Abstract
BACKGROUND & AIMS:
Little is known about the effects of endoscopic balloon dilation (EBD) for strictures of the upper gastrointestinal (UGI) tract in patients with Crohn’s disease (CD). We performed a pooled analysis of the efficacy and safety of EBD for UGI CD-associated strictures.
METHODS:
We searched Embase, Medline, and the Cochrane library, as well as bibliographies of relevant articles, for cohort studies of adults with CD and strictures of the stomach or duodenum (up to the ligament of Treitz) who underwent EBD through December 2016. We obtained data from 7 international referral centers on 94 patients who underwent 141 EBDs. We performed a patient-level meta-analysis of data from published and unpublished cohort studies to determine mechanical and clinical success. We performed a time-to-event analysis to assess symptom recurrence and need for redilation or surgery. The patients analyzed had strictures of the duodenum (n = 107), stomach (n = 30), or spanning both (n = 4).
RESULTS:
The rate of technical success for EBD was 100%, with 87% short-term clinical efficacy; major complications arose from 2.9% of all procedures. During a median follow-up period of 23.1 months, 70.5% of patients had a recurrence of symptoms, 59.6% required redilation, and 30.8% required surgical intervention. Patients whose disease was located in the small bowel had a higher risk for symptom recurrence (hazard ratio [HR], 2.1; P = .003). Asian race (HR, 2.8; P < .001) and location of disease in the small bowel (HR, 1.9; P = .004) increased the need for redilation. Prestenotic dilation was a risk factor for needing surgery earlier (HR, 1.9; P = .001).
CONCLUSIONS:
In a meta-analysis, we found EBD for CD-associated strictures of the UGI to be an effective alternative to surgery, with a high rate of short-term technical and clinical success, moderate long-term efficacy, and an acceptable rate of complications.
Keywords: Therapy, Fibrosis, Stenosis, IBD, Endoscopy
Crohn’s disease (CD) may affect the entire gastrointestinal (GI) tract.1 As a consequence of transmural inflammation and a relapsing and remitting disease course, clinically apparent fibrostenosis of the intestine occurs in 20% of patients within 20 years after initial diagnosis.2 Despite recent advances in the medical treatment of CD, prevention and treatment of stricturing CD remains a large, unmet need.3 Because of the absence of specific antifibrotic therapies,4 CD patients with intestinal obstruction are commonly treated by surgical intervention such as strictureplasty or bowel resection,5 both of which can be associated with significant complications.6,7
Although CD may affect all parts of the GI tract, involvement of the stomach and duodenum is rarely reported. More specifically, the incidence of CD-associated strictures of the upper GI tract is less than 4%.8 Beside the occurrence of strictures, fistulae development in the upper GI tract has been reported as well.9,10 Historically, in the presteroid era, surgery was the only available treatment modality for obstructive duodenal CD, but often was accompanied by a complicated postoperative course with postoperative abscesses.11,12 Since then, with the advent of corticosteroids and immunosuppressive drugs, some case reports have become available that illustrate cases with an at least temporary successful medical treatment.8,9,11 Therefore, stricturing as well as fistulizing complications of the upper GI tract may generate challenging clinical scenarios for both affected CD patients as well as health care providers alike. The very limited body of published evidence for this treatment scenario is aggravates this clinical dilemma further.
Endoscopic balloon dilation (EBD) has emerged as an alternative to surgery and has been proven effective for the treatment of fibrotic CD-associated strictures of the ileocecum. EBD therefore has been implemented in current CD treatment algorithms and guidelines.13–15 EBD for CD-associated strictures of the upper GI tract was reported rarely in a large cohort comprising 35 patients from a single center.16 Therefore, the aim of this pooled analysis of international multicenter cohort studies, combining published cohorts with a multicenter investigation for a patient-level meta-analysis, was to evaluate the safety and efficacy of EBD in upper GI CD-associated strictures and to provide evidence-based guidance for this clinical situation.
Materials and Methods
Literature Search and Data
Detailed information regarding the literature search and data, as well as a PRISMA diagram (Supplementary Figure 1) can be found in the Supplementary materials. Corresponding authors of articles that fulfilled the inclusion and exclusion criteria were contacted via e-mail to obtain single patient-level data for the subjects included in the studies. These data represent part 1 of the pooled individual patient analysis.
In addition, 7 high-volume inflammatory bowel disease endoscopy centers were contacted and they provided clinical data for a total of 24 patients. These data represent part 2 of the pooled individual patient analysis. Of note, comparable criteria were used to assess the performance of dilation procedures as well as treatment outcomes in relation to the already published studies and as defined later.
Data Collection
The definitions used for the explored parameters of included studies16–19 are reported in the Supplementary Materials and Methods section and Supplementary Table 1.
Statistical Analysis
Detailed information about the statistical analysis can be found in the Supplementary Materials and Methods section.
Results
Pooled Individual Patient Analysis
In total, we included 94 patients from 11 different tertiary referral centers for inflammatory bowel disease (located in the United States, Australia, China, Japan, Denmark, Germany, The Netherlands, and Switzerland). There were 141 total dilation procedures. Seventy patients undergoing 112 dilations have been published in multiple individual smaller series previously,16–21 and 24 patients undergoing 29 dilations were not in previously published reports but were added through our multicenter collaboration (Table 1). The demographics of this population are shown in Table 2. The median age at CD diagnosis was 24 ± 10.6 years, and the median age at the time of stricture diagnosis was 33.7 ± 14.3 years. A total of 75.9% of strictures were located in the duodenum, 21.3% of patients developed strictures in the stomach, and 2.8% of patients presented with strictures that spanned from the stomach to the duodenum (Table 2). Most strictures were de novo strictures (89.1%; as opposed to anastomotic strictures) at sites without prior surgery. The median length of stricture was 3 cm (25th percentile, 2; 75th percentile, 10), with 85.4% of strictures being less than 5 cm long. All strictures were dilated by through-the-scope systems and 70.1% of the investigators applied graded dilation. The median maximum balloon diameter used was 15 mm (25th percentile, 14.0 mm; 75th percentile, 18.0 mm), and the vast majority of investigators used a balloon that was 5.5 cm in length (25th percentile, 5.5 cm; 75th percentile, 5.5 cm). The median time of balloon inflation was 2 minutes (25th percentile, 2 min; 75th percentile, 3 min,) and a pressure of 20 psi was applied (Table 3). The technical success rate was 100%, and EBD lead to short-term clinical efficacy in 87% of all patients. Of note, technical success did not result in clinical improvement of obstructive symptoms in all patients.
Table 1.
Pooled Per-Study Analysis
| Study | Rieder16,a | Zhu19,a | Matsui18,a | Bettenworthb | Herfarthb | Hampeb | Gotzb | Dingb | Karstensen17,a | Duijvesteinb | Roglerb | All studies | Published studies | Unpublished studies |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients, | 34 | 23 | 10 | 4 | 7 | 4 | 4 | 1 | 3 | 2 | 2 | 94 | 70 | 24 |
| Dilations, n (included in study) | 76 | 23 | 10 | 7 | 7 | 4 | 4 | 3 | 3 | 2 | 2 | 141 | 112 | 29 |
| Stricture location (nonexclusive) | ||||||||||||||
| Stomach strictures, % | 26.3 | 13 | 50 | 0 | 28.6 | 50 | 0 | 0 | 0 | 50 | 50 | 24.1 (16.2–32.0) | 25.0 (12.1–37.9) | 20.7 (0.00–42.1) |
| Duodenum strictures % | 73.7 | 87 | 90 | 100 | 71.4 | 50 | 100 | 100 | 100 | 50 | 50 | 78.7 (70.4–87.1) | 78.6 (64.2–93.0) | 79.3 (57.9–100.0) |
| Strictures ≤5 cm, % | 93.8 | 66.7 | 0 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 85.4 (62.3–100.0) | 81.3 (28.8–100.0) | 100 |
| TTS balloon dilation, % | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Maximal caliber of dilation, mm | 15 | 15.7 | 16.8 | 15.6 | 16.1 | 13.5 | 14.5 | 12 | 13.3 | 18 | 20 | 15.3 (14.7–15.8) | 15.3 (14.3–16.2) | 15.2 (13.7–16.7) |
| Steroid injection, % | 3.9 | 0 | 0 | 0 | 28.6 | 0 | 0 | 0 | 0 | 0 | 0 | 3.6 (0.20–6.9) | 2.7 (0.00–6.5) | 7.1 (0.00–22.8) |
| Technical success, % | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Short-term clinical efficacy, % | 86.1 | 63.6 | 100 | 100 | 100 | 100 | 50 | 100 | 100 | 100 | 100 | 87.0 (80.1–93.9) | 85.4 (74.4–96.5) | 92.6 (74.1–100.0) |
| Major complications per patient, % | 7.1 | 4.3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4.0 (0.59–7.3) | 5.1 (0.34–9.9) | 0 |
| Major complications per procedure, % | 4.2 | 4.3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2.9 (1.1–4.7) | 3.7 (1.9–5.5) | 0 |
| Cutting techniques used, % | 0 | 0 | 10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.71 (0.00–2.5) | 0.89 (0.00–4.7) | 0 |
| Stent used, % | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 33.3 | 0 | 0 | 0.71 (0.00–2.6) | 0.89 (0.00–4.9) | 0 |
| Redilation during follow-up period, % | 50.7 | 78.3 | 100 | 42.9 | 71.4 | 25 | 25 | 100 | 100 | 50 | 0 | 59.6 (43.7–75.4) | 62.6 (28.3–96.9) | 48.3 (22.7–73.8) |
| Symptomatic recurrence during follow-up period, % | 71.2 | 57.1 | 100 | 83.3 | 71.4 | 0 | 0 | 50 | 100 | 50 | 100 | 70.5 (60.1–80.9) | 75.0 (57.0–93.0) | 56.5 (23.9–89.1) |
| Surgery during follow-up period, % | 32.3 | 34.8 | 30 | 25 | 28.6 | 25 | 50 | 100 | 0 | 0 | 0 | 30.8 (25.7–35.8) | 31.3 (24.4–38.3) | 29.2 (13.9–44.5) |
NOTE. Overall estimates were obtained using survey methodology with study as a clustering effect. Overall estimates are shown as the pooled estimate (95% CI).
TTS, through-the-scope.
Published study.
Unpublished study.
Table 2.
Patient Characteristics
| Total (N = 94) | ||
|---|---|---|
| Factor | n | Statistics |
| Female sex | 94 | 56 (59.6) |
| Race/ethnicity | 92 | |
| Caucasian | 56 (60.9) | |
| African American | 2 (2.2) | |
| Asian | 33 (35.9) | |
| Other | 1 (1.1) | |
| BMI | 75 | 21.0 [17.3, 24.3] |
| Family history of CD | 82 | 4 (4.9) |
| Smoking | 84 | |
| Never | 63 (75.0) | |
| Current | 11 (13.1) | |
| Former | 10 (11.9) | |
| Age at diagnosis, y | 92 | 24.0 ± 10.6 |
| Age at time of stricture diagnosis, y | 94 | 33.7 ± 14.3 |
| Age at time of first dilation, y | 89 | 34.3 ± 14.6 |
| Disease location | ||
| Upper GI | 93 | 93 (100.0) |
| Jejunum/proximal ileum | 93 | 26 (28.0) |
| Ileocecal | 92 | 54 (58.7) |
| Colon | 93 | 41 (44.1) |
| Rectum | 93 | 27 (29.0) |
| Any EIM | 86 | 26 (30.2) |
| Upper GI strictures, n | 94 | |
| 1 | 74 (78.7) | |
| 2 | 18 (19.1) | |
| 3 | 2 (2.1) | |
| Patient outcomes | ||
| Total follow-up time, mo | 88 | 23.1 [9.8, 47.5] |
| Dilations during follow-up evaluation | 73 | |
| 1 | 25 (34.2) | |
| 2 | 13 (17.8) | |
| 3 | 14 (19.2) | |
| 4 | 9 (12.3) | |
| ≥5 | 12 (16.4) | |
| Stricture surgery | 91 | 28 (30.8) |
| Months to surgery | 28 | 3.6 [1.7, 7.3] |
NOTE. Statistics are presented as means ± SD, median is shown as [P25, P75] or N (column %).
BMI, body mass index; EIM, extraintestinal manifestation.
Table 3.
Stricture and Dilation Characteristics
| Total (N = 141) | ||
|---|---|---|
| Factor | n | Statistics |
| Stricture | ||
| Stricture location | 141 | |
| Stomach | 30 (21.3) | |
| Stomach and duodenum | 4 (2.8) | |
| Duodenum | 107 (75.9) | |
| Type of stricture | 64 | |
| Postsurgical/anastomotic | 7 (10.9) | |
| De novo | 57 (89.1) | |
| Length of stricture, cm | 39 | 3.0 [2.0, 10.0] |
| Length of stricture | 103 | |
| >5 cm | 15 (14.6) | |
| ≤5 cm | 88 (85.4) | |
| Prestenotic dilation | 136 | 63 (46.3) |
| PPI at the time of dilation | 137 | 97 (70.8) |
| Anti-TNF at time of dilation | 138 | 30 (21.7) |
| No therapy | 138 | 8 (5.8) |
| Dilation | ||
| Graded dilation | 137 | 96 (70.1) |
| Abnormal mucosa at time of dilation | 139 | 96 (69.1) |
| Maximum caliber of dilation, mm | 134 | 15.0 [14.0, 18.0] |
| Length of balloon, cm | 46 | 5.5 [5.5, 5.5] |
| Time of balloon inflation | 23 | 2.0 [2.0, 3.0] |
| Pressure of dilation, psi | 14 | 20.0 [20.0, 87.0] |
| Steroid injection | 140 | 5 (3.6) |
| Cutting techniques used | 140 | 1 (0.71) |
| Stent placement | 140 | 1 (0.71) |
| Outcomes of dilation | ||
| Technical success | 140 | 140 (100.0) |
| Passage of scope after dilation | 132 | 122 (92.4) |
| Relief of symptoms after dilation, clinical efficacy | 123 | 107 (87.0) |
| Major complications per procedure | 136 | 4 (2.9) |
| Redilation | 136 | 81 (59.6) |
| Months to redilation | 81 | 2.0 [1.2, 7.5] |
| If clinical efficacy, symptom recurrence | 95 | 67 (70.5) |
| Months to symptom recurrence | 67 | 2.0 (1.00, 5.1] |
| Medications between first and second dilation | 141 | 31 (22.0) |
| Duration of medical therapy between first and second dilation, wk | 24 | 6.5 [4.5, 20.2] |
NOTE. Statistics are presented as median [percentile25, percentile75] or N (column %).
PPI, proton pump inhibitor.
Major complications (defined as perforation, bleeding, or a dilation-related need for surgery) occurred in 2.9% per procedure and in 4% per patient, considering the possibility of multiple dilations over time in the same study subject. During a median follow-up period of 23.1 months, 70.5% of patients reported symptomatic recurrence, 59.6% required another dilation, and 30.8% of all patients had to undergo surgical intervention (Tables 2 and 3, and Figure 1A–C).
Figure 1.
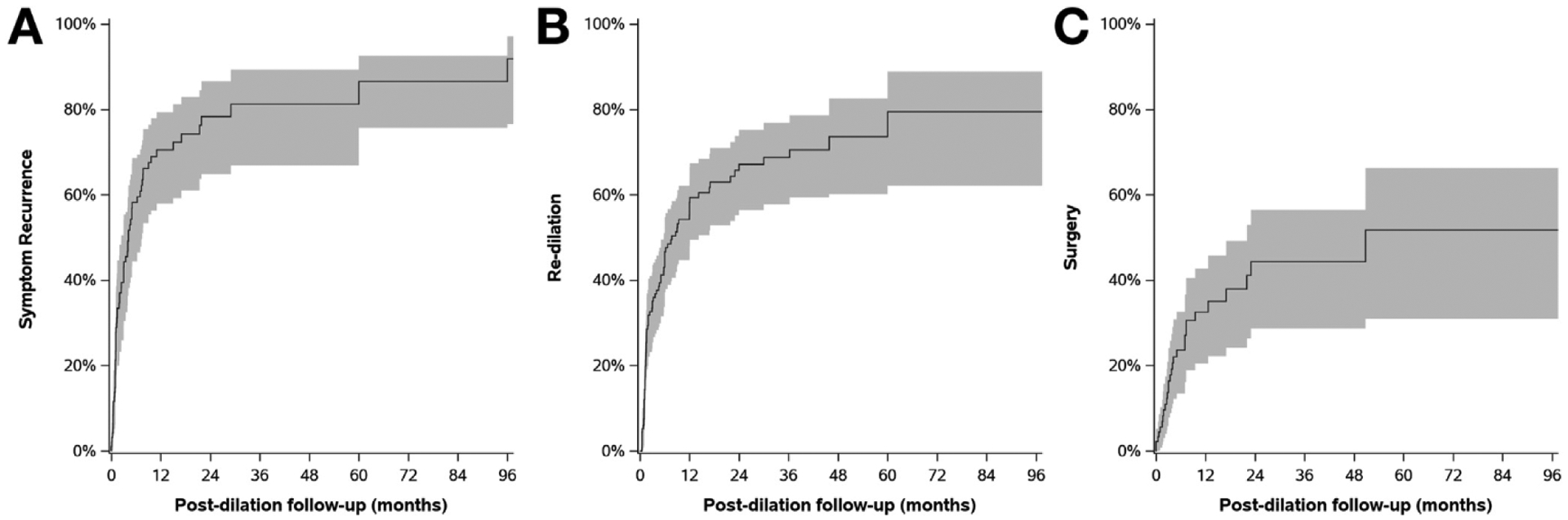
Risk for symptomatic recurrence, redilation, and stricture surgery in patients with endoscopic balloon dilation for primary CD-associated strictures in the upper GI tract over time. (A) Evaluating the future course after endoscopic dilation therapy indicates that symptom recurrence occurred in 58.2% and 70.5% of patients within 6 and 12 months, respectively. (B) Assessing the risk for redilation showed that 46.7% and 58.3% of patients required another dilation within 6 and 12 months after initial EBD, respectively, whereas (C) 23.6% and 32.5% needed surgery within 6 and 12 months after dilation, respectively.
Table 1 presents descriptive statistics for patients from each center as well as the random-effects analysis and measures of variability. The overall rates for symptom, dilation, and surgery-free survival at 6, 12, and 24 months are shown in Table 4.
Table 4.
Postdilation Event Rates
| Postdilation follow-up period, mo | Surgery | Redilation | Symptom recurrence |
|---|---|---|---|
| 6 | 23.6 (13.4–32.6) | 46.7 (37.2–54.7) | 58.2 (44.4–68.6) |
| 12 | 32.5 (20.5–42.8) | 58.3 (48.0–66.5) | 70.5 (57.9–79.3) |
| 24 | 44.3 (28.7–56.5) | 67.1 (56.5–75.2) | 78.3 (64.9–86.6) |
NOTE. Values are presented as the cumulative rate (95% CI).
To assess potential bias, we included both published and unpublished studies (Supplementary Tables 2–5) and performed a sensitivity analysis separately after excluding unpublished studies (Supplementary Tables 6–9). These results are presented and discussed in the Supplementary Materials and Methods section of this article and the data discussed later refer to the complete cohort only.
Factors Associated With Short-Term Dilation Outcome
Given the achievement of technical success in all included subjects, no analysis for factors associated with technical success could be performed. We hence evaluated factors associated with the short-term clinical efficacy of dilation procedures. Patients with active disease in the ileocecum had a lower likelihood of symptom relief in the adjusted and unadjusted analyses (odds ratio, 0.27; 95% CI, 0.058–1.2; P = .087 and odds ratio, 0.27; 95% CI, 0.06–1.2; P = .083, respectively). No other factor was linked to clinical efficacy (Supplementary Table 2).
Factors Associated With Symptom Recurrence
We next assessed factors associated with symptom recurrence. In univariate analysis, disease location in the jejunum/proximal ileum (hazard ratio [HR], 1.8; 95% CI, 1.09–2.9; P = .022) was associated with an increased hazard for symptom recurrence. In contrast, a stricture length shorter than 5 cm (HR, 0.41; 95% CI, 0.24–0.7; P = .001) was associated negatively with time to symptom recurrence. Although disease location in the jejunum/ileum was linked to symptom recurrence in the multivariate analysis (HR, 2.1; 95% CI, 1.3–3.5; P = .003), age at diagnosis was associated with diminished risk (HR, 0.85; 95% CI, 0.72–1.0; P = .054). Univariate and multivariate analyses did not detect any other factors that were linked to an increased risk of symptom recurrence (Supplementary Table 3).
Factors Associated With Need for Redilation
Regarding the need for redilation, univariate as well as multivariate analyses showed that Asian race (HR, 2.8; 95% CI, 1.7–4.5; P < .001 and HR, 2.8; 95% CI, 1.8–4.5; P < .001) and disease location in the jejunum/proximal ileum (HR, 1.7; 95% CI, 1.1–2.6; P = .015 and HR, 1.9; 95% CI, 1.2–2.9; P = .004) were associated with a significantly increased risk of redilation (Supplementary Table 4). None of the other investigated factors, including smoking, stricture location, type of stricture (de novo vs anastomotic), prestenotic dilation, graded dilation or maximum caliber of dilation, or anti-tumor necrosis factor (TNF) treatment were linked to the need for additional endoscopic therapy in the univariate or multivariate analyses (Supplementary Table 4).
Factors Associated With the Need for Surgery
Prestenotic dilation was linked to an increased risk for surgery in the univariate as well as multivariate analyses (HR, 2.0; 95% CI, 1.4–2.7; P < .001 and HR, 1.9; 95% CI, 1.3–2.7; P = .001, respectively) (Supplementary Table 5). In addition, in the univariate analysis, Asian race and younger age at time of dilation were found to be associated with an increased risk for surgery (HR, 1.7; 95% CI, 1.2–2.3; P = .003 and HR, 0.92; 95% CI, 0.87–0.98; P = .007, respectively), while increased body mass index and a positive family history of CD were associated with a reduced risk of need for surgery, but could not be confirmed by the multivariate analysis (HR, 0.91; 95% CI, 0.87–0.96; P < .001 and HR, 0.71; 95% CI, 0.51–0.99; P = .046, respectively). None of the other investigated factors, including smoking, disease location, type of stricture, graded dilation, or maximum caliber of dilation, was linked to need for earlier surgery (Supplementary Table 5).
Complications After Endoscopic Balloon Dilation
Complications associated with dilations occurred in 5 patients. This included 2 perforations and 3 bleeding events. No patient had to undergo dilation-associated surgery. Because of the low number of complications in the cohort, no meaningful analysis for risk factors could be performed. The 2 patients who experienced a perforation were treated by their first dilation procedure, the stricture length was less than 5 cm, and neither patient receive steroid treatment at the time of intervention.
Efficacy of Serial Dilations of Upper Gastrointestinal Strictures
Finally, we analyzed the efficacy of repeat dilations of the same stricture. Data on a second dilation were available for 22 episodes, and a third dilation for 9 episodes. With regard to technical success, all second and third dilations were successful. Although symptomatic relief of symptoms could be achieved in 86.2% of patients through the first dilation, clinical success was achieved in 85% of patients treated by a second dilation and by 88.9% of patients requiring a third dilation. The need for redilation was documented in 61.6% of patients after the first dilation and in 54.5% and 66.7% of patients being treated by a second and third dilation, respectively (all P > .05). Interestingly, time to redilation did not differ significantly between the first, second, and third dilation procedures (P > .05) (Supplementary Table 10).
Discussion
EBD is used frequently for the treatment of CD-associated strictures throughout the gastrointestinal tract. A pooled analysis of 3213 dilation procedures supports the efficacy and safety of this approach.14 Most studies, however, do not provide a separate analysis on the use of EBD for CD-associated strictures of the upper GI tract. More specifically, the 2 largest available studies on this indication include only 24 and 35 patients, respectively,16,19 precluding a thorough analysis of short- and long-term efficacy, safety, and predictors of success.
Our pooled analysis of international multicenter cohort studies comprised individual data sets of 94 CD patients who underwent EBD for upper GI strictures. Although 70 of the 94 analyzed cases were published previously, we were able to include 24 additional cases in the analysis. We found rates for technical and clinical success of 100% and 87%, respectively, and major complications occurred in 2.9% per procedure. During a median follow-up period of 23.1 months, the pooled individual patient analysis showed that 70.5% of patients experienced symptomatic recurrence, 59.6% underwent redilation, and 30.8% of patients required surgery. Patients with small-bowel disease location had a higher hazard for symptom recurrence and need for redilation. Prestenotic dilation was found to be a risk factor for needing an earlier surgery.
A large pooled analysis of EBD for ileocecal strictures reported technical and clinical success rates of 89.1% and 80.8%, respectively.14 Our study shows that dilation therapy for CD-associated strictures of the upper GI tract is comparably successful in the short term. The very high technical success rate observed in our study may result from the fact that we defined this parameter differently from prior studies by the ability to dilate the stricture after starting the procedure (but not by the ability to traverse the stricture after dilation). During a follow-up period of 23 months, long-term outcome parameters for dilation of CD-associated strictures of the upper GI tract such as symptoms recurrence, need for redilation, and surgery were not significantly different compared with the pooled data for CD-associated strictures of the ileocecum during a follow-up period of 24 months (70.5% vs 75.9%, 59.6% vs 73.5%, and 30.8% vs 42.9%, respectively),14 which came as a surprise given the common belief of clinicians that upper GI CD-associated stricture dilation is less durable. Finally, the complications rates per dilation procedure for ileocecal and upper GI strictures were comparable (2.8% vs 2.9%).14 These results are also in line with findings from other meta-analyses on EBD for CD-associated strictures.22,23 We were not able to assess if fluoroscopy impacted the complication rates of EBD because the vast majority of investigators reported using fluoroscopy at the discretion of the endoscopist and did not record its performance systematically. Taken together, our study provides evidence that endoscopic dilation of CD- associated strictures of the upper GI tract by EBD is effective and safe, with rates comparable with dilation therapy for CD-associated strictures of the ileocecum.
Identification of predictive factors for the long-term success of EBD of the upper GI tract would allow risk stratification of patients benefitting from a procedure. Patients with disease location in the jejunum/proximal ileum showed a higher rate of symptom recurrence and need for redilation. The patients with prestenotic dilation were at a higher risk for surgery. Prestenotic dilation is a feature that is not observed in every patient with stricturing CD but is regarded as a sign of advanced, longer-standing strictures with a higher fibrotic component, even though evidence supporting this notion is limited. In our cohort, patients’ symptoms were less likely to improve when prestenotic dilation was present and the time to surgery was shorter. This is in concordance with the recently published efficacy of adalimumab in patients with Crohn’s disease and symptomatic small bowel stricture study, which evaluated the efficacy of anti-TNF treatment for symptomatic small-bowel strictures.3 Patients with prestenotic dilation were at an increased risk for surgery. Because jejunal/proximal ileal disease was found to be associated negatively with symptom recurrence and need for redilation, it can be hypothesized that CD patients with disease manifestation at different locations along the GI tract may suffer from a more severe phenotype, or symptoms classified as obstructive originating from other regions of the GI tract. This assumption is supported by data from population-based studies indicating that CD patients with ileal involvement at the time of diagnosis are at an increased risk for a more aggressive disease phenotype.2 Interestingly, race showed an effect on dilation efficacy. Aside from the fact that Asians may have a higher risk for stricture recurrence, it may be explained by different strategies for the utilization of endoscopy and management strategies in this region.
Interestingly, active smoking was not found to be a risk factor for worse outcome of dilation therapy in our study. There is a body of evidence indicating the smoking aggravates the course of CD,24,25 increases the risk of postoperative recurrence,26,27 and smoking cessation decreases the risk for CD-related surgery.28 One study29 reported an increased risk for stricture recurrence after endoscopic dilation, however, the included patients suffered exclusively from ileocecal strictures.
Given the fact that stricture development follows the location of inflammation, it is logical that an early appropriate medical treatment of inflammatory CD of the upper GI tract may be the best approach to prevent the occurrence of CD-associated strictures. Indeed, a study by Decker et al30 evaluating 20 patients with esophageal CD from the Mayo Clinic (Rochester, MN) in the pre–anti-TNF era found modest treatment effects of steroids or immunomodulatory therapy (clinical response rates, 67% and 55%, respectively), and 3 of 20 patients finally required esophagectomy. In contrast, the findings from a more recent study from the same institution analyzing 24 cases of esophageal CD showed that early aggressive therapy including different anti-TNF agents and systemic and topical steroid therapy resulted in the complete resolution of clinical symptoms in 83% of patients and prevented surgical interventions in all patients.31 Future prospective studies will need to show whether early biologic therapy can prevent the occurrence of strictures or their need for redilation or surgery.
Our study had several limitations. Individual patient data sets were retrieved from 11 different centers and variations in the care patterns and approaches of the endoscopists may have influenced the results. In addition, and as delineated in the Materials and Methods section, definitions regarding parameters such as technical success and clinical efficacy differed between various studies. Key features, however, such as the use of through-the-scope balloons in all cases, maximum caliber of dilations, as well as the duration and pressure of balloon inflation, were quite similar among different centers. Furthermore, we were not able to exclude publication or reporting bias so that patients in whom dilation therapy could not be technically performed may have been under-represented in available publications. The retrospective noncontrolled observational nature of the study did not allow randomization based on risk factors or other criteria. Finally, the time point of evaluation of clinical efficacy was not standardized across studies. However, clinical efficacy was measured closely to dilation in all cases because symptom relief occurs almost immediately postprocedure. According to the Cochrane risk of bias tool, our study carries all potential inherent biases of cohort studies with retrospective data collection. In addition, reporting bias may apply because our study was a pooled analysis of already published studies. Centers with poor outcomes or high complication rates may not publish their cases. However, the largest published study included in this investigation by Singh et al16 included all dilations performed at this tertiary center. Finally, because we have incomplete data for some variables and outcomes attrition, bias may apply. However, of the 39 items assessed for patient characteristics, stricture characteristics, and outcome, 29 items were available in 85% of included patients or more. In particular, short- and long-term outcome parameters were available for the vast majority of patients.
Although our study adds important information to the literature, from a clinical point of view, our study cannot fully answer the question about which patients are treated best by EBD and which by surgical intervention. This clinical dilemma would require a head-to-head trial of the 2 modalities. The main value of this investigation lies in providing practicing providers with robust data for informed decision making in patients with upper GI CD.
Taken together, the results of this large multicenter evaluation of EBD for CD-associated strictures of the upper GI tract show high rates of short-term technical and clinical success. Given the moderate long-term efficacy and acceptable complication rate, EBD is a valuable treatment option in patients with stricturing CD of the upper GI tract when contraindications such as abscess, fistula, phlegmon, dysplasia, or malignancy have been excluded.
Supplementary Material
What You Need to Know.
Background
Intestinal strictures are a common complication of Crohn’s disease (CD). Strictures in patients that coincide with locations of inflammation and can affect the upper gastrointestinal (UGI) tract. Little is known about the efficacy and safety of endoscopic balloon dilation (EBD) for these patients.
Findings
We performed a meta-analysis of multicenter cohort studies of the effects of EBD for CD-associated strictures of the UGI tract. Technical and short-term clinical success rates were 100% and 87%, respectively, although major complications arose from 2.9% of procedures. During a median follow-up period of 23.1 months, 70.5% of patients had a recurrence of symptoms, 59.6% underwent redilation, and 30.8% of patients required surgery. Patients with disease locations in the small bowel had a higher hazard for symptom recurrence and need for redilation. Prestenotic dilation was a risk factor for needing surgery earlier.
Implications for patient care
In a meta-analysis, we found EBD for CD-associated strictures of the UGI tract to be a valuable alternative to surgery, with a high rate of short-term technical and clinical success, moderate long-term efficacy, and an acceptable rate of complications.
Funding
This work was supported by grants from the National Institutes of Health [T32DK083251, P30DK097948 Pilot, K08DK110415] to F.R.
Abbreviations used in this paper:
- CD
Crohn’s disease
- EBD
endoscopic balloon dilatation
- GI
gastrointestinal
- HR
hazard ratio
- TNF
tumor necrosis factor
Footnotes
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Clinical Gastroenterology and Hepatology at www.cghjournal.org, and at https://doi.org/10.1016/j.cgh.2018.11.048.
Conflicts of interest
The authors disclose no conflicts.
References
- 1.Torres J, Mehandru S, Colombel JF, et al. Crohn’s disease. Lancet 2017;389:1741–1755. [DOI] [PubMed] [Google Scholar]
- 2.Thia KT, Sandborn WJ, Harmsen WS, et al. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology 2010; 139:1147–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouhnik Y, Carbonnel F, Laharie D, et al. Efficacy of adalimumab in patients with Crohn’s disease and symptomatic small bowel stricture: a multicentre, prospective, observational cohort (CREOLE) study. Gut 2018;67:53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bettenworth D, Rieder F. Medical therapy of stricturing Crohn’s disease: what the gut can learn from other organs - a systematic review. Fibrogenesis Tissue Repair 2014;7:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rutgeerts P, Geboes K, Vantrappen G, et al. Predictability of the postoperative course of Crohn’s disease. Gastroenterology 1990;99:956–963. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto T, Fazio VW, Tekkis PP. Safety and efficacy of strictureplasty for Crohn’s disease: a systematic review and meta-analysis. Dis Colon Rectum 2007;50:1968–1986. [DOI] [PubMed] [Google Scholar]
- 7.Diederen K, de Ridder L, van Rheenen P, et al. Complications and disease recurrence after primary ileocecal resection in pediatric Crohn’s disease: a multicenter cohort analysis. Inflamm Bowel Dis 2017;23:272–282. [DOI] [PubMed] [Google Scholar]
- 8.Nugent FW, Roy MA. Duodenal Crohn’s disease: an analysis of 89 cases. Am J Gastroenterol 1989;84:249–254. [PubMed] [Google Scholar]
- 9.McCabe RP Jr, Chow CJ, Rothenberger DA. Duodenal-pleural fistula in Crohn’s disease: successful long-term medical management. Inflamm Bowel Dis 2013; 19:E38–E39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steel A, Dyer NH, Matthews HR. Cervical Crohn’s disease with oesophago-pulmonary fistula. Postgrad Med J 1988;64:706–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamamoto T, Allan RN, Keighley MR. An audit of gastroduodenal Crohn disease: clinicopathologic features and management. Scand J Gastroenterol 1999;34:1019–1024. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto T, Bain IM, Connolly AB, et al. Gastroduodenal fistulas in Crohn’s disease: clinical features and management. Dis Colon Rectum 1998;41:1287–1292. [DOI] [PubMed] [Google Scholar]
- 13.Rieder F, Latella G, Magro F, et al. European Crohn’s and Colitis Organisation topical review on prediction, diagnosis and management of fibrostenosing Crohn’s disease. J Crohns Colitis 2016;10:873–885. [DOI] [PubMed] [Google Scholar]
- 14.Bettenworth D, Gustavsson A, Atreja A, et al. A pooled analysis of efficacy, safety, and long-term outcome of endoscopic balloon dilation therapy for patients with stricturing Crohn’s disease. Inflamm Bowel Dis 2017;23:133–142. [DOI] [PubMed] [Google Scholar]
- 15.Gionchetti P, Dignass A, Danese S, et al. European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: part 2: surgical management and special situations. J Crohns Colitis 2017;11:135–149. [DOI] [PubMed] [Google Scholar]
- 16.Singh A, Agrawal N, Kurada S, et al. Efficacy, safety, and long-term outcome of serial endoscopic balloon dilation for upper gastrointestinal Crohn’s disease-associated strictures-a cohort study. J Crohns Colitis 2017;11:1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karstensen JG, Hendel J, Vilmann P. Endoscopic balloon dilatation for Crohn’s strictures of the gastrointestinal tract is feasible. Dan Med J 2012;59:A4471. [PubMed] [Google Scholar]
- 18.Matsui T, Hatakeyama S, Ikeda K, et al. Long-term outcome of endoscopic balloon dilation in obstructive gastroduodenal Crohn’s disease. Endoscopy 1997;29:640–645. [DOI] [PubMed] [Google Scholar]
- 19.Guo F, Huang Y, Zhu W, et al. Efficacy and safety of endoscopic balloon dilation for upper gastrointestinal strictures of Crohn’s disease. Dig Dis Sci 2016;61:2977–2985. [DOI] [PubMed] [Google Scholar]
- 20.Hirai F, Beppu T, Sou S, et al. Endoscopic balloon dilatation using double-balloon endoscopy is a useful and safe treatment for small intestinal strictures in Crohn’s disease. Dig Endosc 2010;22:200–204. [DOI] [PubMed] [Google Scholar]
- 21.Hirai F, Beppu T, Takatsu N, et al. Long-term outcome of endoscopic balloon dilation for small bowel strictures in patients with Crohn’s disease. Dig Endosc 2014;26:545–551. [DOI] [PubMed] [Google Scholar]
- 22.Navaneethan U, Lourdusamy V, Njei B, et al. Endoscopic balloon dilation in the management of strictures in Crohn’s disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc 2016;30:5434–5443. [DOI] [PubMed] [Google Scholar]
- 23.Morar PS, Faiz O, Warusavitarne J, et al. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther 2015;42:1137–1148. [DOI] [PubMed] [Google Scholar]
- 24.Bernstein CN, Rawsthome P, Cheang M, et al. A population-based case control study of potential risk factors for IBD. Am J Gastroenterol 2006;101:993–1002. [DOI] [PubMed] [Google Scholar]
- 25.Lakatos PL, Vegh Z, Lovasz BD, et al. Is current smoking still an important environmental factor in inflammatory bowel diseases? Results from a population-based incident cohort. Inflamm Bowel Dis 2013;19:1010–1017. [DOI] [PubMed] [Google Scholar]
- 26.Sutherland LR, Ramcharan S, Bryant H, et al. Effect of cigarette smoking on recurrence of Crohn’s disease. Gastroenterology 1990;98:1123–1128. [DOI] [PubMed] [Google Scholar]
- 27.De Cruz P, Kamm MA, Hamilton AL, et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet 2015;385:1406–1417. [DOI] [PubMed] [Google Scholar]
- 28.Lawrance IC, Murray K, Batman B, et al. Crohn’s disease and smoking: is it ever too late to quit? J Crohns Colitis 2013; 7:e665–e671. [DOI] [PubMed] [Google Scholar]
- 29.Gustavsson A, Magnuson A, Biomberg B, et al. Smoking is a risk factor for recurrence of intestinal stricture after endoscopic dilation in Crohn’s disease. Aliment Pharmacol Ther 2013; 37:430–437. [DOI] [PubMed] [Google Scholar]
- 30.Decker GA, Loftus EV Jr, Pasha TM, et al. Crohn’s disease of the esophagus: clinical features and outcomes. Inflamm Bowel Dis 2001;7:113–119. [DOI] [PubMed] [Google Scholar]
- 31.De Felice KM, Katzka DA, Raffals LE. Crohn’s disease of the esophagus: clinical features and treatment outcomes in the biologic era. Inflamm Bowel Dis 2015;21:2106–2113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


