facility fell from 74.0% to 69.0% and 3.5% to 3.2%, respectively. However, the proportion discharged to long-term care facilities increased from 22.3% to 26.5%. Older patients were less likely to be discharged home than younger patients (64.5% vs 84.4%) and they were more likely to be discharged to long-term care facilities (32.4% vs. 11.5%).14 Our study extends these findings for older patients with concomitant HF and AMI, and illustrating a slightly increased rate of referral to hospice and palliative care services. Furthermore, the PAL-HF trial showed that an interdisciplinary palliative care intervention in advanced HF patients showed consistent improvement in quality of life, anxiety, depression, and spiritual well-being compared with usual non-palliative care team.15 The higher mortality rate associated with HF in the context of AMI among older patients appears to be associated with lower healthcare cost when compared to older patients without HF, but the mean cost for each hospitalization was $12,411. This estimate is approximated in a report by Kilgore et al.16 who examined Medicare beneficiaries with HF without AMI, and found that the per-patient cost of HF-related hospitalization was $14,631. With more than one million emergency department visits and approximately than 978,135 hospitalizations per year, the healthcare cost burden of HF in the U.S. remain substantial, and efforts to identify gaps in resource utilization and implementation of effective therapies are needed when addressing cardiovascular care for the older adult populations during their AMI admission. In our study, the R-squared for inflation adjusted cost data improves only after the variable of CABG is factored into the multivariable linear regression, which reflects that the contribution of HF to cost is less than the cost attributed to other cardiovascular procedures.
Strengths and Limitations
The study has several strengths. First, this is a large population-based study from the U.S. to demonstrate the association between concomitant HF and AMI with hospital mortality among older patients after adjusting for confounding variables known to increase hospital risks. Second, this is a unique population-based study to examine the contemporary costs of care attributable to HF during their AMI admission among older patients. Third, few studies have explored the disposition of older adults with concomitant HF and AMI. Understanding the relationships between cost of hospital stay, discharge disposition, and length of stay is an important strategy for healthcare organizations to deliver efficient and cost-effective care.
There are few limitations in this study. First, we identified diagnoses in the Premier Healthcare Database using ICD-9 and ICD-10 codes. There is a concern for over or under coding of HF by providers and coders, which can introduce misclassification bias. Second, the odds ratio for mortality from HF in this study may not be at the same magnitude observed in other clinical studies likely because of possible misclassification related to administrative data and the large denominator of AMI patients evaluated in this study. Third, the administrative data do not allow a distinction between having a history of HF vs. acute diagnosis of HF during AMI admission. Fourth, we do not have laboratory data available in Premier Healthcare Database, which limit our ability to understand the trajectory/change of clinical course during hospital admission. Despite these limitations, claims-based analyses have been used in health outcomes research to understand quality care, quantify health outcomes, and examine healthcare utilization and cost in large study population in the U.S.1,2 Finally, we were unable to distinguish between patients with AMI who had diagnosis of HF on presentation and those who developed signs of HF later during the hospital admission, and thus, both groups are combined in one group, as was the case in prior studies.10
CONCLUSION
During their AMI admission, HF is a commonly observed complication in older adults and carries higher risk of death, longer hospital length of stay, and higher likelihood of referral to hospice and rehabilitation facilities when compared to patients without concomitant HF. HF is commonly observed comorbidity among older adults, which carries a higher risk of death, but the risk difference diminishes after 85 years due to other competing risks. Care for these older adults is associated with increased costs of hospitalization and higher referral to hospice care. Measures to identify patients with HF early during their AMI course are necessary for timely initiation of optimal medical and device therapies in the older adult populations.
FUNDING AND FINANCIAL DISCLOSURE:
Dr. Damluji receives research funding from the Pepper Scholars Program of the Johns Hopkins University Claude D. Pepper Older Americans Independence Center funded by the National Institute on Aging P30-AG021334 and mentored patient-oriented research career development award from the National Heart, Lung, and Blood Institute K23-HL153771-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST: The authors declare that they have no relevant interests.
PRESENTATION: This work was presented as a moderated oral presentation at the 2020 American College of Cardiology Scientific Sessions, Chicago, IL.
REFERENCES
- 1.Ortman J and Velkoff V. An Aging Population: The Older Population in the United States Current Population Reports. 2014. [Google Scholar]
- 2.Damluji AA, Resar JR, Gerstenblith G, Gross AL, Forman DE and Moscucci M. Temporal Trends of Percutaneous Coronary Interventions in Older Adults With Acute Myocardial Infarction. Circ Cardiovasc Interv. 2019;12:e007812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Damluji AA, Forman DE, van Diepen S, Alexander KP, Page RL 2nd, Hummel SL, Menon V, Katz JN, Albert NM, Afilalo J, Cohen MG, American Heart Association Council on Clinical C, Council on C and Stroke N. Older Adults in the Cardiac Intensive Care Unit: Factoring Geriatric Syndromes in the Management, Prognosis, and Process of Care: A Scientific Statement From the American Heart Association. Circulation. 2020;141:e6–e32. [DOI] [PubMed] [Google Scholar]
- 4.Damluji AA, Chung SE, Xue QL, Hasan RK, Walston JD, Forman DE, Bandeen-Roche K, Moscucci M, Batchelor W, Resar JR and Gerstenblith G. Physical Frailty Phenotype and the Development of Geriatric Syndromes in Older Adults with Coronary Heart Disease. Am J Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Premier Applied Sciences PI. Premier Healthcare Database White Paper: Data That Informs and Performs. March 2, 2020.
- 6.Damluji AA, Huang J, Bandeen-Roche K, Forman DE, Gerstenblith G, Moscucci M, Resar JR, Varadhan R, Walston JD and Segal JB. Frailty Among Older Adults With Acute Myocardial Infarction and Outcomes From Percutaneous Coronary Interventions. J Am Heart Assoc. 2019;8:e013686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epstein RH and Dexter F. Development and validation of a structured query language implementation of the Elixhauser comorbidity index. J Am Med Inform Assoc. 2017;24:845–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali AS, Rybicki BA, Alam M, Wulbrecht N, Richer-Cornish K, Khaja F, Sabbah HN and Goldstein S. Clinical predictors of heart failure in patients with first acute myocardial infarction. Am Heart J. 1999;138:1133–9. [DOI] [PubMed] [Google Scholar]
- 9.Spencer FA, Meyer TE, Gore JM and Goldberg RJ. Heterogeneity in the management and outcomes of patients with acute myocardial infarction complicated by heart failure: the National Registry of Myocardial Infarction. Circulation. 2002;105:2605–10. [DOI] [PubMed] [Google Scholar]
- 10.Sulo G, Igland J, Vollset SE, Nygard O, Ebbing M, Sulo E, Egeland GM and Tell GS. Heart Failure Complicating Acute Myocardial Infarction; Burden and Timing of Occurrence: A Nation-wide Analysis Including 86 771 Patients From the Cardiovascular Disease in Norway (CVDNOR) Project. J Am Heart Assoc. 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah RV, Holmes D, Anderson M, Wang TY, Kontos MC, Wiviott SD and Scirica BM. Risk of heart failure complication during hospitalization for acute myocardial infarction in a contemporary population: insights from the National Cardiovascular Data ACTION Registry. Circ Heart Fail. 2012;5:693–702. [DOI] [PubMed] [Google Scholar]
- 12.Cooper LB, Psotka MA, Sinha S, Nallamothu BK, deFilippi CR, Batchelor W, O’Connor CM and Damluji AA. Specificity of administrative coding for older adults with acute heart failure hospitalizations. Am Heart J. 2020;223:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hellermann JP, Jacobsen SJ, Gersh BJ, Rodeheffer RJ, Reeder GS and Roger VL. Heart failure after myocardial infarction: a review. Am J Med. 2002;113:324–30. [DOI] [PubMed] [Google Scholar]
- 14.Khan MZ, Khan SU, Khan MS, Butler J and Alkhouli M. Disparities in discharge disposition after hospitalizations for decompensated heart failure. Cardiovasc Revasc Med. 2020. [DOI] [PubMed] [Google Scholar]
- 15.Jackson SL, Tong X, King RJ, Loustalot F, Hong Y and Ritchey MD. National Burden of Heart Failure Events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11:e004873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kilgore M, Patel HK, Kielhorn A, Maya JF and Sharma P. Economic burden of hospitalizations of Medicare beneficiaries with heart failure. Risk Manag Healthc Policy. 2017;10:63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]


