Abstract
Purpose
To support the wellbeing of both patients and their families, our aim was to investigate the satisfaction of non-COVID in- and out-patients regarding safety measures implemented at our radiology unit of a transplant institute against COVID infection.
Materials and Methods
Over a five-month period, adult patients’ feedback was obtained by a questionnaire on the fear of contracting COVID-19 during a radiology examination, the perceived delay in treatment, and the following safety measures implemented: modified schedules to limit the number of patients in the waiting area and to maximize social distancing; assistance by staff when visitors were not admitted; cleaning and disinfection of machines; mask wearing and hand hygiene of staff; and staff advice on hand hygiene and infection control precautions.
Results
Over a five-month period, our preliminary results (387 patients) showed general patient satisfaction (99.1%) with safety measures applied at our radiology unit. Patients were satisfied with distancing and assistance by staff (100%), cleaning and disinfection (91%), mask wearing and hand hygiene of the staff (97%), and staff advice (94%). There was some criticism of the perceived delay in treatment (7.3%) and in the scheduling of the waiting list (5.4%), with 5.4% fearing contracting the virus. Patients’ awareness of safety measures and confidence in the hospital preparedness policy was perceived by all interviewers, and 100% appreciated being questioned.
Conclusion
The feedback given by the non-COVID patient helps to measure the quality in health care, to improve the quality service, and to protect and satisfy more vulnerable patients, also during the COVID-19 pandemic.
Keywords: COVID-19, Patient satisfaction, Radiology, Transplant recipient, Patient safety
Introduction
Even though more than a year has passed since it was declared a global health emergency by the World Health Organization (WHO), the coronavirus disease 2019 (COVID-19) pandemic is still spreading in our communities. To protect the health, safety, and wellbeing of patients/service users, staff, and visitors, prevent the spread of the virus, and to keep patients who need an imaging appointment safe, every radiology department has had to adapt to the new situation created by the COVID-19 pandemic by implementing several changes, learning from it, and reorganizing working procedures. However, during the first pandemic wave, patients were avoiding the hospital for as long as possible because they feared acquiring a COVID-19 infection during hospital visits on top of their chronic illness, and they were choosing not to seek the important treatment they needed [1–7].
Our Italian center is an institute for transplantation and treatments of end-stage organ failure, a reference hospital for the entire Mediterranean area. It is making an extremely strong effort to tackle the current COVID-19 pandemic, with a COVID intensive care unit (ICU) with the highest number of extracorporeal membrane oxygenation ECMO machines available in Sicily, and with a dedicated vaccination team and area built outside the hospital to support the vaccination campaign for transplant recipients, candidates, and senior citizens. Moreover, transplant programs are continuing to provide patients with the possibility to be treated, and complex surgical oncology procedures are regularly performed, thus ensuring continuity of care to patients, in line with the guidelines of the Italian National Transplant Center on the management of organ donors during the COVID-19 pandemic.
There is no emergency room, and the COVID ICU is detached from the institute’s main structure, with dedicated staff and equipment. Given that patients with a condition of immunosuppression, including transplanted patients, are more susceptible, with a higher possibility of over infection [8–10], as well as for all others, the COVID-19 pandemic has led to major changes in clinical activity at our radiology unit as well. In view of our particularly vulnerable patients, we rigorously drafted and applied radiology guidelines and recommendations [11–36] for the safe imaging of adult and pediatric patients and had to adapt our daily activities to implement safety measures to achieve capacity for safety continued operation for all our patients.
To protect our frail patients, what we have learned from the pandemic is the importance of following strict safety guidelines, and the need for close collaboration among radiologists, radiographers, nurses, transporters, and clinicians to provide a united front against the virus during such a critical time.
A set of policies and procedures was prepared and directly applied at our imaging unit, designed to support the care of non-COVID-19 patients, and to maintain radiologic diagnostic, and interventional support for the entire institute.
Some studies have evaluated various aspects of the pandemic’s impact on cancer patients [37–39]; however, to the best of our knowledge, no one has assessed patients’ emotions and confidence in hospital infection prevention by investigating the satisfaction of non-COVID patients with safety measures against COVID-19.
Because understanding the intangible aspects of perception and expectation that contribute to patient satisfaction supports the wellbeing of both patients and their families, our aim was to investigate the satisfaction of non-COVID in- and out-patients regarding safety measures against COVID-19 implemented at our radiology unit during the second pandemic wave.
Materials and methods
Safety measures applied at our institute’s entry point
Our institute implemented screeners at the entrance for all workers and those undergoing patient imaging or procedures. Temperature scanners are used, and everyone is invited to sanitize hands and change face masks with those provided by hospital before entry. In addition, patients requiring hospitalization are swabbed and wait for their “negative” test results before becoming in-patients.
Patients who present with symptoms that could be related to SARS-Cov-2 infection have their exams or hospitalization canceled and are asked to follow up with their primary care physician.
Patients who need an emergency hospitalization, coming from other hospitals and not swabbed, are managed as COVID-positive patients, placed in an isolated room, and all safety measures for droplet precaution are employed. The decision to remove patients from isolation is determined by our infection control staff.
Safety measures applied at our radiology unit.
According to WHO recommendations [11–14], interventional radiology societies’ guidelines [15–18], select publications by the European Societies of Radiology [19–25], and by the Italian Society of Medical Radiology (SIRM) [26–30], and some other papers [31–36], our department adhered strictly to infection control measures, including patient and health care worker screening at the entrance, adequate hand hygiene, equipment hygiene, proper personal protective equipment (PPE) supplies, and workflow reorganization.
In order to sustain hygiene measures and provide the time to sanitize imaging rooms between patients, the overall capacity of the radiology department was reduced. Consequently, to maintain activity for all our patients, a detailed operational plan was prepared to increase the activity in the radiology unit over a period of four weeks, scheduling patients for a specific timetable and avoiding an excess number of patients in the waiting room at any one time. Waiting rooms were adapted respecting the appropriate distance to prevent cross-transmission, and all of our seating has been spaced apart and has special health care-specific fabric that is easy to clean. As part of our efforts to minimize risk, ensure that we adhere to the social distancing guidance, and provide maximum protection for all of our patients and staff, we restricted the number of visitors in health care settings, requesting that no one accompany adult patients to their appointment unless for special needs or accompanying a child requiring imaging. Additional safety measures are in place, including the maintenance of separate waiting areas for patients with symptoms of illness isolated from other patients and regularly disinfected; thorough cleaning of our machines between each patient; and staff wearing of masks and other protective equipment such as gloves and disposable gowns. In addition, our experienced staff was trained to guide patients through their exam in a safe environment, encouraging patients to listen and adhere to staff advice on hand hygiene and infection control precautions on arriving and leaving the area.
In addition, when an emergency hospitalized patient (managed as COVID-positive) needs to be imaged, a dedicated portable X-ray and ultrasound machine is used to image only these kinds of patients in their isolated room. On the other hand, CT scans and interventional procedures are performed at dedicated sites with less foot traffic and dedicated paths. In these cases, the number of staff in direct contact with the patient is reduced and the radiology staff involved wears the necessary PPE, including coverall suit, medical mask, gloves, eye protection, and, when necessary, lead protective equipment. Reusable devices and the rooms are cleaned and disinfected at the end of each procedure.
Patient interview
From September 2020 to February 2021, adult patients' feedback was obtained by a questionnaire. Because no sensitive data were included, informed consent was waived by our Institutional Research Review Board.
In- and out-patients, who went to our radiology unit to undergo radiography, CT scan, MRI, ultrasound, and interventional radiology procedures were questioned.
We created an online custom form for questionnaires using the free access Google form. To avoid contact with a tablet or other devices used to make questionnaires, questions were made as interviews by the radiographers and or radiologist at the end of any radiology procedure, each one using their smartphones.
Because while searching the U.S. National Library of Medicine’s biomedical literature database PubMed we did not find any validated questionnaires aimed at evaluating the satisfaction of non-COVID patients with safety measures against COVID-19 diffusion, our team drew up ten questions for the interview.
Information about the kind of procedure patients underwent was included on the form. In addition, seven questions about the following safety measures implemented were questioned: modified schedules; machine cleaning and disinfection; mask wearing, and hand hygiene for all patients. The fear of contracting COVID-19 during radiology examination and the perceived delay in treatment was also investigated. Instead, because in-patients do not go to the waiting area, questions about the limit in the number of people in the waiting area and seating spacing were drafted only for out-patients. Finally, because visitors were admitted only in cases of all pediatric patients or in cases of out-patients not collaborative or with severe dementia, assistance by staff when visitors were not admitted was also investigated.
Results were analyzed by exporting datasheets from Google form as an Excel file.
To allow the patient to express how much they agree or disagree with the statements included in the questionnaire, responses on satisfaction were scored using a five-point Likert scale as follows: 1 = very dissatisfied; 2 = dissatisfied; 3 = neutral; 4 = satisfied; 5 = very satisfied.
Instead, responses on fear of contracting the virus at our unit were scored as follows: 1 = not at all; 2 = not much; 3 = neutral; 4 = quite a lot; 5 = a lot.
Results
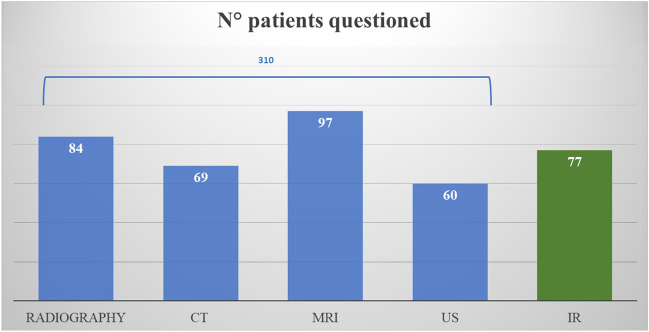
Over a five-month period, 387 patients (40% in-patients and 60% out-patients) were questioned. Patients were 84 for radiography, 69 for CT scan, 97 for MRI, 60 for ultrasound, and 77 for interventional radiology procedures (Fig. 1).
Fig. 1.
Number of patients questioned according to imaging modality. 80.1% for radiography, computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US). The remaining19.9% for interventional radiology (IR)
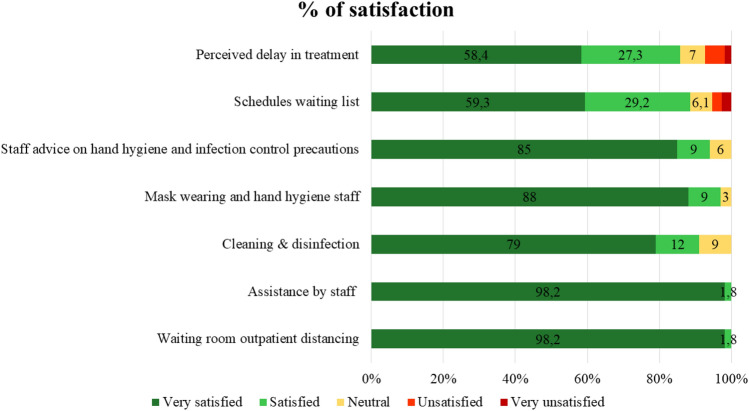
Our results show a general patient satisfaction with safety measures applied at our radiology unit (score 5 = 86.4%; score 4 = 12.7%; score 3 = 0.9%) and, as Fig. 2 shows, not one response had scores of 1 or 2.
Fig. 2.
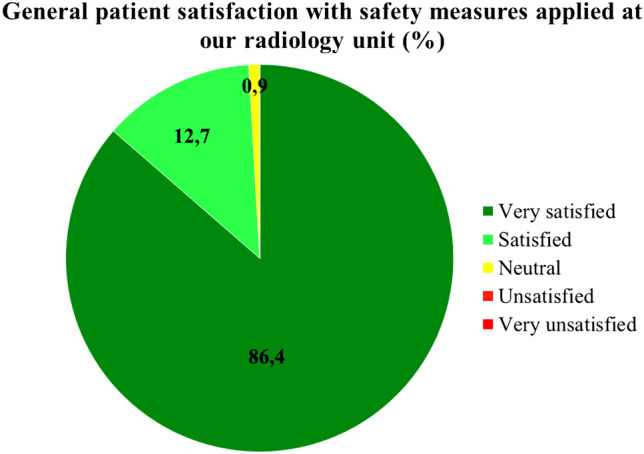
General patient satisfaction with safety measures applied at our radiology unit
In particular, satisfaction was noted regarding the following safety measures: distancing (score 5 = 98.2%; score 4 = 1.8%), assistance by staff when visitors are not admitted (score 5 = 98.2%; score 4 = 1.8%), cleaning and disinfection (score 5 = 79%; score 4 = 12%; score 3 = 9%), mask wearing and hand hygiene by the staff (score 5 = 88%; score 4 = 9%; score 3 = 3%), staff advice on hand hygiene and infection control precautions (score 5 = 85%; score 4 = 9%; score 3 = 6%). Some slight criticism regarding the perceived delay in treatment (score 1 = 1.8%; score 2 = 5.5%), and in the scheduling of the waiting list (score 1 = 2.7%; score 2 = 2.7%) was reported (Fig. 3). Furthermore, despite all safety measures applied, some patients still seemed to fear contracting the virus at our unit (score 1 = 0.9%; score 2 = 4.5%) (Fig. 4). A considerable patient awareness of safety measures and confidence in the hospital preparedness policy was perceived by all interviewees. All patients (100%) appreciated being questioned.
Fig. 3.
Results in percentage of patients’ perceived delay in treatment and satisfaction with the schedules waiting list, and the following safety measures: staff advice on hand hygiene and infection control precautions; mask wearing and hand hygiene of the staff; cleaning and disinfection; assistance by staff when visitors are not admitted; distancing in waiting room
Fig. 4.
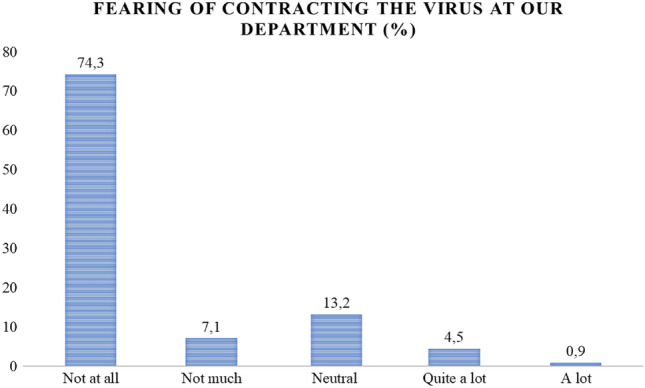
Percentage of patients who still fear contracting the virus at our unit
Discussion
Infection with COVID-19 has affected the entire world since March 2020 and has been shown to be more severe in patients with comorbidities and with a condition of immunosuppression [8–10], so that patients’ perception of the hospital seemed to be changed from a place of safety to one of danger and fear [1–7, 37–39].
Our survey’s results demonstrate that implementing safety measures against COVID-19 diffusion to achieve a safe continual operation and following strict safety guidelines can result in a generally vulnerable patient’s satisfaction with the safety measures applied and, as consequence, the prevalence of fear of contracting the virus during hospital visits, in particular during an imaging procedure, can decrease. To achieve this goal, critical information about the importance of strictly adhering to policies should be reliably passed on to all members of the radiology team, including radiologists, radiographers, nurses, and any others working in the department to create a united front against the virus. Generally, the strict adherence to recommendations is applied to protect the vulnerability of frontline health workers fighting COVID-19, who put themselves and their families at risk to treat patients and contain the spread of this disease. Instead, in a context like ours, the main objective is to protect patients who are more vulnerable than the staff; thus, an incredible commitment to this effort by the staff is necessary. A lack of communication on these important points could pose a serious risk, especially to patients.
On the other hand, because a patient’s perception of time elapsed between appointment time and procedure start time has been proven as a significant predictor of overall mean patient satisfaction scores [40], even if the schedule seemed us to be adequate and well organized, the perceived delay in treatment and in the schedules waiting list suggests that we should re-evaluate workload patterns for a more effective distribution of appointments. If it cannot be applied because it would cause an excess number of patients in the waiting room at any one time, radiologists, radiographers, and nurses’ effective communication with patients should be improved so patients may understand why appointments are organized that way.
Finally, the patients’ awareness and confidence in safety measures and in the hospital preparedness policy, and above all the appreciation to be questioned noted, suggest that assessing patient satisfaction is a core component of practicing radiology activity around the patient. Among the most important factors that determine patient satisfaction are the department’s ability to provide the promised and accurate service that was offered, as well as a sense of confidence and competence [40]. All these factors gain more value at a time like this when patients need to regain trust in hospitals to seek their important treatment. Encouraging patients to provide information, rather than asking questions and giving directions, could help hospitals in making patients understand that their involvement and the quality of care they perceive has an impact on decision-making, even in the war against COVID-19.
This study has some limitations: First, even though the questionnaire was randomly distributed, pediatric patients, patients with severe dementia, or not collaborative were not questioned; second, the sample size was relatively small. Despite this, to our knowledge, this paper is the only one investigating the satisfaction of non-COVID patients with safety measures against COVID-19 diffusion applied at a radiology department.
Conclusion
The COVID-19 pandemic poses unprecedented challenges for provision and maintenance of radiology services. Patient awareness of general safety measures during the second pandemic wave makes them less afraid than during the first. Moreover, because this awareness allows patients to look at safety measures implemented at our radiology department more critically, the feedback given by the non-COVID patient helps to improve the quality of service to protect and satisfy vulnerable patients during a such a particular situation.
Acknowledgements
No funds, Grants, or other support were received.
Authors' contributions
All the authors provided substantial contribution to conception and design of the article, or acquisition, analysis, and interpretation of data, drafting of the article or revising it critically for important intellectual content and approved the final version to be published.
Funding
No funds, grants, or other support were received.
Availability of data and material
Corresponding author Giuseppe Mamone.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The manuscript does not contain clinical studies or patient data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Roberta Gerasia, Email: rgerasia@ismett.edu.
Giuseppe Mamone, Email: gmamone@ismett.edu.
Santina Amato, Email: samato@ismett.edu.
Antonino Cucchiara, Email: acucchiara@ismett.edu.
Giuseppe Salvatore Gallo, Email: gsgallo@ismett.edu.
Corrado Tafaro, Email: ctafaro@ismett.edu.
Giuseppe Fiorello, Email: gfiorello@ismett.edu.
Calogero Caruso, Email: ccaruso@ismett.edu.
Roberto Miraglia, Email: rmiraglia@ismett.edu.
References
- 1.Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020 doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020 doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boeken T, Le Berre A, Mebazaa A, Boulay-Coletta I, Hodel J, Zins M. Non-COVID-19 emergencies: where have all the patients gone? Eur Radiol. 2020 doi: 10.1007/s00330-020-06961-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apisarnthanarak A, Siripraparat C, Apisarnthanarak P, et al. Patients' anxiety, fear, and panic related to coronavirus disease 2019 (COVID-19) and confidence in hospital infection control policy in outpatient departments: A survey from four Thai hospitals. Infect Control Hosp Epidemiol. 2020;1–2:7. doi: 10.1017/ice.2020.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong LE, Hawkins JE, Langness S, Murrell KL, Iris P, Sammann A (2020) Where are all the patients? addressing Covid-19 fear to encourage sick patients to seek emergency care. 10.1056/CAT.20.0193
- 6.Sutcuoglu O, Yazici O, Ozet A, Nuriye O. Harmful consequences of COVID-19 fear in patients with cancer. BMJ Support Palliat Care. 2020 doi: 10.1136/bmjspcare-2020-002628. [DOI] [PubMed] [Google Scholar]
- 7.Vanni G, Materazzo M, Pellicciaro M, et al. Breast cancer and COVID-19: the effect of fear on patients' decision-making process. In Vivo. 2020 doi: 10.21873/invivo.11957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farfour E, Picar C, Beaumont L, et al. Sars-Cov-2 Foch hospital study group. COVID-19 in lung-transplanted and cystic fibrosis patients: be careful. J Cyst Fibros. 2020 doi: 10.1016/j.jcf.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mella A, Mingozzi S, Gallo E, et al. Case series of six kidney transplanted patients with COVID-19 pneumonia treated with tocilizumab. Trans Infect Dis Off J Transpl Soc. 2020 doi: 10.1111/tid.13348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nacif LS, Zanini LY, Waisberg DR, et al. COVID-19 in solid organ transplantation patients: a systematic review. Clinics (Sao Paulo) 2020 doi: 10.6061/clinics/2020/e1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World health Organization (2020) Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): interim guidance; https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed 27 November 2020.
- 12.World health Organization (2020) Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages Interim guidance, https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages Accessed 23 December 2020
- 13.World health Organization (2020) Technical specifications of personal protective equipment for COVID-19 https://www.who.int/publications/i/item/WHO-2019-nCoV-PPE_specifications-2020.1 Accessed 23 December 2020
- 14.World health Organization (2020) Coronavirus disease (COVID-19): Masks https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-masks Accessed 23 December 2020
- 15.CIRSE (2020) Cardiovascular and Interventional Radiological Society of Europe: Checklist for preparing your IR service for COVID-19 https://www.cirse.org/wp-content/uploads/2020/04/CIRSE_APSCVIR_Checklist_COVID19.pdf Accessed 10 December 2020
- 16.BSIR (2020) BSIR guidance regarding PPE use in IR in patients proven or suspected of COVID-19 Infection https://www.bsir.org/mediacentre/news/bsir-guidance-regarding-ppe-use-in-ir-in-patients-proven-or-suspected-of-covid-19-infection/ Accessed 27th March 2020
- 17.Tarantini G, Fraccaro C, Chieffo A, et al. GISE. Italian Society of Interventional Cardiology (GISE) position paper for Cath lab-specific preparedness recommendations for healthcare providers in case of suspected, probable or confirmed cases of COVID-19. Catheter Cardiovasc Interv. 2020 doi: 10.1002/ccd.28888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SERVEI (2020) Guidelines for vascular and interventional radiology units during the COVID-19 outbreak. A consensus statement from the Spanish Society of Vascular and Interventional Radiology (SERVEI) https://servei.org/wp-content/uploads/Guidelines-for-vascular-and-interventional-radiology-units-during-the-COVID-19-outbreak.pdf Accessed 27th March 2020
- 19.ESR (2020) https://www.myesr.org/covid-19-resources Accessed 27th November 2020
- 20.Ding J, Fu H, Liu Y, et al. Prevention and control measures in radiology department for COVID-19. Eur Radiol. 2020 doi: 10.1007/s00330-020-06850-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Politi LS, Balzarini L. The Radiology Department during the COVID-19 pandemic: a challenging, radical change. Eur Radiol. 2020 doi: 10.1007/s00330-020-06871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martín-Noguerol T, Lopez-Ortega R, Ros PR, et al. Teleworking beyond teleradiology: managing radiology departments during the COVID-19 outbreak. Eur Radiol. 2021 doi: 10.1007/s00330-020-07205-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tay KH, Ooi CC, Mahmood MIB, et al. Reconfiguring the radiology leadership team for crisis management during the COVID-19 pandemic in a large tertiary hospital in Singapore. Eur Radiol. 2021 doi: 10.1007/s00330-020-07116-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Devaraj A. Important lessons for infection control in radiology departments during the COVID-19 pandemic. Eur Radiol. 2020 doi: 10.1007/s00330-020-06873-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen RC, Tan TT, Chan LP. Adapting to a new normal? 5 key operational principles for a radiology service facing the COVID-19 pandemic. Eur Radiol. 2020 doi: 10.1007/s00330-020-06862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.SIRM (2020) https://www.sirm.org/wp-content/uploads/2020/11/Sirm_Spallanzani.pdf Accessed 27th November 2020
- 27.SIRM (2020) https://www.sirm.org/wp-content/uploads/2020/04/disinfezioneepuliziaTC.pdf Accessed 27th November 2020
- 28.SIRM (2020) https://www.sirm.org/wp-content/uploads/2020/04/RadDept_prepar_Radiology.pdf Accessed 27th November 2020
- 29.SIRM (2020) https://www.sirm.org/wp-content/uploads/2020/04/Procedure-covid19_cotugno.pdf Accessed 27th November 2020
- 30.SIRM (2020) https://www.sirm.org/wp-content/uploads/2020/04/cleaning_CT-1.pdf Accessed 27th November 2020
- 31.Sheth S, Fetzer D, Frates M, et al. Guidelines for ultrasound in the Radiology Department during the COVID-19 pandemic. Ultrasound Q. 2020 doi: 10.1097/RUQ.0000000000000526. [DOI] [PubMed] [Google Scholar]
- 32.Stogiannos N, Fotopoulos D, Woznitza N, Malamateniou C. COVID-19 in the radiology department: what radiographers need to know. Radiography (Lond) 2020 doi: 10.1016/j.radi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vermani S, Kaushal A, Kaushal J. COVID-19 and the Radiology Department: what we know so far. SN Compr Clin Med. 2020 doi: 10.1007/s42399-020-00554-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azam SA, Myers L, Fields BKK, et al. Coronavirus disease 2019 (COVID-19) pandemic: review of guidelines for resuming non-urgent imaging and procedures in radiology during Phase II. Clin Imaging. 2020 doi: 10.1016/j.clinimag.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mossa-Basha M, Medverd J, Linnau KF, et al. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington. Radiology. 2020 doi: 10.1148/radiol.2020201326. [DOI] [PubMed] [Google Scholar]
- 36.Chandy PE, Nasir MU, Srinivasan S, Klass D, Nicolaou S, Babu SB. Interventional radiology and COVID-19: evidence-based measures to limit transmission. Diagn Interv Radiol. 2020 doi: 10.5152/dir.2020.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Catania C, Spitaleri G, Del Signore E, et al. Fears and perception of the impact of COVID-19 on patients with lung cancer: a mono-institutional survey. Front Oncol. 2020 doi: 10.3389/fonc.2020.584612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen G, Wu Q, Jiang H, et al. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psychooncology. 2020 doi: 10.1002/pon.5451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gultekin M, Ak S, Ayhan A, et al. Perspectives, fears and expectations of patients with gynaecological cancers during the COVID-19 pandemic: a Pan-European study of the European Network of Gynaecological Cancer Advocacy Groups (ENGAGe) Cancer Med. 2020 doi: 10.1002/cam4.3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McDonald AP, Kirk R. (2013) Using lean Six Sigma to improve hospital based outpatient imaging satisfaction. Radiol Manage. 2013;35(1):38–45. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Corresponding author Giuseppe Mamone.
Not applicable.