Abstract
Background
Iron and folic acid supplementation has been the preferred intervention to improve iron stores and prevent anaemia among pregnant women, and it is thought to improve other maternal and birth outcomes.
Objectives
To assess the effects of daily oral iron supplements for pregnant women, either alone or in conjunction with folic acid, or with other vitamins and minerals as a public health intervention in antenatal care.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (10 January 2015). We also searched the WHO International Clinical Trials Registry Platform (ICTRP) (26 February 2015) and contacted relevant organisations for the identification of ongoing and unpublished studies (26 February 2015) .
Selection criteria
Randomised or quasi‐randomised trials evaluating the effects of oral preventive supplementation with daily iron, iron + folic acid or iron + other vitamins and minerals during pregnancy.
Data collection and analysis
We assessed the methodological quality of trials using standard Cochrane criteria. Two review authors independently assessed trial eligibility, extracted data and conducted checks for accuracy. We used the GRADE approach to assess the quality of the evidence for primary outcomes.
We anticipated high heterogeneity among trials and we pooled trial results using a random‐effects model and were cautious in our interpretation of the pooled results: the random‐effects model gives the average treatment effect.
Main results
We included 61 trials. Forty‐four trials, involving 43,274 women, contributed data and compared the effects of daily oral supplements containing iron versus no iron or placebo.
Preventive iron supplementation reduced maternal anaemia at term by 70% (risk ratio (RR) 0.30; 95% confidence interval (CI) 0.19 to 0.46, 14 trials, 2199 women, low quality evidence), iron‐deficiency anaemia at term (RR 0.33; 95% CI 0.16 to 0.69, six trials, 1088 women), and iron deficiency at term by 57% (RR 0.43; 95% CI 0.27 to 0.66, seven trials, 1256 women, low quality evidence). There were no clear differences between groups for severe anaemia in the second or third trimester, or maternal infection during pregnancy (RR 0.22; 95% CI 0.01 to 3.20, nine trials, 2125 women, very low quality evidence; and, RR 1.21; 95% CI 0.33 to 4.46; one trial, 727 women, low quality evidence, respectively), or maternal mortality (RR 0.33; 95% CI 0.01 to 8.19, two trials, 12,560 women, very low quality evidence), or reporting of side effects (RR 1.29; 95% CI 0.83 to 2.02, 11 trials, 2423 women, very low quality evidence). Women receiving iron were on average more likely to have higher haemoglobin (Hb) concentrations at term and in the postpartum period, but were at increased risk of Hb concentrations greater than 130 g/L during pregnancy, and at term.
Compared with controls, women taking iron supplements less frequently had low birthweight newborns (8.4% versus 10.3%, average RR 0.84; 95% CI 0.69 to 1.03, 11 trials, 17,613 women, low quality evidence), and preterm babies (RR 0.93; 95% CI 0.84 to 1.03, 13 trials, 19,286 women, moderate quality evidence). They appeared to also deliver slightly heavier babies (mean difference (MD) 23.75; 95% CI ‐3.02 to 50.51, 15 trials, 18,590 women, moderate quality evidence). None of these results were statistically significant. There were no clear differences between groups for neonatal death (RR 0.91; 95% CI 0.71 to 1.18, four trials, 16,603 infants, low quality evidence), or congenital anomalies (RR 0.88, 95% CI 0.58 to 1.33, four trials, 14,636 infants, low quality evidence).
Twenty‐three studies were conducted in countries that in 2011 had some malaria risk in parts of the country. In some of these countries/territories, malaria is present only in certain areas or up to a particular altitude. Only two of these studies reported malaria outcomes. There is no evidence that iron supplementation increases placental malaria. For some outcomes heterogeneity was higher than 50%.
Authors' conclusions
Supplementation reduces the risk of maternal anaemia and iron deficiency in pregnancy but the positive effect on other maternal and infant outcomes is less clear. Implementation of iron supplementation recommendations may produce heterogeneous results depending on the populations' background risk for low birthweight and anaemia, as well as the level of adherence to the intervention.
Plain language summary
Effects and safety of preventive oral iron or iron + folic acid supplementation for women during pregnancy
During pregnancy, women need iron and folate to meet both their own needs and those of the developing baby. The concern is that if pregnant women become deficient in these nutrients they are unable to supply them in sufficient quantities to their baby. Low folate nutrition before conceiving increases the risk of the baby having neural tube defects. Low iron and folate levels in women can cause anaemia, which can make women tired, faint, and at increased risk of infection.
We included 61 randomised trials in the review with 44 trials involving 43,274 pregnant women contributing to the analyses. The use of iron or iron and folic acid supplements was associated with a reduced risk of anaemia and iron deficiency during pregnancy. There was some indication that maternal iron supplements during pregnancy could improve outcomes for babies (birthweight and preterm birth) but the evidence for this was not of high quality.There is no evidence that iron supplementation increases placental malaria.
Summary of findings
Background
Description of the condition
Iron deficiency is thought to be the most common nutrient deficiency among pregnant women (WHO 1992). Iron deficiency involves an insufficient supply of iron to the cells following depletion of the body's reserves. Its main causes are a diet poor in absorbable iron, an increased requirement for iron (e.g. during pregnancy) not covered through the diet, a loss of iron due to parasitic infections, particularly hookworm, and other blood losses (Crompton 2002; INACG 2002a). Chronic iron deficiency frequently turns into iron‐deficiency anaemia. While iron deficiency is the most common cause of anaemia, other causes such as acute and chronic infections that cause inflammation; deficiencies of folate and of vitamins B2, B12, A, and C; and genetically inherited traits such as thalassaemia and drepanocytosis (sickle‐cell anaemia) may be independent or superimposed causal factors (WHO 2001; WHO 2015a). The global prevalence of anaemia among pregnant women was estimated to be 38.2% in 2011 (WHO 2015b).
Diagnosis of iron‐deficiency and anaemia during pregnancy
Anaemia during pregnancy is diagnosed if a woman's haemoglobin (Hb) concentration is lower than 110 g/L at sea level, although it is recognised that during the second trimester Hb concentrations naturally decrease by approximately 5 g/L (WHO 2011a). Although Hb and, less frequently, hematocrit tests are used to screen for iron deficiency, low Hb or hematocrit values are not specific to iron deficiency.
Iron deficiency in non‐pregnant populations can be measured quite precisely using laboratory tests such as serum ferritin, serum iron, transferrin, transferrin saturation and transferrin receptors. However, these tests are often not readily available and their results may be of limited value in some settings where different infections (e.g. malaria, HIV/AIDS, vaginosis) are highly prevalent (Nel 2015). Furthermore, the results of those tests do not correlate closely with one another because each reflects a different aspect of iron metabolism. For example, serum ferritin concentration is an indicator of iron reserves. During pregnancy, however, serum ferritin levels as well as levels of bone marrow iron fall even in women who ingest daily supplements with high amounts of iron, which casts doubts about their true significance in pregnancy and suggests the need to review cut‐off values (Puolakka 1980; Romslo 1983; Svanberg 1975). Currently, a serum ferritin concentration of less than 15 µg/L in healthy adults is an accepted cut‐off of depleted iron stores, even among pregnant women (WHO 2011b), although the review of cut‐off points is recognised as a research need (Garcia‐Casal 2014). Interestingly, the nadir of maternal serum ferritin occurs by week 28, before higher iron demands are believed to occur, a decrease only partially explained by the normal plasma volume expansion that occurs during pregnancy (Taylor 1982).
The ratio of serum transferrin receptors to serum ferritin has been suggested as a good indicator of iron nutrition among pregnant and non‐pregnant women (Cook 2003). Data from the United States National Health and Nutrition Examination Survey (NHANES) in 1999 to 2006 for 1171 pregnant women using this composed indicator showed that pregnant women in the first trimester had the highest mean total body iron compared with that of pregnant women in the second or third trimesters, and that the prevalence of iron deficiency in pregnant women increased with trimester (Mei 2011). However, the lack of a standard soluble transferrin receptor (sTfR) assay method and a standard reference material, limit the use and comparability of this indicator with other studies (WHO 2014a). There is still a need to improve the definition of the distribution of serum transferrin receptors during pregnancy in populations with different iron status (Nair 2004) in various environments (Milman 2007).
After considering various indicators, a World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) technical consultation concluded that Hb and ferritin were the most efficient combination of indicators for monitoring change in the iron status of a population as a consequence of iron supplementation (WHO/CDC 2005). Unfortunately, only two of the very varied studies on pregnant women were included, and only one of them demonstrated changes with iron supplementation. The use of multiple indicators (Hb, ferritin and sTfRs) is useful for population‐based assessments of iron‐deficiency anaemia, when this is feasible.
Low and high Hb concentrations, iron status and pregnancy outcomes
The consequences of iron‐deficiency anaemia are serious, and can include diminished intellectual and productive capacity (Hunt 2002), and possibly increased susceptibility to infections (Oppenheimer 2001). The lowest rates of low birthweight and premature birth appear to occur when maternal Hb levels are between 95 and 105 g/L during the second trimester of gestation (Murphy 1986; Steer 2000), and between 95 and 125 g of Hb/L at term (Hytten 1964; Hytten 1971). However, the results of several studies suggest that near‐term Hb levels below 95 g/L or even below 110 g/L may be associated with low birthweight, heavier placentas and increased frequency of premature births (Garn 1981; Godfrey 1991; Kim 1992; Klebanoff 1989; Klebanoff 1991; Murphy 1986). There is evidence that maternal Hb levels below 95 g/L before or during the second trimester of gestation are associated with increased risk of giving birth to a low birthweight infant and with premature delivery (Burke 2014). During pregnancy, low Hb levels, indicative of moderate (between 70 and 90 g/L) or severe (less than 70 g/L) anaemia, are associated with increased risk of maternal and child mortality and infectious diseases (INACG 2002b). Favourable pregnancy outcomes occur 30% to 45% less often in anaemic mothers, and it has been estimated that their infants have less than one‐half of normal iron reserves (Bothwell 1981).
Unfortunately, the time between birth and umbilical cord clamping has not been considered in the estimates of impact of maternal iron status and anaemia on the infant's iron reserves, even though late umbilical cord clamping (between one and three minutes) has been shown to improve them significantly (McDonald 2013; Rabe 2012), and is recommended to prevent maternal postpartum haemorrhage (WHO 2012b) and other outcomes (WHO 2014b). Iron deficiency may adversely affect the cognitive performance, development and physical growth of infants (WHO 2001; Black 2011) even in the long term (Lozoff 2006). Moderate or severe iron deficiency during infancy has been shown to have irreversible cognitive effects (Gleason 2007). A recent review concluded that correcting iron deficiency could have a beneficial impact in women's physical performance (Pasricha 2014). Studies in animal models suggest that suffering anaemia during the intrauterine period can lead to long‐term chronic diseases such as hypertension, as part of a phenomenon known as fetal programming (Andersen 2006).
Haemoglobin levels greater than 130 g/L at sea level have also been associated with negative pregnancy outcomes (Hytten 1964; Hytten 1971; Murphy 1986; Scholl 1997; Steer 2000). Large epidemiologic retrospective studies (Murphy 1986; Steer 2000; Xiong 2000), and one prospective study in China (Zhou 1998), have shown that both low and high prenatal Hb concentrations are associated with increased risks for premature delivery and low birthweight. In fact, the incidence of these negative consequences increases dramatically when women's Hb levels, at sea level, are below 95 to 105 g/L at any time in pregnancy or above 130 to 135 g/L after mid‐pregnancy. A randomised clinical trial in Mexico showed associations between prenatal daily iron supplement intake at recommended doses to be associated with high Hb concentrations and the risk for both low birthweight and premature delivery (Casanueva 2003a). A study (Ziaei 2007) also showed that women whose Hb concentration at gestational weeks 32 to 36 was greater than 132 g/L had more low birthweight babies and also higher blood pressure than women with lower Hb concentrations. Unfortunately, any women considered anaemic were excluded from the study. Observational studies have shown that among iron supplemented pregnant women, and particularly among those who are anaemic early in pregnancy, a failure of Hb and/or ferritin levels to decline during the second and third trimesters, and overall high ferritin levels during pregnancy, not due to infection, are associated with adverse pregnancy outcomes. However, when some confounding factors are controlled for, the association between high serum ferritin concentrations and the risk for premature delivery was not significant (Scholl 1998; Scholl 2000; Scholl 2005).
The association between iron deficiency without anaemia and adverse perinatal outcomes is less clear, although some studies have shown iron deficiency to be associated with inadequate pregnancy weight gain, decreased defence against infections, preterm delivery and low birthweight (Garn 1981; Kandoi 1991; Prema 1982; Scholl 1992).
Description of the intervention
The Institute of Medicine recommends that women consume 27 mg/day of iron during pregnancy (IOM 2001). Most women need additional iron as well as sufficient iron stores to prevent iron deficiency (Bothwell 2000), and so direct iron supplementation for pregnant women has been used extensively in most low‐ and middle‐income countries as an intervention to prevent and correct iron deficiency and anaemia during pregnancy. It has been recommended that iron supplements also contain folic acid, an essential B‐vitamin, because of the increased requirements of pregnancy, due to the rapidly dividing cells in the fetus and elevated urinary losses. Other vitamins and minerals for which deficiencies are documented, and when requirements during pregnancy are higher, this may justify their addition to the supplementation formula, although this is an ongoing area of controversy, particularly with differing conclusions on maternal and infant benefits from various reviews (Bhutta 2008; Christian 2010; Haider 2012; Shrimptom 2009).
International organisations have been advocating routine iron and folic acid supplementation for every pregnant woman in areas where anaemia is highly prevalent (Beard 2000; Villar 1997). While iron supplementation, with or without folic acid has been used in a variety of doses and regimens, some current recommendations for all pregnant adolescents and adult women include the provision of a standard daily dose of 30 to 60 mg of elemental iron and 400 μg (0.4 mg) of folic acid starting as soon as possible after gestation begins and continuing for the rest of the pregnancy (WHO 2012a). In settings where anaemia in pregnant women is a severe public health problem (40% of higher), a daily dose of 60 mg of elemental iron is preferred over a lower dose. Additionally, if iron deficiency prevalence in the country is high, (INACG 1998), or if a woman is diagnosed with anaemia in a clinical setting, she should be treated with daily iron (120 mg of elemental iron) and folic acid (400 μg or 0.4 mg) supplementation until her Hb concentration rises to normal (WHO 2012a). Recent data from national surveys from 46 countries during the years 2003 to 2009 estimated that 52% to 75% of mothers had received iron tablets during pregnancy, and that the duration of supplementation was usually short (Lutter 2011).
A dose of 60 mg of elemental iron was first established in 1959 and was based on estimated iron requirements for women during pregnancy (WHO 1959). This same dose was endorsed by subsequent expert consultations (INACG 1998; WHO 1968; WHO 2001). The use of folic acid during pregnancy was first suggested in 1967, during a technical consultation in Geneva, Switzerland. It was considered that a dose of 300 μg (0.3 mg) of folic acid per day throughout pregnancy would help prevent megaloblastic anaemia, which is associated with folate deficiency (WHO 2015a). This consultation was called three years after the start of a worldwide multi‐country collaborative study in India, Israel, Mexico, Poland, South Africa, the United Kingdom, the United States of America, and Venezuela (WHO 1968). The recommended supplemental dose increased to 400 μg (0.4 mg) per day in 1998 after various studies supported its periconceptional use for prevention of neural tube defects (INACG 1998). At the time it was acknowledged that the rationale for providing folic acid supplementation after the first trimester of pregnancy would not be to prevent congenital anomalies but that the 400 µg (0.4 mg) daily dose of folic acid would provide a safe and healthy intake for women during pregnancy and lactation, although probably more than was actually required to produce an optimal Hb response in pregnant women (INACG 1998).
The tolerable upper intake level for iron has been set based on the gastrointestinal side effects associated with high levels of iron consumed on an empty stomach. Iron has the potential to cause direct erosion and irritation of the gastrointestinal mucosa, to cause oxidative damage of lipid membranes, proteins or DNA, can stimulate inflammation or, as an essential nutrient, fertilise the growth of pathogens. High‐dose iron supplements are commonly associated with constipation and other gastrointestinal effects including nausea, vomiting and diarrhoea, with frequency and severity varying according to the amount of elemental iron released in the stomach. The Institute of Medicine has established the tolerable upper limit for iron during pregnancy as 45 mg/day of iron, a daily dose much lower than international recommendations (IOM 2001), although the methodology and assumptions used have been questionable (Schümann 2007). In most industrialised countries, the decision to prescribe or recommend antenatal iron with folic acid supplementation to women during pregnancy is left to the healthcare personnel, and is based on the individual maternal condition (Nisar 2014; Sanghvi 2010). In the United States, iron supplementation as a primary prevention intervention involves smaller daily iron doses (i.e. 30 mg/day), but therapeutic doses of up to 120 mg elemental iron daily are recommended for the treatment of anaemia (CDC 1998). In the UNited Kingdom, the British Committee for Standards in Haematology does not recommend routine iron supplementation for all women in pregnancy (BCSH 2011).
Why it is important to do this review
Several studies have shown that iron supplementation, with or without folic acid during pregnancy, helps cover the iron intake gap and results in a substantial reduction in women's risk of anaemia in late pregnancy, at delivery and six weeks postpartum (Mahomed 1997; Mahomed 2000a; Villar 2003). However, the overall impact of iron supplementation interventions under field conditions has been limited, and the effectiveness of these interventions has been questioned (Beaton 1999). The limited success has been attributed to inadequate infrastructure and poor compliance (Mora 2002), although few studies have evaluated these issues adequately. The effectiveness of iron supplementation for pregnant women has been evaluated mostly in terms of improvement in Hb concentration, rather than improvements in maternal or infant health (Beaton 2000). This narrow scope may have been an important omission in most studies addressing the efficacy, effectiveness and safety of iron and iron with folic acid supplementation during pregnancy.
An additional important consideration arises when providing iron supplements to women is the presence of malaria. Approximately 40% of the world population is exposed to the parasite and it is endemic in over 100 countries (WHO 2010). Of all the complications associated with this disease, anaemia is the most common and causes the highest number of malaria‐related deaths. Malaria in pregnant women increases the risk of maternal death, miscarriage, stillbirth and low birthweight with an associated risk of neonatal death (WHO 2010; WHO 2014c). Provision of iron in malaria‐endemic areas has been a long standing controversy due to concerns that iron therapy may exacerbate infections, in particular malaria in childhood (Oppenheimer 2001). Although the mechanisms by which additional iron can benefit the parasite are far from clear, it is possible that lower‐dose supplementation might be an effective intervention to prevent anaemia and improve malaria treatment in malaria endemic areas since less iron is available for the parasite (NIH 2011). The potential interaction between malaria interventions and iron interventions in pregnancy has not been well studied. Malaria intermittent preventive treatment (IPT) is recommended for pregnant women in areas of high transmission who are particularly vulnerable to contracting malaria or suffering its consequences. A total of 34 out of 45 countries in Africa with ongoing malaria transmission, had adopted IPT for pregnant women as national policy by 2013 (WHO 2014c).
This review updates a previously published Cochrane Review on iron and iron + folic acid supplementation (Peña‐Rosas 2012) that has clearly shown improvements on biochemical and haematological parameters, and evaluates the issues related to dose and formulation as well as the potential benefits and hazards of daily iron supplementation as a preventive intervention for women during pregnancy.
The effectiveness of different iron treatments for anaemia among pregnant women in clinical practice (Reveiz 2011), and the effects of supplementation with iron and vitamin A during pregnancy (Van den Broek 2010) are covered in other Cochrane reviews. A Cochrane review assesses the effectiveness of oral folate supplementation alone during pregnancy on haematological and biochemical parameters during pregnancy and on pregnancy outcomes (Lassi 2013). The effects and safety of periconceptional folate supplementation for preventing birth defects (De‐Regil 2010), and the effects of multiple vitamin and mineral supplements during pregnancy have also been reviewed elsewhere (Haider 2012; Ramakrishnan 2013). A separate review addresses the effectiveness of intermittent iron and folic acid supplementation regimens for women during pregnancy (Peña‐Rosas 2012a).
Objectives
To assess the effects of daily oral use of iron supplements by pregnant women, either alone or in conjunction with folic acid or with other vitamins and minerals as a public health intervention in antenatal care.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised, cluster‐randomised and quasi‐randomised trials comparing the effects of daily oral prenatal supplements of iron, or iron + folic acid or iron + other vitamins and minerals supplements among pregnant women.
We excluded studies that assessed the effects of multiple combinations of vitamins and minerals, except studies that examined the 'additional effect' of iron or iron + folic acid supplements, i.e. when women in all arms of the trial were provided with the same other micronutrient supplements (with the exception of iron or iron + folic acid).
We have not reviewed the effects of supplementation with multiple micronutrients containing iron or iron + folic acid in comparison to supplementation with iron or iron + folic acid or in comparison to placebo or no treatment. We have excluded studies dealing specifically with iron supplementation as a medical treatment. We also excluded trials addressing the effects of intermittent (i.e. weekly, twice weekly) iron supplementation regimens in comparison to daily supplementation regimens.
Types of participants
Pregnant women of any gestational age and parity.
Types of interventions
We have included a range of interventions providing daily oral supplementation (e.g. tablets, capsules) containing iron alone, iron + folic acid or iron + other vitamins and minerals.
The oral supplements forms include tablets or capsules (WHO 2008). Tablets (soluble tablets, effervescent tablets, tablets for use in the mouth, and modified‐release tablets) are solid dosage forms containing one or more active ingredients. They are obtained by single or multiple compression (in certain cases they are moulded) and may be uncoated or coated. Capsules are solid dosage forms with hard or soft shells, various shapes and sizes, that contain a single dose of one or more active ingredients. Capsules may be hard, soft, and modified‐release capsules and are generally intended for oral administration.
Where data were available we planned to compare the following.
Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo).
Any supplements containing iron and folic acid versus same supplements without iron or folic acid (no iron + folic acid or placebo).
Supplementation with iron alone versus no treatment/placebo.
Supplementation with iron + folic acid versus no treatment/placebo.
Supplementation with iron + folic acid versus folic acid alone (without iron) supplementation.
Supplementation with iron + other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation.
Supplementation with iron + folic acid + other vitamins and minerals versus folic acid + same other vitamins and minerals (without iron) supplementation.
Supplementation with iron + folic acid + other vitamins and minerals versus same other vitamins and minerals (without iron + folic acid) supplementation.
Comparisons 3, 5, 6, and 7 are summarised in comparison 1. Comparisons 4 and 8 are summarised in comparison 2. Comparisons 1 and 2 are used in the 'Summary of findings' tables; we have produced separate tables for infant and maternal outcomes (Table 1; Table 2; Table 3; Table 4).
Summary of findings for the main comparison. (Infant outcomes) Any supplements containing iron compared with same supplements without iron or no treatment/placebo (no iron or placebo) for pregnant women.
| (Infant outcomes) Any supplements containing iron compared with same supplements without iron or no treatment/placebo (no iron or placebo) | ||||
|
Patient or population: Pregnant women of any gestational age and parity Setting: Hospital or community‐based antenatal clinics Intervention: Any supplements containing iron Comparison: Same supplements without iron or no treatment/placebo (no iron or placebo) | ||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Low birthweight (less than 2500 g) (ALL) | RR 0.84 (0.69 to 1.03) | 17,613 (11 RCTs) | ⊕⊕⊝⊝ low 1,2 | |
| Birthweight (g) (ALL) | The mean birthweight (g) (ALL) in the intervention group was 23.75 higher (3.02 lower to 50.51 higher) | 18,590 (15 RCTs) | ⊕⊕⊕⊝ moderate 1 | |
| Preterm birth (less than 37 weeks of gestation) (ALL) | RR 0.93 (0.84 to 1.03) | 19,286 (13 RCTs) | ⊕⊕⊕⊝ moderate 1 | |
| Neonatal death (within 28 days after delivery) (ALL) | RR 0.91 (0.71 to 1.18) | 16,603 (4 RCTs) | ⊕⊕⊝⊝ low 1,2 | |
| Congenital anomalies (ALL) | RR 0.88 (0.58 to 1.33) | 14,636 (4 RCTs) | ⊕⊕⊝⊝ low 1,2 | |
| CI: Confidence interval; RR: risk ratio | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1Several studies contributing data had design limitations
2Wide 95% CI crossing the line of no effect
Summary of findings 2. (Maternal outcomes) Any supplements containing iron compared with same supplements without iron or no treatment/placebo (no iron or placebo) for pregnant women.
| (Maternal outcomes) Any supplements containing iron compared with same supplements without iron or no treatment/placebo (no iron or placebo) | ||||
| Patient or population: Pregnant women of any gestational age and parity Settings: Hospital or community‐based antenatal clinics Intervention: Any supplements containing iron Comparison: same supplements without iron or no treatment/placebo (no iron or placebo) | ||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | RR 0.30 (0.19 to 0.46) | 2199 (14 RCTs) | ⊕⊕⊝⊝ low 1,2 | |
| Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks's gestation or more) (ALL) | RR 0.43 (0.27 to 0.66) | 1256 (7 RCTs) | ⊕⊕⊝⊝ low 2,3 | |
| Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | RR 0.33 (0.01 to 8.19) | 12,560 (2 RCTs) | ⊕⊝⊝⊝ very low 4,5 | |
| Side effects (any reported throughout the intervention period) (ALL) | RR 1.29 (0.83 to 2.02) | 2423 (11 RCTs) | ⊕⊝⊝⊝ very low 2,3,6 | |
| Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | RR 0.22 (0.01 to 3.20) | 2125 (9 RCTs) | ⊕⊝⊝⊝ very low 3,6,7 | |
| Infection during pregnancy (including urinary tract infections) (ALL) | RR 1.21 (0.33 to 4.46) | 727 (1 RCT) | ⊕⊕⊝⊝ low 5 | |
| CI: Confidence interval; RR: risk ratio | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1Several studies contributing data had design limitations and one had serious design limitations
2High heterogeneity I² > 80%
3Several studies contributing data had design limitations
4One of the studies contributing data had design limitations
5Wide 95% CI crossing the line of no effect. Low event rate
6Wide 95% CI crossing the line of no effect
7High heterogeneity I² = 69%
Summary of findings 3. (Infant outcomes) Any supplements containing iron and folic acid compared with same supplements without iron nor folic acid (no iron nor folic acid or placebo) for pregnant women.
| Any supplements containing iron and folic acid compared with same supplements without iron nor folic acid (no iron nor folic acid or placebo) | ||||
| Patient or population: Pregnant women of any gestational age and parity Settings: Hospital or community‐based antenatal clinics Intervention: Any supplements containing iron and folic acid Comparison: Same supplements without iron nor folic acid (no iron nor folic acid or placebo) | ||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Low birthweight (less than 2500 g) (ALL) | RR 1.07 (0.31 to 3.74) | 1311 (2 RCTs) | ⊕⊕⊝⊝ low 1,2 | |
| Birthweight (ALL) | The mean birthweight (ALL) in the intervention group was 57.73 higher (7.66 higher to 107.79 higher) | 1365 (2 RCTs) | ⊕⊕⊕⊝ moderate 1 | |
| Preterm birth (less than 37 weeks of gestation) (ALL) | RR 1.55 (0.40 to 6.00) | 1497 (3 RCTs) | ⊕⊕⊝⊝ low 2,3 | |
| Neonatal death (within 28 days after delivery) (ALL) | RR 0.81 (0.51 to 1.30) | 1793 (3 RCTs) | ⊕⊕⊝⊝ low 2,3 | |
| Congenital anomalies (ALL) | RR 0.70 (0.35 to 1.40) | 1652 (1 RCT) | ⊕⊕⊝⊝ low 2,4 | |
| CI: Confidence interval; RR: risk ratio | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1Both studies contributing data had design limitations
2Wide 95% CI crossing the line of no effect
3All studies contributing data had design limitations
4Study contributing data had design limitations
Summary of findings 4. (Maternal outcomes) Any supplements containing iron and folic acid compared with same supplements without iron nor folic acid (no iron nor folic acid or placebo) for pregnant women.
| (Maternal outcomes) Any supplements containing iron and folic acid compared with same supplements without iron nor folic acid (no iron nor folic acid or placebo) | ||||
| Patient or population: Pregnant women of any gestational age and parity Settings: hospital or community‐based antenatal clinics Intervention: Any supplements containing iron and folic acid Comparison: Same supplements without iron nor folic acid (no iron nor folic acid or placebo) | ||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | RR 0.34 (0.21 to 0.54) | 346 (3 RCTs) | ⊕⊕⊕⊝ moderate 1 | |
| Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL) | RR 0.24 (0.06 to 0.99) | 131 (1 RCT) | ⊕⊕⊝⊝ low 2,3 | |
| Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | not estimable | 131 (1 RCT) | ⊕⊕⊝⊝ low 2,4 | |
| Side effects (any reported throughout the intervention period) (ALL) | RR 44.32 (2.77 to 709.09) | 456 (1 RCT) | ⊕⊕⊕⊝ moderate 2 | |
| Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | RR 0.12 (0.02 to 0.63) | 506 (4 RCTs) | ⊕⊝⊝⊝ very low 1,5 | |
| Infection during pregnancy (including urinary tract infections) (ALL) | RR 1.00 (0.15 to 6.53) | 48 (1 RCT) | ⊕⊝⊝⊝ very low 2,6 | |
| CI: Confidence interval; RR: risk ratio | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1Studies contributing data had design limitations
2Study contributing data had design limitations
3Estimate based on small sample size
4Small sample size and no events
5Wide 95% CI crossing the line of no effect and low event rate
6Wide 95% CI crossing the line of no effect, small sample size and low event rate
Interventions that combined daily oral iron or iron + folic acid supplementation with co‐interventions such as education or other approaches were included, only if the other co‐interventions were the same in both the intervention and comparison groups. Studies examining supplemental iron alone or vitamins and minerals provided from supplementary food‐based interventions (i.e. interventions with multiple micronutrient powders, lipid‐based supplements, fortified complementary foods, and other fortified foods) were excluded. Likewise, regimens providing iron supplements in intermittent regimens were excluded from this review.
Types of outcome measures
Maternal, perinatal and postpartum clinical and laboratory outcomes and infant clinical and laboratory outcomes as described below.
Primary
Infant
Low birthweight (less than 2500 g).
Birthweight (in g).
Preterm birth (less than 37 weeks' gestation).
Neonatal death (within 28 days after delivery).
Congenital anomalies, including neural tube defects (as defined by trialists).
Maternal
Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more).
Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more).
Maternal iron‐deficiency anaemia at term (as defined by trialists at 37 weeks' gestation or more).
Maternal death (death while pregnant or within 42 days of termination of pregnancy).
Side effects (any reported throughout intervention period)*.
Severe anaemia at any time during second or third trimesters (Hb less than 70 g/L).
Clinical malaria (as defined by trialists).
Infection during pregnancy (including urinary tract infections and others as specified by trialists).
Secondary
Infant
Very low birthweight (less than 1500 g).
Very premature birth (less than 34 weeks' gestation).
Hb concentration in the first six months (in g/L, counting the last reported measure after birth within this period).
Ferritin concentration in the first six months (in μg/L, counting the last reported measure after birth within this period).
Development and motor skills (as defined by trialists).
Admission to special care unit.
Maternal
Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more).
Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more).
Maternal iron‐deficiency anaemia at or near term ((Hb less than 110 g/L and at least one additional laboratory indicator at 34 weeks' gestation or more).
Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more).
Maternal Hb concentration within six weeks postpartum (in g/L).
Maternal high Hb concentrations at any time during second or third trimester (defined as Hb greater than 130 g/L).
Maternal high Hb concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more).
Moderate anaemia at postpartum (Hb between 80 and 109 g/L).
Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more).
Severe anaemia postpartum (Hb less than 80 g/L).
Puerperal infection (as defined by trialists).
Antepartum haemorrhage (as defined by trialists).
Postpartum haemorrhage (intrapartum and postnatal, as defined by trialists).
Transfusion given (as defined by trialists).
Diarrhoea (as defined by trialists).
Constipation (as defined by trialists).
Nausea (as defined by trialists).
Heartburn (as defined by trialists).
Vomiting (as defined by trialists).
Maternal well being/satisfaction (as defined by trialists).
Placental abruption (as defined by trialists).
Premature rupture of membranes (as defined by trialists).
Pre‐eclampsia (as defined by trialists).
* For trials reporting individual side effects separately but not specifying the number of women reporting any side effects, for our primary outcome, we have selected the side effect with the greatest number of women (in the intervention and control groups combined) reporting that particular problem. We did this to avoid double counting any women reporting more than one side effect.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (10 January 2015).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched the International Clinical Trials Registry Platform (ICTRP) for any ongoing or planned trials (26 February 2015) using the search terms described in Appendix 1.
Searching other resources
For assistance in identifying ongoing or unpublished studies, we also contacted the Departments of Reproductive Health and Research and Nutrition for Health and Development from the World Health Organization (WHO), the nutrition section of the United Nations Children's Fund (UNICEF), the World Food Programme (WFP), the U.S. Centers for Disease Control and Prevention (CDC), the Micronutrient Initiative (MI), the Global Alliance for Improved Nutrition (GAIN), Hellen Keller International (HKI), and the Sight and Life (26 February 2015) .
We did not apply any language or date restrictions.
Data collection and analysis
For methods used when assessing trials identified in the previous version of this review, see Peña‐Rosas 2012.
For this update, we used the following methods when assessing the trials identified by the updated search (Korkmaz 2014; Liu 2012). These methods are based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors independently assessed and selected the trials for inclusion in this review. We resolved any disagreement on eligibility for inclusion by discussion.
It was not possible for us to assess the relevance of the trials blinded because we knew the authors' names, institution, journal of publication and results, when we applied the inclusion criteria.
Data extraction and management
We designed a form to facilitate the process of data extraction and to request additional (unpublished) information from the authors of the original reports. We resolved any disagreements among us by discussion, and, if necessary, sought clarification from the authors of the original reports. We extracted data relating to the setting and cadre from all the included studies specifying whether the intervention was reported as being done by a physician, obstetrician, lay health worker, midwife, dietitian or a combination of health professionals. We also extracted the type of healthcare facility and the geographical location of the intervention, when this information was available.
We entered data onto Review Manager software (RevMan 2014) and checked for accuracy.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion.
(1) Sequence generation (checking for possible selection bias)
We have described for each included study the method used to generate the allocation sequence. We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear.
(2) Allocation concealment (checking for possible selection bias)
We have described for each included study the method used to conceal the allocation sequence and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear.
(3.1) Blinding of participants and personnel (checking for possible performance)
We have described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. For this type of intervention, where different regimens were compared, it would be theoretically possible to blind study participants and staff by providing both active and placebo tablets to women allocated to intermittent regimens and placebo tablets to women in no supplementation arms of trials.
Blinding was assessed separately for different outcomes or classes of outcomes and we have noted where there was partial blinding.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We have described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We assessed losses to follow‐up and post‐randomisation exclusions systematically for each trial.
We have described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We have noted whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. We assessed methods as:
low risk of bias;
high risk of bias; or
unclear.
We considered follow‐up to be adequate if more than 80% of participants initially randomised in a trial were included in the analysis and any loss was balanced across groups, unclear if the percentage of initially randomised participants included in the analysis was unclear, and inadequate if less than 80% of those initially randomised were included in the analysis or if loss was imbalanced in different treatment groups.
(5) Selective reporting bias
We have described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review had been reported);
high risk of bias (where not all the study’s pre‐specified outcomes had been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear.
(6) Other sources of bias
We assessed whether each study was free of other problems that could put it at risk of bias. We have noted for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of further bias;
high risk of further bias;
unclear whether there is a risk of further bias.
(7) Overall risk of bias
We have made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2011) and for primary outcomes have explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the quality of evidence using GRADE
For the assessment across studies, we employed the GRADE approach to interpret findings (Langendam 2013) and the GRADE profiler (GRADEpro 2014) allowed us to import data from Review Manager 5.3 (RevMan 2014) to create 'Summary of findings' (SoF) tables (set out in Table 1; Table 2; Table 3; Table 4). The primary outcomes for each comparison have been listed with estimates of relative effects along with the number of participants and studies contributing data for those outcomes. These tables provide outcome‐specific information concerning the overall quality of evidence from studies included in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes we considered. Only primary outcomes were included in the 'Summary of findings' tables. For each individual outcome, two review authors independently assessed the quality of the evidence using the GRADE approach (Balshem 2010).
For assessments of the overall quality of evidence for each outcome that included pooled data from included trials, we downgraded the evidence from 'high quality' by one level for serious (or by two for very serious) study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias. This assessment was limited only to the trials included in this review and as we did not consider there was a serious risk of indirectness or publication bias, we did not downgrade in these domains.
Measures of treatment effect
For dichotomous data, we present results as summary risk ratio (RR) with 95% confidence intervals (CI).
For continuous data, we have used the mean difference (MD) if outcomes were measured in the same way between trials. We planned to use the standardised mean difference (SMD) to combine trials measuring the same outcome, but using different scales or methods.
Unit of analysis issues
Cluster‐randomised trials
We included cluster‐randomised trials in the analyses along with individually‐randomised trials. Cluster‐randomised trials are labelled with a (C). Where possible, we estimated the intracluster correlation co‐efficient (ICC) from trials' original data sets and reported the design effect. On the basis of this information we used the methods set out in the Handbook to calculate the adjusted sample sizes (Higgins 2011).
We included four cluster‐randomised trials (Christian 2003 (C); Hoa 2005 (C); Menendez 1994 (C); Zeng 2008 (C)). One of these trials did not contribute data to the analysis (Hoa 2005 (C)). For the remaining three cluster‐randomised trials (Christian 2003 (C); Menendez 1994 (C); Zeng 2008 (C)), data have been adjusted to take account of the design effect. In the study by Christian 2003 (C), adjusted data were provided by the author using outcome‐specific ICCs. For the Zeng 2008 (C) trial, we adjusted the published results and calculated an effective sample size by dividing figures by the design effect calculated using the ICC for the trial’s primary outcome: birthweight ICC = 0.03. We used the same sample adjustment for all outcomes. We used the same method for the Menendez 1994 (C) trial, however in this case there was insufficient information in the study reports to allow us to calculate the design effect and so we estimated it using the ICC for Hb at term (ICC = 0.03) reported in another study with similar average cluster sizes (Winichagoon 2003). We used this same ICC for all outcomes.
Where we have identified both cluster‐randomised trials and individually‐randomised trials reporting data for the same outcome, we considered that it was reasonable to combine the results from both if there was little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit was considered to be unlikely.
Cross‐over trials
We did not include cross‐over trials.
Dealing with missing data
For included studies, we noted levels of attrition in the Characteristics of included studies tables. We explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
When possible, we conducted an available case analysis and reinstated previously excluded cases, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial is the number randomised minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
We examined the forest plots for the analyses visually to assess any obvious heterogeneity in terms of the size or direction of treatment effect between studies. We used the I², and Tau² statistics and the P value of the Chi² test for heterogeneity to quantify heterogeneity among the trials in each analysis. The I² statistic quantifies inconsistency and describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error (chance).
Assessment of reporting biases
For our primary outcomes, we investigated publication bias on outcomes with more than 10 trials by examining the funnel plots for signs of asymmetry, although we gave consideration to reasons other than publication bias that could explain the asymmetry, when present.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014).
Because of our experience in conducting other reviews in this area, we anticipated high heterogeneity among trials and we pooled trial results using a random‐effects model and were cautious in our interpretation of the pooled results. We have indicated in the text that the random‐effects model gives the average treatment effect. For statistically significant results where there are high levels of heterogeneity ((I² greater than 50%), we have given the values of I², Tau² and the P value of the Chi² test for heterogeneity and have provided an estimate of the 95% range of underlying intervention effects (prediction interval (PI)).
Subgroup analysis and investigation of heterogeneity
Where more than one trial was included in a comparison, we conducted both overall analysis of the effects of various supplementation regimens on primary outcomes and subgroup analysis on the primary outcomes based on the following criteria:
by gestational age: early, if supplementation started before 20 weeks' gestation or prior to pregnancy; late if supplementation started at 20 weeks of gestation or later; or, unspecified or mixed gestational ages at the start of supplementation;
by anaemic status at start of intervention: anaemic when Hb below 110 g/L during first and third trimesters or below 105 g/L in second trimester; non‐anaemic if Hb 110 g/L or above during first and third trimesters or Hb 105 g/L or above if in second trimester; or unspecified/mixed anaemic status;
by dose of iron: low daily dose of iron if 30 mg or less of elemental iron; medium daily dose of iron (more than 30 mg and less than 60 mg elemental iron) and higher daily dose of iron if dose is 60 mg elemental iron or more);
by type of formulation: slow release iron supplement (as defined by trialists) or normal release iron supplement/not specified;
by iron compound bioavailability in comparison to ferrous sulphate: higher bioavailability: NaFeEDTA; equivalent or lower relative bioavailability: ferrous sulphate, ferrous fumarate, ferrous gluconate; other/not specified;
by malaria risk setting: study carried out in malaria risk‐free countries or study carried out in countries with some malaria risk or explicitly described as a malaria risk study site.
In the subgroup analyses we have provided totals and subtotals and have assessed subgroup differences by interaction tests available in RevMan (RevMan 2014). Where there was evidence of a difference between subgroups, we have reported this in the text and presented the results for the subgroup analyses quoting the Chi² statistic and P value, and the interaction I² value. However, for some outcomes few studies contributed data, and for some outcomes, all the trials were in the same subgroup; as more data become available, in updates of the review, we will explore possible subgroup differences as a means of exploring heterogeneity.
Sensitivity analysis
In previous versions of the review for primary outcomes we conducted sensitivity analysis based on risk of bias. We considered a study to be of high quality if it was assessed as low risk of bias in both the randomisation and allocation concealment and in either blinding or loss to follow‐up. In this updated version of the review, for our main comparisons (comparisons 1 and 2) for primary outcomes we have now graded the overall quality of the evidence (taking into account risk or bias, heterogeneity, imprecision of findings and possible publication bias); we considered that this would give a better indication of the overall quality of evidence at the outcome level. The quality of the evidence is noted both in the text (Effects of interventions) and in tables (Table 1; Table 2; Table 3; Table 4).
For comparisons 3 onwards we have carried out planned sensitivity analysis because for these comparisons the overall quality of the evidence was not graded.
Results
Description of studies
Results of the search
A single search was carried out for this and a related review examining intermittent iron and iron plus folic acid supplementation in pregnancy (Peña‐Rosas 2012a). The study flow is depicted in Figure 1. In this updated review, we have included 61 and excluded 136 trials. Data from two new trials have been included (Korkmaz 2014; Liu 2012) and a trial that was included in the previous version of the review has now been excluded as it was not clear that the control and intervention groups were comparable, and both groups received iron (Hemminki 1991). We confirmed that seven trials are still ongoing. Forty‐four trials involving 43,274 women contributed data for the comparisons in this review.
1.
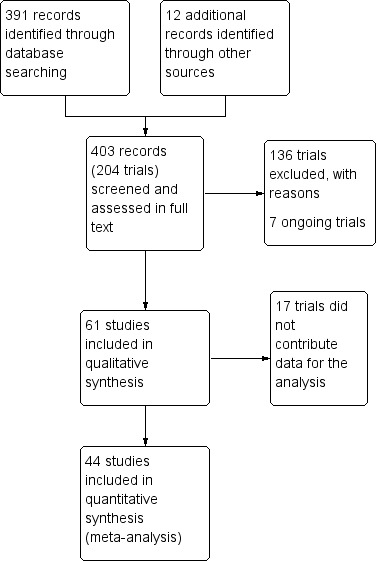
Study flow diagram.
Studies by Chanarin 1965, Dommisse 1983, Fenton 1977, Fleming 1974, Fleming 1985, Foulkes 1982, Freire 1989, Groner 1986, Han 2011, Hoa 2005 (C), Ma 2010, Simmons 1993, Suharno 1993, Sun 2010 and Tholin 1993 were all assessed as eligible for inclusion but these studies have not contributed data to the review. We were not able to include data, either because the studies did not report data on any of the review's prespecified outcomes, or because the results were not presented in a way that allowed us to enter them into the analyses (e.g. results were not reported separately for randomised groups, or standard deviations or standard errors were not reported for continuous outcomes). In addition, two studies that were otherwise eligible for inclusion (Butler 1967; Kuizon 1979) had such serious attrition (up to 80% for some outcomes) that we considered results were difficult to interpret, and we have not included data from these trials in the review. Details of all included studies can be found in the Characteristics of included studies tables.
In addition to the published papers, abstracts and reports identified by the search, several trial authors provided additional unpublished information for inclusion in the review, including individual patient data sets for ad hoc statistical analysis (Butler 1967; Eskeland 1997; Lee 2005); some authors provided re analysed data for this review (Christian 2003 (C); Makrides 2003; Paintin 1966), or additional information useful for description and 'Risk of bias' assessment of the studies (Cogswell 2003; Freire 1989; Harvey 2007; Siega‐Riz 2001; Zeng 2008 (C); Ziaei 2007; Ziaei 2008).
For the trials contributing to the analyses, we have treated a study carried out collaboratively in two different sites as two different trials, one conducted in Rotterdam (Wallenburg 1983) and one conducted in Antwerp (Buytaert 1983). Some trials included more than two arms and may therefore, be included in more than one comparison.
Included studies
Sixty‐one studies were included in this review.
Settings
The studies included in the review were carried out since 1936 in countries across the globe: 24 trials in Europe with 12 trials in United Kingdom (Butler 1967; Chanarin 1965; Chisholm 1966;.Chanarin 1971; Fenton 1977; Foulkes 1982; Harvey 2007; Kerr 1958; Paintin 1966; Taylor 1982 Willoughby 1967; Wills 1947); two trials in Norway (Eskeland 1997; Romslo 1983); one trial in Finland (Puolakka 1980); two trials in Sweden (Svanberg 1975; Tholin 1993); two trials in The Netherlands (Van Eijk 1978; Wallenburg 1983); one each in Denmark (Milman 1991); Ireland (Barton 1994); Belgium (Buytaert 1983); France (De Benaze 1989); and Italy (Tura 1989).
Eleven trials were conducted in the Americas with eight trials conducted in the United States of America (Cogswell 2003; Corrigan 1936; Groner 1986; Holly 1955; Hood 1960; Meier 2003; Pritchard 1958; Siega‐Riz 2001); one in Canada (Cantlie 1971); one in Ecuador (Freire 1989); and one in Jamaica (Simmons 1993). Four trials were conducted in Africa with one trial in South Africa (Dommisse 1983); one in Nigeria (Fleming 1985); one in Gambia (Menendez 1994 (C)); and one in Niger (Preziosi 1997). Four trials were conducted in Iran (Falahi 2010; Ouladsahebmadarek 2011; Ziaei 2007; Ziaei 2008). One trial was conducted in Hong Kong (Chan 2009), and five in China (Han 2011; Liu 2000; Ma 2010; Sun 2010; Zeng 2008 (C)). Three trials were conducted in Australia (Fleming 1974; Hankin 1963; Makrides 2003). Eight trials were conducted in Asia with one trial each in Myanmar (Burma) (Batu 1976); Thailand (Charoenlarp 1988); Nepal (Christian 2003 (C)); Vietnam (Hoa 2005 (C)); Philippines (Kuizon 1979); South Korea (Lee 2005); Indonesia (Suharno 1993); and Turkey (Korkmaz 2014).
Most included trials were published between the years 2000‐2009 and 1980‐1989. Two trials were published before the 1950s, three trials in the period 1950‐1959, seven trials between 1960‐1969, eight trials between 1970‐1979, 13 trials in the period 1980‐1989, nine trials between 1990‐1999, 13 trials in the period 2000‐2009 and only six included trials have been published since 2010 to the present.
Twenty‐three studies were conducted in countries that in 2011 (WHO 2014c; WHO 2011c) had some malaria risk in parts of the country, of diverse characteristics (Batu 1976; Chan 2009; Charoenlarp 1988; Christian 2003 (C); Dommisse 1983; Falahi 2010; Fleming 1985; Freire 1989; Han 2011; Hoa 2005 (C); Kuizon 1979; Lee 2005; Liu 2000; Ma 2010; Menendez 1994 (C); Ouladsahebmadarek 2011; Preziosi 1997; Simmons 1993; Suharno 1993; Sun 2010; Zeng 2008 (C); Ziaei 2007; Ziaei 2008). Only two of these reported malaria outcomes (Fleming 1985; Menendez 1994 (C)). In some of these countries/territories, malaria is present only in certain areas or up to a particular altitude. In many countries, malaria has a seasonal pattern (WHO 2011c). These details as well as information on the predominant malaria species, status of resistance to antimalarial drugs for each country where an included study was conducted were extracted for 2011 (WHO 2011c) and provided in the notes section of the Characteristics of included studies tables. Thirty‐seven of the included trials, mostly from Australia, Canada, United States of America, or countries in Europe were carried out in areas that generally are considered malaria‐free.
Participants
In 24 trials it was specifically stated that all women recruited were non‐anaemic at the start of supplementation (Barton 1994; Buytaert 1983; Cantlie 1971; Chisholm 1966; Cogswell 2003; De Benaze 1989; Eskeland 1997; Falahi 2010; Harvey 2007; Korkmaz 2014; Liu 2000; Makrides 2003; Meier 2003; Liu 2012; Ouladsahebmadarek 2011; Puolakka 1980; Romslo 1983; Siega‐Riz 2001; Svanberg 1975; Tholin 1993; Tura 1989; Wallenburg 1983; Ziaei 2007; Ziaei 2008). For the remaining trials, it was not always stated whether or not women were anaemic and some studies included some women with mild and moderate anaemia so samples were mixed in terms of women's anaemia status at the start of supplementation. In some of these trials it was specifically stated that women with severe anaemia were excluded (Batu 1976; Butler 1967; Chan 2009; Charoenlarp 1988; Kerr 1958; Korkmaz 2014; Paintin 1966; Willoughby 1967). Five studies specifically recruited women with mild and moderate anaemia (Hb between 80 to 110 g/L), but none of these trials contribute data to the review (Han 2011; Ma 2010; Simmons 1993; Suharno 1993; Sun 2010).
In most of the trials, women began taking supplements before 20 weeks' gestation and continued taking supplements up until delivery. In 13 trials supplementation started at or after 20 weeks' gestation (Batu 1976; Chanarin 1965; Chisholm 1966; Eskeland 1997; Fleming 1974; Freire 1989; Hood 1960; Kerr 1958; Korkmaz 2014; Makrides 2003; Menendez 1994 (C); Paintin 1966; Preziosi 1997). In 16 studies it was not clear at what gestational age women started to take supplements, or gestational ages were mixed and samples included both women who started supplements before and after the 20th week of pregnancy (Cantlie 1971; Charoenlarp 1988; Corrigan 1936; Fleming 1985; Hankin 1963; Holly 1955; Kuizon 1979; Lee 2005; Liu 2000; Ma 2010; Meier 2003; Pritchard 1958; Simmons 1993; Suharno 1993; Sun 2010; Willoughby 1967).
Interventions
Daily iron dose
The daily dose of elemental iron in some of the groups in the included trials ranged between 9 mg to 900 mg of elemental iron daily. One trial provided 9 mg elemental iron daily (Eskeland 1997); one trial provided 12 mg elemental iron (Paintin 1966); one trial provided 20 mg elemental iron daily (Makrides 2003); one trial provided 27 mg elemental iron (Eskeland 1997); six trials provided 30 mg elemental iron (Chanarin 1971; Cogswell 2003; Lee 2005; Ouladsahebmadarek 2011; Siega‐Riz 2001; Zeng 2008 (C); one trial provided 40 mg elemental iron (Tura 1989); one trial 45 mg elemental iron (De Benaze 1989); one trial 50 mg elemental iron (Ziaei 2007, Ziaei 2008); and one trial 55 mg elemental iron (Hood 1960); 18 trials provided 60 mg elemental iron (Barton 1994; Batu 1976; Chan 2009; Christian 2003 (C); Falahi 2010; Fenton 1977; Fleming 1974; Fleming 1985; Groner 1986; Han 2011; Hoa 2005 (C); Korkmaz 2014; Ma 2010; Meier 2003; Menendez 1994 (C); Suharno 1993; Sun 2010; Zeng 2008 (C)); two trials provided 65 mg of elemental iron (Kuizon 1979; Taylor 1982); one trial 66 mg elemental iron (Milman 1991); two trials provided 78 mg elemental iron (Cantlie 1971; Freire 1989); one trial provided 80 mg elemental iron (Wills 1947); eight trials provided 100 mg of elemental iron (Foulkes 1982; Hankin 1963; Harvey 2007; Liu 2000; Preziosi 1997; Simmons 1993; Tholin 1993; Van Eijk 1978); five trials provided 105 mg of elemental iron daily (Buytaert 1983; Kerr 1958; Paintin 1966; Wallenburg 1983; Willoughby 1967); one trial provided 112 mg elemental iron (Pritchard 1958); two trials provided 120 mg of elemental iron (Charoenlarp 1988; Dommisse 1983); one trial provided 122 mg of elemental iron (Butler 1967); three trials provided 200 mg of elemental iron (Puolakka 1980; Romslo 1983; Svanberg 1975); one trial 220 mg elemental iron (Hood 1960); one trial 240 mg of elemental iron (Charoenlarp 1988); and one trial 900 mg elemental iron (Chisholm 1966). One trial did not report the amount of iron as elemental iron and only referred the amount provided as a total daily dose 0.6 g of ferrous sulphate (Corrigan 1936), while another referred a dose of 1 g of iron salt daily (Holly 1955).
Folic acid daily dose
For trials providing folic acid daily as part of the intervention, the doses ranged from 10 μg (0.01 mg) folic acid to 5000 μg (5 mg) folic acid daily along with the iron. In one trial each, the dose of folic acid provided was: 10 μg (0.01 mg) folic acid (Chanarin 1965); 30 μg (0.03 mg) folic acid (Chanarin 1965); 100 μg (0.1 mg) of folic acid (Willoughby 1967); 175 μg (0.17 mg) folic acid (Lee 2005); 250 μg (0.25 mg) folic acid (Hoa 2005 (C)); 300 μg (0.3 mg) of folic acid (Willoughby 1967). In three trials, participants received a daily dose of 350 μg (0.35 mg) folic acid (Foulkes 1982; Lee 2005; Taylor 1982). In six trials the daily doses provided to participants in some of the groups were: 400 μg (0.4 mg) folic acid (Christian 2003 (C); Korkmaz 2014; Ma 2010; Simmons 1993; Sun 2010; Zeng 2008 (C)); 450 μg (0.45 mg) folic acid (Willoughby 1967); three trials provided 500 μg (0.5 mg) folic acid daily (Chisholm 1966; Fleming 1974; Siega‐Riz 2001); five trials provided participants in some of the groups with 1000 μg (1 mg) folic acid daily (Barton 1994; Batu 1976; Fleming 1985; Meier 2003; Ziaei 2007); and one trial provided participants in some of the groups with 3400 μg (3.4 mg) of folic acid daily (Butler 1967). Four trials of iron and folic acid supplementation provided 5000 μg (5 mg) folic acid daily (Charoenlarp 1988; Chisholm 1966; Fleming 1974; Menendez 1994 (C).
Type of iron compounds
With the exception of six trials that explicitly described the supplements as slow or sustained release (Buytaert 1983; Hood 1960; Liu 2000; Simmons 1993; Svanberg 1975; Wallenburg 1983), all other trials appeared to be standard preparations.
Eight trials did not specify the iron compound used in the trials and described the iron daily dose only in terms of elemental iron (Barton 1994; Fleming 1985; Foulkes 1982; Korkmaz 2014; Makrides 2003; Ouladsahebmadarek 2011; Paintin 1966; Zeng 2008 (C)).
Most supplements used in trials were equivalent or lower, rather than high relative bioavailability iron compounds (ferrous sulphate and ferrous fumarate). Thirty‐six trials used iron supplements in one of the groups that was provided as ferrous sulphate (Batu 1976; Butler 1967; Buytaert 1983; Chan 2009; Charoenlarp 1988; Cogswell 2003; Corrigan 1936; Dommisse 1983; Falahi 2010; Fenton 1977; Fleming 1974; Freire 1989; Han 2011; Hoa 2005 (C); Holly 1955; Hood 1960; Kerr 1958; Kuizon 1979; Lee 2005; Liu 2000; Ma 2010; Meier 2003; Menendez 1994 (C); Puolakka 1980; Romslo 1983; Siega‐Riz 2001; Simmons 1993; Suharno 1993; Sun 2010; Svanberg 1975; Taylor 1982; Tholin 1993; Van Eijk 1978; Wallenburg 1983; Ziaei 2007; Ziaei 2008). Six trials used ferrous fumarate as the form of iron provided to the participants (Chanarin 1965; Chanarin 1971; Christian 2003 (C); Eskeland 1997; Groner 1986; Milman 1991). One trial used ferrous iron (Cantlie 1971).
Ferrous gluconate was used in six included trials (Chisholm 1966; Hankin 1963; Harvey 2007; Kerr 1958; Pritchard 1958; Wills 1947). Two trials used ferrous betainate hydrochloride (De Benaze 1989; Preziosi 1997), one trial used heme iron from porcine blood (Eskeland 1997), one trial used ferritin in a micro granulated gastric resistant capsule (Tura 1989), one used chelated iron aminoates (Willoughby 1967), and one study (Han 2011) used iron EDTA.
Bioavailability of iron compounds is assessed in comparison (relative) to ferrous sulphate.
Supervision and co‐interventions
In most of the studies, women took the supplements without supervision. Some trials report that intake of the supplements was supervised in all or some of the groups (Batu 1976; Charoenlarp 1988; Preziosi 1997). In Christian 2003 (C), the intake was unsupervised but trial personnel visited women twice each week to monitor supplement intake.
Some studies included co‐interventions in addition to the iron or iron + folic acid supplement. For example, in the study by Cantlie 1971, participants from both groups received one tablet of multiple micronutrient supplement daily containing: 2 mg copper citrate, 6 mg magnesium stearate, 0.3 mg manganese carbonate, 1000 IU vitamin A , 500 IU vitamin D, bone flour 130 mg, 1 mg vitamin B1, 1 mg vitamin B2, 50 mg brewer yeast concentrate, 5 mg niacinamide, 25 mg vitamin C, 0.2 mg sodium iodide and 0.049 μg folate (naturally occurring), and in Christian 2003 (C), all participants were offered a 1000 μg retinol equivalents vitamin A supplement daily and deworming treatment (albendazole 400 mg single dose) in the second and third trimester. In Fleming 1974, all participants received 50 mg of ascorbic acid daily from the first visit until the 20th week. In Fleming 1985, the participants from the groups included in this review received chloroquine 600 mg base once, followed by proguanil 100 mg per day. In Menendez 1994 (C), all pregnant women received a weekly tablet of 5000 μg (5 mg) of folic acid but no antimalarial chemoprophylaxis. In the study by Siega‐Riz 2001, folic acid supplements were prescribed for all women who had received the positive pregnancy test until the first prenatal visit. In Simmons 1993, all women received 400 μg (0.4 mg) of folic acid.
Intervention settings and health worker cadre
In the majority of these studies (52 studies, 86%), the intervention was delivered in hospital or community‐based antenatal clinics usually by physicians or other healthcare professionals including midwives, dieticians or social workers. In eight of the studies the intervention was delivered by community workers, traditional birth attendants or village‐based healthcare staff, and supplements were provided during visits to women's homes or in local community settings. The supplements were provided by village‐based traditional birth attendants in the study by Menendez 1994 (C). In the Han 2011 trial, village nurses made visits to women's homes to deliver supplements and monitor women's health. Community health or village workers were involved in delivering supplementation programmes in the trials by Charoenlarp 1988; Christian 2003 (C); Hoa 2005 (C); Ma 2010; Suharno 1993; and Sun 2010.
Comparisons
Comparison 1: the 44 trials that contributed data compared the effects of any daily oral supplements containing iron versus same daily oral supplements without iron. This included data from 35 trials that compared the effects of daily iron supplementation with the effects of no iron or placebo (Batu 1976; Buytaert 1983; Chan 2009; Chanarin 1971; Charoenlarp 1988; Chisholm 1966; Cogswell 2003; Corrigan 1936; De Benaze 1989; Eskeland 1997; Falahi 2010; Hankin 1963; Harvey 2007; Holly 1955; Hood 1960; Kerr 1958; Korkmaz 2014; Liu 2012; Makrides 2003; Meier 2003; Menendez 1994 (C); Milman 1991; Ouladsahebmadarek 2011; Paintin 1966; Preziosi 1997; Pritchard 1958; Puolakka 1980; Romslo 1983; Svanberg 1975; Tura 1989; Van Eijk 1978; Wallenburg 1983; Willoughby 1967; Wills 1947; Ziaei 2008). Data from eight trials included in this comparison evaluated the effects of daily iron + folic acid supplementation with the effects of no treatment (Barton 1994; Batu 1976; Charoenlarp 1988; Chisholm 1966; Christian 2003 (C); Lee 2005; Taylor 1982; Willoughby 1967). Data from one study (Christian 2003 (C)) which met the criteria for high quality examined groups receiving daily iron + folic acid versus women receiving folic acid (without iron), with vitamin A supplementation as co‐intervention. Six studies provided data comparing the effects of daily iron + folic acid with daily folic acid alone (without iron) supplementation (Batu 1976; Chisholm 1966; Christian 2003 (C); Liu 2012; Zeng 2008 (C); Ziaei 2007). Data from four studies compared women receiving oral iron + other vitamins and minerals with women receiving other vitamins and minerals (without iron) supplementation (Cantlie 1971; Liu 2000; Ouladsahebmadarek 2011; Siega‐Riz 2001). Some trials provide data from different arms of the study for different comparisons. Of all the studies that provided data in this comparison, 15 trials were of high quality according to our pre‐established criteria (Barton 1994; Buytaert 1983; Chisholm 1966; Christian 2003 (C); Cogswell 2003; Eskeland 1997; Harvey 2007; Makrides 2003; Preziosi 1997; Siega‐Riz 2001; Tura 1989; Wallenburg 1983; Zeng 2008 (C); Ziaei 2007; Ziaei 2008).
Comparison 2: eight trials compared the effects of daily iron + folic acid supplementation with the effects of same supplements without iron + folic acid (no iron + folic acid or placebo). Seven of them compared the effects of daily iron + folic acid supplementation with the effects of no treatment (Barton 1994; Batu 1976; Charoenlarp 1988; Chisholm 1966; Lee 2005; Taylor 1982; Willoughby 1967). Only two of these (Barton 1994; Chisholm 1966), met the criteria for high quality. No studies compared women receiving daily oral iron + folic acid + other vitamins and minerals with women receiving other vitamins and minerals (without iron + folic acid). One study (Christian 2003 (C)) included a group that compared daily iron + folic acid supplementation in comparison to no treatment, considering the vitamin A supplementation and deworming as co‐interventions in the compared groups.
Comparison 3: 33 trials compared the effects of daily iron alone supplementation with the effects of no iron or placebo (Batu 1976; Buytaert 1983; Chan 2009; Chanarin 1971; Charoenlarp 1988; Chisholm 1966; Cogswell 2003; Corrigan 1936; De Benaze 1989; Eskeland 1997; Falahi 2010; Hankin 1963; Harvey 2007; Holly 1955; Hood 1960; Kerr 1958; Korkmaz 2014; Makrides 2003; Meier 2003; Menendez 1994 (C); Milman 1991; Paintin 1966; Preziosi 1997; Pritchard 1958; Puolakka 1980; Romslo 1983; Svanberg 1975; Tura 1989; Van Eijk 1978; Wallenburg 1983; Willoughby 1967; Wills 1947; Ziaei 2008). Of these, 12 trials were of high quality according to our pre‐established criteria (Buytaert 1983; Chisholm 1966, Cogswell 2003; Christian 2003 (C); Eskeland 1997; Harvey 2007; Korkmaz 2014; Makrides 2003; Preziosi 1997;Tura 1989; Wallenburg 1983; Ziaei 2008).
Comparison 4: eight trials compared the effects of daily iron + folic acid supplementation with the effects of no treatment (Barton 1994; Batu 1976; Charoenlarp 1988; Chisholm 1966; Christian 2003 (C); Lee 2005; Taylor 1982; Willoughby 1967). Only three of them (Barton 1994; Chisholm 1966; Christian 2003 (C)), met the criteria for high quality. One study (Christian 2003 (C)), included a group that compared daily iron + folic acid supplementation in comparison to no treatment, considering the vitamin A supplementation and deworming as co‐interventions in the compared groups.
Comparison 5: five studies compared the effects of daily iron + folic acid with daily folic acid alone (without iron) supplementation (Batu 1976; Chisholm 1966; Christian 2003 (C); Zeng 2008 (C); Ziaei 2007). Four of the trials met the criteria for high quality (Chisholm 1966; Christian 2003 (C); Zeng 2008 (C); Ziaei 2007). The study (Christian 2003 (C)) included a group that compared daily iron + folic acid supplementation in comparison daily folic acid alone, considering the vitamin A supplementation and deworming as co‐interventions in the compared groups.
Comparison 6: three studies compared women receiving oral iron + other vitamins and minerals with women receiving other vitamins and minerals (without iron) supplementation (Cantlie 1971; Ouladsahebmadarek 2011; Siega‐Riz 2001). One of the studies met the criteria for high quality (Siega‐Riz 2001). One group in the study Liu 2000, provided iron with vitamin C, but the comparison groups had different nutrients.
Comparison 7: no studies compared women receiving daily iron + folic acid + other vitamins and minerals versus women receiving folic acid and other vitamins and minerals (without iron).
Comparison 8: no studies compared women receiving daily oral iron + folic acid + other vitamins and minerals with women receiving same other vitamins and minerals (without iron + folic acid).
See the tables of Characteristics of included studies for a detailed description of all the studies. All included studies met the pre‐stated inclusion criteria.
Excluded studies
Altogether, we excluded 136 studies; some studies were excluded for more than one reason. The main reason for excluding studies was that participants in all arms of trials received iron and were therefore not eligible for any of the comparisons included in this review. This reason applied to a total of 95 trials.
In 49 trials women received different types of iron (for example ferrous iron versus iron fumarate), or women received iron with or without other vitamins or supplements (Afifi 1978; Babior 1985; Balmelli 1974; Burslem 1968; Buss 1981; Carrasco 1962; Castren 1968; Chanarin 1968; Coelho 2000; Dawson 1987; Dijkhuizen 2004; Ekstrom 1996; Fletcher 1971; Giles 1971; Gringras 1982; Hartman‐Craven 2009; Hosokawa 1989; Hossain 2014; Kaestel 2005; Kann 1988; Lira 1989; Ma 2008; Mbaye 2006; Metz 1965; Hemminki 1991; Milman 2014; Parkkali 2013: Morrison 1977; Nogueira 2002; Ogunbode 1984; Ogunbode 1992; Osrin 2005; Payne 1968; Rae 1970; Ramakrishnan 2003; Rayado 1997; Rolschau 1979; Roth 1980; Rybo 1971; Saha 2007; Shatrugna 1999; Sjostedt 1977; Srisupandit 1983; Stone 1975; Trigg 1976; Weil 1977; West 2014; Willoughby 1966; Willoughby 1968;).
In 38 trials both groups received iron and either different doses or regimens of iron supplementation were compared (Aaseth 2001; Ahn 2006; Arija 2014; Brown 1972; Guldholt 1991; Horgan 1966; Madan 1999; Milman 2005; Nguyen 2008; Reddaiah 1989; Thane‐Toe 1982; Thomsen 1993; Vogel 1963; Zhou 2009), or different types of regimen (for example, daily versus weekly iron) (Agrawal 2011; Bhatla 2009; Casanueva 2003a; Chew 1996a; Chew 1996b; Ekstrom 2002; Gomber 2002; Goonewardene 2001; Grover 1998; Hemminki 1991; Liu 1996; Mukhopadhyay 2004; Mumtaz 2000; Peña‐Rosas 2003; Pita Martin 1999; Quintero 2004; Ridwan 1996; Robinson 1998; Rukhsana 2006; Winichagoon 2003; Yecta 2011; Young 2000; Yu 1998; Zamani 2008). (Daily versus intermittent oral iron regimens in pregnancy are examined in a related Cochrane review (Peña‐Rosas 2012a)).
In seven trials different types of administration were compared (for example, intravenous iron versus oral supplements) (Bencaiova 2007; Kumar 2005; Sinha 2011; Sood 1979; Swain 2011; Wali 2002; Zutschi 2004).
In two trials both groups received iron and one group received an additional intervention such as education (Adhikari 2009; Sachdeva 1993).
The second most frequent reason for exclusion was that the studies were not prospective, parallel, randomised controlled trials. A total of 20 trials were excluded for this reason (Abel 2000; Angeles‐Agdeppa 2003; Berger 2003; Chawla 1995; Dawson 1962; Edgar 1956; Gopalan 2004; Iyengar 1970; Kulkarni 2010; Menon 1962; Morgan 1961; Ortega‐Soler 1998; Osifo 1970; Powers 1985; Roztocil 1994; Sandstad 2003; Schoorl 2012; Tange 1993; Wu 1998; Young 2010).
The remaining studies were excluded for other reasons: the studies by Bergsjo 1987 and Steer 1992 were not completed, and results are not available for the Hawkins 1987 trial; studies by Hermsdorf 1986, Tampakoudis 1996 and Tan 1995 were reported as abstracts and there was insufficient information on methods to allow us to assess risk of bias; Cook 1990, Khambalia 2009 and Picha 1975 did not examine iron supplementation in pregnant women; and Hampel 1974 recruited women, and reported outcomes at different gestational ages so we were unable to interpret results; Bokhari 2011 and McKenna 2002 looked at iron fortified food or drink; in the study from Khambalia 2009 the iron and folic acid were delivered as point‐of‐use fortification of foods (Sprinkles®); and finally, Blot 1980 and Seck 2008 examined comparisons outside the scope of this review.
Risk of bias in included studies
See the 'Risk of bias' tables included in Characteristics of included studies for an assessment of the risk of bias for each included trial and Figure 2 and Figure 3 for an overall summary of the methodological quality of all included trials. In the description below we have summarised risk of bias only for those 44 trials contributing outcome data to the review.
2.
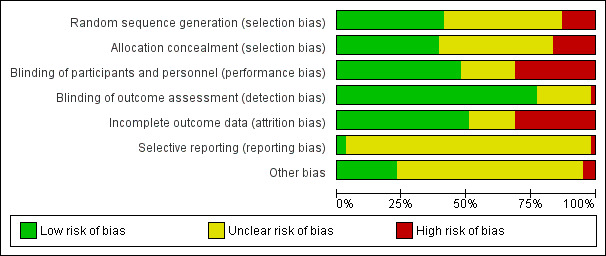
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
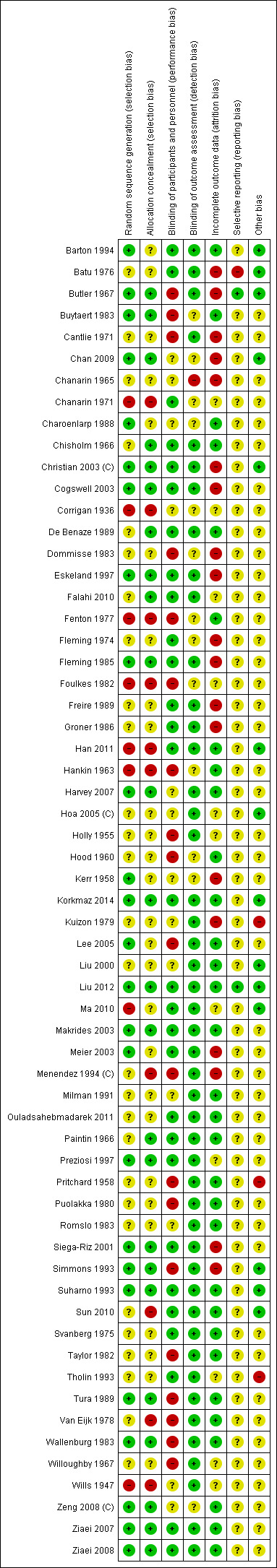
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
In the 'Summary of findings' tables we examined risk of bias for each outcome separately, considering only those trials contributing data for each primary outcome.
Allocation
Sequence generation
We assessed 21 trials as having adequate methods for generating the randomisation sequence (Barton 1994; Buytaert 1983; Chan 2009; Charoenlarp 1988; Christian 2003 (C); Cogswell 2003; Eskeland 1997; Harvey 2007; Kerr 1958; Korkmaz 2014; Lee 2005; Liu 2012; Makrides 2003; Meier 2003; Preziosi 1997; Siega‐Riz 2001; Tura 1989; Wallenburg 1983; Zeng 2008 (C); Ziaei 2007; Ziaei 2008). Eighteen trials did not report or did not state clearly the randomisation method used (Batu 1976; Cantlie 1971; Chisholm 1966; De Benaze 1989; Falahi 2010; Holly 1955; Hood 1960; Menendez 1994 (C); Milman 1991; Ouladsahebmadarek 2011; Paintin 1966; Pritchard 1958; Puolakka 1980; Romslo 1983; Svanberg 1975; Taylor 1982; Van Eijk 1978; Willoughby 1967). Four trials were quasi‐randomised using alternate sequence allocation (Chanarin 1971; Corrigan 1936; Hankin 1963; Wills 1947).
In three of these trials clusters rather than individual women were randomised (Christian 2003 (C); Menendez 1994 (C); Zeng 2008 (C)).
Allocation concealment
We judged that 20 trials had adequate methods of allocation concealment (Buytaert 1983; Chan 2009; Chisholm 1966; Christian 2003 (C); Cogswell 2003; De Benaze 1989; Eskeland 1997; Falahi 2010; Harvey 2007; Korkmaz 2014; Liu 2012; Makrides 2003; Paintin 1966; Preziosi 1997; Siega‐Riz 2001; Tura 1989; Wallenburg 1983; Zeng 2008 (C); Ziaei 2007; Ziaei 2008). The method of concealing allocation used in the remaining trials was unclear (Barton 1994; Batu 1976; Cantlie 1971; Charoenlarp 1988; Holly 1955; Hood 1960; Kerr 1958; Liu 2000; Lee 2005; Meier 2003; Milman 1991; Ouladsahebmadarek 2011; Pritchard 1958; Puolakka 1980; Romslo 1983; Svanberg 1975; Taylor 1982; Willoughby 1967). Some trials used an inadequate method or did not use any allocation concealment at all (Chanarin 1971; Corrigan 1936; Hankin 1963; Liu 2000; Menendez 1994 (C); Van Eijk 1978; Wills 1947).
Blinding
Blinding of participants, staff (performance bias)
Investigators in 20 trials attempted to blind participants and staff by using placebos of similar appearance to active treatment or coded or opaque bottles (Barton 1994; Batu 1976; Chanarin 1971; Chisholm 1966; Christian 2003 (C); Cogswell 2003; De Benaze 1989; Eskeland 1997; Falahi 2010; Korkmaz 2014; Liu 2012; Makrides 2003; Meier 2003; Ouladsahebmadarek 2011; Paintin 1966; Preziosi 1997; Siega‐Riz 2001; Svanberg 1975; Ziaei 2007; Ziaei 2008). In the remaining trials, blinding was either not mentioned or not attempted, or we were not clear whether or not attempted blinding would be convincing to women and or staff (e.g. where placebo and active treatment were not identical).
Blinding of outcome assessors (detection bias)
The majority of the trials (34) were assessed as being at low risk of bias for detection bias, this was irrespective of whether or not a placebo was provided as we judged that for most outcomes (e.g. Hb level or iron‐deficiency anaemia), the fact that there was no blinding of women or staff providing care was unlikely to impact on these sorts of laboratory outcomes. In nine cases we were not clear whether lack of blinding could lead to bias (Buytaert 1983; Chan 2009; Chanarin 1971; Charoenlarp 1988; Corrigan 1936; Hankin 1963; Hood 1960; Kerr 1958; Zeng 2008 (C)). This was because in some cases lack of blinding may have led to a change in clinical management of some women (e.g. women who developed anaemia were identified and withdrawn from trials or received additional treatment), or we thought that only certain outcomes would be blinded and others would not be (e.g. where those staff providing an unmasked intervention also collected data on side effects).
Incomplete outcome data
We judged that trials with more than 20% loss to follow‐up, or with imbalanced loss to follow‐up in different arms of trials were inadequate in terms of completeness of outcome data. Ten trials were assessed as having high levels of attrition, or loss was not balanced across groups and may have occurred for reasons associated with treatment (for example, if women were withdrawn from trials if they experienced side effects) (Batu 1976; Cantlie 1971; Chan 2009; Christian 2003 (C); Cogswell 2003; Eskeland 1997; Kerr 1958; Meier 2003; Menendez 1994 (C); Siega‐Riz 2001).
Selective reporting
We did not formally assess outcome reporting bias; for most of the included trials we did not have access to study protocols and assessing outcome reporting bias from published reports alone can be difficult. However, we have noted in the Characteristics of included studies tables where we suspected a problem relating to outcome reporting. Although for most outcomes too few studies contributed data to allow us to examine possible publication bias through generating funnel plots, in the data and analyses tables and in the forest plots, we have arranged studies by weight to allow us to visually examine plots to decide whether there is any evidence of a greater effect size in smaller studies.
Other potential sources of bias
We have noted other concerns about studies in the notes and other 'Risk of bias' sections of the Characteristics of included studies tables.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
In this review we have included data from 44 trials, involving 43,274 women although in trials that included more than two treatment arms, we may not have included all arms in our analyses. We have organised the summary of results by supplementation regimens compared, and by primary and secondary outcomes. Most of the included studies focused on haematological indices and few reported on any of the other outcomes prespecified in the review protocol. Many of the findings showed heterogeneity that could not be explained by standard sensitivity analyses including quality assessment, and so we used a random‐effects model to analyse the results. All results therefore represent the average treatment effect. Using random‐effects means that for many outcomes the width of the 95% CIs is increased compared with using a fixed‐effect model.
See the Data and analyses section for detailed results on primary and secondary outcomes.
For each comparison we have indicated the number of studies contributing data to that comparison. Some studies, with more than two treatment arms are included in more than one comparison. For most outcomes only a relatively small proportion of studies included in the comparison reported data; for some outcomes a single study reported results; for this reason we have indicated for each outcome the number of studies contributing data and the number of women included in those studies. For those outcomes including data from cluster‐randomised trials the number included is the effective sample size; that is, sample sizes and event rates have been adjusted for cluster‐trials to take account of the design effect.
(1) Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo) (44 studies)
Infant outcomes
Low birthweight (less than 2500 g)
Overall, iron supplements reduced the prevalence of low birthweight (less than 2500 g) although using random‐effects analysis the difference between groups did not reach statistical significance. Among 17,613 women in 11 trials, 8.4% of those who took daily iron supplementation during pregnancy had a baby with birthweight below 2500 g versus 10.2% of those who received no iron or placebo (average risk ratio (RR) 0.84; 95% confidence interval (CI) 0.69 to 1.03, evidence assessed as low quality) (Analysis 1.1). There was no clear evidence of differences between subgroups (Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5), or obvious funnel plot asymmetry (Figure 4).
1.1. Analysis.
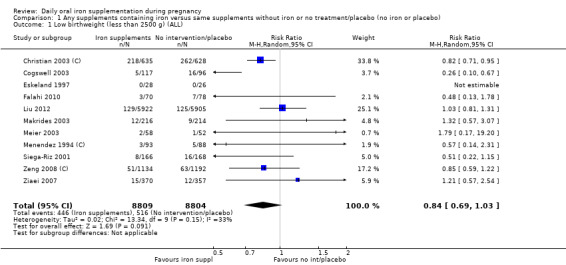
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 1 Low birthweight (less than 2500 g) (ALL).
1.2. Analysis.
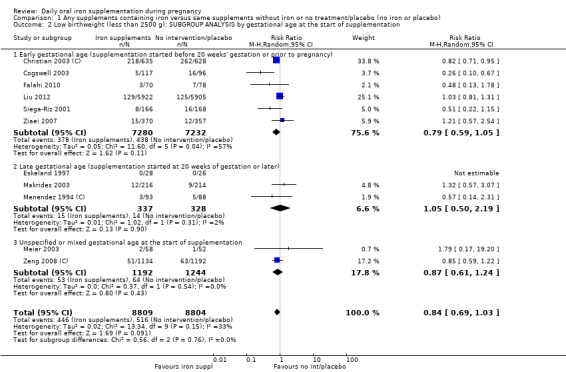
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.3. Analysis.
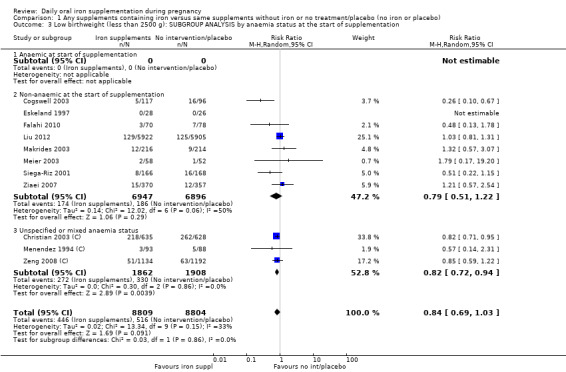
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.4. Analysis.
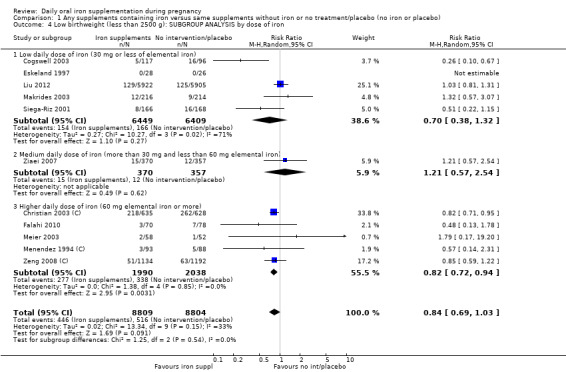
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron.
1.5. Analysis.
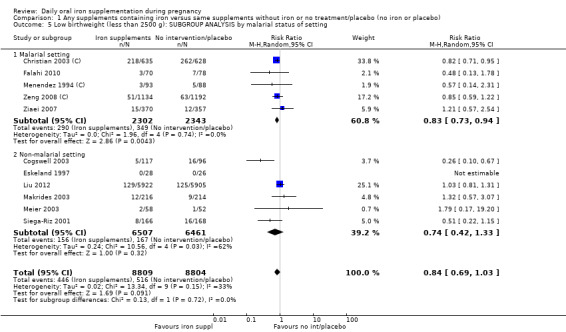
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting.
4.
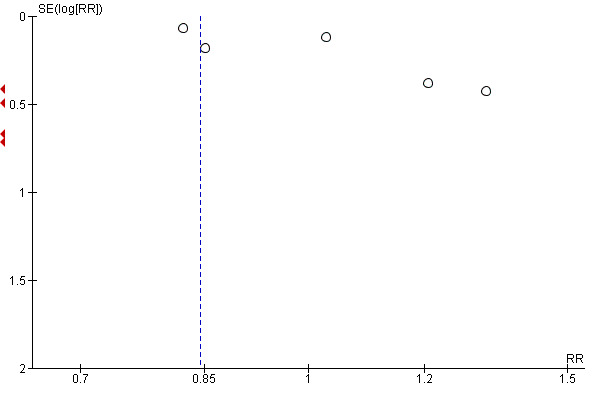
Funnel plot of comparison: 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), outcome: 1.1 Low birthweight (less than 2500 g) (ALL).
Birthweight (g)
Among infants born to 18,590 participants in 15 trials, women receiving supplements had slightly heavier newborns compared with women in the control group, but the difference between groups was not statistically significant. The mean difference (MD) in birthweight between those whose mothers had taken iron supplements and those whose mothers had not was 23.75 g (95% CI ‐3.02 to 50.51, moderate quality evidence) (Analysis 1.6). We did not find evidence of subgroup differences (Analysis 1.7; Analysis 1.8; Analysis 1.9; Analysis 1.10), or obvious funnel plot asymmetry (Figure 5).
1.6. Analysis.
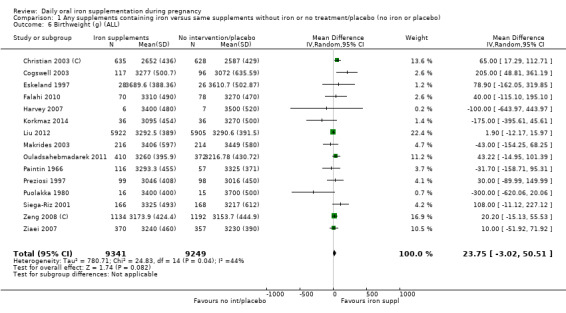
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 6 Birthweight (g) (ALL).
1.7. Analysis.
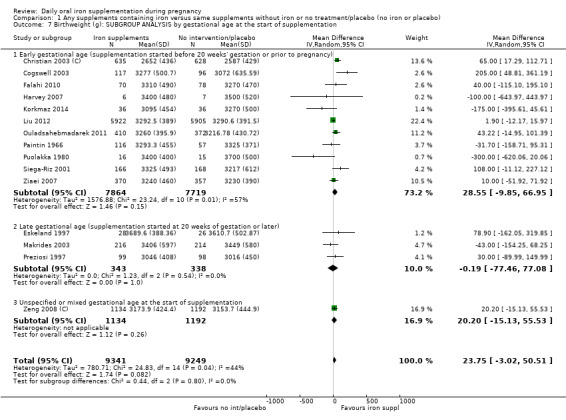
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.8. Analysis.
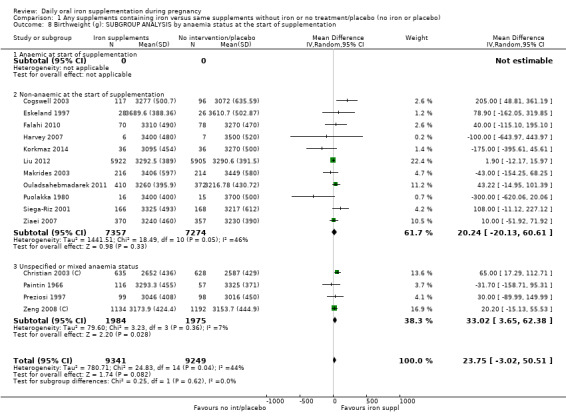
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.9. Analysis.
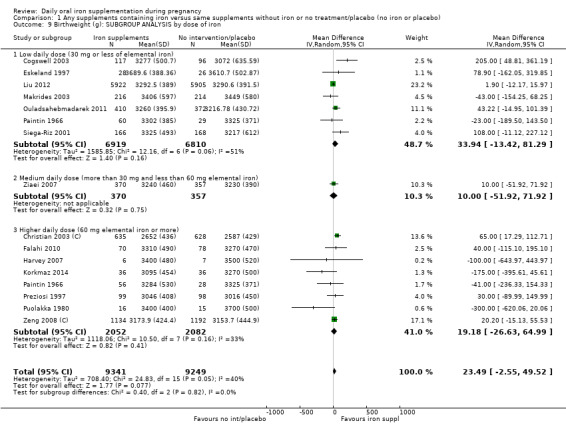
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron.
1.10. Analysis.
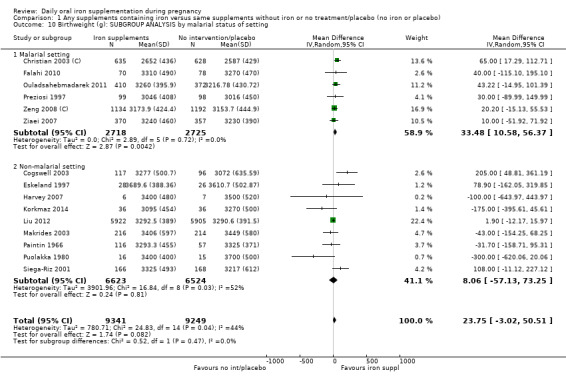
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting.
5.
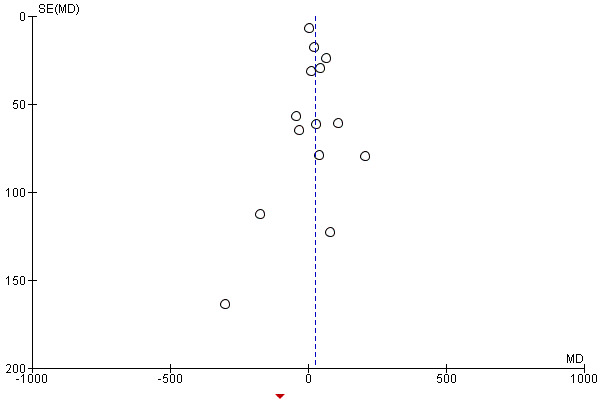
Funnel plot of comparison: 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), outcome: 1.6 Birthweight (g) (ALL).
Preterm birth (less than 37 weeks' gestation)
Thirteen trials with 19,286 women provided data on preterm birth (before 37 week's gestation); while women receiving iron supplements were less likely to experience premature delivery the difference between groups did not reach statistical significance (average RR 0.93; 95% CI 0.84 to 1.03, moderate quality evidence).There was no clear evidence of differences between subgroups (Analysis 1.12; Analysis 1.13; Analysis 1.14; Analysis 1.15). Visual inspection of the funnel plot for this outcome suggested that smaller studies tended to report more pronounced treatment effects (Figure 6).
1.12. Analysis.
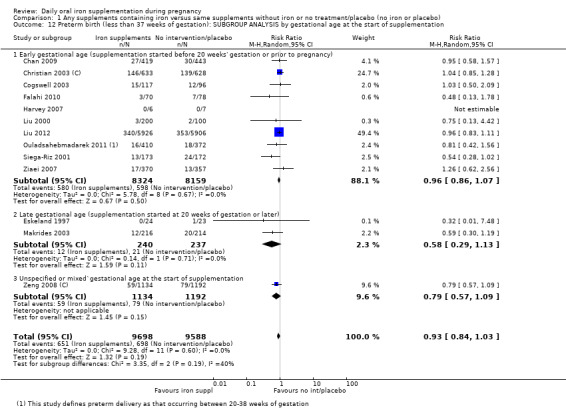
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 12 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.13. Analysis.
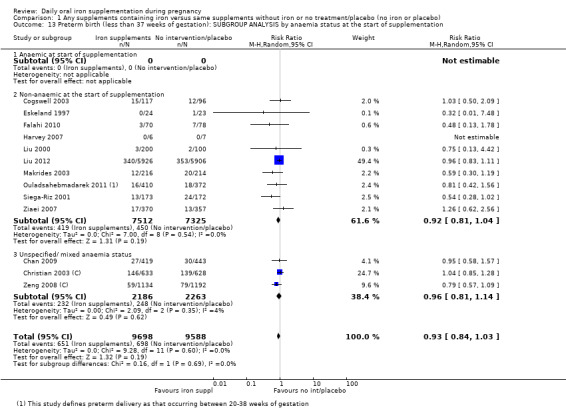
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 13 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.14. Analysis.
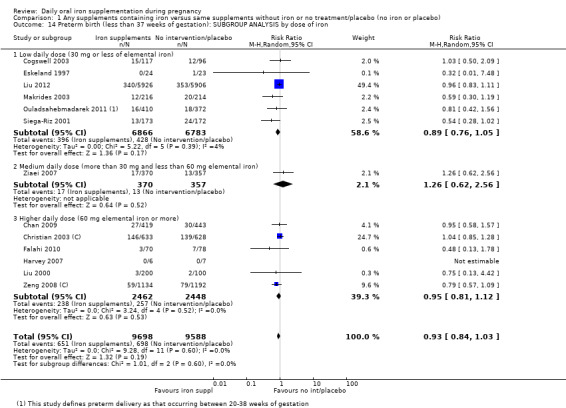
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 14 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron.
1.15. Analysis.
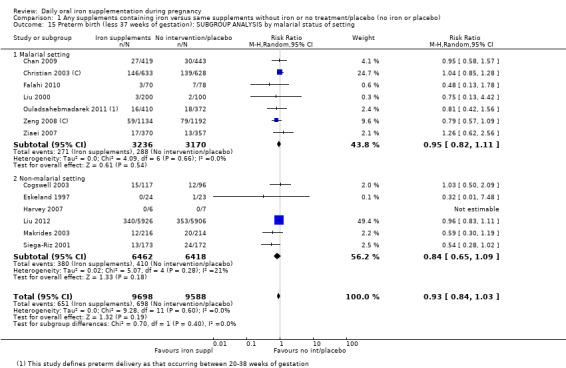
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting.
6.
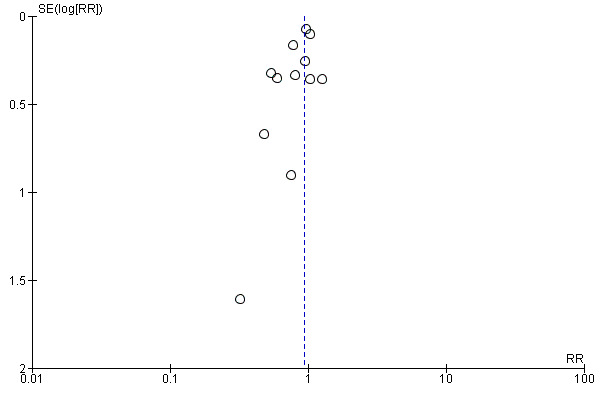
Funnel plot of comparison: 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), outcome: 1.11 Preterm birth (less than 37 weeks of gestation) (ALL).
Neonatal death
Four studies with 16,603 participants reported neonatal mortality and there was no clear evidence of any difference between groups (average RR 0.91; 95% CI 0.71 to 1.18, low quality evidence) (Analysis 1.16). We did not find evidence of subgroup differences for this outcome (Analysis 1.17; Analysis 1.18; Analysis 1.19; Analysis 1.20).
1.16. Analysis.
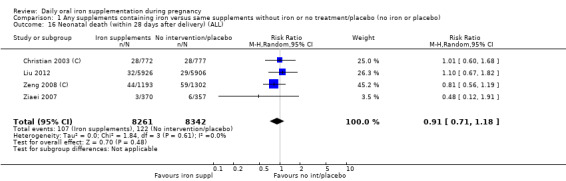
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 16 Neonatal death (within 28 days after delivery) (ALL).
1.17. Analysis.
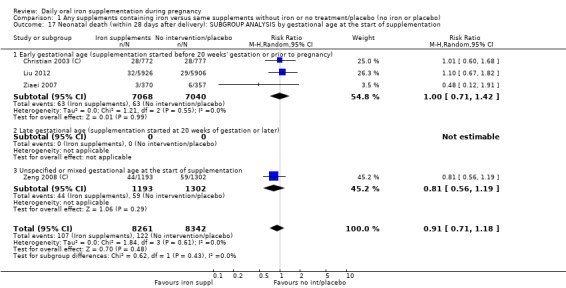
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 17 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.18. Analysis.
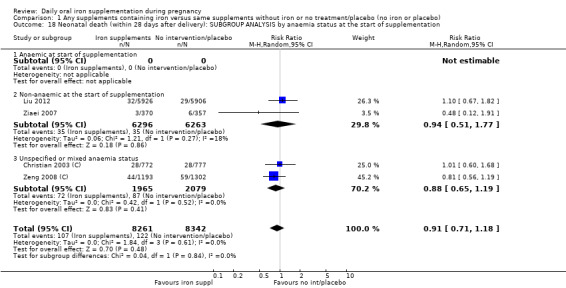
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 18 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.19. Analysis.
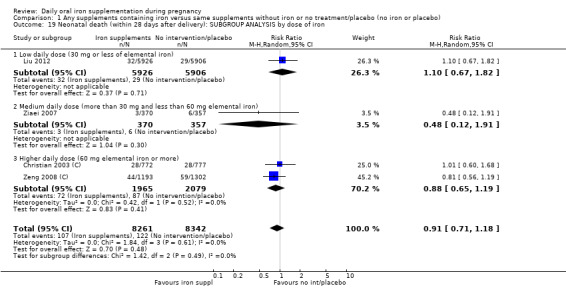
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 19 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron.
1.20. Analysis.
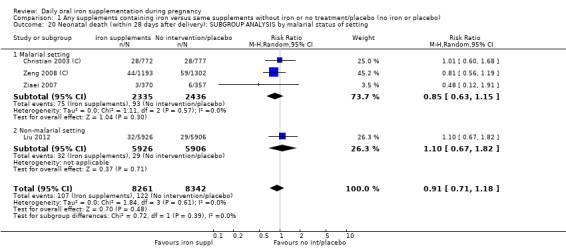
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 20 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting.
Congenital anomalies
Four studies with 14,636 women reported the number of infants with congenital anomalies; there was no clear evidence of any difference between groups (average RR 0.88; 95% CI 0.58 to 1.33) (Analysis 1.21).
1.21. Analysis.
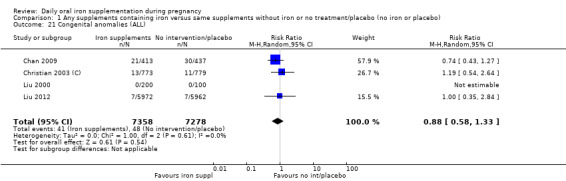
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 21 Congenital anomalies (ALL).
Maternal primary outcomes
Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more)
Among 2199 women in 14 trials (Batu 1976; Chanarin 1971; Chisholm 1966; Cogswell 2003; De Benaze 1989; Eskeland 1997; Holly 1955; Liu 2000; Makrides 2003; Milman 1991; Preziosi 1997; Pritchard 1958; Puolakka 1980; Romslo 1983), 13.06% of those who received daily iron supplements during pregnancy had anaemia at term in comparison with 35.71% who did not receive iron (average RR 0.30; 95% CI 0.19 to 0.46, low quality evidence) (Analysis 1.26). However, because the heterogeneity in study results was substantial our results have to be interpreted with caution (heterogeneity: Tau² = 0.40, I² = 80%, Chi² test for heterogeneity P < 0.00001. We did not find any differences between subgroups in most of the subgroup analyses (Analysis 1.27; Analysis 1.28; Analysis 1.29; Analysis 1.30), although the treatment effect appeared more pronounced in non‐malarial settings (Analysis 1.30: Test for subgroup differences: Chi² = 11.85, df = 1 (P = 0.0006), I² = 91.6%). Visual inspection of the funnel plot for this outcome suggested that the treatment effect was more pronounced in smaller studies (not shown) although we did not downgrade for publication bias.
1.26. Analysis.
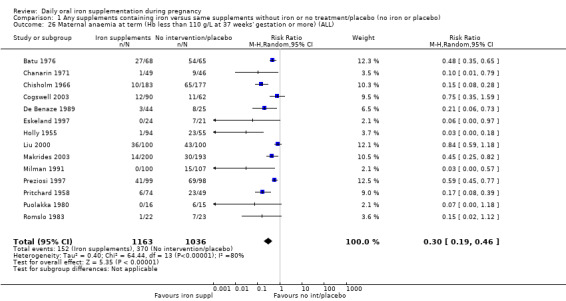
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 26 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL).
1.27. Analysis.
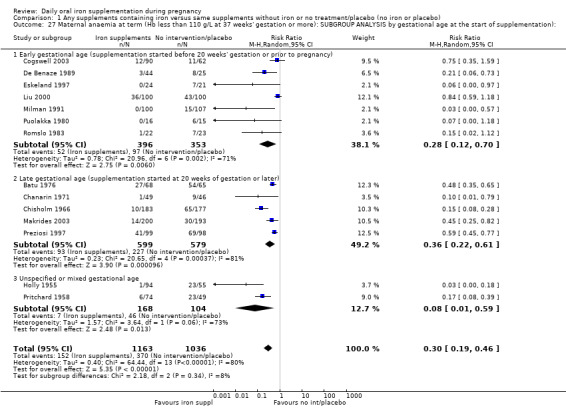
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 27 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation):.
1.28. Analysis.
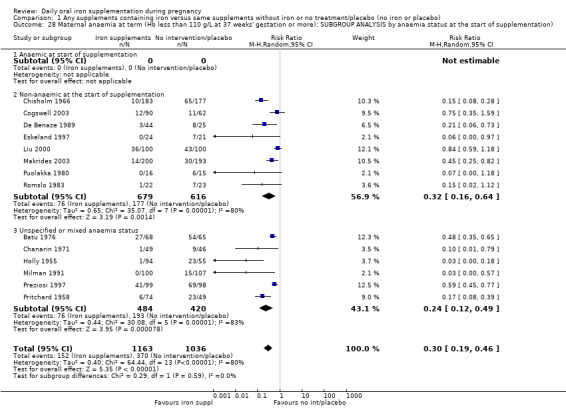
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 28 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation).
1.29. Analysis.
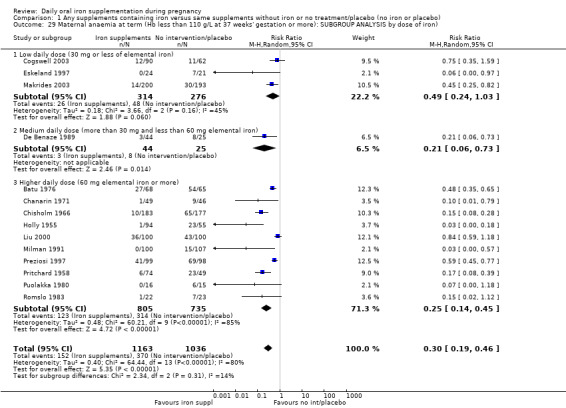
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 29 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron).
1.30. Analysis.
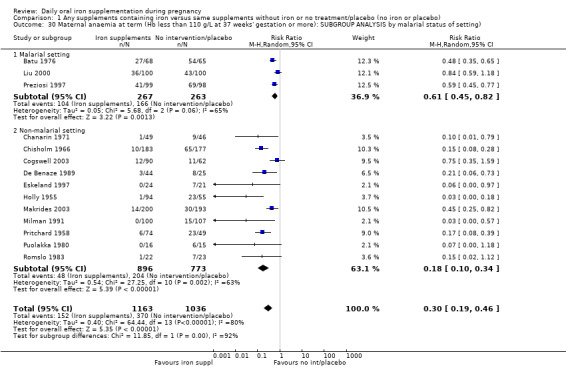
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 30 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting).
Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more)
Seven studies (1256 women) reported data for this outcome, with women in groups receiving iron as part of supplements being less likely to have iron deficiency at term (average RR 0.43; 95% CI 0.27 to 0.66, low quality evidence) (Analysis 1.31). Subgroup analyses suggested that mixed or unspecified anaemia status at the start of supplementation and higher doses of iron were associated with more pronounced treatment effects (test for subgroup differences: Chi² = 10.96, df = 1 (P = 0.0009), I² = 90%, and, Chi² = 19.52, df = 2 (P = 0.0001), I² = 89%, respectively) (Analysis 1.33; Analysis 1.34).
1.31. Analysis.
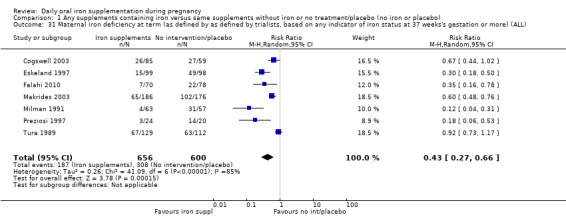
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 31 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks's gestation or more) (ALL).
1.33. Analysis.
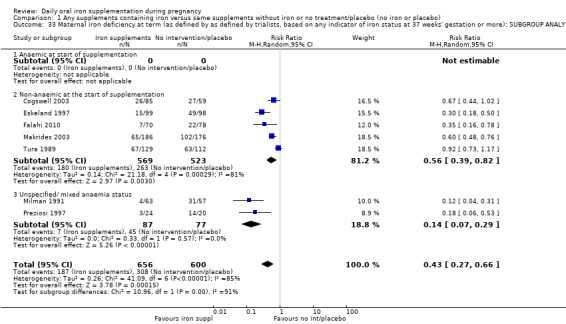
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 33 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.34. Analysis.
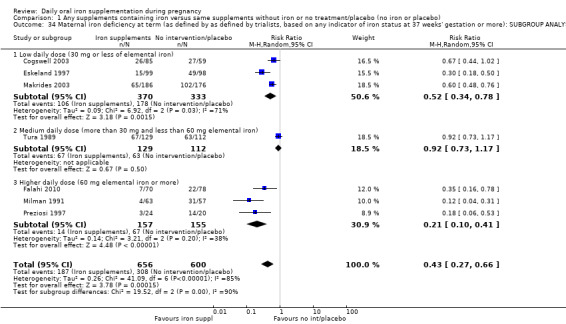
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 34 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
Maternal iron‐deficiency anaemia at term (Hb below 110 g/L and at least one additional laboratory indicator at 37 weeks' gestation or more)
Data from six trials involving 1088 women showed that 4.4% of women who received daily iron supplements and 13.2% of those who did not had iron‐deficiency anaemia at term (average RR 0.33; 95% CI 0.16 to 0.69). We did not find evidence of differences between subgroups (Analysis 1.37; Analysis 1.38; Analysis 1.39; Analysis 1.40).
1.37. Analysis.
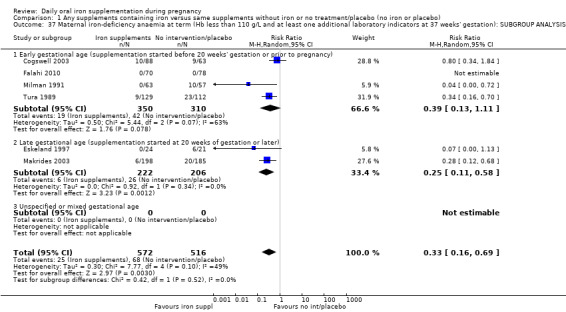
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 37 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.38. Analysis.
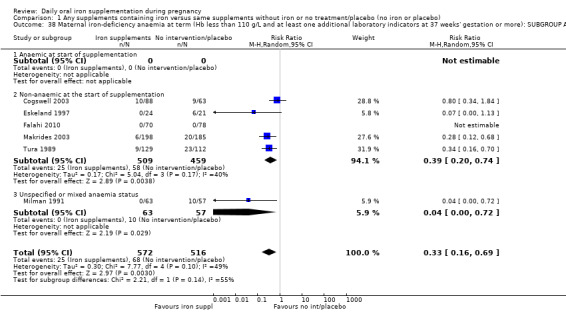
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 38 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.39. Analysis.
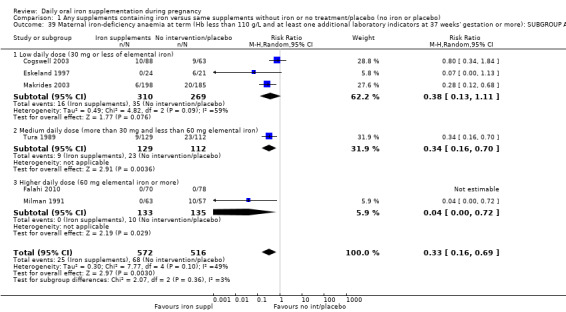
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 39 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
1.40. Analysis.
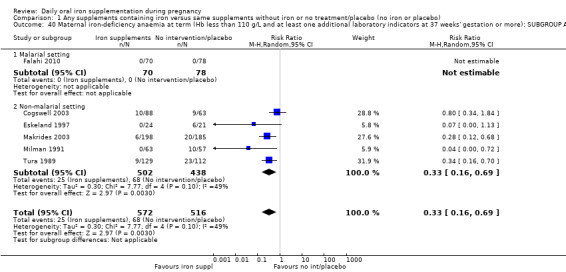
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 40 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
Maternal death
In two studies including 12,560 women, there was no clear difference between groups for maternal mortality (average RR 0.33; 95% CI 0.01 to 8.19, very low quality evidence) (Analysis 1.41).
1.41. Analysis.
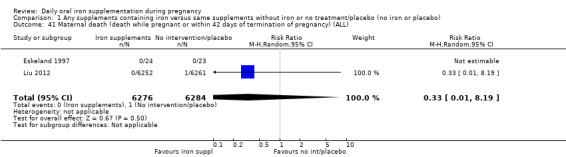
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 41 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL).
Side effects (any)
Data from 11 trials involving 2423 women suggest that there was no clear difference between groups receiving iron and those receiving placebo or no iron for reporting side effects (25.3% versus 9.91% reporting side effects respectively; average RR 1.29; 95% CI 0.83 to 2.02) (Analysis 1.42). However, the heterogeneity between the treatment effects is substantial and the results have to be interpreted with caution (heterogeneity: T2 = 0.30, I = 81%, Chi test for heterogeneity P < 0.00001). There were no clear subgroup differences (Analysis 1.43; Analysis 1.44; Analysis 1.45; Analysis 1.46). There was no obvious funnel plot asymmetry for this outcome (not shown).
1.42. Analysis.
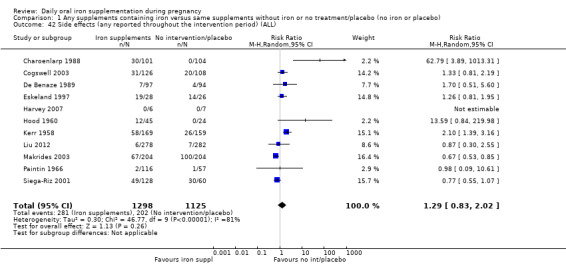
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 42 Side effects (any reported throughout the intervention period) (ALL).
1.43. Analysis.
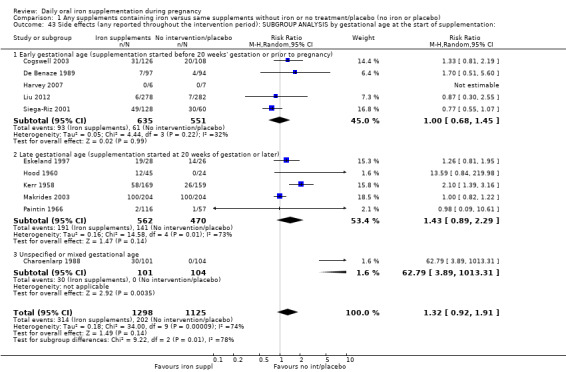
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 43 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by gestational age at the start of supplementation:.
1.44. Analysis.
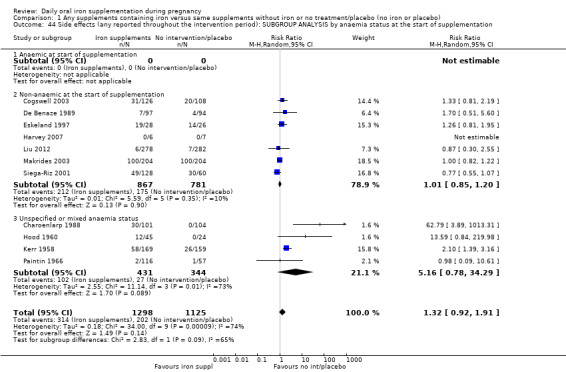
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 44 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.45. Analysis.
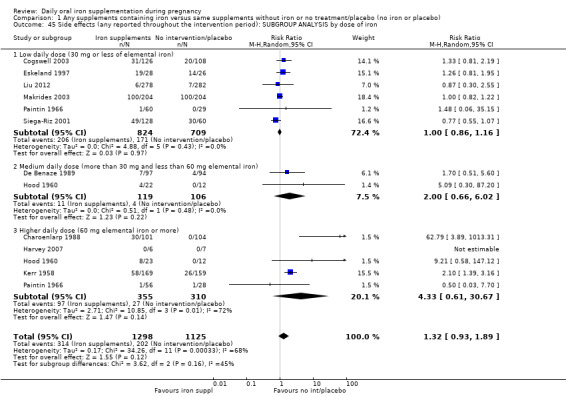
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 45 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by dose of iron.
1.46. Analysis.
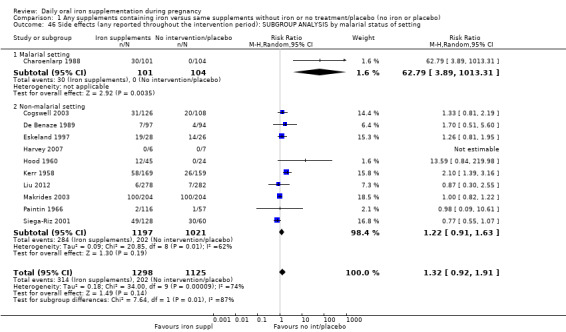
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 46 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by malarial status of setting.
Severe (Hb < 70/L) anaemia at any time during the second or third trimester
Nine trials with 2125 women reported results for this outcome, but estimable data were available for only three trials involving 786 women; this showed that women who received iron supplements were as likely to become severely anaemic during second and third trimesters (average RR 0.22; 95% CI 0.01 to 3.20, very low quality evidence). In many cases, women who became anaemic were treated and excluded from the analysis in the trials, independently of the group assigned, so very few cases became severely anaemic. As only three trials contributed estimable data, this result and the associated subgroup analysis have to be interpreted with caution.
Other maternal primary outcomes
In one study (727 women), there was no clear difference in infection during pregnancy (Analysis 1.53), low quality evidence.
1.53. Analysis.
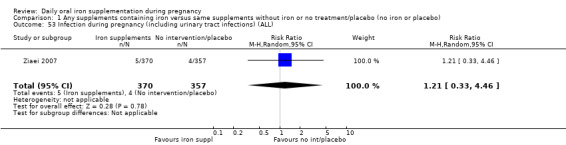
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 53 Infection during pregnancy (including urinary tract infections) (ALL).
Two studies reported on placental malaria and parasitaemia (Fleming 1985; Menendez 1994 (C)) and found no differences between groups.
Infant secondary outcomes
Very premature birth (less than 34 weeks' gestation)
This outcome was reported in five trials with 3743 women; results suggest that babies born to mothers receiving iron were less likely to be born before 34 weeks' gestation (average RR 0.51; 95% CI 0.29 to 0.91) (Analysis 1.59).
1.59. Analysis.
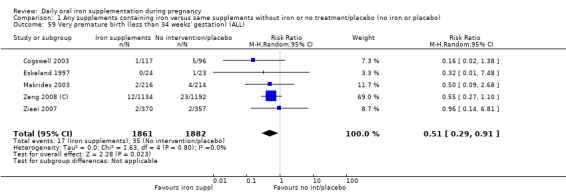
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 59 Very premature birth (less than 34 weeks' gestation) (ALL).
Infant ferritin concentration at six months in μg/L
This outcome was measured in a single study with 197 participants; at six months the MD was 11.00 (95% CI 4.37 to 17.63) (Analysis 1.61).
1.61. Analysis.
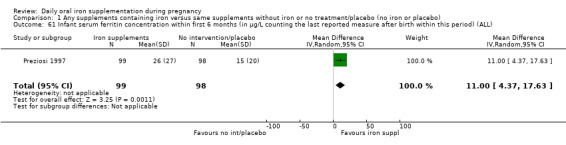
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 61 Infant serum ferritin concentration within first 6 months (in μg/L counting the last reported measure after birth within this period) (ALL).
Other infant secondary outcomes
There was no evidence of statistically significant differences between groups for the following infant secondary outcomes: very low birthweight; low Apgar score at five minutes; mean infant Hb levels at three and six months; admission to special care; head circumference at birth; and stunting at long‐term follow‐up.
No trials reported on the remaining prespecified infant secondary outcomes such as infant anaemia or infant iron‐deficiency anaemia at birth or soon after.
Maternal secondary outcomes
Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) and within six weeks postpartum period (in g/L)
Haemoglobin concentration at or near term was reported in 19 studies, involving 3704 participants. There were high levels of heterogeneity for this outcome and results should be interpreted with caution. Women who received iron were on average likely to have higher Hb levels at term (MD 8.88 g/L; 95% CI 6.96 to 10.80) (heterogeneity: Tau² = 13.92, I² = 87%, Chi² test for heterogeneity P < 0.00001) (Analysis 1.66).
1.66. Analysis.
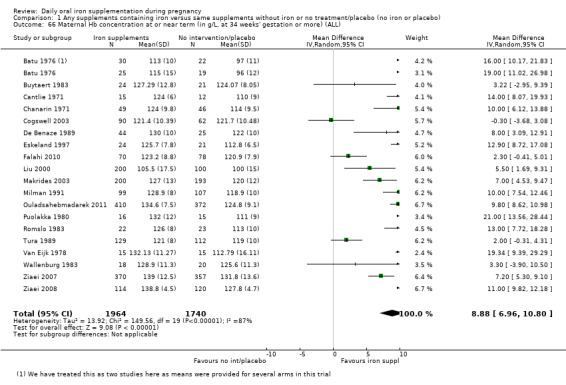
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 66 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL).
At six weeks postpartum, the difference between groups remained significant with women receiving iron as part of supplements having higher Hb levels (MD 7.61; 95% CI 5.50 to 9.72; reported in seven studies with 956 women) (heterogeneity: Tau² = 3.09, I² = 40%, Chi² test for heterogeneity P = 0.12) (Analysis 1.67).
1.67. Analysis.
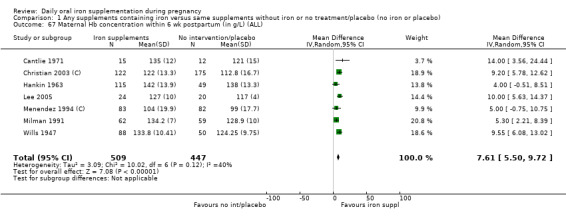
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 67 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL).
Maternal high Hb concentrations (Hb greater than 130 g/L) at any time during second or third trimester
There was evidence from nine studies (2188 women) with estimable data that high Hb concentrations were more likely in the second and third trimesters in women who had received iron as part of supplements (average RR 2.37; 95% CI 1.34 to 4.21). There was high heterogeneity for this outcome ( heterogeneity: Tau² = 0.57, I² = 89%, Chi² test for heterogeneity P < 0.00001 ) (Analysis 1.68).
1.68. Analysis.
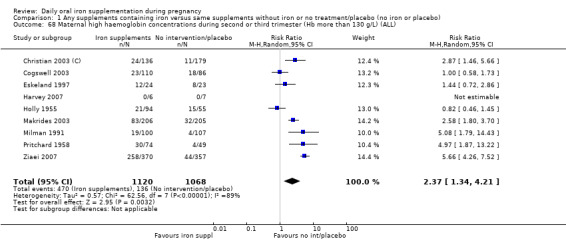
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 68 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL).
Maternal high Hb concentrations at term (defined as Hb greater than 130 g/L at 37 weeks' gestation or more)
Women who received iron were at higher risk of haemoconcentration at term (average RR 3.07; 95% CI 1.18 to 8.02; reported in eight studies 2156 women). Again, there was high heterogeneity for this outcome and results should be interpreted cautiously (heterogeneity: Tau² = 1.34, I² = 96%, Chi² test for heterogeneity P < 0.00001, 95% PI 0.19 to 39.15) (Analysis 1.69).
1.69. Analysis.
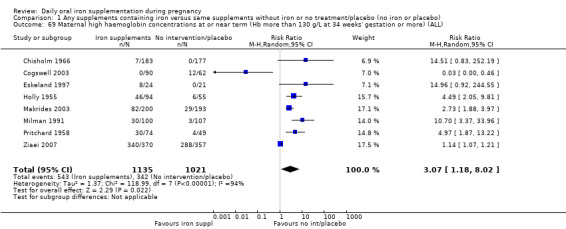
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 69 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL).
Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more)
Data from eight trials involving 1819 women reported results for this outcome; in six trials no cases of severe anaemia were identified, so only two trials with 494 women contributed estimable data. Results from these two trials showed no significant difference between women who receive iron or not (average RR 0.47; 95% CI 0.01 to 44.11) (Analysis 1.70).
1.70. Analysis.
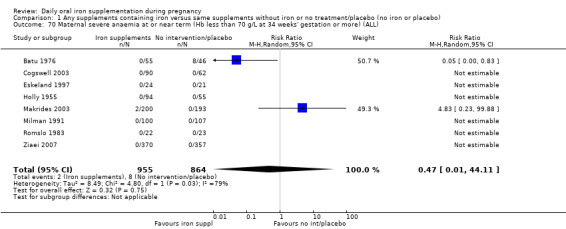
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 70 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL).
Severe anaemia at postpartum (Hb less than 80 g/L)
While eight trials reported severe anaemia in the postnatal period only two studies with estimable data for 553 women contributed to this analysis; women receiving iron as part of supplements were less at risk of severe anaemia in the weeks after the birth (average RR 0.04; 95% CI 0.01 to 0.28) (Analysis 1.71).
1.71. Analysis.
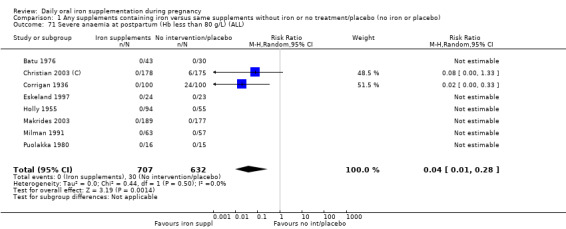
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 71 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL).
Transfusion provided
The number of women receiving transfusions was reported in two studies (759 participants), with no apparent difference between groups (average RR 0.96; 95% CI 0.10 to 8.98) (Analysis 1.76).
1.76. Analysis.
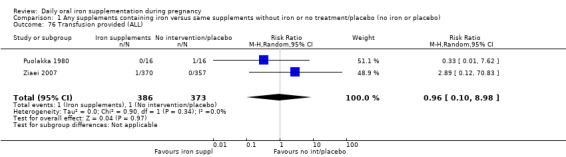
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 76 Transfusion provided (ALL).
Puerperal infection
There was a statistically significant difference between groups in the number of women reported to have puerperal infection; with women receiving iron being at reduced risk, (four studies, 4374 participants) (average RR 0.68; 95% CI 0.50 to 0.92) (Analysis 1.73).
1.73. Analysis.
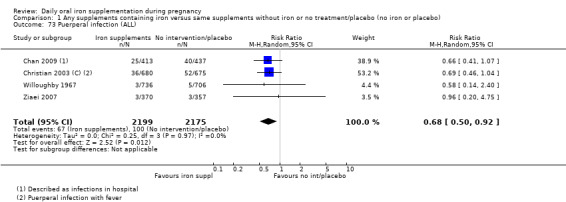
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 73 Puerperal infection (ALL).
Other secondary outcomes
There was no statistically significant evidence of differences between groups for the following secondary outcomes: ante‐ or postpartum haemorrhage, individual side effects, maternal well being, placental abruption, preterm rupture of the membranes, pre‐eclampsia and moderate anaemia in the postpartum period. Several of these outcomes were reported in only a small number of studies.
No trials reported on the remaining prespecified secondary outcomes.
(2) Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo) (eight studies)
Infant primary outcomes
Low birthweight (less than 2500 g)
Two trials with 1311 participants examined this outcome (Christian 2003 (C); Taylor 1982). There was no clear evidence of significant differences between infants of women receiving daily iron + folic acid supplementation versus no supplements (average RR 1.07; 95% CI 0.31 to 3.74, low quality evidence) (Analysis 2.1). Data from the same two trials suggest that infant birthweight was higher in the supplemented group (MD 57.73; 95% CI 7.66 to 107.79, moderate quality evidence) (Analysis 2.8).
2.1. Analysis.
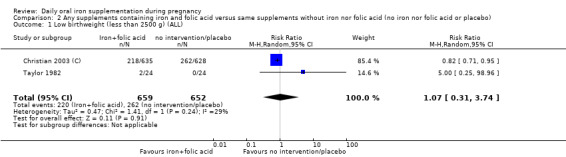
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 1 Low birthweight (less than 2500 g) (ALL).
2.8. Analysis.
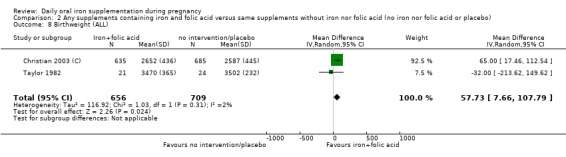
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 8 Birthweight (ALL).
Preterm birth (less than 37 weeks' gestation)
Three studies with 1497 women examined this outcome (Christian 2003 (C); Lee 2005; Taylor 1982). We found no evidence of differences in the numbers experiencing preterm birth between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (average RR 1.55; 95% CI 0.40 to 6.00, low quality evidence). Only one of these trials met the criteria for high quality (Christian 2003 (C)) (Analysis 2.3). There were no significant differences between subgroups (Analysis 2.4; Analysis 2.5; Analysis 2.6; Analysis 2.7).
2.3. Analysis.
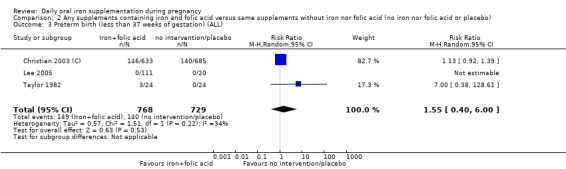
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 3 Preterm birth (less than 37 weeks of gestation) (ALL).
2.4. Analysis.
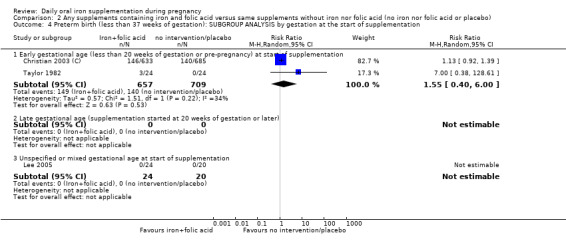
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 4 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestation at the start of supplementation.
2.5. Analysis.
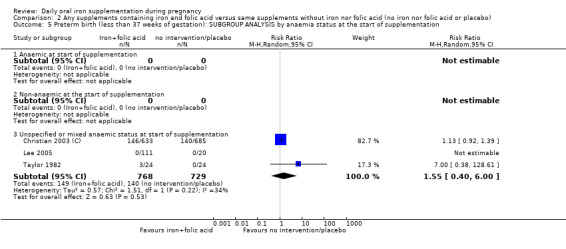
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 5 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
2.6. Analysis.
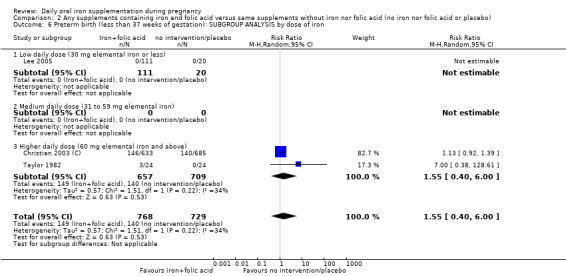
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 6 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron.
2.7. Analysis.
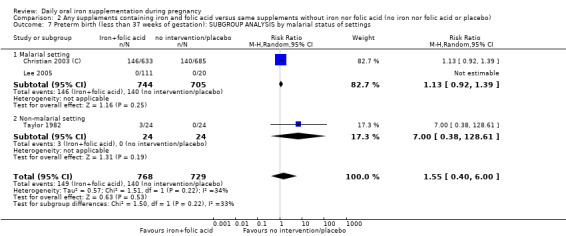
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 7 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of settings.
Neonatal death
Three studies (1793 participants) reported on this outcome (Barton 1994; Christian 2003 (C); Taylor 1982); there were a total of 69 perinatal deaths, and no clear evidence of any difference between groups (average RR 0.81; 95% CI 0.51 to 1.30, low quality evidence) (Analysis 2.2). No subgroup differences were apparent.
2.2. Analysis.
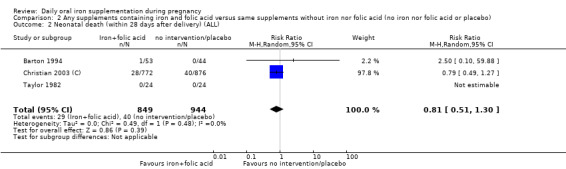
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 2 Neonatal death (within 28 days after delivery) (ALL).
Congenital anomalies
One study with 1652 women reported the number of infants with congenital anomalies; and there was no clear evidence of any difference between groups (RR 0.70; 95% CI 0.35 to 1.40), low quality evidence (Analysis 2.13).
2.13. Analysis.
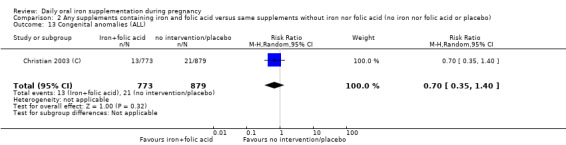
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 13 Congenital anomalies (ALL).
Maternal primary outcomes
Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more)
The data from three trials including 346 women (Barton 1994; Batu 1976; Chisholm 1966) suggest that women who routinely receive daily iron and folic acid supplementation during pregnancy are less likely to have anaemia at term than those not taking any iron and folic acid supplements at all (defined as Hb less than 110 g/L) (7.2% versus 28.3%; average RR 0.34; 95% CI 0.21 to 0.54, moderate quality evidence) (Analysis 2.14). Only one study with no estimable data met the prespecified criteria for high quality. We did not identify any differences between subgroups.
2.14. Analysis.
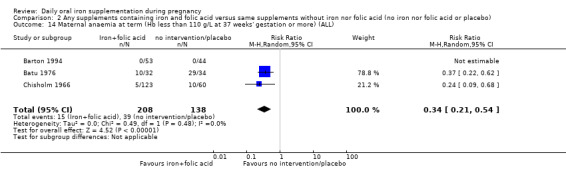
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 14 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL).
Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more)
Data from one trial involving 131 women (Lee 2005) suggest that women who routinely receive daily oral supplementation with iron are less likely to have iron deficiency at term than women taking placebo or not taking any iron and folic acid supplements at all although the difference between groups did not reach statistical significance (3.6% versus 15%; RR 0.24; 95% CI 0.06 to 0.99, low quality evidence) (Analysis 2.19).
2.19. Analysis.
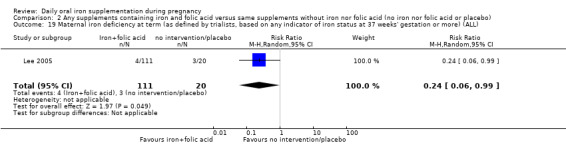
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 19 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL).
Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicator at 37 weeks' gestation or more)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo in the single trial including 131 women contributing data to this analysis (RR 0.43; 95% CI 0.17 to 1.09) (Analysis 2.20). The study contributing data did not meet prespecified criteria for high quality.
2.20. Analysis.
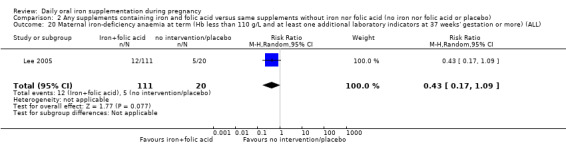
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 20 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL).
Side effects (any)
One trial including 456 women (Charoenlarp 1988) suggests that women routinely receiving iron and folic acid supplementation are more likely to report any side effects; none of those receiving no supplementation reported side effects, however, the CI is very broad for this finding (RR 44.32; 95% CI 2.77 to 709.09) (Analysis 2.22), moderate quality evidence. This trial did not meet criteria for high methodological quality.
2.22. Analysis.
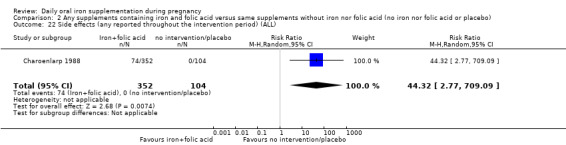
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 22 Side effects (any reported throughout the intervention period) (ALL).
Severe anaemia at any time during second and third trimester (Hb less than 70 g/L)
Four studies including 506 women had estimable data for this outcome; there was no evidence of a statistically significant difference between groups (RR 0.12; 95% CI 0.02 to 0.63, very low quality evidence) (Analysis 2.23).
2.23. Analysis.
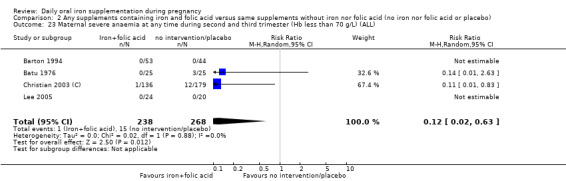
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 23 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL).
Other outcomes
One trial with 48 women reported on infection in pregnancy (Taylor 1982); there were four events in total, two in each group (Analysis 2.29), very low quality evidence. A single study reported on maternal deaths and there were no estimable data (Analysis 2.21), low quality evidence.
2.29. Analysis.
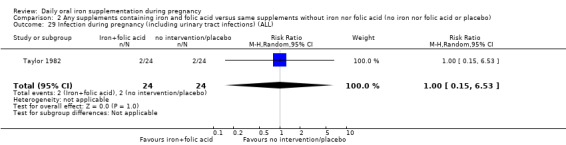
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 29 Infection during pregnancy (including urinary tract infections) (ALL).
2.21. Analysis.
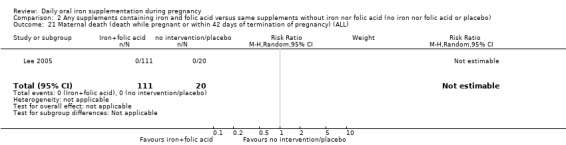
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 21 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL).
There were no data on the remaining prespecified primary outcomes.
Infant secondary outcomes
No evidence of significant differences was found between infants from these groups of women receiving daily iron + folic acid supplementation and those taking placebo or not taking any supplements at all in the following secondary outcomes: very low birthweight (less than 1500 g), very premature delivery, or admission to special care unit.
No trials reported on the remaining infant secondary outcomes.
Maternal secondary outcomes
Maternal Hb concentration at term (in g/L at 34 weeks' gestation or more)
The data from three trials including 140 women (Barton 1994; Batu 1976; Taylor 1982) suggest that women who routinely receive daily iron and folic acid supplementation reach term with higher Hb concentration than women taking placebo or not taking any iron and folic acid supplement at all (MD 16.13 g/L; 95% CI 12.74 to 19.52) (Analysis 2.36). The effect of iron‐folic acid supplementation was associated with higher Hb concentrations in the single high‐quality trial (MD 17.10; 95% CI 8.44 to 25.76) (Barton 1994).
2.36. Analysis.
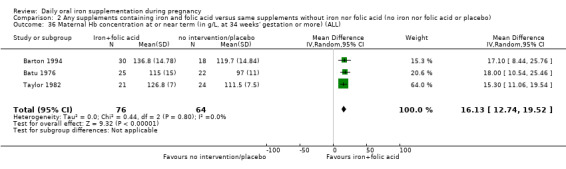
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 36 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL).
Maternal high Hb concentrations at term (defined as Hb greater than 130 g/L)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (Analysis 2.39).
2.39. Analysis.
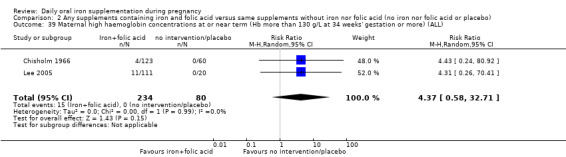
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 39 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL).
Maternal high Hb concentrations at any time during second or third trimesters (defined as Hb greater than 130 g/L)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (RR 1.78; 95% CI 0.63 to 5.04, two studies, 446 women) (Analysis 2.38).
2.38. Analysis.
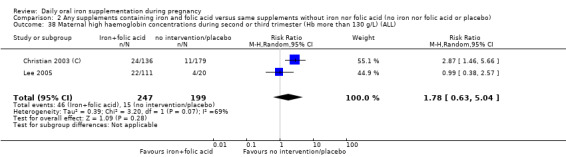
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 38 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL).
Maternal Hb concentration within six weeks postpartum in g/L
Two studies (Christian 2003 (C); Taylor 1982) involving 459 women reported this outcome. The data from these trials suggest that women receiving daily iron + folic acid supplementation achieve a higher concentration of Hb at one month postpartum than women not taking any supplements at all (MD 10.07; 95% CI 7.33 to 12.81) (Analysis 2.37) but no firm conclusions can be drawn given the scarcity of the data.
2.37. Analysis.
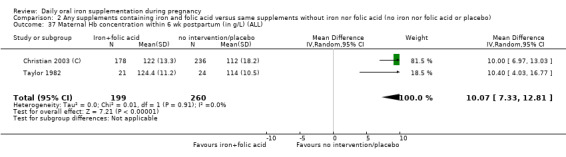
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 37 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL).
Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more)
Three trials reported severe anaemia at or near term; there were estimable data for only one trial and overall only three women were identified with severe anaemia (Analysis 2.41).
2.41. Analysis.
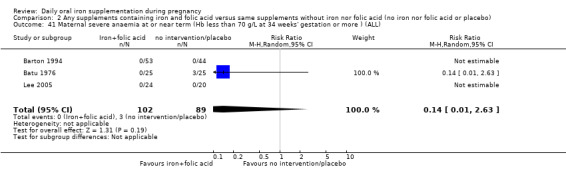
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 41 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more ) (ALL).
Maternal severe or moderate anaemia at postpartum (Hb less than 80 g/L)
Two of three trials reported estimable data for moderate anaemia in the postpartum period and women receiving iron were less likely to have anaemia (RR 0.33; 95% CI 0.17 to 0.65) (Analysis 2.40). For severe anaemia in the postpartum period only one trial of three reported estimable data with all cases of severe anaemia occurring in the women who did not receive supplements (RR 0.05; 95% CI 0.00 to 0.76) (Analysis 2.42). The scarcity of data makes it difficult to draw any firm conclusions on these outcomes.
2.40. Analysis.
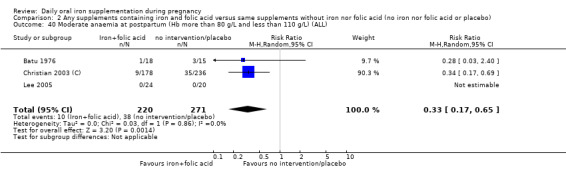
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 40 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL).
2.42. Analysis.
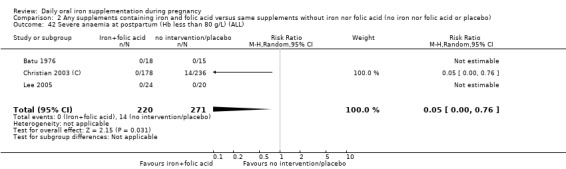
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 42 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL).
Other secondary maternal outcomes
No evidence of significant differences was found in the following secondary outcomes: puerperal infection, antepartum haemorrhage, postpartum haemorrhage, placental abruption, and pre‐eclampsia. No trials reported on the remaining maternal secondary outcomes.
(3) Supplementation with iron alone versus no treatment/placebo (33 studies)
Infant primary outcomes
Low birthweight (less than 2500 g)
Overall, we found no statistically significant difference in the prevalence of low birthweight (less than 2500 g) between newborns of mothers in these two groups (Analysis 3.1). Among 1136 women in six trials (Cogswell 2003; Eskeland 1997; Falahi 2010; Makrides 2003; Meier 2003; Menendez 1994 (C)), 4.3% of those who took daily iron supplementation during pregnancy had a baby with a birthweight below 2500 g versus 6.9% of those who received no iron or placebo (average RR 0.63; 95% CI 0.30 to 1.32) (Analysis 3.1). When we limited our analysis to studies meeting criteria for high quality (Cogswell 2003; Eskeland 1997; Makrides 2003; Menendez 1994 (C)), the difference in the percentage of mothers with low birthweight babies remained non‐significant (data not shown). There were no clear differences between subgroups Analysis 3.2; Analysis 3.3; Analysis 3.4; Analysis 3.5).
3.1. Analysis.
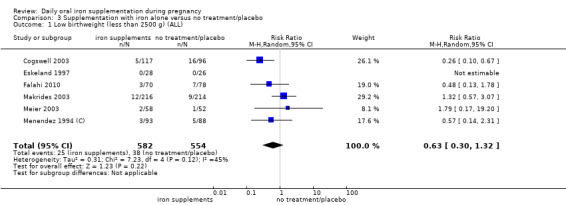
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 1 Low birthweight (less than 2500 g) (ALL).
3.2. Analysis.
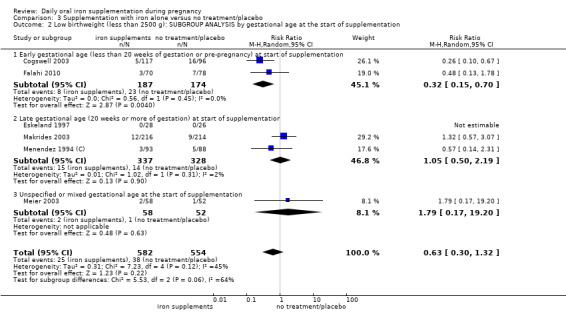
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.3. Analysis.
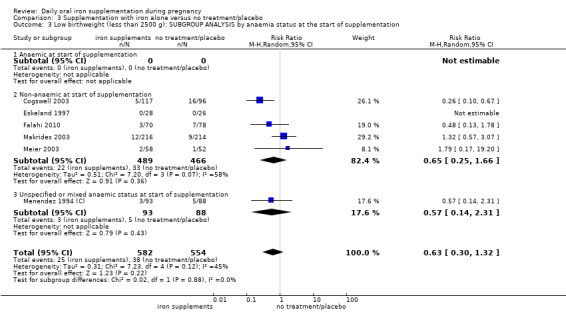
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.4. Analysis.
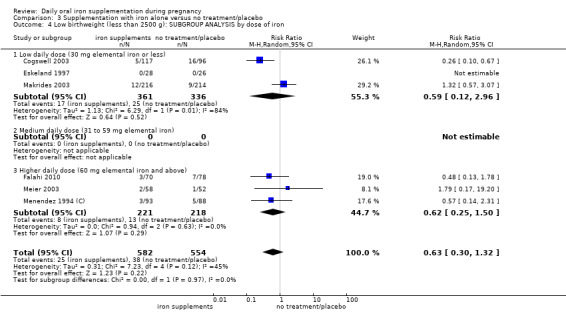
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron.
3.5. Analysis.
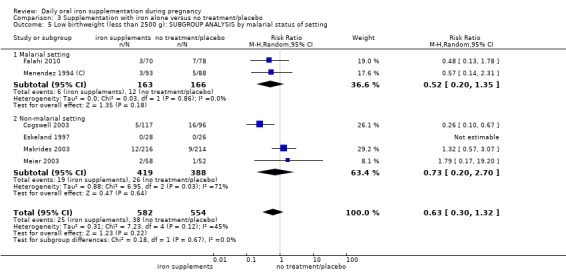
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting.
Birthweight (g)
We found no significant difference in birthweight (Analysis 3.6), in children from mothers of the two groups. Among infants born to 1331 participants in nine trials (Cogswell 2003; Eskeland 1997; Falahi 2010; Harvey 2007; Korkmaz 2014; Makrides 2003; Paintin 1966; Preziosi 1997; Puolakka 1980), the MD in birthweight between those whose mothers had taken iron supplements and those whose mothers had not was ‐1.04 g and was not statistically significant (95% CI ‐78.77 to 76.70) . When we temporarily removed from the analysis the studies that did not meet our criteria for high quality the results remained non‐significant (data not shown). No subgroup differences were apparent (Analysis 3.7; Analysis 3.8; Analysis 3.9; Analysis 3.10).
3.6. Analysis.
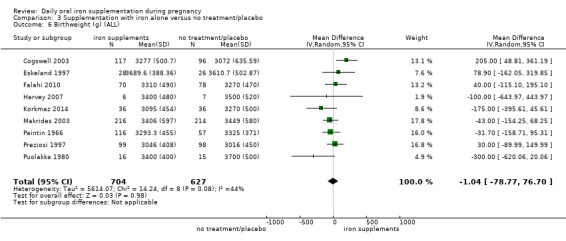
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 6 Birthweight (g) (ALL).
3.7. Analysis.
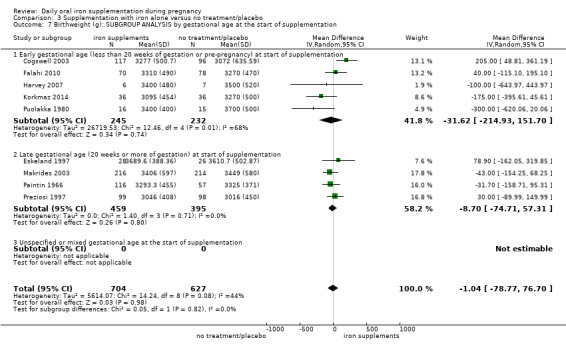
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.8. Analysis.
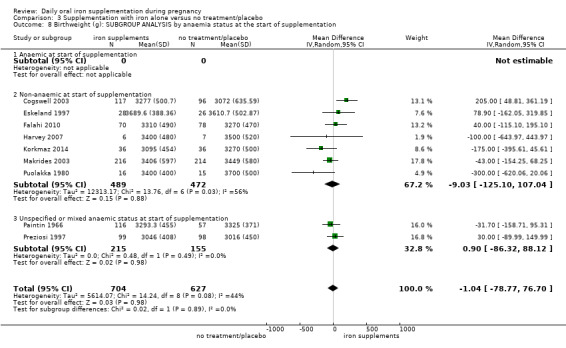
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.9. Analysis.
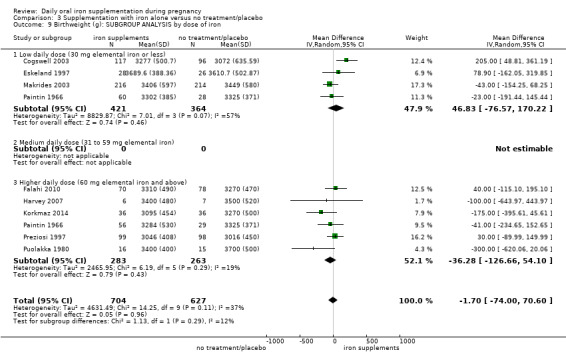
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron.
3.10. Analysis.
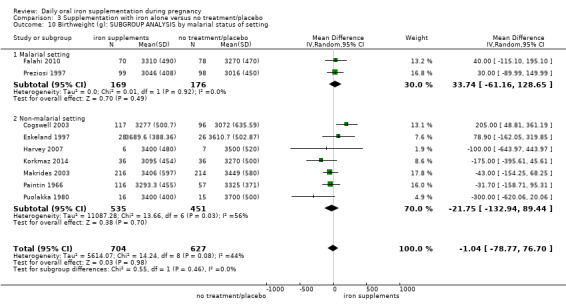
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting.
Preterm birth (less than 37 weeks' gestation)
Six trials with data for 1713 women provided data on preterm birth (before 37 weeks' gestation). There were no clear differences between groups for this outcome (average RR 0.82; 95% CI 0.58 to 1.14) (Analysis 3.11). When we temporarily removed from the analysis the one study that did not meet our criteria for high quality (Chan 2009), the results remained non‐significant (data not shown). We found no significant differences between subgroups (Analysis 3.12; Analysis 3.13; Analysis 3.14; Analysis 3.15).
3.11. Analysis.
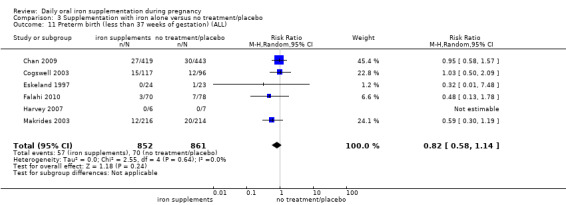
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 11 Preterm birth (less than 37 weeks of gestation) (ALL).
3.12. Analysis.
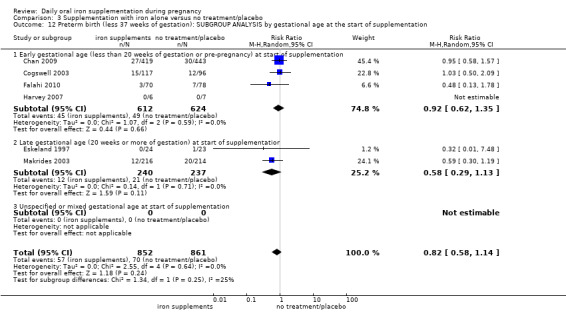
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 12 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.13. Analysis.
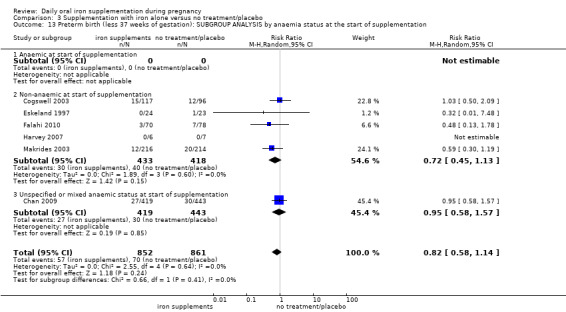
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 13 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.14. Analysis.
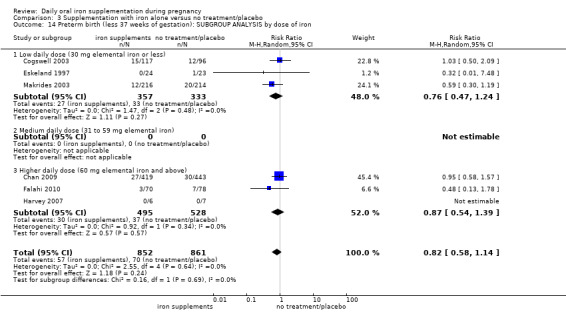
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 14 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron.
3.15. Analysis.
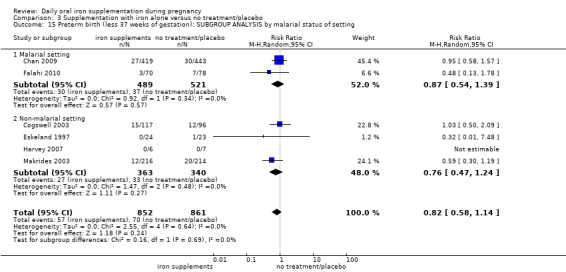
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting.
Other primary infant outcomes
There were no estimable data for neonatal mortality (Analysis 3.16). Two studies reported the number of infants with congenital anomalies; again, there was no clear evidence of any difference between groups (average RR 0.86; 95% CI 0.55 to 1.35; 2402 participants) (Analysis 3.17).
3.17. Analysis.
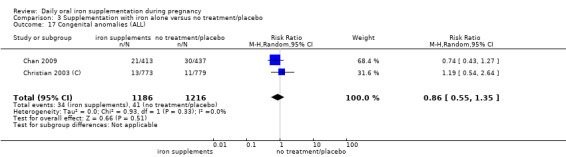
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 17 Congenital anomalies (ALL).
Maternal primary outcomes
Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more)
Among 2136 women in 14 trials (Batu 1976; Chanarin 1971; Chisholm 1966; Cogswell 2003; De Benaze 1989; Eskeland 1997; Holly 1955; Liu 2000; Makrides 2003; Milman 1991; Preziosi 1997; Pritchard 1958; Puolakka 1980; Romslo 1983), 12.5% of those who received daily iron supplements during pregnancy and 34.3% who did not receive iron had anaemia at term (average RR 0.29; 95% CI 0.19 to 0.47 (Analysis 3.18). However, because the heterogeneity in study results was substantial our results have to be interpreted with caution (heterogeneity: Tau² = 0.44, I² = 80%, Chi² test for heterogeneity P < 0.0001. When we temporarily removed studies from the analyses that did not meet our criteria for high quality, the difference between groups remained significant and heterogeneity was reduced although it remained over 50% (data not shown). We did not find differences between subgroups in terms of women's gestational age or anaemia status at the start of supplementation, or for the dose of iron (Analysis 3.19; Analysis 3.20; Analysis 3.21). The treatment effect appeared more pronounced in non‐malarial settings, however only two of the trials contributing data to this analysis were carried out in a malarial setting so any difference between these subgroups may have occurred by chance (test for subgroup differences: Chi² = 11.75, df = 1 (P = 0.0006), I² = 91.5%) (Analysis 3.22).
3.18. Analysis.
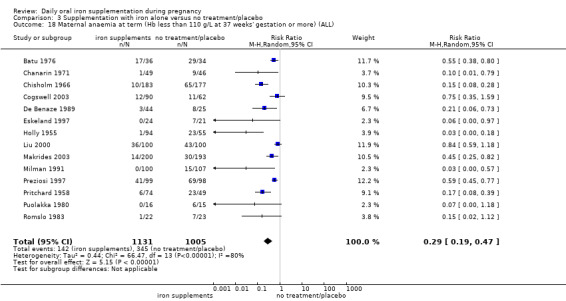
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL).
3.19. Analysis.
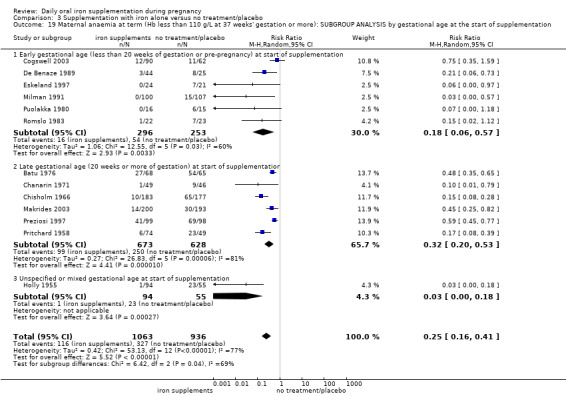
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 19 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.20. Analysis.
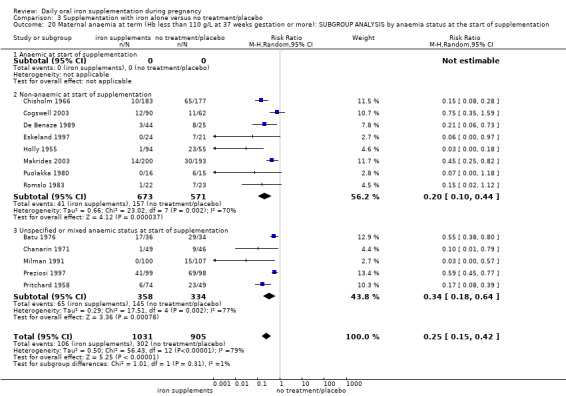
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 20 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.21. Analysis.
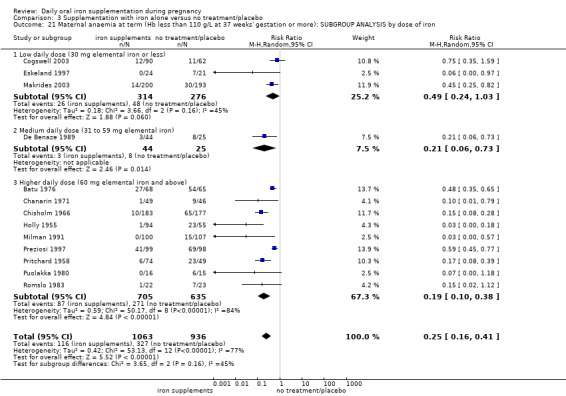
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 21 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
3.22. Analysis.
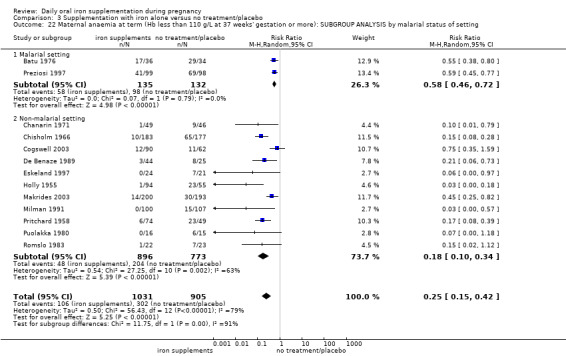
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 22 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more)
Data from seven trials involving 1256 women (Cogswell 2003; Eskeland 1997; Falahi 2010; Makrides 2003; Milman 1991; Preziosi 1997; Tura 1989) showed that 28.5% of women who received daily iron supplements had iron‐deficiency at term, compared with 51.3% of those who received no iron supplements (average RR 0.43; 95% CI 0.27 to 0.66) (Analysis 3.23). The heterogeneity between the treatment effects is high and the results should be interpreted with caution (heterogeneity: Tau² = 0.26, I² = 85%, Chi² test for heterogeneity P < 0.00001). Subgroup analyses indicated that mixed or unspecified anaemia status at the start of supplementation and higher doses of iron were associated with more pronounced treatment effects (test for subgroup differences: Chi² = 10,96 df = 1 (P = 0.0009), I² = 90.9%, and Chi² = 19.52, df = 2 (P = 0.0001), I² = 89.8%, respectively (Analysis 3.25; Analysis 3.26).
3.23. Analysis.
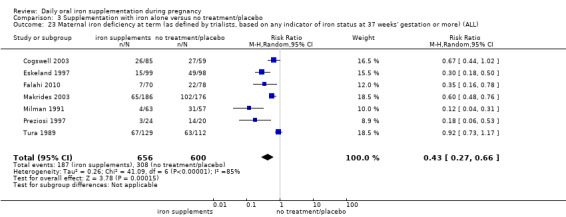
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 23 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL).
3.25. Analysis.
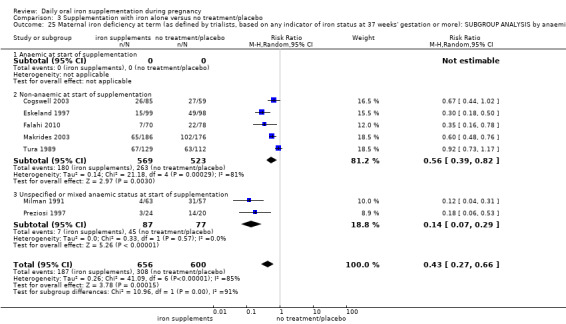
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 25 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.26. Analysis.
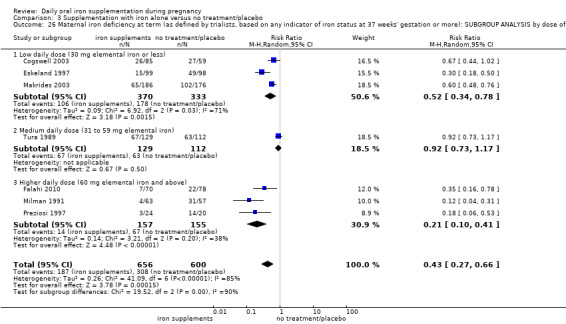
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 26 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
Maternal iron‐deficiency anaemia at term (Hb below 110 g/L and at least one additional laboratory indicator at 37 weeks' gestation or more)
Data from six trials involving 1088 women (Cogswell 2003; Eskeland 1997; Falahi 2010; Makrides 2003; Milman 1991; Tura 1989) showed that 4.4% of women who received daily iron supplements and 13.2% of those who did not, had iron‐deficiency anaemia at term (average RR 0.33; 95% CI 0.16 to 0.69). The heterogeneity between the treatment effects was moderate (I² 49%) (Analysis 3.28). There were no differences identified between subgroups (Analysis 3.29; Analysis 3.30; Analysis 3.31; Analysis 3.32).
3.28. Analysis.
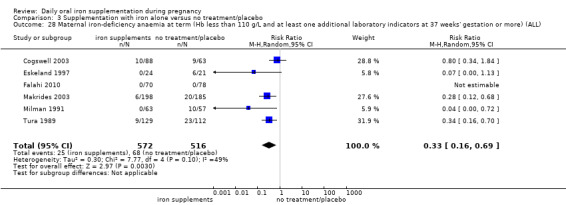
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 28 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL).
3.29. Analysis.
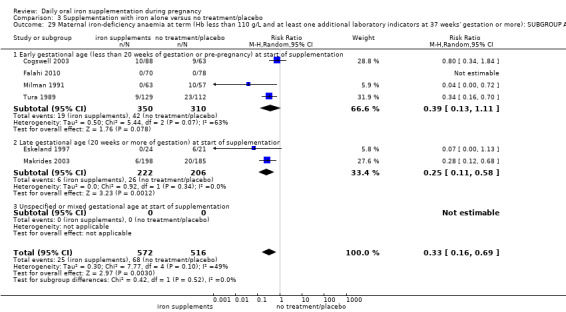
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 29 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.30. Analysis.
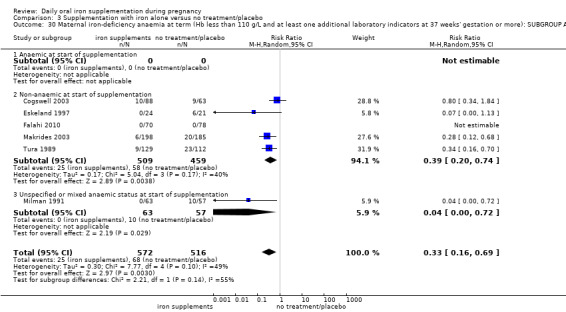
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 30 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.31. Analysis.
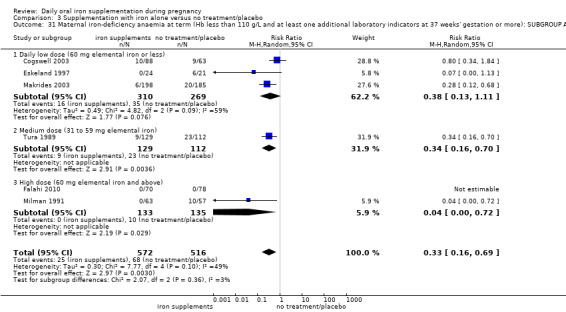
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 31 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
3.32. Analysis.
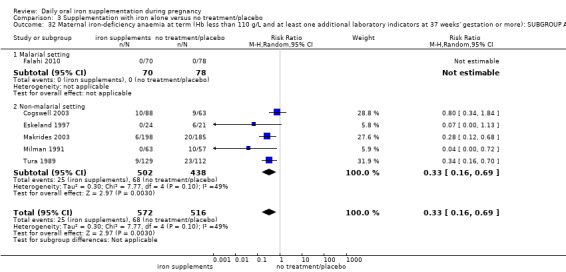
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 32 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
Side effects (any)
Data from nine trials (Charoenlarp 1988; Cogswell 2003; De Benaze 1989; Eskeland 1997; Harvey 2007; Hood 1960; Kerr 1958; Makrides 2003; Paintin 1966) suggest that women who receive daily oral iron supplementation are more likely to report side effects of any kind than women taking placebo or not taking any iron supplements although the difference between groups was of borderline statistical significance (29% versus 21%; (average RR 1.59; 95% CI 1.00 to 2.52; nine studies, 1677 participants; I² = 75%)) (Analysis 3.34). However, the heterogeneity between the treatment effects is substantial and the results have to be interpreted with caution. The difference between groups appeared more pronounced in malarial settings although this was due to the findings in a single study carried out in a malarial setting (test for subgroup differences: Chi² = 7.09, df = 1 (P = 0.008), I² = 85.9%) (Analysis 3.38). When we restricted the analyses to those trials meeting criteria for high quality, the difference between groups did not reach statistical significance (data not shown).
3.34. Analysis.
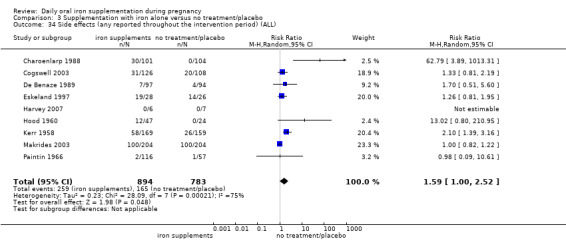
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 34 Side effects (any reported throughout the intervention period) (ALL).
3.38. Analysis.
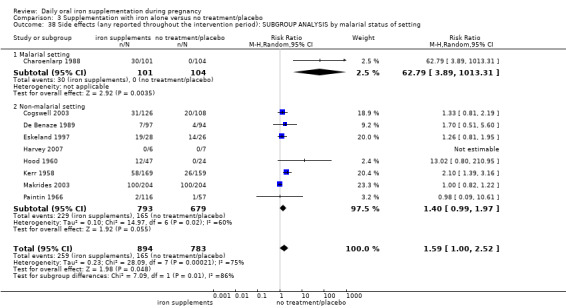
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 38 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by malarial status of setting.
Maternal severe (Hb < 70 g/L) anaemia at any time during the second or third trimester
Data from seven trials involving 1078 women was available for this outcome, although only two trials with 466 women reported estimable data which showed that women who received iron supplements were as likely to become severely anaemic during second and third trimesters (average RR 0.75; 95% CI 0.02 to 29.10) as those not receiving iron (Analysis 3.39). However, results are difficult to interpret as very few trials reported events, and in many cases women who became anaemic were treated and excluded from the analysis in the trials. We found no differences between subgroups (Analysis 3.40; Analysis 3.41; Analysis 3.42; Analysis 3.43).
3.39. Analysis.
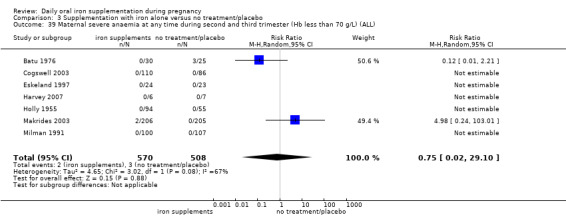
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 39 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL).
3.40. Analysis.
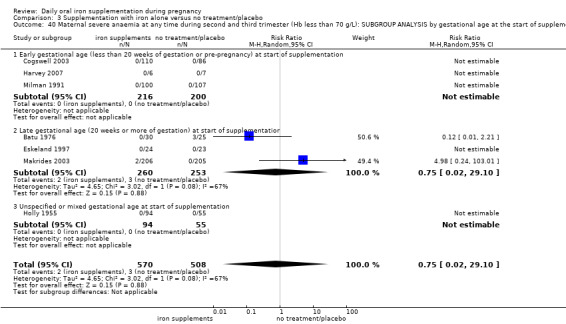
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 40 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.41. Analysis.
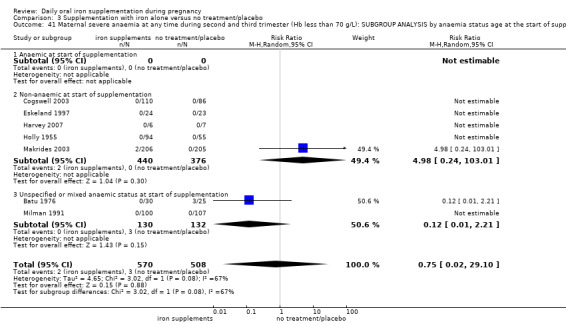
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 41 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status age at the start of supplementation.
3.42. Analysis.
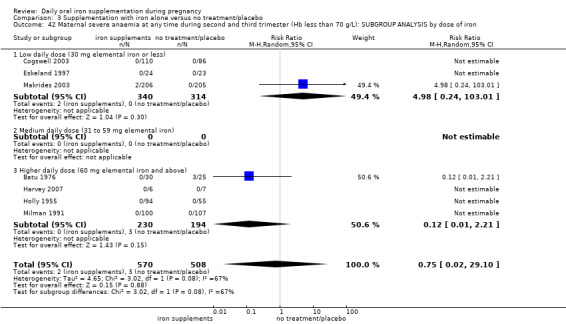
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 42 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron.
3.43. Analysis.
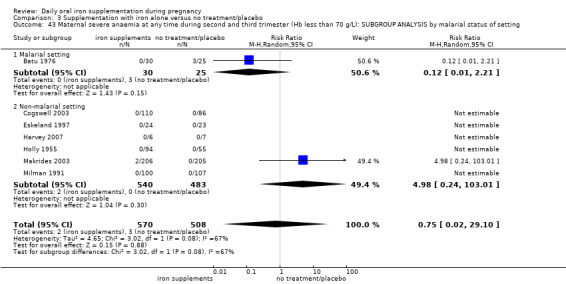
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 43 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting.
Other maternal primary outcomes
Maternal mortality was reported in one small trial including 47 women and no events were reported (Analysis 3.33). Infection during pregnancy was not reported.
3.33. Analysis.
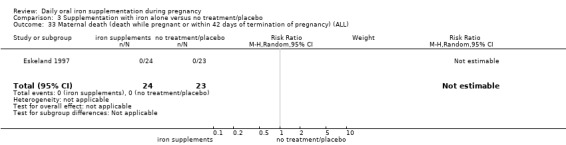
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 33 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL).
No studies reported findings for other maternal primary outcomes: malaria.
Infant secondary outcomes
Infant ferritin concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period)
The MD was 11.00 μg/L; 95% CI 4.37 to 17.63 μg/L (one trial involving 197 women) (Preziosi 1997) (Analysis 3.49).
3.49. Analysis.
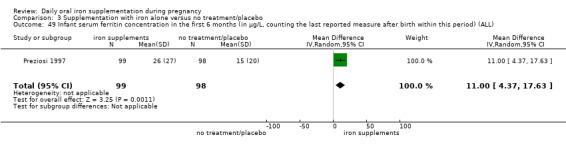
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 49 Infant serum ferritin concentration in the first 6 months (in μg/L, counting the last reported measure after birth within this period) (ALL).
Very premature birth (less than 34 weeks' gestation)
This outcome was reported in three trials, involving 690 participants; results suggest that babies born to mothers receiving iron were less likely to be born before 34 weeks' gestation (average RR 0.32; 95% CI 0.10 to 1.09) (Analysis 3.47).
3.47. Analysis.
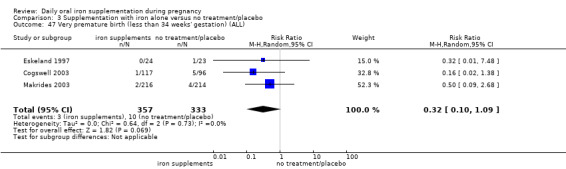
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 47 Very premature birth (less than 34 weeks' gestation) (ALL).
Other infant secondary outcomes
We found no evidence of significant difference by treatment group in the following secondary outcomes: very low birthweight (less than 1500 g) (Analysis 3.46); infant Hb concentration in the first six months (in g/L, counting the last reported measure after birth within this period) (Analysis 3.48); admission to special care unit (Analysis 3.50). No trials reported on the remaining infant secondary outcomes such as infant anaemia or infant iron‐deficiency anaemia at birth or soon after.
3.46. Analysis.
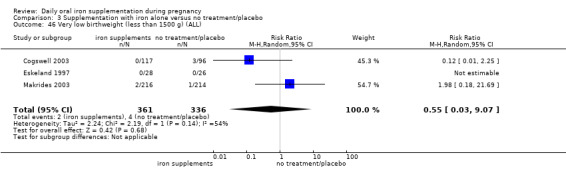
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 46 Very low birthweight (less than 1500 g) (ALL).
3.48. Analysis.
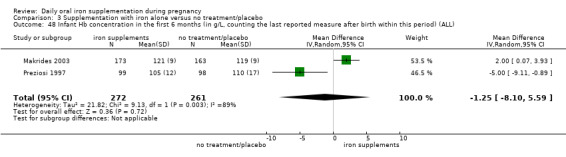
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 48 Infant Hb concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period) (ALL).
3.50. Analysis.
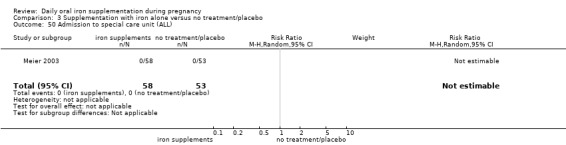
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 50 Admission to special care unit (ALL).
Maternal secondary outcomes
Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more)
Among 1851 women who participated in 16 trials (Batu 1976; Buytaert 1983; Cantlie 1971; Chanarin 1971; Cogswell 2003; De Benaze 1989; Eskeland 1997; Falahi 2010; Makrides 2003; Milman 1991; Puolakka 1980; Romslo 1983; Tura 1989; Van Eijk 1978; Wallenburg 1983; Ziaei 2008), those who took iron supplements had a mean Hb concentration 8.95 g/L higher at term in comparison to those who took no iron supplements at all (MD 8.95; 95% CI 6.37 to 11.53 g/L) (Analysis 3.54). However, because the heterogeneity among the treatment effects found in individual studies was substantial our results have to be interpreted with caution (heterogeneity: Tau² = 21.70, I² = 89%, Chi² test for heterogeneity P < 0.00001). When we restricted the analysis to studies meeting the criteria for high quality the difference between groups remained significant (data not shown).
3.54. Analysis.
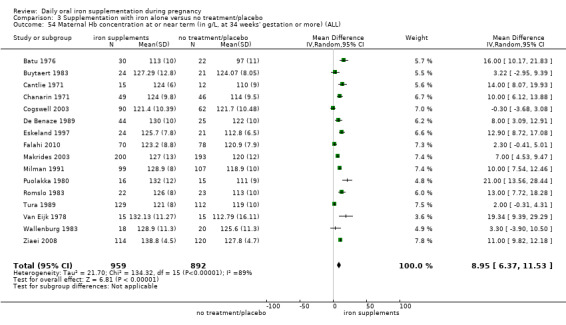
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 54 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL).
Maternal Hb concentration within six weeks postpartum (in g/L)
The data from six trials involving 659 women (Cantlie 1971; Hankin 1963; Lee 2005; Menendez 1994 (C); Milman 1991; Wills 1947) suggest that women that routinely receive daily iron supplementation have a higher concentration of Hb within six weeks postpartum than those taking placebo or not taking any iron supplements at all (MD 7.26 g/L; 95% CI 4.78 to 9.74 g/L). Heterogeneity of the results is Tau² = 3.99, I² = 44%, Chi² test for heterogeneity P < 0.0001 (Analysis 3.55).
3.55. Analysis.
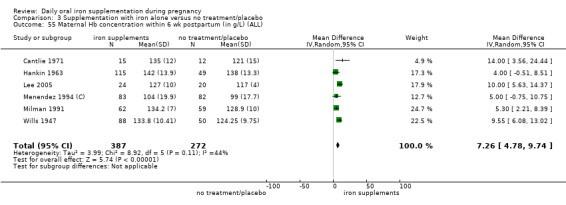
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 55 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL).
Maternal high Hb concentrations at any time during second or third trimester (Hb greater than 130 g/L)
Seven trials evaluated the effects of oral routine supplementation with iron alone and high Hb concentrations at any time during the second or third trimesters (Cogswell 2003; Eskeland 1997; Harvey 2007; Holly 1955; Makrides 2003; Milman 1991; Pritchard 1958). Among women who received daily iron supplements, 30.6% were found to have high Hb concentrations at some time during their second or third trimesters, compared with 15.2% of those who received no iron supplements (average RR 1.90; 95% CI 1.07 to 3.35; seven studies, 1146 participants; I² = 80%) (Analysis 3.56). However, because the heterogeneity between studies was substantial, the results have to be interpreted with caution. The difference between groups remained significant when we temporarily removed from the analysis those studies which did not meet our criteria for high quality (data not shown).
3.56. Analysis.
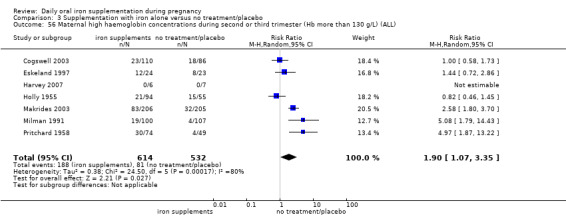
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 56 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL).
Maternal high Hb concentrations at or near term (defined as Hb greater than 130 g/L, at 34 weeks' gestation or more)
Data from seven trials (Chisholm 1966; Cogswell 2003; Eskeland 1997; Holly 1955; Makrides 2003; Milman 1991; Pritchard 1958) indicated that 30.1% of women who took daily iron supplementation during pregnancy and 9.87% of those who did not had high Hb concentrations at term ((average RR 3.80; 95% CI 1.74 to 8.28; seven studies, 1189 participants; I² = 69%) (Analysis 3.57). The heterogeneity between the treatment effects was substantial and the results have to be interpreted with caution. The difference between groups remained significant when we restricted the analysis to studies meeting criteria for high quality (data not shown).
3.57. Analysis.
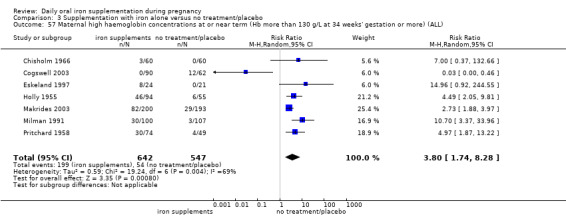
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 57 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL).
Transfusion provided
The data from a single trial (Puolakka 1980) suggest no clear differences between women that routinely receive daily iron supplementation and those that do not (average RR 0.33; 95% CI 0.01 to 7.62; 32 participants) (Analysis 3.64).
3.64. Analysis.
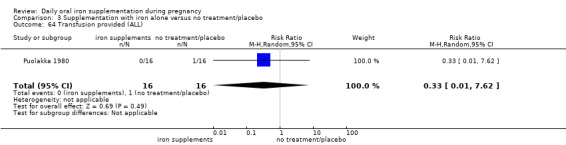
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 64 Transfusion provided (ALL).
Maternal well being/satisfaction
Eskeland 1997 assessed maternal well being at 28 and 36 weeks' gestation, and found no differences between the iron supplemented mothers or those receiving placebo (Analysis 3.70).
3.70. Analysis.
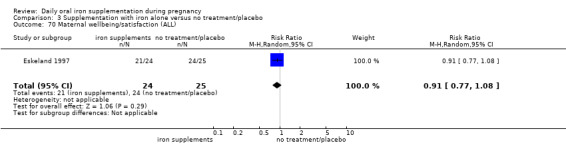
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 70 Maternal wellbeing/satisfaction (ALL).
Other secondary outcomes
There was no evidence of significant differences between women receiving daily iron supplementation and women receiving placebo or not taking any iron supplements at all, in the following secondary outcomes: diarrhoea, placental abruption, pre‐eclampsia, moderate anaemia at postpartum, maternal severe anaemia a postpartum; puerperal infection, antepartum haemorrhage and postpartum haemorrhage, constipation, nausea, heartburn, or vomiting. No trials reported on the remaining secondary outcomes.
(4) Supplementation with iron + folic acid versus no treatment/placebo (eight studies)
Infant primary outcomes
Low birthweight (less than 2500 g)
Two studies with 1311 participants examined this outcome (Christian 2003 (C); Taylor 1982). There was no clear evidence of significant differences between infants of women receiving daily iron + folic acid supplementation versus no supplements (average RR 1.07; 95% CI 0.31 to 3.74) (Analysis 4.1).
4.1. Analysis.
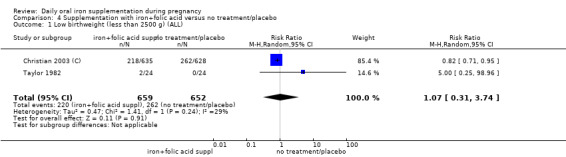
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 1 Low birthweight (less than 2500 g) (ALL).
Data from these trials suggest that infant birthweight were 57.73 g heavier 95% CI 7.66 to 107.79 g in comparison to no treatment/placebo (Analysis 4.2). One trial (Christian 2003 (C)) met our criteria for high quality.
4.2. Analysis.
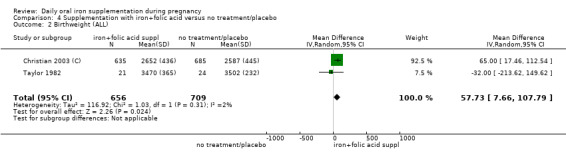
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 2 Birthweight (ALL).
Preterm birth (less than 37 weeks' gestation)
Three studies with 1497 participants examined this outcome (Christian 2003 (C); Lee 2005; Taylor 1982). We found no evidence of differences in the numbers experiencing preterm birth between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (Analysis 4.3). One of these trials met the criteria for high quality (Christian 2003 (C)). There were no subgroup differences; only two of these trials had estimable data for this outcome (Analysis 4.4; Analysis 4.5; Analysis 4.6; Analysis 4.7).
4.3. Analysis.
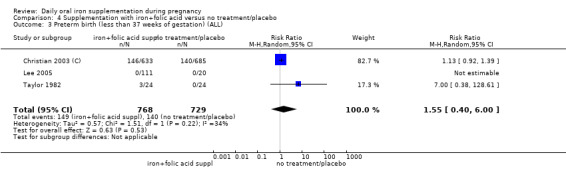
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 3 Preterm birth (less than 37 weeks of gestation) (ALL).
4.4. Analysis.
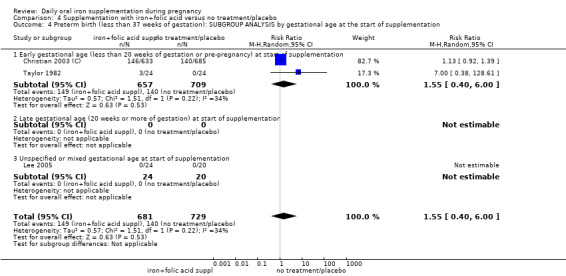
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 4 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
4.5. Analysis.
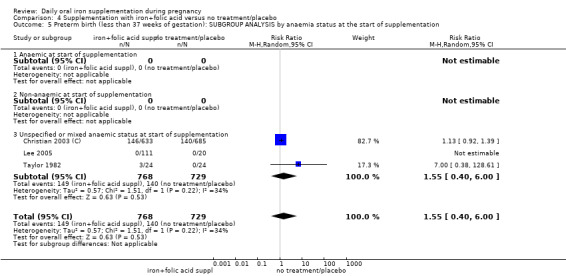
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 5 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
4.6. Analysis.
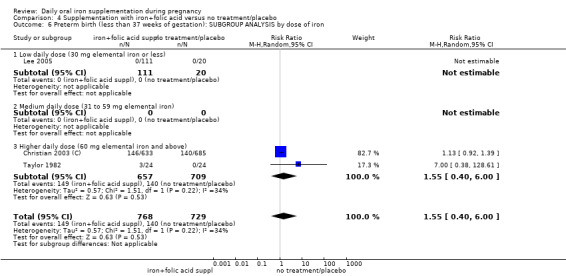
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 6 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron.
4.7. Analysis.
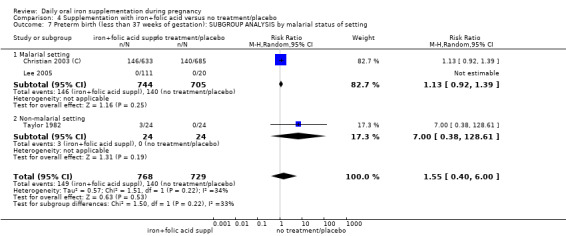
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 7 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting.
Neonatal death
Three studies with 1793 women reported on this outcome (Barton 1994; Christian 2003 (C); Taylor 1982); there was no clear evidence of any difference between groups (average RR 0.81; 95% CI 0.51 to 1.30) (Analysis 4.8).
4.8. Analysis.
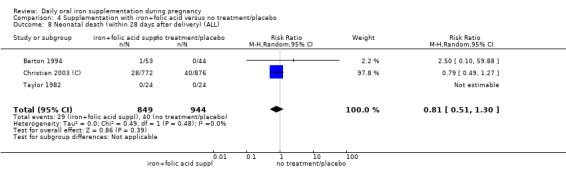
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 8 Neonatal death (within 28 days after delivery) (ALL).
Congenital anomalies
Only one study (1652 participants) reported data on this outcome (Christian 2003 (C)) and there appears to be no differences between the groups compared (RR 0.70; 95% CI 0.35 to 1.40) (Analysis 4.13).
4.13. Analysis.
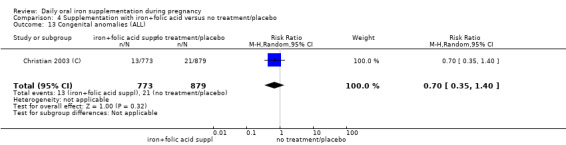
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 13 Congenital anomalies (ALL).
Maternal primary outcomes
Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more)
The data from three trials including 346 women (Barton 1994; Batu 1976; Chisholm 1966) suggest that women who routinely receive daily iron and folic acid supplementation during pregnancy are less likely to have anaemia at term than those not taking any iron and folic acid supplements at all (defined as Hb less than 110 g/L) (7.2% versus 28.2%; average RR 0.34; 95% CI 0.21 to 0.54) (Analysis 4.14). Only one study with no estimable data met the prespecified criteria for high quality. There was no evidence of subgroup differences.
4.14. Analysis.
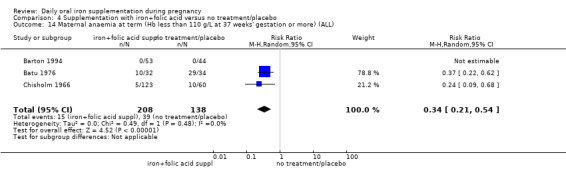
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 14 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL).
Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more)
Data from one trial involving 131 women (Lee 2005) suggest that women who routinely receive daily oral supplementation with iron are less likely to have iron deficiency at term than women taking placebo or not taking any iron and folic acid supplements at all, although the difference between groups did not reach statistical significance (3.6% versus 15%; RR 0.24; 95% CI 0.06 to 0.99) (Analysis 4.19).
4.19. Analysis.
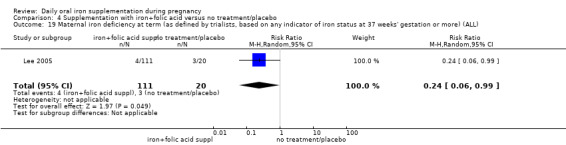
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 19 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL).
Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicator at 37 weeks' gestation or more)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo in the single trial contributing data to this analysis (RR 0.43; 95% CI 0.17 to 1.09) (Analysis 4.20). The study (131 participants) contributing data did not meet the prespecified criteria for high quality.
4.20. Analysis.
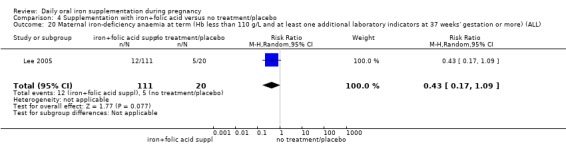
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 20 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL).
Side effects (any)
One trial including 456 women (Charoenlarp 1988) suggests that women routinely receiving iron and folic acid supplementation are more likely to report any side effects; none of those receiving no supplementation reported side effects, however the CI is very broad for this finding (average RR 44.32; 95% CI 2.77 to 709.09) (Analysis 4.22). This trial did not meet the criteria for high methodological quality.
4.22. Analysis.
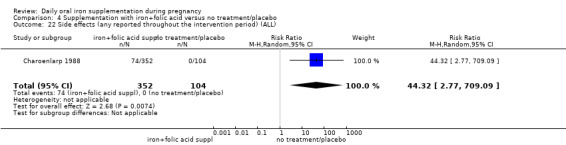
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 22 Side effects (any reported throughout the intervention period) (ALL).
Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L)
Two of four trials reported estimable data for this outcome and results suggest that women were less likely to be identified with severe anaemia in the group receiving iron (average RR 0.12; 95% CI 0.02 to 0.63) (Analysis 4.23).
4.23. Analysis.
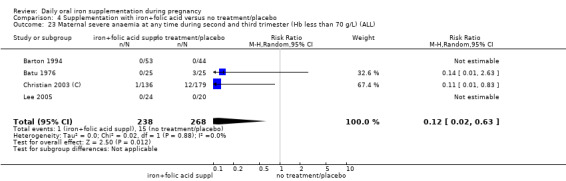
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 23 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL).
Other outcomes
One trial with 48 women reported on infection in pregnancy (Taylor 1982); there were four events in total, two in each group (Analysis 4.25). A single study reported on maternal deaths and there were no estimable data (Analysis 4.21). There were no data on the remaining prespecified primary outcomes.
4.25. Analysis.
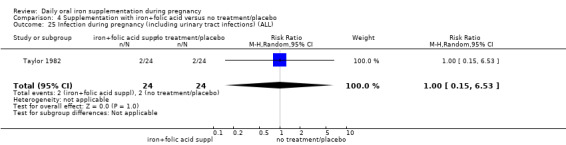
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 25 Infection during pregnancy (including urinary tract infections) (ALL).
4.21. Analysis.
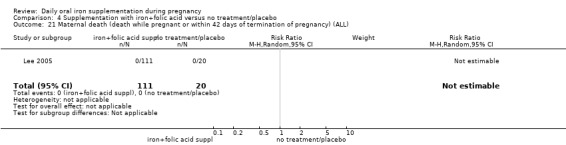
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 21 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL).
Infant secondary outcomes
No evidence of significant differences was found between infants from these groups of women receiving daily iron + folic acid supplementation and those taking placebo or not taking any supplements at all in the following secondary outcomes: very low birthweight (less than 1500 g), very premature birth (less than 34 weeks) or admission to special care unit.
There were no data on other infant secondary outcomes.
Maternal secondary outcomes
Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more)
The data from three trials including 346 women (Barton 1994; Batu 1976; Chisholm 1966) suggest that women who routinely receive daily iron and folic acid supplementation during pregnancy are less likely to have anaemia at term than those not taking any iron and folic acid supplements at all (defined as Hb less than 110 g/L) (7.2% versus 28.2%; average RR 0.34; 95% CI 0.21 to 0.54) (Analysis 4.31). Only one study with no estimable data met the prespecified criteria for high quality.
4.31. Analysis.
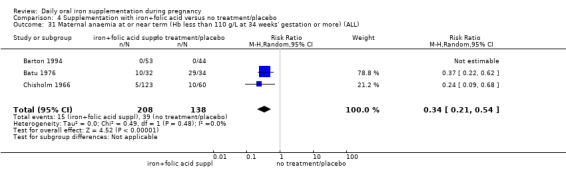
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 31 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL).
Maternal iron deficiency at or near term (as defined by as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more)
Data from one trial involving 131 women (Lee 2005), suggest that women who routinely receive daily oral supplementation with iron are less likely to have iron deficiency at term than women taking placebo or not taking any iron and folic acid supplements at all, although the difference between groups was not statistically significant (3.6% versus 15%; RR 0.24; 95% CI 0.06 to 0.99) (Analysis 4.32).
4.32. Analysis.
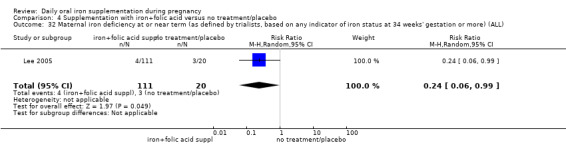
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 32 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL).
Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicator at 34 weeks' gestation or more)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo in the single trial contributing data to this analysis (Analysis 4.33). The study contributing data did not meet the prespecified criteria for high quality.
4.33. Analysis.
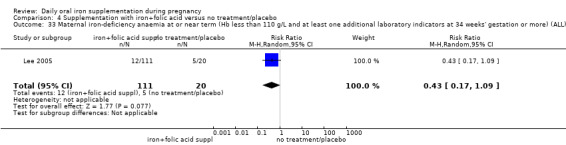
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 33 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL).
Maternal Hb concentration at or near term (in g/L at 34 weeks' gestation or more)
The data from three trials including 140 women (Barton 1994; Batu 1976; Taylor 1982) suggest that women who routinely receive daily iron and folic acid supplementation reach term with a higher Hb concentration than women taking placebo or not taking any iron and folic acid supplement at all (MD 16.13 g/L; 95% CI 12.74 to 19.52) (Analysis 4.34). The effect of iron‐folic acid supplementation was associated with higher Hb concentrations in the single high‐quality trial (MD 17.10; 95% CI 8.44 to 25.76) (Barton 1994).
4.34. Analysis.
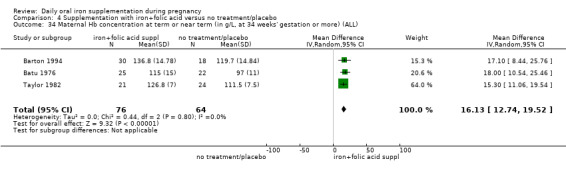
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 34 Maternal Hb concentration at term or near term (in g/L, at 34 weeks' gestation or more) (ALL).
Maternal high Hb concentrations at any time during second or third trimesters (defined as Hb greater than 130 g/L)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (Analysis 4.36).
4.36. Analysis.
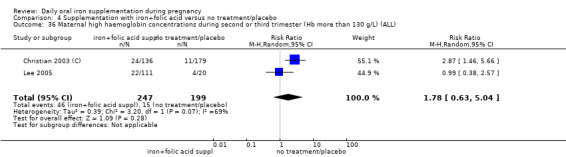
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 36 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL).
Maternal high Hb concentrations at term (defined as Hb greater than 130 g/L at 37 weeks' gestation or more)
No evidence of significant differences was found between women who received daily iron and folic acid supplements and those receiving no treatment or placebo (Analysis 4.37).
4.37. Analysis.
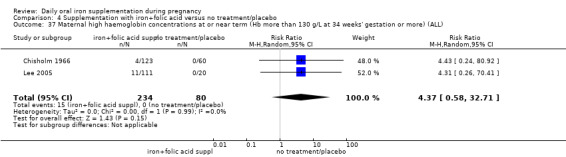
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 37 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL).
Maternal Hb concentration within six weeks postpartum in g/L
Two studies (Christian 2003 (C); Taylor 1982) involving 459 women reported this outcome. The data from these trials suggest that women receiving daily iron + folic acid supplementation achieve a higher concentration of Hb within six weeks postpartum than women not taking any supplements at all (MD 10.07; 95% CI 7.33 to 12.81) (Analysis 4.35), but no firm conclusions can be made given the scarcity of the data.
4.35. Analysis.
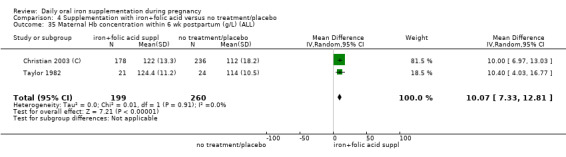
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 35 Maternal Hb concentration within 6 wk postpartum (g/L) (ALL).
Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more)
Three trials reported severe anaemia at term, but only one study had cases (Analysis 4.39).
4.39. Analysis.
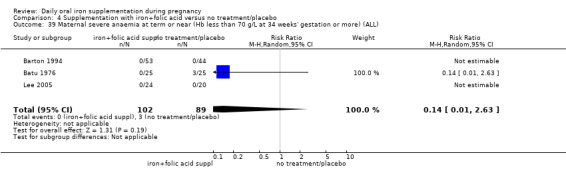
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 39 Maternal severe anaemia at term or near (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL).
Maternal severe or moderate anaemia at postpartum (Hb less than 80 g/L)
There was only one trial with estimable data on women with severe or moderate anaemia in the postpartum period (Analysis 4.38; Analysis 4.40). The scarcity of data makes it difficult to draw any conclusions on these outcomes.
4.38. Analysis.
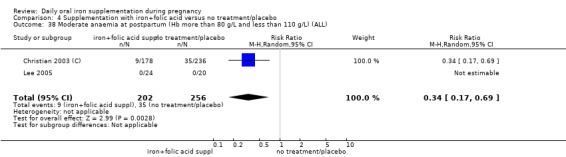
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 38 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL).
4.40. Analysis.
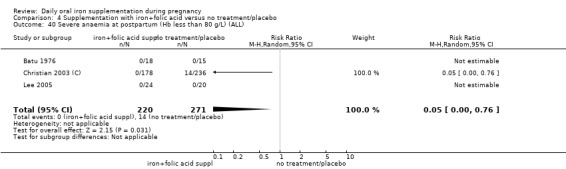
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 40 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL).
Other secondary maternal outcomes
No evidence of significant differences was found in the following secondary outcomes: very premature delivery, moderate anaemia at term, moderate anaemia at any time during second or third trimesters, puerperal infection, antepartum haemorrhage, postpartum haemorrhage, placental abruption and pre‐eclampsia. No trials reported on the remaining maternal secondary outcomes.
(5) Supplementation with iron + folic acid versus folic acid alone (without iron) supplementation (five studies)
The study by Zeng 2008 (C) was a cluster‐randomised trial and the sample size and event rate have been adjusted to take account of the design effect. In the results below we have used the effective sample size rather than the total number of women included in the study.
Infant primary outcomes
Low birthweight (less than 2500 g)
Four studies with an effective sample size of 16,146 contributed data to this outcome, all studies met the criteria for high quality (Christian 2003 (C); Liu 2012 ; Zeng 2008 (C); Ziaei 2007). There was a slight difference between groups receiving iron and folic acid versus folic acid alone (average RR 0.88; 95% CI 0.78 to 1.00) (Analysis 5.1). These studies reported mean infant birthweight but there was no difference between groups (MD 19.50; 95% CI ‐6.90 to 45.89) (Analysis 5.6).
5.1. Analysis.
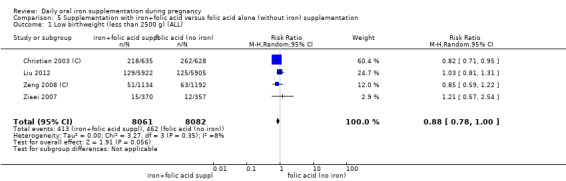
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 1 Low birthweight (less than 2500 g) (ALL).
5.6. Analysis.
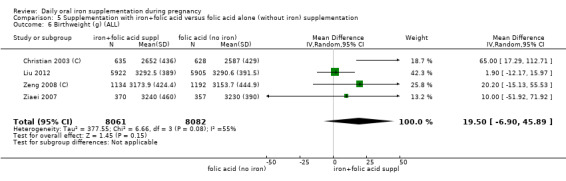
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 6 Birthweight (g) (ALL).
Preterm birth (less than 37 weeks' gestation)
Four studies with an effective sample size of 16,146 contributed data to this outcome; all studies met the criteria for high quality (Christian 2003 (C); Liu 2012 ; Zeng 2008 (C); Ziaei 2007). There was no statistically significant difference between groups receiving iron and folic acid versus folic acid alone and no subgroup differences were apparent (average RR 0.97; 95% CI 0.87 to 1.08) (Analysis 5.11).
5.11. Analysis.
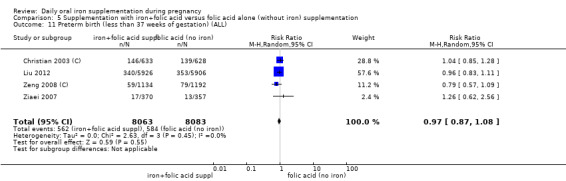
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 11 Preterm birth (less than 37 weeks of gestation) (ALL).
Neonatal death
Four studies (16,603 participants) (Christian 2003 (C); Liu 2012; Zeng 2008 (C); Ziaei 2007) contributed data; there was no evidence of a difference between groups (average RR 0.91; 95% CI 0.71 to 1.18) (Analysis 5.16). There were no differences between subgroups identified.
5.16. Analysis.
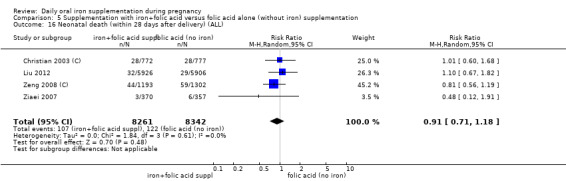
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 16 Neonatal death (within 28 days after delivery) (ALL).
Congenital anomalies
Two studies with 13,586 women reported the number of infants with congenital anomalies; and there was no clear evidence of any difference between groups (average RR 0.78; 95% CI 0.44 to 1.39) (Analysis 5.21).
5.21. Analysis.
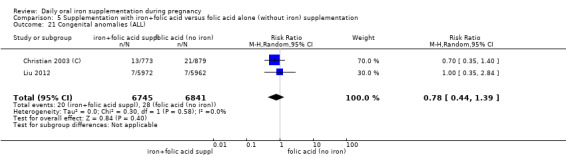
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 21 Congenital anomalies (ALL).
Maternal primary outcomes
Maternal anaemia at term (at 37 weeks' gestation or more)
Two studies with 303 women reported on the number of women with anaemia at term (Batu 1976; Chisholm 1966). The group receiving iron and folic acid were less likely to be anaemic compared to those receiving folic acid alone (9.7% versus 30.4%; average RR 0.34; 95% CI 0.21 to 0.55) (Analysis 5.22). The result remained significant when the study that did not meet our criteria for high quality was removed (data not shown). We did not find subgroup differences.
5.22. Analysis.
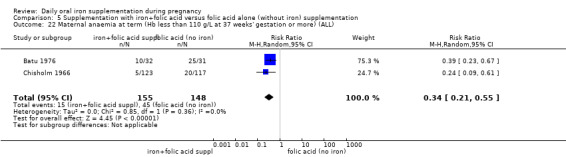
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 22 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL).
Maternal iron‐deficiency anaemia at term (at 37 weeks' gestation or more)
A single study (Ziaei 2007) reported on the number of women with iron‐deficiency anaemia at term; there were no estimable data for this outcome (Analysis 5.28).
5.28. Analysis.
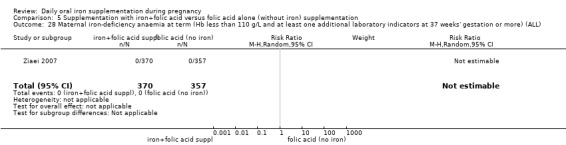
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 28 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL).
Side effects (any)
One study reported on side effects (Ziaei 2007). There were no significant differences between the compared groups (Analysis 5.30).
5.30. Analysis.
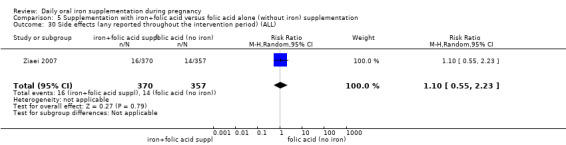
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 30 Side effects (any reported throughout the intervention period) (ALL).
Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L)
Three studies reported on maternal severe anaemia in pregnancy although there were estimable data for only one (Christian 2003 (C)). In this study women receiving supplements were less likely to be identified with severe anaemia (average RR 0.06; 95% CI 0.01 to 0.47) (Analysis 5.31).
5.31. Analysis.
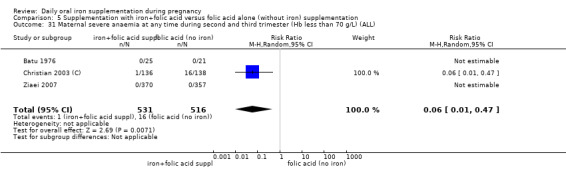
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 31 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL).
Infection during pregnancy
This outcome was reported in a single study with 727 women. There was no evidence of significant differences between groups (Analysis 5.33).
5.33. Analysis.
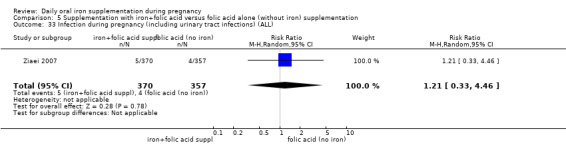
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 33 Infection during pregnancy (including urinary tract infections) (ALL).
Studies did not provide data on our remaining maternal prespecified outcomes (maternal iron deficiency, maternal death or clinical malaria).
Infant secondary outcomes
There was no evidence of differences between groups for very premature birth, very low birthweight. There were no data reported on our remaining infant secondary outcomes.
Maternal secondary outcomes
Maternal anaemia at or near term (at 34 weeks' gestation or more)
Two studies with 303 women reported on the number of women with anaemia at term (Batu 1976; Chisholm 1966). The group receiving iron and folic acid were less likely to be anaemic compared to those receiving folic acid alone (9.7% versus 30.4%; average RR 0.34; 95% CI 0.21 to 0.55) (Analysis 5.39). The result remained significant when the study that did not meet our criteria for high quality was removed (data not shown).
5.39. Analysis.
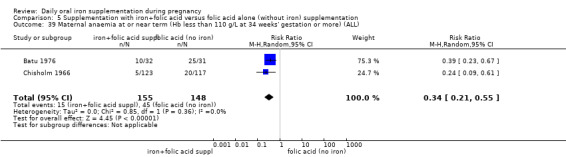
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 39 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL).
Maternal iron‐deficiency anaemia at or near term (at 34 weeks' gestation or more)
A single study (Ziaei 2007) reported on the number of women with iron‐deficiency anaemia at term; there were no estimable data for this outcome (Analysis 5.41).
5.41. Analysis.
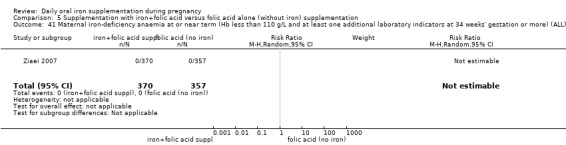
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 41 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL).
Maternal Hb at or near term (in g/L, at 34 weeks' gestation or more)
Two studies with 771 women contributed data to this outcome (Batu 1976; Ziaei 2007). The mean concentration of Hb was higher in the women receiving iron and folic acid as opposed to those receiving folic acid alone (MD 12.44; 95% CI 0.95 to 23.93). However, with only two studies contributing data this result should be treated with caution (Analysis 5.42).
5.42. Analysis.
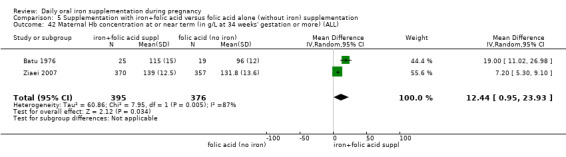
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 42 Maternal Hb concentration at or near term (in g/L at 34 weeks' gestation or more) (ALL).
Maternal high Hb concentrations at or near term (at 37 weeks' gestation or more) and during pregnancy
Two studies with 967 participants reported data for the number of women with high Hb concentrations at term (Chisholm 1966; Ziaei 2007). The evidence of difference between groups was not statistically significant (average RR 1.87; 95% CI 0.32 to 10.84) (Analysis 5.45).
5.45. Analysis.
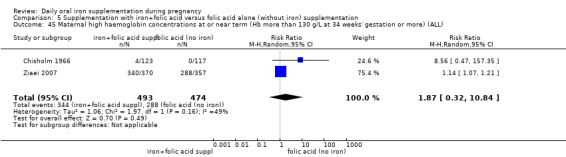
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 45 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL).
Two studies with 1042 women reported on high Hb concentrations in the third trimester of pregnancy. Women receiving iron in addition to folic acid were more likely to have high Hb concentrations during pregnancy (average RR 4.33; 95% CI 2.26 to 8.30) (Analysis 5.44).
5.44. Analysis.
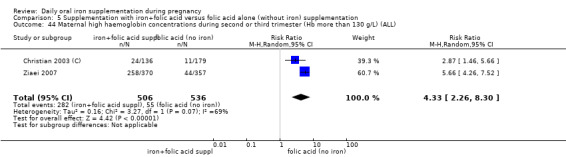
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 44 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL).
Other outcomes
There was no evidence of significant differences between groups for the following secondary outcomes: maternal high Hb concentrations during second or third trimester, puerperal infection, antepartum haemorrhage, postpartum haemorrhage, transfusion provided, diarrhoea, heartburn, nausea or constipation, placental abruption, premature rupture of the membranes or pre‐eclampsia.
Studies did not report data on our remaining maternal secondary outcomes.
(6) Supplementation with iron + other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation (three studies)
We have included data from three trials (Cantlie 1971;Ouladsahebmadarek 2011; Siega‐Riz 2001).
Infant primary outcomes
Two studies provided data for this comparison (Ouladsahebmadarek 2011; Siega‐Riz 2001).
There was no evidence of a statistically significant differences between groups for low birthweight or preterm birth (Analysis 6.1; Analysis 6.3). Mean birthweight was slightly greater in the iron supplemented group (Analysis 6.2). There were no data on perinatal death or other prespecified primary outcomes.
6.1. Analysis.
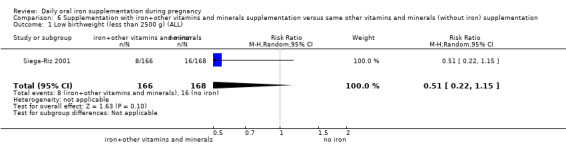
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 1 Low birthweight (less than 2500 g) (ALL).
6.3. Analysis.
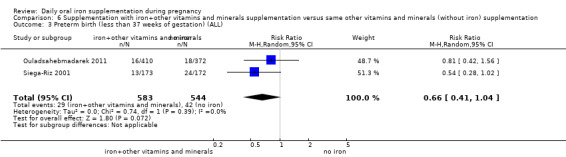
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 3 Preterm birth (less than 37 weeks of gestation) (ALL).
6.2. Analysis.
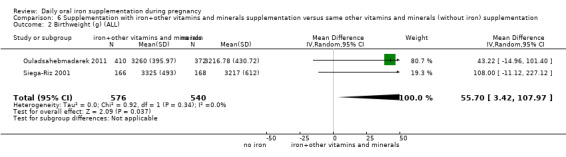
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 2 Birthweight (g) (ALL).
Maternal primary outcomes
One study provided data on side effects and no significant differences between groups were identified (Analysis 6.10). No studies provided information on maternal anaemia at term, maternal infection or any of our other prespecified maternal outcomes.
6.10. Analysis.
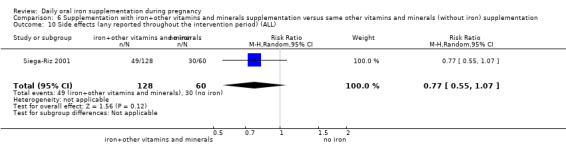
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 10 Side effects (any reported throughout the intervention period) (ALL).
Infant secondary outcomes
There were no data reported for our remaining infant secondary outcomes.
Maternal secondary outcomes
Two studies with 809 women reported on mean maternal Hb levels at term and women receiving iron were more likely to have higher Hb levels compared with those without iron (average RR 10.85; 95% CI 7.29 to 14.42) (Analysis 6.22). Cantlie 1971 also reported on mean maternal Hb levels in the postpartum period and women receiving iron in addition to other vitamins and minerals were more likely to have higher Hb levels compared with those receiving other vitamins and minerals without iron (MD 14.00; 95% CI 3.56 to 24.44) (Analysis 6.23).
6.22. Analysis.
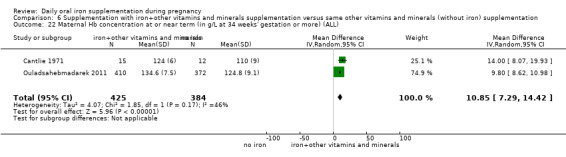
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 22 Maternal Hb concentration at or near term (in g/L at 34 weeks' gestation or more) (ALL).
6.23. Analysis.
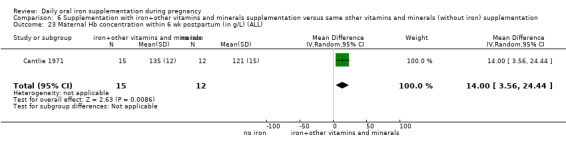
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 23 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL).
Siega‐Riz 2001 reported on side effects; there were no differences between groups in terms of the number of women suffering constipation, vomiting or heartburn (Analysis 6.33; Analysis 6.35; Analysis 6.36). Women in the iron supplemented group were slightly more likely to experience diarrhoea (Analysis 6.37).
6.33. Analysis.
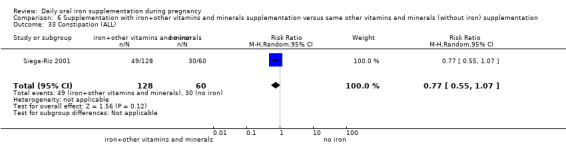
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 33 Constipation (ALL).
6.35. Analysis.
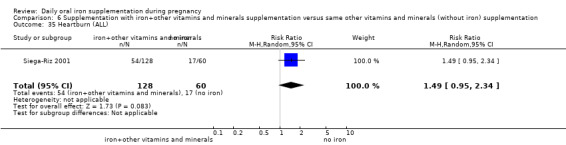
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 35 Heartburn (ALL).
6.36. Analysis.
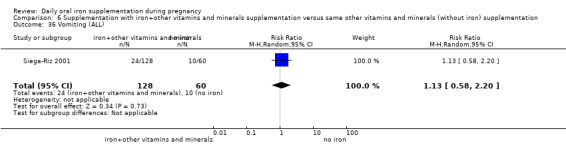
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 36 Vomiting (ALL).
6.37. Analysis.
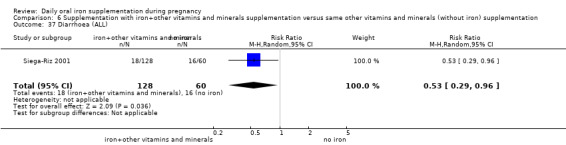
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 37 Diarrhoea (ALL).
Ouladsahebmadarek 2011 reported on placental abruption, premature rupture of the membranes and pre‐eclampsia for 782 women; there were no significant differences between groups for any of these outcomes (Analysis 6.39; Analysis 6.40; Analysis 6.41).
6.39. Analysis.
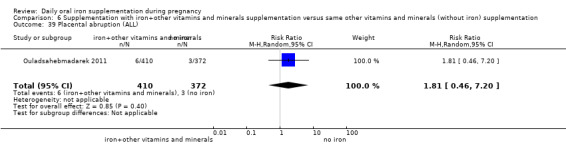
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 39 Placental abruption (ALL).
6.40. Analysis.
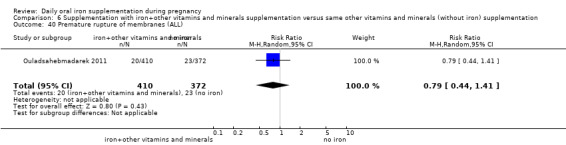
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 40 Premature rupture of membranes (ALL).
6.41. Analysis.
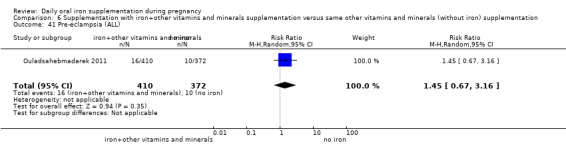
Comparison 6 Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation, Outcome 41 Pre‐eclampsia (ALL).
No information was reported on our remaining maternal secondary outcomes.
(7) Daily oral iron + folic acid + other vitamins and minerals supplementation versus daily oral folic acid + same other vitamins and minerals (without iron) supplementation (no studies)
No studies compared women receiving daily oral iron + folic acid + other vitamins and minerals supplementation versus daily oral folic acid + same other vitamins and minerals (without iron) supplementation.
(8) Daily oral iron + folic acid + other vitamins and minerals supplementation versus daily oral same other vitamins and minerals (without iron nor folic acid) supplementation (no studies)
No studies compared women receiving daily oral iron + folic acid + other vitamins and minerals with women receiving other vitamins and minerals (without either folic acid or iron).
Discussion
Summary of main results
We have set out a summary of our main findings along with an overall assessment of the quality of the evidence in additional tables (Table 1; Table 2; Table 3; Table 4).
Forty‐four trials compared the effects of daily oral supplements containing iron versus no iron or placebo. The majority of them (35) compared arms receiving iron alone versus no treatment and placebo. Compared with controls, women taking iron supplements were less likely to have low birthweight and preterm newborns and have heavier babies although these findings did not reach statistical significance. Results also suggest that babies born to mothers receiving iron were less likely to be born before 34 weeks' gestation. For other infant outcomes there were no clear differences between groups.
Regarding maternal outcomes, women receiving iron compared with those receiving no treatment or placebo were less likely to be anaemic at term (13.06% versus 35.71%) and were less likely to have iron deficiency (28.50% versus 51.33%) and iron‐deficiency anaemia at term (4.37% versus 13.18%). Women who received iron supplements appeared more likely than controls to report side effects (25.30% versus 9.91%), although this was not statistically significant. Participants also had increased risk of high haemoglobin (Hb) concentrations at any time during second or third trimester and at term. Women receiving iron were also on average more likely to have higher Hb levels at term and in the postpartum period. For several outcomes where there was evidence of differences between groups, the size of the treatment effect in individual studies varied considerably, and so our results should be interpreted with caution.
Only nine trials compared the effects of daily iron + folic acid supplementation with the effects of same supplements without iron + folic acid. There were clear positive effects on maternal haematological status while the effects on infant outcomes were uncertain.
Overall completeness and applicability of evidence
This review included 61 randomised controlled trials carried out since 1936 in 27 countries across the globe. Trials were mostly conducted during the last 20 years. There was some equilibrium between the trials that included non‐anaemic women and those focused on populations with high prevalence of anaemia as well among the trials assessing early or late gestational iron supplementation. Although it was not possible to extract data from all the trials, these numbers clearly reflect the wide applicability of this review.
We addressed the effects of the use of iron or iron + folic acid by pregnant women, either provided alone or in combination with other vitamins and minerals. The effects can be determined if the differences between the comparison groups relies only in the presence of iron or iron + folic acid, that is, we are estimating the effects of the addition of iron or iron + folic acid to the pregnant women independently of any other co‐interventions given to both groups being compared.
Most of the trials focused primarily on maternal changes in Hb and on some haematological indices after a certain period of supplementation. The results consistently show that iron supplementation in pregnancy improves maternal haematological outcomes independently of the dosage. However, those women who consumed higher amounts of iron (60 mg of iron or more per day) tended to have higher Hb values at the end or near term of pregnancy. In some cases, women reached levels above the threshold of 130 g/L at sea level which may be associated with negative pregnancy outcomes, including preterm birth, low birthweight and pre‐eclampsia. Although the clinical significance of high Hb concentration is still being debated, it seems sensible to provide supplements with lower iron concentrations to those populations with lower prevalence of anaemia and iron deficiency.
Side effects are also a clear drawback to most current iron compounds used as supplements, either alone or with folic acid. The results of this review suggest that women who consume daily supplements containing 60 mg of elemental iron or more may be more likely to report side effects, particularly diarrhoea, than those who consume lower doses per day although differences between subgroups were not statistically significant. This concurs with the Institute of Medicine's approach which set 45 mg of elemental iron as the upper tolerable limit per day based on the likelihood of having side effects (IOM 2001). As a result, investigators are now testing highly bioavailable iron compounds (e.g. FeNaEDTA) that may produce fewer side effects and that can be administered at low doses, but their information in pregnant women is still limited.
This updated version includes two new trials, showing that the amount of evidence in this area grows slowly. Although the results indicate that iron may have positive effects on infant outcomes, the effects on low birthweight and infant weight at birth are less clear than in the previous version of this review and no longer reached statistical significance. There are two possible reasons for this. First, trials were conducted in areas where the background risk for low birthweight is not as high as in previous studies and thus the effect of supplements is less prominent. Secondly, the selection of random‐effects as analytical model results in broader confidence intervals than a fixed‐effect model and gives less weight to large trials with a large number of events. In the previous version, a single trial reporting an 18% reduction in low birthweight was responsible of 46% of the overall effect in this outcome while in this version the contribution of such trial was diluted to 33%.
Quality of the evidence
The overall quality of the evidence in this review is mixed, with many studies being at risk of bias. In more than half of the included trials the methods used to conceal allocation were not described. Blinding of women, care providers and outcome assessors was not attempted in more than a third of trials, although in some studies technical staff carrying out laboratory investigations were reported to be unaware of group allocation. While for some outcomes (e.g. infant birthweight), the lack of blinding may have been unlikely to have had any impact on results, for others (e.g. maternal reports of side effects to care providers), lack of blinding may represent a potentially serious source of bias. Attrition was a problem in some studies and it was not always clear that loss was balanced across groups.
The overall quality of the evidence for iron supplementation versus no iron was moderate for birthweight, preterm birth and maternal infection. The evidence was rated as low quality for low birthweight, neonatal death, congenital anomalies, maternal severe anaemia, and infections during pregnancy, maternal anaemia at term and maternal iron deficiency at term; whereas, it was of very low quality for maternal death and side effects (seeTable 1).
The overall quality of the evidence for iron + folic acid supplementation versus no iron + folic acid was moderate for maternal anaemia at term, side effects and low birthweight. The evidence was of low or very low quality for other outcomes due to imprecision and heterogeneity (seeTable 2).
Potential biases in the review process
We were aware of the possibility of introducing bias at every stage of the reviewing process. In this updated review, we tried to minimise bias in a number of ways; two review authors assessed eligibility for inclusion, carried out data extraction and assessed risk of bias. Each worked independently. Nevertheless, the process of assessing risk of bias, for example, is not an exact science and includes many personal judgements. Further, the process of reviewing research studies is known to be affected by prior beliefs and attitudes. It is difficult to control for this type of bias in the reviewing process.
While we attempted to be as inclusive as possible in the search strategy, the literature identified was predominantly written in English and published in North American and European journals. Although we did attempt to assess reporting bias, constraints of time meant that this assessment largely relied on information available in the published trial reports and thus, reporting bias was not usually apparent.
Assessing the quality of the evidence relating to specific outcomes is a difficult process, but we attempted to produce 'Summary of findings' tables using a transparent process. Two review authors independently assessed the evidence for each outcome for each quality domain and discussed any disagreements. The inclusion of the new trials modified the overall quality of the evidence in low birthweight from moderate to low.
Agreements and disagreements with other studies or reviews
Iron supplementation to pregnant women has been a long standing public health intervention that has been subject to multiple reviews, some of which also include a meta‐analysis. In general, those meta‐analyses tend to report the results in a segmented manner. Most of them are focused only on maternal anaemia (Sloan 2002; Yakoob 2011), while others also include a few infant outcomes (Imdad 2012). This topic has also been studied from the social determinants perspective (Nagata 2011). Our results are not in agreement with a recent systematic review (Cantor 2015) that did not find conclusive evidence on whether routine prenatal iron supplementation improved maternal or infant clinical health outcomes, but only might improve maternal haematologic indices. This systematic review included only English‐language articles and addressed other aspects such as the benefits or harms of screening iron deficiency anaemia in pregnant women. Unlike our review, the authors included also non‐randomised, controlled trials; and cohort studies addressing their questions and excluded what authors had assessed as poor‐quality studies if deemed good‐ and fair‐quality studies were available.
A recent overview of reviews on the prevention and treatment of maternal anaemia identified 11 systematic reviews assessing the effects of iron and folic acid supplementation during the antenatal period, but only five were deemed as high quality, using A Measurement Tool to Assess Systematic Reviews (short AMSTAR) as the assessment tool for methodological quality (Parker 2012).
This Cochrane review is the most comprehensive assessment on the effects of daily iron supplementation on both maternal and infant outcomes. After two updates, there is consistent evidence that providing iron supplements to pregnant women as part of the antenatal care helps improve gestational outcomes and that these benefits can be observed at lower iron doses than usual, with less side effects.
Authors' conclusions
Implications for practice.
Available data from 44 studies indicate that in comparison with receiving no iron or a placebo, women receiving daily iron supplements had:
lower risk of anaemia at term;
higher haemoglobin (Hb) concentrations at term and six weeks postpartum. Women who received higher iron doses tended to have the highest Hb concentrations;
higher risk of high Hb concentrations during the second and third trimesters of pregnancy;
borderline lower risk of delivering low birthweight babies;
borderline lower risk of giving birth to infants less than 37 weeks' gestation;
lower risk of giving birth to infants less than 34 weeks' gestation.
The lack of data impeded any evaluation of the effects of iron supplementation on maternal mortality.
Relatively few studies assessed the combined effects of iron and folic acid on maternal and infant outcomes. There were clear positive effects on maternal haematological status while the effects on infant outcomes were uncertain.
Supplementation with iron to pregnant women may be used as a preventive strategy to improve maternal and infant outcomes in all settings, although the magnitude of the effect may vary depending on the background risk of anaemia and low birthweight. In malaria endemic areas, it seems sensible to complement iron and folic acid supplementation programmes with measures to prevent, diagnose and treat malaria. In order to improve the success of this intervention in public health, it is important to encourage the establishment of logistic procedures that facilitate and improve accessibility to supplements and foster compliance.
Implications for research.
On the basis of the results of this review, researchers could consider investigating the following points regarding the use of iron or iron + folate supplements by pregnant women:
identify the mechanisms involved in high Hb concentrations during various gestational ages and its functional consequences;
the effects of providing other micronutrients than iron and folic acid on maternal and infant outcomes;
the assessment of effectiveness, safety, and affordability of novel iron supplementation compounds for use in public health pre‐pregnancy and prenatal preventive supplementation programmes.
A better documentation of haematological indicators pre and post intervention, congenital anomalies, and side and adverse effects, including malaria‐related outcomes, is encouraged.
Feedback
Hemminki, June 2008
Summary
My trial, Hemminki 1989a, is excluded from this review and it is not clear why. The comment in Characteristics of excluded studies is "Only women who were anaemic received iron in the unsupplemented group thus making any comparisons among the groups biased for the purposes of this review." What bias is being referred to? Hemminki 1989a was in the previous version of this review. It was a randomised trial, analysed by intention to treat, having outcome data for all women randomised, and a high compliance (about 80% of women in both groups received the treatment they were allocated to). The 20% of women who received iron in the non‐routine supplementation group was as expected. There are two options for dealing with women whose haemoglobin falls below a pre‐specified cut‐off in the non‐routine supplemented group: 1. give them iron, as in my study where 20% of women in the non‐routine treatment group had iron; or 2. call those who take iron non‐compliant and do the analysis by intention to treat, as did some of the included studies.
What is the difference between these two strategies? They seem to me to be essentially the same.
The effect of routine iron therapy on substantive health outcomes remains unclear. It is a real pity that you have excluded Hemminki 1989a, based on criteria I consider inappropriate: it had a large number of women, several health outcomes including long term follow up, and was well conducted.
A minor issue is that it is misleading to call this trial Hemminki 1989a. Although the study design was published in 1989, the main results were not published until 1991. Hence a more appropriate study identifier would be ‘Hemminki 1991’.
(Summary of feedback from Elina Hemminki, June 2008)
Reply
We agree that your trial was well conducted, had a large number of women and looked at several health outcomes including long term follow up. We did review all publications on the work you have conducted on assessing the effects of routine versus selective iron supplementation during pregnancy. This systematic review aims to assess the effectiveness and safety of daily and intermittent use of iron supplements by pregnant women, either alone or in conjunction with folic acid given as a preventive universal measure. Your trial provided 100 mg of elemental iron daily with various choice of iron compounds and dosage as determined individually by the midwives to all women in the routine iron supplementation group. For women in the "selective iron supplementation group", treatment with iron supplements as slow release form for two months or until the hematocrit increased to 0.32 was provided only to those whose hematocrit was lower than 0.30 on two consecutive visits. Consequently, we have included your trial in the included studies and we thank you for the additional data you have provided us for this analysis. Your study compared the effects of routine versus selective iron supplementation, an issue that certainly deserves better understanding and that reflects current practices.
We have changed the study identifier to Hemminki 1991 as requested.
Contributors
Juan Pablo Peña‐Rosas, MD, PhD, MPH
What's new
| Date | Event | Description |
|---|---|---|
| 5 March 2015 | New citation required but conclusions have not changed | For most of the primary outcomes results have not changed since the previous version. Effects on low birthweight, formerly borderline significant, are no longer so. |
| 5 March 2015 | New search has been performed | The review has been updated and a new author has joined the review team. Two new studies have been included (Korkmaz 2014; Liu 2012) and one study that was previously included has now been excluded after discussions among the review authors (Hemminki 1991). The review now includes a total of 61 trials. |
History
Protocol first published: Issue 2, 2004 Review first published: Issue 3, 2006
| Date | Event | Description |
|---|---|---|
| 1 November 2012 | New citation required and conclusions have changed | This review updates part of Peña‐Rosas 2009 to only evaluate the effects of oral daily iron supplementation regimens. The effects of intermittent iron supplementation regimens are evaluated in a separate review (Peña‐Rosas 2012a). |
| 2 July 2012 | New search has been performed | In this split review we updated the search and used the latest Cochrane methodological guidance. We included information on the health worker cadre and malaria setting. Specific changes to the previous version are described in the section Differences between protocol and review. Two new authors have contributed to this review. |
| 16 June 2009 | New search has been performed | Search updated. Ten new trials included (Cantlie 1971; Christian 2003 (C); Hemminki 1991a; Harvey 2007;Lee 2005; Meier 2003; Mukhopadhyay 2004; Siega‐Riz 2001; Ziaei 2007; Ziaei 2008). One trial included is now excluded (Ortega‐Soler 1998). Twenty‐seven new trials excluded. |
| 16 June 2009 | New citation required but conclusions have not changed | In this update, trials assessing the effect of iron or folic acid when given in combination with other micronutrients were included as long as both groups being compared in the daily regimens received the same other micronutrient interventions. This has resulted in four trials previously excluded now being included (Cantlie 1971; Christian 2003 (C); Hemminki 1991a; Siega‐Riz 2001). |
| 20 October 2008 | Feedback has been incorporated | Feedback from Elina Hemminki added with response from author. |
| 15 April 2008 | Amended | Converted to new review format. |
Notes
We have again gone through the inclusion criteria for all the trials identified in the search strategy and those included and excluded in previous versions of this review, now in an updated version after its split into two reviews to assess the effects of daily iron supplementation and intermittent iron supplementation for women during pregnancy as a preventive strategy. The study by Hemminki 1991 evaluates selective (providing iron only if participants become anaemic at any point during the study period) versus routine provision of iron supplements (providing iron to all participants independently of their haemoglobin (Hb) or ferritin concentrations). After careful discussions we have decided to exclude this study from this version of the review, as it in fact dealing with treatment of iron‐deficiency anaemia, a topic covered in another review in comparison to preventive provision as here. Participants in the routine group received iron throughout pregnancy regardless of Hb level, starting at the latest in the 17th week of gestation. A dose of 100 mg elemental iron per day was recommended, but this could be tailored according to the midwife's judgment. Participants in the selective group were any pregnant women after the 14th week of gestation showing a hematocrit (HCT) < 0.30 (Hb < 100 g/L) in two consecutive visits. If the Hb was still less than 100 g/L and/or mean cellular volume (MCV) was less than 82, and a low ferritin was found, 50 mg iron twice a day as ferrous sulphate was recommended. The length of the treatment was to be two months or until the HCT was >10.32 or higher (Hb 110 g/L) or higher). By request of the midwives, the treatment schedule was relaxed later during the trial: iron therapy was begun if the mother's HCT was 0.31 or below after the 33rd week. The participants received different doses of iron and also different iron compounds as decided by the health cadre workers following prenatal care. This study cannot be analysed as the same intervention as the studies randomised to receive or not receive the iron supplement or a placebo or no supplementation. We have thus agreed to exclude this study from the review and describe well the reasons for exclusion in the Characteristics of excluded studies.
Acknowledgements
We would like to thank the trial authors who have contributed additional data for this review; and Richard Riley and Simon Gates who provided statistical advice. In addition, we would like to thank the staff at the editorial office of the Cochrane Pregnancy and Childbirth Group in Liverpool for their support in the preparation of this review and, in particular, Professor Zarko Alfirevic.
We would like to thank Fernando Viteri for his contribution to co‐writing the initial protocol and first two versions of the review, for providing technical support and guidance on earlier versions, and for commenting on the current update (2015).
The World Health Organization (WHO) and Juan Pablo Peña‐Rosas, Luz Maria De‐Regil, Maria N Garcia‐Casal, and Therese Dowswell retain copyright and all other rights in their respective contributions to the manuscript of this updated review as submitted for publication.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Search terms used for additional author searching
Review authors searched the WHO International Clinical Trials Registry Platform (ICTRP) for any ongoing or planned trials on 26 February 2015 using the terms "iron supplementation and pregnancy"; "iron and pregnancy"; "daily iron and pregnancy"; "iron supplements and pregnancy"; "daily supplements and pregnancy" and "anaemia and pregnancy". Duplicates were removed.
Data and analyses
Comparison 1. Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 11 | 17613 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.03] |
| 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 11 | 17613 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.03] |
| 2.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 6 | 14512 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.59, 1.05] |
| 2.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 3 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.50, 2.19] |
| 2.3 Unspecified or mixed gestational age at the start of supplementation | 2 | 2436 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.61, 1.24] |
| 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 11 | 17613 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.03] |
| 3.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Non‐anaemic at the start of supplementation | 8 | 13843 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.51, 1.22] |
| 3.3 Unspecified or mixed anaemia status | 3 | 3770 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.72, 0.94] |
| 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron | 11 | 17613 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.03] |
| 4.1 Low daily dose of iron (30 mg or less of elemental iron) | 5 | 12858 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.38, 1.32] |
| 4.2 Medium daily dose of iron (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.57, 2.54] |
| 4.3 Higher daily dose of iron (60 mg elemental iron or more) | 5 | 4028 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.72, 0.94] |
| 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting | 11 | 17613 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.03] |
| 5.1 Malarial setting | 5 | 4645 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.73, 0.94] |
| 5.2 Non‐malarial setting | 6 | 12968 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.42, 1.33] |
| 6 Birthweight (g) (ALL) | 15 | 18590 | Mean Difference (IV, Random, 95% CI) | 23.75 [‐3.02, 50.51] |
| 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 15 | 18590 | Mean Difference (IV, Random, 95% CI) | 23.75 [‐3.02, 50.51] |
| 7.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 11 | 15583 | Mean Difference (IV, Random, 95% CI) | 28.55 [‐9.85, 66.95] |
| 7.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 3 | 681 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐77.46, 77.08] |
| 7.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2326 | Mean Difference (IV, Random, 95% CI) | 20.20 [‐15.13, 55.53] |
| 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 15 | 18590 | Mean Difference (IV, Random, 95% CI) | 23.75 [‐3.02, 50.51] |
| 8.1 Anaemic at start of supplementation | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Non‐anaemic at the start of supplementation | 11 | 14631 | Mean Difference (IV, Random, 95% CI) | 20.24 [‐20.13, 60.61] |
| 8.3 Unspecified or mixed anaemia status | 4 | 3959 | Mean Difference (IV, Random, 95% CI) | 33.02 [3.65, 62.38] |
| 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron | 15 | 18590 | Mean Difference (IV, Random, 95% CI) | 23.49 [‐2.55, 49.52] |
| 9.1 Low daily dose (30 mg or less of elemental iron) | 7 | 13729 | Mean Difference (IV, Random, 95% CI) | 33.94 [‐13.42, 81.29] |
| 9.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Mean Difference (IV, Random, 95% CI) | 10.0 [‐51.92, 71.92] |
| 9.3 Higher daily dose (60 mg elemental iron or more) | 8 | 4134 | Mean Difference (IV, Random, 95% CI) | 19.18 [‐26.63, 64.99] |
| 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting | 15 | 18590 | Mean Difference (IV, Random, 95% CI) | 23.75 [‐3.02, 50.51] |
| 10.1 Malarial setting | 6 | 5443 | Mean Difference (IV, Random, 95% CI) | 33.48 [10.58, 56.37] |
| 10.2 Non‐malarial setting | 9 | 13147 | Mean Difference (IV, Random, 95% CI) | 8.06 [‐57.13, 73.25] |
| 11 Preterm birth (less than 37 weeks of gestation) (ALL) | 13 | 19286 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 12 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 13 | 19286 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 12.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 10 | 16483 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.86, 1.07] |
| 12.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 2 | 477 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.29, 1.13] |
| 12.3 Unspecified or mixed`gestational age at the start of supplementation | 1 | 2326 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.09] |
| 13 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 13 | 19286 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 13.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Non‐anaemic at the start of supplementation | 10 | 14837 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.81, 1.04] |
| 13.3 Unspecified/ mixed anaemia status | 3 | 4449 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.81, 1.14] |
| 14 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron | 13 | 19286 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 14.1 Low daily dose (30 mg or less of elemental iron) | 6 | 13649 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.76, 1.05] |
| 14.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.62, 2.56] |
| 14.3 Higher daily dose (60 mg elemental iron or more) | 6 | 4910 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.81, 1.12] |
| 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting | 13 | 19286 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 15.1 Malarial setting | 7 | 6406 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.82, 1.11] |
| 15.2 Non‐malarial setting | 6 | 12880 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.65, 1.09] |
| 16 Neonatal death (within 28 days after delivery) (ALL) | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 17 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 17.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 3 | 14108 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.71, 1.42] |
| 17.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2495 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.56, 1.19] |
| 18 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 18.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18.2 Non‐anaemic at the start of supplementation | 2 | 12559 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.51, 1.77] |
| 18.3 Unspecified or mixed anaemia status | 2 | 4044 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.65, 1.19] |
| 19 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 19.1 Low daily dose (30 mg or less of elemental iron) | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.82] |
| 19.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.12, 1.91] |
| 19.3 Higher daily dose (60 mg elemental iron or more) | 2 | 4044 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.65, 1.19] |
| 20 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 20.1 Malarial setting | 3 | 4771 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.63, 1.15] |
| 20.2 Non‐malarial setting | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.82] |
| 21 Congenital anomalies (ALL) | 4 | 14636 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.58, 1.33] |
| 22 Congenital anomalies: SUBGROUP ANALYSIS by gestational age at the start of supplementation) | 4 | 14636 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.58, 1.33] |
| 22.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 4 | 14636 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.58, 1.33] |
| 22.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22.3 Unspecified or mixed gestational age at the start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Congenital anomalies: SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 14636 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.58, 1.33] |
| 23.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 Non‐anaemic at the start of supplementation | 2 | 12234 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.35, 2.84] |
| 23.3 Unspecified or mixed anaemia status | 2 | 2402 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.55, 1.35] |
| 24 Congenital anomalies: SUBGROUP ANALYSIS by dose of iron | 4 | 14636 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.58, 1.33] |
| 24.1 Low daily dose (30 mg or less of elemental iron) | 1 | 11934 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.35, 2.84] |
| 24.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.3 Higher daily dose (60 mg elemental iron or more) | 3 | 2702 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.55, 1.35] |
| 25 Congenital anomalies: SUBGROUP ANALYSIS by malarial status of setting | 4 | 14633 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.62, 1.26] |
| 25.1 Malarial setting | 3 | 2699 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.60, 1.26] |
| 25.2 Non‐malarial setting | 1 | 11934 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.35, 2.84] |
| 26 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 27 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation): | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 27.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 7 | 749 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.12, 0.70] |
| 27.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 5 | 1178 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.22, 0.61] |
| 27.3 Unspecified or mixed gestational age | 2 | 272 | Risk Ratio (M‐H, Random, 95% CI) | 0.08 [0.01, 0.59] |
| 28 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation) | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 28.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28.2 Non‐anaemic at the start of supplementation | 8 | 1295 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.16, 0.64] |
| 28.3 Unspecified or mixed anaemia status | 6 | 904 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.12, 0.49] |
| 29 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron) | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 29.1 Low daily dose (30 mg or less of elemental iron) | 3 | 590 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.24, 1.03] |
| 29.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.06, 0.73] |
| 29.3 Higher daily dose (60 mg elemental iron or more) | 10 | 1540 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.14, 0.45] |
| 30 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting) | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 30.1 Malarial setting | 3 | 530 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.45, 0.82] |
| 30.2 Non‐malarial setting | 11 | 1669 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.10, 0.34] |
| 31 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks's gestation or more) (ALL) | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 32 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 32.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 4 | 653 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.22, 0.93] |
| 32.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 3 | 603 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.18, 0.72] |
| 32.3 Unspecified or mixed gestational age | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 33.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33.2 Non‐anaemic at the start of supplementation | 5 | 1092 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.39, 0.82] |
| 33.3 Unspecified/ mixed anaemia status | 2 | 164 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.07, 0.29] |
| 34 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 34.1 Low daily dose (30 mg or less of elemental iron) | 3 | 703 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.34, 0.78] |
| 34.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.73, 1.17] |
| 34.3 Higher daily dose (60 mg elemental iron or more) | 3 | 312 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.10, 0.41] |
| 35 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 35.1 Malarial setting | 2 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.53] |
| 35.2 Non‐malarial setting | 5 | 1064 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.30, 0.78] |
| 36 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 37 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 37.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 4 | 660 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.13, 1.11] |
| 37.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 2 | 428 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.11, 0.58] |
| 37.3 Unspecified or mixed gestational age | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 38.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38.2 Non‐anaemic at the start of supplementation | 5 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.20, 0.74] |
| 38.3 Unspecified or mixed anaemia status | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.00, 0.72] |
| 39 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 39.1 Low daily dose (30 mg or less of elemental iron) | 3 | 579 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.13, 1.11] |
| 39.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.16, 0.70] |
| 39.3 Higher daily dose (60 mg elemental iron or more) | 2 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.00, 0.72] |
| 40 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 40.1 Malarial setting | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.2 Non‐malarial setting | 5 | 940 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 41 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 2 | 12560 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 8.19] |
| 42 Side effects (any reported throughout the intervention period) (ALL) | 11 | 2423 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.83, 2.02] |
| 43 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by gestational age at the start of supplementation: | 11 | 2423 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.92, 1.91] |
| 43.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 5 | 1186 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.68, 1.45] |
| 43.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 5 | 1032 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.89, 2.29] |
| 43.3 Unspecified or mixed gestational age | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 62.79 [3.89, 1013.31] |
| 44 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 11 | 2423 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.92, 1.91] |
| 44.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 44.2 Non‐anaemic at the start of supplementation | 7 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.85, 1.20] |
| 44.3 Unspecified or mixed anaemia status | 4 | 775 | Risk Ratio (M‐H, Random, 95% CI) | 5.16 [0.78, 34.29] |
| 45 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by dose of iron | 11 | 2423 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.93, 1.89] |
| 45.1 Low daily dose (30 mg or less of elemental iron) | 6 | 1533 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.86, 1.16] |
| 45.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 2 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.66, 6.02] |
| 45.3 Higher daily dose (60 mg elemental iron or more) | 5 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 4.33 [0.61, 30.67] |
| 46 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by malarial status of setting | 11 | 2423 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.92, 1.91] |
| 46.1 Malarial setting | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 62.79 [3.89, 1013.31] |
| 46.2 Non‐malarial setting | 10 | 2218 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.91, 1.63] |
| 47 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 9 | 2125 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 3.20] |
| 48 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 9 | 2125 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 3.20] |
| 48.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 5 | 1417 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.47] |
| 48.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 3 | 559 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.00, 46.15] |
| 48.3 Unspecified or mixed gestational age | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 49 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 9 | 2125 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 3.20] |
| 49.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 49.2 Non‐anaemic at the start of supplementation | 5 | 1394 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 49.3 Unspecified or mixed anaemia status | 4 | 731 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.30] |
| 50 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron | 9 | 2125 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 3.20] |
| 50.1 Low daily dose (30 mg or less of elemental iron) | 3 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 50.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 50.3 Higher daily dose (60 mg elemental iron or more) | 5 | 744 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.30] |
| 51 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting | 9 | 2125 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 3.20] |
| 51.1 Malarial setting | 3 | 1102 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.30] |
| 51.2 Non‐malarial setting | 6 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 52 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 53 Infection during pregnancy (including urinary tract infections) (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 54 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 54.1 Early gestational age (supplementation started before 20 weeks' gestation or prior to pregnancy) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 54.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 54.3 Unspecified or mixed gestational age | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 55 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 55.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 55.2 Non‐anaemic at the start of supplementation | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 55.3 Unspecified or mixed anaemia status | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 56 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by dose of iron | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 56.1 Low daily dose (30 mg or less of elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 56.2 Medium daily dose (more than 30 mg and less than 60 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 56.3 Higher daily dose (60 mg elemental iron or more) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 57 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by malarial status of setting | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 57.1 Malarial setting | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 57.2 Non‐malarial setting | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 58 Very low birthweight (less than 1500 g) (ALL) | 5 | 2687 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.31, 1.74] |
| 59 Very premature birth (less than 34 weeks' gestation) (ALL) | 5 | 3743 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.29, 0.91] |
| 60 Infant Hb concentration within the first 6 months (in g/L counting the last reported measure after birth within this period) (ALL) | 2 | 533 | Mean Difference (IV, Random, 95% CI) | ‐1.25 [‐8.10, 5.59] |
| 61 Infant serum ferritin concentration within first 6 months (in μg/L counting the last reported measure after birth within this period) (ALL) | 1 | 197 | Mean Difference (IV, Random, 95% CI) | 11.0 [4.37, 17.63] |
| 62 Admission to special care unit (ALL) | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 14 | 2199 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.19, 0.46] |
| 64 Maternal iron deficiency at or near term (as defined by as defined by trialists, based on any indicator of iron status at 34 weeks's gestation or more)) (ALL) | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 65 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 66 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL) | 19 | 3704 | Mean Difference (IV, Random, 95% CI) | 8.88 [6.96, 10.80] |
| 67 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL) | 7 | 956 | Mean Difference (IV, Random, 95% CI) | 7.61 [5.50, 9.72] |
| 68 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 9 | 2188 | Risk Ratio (M‐H, Random, 95% CI) | 2.37 [1.34, 4.21] |
| 69 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 8 | 2156 | Risk Ratio (M‐H, Random, 95% CI) | 3.07 [1.18, 8.02] |
| 70 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL) | 8 | 1819 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.01, 44.11] |
| 71 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 8 | 1339 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.01, 0.28] |
| 72 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 3 | 766 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.12, 2.51] |
| 73 Puerperal infection (ALL) | 4 | 4374 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.50, 0.92] |
| 74 Antepartum haemorrhage (ALL) | 2 | 1157 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.51, 4.31] |
| 75 Postpartum haemorrhage (ALL) | 4 | 1488 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.59, 1.49] |
| 76 Transfusion provided (ALL) | 2 | 759 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.10, 8.98] |
| 77 Diarrhoea (ALL) | 3 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.32, 0.93] |
| 78 Constipation (ALL) | 4 | 1495 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.62, 1.43] |
| 79 Nausea (ALL) | 4 | 1377 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.72, 2.03] |
| 80 Heartburn (ALL) | 3 | 1323 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.86, 1.66] |
| 81 Vomiting (ALL) | 4 | 1392 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.59, 1.30] |
| 82 Maternal wellbeing/satisfaction (ALL) | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.77, 1.08] |
| 83 Placental abruption (ALL) | 3 | 2951 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.56, 3.59] |
| 84 Premature rupture of membranes (ALL) | 3 | 1581 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.72, 1.22] |
| 85 Pre‐eclampsia (ALL) | 4 | 1704 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.87, 3.07] |
1.11. Analysis.
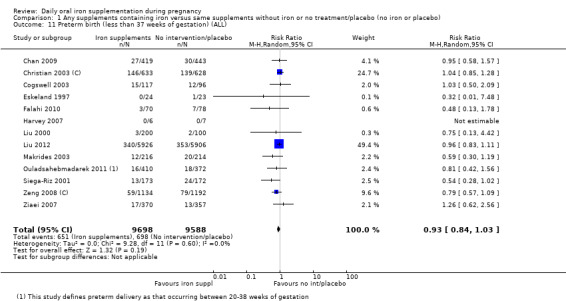
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 11 Preterm birth (less than 37 weeks of gestation) (ALL).
1.22. Analysis.
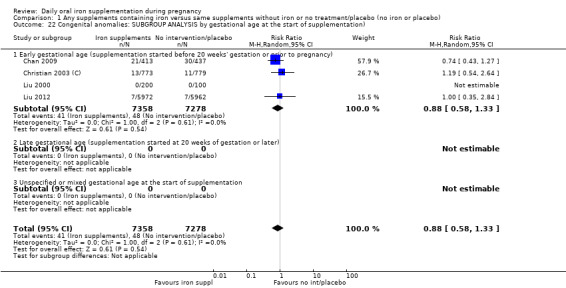
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 22 Congenital anomalies: SUBGROUP ANALYSIS by gestational age at the start of supplementation).
1.23. Analysis.
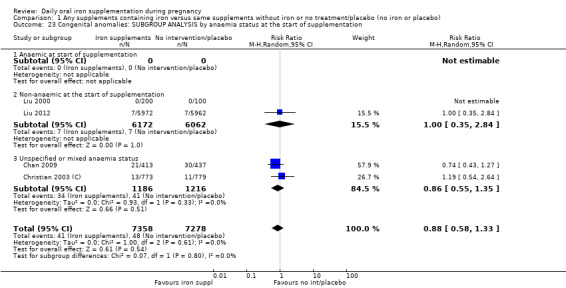
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 23 Congenital anomalies: SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.24. Analysis.
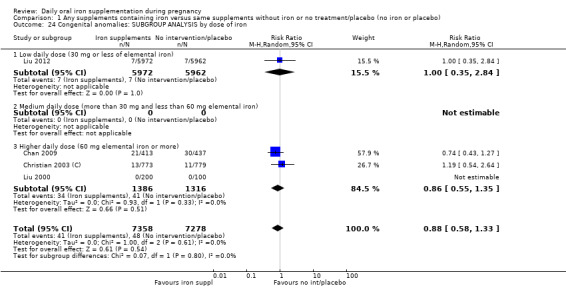
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 24 Congenital anomalies: SUBGROUP ANALYSIS by dose of iron.
1.25. Analysis.
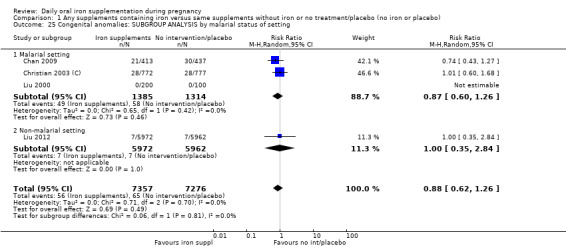
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 25 Congenital anomalies: SUBGROUP ANALYSIS by malarial status of setting.
1.32. Analysis.
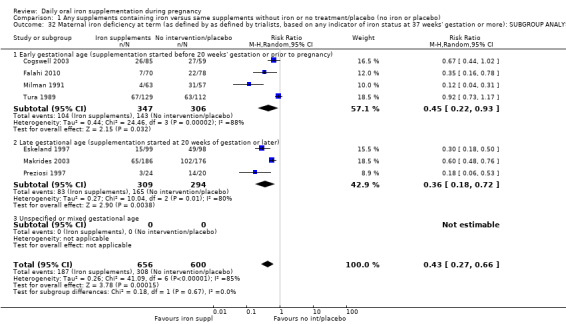
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 32 Maternal iron deficiency at term (as defined by as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.35. Analysis.
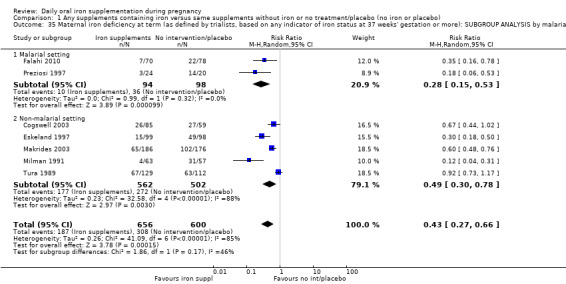
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 35 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
1.36. Analysis.
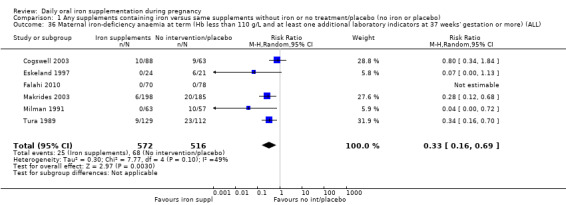
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 36 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL).
1.47. Analysis.
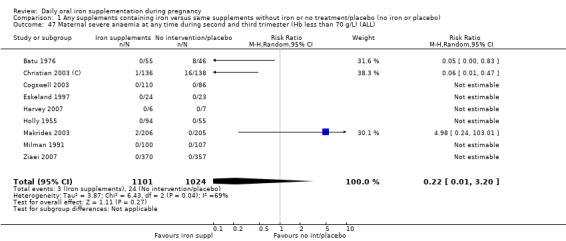
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 47 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL).
1.48. Analysis.
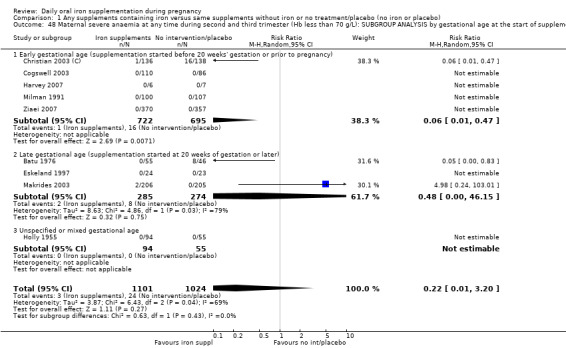
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 48 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.49. Analysis.
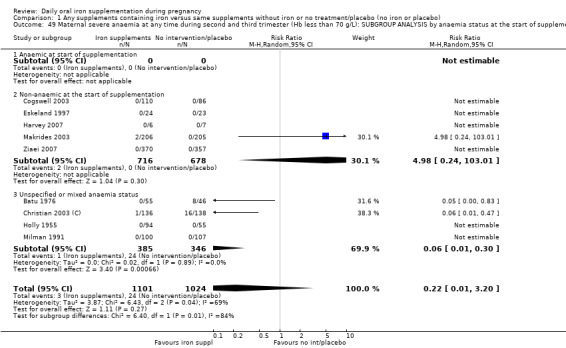
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 49 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.50. Analysis.
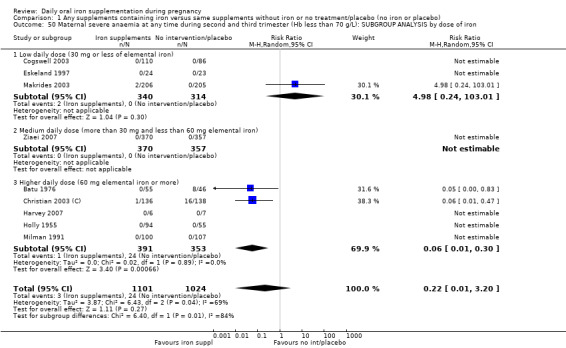
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 50 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron.
1.51. Analysis.
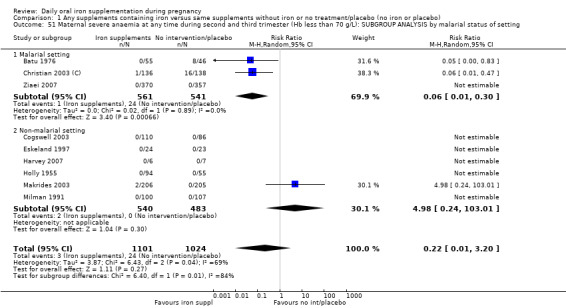
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 51 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting.
1.54. Analysis.
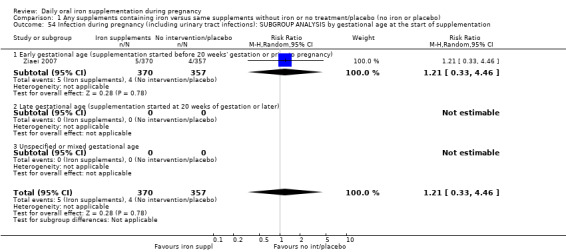
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 54 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
1.55. Analysis.
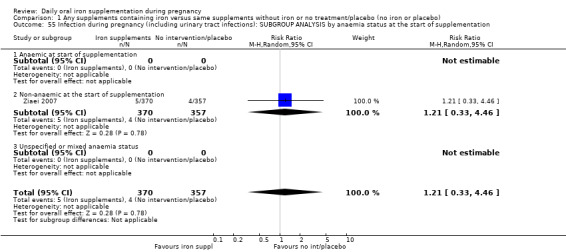
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 55 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
1.56. Analysis.
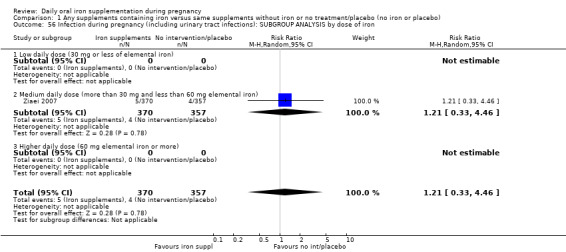
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 56 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by dose of iron.
1.57. Analysis.
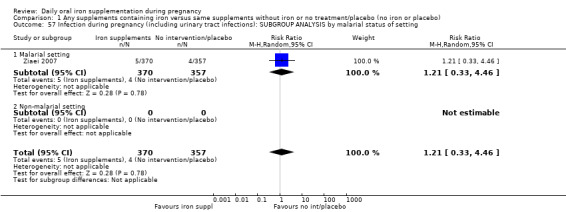
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 57 Infection during pregnancy (including urinary tract infections): SUBGROUP ANALYSIS by malarial status of setting.
1.58. Analysis.
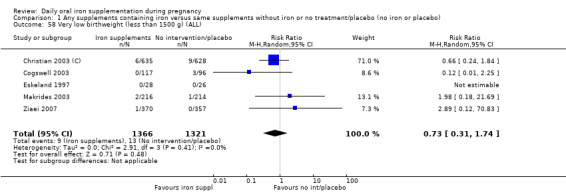
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 58 Very low birthweight (less than 1500 g) (ALL).
1.60. Analysis.
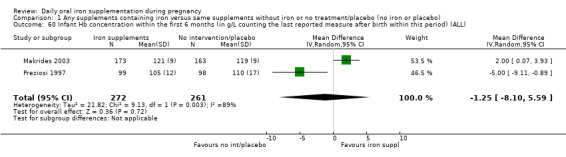
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 60 Infant Hb concentration within the first 6 months (in g/L counting the last reported measure after birth within this period) (ALL).
1.62. Analysis.
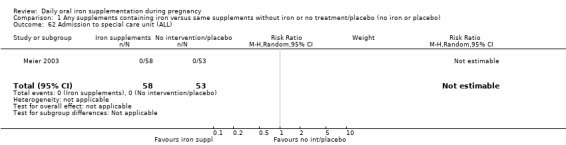
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 62 Admission to special care unit (ALL).
1.63. Analysis.
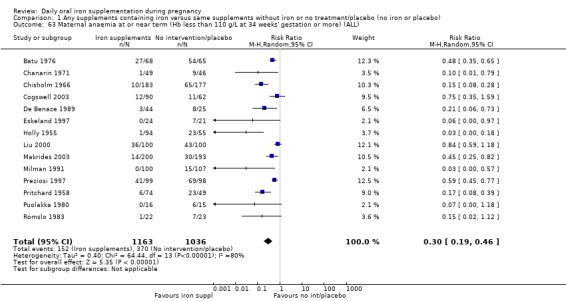
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 63 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL).
1.64. Analysis.
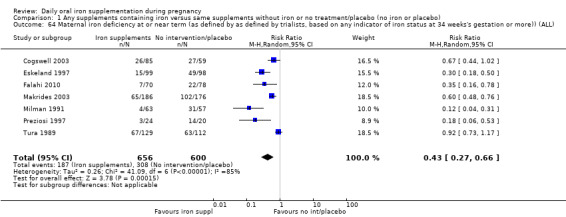
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 64 Maternal iron deficiency at or near term (as defined by as defined by trialists, based on any indicator of iron status at 34 weeks's gestation or more)) (ALL).
1.65. Analysis.
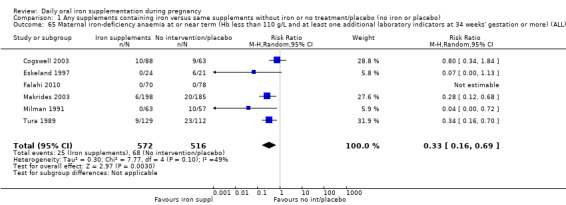
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 65 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL).
1.72. Analysis.
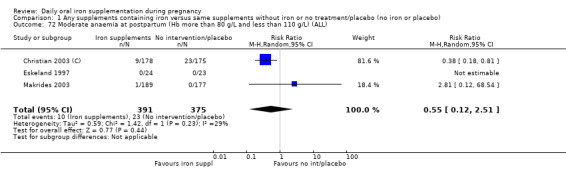
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 72 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL).
1.74. Analysis.
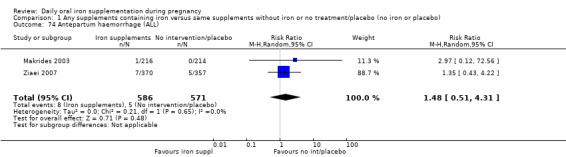
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 74 Antepartum haemorrhage (ALL).
1.75. Analysis.
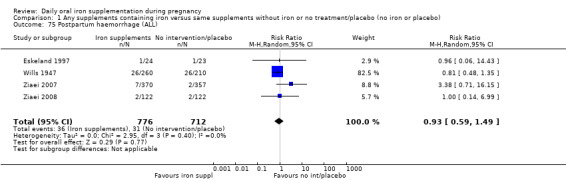
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 75 Postpartum haemorrhage (ALL).
1.77. Analysis.
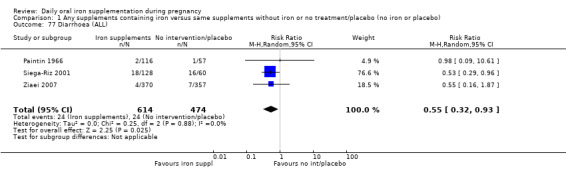
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 77 Diarrhoea (ALL).
1.78. Analysis.
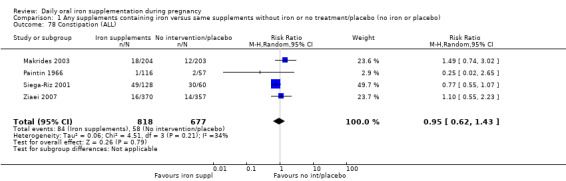
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 78 Constipation (ALL).
1.79. Analysis.
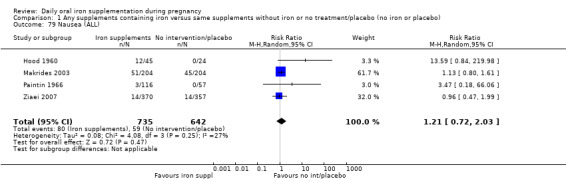
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 79 Nausea (ALL).
1.80. Analysis.
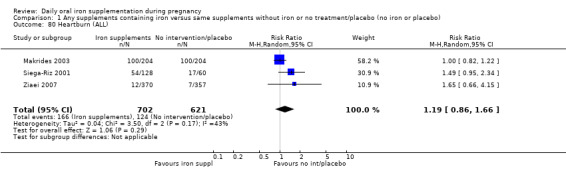
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 80 Heartburn (ALL).
1.81. Analysis.
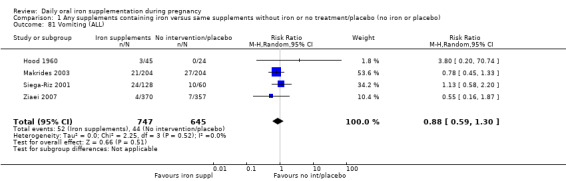
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 81 Vomiting (ALL).
1.82. Analysis.
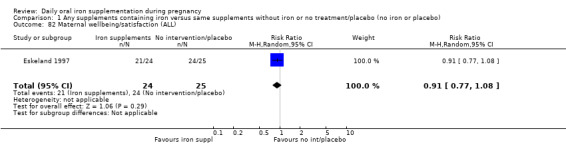
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 82 Maternal wellbeing/satisfaction (ALL).
1.83. Analysis.
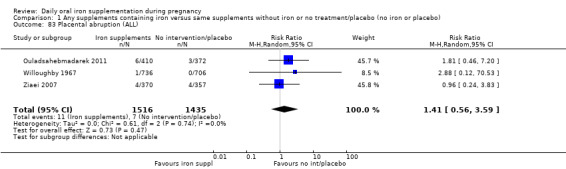
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 83 Placental abruption (ALL).
1.84. Analysis.
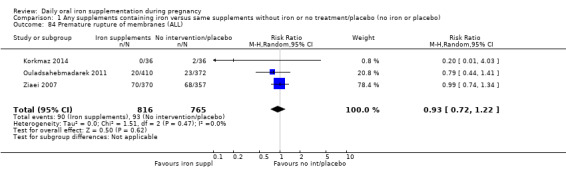
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 84 Premature rupture of membranes (ALL).
1.85. Analysis.
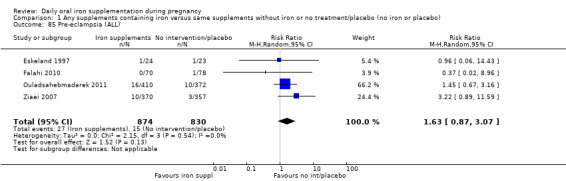
Comparison 1 Any supplements containing iron versus same supplements without iron or no treatment/placebo (no iron or placebo), Outcome 85 Pre‐eclampsia (ALL).
Comparison 2. Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 2 | 1311 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.31, 3.74] |
| 2 Neonatal death (within 28 days after delivery) (ALL) | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 3 Preterm birth (less than 37 weeks of gestation) (ALL) | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 4 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestation at the start of supplementation | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 2 | 1366 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 4.2 Late gestational age (supplementation started at 20 weeks of gestation or later) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Unspecified or mixed gestational age at start of supplementation | 1 | 44 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Non‐anaemic at the start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Unspecified or mixed anaemic status at start of supplementation | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 6 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 6.1 Low daily dose (30 mg elemental iron or less) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Higher daily dose (60 mg elemental iron and above) | 2 | 1366 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 7 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of settings | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 7.1 Malarial setting | 2 | 1449 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.92, 1.39] |
| 7.2 Non‐malarial setting | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 7.00 [0.38, 128.61] |
| 8 Birthweight (ALL) | 2 | 1365 | Mean Difference (IV, Random, 95% CI) | 57.73 [7.66, 107.79] |
| 9 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestation at the start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 9.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 9.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 10.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Non‐anaemic at start of supplementation | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.10, 59.88] |
| 10.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 1696 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.49, 1.27] |
| 11 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 11.1 Low daily dose (30 mg elemental iron or less) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Higher daily dose (60 mg elemental iron and above) | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 12 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status at the start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 12.1 Malarial setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.49, 1.27] |
| 12.2 Non‐malarial setting | 2 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.10, 59.88] |
| 13 Congenital anomalies (ALL) | 1 | 1652 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.35, 1.40] |
| 14 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 15 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestation at the start of supplementation | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 15.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.22, 0.62] |
| 15.3 Unspecified or mixed gestational age at start of supplementation | 1 | 183 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.68] |
| 16 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 16.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Non‐anaemic at start of supplementation | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.68] |
| 16.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.22, 0.62] |
| 17 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 17.1 Low daily dose (30 mg elemental iron or less) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Higher daily dose (60 mg elemental iron and above) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 18.1 Malarial setting | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.22, 0.62] |
| 18.2 Non‐malarial setting | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.68] |
| 19 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.06, 0.99] |
| 20 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.17, 1.09] |
| 21 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Side effects (any reported throughout the intervention period) (ALL) | 1 | 456 | Risk Ratio (M‐H, Random, 95% CI) | 44.32 [2.77, 709.09] |
| 23 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 24 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestation at the start of supplementation | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 24.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 456 | Risk Ratio (M‐H, Random, 95% CI) | 0.11 [0.01, 0.83] |
| 24.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.63] |
| 24.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 25.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Non‐anaemic at start of supplementation | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.3 Unspecified or mixed anaemic status at start of supplementation | 3 | 409 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 26 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 26.1 Low daily dose (30 mg elemental iron or less) | 1 | 44 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26.3 Higher daily dose (60 mg elemental iron and above) | 3 | 462 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 27 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 27.1 Malarial setting | 3 | 409 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 27.2 Non‐malarial setting | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Infection during pregnancy (including urinary tract infections) (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.15, 6.53] |
| 30 Very low birthweight (less than 1500 g) (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 98.96] |
| 31 Very premature birth (less than 34 weeks' gestation) (ALL) | 2 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 98.96] |
| 32 Admission to special care unit (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 34 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.06, 0.99] |
| 35 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.17, 1.09] |
| 36 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL) | 3 | 140 | Mean Difference (IV, Random, 95% CI) | 16.13 [12.74, 19.52] |
| 37 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL) | 2 | 459 | Mean Difference (IV, Random, 95% CI) | 10.07 [7.33, 12.81] |
| 38 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 2 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.63, 5.04] |
| 39 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 2 | 314 | Risk Ratio (M‐H, Random, 95% CI) | 4.37 [0.58, 32.71] |
| 40 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.17, 0.65] |
| 41 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more ) (ALL) | 3 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.63] |
| 42 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 0.76] |
| 43 Puerperal infection (ALL) | 1 | 2863 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.13, 2.28] |
| 44 Antepartum haemorrhage (ALL) | 2 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.22, 7.12] |
| 45 Postpartum haemorrhage (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 46 Placental abruption (ALL) | 1 | 2863 | Risk Ratio (M‐H, Random, 95% CI) | 8.19 [0.49, 138.16] |
| 47 Pre‐eclampsia (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.13, 70.16] |
2.9. Analysis.
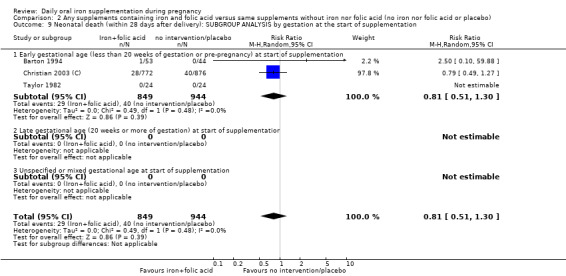
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 9 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestation at the start of supplementation.
2.10. Analysis.
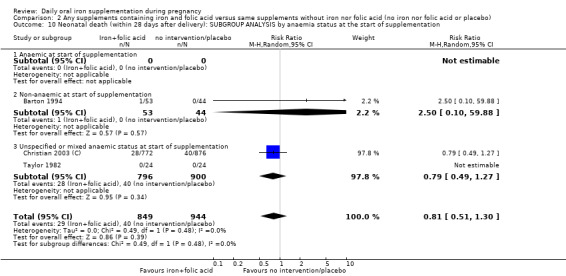
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 10 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
2.11. Analysis.
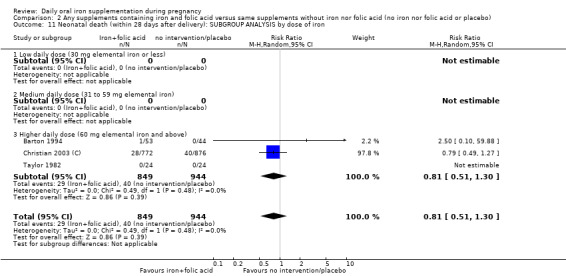
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 11 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron.
2.12. Analysis.
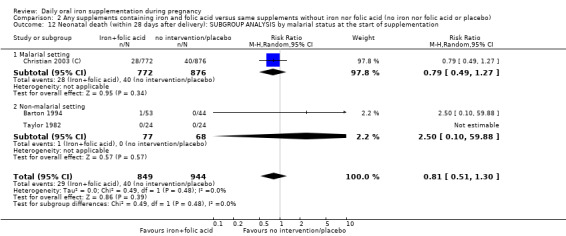
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 12 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status at the start of supplementation.
2.15. Analysis.
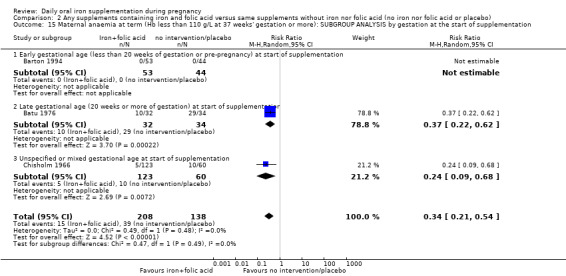
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 15 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestation at the start of supplementation.
2.16. Analysis.
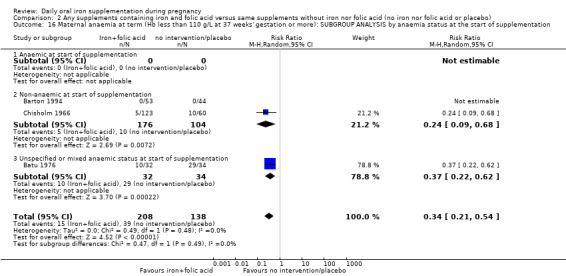
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 16 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
2.17. Analysis.
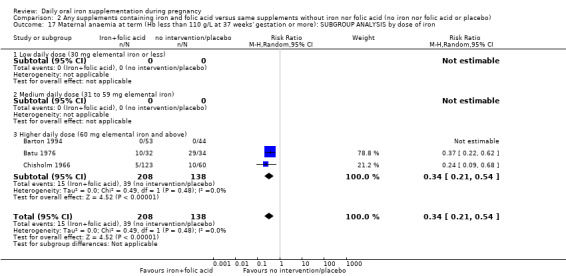
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 17 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
2.18. Analysis.
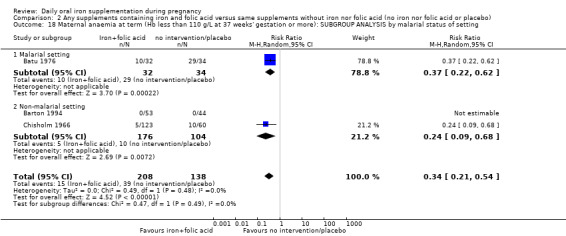
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
2.24. Analysis.
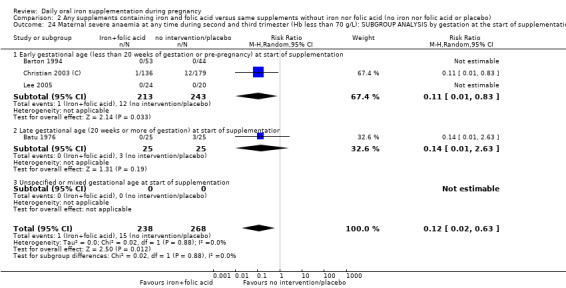
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 24 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestation at the start of supplementation.
2.25. Analysis.
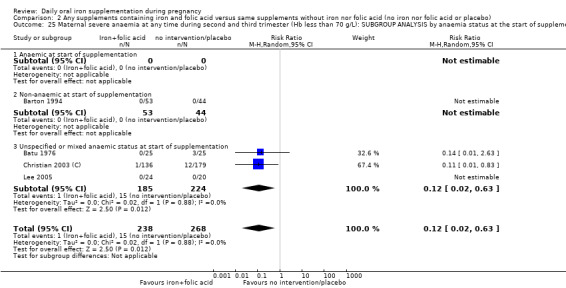
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 25 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
2.26. Analysis.
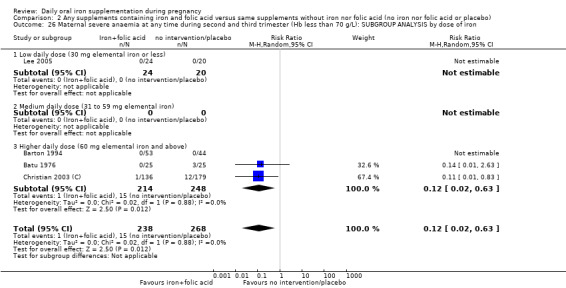
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 26 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron.
2.27. Analysis.
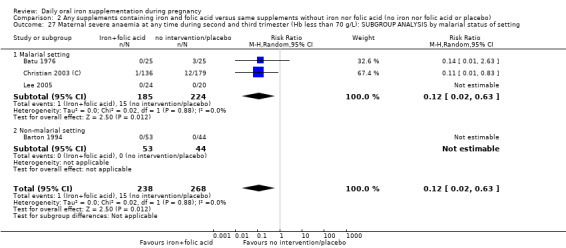
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 27 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting.
2.30. Analysis.
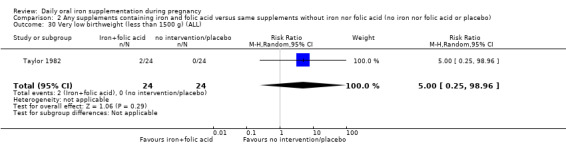
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 30 Very low birthweight (less than 1500 g) (ALL).
2.31. Analysis.
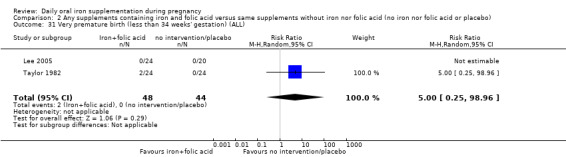
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 31 Very premature birth (less than 34 weeks' gestation) (ALL).
2.32. Analysis.
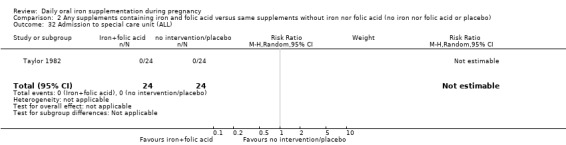
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 32 Admission to special care unit (ALL).
2.33. Analysis.
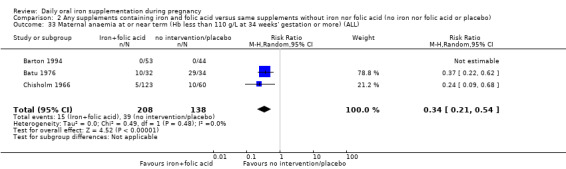
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 33 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL).
2.34. Analysis.
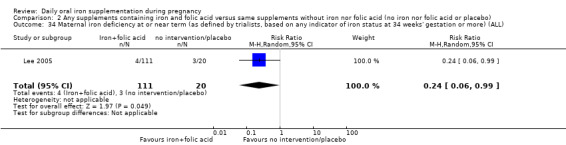
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 34 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL).
2.35. Analysis.
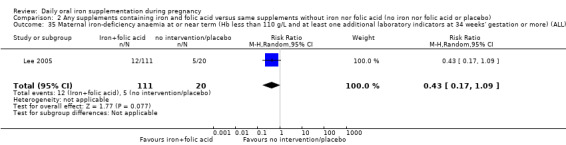
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 35 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL).
2.43. Analysis.
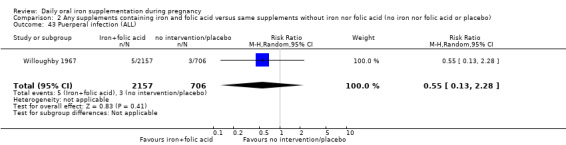
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 43 Puerperal infection (ALL).
2.44. Analysis.
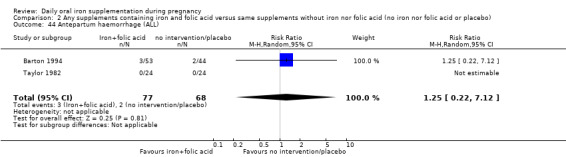
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 44 Antepartum haemorrhage (ALL).
2.46. Analysis.
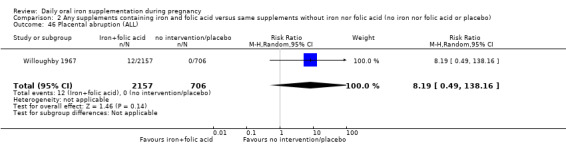
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 46 Placental abruption (ALL).
2.47. Analysis.
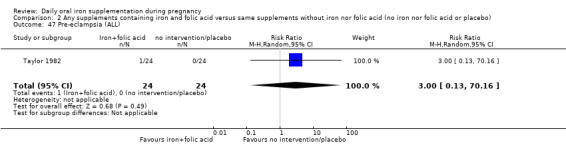
Comparison 2 Any supplements containing iron and folic acid versus same supplements without iron nor folic acid (no iron nor folic acid or placebo), Outcome 47 Pre‐eclampsia (ALL).
Comparison 3. Supplementation with iron alone versus no treatment/placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 6 | 1136 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.32] |
| 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 6 | 1136 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.32] |
| 2.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 2 | 361 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.15, 0.70] |
| 2.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 3 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.50, 2.19] |
| 2.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.17, 19.20] |
| 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 6 | 1136 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.32] |
| 3.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Non‐anaemic at start of supplementation | 5 | 955 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.25, 1.66] |
| 3.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 181 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.14, 2.31] |
| 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron | 6 | 1136 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.32] |
| 4.1 Low daily dose (30 mg elemental iron or less) | 3 | 697 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.12, 2.96] |
| 4.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Higher daily dose (60 mg elemental iron and above) | 3 | 439 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.25, 1.50] |
| 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting | 6 | 1136 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.32] |
| 5.1 Malarial setting | 2 | 329 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.20, 1.35] |
| 5.2 Non‐malarial setting | 4 | 807 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.20, 2.70] |
| 6 Birthweight (g) (ALL) | 9 | 1331 | Mean Difference (IV, Random, 95% CI) | ‐1.04 [‐78.77, 76.70] |
| 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 9 | 1331 | Mean Difference (IV, Random, 95% CI) | ‐1.04 [‐78.77, 76.70] |
| 7.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 5 | 477 | Mean Difference (IV, Random, 95% CI) | ‐31.62 [‐214.93, 151.70] |
| 7.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 4 | 854 | Mean Difference (IV, Random, 95% CI) | ‐8.70 [‐74.71, 57.31] |
| 7.3 Unspecified or mixed gestational age at the start of supplementation | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 9 | 1331 | Mean Difference (IV, Random, 95% CI) | ‐1.04 [‐78.77, 76.70] |
| 8.1 Anaemic at start of supplementation | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Non‐anaemic at start of supplementation | 7 | 961 | Mean Difference (IV, Random, 95% CI) | ‐9.03 [‐125.10, 107.04] |
| 8.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 370 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐86.32, 88.12] |
| 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron | 9 | 1331 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐72.00, 70.60] |
| 9.1 Low daily dose (30 mg elemental iron or less) | 4 | 785 | Mean Difference (IV, Random, 95% CI) | 46.83 [‐76.57, 170.22] |
| 9.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Higher daily dose (60 mg elemental iron and above) | 6 | 546 | Mean Difference (IV, Random, 95% CI) | ‐36.28 [‐126.66, 54.10] |
| 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting | 9 | 1331 | Mean Difference (IV, Random, 95% CI) | ‐1.04 [‐78.77, 76.70] |
| 10.1 Malarial setting | 2 | 345 | Mean Difference (IV, Random, 95% CI) | 33.74 [‐61.16, 128.65] |
| 10.2 Non‐malarial setting | 7 | 986 | Mean Difference (IV, Random, 95% CI) | ‐21.75 [‐132.94, 89.44] |
| 11 Preterm birth (less than 37 weeks of gestation) (ALL) | 6 | 1713 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.14] |
| 12 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 6 | 1713 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.14] |
| 12.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 4 | 1236 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.62, 1.35] |
| 12.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 2 | 477 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.29, 1.13] |
| 12.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 6 | 1713 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.14] |
| 13.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Non‐anaemic at start of supplementation | 5 | 851 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.45, 1.13] |
| 13.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 862 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.58, 1.57] |
| 14 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron | 6 | 1713 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.14] |
| 14.1 Low daily dose (30 mg elemental iron or less) | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.47, 1.24] |
| 14.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Higher daily dose (60 mg elemental iron and above) | 3 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.54, 1.39] |
| 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting | 6 | 1713 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.14] |
| 15.1 Malarial setting | 2 | 1010 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.54, 1.39] |
| 15.2 Non‐malarial setting | 4 | 703 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.47, 1.24] |
| 16 Neonatal death (within 28 days after delivery) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Congenital anomalies (ALL) | 2 | 2402 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.55, 1.35] |
| 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 14 | 2136 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.19, 0.47] |
| 19 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 13 | 1999 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.16, 0.41] |
| 19.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 6 | 549 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.06, 0.57] |
| 19.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 6 | 1301 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.20, 0.53] |
| 19.3 Unspecified or mixed gestational age at start of supplementation | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 0.03 [0.00, 0.18] |
| 20 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 13 | 1936 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.15, 0.42] |
| 20.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Non‐anaemic at start of supplementation | 8 | 1244 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.10, 0.44] |
| 20.3 Unspecified or mixed anaemic status at start of supplementation | 5 | 692 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.18, 0.64] |
| 21 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 13 | 1999 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.16, 0.41] |
| 21.1 Low daily dose (30 mg elemental iron or less) | 3 | 590 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.24, 1.03] |
| 21.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.06, 0.73] |
| 21.3 Higher daily dose (60 mg elemental iron and above) | 9 | 1340 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.10, 0.38] |
| 22 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 13 | 1936 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.15, 0.42] |
| 22.1 Malarial setting | 2 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.46, 0.72] |
| 22.2 Non‐malarial setting | 11 | 1669 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.10, 0.34] |
| 23 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL) | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 24 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 24.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 4 | 653 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.22, 0.93] |
| 24.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 3 | 603 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.18, 0.72] |
| 24.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 25.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Non‐anaemic at start of supplementation | 5 | 1092 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.39, 0.82] |
| 25.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 164 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.07, 0.29] |
| 26 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 26.1 Low daily dose (30 mg elemental iron or less) | 3 | 703 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.34, 0.78] |
| 26.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.73, 1.17] |
| 26.3 Higher daily dose (60 mg elemental iron and above) | 3 | 312 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.10, 0.41] |
| 27 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 27.1 Malarial setting | 2 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.53] |
| 27.2 Non‐malarial setting | 5 | 1064 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.30, 0.78] |
| 28 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 29 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 29.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 4 | 660 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.13, 1.11] |
| 29.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 2 | 428 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.11, 0.58] |
| 29.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 30.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30.2 Non‐anaemic at start of supplementation | 5 | 968 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.20, 0.74] |
| 30.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.00, 0.72] |
| 31 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 31.1 Daily low dose (60 mg elemental iron or less) | 3 | 579 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.13, 1.11] |
| 31.2 Medium dose (31 to 59 mg elemental iron) | 1 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.16, 0.70] |
| 31.3 High dose (60 mg elemental iron and above) | 2 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.00, 0.72] |
| 32 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 32.1 Malarial setting | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32.2 Non‐malarial setting | 5 | 940 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 33 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 1 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 34 Side effects (any reported throughout the intervention period) (ALL) | 9 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.00, 2.52] |
| 35 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 9 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.00, 2.52] |
| 35.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 438 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.87, 2.19] |
| 35.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 5 | 1034 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.89, 2.28] |
| 35.3 Unspecified or mixed gestational age at start of supplementation | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 62.79 [3.89, 1013.31] |
| 36 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 9 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.00, 2.52] |
| 36.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 36.2 Non‐anaemic at start of supplementation | 5 | 900 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.28] |
| 36.3 Unspecified or mixed anaemic status at start of supplementation | 4 | 777 | Risk Ratio (M‐H, Random, 95% CI) | 5.11 [0.78, 33.60] |
| 37 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by dose of iron | 9 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [1.02, 2.43] |
| 37.1 Low daily dose (30 mg elemental iron or less) | 4 | 785 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.90, 1.26] |
| 37.2 Medium daily dose (31 to 59 mg elemental iron) | 2 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 2.00 [0.66, 6.02] |
| 37.3 Higher daily dose (60 mg elemental iron and above) | 5 | 667 | Risk Ratio (M‐H, Random, 95% CI) | 5.53 [0.81, 37.89] |
| 38 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by malarial status of setting | 9 | 1677 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.00, 2.52] |
| 38.1 Malarial setting | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 62.79 [3.89, 1013.31] |
| 38.2 Non‐malarial setting | 8 | 1472 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.99, 1.97] |
| 39 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 7 | 1078 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 40 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 7 | 1078 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 40.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 416 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 40.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 3 | 513 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 40.3 Unspecified or mixed gestational age at start of supplementation | 1 | 149 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by anaemia status age at the start of supplementation | 7 | 1078 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 41.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41.2 Non‐anaemic at start of supplementation | 5 | 816 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 41.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.01, 2.21] |
| 42 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by dose of iron | 7 | 1078 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 42.1 Low daily dose (30 mg elemental iron or less) | 3 | 654 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 42.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 42.3 Higher daily dose (60 mg elemental iron and above) | 4 | 424 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.01, 2.21] |
| 43 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L): SUBGROUP ANALYSIS by malarial status of setting | 7 | 1078 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 29.10] |
| 43.1 Malarial setting | 1 | 55 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.01, 2.21] |
| 43.2 Non‐malarial setting | 6 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [0.24, 103.01] |
| 44 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 45 Infection during pregnancy (including urinary tract infections) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 46 Very low birthweight (less than 1500 g) (ALL) | 3 | 697 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.03, 9.07] |
| 47 Very premature birth (less than 34 weeks' gestation) (ALL) | 3 | 690 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.10, 1.09] |
| 48 Infant Hb concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period) (ALL) | 2 | 533 | Mean Difference (IV, Random, 95% CI) | ‐1.25 [‐8.10, 5.59] |
| 49 Infant serum ferritin concentration in the first 6 months (in μg/L, counting the last reported measure after birth within this period) (ALL) | 1 | 197 | Mean Difference (IV, Random, 95% CI) | 11.0 [4.37, 17.63] |
| 50 Admission to special care unit (ALL) | 1 | 111 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 51 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 13 | 1696 | Risk Ratio (M‐H, Random, 95% CI) | 0.29 [0.18, 0.46] |
| 52 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL) | 7 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.27, 0.66] |
| 53 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 6 | 1088 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.16, 0.69] |
| 54 Maternal Hb concentration at or near term (in g/L, at 34 weeks' gestation or more) (ALL) | 16 | 1851 | Mean Difference (IV, Random, 95% CI) | 8.95 [6.37, 11.53] |
| 55 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL) | 6 | 659 | Mean Difference (IV, Random, 95% CI) | 7.26 [4.78, 9.74] |
| 56 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 7 | 1146 | Risk Ratio (M‐H, Random, 95% CI) | 1.90 [1.07, 3.35] |
| 57 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 7 | 1189 | Risk Ratio (M‐H, Random, 95% CI) | 3.80 [1.74, 8.28] |
| 58 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 3 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.02, 13.91] |
| 59 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL) | 7 | 1046 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.02, 27.81] |
| 60 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 7 | 953 | Risk Ratio (M‐H, Random, 95% CI) | 0.02 [0.00, 0.33] |
| 61 Puerperal infection (ALL) | 2 | 2292 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.41, 1.03] |
| 62 Antepartum haemorrhage (ALL) | 1 | 430 | Risk Ratio (M‐H, Random, 95% CI) | 2.97 [0.12, 72.56] |
| 63 Postpartum haemorrhage (ALL) | 3 | 761 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.51, 1.34] |
| 64 Transfusion provided (ALL) | 1 | 32 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.62] |
| 65 Diarrhoea (ALL) | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.09, 10.61] |
| 66 Constipation (ALL) | 2 | 580 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.18, 4.40] |
| 67 Nausea (ALL) | 3 | 650 | Risk Ratio (M‐H, Random, 95% CI) | 2.38 [0.49, 11.52] |
| 68 Heartburn (ALL) | 1 | 408 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.82, 1.22] |
| 69 Vomiting (ALL) | 2 | 477 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.38, 2.07] |
| 70 Maternal wellbeing/satisfaction (ALL) | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.77, 1.08] |
| 71 Placental abruption (ALL) | 1 | 1442 | Risk Ratio (M‐H, Random, 95% CI) | 2.88 [0.12, 70.53] |
| 72 Premature rupture of membranes (ALL) | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 0.2 [0.01, 4.03] |
| 73 Pre‐eclampsia (ALL) | 1 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.06, 14.43] |
3.24. Analysis.
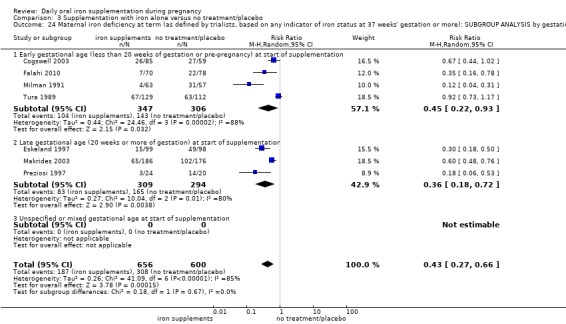
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 24 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.27. Analysis.
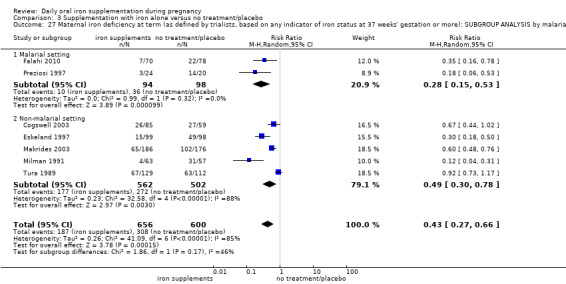
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 27 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
3.35. Analysis.
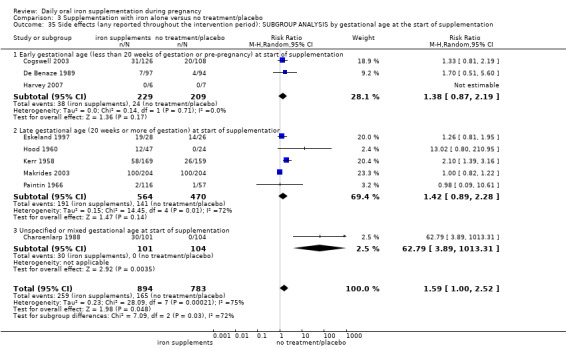
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 35 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
3.36. Analysis.
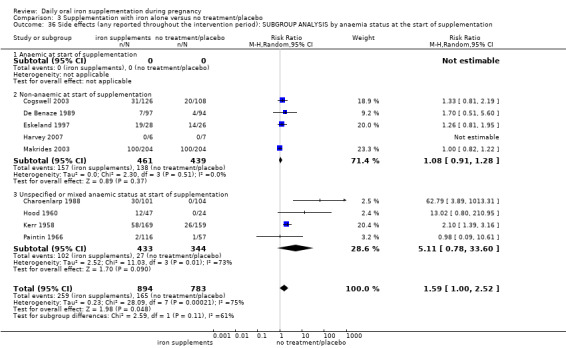
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 36 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
3.37. Analysis.
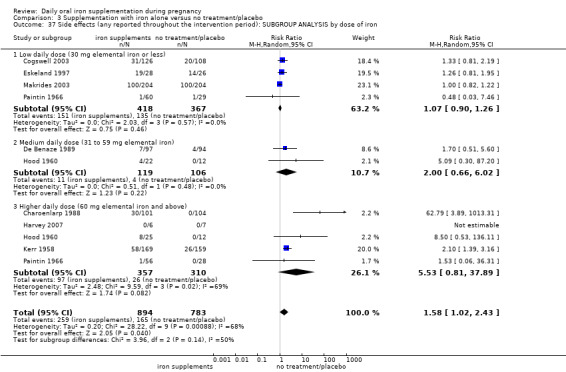
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 37 Side effects (any reported throughout the intervention period): SUBGROUP ANALYSIS by dose of iron.
3.51. Analysis.
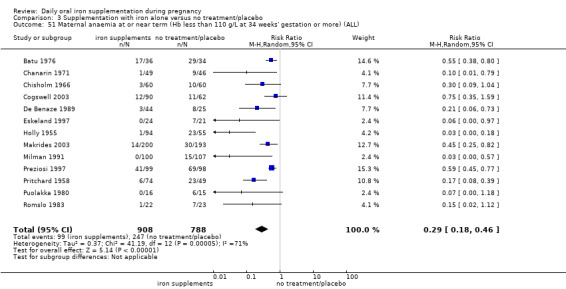
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 51 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL).
3.52. Analysis.
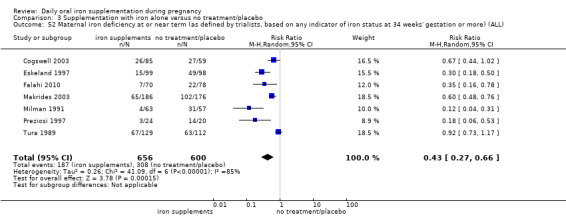
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 52 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL).
3.53. Analysis.
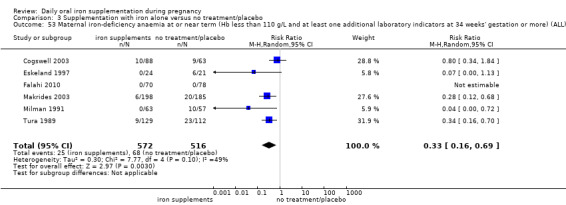
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 53 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL).
3.58. Analysis.
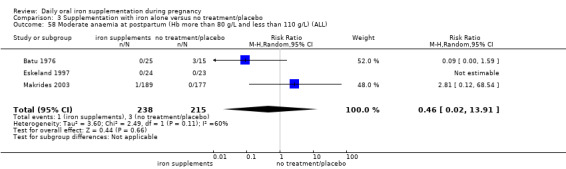
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 58 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL).
3.59. Analysis.
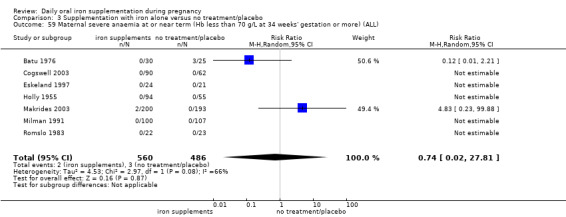
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 59 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL).
3.60. Analysis.
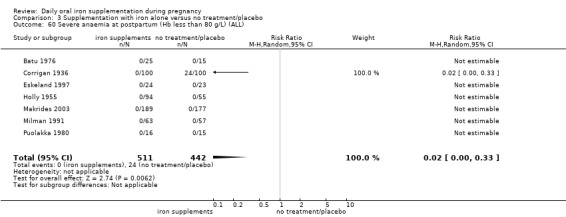
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 60 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL).
3.61. Analysis.
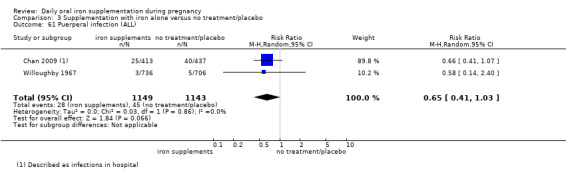
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 61 Puerperal infection (ALL).
3.62. Analysis.
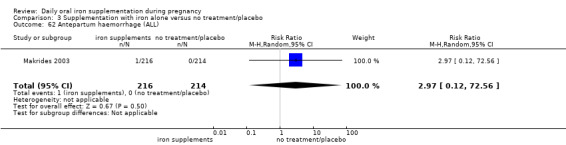
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 62 Antepartum haemorrhage (ALL).
3.63. Analysis.
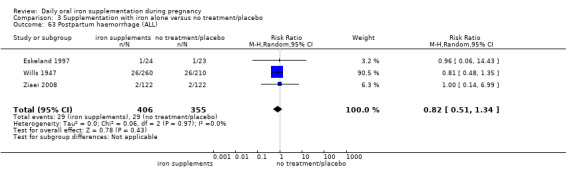
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 63 Postpartum haemorrhage (ALL).
3.65. Analysis.
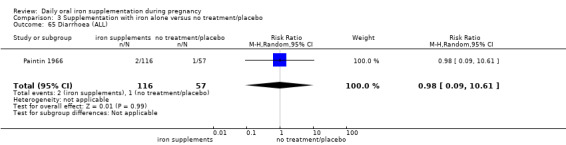
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 65 Diarrhoea (ALL).
3.66. Analysis.
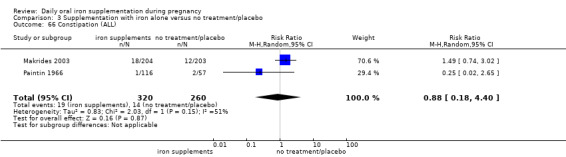
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 66 Constipation (ALL).
3.67. Analysis.
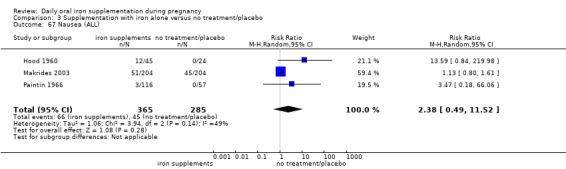
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 67 Nausea (ALL).
3.68. Analysis.
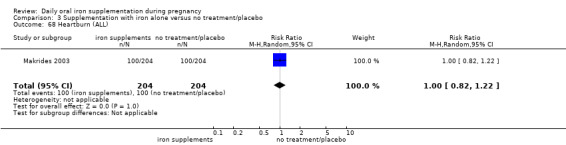
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 68 Heartburn (ALL).
3.69. Analysis.
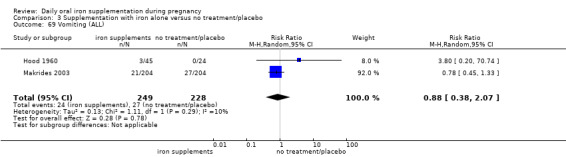
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 69 Vomiting (ALL).
3.71. Analysis.
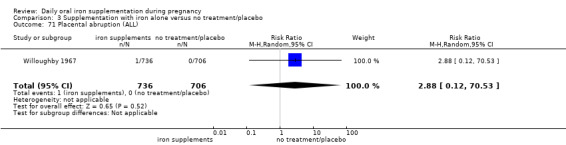
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 71 Placental abruption (ALL).
3.72. Analysis.
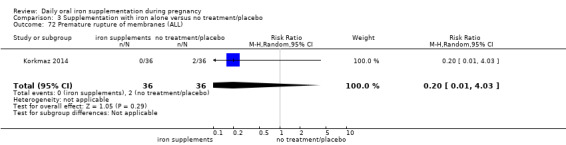
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 72 Premature rupture of membranes (ALL).
3.73. Analysis.
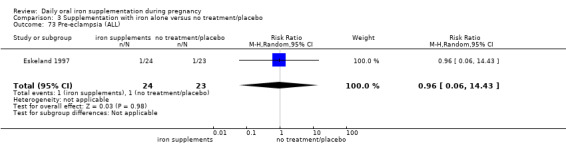
Comparison 3 Supplementation with iron alone versus no treatment/placebo, Outcome 73 Pre‐eclampsia (ALL).
Comparison 4. Supplementation with iron+folic acid versus no treatment/placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 2 | 1311 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.31, 3.74] |
| 2 Birthweight (ALL) | 2 | 1365 | Mean Difference (IV, Random, 95% CI) | 57.73 [7.66, 107.79] |
| 3 Preterm birth (less than 37 weeks of gestation) (ALL) | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 4 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 3 | 1410 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 4.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 2 | 1366 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 4.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Unspecified or mixed gestational age at start of supplementation | 1 | 44 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 5.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Non‐anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Unspecified or mixed anaemic status at start of supplementation | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 6 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 6.1 Low daily dose (30 mg elemental iron or less) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Higher daily dose (60 mg elemental iron and above) | 2 | 1366 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 7 Preterm birth (less than 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting | 3 | 1497 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.40, 6.00] |
| 7.1 Malarial setting | 2 | 1449 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.92, 1.39] |
| 7.2 Non‐malarial setting | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 7.00 [0.38, 128.61] |
| 8 Neonatal death (within 28 days after delivery) (ALL) | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 9 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 9.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 9.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at start of supplementation | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 10.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Non‐anaemic at start of supplementation | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.10, 59.88] |
| 10.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 1696 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.49, 1.27] |
| 11 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 11.1 Low daily dose (30 mg elemental iron or less) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Higher daily dose (60 mg elemental iron and above) | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 12 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting | 3 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.51, 1.30] |
| 12.1 Malarial setting | 1 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.49, 1.27] |
| 12.2 Non‐malarial setting | 2 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.10, 59.88] |
| 13 Congenital anomalies (ALL) | 1 | 1652 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.35, 1.40] |
| 14 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 15 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 15.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 2 | 249 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 15.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 16.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Non‐anaemic at start of supplementation | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.68] |
| 16.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.22, 0.62] |
| 17 Maternal anaemia at term (Hb less than 110 g/Lat 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 17.1 Low daily dose (30 mg elemental iron or less) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Higher daily dose (60 mg elemental iron and above) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 18.1 Malarial setting | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.22, 0.62] |
| 18.2 Non‐malarial setting | 2 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.68] |
| 19 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.06, 0.99] |
| 20 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.17, 1.09] |
| 21 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Side effects (any reported throughout the intervention period) (ALL) | 1 | 456 | Risk Ratio (M‐H, Random, 95% CI) | 44.32 [2.77, 709.09] |
| 23 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 4 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.02, 0.63] |
| 24 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Infection during pregnancy (including urinary tract infections) (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.15, 6.53] |
| 26 Very low birthweight (less than 1500 g) (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 98.96] |
| 27 Very premature birth (less than 34 weeks' gestation) (ALL) | 2 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 5.0 [0.25, 98.96] |
| 28 Infant Hb concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Infant serum ferritin concentration in the first 6 months (in μg/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Admission to special care unit (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.54] |
| 32 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.06, 0.99] |
| 33 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.17, 1.09] |
| 34 Maternal Hb concentration at term or near term (in g/L, at 34 weeks' gestation or more) (ALL) | 3 | 140 | Mean Difference (IV, Random, 95% CI) | 16.13 [12.74, 19.52] |
| 35 Maternal Hb concentration within 6 wk postpartum (g/L) (ALL) | 2 | 459 | Mean Difference (IV, Random, 95% CI) | 10.07 [7.33, 12.81] |
| 36 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 2 | 446 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [0.63, 5.04] |
| 37 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 2 | 314 | Risk Ratio (M‐H, Random, 95% CI) | 4.37 [0.58, 32.71] |
| 38 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 2 | 458 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.17, 0.69] |
| 39 Maternal severe anaemia at term or near (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL) | 3 | 191 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.63] |
| 40 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 3 | 491 | Risk Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 0.76] |
| 41 Puerperal infection (ALL) | 1 | 2863 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.13, 2.28] |
| 42 Antepartum haemorrhage (ALL) | 2 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.22, 7.12] |
| 43 Postpartum haemorrhage (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 44 Placental abruption (ALL) | 1 | 2863 | Risk Ratio (M‐H, Random, 95% CI) | 8.19 [0.49, 138.16] |
| 45 Pre‐eclampsia (ALL) | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.13, 70.16] |
4.9. Analysis.
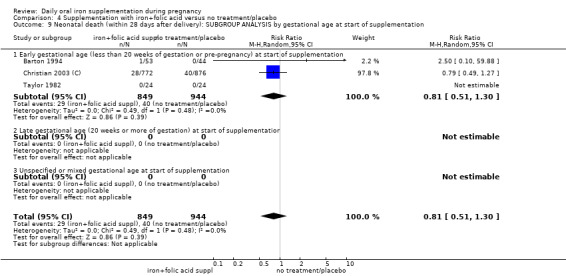
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 9 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at start of supplementation.
4.10. Analysis.
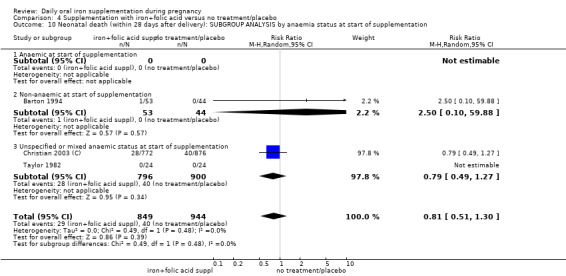
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 10 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by anaemia status at start of supplementation.
4.11. Analysis.
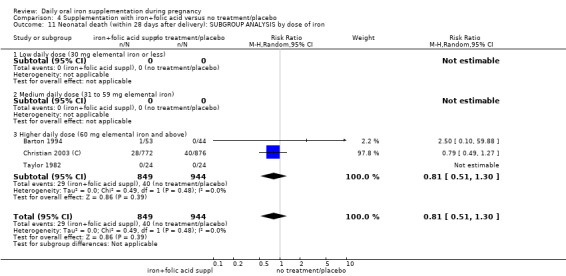
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 11 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron.
4.12. Analysis.
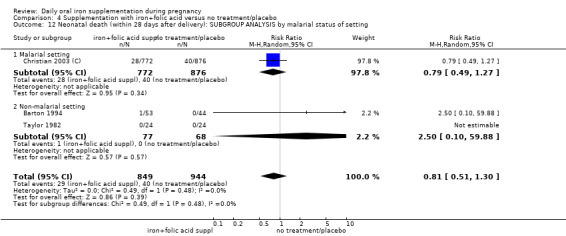
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 12 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting.
4.15. Analysis.
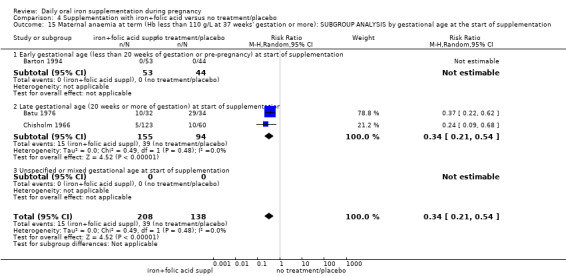
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 15 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
4.16. Analysis.
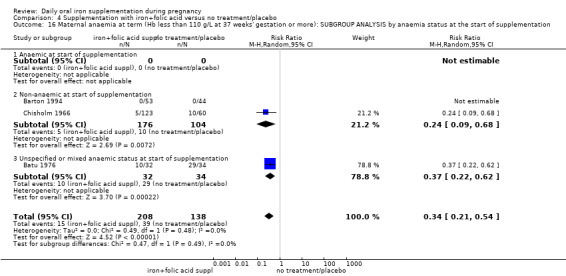
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 16 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
4.17. Analysis.
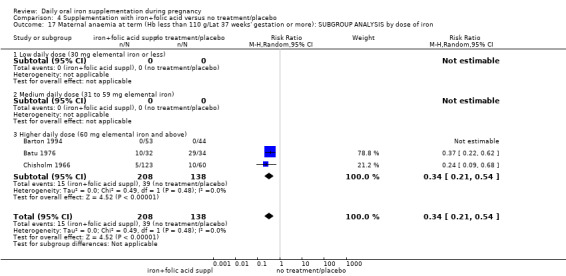
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 17 Maternal anaemia at term (Hb less than 110 g/Lat 37 weeks' gestation or more): SUBGROUP ANALYSIS by dose of iron.
4.18. Analysis.
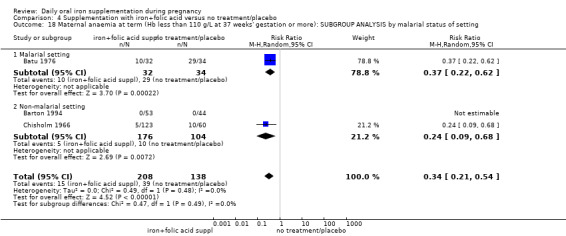
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 18 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by malarial status of setting.
4.26. Analysis.
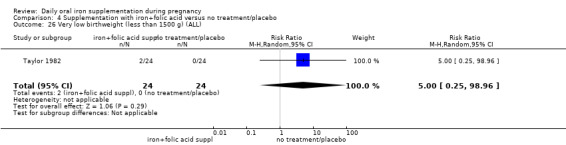
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 26 Very low birthweight (less than 1500 g) (ALL).
4.27. Analysis.
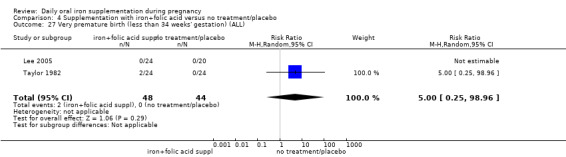
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 27 Very premature birth (less than 34 weeks' gestation) (ALL).
4.30. Analysis.
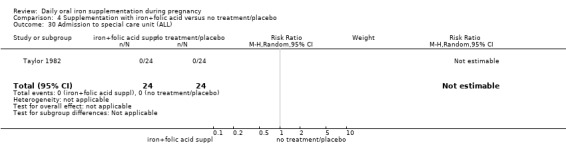
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 30 Admission to special care unit (ALL).
4.41. Analysis.
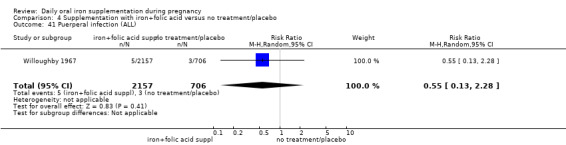
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 41 Puerperal infection (ALL).
4.42. Analysis.
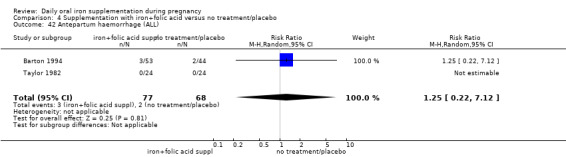
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 42 Antepartum haemorrhage (ALL).
4.44. Analysis.
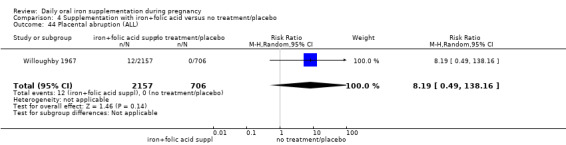
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 44 Placental abruption (ALL).
4.45. Analysis.
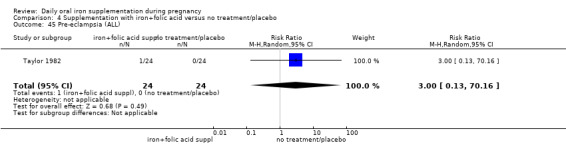
Comparison 4 Supplementation with iron+folic acid versus no treatment/placebo, Outcome 45 Pre‐eclampsia (ALL).
Comparison 5. Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 4 | 16143 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 1.00] |
| 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 4 | 16143 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 1.00] |
| 2.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 13817 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.75, 1.11] |
| 2.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2326 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.59, 1.22] |
| 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 16143 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 1.00] |
| 3.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Non‐anaemic at start of supplementation | 2 | 12554 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.83, 1.32] |
| 3.3 Unspecified or mixed anaemia status | 2 | 3589 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.72, 0.94] |
| 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron | 4 | 16143 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 1.00] |
| 4.1 Low daily dose (30 mg elemental iron or less) | 1 | 11827 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.81, 1.31] |
| 4.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.57, 2.54] |
| 4.3 Higher daily dose (60 mg elemental iron and above) | 2 | 3589 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.72, 0.94] |
| 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting | 4 | 16143 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 1.00] |
| 5.1 Malarial setting | 3 | 4316 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.73, 0.95] |
| 5.2 Non‐malarial setting | 1 | 11827 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.81, 1.31] |
| 6 Birthweight (g) (ALL) | 4 | 16143 | Mean Difference (IV, Random, 95% CI) | 19.50 [‐6.90, 45.89] |
| 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 4 | 16143 | Mean Difference (IV, Random, 95% CI) | 19.50 [‐6.90, 45.89] |
| 7.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 13817 | Mean Difference (IV, Random, 95% CI) | 22.47 [‐18.18, 63.12] |
| 7.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2326 | Mean Difference (IV, Random, 95% CI) | 20.20 [‐15.13, 55.53] |
| 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 16143 | Mean Difference (IV, Random, 95% CI) | 19.50 [‐6.90, 45.89] |
| 8.1 Anaemic at start of supplementation | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Non‐anaemic at start of supplementation | 2 | 12554 | Mean Difference (IV, Random, 95% CI) | 2.30 [‐11.42, 16.01] |
| 8.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 3589 | Mean Difference (IV, Random, 95% CI) | 39.61 [‐3.90, 83.13] |
| 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron | 4 | 16143 | Mean Difference (IV, Random, 95% CI) | 19.50 [‐6.90, 45.89] |
| 9.1 Low daily dose (30 mg elemental iron or less) | 1 | 11827 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐12.17, 15.97] |
| 9.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 727 | Mean Difference (IV, Random, 95% CI) | 10.0 [‐51.92, 71.92] |
| 9.3 Higher daily dose (60 mg elemental iron and above) | 2 | 3589 | Mean Difference (IV, Random, 95% CI) | 39.61 [‐3.90, 83.13] |
| 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting | 4 | 16143 | Mean Difference (IV, Random, 95% CI) | 19.50 [‐6.90, 45.89] |
| 10.1 Malarial setting | 3 | 4316 | Mean Difference (IV, Random, 95% CI) | 32.23 [0.86, 63.60] |
| 10.2 Non‐malarial setting | 1 | 11827 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐12.17, 15.97] |
| 11 Preterm birth (less than 37 weeks of gestation) (ALL) | 4 | 16146 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.08] |
| 12 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 4 | 16146 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.08] |
| 12.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 13820 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.88, 1.12] |
| 12.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2326 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.57, 1.09] |
| 13 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 16146 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.08] |
| 13.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Non‐anaemic at start of supplementation | 2 | 12559 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.84, 1.12] |
| 13.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 3587 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.71, 1.22] |
| 14 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron | 4 | 16146 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.08] |
| 14.1 Low daily dose (30 mg elemental iron or less) | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.83, 1.11] |
| 14.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.62, 2.56] |
| 14.3 Higher daily dose (60 mg elemental iron and above) | 2 | 3587 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.71, 1.22] |
| 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting | 4 | 16146 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.08] |
| 15.1 Malarial setting | 3 | 4314 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.78, 1.20] |
| 15.2 Non‐malarial setting | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.83, 1.11] |
| 16 Neonatal death (within 28 days after delivery) (ALL) | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 17 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 17.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 3 | 14108 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.71, 1.42] |
| 17.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Unspecified or mixed gestational age at the start of supplementation | 1 | 2495 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.56, 1.19] |
| 18 Neonatal death (within 28 days after delivery) : SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 18.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18.2 Non‐anaemic at start of supplementation | 2 | 12559 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.51, 1.77] |
| 18.3 Unspecified or mixed anaemic status at start of supplementation | 2 | 4044 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.65, 1.19] |
| 19 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 19.1 Low daily dose (30 mg elemental iron or less) | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.82] |
| 19.2 Medium daily dose (31 to 59 mg elemental iron) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.12, 1.91] |
| 19.3 Higher daily dose (60 mg elemental iron and above) | 2 | 4044 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.65, 1.19] |
| 20 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting | 4 | 16603 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.71, 1.18] |
| 20.1 Malarial setting | 3 | 4771 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.63, 1.15] |
| 20.2 Non‐malarial setting | 1 | 11832 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.82] |
| 21 Congenital anomalies (ALL) | 2 | 13586 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.44, 1.39] |
| 22 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 23 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 23.1 Early gestational age (less than 20 weeks of gestation or pre‐pregnancy) at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 23.2 Late gestational age (20 weeks or more of gestation) at start of supplementation | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 23.3 Unspecified or mixed gestational age at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 24.1 Anaemic at start of supplementation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 24.2 Non‐anaemic at start of supplementation | 1 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.61] |
| 24.3 Unspecified or mixed anaemic status at start of supplementation | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.23, 0.67] |
| 25 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more ): SUBGROUP ANALYSIS by dose of iron | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 25.1 Low daily dose (30 mg elemental iron or less) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.2 Medium daily dose (31 to 59 mg elemental iron) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25.3 Higher daily dose (60 mg elemental iron and above) | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 26 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more ): SUBGROUP ANALYSIS by malarial status of setting | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 26.1 Malarial setting | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.23, 0.67] |
| 26.2 Non‐malarial setting | 1 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.61] |
| 27 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Side effects (any reported throughout the intervention period) (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.55, 2.23] |
| 31 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 3 | 1047 | Risk Ratio (M‐H, Random, 95% CI) | 0.06 [0.01, 0.47] |
| 32 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Infection during pregnancy (including urinary tract infections) (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.33, 4.46] |
| 34 Very low birthweight (less than 1500 g) (ALL) | 2 | 1990 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.28, 2.01] |
| 35 Very premature birth (less than 34 weeks' gestation) (ALL) | 2 | 3053 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.30, 1.12] |
| 36 Infant Hb concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 37 Infant serum ferritin concentration in the first 6 months (in μg/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 38 Admission to special care unit (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.21, 0.55] |
| 40 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 41 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 42 Maternal Hb concentration at or near term (in g/L at 34 weeks' gestation or more) (ALL) | 2 | 771 | Mean Difference (IV, Random, 95% CI) | 12.44 [0.95, 23.93] |
| 43 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL) | 1 | 297 | Mean Difference (IV, Random, 95% CI) | 9.20 [5.78, 12.62] |
| 44 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 2 | 1042 | Risk Ratio (M‐H, Random, 95% CI) | 4.33 [2.26, 8.30] |
| 45 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 2 | 967 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [0.32, 10.84] |
| 46 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 1 | 353 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.18, 0.81] |
| 47 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL) | 2 | 773 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 48 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 2 | 386 | Risk Ratio (M‐H, Random, 95% CI) | 0.08 [0.00, 1.33] |
| 49 Puerperal infection (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.20, 4.75] |
| 50 Antepartum haemorrhage (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.43, 4.22] |
| 51 Postpartum haemorrhage (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 3.38 [0.71, 16.15] |
| 52 Transfusion provided (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 2.89 [0.12, 70.83] |
| 53 Diarrhoea (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.16, 1.87] |
| 54 Constipation (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.55, 2.23] |
| 55 Nausea (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.47, 1.99] |
| 56 Heartburn (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.65 [0.66, 4.15] |
| 57 Vomiting (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 58 Maternal wellbeing/satisfaction (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 59 Placental abruption (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.24, 3.83] |
| 60 Premature rupture of membranes (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.74, 1.34] |
| 61 Pre‐eclampsia (ALL) | 1 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 3.22 [0.89, 11.59] |
| 62 Mental development index in infants at 3 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 63 Mental development index in infants at 6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 64 Mental development index in infants at 12 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 65 Mental development index in infants at 18 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 66 Mental development index in infants at 24 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 67 Mental development index in infants at 18 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 68 Psychomotor development index in infants at 3 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 69 Psychomotor development index in infants at 6 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 70 Psychomotor development index in infants at 12 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 71 Psychomotor development index in infants at 24 months | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.2. Analysis.
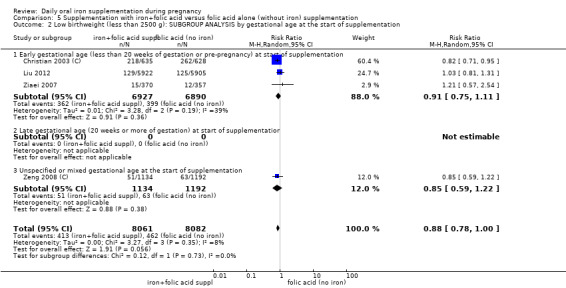
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 2 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
5.3. Analysis.
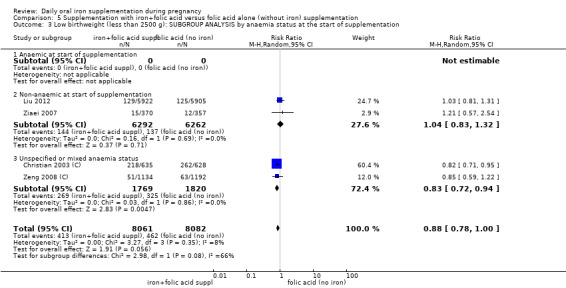
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 3 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
5.4. Analysis.
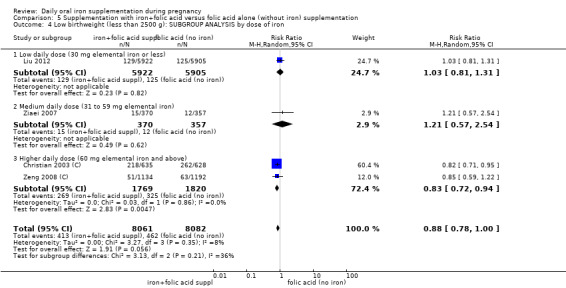
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 4 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by dose of iron.
5.5. Analysis.
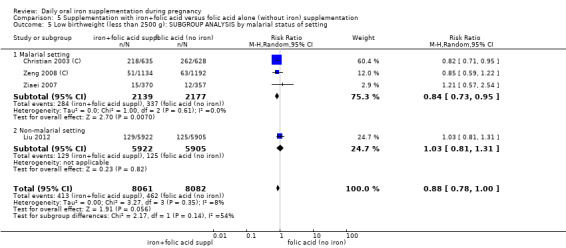
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 5 Low birthweight (less than 2500 g): SUBGROUP ANALYSIS by malarial status of setting.
5.7. Analysis.
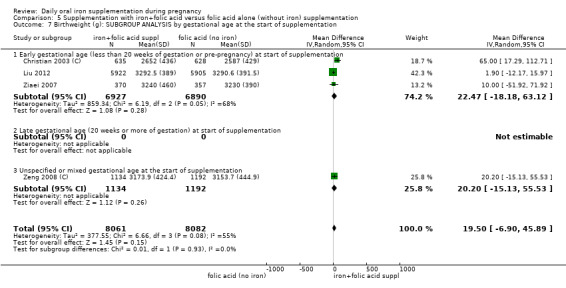
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 7 Birthweight (g): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
5.8. Analysis.
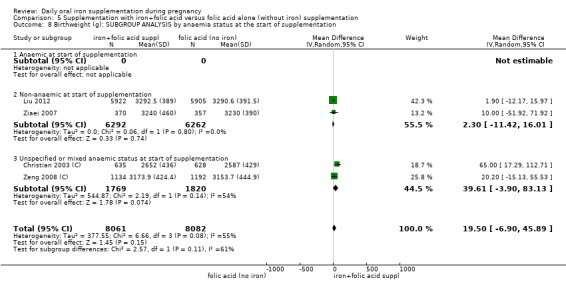
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 8 Birthweight (g): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
5.9. Analysis.
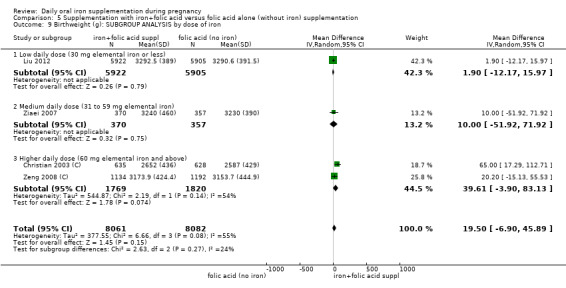
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 9 Birthweight (g): SUBGROUP ANALYSIS by dose of iron.
5.10. Analysis.
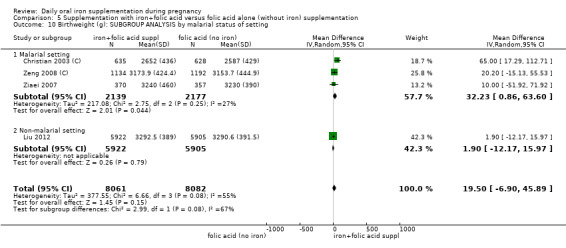
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 10 Birthweight (g): SUBGROUP ANALYSIS by malarial status of setting.
5.12. Analysis.
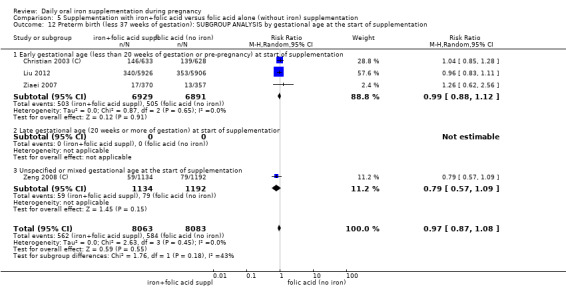
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 12 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
5.13. Analysis.
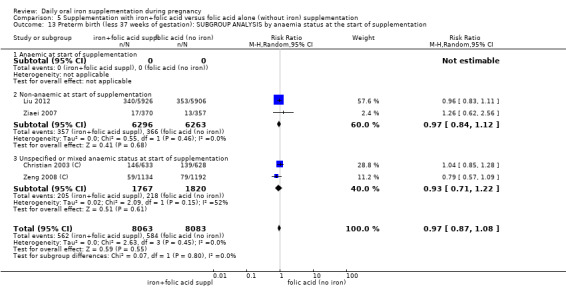
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 13 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
5.14. Analysis.
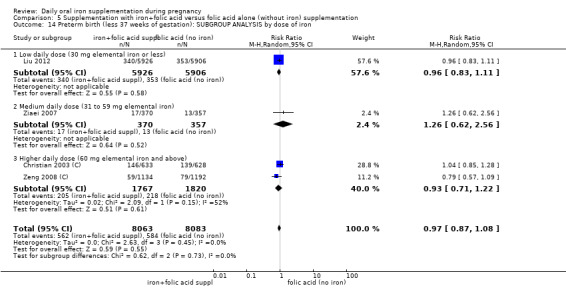
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 14 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by dose of iron.
5.15. Analysis.
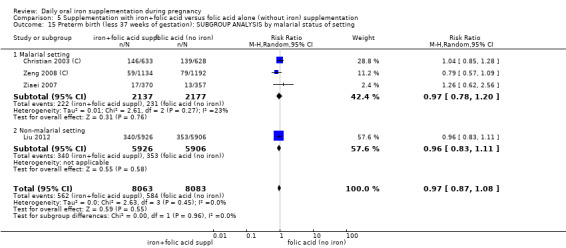
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 15 Preterm birth (less 37 weeks of gestation): SUBGROUP ANALYSIS by malarial status of setting.
5.17. Analysis.
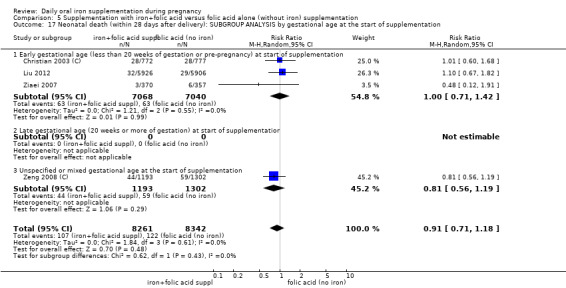
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 17 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
5.18. Analysis.
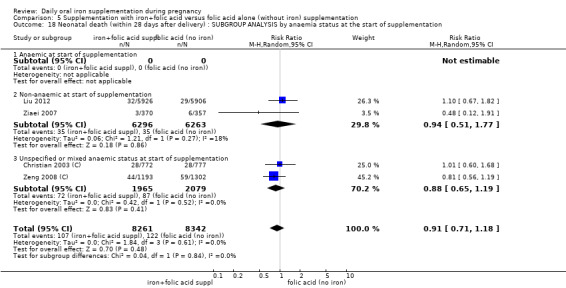
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 18 Neonatal death (within 28 days after delivery) : SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
5.19. Analysis.
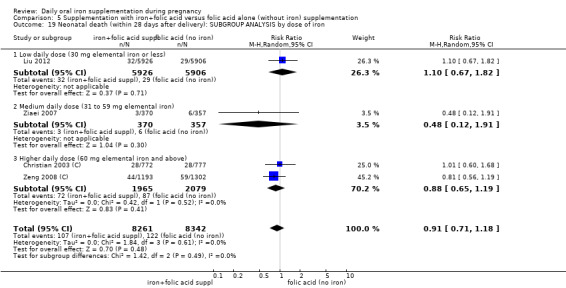
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 19 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by dose of iron.
5.20. Analysis.
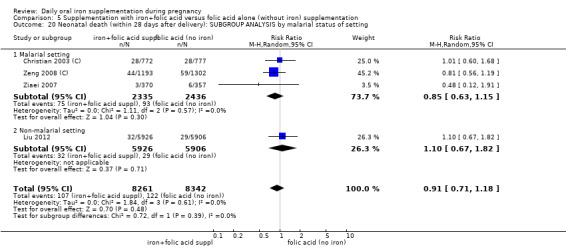
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 20 Neonatal death (within 28 days after delivery): SUBGROUP ANALYSIS by malarial status of setting.
5.23. Analysis.
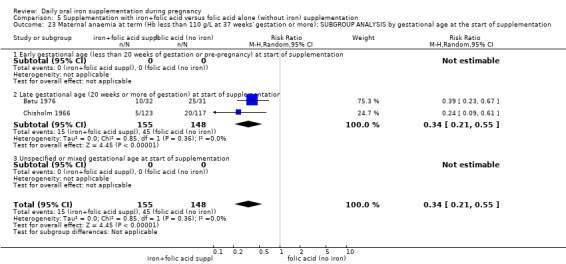
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 23 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by gestational age at the start of supplementation.
5.24. Analysis.
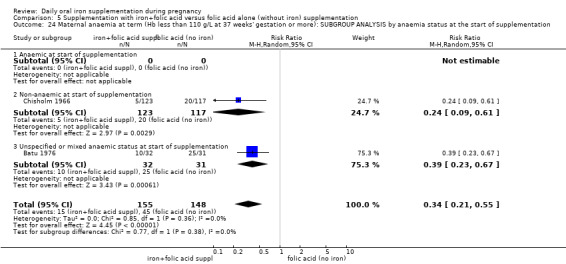
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 24 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more): SUBGROUP ANALYSIS by anaemia status at the start of supplementation.
5.25. Analysis.
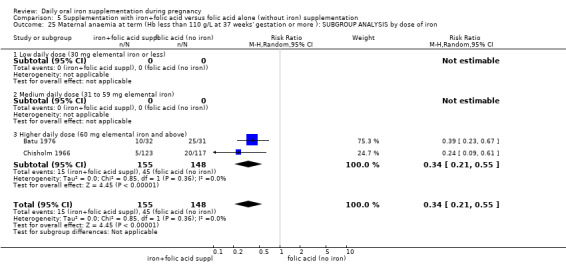
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 25 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more ): SUBGROUP ANALYSIS by dose of iron.
5.26. Analysis.
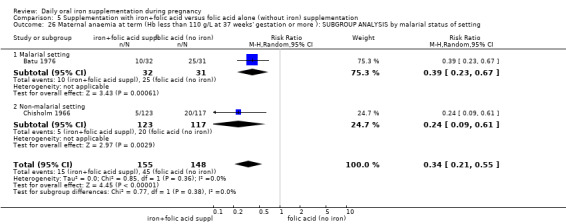
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 26 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more ): SUBGROUP ANALYSIS by malarial status of setting.
5.34. Analysis.
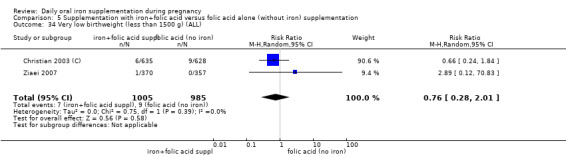
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 34 Very low birthweight (less than 1500 g) (ALL).
5.35. Analysis.
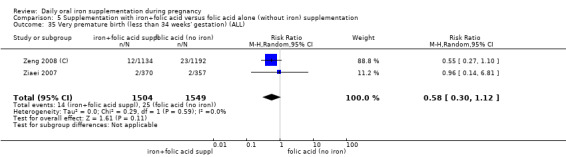
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 35 Very premature birth (less than 34 weeks' gestation) (ALL).
5.43. Analysis.
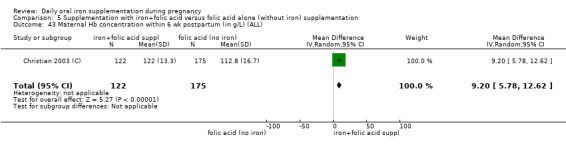
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 43 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL).
5.46. Analysis.
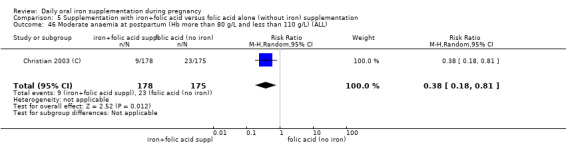
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 46 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL).
5.47. Analysis.
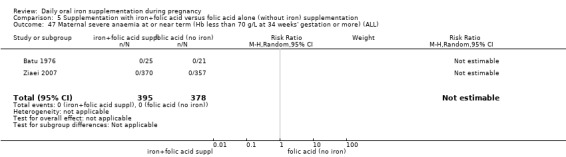
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 47 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL).
5.48. Analysis.
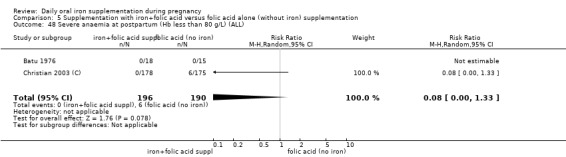
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 48 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL).
5.49. Analysis.
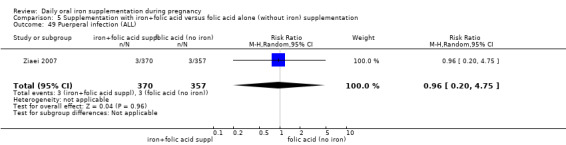
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 49 Puerperal infection (ALL).
5.50. Analysis.
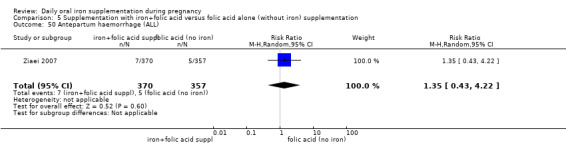
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 50 Antepartum haemorrhage (ALL).
5.51. Analysis.
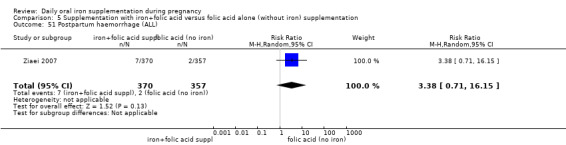
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 51 Postpartum haemorrhage (ALL).
5.52. Analysis.
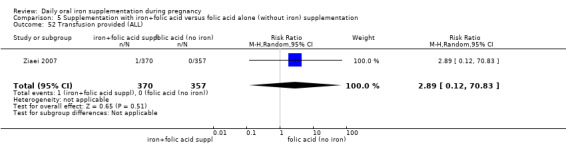
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 52 Transfusion provided (ALL).
5.53. Analysis.
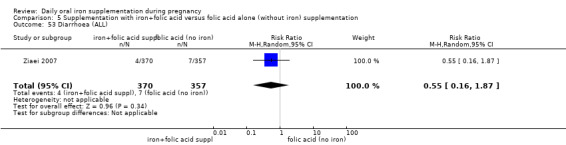
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 53 Diarrhoea (ALL).
5.54. Analysis.
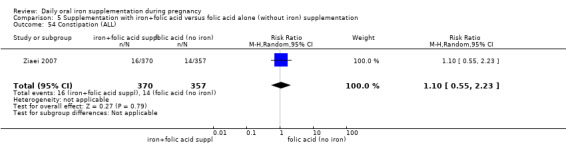
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 54 Constipation (ALL).
5.55. Analysis.
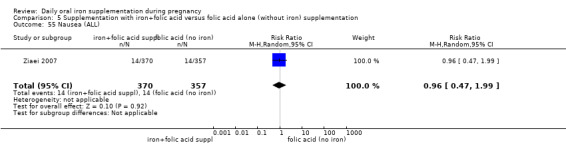
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 55 Nausea (ALL).
5.56. Analysis.
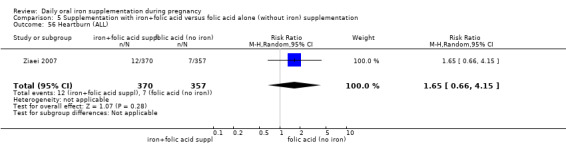
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 56 Heartburn (ALL).
5.59. Analysis.
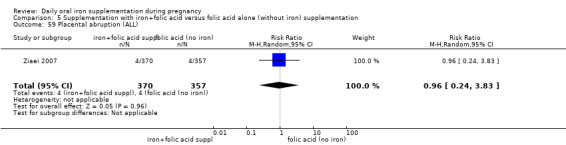
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 59 Placental abruption (ALL).
5.60. Analysis.
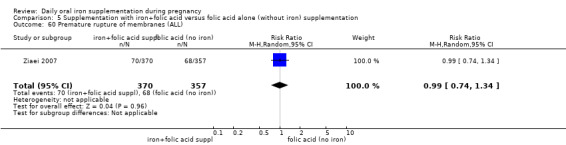
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 60 Premature rupture of membranes (ALL).
5.61. Analysis.
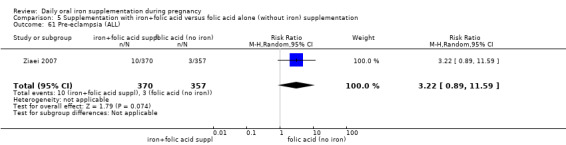
Comparison 5 Supplementation with iron+folic acid versus folic acid alone (without iron) supplementation, Outcome 61 Pre‐eclampsia (ALL).
Comparison 6. Supplementation with iron+other vitamins and minerals supplementation versus same other vitamins and minerals (without iron) supplementation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Low birthweight (less than 2500 g) (ALL) | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.22, 1.15] |
| 2 Birthweight (g) (ALL) | 2 | 1116 | Mean Difference (IV, Random, 95% CI) | 55.70 [3.42, 107.97] |
| 3 Preterm birth (less than 37 weeks of gestation) (ALL) | 2 | 1127 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.41, 1.04] |
| 4 Neonatal death (within 28 days after delivery) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Congenital anomalies (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Maternal anaemia at term (Hb less than 110 g/L at 37 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Maternal iron deficiency at term (as defined by trialists, based on any indicator of iron status at 37 weeks' gestation or more)(ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Maternal iron‐deficiency anaemia at term (Hb less than 110 g/L and at least one additional laboratory indicators at 37 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Maternal death (death while pregnant or within 42 days of termination of pregnancy) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Side effects (any reported throughout the intervention period) (ALL) | 1 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.55, 1.07] |
| 11 Maternal severe anaemia at any time during second and third trimester (Hb less than 70 g/L) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Maternal clinical malaria | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Infection during pregnancy (including urinary tract infections) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Very low birthweight (less than 1500 g) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Very premature birth (less than 34 weeks' gestation) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Infant Hb concentration in the first 6 months (in g/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Infant serum ferritin concentration in the first 6 months (in μg/L, counting the last reported measure after birth within this period) (ALL) | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Admission to special care unit (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Maternal anaemia at or near term (Hb less than 110 g/L at 34 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Maternal iron deficiency at or near term (as defined by trialists, based on any indicator of iron status at 34 weeks' gestation or more)(ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Maternal iron‐deficiency anaemia at or near term (Hb less than 110 g/L and at least one additional laboratory indicators at 34 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Maternal Hb concentration at or near term (in g/L at 34 weeks' gestation or more) (ALL) | 2 | 809 | Mean Difference (IV, Random, 95% CI) | 10.85 [7.29, 14.42] |
| 23 Maternal Hb concentration within 6 wk postpartum (in g/L) (ALL) | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 14.0 [3.56, 24.44] |
| 24 Maternal high haemoglobin concentrations during second or third trimester (Hb more than 130 g/L) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Maternal high haemoglobin concentrations at or near term (Hb more than 130 g/L at 34 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 26 Moderate anaemia at postpartum (Hb more than 80 g/L and less than 110 g/L) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Maternal severe anaemia at or near term (Hb less than 70 g/L at 34 weeks' gestation or more) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 28 Severe anaemia at postpartum (Hb less than 80 g/L) (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 29 Puerperal infection (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 30 Antepartum haemorrhage (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 31 Postpartum haemorrhage (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 32 Transfusion provided (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 33 Constipation (ALL) | 1 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.55, 1.07] |
| 34 Nausea (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Heartburn (ALL) | 1 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.34] |
| 36 Vomiting (ALL) | 1 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.58, 2.20] |
| 37 Diarrhoea (ALL) | 1 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.29, 0.96] |
| 38 Maternal wellbeing/satisfaction (ALL) | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 39 Placental abruption (ALL) | 1 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [0.46, 7.20] |
| 40 Premature rupture of membranes (ALL) | 1 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.44, 1.41] |
| 41 Pre‐eclampsia (ALL) | 1 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.67, 3.16] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Barton 1994.
| Methods | RCT, 2‐arm trial with individual randomisation. | |
| Participants | 97 healthy women attending prenatal care at National Maternity Hospital, Dublin, Ireland with singleton pregnancy, during their first trimester of pregnancy, and with Hb equal or higher than 140 g/L were assigned to the groups. Women were excluded if they had a recent blood transfusion, chronic respiratory disease, chronic hypertension, renal disease, diabetes mellitus, history of haematologic disorder and alcohol dependence. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups:
group 1: received 60 mg elemental iron and 500 μg (0.5 mg) of folic acid to be taken by mouth twice daily;
group 2: placebo tablets also to be taken by mouth twice daily.
Supplementation started at 12 weeks until delivery. No postpartum supplementation. Setting and health worker cadre: the intervention was performed by physicians at the National Maternity Hospitalin Dublin, Ireland. |
|
| Outcomes | Maternal: Hb, HCT, serum erythropoietin concentrations at baseline and at 24, 28, 32, 36 and 40 weeks; serum ferritin at baseline and at 36 weeks; number of hypertensive disorders, antepartum haemorrhage, caesarean delivery. Infant: perinatal death, birthweight below 10th percentile, Apgar score, need for neonatal resuscitation and admission to neonatal intensive care unit data recorded but not reported in paper. Cord blood values of Hb, HCT, serum ferritin, and erythropoietin concentrations. | |
| Notes | Unsupervised.
No participants were withdrawn because of anaemia.
Compliance not reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks of gestation) (12 weeks until delivery). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (60 mg elemental iron or more) (120 mg elemental iron). Iron release formulation: normal release/not specified. Iron compound: not specified. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information reported on the method used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Reported as double blind. The placebo tablets were identical in size, colour and shape to the iron and folic acid supplements and contained the same excipients. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was not clear whether those assessing outcomes were aware of allocation, but it is unlikely that this possible lack of blinding affected the laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | No baseline imbalance apparent. |
Batu 1976.
| Methods | RCT, 4‐arm trial with individual randomisation. | |
| Participants | 133 women referred to investigators from a population of women attending an antenatal clinic for the fist time in Yangoon (also known as Rangoon), Myanmar (Burma). Women with severe anaemia were excluded from the trial during the intervention for treatment. | |
| Interventions | Participants were randomly assigned to 1 of 4 groups starting at 22‐25 weeks:
group 1: 60 mg of elemental iron (as ferrous sulphate), and 1 placebo tablets twice daily;
group 2: 1 tablet containing 60 mg of elemental iron (as ferrous sulphate), and 1 tablet containing 500 μg (0.5 mg) of folic acid twice daily; group 3: 2 placebo tablets twice daily; group 4: 1 placebo tablet and 1 tablet containing 500 μg (0.5 mg) of folic acid twice daily. Administration of the treatments was carefully supervised. Supplementation started at 22‐25 weeks until term. Setting and health worker cadre: the intervention was performed by physicians at an antenatal clinic in Rangoon, Burma. |
|
| Outcomes | Maternal: Hb concentrations at baseline, at term (38‐40th week) and 4‐7 weeks postpartum, serum iron, serum and red cell folate activity and hypersegmented polymorph count at baseline, at 38‐40th week and postpartum. | |
| Notes | Supervised. 32 women who had taken other supplements or whose Hb level at full term was not available were excluded from the analysis. 3 women from group 3 and 2 from group 4 developed severe anaemia and were also withdrawn from analysis. Gestational age at start of supplementation: late gestational age (more than 20 weeks at the start of supplementation) (22‐25 weeks' gestation). Anaemic status at start of supplementation: unspecified/mixed anaemia status at the start of supplementation (women with severe anaemia excluded). Daily iron dose: higher daily dose (60 mg elemental iron or more) (120 mg of elemental iron). Iron release formulation: normal release iron supplement/not specified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due predominantly to P. falciparum exists throughout the year at altitudes below 1000 m, excluding the main urban areas of Mandalayand Yangon. Risk is highest in remote rural, hilly and forested areas. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. Mefloquine resistance reported in Kayin state and the eastern part of Shan state. P. vivax resistance to chloroquine reported. Human P. knowlesi infection reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated; "randomly placed in one of four treatment regimens". |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information reported on the method used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo‐controlled trial so it is likely that staff and women were blind to allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was not clear whether those assessing outcomes were aware of allocation, but it is unlikely that this possible lack of blinding affected the laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 37 women (28%) were excluded for analysis. 133 women randomised "32 women who had taken other hematinics or whose Hb level at full term was not available were excluded". 5 women developed anaemia and were given treatment. Loss was not balanced across groups. |
| Selective reporting (reporting bias) | High risk | 32 women who had taken other supplements or whose Hb level at full term was not available were excluded from the analysis. 3 women from group 3 and 2 from group 4 developed severe anaemia and were also withdrawn from analysis. |
| Other bias | Low risk | No baseline imbalance apparent. |
Butler 1967.
| Methods | RCT, 3‐arm trial with individual randomisation. | |
| Participants | 200 women before 20th week of gestation and Hb above 100 g/L attending antenatal clinic at the Maternity Hospital in Glossop Terrace, Cardiff, United Kingdom were studied. Exclusion criteria included urinary infection and threatened miscarriage, confusion over therapy, intercurrent illness and difficult veins, intolerant to the iron form, premature labor. | |
| Interventions | Participants were randomly allocated to 1 of 3 groups:
group 1: received 122 mg of elemental iron (as ferrous sulphate) daily;
group 2: received 122 mg of elemental iron (as ferrous sulphate) + 3400 μg (3.4 mg) of folic acid daily;
group 3: received no intervention. A group 4 was formed as some participants (n = 38) from group 3 received iron supplements for treatment of anaemia in the course of the intervention. They are excluded from the analysis. Women were supplemented from week 20 to 40 of gestation. Setting and health worker cadre: the intervention was performed by obstetricians and hematologists at the antenatal clinic, Cardiff Maternity Hospital in Cardiff, United Kingdom. |
|
| Outcomes | Maternal: Hb concentrations, blood and plasma volume, HCT (not reported), MCV, albumin and globulin fractions at weeks 20, 28, 36 and 40 of gestation and at the first postanal visit, oedema, intrapartum haemorrhage. | |
| Notes | Unsupervised.
154 women were followed through to the postnatal visit. Only 16 women (30%) in the no‐treatment group remained untreated.
Compliance not reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: mixed anaemia status (Hb above 100 g/L). Daily iron dose: higher daily dose (60 mg of elemental iron or more) (122 mg elemental iron). Iron release formulation: normal release iron supplement/not specified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised list stratified by age, parity and initial Hb level. |
| Allocation concealment (selection bias) | Low risk | The code was not opened for the iron and iron + folic acid group until the end of the investigation, thus clinical staff could not anticipate the randomisation sequence. There was no treatment for 1 group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participant and provider were blinded to treatment for groups 1 and 2. The control group received no treatment and did not get a placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was not clear whether those assessing outcomes were aware of allocation, but it is unlikely that this possible lack of blinding affected the laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% were lost to follow‐up to the postnatal visit. 154 women were randomised and for many outcomes there were missing data. 70% of the 54 women initially allocated to the no treatment group received iron supplements for anaemia (as there was no placebo, staff would be aware that women were not receiving supplements). Results for those women treated or not treated in the control group were reported separately. Results are therefore difficult to interpret. |
| Selective reporting (reporting bias) | Low risk | Authors provided the full database for this review. |
| Other bias | Low risk | No baseline imbalance apparent. |
Buytaert 1983.
| Methods | RCT, 2‐arm trial with individual randomisation. | |
| Participants | 45 non‐anaemic women with singleton pregnancy and no major illnesses attending the University Hospital Obstetric and Gynaecologic Clinic in Antwerp, Belgium. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups:
group 1: received 105 mg of elemental iron (as ferrous sulphate sustained release preparation) daily;
group 2: received no iron supplement.
Supplementation started at 14‐16th week of gestation and continued until delivery. Setting and health worker cadre: the intervention was performed by obstetricians at the University Hospital Obstetrical Clinic of the Erasmus University at Rotterdam, The Netherlands or the University Hospital Obstetric and Gynecologic Clinic in Antwerp, Belgium. |
|
| Outcomes | Maternal: Hb, serum iron, serum transferrin and serum ferritin concentrations at 16, 28, 36 weeks, delivery and 6 weeks postpartum. | |
| Notes | Unsupervised. The randomisation was made for each clinic in Antwerp, and the results are presented separately by clinic. Compliance not reported. We treated this study carried out collaboratively in 2 different sites as 2 different trials, 1 conducted in Rotterdam (Wallenburg 1983) and 1 conducted in Antwerp (Buytaert 1983). Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation) (14th‐16th week). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher dose of iron (60 mg of elemental iron or more) (105 mg elemental iron). Iron release formulation: sustained release preparation. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random table numbers. |
| Allocation concealment (selection bias) | Low risk | By means of sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participant nor provider blinded. No placebo used. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Management was altered depending on outcomes (women in the no treatment group who developed anaemia were treated). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Cantlie 1971.
| Methods | RCT, 2‐arm trial with individual randomisation. | |
| Participants | 27 apparently healthy non‐anaemic pregnant women 17‐35 years of age from 4 participating obstetricians' private practice clinics from Montreal, Canada in their 1‐5th month of pregnancy with Hb 120 g/L or higher in first trimester and 110 g/L or higher in second trimester. Women with history of pathological blood loss or gross dietary imbalance were excluded. | |
| Interventions | Participants were randomly assigned to 2 groups:
group 1 received 39 mg elemental iron (Mol‐Iron®, ferrous iron) to be taken twice daily with meals (total daily 78 mg elemental iron);
group 2 who received no iron tablets. As a co‐intervention, both groups received 1 tablet of multiple micronutrient supplement daily containing: 2 mg copper citrate, 6 mg magnesium stearate, 0.3 mg manganese carbonate, 1000 IU vitamin A , 500 IU vitamin D, bone flour 130 mg, 1 mg vitamin B1, 1 mg vitamin B2, 50 mg brewer yeast concentrate, 5 mg niacinamide, 25 mg vitamin C, 0.2 mg sodium iodide and 0.049 μg folate (naturally occurring). Duration of supplementation unclear. Setting and health worker cadre: the intervention was performed by obstetricians and hematologists at the McGill University Medical Clinic, Royal Victoria Hospital in Montreal, Canada. Participant, of higher SES, were of recruited from private obstetrical practices. |
|
| Outcomes | Maternal: Hb concentration, PCV, reticulocyte count, sedimentation rate, total white blood cell and differential counts, serum iron, unsaturated and total iron binding capacity, serum B12, serum and RBC folate at baseline and at 32, 36, 39th weeks and 7 days postpartum. | |
| Notes | Supervision unclear.
Compliance not reported. Gestational age at start of supplementation: mixed gestational age (1‐5th month of pregnancy). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (60 mg elemental iron or more) (78 mg elemental iron). Iron release formulation: normal release iron supplement/not specified. Iron compound: Mol‐Iron®, ferrous iron. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated; "divided randomly". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Women and staff were not blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was not clear whether those assessing outcomes were aware of allocation, but it is unlikely that this possible lack of blinding affected the laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 27 women were randomised. 26 mentioned in the discussion; denominators were not provided for the results. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | Women in the intervention group had higher median serum folate levels at baseline (not sig). |
Chan 2009.
| Methods | RCT (placebo controlled) 2‐arm trial, individual randomisation. | |
| Participants | 1164 pregnant women with singleton pregnancies with a gestational age of 16 weeks or less able to understand English or Chinese attending their first antenatal care visit at Queen Mary Hospital, Hong Kong between April 2005 and March 2007. Exclusion criteria: women with existing diabetes, haemoglobinopathies, Hb levels < 80 g/L or > 140 g/L, women with possible thalassaemia (MCV < 80), women diagnosed with gestational diabetes at booking. |
|
| Interventions | Participants were randomly assigned to 1 of 2 groups:
group 1: (n = 565 women) received 60 mg of elemental iron orally (as 300 mg ferrous sulphate) daily;
group 2: (n = 599 women) received daily placebo indistinguishable in appearance from the active supplements. Women in both groups were provided with a supply for 16 weeks. At 28‐30 weeks further supplements were provided (up to 36 weeks) as long as women had not developed gestational diabetes mellitus or Hb level was > 140 g/L. If women in the placebo group developed anaemia (Hb < 80 g/L), they were given iron supplements as clinically indicated. Baseline investigations included a full blood count including Hb and HCT, MCV, white cells and platelets along with serum ferritin concentration. A OGIT was carried out at baseline for women with risk factors for gestational diabetes (e.g. advanced maternal age, family history of diabetes). Otherwise women in both groups received standard antenatal care. Setting and health worker cadre: the intervention was performed by physicians at a regional university teaching hospital in Hong Kong. |
|
| Outcomes | Follow‐up at 28 weeks and 36 weeks' gestation and delivery and 3 days postpartum. Main outcome: development of gestational diabetes at 28 or 36 weeks. (According to WHO criteria for impaired glucose tolerance test (OGTT 2‐hour value > or = 7.8 < 11.1 mmol/L) or diabetes (OGTT 2‐hour value > or = 11.1 mmol) both were considered as gestational diabetes mellitus). Other maternal outcomes: Hb (g/L), serum transferrin (g/L), serum ferritin (pmol/L), compliance, glucose level, mode of delivery. Neonatal outcomes: gestational age at delivery, preterm delivery, birthweight, Apgar score at 1 and 5 minutes, arterial blood pH, Hb of cord blood (g/L), ferritin of cord blood (pmol/L), jaundice, birth trauma, infection, congenital abnormality or metabolic disorder. |
|
| Notes | Very high attrition (> 50% for outcomes at 36 weeks). 45.6% of controls and 43.1% of women in the study group were taking additional vitamin supplements. As the results reported in the paper were not completely clear to us we preferred not to use the reported SDs and removed the information from this trial for continuous variables, while awaiting clarification from the authors. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks) (16 weeks or less). Anaemic status at start of supplementation: mixed anaemia status (Hb levels > 80 and < 140 g/L). Daily iron dose: higher dose (60 mg elemental iron). Iron release formulation:normal release iron supplement/not specified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by a research nurse who was not involved in patient recruitment. Block randomisation with computer generation of sequence. The block size was 100. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. The envelopes were sequentially numbered and sealed (by nurse A who did the block randomisation) and all the envelopes were accounted for. The research assistant who recruited the patients (nurse B) would sequentially open the numbered envelopes after the patient had consented to participate in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants blinded; placebo‐controlled. After randomisation “The participants but not the research assistants were blinded to group assignment”. Staff and research nurses were aware of the group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes were assessed by the principle investigator (the outcomes are mainly objective outcomes such as OGTT results, blood counts, birthweight, etc).Women who developed anaemia were treated and those developing gestational diabetes withdrawn. Compliance, side effect and other outcomes reported as well as laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1164 women were randomised. It was stated that an ITT analysis was performed but data tables suggest there were missing data for most outcomes at 28 and 36 weeks and at delivery; e.g. at 28 weeks 90.3% attended for follow‐up. Neonatal outcome data were available for 74% of those randomised. There were very high levels (> 50%) of missing data for lab values at 36 weeks. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | No baseline imbalance between groups apparent. |
Chanarin 1965.
| Methods | Randomised controlled trial with 3 arms. | |
| Participants | 190 pregnant women before 16 week of gestational age attending antenatal clinic for the first time in St Mary's Hospital in London, England, United Kingdom were invited to participate in the study and 189 accepted. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups:
group 1 received 3 tablets containing 100 mg of ferrous fumarate to be taken daily (total 300 mg ferrous fumarate daily);
group 2 received 3 tablets containing 100 mg of ferrous fumarate with 10 μg (0.01 mg) folic acid (total 300 mg ferrous fumarate and 30 μg (0.03 mg) folic acid daily;
group 3 placebo (containing lactose). Setting and health worker cadre: the intervention was performed by obstetricians and pathologists at the antenatal clinic of St. Mary's Hospital in London, United Kingdom. |
|
| Outcomes | The outcomes measured include full blood count at 20th, 30th, 35th and 39th week of gestation and 6th day after delivery. | |
| Notes | The paper does not report SDs in the variables measured and no data can be extracted. The trial is included but does not contribute data for the analysis. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: unspecified or mixed anaemia status. Daily iron dose: higher daily dose (60 mg of elemental iron or more). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous fumarate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Methods not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Partial blinding. This was a placebo‐controlled trial bottles containing medication were colour coded but it was stated that staff were not aware of the colour coding during the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | It was stated that some women in the placebo group with anaemia were treated and withdrawn from the analysis for haematological outcomes; it was not clear whether staff were aware of allocation at the point of withdrawing these women. Excluding this section of the sample makes findings for the placebo group biased for these outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 189 women were randomised but only 154 completed the study but not all samples could be obtained from every participant. 35 women were further withdrawn from the trial. 9 participants in the placebo group and 1 in the iron + folic acid group required parenteral iron nutrition and were withdrawn from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Chanarin 1971.
| Methods | Quasi‐RCT. 5‐arm trial with individual randomisation. | |
| Participants | 251 women attending antenatal clinic at St Mary's Hospital, London, United Kingdom before 20th week of gestation. | |
| Interventions | Participants were allocated by sequence to 1 of 5 groups:
group 1: oral dose of 30 mg of elemental iron (as ferrous fumarate) daily;
group 2: oral dose of 60 mg of elemental iron (as ferrous fumarate) daily;
group 3: oral dose of 120 mg of elemental iron (as ferrous fumarate) daily;
group 4: placebo;
group 5: 1 g of iron (Imferon, 4 x 250 mg) intravenously before week 20, and thereafter oral 60 mg of elemental iron (as ferrous fumarate) daily (not included in this review).
Supplementation started at 20th week until 37th week. Only the data related to comparisons of group 1: oral dose of 30 mg of elemental iron daily with group 4: placebo are used in this review given that no data for the other groups could be desegregated. Setting and health worker cadre: the intervention was performed by obstetricians and pathologists at the antenatal clinic of St. Mary's Hospital in London, United Kingdom. |
|
| Outcomes | Maternal: full blood count, serum iron at 20, 25, 30 and 37th week. Sternal marrow aspiration at 37 weeks; antepartum haemorrhage, threatened abortion, urinary tract infection, fetal abnormalities, pregnancy hypertension, premature delivery and puerperal infection measured but not reported by groups. Infant: birthweight (not reported by groups). | |
| Notes | Compliance not reported. Gestational age at start of supplementation: late gestational age (supplementation started at 20 weeks' gestation). Anaemic status at start of supplementation: unspecified/mixed anaemia status. Daily iron dose: different doses in different arms of trial (group 1 lower daily dose: 30 mg; group 2 and 3 higher daily dose 60 mg or more). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous fumarate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised study, assignment by sequence. |
| Allocation concealment (selection bias) | High risk | Women were "allocated in sequence to one of five groups"; allocation order could therefore be anticipated. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | 1 of 5 groups was given an IV medication (not included in this review). The other 4 were given iron or placebo tablets and for the oral medication it was stated that women and staff were not aware of which treatment women were receiving. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Women who developed anaemia were withdrawn from the study. It was not clear at what point investigators were aware of treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was not clear exactly how many women were randomised; there were approximately 50 in each of 5 groups. 11 women (9 from the placebo group) were withdrawn and given treatment for anaemia "after allowance had been made for the subjects dropping out of the study... there were just under 50 subjects in each group". |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Charoenlarp 1988.
| Methods | RCT. Series of treatment conditions. | |
| Participants | 325 pregnant women with Hb (AA) and 232 pregnant women with Hb (AE) attending midwife centres in 80 villages from the Varin Chamrab district of Ubon Province, Thailand. Chronic illness, complicated pregnancy, severe anaemia (Hb < 80 g/L), haemoglobinopathies Hb (EE) and (EF), and unwillingness to co‐operate were reason for exclusion. Individuals with Hb (AA) have normal Hb genes. Individuals with Hb (AE) have a heterozygous Hb E trait with normal Hb gene (A‐adults) and an abnormal Hb gene (E). This is usually a clinically insignificant condition. | |
| Interventions | Participants were divided into 2 groups according to Hb (AA) and Hb (AE) and studied separately. Women from each group were randomly assigned to 1 of the following 11 interventions: group 1: placebo, supervised; group 2, 120 mg of elemental iron (as ferrous sulphate) and 5000 μg (5 mg) folic acid daily supervised; group 3, 240 mg of elemental iron (as ferrous sulphate) daily supervised; group 4: 240 mg of elemental iron (as ferrous sulphate) daily supervised; group 5: 120 mg elemental iron (as ferrous sulphate) and 5000 μg (5 mg) of folic acid, motivated but unsupervised; group 6: 240 mg of elemental iron (as ferrous sulphate) and 5000 μg (5 mg) of folic acid daily, motivated but unsupervised. For the Hb (AE) group, women were randomly assigned to 1 of the following groups: group 7: placebo, supervised; group 8: 240 mg elemental iron (as ferrous sulphate) and 5000 μg (5 mg) of folic acid daily, supervised; group 9: 240 mg of elemental iron (as ferrous sulphate) daily, supervised; group 10: 120 mg of elemental iron (as ferrous sulphate) and 5000 μg (5 mg) of folic acid daily, motivated but unsupervised; group 11: 240 mg of elemental iron and 5000 μg (5 mg) of folic acid daily, motivated but unsupervised. Starting and ending time of supplementation not stated. Setting and health worker cadre: the intervention was performed by community health workers under the supervision of a midwife and was delivered to the home of participants living in villages near Ubon, Thailand. Intervention was coordinated from village midwife centres. |
|
| Outcomes | Maternal: Hb, serum ferritin after 10 and 15 weeks of supplementation, and side effects. | |
| Notes | Groups 1, 2, 3, 4, 7, 8, 9 supervised. Groups 5, 6, 10 and 11 motivated but unsupervised. For purposes of analysis, the groups were merged by iron alone or iron‐folic acid, and included as daily higher doses in both cases.
Compliance not reported. Gestational age at start of supplementation: gestational age not specified. Anaemic status at start of supplementation: unspecified/mixed anaemia status. Daily iron dose: higher daily dose (60 mg or more of elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria: Malaria risk exists throughout the year in rural, especially forested and hilly, areas of the whole country, mainly towards the international borders, including the southernmost provinces. There is no risk in cities (e.g. Bangkok, Chiang Mai city, Pattaya), Samui island and the main tourist resorts of Phuket island. However, there is a risk in some other areas and islands. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. Resistance to mefloquine and to quinine reported from areas near the borders with Cambodia and Myanmar. P. vivax resistance to chloroquine reported. Human P. knowlesi infection reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Set of random tables. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo controlled study but 2 of the groups had tablets under supervision (not blinded) and some of the tablets had an odd taste, so this may have affected compliance and reporting of side effects. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment was only partially blinded and it is not clear what he impact of lack of blinding would be on some outcomes, although laboratory outcomes would be likely to be of low risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ranged from 10% to 15%. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Chisholm 1966.
| Methods | RCT, 6 arms. | |
| Participants | 360 non‐anaemic women attending antenatal clinic at Radcliffe Infirmary, Oxford, United Kingdom before 28th week of gestation, who had not taken iron supplements in the preceding 8 weeks and with Hb >= 102 g/L or a normal serum iron reading. Exclusion criteria: Hb < 110 g/L and serum iron less than 60 μg/L. | |
| Interventions | Participants were randomly assigned to 1 of various combinations of elemental iron as ferrous gluconate and folic acid, as follows:
group 1: 900 mg elemental iron alone daily;
group 2: 900 mg elemental iron and 500 μg (0.5 mg) folic acid daily;
group 3: 900 mg elemental iron and 5000 μg (5 mg) folic acid daily;
group 4: placebo;
group 5: 500 μg (0.5 mg) folic acid daily;
group 6: 5000 μg (5 mg) of folic acid daily. Iron and folic acid placebos were used.
Supplementation started at 28th week until 40th week. Setting and health worker cadre: the intervention was performed by physicians at the antenatal clinic of The Radcliffe Infirmary, Oxford, United Kingdom. |
|
| Outcomes | Maternal: Hb, HCT, serum iron, serum folic acid activity, serum vitamin B12 estimation at 28 weeks of gestation and before delivery. | |
| Notes | Unsupervised.
For purposes of this review, placebo group was the group who received neither iron nor folic acid. Groups 2 and 3 were merged for iron‐folic acid comparisons.
Compliance not reported. Gestational age at start of supplementation: late gestational age (from 28 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (60 mg or more of elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | External randomisation. |
| Allocation concealment (selection bias) | Low risk | Bottles containing the tablets had been numbered by random selection at source and the code was unknown during trial. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind trial. Placebo‐controlled and placebo and active treatment described as indistinguishable. Bottles containing tablets were numbered and treatment allocation was not revealed until after the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Women with anaemia were treated (irrespective or allocation). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up apparent. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Christian 2003 (C).
| Methods | Cluster‐randomised trial with 5 treatment arms. | |
| Participants | 4998 married pregnant women (with positive pregnancy test) living in the south eastern plains district of Sarlahi, Nepal. Widows were excluded. | |
| Interventions | Participants were randomly assigned to 1 of 5 groups:
group 1 received 1000 μg retinol equivalents vitamin A (control) daily;
group 2 received 1000 μg retinol equivalents vitamin A and 400 μg (0.4 mg) folic acid daily;
group 3 received 1000 μg retinol equivalents vitamin A, 400 μg (0.4 mg) folic acid and 60 mg elemental iron (as ferrous fumarate) daily;
group 4 received 1000 μg retinol equivalents vitamin A, 400 μg (0.4 mg) folic acid, 60 mg of elemental iron (as ferrous fumarate) and 30 mg of zinc sulphate daily;
group 5 received 1000 μg retinol equivalents vitamin A, 400 μg (0.4 mg) folic acid, 60 mg elemental iron (as ferrous fumarate), 30 mg of zinc, 10 μg vitamin D, 10 mg vitamin E, 1.6 mg thiamine, 1.8 mg riboflavin, 20 mg niacin, 2.2 mg vitamin B6, 2.6 μg vitamin B12, 100 mg vitamin C, 65 μg vitamin K, 2 mg cooper, and 100 mg magnesium daily. Only groups 1, 2 and 3 are considered in this review. Supplementation started at recruitment and continued until 3 months postpartum in the case of live births of 5 weeks or more after a miscarriage or stillbirth. All participating women were offered deworming treatment (albendazole 400 mg single dose) in the second and third trimester. Supplementation lasted 257.5 days in group 1 (control) and 251.7 days in the group 3 receiving vitamin A, iron and folic acid. Comparisons: group 3 vs group 1: effect of iron supplementation with folic acid; group 3 vs group 2: effect of iron supplementation alone. Setting and health worker cadre: the intervention was performed by community health workers in the home of the participants in remote villages in Sarlahi, Nepal. In Nepal, 8% of women received assistance from an auxiliary nurse midwife or doctor. Dosing and supplement replenishment was done by 426 local female workers, 1 per sector, or about 40 households. |
|
| Outcomes | Maternal: premature delivery, Hb and iron status at baseline in the third trimester (scheduled at 32 week of gestation) and Hb at 6 weeks postpartum, prevalence of anaemia in third trimester and at 6‐week postpartum, severe anaemia postpartum, moderate anaemia during third trimester, moderate anaemia postpartum, moderate high Hb concentrations during third trimester Infant: birthweight, prevalence of low birthweight, perinatal mortality, neonatal mortality, infant deaths, small‐for‐gestational age. | |
| Notes | Supplementation with 1000 μg retinol equivalents vitamin A (control) daily and deworming treatment (albendazole 400 mg single dose) in the second and third trimester at were co‐interventions for purposes of the analysis. Unsupervised but trial personnel visited women twice each week to monitor supplement intake. Compliance during pregnancy measured by pill count was high (median 88%) and did not vary by groups. 98% of the women accepted the albendazole treatment at both times (second and third trimesters). Approximate 50% of women started supplementation before 9 weeks of gestational age. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation:unspecified/mixed anaemia status. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous fumarate. Malaria setting: yes. As of 2011: Malaria risk due predominantly to P. vivax exists throughout the year in rural areas of the 20 Terai districts bordering India, with occasional outbreaks of P. falciparum from July to October inclusive. Seasonal transmission of P. vivax takes place in 45 districts of the inner Terai and mid hills. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cluster‐randomisation. No evidence of recruitment bias. Participants did not know beforehand which cluster they were in. |
| Allocation concealment (selection bias) | Low risk | Coded. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This was described as a double‐blind trial. It was reported that the study supplements were identical in appearance and women, staff, investigators and statisticians were not aware of supplement codes until the end of the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Field staff and investigators were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | This was a cluster‐randomised trial, baseline characteristics did not differ by treatment group in age at baseline, SES, parity, gestational age at enrolment, previous miscarriage. The level of compliance did not differ by groups. Analysis was adjusted for cluster‐design effect. |
Cogswell 2003.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 275 legally competent, non‐imprisoned, non‐anaemic, low‐income pregnant women at < 20 weeks of gestation with ferritin levels above 20 μg/L enrolled at the Cuyahoga County, MetroHealth Center, Supplemental Nutrition Program for Women, Infants and Children in Cleveland, Ohio, USA. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 1 gelatin capsule containing 30 mg of elemental iron (as ferrous sulphate) daily; group 2 received 1 placebo soft gelatin capsule daily for 119 days. Supplementation started at an average of 11 weeks of gestation until delivery. | |
| Outcomes | Maternal: prevalence of anaemia at 28 and 38 weeks, side effects, compliance to treatment, maternal weight gain, iron status (MCV, Hb concentration, serum ferritin, erythrocyte protoporphyrin concentrations at 28 and 38 weeks.
Infant: birthweight, birth length, proportion of low birthweight, low birthweight and premature, small‐for‐gestational age. Setting and health worker cadre: the intervention was performed by a dietician at the Cuyahoga County, MetroHealth Medical Center, Supplemental Nutrition Program for Women, Infants and Children in Cleveland, Ohio, United States of America. |
|
| Notes | Unsupervised. Women were re‐evaluated at 28 weeks of gestation, and according to Hb concentrations at that time were prescribed treatment following the Institute of Medicine guidelines for iron supplementation during pregnancy.
Compliance was 63.4% and 65.2% in groups 1 and 2 respectively. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: lower daily dose (30 mg of elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By computerised random numbers. |
| Allocation concealment (selection bias) | Low risk | Placebo‐controlled trial. Randomisation by study data manager. The placebo and active treatment were indistinguishable and all staff were blind to group allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo‐controlled trial, with placebo indistinguishable from the active treatment. Bottles were coded and treatment group was only known to a data manager. It was stated that women and staff were not aware of treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was stated that laboratory analysts and staff collecting information on side effects were blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Corrigan 1936.
| Methods | Quasi‐randomised trial with allocation by odd or even numbers. 2‐arm trial. | |
| Participants | 200 normal pregnant women attending antenatal care clinic with 3‐7 months of gestational age at Boston City Hospital, Boston, USA. | |
| Interventions | Participants were assigned a number in order. Patients who had been assigned an odd number received 0.2 g of ferrous sulphate (3 tablets daily to be taken after meals ‐ total daily dose 0.6 g); patients with even numbers received placebo that were identical in appearance and size and contained lactose but not ferrous sulphate. Supplements were from recruitment until delivery. Women who took less than 1 of the 2 tablets prescribed daily were excluded. Setting and health worker cadre: the intervention was performed by physicians at the antepartum clinic of Boston City Hospital, Boston, Massachusetts, United States of America. |
|
| Outcomes | Number of women with anaemia at 1‐week postpartum. (Figures were also provided for the mean Hb level at 1‐week postpartum but no SD was provided and we were not able to include these data in the analysis.) | |
| Notes | Mean Hb in the intervention group 117 g/L and 112 g/L in the control group. Gestational age at start of supplementation: mixed gestational age. Anaemic status at start of supplementation: not specified. Daily iron dose: higher daily dose (60 mg or more). Iron release formulation: not specified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised trial, odd/even numbers. |
| Allocation concealment (selection bias) | High risk | Alternate allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | This study was placebo‐controlled but the method of randomisation may have meant that staff were aware of treatment allocation. Also women who did not comply were excluded (and it is possible that there were systematic differences between groups in compliance). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcomes reported unlikely to have been affected by lack of blinding (although it was not clear how many women were excluded after randomisation). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 200 women were randomised and it was stated that women that did not comply (that took on average less than 1 of the prescribed tablets daily) or in whom sepsis or haemorrhage developed during pregnancy, birth or the early postnatal period were excluded. It was not clear how many women were excluded for these reasons and it was not clear whether or not there was any ITT analysis. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | Most of the results were provided in graphs and were not simple to interpret and we have included all of these results in the analyses. Women were described as similar at baseline. The denominators for results were not clear. |
De Benaze 1989.
| Methods | RCT, 2‐arm trial with individual randomisation. | |
| Participants | 191 non‐anaemic pregnant women with 12‐18 weeks of gestation attending antenatal care clinic at the Maternity at Poissy Hospital, Paris, France. Exclusion criteria included women who had taken iron or folate supplements in the prior 6 months and those with language barriers for proper communication. Supplementation started at 12‐18 weeks until delivery. | |
| Interventions | Participants were randomly allocated to 1 of 2 groups:
group 1: daily intake of 45 mg of elemental iron (as ferrous betainate hydrochloride) (15 mg elemental iron per tablet);
group 2: placebo tablets. Setting and health worker cadre: the intervention was performed by physicians at the Maternity Ward of Poissy Hospital, Poissy, France. |
|
| Outcomes | Maternal: Hb, MCV, serum iron, total iron binding capacity, transferrin saturation, serum ferritin at baseline, at 5 months, at 7 months, at delivery and 2 months postpartum. | |
| Notes | Unsupervised.
Serum ferritin values presented as arithmetic and geometric means. No SD in transformed ferritin values is presented. Women in the placebo group were prescribed treatment after delivery thus not allowing comparisons at 2 months postpartum among the groups.
Compliance reported as good. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: medium daily dose (45 mg elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous betainate hydrochloride. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but method used unclear. |
| Allocation concealment (selection bias) | Low risk | Placebo‐controlled trial. Active and placebo tablets were in identical packaging and packages were provided randomly. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | (Assessment from translated notes). Placebo‐controlled trial with active and placebo supplements in identical packaging and tablets were identical in appearance. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Placebo‐controlled trial and laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Dommisse 1983.
| Methods | RCT, 2‐arm trial with individual randomisation. | |
| Participants | 146 pregnant women with less than 20 weeks of gestation who had not received iron therapy recently attending the Peninsula Maternity Service, Department of Obstetrics and Gynecology, University of Cape Town, Groote Schuur Hospital, South Africa. | |
| Interventions | Participants were randomly allocated to receive either a multivitamin tablet twice a day or a multivitamin tablet in conjunction with a standard ferrous sulphate tablet twice a day providing a total of 120 mg of elemental iron daily. Setting and health worker cadre: the intervention was performed by obstetricians and professional staff at the Peninsula Maternity Service of the Department of Obstetrics and Gynecology of the University of Cape Town and Groote Schuur Hospital in Cape Town, South Africa. |
|
| Outcomes | Hb, PCV, MCV, MCHC, serum iron, transferrin, red cell folate, ferritin, iron storage depletion at baseline and at 36 weeks' gestation, compliance. | |
| Notes | Mean Hb and other outcomes at term were reported, but no SDs were provided. We have therefore not been able to include data from this trial in the review. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: mixed/not specified. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due predominantly to P. falciparum exists throughout the year in the low altitude areas of Mpumalanga Province (including the Kruger National Park), Northern Province and north‐eastern KwaZulu‐Natal as far south as the Tugela River. Risk is highest from October to May inclusive. Resistance to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were randomly allocated." |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding mentioned. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No blinding but all outcomes were laboratory measures. The large number of women excluded after randomisation is likely to have affected results and compliance (assessed by unblinded staff) may have been systematically different in the 2 arms of the trial. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 146 were randomised but when compliance was assessed as poor or doubtful, the participant was excluded from the trial. 21 patients were excluded for poor or doubtful compliance and 20 patients delivered before 36th weeks' gestation. Only 105 completed the trial. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Eskeland 1997.
| Methods | RCT, 3‐arm trial with individual randomisation. | |
| Participants | 90 healthy non‐anaemic pregnant women with singleton pregnancy of less than 13 weeks, attending an inner city maternity centre in Bergen, Norway and willing to participate. Exclusion criteria: uncertain gestational age according to menstrual history, Hb concentration < 110 g/L, chronic disease or pregnancy complications (hypertension, diabetes, bleeding), multiple pregnancy, liver enzymes out of normal range and logistic difficulties foreseen at baseline (moving out of area). | |
| Interventions | Participants were randomly allocated to 1 of the following:
group 1: 3 tablets containing 1.2 mg heme iron from porcine blood and 9 mg of elemental iron (as ferrous fumarate) (Hemofer®) and 1 placebo tablet (total 27 mg elemental iron a day);
group 2: 1 tablet containing 27 mg elemental iron (as iron fumarate) with 100 mg vitamin C (Collet®) and 3 placebo tablets;
group 3: 4 placebo tablets.
Supplementation started at 20th week until 38‐40th week. Setting and health worker cadre: the intervention was performed by midwives and physicians at an inner city maternity centre in Bergen, Norway. |
|
| Outcomes | Maternal: Hb, RBC count, HCT, MCV, MCH, MCHC, reticulocytes, serum iron, total iron binding capacity, serum transferrin, erythrocyte protoporphyrin at baseline and at 20, 28, 38 weeks, 8 weeks postpartum, and 6 months postpartum; pregnancy complications: hypertension, pre‐eclampsia, forceps, postpartum haemorrhage, maternal well being and breastfeeding duration. Infant: birthweight and length. | |
| Notes | Unsupervised.
Only groups 1 and 3 (placebo) were included in this review.
Compliance was 81% and 82% in groups 1 and 3 respectively. Gestational age at start of supplementation: late gestational age (supplementation started at or after 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: lower daily dose (less than 30 mg elemental iron daily). Iron release formulation: normal release preparation/not specified. Iron compound: iron fumarate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated. |
| Allocation concealment (selection bias) | Low risk | This was a placebo‐controlled trial. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as a double‐blind trial (placebo controlled). It was stated that staff providing care were not aware of treatment allocation and were only given information about Hb. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind trial and laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 23% and 21% in groups included. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Falahi 2010.
| Methods | RCT, 2 arms with individual randomisation | |
| Participants | 148 non‐anaemic pregnant women, 20‐35 years of age with gestational age less than 20 weeks, primigravidae, BMI less than 25 and less than 30 and Hb concentrations lower than 110 g/L and serum ferritin higher than 20 μg/L who visited the gynaecology centre in Khorramabad city, Lorestan Province, Western Iran. Participants who had diabetes mellitus, renal disease, coronary heart disease, or reported having used multivitamins and minerals, drugs or being on a special diet were excluded. | |
| Interventions | Participants were randomly allocated to 1 of to groups:
group 1 (n = 70) received tablets containing 60 mg elemental iron (as ferrous sulphate);
group 2 (n = 78) received placebo tablets until delivery. Women who were anaemic or iron deficient were referred for medical evaluation and treated. Setting and heath worker cadre: the intervention was performed by physicians at a gynaecology centre in Khorramabad city, Lorestan Province, Western Iran. |
|
| Outcomes | Hb concentration, serum ferritin at baseline, week 28 and at delivery; birthweight, birth length, pregnancy duration. | |
| Notes | Gestational age at start of supplementation: early gestational age (supplementation started less than 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: high daily dose (60 mg elemental iron daily). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due to P. vivax and P. falciparum exists from March to November inclusive in rural areas of the provinces of Hormozgan and Kerman (tropical part) and the southern part of Sistan‐Baluchestan. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | This was a placebo‐controlled trial. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as a triple‐blind trial, placebo‐controlled. Placebos described as indistinguishable from active supplements. It was stated that participants and staff were not aware of treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was stated that staff and analysts were not aware of treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 148 women were randomised. It was not clear whether any women were lost to follow‐up or if there were any missing data. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | Groups appeared comparable at baseline. |
Fenton 1977.
| Methods | Quasi‐randomised trial, 2 arms with individual randomisation. | |
| Participants | 154 pregnant women with less than 14 weeks of gestation, and who had not received or were receiving treatment for a blood disorder at clinic in Cardiff, United Kingdom. | |
| Interventions | Participants were divided into 2 groups according to the day in which they attended the clinic in Cardiff: group 1 received 60 mg of elemental iron (as ferrous sulphate) daily and group 2 received no iron supplement. Setting and health worker cadre: the intervention was performed by physicians at the Antenatal Clinic of the Welsh National School of Medicine at the University Hospital of Wales, Cardiff, United Kingdom. |
|
| Outcomes | Hb concentration, MCV, serum ferritin, serum iron and total iron binding capacity were measured at 10‐14 weeks and at term. | |
| Notes | The data in the paper are presented with no SD values. No data can be extracted from the publication for this review. Gestational age at start of supplementation: early gestational age. Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg or elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | By day of clinic attendance. |
| Allocation concealment (selection bias) | High risk | By day of clinic attendance. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Laboratory outcomes but women were treated for anaemia and this may have affected results for this outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women appear to be accounted for in the analyses; separate figures are provided for women in the control arm who received supplements. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Fleming 1974.
| Methods | RCT with randomisation by blocks of 50 consecutive participants into 5 arms. | |
| Participants | 146 consecutive pregnant women attending a public antenatal clinic in Western Australia before the 20th week of gestation who had not received iron supplements and were willing to participate. Women with Hb < 100.0 g/L were excluded. | |
| Interventions | Participants were randomly assigned in sequences of 50 to 1 of the 5 interventions groups:
group 1 received placebo;
group 2 received 60 mg of elemental iron (as ferrous sulphate);
group 3 received 500 μg (0.5 mg) of folic acid;
group 4 received 60 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid;
group 5 received 60 mg of elemental iron (as ferrous sulphate) and 5000 μg (5 mg) of folic acid. Supplementation with iron was from 20th week of gestation until delivery. All women had received 50 mg of ascorbic acid daily from the first visit until the 20th week. Setting and health worker cadre: the intervention was performed by obstetricians at a public antenatal clinic in western Australia. Patients were of a low SES. |
|
| Outcomes | Hb, serum and red cell folate, serum vitamin B12 at first attendance, and at 20, 28, 35 weeks and at delivery, and 6 weeks postpartum; pregnancy complications, anaemia defined as Hb lower than 100 g/L, premature delivery, abortion, compliance; birthweight, placental weight, Apgar score at delivery (full outcome data were not reported for group 5, which received a higher dose of folic acid). | |
| Notes | More than 20% of the women were lost to follow‐up. We decided not to include outcome data for mean Hb at term, as the SDs provided in the paper represent a single SD for all groups and this assumes that distributions were similar in each treatment group. Gestational age at start of supplementation: late gestational age (supplementation started at or after 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "they were allotted according to randomised sequences of 50." |
| Allocation concealment (selection bias) | Unclear risk | Not clear, women were provided with colour‐coded packages which identified the regimens. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | It was stated that the contents of the treatment packages were not known to women or investigators until after the completion of the trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Laboratory outcomes, women with anaemia excluded post randomisation although loss appeared balanced across groups. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 146 women randomised, 89 women completed the trial and women were removed from the trial for reasons that may have related to outcomes (e.g. women developed anaemia). |
| Selective reporting (reporting bias) | Unclear risk | There was high attrition in this trial and data were not reported for all treatment groups. |
| Other bias | Unclear risk | No other bias apparent. |
Fleming 1985.
| Methods | RCT, 5 arms with individual randomisation. | |
| Participants | 200 apparently healthy primigravidae Hausa women living in Zaria, Nigeria and planning to deliver in Zaria, with less than 24 weeks of gestation, who had not taken any antimalarial treatment or iron supplements in current pregnancy. | |
| Interventions | Participants were randomly assigned to 1 of 5 groups:
group 1: received no active treatment;
group 2: received chloroquine 600 mg base once, followed by proguanil 100 mg per day;
group 3 received in addition to chloroquine and proguanil, 60 mg elemental iron daily;
group 4 received in addition to chloroquine and proguanil, 1000 μg (1 mg) of folic acid daily;
group 5: in addition to chloroquine and proguanil received 60 mg of elemental iron and 1000 μg (1 mg) of folic acid daily. Setting and health worker cadre: the intervention was performed by an obstetrician working with a Hausa‐speaking social worker in Zaria. |
|
| Outcomes | Full blood count, malarial parasites, serum and red cell folate, at first attendance, 28 week and 36 weeks gestational age, at delivery, and at 6 weeks postpartum, serum vitamin B12 at first attendance and at 36 weeks gestational age, Hb electrophoresis and fetal microscopy once, and bone marrow at delivery, clinical malaria. | |
| Notes | Relevant groups are: group 3 vs group 2 for comparison 2: daily oral supplementation with iron alone vs no treatment/placebo. group 4 vs group 5 for comparison 4: daily oral iron + folic acid supplementation vs daily oral folic acid alone (without iron) supplementation. Results were not reported separately for each randomised group and we have been unable to include data from this trial in the review. Gestational age at start of supplementation: mixed gestational age (up to 24 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: not clear. Malaria setting: yes. Described as a malaria endemic area: 28% of P falciparum in the sample and 40% of those anaemic. As of 2011: Malaria risk due predominantly to P. falciparum exists throughout the year in the whole country. Resistance to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | Low risk | Treatment allocation code; "Neither the researchers nor the patients were aware of the treatment allocated until after the completion of the study". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and researchers blinded. Placebos were provided which were packaged so that they "could not be distinguished by sight". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Women who were excluded because they developed anaemia or "defaulted"; were replaced. Further loss to follow‐up occurred during the trial; it was not clear how many women were followed up at each data collection point. 89 out of 200 women randomised delivered in the hospital and no complete, clear data could be extracted for the outcomes of interest in this review. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Foulkes 1982.
| Methods | Quasi‐randomised trial, 2 arms with individual randomisation. | |
| Participants | 568 apparently healthy pregnant women with less than 20 weeks of pregnancy and no prior iron supplementation. | |
| Interventions | Participants were allocated alternatively to receive 100 mg of elemental iron and 350 μg (0.35 mg) folic acid daily or no treatment. | |
| Outcomes | Ferritin and Hb concentrations were measured at baseline and at 28 and 36 weeks of gestation and 2 days postpartum. MCV and MCH were measured at 2 days postpartum. Number of women developing anaemia in the 2nd and 3rd trimester was reported (Hb < 105 g/L). Setting and health worker cadre: the intervention was performed by obstetricians at Southmead Hospital in Bristol, United Kingdom. |
|
| Notes | Only means and median are presented for continuous outcomes. No SDs are reported and for ferritin concentrations no ln‐transformed data are presented. Limited data were extractable from the paper and subsequent communication with the author. The paper reported the number of women developing Hb < 105 g/L from the start of supplementation to delivery. No data were extracted from this trial. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: not clear. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternation. |
| Allocation concealment (selection bias) | High risk | Alternate allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. No placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Women who did not comply or who became anaemic were treated. Outcomes reported unlikely to be affected by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 537 women randomised, then 67 excluded post‐randomisation for reasons that may have related to outcomes (non‐compliance). Subsequent loss to follow‐up was not clear as denominators were not reported in the text or figures. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Freire 1989.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 412 non‐black pregnant women with 26 ± 2 weeks of gestation, who had not received iron supplements in the previous 6 months, from low SES using the prenatal unit of public obstetric hospital in Quito, Ecuador. | |
| Interventions | Participants were randomly assigned to receive 2 tablets containing 78 mg of elemental iron (as ferrous sulphate) daily or placebo during a period of 2 months. Setting and health worker cadre: the intervention was performed by physicians in the Prenatal Unit of Quito's public obstetric hospital in Quito, Ecuador. |
|
| Outcomes | Hb, PCV, red cell indices, serum ferritin, total iron binding capacity, serum folate, serum vitamin B12 at baseline and after 2 months. Prevalence of iron deficiency was estimated by response to therapy. | |
| Notes | Apart from mean Hb levels at term no other prespecified outcomes from this review are presented in the paper. No data can be extracted from this trial. Gestational age at start of supplementation: late gestational age (supplementation started after 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: high daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. The study was conducted in Quito where there is no risk of malaria. As of 2011: Malaria risk – P. vivax (87%), P. falciparum (13%) – exists throughout the year below 1500 m, with moderate transmission risk in coastal provinces. There is no risk in Guayaquil, Quito and other cities of the inter‐Andean region. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described ("randomly assigned"). |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as "double‐blind", placebo tablets provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 412 women were recruited and 240 followed up. Loss to follow‐up was 41.7% and there were missing data for some outcomes. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Groner 1986.
| Methods | RCT, 2 arms, individual randomisation. | |
| Participants | 40 pregnant women attending antenatal care at the Adolescent Pregnancy Clinic and Obstetrics Clinics at the John Hopkins and Sinai Hospital in Baltimore, Maryland, USA at or before 16 weeks of pregnancy with HCT equal or above 31%. 2 women objected to the randomisation and 13 dropped out of the study. Both groups received multiple micronutrients. Supplementation lasted a month. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups:
group 1 (n = 16) received 60 mg of elemental iron (as ferrous fumarate) and prenatal vitamins daily; group 2 (n = 9) received only the prenatal vitamins with no iron. Setting and health worker cadre: the intervention was performed by physicians at the Adolescent Pregnancy Clinic and Obstetrics Clinic of Johns Hopkins and Sinai Hospitals in Baltimore, Maryland, United States of America. |
|
| Outcomes | Psychometric tests (arithmetic, total digit span, digit symbol, vocabulary and others) were performed and haematologic status was measured at baseline and after a month. | |
| Notes | Haematologic outcomes cannot be extracted from the paper. None of the other outcomes were sought. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous fumarate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Each subject was handed an unlabeled bottle of capsules... The test administrator was also unaware of the content of the capsules distributed." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was stated that the test administrator was not aware of the treatment group. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 15 of the 40 women randomised were not followed up. Group size at follow‐up was not balanced (16 vs 9). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Han 2011.
| Methods | Quasi‐randomised control trial with 3 arms and individual allocation to groups by order of enrolment. | |
| Participants | 153 anaemic pregnant women 12 to 24 weeks' gestation, age range 20‐30 years, with 80 ≤ Hb <110 g/L, no dietary supplements use during the previous 2 months and no abnormal pregnancy response recruited from the communities of Shen county, Shandong province, China. | |
| Interventions | Participants were allocated to 1 of the 3 groups in the order of enrolment:
group 1 (n = 51) was the placebo control;
group 2 (n = 51) received supplement daily containing 60 mg elemental iron (as ferrous sulphate);
group 3 (n = 51) received a supplement daily containing 60 mg elemental iron (as NaFeEDTA). The capsules were labelled in red, yellow and blue colour and manufactured by Hurun’s company (a Chinese food‐additive company, Beijing). The intervention lasted 2 months. Women were visited at home once each week by the village nurse to replenish supplements and to monitor compliance by counting and recording the number of supplements that were taken. Setting and health worker cadre: the intervention was performed by village nurses in house visits to the participants in the communities of Shen county, Shandong province, China. |
|
| Outcomes | Hb concentration; plasma iron; soluble transferrin receptor; total iron‐binding capacity; MDA; SOD; glutathione peroxidase. | |
| Notes | The participants in the placebo group in this study were given iron supplementation with NaFeEDTA or foods rich in iron, such as the hemachrome‐iron from animal foodstuff, such as meat, fish and sea foods, immediately after the trial. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: anaemic status. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate and iron EDTA. Malaria setting: yes. As of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Individual allocation to groups by order of enrolment. |
| Allocation concealment (selection bias) | High risk | The capsules were labelled in red, yellow and blue colour and manufactured by Hurun’s company (a Chinese food‐additive company, Beijing). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Trial participants and the research team were unaware of the treatment assignment. The trial was unblinded after analysis of the primary outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trial participants and the research team were unaware of the treatment assignment. The trial was unblinded after analysis of the primary outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data were available for 147 women, 96.1% of the original number of 153 pregnant women. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The groups did not differ in age, gestational stage, gravidity, haematological status, levels of MDA, SOD and GSH‐Px at baseline. |
Hankin 1963.
| Methods | Quasi‐randomised trial, 2 arms with individual randomisation. | |
| Participants | 174 primigravidae or secundigravidae at their first visit at the antenatal Clinic of Queen Elizabeth Hospital in Woodville, Australia with ability to write and speak English. | |
| Interventions | Participants were divided into a supplemented group receiving a daily dose of 100 mg of elemental iron (as ferrous gluconate) or a control group that was un supplemented.
Supplementation started during 2nd trimester and ending time is unclear. Setting and health worker cadre: the intervention was performed by physicians at the Queen Elisabeth Hospital in Woodville, South Australia. |
|
| Outcomes | Maternal: Hb and HCT at 20‐30 weeks, 30‐40 weeks, at 5 days, at 6 weeks and at 3 months postpartum. Infant: Hb from umbilical cord, at 6 week, at 3 months and at 6 months of age (not reported). | |
| Notes | Unsupervised.
Compliance not reported. Gestational age at start of supplementation: mixed/unspecified gestational age. Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised, alternate by day of the week. |
| Allocation concealment (selection bias) | High risk | Alternate allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding, no placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Women in the control group who had low Hb were analysed with the treated group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5% excluded. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Harvey 2007.
| Methods | RCT, 2 arms, individual randomisation. | |
| Participants | 13 apparently healthy non‐anaemic non‐smokers pregnant women aged 18‐40 years and < 14 weeks of gestation with singleton pregnancy recruited through local medical practitioners and the Maternity Department of the Norfolk and Norwich University Hospital, England, United Kingdom. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 100 mg elemental iron (as ferrous gluconate) daily after food and group 2 received a placebo. Supplementation started at 16th week of gestation until delivery. Setting and health worker cadre: The intervention was performed by midwives and obstetricians at Maternity Department of the Norfolk and Norwich University Hospital in Norwich, United Kingdom. |
|
| Outcomes | Maternal: Hb, serum ferritin, transferrin receptor, plasma zinc, exchangeable zinc pool, zinc excretion and zinc absorption at 16, 24 and 34 weeks of gestation. Infant: birthweight (not reported). | |
| Notes | Unsupervised.
Compliance not reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coded bottles were provided by manufacturer. |
| Allocation concealment (selection bias) | Low risk | Supplied in coded opaque bottles. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as a single‐blind, placebo‐controlled trial. Placebo and active tablets were described as identical. Women blinded not clear that staff were. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators not blinded. Laboratory outcomes likely to be low risk of bias from blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Hoa 2005 (C).
| Methods | Randomisation may have been by cluster (communes) rather than individual women. Block randomised trial with 4 arms. | |
| Participants | 202 apparently healthy pregnant women 20‐32 years of age attending health clinics from 12 communes in Dong HungDistrict, Thai Binh Province, Vietnam with 14‐18 weeks of gestation who agreed to participate in the study were selected to participate. | |
| Interventions | Participants were assigned through block randomly assigned to 1 of 4 interventions: group 1 (n = 44) received 400 mL fortified milk with iron (ferrous fumarate), 17.5 mg vitamin C and 200 μg (0.2 mg) folic acid daily; group 2 (n = 41) received 400 mL of fortified milk containing 17.5 mg vitamin C and 200 μg (0.2 mg) folic acid but no iron daily; group 3 (n = 40) received 1 tablet containing 60 mg of elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) folic acid daily; group 4 (n = 43) received 1 placebo tablet daily. Setting and health worker cadre: the intervention was performed by community health workers working from a commune health centre operated by the National Ministry of Health in the rural delta area of the Red River in northern Vietnam (Dong Hung District, Thai Binh Province). |
|
| Outcomes | Hb at baseline, 5, 10, 16 weeks after start of the study, total iron‐binding capacity, serum transferrin saturation, anaemia, iron deficiency, weight, presence of hookworms. | |
| Notes | For purposes of this review groups 3 vs group 4 comparing iron and folic acid supplements are relevant. However, no data on outcomes of interest could be extracted from the published report. It was reported in the paper that the "decrease in haemoglobin concentration in the supplemented groups was significantly less"; and that, "the transferrin saturation level increased slightly in the supplement group". Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: unspecified/mixed anaemia status. Daily iron dose: higher dose (60 mg of elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due predominantly to P. falciparum exists in the whole country, excluding urban centres, the Red River delta, the Mekong delta, and the coastal plain areas of central Viet Nam. High‐risk areas are the highland areas below 1500 m south of 18˚N, notably in the 4 central highlands provinces Dak Lak, Dak Nong, Gia Lai and Kon Tum, Binh Phuoc province, and the western parts of the coastal provinces Khanh Hoa, Ninh Thuan, Quang Nam and Quang Tri. Resistance to chloroquine, sulphadoxine–pyrimethamine and mefloquine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It was not clear whether individual women or communes were randomised "For practical reasons it was possible to implement only 1 type of intervention per commune (block randomly adjusted)". It was not clear whether staff were aware of allocation before randomisation. |
| Allocation concealment (selection bias) | Unclear risk | Little information about study methods was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Partial blinding. Placebo preparations were provided. Described as single‐blind. Staff aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Likely to be low risk for laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up not described. Not clear if any clusters were lost. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | Groups appeared comparable at baseline. Data from this study were not included in the review. |
Holly 1955.
| Methods | RCT, 3 arms with individual randomisation. | |
| Participants | 207 pregnant women with less than 26 weeks of gestation and Hb > 100 g/L attending antenatal care clinic in Nebraska, USA. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 received 1 g of an iron salt daily; group 2 received 0.8‐1.2 g of ferrous sulphate and 60‐90 mg of cobalt chloride daily; group 3 received no treatment. Supplementation started at various times before 26th week of gestation for each of the participants until delivery. Setting and health worker cadre: the intervention was performed by obstetricians at the Department of Obstetrics and Gynecology of the Univeristy of Nebraska, College of Medicine in Omaha, Nebraska, United States of America. |
|
| Outcomes | Maternal: Hb, HCT, serum iron, erythrocyte protoporphyrin at 3‐6 months and pre‐delivery. | |
| Notes | Unsupervised.
3 iron compounds (n = 94) were used: ferrous gluconate (n = 40), ferrous sulphate (n = 32) and Mol‐Iron® (n = 22). The iron‐treated groups with different iron salts were merged together by the author as iron‐treated group since the results were comparable. The iron and cobalt treatment group is not included in this review.
Compliance not reported. Gestational age at start of supplementation: mixed gestational age at the start of supplementation (before 26 weeks). Anaemic status at start of supplementation: mixed anaemia status (Hb > 100 g/L). Daily iron dose: higher daily dose (60 mg or more elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: mixed (groups merged in analysis). Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither participants nor provider blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Laboratory outcomes reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up not described. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Hood 1960.
| Methods | RCT, 3 arms, individual randomisation. | |
| Participants | 75 consecutive apparently healthy pregnant women with 32‐34 weeks of gestation attending the maternity clinic at St Anthony's Hospital, Oklahoma City, Oklahoma, USA. | |
| Interventions | Participants were randomly divided in 3 groups: group 1 served as control and received no treatment; group 2 received 220 mg elemental iron (as ferrous sulphate) daily; and group 3 received 55 mg elemental iron (as sustained release ferrous sulphate) daily.
Supplementation started at 32‐34 weeks of gestation until delivery. Setting and health worker cadre: the intervention was performed by obstetricians at the Department of Obstetrics and Gynecology of St. Anthony's Hospital in Oklahoma City, Oklahoma, United States of America. |
|
| Outcomes | Maternal: Hb, HCT, incidence and severity of side effects on a weekly basis until delivery. | |
| Notes | Unsupervised.
For any iron vs no treatment comparison groups were merged.
Compliance not reported. Gestational age at start of supplementation: late gestational age (supplementation started after 20 weeks' gestation). Anaemic status at start of supplementation: unspecified/mixed anaemia. Daily iron dose: medium dose (55 mg elemental iron) and higher dose (220 mg elemental iron). Iron release formulation: sustained release preparation and normal release preparation/not specified. Iron compound: ferrous sulphate and sustained release ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither participant nor provider blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessor unclear. Low risk for laboratory outcomes but uncertain risk of bias for reported side effects. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Kerr 1958.
| Methods | RCT, 4 arms with individual randomisation. | |
| Participants | 430 apparently healthy women with 24‐25 weeks of singleton pregnancy and Hb equal or above 104 g/L attending antenatal clinic at Simpson Memorial Maternity Pavillion, Edinburgh, United Kingdom. | |
| Interventions | Participants were randomly allocated to 1 of 4 groups: group 1 received 35 mg of elemental iron (as ferrous sulphate) 3 times a day; group 2 received 35 mg of elemental iron (as ferrous gluconate) 3 times a day; group 3 received 35 mg of elemental iron (as ferrous gluconate) with 25 mg of ascorbic acid, 3 times a day; group 4 received placebo. Supplementation started at 24‐25th week of gestation until term. Setting and health worker cadre: the intervention was performed by physicians at the Simpson Memorial Maternity Pavilion in Edinburgh, United Kingdom. |
|
| Outcomes | Maternal: Hb, red cell count, HCT at baseline and at 37th week. | |
| Notes | Unsupervised.
Groups 1 and 2 were merged for analysis. Group 3 was not used in this review.
Compliance not measured. Gestational age at start of supplementation: late gestational age (supplementation started after 20 weeks' gestation). Anaemic status at start of supplementation: unspecified/mixed anaemia status (no severe anaemia, all had Hb equal or above 104 g/L). Daily iron dose: higher iron dose (all treatment groups received more than 60 mg of elemental iron daily (105 mg)). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By cards shuffle. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Partial blinding. Placebo and all supplements described as identical. Women were blinded, but medical staff were aware of which was the control group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Low risk for laboratory outcomes. Possible risk of bias for dietary survey and reporting of side effects. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 23% of participants were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Korkmaz 2014.
| Methods | Randomised double‐blind placebo‐controlled trial with 3 arms. | |
| Participants | 108 pregnant women with singleton pregnancies without a risk factor for poor pregnancy outcome, systemic disorder, any medication and any previous surgery attending outpatient clinic of Dr Sami Ulus Maternity and Women’s Health Training and Research Hospital, Ankara, Turkey.between November 2010 and January 2012. Women with iron‐deficiency anaemia (determined according to Hb lower than 110 g/L), pre‐existing diabetes, prior gestational diabetes, a history of stillbirth, multiple gestation, active chronic systemic disease and the smokers were excluded. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 (n = 36) received 400 ug (0.4 mg) folic acid daily; group 2 (n = 36) received 60 mg elemental iron daily; group 3 (n = 36) received placebo. Supplementation started at 6th week of gestation until term. | |
| Outcomes | Antepartum, intrapartum and neonatal information were abstracted from the antenatal medical records and from inpatient hospital records. Gestational age at delivery, Apgar (1st min), Apgar (5th min), birthweight (g), albumin (mg/dL), serum GGT (IU/L), weight gain (kg), post‐term deliveries (beyond the 42nd week of gestation), the preterm premature rupture of membranes (spontaneous membrane rupture before 37th week of gestation). |
|
| Notes | Gestational age at start of supplementation: early, if supplementation started before 20 weeks' gestation. Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: 60 mg elemental iron. Iron release formulation: normal release preparation/unspecified. Iron compound: other/not specified. Malaria setting: malaria‐free. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation using a pre‐generated randomisation scheme created by the website randomization.com. |
| Allocation concealment (selection bias) | Low risk | All study medications were prepared by a clinician unaware of the patient’s allocated study group in identical drug packages. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to the groups.Packages were given by a blinded attending physician. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded to the groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There are no losses to follow‐up reported in any of the groups. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | No other bias apparent. |
Kuizon 1979.
| Methods | RCT, 4 groups (with supplementation depending on Hb levels at baseline) individual randomisation. | |
| Participants | 385 pregnant women attending antenatal care at government health centres in Greater Manila area, Philippines. Mean gestation at recruitment was approximately 21 weeks until delivery. Women were assessed at baseline and women with anaemia ( Hb < 120 g/L in 1st and < 110 g/L in 2nd trimester) received a higher dose of supplements. | |
| Interventions | Participants were randomly assigned to 1 of 4 groups: group 1 received placebo (anaemic and non‐anaemic women received 1 placebo capsule); group 2 received 65 mg of elemental iron ( as 325 mg ferrous sulphate) women received either 1 or 3 oral tablets daily; group 3 received 100 mg ascorbic acid (either 1 or 3 oral tablets daily); group 4 received 65 mg elemental oral iron (as ferrous sulphate) plus 100 mg ascorbic acid ‐ women received either 1 or 3 tablets. Supplementation started from recruitment in 1st and second trimester until delivery. Setting and health worker cadre: the intervention was performed by health centre staff at government health centres and maternity clinics in the greater Manila area, Manila, Phillipines. |
|
| Outcomes | Mean Hb concentration at 32 and 39 weeks (for women anaemic and not anaemic at baseline), HCT at 32 and 39 weeks, serum iron at 32 and 39 weeks, transferring saturation levels at 32 and 39 weeks. | |
| Notes | Attrition in this study was very high (half of the women were lost to follow‐up by 32 weeks' gestation and more than 75% by term). For this reason we have not included data from this study in our data and analyses tables. Gestational age at start of supplementation: mixed gestational age at the start of supplementation (mean gestation at start of supplementation was 21 weeks). Anaemic status at start of supplementation: mixed anaemia status (dose depended on Hb level at baseline). Daily iron dose: higher daily dose (greater than 60 mg of elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk exists throughout the year in areas below 600 m, except in the 22 provinces of Aklan, Albay, Benguet, Biliran, Bohol, Camiguin, Capiz, Catanduanes, Cavite, Cebu, Guimaras, Iloilo, Northern Leyte, Southern Leyte, Marinduque, Masbate, Eastern Samar, Northern Samar, Western Samar, Siquijor, Sorsogon, Surigao Del Norte and metropolitan Manila. No risk is considered to exist in urban areas or in the plains. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. Human P. knowlesi infection reported in the province of Palawan. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | "randomly assigned." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo was provided but women received different doses (and number of tablets).It was not clear if staff were aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was not clear if outcome assessment was blind. Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Very high attrition. 679 women recruited. In non‐anaemic women, 189/385 followed up (49%). In anaemic group 146/294 (50%) followed up at 32 weeks by 39 weeks only 94/385 non‐anaemic women followed up (24%) and 60 in anaemic group (20%). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | High risk | The reasons for the very high levels of attrition were not explained (except that some women delivered before term). The very high loss to follow‐up means that results are very difficult to interpret. |
Lee 2005.
| Methods | RCT, 5 arms with individual randomisation. | |
| Participants | 154 apparently healthy pregnant women seeking prenatal care in Gwangju, South Korea during first trimester of pregnancy who did not receive other supplements or medications throughout pregnancy and who were willing to participate. | |
| Interventions | Participants were randomly allocated to 1 of 5 groups: group 1 received 30 mg elemental iron (as ferrous sulphate) and 175 μg (0.17 mg) folic acid daily from first trimester until delivery; group 2 received 60 mg of elemental iron (as ferrous sulphate) with 350 μg (0.35 mg) of folic acid from first trimester until delivery; group 3 received 30 mg elemental iron (as ferrous sulphate) and 175 μg (0.17 mg) of folic acid from 20th week of gestation until delivery; group 4 received 60 mg elemental iron (as ferrous sulphate) and 350 μg (0.35 mg) of folic acid from 20th week of gestation until delivery; control group no supplement. Setting and health worker cadre: the intervention was performed by physicians at a hospital and health centre in Gwangju, Korea. |
|
| Outcomes | Maternal: Hb, HCT, serum ferritin, serum soluble transferrin receptor concentrations at baseline and during first, second, third trimester of pregnancy and at delivery. | |
| Notes | Unsupervised.
Compliance not reported. included in comparison 3: daily iron + folic acid vs no treatment/placebo and only different groups included in the subgroup analysis by gestational age at start of supplementation (early (group 1 + group 2); late (group 3 + group 4); and by iron dose: low (group 1 + group 3); higher (group 2 + group 4). Gestational age at start of supplementation: mixed gestational ages (different arms started supplementation before or after 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: mixed (with different arms receiving lower (30 mg) and higher (60 mg) of elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: limited malaria risk due exclusively to P. vivax exists mainly in the northern areas of Gangwon‐do and Gyeonggi‐do Provinces and Incheon City (towards the Demilitarized Zone or DMZ). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Described as "truly random" but the method was not stated. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding (and some women requested a change in assigned group). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Liu 2000.
| Methods | RCT with 3‐arms, and individual randomisation. | |
| Participants | 300 pregnant women with 24‐28 weeks of gestation with no had organic disease and Hb level higher than 100 g/L who received antenatal examinations in Second Affiliated Hospital, Zhujiang Hospital, the First Military Medical University, Guangzhou, China from January 1998 to January 1999. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 received 1 tablet daily containing 100 mg elemental iron (as ferrous sulphate sustained‐release) with 500 mg vitamin C and B‐complex vitamins (amounts not reported) administered orally for 4 consecutive weeks; group 2 received conventional iron supplement (as 300 mg ferrous sulphate) administered 3 times a day to meals for 4 consecutive weeks; group 3 did not receive any iron supplementation. Setting and health worker cadre: intervention and outcome assessment were conducted by physicians from the Obstetric & Gynecology Department, Zhujiang Hospital, the First Military Medical University, Guangzhou, China. |
|
| Outcomes | RBC, Hb and serum ferritin at baseline at after 4 weeks of intervention and before delivery. Anaemia, iron deficiency, fatigue, dizziness, shortness of breath, and pale mucous membranes and skin, tinnitus, presence of stomatitis or glossitis, premature birth, average Apgar score, congenital malformations. Side effects reported: nausea and loss of appetite, severe gastrointestinal reactions including vomiting, abdominal pain, and diarrhoea, metallic taste in the mouth, black staining of their teeth. Blood tests and serum ferritin measurement were performed for the gravidas after 4 and 8 weeks of supplementation and before delivery. The Apgar scoring and physical examinations were performed for the newborns after delivery. | |
| Notes | Gestational age at start of supplementation: late gestational age (supplementation started at 20 weeks' gestation or later). Only groups included in the comparisons are group 2 and group 3 who did not receive supplements. Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: high daily dose (60 mg or more mg iron daily). Iron release formulation: normal and slow release preparation for group 1 (not included in the comparisons in this review). Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported as randomised but method unclear. |
| Allocation concealment (selection bias) | Unclear risk | There is insufficient information to permit judgement. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No blinding mentioned but this was a placebo‐controlled trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data reported as complete for all the participants reported as randomised. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | There were no significant differences in terms of age, gestational age, body weight, and H level among the 3 groups (all P > 0.05). |
Liu 2012.
| Methods | 3‐arm double‐blind randomised controlled trial, individually‐randomised. Randomisation was stratified by county, and random block sizes of 3, 6, and 9 were used to ensure geographical balance with an approximately equal distribution of treatments within and across study counties. | |
| Participants | 18775 nulliparous pregnant women 20 years of age or older, with mild or no anaemia (Hb level greater than 100 g/L),with no more than 20 weeks of gestation attending prenatal care in 5 rural counties in Hebei Province, northern China, where basic health services were provided through 3‐tier (county, township, and village) healthcare networks of northern China, from May 2006 through April 2009. Additionally, eligible women had not consumed micronutrient supplements other than folic acid in the prior 6 months. Women were followed monthly from early pregnancy through delivery and at 4–8 weeks postpartum. Their infants were followed monthly from birth until 1 year of age. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 (n = 6261) received 400 µg (0.4 mg) folic acid daily (control); group 2 (n = 6252) received 30 mg elemental iron (as ferrous fumarate) plus 400 µg (0.4 mg) folic acid daily; group 3 (n = 6262) received 30 mg elemental iron (as ferrous fumarate) with 400 µg (0.4 mg) folic acid daily and 800 μg vitamin A, 10 mg vitamin E, 5 μg vitamin D, 70 mg vitamin C, 1.4 mg thiamine, 1.4 mg riboflavin, 1.9 mg vitamin B6, 2.6 μg vitamin B12, 18 mg niacin, 15 mg zinc, 2 mg copper, 150 μg iodine, and 65 μg selenium. The supplements were provided before 20 weeks of gestation to delivery. Each woman received 2 bottles of supplements at enrolment and 1 at monthly follow‐up visits. Each bottle contained 31 supplements, including the type of the supplements per group according to lot number. Only groups 1 and 2 are considered in this review (folic acid vs iron + folic acid). Health worker cadre: trained county or township physicians completed relevant measurements and collected data based on a perinatal and child healthcare surveillance system. At enrolment, the physician assigned women the next lot number on the randomisation schedule and provdied the supplements. |
|
| Outcomes | Perinatal mortality, neonatal deaths, infant deaths, maternal Hb concentration and anaemia at 24 to 28 weeks of gestation, birthweight, birth length, duration of gestation, preterm delivery, compliance. | |
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A statistician external to the study randomly assigned ten 4‐digit lot numbers to each of the 3 supplement types (masked to the formulation and allocation) and generated the assignment list for each county proportional to the expected number of participants; within each county and block, lot numbers were randomly assigned using RANUNI in SAS statistics software (SAS Institute Inc)." |
| Allocation concealment (selection bias) | Low risk | Ten 4‐digit lot numbers to each of the 3 supplement types (masked to the formulation and allocation). At enrolment, the physician assigned women the next lot number on the randomisation schedule. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Aside from a pharmaceutical engineer who ensured allocation of lot numbers to the correct supplement formulations, all others (ie, participants, local physicians, study personnel, and investigators) were masked to the identity of the supplements. Treatment codes were broken after completion of the study and main analyses." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Aside from a pharmaceutical engineer who ensured allocation of lot numbers to the correct supplement formulations, all others (ie, participants, local physicians, study personnel, and investigators) were masked to the identity of the supplements. Treatment codes were broken after completion of the study and main analyses." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were 299/6261 (4.77%) losses to follow‐up in the group 1; 280/6252 (4.47%) in group 2: and 299/6262 (4.77%) in the group 3 for various reasons: permanently moved, induced abortions, spontaneous abortions, dropped out or maternal death. The attrition was balanced among groups. |
| Selective reporting (reporting bias) | Low risk | There appears to be no selective reporting. Trial Registration: clinicaltrials.gov Identifier: NCT00133744. |
| Other bias | Low risk | No other bias apparent. |
Ma 2010.
| Methods | RCT with 4 arms including a placebo and individual randomisation. | |
| Participants | 164 anaemic pregnant women (80 g/L, Hb, 110 g/L), 12–24 weeks' gestation and 20–35 years old recruited between March 2004 and September 2006 from the community hospitals of Shen County in the central area of China. | |
| Interventions | Participants were randomly allocated to 1 of 4 groups for this 2‐month intervention in the order of recruitment: group 1 (n = 41) received placebo; group 2 (n = 41) received 60 mg elemental iron (as ferrous sulphate); group 3 (n = 41) received 60 mg elemental iron (as ferrous sulphate) and 400 μg (0.4 mg) folic acid daily; group 4 (n = 41) received 60 mg elemental iron (as ferrous sulphate), and 400 μg (0.4 mg) folic acid, 2 mg retinol and 1 mg riboflavin daily. Setting and health worker cadre: In each community, a local female community health worker called ‘village nurse’ was responsible for the recruitment and distribution of the supplements. Women were recruited from the community hospitals and then home‐visited once a week by the village nurse to replenish supplements and to monitor compliance by counting and recording the number of supplements that were taken. The nurse also provided counselling about the possible side effects. |
|
| Outcomes | Hb, plasma iron, ferritin, folic acid, retinol riboflavin after the 2 months intervention. Other outcomes included membrane fluidity, oxidative stress markers such as GSH‐Px, SOD, and MDA. | |
| Notes | This study is included but does not provide any data that can be useful for purposes of this review. Gestational age at start of supplementation: unspecified or mixed gestational ages at the start of supplementation. Anaemic status at start of supplementation: anaemic. Daily iron dose: high daily dose (60 mg or more mg iron daily). Iron release formulation: normal. Iron compound: ferrous sulphate. Malaria setting: yes. Malaria as of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised as participants were randomly allocated to 1 of 4 groups for this 2‐month intervention in the order of recruitment: group. |
| Allocation concealment (selection bias) | Unclear risk | Tretaments were colour coded. It was stated that the code was not revealed until after the analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This was a placebo‐controlled trial. It was stated that women and staff were blind to treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 164 women were randomised and 145 (88%) were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | No other bias apparent. |
Makrides 2003.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 430 non‐anaemic pregnant women attending antenatal clinics at Women's and Children's Hospital in Adelaide, Australia with singleton or twin pregnancies and informed consent. Exclusion criteria: diagnosis of thalassaemia, history of drug or alcohol abuse and history of vitamin and mineral preparations containing iron prior to enrolment in study. | |
| Interventions | Participants were randomly assigned to receive 1 tablet containing 20 mg of elemental iron daily between meals from week 20 until delivery or a placebo tablet. Setting and health worker cadre: the intervention was performed by Pediatricians and Obstetricians in a maternity hospital in Adelaide, Australia. |
|
| Outcomes | Maternal: Hb concentration at 28 weeks, at delivery, and at 6 months postpartum; ferritin concentration at delivery and at 6 months postpartum; maternal gastrointestinal side effects at 24 and 36 weeks of gestation; serum zinc at delivery and at 6 months postpartum; maternal well being at 36 week of gestation, at 6 weeks and at 6 months postpartum; pregnancy outcomes: type of birth, blood loss at delivery, gestational age. At 4 years postpartum: general health of mothers using the SF‐36, a self‐administered questionnaire that assesses 8 concepts of health. Infant: birthweight, birth length, birth head circumference, Apgar scores, and level of nursery care. Follow‐up at 4 years: intelligence quotient (IQ) using Stanford‐Binet Intelligence Scale, child behaviour using Strength and Difficulties Questionnaire parent‐report form. | |
| Notes | Unsupervised but monthly phone calls to encourage compliance.
If anaemia was detected in the routine 28‐week blood sample or if the clinician considered her Hb too low, the woman was advised to purchase and take a high‐dose iron supplement (containing > 80 mg elemental iron per tablet) until the end of pregnancy.
Compliance was 86% and 85% in the iron and placebo groups respectively. Gestational age at start of supplementation: late gestational age (supplementation started at 20 weeks' gestation or later). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: lower daily dose (less than 30 mg iron daily) (20 mg). Iron release formulation: normal release preparation. Iron compound: not clear. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence with balanced blocks and stratified for parity. |
| Allocation concealment (selection bias) | Low risk | Opaque bottles marked with sequential numerical code prepared by the Pharmacy Department of Women's & Children's Hospital. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | This was described as a double‐blind trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. Side effects likely to be recorded by blinded staff. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Meier 2003.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 144 non‐iron deficient adolescents 15‐18 years old in their first pregnancy and adult women 19 or older in their first or greater pregnancy attending prenatal care at Marshfield Clinic, Wisconsin, USA. | |
| Interventions | Participants were randomly assigned to receive once daily 60 mg of elemental iron (as ferrous sulphate) or a placebo. All women received 1000 μg (1 mg) of folic acid daily. | |
| Outcomes | Maternal: prevalence of iron‐deficiency anaemia, compliance to treatment, side effects, vomiting, nausea, constipation, diarrhoea, caesarean section, serum ferritin and Hb concentrations at 24‐28 weeks' gestation and at 36‐40 weeks' gestation.
infant: perinatal morbidity and mortality, birthweight, birth length, Apgar scores at 1 and 5 minutes, admission to neonatal unit, prevalence of birthweight. Setting and health worker cadre: the intervention was performed at multicentre clinic in central Wisconsin. |
|
| Notes | Unsupervised.
All adolescents and adult pregnant women who developed iron‐deficiency anaemia at 24‐28 weeks' gestation were offered 60 mg elemental iron 3 times a day.
Compliance was assessed through pill counts and ranged from 32% to 124% (median 95.5% in iron supplemented group and 87.4% in placebo group. Gestational age at start of supplementation: unspecified/mixed gestational age. Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified by age group. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo‐controlled, double‐blind trial. The placebo was reported to be identical in appearance to the active treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Menendez 1994 (C).
| Methods | Cluster‐randomised trial, 2‐arm trial. | |
| Participants | 550 multi gravidae pregnant women with less than 34 weeks of gestation attending antenatal care clinics in 18 villages near the town of Farafenni, in North Bank Division, Gambia where malaria is endemic with high transmission during 4‐5 months a year. | |
| Interventions | Participants were allocated randomly by compound of residence to receive 60 mg of elemental iron (as ferrous sulphate) or placebo. All pregnant women received a weekly tablet of 5000 μg (5 mg) of folic acid but no antimalarial chemoprophylaxis.
Supplementation started at 23‐24 weeks until delivery. Setting and health worker cadre: the intervention was performed by traditional birth attendants in villages in the North Bank Division of The Gambia within the national village‐based primary healthcare program. |
|
| Outcomes | Maternal: Hb concentrations at baseline, 4‐6 weeks before delivery and 1 week postpartum; plasma iron, total iron binding capacity, transferrin saturation, deposition of malaria pigment in placenta. Infant: birthweight within 7 days of delivery. | |
| Notes | Unsupervised.
Malaria prophylaxis is provided to primigravidae in The Gambia. 30 women with PCV less than 25% after enrolment (17 in iron group and 13 in placebo) were treated and withdrawn from study and analysis. Additionally, 29 women (7 in iron and 22 in placebo group) had PCV below 25% at the second visit and were also withdrawn from study. No differences in the prevalence and severity of peripheral blood or placental malaria infection. No increase in the susceptibility to malaria infection in the 2 groups.
Compliance: estimated tablet consumption was 81.1 and 81.7 tablets in the iron and placebo groups respectively. Gestational age at start of supplementation: late gestational age (more than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: unspecified/mixed anaemia status. Daily iron dose: higher daily dose (60 mg daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: high malaria risk area. As of 2011: Malaria risk due predominantly to P. falciparum exists throughout the year in the whole country. Resistance to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but method unclear. |
| Allocation concealment (selection bias) | High risk | Not described. Active treatment and placebo were different colours. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Partial blinding. This was a placebo‐controlled trial but the active and placebo supplements were different colours. Women were likely to be blind but staff may have been aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Laboratory outcomes unlikely to have been affected by partial blinding. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | This was a cluster‐randomised trial, there was no clear baseline imbalance. Data in the original analysis were not adjusted for cluster deign effect but have been adjusted in this review. |
Milman 1991.
| Methods | RCT 2 arms with individual randomisation. | |
| Participants | 248 healthy Caucasian Danish women attending birth clinic in Copenhagen, Denmark within 9‐18 weeks of gestation and normal pregnancy. Exclusion criteria: complicated delivery, excessive smoking (> 9 cigarettes/day). | |
| Interventions | Participants were randomly assigned to receive 66 mg of elemental iron (as ferrous fumarate) daily (n = 121) or placebo (n = 127) until delivery.
Supplementation started at 8‐9th week until delivery. Setting and health worker cadre: the intervention was performed by obstetricians at the Birth Clinic of the Department of Obstetrics, Herning Hospital in Copenhagen, Denmark. |
|
| Outcomes | Maternal: Hb, HCT, erythrocyte indices, iron status, serum ferritin, serum transferrin saturation, serum erythropoietin at baseline and every 4th week until delivery, and 1‐8 weeks after delivery in subsample; pregnancy complications. Infant: birthweight, serum ferritin, transferrin saturation and serum erythropoietin in umbilical cord. | |
| Notes | Unsupervised.
Of the 248 women, 20 placebo and 21 iron treated were excluded by the authors in some of the analysis for the following reasons: withdrawn consent, 10; uterine bleeding episodes, 5; placental insufficiency, placenta praevia and abruptio placenta, 7; pre‐eclampsia, 3; partus prematurus, 5; excessive smoking, 3. Sample size has been adjusted for ITT.
Compliance: number of tablets consumed was 159 +/‐ 38 and 93 +/‐ 43 tablets in the iron treated and placebo groups respectively. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: mixed anaemia status at baseline. Daily iron dose: higher daily dose (60 mg or more of elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous fumarate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as double‐blind, placebo‐controlled trial. Not clear whether blinding was effective, there was a major disparity in the number of tablets consumed by women in the active treatment and placebo groups (means 159 vs 93). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | For laboratory outcomes the impact of blinding on outcomes was likely to be small. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Ouladsahebmadarek 2011.
| Methods | RCT with 2‐arms and individual randomisation. | |
| Participants | 960 healthy women at first trimester of pregnancy with Hb > 120 g/L and blood pressure < 140/90 mmHg from Alzahra University dependent hospital in Vanak,Tehran, Iran. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received daily 1 multiple micronutrient + 30 mg elemental iron from week 13 of gestation until delivery; group 2 received daily 1 daily multiple micronutrient + placebo tablet from 13 weeks of pregnancy until delivery. Setting and health worker cadre: the intervention was conducted by obstetricians and gynaecologists from the Alzahra hospital, in Iran. |
|
| Outcomes | Hb concentrations, HCT, serum iron, serum ferritin, total iron binding capacity at baseline and at delivery, birthweight, gestational age at birth, prematurity, Intrauterine growth retardation, 1' Apgar score, 5 min Apgar score, admission duration in neonatal care intensive unit, premature rupture of membranes, placenta abruption, pre‐eclampsia, periventricular‐intraventricular haemorrhage (PIH), gestational diabetes, intrauterine fetal death (IUFD), oligohydramnios. | |
| Notes | Both groups were matched for mother's age, BMI, parity, previous obstetric history and iron parameters. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation:non‐anaemic status at the start of supplementation. Daily iron dose: 30 mg elemental iron. Iron release formulation: normal release preparation/not specified. Iron compound: not specified. Malaria setting: yes. As of 2011: Malaria risk due to P. vivax and P. falciparum exists from March to November inclusive in rural areas of the provinces of Hormozgan and Kerman (tropical part) and the southern part of Sistan‐Baluchestan. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and care provider were blinded to the intervention groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor not described. Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were 56 loses to follow‐up in the group 1 (iron) in comparison to 49 participants lost to follow‐up in the placebo group. 70/480 (14.6%) were excluded in the group 1 in comparison to 108/480 (22.5%) in the placebo group. Overall attrition was 18%. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Paintin 1966.
| Methods | RCT, 3 arms with individual randomisation. | |
| Participants | 180 primigravidae women with less than 20 weeks' gestation and Hb > 100 g/L attending antenatal clinic in Aberdeen Maternity Hospital, United Kingdom. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 received 3 tablets containing 4 mg elemental iron each (total 12 mg daily); group 2 received 3 tablets containing 35 mg elemental iron (total 105 mg elemental iron daily); group 3 received placebo. Intervention was from week 20 to week 36 of gestation. Setting and health worker cadre: the intervention was performed by clinic and laboratory staff of the Obstetric Medicine Research Unit of Aberdeen Maternity Hospital and Castle Terrace Antenatal Clinic in Aberdeen, United Kingdom. |
|
| Outcomes | Maternal: Hb, HCT at baseline, and at weeks 20, 30, 36 of gestation and 7‐13 days postpartum; plasma volume at 30 weeks, total red cell volume, serum iron and total iron binding capacity at 30 weeks, subjective health and side effects at 30 weeks. | |
| Notes | Unsupervised.
Compliance estimated by measuring tablets returned. Authors report good compliance. Gestational age at start of supplementation: late gestational age (20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: unspecified/mixed anaemia status at the start of supplementation. Daily iron dose: mixed doses (lower dose group ‐ 12 mg daily; higher dose group 105 mg daily). Iron release formulation: normal release preparation/not specified. Iron compound: not specified. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Placebo‐controlled with sequentially numbered packages. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | It was stated that women and staff were blind to treatment allocation. Placebo described as identical. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was stated that laboratory staff were blind to allocation until after the trial had been completed. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5%. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Preziosi 1997.
| Methods | RCT 2 arms with individual randomisation. | |
| Participants | 197 healthy pregnant women 17‐40 years of age, with 28 +/‐ 3 weeks of gestation attending antenatal care clinic in a Mother‐Child Health Centre in Niamey, Niger. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 100 mg of elemental iron (as ferrous betainate) daily; group 2 received placebo. Supplementation was from 28 +/‐ 3 weeks of gestation until delivery. Setting and health worker cadre: the intervention was performed by physicians at an isolated, urban maternal and child health centre serving low‐ or middle‐class villagers in Niger. |
|
| Outcomes | Maternal: Hb concentration, MCV, HCT, erythrocyte protoporphyrin, serum iron, transferrin, total iron binding capacity, serum ferritin concentrations, at baseline and at the first stage of labour and at 3 and 6 months postpartum, prevalence of iron deficiency and iron‐deficiency anaemia. Infant: birthweight and length, Hb concentration, MCV, erythrocyte protoporphyrin, serum iron, transferrin saturation, serum ferritin concentrations at birth and at 3 and 6 months; Apgar scores. | |
| Notes | Supervised by physicians who recorded tablet consumption.
Compliance not reported. Gestational age at start of supplementation: late gestational age (more than 20 weeks' gestation). Anaemic status at start of supplementation: mixed anaemia status at baseline. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous betainate. Malaria setting: high risk malaria setting. As of 2011: Malaria risk due predominantly to P. falciparum exists throughout the year in the whole country. Chloroquine‐resistant P. falciparum reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By random numbers. |
| Allocation concealment (selection bias) | Low risk | Packages of tablets numbered by manufacturer. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, placebo‐controlled trial. Placebo prepared by manufacturer. Women and staff blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Most outcomes reported were laboratory results, newborn outcomes were reported, but these were most likely recorded by clinic staff blind to allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up not described. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Pritchard 1958.
| Methods | RCT 3 arms with individual randomisation. | |
| Participants | 172 pregnant women believed to be in the second trimester of pregnancy by date of last menstrual period attending antenatal care clinic in Parland Memorial Hospital, Dallas, Texas, USA. | |
| Interventions | Participants were randomly assigned to 1 of 3 interventions: group 1 received 1000 mg of iron intramuscularly as iron‐dextran; group 2 received 112 mg of elemental iron (as ferrous gluconate) daily in 3 tablets; group 3 received placebo tablets. Supplementation started during 2nd trimester until delivery. Setting and health worker cadre: the intervention was performed by physicians at a prenatal clinic in the United States of America. |
|
| Outcomes | Maternal: Hb concentration at baseline and at delivery. | |
| Notes | Unsupervised.
Only groups 2 (oral iron) and 3 (placebo) were included in this review.
Compliance not reported. Gestational age at start of supplementation: mixed gestational age at the start of supplementation (2nd trimester). Anaemic status at start of supplementation: mixed anaemia status at baseline. Daily iron dose: higher daily dose (more than 60 mg elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Partial blinding. Placebo and active treatment compared. It was not clear whether staff were aware of allocation. It was stated that women given active supplements were repeatedly urged to take the tablets. It was not clear whether or not the placebo group received the same instruction. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessor not blinded. Outcomes reported unlikely to be affected by any lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up not described (no loss to follow‐up apparent). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | High risk | No other bias apparent. |
Puolakka 1980.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 32 healthy non‐anaemic pregnant women attending antenatal care at maternity centres of Oulu University Central Hospital, Finland with uncomplicated pregnancy of less than 16 weeks, and no earlier haematological problems. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 200 mg of elemental iron (as ferrous sulphate) daily; group 2 received no treatment. Supplementation started at 16th week of gestation until 1 month postpartum. Setting and health worker cadre: the intervention was performed by obstetricians at maternity centres in Oulu, Finland. |
|
| Outcomes | Maternal: Hb, HCT, RBC count, leucocyte count, reticulocytes, MCV, MCH, serum iron, total iron binding capacity, transferrin, vitamin B12, whole folate, and serum ferritin concentration at baseline, and at weeks, 16, 20, 24, 28, 32, 36, 40 and 5 days, 1, 2, and 6 months postpartum. Bone marrow aspirates at 16th and 32nd week and at 2 months postpartum. Infant: birthweight, Apgar scores at 5 minutes. | |
| Notes | Unsupervised.
Compliance not reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | "randomly divided into two groups." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding mentioned. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. It was stated that no women discontinued the study. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Romslo 1983.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 52 healthy pregnant women attending outpatient Women's clinic at Haukeland Hospital, Bergen, Norway within first 10 weeks of a normal singleton pregnancy with uncomplicated delivery at 37‐42 weeks. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 200 mg of elemental iron (as ferrous sulphate) daily; group 2 received placebo. Supplementation started at 10 weeks of gestation. Setting and health worker cadre: the intervention was performed by physicians at the outpatient clinic of the Women's Clinic, Haukeland Hospital in Bergen, Norway. |
|
| Outcomes | Maternal: Hb, HCT, PCV, erythrocyte count, leucocyte count, MCV, MCH, MCHC, serum iron, iron binding capacity, erythrocyte protoporphyrin, serum ferritin at baseline and every month during 2nd trimester and every 2 weeks until delivery. Infant: birthweight and Apgar scores. | |
| Notes | Unsupervised.
Compliance measured by tablet count was 55% in the iron‐treated group. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | "randomly divided into two groups." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo‐controlled trial – placebo was reported to look and taste the same as active treatment. Not clear if staff blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% (7/52 lost to follow‐up). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Siega‐Riz 2001.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 429 non‐anaemic, iron replete women with less than 20 weeks of gestation attending who had not taken supplements containing iron in the last month, with a singleton pregnancy attending the prenatal clinic at the Wake County Human services in Raleigh, North Carolina, USA. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received multivitamin/mineral supplements containing 30 mg of iron (as ferrous sulphate) daily; group 2 received multivitamin/mineral supplements containing 0 mg of iron (no iron) until 29 weeks of gestation. Supplementation started on average at 12 weeks. The multivitamin/mineral supplement contained the following: 4000 IU vitamin A; 400 IU vitamin D; 70 mg vitamin C; 500 μg (0.5 mg) folic acid; 1.5 mg thiamine; 1.6 mg riboflavin; 17 mg niacin; 2.6 mg vitamin B6; 2.5 μg vitamin B1; 200 mg calcium; 100 mg magnesium; 1.5 mg copper; 15 mg zinc. Folic acid supplements were prescribed for all women who had received the positive pregnancy test until the first prenatal visit. Setting and health worker cadre: the intervention was performed by physicians at a clinic serving patients of a low socioeconomic group in Raleigh, North Carolina, United States of America. |
|
| Outcomes | Maternal: prevalence of anaemia, iron repletion and iron‐deficiency anaemia at 26‐29 weeks, side effects, compliance to treatment, iron status (Hb concentration, serum ferritin at 26‐29 weeks, preterm delivery. Infant: birthweight, proportion of low birthweight, small‐for‐gestational age. | |
| Notes | Unsupervised.
Compliance measured by pill counts and a questionnaire and was 66% in the iron group and 63% in the control group. Compliance was also measured by the Medication Event Monitoring System (MEMS) in a subsample of 100 women. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: lower daily dose (30 mg or less elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound:ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By using random number generator. |
| Allocation concealment (selection bias) | Low risk | Tretament provided in coded bottles by pharmacy. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as double‐blind, randomised trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | More than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Simmons 1993.
| Methods | RCT, 3 arms with individual randomisation | |
| Participants | 376 pregnant women with ages between 16‐35 years, with mild anaemia (Hb concentrations between 80‐110 g/L) attending 8 maternal and child health centres in Kingston, St. Andrews and Spanish Town, Jamaica, with gestational age between 14‐22 weeks. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 received 1 placebo tablet daily; group 2 received 100 mg of elemental iron (as ferrous sulphate) daily; group 3 received 50 mg of elemental iron (in a gastric delivery system capsule) daily. All women received 400 μg (0.4 mg) of folic acid. Setting and health worker cadre: the intervention was performed by clinic nurses and field workers at maternal and child health centres in urban areas of Jamaica. |
|
| Outcomes | Hb, HCT, MCV, white cell count, serum iron, total iron binding capacity, serum ferritin, serum transferrin receptor, at baseline, at 6 weeks and at 12 weeks after start of supplementation as well as side effects. | |
| Notes | Gestational ages differed in the participants and we have not included outcome data from this trial in the review. Gestational age at start of supplementation: mixed gestational age (up to 22 weeks' gestation at recruitment). Anaemic status at start of supplementation: anaemic at the start of supplementation (mild anaemia Hb 80‐110 g/L). Daily iron dose: mixed dose (medium dose group ‐ 50 mg elemental iron in gastric delivery system capsule; higher dose group 100 mg of elemental iron). Iron release formulation: gastric delivery system capsule (controlled release preparation). Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: very limited risk of P. falciparum malaria may occur in the Kingston St Andrew Parish. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By random number table. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes distributed to clinics (not clear if envelopes were opaque). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Partial blinding. A placebo was provided but this was a single table while women in treatment groups received either 2 tablets or a capsule. It was stated that women were not told which preparations contained iron but staff would be aware of treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 376 women were recruited. 275 women were followed up (73.1%) but laboratory results were available for 66% of the original sample. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | The 3 groups were reported to have similar characteristics at baseline. |
Suharno 1993.
| Methods | RCT 4 arms with individual randomisation. | |
| Participants | 305 women randomised and follow‐up data were available for 251 pregnant women aged 17‐35 years, parity 0‐4 and Hb concentrations between 80 and 109 g/L from rural villages in Bogor, West Java, Indonesia. Women recruited at 16‐24 weeks' gestation. | |
| Interventions | Participants were randomly allocated to 1 of 4 groups: group 1 received 2.4 mg of retinol and 1 placebo iron tablet daily; group 2 received 60 mg of elemental iron (as ferrous sulphate) and a placebo vitamin A tablet daily; group 3 received 2.4 mg of retinol and 60 mg of elemental iron (as ferrous sulphate); group 4 received 2 placebos for 8 weeks. Setting and health worker cadre: the intervention was performed by village workers among middle and low socioeconomic groups in rural villages in Bogor, West Java, Indonesia. |
|
| Outcomes | Hb, HCT, serum ferritin, serum iron, total iron binding capacity, serum retinol, transferrin saturation, at baseline and after 8 weeks of supplementation (2nd and 3rd trimester). | |
| Notes | Relevant comparison in this review: group 3 (iron + vit A) vs group 1 (vit A but no iron) for comparison 5: daily oral iron + other vitamins and minerals supplementation vs daily oral same other vitamins and minerals (without iron) supplementation. group 2 (iron + placebo) vs group 4 (placebo) for comparison 2: daily oral supplementation with iron alone vs no treatment/placebo. No prespecified outcome available for extraction. No data included. Gestational age at start of supplementation: mixed gestational age at the start of supplementation (16‐24 weeks' gestation). Anaemic status at start of supplementation: anaemic at the start of supplementation (Hb < 110 g/L). Daily iron dose: higher daily dose (60 mg elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: high malaria risk area. As of 2011: Malaria risk exists throughout the year in all areas of the 5 eastern provinces of East Nusa Tenggara, Maluku, North Maluku, Papua and West Papua. In other parts of the country, there is malaria risk in some districts, except in Jakarta Municipality, in big cities. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. P. vivax resistant to chloroquine reported. Human P. knowlesi infection reported in the province of Kalimantan. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Carried out by independent researcher. |
| Allocation concealment (selection bias) | Low risk | "Subjects were allocated a sequential number from 1 to 305. An independent researcher randomly labelled the iron and placebo preparations" which were colour coded. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as a double‐masked study and placebo provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Allocation was not revealed until after the study was completed. Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 305 women were randomised and follow‐up data were available for 251 (83%). Reasons for loss to follow‐up were described and were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | Groups appeared similar at baseline. |
Sun 2010.
| Methods | Quasi‐randomised trial with individual assignment in order of enrolment. | |
| Participants | 186 anaemic pregnant women, 12 to 24‐weeks' gestation, age between 20‐30 years with Hb concentration ≥ 80 and < 110 g/L, no dietary supplements during the previous 2 months and no abnormal pregnancy response from the communities of Shen County in a central rural area of China. | |
| Interventions | Participants were randomly allocated in the order of enrolment to 1 of 4 groups: group 1 (n = 47) was supplemented daily with 60 mg elemental iron (as ferrous sulphate); group 2 (n = 46) received with 60 mg elemental iron (as ferrous sulphate) and 400 μg (0.4 mg) folic acid; group 3 (n = 46) with 60 mg elemental iron (as ferrous sulphate), 2 mg retinol and 400 μg (0.4 mg) folic acid; group 4 (n = 47) was the placebo control group. The capsules were coloured red, yellow, green and blue during manufacture by Hurun (a Chinese food‐additive company, Beijing). The capsules were to be taken daily for 2 months. Setting and health worker cadre: the study was carried out in communities of Shen County in a central rural area of China. Women were home‐visited once a week by the village nurse to replenish supplements and to monitor compliance by counting and recording the number of supplements that were taken. |
|
| Outcomes | Hb concentration; plasma iron; plasma retinol and plasma folate; erythrocyte protoporphyrin; interleukin 2; lymphocyte proliferation at baseline and after 2 months intervention. | |
| Notes | Relevant comparisons for this review: group 1 (n = 47) was supplemented daily with 60 mg elemental iron (as ferrous sulphate) vs group 4 (n = 47) was the placebo control group. group 2 (n = 46) received with 60 mg elemental iron (as ferrous sulphate) and 400 μg (0.4 mg) folic acid vs group 4 (n = 47) was the placebo control group. Gestational age at start of supplementation: mixed gestational age at the start of supplementation (12‐24 weeks' gestation). Anaemic status at start of supplementation: anaemic at the start of supplementation (Hb < 110 g/L). Daily iron dose: higher daily dose (60 mg elemental iron). Iron release formulation: normal release preparation/not specified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. Supported by Danone Nutrition Institute China. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported as randomly assigned but method unclear. It is reported that the assignment to the groups was done in order of enrolment. |
| Allocation concealment (selection bias) | High risk | The capsules were coloured red, yellow, green and blue during manufacture and the assignment was done in order of enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, care providers and outcome assessors were blinded to the intervention groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, care providers and outcome assessors were blinded to the intervention groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low losses to follow‐up and they were balanced among the groups. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Low risk | There were no substantial differences between the groups in any of the baseline characteristics. |
Svanberg 1975.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 60 healthy primiparous women attending antenatal care clinic in Goteborg, Sweden with uncomplicated pregnancy and less than 14 weeks of gestation and with Hb concentrations above 120 g/L who had not received iron supplements in the previous 6 months or parenteral iron at any previous time. Women whose Hb concentration fell below 100 g/L during the study period were excluded and received immediate therapy. | |
| Interventions | Participants were randomly allocated to receive 200 mg of elemental iron (as a sustained release preparation of ferrous sulphate) daily or placebo from 12 weeks of gestation until 9 weeks post delivery. Setting and health worker cadre: the intervention was performed by physicians at the University of Göthenburg in Sweden. |
|
| Outcomes | Maternal: iron absorption measurements; Hb concentration, HCT, bone marrow haemosiderin, MCHC, total iron binding capacity, transferrin saturation at baseline, and at weeks 16, 20, 24, 28, 32, and 35; and 8‐10 weeks after delivery. | |
| Notes | Unsupervised.
Compliance measured by remaining pills count was 86 +/‐ 3%. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher dose (more than 60 mg elemental iron daily). Iron release formulation: sustained release preparation of ferrous sulphate. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, care provide, and outcome assessor blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants, care provider, and outcome assessor blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Taylor 1982.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 48 healthy pregnant women with no adverse medical or obstetric history attending antenatal care clinic in Newcastle, England, United Kingdom before 12 weeks of gestation. | |
| Interventions | Participants were randomly allocated to 1 of 2 groups: group 1 receive about 65 mg elemental iron (as 325 mg of ferrous sulphate) and 350 μg (0.35 mg) of folic acid daily from 12 weeks until delivery; group 2 received no supplements. Setting and health worker cadre: the intervention was performed by physicians at the Princess Mary Maternity Hospital in Newcastle upon Tyne, United Kingdom. |
|
| Outcomes | Maternal: Hb concentration, serum ferritin, MCV at 12 weeks and every 4 weeks until delivery, and at 6 days, 6 weeks and 6 months after delivery; plasma volume at 12 and 36 weeks of gestation. Infant: birthweight, infant death, admission to special care unit. | |
| Notes | Unsupervised.
Compliance not reported. Gestational age at start of supplementation: early gestational age (less than 20 weeks' gestation at the start of supplementation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | "Randomly assigned". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Tholin 1993.
| Methods | RCT, 3‐arm trial with individual randomisation. | |
| Participants | 83 healthy nulliparous non‐vegetarian, non‐anaemic pregnant women with serum ferritin concentrations above 10 μg/L. | |
| Interventions | Participants were randomly assigned to 1 of 3 groups: group 1 received 100 mg of elemental iron (as ferrous sulphate) daily; group 2 received placebo; group 3 received dietary advice only. Setting and health worker cadre: the intervention was performed by physicians at the Maternal Health Unit of Ostersund Hospital in Ostersund, Sweden. |
|
| Outcomes | Blood Hb, serum ferritin and blood manganese were determined at baseline before 15th week of gestation, between 25‐28 weeks, and between 35‐40 weeks of gestation. Median and ranges are presented. | |
| Notes | The aim of this study was to examine the relationship between iron and zinc levels during pregnancy. No outcomes were extractable from this report for this review. Median serum zinc levels were reported by randomisation group "levels did not differ between groups". Median Hb levels were reported for women who had normal vs complicated deliveries (rather than by randomisation group. Results for mean Hb and serum ferritin levels were depicted in graphs. Gestational age at start of supplementation: early gestational age at the start of supplementation (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as "randomly assigned". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blind for iron supplemented group. Placebo‐controlled trial with outcome assessment by an obstetrician blind to group assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There were some discrepancies in the figures reported in 2 study publications. (We have not included data from this trial in the review.) |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | High risk | Results were not simple to interpret and some results were not reported according to randomisation group. |
Tura 1989.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 254 non‐anaemic non‐iron deficient healthy pregnant women from multiple centres in Italy between 12‐16 weeks of gestation. Exclusion criteria: acquired or congenital anaemia, haemoglobinopathies, thalassaemia, medically or surgically treated cardiopathy, abortion, hypertension, gastric resection, metabolic or endocrine disorder, hepatic or renal disease, epilepsy or another neurological disease, previously treated for cancer, alcohol or substance dependence. | |
| Interventions | Participants were randomly assigned to receive 40 mg of elemental iron (containing 250 g of ferritin in a micro granulated gastric‐resistant capsule) daily or no treatment from 12‐16 weeks of gestation until the end of puerperium. Setting and health worker cadre: the intervention was performed by physicians in health centres in Italy. |
|
| Outcomes | Maternal: Hb concentration, RBC count, MCV, serum iron, total transferrin, transferrin saturation, serum ferritin at 12‐16 weeks, 2 times during pregnancy, at 38‐42 weeks, and at puerperium 48‐52 weeks. | |
| Notes | Unsupervised.
The study included another sample of women who were iron deficient and received 2 forms of iron preparation. This sample is not used in this review.
Compliance reported as higher than 98.5%. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: medium iron dose (more than 30 and less than 60 mg). Iron release formulation: micro granulated gastric resistant capsule. Iron compound: not specified. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By random number lists. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes progressively numbered. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of blinding. No placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Van Eijk 1978.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 30 pregnant women with uncomplicated pregnancies and deliveries attending antenatal care clinic at the University Hospital Obstetric Unit in Rotterdam, Netherlands. | |
| Interventions | Participants received 100 mg of elemental iron (as ferrous sulphate) daily or no treatment from the third month of gestation until delivery. Follow‐up was until 12 weeks after delivery. Setting and health worker cadre: the intervention was performed by physicians at the Univeristy Hospital Obstetrical Clinic in Rotterdam, the Netherlands. |
|
| Outcomes | Maternal: Hb concentration, serum iron, serum ferritin, transferrin concentration at baseline and every 3‐4 weeks until delivery, and 3 months after delivery. Infant: Hb concentration, transferrin, serum iron, serum ferritin in cord blood at term. | |
| Notes | Unsupervised.
Compliance not reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: mixed/unspecified anaemia status. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | High risk | Not used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Wallenburg 1983.
| Methods | RCT, 2 arms with individual randomisation. | |
| Participants | 44 non‐anaemic Caucasian women with singleton pregnancy and no major illnesses attending the University Hospital Obstetrical Clinic of the Erasmus University in Rotterdam who had not received iron supplementation during their first visit. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1: received 105 mg of elemental iron (as ferrous sulphate) daily in a sustained release preparation; group 2: received no iron supplement. Supplementation started at 14‐16th week of gestation until delivery. Setting and health worker cadre: the intervention was performed by physicians at the Antenatal Clinic of the University Hospital Dijkzigt in Rotterdam, the Netherlands. |
|
| Outcomes | Maternal: Hb, serum iron, serum transferrin and serum ferritin concentrations at 16, 28, 36 weeks, delivery, 6 and 12 weeks postpartum. | |
| Notes | Unsupervised.
Compliance not reported. We treated this study carried out collaboratively in 2 different sites as 2 different trials, 1 conducted in Rotterdam (Wallenburg 1983) and 1 conducted in Antwerp (Buytaert 1983). Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By random table numbers. |
| Allocation concealment (selection bias) | Low risk | By means of sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participant nor provider blinded. No placebo used. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 20% losses to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Willoughby 1967.
| Methods | RCT. 5‐arm trial. | |
| Participants | 3599 pregnant women with Hb above 100 g/L at their antenatal care clinic visit at Queen's Mother's Hospital in Glasgow, Scotland, United Kingdom. Women who reported not taken the tablets regularly were excluded as well as those diagnosed with anaemia during the study. | |
| Interventions | Participants were randomly allocated to 1 of 5 interventions: group 1 received no prophylactic supplements; group 2 received 105 mg of elemental iron daily (as chelated iron aminoates); group 3 received 105 mg of elemental iron with 100 μg (0.1 mg) of folic acid; group 4 received 105 mg of elemental iron daily with 300 μg (0.3 mg) of folic acid; group 5 received 105 mg elemental iron daily with 450 μg (0.45 mg) of folic acid. Starting and ending time of supplementation variable. Setting and health worker cadre: the intervention was performed by a team of nurses and physicians at the Antenatal Clinic of the Queen Mother's Hospital in Glasgow, United Kingdom. |
|
| Outcomes | Maternal: Hb concentration at baseline and in every visit, at early puerperium and during postnatal visit; incidence of obstetric complications. incidence of megaloblastic anaemia. Infant: Hb and whole blood folate levels a 6 weeks of age. Incidence of neonatal complications. | |
| Notes | Unsupervised.
Groups 3‐5 were merged for the purposes of this review.
Women were excluded from the trial and the analysis if they were diagnosed as anaemic.
Compliance not reported. Gestational age at start of supplementation: mixed gestational age at the start of supplementation. Anaemic status at start of supplementation: mixed anaemia status (Hb > 100 g/L). Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: not clear? normal release preparation/unspecified. Iron compound: chelated iron aminoates. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding. Women with anaemia or non‐compliant were withdrawn from the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Less than 20% losses to follow‐up. However, women were excluded from the trial and the analysis if they were diagnosed as anaemic. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Wills 1947.
| Methods | Quasi‐randomised trial with 2 arms with individual randomisation. | |
| Participants | 500 pregnant women attending antenatal care clinic at the Royal Free Hospital in London, England, United Kingdom during wartime, with ages between 18‐43 years. Women with severe anaemic or rheumatoid arthritis were excluded. | |
| Interventions | Participants were alternatively allocated to receive 580 mg of elemental iron (as ferrous gluconate) daily or placebo from their first visit.
Supplementation starting variable and ending time unclear. Setting and health worker cadre: the intervention was performed by nurses and physicians at the Antenatal Clinic of the Obstetrical Department at the Roryal Free Hspital in London, United Kingdom. |
|
| Outcomes | Maternal: Hb concentration using the Haldane method at baseline and every 4 weeks until delivery, then day 1, 2‐4 days, 5‐16 days and 6 weeks postpartum; serum protein and pregnancy complications (not reported by group). Infant: birthweight (not reported). | |
| Notes | Unsupervised.
The study was conducted during wartime and a bomb incident interrupted the work allowing only a small portion of original sample studied and reported. Women were receiving special food rations.
Compliance not reported. Gestational age at start of supplementation: mixed gestational age (variable). Anaemic status at start of supplementation: mixed anaemia status/unspecified. Daily iron dose: higher daily dose (more than 60 mg elemental iron daily). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous gluconate. Malaria setting: non‐malarial setting. As of 2011: Malaria: no risk. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised, alternate. |
| Allocation concealment (selection bias) | High risk | Alternate allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Placebo provided but authors suggest blinding may not have been convincing to staff. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | It was suggested that laboratory staff may have been aware of allocation but this was unlikely to have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | More than 20% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Zeng 2008 (C).
| Methods | Cluster‐randomised trial (3 arms). Villages were assigned to interventions. Villages were stratified and there was block randomisation to ensure geographical balance in 2 participating counties. | |
| Participants | 5828 eligible pregnant women with less than 28 weeks and resident in 2 poor rural counties in Shaanxi Province of north west China participated in the study. Village doctors recruited women by active surveillance. In the study areas there were no specific policies for the distribution of multiple micronutrients or iron‐folic acid supplements even in disadvantaged areas although folic acid supplements were promoted to prevent NTDs.Their villages were randomly assigned for women to receive 1 of 3 groups. | |
| Interventions | Their villages were randomly assigned for participants to receive 1 of 3 groups: group 1, daily antenatal multiple micronutrients containing 30 mg elemental iron, 400 µg (0.4 mg) folic acid and 15 mg zinc, 2 mg copper, 65 µg selenium, 150 µg iodine, 800 µg vitamin A, 1.4 mg vitamin B1 (thiamine), 1.4 mg vitamin B2 (riboflavin), 1.9 mg vitamin B6, 2.6 µg vitamin B12, 5 µg vitamin D, 70 mg vitamin C, 10 mg vitamin E, and 18 mg niacin; group 2 who received a tablet containing 60 mg elemental iron and 400 μg (0.4 mg) of folic acid; group 3 received a tablet containing 400 μg (0.4 mg) folic acid alone (control). Setting and health worker cadre: the intervention was performed by local maternal and child health workers in rural, antenatal clinics and local health facilities in Shaanxi Province, China. |
|
| Outcomes | Birthweight within 1 hour of delivery, low birthweight, birth length, gestational age at birth, preterm delivery, small‐for‐gestational age babies, maternal Hb concentration in the third trimester (gestation 28‐32 weeks), anaemia in the third trimester, fetal losses during pregnancy, birth outcome, delivery information, neonatal and maternal deaths; neonatal survival at the 6 weeks, perinatal deaths, neonatal deaths, stillbirths. A follow‐up publication describes a follow‐up to 850 children born to women who participated in the study and focused on mental development outcomes using the Bayley scales of infant development at 3,6,12, and 24 months of age. | |
| Notes | We have only included groups 2 (iron + folic acid) and 3 (folic acid alone) in the analyses. In the data tables we have adjusted the raw data presented in the paper to take account of the cluster‐design effect. We have calculated an effective sample size by dividing figures by the design effect calculated using the ICC for the trial’s primary outcome: birthweight ICC = 0.03. We have used the same sample adjustment for all outcomes. 65.9 of women in group 2 (iron + folic acid) and 65.2% of women in group 3 (folic acid) started supplementation before 16 weeks of gestational age. Gestational age at start of supplementation: mixed/unspecified gestational age. Anaemic status at start of supplementation: mixed anaemia status. Daily iron dose: higher dose group (60 mg elemental iron daily) in 1 group and 30 mg in another group (multiple micronutrients). Iron release formulation: normal release preparation/unspecified. Iron compound: unspecified. Malaria setting: yes. As of 2011: Malaria risk, including P. falciparum malaria, exists in Yunnan and to a lesser extent in Hainan. P. falciparum resistance to chloroquine and sulphadoxine–pyrimethamine reported. Limited risk of P. vivax malaria exists in southern and some central provinces, including Anhui, Ghuizhou, Henan, Hubei, Jiangsu. There is no malaria risk in urban areas. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The randomisation schedule was generated off site with a pseudo‐random number generator.” Recruitment bias was unlikely. |
| Allocation concealment (selection bias) | Low risk | Off‐site randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Cluster trial all women in village received the same intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Low risk for laboratory outcomes but unclear for other outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Total clusters (531). Total women 5828 (in 3 groups, 2 groups included in the analyses, total randomised 3929). Overall 133 women lost to follow‐up and 279 stopped taking supplements and were excluded (7% lost to follow‐up). 3270 women in groups 1 and 2 had live births (3306 babies). Approximately 6% further missing data for primary outcome (infant birthweight). Further missing data for other outcomes. Available case analysis for primary outcome (LBW). |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | The trial was stopped early because of funding constraints. The treatment groups appeared similar at baseline. Results were adjusted for cluster design effect. |
Ziaei 2007.
| Methods | RCT 2 arms with individual randomisation. | |
| Participants | 750 apparently healthy non‐smoking non‐anaemic (with Hb higher or equal to 132 g/L) pregnant women in early stage of second trimester, BMI 19.8‐26 kg/m2 and age 17‐35 years with singleton pregnancy attending prenatal care in Tehran, Iran. Women with history of threatened abortion in the present pregnancy or diseases related with polycythaemia such as asthma and chronic hypertension were not included. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 50 mg of elemental iron (as ferrous sulphate) + 1000 μg (1 mg) folic acid daily; group 2 received placebo and 1000 μg (1 mg) of folic acid daily. Setting and health worker cadre: the intervention was performed by midwives and physicians at multiple urban clinical centres in Tehran, Iran. |
|
| Outcomes | Maternal: Hb at 24‐28 weeks, 32‐36 weeks, premature delivery, weight gain, caesarean sections, hypertensive disorders, severe anaemia, high Hb concentrations, iron deficiency, iron‐deficiency anaemia, MCV, MCH and MCHC at term, severe anaemia and high Hb concentrations at any time during 2‐3 trimesters, symptomatic tract infection, puerperal infection, antepartum and postpartum haemorrhage, transfusion provided, side effects (any), diarrhoea, constipation, nausea, heartburn, vomiting, placental abruption, premature rupture of membranes. Infant: birthweight, perinatal mortality rate, low Apgar at 10th minute, small‐for‐gestational age. |
|
| Notes | Unsupervised.
Supplementation started 13.07 ± 2.02 weeks' gestation for group 1 and 13.66 ± 3.45 weeks' gestation for the placebo group and lasted until after delivery.
No compliance reported. Gestational age at start of supplementation: early gestational age at the start of supplementation (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non‐anaemic. Daily iron dose: medium iron dose (50 mg elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due toP. vivax and P. falciparum exists from March to November inclusive in rural areas of the provinces of Hormozgan and Kerman (tropical part) and the southern part of Sistan‐Baluchestan. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By means of table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Coded bottles. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and care provider and outcome assessor blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and care provider and outcome assessor blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
Ziaei 2008.
| Methods | RCT 2 arms with individual randomisation. | |
| Participants | 244 pregnant women 17‐35 years of age attending prenatal care in Tehran, Iran, with BMI between 19.8‐26 kg/m2, and 13‐18 weeks of gestation, with singleton pregnancy and non‐anaemic (Hb 132 g/L or higher) and normal serum ferritin (15 μg/L or higher). Women who smoked, had history of diseases such as polycythaemia, asthma, or chronic hypertension, or a history or threatened abortion in the present pregnancy were excluded. | |
| Interventions | Participants were randomly assigned to 1 of 2 groups: group 1 received 50 mg of elemental iron (as ferrous sulphate) daily; group 2 received placebo from 20th week of gestation until delivery. All women received 50 mg elemental iron (as ferrous sulphate) after delivery for 6 weeks. Setting and health worker cadre: the intervention was performed by midwives and physicians at a prenatal clinic in Tehran, Iran. |
|
| Outcomes | Maternal: Hb, HCT, serum ferritin at baseline, at time of delivery, 1 week postpartum and 6 weeks postpartum, postpartum haemorrhage, caesarean sections. | |
| Notes | Unsupervised.
No compliance reported. Gestational age at start of supplementation: early gestational age (supplementation started before 20 weeks' gestation). Anaemic status at start of supplementation: non anaemic. Daily iron dose: medium dose (50 mg elemental iron). Iron release formulation: normal release preparation/unspecified. Iron compound: ferrous sulphate. Malaria setting: yes. As of 2011: Malaria risk due to P. vivax and P. falciparum exists from March to November inclusive in rural areas of the provinces of Hormozgan and Kerman (tropical part) and the southern part of Sistan‐Baluchestan. P. falciparum resistant to chloroquine and sulphadoxine–pyrimethamine reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By means of table of random numbers. |
| Allocation concealment (selection bias) | Low risk | Coded bottles. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and care provider blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Low risk for laboratory outcomes and other outcomes likely to have been recorded by blinded staff. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Less than 5% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | There is insufficient information to permit judgement. |
| Other bias | Unclear risk | No other bias apparent. |
BMI: body mass index Fe: iron GGT: gamma‐glutamyl transferase GSH‐Px: glutathione peroxidase Hb: haemoglobin HCT: hematocrit (same as PCV: packed cell volume) ICC: intraclass correlation co‐efficient ITT: intention‐to‐treat IV: intravenous LBW: low birthweight MCH: mean corpuscular (or cell) haemoglobin MCHC: mean corpuscular (or cell) haemoglobin concentration MCV: mean corpuscular (or cell) volume MDA: malondialdehyde OGIT: oral glucose intolerance test OGTT: oral glucose tolerance test PCV: packed cell volume (same as HCT: hematocrit) RBC: red blood cell RCT: randomised clinical trial SD: standard deviation SES: socioeconomic status SOD: superoxide dismutase vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aaseth 2001 | 67 non‐anaemic pregnant women attending prenatal care clinics in Kingsvinger Hospital, in Kingsvinger, Norway were allocated to a daily regimen of either 100 mg Fe or 15 mg Fe. Both groups received iron at different doses. No comparisons allowed within the scope of this review. |
| Abel 2000 | Community‐based study in Vellore district, India using a pre‐post experimental design measuring the impact of an iron supplementation program, helminthic treatment and education intervention in the prevalence of anaemia in the different trimesters of pregnancy. The same pregnant women were not followed. The type of study is not eligible for inclusion in this review. |
| Adhikari 2009 | 320 pregnant women attending the Tribhuvan University Teaching Hospital, Nepal for antenatal care were randomised to 1 of 4 groups:
group 1: 60 mg elemental iron daily (as ferrous sulphate);
group 2: 60 mg elemental iron daily (as ferrous sulphate) with a count of unused pills at antenatal appointments;
group 3: 60 mg elemental iron daily (as ferrous sulphate) with education (direct counselling and colour brochure) on iron and anaemia;
group 4: 60 mg elemental iron daily (as ferrous sulphate) with pill count and education (direct counselling and colour brochure) on iron and anaemia. In this randomised trial the aim of the intervention was to increase compliance and all 4 intervention groups received daily iron supplements. The type of interventions do not allow for comparisons within the scope of this review. |
| Afifi 1978 | 260 pregnant women from Cairo, Egypt (formerly part of United Arab Republic) were randomly allocated to 1 of 2 groups:
group 1 received 130 mg elemental iron daily (a slow release ferrous sulphate preparation, Plexafer‐F®) and 360 μg (0.36 mg) folic acid;
group 2 received iron (as ferrous sulphate, no dose reported) in addition to 5000 μg (5 mg) folic acid. Both groups received daily iron supplementation in different preparations. The type of interventions do not allow for comparisons within the scope of this review. |
| Agrawal 2011 | 75 pregnant women aged 19 to 40 years attending the department of Obstetrics and Gynaecology, Kasturba Hospital, Manipal India, with normal Hb levels between 13‐16 weeks' gestation will be randomly assigned to 2 supplementation groups:
group 1: ferrous fumarate with 98.6 mg of elemental iron (Continuous group) 1 capsule daily (all days a week);
group 2: ferrous fumarate with 98.6 mg of elemental iron (Intermittent group) 1 capsule daily 4 days a week (i.e. from Monday to Thursday). The supplementation period will start at 13‐16 weeks and continued up to delivery and in postnatal period. The study was excluded because there are 2 groups receiving iron, 1 group daily and the other intermittently. This type of comparison is outside the scope of this review. |
| Ahn 2006 | 209 pregnant women between 18 and 45 years of age, attending outpatient obstetric clinics at North York General Hospital and the Hospital for Sick Children in Toronto, Canada were randomly assigned to receive multiple micronutrient supplements containing 60 mg of elemental iron (as ferrous fumarate) (Materna®) or another supplement (PregVit®) to be taken twice daily with the morning dose containing 35 mg of elemental iron (as ferrous fumarate) and the evening dose containing 300 mg calcium, and other vitamins and minerals. Both groups received daily iron in different doses as well as other vitamins and minerals. The type of interventions do not allow for comparisons within the scope of this review. |
| Alaoddolehei 2012 | 145 healthy pregnant women 20 to 40 years of age with Hb 110g/L or higher at 20 weeks' gestation attending the Gynecology and Obstetrics Clinic, Babol, Iran, from October 2002 to September 2005 were assigned (on the basis of number given them at first visit) to 1 of 2 groups: group 1 (even numbers, n = 73) received daily iron supplement at 50 mg/day; group 2 (odd numbers, n = 72) received an intermittent dose of 3 times per week (50 mg/each time) from 20th week gestation until delivery. Women with β minor thalassaemia, Hb less than 11 g/dL, more than 1 delivery and diagnosed with internal and infectious diseases were excluded. Blood samples were assessed for complete blood count (Hb, HCT, RBC) , iron, ferritin and zinc at baseline in the first trimester in all participants. Both groups received iron supplements in different regimens.The type of interventions is outside the scope of this review. |
| Angeles‐Agdeppa 2003 | 744 apparently healthy pregnant (with less than 20 weeks) and non‐pregnant women of reproductive age (15‐49 years) from the municipalities of Calasiao, Binmaley and Santa Barbara, Philippines who were pregnant or most likely to become pregnant within the 12‐month duration of the study, and who volunteered to participate in the study were provided 2 preparations of iron‐folic acid supplements. Women with severe anaemia or history of malaria were excluded. Non‐pregnant women were prescribed 4 capsules monthly each containing 60 mg of elemental iron and 3500 μg (3.5 mg) folic acid to be taken once weekly before bedtime (to be purchased by the women in local drugstores). Pregnant women received free of cost 4 capsules monthly each containing 120 mg of elemental iron and 3500 μg (3.5 mg) of folic acid to be taken once a week before bedtime until delivery and for 3 months thereafter. Pregnant women seen at the health centres with 20 weeks or more of gestation were advised to take their usual daily dose of iron‐folic acid tablets containing 60 mg of elemental iron and 500 μg (0.5 mg) of folic acid. Women were followed for 12 months. Hb, HCT, MCV, MCHC Hb concentration, serum ferritin, transferrin receptors, prevalence of iron deficiency and anaemia, compliance were assessed at baseline, 4.5, 9 and 12 months. There was not randomisation and the control group was not appropriate for comparisons. The type of comparisons are not relevant for the scope of this review. |
| Arija 2014 | 878 non‐anaemic pregnant women older than 18 years of age with ≤ 12 weeks' gestation without anaemia (Hb > 110 g/L), capable of understanding the official State languages (Castilian or Catalan) at early gestation stage, and their subsequent newborns attending 10 Primary Care Centers from Catalunya (Spain) of the Catalunya Sexual and Reproductive Healthcare Service [Atención a la Salud Sexual y Reproductiva (ASSIR)] of the Catalan Institute of Health [Instituto Catalán de la Salud (ICS)] subdivided in 2 strata as a function of the Hb levels at the start of the pregnancy. Women with multiple pregnancy, taking > 10 mg iron during the months prior to week 12, hypersensitivity to egg protein (due to the iron prescription formula contains ovalbumin), previous serious illness (immunosuppressed status) or chronic illness that could affect the nutritional development (e.g. cancer, diabetes), malabsorption, and liver disease such as chronic hepatitis or cirrhosis. Participants are randomly assigned to 1 of 2 groups per stratum starting from around the 12th week of gestation and continuing up to partum:
group 1: women will receive of 20 mg elemental iron (150 mg ferrimanitol ovoalbumin);
group 2: women will receive 80 mg per day of elemental iron (600 mg ferrimanitol ovoalbumin). The reference dose is the control group: women will receive 40 mg elemental iron (300 mg ferrimanitol ovoalbumin), similar to that routinely prescribed in clinical practice. The study was excluded because all women receive iron supplements. The type of intervention is outside the scope of this review. EudraCT Number: 2012‐005480‐28. |
| Babior 1985 | 15 healthy pregnant women 22‐32 years old, in the first trimester of pregnancy from Boston, Massachusetts, USA were randomly assigned to 3 different multiple micronutrient preparations to assess absorption of iron. All women received iron in the multiple micronutrient supplements. The type of interventions is not relevant for the scope of this review. |
| Balmelli 1974 | 42 pregnant women attending antenatal care clinic at the Hospital University of Berne, Switzerland were randomly assigned to 1 of 2 groups: group 1 received 37 mg elemental iron (as ferrous sulphate) and succinic acid 3 times daily (total daily dose of 111 mg elemental iron and 555 mg succinic acid);
group 2 received 37 mg elemental iron (as ferrous sulphate) and succinic acid 3 times daily (total daily dose of 111 mg elemental iron and 555 mg succinic acid) and 1 tablet 3 times a day containing 100 μg (0.1 mg) folic acid and 100 μg vitamin B12. Both groups received iron supplements. The type of interventions is outside the scope of this review. |
| Bencaiova 2007 | 260 women with singleton pregnancy in Zurich, Switzerland, were randomised at 21‐24 weeks of gestation to receive either intravenous iron group (further divided into 2 doses of 200 mg iron saccharate or 3 doses of 200 mg iron) or 80 mg elemental iron (as ferrous sulphate) daily. Both groups received iron in different routes of administration. No comparisons allowed within the scope of this review. |
| Berger 2003 | 864 apparently healthy married pregnant and non‐pregnant nulliparous women of reproductive age planning to have a child soon from 19 rural communes of the Thanh Mien district in Hai Duong province, Vietnam were invited to participate and assigned to 1 of the following interventions according to their pregnancy status at baseline: women who were pregnant received free of charge UNICEF tablets containing 60 mg of elemental iron and 250 μg (0.25 mg) of folic acid to be taken daily and women who were non‐pregnant were prescribed pink packs of tablets containing 60 mg of elemental iron and 3500 μg (3.5 mg) of folic acid that they could buy at their village from the Women's Union, to be taken once weekly. If these women became pregnant, women received red packs of tablets containing 120 mg of elemental iron and 3500 μg (3.5 mg) of folic acid free of charge to be taken once weekly. After delivery women were given tablets containing 60 mg of elemental iron and 0.5 mg of folic acid free of charge for 3 months to be taken weekly. Hb concentration, serum ferritin, and serum ferritin receptors, prevalence of anaemia and iron deficiency and compliance were measured at baseline, at 4.5, 9 and 12 months. This is not a randomised study and no comparisons can be made for the aims of this review. |
| Bergsjo 1987 | Planned study registered at the Oxford Database of Perinatal Trials. Author contacted and informed the project was not completed. |
| Bhatla 2009 | 109 pregnant non‐anaemic women between 14 and 18 weeks (49% vegetarian) with no prior intake of iron supplements in the Department of Obstetrics and Gynaecology of the All India Institute of Medical Sciences in New Delhi, India were randomly allocated into 1 of 3 different groups: group 1 (n = 37) received the standard Government of India supply of Irofol® tablets containing 100 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) folic acid (Nestor Pharmaceuticals Ltd., Faridabad, Haryana, India) to be taken once daily;
group 2 (n = 36) received the standard Government of India supply of Irofol® tablets containing 100 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) folic acid and were instructed to take 2 tablets on any 1 day of the week; 1 before lunch and the other before dinner (total 200 mg elemental iron and 1000 μg (1 mg) folic acid per week) with no tablets taken during the rest of the week;
group 3 (n = 36) received Ferium® tablets iron (III)‐hydroxide poly maltose complex tablets daily containing Iron (III) Hydroxide Polymaltose containing 100 mg elemental iron and 350 μg (0.35 mg) folic acid to be taken 1 tablet daily (Emcure Pharmaceuticals Ltd., Pune). All groups received health education regarding the importance of diet in pregnancy, iron‐rich foods and appropriate dietary practices and were instructed to take the tablets 30 min before meals and not with tea, coffee or milk. All women were also advised to take calcium supplements after meals. All groups received iron with different regimens. The type of interventions are not within the scope of this review. |
| Blot 1980 | 203 pregnant women attending prenatal care clinics in Antonie Beclere Hospital, Paris, France during their 6th month visit were randomly allocated to either 105 mg of elemental iron with 500 mg of ascorbic acid or a placebo. The intervention group received iron with ascorbic acid in comparison to placebo. The type of intervention do not allow for comparisons within the scope of this review. |
| Bokhari 2011 | 33 healthy non‐smokers Caucasian, primiparous, with singleton pregnancy (week 20 to week 30) pregnant women with pre pregnancy BMI between 19.8 and 26 not taking medicines known to influence iron status nor iron supplements and free from gastrointestinal disorders or allergies were randomised to eat 3–4 slices of iron‐rich or control bread daily for 6 weeks. Women with Hb concentrations not within the normal range (below 70 g/L or over 160 g/L) were excluded. Low versus high iron fortified breads were compared. Two 24‐hour‐prompted (multiple‐pass) dietary recalls were completed, and validated algorithms were used to determine the amount of ‘available iron’ from the diet. Findings from this study show that iron‐rich staple foods can help women reach dietary targets for iron. Further research using fortified staple foods containing higher levels of iron is now warranted to establish physiological benefits. The study was excluded because food fortification is out of the scope of this review. The intervention is outside of the scope of this review. |
| Bokhari 2012 | 65 pregnant women 18–45 years between weeks 20 and 30 gestation were recruited from South Manchester University Hospital antenatal clinic, United Kingdom and 33 participants that attended their first appointment were randomised to 1 of 2 groups:group 1 were provided 3–4 slices of functional bread containing flour (Eragrostis tef) that was naturally rich in iron (2.1 mg iron per 50 g slice) and added enzyme phytase or control bread daily for 6 weeks. Participants substituted the bread they would normally eat with the intervention provided. Two 24‐hour‐prompted (multiple‐pass) dietary recalls were completed, and validated algorithms were used to determine the amount of ‘available iron’ from the diet. Levels of total ‘available iron’ were similar in both groups and correlated positively with total dietary iron. This study assessed the effects of an iron rich bread with a control bread. The type of intervention is outside of the scope of this review. |
| Brown 1972 | 109 pregnant women attending prenatal care clinics in Manchester, England, United Kingdom were randomly allocated to 1 of 3 groups:
group 1 received 1 tablet daily given in 'reminder packs';
group 2 received 1 tablet daily given in loose forms;
group 3 received 2 tablets daily given in loose form. Tablets contained 50 mg of elemental iron (as slow release ferrous sulphate) and 400 μg (0.4 mg) of folic acid. All groups received iron daily. The type of interventions do not allow for comparisons within the scope of this review. |
| Burslem 1968 | 472 pregnant women attending the booking clinic in Manchester, England, United Kingdom were alternatively allocated to 2 forms of iron:
group 1 received 105 mg elemental iron (as a slow release ferrous sulphate preparation) and a tablet containing 5000 μg (5 mg) folic acid daily; group 2 received 3 tablets of combined conventional 60 mg elemental iron (as ferrous sulphate) and 1 tablet containing 5000 μg (5 mg) folic acid for a total of 180 mg elemental iron daily. Both groups received daily iron supplementation in different preparations. The type of interventions do not allow for comparisons within the scope of this review. |
| Buss 1981 | 18 pregnant women were randomly assigned to receive either a tablet containing 80 mg of elemental iron with a new mucous membrane vaccine (Tardyferon®) or a tablet containing 80 mg elemental iron with 350 μg (0.35 mg) folic acid (Tardyferon‐Fol®) for a period of 3 months. All women received daily iron. The type of interventions do not allow for comparisons within the scope of this review. |
| Carrasco 1962 | 2 liquid preparations were used in this study: 1 with D‐sorbitol and the other without. Both preparations contained vitamin B12, vitamin B6, ferric pyrophosphate and folic acid.The type of interventions do not allow for comparisons within the scope of this review. |
| Casanueva 2003a | 120 singleton pregnant women attending the Instituto Nacional de Perinatologia in Mexico City, Mexico with Hb concentrations higher than 115 g/L at 20 weeks of gestation (equivalent to 105 g/L at sea level) were randomly assigned to 1 of 2 groups: group 1: 1 tablet containing 60 mg of elemental iron (as ferrous sulphate), 200 μg (0.2 mg) folic acid and 1 μg vitamin B12 given daily; group 2: 2 tablets (total 120 mg of elemental iron (as ferrous sulphate), 400 μg (0.4 mg) folic acid, and 2 μg vitamin B12) to be taken once weekly. The groups received either daily supplementation or weekly supplementation at no cost. Supplement tablets were identical in content and were to be ingested from the 20th week of pregnancy until delivery. No comparisons allowed within the scope of this review. |
| Castren 1968 | 126 healthy pregnant women attending Maternity Centres of Turku, Finland were assigned to 1 of 2 groups: group 1 (n = 63) received 3 tablets a day providing a total 120 mg elemental iron (as ferrous sulphate) daily; group 2 (n = 63) received 3 tablets a day providing total 120 mg elemental iron (as ferrous sulphate) + 9000 μg (9 mg) folic acid daily from their first visit at 10‐20th week of gestation until term. Both groups received iron. The type of intervention is outside the scope of this review. |
| Chanarin 1968 | 206 women attending the antenatal clinic at St. Mary's Hospital, London, United Kingdom with less than 16 weeks pregnant at the first attendance. At the 20th week they were allotted to 1 of 2 groups: group 1 received tablets to be taken once daily containing 260 mg ferrous fumarate; group 2 received tablets to be taken daily containing 260 mg ferrous fumarate and 100 μg (0.1 mg) of folic acid. Iron deficiency was largely eliminated by giving 1 g of intravenous iron dextran as 4 250 mg doses at weekly intervals to all participants in early pregnancy. Both groups received iron. The type of comparison is not within the scope of this review. |
| Chawla 1995 | 81 pregnant women with 20 +/‐ weeks of gestation from Ludhiana City, India were divided to 1 of 3 groups: group 1 received 60 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid daily; group 2, 60 mg of elemental iron (as ferrous sulphate) and 2,000,000 IU of vitamin A; group 3, who did not receive any supplements. Supplementation was for a period of 15 weeks. Outcomes measured included Hb, RBC count, total iron binding capacity, transferrin saturation, serum iron, serum vitamin A at baseline and at 36 +/‐ 2 weeks of gestation. Poor methodological quality. Pregnant women who were willing to go to the hospital or centre once a week to collect the iron supplements were included in the groups 1 and 2. The rest of the participants were included in the control group. This is not a randomised trial. |
| Chew 1996a | 256 clinically healthy pregnant women from low SES attending 1 antenatal care clinic in Guatemala City, Guatemala and Hb > 80 g/L were recruited. City of Guatemala is at 1500 m above sea level, so values were adjusted by altitude subtracting 5 g/L in Hb. Participants were randomly assigned to 1 of 2 groups: group 1: daily supervised intake of 60 mg elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) folic acid; group 2: weekly supervised intake of 180 mg of elemental iron (as ferrous sulphate) and 3500 μg (3.5 mg) of folic acid in 1 intake once a week. Supplementation started at different gestational age for each participant. Average gestational age at start was 20.5 weeks until 38th week. All groups received iron with different regimens. The type of interventions are not within the scope of this review |
| Chew 1996b | 120 clinically healthy pregnant women attending 1 antenatal care clinic in Guatemala City, Guatemala with Hb > 80 g/L were recruited. Women were from low SES. City of Guatemala is 1500 m above sea level, so values were adjusted by altitude subtracting 5 g/L in Hb. Participants from low SES were randomly assigned to 1 of 2 groups: group 3: daily unsupervised intake of 60 mg elemental iron (as ferrous sulphate) and 0.5 mg folic acid; or group 4: weekly unsupervised intake of 180 mg of elemental iron (as ferrous sulphate) and 3.5 mg of folic acid in 1 intake once a week. Supplementation started at an average of 20.5 weeks of gestation until 38th week. All groups received iron with different regimens. The type of interventions are not within the scope of this review. |
| Coelho 2000 | 100 pregnant women with 20‐34 weeks of gestation attending the antenatal clinic at The Bandra Holy Family Hospital, Bandra, Mumbai India were randomly assigned to 1 of 2 groups: group 1 received 30 mg elemental iron + other essential vitamins and minerals daily; groups 2 received 116 mg elemental iron, folic acid, zinc and vitamin C daily. Outcomes included Hb concentration, maternal weight gain, infant birthweight and maternal compliance and side effects Both groups received iron supplementation. Both groups received daily iron supplementation. The types of interventions do not allow for comparisons within the scope of this review. |
| Cook 1990 | 200 women at Kansas University Medical Center, Kansas, USA were randomly assigned to receive 50 mg elemental iron daily given either as Gastric Delivery System (GDS) or conventional ferrous sulphate . Gastrointestinal side effects were evaluated. The participants were non‐pregnant women. |
| Dawson 1962 | 2498 pregnant women attending antenatal care clinic in Crumpsal Hospital, Manchester United Kingdom were grouped to receive folic acid or as controls. The assignment was not randomised. Participants whose Hb fell below 100 g/L after 28th week received oral iron if they had not previously received oral iron, had not reached the 36th week of gestation and had a MCHC of less than 30%. If these participants had been receiving oral iron, iron was then provided parenterally. The type of interventions and comparisons are outside the scope of this review. |
| Dawson 1987 | 42 healthy women with less than 16 weeks of pregnancy entering prenatal care at the Department of Obstetrics and Gynecology, University of Texas, Texas, USA were randomly assigned to receive either a multiple micronutrient supplement containing 65 mg of elemental iron or 1 multiple micronutrient supplement with no iron, calcium, zinc and copper and pantothenic acid. Both groups received different multiple micronutrient supplement formulations. No comparisons allowed within the scope of this review. |
| Dijkhuizen 2004 | 170 pregnant women with less than 20 weeks' gestation from 13 adjacent villages in a rural area in Bogor District, West Java, Indonesia were randomly assigned to receive daily supplementation with B‐carotene (4.5 mg), zinc (30 mg), both, or placebo containing 30 mg elemental iron and 400 μg (0.4 mg) folic acid. Both groups received daily iron and folic acid. The types of interventions do not allow for comparisons within the scope of this review. |
| Edgar 1956 | 179 pregnant women with Hb levels below 105 g/L and more than 16 weeks of gestation volunteered for this study and were divided into 4 supplementation groups according to the stage of pregnancy at which iron was introduced: 16th week, 20th week, 24th week, and non‐supplemented controls. 37% of these women were lost to follow‐up and were excluded from the final analysis. This is not a randomised trial. |
| Ekstrom 1996 | 176 pregnant women attending Ilula Lutheran Health Centre's antenatal service in Iringa region, Tanzania with 21‐26 weeks of gestational age and Hb > 80 g/L were randomly assigned to receive 120 mg elemental iron (as ferrous sulphate in conventional form) daily or 50 mg elemental iron as gastric delivery system (GDS) daily. Both groups received daily iron supplementation in different preparations. The types of interventions do not allow for comparisons within the scope of this review. |
| Ekstrom 2002 | 209 apparently healthy women attending antenatal care clinics in rural areas of Mymemsingh thana, Bangladesh, with fundal height of 14‐22 cm (18‐24 weeks of gestation), who had not used iron supplements prior to the study. Exclusion criteria: women with Hb concentrations < 80 g/L. Each clinic was randomly assigned to 1 of 2 interventions: 60 mg of elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) folic acid given in 1 tablet daily, or 120 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) folic acid once a week (given in 2 tablets 1 day of the week). Supplementation continued until 6 weeks postpartum. Supplementation started at baseline for 12 weeks. All groups received iron with different regimens. The type of interventions are not within the scope of this review. |
| Fletcher 1971 | 643 pregnant women attending antenatal clinic in London, England, United Kingdom were randomly assigned to 1 of 2 groups: group 1 received 200 mg of ferrous sulphate daily; group 2 received 200 mg of ferrous sulphate with 5000 μg (5 mg) of folic acid daily. Both groups received iron. No comparisons allowed within the scope of this review. |
| Giles 1971 | 528 pregnant women in the first antenatal care visit at the Royal Women’s Hospital Melbourne, Australia patients were divided in 4 groups: group 1 those attending the antenatal clinic for the first time before 10 weeks of gestation; group 2 those attending the antenatal clinic for the first time from 10‐20 weeks of gestation; group 3 those attending the antenatal clinic for the first time from 20‐30 weeks of gestation; group 4 those attending the antenatal clinic for the first time at or after 30 weeks of gestation. They received a 200 mg ferrous sulphate and 5 a mg folic acid tablet a day, for the remaining of the pregnancy and 5 mg of folic acid were administered to 1 group (n = 265) and a placebo (n = 263) to the other. The study was excluded because both study groups received iron, and the difference was the supplementation or not with 5 mg of folic acid daily. This type of comparison is outside the scope of this review. |
| Gomber 2002 | 40 apparently healthy women with singleton pregnancy in their second trimester (between 16‐24 weeks of gestation), living in urban slums, from low SES attending Guru Teg Bahadur Hospital, Delhi, India were randomly assigned to receive 1 tablet containing 100 mg of elemental iron (as ferrous sulphate) with 500 μg (0.5 mg) folic acid daily or once a week. Weekly intake was supervised. Duration of supplementation was 100 days. Hb and HCT concentrations at baseline, at 4 weeks, 8 weeks and 14 weeks of supplementation, serum ferritin concentration, at baseline, at 14 weeks of supplementation and at delivery. Both groups received iron and folic acid in different regimens (daily versus weekly). The type of interventions do not allow for comparisons within the scope of this review. |
| Goonewardene 2001 | 92 pregnant women from 14‐24 weeks of gestation attending the university antenatal clinic, in Galle, Sri Lanka were randomly assigned to 1 of 3 regimens: group 1 (n = 26) received a tablet containing 100 mg of elemental iron (as ferrous fumarate), with additional micronutrients once a week; group 2 (n = 35) received the same tablet but 3 times a week; group 3 (n = 31) received the same supplement in a daily fashion. All groups were receiving iron and multiple micronutrients with different regimens (daily, weekly, 3 times a week). The type of interventions do not allow for comparisons within the scope of this review. |
| Gopalan 2004 | 900 pregnant women of poor SES attending government antenatal care clinics in New Delhi, India were grouped in 3 groups: group 1 (n = 300) received routine antenatal care; group 2 (n = 300) received 100 mg of elemental iron and 500 μg (0.5 mg) folic acid daily from the 20th week of gestation; group 3 (n = 300) received 100 mg of elemental iron and 500 μg (0.5 mg) folic acid daily from the 20th week of gestation and additionally 900 mg of alpha linolenic acid from the 22nd week of gestation. Outcomes assessed included birthweight, low birthweight, premature delivery. The study is not reported as randomised and is excluded in the first screening for eligibility. |
| Goshtasebi 2012 | 370 pregnant women were randomly assigned to receive either daily or twice weekly iron supplementation during pregnancy. There were no significant differences in initial and delivery Hb and HCT levels between the 2 groups. Ferritin concentrations were significantly lower in the twice‐weekly group at delivery, but hypoferritinaemia (ferritin < 15 microg/L) was not observed in either group. The frequency of nausea, vomiting and constipation was significantly lower in the twice‐weekly group. The type of intervention is not within the scope of this review. |
| Gringras 1982 | 40 pregnant women attending antenatal care clinic in Cheshire, England, United Kingdom were given a tablet containing 47 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid daily or a tablet containing 100 mg of elemental iron (as ferrous glycine sulphate) daily. Both groups received iron. No comparisons allowed within the scope of this review. |
| Grover 1998 | 200 pregnant women with gestation 16‐24 weeks attending for care in rural health centre in Gazipur village in East Delhi, India from Jan‐Dec 1994 with Hb 70 g/L or more and no tuberculosis, chronic diseases, "toxaemia", bleeding piles were randomly assigned to 1 of 2 groups: group 1: women received 100 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid on alternate days: (data available for 56 women); group 2: women received 100 mg of elemental iron daily (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid (data available for 64 women). It is not clear how the doses were supplied. The type of interventions do not allow for comparisons within the scope of this review. |
| Guldholt 1991 | 192 pregnant women in Horsens Hospital, Denmark were consecutively randomised to receive 1 of 2 treatments: group 1: received a daily vitamin‐mineral tablet containing 15 mg of elemental iron; group 2: received a daily vitamin‐mineral tablet containing 100 mg of elemental iron. Both groups received iron in different doses. No comparisons allowed within the scope of this review. |
| Hampel 1974 | 65 untreated and 54 treated pregnant women in West Berlin, Germany were assessed during pregnancy for Hb concentrations, iron and folate levels, total iron binding capacity, and RBC count. No data are presented for outcomes prespecified in the review. Women were of different gestational age. No outcomes can be extracted from the paper. |
| Hanieh 2013 | 1258 pregnant women older than 16 years of age and with less than 16 week gestation living in 104 communes from Ha Nam province, a malaria‐free province in Viet Nam were assigned at the cluster (commune) level to 1 of 3 groups: group 1 received 60 mg elemental iron plus 400 ug (0.4 mg) folic acid daily; group 2 received 60 mg elemental iron plus 1500 ug (1.5 mg) folic acid per capsule; administered as 2 capsules/week; group 3 received 60 mg elemental iron plus 1500 ug (1.5 mg) plus a variation of the dose of micronutrients in the UNIMMAP daily supplement; administered as 2 capsules/week. Women were excluded if they had a high‐risk pregnancy—multi‐fetal pregnancy (confirmed on palpation or ultrasound), a significant medical condition or if they had severe anaemia (Hb concentration lower than 80 g/L) at enrolment were referred to the commune health station for further management. A placebo control was not contemplated, as it was considered unethical to withhold iron supplementation during pregnancy. Primary outcome was birthweight. The type of intervention is outside the scope of this review. |
| Hartman‐Craven 2009 | In this cross‐over study 2 types of multivitamin supplements were compared: 18 healthy pregnant women 24‐32 weeks' gestation attending a Toronto hospital were recruited and received 2 different supplements in a random order and followed up over 8 hours. Both preparations contained iron and folic acid (although in different doses). The aim of the study was to see whether absorption was improved with a powdered preparation. |
| Hawkins 1987 | No report available of the study results. |
| Hemminki 1991 | 2960 pregnant women were recruited by midwives in 27 maternity health centres in Tampere (15 centres) and in 5 neighbouring communities (12 centres) in Finland, and randomised into 2 groups: selective and routine iron supplementation. Routine group: Women received iron throughout pregnancy regardless of Hb level, starting at the latest in the 17th week of gestation. A dose of 100 mg elemental iron per day was recommended, but this could be tailored according to the midwife's judgment. Intervention group: any pregnant women after the 14th week of gestation showing HCT < 0.30 (Hb < 100 g/L) in 2 consecutive visits If the Hb was still less than 100 g/L and/or MCV was less than 82 and a low ferritin was found, 50 mg iron twice a day as ferrous sulphate was recommended. The length of the treatment was to be 2 months or until the HCT was > 10.32 or higher (Hb 110 g/L) or higher). By request of the midwives the treatment schedule was relaxed later during the trial: iron therapy was begun if the mother's HCT was 0.31 or below after the 33rd week. Mothers were followed until the postpartum check‐up, and data were collected by 5 different questionnaires and abstracted from the infant's patient record. There were some changes during the trial. For example in group 2 “By request of the midwives the treatment schedule was relaxed later during the trial “or in group 1, iron doses or compounds “could be tailored according to the midwife's judgment”. The study was excluded because there was not comparable control group because both groups received iron. The routine group received 100 mg of iron as elemental iron and was composed of anaemic and non‐anaemic women. In group 2, anaemic women received 2 doses of 50 mg of iron as ferrous sulphate in slow release form, while for non‐anaemic women it was not clear if women received routine treatment. Group 2 was separated into anaemic and non‐anaemic women. Both groups received iron. |
| Hermsdorf 1986 | 120 unselected pregnant women were given 114 mg of elemental iron daily from week 15 until delivery, or not treatment. Only an abstract with insufficient data available. |
| Horgan 1966 | 42 apparently healthy pregnant women attending 2 antenatal care clinics in London, England were assigned to 1 of 3 interventions: group 1 received 200 mg ferrous sulphate with 5000 μg (5 mg) of folic acid 3 times a day; group 2 received 350 mg of ferrous aminoate with 50 μg (0.05 mg) folic acid 3 times a day; group 3 received 200 mg of ferrous sulphate with 500 μg (0.5 mg) folic acid once a day. Intervention period was 3 weeks. All groups received daily iron and folic acid. No comparisons allowed within the scope of this review. |
| Hosokawa 1989 | 84 anaemic women seeking antenatal care in the Department of Obstetrics and Gynaecology of the Fukui School of Medicine Hospital, Japan were randomly assigned to receive 100 mg of elemental iron (as ferrous sulphate) daily after the evening meal, or the same dose + vitamin C for 4 weeks. Both groups received daily iron. No comparisons allowed within the scope of this review. |
| Hossain 2014 | 200 pregnant women attending the outpatient obstetric clinic at the Civil Hospital Karachi in Karachi, Pakistan with 20 weeks or less of gestation, a singleton pregnancy, and normoglycaemic and normotensive at the time of antenatal booking were randomly allocated to 1 of 2 groups: group 1 (n = 100) received routine antenatal care, which included ferrous sulphate 200 mg, twice daily, and 600 mg of calcium lactate daily; group 2 (n = 100) received routine antenatal care regimen and an oral liquid formulation (400 IU/drop) of vitamin D3 at a daily dose of 4000 IU (10 drops daily) starting at completed 20 weeks of gestation. Women with history of gestational diabetes, hypertension, thyroid disorder, chronic liver disease, and evidence of fetal anomaly in current pregnancy were excluded. Both groups received iron. the type of interventions is outside the scope of this review. |
| Itam 2003 | 266 pregnant women from Calabar coastal southeastern Nigeria were randomly assigned to 1 of 3 groups: group 1 received a supplement containing iron (as 300 mg ferrous fumarate), 5000 ug (5 mg) folic acid, 10 ug vitamin B12, 25 mg vitamin C, 0.3 mg zinc sulphate and 0.3 mg magnesium sulphate; group 2 received iron (as 200mg ferrous sulphate) and 5000 ug (5 mg) folic acid once daily; group 3 received iron (as 200 mg ferrous sulphate) 3 times daily and 5000 ug (5 mg) folic acid once daily. The intervention lasted from 18th week of gestation till term. There were also 2 subgroups under each major group anaemic and non‐anaemic groups. Blood samples were collected from each participant on admission into the study and every 2 weeks and analysed for packed cell volume (HCT), Hb, MCHC, reticulocytes and ferritin levels. All participants received iron at different doses and regimens. The type of intervention is outside the scope of this review. |
| Iyengar 1970 | 800 pregnant women with less than 24 weeks of gestation and Hb > 85 g/L in India were assigned by rotation to 1 of 4 groups:
group 1 received placebo tablets;
group 2 received 30 mg of elemental iron as ferrous fumarate in a single tablet daily; group 3 received 30 mg of elemental iron (as ferrous fumarate) with 500 μg (0.5 mg) folic acid in a single tablet; group 4 received in addition to iron and folic acid, 2 μg of vitamin B12 in a single tablet. Loss to follow‐up was 65%. This is not a randomised trial. |
| Kaestel 2005 | 2100 pregnant women (22 +/‐ 7 weeks' gestation at entry) attending antenatal clinics in Bissau, Guinea‐Bissau or who were identified by The Bandim Health project were randomly assigned to receive daily multi micronutrient tablet containing 1 RDA of 15 micronutrients, or daily multi micronutrients containing 2 times the RDA except for iron that was maintained at 1 RDA or a conventional prenatal daily iron (60 mg elemental iron) and 400 μg (0.4 mg) folic acid supplement. In a follow‐up analysis (Andersen 2010), of the previous study a 2‐year follow‐up examined the effects of the interventions on fetal loss and under 2 mortality. 2169 women were recruited from 4 suburban districts followed by the Bandim Health project in collaboration with the Danish Epidemiology Science Centre in Guinea‐Bissau. Women with severe anaemia (Hb less than 70 g/L) received 60 mg elemental iron daily in addition to the intervention. All participants received impregnated bed net at inclusion and were provided weekly anti‐malarial prophylaxis with chloroquine phosphate (300 mg base) throughout pregnancy. Also women with more than 10 parasite per 200 leucocytes were offered anti‐malarial treatment with chloroquine. All groups receive iron and folic acid daily. No comparisons allowed within the scope of this review. |
| Kann 1988 | 36 healthy non‐anaemic pregnant women in second or third trimesters of gestation were randomly assigned to receive 1 of 4 groups: group 1 received a tablet (Stuartnatal® 1 + 1) containing 65 mg elemental iron, 1000 μg (1 mg) folic acid and 12 additional micronutrients daily; group 2 received a tablet (Stuart Prenatal®) containing 60 mg elemental iron, 800 μg (0.8 mg) folic acid and 11 additional micronutrients; group 3 received a tablet (Materna®) containing 60 mg elemental iron, 1000 μg (1 mg) folic acid and 17 additional micronutrients daily; group 4 received a tablet (Natalins Rx®) containing 60 mg elemental iron, 1000 μg (1 mg) folic acid and 14 additional micronutrients daily. All participants received iron and multiple micronutrients. No comparisons allowed within the scope of this review. |
| Khambalia 2009 | In this randomised trial carried out in Bangladesh childless, non‐pregnant married women under 40 were randomised to receive food supplements (sprinkles) containing either iron and folic acid or folic acid alone. 272 women were randomised and women were followed up for 9 months. If women became pregnant they were withdrawn from the study and ALL pregnant women received both iron and folic acid. The study was excluded as it focused on a non‐pregnant population. |
| Kulkarni 2010 | This study was secondary analysis of the data from the Christian 2003 (C) study included in the review. |
| Kumar 2005 | 220 pregnant women with a singleton pregnancy and Hb between 80‐110 g/L at 16‐24 weeks' gestation from New Delhi, India were randomly allocated to receive daily oral iron therapy of 100 mg elemental iron (as ferrous sulphate) with 500 μg (0.5 mg) folic acid or 250 mg of iron sorbitol intramuscularly and repeated at an interval of 4‐6 weeks. This trial compares the effects of daily oral iron with 2 injections of high dose parenteral iron. No comparisons allowed within the scope of this review. |
| Lira 1989 | 199 pregnant women with less than 16 weeks' gestation attending antenatal care at the Hospital Clinica Universidad Catolica ein Santiago, Chile were randomly assigned to 1 of 2 groups: group 1 (n = 78) received 105 mg elemental iron (as ferrous sulphate) and 500 mg ascorbic acid; group 2 (n = 75) received 105 mg elemental iron (as ferrous sulphate), 500 mg ascorbic acid and 350 ug (0.35 mg) folic acid daily. There were 36 losses to follow‐up. Both groups received iron. The type of interventions provided is outside the scope of this review. |
| Liu 1996 | 395 healthy, anaemic and non‐anaemic, pregnant women attending prenatal care at 2 outpatient clinics in Xianjiang, China. Women with Hb < 80 g/L were excluded. Maternal age was 25.15 ± 2.28 years. Women were randomly assigned to 1 of 3 groups: group 1: 60 mg elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) of folic acid daily; group 2: 120 mg of elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid daily; group 3: 120 mg elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid once weekly. All women randomised to treatments received iron. A control group that received no iron was composed of women who did not want to participate in the study and did not receive any iron supplements. |
| Ma 2008 | 366 pregnant women between 20‐35 years of age women in rural China with 12–24 weeks' gestation; with Hb 105 g/L or lower, all receiving 60 mg elemental iron and 400 μg (0.4 mg) folic acid were randomly assigned to 1 of 4 groups:
group 1 (n = 93) received daily 60 mg elemental iron (as ferrous sulphate) and 400 μg (0.4 mg) folic acid;
group 2 (n = 91) received daily 60 mg elemental iron (as ferrous sulphate), 400 μg (0.4 mg) folic acid + 2000 μg retinol (as retinyl palmitate); group 3 (n = 91) received daily 60 mg elemental iron (as ferrous sulphate), 400 μg (0.4 mg) folic acid + 1.0 mg riboflavin;
group 4 (n = 91) received daily 60 mg elemental iron (as ferrous sulphate), 400 μg (0.4 mg) folic acid, 2000 μg retinol (as retinyl palmitate) + 1.0 mg riboflavin. The intervention lasted 2 months. All groups received iron. The type of comparisons are outside the scope of this review. |
| Madan 1999 | 109 apparently healthy pregnant women with 16‐24 weeks of gestation who had not received iron supplements were randomly assigned to 1 of 3 groups:
group 1 received 60 mg of elemental iron + 500 μg (0.5 mg) of folic acid once daily;
group 2 received 120 mg of elemental iron + 500 μg (0.5 mg) of folic acid once daily;
group 3 received 120 mg of elemental iron twice daily + 500 μg (0.5 mg) of folic acid. Duration of supplementation was 12‐14 weeks. All participants received iron and folic acid daily. No comparisons are allowed within the scope of this review. |
| Marin 2012 | 360 pregnant women 16 years or older from La Plata, Buenos Aires province, Argentina or who lived in the region for over a year; and who voluntary accepted to participate in the study (consent agreement) were randomly assigned to 1 of 2 groups:
group 1 (n = 174) received free medicines from the health centre near their homes consisting of 60 mg of elemental iron (as ferrous sulphate) once (prophylaxis) or twice (treatment) daily and 5000 ug (5 mg) folic acid daily;
group 2 (n = 186) were contacted monthly by a member of the health team in order to personalise free iron dispense 60 mg of elemental iron (as ferrous sulphate) once (prophylaxis) or twice (treatment) daily and 5000 ug (5 mg) folic acid daily during all pregnancy period until 45 days after the delivery. This medicine was always dispensed by that same health professional either through the health centre, or in case that the patient did not attend her periodical consultation, drugs were dispensed at the participant's home. All women received iron and folic acid. The difference was on the access to the supplements or the personalised assistance and delivery of the intervention. The type of interventions are outside the scope of this review. |
| Mbaye 2006 | 1035 pregnant women attending mother and child health clinics near the town of Farafenni, The Gambia were randomised to receive either folic acid (500‐1500 μg/day) together with oral iron (47 mg of ferrous sulphate per tablet) or oral iron alone (60 mg of ferrous sulphate per tablet) daily for 14 days. All women received treatment with 3 tablets of SP (25 mg of pyrimethamine and 500 mg of sulphadoxine). Both groups received iron daily. No comparisons allowed within the scope of this review. |
| McKenna 2002 | 102 healthy pregnant women attending antenatal clinics at the Royal Jubilee Maternity Hospital in Belfast, Ireland with a singleton pregnancy and Hb > 104 g/L and known gestational age of less than 20 weeks who were non‐compliers with routine prescription of 200 mg of ferrous sulphate daily, were randomly assigned to receive 2 sachets of 24 mL each of Spatone® water containing 10 mg of elemental iron or placebo. Participants were instructed to take the 2 sachets daily half an hour before breakfast diluting it in orange juice. Primary outcomes were compliance and side effects. Duration of intervention was from week 22 to week 28 of gestation. The intervention is not an iron supplement but an iron‐fortified water product. |
| Menon 1962 | 273 healthy pregnant women with 16‐24 weeks of gestation and Hb concentrations at or above 105 g/L attending antenatal care clinics were divided in order in which they were registered in 3 groups:
group 1 was given 5 g of ferrous sulphate daily;
group 2 received 5000 μg (5 mg) of folic acid daily;
group 3 received 5 g of ferrous sulphate and 5000 μg (5 mg) of folic acid daily. All participants were given 3 multivitamin tablets daily containing vitamin A, vitamin B, C and D. The study was not randomised. |
| Metz 1965 | 355 Bantu and white pregnant women attending antenatal clinics at the Baragwanath and South Rand Hospitals, Johannesburg, South Africa were allocated by random numbers to 1 of 3 groups:
group 1 received 200 mg of iron by mouth;
group 2 received 5000 μg (5 mg) of folic acid daily by mouth in addition to the iron;
group 3 received 50 μg of vitamin B12 by mouth in addition to the folic acid and iron. In the white participants, supplementation was started after the 24th week while Bantu participants started after the 28th. Both groups received iron. The type of comparisons are outside the scope of this review, |
| Milman 2005 | 427 healthy Danish pregnant women living in the northeastern part of Copenhagen County, Denmark were randomly allocated to receive iron (as ferrous fumarate) in daily doses of 20 mg (n = 105), 40 mg (n = 108), 60 mg (n = 106), and 80 mg (n = 108) from 18 weeks of gestation. Hb, serum ferritin, and serum soluble transferrin receptor concentrations were measured at 18 weeks (inclusion), 32 weeks, and 39 weeks of gestation and 8 weeks postpartum. All women received iron daily. No comparisons allowed within the scope of this review. |
| Milman 2014 | 80 healthy ethnic Danish pregnant women, urban and rural residents attending the antenatal care clinic, were allocated in 2 groups to compare the effects of oral ferrous bisglycinate 25 mg iron/day vs ferrous sulphate 50 mg iron/day. Women were allocated to ferrous bisglycinate 25 mg elemental iron (Aminojern®) (n = 40) or ferrous sulphate 50 mg elemental iron (n = 40) from 15 to 19 weeks of gestation to delivery. Haematological status (Hb, red blood cell indices) and iron status (plasma iron, plasma transferrin, plasma transferrin saturation, and plasma ferritin) were measured at 15‐19 weeks (baseline), 27‐28 weeks and 36‐37 weeks of gestation. The study was excluded because both study groups received iron. This type of comparison is outside the scope of this review. |
| Mitra 2012 | 959 low‐income postpartum girls and women aged 13 years and older, between 2 and 6 weeks after delivery, and certified for WIC from 11 clinics selected the Mississippi Primary Health Care Association and the Mississippi Department of Health, in Mississippi, United States of America. The clinics were randomised to 1 of 3 groups:
group 1 (n = 364, 4 clinics) women received universal anaemia screening and treatment of anaemic women as iron supplement containing 65 mg of elemental Fe (as 325 mg ferrous sulphate);
group 2, (n = 348, 3 clinics) received universal iron supplements daily containing 65 mg of elemental Fe (as 325 mg ferrous sulphate) for 2 months to all low‐income women;
group 3, (n = 247, 4 clinics) only women at high risk and diagnosis of anaemia were treated iron supplement containing 65 mg of elemental Fe (as 325 mg ferrous sulphate (control). Supplements were provided free of charge to the women in the control group. All study participants within each clinic received the same treatment. Women were followed up at 6 months after delivery. Hb was measured at baseline and at follow‐up. The primary outcome variable was the proportion of women with anaemia after treatment. The participants were post partum women. The type of participants is outside the scope of this review. |
| Morgan 1961 | 356 pregnant women attending 2 different antenatal care clinics at the King Edward Memorial Hospital for Women in Subiaco, Australia received according to the clinic they visited, either no treatment or 100 mg of elemental iron (as ferrous gluconate) daily. No systematic allocation was used in this open trial. |
| Morrison 1977 | 105 pregnant women attending the University Unit, Mater Misericordiae Mothers' Hospital, South Brisbane, Australia, with normal height, weight and nutrition for the Australian population and with no previous adverse medical, surgical or obstetrical history were allotted by random selection to 1 of 4 types of supplements:
group 1 received 50 mg of elemental iron (as dried ferrous sulphate) daily;
group 2 received 80 mg elemental iron (as dried ferrous sulphate) with 300 μg (0.3 mg) folic acid daily;
group 3 received 105 mg elemental iron (as ferrous sulphate);
group 4 received 105 mg of elemental iron (as ferrous sulphate) with 300 μg (0.3 mg) of folic acid. All groups received iron daily. No comparisons allowed within the scope of this review. |
| Mukhopadhyay 2004 | 111 apparently healthy pregnant women with less than 20 weeks and no prior intake of iron supplements during this pregnancy with Hb equal or higher than 100 g/L and singleton pregnancy in New Delhi, India were randomly assigned to 1 of 2 groups:
group 1 received 2 tablets of 100 mg elemental iron and 500 μg (0.5 mg) folic acid each (total 200 mg elemental iron and 1000 μg (1 mg) folic acid, to be taken only once a week, 1 tablet before lunch and another tablet before dinner;
group 2 received 1 tablet of 100 mg elemental iron and 500 μg (0.5 mg) folic acid daily. Women were advised to take the supplements 30 minutes before the meals and not with tea, coffee or milk. Also, women were advised to take calcium supplements after meals (500 mg elemental calcium twice daily). Iron supplementation started between 14 and 20 weeks until delivery. Deworming, if required, was carried out with Mebendazole 100 mg twice a day for 3 days in the second trimester. Both groups received iron and folic acid in different regimens (daily versus weekly). |
| Mumtaz 2000 | 191 anaemic pregnant women between the ages of 17‐35 years of age, and uneventful obstetric history attending the Maternity wing of the Federal Government Services Hospital in Islamabad and the Maternal & Child Health Clinic at the Christian Mission Hospital in Taxila, Pakistan were randomly assigned to 1 of 2 interventions:
group 1 received 40 mg elemental iron (as ferrous sulphate) with 1000 μg (1 mg) of folic acid once daily;
group 2 received 40 mg elemental iron (as ferrous sulphate) with 1000 μg (1 mg) of folic acid on 2 days of the week and placebo the rest of the days. Participants and care providers were blinded to the treatments. Outcomes measured included Hb concentration and serum ferritin at baseline and during the 3 following consecutive visits as well as compliance and weight. Change in Hb Z‐scores after supplementation was the main outcome variable, in women from different gestational ages and duration of intervention. Both groups received iron and folic acid in different regimens (daily versus bi‐weekly). |
| Nguyen 2008 | 167 pregnant women with less than 20 weeks of gestation who called either Motherisk General Information line or the Motherisk Nausea and Vomiting of Pregnancy (NVP) Helpline (Hospital for Sick Children, Toronto) and had not started taking or had discontinued any multivitamin due to adverse events were randomly assigned to 1 of 2 groups:
group 1 were provided, a small‐size supplement (PregVit®), containing 35 mg elemental iron (as ferrous fumarate) and multivitamins;
group 2 who received high iron content, small size supplement (Orifer F®) containing 60 mg elemental iron (as ferrous sulphate) and multivitamins. Follow‐up interviews documented pill intake and adverse events. Participants from both groups received iron in different amounts and compounds. |
| Nogueira 2002 | 74 low‐income pregnant adolescents ranging from 13‐18 years of age attending antenatal care at the Evangelina Rosa Maternity Hospital in Teresina, Piaui State, Brazil were distributed into 5 groups:
group 1 received 120 mg elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) of folic acid daily;
group 2 received 80 mg elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) folic acid daily;
group 3 received 120 mg of elemental iron, with 5 mg of zinc sulphate and 250 μg (0.25 mg) of folic acid daily;
group 4 received 80 mg of elemental iron (as ferrous sulphate), with 5 mg of zinc sulphate and 250 μg (0.25 mg) of folic acid daily; group 5 received 120 mg elemental iron (as ferrous sulphate, routine regime locally). All groups received iron and 2 groups received zinc in addition to iron and folic acid. No comparisons allowed within the scope of this review. |
| Ogunbode 1984 | 80 apparently healthy non‐anaemic pregnant women attending University College Hospital and Inalende Maternity Hospital in Ibadan, Nigeria during the first and second trimesters of pregnancy were randomly allocated to 1 of 2 groups:
group 1 (n = 39) received 1 tablet Ferrograd Folic 500 Plus® daily, a sustained‐released formulation containing ferrous sulphate and folic acid (composition is not available);
group 2 (n = 41) received a capsule containing 200 mg ferrous sulphate and 5000 μg (5 mg) of folic acid.
All patients were also provided 25 mg weekly of pyrimethamine throughout pregnancy as an anti‐malarial agent. Patients who became anaemic during pregnancy were excluded from the study and analysis. Outcomes measured included reticulocyte count, HCT, anaemia, and side effects. Both groups received iron and folic acid supplements, thus making the comparisons not suitable for this review. |
| Ogunbode 1992 | 315 apparently healthy pregnant women attending 4 prenatal care clinics in 4 geographical areas of Nigeria with mild to moderate anaemia (as defined by HCT between 26% to 34%) and 18‐28 weeks of gestation, single pregnancies, no complications and who consented to participate in the study were randomly allocated to 1 of 2 groups:
group 1 (n = 159) received 1 daily capsule of a multiple micronutrient supplement Chemiron® containing 300 mg of ferrous fumarate, 5000 μg (5 mg) folic acid, 10 μg vitamin B12, 25 mg of vitamin C, 0.3 mg magnesium sulphate and 0.3 mg of zinc sulphate;
group 2 (n = 156) received a capsule containing 200 mg ferrous sulphate and 5000 μg (5 mg) of folic acid. All patients were also provided 600 mg of chloroquine to be taken under supervision and 25 mg weekly of pyrimethamine throughout pregnancy. Patients who became anaemic during pregnancy were excluded of the study and analysis. Outcomes measured included blood Hb, anaemia, HCT, serum ferritin levels, side effects. A second published study followed these same women and their infants. Both groups received iron and folic acid supplements, thus making the comparisons not suitable for this review. |
| Ortega‐Soler 1998 | 41 healthy pregnant women, attending prenatal care clinics at Hospital Diego Paroissien in La Matanza, Province of Buenos Aires, Argentina with serum ferritin below 50 mg/mL were assigned to 1 of 2 groups:
group 1 received 100 mg of elemental iron daily (as ferric maltosate);
group 2 received no treatment.
Supplementation started at 21 +/‐ 7 weeks of gestation until birth. Maternal outcomes measured included: Hb, erythrocyte protoporphyrin, serum ferritin at baseline and term, dietary intake. The iron intake was unsupervised and compliance was not reported. The trial is not randomised nor quasi‐randomised so it does not fill the inclusion criteria for this review. |
| Osifo 1970 | 52 pregnant women 18‐40 years of age with 15‐22 weeks of gestation attending routine prenatal care in the village of Osegere, Nigeria with no complications were divided into 3 groups based on the day of the week convenient to them to attend the weekly clinic:
group 1 received iron supplements (200 mg ferrous sulphate) 3 times a day;
group 2 received iron supplements (200 mg ferrous sulphate) 3 times a day plus a tablet containing 5000 µg (5 mg) folic acid daily;
group 3 received iron supplements (200 mg ferrous sulphate) 3 times a day plus a tablet containing 5000 µg (5 mg) folic acid daily and 800 mg of cholorique sulphate (Nivaquine; May & Baker Ltd, Dagenham, Essex) at first and 25 mg of pyrimethamine (Daraprim; Burroughs Wellcome, 10 Lancaster Onike Road, Yaba, Lagos, Nigeria) weekly. Blood samples were collected each week and assessed for Hb and HCT concentrations. The study is not randomised and all the women received iron supplements. The type of study design and the type of interventions are outside the scope of this review. |
| Osrin 2005 | 1200 healthy pregnant women with a singleton pregnancy and less than 20 weeks' gestation attending an antenatal clinic at Janakpur zonal hospital in Nepal, were randomly assigned to receive routine 60 mg elemental iron daily and 400 μg (0.4 mg) folic acid supplements or a multiple micronutrient supplement containing 15 vitamins and minerals including 30 mg elemental iron and 400 μg (0.4 mg) folic acid. Both groups received iron and folic acid. No comparisons allowed within the scope of this review. |
| Parkkali 2013 | 4326 non‐high risk pregnant women 18 years of age or older attending prenatal care consultation at the 2 health centres (1° de Maio and Machava) in Maputo, Mozambique, a setting of endemic malaria and high prevalence of HIV. In this pragmatic randomised controlled trial to compare 2 iron administration policies were evaluated. Participants randomly allocated to 1 of 2 groups:
group 1 (n = 2184) received routine iron 60 mg (as ferrous sulphate) and 400 μg (0.4 mg) of folic acid daily throughout pregnancy;
group 2 (n = 2142) were assigned to the selective intervention (i.e, regular screening for Hb level and treatment for anaemia only after diagnosis) where they were screened and treated for anaemia and daily intake of 1000 µg (1 mg) of folic acid). In group 2 (selective iron group), women’s Hb levels were measured at each visit by the study nurses using a rapid Hb measure, HemoCue Hb 201+, (Hemocue AB, Ängelholm, Sweden). If the Hb was 90 g/L or more, they received 30 tablets of 1000 µg (1 mg) of folic acid per day. If their Hb was below the cut‐off of < 90 g/L Hb, they received a monthly double dose of iron (60 mg + 60 mg) for the treatment of anaemia. The usual care recommendations at the time of the trial included daily 60 mg elemental iron + 400 μg folic acid) throughout pregnancy; 1 dose of mebendazol 500 mg for intestinal parasite; 3 doses of sulphadoxine pyrimethamine for malaria prophylaxis (started around 20 weeks' gestation, or when quickening occurs or when the fetal heart is heard); Hb measurement (Lovibond is routinely used) and syphilis screening at the first prenatal visit and 3 doses of tetanus vaccine (at the fifth and seventh months and at delivery). Women received different doses of iron and folic acid. The comparisons in this study are outside the scope of this review. |
| Payne 1968 | 200 pregnant women attending antenatal clinics in Glasgow, Scotland with less than 20 weeks' gestation, whose antenatal care was undertaken wholly by the hospital antenatal clinic and who subsequently had a normal delivery, were randomly allocated to receive 200 mg of ferrous sulphate daily or 200 mg of ferrous sulphate with 1700 μg (1.7 mg) of folic acid daily throughout pregnancy. Both groups received iron. No comparisons allowed within the scope of this review. |
| Peña‐Rosas 2003 | 116 pregnant women of 10‐30 week of gestational age attended antenatal care clinics in Trujillo, Venezuela were randomly allocated to receive a 120 mg oral dose of iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid weekly (n = 52) or 60 mg elemental iron (as ferrous sulphate) and 250 μg (0.25 mg) folic acid and a placebo twice weekly (n = 44). Hb, HCT, serum ferritin and transferrin saturation were estimated at baseline and at 36‐39 week of gestation. All groups received iron and folic acid in 2 intermittent regimens with no control group. No comparisons allowed within the scope of this review. |
| Picha 1975 | In a randomised double‐blind study the new effervescent iron tablet Loesferron® was tested in 57 postpartum women. The participants were not pregnant women. |
| Pita Martin 1999 | 203 healthy pregnant women with normal blood pressure at first visit, attending antenatal care clinic at Diego Paroissien Hospitalin the Province of Buenos Aires, Argentina were included in the study, but in this review only 41 women who were randomised and completed the study were included in the analysis. Participants were assigned to 1 of 3 groups:
group 1 received 60 mg of elemental iron (as ferrous fumarate) daily;
group 2 received 60 mg elemental iron (as ferrous fumarate) every 3 days;
group 3 received no treatment. Supplementation started at 8‐28 weeks until 34‐37 weeks of gestation. Outcomes: maternal: Hb, HCT, erythroporphyrin, serum ferritin concentration at baseline and at 34‐37 weeks' gestation, premature delivery, birthweight. Unsupervised. Compliance not reported. Women from control group (group 3) were not assigned randomly. These women were recruited but due to delays in the acquisition of the iron tablets and the progression of their pregnancies without supplementation they were left as controls in the study. |
| Powers 1985 | 81 pregnant 14‐36 weeks of gestation or lactating (1‐20 months postpartum) women with Hb less than 140 g/L living in a village in The Gambia were allocated to 1 of 4 groups:
group 1 received daily placebo;
group 2 received 5 mg riboflavin;
group 3 received 30 mg ferrous sulphate;
group 4 received 30 mg ferrous sulphate + 5 mg riboflavin. At the beginning of the study and at 3 and 6 weeks thereafter women were examined clinically and blood samples collected for haematological and biochemical measurements. This is not a randomised trial. |
| Quintero 2004 | 107 healthy pregnant women with 6‐20 weeks of gestation who had not received iron supplements during the current pregnancy attending 19 health units in the State of Morelos, Mexico were randomly assigned by block pairs to receive either 120 mg of elemental iron (as ferrous sulphate) in a single dose daily or once weekly. Hb concentration, prevalence of anaemia and nutrient consumption at baseline and after 10 weeks of supplementation were measured. Both groups received iron in different regimens (daily versus weekly). Gestational ages were variable among the participants. |
| Rae 1970 | In this quasi‐randomised trial, pregnant women attending antenatal clinic at the Department of Obstetrics and Department of Haematology, Walton Hospital, Liverpool, United Kingdom were assigned to 1 of 2 groups:
group 1 received 200 mg ferrous gluconate 3 times a day throughout pregnancy;
group 2 received 200 mg ferrous gluconate + 5000 μg (5 mg) 3 times a day. Both groups received iron daily. The type of comparison is outside of the scope of this review. |
| Ramakrishnan 2003 | 873 pregnant women living near Cuernavaca, Morelos, Mexico with less than 13 weeks of gestation who did not use micronutrient supplements were randomly assigned to receive a daily multiple micronutrient supplement or a daily iron‐only supplement. Both supplements contained 60 mg of elemental iron (as ferrous sulphate). Supplement intake was supervised by trained workers from registration until delivery by home visits 6 days a week. No comparison allowed within the scope of this review. |
| Rayado 1997 | 394 healthy non‐anaemic adult pregnant women with 24‐32 weeks of gestation and singleton pregnancy from Fuentalabra, Spain were randomly assigned to 1 of 2 groups:
group 1 received 40 mg of elemental iron (as iron mannitol albumin) daily;
group 2 received 40 mg elemental iron (as iron protein succinylate) daily. Both groups received iron daily. No comparisons allowed within the scope of this review. |
| Reddaiah 1989 | 110 pregnant women attending the antenatal clinic at Comprehensive Rura Health Services Project Hospital, Ballabgarh, India, with 16‐24 weeks of gestation were randomly assigned to 1 of 3 groups:
group 1 received 60 mg elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid daily;
group 2 received 120 mg elemental iron (as ferrous sulphate) with 500 μg (0.5 mg) of folic acid daily;
group 3 received 240 mg elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) of folic acid daily. All groups received iron daily. No comparisons allowed within the scope of this review. |
| Ridwan 1996 | 176 pregnant women with 8‐24 weeks of gestation attending antenatal care at 6 health centres in West Java, Indonesia. Health centres were randomised to 1 of 2 interventions: weekly regimen, where women received 120 mg of elemental iron (as ferrous sulphate) with 500 μg (0.5 mg) of folic acid; or daily regimen where women received 60 mg of elemental iron (as ferrous sulphate) with 250 μg (0.25 mg) of folic acid daily until week 28‐32 of gestation. Supplementation started at 8‐24 weeks until 28‐32 weeks of gestation. Both groups received iron in different regimens. |
| Robinson 1998 | 680 pregnant women served by 11 health centres from 5 sub‐districts on or near the western end of the island of Seram in the Province of Maluku, Indonesia were assigned to 1 of 2 interventions:
group 1 received 60 mg of elemental iron (as ferrous sulphate) with 250 μg (0.25 mg) of folic acid daily by a traditional birth attendant;
group 2 received 120 mg of elemental iron (as ferrous sulphate) with 500 μg (0.5 mg) of folic acid once a week by the traditional home visiting birth attendants. A control group was formed by participants receiving traditional iron supplements (60 mg elemental iron) with folic acid from health centres, self‐administered without incentive. Groups 1 and 2 both received iron in different regimens. The control group was not assigned the traditional iron supplement. |
| Rolschau 1979 | 36 pregnant women were selected consecutively, paired 2 and 2, and allotted to 2 groups, 1 of which was supplied daily with 5000 ug (5 mg) folic acid, and the second with tablets without folic acid, from the 23rd week of pregnancy. The type of comparison is outside the scope of this review. |
| Roth 1980 | 23 pregnant women were assigned to 1 of 2 groups during August 1976 and September 1977: group 1 (n = 11) received a supplement daily 'Tardyferon‐Fol ®" containing 80 mg ferrous sulphate and 350 ug (0.35 mg) folic acid; group 2 (n = 12) received a supplement daily' Tardyferon®" containing 80 mg ferrous sulphate. Both groups received iron. The type of intervention is outside the scope of this review. |
| Roztocil 1994 | 84 non‐anaemic pregnant women at Mazarik University Brno in Czech Republic were treated from 20‐24 weeks with 1 capsule of Actiferrin Compositum®, and from 36 weeks to delivery with 2 capsules. The group was compared with 57 non‐anaemic pregnant women who received no supplements. The supplement contained 34.5 mg of elemental iron (as ferrous sulphate), 500 μg (0.5 mg) of folic acid, and 0.3 mg of cyanocobalamin. This is not a randomised trial. No comparisons allowed within the scope of this review. |
| Rukhsana 2006 | 90 pregnant women attending the Department of Obstetrics and Gynaecology Jinnah Postgraduate Medical Centre Karachi, with clinical sings of anaemia (Hb < 110 g/L) were randomly assigned to 1 of 3 supplementation groups (30 women in each group):
group 1 received 60 mg iron/daily;
group 2 60 mg iron/once a week;
group 3 120 mg iron/once a week for 12 weeks.
Hb, RBC count, red cell indices and reticulocyte count were measured and results compared to baseline to 12 weeks and between groups. The study was excluded because there were 3 groups receiving iron, 1 group daily and the other 2 intermittently. This type of comparison is outside the scope of this review. |
| Rybo 1971 | 117 pregnant women between 20‐29 weeks of gestation were alternatively assigned during 3 consecutive 2 weeks periods to receive daily tablets containing 200 mg of elemental iron (as ferrous sulphate), 200 mg of elemental iron (as a sustained released iron) or placebo. After each 2‐week treatment period women were questioned about possible side effects. No side effects are reported by group assigned. No comparisons are allowed within the scope of this review. |
| Sachdeva 1993 | In this study carried out in rural India 66 pregnant women from low‐ and middle‐income groups received nutritional supplements. Women in both groups received both iron and folic acid supplements. In addition, women in the experimental group received a calcium supplement, individual and group counselling and a booklet about nutrition in pregnancy. All women received iron and folic acid supplements (the dose and regimen were not clear) and it was not clear that allocation to groups was random. |
| Saha 2007 | 100 pregnant women aged 20‐40 years at 14 to 27 weeks' gestation, with Hb < 90 g/L, and serum ferritin < 12 μg/L, attending the Department of Pharmacology and the Department of Obstetrics and Gynaecology at the Postgraduate Institute of Medical Education and Research, Chandigarh, India were randomly assigned to 1 of 2 groups:
group 1 received 100 mg elemental iron (as iron polymaltose complex) and 500 μg (0.5 mg) folic acid daily;
group 2 received 120 mg elemental iron (as ferrous sulphate) and 500 μg (0.5 mg) folic acid daily for 8 weeks. Both groups received iron and folic acid. No comparisons can be made within the scope of this review. |
| Sandstad 2003 | 233 pregnant women attending their second antenatal care visit at the University Health Services of Oslo, Norway with serum ferritin concentration < 60 μg/L were randomised to 2 different iron preparations:
group 1 received 1 tablet containing 60 mg of elemental iron (as ferrous sulphate) daily;
group 2 received 3 tablets each containing 1.2 mg of heme iron from porcine blood plus 8 mg of elemental iron (as ferrous fumarate) per tablet (total 3.6 heme iron and 24 mg elemental iron) daily.
A third group (n = 93) of pregnant women who had been given advice to take or not the iron supplements according to the centre recommendations were enrolled in the trial at 6 weeks postpartum and served as control. The study groups were not randomised to the interventions and no comparisons can be made within the scope of this review. |
| Schoorl 2012 | 25 pregnant women in the third trimester of pregnancy with suspected IDE during pregnancy (Hb ≤ 110g/L, Ret‐He < 29.6 pg, zinc protoporphyrin > 75 mol/mol hem) participated in the study, receiving ferrous fumarate (200 mg 2 times a day, approx. 200 mg iron a day) according to local practice during 4 weeks. From the first trimester of pregnancy, 400 ug of folic acid was given as supplement in a multivitamin tablet (Centrum® Materna). Blood samples were drawn to establish haemocytometric parameters to evaluate RBC and reticulocyte Hb content. The study was excluded because there was a single group of women receiving iron during the third trimester of pregnancy without control, placebo or other intervention groups. There was not randomisation. This type of interventions is outside the scope of this review. |
| Seck 2008 | 221 apparently healthy pregnant women, had not used iron supplements prior to enrolment, who were 12 to 16 weeks were recruited from 6 health centres in Dakar, Senegal during their first prenatal visit, and randomly assigned to receive either a prescription to purchase iron/folic acid tablets to be taken daily, according to official policy, or to receive free tablets. Compliance was assessed 20 weeks after enrolment through interviews and pill count. All women received iron. No comparisons allowed within the scope of this review. |
| Shatrugna 1999 | 115 healthy pregnant women with 20‐28 weeks of gestation attending the antenatal clinic of the National Institute of Nutrition, Government Maternity Hospital, India were randomly assigned to 1 of 11 different formulations and doses of iron and then undergo iron tolerance tests. They received ferrous sulphate tablets containing 60 mg, 12 mg, and 180 mg of elemental iron; formulations containing 60 mg of elemental iron as pure ferrous sulphate salt, ferrous fumarate tablets, ferrous fumarate syrup, excipients added to pure ferrous sulphate salts; powdered ferrous sulphate tablets, iron tablets distributed by the National Nutritional Anaemia Prophylaxis Programme and pure ferrous salt in gelatin capsules. All women received iron. No comparisons allowed within the scope of this review. |
| Sinha 2011 | 50 pregnant women between 16‐20 weeks of gestation with Hb equal or greater than 100 g/L in Allahabad, in the north Indian state of Uttar Pradesh, India were randomly assigned to 1 of 2 groups: group 1 (n = 22): women received 2 doses of 400 mg iron sucrose infusion, 1 at 16‐20 weeks' gestation and a second infusion at 28‐32 weeks' gestation; group 2 (n = 28): women received 100 mg oral ferrous ascorbate daily starting at 16‐20 weeks' gestation. The type of intervention is outside the scope of this review. |
| Sjostedt 1977 | 300 pregnant women attending the Maternity Welfare Center, in Oulu, Finland before the 5th month of pregnancy were randomly assigned to 1 of 3 groups:
group 1 received 100 mg of elemental iron (as sustained‐release tablets) daily;
group 2 received 200 mg of elemental iron daily (as sustained‐release tablets);
group 3 received 200 mg of elemental iron daily (as rapidly disintegrating ferrous sulphate tablets). All groups received iron in different doses and formulations. |
| Sood 1979 | 151 healthy pregnant women with Hb > 50 g/L who had not received iron supplements during the last 6 months from Delhi and Vellore, India were divided in 1 of 3 strata according to Hb concentration (50‐79 g/L; 80‐109 g/L;110 g/L and above) and within each strata were allocated randomly to 1 of 5 interventions:
group 1 received 120 mg of elemental iron (as ferrous sulphate) 6 days a week;
group 2 received 100 mg of elemental iron (as iron dextran complex) intramuscular twice per week;
group 3 received iron as group 1 + pteroylmonoglutamic acid 5 mg/d 6 days a week + cyanocobalamin 100 μg intramuscular once per 14 d; group 4 received 100 mg of elemental iron intramuscular + pteroylmonoglutamic acid + cyanocobalamin 100 μg intramuscular;
group 5 received iron dextran complex intramuscular in a single total dose infusion + 5 mg/d pteroylmonoglutamic acid + 100 μg intramuscular cyanocobalamin once per 14 days. All groups received iron at different doses and routes. No comparisons allowed within the scope of this review. |
| Srisupandit 1983 | 567 pregnant women 16‐30 years of age with 18‐26 weeks' gestation attending antenatal care clinic, in the department of Obstetrics and Gynecology of the Siriraj Hospital, Thailand were randomly assigned to 1 of 3 groups; group 1 received 60 mg elemental iron daily; group 2 received 180 mg elemental iron daily; group 3 received 180 mg elemental iron and 5000 ug (5 mg) folic acid daily. The intervention lasted 3 months. THere were 101 losses to follow‐up. All participants received iron. The type of interventions is outside the scope of this review. |
| Steer 1992 | Trial abandoned. No data available. |
| Stone 1975 | 248 healthy pregnant women attending hospital antenatal clinic in London, England, were allocated randomly to receive 105 mg of elemental iron (as ferrous sulphate slow release dose) and 350 μg (0.35 mg) of folic acid daily or 80 mg of elemental iron (as ferrous fumarate) and 400 μg (0.4 mg) of folic acid daily in a standard preparation. Both groups received iron in different doses and preparations. No comparisons allowed within the scope of this review. |
| Swain 2011 | 100 women with uncomplicated pregnancy were assigned to received either injectable iron sucrose (400 mg diluted in 400 mL of normal saline) over 2‐3 hours or to receive oral dose of 100 mg elemental iron daily. The interventions in this trial are outside of the scope of this review. |
| Tampakoudis 1996 | 82 pregnant women with Hb concentrations 140 g/L or above attending clinic in Thessaloniki, Greece were randomised to receive 80 mg iron protein succinylate daily or a placebo. Serial Hb, HCT and serum erythropoietin were measured from maternal blood and cord blood on delivery; serum ferritin measured in frequent intervals. Abstract only available. Insufficient information to assess characteristics of the trial. |
| Tan 1995 | 285 healthy middle‐class pregnant women with Hb concentration above 100 g/L attending antenatal clinic at the University Hospital at Kuala Lumpur, Malaysia were assigned to receive daily iron supplements or no treatment. Abstract only available. No additional information was available, including doses, regimens or any other characteristics of the trial. |
| Tange 1993 | 128 anaemic and non‐anaemic pregnant females aged 10‐19 years old, with an average gestation of 16 weeks, were grouped for 3 levels of iron supplementation:
group 1 (n = 42 non‐anaemic participants) received placebo (no iron);
group 2 (n = 41 anaemic and non‐anaemic participants) received 22 mg of elemental iron daily;
group 3 (n = 45 anaemic and non‐anaemic participants) received 55 mg elemental iron daily. Women were supplemented from 16 weeks until delivery. Outcomes assessed included Hb, HCT, RBC count, MCV, serum iron, serum transferring and serum, ferritin measured every 4 weeks. The study is not reported as randomised and is excluded in the first screening for eligibility. |
| Thane‐Toe 1982 | 135 healthy pregnant women between 22‐28 weeks of gestation attending antenatal clinic in Burma, were randomly assigned to receive a daily dose of 60 mg, 120 mg or 240 mg of elemental iron (as ferrous sulphate). A control group was composed by 47 apparently healthy adults (17 males and 30 single women). Control groups are not appropriate. No comparisons allowed within the scope of this review. |
| Thomsen 1993 | 52 healthy non‐anaemic nulliparous women with normal singleton pregnancy and serum ferritin levels above 15 mg/L at 16th week in Herlev, Denmark were randomly assigned to receive either a daily tablet containing 18 mg elemental iron or a daily tablet containing 100 mg of elemental iron from 16 weeks until delivery. All women received 300 μg (0.3 mg) of folic acid daily. All women received iron in different doses. No comparisons allowed within the scope of this review. |
| Trigg 1976 | 158 pregnant women seeking antenatal care with general practitioners in the former South‐east England Faculty of the Royal College of General Practitioners, in South England, United Kingdom were assigned to 1 of 2 groups: group 1 (n = 76) received 50 mg ferrous sulphate daily to 76 pregnant women was compared with giving ferrous sulphate 50 mg daily + 500 μg (0.5 mg) folic acid. After the first test, patients were randomly allocated to 1 of the 2 treatments which was either a minimum of 50 mg of ferrous sulphate daily or a minimum of 50 mg of ferrous sulphate plus 500 μg (0.5 mg) of folic acid daily, and afterwards allocation was in sequence. Both groups received iron. The type of comparison is not within the scope of this review. |
| Vogel 1963 | 191 consecutive pregnant when attending antenatal care clinics and at 32 weeks of gestation were divided in 2 groups by alternate allocation by clinic: group 1 received 140 mg of elemental iron daily (as ferrous gluconate) in 4 tablets; group 2 received 150 mg elemental iron daily (as ferrous glutamate) in 3 tablets. All women received iron in different dose and number of tablets. No comparisons allowed within the scope of this review. |
| Wali 2002 | 60 iron‐deficient anaemic pregnant women with the gestational age of 12‐34 weeks were randomly assigned to 1 of 3 groups:
group 1 (n = 15) received intravenous 500 mg of iron sucrose for storage;
group 2 (n = 20) received intravenous iron sucrose according to deficit calculated as per formula with 200 mg of iron was given for storage;
group 3 received intramuscular iron Sorbitol in the dose used as practice. All groups received iron intravenously or intramuscularly. |
| Weil 1977 | 29 attending a clinic at University of Basel, Switzerland between May and November 1976 with 20 weeks' gestation were randomly assigned in 1 of 2 groups: group 1 (n = 15) received 80 mg elemental iron slow release as ferrous sulphate (Tardyferon®); group 2 (n = 14) received 80 mg elemental iron slow release as ferrous sulphate + 350 μg (0.35 mg) folic acid (gino‐Tardyferon®) until term. Women who had already taken multiple micronutrient supplements containing folic acid were excluded from the study. Both groups received iron. The type of interventions is outside the scope of this review. |
| West 2014 | 28,516 pregnant women were provided supplements containing 15 micronutrients (14,374) or iron–folic acid alone (14,142), taken daily from early pregnancy to 12 weeks postpartum, to assess effects of antenatal multiple micronutrient vs iron–folic acid supplementation on 6‐month infant mortality and adverse birth outcomes. Surveillance included 127,282 women; 44,567 became pregnant and were included in the analysis and delivered 28,516 live‐born infants. Median gestation at enrolment was 9 weeks. The study was excluded because it was conceived to assess effects of antenatal multiple micronutrient vs iron–folic acid supplementation on 6‐month infant mortality and adverse birth outcomes and it is not possible to evaluate the role of iron alone on the proposed outcomes. This type of interventions is outside the scope of this review. |
| Willoughby 1966 | 350 consecutive pregnant women attending antenatal care clinic were allocated to 1 of 5 groups:
group 1 received no hematinic supplements;
group 2 received 105 mg of elemental iron daily (as iron chelate aminoates);
group 3 received 105 mg of elemental iron daily with 100 μg (0.1 mg) of folic acid;
group 4 received 105 mg of elemental iron daily with 300 μg (0.3 mg) of folic acid;
group 5 received 105 mg of elemental iron daily with 450 μg (0.45 mg) of folic acid. All women received a multivitamin preparation (Vivatel®) free of folic acid. This is not a randomised trial. |
| Willoughby 1968 | 68 pregnant women attending antenatal care clinic in Queen Mother's Hospital in Scotland, were randomly allocated to receive 195 mg of elemental iron alone daily or 195 mg of elemental iron in conjunction with 300 μg (0.3 mg) of folic acid daily. Both groups received iron. No comparisons allowed within the scope of this review. |
| Winichagoon 2003 | 484 healthy pregnant women with 13‐17 weeks of gestation who had not received iron supplements before enrolling in the study, and who had a Hb concentration > 80 g/L attending antenatal care clinics at the district hospital and 7 health centres from 54 villages in the Province of Khon‐Kaen in northeast Thailand. The villages were grouped according to size and then randomised in 4 clusters to 1 of 3 interventions: group 1 received a daily regimen providing 60 mg of elemental iron (as ferrous sulphate) with 250 μg (0.25 mg) of folic acid daily; group 2 received 120 mg of elemental iron with 3500 μg (3.5 mg) of folic acid once a week; group 3 received 180 mg of elemental iron (as ferrous sulphate) with 3500 μg (3.5 mg) of folic acid once a week. Supplementation started at 15 +/‐ 2 weeks until delivery. All groups receive iron in different regimens (weekly versus daily) or doses. No comparisons allowed within the scope of this review. |
| Wu 1998 | 369 pregnant women attending antenatal care at Beijing Hospital, China were divided into 2 groups according to their initial Hb concentrations. Women with Hb 110 g/L or above were randomly assigned to 1 of 2 groups:
group 1 (n = 96) received 1 daily tablet of maternal supplement containing 60 mg of elemental iron in addition to other micronutrients including calcium and magnesium;
group 2 (n = 95) served as control and received no supplements. Another group of women with Hb < 110 g/L (treatment group) were randomly assigned to 1 of 3 groups: group 1 received 1 tablet of maternal supplement daily; group 2 received 0.9 g of ferrous sulphate daily; group 3 received 1 tablet of Ferroids, a sustained released preparation daily. In the preventive group, women entered the study from 20‐24 gestational weeks. In the treatment groups, women less than 36 gestational weeks were accepted. No comparisons allowed within the scope of this review. This is not a randomised trial. |
| Yecta 2011 | 210 pregnant women with 17–20 weeks' gestation and singleton pregnancies, no known disease, and Hb levels higher than 110 g/L attending local public healthcare centres at 7 prenatal healthcare clinics between September 2007 and February 2009 in the urban regions of Urmia city North West Iran were randomly assigned to 1 of 3 groups:
group 1 (n = 70) received 2 iron supplementation tablets once weekly providing 100 mg elemental iron per week (as ferrous sulfate);
group 2 (n = 70) received 1 tablet twice weekly providing 100 mg elemental iron per week (as ferrous sulfate);
group 3 (n = 70) received 1 tablet daily containing 50 mg elemental iron per day (as ferrous sulfate). No additional micronutrients were supplied. Hb and serum ferritin levels were measured at 20, 28, and 38 weeks. Pregnancy and birth outcomes (pregnancy termination, method of delivery, birthweight, stillbirth) were reported. All participants received iron in different regimens. The type of interventions is outside the scope of this review. |
| Young 2000 | 413 healthy non‐severely anaemic pregnant women attending antenatal care at Ekwendeni Hospital or its mobile clinics in northern Malawi with less than 30 weeks of gestation at their first visit, stratified by initial Hb concentration before randomisation. Supplementation starting time variable (22.2 +/‐ 4.8 weeks) and ending time variable (32.2 +/‐ 4.4 weeks of gestation). Participants were randomly assigned within each anaemia grade category to 1 of 2 interventions:
group 1 received 120 mg of elemental iron (as ferrous sulphate) with 500 ?g (0.5 mg) of folic acid once a week;
group 2 received 60 mg of elemental iron (as ferrous sulphate) with 250 ?g (0.25 mg) of folic acid daily. Outcomes: maternal: Hb concentration at baseline and after 8 weeks of supplementation; compliance, presence of side effects, and prevalence of anaemia. All women received iron and folic acid in different regimens (daily versus weekly). No comparisons allowed within the scope of this review. |
| Young 2010 | This trial examines the relative differences in heme (animal‐based) and non‐heme (ferrous sulphate) iron utilisation in 20 non‐smoking, pregnant women (19 yeas or older; n = 10) and adolescents
(18 years of age or younger; n = 10) from the Strong Midwifery Group and the Rochester Adolescent Maternity Program in Rochester, NY, USA and 12 healthy, non‐smoking, non‐pregnant women ages 18–27 years recruited in 2009 from Ithaca, NY, USA. Women were randomly assigned to receive both an animal‐based heme meal (intrinsically labelled 58Fe pork) and labelled ferrous sulphate (57Fe) fed on alternate days. The type of design and the comparisons of this study are outside the scope of this review. |
| Yu 1998 | 51 healthy pregnant women with 18‐22 weeks of gestation who had not taken supplements or medication in the previous 6 months attending public health centre in Ulsan, South Korea were randomly assigned to 1 of 2 groups:
group 1 received 160 mg of elemental iron (as ferrous sulphate) in 1 intake once a week;
group 2 received 80 mg of elemental iron (as ferrous sulphate) daily. Women with low Hb were assigned by the trialists to daily regimen. Supplementation started at 20.1 weeks and 20.2 weeks of gestation for groups 1 and 2, respectively. Both groups receive iron in different regimens (weekly versus daily). No comparisons allowed within the scope of this review. |
| Zamani 2008 | 152 healthy, non‐anaemic pregnant women aged 18‐38 years, 15‐16 weeks’ gestation (gestation estimated by menstrual dates and ultrasound) attending 2 clinics for prenatal care in Isfahan, Iran. ("In Iran, it is mandatory to prescribe iron (1 tablet containing 45 mg elemental iron (as ferrous sulphate) per day) and folic acid supplements to pregnant women after the 15th‐ 18th week of gestation"). Exclusion criteria: current anaemia (Hb < 110 g/L), past history of anaemia, thalassaemia, or other blood disorders, history of previous obstetric problems (haemorrhage, pregnancy‐induced hypertension, diabetes) or any other chronic systemic disorder. Participants were assigned to 1 of 2 groups: group 1 (experimental group) received 2 tablets of 45 mg elemental iron (as ferrous sulphate) taken on a single day each week. “Women in the trial group were instructed to choose any day of the week and to take 2 tablets of 45 mg elemental iron (as ferrous sulphate) each on the same day every week, 1 in the morning and 1 before dinner” i.e. 90 mg of “elemental iron (as ferrous sulphate) 1 day per week in 2 takes”. (Supplied as 8 tablets every 4 weeks) for 16 weeks (from recruitment at 16‐18 weeks); group 2 (control group) were to take 1 tablet containing 45 mg elemental iron (as ferrous sulphate) daily for 16 weeks (from recruitment at 16‐18 weeks). Supplied as 28 tablets every 4 weeks. Both groups receive iron in different regimens (weekly versus daily). No comparisons allowed within the scope of this review. |
| Zhou 2009 | 180 anaemic women (Hb < 110 g/L) attending antenatal care at the Children, Youth and Women's Health Service, Adelaide, Australia with 24‐32 weeks of gestation and a singleton pregnancy. Women were excluded if they were taking iron or vitamins and minerals supplements, had presumptive diagnosis of non iron‐deficiency‐related anaemia, history of thalassaemia, drug or alcohol abuse and/or diabetes requiring insulin or a known fetal abnormality. Women were randomly assigned to receive a daily dose of 20, 40 or 80 mg of elemental iron (as ferrous sulphate) for 8 weeks or until birth. The primary outcomes measured were Hb levels, anaemia at the end of the intervention and gastrointestinal side effects during treatment. All women received iron at different doses. No comparisons allowed within the scope of this review. |
| Zutschi 2004 | 200 apparently pregnant women with 24‐26 weeks of gestation, with singleton pregnancy and moderate anaemia (Hb > 80 g/L and < 110 g/L) were randomly assigned to receive injectable iron‐sorbitol‐citrate in 3 intramuscular doses of 150 mg each at 4 weeks intervals or 100 mg of elemental iron daily. Hb concentrations were measured at baseline, every 4 weeks and at delivery. The study compares 2 routes of iron administration. Both groups receive iron. No comparisons allowed within the scope of this review. |
BMI: body mass index Fe: iron Hb: haemoglobin HCT: hematocrit (same as PCV: packed cell volume) IDE: iron‐deficient erythropoiesis IU: international units MCV: mean corpuscular (or cell) haemoglobin concentration RBC: red blood cell RDA: Recommended Dietary Allowance SES: socioeconomic status
Characteristics of studies awaiting assessment [ordered by study ID]
Parisi 2013.
| Methods | Randomised control trial with 4 arms. |
| Participants | 80 healthy non anaemic pregnant women (Hb less than 105 g/L) consecutively recruited at 12‐14 weeks of gestation in the Unit of Obstetrics and Gynecology, University of Milan, Italy. |
| Interventions | Participants were randomised to 1 of 4 groups: group 1: (n = 20) controls; group 2 (n = 20) received ferrous iron 30 mg daily; group 3 (n = 20) received liposomial iron 14 mg (SideralR Pharmanutra) daily; group 4 (n = 20) received liposomial iron 28 mg/daily. The supplementation continued until 6 weeks postpartum. |
| Outcomes | BMI, haemoglobin, ferritin, anaemia, placental weight, blood losses and gestational age at delivery, birthweight. |
| Notes | There is only an abstract available with very limited information. |
BMI: body mass index Hb: haemoglobin
Characteristics of ongoing studies [ordered by study ID]
Dibley 2012.
| Trial name or title | A trial to evaluate the impact of an early start to iron/folic acid supplementation in pregnancy on deaths of newborns in rural Bangladesh. |
| Methods | Community‐based cluster‐randomised controlled trial. The interventions will be assigned to eligible clusters using a fixed randomisation scheme with uniform allocation ratio of treatments, stratified by Sub‐Districts (upazilla) and in blocks of 5 or 10 to ensure geographic balance across each geographic area. The random allocation sequence will be generated using SAS software. |
| Participants | 32,000 pregnant women registered in the 202 study clusters trained by Bangladesh Rural Advancement Committee, an NGO based in Bangladesh. Exclusion criteria: 1) clusters on the sampling frame will be excluded if there are other interventions to improve antenatal iron/folic acid distribution currently being implemented either by government or non‐government sectors. 2) clusters located in areas where access is extremely difficult, for example, low land areas which are prone to flooding for extended periods of the year, will also be excluded. 3) cohort evaluation: pregnant women with more than 16 weeks of gestational age at enrolment will be excluded from ‘cohort’ follow‐up. |
| Interventions | Clusters will be assigned to 1 of 2 interventions: group 1: women in this group will receive a daily dose of 60 mg elemental iron + 400 μg (0.4 mg) folic acid supplementation early in pregnancy (in the first trimester) to be taken orally and sustained for at least 180 days, ensure resupply of supplements through fortnightly visits, and provide counselling in support of early uptake, continued use of the supplements until delivery, and compliance with the supplementation regimen; group 2: women receive standard treatment, the usual antenatal and postnatal care services provided by the Bangladesh Ministry of Health, which are supported by BRAC Essential Health Care Program. |
| Outcomes | Primary: infant deaths occurring in the first month of life assessed by the data collected by the trained research field worker visits. at 4 weeks and 6 weeks after delivery. Secondary: percentage of women using iron/folic acid as prescribed in the first trimester of pregnancy assessed by data collected by trained research field worker visits; percentage of live births with low birthweight (weighing < 2500 g) (intensive); percentage of live births with preterm delivery (intensive). Preterm delivery is defined as a birth occurring with gestational age before 37 weeks of gestation and includes early preterm delivery (< 34 weeks) based on maternal report of the date of last menstrual period; percentage of neonatal deaths attributable to preterm delivery asphyxia; percentage of neonatal deaths attributable to preterm delivery; mean marginal additional expenditure associated with early iron/folic acid supplementation, and the mean cost per neonatal death prevented referring to health service costs. |
| Starting date | Anticipated or actual date of first participant enrolment:1/12/2012. |
| Contact information | Dr Tanvir Huda CHNRI Secretariat Coordinator, Centre for Child and Adolescent Health, ICDDR,B; Mohakhali, Dhaka 1212 Bangladesh Phone: +880 2 9840523‐32/Ext. 3820 Email: thuda@icddrb.org Prof Michael Dibley Sydney School of Public Health, Room: 307A, Edward Ford Building (A27), University of Sydney, NSW 2006 Australia Phone: +61 2 9351 3620 and +61 2 9351 5049 E‐mail: michael.dibley@sydney.edu.au |
| Notes | Funded by the National Health & Medical Research Council of Australia. Primary sponsors: The University of Sydney, Australia and the International Centre for Diarrhoeal Disease Research, Bangladesh. Collaborator: Bangladesh Rural Advancement Committee (BRAC). |
Fawzi 2010.
| Trial name or title | Prenatal iron supplements: safety and efficacy in Tanzania. |
| Methods | Randomised clinical trial. |
| Participants | Inclusion criteria: ‐ at or before 19 weeks of gestation ‐ primigravida or secundigravidae ‐ not‐anaemic (defined as Hb < 85 g/L) ‐ not iron deficient (defined as serum ferritin < 12 µg/L) ‐ HIV‐uninfected ‐ intend to stay in Dar es Salaam until delivery and for at least 6 weeks thereafter. Exclusion criteria: ‐ after 19 weeks' gestation ‐ not primigravida or secundigravidae ‐ anaemic ‐ iron deficient ‐ HIV‐infected ‐ high iron stores at baseline (i.e. serum ferritin > 200 µg/L) ‐ do not intend to stay in Dar es Salaam until delivery and for at least 6 weeks thereafter. |
| Interventions | 60 mg elemental iron (as ferrous sulphate) versus placebo. |
| Outcomes | Primary: incidence of placental malaria (time frame: delivery); infant birthweight (time frame: delivery); maternal Hb (time frame: 20 weeks' gestation); maternal Hb (time frame: 30 weeks' gestation); maternal Hb (time frame: 6 weeks postpartum); maternal Hb (time frame: delivery); placental malaria parasite density (time frame: delivery). Secondary: low birthweight (time frame: delivery); maternal anaemia (time frame: 20 weeks' gestation); maternal anaemia (time frame: 30 weeks' gestation); maternal anaemia (time frame: 6 weeks postpartum); maternal anaemia (time frame: delivery); maternal malaria infection (time frame: 20 weeks' gestation); maternal malaria infection (time frame: 30 weeks' gestation); maternal malaria infection (time frame: 6 weeks postpartum); maternal malaria infection (time frame: delivery). |
| Starting date | June 2010. |
| Contact information | Wafaie W Fawzi, MD, DrPh Telephone: +1 617 432‐5299 Email: mina@hsph.harvard.edu Harvard School of Public Health Zul Premji, MD, MSC, PhD Muhimbili University of Health and Allied Sciences |
| Notes | Funded by Harvard School of Public Health and Muhimbili University of Health and Allied Sciences. |
Hamzehgardeshi 2009.
| Trial name or title | A randomised placebo‐controlled trial to determine the effect of iron supplementation on hematological indices in pregnant women with haemoglobin ≥13.2 g/dL. |
| Methods | A randomised, double‐blind, placebo‐controlled trial. |
| Participants | 87 pregnant women 17‐35 years of age, Hb more than or equal to 132 g/L and ferritin ≥ 143 g/L with 13‐18 weeks of gestation, body mass index (BMI) between 19.8 and 26 kg/m2 and singleton pregnancy. |
| Interventions | Participants will be randomly assigned to 1 of 2 groups: group 1 ferrous sulphate, 150 mg tablet with 50 mg ferrous elemental, daily, from 20th gestational week to the end of pregnancy and group 2 placebo tablets, 1 tablet daily, from 20th gestational week to the end of pregnancy. |
| Outcomes | Hb, HCT, MCV, MCH, MCHC, and RBCs were measured in 24‐28 and 32‐36 gestational weeks. |
| Starting date | March 20, 2002. |
| Contact information | Zeinab Hamzehgardeshi Tarbiat Modarres University, Tehran University of Medical Siences . 00981543246883 hamzeh@razi.ac.ir |
| Notes | Source of funding: Tarbiat Modarres University. |
Jafarbegloo 2010.
| Trial name or title | Gastrointestinal complications of iron supplement in pregnant women. |
| Methods | Double‐blind clinical trial with 2 arms. |
| Participants | 139 pregnant women with Hb higher than 132 g/L from the 20th week to the end of pregnancy. |
| Interventions | Participants are randomly assigned to 1 of 2 groups: group 1 (n = 88): 1 ferrous sulphate pill containing 50 mg elemental iron (as ferrous sulphate) daily; group 2 (n = 51): received 1 placebo tablet daily. Supplementation started from the 20th week to the end of pregnancy. |
| Outcomes | Side effects at 24th and 36th weeks of gestation. |
| Starting date | June 22, 2003. |
| Contact information | Esmat Jafarbegloo Qom university of medical sciences Shahre Qaem street‐ Nursing & Midwifery school Qom Iran, Islamic Republic Of Phone: 00982517225100 Fax: 00982517225888 jafarbegloo@muq.ac.ir |
| Notes | Source of funding: Researcher. |
Mwangi 2011.
| Trial name or title | A randomised trial to assess the safety and efficacy or iron supplementation in Kenyan pregnant women. |
| Methods | Randomised, placebo control double‐blind trial. |
| Participants | 470 pregnant women aged 15‐45 years, with gestational age < 23 weeks resident in the in Nyanza province, Kenya. Exclusion criteria includes failure to provide a blood sample, initial Hb concentration < 90 g/L, reported medical history suggestive of sickle cell anaemia, epilepsy, diabetes, obstetric history suggestive of eclampsia or pre‐eclampsia, obvious mental retardation or metabolic disorder, no written consent, carrying multiples, women planning to leave the homestead or to be absent for prolonged periods in the course of the pregnancy or within a 1‐month period thereafter, or women planning to deliver outside the research clinic. |
| Interventions | Participants will be randomly assigned to 1 of 2 groups: group 1 will receive daily supplementation with 60 mg elemental iron (as ferrous fumarate); group 2 will receive placebo. |
| Outcomes | Primary outcomes: maternal plasmodium infection at parturition as assessed by dipstick tests and PCR. Secondary outcomes: maternal iron status at 1‐month after delivery, neonatal iron stores at 1‐month of age as assessed by plasma ferritin concentration; and maternal intestinal pathogens at 1‐month after delivery. |
| Starting date | Starting date September 2011. Estimated study completion date: April 2013. |
| Contact information | Contact: Martin N Mwangi, MSc +254 734 018863 martinndegwa.mwangi@wur.nl Contact: Pauline EA Andang'o, PhD +254 728 485729 paulango@hotmail.com |
| Notes | Sponsors and collaborators: London School of Hygiene and Tropical Medicine; University of Nairobi; Maseno University, Kenya; Wageningen University. |
Ramakrishnan 2012.
| Trial name or title | Impact of pre‐pregnancy micronutrient supplementation on maternal and child outcomes. |
| Methods | 6 arms double‐blind randomised controlled trial. |
| Participants | Eligible and willing women of reproductive age (WRA) from rural Vietnam. |
| Interventions | Aproximately 5000 women of reproductive age will be randomly assigned to 1 of the following 3 groups of pre‐pregnancy weekly supplementation: 1) folic acid 2800 μg (control), 2) iron and folic acid (iron 60 mg, folic acid 2800 μg), and 3) multiple micronutrients (vitamin A 800 μg, 600 IU vitamin D, 10 mg vitamin E, 70 mg vitamin C, 1.4 mg thiamine, 1.4 mg riboflavin, 18 mgNiacin, 1.9 mg vitamin B6, 2.6 μg vitamin B12, 15 mg zinc, 2 mg copper, 65 μg selenium, 150 μg iodine + 2800 μg folic acid, 60 mg iron. Aproximately 1650 will become pregnant and will receive daily IFA during pregnancy. The mother‐infant pair will be follow to study anthropometrical and haematological parameters. |
| Outcomes | Key outcome measures will be 1) offspring's size and gestational age at birth 2) offspring's iron status at birth and 3 months of age and 3) maternal iron status at the beginning of pregnancy, 1 and 3 months postpartum. |
| Starting date | August 13, 2012. |
| Contact information | Usha Ramakrishnan |
| Notes | This project is a collaborative effort between Emory University, USA and Thainguyen University of Medicine and Pharmacy, Vietnam. Source of funding: Emory University, Micronutrient Initiative and The Mathile Institute for the Advancement of Human Nutrition This study is timely and responds to the WHO Global Expert Consultation (2007) which identified the need to evaluate the long term benefits of weekly IFA and MM supplementation in WRA. The findings will provide the necessary evidence to policy makers to recommend weekly MM or IFA supplements to WRA to improve birth outcomes. The central hypothesis is that pre‐pregnancy weekly IFA or MM supplementation followed by prenatal IFA and MM supplementation respectively, will improve birth outcomes as well as maternal and infant iron status compared to current practice of providing only prenatal IFA supplements. This hypothesis will be tested by conducting a randomised double‐blinded placebo‐controlled trial in Vietnam. |
Zhao 2014.
| Trial name or title | Impact of iron/folic acid vs folic acid supplements during pregnancy on maternal and child health. |
| Methods | 2‐arms double blind controlled trial. |
| Participants | 2367 pregnant women 18 years and older attending prenatal care clinic in 3 hospitals (Sanhe Maternity and Child Health Care Center, Sanhe General County Hospital, and Sanhe Hospital of Traditional Chinese Medicine) in Beijjing, China enrolled from June 2009 through December 2011 with uncomplicated singleton pregnancies and first prenatal visits at 20 weeks or less of gestation. |
| Interventions | Participants will be assigned to 1 of 2 groups: group 1 will receive 1 with placebo and 1 with 400 µg (0.4 mg) folic acid from enrolment to delivery; group 2: will receive 2 capsules per day: 1 with 60 mg elemental iron (as 300 mg ferrous sulphate and the other with 400 µg (0.4 mg) folic acid from enrolment to delivery. Participants received a 3‐month supply of each supplement upon enrolment and at the second study visit (26‐30 weeks). |
| Outcomes | iron status, pregnancy outcomes, including pregnancy and delivery complications, preterm rate, perinatal death rate, and birth rate, weight changes during pregnancy, and rates of pregnancy diabetes, pregnancy high blood pressure, fetus growth restriction, low birthweight, and fetal macrosomia. |
| Starting date | June 2009. |
| Contact information | Zhao Gengli, MD Peking University First Hospital Beijing, China |
| Notes | Data collection ended on December 2011 (Final data collection date for primary outcome measure). Funded by researcher and Vifor Inc (pharmaceutical company). |
IFA: iron and folic acid Hb: haemoglobin HCT: hematocrit (same as PCV: packed cell volume) MCH: mean cell haemoglobin MCHC: mean cell haemoglobin concentration MCV: mean cell volume MM: multiple micronutrient RBC: red blood cell PCR: polymerase chain reaction
Differences between protocol and review
This review updates Peña‐Rosas 2012. It includes two new trials and excluded one previously included study as it does not meet the inclusion criteria of this review.
Peña‐Rosas 2012 in turn updated part of Peña‐Rosas 2009 to only evaluate the effects of oral daily iron supplementation regimens. In the Peña‐Rosas 2012 update, we included 60 trials; 40 of these studies were included in the previous version of the review; but 10 had been excluded because they did not report outcomes of interest or the data reported were not extractable. In the Peña‐Rosas 2012 version, we included trials that complied with the eligibility criteria, even if there were no data extractable or did not report the outcomes of interest.
In a previous version of this review, daily and intermittent provision of iron supplements were included. This review, however, only focuses on daily iron supplementation. The effects of intermittent iron supplementation are addressed in a separate review (Peña‐Rosas 2012a).
Outcomes
Only pre‐specified primary and secondary outcomes are reported. The non pre‐specified outcomes that were included in previous versions were removed from this updated version and the overall number of haematological outcomes was reduced for clarity.
We have added a description of the lay health worker setting for each trial. We have included a timeframe for haematological variables: at or near term (34 weeks or more gestational age) in addition to at term (37 weeks or more of gestational age).
We have added the outcome 'congenital anomalies' instead of birth defects as this name reflects adequately a condition existing at birth and often before birth, which involves defects in or damage to a developing fetus.
A new search was conducted (2 July 2012) and the comparisons were changed to evaluate the effects of daily tablets containing iron (alone or with any other micronutrients) versus no iron; iron alone; iron and folic acid; as well as the additional effects of iron alone or iron and folic acid when given in addition to other micronutrients in pregnancy.
Methods
This review uses the latest Cochrane methodological guidance (Higgins 2011), particularly on:
the use of formal tests for subgroup analyses using random‐effects models;
the adjustment of cluster trials;
the inclusion of 'Summary of findings' tables to assess the overall quality of the evidence for primary outcomes.
For comparisons 1 and 2 we graded the evidence using the GRADE approach and included summary of findings tables; and so for these comparisons we did not carry out sensitivity analysis based on risk of bias as the grade summary provides a better summary of the overall quality of the evidence.
We included three additional subgroup analysis: by type of iron compound, iron compound release, and malaria setting.
Contributions of authors
Juan Pablo Peña‐Rosas wrote the initial protocol and first two versions of the review. Juan Pablo Peña‐Rosas abstracted the trial data and carried out the analysis. For this update Maria Nieves Garcia‐Casal and Therese Dowswell extracted the data from additional trials in the search, Luz Maria De‐Regil and Therese Dowswell produced the GRADE evidence profiles for the critical outcomes. Therese Dowswell wrote the description of the updated results and all authors contributed to the final preparation of this version.
Sources of support
Internal sources
-
Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, World Health Organization, Switzerland.
Juan Pablo Peña‐Rosas is a full time staff of the World Health Organization.
University of Liverpool, UK.
External sources
-
Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, World Health Organization, Switzerland.
Dr Maria Nieves Garcia‐Casal worked as a full‐time consultant for WHO during the preparation of this work.
-
NIHR NHS Cochrane Collaboration Programme, UK.
(TD 2012 update) was supported by the NIHR NHS Cochrane Collaboration Programme grant scheme award for NHS‐prioritised centrally‐managed, pregnancy and childbirth systematic reviews: CPGS 10/4001/02
-
The Bill & Melinda Gates Foundation, USA.
The World Health Organization gratefully acknowledges the financial contribution of The Bill &Melinda Gates Foundation towards the development of systematic reviews of the evidence on the effects of nutrition interventions.
Declarations of interest
We certify that we have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of the review (e.g. employment, consultancy, stock ownership, honoraria, expert testimony).
Juan Pablo Peña‐Rosas was author of an excluded study on iron and folic acid intermittent supplementation.
Luz Maria De‐Regil is full‐time staff member of the Micronutrient Initiative, an International Organization that delivers vitamin interventions to children, women of reproductive age and pregnant women, including iron and folic acid supplementation in eight countries in Africa and South East Asia.
Disclaimer: Juan Pablo Peña‐Rosas is currently a staff member of the World Health Organization. Maria Nieves Garcia‐Casal is a Consultant working for the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization.
Therese Dowswell's institution (the University of Liverpool) has received an NIHR Cochrane Programme Grant and Therese is currently employed on this project. As part of her role, Therese helps volunteer review teams prepare Cochrane reviews. This review is not part of that portfolio of reviews. In the last 36 months Therese has received funding from the WHO to work on other Cochrane reviews. The Funders have no influence on the content or conclusions of the reviews Therese works on.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Barton 1994 {published data only (unpublished sought but not used)}
- Barton DPJ, Joy MT, Lappin TRJ, Afrasiabi M, Morel JG, O'Riordan J, et al. Maternal erythropoietin in singleton pregnancies: a randomized trial on the effect of oral hematinic supplementation. American Journal of Obstetrics and Gynecology 1994;170:896‐901. [DOI] [PubMed] [Google Scholar]
- Murphy JF. Randomised double blind control trial of iron/placebo administration to pregnant women with high booking Hb concentrations (Hb>149/dl). Personal communication 1988.
Batu 1976 {published data only}
- Batu AT, Toe T, Pe H, Nyunt KK. A prophylactic trial of iron and folic acid supplements in pregnant Burmese women. Israel Journal of Medical Sciences 1976;12:1410‐7. [PubMed] [Google Scholar]
Butler 1967 {published and unpublished data}
- Butler EB. The effect of iron and folic acid in normal pregnancy (MD thesis). Vol. 1, Cardiff: Welsh National School of Medicine, 1967. [Google Scholar]
- Butler EB. The effect of iron and folic acid in normal pregnancy (MD thesis). Vol. 2 (Appendixes), Cardiff: Welsh National School of Medicine, Department of Obstetrics, 1967. [Google Scholar]
- Butler EB. The effect of iron and folic acid on red cell and plasma volume in pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1968;75:497‐510. [DOI] [PubMed] [Google Scholar]
Buytaert 1983 {published data only}
- Buytaert G, Wallenburg HCS, Eijk HG, Buytaert P. Iron supplementation during pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology 1983;15:11‐6. [DOI] [PubMed] [Google Scholar]
Cantlie 1971 {published data only}
- Cantlie GSD, Leeuw NKM, Lowenstein L. Iron and folate nutrition in a group of private obstetrical patients. American Journal of Clinical Nutrition 1971;24:637‐41. [DOI] [PubMed] [Google Scholar]
Chan 2009 {published and unpublished data}
- Chan KK, Chan BC, Lam KF, Tam S, Lao TT. Iron supplement in pregnancy and development of gestational diabetes‐‐a randomised placebo‐controlled trial. BJOG: an international journal of obstetrics and gynaecology 2009;116(6):789‐98. [DOI] [PubMed] [Google Scholar]
Chanarin 1965 {published data only}
- Chanarin I, Rothman D, Berry V. Iron deficiency and its relation to folic acid status in pregnancy: results of a clinical trial. British Medical Journal 1965;1:480‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chanarin 1971 {published data only}
- Chanarin I, Rothman D. Further observations on the relation between iron and folate status in pregnancy. British Medical Journal 1971;2:81‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Charoenlarp 1988 {published data only}
- Charoenlarp P, Dhanamitta S, Kaewvichit R, Silprasert A, Suwanaradd C, Na‐Nakorn S, et al. A WHO collaborative study on iron supplementation in Burma and in Thailand. American Journal of Clinical Nutrition 1988;47(2):280‐97. [DOI] [PubMed] [Google Scholar]
Chisholm 1966 {published data only}
- Chisholm M. A controlled clinical trial of prophylactic folic acid and iron in pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1966;73:191‐6. [DOI] [PubMed] [Google Scholar]
Christian 2003 (C) {published and unpublished data}
- Christian P. (personal communication) 02 October 2012.
- Christian P. (personal communication) 28 September 2007.
- Christian P, Darmstadt GL, Wu L, Khatry SK, LeClerq SC, Katz J, et al. The effect of maternal micronutrient supplementation on early neonatal morbidity in rural Nepal: a randomised, controlled, community trial. Archives of Disease in Childhood 2008;93(8):660‐4. [DOI] [PubMed] [Google Scholar]
- Christian P, Jiang T, Khatry SK, LeClerq SC, Shrestha SR, West KP Jr. Antenatal supplementation with micronutrients and biochemical indicators of status and subclinical infection in rural Nepal. American Journal of Clinical Nutrition 2006;83:788‐94. [DOI] [PubMed] [Google Scholar]
- Christian P, Khatry SK, Katz J, Pradhan EK, LeClerq SC, Shrestha SR, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. BMJ 2003;326(7389):571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian P, Khatry SK, LeClerq SC, Dali SM. Effects of prenatal micronutrient supplementation on complications of labor and delivery and puerperal morbidity in rural Nepal. International Journal of Gynecology & Obstetrics 2009;106(1):3‐7. [DOI] [PubMed] [Google Scholar]
- Christian P, Murray‐Kolb LE, Khatry SK, Katz J, Schaefer BA, Cole PM, et al. Prenatal micronutrient supplementation and intellectual and motor function in early school‐aged children in Nepal. JAMA 2010;304(24):2716‐23. [DOI] [PubMed] [Google Scholar]
- Christian P, Shrestha J, LeClerq SC, Khatry SK, Jiang T, Wagner T, et al. Supplementation with micronutrients in addition to iron and folic acid does not further improve the hematologic status of pregnant women in rural Nepal. Journal of Nutrition 2003;133(11):3492‐8. [DOI] [PubMed] [Google Scholar]
- Christian P, Stewart CP, LeClerq SC, Wu L, Katz J, West KP Jr, et al. Antenatal and postnatal iron supplementation and childhood mortality in rural Nepal: a prospective follow‐up in a randomized, controlled community trial. American Journal of Epidemiology 2009;170(9):1127‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian P, West KP, Khatry SK, Leclerq SC, Pradhan EK, Katz J, et al. Effects of maternal micronutrient supplementation on fetal loss and infant mortality: a cluster‐randomized trial in Nepal. American Journal of Clinical Nutrition 2003;78(6):1194‐202. [DOI] [PubMed] [Google Scholar]
- Katz J, Christian P, Dominici F, Zeger SL. Treatment effects of maternal micronutrient supplementation vary by percentiles of the birth weight distribution in rural Nepal. Journal of Nutrition 2006;136(5):1389‐94. [DOI] [PubMed] [Google Scholar]
- Nanayakkara‐Bind A, Schulze K, Wu L, Le SC, Khatry SK, Christian P. Effects of antenatal micronutrient supplementation on cortisol and erythropoietin in pregnant Nepalese women. FASEB Journal 2011;25:779.15. [Google Scholar]
- Stewart CP, Christian P, LeClerq SC, West KP Jr, Khatry SK. Antenatal supplementation with folic acid + iron + zinc improves linear growth and reduces peripheral adiposity in school‐age children in rural Nepal. American Journal of Clinical Nutrition 2009;90(1):132‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart CP, Christian P, Schulze KJ, Arguello M, Leclerq SC, Khatry SK, et al. Low maternal vitamin B‐12 status is associated with offspring insulin resistance regardless of antenatal micronutrient supplementation in rural Nepal. Journal of Nutrition 2011;141(10):1912‐7. [DOI] [PubMed] [Google Scholar]
- Stewart CP, Christian P, Schulze KJ, Leclerq SC, West KP Jr, Khatry SK. Antenatal micronutrient supplementation reduces metabolic syndrome in 6‐ to 8‐year‐old children in rural Nepal. Journal of Nutrition 2009;139(8):1575‐81. [DOI] [PubMed] [Google Scholar]
- Stewart CP, Katz J, Khatry SK, LeClerq SC, Shrestha SR, West KP Jr, et al. Preterm delivery but not intrauterine growth retardation is associated with young maternal age among primiparae in rural Nepal. Maternal & Child Nutrition 2007;3(3):174‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cogswell 2003 {published and unpublished data}
- Cogswell ME, Parvanta I, Ickes L, Yip R, Brittenham GM. Individual patient data (as supplied 4 February 2004). Data on file.
- Cogswell ME, Parvanta I, Ickes L, Yip R, Brittenham GM. Iron supplementation during pregnancy, anemia, and birth weight: a randomized controlled trial. American Journal of Clinical Nutrition 2003;78(4):773‐81. [DOI] [PubMed] [Google Scholar]
- Cogswell ME, Parvanta I, Yip R, Brittenham GM. Iron supplementation during pregnancy for initially non‐anemic, iron replete women ‐ decreased prevalence of low birth weight infants. Report of the 2001 INACG Symposium. Why iron is important and what to do about it: a new perspective. Washington D.C.: ILSI Human Nutrition Institute, 2002; Vol. 1:42, Abstract no: 7.
- Cogswell ME, Parvanta I, Yip R, Brittenham GM. Low iron during pregnancy increases the risk of delivering preterm or small infants. Report of the 2001 INACG Symposium. Why iron is important and what to do about it: a new perspective. Washington DC: ILSI Human Nutrition Institute, 2002; Vol. 1:42, Abstract no: 8.
Corrigan 1936 {published data only}
- Corrigan JC, Strauss MB. The prevention of hypochromic anemia in pregnancy. JAMA 1936;106(13):1088‐90. [Google Scholar]
De Benaze 1989 {published data only}
- Benaze C, Galan P, Wainer R, Hercberg S. Prevention of iron deficient anemia during pregnancy by early iron supplementation: a controlled trial. Revue d Epidemiologie et de Sante Publique 1989;37:109‐18. [PubMed] [Google Scholar]
Dommisse 1983 {published data only}
- Dommisse J, Bell DJH, Du Toit ED, Midgley V, Cohen M. Iron‐storage deficiency and iron supplementation in pregnancy. South African Medical Journal 1983;64:1047‐51. [PubMed] [Google Scholar]
Eskeland 1997 {published and unpublished data}
- Eskeland B. Database provided by authors (as supplied 22 February 2004). Data on file.
- Eskeland B, Malterud K, Ulvik RJ, Hunskaar S. Iron supplementation in pregnancy: is less enough? A randomized, placebo controlled trial of low dose iron supplementation with and without heme iron. Acta Obstetricia et Gynecologica Scandinavica 1997;76(9):822‐8. [DOI] [PubMed] [Google Scholar]
Falahi 2010 {published data only}
- Falahi E. Effect of prophylactic iron supplementation on pregnancy outcome. IRCT Iranian Registry of Clinical Trials (www.irct.ir) (accessed 6 December 2010) 2010.
- Falahi E, Akbari S, Ebrahimzade F, Gargari BP. Impact of prophylactic iron supplementation in healthy pregnant women on maternal iron status and birth outcome. Food and Nutrition Bulletin 2011;32(3):213‐7. [DOI] [PubMed] [Google Scholar]
Fenton 1977 {published data only}
- Fenton V, Cavill I, Fisher J. Iron stores in pregnancy. British Journal of Haematology 1977;37:145‐9. [PubMed] [Google Scholar]
Fleming 1974 {published data only}
- Fleming AF, Martin JD, Hahnel R, Westlake AJ. Effects of iron and folic acid antenatal supplements on maternal haematology and fetal wellbeing. Medical Journal of Australia 1974;2:429‐36. [DOI] [PubMed] [Google Scholar]
Fleming 1985 {published data only}
- Fleming AF. Anaemia in pregnancy in the Guinea Savanna of Nigeria. In: Ludwig H, Thomsen K editor(s). Gynecology and Obstetrics. Berlin: Springer‐Verlag, 1986:122‐4. [Google Scholar]
- Fleming AF, Ghatoura GBS, Harrison KA, Briggs ND, Dunn DT. The prevention of anaemia in pregnancy in primigravidae in the guinea savanna of Nigeria. Annals of Tropical Medicine and Parasitology 1986;80:211‐33. [DOI] [PubMed] [Google Scholar]
- Harrison KA, Fleming AF, Briggs ND, Rossiter CE. Child‐bearing, health and social priorities: a survey of 22,774 consecutive hospital births in Zaria, Northern Nigeria. 5. Growth during pregnancy in Nigerian teenage primigravidae. British Journal of Obstetrics and Gynaecology 1985;92(5):32‐9. [PubMed] [Google Scholar]
Foulkes 1982 {published data only}
- Foulkes J, Goldie DJ. The use of ferritin to assess the need for iron supplements in pregnancy. Journal of Obstetrics and Gynaecology 1982;3:11‐6. [Google Scholar]
Freire 1989 {published data only (unpublished sought but not used)}
- Freire WB. Hemoglobin as a predictor of response to iron therapy and its use in screening and prevalence estimates. American Journal of Clinical Nutrition 1989;50:1442‐9. [DOI] [PubMed] [Google Scholar]
Groner 1986 {published data only}
- Groner JA, Holtzman NA, Charney E, Mellits ED. A randomized trial of oral iron on tests of short‐term memory and attention span in young pregnant women. Journal of Adolescent Health Care 1986;7:44‐8. [DOI] [PubMed] [Google Scholar]
Han 2011 {published data only}
- Han XX, Sun YY, Ma AG, Yang F, Zhang FZ, Jiang DC, et al. Moderate NaFeEDTA and ferrous sulfate supplementation can improve both hematologic status and oxidative stress in anemic pregnant women. Asia Pacific Journal of Clinical Nutrition 2011;20(4):514‐20. [PubMed] [Google Scholar]
Hankin 1963 {published data only}
- Hankin ME. The value of iron supplementation during pregnancy. Australian and New Zealand Journal of Obstetrics and Gynaecology 1963;3:111‐8. [DOI] [PubMed] [Google Scholar]
- Hankin ME, Symonds EM. Body weight, diet and pre‐eclamptic toxaemia in pregnancy. Australian and New Zealand Journal of Obstetrics and Gynaecology 1962;4:156‐60. [Google Scholar]
Harvey 2007 {published and unpublished data}
- Fairweather‐Tait S. Personal communication. 2007 September 5.
- Harvey LJ, Dainty JR, Hollands WJ, Bull VJ, Hoogewerff JA, Foxall RJ, et al. Effect of high‐dose iron supplements on fractional zinc absorption and status in pregnant women. American Journal of Clinical Nutrition 2007;85:131‐6. [DOI] [PubMed] [Google Scholar]
Hoa 2005 (C) {published data only}
- Hoa PT, Khan NC, Beusekom C, Gross R, Conde WL, Khoi HD. Milk fortified with iron or iron supplementation to improve nutritional status of pregnant women: an intervention trial from rural Vietnam. Food & Nutrition Bulletin 2005;26(1):32‐8. [DOI] [PubMed] [Google Scholar]
Holly 1955 {published data only}
- Holly RG. Anemia in pregnancy. Obstetrics & Gynecology 1955;5:562‐9. [PubMed] [Google Scholar]
Hood 1960 {published data only}
- Hood WE, Bond WL. Iron deficiency prophylaxis during pregnancy. Obstetrics & Gynecology 1960;16:82‐4. [PubMed] [Google Scholar]
Kerr 1958 {published data only}
- Kerr DNS, Davidson S. The prophylaxis of iron‐deficiency anemia in pregnancy. Lancet 1958;2:483‐8. [DOI] [PubMed] [Google Scholar]
Korkmaz 2014 {published data only}
- Korkmaz V, Ozkaya E, Seven BY, Duzguner S, Karsli MF, Kucukozkan T. Comparison of oxidative stress in pregnancies with and without first trimester iron supplement: a randomized double‐blind controlled trial. Journal of Maternal‐Fetal and Neonatal Medicine 2014;27(15):1535‐8. [DOI] [PubMed] [Google Scholar]
Kuizon 1979 {published data only}
- Kuizon MD, Platon TP, Ancheta LP, Angeles JC, Nunez CB, Macapinlac MP. Iron supplementation studies among pregnant women. Southeast Asian Journal of Tropical Medicine and Public Health 1979;10(4):520‐7. [PubMed] [Google Scholar]
Lee 2005 {published and unpublished data}
- Lee JI, Lee JA, Lim HS. Effect of time of initiation and dose of prenatal iron and folic acid supplementation on iron and folate nutriture of Korean women during pregnancy. American Journal of Clinical Nutrition 2005;82(4):843‐9. [DOI] [PubMed] [Google Scholar]
- Lim HS. Personal communication 2007 September 27.
Liu 2000 {published data only}
- Liu M, He Y, Lu J. Study of the efficacy of ferroids tablets in preventing hypoferric anemia during pregnancy. New Chinese Medicine 2000;31(5):277‐8. [Google Scholar]
Liu 2012 {published data only}
- Cogswell ME. Impact of prenatal vitamin/mineral supplements on perinatal mortality. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 21 March 2006) 2006.
- Liu JM, Mei Z, Ye R, Serdula M, Li HT, Cogswell M. Impact of iron‐contained micronutrient supplementation on macrosomia and large for gestational age births. FASEB Journal 2012;26:1021‐2. [Google Scholar]
- Liu JM, Mei Z, Ye R, Serdula MK, Ren A, Cogswell ME. Micronutrient supplementation and pregnancy outcomes: Double‐blind randomized controlled trial in China. JAMA Internal Medicine 2013;173(4):276‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mei Z, Serdula MK, Liu JM, Flores‐Ayala RC, Wang L, Ye R, et al. Iron‐containing micronutrient supplementation of Chinese women with no or mild anemia during pregnancy improved iron status but did not affect perinatal anemia. Journal of Nutrition 2014;144(6):943‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ma 2010 {published data only}
- Ma AG, Schouten EG, Sun YY, Yang F, Han XX, Zhang FZ, et al. Supplementation of iron alone and combined with vitamins improves haematological status, erythrocyte membrane fluidity and oxidative stress in anaemic pregnant women. British Journal of Nutrition 2010;104(11):1655‐61. [DOI] [PubMed] [Google Scholar]
Makrides 2003 {published and unpublished data}
- Makrides M. Personal communication 2004 April 12.
- Makrides M, Crowther CA, Gibson RA, Gibson RS, Skeaff CM. Efficacy and tolerability of low‐dose iron supplements during pregnancy: a randomised controlled trial. American Journal of Clinical Nutrition 2003;78:145‐53. [DOI] [PubMed] [Google Scholar]
- Makrides M, Crowther CA, Gibson RA, Gibson RS, Skeaff CM. Low‐dose iron supplements in pregnancy prevent iron deficiency at the end of pregnancy and during the post‐partum period: the results of a randomised controlled trial [abstract]. Perinatal Society of Australia and New Zealand 7th Annual Congress; 2003 March 9‐12; Tasmania, Australia. 2003:P99.
- Parsons AG, Zhou SJ, Spurrier NJ, Makrides M. Effect of iron supplementation during pregnancy on the behaviour of children at early school age: long‐term follow‐up of a randomised controlled trial. British Journal of Nutrition 2008;99(5):1133‐9. [DOI] [PubMed] [Google Scholar]
- Zhou SH, Gibson RA, Crowther CA, Baghurst P, Makrides M. Effect of iron supplementation during pregnancy on the intelligence quotient and behavior of children at 4 years of age: long term follow‐up of a randomized controlled trial. American Journal of Clinical Nutrition 2006;83(5):1112‐7. [DOI] [PubMed] [Google Scholar]
- Zhou SJ, Gibson RA, Makrides M. Routine iron supplementation in pregnancy has no effect on iron status of children at six months and four years of age. Journal of Pediatrics 2007;151(4):438‐40. [DOI] [PubMed] [Google Scholar]
Meier 2003 {published data only}
- Meier PR, Nickerson HJ, Olson KA, Berg RL, Meyer JA. Prevention of iron deficiency anemia in adolescent and adult pregnancies. Clinical Medicine and Research 2003;1(1):29‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Menendez 1994 (C) {published data only}
- Menendez C, Todd J, Alonso PL, Francis N, Lulat S, Ceesay S, et al. The effects or iron supplementation during pregnancy, given by traditional birth attendants, on the prevalence of anaemia and malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1994;88:590‐3. [DOI] [PubMed] [Google Scholar]
- Menendez C, Todd J, Alonso PL, Francis N, Lulat S, Ceesay S, et al. The response to iron supplementation of pregnant women with the haemoglobin genotype AA or AS. Transactions of the Royal Society of Tropical Medicine and Hygiene 1995;89(3):289‐92. [DOI] [PubMed] [Google Scholar]
Milman 1991 {published data only}
- Milman N, Agger AO, Nielsen OJ. Iron supplementation during pregnancy. Effect on iron status markers, serum erythropoietin and human placental lactogen. A placebo controlled study in 207 Danish women. Danish Medical Bulletin 1991;38(6):471‐6. [PubMed] [Google Scholar]
- Milman N, Agger AO, Nielson OJ. Iron status markers and serum erythropoietin in 120 mothers and newborn infants: effect of iron supplementation in normal pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1994;73:200‐4. [DOI] [PubMed] [Google Scholar]
- Milman N, Byg KE, Agger AO. Hemoglobin and erythrocyte indices during normal pregnancy and postpartum in 206 women with and without iron supplementation. Acta Obstetricia et Gynecologica Scandinavica 2000;79(2):89‐98. [DOI] [PubMed] [Google Scholar]
- Milman N, Graudal N, Agger AO. Iron status markers during pregnancy. No relationship between levels at the beginning of the second trimester, prior to delivery and post partum. Journal of Internal Medicine 1995;237:261‐7. [DOI] [PubMed] [Google Scholar]
- Milman N, Graudal N, Nielsen OJ, Agger AO. Serum erythropoietin during normal pregnancy: relationship to hemoglobin and iron status markers and impact of iron supplementation in a longitudinal, placebo‐controlled study on 118 women. International Journal of Hematology 1997;66(2):159‐68. [DOI] [PubMed] [Google Scholar]
- Milman N, Graudal NA, Agger AO. Iron status markers during normal pregnancy in 120 women. No clinically useful relationship between levels in the second trimester, later in pregnancy, and post partum. Ugeskrift for Laeger 1995;157:6571‐5. [PubMed] [Google Scholar]
Ouladsahebmadarek 2011 {published data only}
- Ouladsahebmadarek E, Sayyah‐Melli M, Taghavi S, Abbasalizadeh S, Seyedhejazie M. The effect of supplemental iron elimination on pregnancy outcome. Pakistan Journal of Medical Sciences 2011;27(3):641‐5. [Google Scholar]
Paintin 1966 {published and unpublished data}
- Paintin DB, Thompson AM, Hytten FE. Personal communication 1986.
- Paintin DB, Thomson AM, Hytten FE. Iron and haemoglobin level in pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1966;73:181‐90. [Google Scholar]
Preziosi 1997 {published data only}
- Preziosi P, Prual A, Galan P, Daouda H, Boureima H, Hercberg S. Effect of iron supplementation on the iron status of pregnant women: consequences for newborns. American Journal of Clinical Nutrition 1997;66:1178‐82. [DOI] [PubMed] [Google Scholar]
Pritchard 1958 {published data only}
- Pritchard J, Hunt C. A comparison of the hematologic responses following the routine prenatal administration of intramuscular and oral iron. Surgery, Gynecology and Obstetrics 1958;106:516‐8. [PubMed] [Google Scholar]
Puolakka 1980 {published data only}
- Puolakka J, Janne O, Pakarinen A, Jarvinen PA, Vihko R. Serum ferritin as a measure of iron stores during and after normal pregnancy with and without iron supplement. Acta Obstetricia et Gynecologica Scandinavica 1980;95:43‐51. [DOI] [PubMed] [Google Scholar]
Romslo 1983 {published data only}
- Romslo I, Haram K, Sagen N, Augensen K. Iron requirements in normal pregnancy as assessed by serum ferritin, serum transferrin saturation and erythrocyte protoporphyrin determinations. British Journal of Obstetrics and Gynaecology 1983;90:101‐7. [DOI] [PubMed] [Google Scholar]
Siega‐Riz 2001 {published and unpublished data}
- Bodnar LM, Davidian M, Siega‐Riz AM, Tsiatis AA. Marginal structural models for analyzing causal effects of time‐dependent treatments: an application in perinatal epidemiology. American Journal of Epidemiology 2004;159(10):926‐34. [DOI] [PubMed] [Google Scholar]
- Jasti S, Siega‐Riz AM, Cogswell ME, Hartzema AG. Correction for errors in measuring adherence to prenatal multivitamin/mineral supplement use among low‐income women. Journal of Nutrition 2006;136(2):479‐83. [DOI] [PubMed] [Google Scholar]
- Jasti S, Siega‐Riz AM, Cogswell ME, Hartzema AG, Bentley ME. Pill count adherence to prenatal multivitamin/mineral supplement use among low‐income women. Journal of Nutrition 2005;135(5):1093‐101. [DOI] [PubMed] [Google Scholar]
- Siega‐Riz A, Hartzema A, Turnbull C, Thorp JJ, McDonald T. A trial of selective versus routine iron supplementation to prevent third trimester anemia during pregnancy. American Journal of Obstetrics and Gynecology 2001; Vol. 185, issue 6 Suppl:S119.
- Siega‐Riz AM, Hartzema AG, Turnbull C, Thorp J, McDonald T, Cogswell ME. The effects of prophylactic iron given in prenatal supplements on iron status and birth outcomes: a randomized controlled trial. American Journal of Obstetrics and Gynecology 2006;194(2):512‐9. [DOI] [PubMed] [Google Scholar]
Simmons 1993 {published data only}
- Simmons WK, Cook JD, Bingham KC, Thomas M, Jackson J, Jackson M, et al. Evaluation of a gastric delivery system for iron supplementation in pregnancy. American Journal of Clinical Nutrition 1993;58:622‐6. [DOI] [PubMed] [Google Scholar]
Suharno 1993 {published data only}
- Suharno D, West CE, Karyadi D, Hautvast JGA. Supplementation with vitamin A and iron for nutritional anaemia in pregnant women in West Java, Indonesia. Lancet 1993;342:1325‐8. [DOI] [PubMed] [Google Scholar]
Sun 2010 {published data only}
- Sun YY, Ma AG, Yang F, Zhang FZ, Luo YB, Jiang DC, et al. A combination of iron and retinol supplementation benefits iron status, IL‐2 level and lymphocyte proliferation in anemic pregnant women. Asia Pacific Journal of Clinical Nutrition 2010;19(4):513‐9. [PubMed] [Google Scholar]
Svanberg 1975 {published data only}
- Svanberg B, Arvidsson B, Norrby A, Rybo G, Solvell L. Absorption of supplemental iron during pregnancy ‐ a longitudinal study with repeated bone marrow studies and absorption measurements. Acta Obstetricia et Gynecologica Scandinavica 1975;48:87‐108. [DOI] [PubMed] [Google Scholar]
Taylor 1982 {published and unpublished data}
- Taylor DJ, Lind T. Red cell mass during and after normal delivery. British Journal of Obstetrics and Gynaecology 1979;86(5):364‐70. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Mallen C, McDougall N, Lind T. Personal communication 1982.
- Taylor DJ, Mallen C, McDougall N, Lind T. Effect of iron supplementation on serum ferritin levels during and after pregnancy. British Journal of Obstetrics and Gynaecology 1982;89:1011‐7. [DOI] [PubMed] [Google Scholar]
Tholin 1993 {published data only}
- Tholin K, Hallmans G, Sandstrom B, Goop M, Palm R, Abrahamsson M. Serum zinc, iron supplementation and pregnancy outcome. TEMA 8: Proceedings of the Eighth International Symposium on Trace Elements in Man and Animals; 1993 May 16‐22; Dresden, Germany. 1993:894‐5.
- Tholin K, Sandstrom B, Palm R, Hallmans G. Changes in blood manganese levels during pregnancy in iron supplemented and non supplemented women. Journal of Trace Elements in Medicine and Biology 1995;9(1):13‐7. [DOI] [PubMed] [Google Scholar]
Tura 1989 {published data only}
- Tura S, Carenza L, Baccarani M, Bagnara M, Bocci A, Bottone P, et al. Therapy and iron supplements with ferritin during pregnancy. A randomized prospective study of 458 cases. Recenti Progessi in Medicina 1989;80:607‐14. [PubMed] [Google Scholar]
Van Eijk 1978 {published data only}
- Eijk HG, Kroos MJ, Hoogendoorn GA, Wallenburg HC. Serum ferritin and iron stores during pregnancy. Clinica Chimica Acta 1978;83(1‐2):81‐91. [DOI] [PubMed] [Google Scholar]
Wallenburg 1983 {published data only}
- Buytaert G, Wallenburg HCS, Eijk HG, Buytaert P. Iron supplementation during pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology 1983;15:11‐6. [DOI] [PubMed] [Google Scholar]
- Wallenburg HCS, Eijk HG. Effect of oral iron supplementation during pregnancy on maternal and fetal iron status. Journal of Perinatal Medicine 1984;12:7‐12. [DOI] [PubMed] [Google Scholar]
Willoughby 1967 {published data only}
- Willoughby ML, Jewell FJ. Investigation of folic acid requirements in pregnancy. British Medical Journal 1966;2(5529):1568‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby MLN. An investigation of folic acid requirements in pregnancy. II. British Journal of Haematology 1967;13:503‐9. [DOI] [PubMed] [Google Scholar]
- Willoughby MLN, Jewell FG. Folate status throughout pregnancy and in postpartum period. British Medical Journal 1968;4:356‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wills 1947 {published data only}
- Wills L, Hill G, Bingham K, Miall M, Wrigley J. Haemoglobin levels in pregnancy: the effect of the rationing scheme and routine administration of iron. British Journal of Nutrition 1947;1:126‐38. [DOI] [PubMed] [Google Scholar]
Zeng 2008 (C) {published data only (unpublished sought but not used)}
- Chang S, Zeng L, Brouwer ID, Kok FJ, Yan H. Effect of iron deficiency anemia in pregnancy on child mental development in rural China. Pediatrics 2013;131(3):e755‐e763. [DOI] [PubMed] [Google Scholar]
- Cheng Y, Dibley MJ, Zhang X, Zeng L, Yan H. Assessment of dietary intake among pregnant women in a rural area of western China. BMC Public Health 2009;9(9):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Yan H, Zeng L, Cheng Y, Liang W, Dang S, et al. Effects of maternal multimicronutrient supplementation on the mental development of infants in rural western China: follow‐up evaluation of a double‐blind, randomized, controlled trial. Pediatrics 2009;123(4):e685‐e692. [DOI] [PubMed] [Google Scholar]
- Wang W, Yan H, Zeng L, Cheng Y, Wang D, Li Q. No effect of maternal micronutrient supplementation on early childhood growth in rural western China: 30 month follow‐up evaluation of a double blind, cluster randomized controlled trial. European Journal of Clinical Nutrition 2012;66(2):261‐8. [DOI] [PubMed] [Google Scholar]
- Yan H. Impact of iron/folate versus multi‐micronutrient supplementation during pregnancy on birth weight: a randomised controlled trial in rural Western China. Current Controlled Trials (www.controlled‐trials.com) (accessed 15 February 2007) 2007.
- Zeng L, Dibley MJ, Cheng Y, Dang S, Chang S, Kong L, et al. Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ 2008;337:a2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng L, Yan H, Cheng Y, Dang S, Dibley MJ. Adherence and costs of micronutrient supplementation in pregnancy in a double‐blind, randomized, controlled trial in rural western China. Food and Nutrition Bulletin 2009;30(4 Suppl):S480‐S487. [DOI] [PubMed] [Google Scholar]
- Zeng L, Yan H, Cheng Y, Dibley MJ. Modifying effects of wealth on the response to nutrient supplementation in pregnancy on birth weight, duration of gestation and perinatal mortality in rural western China: double‐blind cluster randomized controlled trial. International Journal of Epidemiology 2011;40(2):350‐62. [DOI] [PubMed] [Google Scholar]
Ziaei 2007 {published and unpublished data}
- Jafarbegloo E. Gastrointestinal complications of iron supplement in pregnant women. IRCT Iranian Registry of Clinical Trials (www.irct.ir) (accessed 6 December 2010) 2010.
- Ziaei S. Personal communication 2007 October 1.
- Ziaei S, Norrozi M, Faghihzadeh S, Jafarbegloo E. A randomised placebo‐controlled trial to determine the effect of iron supplementation on pregnancy outcome in pregnant women with haemoglobin > or = 13.2 g/dl. BJOG: an international journal of obstetrics and gynaecology 2007;114(6):684‐8. [DOI] [PubMed] [Google Scholar]
Ziaei 2008 {published and unpublished data}
- Hamzehgardeshi Z. A randomized placebo‐controlled trial to determine the effect of iron supplementation on hematological indices in pregnant women with hemoglobin > 13.2 g/dl. IRCT Iranian Registry of Clinical Trials (www.irct.ir) (accessed 6 December 2010) 2010.
- Janghorban R, Ziaei S, Faghihzade S. Evaluation of serum copper level in pregnant women with high hemoglobin. Iranian Journal of Medical Sciences 2006;31(3):170‐2. [Google Scholar]
- Ziaei S. Iron status markers in non‐anemic pregnant women with or without iron supplementation in pregnancy. Personal communication 2007 October 9.
- Ziaei S, Janghorban R, Shariatdoust S, Faghihzadeh S. The effects of iron supplementation on serum copper and zinc levels in pregnant women with high‐normal hemoglobin. International Journal of Gynecology & Obstetrics 2008;100:133‐5. [DOI] [PubMed] [Google Scholar]
- Ziaei S, Mehrnia M, Faghihzadeh S. Iron status markers in nonanemic pregnant women with and without iron supplementation. International Journal of Gynecology & Obstetrics 2008;100:130‐2. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aaseth 2001 {published data only}
- Aaseth J, Thomassen Y, Ellingsen DG, Stoa‐Birketvedt G. Prophylactic iron supplementation in pregnant women in Norway. Journal of Trace Elements in Medicine & Biology 2001;15(2‐3):167‐74. [DOI] [PubMed] [Google Scholar]
Abel 2000 {published data only}
- Abel R, Rajaratnam J, Kalaimani A, Kirubakaran S. Can iron status be improved in each of the three trimesters? A community base study. European Journal of Clinical Nutrition 2000;54:490‐3. [DOI] [PubMed] [Google Scholar]
Adhikari 2009 {published data only}
- Adhikari K, Liabsuetrakul T, Pradhan N. Effect of education and pill count on hemoglobin status during prenatal care in Nepalese women: a randomized controlled trial. Journal of Obstetrics and Gynaecology Research 2009;35(3):459‐66. [DOI] [PubMed] [Google Scholar]
Afifi 1978 {published data only}
- Afifi AM. Plexafer‐F in the management of latent iron deficiency in pregnancy. Journal of International Medical Research 1978;6:34‐40. [DOI] [PubMed] [Google Scholar]
Agrawal 2011 {published data only}
- Agrawal N. Impact of two oral iron supplementation regimens (intermittently and continuously/daily) for prevention of anaemia in pregnancy in women with normal haemoglobin levels. Clinical Trials Registry ‐ India (accessed 31 May 2013) 2011.
Ahn 2006 {published data only}
- Ahn E, Pairaudeau N, Pairaudeau N, Cerat Y, Couturier B, Fortier A, et al. A randomized cross over trial of tolerability and compliance of a micronutrient supplement with low iron separated from calcium vs high iron combined with calcium in pregnant women. BMC Pregnancy and Childbirth 2006;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alaoddolehei 2012 {published data only}
- Alaoddolehei H, Samiei H, Sadighian F, Kalantari N. Efficacy of daily versus intermittent administration of iron supplementation in anemia or blood indices during pregnancy. Caspian Journal of Internal Medicine 2012;4(1):569‐73. [PMC free article] [PubMed] [Google Scholar]
Angeles‐Agdeppa 2003 {published data only (unpublished sought but not used)}
- Angeles‐Agdeppa I. The effects of a community‐based weekly iron‐folate supplementation on hemoglobin and iron status of pregnant and non‐pregnant women in Philippines. Meeting on weekly iron/folic acid supplementation for preventing anaemia in women of reproductive age in the Western Pacific Region report; 2003 Sept 29 ‐ Oct 1; Manila, Philippines. Manila, Philippines: WHO, 2003.
- Angeles‐Agdeppa I, Paulino LS, Ramos AC, Etorma UM, Cavalli‐Sforza T, Milani S. Government‐industry partnership in weekly iron‐folic acid supplementation for women of reproductive age in the Philippines: impact on iron status. Nutrition Reviews 2005;63(12 Pt 2):S116‐S125. [DOI] [PubMed] [Google Scholar]
- Paulino LS, Angeles‐Agdeppa I, Etorma UM, Ramos AC, Cavalli‐Sforza T. Weekly iron‐folic acid supplementation to improve iron status and prevent pregnancy anemia in Filipino women of reproductive age: the Philippine experience through government and private partnership. Nutrition Reviews 2005;63(12 Pt 2):S109‐S115. [DOI] [PubMed] [Google Scholar]
Arija 2014 {published data only}
- Arija V, Fargas F, March G, Abajo S, Basora J, Canals J, et al. Adapting iron dose supplementation in pregnancy for greater effectiveness on mother and child health: protocol of the ECLIPSES randomized clinical trial. BMC Pregnancy and Childbirth 2014;14(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Babior 1985 {published data only}
- Babior BM, Peters WA, Briden PM, Cetrulo CL. Pregnant women's absorption of iron from prenatal supplements. Journal of Reproductive Medicine 1985;30:355‐7. [PubMed] [Google Scholar]
Balmelli 1974 {published data only}
- Balmelli GP, Huser HJ. Folic acid deficiency in pregnant women in Switzerland [Zur Frage des Folsäuremangels beiSchwangeren in der Schweiz]. Schweizerische Medizinische Wochenschrift 1974;104(10):351‐6. [PubMed] [Google Scholar]
Bencaiova 2007 {published data only (unpublished sought but not used)}
- Bencaiova G, Mandach U, Zimmerman R. Optimal prophylaxis of a lack of iron and iron‐deficiency anemia in the pregnancy: a randomized study [Optimale Prophylaxe e Ines Elsenmangels und elner Eisenmangelanamie In der Schwangerschaft: eine randomisierte Studie]. Gynakologisch‐Geburtshilfliche Rundschau 2007;47:140. [Google Scholar]
- Bencaiova G, Mandach U, Zimmermann R. Iron prophylaxis in pregnancy: intravenous route versus oral route. European Journal of Obstetrics & Gynecology and Reproductive Biology 2009;144(2):135‐9. [DOI] [PubMed] [Google Scholar]
Berger 2003 {published data only (unpublished sought but not used)}
- Berger J. Effectiveness of weekly iron/folate supplementation on anaemia and iron status in women of reproductive age in rural Viet Nam. Meeting on weekly iron/folic acid supplementation for preventing anaemia in women of reproductive age in the Western Pacific Region report; 2003 Sept 29‐Oct 1; Manila, Philippines. Manila, Philippines: WHO, 2003.
- Berger J, Thanh HT, Cavalli‐Sforza T, Smitasiri S, Khan NC, Milani S, et al. Community mobilization and social marketing to promote weekly iron‐folic acid supplementation in women of reproductive age in Vietnam: impact on anemia and iron status. Nutrition Reviews 2005;63(12 Pt 2):S95‐S108. [DOI] [PubMed] [Google Scholar]
- Hoa PT, Berger J, Paliakara N, Nhien NV, Morestin‐Cadet S, Quyen DT, et al. Weekly iron‐folate supplementation in women in reproductive age in Vietnam: a new approach to control iron deficiency anemia during pregnancy. INACG Symposium; 2001 Feb 15‐16; Hanoi, Vietnam. 2001:45, Abstract No: 18.
- Khan NC, Thanh HT, Berger J, Hoa PT, Quang ND, Smitasiri S, et al. Community mobilization and social marketing to promote weekly iron‐folic acid supplementation: a new approach toward controlling anemia among women of reproductive age in Vietnam. Nutrition Reviews 2005;63(12 Pt 2):S87‐S94. [DOI] [PubMed] [Google Scholar]
Bergsjo 1987 {published data only}
- Bergsjo P. The effects of iron supplementation in pregnancy. Personal communication 1987.
Bhatla 2009 {published data only}
- Bhatla N, Kaul N, Lal N, Kriplani A, Agarwal N, Saxena R, et al. Comparison of effect of daily versus weekly iron supplementation during pregnancy on lipid peroxidation. Journal of Obstetrics and Gynaecology Research 2009;35(3):438‐45. [DOI] [PubMed] [Google Scholar]
Blot 1980 {published data only}
- Blot I, Papiernik E, Kalwatsser JP, Werner E, Tchernia G. Influence of routine administration of folic acid and iron during pregnancy. Gynecologic and Obstetric Investigation 1981;12:294‐304. [DOI] [PubMed] [Google Scholar]
- Blot I, Tchernia G, Chenayer M, Hill C, Hajeri H, Leluc R. Iron deficiency in the pregnant woman. Its repercussions on the newborn. The influence of systematic iron treatment. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1980;9:489‐95. [PubMed] [Google Scholar]
- Tchernia G, Blot I, Rey A, Kaltwasser JP, Zittoun J, Papiernik E. Maternal folate status, birthweight and gestational age. Developmental Pharmacology Therapeutics 1982;4 Suppl:58‐65. [PubMed] [Google Scholar]
- Zittoun J, Blot I, Hill C, Zittoun R, Papiernik E, Tchernia G. Iron supplements vs placebo during pregnancy: its effects on iron and folate status on mothers and newborns. Annals of Nutrition and Metabolism 1983;27:320‐7. [DOI] [PubMed] [Google Scholar]
Bokhari 2011 {published data only}
- Bokhari EJ. A functional food for the prevention of iron‐deficiency anemia. ClinicalTrial.gov (http://clinicaltrials.gov) (accessed 19 July 2011) 2011.
- Bokhari F, Derbyshire EJ, Li W, Brennan CS. Can an iron‐rich staple food help women to achieve dietary targets in pregnancy?. International Journal of Food Sciences & Nutrition 2012;63(2):199‐207. [DOI] [PubMed] [Google Scholar]
Bokhari 2012 {published data only}
- Bokhari F, Derbyshire EJ, Hickling D, Li W, Brennan CS. A randomized trial investigating an iron‐rich bread as a prophylaxis against iron deficiency in pregnancy. International Journal of Food Sciences & Nutrition 2012;63(4):461‐7. [DOI] [PubMed] [Google Scholar]
Brown 1972 {published data only}
- Brown GM, Dawson DW. Prevention of anaemia in pregnancy. Current Medical Research and Opinion 1972;1:93‐9. [DOI] [PubMed] [Google Scholar]
Burslem 1968 {published data only}
- Burslem RW, Poller L, Wacks H. A trial of slow release ferrous sulphate (Ferrogradumet) in prevention of iron deficiency in pregnancy. Acta Haematologica 1968;40:200‐4. [DOI] [PubMed] [Google Scholar]
Buss 1981 {published data only}
- Buss M. Therapy of iron‐folic acid deficiency in pregnancy [Therapie des Eisen‐Folsauremangels in der Schwangerschaft]. Zeitschrift fur Allgemeinmedizin 1981;57(22):1526‐32. [PubMed] [Google Scholar]
Carrasco 1962 {published data only}
- Carrasco E, Jose F, Samson G, Germar E, Padilla B. Effect of D‐sorbitol on the absorption and transfer of nutrients from mother to fetus. American Journal of Clinical Nutrition 1962;11:533‐6. [DOI] [PubMed] [Google Scholar]
Casanueva 2003a {published and unpublished data}
- Casanueva E. Weekly iron‐folate (Fe‐fol) supplementation during pregnancy in Mexican women. Personal communication 2003.
- Casanueva E, Viteri FE, Mares‐Galindo M, Meza‐Camacho C, Loria A, Schnaas L, et al. Weekly iron as a safe alternative to daily supplementation for nonanemic pregnant women. Archives of Medical Research 2006;37(5):674‐82. [DOI] [PubMed] [Google Scholar]
Castren 1968 {published data only}
- Castren O, Levanto A, Rauramo L, Ruponen S. Preventive iron and folic acid therapy in pregnancy. Annales Chirurgiae et Gynaecologiae Fenniae 1968;57:382‐6. [PubMed] [Google Scholar]
Chanarin 1968 {published data only}
- Chanarin I, Rothman D, Ward A, Perry J. Folate status and requirement in pregnancy. British Medical Journal 1968;2:390‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chawla 1995 {published data only}
- Chawla PK, Puri R. Impact of nutritional supplements on hematological profile of pregnant women. Indian Pediatrics 1995;32:876‐80. [PubMed] [Google Scholar]
Chew 1996a {published and unpublished data}
- Chew F, Torun B, Viteri FE. Comparison of weekly and daily iron supplementation to pregnant women in Guatemala (supervised and unsupervised). FASEB Journal 1996;10:A4221. [Google Scholar]
- Chew F, Torun B, Viteri FE. Individual patient data (as supplied 15 January 2004). Data on file.
- Chew F, Torún B, Viteri FE. Comparison of daily and weekly iron supplementation in pregnant women with and without direct supervision [Comparación de la suplementación diaria o semanal de hierro en mujeres embarazadas con y sin supervisión directa]. XI Congreso Latino Americano de Nutrición, Libro de Resumenes. Guatemala: SLAN, 1997:94.
Chew 1996b {published and unpublished data}
- Chew F, Torun B, Viteri FE. Comparison of weekly and daily iron supplementation to pregnant women in Guatemala (supervised and unsupervised). FASEB Journal 1996;10:A4221. [Google Scholar]
- Chew F, Torun B, Viteri FE. Individual patient data (as supplied 15 January 2004). Data on file.
- Chew F, Torún B, Viteri FE. Comparison of daily and weekly iron supplementation in pregnant women with and without direct supervision [Comparación de la suplementación diaria o semanal de hierro en mujeres embarazadas con y sin supervisión directa]. XI Congreso Latino Americano de Nutrición, Libro de Resumenes. Guatemala: SLAN, 1997:94.
Coelho 2000 {published data only}
- Coelho K, Ramdas S, Pillai S. A comparative study of changes in haemoglobin with high and low dose iron preparations in pregnant women. Journal of Obstetrics and Gynecology of India 2000;50(2):37‐9. [Google Scholar]
Cook 1990 {published data only}
- Cook JD, Carriaga M, Kahn SG, Schalch W, Skikne BS. Gastric delivery system for iron supplementation. Lancet 1990;335(8698):1136‐9. [DOI] [PubMed] [Google Scholar]
Dawson 1962 {published data only}
- Dawson DW, More JRS, Aird DC. Prevention of megaloblastic anaemia in pregnancy by folic acid. Lancet 1962;2:1015‐20. [DOI] [PubMed] [Google Scholar]
Dawson 1987 {published data only}
- Dawson EB, McGanity WJ. Protection of maternal iron stores in pregnancy. Journal of Reproductive Medicine 1987;32(6 Suppl):478‐87. [PubMed] [Google Scholar]
Dijkhuizen 2004 {published data only}
- Dijkhuizen MA, Wieringa FT, West CE, Muhilal. Zinc plus beta‐carotene supplementation of pregnant women is superior to beta‐carotene supplementation alone in improving vitamin A status in both mothers and infants. American Journal of Clinical Nutrition 2004;80(5):1299‐307. [DOI] [PubMed] [Google Scholar]
Edgar 1956 {published data only}
- Edgar W, Rice HM. Administration of iron in antenatal clinics. Lancet 1956;1:599‐602. [DOI] [PubMed] [Google Scholar]
Ekstrom 1996 {published data only}
- Ekstrom EM, Kavishe FP, Habicht J, Frongillo EA, Rasmussen KM, Hemed L. Adherence to iron supplementation during pregnancy in Tanzania: determinants and hematologic consequences. American Journal of Clinical Nutrition 1996;64:368‐74. [DOI] [PubMed] [Google Scholar]
Ekstrom 2002 {published and unpublished data}
- Ekstrom EC. Personal communication 2004 April 12.
- Ekstrom EC, Hyder SM, Chowdhury AM, Chowdhury SA, Lonnerdal B, Habicht JP, et al. Efficacy and trial effectiveness of weekly and daily iron supplementation among pregnant women in rural Bangladesh: disentangling the issues. American Journal of Clinical Nutrition 2002;76(6):1392‐400. [DOI] [PubMed] [Google Scholar]
- Hyder SM, Persson LA, Chowdhury AM, Ekstrom EC. Do side‐effects reduce compliance to iron supplementation? A study of daily‐ and weekly‐dose regimens in pregnancy. Journal of Health, Population and Nutrition 2002;2:175‐9. [PubMed] [Google Scholar]
- Hyder SM, Persson LA, Chowdhury R, Lonnerdal B, Ekstrom EC. Impact of daily and weekly iron supplementation to women in pregnancy and puerperium on haemoglobin and iron status six weeks postpartum: results from a community‐based study in Bangladesh. Scandinavian Journal of Nutrition 2003;47(1):19‐25. [Google Scholar]
Fletcher 1971 {published data only}
- Fletcher J, Gurr A, Fellingham F, Prankerd T, Brant H, Menzies D. The value of folic acid supplements in pregnancy. Journal of Obstetrics and Gynaecology of the British Empire 1971;78:781‐5. [DOI] [PubMed] [Google Scholar]
Giles 1971 {published data only}
- Giles PF, Harcourt AG, Whiteside MG. The effect of prescribing folic acid during pregnancy on birthweight and duration of pregnancy. A double blind trial. Medical Journal of Australia 1971;2:17‐21. [PubMed] [Google Scholar]
Gomber 2002 {published data only}
- Gomber S, Agarwal KN, Mahajan C, Agarwal N. Impact of daily versus weekly hematinic supplementation on anemia in pregnant women. Indian Pediatrics 2002;39(4):339‐46. [PubMed] [Google Scholar]
Goonewardene 2001 {published data only}
- Goonewardene M, Liyanage C, Fernando R. Intermittent oral iron supplementation during pregnancy. Ceylon Medical Journal 2001;46(4):132‐5. [DOI] [PubMed] [Google Scholar]
Gopalan 2004 {published data only}
- Gopalan S, Patnaik R, Ganesh K. Feasible strategies to combat low birth weight and intra‐uterine growth retardation. Journal of Pediatric Gastroenterology and Nutrition 2004;39(Suppl 1):S37. [Google Scholar]
Goshtasebi 2012 {published data only}
- Goshtasebi A, Alizadeh M. Impact of twice weekly versus daily iron supplementation during pregnancy on maternal and fetal haematological indices: A randomized clinical trial [lImpact d'une prise de complement en fer bihebdomadaire par rapport a une prise quotidienne pendant la grossesse sur des indices hematologiques maternels et foetaux: Une etude clinique randomisee]. Eastern Mediterranean Health Journal 2012;18(6):561‐6. [DOI] [PubMed] [Google Scholar]
Gringras 1982 {published data only}
- Gringras M. A comparison of two combined iron‐folic acid preparations in the prevention of anaemia in pregnancy. Journal of International Medical Research 1982;10:268‐70. [DOI] [PubMed] [Google Scholar]
Grover 1998 {published data only}
- Grover V, Aggarwal OP, Gupta A, Kumar P, Tiwari RS. Effect of daily and alternate day iron and folic acid supplementation to pregnant females on the weight of the newborn. Indian Journal of Community Medicine 1998;23(4):165‐8. [Google Scholar]
Guldholt 1991 {published data only}
- Guldholt IS, Trolle BG, Hvidman LE. Iron supplementation during pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1991;70:9‐12. [DOI] [PubMed] [Google Scholar]
Hampel 1974 {published data only}
- Hampel K, Roetz R. Influence of a long‐time substitution with a folate‐iron combination in pregnancy on serum folate and serum iron and on hematological parameters. Geburtshilfe und Frauenheilkunde 1974;34:409‐17. [PubMed] [Google Scholar]
Hanieh 2013 {unpublished data only}
- Biggs BA. A randomised controlled trial to compare the impact on birth weight of daily iron‐folic acid, twice weekly iron‐folic acid and twice weekly multiple micronutrient supplementation for pregnant women in Ha Nam province, Vietnam. Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) (accessed 17 January 2011) 2011.
- Hanieh S, Ha TT, Simpson JA, Casey GJ, Khuong NC, Thoang DD, et al. The effect of intermittent antenatal iron supplementation on maternal and infant outcomes in rural Viet Nam: a cluster randomised trial. PLoS Medicine 2013;10(6):e1001470. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartman‐Craven 2009 {published data only}
- Hartman‐Craven B, Christofides A, O'Connor DL, Zlotkin S. Relative bioavailability of iron and folic acid from a new powdered supplement compared to a traditional tablet in pregnant women. BMC Pregnancy and Childbirth 2009;9:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawkins 1987 {published data only}
- Hawkins DF. Relative efficacy of sustained release iron and iron with folic acid treatment in pregnancy. Personal communication 1987.
Hemminki 1991 {published and unpublished data}
- Hemminki E, Merilainen J. Long‐term effects of iron prophylaxis during pregnancy. International Journal of Gynecology & Obstetrics 1994;46:3. [Google Scholar]
- Hemminki E, Merilainen J. Long‐term follow‐up of mothers and their infants in a randomized trial on iron prophylaxis during pregnancy. American Journal of Obstetrics and Gynecology 1995;173:205‐9. [DOI] [PubMed] [Google Scholar]
- Hemminki E, Rimpela U. A randomized comparison of routine vs selective iron supplementation during pregnancy. Journal of the American College of Nutrition 1991;10:3‐10. [DOI] [PubMed] [Google Scholar]
- Hemminki E, Rimpela U. Iron supplementation, maternal packed cell volume, and fetal growth. Archives of Disease in Childhood 1991;66:422‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemminki E, Rimpela U, Yla‐Outinen A. Iron prophylaxis during pregnancy and infections. International Journal of Vitamin and Nutrition Research 1991;61:370‐1. [PubMed] [Google Scholar]
- Hemminki E, Uski A, Koponen P, Rimpela U. Iron supplementation during pregnancy ‐ experiences of a randomized trial relying on health service personnel. Controlled Clinical Trials 1989;10:290‐8. [DOI] [PubMed] [Google Scholar]
Hermsdorf 1986 {published data only}
- Hermsdorf J, Ring D, Retzke U, Bruschke G. Oral iron prophylaxis during pregnancy. A longitudinal study about hematologic and clinical parameters in treated and non‐treated pregnant women. Proceedings of 10th European Congress of Perinatal Medicine; 1986 August 12‐16; Leipzig, Germany. 1986:84.
Horgan 1966 {published data only}
- Horgan M, Woodliff M, Mangion J. A combined iron and folic‐acid preparation in the prophylaxis of anaemia of pregnancy. Practitioner 1966;197:683‐6. [PubMed] [Google Scholar]
Hosokawa 1989 {published data only}
- Hosokawa K. Studies on anemia in pregnant women: therapeutic efficacy of iron monotherapy vs. combination therapy with iron and vitamin C. Rinsho to Kenkyu (The Japanese Journal of Clinical and Experimental Medicine) 1989;66(10):3329‐35. [Google Scholar]
Hossain 2014 {published data only}
- Hossain N, Kanani FH, Ramzan S, Kausar R, Ayaz S, Khanani R, et al. Obstetric and neonatal outcomes of maternal vitamin D supplementation: Results of an open label randomized controlled trial of antenatal vitamin D supplementation in Pakistani women. Journal of Clinical Endocrinology and Metabolism 2014;99(7):2448‐55. [DOI] [PubMed] [Google Scholar]
Itam 2003 {published data only}
- Itam IH. The effect of "Chemiron" on haematological parameters and ferritin levels in pregnant Nigerian women in Calabar. Mary Slessor Journal of Medicine 2003;3(2):17‐24. [Google Scholar]
Iyengar 1970 {published data only}
- Iyengar L. Effect of folic acid supplementation on birth weight of infants. American Journal of Obstetrics and Gynaecology 1974;122:332‐6. [DOI] [PubMed] [Google Scholar]
- Iyengar L. Folic acid requirements of Indian pregnant women. American Journal of Obstetrics and Gynecology 1971;111(1):13‐6. [DOI] [PubMed] [Google Scholar]
- Iyengar L, Apte SV. Prophylaxis of anemia in pregnancy. American Journal of Clinical Nutrition 1970;23:725‐30. [DOI] [PubMed] [Google Scholar]
Kaestel 2005 {published data only}
- Andersen GS, Friis H, Michaelsen KF, Rodrigues A, Benn CS, Aaby P, et al. Effects of maternal micronutrient supplementation on fetal loss and under‐2‐years child mortality: long‐term follow‐up of a randomised controlled trial from Guinea‐Bissau. African Journal of Reproductive Health 2010;14(2):17‐26. [PubMed] [Google Scholar]
- Kaestel P, Michaelsen KF, Aaby P, Friis H. Effects of prenatal multimicronutrient supplements on birth weight and perinatal mortality: a randomised, controlled trial in Guinea‐Bissau. European Journal of Clinical Nutrition 2005;59(9):1081‐9. [DOI] [PubMed] [Google Scholar]
Kann 1988 {published data only}
- Kann J, Lyon JA, Bon C. Availability of iron from four prenatal multivitamin/multimineral products. Clinical Therapeutics 1988;10:287‐93. [PubMed] [Google Scholar]
Khambalia 2009 {published data only}
- Khambalia A. Periconceptional iron supplementation and iron and folate status among pregnant and non‐pregnant women in rural Bangladesh [thesis]. Toronto: University of Toronto, 2009. [Google Scholar]
- Khambalia A, O'Connor D, Zlotkin S. Reduced anemia and improved iron and folate status before and after pregnancy among females in rural Bangladesh is related to length of adherence to periconceptional iron and folic acid supplementation. Faseb Journal 2014;23(1):Abstract no: 917.6. [Google Scholar]
- Khambalia AZ, O'Connor DL, Macarthur C, Dupuis A, Zlotkin SH. Periconceptional iron supplementation does not reduce anemia or improve iron status among pregnant women in rural Bangladesh. American Journal of Clinical Nutrition 2009;90(5):1295‐302. [DOI] [PubMed] [Google Scholar]
Kulkarni 2010 {published data only}
- Kulkarni B, Christian P, LeClerq SC, Khatry SK. Determinants of compliance to antenatal micronutrient supplementation and women's perceptions of supplement use in rural Nepal. Public Health Nutrition 2010;13(1):82‐90. [DOI] [PubMed] [Google Scholar]
Kumar 2005 {published data only}
- Kumar A, Jain S, Singh NP, Singh T. Oral versus high dose parenteral iron supplementation in pregnancy. International Journal of Gynecology & Obstetrics 2005;89:7‐13. [DOI] [PubMed] [Google Scholar]
Lira 1989 {published data only}
- Lira P, Barrena N, Foradori A, Gormaz G, Grebe G. Folate deficiency in pregnancy: effect of supplementary folic acid [Deficienca de folatos en el embarazo: efecto de una suplementacion con acido folico]. Sangre 1989;34(1):24‐7. [PubMed] [Google Scholar]
Liu 1996 {published and unpublished data}
- Liu XN, Liu PY. The effectiveness of weekly iron supplementation regimen in improving the iron status of Chinese children and pregnant women. Biomedical and Environmental Sciences 1996;9:341‐7. [PubMed] [Google Scholar]
- Liu XN, Liu PY, Viteri FE. Individual patient data (as supplied December 2003). Data on file.
Ma 2008 {published data only}
- Ma AG, Schouten EG, Zhang FZ, Kok FJ, Yang F, Jiang DC, et al. Retinol and riboflavin supplementation decreases the prevalence of anemia in Chinese pregnant women taking iron and folic acid supplements. Journal of Nutrition 2008;138(10):1946‐50. [DOI] [PubMed] [Google Scholar]
Madan 1999 {published data only}
- Madan N, Prasannaraj P, Rusia U, Sundaram KR, Nath LM, Sood SK. Monitoring oral iron therapy with protoporphyrin/heme ratios in pregnant women. Annals of Hematology 1999;78(6):279‐83. [DOI] [PubMed] [Google Scholar]
Marin 2012 {published data only}
- Marin GH, Mestorino N, Errecalde J, Huber B, Uriarte A, Orchuela J. Personalised iron supply for prophylaxis and treatment of pregnant women as a way to ensure normal iron levels in their breast milk. Journal of Medicine & Life 2012;5(1):29‐32. [PMC free article] [PubMed] [Google Scholar]
Mbaye 2006 {published data only}
- Mbaye A, Richardson K, Balajo B, Dunyo S, Shulman C, Milligan P, et al. Lack of inhibition of the anti‐malarial action of sulfadoxine‐pyrimethamine by folic acid supplementation when used for intermittent preventive treatment in Gambian primigravidae. American Journal of Tropical Medicine & Hygiene 2006;74(6):960‐4. [PubMed] [Google Scholar]
McKenna 2002 {published data only (unpublished sought but not used)}
- McKenna D, Spence D, Dornan J. A randomised, double‐blind, placebo‐controlled trial investigating the place of spatone‐iron plus as a prophylaxis against iron deficiency in pregnancy [abstract]. Journal of Obstetrics and Gynaecology 2002;22(2 Suppl):S45. [Google Scholar]
- McKenna D, Spence D, Haggan SE, McCrum E, Dornan JC, Lappin TR. A randomised trial investigating an iron‐rich natural mineral water as a prophylaxis against iron deficiency in pregnancy. Clinical and Laboratory Haematology 2003;25(2):99‐103. [DOI] [PubMed] [Google Scholar]
Menon 1962 {published data only}
- Menon MKK, Rajan L. Prophylaxis of anaemia in pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1962;12:382‐9. [Google Scholar]
Metz 1965 {published data only}
- Baumslag N, Edelstein T, Metz J. Reduction of incidence of prematurity by folic acid supplementation in pregnancy. British Medical Journal 1970;1:16‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz J, Festenstein H, Welch P. Effect of folic acid and vitamin B12 supplementation on test of folate and Vitamin B12 nutrition in pregnancy. American Journal of Clinical Nutrition 1965;16:472‐9. [DOI] [PubMed] [Google Scholar]
Milman 2005 {published data only}
- Milman N, Bergholt T. Postpartum anemia ‐ Defining threshold hemoglobin values. International Journal of Gynecology and Obstetrics 2012;119(Suppl 3):S829. [Google Scholar]
- Milman N, Bergholt T, Eriksen L, Byg KE, Graudal N, Pedersen P, et al. Iron prophylaxis during pregnancy ‐ how much iron is needed? A randomized dose‐response study of 20‐80 mg ferrous iron daily in pregnant women. Acta Obstetricia et Gynecologica Scandinavica 2005;84:238‐47. [DOI] [PubMed] [Google Scholar]
- Milman N, Byg KE, Bergholt T, Eriksen L. Side effects of oral iron prophylaxis in pregnancy ‐ myth or reality?. Acta Haematologica 2006;115(1‐2):53‐7. [DOI] [PubMed] [Google Scholar]
- Milman N, Byg KE, Bergholt T, Eriksen L, Hvas AM. Body iron and individual iron prophylaxis in pregnancy ‐ should the iron dose be adjusted according to serum ferritin?. Annals of Hematology 2006;85(9):567‐73. [DOI] [PubMed] [Google Scholar]
Milman 2014 {published data only}
- Milman N, Jonsson L, Dyre P, Pedersen PL, Larsen LG. Ferrous bisglycinate 25 mg iron is as effective as ferrous sulfate 50 mg iron in the prophylaxis of iron deficiency and anemia during pregnancy in a randomized trial. Journal of Perinatal Medicine 2014;42(2):197‐206. [DOI] [PubMed] [Google Scholar]
Mitra 2012 {published data only}
- Mitra AK, Khoury AJ. Universal iron supplementation: a simple and effective strategy to reduce anaemia among low‐income, postpartum women. Public Health Nutrition 2012;15(3):546‐53. [DOI] [PubMed] [Google Scholar]
Morgan 1961 {published data only}
- Morgan EH. Plasma‐iron and haemoglobin levels in pregnancy. Lancet 1961;1:9‐12. [DOI] [PubMed] [Google Scholar]
- Morgan EH. Plasma‐iron and haemoglobin levels in pregnancy. Personal communication 1987 January 19.
Morrison 1977 {published data only}
- Morrison J, Bell J, Chang AMZ, Larkin PK. A comparative trial of haematinic supplements in pregnancy. Medical Journal of Australia 1977;1:482‐4. [DOI] [PubMed] [Google Scholar]
Mukhopadhyay 2004 {published data only}
- Mukhopadhyay A, Bhatla N, Kriplani A, Agarwal N, Saxena R. Erythrocyte indices in pregnancy: effect of intermittent iron supplementation. National Medical Journal of India 2004;17(3):135‐7. [PubMed] [Google Scholar]
- Mukhopadhyay A, Bhatla N, Kriplani A, Pandey RM, Saxena R. Daily versus intermittent iron supplementation in pregnant women: hematological and pregnancy outcome. Journal of Obstetrics and Gynaecology Research 2004;30(6):409‐17. [DOI] [PubMed] [Google Scholar]
Mumtaz 2000 {published data only}
- Mumtaz Z, Shahab S, Butt N, Rab MA, DeMuynck A. Daily iron supplementation is more effective than twice weekly iron supplementation in pregnant women in Pakistan in a randomized double‐blind clinical trial. Journal of Nutrition 2000;130(11):2697‐702. [DOI] [PubMed] [Google Scholar]
Nguyen 2008 {published data only}
- Gill SK, Nguyen P, Koren G. Adherence and tolerability of iron‐containing prenatal multivitamins in pregnant women with pre‐existing gastrointestinal conditions. Journal of Obstetrics and Gynaecology 2009;29(7):594‐8. [DOI] [PubMed] [Google Scholar]
- Nguyen P, Nava‐Ocampo A, Levy A, O'Connor DL, Einarson TR, Taddio A, et al. Effect of iron content on the tolerability of prenatal multivitamins in pregnancy. BMC Pregnancy and Childbirth 2008;8:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nogueira 2002 {published data only}
- Nogueira NDN, Macedo ADS, Parente JV, Cozzolino SMF. Nutritional profile of newborns of adolescent mothers supplemented with iron, in different concentrations, zinc and pholic acid. Revista de Nutricao 2002;15:193‐200. [Google Scholar]
- Nogueira Ndo N, Parente JV, Cozzolino SM. Changes in plasma zinc and folic acid concentrations in pregnant adolescents submitted to different supplementation regimens. Cadernos de Saude Publica 2003;19(1):155‐60. [DOI] [PubMed] [Google Scholar]
Ogunbode 1984 {published data only}
- Ogunbode O, Damole IO. Prophylaxis of anaemia in obstetric patients: administration of Ferrograd Folic 500 Plus compared with conventional iron and folic supplementation. Current Therapeutic Research, Clinical and Experimental 1984;35:1043‐8. [Google Scholar]
Ogunbode 1992 {published data only}
- Ogunbode O, Otubu JAM, Akeredolu OO, Akintunde EA, Olatunji PO, Jolayemi ET. The effect of Chemiron capsules on maternal and fetal hematologic indices, including birth weight. Current Therapeutic Research, Clinical and Experimental 1992;51:634‐46. [Google Scholar]
- Ogunbode O, Otubu JAM, Briggs ND, Adeleye JA. Chemiron ‐ A new hematinic preparation. How effective during pregnancy?. Current Therapeutic Research, Clinical & Experimental 1992;51:163‐73. [Google Scholar]
Ortega‐Soler 1998 {unpublished data only}
- Ortega‐Soler CR, Langini SH, Fleishman S, Lopez LB, Garcia M, Guntin R, et al. Iron nutritional status in pregnant women with and without iron supplementation [Estado nutricional con respecto al hierro (Fe) en gestantes con y sin suplementacion]. Personal communication 1998.
Osifo 1970 {published data only}
- Osifo BO. The effect of folic acid and iron in the prevention of nutritional anaemias in pregnancy in Nigeria. British Journal of Nutrition 1970;24(3):689‐94. [DOI] [PubMed] [Google Scholar]
Osrin 2005 {published data only}
- Adhikari R, Manandhar D, Costello A, Tompkins A, Filteau S, Osrin D, et al. The effects of antenatal multiple micronutrient supplementation on birthweight, gestation and infection: a double blind, randomised controlled trial conducted in Nepal: study protocol. MIRA Janakpur Multiple Micronutrient Supplementation 2003.
- Osrin D, Vaidya A, Shrestha Y, Baniya RB, Manandhar DS, Adhikari RK, et al. Effects of antenatal multiple micronutrient supplementation on birthweight and gestational duration in Nepal: double‐blind, randomised controlled trial. Lancet 2005;365:955‐62. [DOI] [PubMed] [Google Scholar]
Parkkali 2013 {published data only}
- Hemminki E. Routine iron prophylaxis during pregnancy (PROFEG). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 20 February 2008).
- Parkkali S, Abacassamo F, Nwaru BI, Salome G, Augusto O, Regushevskaya E, et al. Comparison of routine prenatal iron prophylaxis and screening and treatment for anaemia: Pregnancy results and preliminary birth results from a pragmatic randomised controlled trial (PROFEG) in Maputo, Mozambique. BMJ Open 2013;3(2):001948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkkali S, Abacassamo F, Salome G, Augusto O, Nikula M, on behalf of the PROFEG‐group. Routine iron prophylaxis during pregnancy. Effects on maternal and child health in Maputo City and the urban part of Maputo Province, Mozambique. Report of a pilot study. Profeg Group, 2007. [Google Scholar]
Payne 1968 {published data only}
- Payne RW. Prophylaxis of anaemia in pregnancy. Journal of the Royal College of General Practitioners 1968;16:353‐8. [PMC free article] [PubMed] [Google Scholar]
Peña‐Rosas 2003 {published data only}
- Pena‐Rosas JP, Nesheim M, Garcia‐Casal MN, Crompton DWT, Sanjur D, Viteri FE, et al. Intermittent iron supplementation regimens are able to maintain safe maternal hemoglobin concentrations during pregnancy in Venezuela. Journal of Nutrition 2004;134(5):1099‐104. [DOI] [PubMed] [Google Scholar]
Picha 1975 {published data only}
- Picha E. Iron treatment by effervescent tablets [Ein neuer Weg der Eisentherapie]. Geburtshilfe und Frauenheilkunde 1975;35(10):792‐5. [PubMed] [Google Scholar]
Pita Martin 1999 {published and unpublished data}
- Pita Martin de Portela ML. Personal communication 2004 March 22.
- Pita Martin de Portela ML, Langini SH, Fleischman S, Garcia M, Lopez LB, Guntin R, et al. Effect of iron supplementation and its frequency during pregnancy. Medicina 1999;59:430‐6. [PubMed] [Google Scholar]
Powers 1985 {published data only}
- Powers HJ, Bates CJ, Lamb WH. Haematological response to supplements of iron and riboflavin to pregnant and lactating women in rural Gambia. Human Nutrition. Clinical Nutrition 1985;39(2):117‐29. [PubMed] [Google Scholar]
Quintero 2004 {unpublished data only}
- Quintero Gutierrez AG, Gonzalez Rosendo G, Cedillo Espana F, Rivera‐Dommarco J. Single weekly iron supplementation in pregnant women. Personal communication 2004 February 17.
Rae 1970 {published data only}
- Rae PG, Robb PM. Megaloblastic anaemia of pregnancy: a clinical and laboratory study with particular reference to the total and labile serum folate levels. Journal of Clinical Pathology 1970;23:379‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramakrishnan 2003 {published data only}
- Ramakrishnan U, Gonzalez‐Cossio T, Neufeld LM, Rivera J, Martorell R. Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron‐only supplementation: a randomized controlled trial in a semirural community in Mexico. American Journal of Clinical Nutrition 2003;77(3):720‐5. [DOI] [PubMed] [Google Scholar]
Rayado 1997 {published data only}
- Rayado B, Carrillo JA, Fernandez‐Esteban JA, Gomez‐Cedillo A, Martin M, Coronel P. A comparative study of 2 ferrous proteins in the prevention of iron deficiency anaemia during pregnancy. Clinica e Investigacion en Ginecologia y Obstetricia 1997;24:46‐50. [Google Scholar]
Reddaiah 1989 {published data only}
- Reddaiah VP, Raj PP, Ramachandran K, Nath LM, Sood SK, Madan N, et al. Supplementary iron dose in pregnancy anemia prophylaxis. Indian Journal of Pediatrics 1989;56:109‐14. [DOI] [PubMed] [Google Scholar]
Ridwan 1996 {published and unpublished data}
- Ridwan E, Schultink W, Dillon D, Gross R. Effects of weekly iron supplementation on pregnant Indonesian women are similar to those of daily supplementation. American Journal of Clinical Nutrition 1996;63(6):884‐90. [DOI] [PubMed] [Google Scholar]
- Schultink W, Ridwan E, Dillon D, Gross R. Individual patient data (as supplied 12 January 2004). Data on file.
Robinson 1998 {published and unpublished data}
- Robinson JS. Individual patient data (as supplied 11 March 2004). Data on file.
- Robinson JS. Working with traditional birth attendants to improve iron tablet utilization by pregnant women. MotherCare Technical Working Paper #7. Arlington, VA 1998.
- Robinson JS, Sopacua J, Napitapulu J. Using traditional birth attendants to improve iron tablet utilization by pregnant women. Maluku Province, Indonesia. Draft paper. Mother Care Project. Project Concern International San Diego CA 1999.
- Robinson JS, Yip R. Weekly versus daily iron tablet supplementation in pregnant women in Indonesia. Draft paper 2000.
Rolschau 1979 {published data only}
- Rolschau J, Date J, Kristoffersen K. Folic acid supplement and intrauterine growth. Acta Obstetricia et GynecologicaScandinavica 1979;58:343‐6. [DOI] [PubMed] [Google Scholar]
Roth 1980 {published data only}
- Roth F, Mauracher E. Folic acid treatment during pregnancy [Folsauresubstitution bei schwangeren]. Geburtshilfe und Frauenheilkunde 1980;40:253‐8. [DOI] [PubMed] [Google Scholar]
Roztocil 1994 {published data only}
- Roztocil A, Charvatova M, Harastova L, Zahradkova J, Studenik P, Sochorova V, et al. Anti‐anemia therapy with prophylactic administration of fe2+ in normal pregnancy and its effect on prepartum hematologic parameters in the mother and neonate. Ceska Gynekologie 1994;59(3):130‐3. [PubMed] [Google Scholar]
Rukhsana 2006 {published data only}
- Rukhsana N, Bano H, Gurbakhshani AL, Dudani AL, Jafri TK, Mannan A. Changes in hemoglobin, red cell count, red cell indices and reticulocyte count in response to daily versus intermittent oral iron supplementation during pregnancy in local population. Medical Channel 2006;12(3):7‐10. [Google Scholar]
Rybo 1971 {published data only}
- Rybo G, Solvell L. Side‐effect studies on a new sustained release iron preparation. Scandinavian Journal of Hematology 1971;8(4):257‐64. [DOI] [PubMed] [Google Scholar]
Sachdeva 1993 {published data only}
- Sachdeva R, Mann SK. Impact of nutrition education and medical supervision on pregnancy outcome. Indian Pediatrics 1993;30(11):1309‐14. [PubMed] [Google Scholar]
Saha 2007 {published data only}
- Saha L, Pandhi P, Gopalan S, Malhotra S, Saha PK. Comparison of efficacy, tolerability, and cost of iron polymaltose complex with ferrous sulphate in the treatment of iron deficiency anemia in pregnant women. Medscape General Medicine 2007;9(1):1. [PMC free article] [PubMed] [Google Scholar]
Sandstad 2003 {published data only}
- Sandstad B, Borch‐Iohnson B, Andersen GM, Dahl‐Jorgensen B, Froysa I, Leslie C, et al. Selective iron supplementation based on serum ferritin values early in pregnancy: are the Norwegian recommendations satisfactory?. Acta Obstetricia et Gynecologica Scandinavica 2003;82:537‐42. [DOI] [PubMed] [Google Scholar]
Schoorl 2012 {published data only}
- Schoorl M, Schoorl M, Gaag D, Bartels P. Effects of iron supplementation on red blood cell haemoglobin content in pregnancy. Hematology Reports 2012;4(e24):91‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seck 2008 {published data only}
- Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutrition 2008;11(6):596‐605. [DOI] [PubMed] [Google Scholar]
- Seck BC, Jackson RT. Providing iron/folic acid tablets free of charge improves compliance in pregnant women in Senegal. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;103(5):485‐92. [DOI] [PubMed] [Google Scholar]
Shatrugna 1999 {published data only}
- Shatrugna V, Raman L, Kailash U, Balakrishna N, Rao KV. Effect of dose and formulation on iron tolerance in pregnancy. National Medical Journal of India 1999;12(1):18‐20. [PubMed] [Google Scholar]
Sinha 2011 {published data only}
- Sinha V, Dayal M, Mehrotra R, Mishra V. Intravenous iron sucrose versus oral ferrous ascorbate in the prevention of anaemia in pregnant women. 54th All India Congress of Obstetrics and Gynaecology; 2011 January 5‐9; Hyderabad, Andhra Pradesh, India. 2011:72.
Sjostedt 1977 {published data only}
- Sjostedt JE, Manner P, Nummi S, Ekenved G. Oral iron prophylaxis during pregnancy ‐ a comparative study on different dosage regimens. Acta Obstetricia et Gynecologica Scandinavica 1977;66:3‐9. [DOI] [PubMed] [Google Scholar]
Sood 1979 {published data only}
- Sood SK, Ramachandran K, Rani K, Ramalingaswami V, Mathan VI, Ponniah J, et al. WHO sponsored collaborative studies on nutritional anaemia in India. The effect of parenteral iron administration in the control of anaemia of pregnancy. British Journal of Nutrition 1979;42:399‐406. [DOI] [PubMed] [Google Scholar]
Srisupandit 1983 {published data only}
- Srisupandit S, Pootrakul P, Areekul S, Neungton S, Mokkaves J, Kiriwat O, et al. A prophylactic supplementation of iron and folate in pregnancy. Southeast Asian Journal of Tropical Medicine and Public Health 1983;14(3):317‐23. [PubMed] [Google Scholar]
Steer 1992 {published data only}
- Steer PJ. Trial to assess the effects of iron and folate supplementation on pregnancy outcome [trial abandoned]. Personal communication 1992.
Stone 1975 {published data only}
- Stone M, Elder MG. The relative merits of a slow‐release and a standard iron preparation during pregnancy. Current Medical Research and Opinion 1975;3:469‐72. [Google Scholar]
Swain 2011 {published data only}
- Swain S, Mahapatra PC, Majhi C, Das TK. Two doses of parenteral iron sucrose injection as anaemia prophylaxis in pregnancy. 54th All India Congress of Obstetrics and Gynaecology; 2011 January 5‐9; Hyderabad, Andhra Pradesh, India. 2011:181.
Tampakoudis 1996 {published data only}
- Tampakoudis P, Tantanassis T, Tsatalas K, Lazaridis E, Tsalikis T, Venetis C, et al. A randomized trial on the effect of oral supplementation with iron protein succinylate in singleton pregnancies. The role of maternal erythropoietin as a marker. Prenatal and Neonatal Medicine 1996;1 Suppl 1:181. [Google Scholar]
Tan 1995 {published data only}
- Tan CH, Ng KB. The effect of oral iron on the haemoglobin concentration during the second half of pregnancy. 27th British Congress of Obstetrics and Gynaecology 1995 July 4‐7; Dublin, Ireland. Royal College of Obstetricians & Gynaecologists, 1995:101.
Tange 1993 {published data only}
- Tange E, Weigand E, Mbofung CM. Effect of iron supplementation on anemic and non‐anemic pregnant teenagers in Cameroon. TEMA 8: Proceedings of the Eighth International Symposium on Trace Elements in Man and Animals; 1993 May 16‐22; Dresden, Germany. 1993:220‐3.
Thane‐Toe 1982 {published data only}
- Thane‐Toe, Thein‐Than. The effects of oral iron supplementation on ferritin levels in pregnant Burmese women. American Journal of Clinical Nutrition 1982;35(1):95‐9. [DOI] [PubMed] [Google Scholar]
Thomsen 1993 {published data only}
- Thomsen JK, Prien‐Larsen JC, Devantier A, Fogh‐Andersen N. Low dose iron supplementation does not cover the need for iron during pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1993;72:93‐8. [DOI] [PubMed] [Google Scholar]
Trigg 1976 {published data only}
- Trigg KH, Rendall EJC, Johnson A, Fellingham FR, Prankerd TAJ. Folate supplements during pregnancy. Journal of the Royal College of General Practitioners 1976;26(164):228‐30. [PMC free article] [PubMed] [Google Scholar]
Vogel 1963 {published data only}
- Vogel L, Steingold L, Suchet J. Iron therapy in the treatment of anaemia in pregnancy. Lancet 1963;1:1296‐9. [DOI] [PubMed] [Google Scholar]
Wali 2002 {published data only}
- Wali A, Mushtaq A, Nilofer. Comparative study‐‐efficacy, safety and compliance of intravenous iron sucrose and intramuscular iron sorbitol in iron deficiency anemia of pregnancy. Journal of the Pakistan Medical Association 2002;52(9):392‐5. [PubMed] [Google Scholar]
Weil 1977 {published data only}
- Weil A, Mauracher E. Folic acid and pregnancy, a real problem? [Acide folique et gravidité, problème réel?]. Schweizer Medizinische Wochenschrift 1977;107(52):1943‐7. [PubMed] [Google Scholar]
West 2014 {published data only}
- West K, Shamim A, Mehra S, Labrique A, Ali H, Shaikh S, et al. Effect of maternal multiple micronutrient vs iron–folic acid supplementation on infant mortality and adverse birth outcomes in rural Bangladesh. The JiVitA‐3 randomized trial. JAMA 2014;312(24):2649‐58. [DOI: 10.1001/jama.2014.16819] [DOI] [PubMed] [Google Scholar]
Willoughby 1966 {published data only}
- Willoughby M, Jewell F. Investigation of folic acid requirements in pregnancy. British Medical Journal 1966;2:1568‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Willoughby 1968 {published data only}
- Willoughby MLN, Jewell FG. Folate status throughout pregnancy and in postpartum period. British Medical Journal 1968;4:356‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winichagoon 2003 {unpublished data only}
- Winichagoon P, Lertmullikaporn N, Chitcumroonchokechai C, Thamrongwarangkul T. Daily versus weekly iron supplementation to pregnant women in rural northeast Thailand. Personal communication 2003.
Wu 1998 {published data only}
- Wu Y, Weng L, Wu L. Clinical experience with iron supplementation in pregnancy. Chung‐Hua Fu Chan Ko Tsa Chih [Chinese Journal of Obstetrics & Gynecology] 1998;33(4):206‐8. [PubMed] [Google Scholar]
Yecta 2011 {published data only}
- Yekta Z, Pourali R, Mladkova N, Ghasemi‐Rad M, Boromand F, Tappeh KH. Role of iron supplementation in promoting maternal and fetal outcome. Therapeutics and Clinical Risk Management 2011;7:421–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2000 {published data only}
- Young MW, Lupafya E, Kapenda E, Bobrow EA. The effectiveness of weekly iron supplementation in pregnant women of rural northern Malawi. Tropical Doctor 2000;30(2):84‐8. [DOI] [PubMed] [Google Scholar]
Young 2010 {published data only}
- Young MF, Griffin I, Pressman E, McIntyre AW, Cooper E, McNanley T, et al. Utilization of iron from an animal‐based iron source is greater than that of ferrous sulfate in pregnant and nonpregnant women. Journal of Nutrition 2010;140(12):2162‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yu 1998 {published and unpublished data}
- Yu KH, Yoon JS. The effect of weekly iron supplementation on iron and zinc nutritional status in pregnant women. Korean Journal of Nutrition 1998;31(8):1270‐82. [Google Scholar]
- Yu KH, Yoon, JS. Individual patient data (as supplied 11 March 2004). Data on file.
Zamani 2008 {published data only}
- Zamani AR, Farajzadegan Z, Ghahiri A, Khademloo M, Golshiri P. Effectiveness of twice weekly iron supplementation compared with daily regimen in reducing anemia and iron deficiency during pregnancy: a randomized trial in Iran. Journal of Research in Medical Sciences 2008;13(5):230‐9. [Google Scholar]
Zhou 2009 {published data only}
- Zhou SJ, Gibson RA, Crowther CA, Makrides M. Should we lower the dose of iron when treating anaemia in pregnancy? A randomized dose‐response trial. European Journal of Clinical Nutrition 2009;63(2):183‐90. [DOI] [PubMed] [Google Scholar]
Zutschi 2004 {published data only}
- Zutschi V, Batra S, Ahmad SS, Khera N, Chauhan G, Gandhi G, et al. Injectable iron supplementation instead of oral therapy for antenatal care. Journal of Obstetrics and Gynecology of India 2004;54(1):37‐8. [Google Scholar]
References to studies awaiting assessment
Parisi 2013 {published data only}
- Parisi F, Fuse F, Brunetti M, Mazzocco M, Berti C, Cetin I. Effects of different regimens of iron supplementation on iron status and pregnancy outcomes in a cohort of healthy pregnant women: a randomized control trial. Journal of Perinatal Medicine 2013;41(Suppl 1):Abstract no:595. [Google Scholar]
References to ongoing studies
Dibley 2012 {published data only}
- A trial to evaluate the impact of an early start to iron/folic acid supplementation in pregnancy on deaths of newborns in rural Bangladesh. Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) (accessed 2 July 2012) 2012.
Fawzi 2010 {published data only}
- Fawzi W. Prenatal iron supplements: safety and efficacy in Tanzania. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 12 November 2010) 2010.
Hamzehgardeshi 2009 {published data only}
- Hamzehgardeshi Z. A randomized placebo‐controlled trial to determine the effect of iron supplementation on hematological indices in pregnant women with hemoglobin ≥13.2 g/dl. IRCT Iranian Registry of Clinical Trials (www.irct.ir) (accessed 6 December 2010) 2010.
Jafarbegloo 2010 {published data only}
- Jafarbegloo E. Gastrointestinal complications of iron supplement in pregnant women. IRCT Iranian Registry of Clinical Trials (www.irct.ir) (accessed 6 December 2010) 2010.
Mwangi 2011 {published data only}
- Mwangi MN. A randomised trial to assess the safety and efficacy or iron supplementation in Kenyan pregnant women. ClinicalTrials.gov (http://clinicaltrials.gov) (accessed 11 March 2011) 2011.
- Mwangi MN, Andang'o PEA, Mwangi AM, Verhoef H, Savelkoul H. Safety and efficacy of fortification versus fortification plus supplementation with iron in African pregnant women: A randomised controlled trial. Annals of Nutrition and Metabolism 2013;63(Suppl):1162‐1163. [Google Scholar]
Ramakrishnan 2012 {published data only}
- Ramakrishnan U. Impact of pre‐pregnancy micronutrient supplementation on maternal and child outcomes. http://clinicaltrials.gov/ct2/show/record/NCT01665378 (accessed 20 September 2012) 2012.
Zhao 2014 {published data only}
- Zhao G. Impact of iron/folic acid versus folic acid supplements during pregnancy on maternal and children's health: a randomized controlled trial in China. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 27 August 2014] 2014.
Additional references
Andersen 2006
- Andersen HS, Gambling L, Holtrop G, McArdle HJ. Maternal iron deficiency identifies critical windows for growth and cardiovascular development in the rat postimplantation embryo. Journal of Nutrition 2006;136(5):1171‐7. [DOI] [PubMed] [Google Scholar]
Balshem 2010
- Balshem H, Helfanda M, Schunemann HJ, Oxman AD, Kunze R, Brozek J, et al. GRADE guidelines: rating the quality of evidence: introduction. Journal of Clinical Epidemiology 2010;64(4):401‐6. [DOI] [PubMed] [Google Scholar]
BCSH 2011
- British Committee for Standards in Haematology. UK guidelines on the management of iron deficiency in pregnancy. Vol. (http://www.bcshguidelines.com/documents/UK_Guidelines_iron_deficiency_in_pregnancy.pdf, accessed on 18 May 2015), London: British Society for Haematology, 2011. [Google Scholar]
Beard 2000
- Beard J. Effectiveness and strategies of iron supplementation during pregnancy. American Journal of Clinical Nutrition 2000;71(5):1288S‐1294S. [DOI] [PubMed] [Google Scholar]
Beaton 1999
- Beaton GH, McCabe G. Efficacy of intermittent iron supplementation in the control of iron deficiency anaemia in developing countries. An analysis of experience. Ottawa: The Micronutrient Initiative, 1999. [Google Scholar]
Beaton 2000
- Beaton GH. Iron needs during pregnancy: do we need to rethink our targets?. American Journal of Clinical Nutrition 2000;72(1 Suppl):265S‐271S. [DOI] [PubMed] [Google Scholar]
Bhutta 2008
- Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet 2008;371(9610):417‐40. [DOI] [PubMed] [Google Scholar]
Black 2011
- Black M, Quigg A, Hurley K, Pepper M. Iron deficiency and iron‐deficiency anemia in the first two years of life: strategies to prevent loss of developmental potential. Nutrition Reviews 2011;69(Suppl 1):S64‐S70. [DOI] [PubMed] [Google Scholar]
Bothwell 1981
- Bothwell TH, Charlton RW, editors. Iron Deficiency in Women. Washington DC: Nutrition Foundation, 1981. [Google Scholar]
Bothwell 2000
- Bothwell TH. Iron requirements in pregnancy and strategies to meet them. American Journal of Clinical Nutrition 2000;72(1 Suppl):257S‐264S. [DOI] [PubMed] [Google Scholar]
Burke 2014
- Burke R, Leon J, Suchdev P. Identification, prevention and treatment of iron deficiency during the first 1000 days. Nutrients 2014;6(10):4093‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cantor 2015
- Cantor AG, Bougatsos C, Dana T, Blazina I, McDonagh M. Routine iron supplementation and screening for iron deficiency anemia in pregnancy: a systematic review for the U.S. Preventive Services Task Force. Annals of Internal Medicine 2015;162(8):566‐76. [DOI] [PubMed] [Google Scholar]
CDC 1998
- Centers for Disease Control and Prevention. Recommendations to prevent and control iron deficiency in the United States. Morbidity and Mortality Weekly Report 1998;47(RR‐3):1‐29. [PubMed] [Google Scholar]
Christian 2010
- Christian P. Micronutrients, birth weight, and survival. Annual Review of Nutrition 2010;30:83‐104. [DOI] [PubMed] [Google Scholar]
Cook 2003
- Cook JD, Flowers CH, Skikne BS. The quantitative assessment of body iron. Blood 2003;101(9):3359‐64. [DOI] [PubMed] [Google Scholar]
Crompton 2002
- Crompton DW, Nesheim MC. Nutritional impact of intestinal helminthiasis during the human life cycle. Annual Review of Nutrition 2002;22:35‐59. [DOI] [PubMed] [Google Scholar]
De‐Regil 2010
- De‐Regil LM, Fernández‐Gaxiola AC, Dowswell T, Peña‐Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database of Systematic Reviews 2010, Issue 10. [DOI: 10.1002/14651858.CD007950.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Garcia‐Casal 2014
- Garcia‐Casal MN, Peña‐Rosas JP, Pasricha SR. Rethinking ferritin cutoffs for iron deficiency and overload. Lancet Hematology 2014;1:e92‐e94. [DOI] [PubMed] [Google Scholar]
Garn 1981
- Garn SM, Ridella SA, Petzold AS, Falkner F. Maternal hematologic levels and pregnancy outcomes. Seminars in Perinatology 1981;5:155‐62. [PubMed] [Google Scholar]
Gleason 2007
- Gleason G, Scrimshaw NS. An overview of the functional significance if iron deficiency. In: Kraemer K, Zimmermann MB editor(s). Nutritional Anemia. Vol. 1, Basel, Switzerland: Sight and Life, 2007:45‐58. [Google Scholar]
Godfrey 1991
- Godfrey KM, Redman CW, Barker DJ, Osmond C. The effect of maternal anaemia and iron deficiency on the ratio of fetal weight to placental weight. British Journal of Obstetrics and Gynaecology 1991;98(9):886‐91. [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro. [Computer program on www.gradepro.org]. Version 2015. McMaster University, 2014.
Haider 2012
- Haider BA, Bhutta ZA. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD004905.pub3] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hunt 2002
- Hunt JM. Reversing productivity losses from iron deficiency: the economic case. Journal of Nutrition 2002;132(4 Suppl):794S‐801S. [DOI] [PubMed] [Google Scholar]
Hytten 1964
- Hytten FE, Leitch I. The Physiology of Human Pregnancy. Oxford: Blackwell Scientific Publications, 1964:14. [Google Scholar]
Hytten 1971
- Hytten FE, Leitch I, Baird D. The Physiology of Human Pregnancy. 2nd Edition. Oxford: Blackwell Scientific Publications, 1971. [Google Scholar]
Imdad 2012
- Imdad A, Bhutta ZA. Routine iron/folate supplementation during pregnancy: effect on maternal anaemia and birth outcomes. Paediatric and Perinatal Epidemiology 2012;26 (Suppl. 1):168–77. [DOI] [PubMed] [Google Scholar]
INACG 1998
- Stoltzfus R, Dreyfuss M. Guidelines for the use of iron supplements to prevent and treat iron deficiency anaemia. Washington DC: ILSI Press, 1998. [Google Scholar]
INACG 2002a
- International Nutritional Anemia Consultative Group. Anemia, iron deficiency and iron deficiency anemia. INACG, 2002. [Google Scholar]
INACG 2002b
- International Nutritional Anemia Consultative Group (INACG). Why is iron important and what to do about it: a new perspective. Report of the 2001 INACG Symposium; 2001 February 15‐16; Hanoi, Vietnam. 2002:1‐50.
IOM 2001
- Institute of Medicine. Iron. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington DC: National Academy Press, 2001:290‐393. [PubMed] [Google Scholar]
Kandoi 1991
- Kandoi A, Bhatia BD, Pandey LK, Pandey S, Sen PC, Satya K. Cellular immunity status in anaemia in pregnancy. Indian Journal of Medical Research 1991;94:11‐5. [PubMed] [Google Scholar]
Kim 1992
- Kim I, Hungerford DW, Yip R, Kuester SA, Zyrkowski C, Trowbridge FL. Pregnancy nutrition surveillance system‐‐United States, 1979‐1990. Morbidity and Mortality Weekly Report 1992;41(7):25‐41. [PubMed] [Google Scholar]
Klebanoff 1989
- Klebanoff MA, Shiono PH, Berendes HW, Rhoads GG. Facts and artifacts about anemia and preterm delivery. JAMA 1989;262(4):511‐5. [PubMed] [Google Scholar]
Klebanoff 1991
- Klebanoff MA, Shiono PH, Selby JV, Trachtenberg AI, Graubard BI. Anemia and spontaneous preterm birth. American Journal of Obstetrics and Gynecology 1991;164(1):59‐63. [DOI] [PubMed] [Google Scholar]
Langendam 2013
- Langendam MW, Akl EA, Dahm P, Glasziou P, Guyatt G, Schünemann HJ. Assessing and presenting summaries of evidence in Cochrane Reviews. Systematic Reviews 2013;2:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lassi 2013
- Lassi ZS, Salam RA, Haider BA, Bhutta ZA. Folic acid supplementation during pregnancy for maternal health and pregnancy outcomes. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD006896.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lozoff 2006
- Lozoff B, Jimenez E, Smith JB. Double burden of iron deficiency in infancy and low socioeconomic status: a longitudinal analysis of cognitive test scores to age 19 years. Archives of Pediatrics & Adolescent Medicine 2006;160(11):1108‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lutter 2011
- Lutter CK, Daelmans BM, Onis M, Kothari MT, Ruel MT, Arimond M, et al. Undernutrition, poor feeding practices, and low coverage of key nutrition interventions. Pediatrics 2011;128(6):e1418‐e1427. [DOI] [PubMed] [Google Scholar]
Mahomed 1997
- Mahomed K. Folate supplementation in pregnancy. Cochrane Database of Systematic Reviews 1997, Issue 3. [DOI: 10.1002/14651858.CD000183] [DOI] [PubMed] [Google Scholar]
McDonald 2013
- McDonald SJ, Middleton P, Dowswell T, Morris PS. Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD004074.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mei 2011
- Mei Z, Cogswell ME, Looker AC, Pfeiffer CM, Cusick SE, Lacher DA, et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999‐2006. American Journal of Clinical Nutrition 2011;93(6):1312‐20. [DOI] [PubMed] [Google Scholar]
Milman 2007
- Milman N, Bergholt T, Byg KE, Eriksen L, Hvas AM. Reference intervals for haematological variables during normal pregnancy and postpartum in 434 healthy Danish women. European Journal of Haematology 2007;79(1):39‐46. [DOI] [PubMed] [Google Scholar]
Mora 2002
- Mora JO. Iron supplementation: overcoming technical and practical barriers. Journal of Nutrition 2002;132(4 Suppl):853S‐855S. [DOI] [PubMed] [Google Scholar]
Murphy 1986
- Murphy JF, O'Riordan J, Newcombe RG, Coles EC, Pearson JF. Relation of haemoglobin levels in first and second trimesters to outcome. Lancet 1986;3(1):992‐5. [DOI] [PubMed] [Google Scholar]
Nagata 2011
- Nagata JM, Gatti LR, Barg FK. Social determinants of iron supplementation among women of reproductive age: asystematic review of qualitative data. Maternal Child Nutrition 2012;8(1):1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nair 2004
- Nair KM, Bhaskaram P, Balakrishna N, Ravinder P, Sesikeran B. Response of hemoglobin, serum ferritin, and serum transferrin receptor during iron supplementation in pregnancy: a prospective study. Nutrition 2004;20(10):896‐9. [DOI] [PubMed] [Google Scholar]
Nel 2015
- Nel E, Kruger H, Baumgartner J, Faber M, Smuts C. Differential ferritin interpretation methods that adjust for inflammation yield discrepant iron deficiency prevalence. Maternal and Child Nutrition 2015; Vol. Epub ahead of print. [DOI] [PMC free article] [PubMed]
NIH 2011
- NIH Iron and Malaria Technical Working Group. Chapter 2: Mechanisms. In: Raiten D, Namaste S, Brabin B editor(s). Considerations for the Safe and Effective Use of Iron Interventions. Bethesda: Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), 2011 (in press):16‐51. [Google Scholar]
Nisar 2014
- Nisar Y, Dibley M, Mir A. Factors associated with non‐use of antenatal iron and folic acid supplements among Pakistani women: a cross sectional household survey. BMC Pregnancy and Childbirth 2014;14:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oppenheimer 2001
- Oppenheimer SJ. Iron and its relation to immunity and infectious disease. Journal of Nutrition 2001;131:616S‐635S. [DOI] [PubMed] [Google Scholar]
Parker 2012
- Parker JA, Barroso F, Stanworth SJ, Spiby H, Hopewell S, Doree CJ, et al. Gaps in the evidence for prevention and treatment of maternal anaemia: a review of systematic reviews. BMC Pregnancy Childbirth 2012;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pasricha 2014
- Pasricha SR, Low M, Thompson J, Farrell A, De‐Regil LM. Iron supplementation benefits physical performance in women of reproductive age: a systematic review and meta‐analysis. Journal of Nutrition 2014;144(6):906‐14. [DOI] [PubMed] [Google Scholar]
Peña‐Rosas 2012a
- Peña‐Rosas JP, De‐Regil LM, Dowswell T, Viteri FE. Intermittent oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD009997] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prema 1982
- Prema K, Ramalakshmi BA, Madhavapeddi R, Babu S. Immune status of anaemic pregnant women. British Journal of Obstetrics and Gynaecology 1982;89:222‐5. [DOI] [PubMed] [Google Scholar]
Rabe 2012
- Rabe H, Diaz‐Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD003248.pub3] [DOI] [PubMed] [Google Scholar]
Ramakrishnan 2013
- Ramakrishnan U, Grant FK, Imdad A, Bhutta ZA, Martorell R. Effect of multiple micronutrient versus iron‐folate supplementation during pregnancy on intrauterine growth. Nestle Nutrition Institute Workshop Series 2013;74:53‐62. [DOI] [PubMed] [Google Scholar]
Reveiz 2011
- Reveiz L, Gyte GM, Cuervo LG, Casasbuenas A. Treatments for iron‐deficiency anaemia in pregnancy. Cochrane Database of Systematic Reviews 2011, Issue 10. [DOI: 10.1002/14651858.CD003094.pub3] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sanghvi 2010
- Sanghvi T, Harvey P, Wainwright E. Maternal iron‐folic acid supplementation programs: evidence of impact and implementation. Food & Nutrition Bulletin 2 2010;31(Suppl 2):S100‐S107. [DOI] [PubMed] [Google Scholar]
Scholl 1992
- Scholl TO, Hediger, ML, Fischer RL, Shearer JW. Anaemia vs. iron deficiency: increased risk of preterm delivery in a prospective study. American Journal of Clinical Nutrition 1992;55:985‐8. [DOI] [PubMed] [Google Scholar]
Scholl 1997
- Scholl TO, Hediger ML, Bendich A, Schall JI, Smith WK, Krueger PM. Use of multivitamin/mineral prenatal supplements: influence on the outcome of pregnancy. American Journal of Epidemiology 1997;146:134‐41. [DOI] [PubMed] [Google Scholar]
Scholl 1998
- Scholl TO. High third‐trimester ferritin concentration: associations with very preterm delivery, infection, and maternal nutritional status. Obstetrics & Gynecology 1998;92:161‐6. [DOI] [PubMed] [Google Scholar]
Scholl 2000
- Scholl TO, Reilly T. Anemia, iron and pregnancy outcome. Journal of Nutrition 2000;130(Suppl 2):443S‐447S. [DOI] [PubMed] [Google Scholar]
Scholl 2005
- Scholl TO. Iron status during pregnancy: setting the stage for mother and infant. American Journal of Clinical Nutrition 2005;81(5):1218S‐1222S. [DOI] [PubMed] [Google Scholar]
Schümann 2007
- Schümann K, Ettle T, Szegner B, Elsenhans B, Solomons NW. On risks and benefits of iron supplementation recommendations for iron intake revisited. Journal of Trace Elements in Medicine and Biology 2007;21(3):147‐68. [DOI] [PubMed] [Google Scholar]
Shrimptom 2009
- Shrimpton R, Huffman SL, Zehner ER, Darnton‐Hill I, Dalmiya N. Multiple micronutrient supplementation during pregnancy in developing‐country settings: policy and program implications of the results of a meta‐analysis. Food and Nutrition Bulletin 2009;30(4Suppl):S556‐S573. [DOI] [PubMed] [Google Scholar]
Sloan 2002
- Sloan NL, Jordan E, Winikoff B. Effects of iron supplementation on maternal hematologic status in pregnancy. American Journal of Public Health 2002;92(2):288‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steer 2000
- Steer PJ. Maternal hemoglobin concentration and birth weight. American Journal of Clinical Nutrition 2000;71(5 Suppl):1285S‐1287S. [DOI] [PubMed] [Google Scholar]
Van den Broek 2010
- Broek N, Dou L, Othman M, Neilson JP, Gates S, Gülmezoglu AM. Vitamin A supplementation during pregnancy for maternal and newborn outcomes. Cochrane Database of Systematic Reviews 2010, Issue 11. [DOI: 10.1002/14651858.CD008666.pub2] [DOI] [PubMed] [Google Scholar]
Villar 1997
- Villar J, Bergsjo P. Scientific basis for the content of routine antenatal care. I. Philosophy, recent studies and power to eliminate or alleviate adverse maternal outcomes. Acta Obstetricia et Gynecologica Scandinavica 1997;76(1):1‐14. [DOI] [PubMed] [Google Scholar]
Villar 2003
- Villar J, Merialdi M, Gulmezoglu AM, Abalos E, Carroli G, Kulier R, et al. Nutritional interventions during pregnancy for the prevention or treatment of maternal morbidity and preterm delivery: an overview of randomized controlled trials. Journal of Nutrition 2003;5(Suppl 2):1606S‐1625S. [DOI] [PubMed] [Google Scholar]
WHO 1959
- World Health Organization. Iron Deficiency Anaemias: Report of a WHO study group. WHO Technical Report Series #182. Geneva: World Health Organization, 1959. [PubMed] [Google Scholar]
WHO 1968
- World Health Organization. Nutritional Anaemias: Report of a WHO Scientific Group: WHO Technical Report Series #405. Geneva: World Health Organization, 1968. [PubMed] [Google Scholar]
WHO 1992
- World Health Organization. The Prevalence of Anaemia in Women: a Tabulation of Available Information. 2nd Edition. Geneva: World Health Organization, 1992. [Google Scholar]
WHO 2001
- World Health Organization. Iron Deficiency Anaemia Assessment Prevention and Control: a Guide For Program Managers. Geneva: World Health Organization, 2001. [Google Scholar]
WHO 2008
- World Health Organization. The International Pharmacopoeia. (http://apps.who.int/phint/en/p/about/) (accessed 2008) 2008.
WHO 2010
- World Health Organization. Malaria. In: Poumerol G, Wilder‐Smith A editor(s). Malaria. International Travel and Health. Situation as on 1 January 2010. Geneva: World Health Organization, 2010. [Google Scholar]
WHO 2011a
- World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. http://www.who.int/iris/bitstream/10665/85839/http://apps.who.int//iris/bitstream/10665/85839/3/WHO_NMH_NHD_MNM_11.1_eng.pdf?ua=1 (accessed 18 May 2015) 2011.
WHO 2011b
- World Health Organization. Serum ferritin concentrations for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System (WHO/NMH/NHD/MNM/11.2) (http://www.who.int/vmnis/indicators/ferritin/en/index.html (accessed April 29 2011) 2011.
WHO 2011c
- World Health Organization. E‐book International Travel and Health 2011 (PDF format). Geneva: World Health Organization, 2011. [Google Scholar]
WHO 2012a
- World Health Organization. Guideline: daily iron and folic acid supplementation in pregnant women. (http://apps.who.int/iris/bitstream/10665/77770/1/9789241501996_eng.pdf, accessed 18 May 2015) 2012. [PubMed]
WHO 2012b
- World Health Organization. WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
WHO 2014a
- World Health Organization. Serum transferrin receptor levels for the assessment of iron status and iron deficiency in populations. Vitamin and Mineral Nutrition Information System (WHO/NMH/NHD/MNM/14.6). (http://apps.who.int/iris/bitstream/10665/133707/1/WHO_NMH_NHD_EPG_14.6_eng.pdf?ua=1, accessed 18 May 2015) 2014.
WHO 2014b
- World Health Organization. Guideline: delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. (http://www.who.int/iris/bitstream/10665/148793/http://apps.who.int//iris/bitstream/10665/148793/1/9789241508209_eng.pdf, accessed 18 May 2015) 2014. [PubMed]
WHO 2014c
- World Health Organization. World Malaria Report 2014. (http://apps.who.int/iris/bitstream/10665/144852/2/9789241564830_eng.pdf, accessed 18 May 2015) 2014.
WHO 2015a
- World Health Organization. Serum and red blood cell folate concentrations for assessing folate status in populations. Vitamin and Mineral Nutrition Information System (WHO/NMH/NHD/EPG/15.01). (http://www.who.int/iris/bitstream/10665/162114/http://apps.who.int//iris/bitstream/10665/162114/1/WHO_NMH_NHD_EPG_15.01.pdf, accessed 18 May 2015) 2015.
WHO 2015b
- World Health Organization. Global prevalence of anaemia in 2011. Geneva: World Health Organization, 2015. [Google Scholar]
WHO/CDC 2005
- World Health Organization, Centers for Disease Control and Prevention. Assessing the iron status of populations. Report of a Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level. Geneva, Switzerland: World Health Organization and Centers for Disease Control and Prevention, 2005:1‐30. [Google Scholar]
Xiong 2000
- Xiong X, Buekens P, Alexander S, Demianczuk N, Wollast E. Anemia during pregnancy and birth outcome: a meta‐analysis. American Journal of Perinatology 2000;17(3):137‐46. [DOI] [PubMed] [Google Scholar]
Yakoob 2011
- Yakoob MY, Bhutta ZA. Effect of routine iron supplementation with or without folic acid on anemia during pregnancy. BMC Public Health 2011;11 Suppl 3:S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 1998
- Zhou LM, Yang WW, Hua JZ, Deng CQ, Tao X, Stoltzfus RJ. Relation of hemoglobin measured at different times in pregnancy to preterm birth and low birth weight in Shanghai, China. American Journal of Epidemiology 1998;148(10):998‐1006. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Mahomed 1998b
- Mahomed K. Iron and folate supplementation in pregnancy. Cochrane Database of Systematic Reviews 1998, Issue 3. [DOI: 10.1002/14651858.CD001135] [DOI] [PubMed] [Google Scholar]
Mahomed 2000a
- Mahomed K. Iron supplementation in pregnancy. Cochrane Database of Systematic Reviews 2000, Issue 1. [DOI: 10.1002/14651858.CD000117] [DOI] [PubMed] [Google Scholar]
Mahomed 2006a
- Mahomed K. Iron supplementation in pregnancy. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD000117.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mahomed 2006b
- Mahomed K. Iron and folate supplementation in pregnancy. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD001135.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peña‐Rosas 2004
- Peña‐Rosas JP, Viteri FE, Mahomed K. Oral iron supplementation with or without folic acid for women during pregnancy. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD004736] [DOI] [PubMed] [Google Scholar]
Peña‐Rosas 2006
- Peña‐Rosas JP, Viteri FE. Effects of routine oral iron supplementation with or without folic acid for women during pregnancy. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004736.pub2] [DOI] [PubMed] [Google Scholar]
Peña‐Rosas 2009
- Peña‐Rosas JP, Viteri FE. Effects and safety of preventive oral iron or iron+folic acid supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD004736.pub3] [DOI] [PubMed] [Google Scholar]
Peña‐Rosas 2012
- Peña‐Rosas JP, De‐Regil LM, Dowswell T, Viteri FE. Daily oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD004736.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


