Abstract
During the coronavirus disease 19 (COVID-19) pandemic, extracorporeal membrane oxygenation (ECMO) has been proposed as a possible therapy for COVID-19 patients with acute respiratory distress syndrome. This pictorial review is intended to provide radiologists with up-to-date information regarding different types of ECMO devices, correct placement of ECMO cannulae, and imaging features of potential complications and disease evolution in COVID-19 patients treated with ECMO, which is essential for a correct interpretation of diagnostic imaging, so as to guide proper patient management.
Keywords: Coronavirus disease 19 (COVID-19), Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Acute respiratory distress syndrome (ARDS), Extracorporeal membrane oxygenation (ECMO), X-ray, Computed tomography
Introduction
In January 2020, several cases of interstitial pneumonia were reported in Wuhan, China. Since mid-January 2020, the first cases of the disease were also found outside of China, and on 11 March 2020 the World Health Organization declared the coronavirus disease 19 (COVID-19) outbreak a pandemic [1]. A novel coronavirus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified as the causative agent of the disease [2, 3].
The clinical spectrum of COVID-19 can range from no symptoms to critical illness, with an estimated incidence of acute respiratory distress syndrome (ARDS) among hospitalized COVID-19 patients hovering around 33% [4, 5]. While the reference standard for diagnosis is real-time reverse-transcription polymerase chain reaction (rt-PCR) test applied on respiratory tract specimens, chest multidetector computed tomography (CT) may help in the early detection, management, and follow-up of COVID-19 pneumonia [5–9]. Typical CT features of COVID-19 pneumonia include bilateral ground glass opacities with a predominant posterior and peripheral distribution, parenchymal consolidations with or without air bronchogram, interlobular septal thickening and crazy paving pattern, usually without pleural effusion or enlarged mediastinal lymph nodes [10–12].
In patients with COVID-19-unrelated ARDS, extracorporeal membrane oxygenation (ECMO) can be resorted to as a rescue therapy, allowing for temporary replacement of lung and/or heart function with artificial analogs in cardiac or pulmonary failure refractory to conventional clinical treatment [13]. The evidence collected so far in the literature has yielded mixed results, but several studies [14, 15] have reported a survival rate in patients with COVID-19-related ARDS treated with ECMO not lower compared to those with COVID-19-unrelated ARDS [16, 17]. Due to the use of ECMO in COVID-19 patients, there is an obvious need for radiologists to be familiar with the normal appearance of ECMO devices and the radiological findings of ECMO-related complications. While some articles have reported the main imaging findings in patients with ECMO [18–21], to the best of our knowledge no systematic reports of the imaging findings of ECMO in COVID-19 patients have been published to date.
Our purpose is to overview the imaging appearance of the catheters of ECMO devices in patients with COVID-19-related ARDS, as well as of potential complications that may arise secondary to either ECMO device placement or COVID-19 infection.
ECMO: pathophysiological rationale and configurations
The ECMO circuit consists of a pump that propels the patient's blood to an oxygen membrane (allowing the blood to be enriched with oxygen and to eliminate carbon dioxide) and two access routes (one for drainage and one for return of the blood to the patient) [22, 23]. ECMO can be implemented using a venovenous (VV) or venoarterial (VA) configuration modality. VV-ECMO is used in patients with reversible respiratory failure and preserved cardiac function, whereas VA-ECMO is used in patients with cardiac failure, irrespective of lung function being preserved or not.
According to the Extracorporeal Life Support Organization (ELSO) recommendations, VV-ECMO may be utilized for patients with COVID-19 and severe respiratory failure with expected outcomes comparable to patients supported with VV-ECMO before the COVID-19 pandemic. On the other hand, VA-ECMO may be utilized for patients with COVID-19 and severe cardiac failure. However, the experience regarding VA-ECMO in COVID-19 patients is more limited [24].
In VA-ECMO, the drainage cannula is generally inserted into the internal jugular vein or into the femoral vein. The return cannula is preferentially placed into the femoral artery.
The classic VV-ECMO configuration consists of two cannulae: a) the drainage cannula inserted into the femoral vein, with the tip at the junction between the inferior vena cava (IVC) and the right atrium, and b) the return cannula inserted into the internal jugular vein, with the tip to the level of the superior vena cava (SVC)-right atrial junction (Fig. 1a).
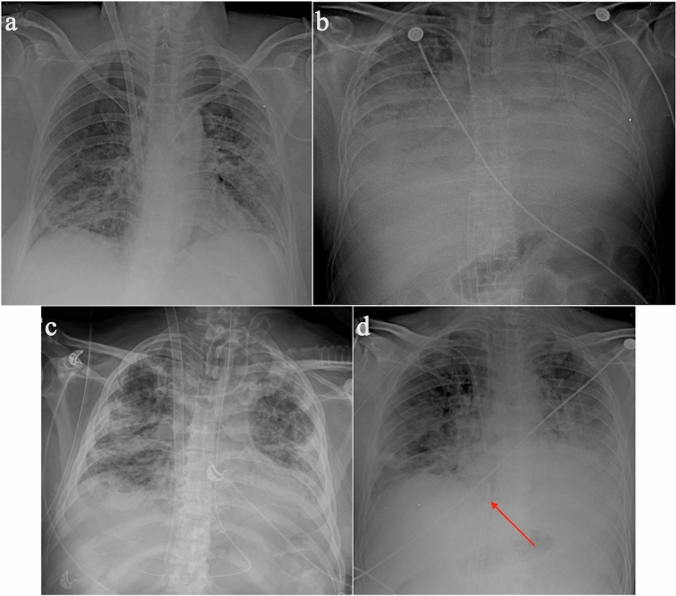
Fig. 1.
Chest radiographs (antero-posterior view) showing a correct placement of VV-ECMO, b correct placement of femorofemoral ECMO, c correct placement of double lumen ECMO, d incorrect placement of femorofemoral ECMO. The tip of the drainage cannula (arrow) is too close to the tip of the return cannula
Another configuration is femorofemoral ECMO (also known as a double VV-ECMO cannulation), in which the drainage cannula is introduced into the femoral vein and advanced upwards until the tip reaches the distal IVC. The return cannula is inserted into the contralateral femoral vein with the tip in the right atrium (Fig. 1b).
The third configuration is the dual lumen VV-ECMO. It consists of a single cannula with a double lumen inserted from the right internal jugular vein with its tip in the IVC [25] (Fig. 1c).
According to the aforementioned ELSO guidelines, in COVID-19 patients dual lumen cannulae should be avoided if possible, as they take relatively longer time to be inserted and are associated with a higher risk of thrombotic complications and malpositioning, requiring repeat echocardiography with associated greater resource utilization and staff exposure [26].
Positioning of ECMO cannulae: imaging findings
After the placement of ECMO cannulae, an X-ray of the chest and abdomen should be performed to evaluate their position and the distance between them, and to detect potential complications such as pneumothorax or hemothorax.
In VV-ECMO, a distance of 15 cm between the tips of the two cannulae is recommended to avoid the phenomenon of “recirculation”, by which oxygenated blood coming to the return cannula is withdrawn through the drainage cannula without passing through the systemic circulation (Fig. 1d) [27]. A return cannula placed too inferiorly, or a drainage cannula placed too high may cause obstruction of hepatic outflow or SVC, respectively [19]. A high placement of the cannula tip in the upper SVC is associated with a higher risk of complications such as pulmonary embolism and catheter-related sepsis, whereas placement of the cannula in the RA increases the risk of cardiac tamponade. Correct positioning of the cannula is obtained when its tip is placed within the most caudal 3 cm of the SVC, but this goal is difficult to achieve. For this purpose, contrast-enhanced trans-thoracic echocardiography has been described as a useful tool for detecting tip position [28, 29].
Imaging follow-up
According to the ELSO guidelines, ultrasonography and chest or abdomen X-rays may be performed safely at bedside as indicated, whereas multidetector CT should only be used if imaging findings may change patient management or outcome [26]. This is because CT imaging requires transferring a critically ill patient to the radiology department, thereby increasing the risk of complications (such as cannula dislodgement). However, there is no clear indication about the optimal interval at which chest X-rays should be repeated to monitor lung involvement.
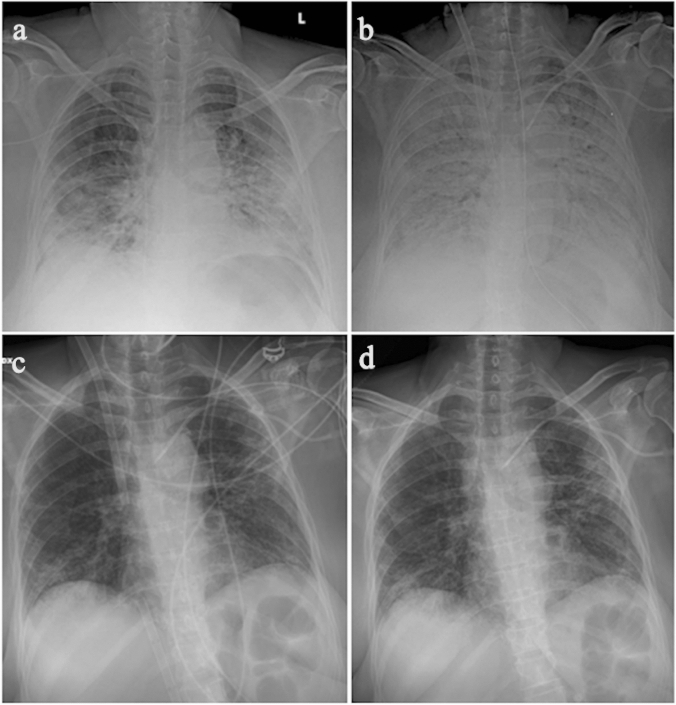
Generally, imaging of the lung parenchyma of patients with COVID-19-unrelated ARDS is of limited value in the first 7–14 days of ECMO support, due to lung opacification reflecting changes in pulmonary physiology and hemodynamics and an abrupt decrease in airway pressure. Furthermore, an improvement in lung aeration is best assessed clinically. Therefore, a chest X-ray performed immediately before and after ECMO placement, followed by chest X-ray every 2–3 days, is considered to be sufficient if the patient is stable [20] (Fig. 2).
Fig. 2.
Chest radiographs a before and b after ECMO placement, showing correct placement of cannulae and complete whiteout of both lungs. c Chest radiographs performed at day 9 showing improvement in lung aeration and d) performed after ECMO removal, respectively
Lung ultrasonography may represent an alternative to chest X-ray and CT [30]. Møller-Sørensen et al. found that in patients with COVID-19 treated with VV-ECMO, lung ultrasonography can distinguish patients with improving pulmonary function from those with stationary or deteriorating pulmonary function [31]. However, according to the Multinational Consensus Statement from the Fleischner Society, avoidance of non-value-added imaging is particularly important in the COVID-19 patient population to minimize exposure risk in radiology technologists and to conserve personal protection equipment [32]. In this context, it should also be taken into account that several studies have shown no difference in mortality or ventilator days for patients in the intensive care unit imaged on-demand, compared with a daily routine protocol [33–35].
Imaging of ECMO-related complications
Complications may be related either to the patient or to mechanical factors. The latter may involve circulatory impairment, most commonly due to clots in the circuit, cannula migration/misplacement, and oxygenator failure.
In the EOLIA international clinical trial, patient-related ECMO complications were pneumothorax, acute kidney failure, cardiac arrest, neurological (e.g., hemorrhagic stroke) and infective (ventilator-associated pneumonia) complications, and bleeding [36]. In patients with COVID-19-related ARDS treated with ECMO, bleeding (42%) and thromboembolic events were quite common, with 19% having pulmonary embolism during ECMO. Nosocomial infections have also been reported frequently [37].
While chest X-ray can reveal complications such as pneumothorax or hemothorax [38], multidetector CT is the preferred modality for the assessment of thoracic complications that cannot be fully evaluated on X-rays, but also of distant complications (such as stroke or arterial/venous thrombus in large vessels). Ultrasonography and Doppler ultrasonography can be used to evaluate complications at insertion sites, including hematomas, pericannular thrombus, or deep vein thrombosis. The main complications that can be encountered in COVID-19 patients on ECMO are summarized in Table 1.
Table 1.
Main potential complications occurring in COVID-19 patients treated with ECMO
| Potential complication sites | Main clinical and radiological findings |
|---|---|
| Chest | Pulmonary embolism |
| Pneumothorax | |
| Pneumomediastinum | |
| Pulmonary opacities | |
| Pulmonary cavitation | |
| Pleural effusion | |
| Brain | Hemorrhage |
| Cerebral edema | |
| Meningoencephalitis | |
| Encephalopathy | |
| Encephalomyelitis | |
| Vascular | Venous thrombosis |
| Bleeding | |
| Vessel wall dissection | |
| Pseudoaneurysm | |
| Limb ischemia | |
| Abdomen | Pancreatitis |
| Mesenteric ischemia | |
| Colitis | |
| Terminal ileitis | |
| Diverticulitis | |
| Acute renal failure |
Pneumothorax and pneumomediastinum
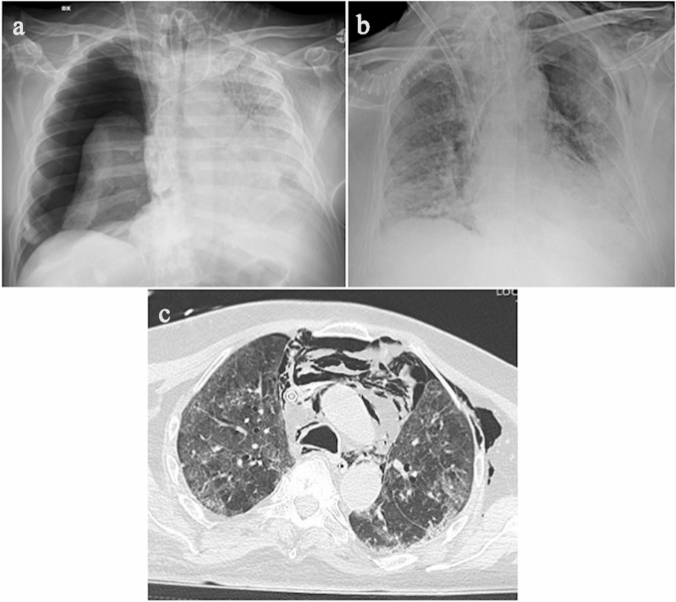
ECMO patients are usually also intubated and treated with high-flow ventilation, so they may be subject to barotrauma. Pneumothorax and pneumomediastinum are frequent complications in COVID-19 patients treated with high-flow ventilation (Fig. 3), as barotrauma may affect up to 15% of them [39]. Less commonly, COVID-19 patients can develop spontaneous pneumothorax and/or pneumomediastinum, as reported by Martinelli et al. in a large multicenter study. Pneumothorax can be diagnosed either incidentally or following marked respiratory deterioration characterized by hypercapnia, acidosis, and increased oxygen demand [40]. A proposed pathophysiological explanation for spontaneous pneumothorax/pneumomediastinum in COVID-19 patients involves diffuse alveolar barrier damage with consequent air leak [41], with air flowing from the pulmonary interstitium toward the pulmonary hilum and mediastinum due to the pressure gradient between the lung periphery and the mediastinal spaces [42].
Fig. 3.
a Chest radiograph showing right pneumothorax. b Chest radiograph and c axial CT image showing pneumomediastinum, left pneumothorax and left subcutaneous emphysema
Infection
In COVID-19 patients, bacterial pneumonia is the most common respiratory complication (Fig. 4) [43]. Aspergillosis has been reported in 10.2% of patients admitted to the intensive care unit [44]. Bacterial infection can be diagnosed as secondary pneumonia or bacteremia during COVID-19 hospitalization and has been reported in about 6–15% of patients in whom bacterial infection had been confirmed [45, 46]. However, it is difficult to differentiate between COVID-19 pneumonia and bacterial pneumonia based on clinical features alone, and only few papers have reported the pathogen species or timing of specimen collection. The most recent guidelines from the UK National Institute for Health and Care Excellence indicate that antibiotics should only be used in COVID-19 cases if there is a clinical suspicion of bacterial infection beyond symptoms of COVID-19 pneumonia (e.g., characteristic symptoms, a neutrophil count outside the normal range, or lobar consolidation on chest imaging) [47]. In patients receiving ECMO treatment, antibiotics can be used to prevent nosocomial infection, although their efficacy remains unclear [48].
Fig. 4.

Axial CT image demonstrating bilateral lung consolidation in a COVID-19 patient with New Delhi Metallo-β-Lactamase (NDM)-producing Klebsiella pneumoniae
In invasively ventilated patients, ventilator-associated pneumonia is a further complication that should be considered. It is defined as a type of pneumonia that occurs 48 to 72 h after intubation in invasively ventilated patients.
Neurological complications
Neurological complications are a broad spectrum, possibly due to viral dissemination in the central nervous system or to an inflammatory response or immune dysregulation [49]. Those associated with radiological findings include acute cerebrovascular disease, meningoencephalitis, encephalopathy, and encephalomyelitis [50, 51].
During ECMO treatment, systemic anticoagulation is required to reduce circuit clotting. Consequently, one of the most common complications is extensive hemorrhage. Hemorrhagic stroke (Fig. 5) is one of the most frequent and severe neurological complications in COVID-19 patients with ECMO [52, 53]. Patients on ECMO are continuously monitored through neurological examinations (e.g., response to verbal directives or pain, brainstem reflexes, eye opening, and pupil examinations), and a head CT scan is warranted when a neurological event occurs [52].
Fig. 5.

Axial CT image showing intraventricular hemorrhage in a COVID-19 patient with ECMO
Hemorrhage
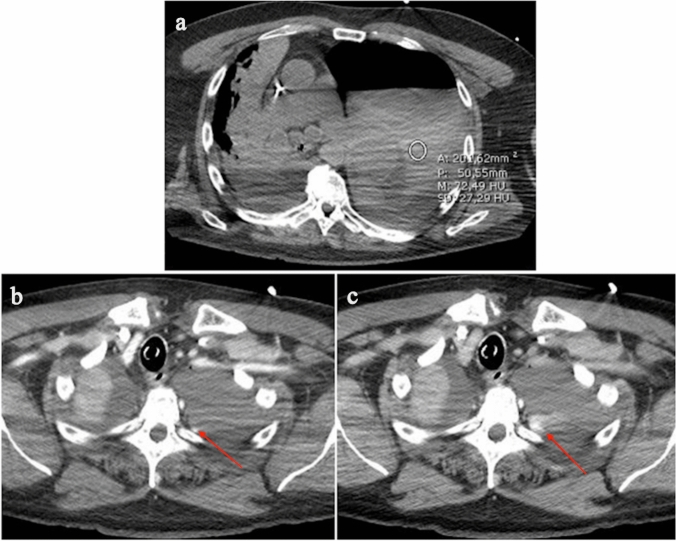
One of the risks related to circulatory components is the presence of clots in the circuit. Hence, anticoagulant therapy is warranted to prevent ECMO circuit from clotting and consequently to minimize the risk of thromboembolic events, such as stroke. Unfortunately, anticoagulation therapy increases the risk of hemorrhage [54]. When heparin is used as an anticoagulant, the hemostatic balance and anticoagulation are usually monitored by assessing activated clotting time (ACT), aPTT, PT, fibrinogen, anti-FXa assay, and platelet count [52, 54]. Several studies have reported intracranial cerebral hemorrhage in patients with COVID-19 [53, 55, 56]. A recent study performed on 1003 COVID-19 patients treated with ECMO has reported a 6% incidence of CNS hemorrhage [14]. The catheter insertion sites, the upper aerodigestive tract (including nose and mouth), the gastrointestinal tract, the genitourinary tract, and the thoracic and abdominal cavities are other relatively common sites of bleeding (Fig. 6). High blood pressure, low carbon dioxide blood levels, gastritis or peptic ulcer, and hematological conditions (e.g., deficiency of coagulation factors including factor XIII, thrombocytopenia, acquired von Willebrand syndrome, and platelet function defects) may cause bleeding [54].
Fig. 6.
a Precontrast chest CT image showing hemopneumothorax in a COVID-19 patient with ECMO, rapidly decreasing hemoglobin level and hypotension. Post-contrast CT images in the b arterial (arrow) and c venous phase show active bleeding (arrow)
The pathogenesis of spontaneous bleeding in patients with COVID-19 is unclear. Two possible explanations include increased serum proinflammatory cytokines and endothelial cell damage [57]. Prophylactic antithrombotic treatment is a risk factor [58].
Vascular complications
Ischemia of one or more limbs is the most common vascular complication in patients with VA-ECMO, with a reported prevalence ranging from 10 to 70%. The risk of ischemia is greater with larger cannulas (> 20Fr), in women, young patients, and in the presence of peripheral arterial disease. Possible clinical scenarios include pain, pallor, poikilothermia, motor or sensory deficit, and gangrene. Infection of the catheter insertion site, retroperitoneal bleeding, vessel wall dissection, and pseudoaneurysm formation are other common vascular complications (Fig. 7). Cellulitis, drainage around the cannula, and tissue induration can be indicators of superficial infection, whereas fever, hypotension, increased white cell count, and bacteremia are signs of systemic sepsis. Pseudoaneurysm usually presents with a painful pulsatile swelling at the access site, whereas arterial dissection is often asymptomatic (unless hemodynamically significant) [59]. In 2016, Tanaka et al. reported a 18% and 49% rate of survival to hospital discharge in patients receiving VA-ECMO with and without vascular complications, respectively [60].
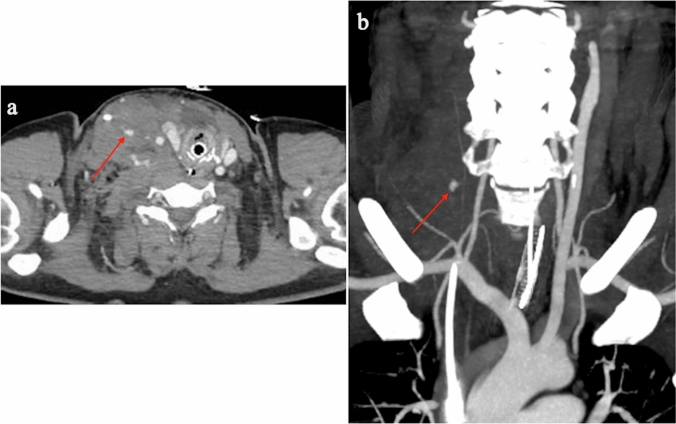
Fig. 7.
Contrast-enhanced CT showing active bleeding fed from branches of the right superior thyroid artery [a, axial image (arrow), b, maximum intensity projection (MIP) view (arrow)]
Venous thrombosis and pulmonary embolism
COVID-19 is associated with an inflammatory state and coagulopathy, implying higher rates of venous (Fig. 8a, b) and arterial thrombosis and overall increased mortality [61–66]. A recent retrospective analysis performed on COVID-19 patients treated with ECMO has reported a 19% incidence of pulmonary embolism (Fig. 8c) [15]. On the other hand, none of the patients from the EOLIA trial developed pulmonary embolism. As a result, pulmonary embolism is probably a complication of COVID-19 disease rather than of ECMO [37]. Clinical parameters (e.g., worsening PaO2/FiO2 despite nitric oxide inhalation or after prone positioning, hemodynamic deterioration requiring fluid challenge and/or increased norepinephrine infusion rate, or dilated right ventricle without acute cor pulmonale), laboratory data (including significant or rapid elevation of D-dimer values despite anticoagulation), or both are indications for venous thromboembolism detection [62].
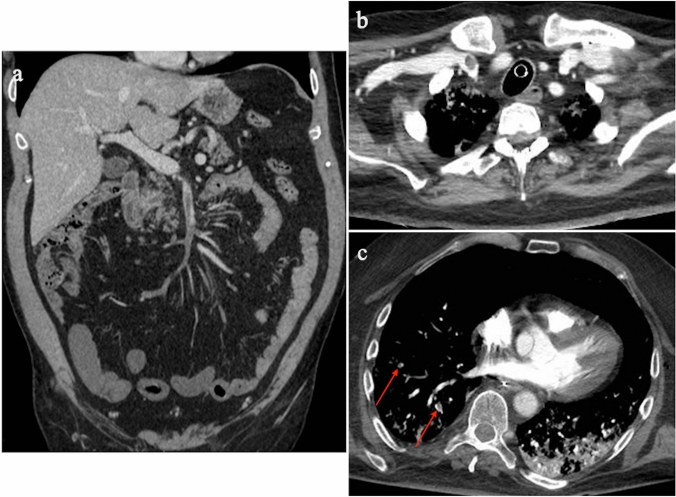
Fig. 8.
Thromboembolic complications detected incidentally on CT examinations of COVID-19 patients treated with VV-ECMO. a Coronal reformatted CT image of a patient with VV-ECMO and thrombosis of the superior mesenteric vein extending to several jejuno-ileal branches. b Axial CT image of a patient with thrombosis of the right internal jugular vein, in whom VV-ECMO had been removed two days earlier. c CT pulmonary angiography examination showing pulmonary embolism (arrows) at the posterior and anterior segments of the right lower lobe
Other COVID-19-related complications
Gastrointestinal involvement is a very common extrathoracic manifestation of COVID-19, probably as a consequence of SARS-CoV-2 cytotoxicity mediated by viral binding to angiotensin converting enzyme 2 (ACE-2) receptors expressed in the gastrointestinal tract [67, 68]. Transaminitis, severe ileus, and mesenteric ischemia are the most common gastrointestinal complications [69], with diarrhea, nausea, vomiting, and abdominal pain being the most frequent gastrointestinal symptoms [70]. Colitis and terminal ileitis have also been reported as complications in patients treated in intensive care units with vasopressors and ECMO as supportive therapies [71]. COVID-19-associated diverticulitis (Fig. 9a) has also been described [72].
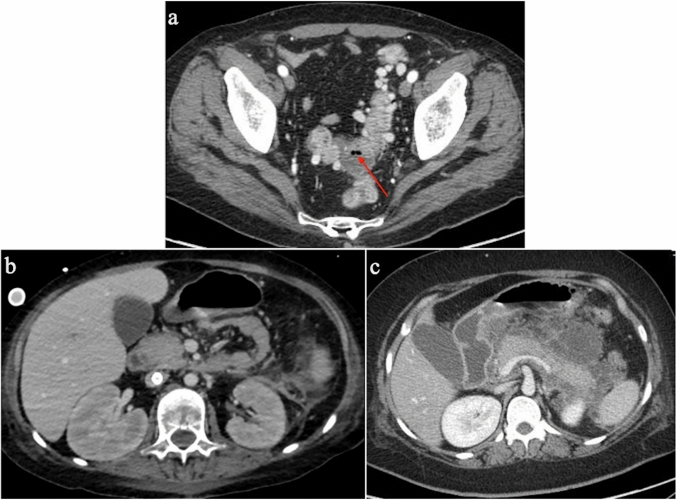
Fig. 9.
Potential abdominal complications of COVID-19 in patients treated with VV-ECMO. a Axial CT image shows diverticulitis complicated by a peridiverticular abscess with covered bowel perforation (arrow). b Axial CT image obtained in a patient with multiple organ failure and suspected abdominal bleeding. Notice initial swelling of both kidneys with loss of cortico-medullary differentiation. c Axial CT image obtained in a patient with peripancreatic fluid collections from acute pancreatitis
The presence of ACE2 receptors on kidney podocytes and proximal convoluted tubule cells could also explain the role of SARS-CoV-2 infection in the pathophysiology of acute renal failure [67]. Acute kidney injury (Fig. 9b) is one of the most common renal complications and is burdened by an increased risk of mortality ([43]).
Wang et al. [73] found a 17% incidence of pancreatic injury in patients with COVID-19 pneumonia. Pancreatitis can be diagnosed with a blood test and confirmed by clinical and radiological assessment (Fig. 9c). Unfortunately, its underlying pathophysiology is currently unknown [74].
Conclusion
COVID-19 is a potentially life-threatening systemic disease that may require ECMO as a salvage therapy in patients who develop acute respiratory distress syndrome. Radiologists should have a comprehensive knowledge of ECMO devices and of the potential complications that may be encountered in COVID-19 patients treated with ECMO, which is essential for their proper management.
Authors contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by VM, ZF, and NB. The first draft of the manuscript was written by MG, VM, and LF, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Open access funding provided by Università di Pisa within the CRUI-CARE Agreement.
Declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethics approval
No ethical approval was required due to the nature of the manuscript (review article).
Footnotes
Michela Gabelloni and Lorenzo Faggioni: Co-first authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wong RSY. The SARS-CoV-2 outbreak: an epidemiological and clinical perspective. SN Compr Clin Med. 2020;2:1983–1991. doi: 10.1007/s42399-020-00546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coppola F, Faggioni L, Neri E, et al. Impact of the COVID-19 outbreak on the profession and psychological wellbeing of radiologists: a nationwide online survey. Insights Imaging. 2021;12:23. doi: 10.1186/s13244-021-00962-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020;24:516. doi: 10.1186/s13054-020-03240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gaia C, Maria Chiara C, Silvia L, et al. Chest CT for early detection and management of coronavirus disease (COVID-19): a report of 314 patients admitted to emergency department with suspected pneumonia. Radiol Med. 2020;125:931–942. doi: 10.1007/s11547-020-01256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carotti M, Salaffi F, Sarzi-Puttini P, et al. Chest CT features of coronavirus disease 2019 (COVID-19) pneumonia: key points for radiologists. Radiol Med. 2020;125:636–646. doi: 10.1007/s11547-020-01237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salvatore C, Roberta F, de Angela L, et al. Clinical and laboratory data, radiological structured report findings and quantitative evaluation of lung involvement on baseline chest CT in COVID-19 patients to predict prognosis. Radiol Med. 2021;126:29–39. doi: 10.1007/s11547-020-01293-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caruso D, Polici M, Zerunian M, et al. Quantitative chest CT analysis in discriminating COVID-19 from non-COVID-19 patients. Radiol Med. 2021;126:243–249. doi: 10.1007/s11547-020-01291-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Palmisano A, Scotti GM, Ippolito D, et al. Chest CT in the emergency department for suspected COVID-19 pneumonia. Radiol Med. 2021;126:498–502. doi: 10.1007/s11547-020-01302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caruso D, Guido G, Zerunian M, et al. Post-acute sequelae of COVID-19 pneumonia: six-month chest CT follow-up. Radiology. 2021;301:E396–E405. doi: 10.1148/radiol.2021210834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caruso D, Polidori T, Guido G, et al. Typical and atypical COVID-19 computed tomography findings. World J Clin Cases. 2020;8:3177–3187. doi: 10.12998/wjcc.v8.i15.3177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Booz C, Vogl TJ, Joseph Schoepf U, et al. Value of minimum intensity projections for chest CT in COVID-19 patients. Eur J Radiol. 2021;135:109478. doi: 10.1016/j.ejrad.2020.109478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khodeli N, Chkhaidze Z, Partsakhashvili J, et al. Practical and theoretical considerations for ECMO system development extracorporeal membrane oxygenation. Adv Ther. 2016 doi: 10.5772/64267. [DOI] [Google Scholar]
- 14.Barbaro RP, MacLaren G, Boonstra PS, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. 2020;396:1071–1078. doi: 10.1016/S0140-6736(20)32008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt M, Hajage D, Lebreton G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8:1121–1131. doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Combes A, Peek GJ, Hajage D, et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46:2048–2057. doi: 10.1007/s00134-020-06248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramanathan K, Shekar K, Ling RR, et al. Extracorporeal membrane oxygenation for COVID-19: a systematic review and meta-analysis. Crit Care. 2021;25:211. doi: 10.1186/s13054-021-03634-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Douraghi-Zadeh D, Logaraj A, Lazoura O, et al. Extracorporeal membrane oxygenation (ECMO): Radiographic appearances, complications and imaging artefacts for radiologists. J Med Imaging Radiat Oncol. 2021 doi: 10.1111/1754-9485.13280. [DOI] [PubMed] [Google Scholar]
- 19.Lee S, Chaturvedi A. Imaging adults on extracorporeal membrane oxygenation (ECMO) Insights Imaging. 2014;5:731–742. doi: 10.1007/s13244-014-0357-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnacle AM, Smith LC, Hiorns MP. The role of imaging during extracorporeal membrane oxygenation in pediatric respiratory failure. AJR Am J Roentgenol. 2006;186:58–66. doi: 10.2214/AJR.04.1672. [DOI] [PubMed] [Google Scholar]
- 21.Hosmane SR, Barrow T, Ashworth A, Smith E. Extracorporeal membrane oxygenation: a radiologists’ guide to who, what and where. Clin Radiol. 2015;70:e58–66. doi: 10.1016/j.crad.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 22.de Chaves RCF, Rabello Filho R, Timenetsky KT, et al. Extracorporeal membrane oxygenation: a literature review. Rev Bras Ter Intensiva. 2019;31:410–424. doi: 10.5935/0103-507X.20190063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reeb J, Olland A, Renaud S, et al. Principi e indicazioni dell’assistenza circolatoria e respiratoria extracorporea in chirurgia toracica. EMC Tec Chir Chir Gener. 2017;17:1–18. doi: 10.1016/s1636-5577(17)82113-1. [DOI] [Google Scholar]
- 24.Badulak J, Antonini MV, Stead CM, et al. Extracorporeal membrane oxygenation for COVID-19: updated 2021 guidelines from the extracorporeal life support organization. ASAIO J. 2021;67:485–495. doi: 10.1097/MAT.0000000000001422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel AR, Patel AR, Singh S, et al. Venovenous extracorporeal membrane oxygenation therapy in adults. Cureus. 2019 doi: 10.7759/cureus.5365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shekar K, Badulak J, Peek G, et al. Extracorporeal life support organization Coronavirus Disease 2019 interim guidelines: a consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers. ASAIO J. 2020;66:707–721. doi: 10.1097/MAT.0000000000001193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banfi C, Pozzi M, Siegenthaler N, et al. Veno-venous extracorporeal membrane oxygenation: cannulation techniques. J Thorac Dis. 2016;8:3762–3773. doi: 10.21037/jtd.2016.12.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vezzani A, Brusasco C, Palermo S, et al. Ultrasound localization of central vein catheter and detection of postprocedural pneumothorax: an alternative to chest radiography. Crit Care Med. 2010;38:533–538. doi: 10.1097/CCM.0b013e3181c0328f. [DOI] [PubMed] [Google Scholar]
- 29.Vezzani A, Manca T, Brusasco C, et al. Diagnostic value of chest ultrasound after cardiac surgery: a comparison with chest X-ray and auscultation. J Cardiothorac Vasc Anesth. 2014;28:1527–1532. doi: 10.1053/j.jvca.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 30.Di Serafino M, Notaro M, Rea G, et al. The lung ultrasound: facts or artifacts? In the era of COVID-19 outbreak. Radiol Med. 2020;125:738–753. doi: 10.1007/s11547-020-01236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Møller-Sørensen H, Gjedsted J, Jørgensen VL, Hansen KL. COVID-19 assessment with bedside lung ultrasound in a population of intensive care patients treated with mechanical ventilation and ECMO. Diagnostics. 2020;10:447. doi: 10.3390/diagnostics10070447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest. 2020;158:106–116. doi: 10.1016/j.chest.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oba Y, Zaza T. Abandoning daily routine chest radiography in the intensive care unit: meta-analysis. Radiology. 2010;255:386–395. doi: 10.1148/radiol.10090946. [DOI] [PubMed] [Google Scholar]
- 34.Hejblum G, Chalumeau-Lemoine L, Ioos V, et al. Comparison of routine and on-demand prescription of chest radiographs in mechanically ventilated adults: a multicentre, cluster-randomised, two-period crossover study. Lancet. 2009;374:1687–1693. doi: 10.1016/s0140-6736(09)61459-8. [DOI] [PubMed] [Google Scholar]
- 35.Expert Panel on Thoracic Imaging. Laroia AT, Donnelly EF, et al. ACR appropriateness criteria® intensive care unit patients. J Am Coll Radiol. 2021;18:S62–S72. doi: 10.1016/j.jacr.2021.01.017. [DOI] [PubMed] [Google Scholar]
- 36.Combes A, Hajage D, Capellier G, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 37.MacLaren G, Combes A, Brodie D. What’s new in ECMO for COVID-19? Intensive Care Med. 2021;47:107–109. doi: 10.1007/s00134-020-06284-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moroni C, Cozzi D, Albanesi M, et al. Chest X-ray in the emergency department during COVID-19 pandemic descending phase in Italy: correlation with patients’ outcome. Radiol Med. 2021;126:661–668. doi: 10.1007/s11547-020-01327-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGuinness G, Zhan C, Rosenberg N, et al. Increased incidence of barotrauma in patients with COVID-19 on invasive mechanical ventilation. Radiology. 2020;297:E252–E262. doi: 10.1148/radiol.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martinelli AW, Ingle T, Newman J, et al. COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J. 2020 doi: 10.1183/13993003.02697-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elhakim TS, Abdul HS, Pelaez Romero C, Rodriguez-Fuentes Y. Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19 pneumonia: a rare case and literature review. BMJ Case Rep. 2020 doi: 10.1136/bcr-2020-239489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Damous SHB, dos Santos Junior JP, Pezzano ÁVA, et al. Pneumomediastinum complicating COVID-19: a case series. Eur J Med Res. 2021;26:1–6. doi: 10.1186/s40001-021-00585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Drake TM, Riad AM, Fairfield CJ, et al. Characterisation of in-hospital complications associated with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol UK: a prospective, multicentre cohort study. Lancet. 2021;398:223–237. doi: 10.1016/S0140-6736(21)00799-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mitaka H, Kuno T, Takagi H, Patrawalla P. Incidence and mortality of COVID-19-associated pulmonary aspergillosis: A systematic review and meta-analysis. Mycoses. 2021;64:993–1001. doi: 10.1111/myc.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Farrell JM, Zhao CY, Tarquinio KM, Brown SP. Causes and consequences of COVID-19-associated bacterial infections. Front Microbiol. 2021 doi: 10.3389/fmicb.2021.682571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71:2459–2468. doi: 10.1093/cid/ciaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.COVID-19 rapid guideline: antibiotics for pneumonia in adults in hospital (2021) National Institute for Health and Care Excellence (NICE), London [PubMed]
- 48.Kondo Y, Ohbe H, Aso S, et al. Efficacy of prophylactic antibiotics during extracorporeal membrane oxygenation: a nationwide cohort study. Ann Am Thorac Soc. 2021;18:1861–1867. doi: 10.1513/AnnalsATS.202008-974OC. [DOI] [PubMed] [Google Scholar]
- 49.Favas TT, Dev P, Chaurasia RN, et al. Neurological manifestations of COVID-19: a systematic review and meta-analysis of proportions. Neurol Sci. 2020;41:3437–3470. doi: 10.1007/s10072-020-04801-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guerrero JI, Barragán LA, Martínez JD, et al. Central and peripheral nervous system involvement by COVID-19: a systematic review of the pathophysiology, clinical manifestations, neuropathology, neuroimaging, electrophysiology, and cerebrospinal fluid findings. BMC Infect Dis. 2021;21:515. doi: 10.1186/s12879-021-06185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lombardi AF, Afsahi AM, Gupta A, Gholamrezanezhad A. Severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), influenza, and COVID-19, beyond the lungs: a review article. Radiol Med. 2021;126:561–569. doi: 10.1007/s11547-020-01311-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fletcher-Sandersjöö A, Thelin EP, Bartek J, Jr, et al. Management of intracranial hemorrhage in adult patients on extracorporeal membrane oxygenation (ECMO): An observational cohort study. PLoS ONE. 2017;12:e0190365. doi: 10.1371/journal.pone.0190365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heman-Ackah SM, Su YS, Spadola M, et al. Neurologically devastating intraparenchymal hemorrhage in COVID-19 patients on extracorporeal membrane oxygenation: a case series. Neurosurgery. 2020;87:E147–E151. doi: 10.1093/neuros/nyaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thomas J, Kostousov V, Teruya J. Bleeding and thrombotic complications in the use of extracorporeal membrane oxygenation. Semin Thromb Hemost. 2017;44:020–029. doi: 10.1055/s-0037-1606179. [DOI] [PubMed] [Google Scholar]
- 55.Cheruiyot I, Sehmi P, Ominde B, et al. Intracranial hemorrhage in coronavirus disease 2019 (COVID-19) patients. Neurol Sci. 2021;42:25–33. doi: 10.1007/s10072-020-04870-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Masur J, Freeman CW, Mohan S. A double-edged sword: neurologic complications and mortality in extracorporeal membrane oxygenation therapy for COVID-19-related severe acute respiratory distress syndrome at a tertiary care center. AJNR Am J Neuroradiol. 2020;41:2009–2011. doi: 10.3174/ajnr.A6728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ciceri F, Beretta L, Scandroglio AM, et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc. 2020;22:95–97. doi: 10.51893/2020.2.pov2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Palumbo D, Guazzarotti G, De Cobelli F. Spontaneous major hemorrhage in COVID-19 patients: another brick in the wall of SARS-CoV-2-associated coagulation disorders? J Vasc Interv Radiol. 2020;31:1494–1496. doi: 10.1016/j.jvir.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pillai AK, Bhatti Z, Bosserman AJ, et al. Management of vascular complications of extra-corporeal membrane oxygenation. Cardiovasc Diagn Ther. 2018;8:372–377. doi: 10.21037/cdt.2018.01.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tanaka D, Hirose H, Cavarocchi N, Entwistle JWC. The impact of vascular complications on survival of patients on venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg. 2016;101:1729–1734. doi: 10.1016/j.athoracsur.2015.10.095. [DOI] [PubMed] [Google Scholar]
- 61.Malas MB, Naazie IN, Elsayed N, et al. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: A systematic review and meta-analysis. EClinicalMedicine. 2020;29:100639. doi: 10.1016/j.eclinm.2020.100639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chi G, Lee JJ, Jamil A, et al. Venous thromboembolism among hospitalized patients with COVID-19 undergoing thromboprophylaxis: a systematic review and meta-analysis. J Clin Med Res. 2020 doi: 10.3390/jcm9082489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ippolito D, Giandola T, Maino C, et al. Acute pulmonary embolism in hospitalized patients with SARS-CoV-2-related pneumonia: multicentric experience from Italian endemic area. Radiol Med. 2021;126:669–678. doi: 10.1007/s11547-020-01328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Masselli G, Almberger M, Tortora A, et al. Role of CT angiography in detecting acute pulmonary embolism associated with COVID-19 pneumonia. Radiol Med. 2021 doi: 10.1007/s11547-021-01415-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ierardi AM, Gaibazzi N, Tuttolomondo D, et al. Deep vein thrombosis in COVID-19 patients in general wards: prevalence and association with clinical and laboratory variables. Radiol Med. 2021;126:722–728. doi: 10.1007/s11547-020-01312-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Caruso D, Zerunian M, Pucciarelli F, et al. Imaging of abdominal complications of COVID-19 infection. BJR Open. 2021;2:20200052. doi: 10.1259/bjro.20200052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vaidya T, Nanivadekar A, Patel R. Imaging spectrum of abdominal manifestations of COVID-19. World J Radiol. 2021;13:157–170. doi: 10.4329/wjr.v13.i6.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moheb ME, El Moheb M, Naar L, et al. Gastrointestinal complications in critically ill patients with and without COVID-19. JAMA. 2020;324:1899. doi: 10.1001/jama.2020.19400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keshavarz P, Rafiee F, Kavandi H, et al. Ischemic gastrointestinal complications of COVID-19: a systematic review on imaging presentation. Clin Imaging. 2021;73:86–95. doi: 10.1016/j.clinimag.2020.11.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Martin S, Pierce J, Kikano EG, et al. Considerations in imaging interpretations for colitis in critically ill patients during the COVID-19 era. Emerg Radiol. 2021;28:699–704. doi: 10.1007/s10140-021-01925-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Weissman S, Belyayeva A, Sharma S, et al. SARS-CoV-2 and acute diverticulitis: the expanding gastrointestinal manifestations of COVID-19 infection. J Transl Int Med. 2021;9:59–60. doi: 10.2478/jtim-2021-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang F, Wang H, Fan J, et al. Pancreatic injury patterns in patients with Coronavirus Disease 19 pneumonia. Gastroenterology. 2020;159:367–370. doi: 10.1053/j.gastro.2020.03.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kurihara Y, Maruhashi T, Wada T, et al. Pancreatitis in a patient with severe Coronavirus Disease pneumonia treated with veno-venous extracorporeal membrane oxygenation. Intern Med. 2020;59:2903–2906. doi: 10.2169/internalmedicine.5912-20. [DOI] [PMC free article] [PubMed] [Google Scholar]