Abstract
OBJECTIVE
The Environmental Determinants of Diabetes in the Young (TEDDY) study is uniquely capable of investigating age-specific differences associated with type 1 diabetes. Because age is a primary driver of heterogeneity in type 1 diabetes, we sought to characterize by age metabolic derangements prior to diagnosis and clinical features associated with diabetic ketoacidosis (DKA).
RESEARCH DESIGN AND METHODS
The 379 TEDDY children who developed type 1 diabetes were grouped by age at onset (0–4, 5–9, and 10–14 years; n = 142, 151, and 86, respectively) with comparisons of autoantibody profiles, HLAs, family history of diabetes, presence of DKA, symptomatology at onset, and adherence to TEDDY protocol. Time-varying analysis compared those with oral glucose tolerance test data with TEDDY children who did not progress to diabetes.
RESULTS
Increasing fasting glucose (hazard ratio [HR] 1.09 [95% CI 1.04–1.14]; P = 0.0003), stimulated glucose (HR 1.50 [1.42–1.59]; P < 0.0001), fasting insulin (HR 0.89 [0.83–0.95]; P = 0.0009), and glucose-to-insulin ratio (HR 1.29 [1.16–1.43]; P < 0.0001) were associated with risk of progression to type 1 diabetes. Younger children had fewer autoantibodies with more symptoms at diagnosis. Twenty-three children (6.1%) had DKA at onset, only 1 (0.97%) of 103 with and 22 (8.0%) of 276 children without a first-degree relative (FDR) with type 1 diabetes (P = 0.008). Children with DKA were more likely to be nonadherent to study protocol (P = 0.047), with longer duration between their last TEDDY evaluation and diagnosis (median 10.2 vs. 2.0 months without DKA; P < 0.001).
CONCLUSIONS
DKA at onset in TEDDY is uncommon, especially for FDRs. For those without familial risk, metabolic monitoring continues to provide a primary benefit of reduced DKA but requires regular follow-up. Clinical and laboratory features vary by age at onset, adding to the heterogeneity of type 1 diabetes.
Introduction
Worldwide, >1.1 million children and adolescents are estimated to have type 1 diabetes, with >132,000 new cases each year (1). β-cell dysfunction, insulinopenia, and metabolic derangement are known pathophysiologic disturbances of this disease, with the most severe presentation, diabetic ketoacidosis (DKA), occurring in more than a third of newly diagnosed pediatric patients (2,3). Following islet autoantibody seroconversion, metabolic changes have been demonstrated to occur in the months and years prior to diabetes onset (4–10). Therefore, early glucose abnormalities (e.g., dysglycemia) are used in differentiation of stages of type 1 diabetes and enrollment in prevention clinical trials (11). However, age is a well-known factor accounting for heterogeneity in the rate of decline in β-cell function and disease progression (12). Therefore, variation in clinical and laboratory characteristics at diabetes onset within age groups may contribute to our understanding of disease progression and identify additional features present in those with a more severe clinical presentation, such as DKA at onset.
We examined age variant categories (0–4, 5–9, and 10–14 years) and family history, HLAs, autoantibody profiles, and widely available metabolic and β-cell function markers (glucose and insulin) along with occurrence of DKA in participants in The Environmental Determinants of Diabetes in the Young (TEDDY) study. TEDDY is a large international cohort of genetically high-risk children followed since birth. Such characterization may allow better understanding of variability of presentation of type 1 diabetes in children and which children might be at risk for developing DKA at onset. This analysis could promote design of immune and omics studies to better understand these differences, while continuing to highlight the benefits of screening and frequency of monitoring for type 1 diabetes risk.
Research Design and Methods
Participants and Monitoring
TEDDY participants were tested at, or shortly after, birth for high-risk HLA genotypes. The study screened newborns from the general population and among first-degree relatives (FDRs) of those with type 1 diabetes (13). This large cohort of children from four countries (Finland, Germany, Sweden, and the U.S.) were followed every 3 months from age 3 months to 4 years and then every 3–6 months based on autoantibody status until the age of 15 years or diabetes onset (14). Oral glucose tolerance tests (OGTTs) were completed every 6 months in participants with two or more autoantibodies starting at age 3 years. The TEDDY OGTT consists of only two time points (0 and 120 min) and collects glucose, insulin, and C-peptide (15). Children with two or more recorded OGTTs during follow-up were included in the analysis. Dysglycemia is defined during an OGTT as fasting plasma glucose of 5.6–6.9 mmol/L (100–125 mg/dL) or 2-h plasma glucose of 7.8–11.0 mmol/L (140–199 mg/dL). Markers of insulin sensitivity were assessed: fasting glucose-to-insulin ratio (glucose in mmol/L and insulin in μIU/mL) and HOMA-IS (22.5/[fasting insulin in μIU/mL ∗ fasting glucose in mmol/L]). BMI thresholds for underweight (<5th percentile) were based on WHO standards (https://www.who.int/childgrowth/en/) and overweight and obese thresholds determined by the International Obesity Task Force (derived from international databases and linked with adult BMI cutoffs for overweight and obese) (16). Children <2 years of age were excluded from BMI measurement (n = 34).
Genetic Risk and Autoantibodies
PCR-based genotyping was performed at birth to categorize HLA class II DR-DQ genetic risk. The highest risk categories were HLA-DR-DQ 3-2/4-8 (DR3/4), HLA-DR-DQ 4-8/4-8 (DR4/4), HLA-DR-DQ 4-8/8-4 (DR4/8), HLA-DR3/3 (DR3/3), and additional HLA categories for FDR eligibility. FDR-specific HLAs include DR4/1, DR4/9, DR4/13, DR3/9, DR4/4-DQB1*20×, and DR4/4-DQB1*304 (13), which were evaluated separately because these children have a familial increase in risk that is not common in the general population of children in TEDDY.
Measurement of insulin autoantibodies (IAAs), GAD autoantibodies (GADAs), and insulinoma-associated antigen 2 autoantibodies was done per previously reported protocols at two separate laboratories (14,17). Zinc transporter 8 autoantibodies was added in January 2012, and results were available for all participants who developed diabetes. Islet autoantibody positivity was based on persistent autoantibodies at two consecutive visits confirmed by both laboratories. The date of first confirmed autoantibody presence was then used for analysis.
Diagnosis Data Collection Including DKA Reporting
The diagnosis of diabetes, using American Diabetes Association criteria (14), was documented in a standardized form by TEDDY clinicians. DKA at diagnosis was captured through report of direct laboratory measurement of pH/bicarbonate levels or free-text response from a physician or medical provider as to the presence of DKA. Demographic information, symptoms at diagnosis, and continuation in monitoring were collected.
Statistical Analysis
Age categories were based on clinically useful categories and historical age groups commonly used in the type 1 diabetes literature (18–20): early childhood (0–4 years), school-age (5–9 years), and early adolescence (10–14 years). Adherence to protocol prior to diagnosis was defined as whether or not a child was lost to follow-up (LTFU) or withdrew (WD) and never rejoined the study prior to diagnosis with diabetes. Fisher exact test or χ2 test was used to compare proportional/binary differences. For the clinical features, comparisons in median value between age groups were performed using Mann-Whitney U test. Incidence of type 1 diabetes and DKA was described as a rate per 1,000 person-years. Exact 95% CIs for the incidence rates were calculated using the χ2 relationship assuming a Poisson distribution. Estimated rate differences were assessed using a log-linked Poisson model with an offset to account for different observation periods for different participants. Stratified multivariable Cox proportional hazards models were used to assess risk of diabetes in those with persistent confirmed autoantibodies adjusted for age at time of initial autoantibody seroconversion and country of residence. For metabolic measures, change from first recorded OGTT on risk of progression to type 1 diabetes was assessed longitudinally using time-varying multivariate Cox proportional hazards models in those children eligible for OGTT collection. We also assessed age effects on the change in OGTT measure from baseline to progression to type 1 diabetes using an interaction term in the modeling. Additionally, glucose impairment, defined as the first impaired fasting or stimulated recorded measure, was evaluated from time from first glucose impairment to progression to type 1 diabetes using a stratified Cox proportional hazards model. Multivariate models were adjusted for age at baseline OGTT, baseline recorded OGTT measure, months since two or more positive autoantibodies, combination of first persistent autoantibodies, sex, HLA DR-DQ genotype, and family history of type 1 diabetes at birth unless otherwise noted. Data were analyzed using Statistical Analysis System Software (version 9.4; SAS Institute, Cary, NC) and GraphPad PRISM (version 7.04; GraphPad Software, Inc., San Diego, CA) for figures. Two-tailed P values <0.05 were considered significant.
Results
Demographics, HLAs, and Autoantibody Profiles of TEDDY Participants Who Developed Diabetes
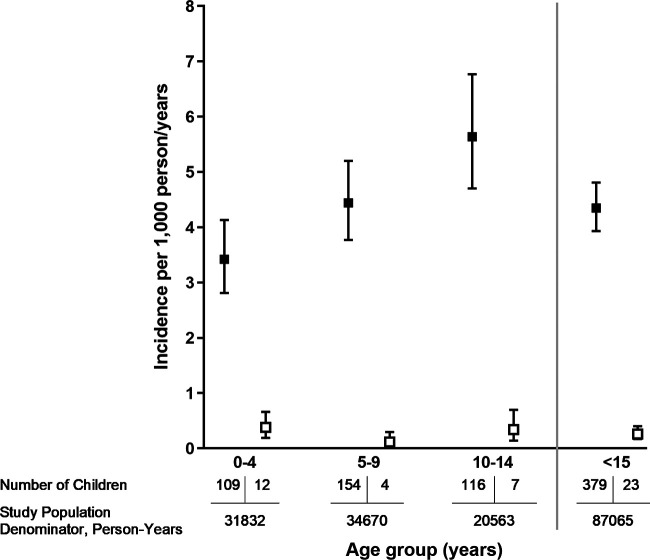
The TEDDY study screened 424,788 newborns in the general population and in families with type 1 diabetes from September 2004 to February 2010 and enrolled 8,676 newborns. There were 8,502 enrolled HLA-eligible children with autoantibody data available. As of 31 July 2020, 379 (4.46%) children had developed type 1 diabetes and are the focus of this analysis (Supplementary Fig. 1). A random glucose level (as compared with fasting glucose or 2-h glucose following OGTT) was most commonly used to diagnose diabetes across all ages (49.2%) (P < 0.0001). At the time of this analysis, the TEDDY participants had surpassed 10 years of age, with a median age of 12.9 years (interquartile range 11.6–14.1) at the most recent visit. The children who developed diabetes had a significantly different HLA distribution as compared with those who did not in the TEDDY study (P < 0.0001). Proportional differences in clinical and laboratory features by age group are presented in Table 1, with clear differences by age at onset. Overall incidence of type 1 diabetes was 4.35 cases per 1,000 person-years (95% CI 3.93–4.81). Type 1 diabetes incidence by age group (cases [95% CI] per 1,000 person-years) was as follows: 3.42 (2.81–4.13) in those age 0–4.99 years, 4.44 (3.77–5.20) in those age 5–9.99 years, and 5.64 (4.66–6.77) in those age 10–14.99 years (Fig. 1). Children 0–4 years of age had a significantly lower incidence of diabetes as compared with children age 5–9 (P = 0.038) and 10–14 years (P = 0.0002). Incidence of type 1 diabetes for children without an FDR was lower at 3.55 (95% CI 3.14–3.99) compared with 11.13 (9.09–13.50) cases per 1,000 person-years in those with an FDR across all age groups (P < 0.001) (Supplementary Fig. 2). The FDR excess risk was highest in children age 0–4 years, with the highest proportion of paternal type 1 diabetes in this age group.
Table 1.
Demographics of the TEDDY cohort diagnosed with type 1 diabetes as of 31 July 2020
| Type 1 diabetes | P * | ||||
|---|---|---|---|---|---|
| None (n = 8,123) | Age 0–4 years (n = 142) | Age 5–9 years (n = 151) | Age 10–14 years (n = 86) | ||
| Female sex | 4,017 (49.5) | 70 (49.3) | 68 (45.0) | 36 (41.9) | 0.53 |
| FDR | 797 (9.81) | 48 (33.8) | 34 (22.5) | 21 (24.4) | 0.08 |
| Family member with T1D at screening | 0.06 | ||||
| Mother | 308 (3.8) | 10 (7.0) | 6 (4.0) | 9 (10.5) | |
| Father | 394 (4.9) | 28 (19.1) | 16 (10.6) | 7 (8.1) | |
| Sibling | 95 (1.2) | 10 (7.0) | 12 (7.9) | 5 (5.8) | |
| N by site† | 0.021 | ||||
| Colorado | 1,272 (15.7) | 20 (14.1) | 28 (18.5) | 20 (23.3) | |
| Georgia/Florida | 908 (11.2) | 8 (5.6) | 16 (10.6) | 8 (9.3) | |
| Washington | 1,299 (16.0) | 14 (9.9) | 15 (9.9) | 8 (9.3) | |
| Finland | 1,703 (21.0) | 44 (31.0) | 35 (23.2) | 22 (25.6) | |
| Germany | 535 (6.6) | 25 (17.6) | 9 (6.0) | 5 (5.8) | |
| Sweden | 2,397 (29.5) | 31 (21.8) | 48 (31.8) | 23 (26.7) | |
| HLA | <0.0001 | ||||
| DR3/4 | 3,108 (38.3) | 78 (54.9) | 84 (55.6) | 48 (55.8) | |
| DR4/4 | 1,592 (19.6) | 16 (11.3) | 36 (23.8) | 17 (19.8) | |
| DR4/8 | 1,420 (17.5) | 18 (12.7) | 18 (11.9) | 12 (13.9) | |
| DR3/3 | 1,749 (21.5) | 17 (12.0) | 10 (6.6) | 6 (7.0) | |
| FDR specific‡ | 254 (3.1) | 13 (9.1) | 3 (2.0) | 3 (3.5) | |
| N of autoantibodies at diagnosis or last clinical visit | 0.0002 | ||||
| 0 | 7,613 (93.7) | 15 (10.6) | 16 (10.6) | 10 (11.6) | |
| 1 | 289 (3.6) | 17 (12.0) | 8 (5.3) | 5 (5.8) | |
| 2 | 77 (0.95) | 37 (26.1) | 16 (10.6) | 15 (17.4) | |
| 3 | 67 (0.82) | 42 (29.6) | 40 (26.5) | 18 (20.9) | |
| 4 | 77 (0.95) | 31 (21.8) | 71 (47.0) | 38 (44.2) | |
| DKA at diagnosis | 13 (9.2) | 4 (2.6) | 6 (7.0) | 0.06 | |
| Symptoms at diagnosis | |||||
| Symptomatic (yes) | 92(64.8) | 73(48.3) | 42(48.8) | 0.017 | |
| Polydipsia (yes) | 71(59.2) | 57(50.9) | 30(53.6) | 0.41 | |
| Polyphagia (yes) | 4(3.3) | 10(9.0) | 2(3.6) | 0.44 | |
| Polyuria (yes) | 75(62.5) | 61(54.5) | 37(66.1) | 0.020 | |
| Hospitalized (yes) | 112(78.9) | 107(70.9) | 50(58.1) | 0.005 | |
| N reporting weight loss | 31 | 28 | 18 | 0.0006 | |
| Median (IQR) | 0.80 (0.40–1.40) | 1.33 (0.89–2.39) | 2.00 (0.90–3.00) | ||
| Median (IQR) age at diagnosis, years | 2.79 (1.79–4.08) | 7.77 (6.43–8.92) | 11.51 (10.73–12.56) | <0.0001 | |
| Enrollment status at diagnosis | 0.048 | ||||
| Regular visits/on study | 127 (89.4) | 123 (81.5) | 65 (75.6) | ||
| LTFU/WD | 15 (10.6) | 28 (18.5) | 21 (24.4) | ||
T1D, type 1 diabetes.
P value of comparison for each characteristic among children diagnosed with type 1 diabetes before 5, between 5 and 9, and between 10 and 14 years of age.
Seven children are followed in the U.S. at auxiliary sites located at the Children’s Hospital of Pittsburgh and the Naomi Berrie Diabetes Center.
FDR-specific HLA DR-DQ genotypes (DR4/1, DR4/9, DR4/13, DR3/9, DR4/4-DQB1*20×, and DR4/4-DQB1*304).
Figure 1.
Incidence of type 1 diabetes in TEDDY children (n = 379, solid box) and DKA incidence (open box) by age group. Number of children and study population denominator displayed below each group.
Type 1 diabetes incidence (cases [95% CI] per 1,000 person-years) among those with at least one persistent confirmed autoantibody was 70.29 (58.64–83.57) in those with IAAs first, 42.87 (34.39–52.82) in those with GADAs first, and 156.31 (128.10–188.88) in those with multiple autoantibodies first (Supplementary Fig. 3). Incidence of type 1 diabetes varied by the first appearing autoantibody, with the highest incidence in children with multiple autoantibodies (P < 0.001) versus either GADAs or IAAs first, while there was no significant difference if IAAs or GADAs were first (P = 0.31) after adjusting for age at seroconversion. There was no significant difference by FDR status (paternal, maternal, or sibling) in whether IAAs or GADAs were present first after adjusting for age at time of seroconversion. Autoantibodies were not identified in 41 (10.8%) of the 379 children who developed diabetes. Thirty-seven of these children had WD from TEDDY or were LTFU (age 0–4 years, n = 11; 5–9, n = 16; 10–14, n = 10). Four children in the 0–4 years age group were enrolled and either were autoantibody negative at diagnosis or did not meet the TEDDY definition of persistent confirmed autoantibody positivity. Of the remaining 338 of 379 children diagnosed, 68.3% had one confirmed autoantibody at initial seroconversion, with only 8.9% having a single autoantibody at diagnosis (7 of the 30 single autoantibody–positive children at diagnosis WD or were LTFU). At diagnosis, 17.9%, 26.4%, and 36.9% of participants had two, three, or four autoantibodies, respectively. Those diagnosed at a younger age had proportionally fewer autoantibodies, and those diagnosed at an older age were more likely to have four autoantibodies, as shown in Table 1.
Characteristics of TEDDY Participants Who Developed DKA
Incidence of DKA, which occurred in 23 children, varied by country (cases [95% CI] per 1,000 person-years), with Sweden (0.11 [0.02–0.31]) having a lower rate as compared with the U.S. (0.40 [0.22–0.67]; P = 0.038) and Germany (0.55 [0.11–1.61]; P = 0.045). Finland (0.16 [0.03–0.47]; P = 0.62) had a similar rate to Sweden; however, there were no significant differences compared with the other countries. Those in the youngest age group (0–4 years) in our study had a higher incidence of DKA (0.38 [0.19–0.66]) compared with those age 5–9 years (0.12 [0.03–0.30]; P = 0.040), but not with those age 10–14 years (0.34 [0.14–0.70]; P = 0.83) (Fig. 1). Symptoms at diabetes onset were more likely to be present in the youngest group compared with the older groups (64.8% vs. 48.3% and 48.8%, respectively; P = 0.024). All children who presented with DKA reported at least one symptom at onset.
Twenty-three episodes of DKA at onset (6.1%) were present, with 16 documented as mild-moderate DKA (pH ≥7.1 and <7.3), six as severe DKA (pH <7.1), and one without laboratory confirmation available. A majority, ∼60% of cases, occurred in the U.S. Table 2 details the 23 participants with DKA. HLA DR3/4 was the most prevalent haplotype (n = 14 [60.9%] of 23) among those who presented with DKA. Of those with DKA at diagnosis, only one (4.3%) of the 23 children had an FDR with type 1 diabetes (majority were non-FDR), compared with 102 (28.7%) with an FDR of 356 without DKA at diagnosis (P = 0.008). Nine (39.1%) of the 23 children with DKA at the time of type 1 diabetes diagnosis were autoantibody negative/unknown; seven of these nine children WD or were LTFU from the study at a median (interquartile range [IQR]) of 6.1 (1.9–7.3) years prior to diagnosis. Additionally, two of the 23 children with DKA did not meet the TEDDY definition of persistent confirmed autoantibody positivity.
Table 2.
Characteristics of the 23 DKA cases at diabetes diagnosis in TEDDY
| Age at diagnosis of T1D, years | Age at last clinical visit, years | Clinic | HLA | Race and ethnicity | Age at seroconversion, years | First appearing AAb | N of AAbs confirmed and persistent at seroconversion (0, 1, 2, 3, 4) | N of AAbs confirmed and persistent at diagnosis (0, 1, 2, 3, 4) | Enrolled or WD or LTFU (WD) | DKA severity (mild/moderate, severe, or unknown) | Polydipsia | Polyphagia | Polyuria | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.69 | 0.69 | Finland | DR3/4 | Non-Hispanic White | 0.50 | None | 0 | 0* | E | Severe | Unknown | Unknown | Unknown |
| 2 | 0.87 | 0.87 | WA | DR4/8 | Non-Hispanic White | 0.81 | GADAs, IAAs | 2 | 2 | E | Mild/moderate | Yes | No | Yes |
| 3 | 0.90 | 0.90 | Sweden | DR3/4 | Unknown | 0.54 | IAAs | 1 | 1 | E | Severe | Yes | Unknown | Yes |
| 4 | 0.97 | 0.97 | Sweden | DR3/4 | Unknown | 0.76 | GADAs, IAAs | 2 | 2 | E | Mild/moderate | Yes | No | Yes |
| 5 | 1.22 | 1.22 | CO | DR4/8 | Hispanic | 1.22 | IAAs | 1 | 1 | E | Severe | Yes | No | Yes |
| 6 | 1.43 | 1.43 | CO | DR3/4 | Hispanic | 1.29 | IAAs | 1 | 1 | E | Mild/moderate | Yes | No | Yes |
| 7 | 2.32 | 2.32 | Finland | DR3/4 | Non-Hispanic White | 1.85 | GADAs, IAAs | 2 | 3 | E | Mild/moderate | Yes | No | Yes |
| 8 | 2.47 | 2.47 | Germany | DR3/4 | Non-Hispanic White | 1.01 | GADAs, IAAs | 2 | 2 | E | Mild/moderate | Yes | No | Yes |
| 9 | 2.67 | 0.28 | WA | DR3/4 | Unknown | 0.28 | None | 0 | 0 | WD | Mild/moderate | Yes | Unknown | Yes |
| 10 | 3.07 | 1.75 | WA | DR3/4 | Hispanic | 1.10 | None | 0 | 0 | WD | Mild/moderate | Yes | Unknown | Yes |
| 11 | 3.38 | 3.38 | WA | DR4/4 | Non-Hispanic White | 2.53 | None | 0 | 0 | E | Mild/moderate | Yes | Yes | Yes |
| 12 | 3.92 | 1.42 | WA | DR3/4 | African American | 1.38 | None | 0 | 0 | WD | Mild/moderate | Yes | No | Yes |
| 13 | 4.99 | 4.99 | Germany | DR3/3 | Non-Hispanic White | 1.54 | GADAs | 1 | 4 | E | Mild/moderate | Unknown | Unknown | Unknown |
| 14 | 8.74 | 8.74 | Germany | DR4/4 | Non-Hispanic White | 8.74 | IA-2As, IAAs | 2 | 2 | WD | Mild/moderate | Yes | No | Yes |
| 15 | 8.92 | 8.92 | CO | DR3/4 | Hispanic | 0.25 | None | 0 | 0 | WD | Mild/moderate | Yes | Yes | Yes |
| 16 | 9.20 | 9.20 | CO | DR4/4 | Hispanic | 0.27 | None | 0 | 0 | WD | Mild/moderate | Yes | No | Yes |
| 17 | 9.86 | 9.86 | CO | DR3/4 | Hispanic | 6.46 | GADAs | 1 | 1 | E | Severe | Yes | No | Yes |
| 18 | 10.30 | 3.11 | FL/GA | DR3/4 | Non-Hispanic White | 2.74 | None | 0 | 0 | WD | Severe | Yes | Unknown | Yes |
| 19 | 10.61 | 10.61 | CO | DR3/4 | Hispanic | 6.24 | GADAs, ZnT8As | 2 | 4 | E | Mild/moderate | Yes | No | Yes |
| 20 | 10.87 | 10.87 | Finland | DR3/4 | Non-Hispanic White | 10.87 | GADAs, IA-2As | 2 | 2 | E | Mild/moderate | Yes | No | Yes |
| 21 | 11.31 | 11.31 | WA | DR4/8 | Other | 11.31 | IAAs | 1 | 1 | E† | Severe | Yes | No | Yes |
| 22 | 11.33 | 11.33 | Sweden | DR4/4 | Unknown | 0.75 | IAAs | 1 | 4 | WD | Mild/moderate | Yes | Unknown | Yes |
| 23 | 13.54 | 5.09 | WA | DR4/8 | Non-Hispanic White | 4.72 | None | 0 | 0* | WD | Mild/moderate | Yes | No | Yes |
AAb, autoantibody; E, enrolled; T1D, type 1 diabetes; ZnT8A, Zinc transporter 8 autoantibody.
Did not meet the TEDDY definition of persistent confirmed autoantibody positivity.
Participant WD from TEDDY then rejoined (enrolled) prior to T1D diagnosis.
Weight loss was reported in ∼20% of the 379 children diagnosed with type 1 diabetes (median [IQR] weight loss 1.0 [0.7–2.2] kg). In the children who presented with DKA at onset, 56.5% (n = 13 of 23) reported a median (IQR) weight loss of 2.0 (1.4–5.0) kg. None who developed DKA were overweight or obese at the time of diagnosis, and three were underweight (eight were age <2 years or missing BMI data). Of those diagnosed with diabetes with BMI information available (n = 306 of 379), 14.4% were overweight, 4.9% were obese, and 5.2% were underweight. Thirty-two percent were overweight or obese in the 10–14 years age group. The oldest participant diagnosed with DKA was 13 years of age, with 87% of the children with DKA ≤10 years of age.
Incidence of DKA among those who did not adhere to the protocol (cases [95% CI] per 1,000 person-years) was higher (0.48 [0.22–0.91]) than among those who did adhere (0.20 [0.11–0.34]; P = 0.047). Of the 23 children with DKA, 12 (52.2%) had not had a blood draw within TEDDY in >7 months, and nine children (39.1%) WD or were LTFU. The median time between the last blood draw and diagnosis visit within TEDDY was 10.2 months (IQR 2.3–37.1) compared with 2.0 months (IQR 0.7–3.5) for the 356 participants without DKA at diagnosis (P < 0.001). Adherence with regular visits in the children who were diagnosed with type 1 diabetes was achieved by 83.1% of participants (higher in the younger age groups) (P = 0.05).
Between 31 January and 31 July 2020, the coronavirus disease 2019 pandemic escalated in severity in all countries involved in TEDDY. During this time, 11 patients presented with type 1 diabetes within TEDDY and none presented with DKA. The median time since the last TEDDY visit in these children diagnosed with diabetes was 2.1 months (IQR 0.7–5.9), and the median (IQR) weight loss was 2.2 (1.3–3.0) kg.
OGTT Metabolic Changes Associated With Progression to Type 1 Diabetes
We assessed if a change in metabolic measure from the first OGTT affected the risk of progression to type 1 diabetes. Specifically, fasting (0-min) and stimulated (120-min) glucose, fasting insulin, glucose-to-insulin ratio, and HOMA-IS were evaluated. Given the paucity of OGTT data in children <5 years of age, only those age >4 years were assessed in this analysis of metabolic markers. Two or more OGTTs were collected during follow-up in 65.6% (n = 345 of 526) of the eligible children >4 years of age; 48.4% (n = 167 of 345) of these children were diagnosed with type 1 diabetes. OGTT eligible children (n = 345) who progressed to type 1 diabetes had fewer recorded OGTTs during follow-up [median (IQR) 7 (4–11) vs. 9 (6–13), P = 0.001]. The overall median (IQR) age at the first OGTT was 61.1 (44.1–94.7) months, with a median (IQR) of 6.0 (3.4–11.6) months after development of two or more positive autoantibodies.
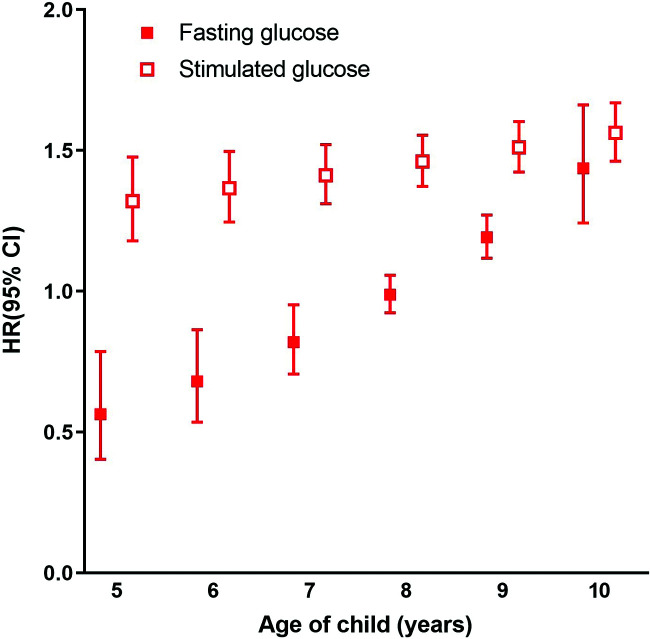
An increase of one unit from baseline (i.e., first OGTT in TEDDY) in fasting glucose, stimulated glucose, or glucose-to-insulin ratio and a decrease of one unit in fasting insulin were significantly associated with risk of progression to type 1 diabetes in the subset of eligible children with serial OGTT data. Age heterogeneity was observed for change from baseline fasting glucose (P < 0.0001 for interaction) and stimulated glucose (P = 0.008 for interaction) with regard to risk of progression to type 1 diabetes. As age increased, a change from baseline fasting and stimulated glucose was associated with an increasing risk of progression to type 1 diabetes (Fig. 2). There was no significant difference by age for fasting insulin and glucose-to-insulin ratio with regard to progression.
Figure 2.
Age-specific HRs (with 95% CIs) associated with a one-unit increase in either fasting glucose (solid box) or 120-min stimulated blood glucose (open box) with regard to progression of type 1 diabetes. The risk of progression to type 1 diabetes was constant over time (age) for baseline levels of fasting and stimulated glucose.
Overall, an increase of one unit from baseline in fasting glucose (hazard ratio [HR] 1.09 [95% CI 1.04–1.14]; P = 0.0003), stimulated glucose (HR 1.50 [1.42–1.59]; P < 0.0001), or glucose-to-insulin ratio (HR 1.29 [1.16–1.43]; P < 0.0001) was associated with an increased risk of progression to type 1 diabetes. An increase of one unit in fasting insulin from baseline was associated with an 11% lower risk of progression to type 1 diabetes (HR 0.89 [0.83–0.95]; P = 0.0009), accounting for age at baseline OGTT, baseline recorded OGTT measure, months since two or more positive autoantibodies, combination of first persistent autoantibodies, sex, HLA DR-DQ genotype, and family history of type 1 diabetes at birth. No significant interactive age effects were noted for baseline fasting (P = 0.10) or stimulated glucose (P = 0.99) or glucose-to-insulin ratio (P = 0.33) on type 1 diabetes risk. However, a higher baseline fasting glucose (HR 1.60 [1.11–2.32]; P = 0.013), stimulated glucose (HR 1.96 [1.70–2.27]; P < 0.0001), or glucose-to-insulin ratio (HR 1.20 [1.03–1.39]; P = 0.016) was associated with an increased risk of progression to type 1 diabetes. Baseline fasting insulin was not shown to be significantly associated with progression (P = 0.17). Change from baseline or baseline HOMA-IS was not found to be associated with progression. Longitudinal OGTT measurements demonstrated marked variability over time. Median values for fasting glucose, stimulated glucose, and glucose-to-insulin ratio were higher, while fasting insulin values were lower, for children who progressed to type 1 diabetes (Supplementary Fig. 4).
Furthermore, in these children with reported OGTT metabolic measures, impaired fasting glucose (5.6–6.9 mmol/L) and impaired glucose tolerance (2-h glucose 7.8–11.0 mmol/L) were present in 48.1% (n = 166 of 345). Combined, dysglycemia was present in 69.9% (n = 241 of 345) of the all children and in 85% (n = 142 of 167) of those who progressed to type 1 diabetes, at a median (IQR) time from first presentation of dysglycemia of 1.58 (0.96–3.04) years prior to diagnosis. Glucose impairment (fasting or stimulated) was associated with a >5.5-fold increased risk of progression to type 1 diabetes from first dysglycemic presentation (HR 5.52 [95% CI 3.50–8.81]; P < 0.0001).
Children with two or more recorded OGTTs (n = 345), as compared with those without (no OGTT, n = 133; only one OGTT, n = 48), had a longer follow-up (median [IQR] 134.7 (104.6–155.4) vs. 109.9 (54.0–143.1) months; P < 0.0001), were more likely to be male (P = 0.038), were more likely not have a family history of type 1 diabetes (P < 0.001), were less likely to be from Germany (P < 0.0001), and were less likely to carry the FDR-specific HLA DR-DQ genotypes (P < 0.0001). Overall, this population with OGTT data was less likely to represent those who are FDRs of individuals with type 1 diabetes.
Conclusions
Type 1 diabetes incidence increased 3–4% annually in the late 20th century, with the greatest increase in the youngest children (5.4% increase in those age 0–4 years) (21). Children who develop autoantibodies and progress to type 1 diabetes early in life have less functional β-cell mass (22) and higher rates of DKA at diagnosis (23). However, children who are closely monitored have significantly lower rates of DKA than the general population (24,25). We analyzed differences in age, genetic, autoantibody, and metabolic profiles among TEDDY children who developed type 1 diabetes and characteristics associated with DKA at diagnosis.
Genetic predisposition accounts for up to 50% of known type 1 diabetes risk, with predominant risk from HLA class II genotype variants (26). The proportion of HLA DR3/4, the highest risk haplotype, was similar across all age groups in our study and different from those in the TEDDY cohort who did not develop diabetes. Overall, however, the genetic profiles varied between age groups among those who developed type 1 diabetes. Genetic heterogeneity may explain some of the phenotypic variation within type 1 diabetes presentation. Additionally, those diagnosed in the youngest age group were more likely to be an FDR. While FDR status (mother, father, or sibling) was not significantly different by age of onset in this study, the Finnish Pediatric Diabetes Register observational study demonstrated a younger age at onset when the FDR was a parent compared with a sibling but did not find a significant difference in age at onset between familial and sporadic cases (27). While paternal type 1 diabetes has an increased risk of proband type 1 diabetes (27–29), we found the highest proportion of paternal FDRs in those diagnosed between age 0 and 4 years. However, the type of FDR did not influence the type of first-appearing autoantibody. The incidence of type 1 diabetes was highest for those presenting with multiple autoantibodies as first appearance of autoantibodies as compared with either IAAs or GADAs first.
Early age of islet autoantibody development and risk of type 1 diabetes have been well assessed in pediatric studies (30–32). The frequency of IAA positivity at initial seroconversion decreased with increasing age category. In our study, a majority of participants initially presented with a single autoantibody but progressed to multiple autoantibodies by the time of diagnosis, with only 7.9% remaining single autoantibody positive at diagnosis. Children diagnosed at younger ages have, by definition, less time to develop autoantibodies, and as such, we observed four autoantibodies at diagnosis more often in older children. Autoantibody seroconversion may not have been captured in all participants because 23% of single autoantibody–positive participants WD or were LTFU. Furthermore, a majority (90%) of autoantibody-negative children WD or were LTFU.
Time leading up to diabetes onset is marked by rising glucose levels, waning insulin production, and reduced β-cell glucose sensitivity (33). Time-varying analysis identified that an increase in glucose (fasting or 120-min), an increase in glucose-to-insulin ratio, or a decrease in fasting insulin in longitudinally collected OGTTs increased the risk of type 1 diabetes progression, irrespective of age (analysis only in those age >4 years). Metabolic values (fasting glucose, stimulated glucose, or glucose-to-insulin ratio) at first OGTT occurrence in TEDDY were also associated with risk of progression.
While metabolic markers can fluctuate up and down from visit to visit, their absolute increase over time was found to increase the risk of progression. This risk increased with each year from age 5 to 10 years as the fasting glucose and stimulated glucose rose one unit from baseline. A metabolic marker in combination with a marker of β-cell function may provide increased specificity of risk across many ages. In our study, a glucose-to-insulin ratio (fasting) at first measurement and increase over time were associated with risk of progression to type 1 diabetes, along with fasting and 120-min glucose measures. Multiple measures that include fasting and stimulated values may be of benefit for monitoring at-risk children, because the DPT-1 study, which recruited patients as young as 3 years of age (median age 11 years), demonstrated impaired β-cell function following stimulus but normal β-cell function in the fasting state (34). However, both a random plasma glucose ≥7.8 mmol/L (140 mg/dL) and dysglycemia as part of an OGTT were found to predict the onset of type 1 diabetes in the DIPP study (35). In addition, a 10% increase in HbA1c was shown to be associated with an approximate sixfold increased risk of progression to type 1 diabetes in TEDDY children (36). Furthermore, this study supports the need for physiologic studies to better understand the mechanisms contributing to insulin sensitivity and insulin deficiency prior to diabetes onset. While a number of TEDDY-collected variables have been studied as part of efforts to improve type 1 diagnosis prediction models, metabolic data remain somewhat limited and are often not included (37).
The main strength of this analysis is that TEDDY is a large prospective observational study that collects clinical data, including metabolic markers, on children at genetically high risk for type 1 diabetes every 3–6 months in those who develop islet autoimmunity. This granularity provides a clearer picture of the variability of clinical measures leading up to diagnosis with type 1 diabetes. However, the primary limitation of this analysis is the use of the two–time point OGTT (0 and 120 min) in TEDDY. Additional metabolic measures could not be applied, because a six-point OGTT was not collected. C-peptide response (30–0 min C-peptide) or combined glucose and C-peptide markers (e.g., Index60, which combines fasting and 60-min measures from an OGTT) may offer more refined risk of diabetes progression (2,38). A very high metabolic risk marker, such as these, may be a sign of imminent progression. There were fewer participants with OGTT data as a result of the burden of collection (especially in those age <3 years who are not eligible for an OGTT per protocol), making direct comparisons difficult. Small numbers of children developed DKA, also inhibiting statistical comparisons. Other limitations of the study include the fact that not all participants have reached the clinical end point of 15 years (or diabetes diagnosis), but all participants have surpassed age 10 years. Also, it is important to remember that the TEDDY population is a genetically preselected group with high-risk HLAs, and findings may not be generalizable to the entire population, because these HLA predispose, in general, to an earlier age at diagnosis. The TEDDY study does, however, include children with and without relatives with type 1 diabetes, similar to the frequency reported by most countries. Newer population-based efforts to screen for autoantibodies (e.g., Global Platform for the Prevention of Autoimmune Diabetes in Europe) include additional type 1 diabetes–related single nucleotide polymorphisms that increase the risk of islet autoimmunity in addition to the presence of class II HLAs (39). While race and ethnicity are not categorized consistently across TEDDY sites, the generalizability of these results across racial and ethnic groups would need further evaluation.
Early detection of diabetes and the prevention of DKA are the hallmarks of prospective monitoring studies, and this continues to be a positive outcome of the TEDDY study, with only 6% of children diagnosed with type 1 diabetes presenting with DKA compared with >30% in U.S. youth and adults (3,40). The rate of DKA is known to vary widely by country, at 12–21% in Finland, Sweden, and Germany (41–43). Those countries that have lower rates of DKA within TEDDY also have lower population rates of DKA (24). While all participants in the TEDDY monitoring program are educated on the symptoms of diabetes and the risk of DKA, those with first-hand experience may be more attuned to and suspicious of new symptoms and may be performing spontaneous home glucose monitoring, which may account for the lower rate of DKA in those with an FDR. An alarming increase in DKA has been seen over the years (40). TEDDY and other prospective studies have been able to diagnose children and adults earlier in the disease course (24,25,44). Furthermore, the prevention of DKA can improve long-term outcomes (45,46). Higher DKA rates in the youngest children, who have the highest risk of mortality, were again corroborated.
Children followed in accordance with the TEDDY protocol have a lower frequency of DKA compared with children who WD from the study, were LTFU, or had longer time between visits. Because more than half of children with DKA had not been seen in TEDDY in >7 months, semiannual OGTTs could be proposed for monitoring genetically high-risk children. Of note, outside of scheduled OGTTs, maintaining consistent phone contact and promoting community awareness also remain essential in preventing DKA. The benefit of monitoring is significantly lower if adequate follow-up is not maintained. Until a successful prevention therapy becomes standard of care, the main goal of monitoring studies, beyond enhancing our understanding of the natural history of the disease, remains to decrease the morbidity and mortality associated with unexpected new-onset type 1 diabetes. Within TEDDY, the rate of DKA is markedly reduced, with the tradeoff of some parental anxiety around positive autoantibody test results and the risk of type 1 diabetes (47).
Additional anxieties may be at play during major stresses, such as a global pandemic. As with any disease that can become life threatening if unrecognized, the concern among the medical community is that families may delay seeking health care and the rates of DKA could increase further. Since the coronavirus disease 2019 pandemic started, there have been variable data on the rate of type 1 diabetes reported in the literature, with increased cases, no change, and decreased cases of type 1 diabetes all reported (48–50). Unfortunately, during the pandemic, an increased rate of DKA has been reported in children with newly diagnosed type 1 diabetes in the German Diabetes Prospective Follow-up Registry (51). However, in the prospective TEDDY study, there did not appear to be an increase in the number of cases or in DKA between 31 January and 31 July 2020, but larger data collection over longer periods of time is required for conclusive results. Public health initiatives, including the use of telemedicine, must continue to provide education regarding the symptoms of diabetes to avoid delays in treatment and the risk of life-threatening DKA.
In conclusion, this study details heterogeneous and age-related clinical and laboratory features observed at and before the diagnosis of type 1 diabetes in a large cohort of high–genetic risk children. Observational prospective studies continue to clarify the need for multifactorial approaches to understand the natural history of this heterogeneous disease. Following identification of high-risk groups (high-risk HLA DR and presence of islet autoantibodies), we can provide some reassurance that this population of children had changing metabolic measures seen prior to onset. Whether fasting glucose, 120-min glucose, or glucose-to-insulin ratio will be the most ideal for monitoring or if other metabolic measures that use multipoint OGTT data and identify very high-risk populations are the most ideal is yet to be determined. As rates of type 1 diabetes continue to increase, we must continue to refine the tools for identifying high-risk children in order to prevent DKA and ultimately prevent and reverse type 1 diabetes.
Article Information
Acknowledgments. The authors acknowledge Åke Lernmark for valued review and guidance.
Funding. The TEDDY Study Group is funded by U01 DK63829, U01 DK63861, U01 DK63821, U01 DK63865, U01 DK63863, U01 DK63836, U01 DK63790, UC4 DK63829, UC4 DK63861, UC4 DK63821, UC4 DK63865, UC4 DK63863, UC4 DK63836, UC4 DK95300, UC4 DK100238, UC4 DK106955, UC4 DK112243, UC4 DK117483, U01 DK124166, and contract HHSN267200700014C from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Allergy and Infectious Diseases, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute of Environmental Health Sciences, Centers for Disease Control and Prevention, and JDRF. This work was supported in part by the National Institutes of Health/National Center for Advancing Translational Sciences Clinical and Translational Science Awards to the University of Florida (UL1 TR000064) and the University of Colorado (UL1 TR002535).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. L.M.J. researched the data and wrote the manuscript. K.V. analyzed the data, wrote the manuscript, contributed to discussion, and reviewed and edited the manuscript. R.V., K.W., J.T., A.K.S., P.G., B.A., M.L., W.A.H., J.-X.S., M.R., A.-G.Z., and J.P.K. reviewed/edited the manuscript. H.E.L. and M.J.H. conceptualized this study, evaluated the data, and reviewed/edited the manuscript. M.J.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
H.E.L. and M.J.H. share senior authorship.
This article contains supplementary material online at https://doi.org/10.2337/figshare.17209328.
A complete list of the TEDDY Study Group can be found in the supplementary material online.
Contributor Information
Collaborators: TEDDY Study Group:, Marian Rewers, Aaron Barbour, Kimberly Bautista, Judith Baxter, Daniel Felipe-Morales, Brigitte I. Frohnert, Marisa Stahl, Patricia Gesualdo, Rachel Haley, Michelle Hoffman, Rachel Karban, Edwin Liu, Alondra Munoz, Jill Norris, Stesha Peacock, Hanan Shorrosh, Andrea Steck, Megan Stern, Kathleen Waugh, Jorma Toppari, Olli G. Simell, Annika Adamsson, Sanna-Mari Aaltonen, Suvi Ahonen, Mari Åkerlund, Leena Hakola, Anne Hekkala, Henna Holappa, Heikki Hyöty, Anni Ikonen, Jorma Ilonen, Sanna Jokipuu, Leena Karlsson, Jukka Kero, Miia Kähönen, Mikael Knip, Minna-Liisa Koivikko, Katja Kokkonen, Merja Koskinen, Mirva Koreasalo, Kalle Kurppa, Salla Kuusela, Jarita Kytölä, Sinikka Lahtinen, Jutta Laiho, Tiina Latva-aho, Laura Leppänen, Katri Lindfors, Maria Lönnrot, Elina Mäntymäki, Markus Mattila, Maija Miettinen, Katja Multasuo, Teija Mykkänen, Tiina Niininen, Sari Niinistö, Mia Nyblom, Sami Oikarinen, Paula Ollikainen, Zhian Othmani, Sirpa Pohjola, Jenna Rautanen, Anne Riikonen, Minna Romo, Satu Simell, Aino Stenius, Päivi Tossavainen, Mari Vähä-Mäkilä, Eeva Varjonen, Riitta Veijola, Irene Viinikangas, Suvi M. Virtanen, Jin-Xiong She, Desmond Schatz, Diane Hopkins, Leigh Steed, Jennifer Bryant, Katherine Silvis, Michael Haller, Melissa Gardiner, Richard McIndoe, Ashok Sharma, Stephen W. Anderson, Laura Jacobsen, John Marks, P.D. Towe, Anette G. Ziegler, Ezio Bonifacio, Cigdem Gezginci, Anja Heublein, Eva Hohoff, Sandra Hummel, Annette Knopff, Charlotte Koch, Sibylle Koletzko, Claudia Ramminger, Roswith Roth, Jennifer Schmidt, Marlon Scholz, Joanna Stock, Katharina Warncke, Lorena Wendel, Christiane Winkler, Åke Lernmark, Daniel Agardh, Carin Andrén Aronsson, Maria Ask, Rasmus Bennet, Corrado Cilio, Susanne Dahlberg, Malin Goldman Tsubarah, Emelie Ericson-Hallström, Annika Björne Fors, Lina Fransson, Thomas Gard, Monika Hansen, Susanne Hyberg, Berglind Jonsdottir, Helena Elding Larsson, Marielle Lindström, Markus Lundgren, Marlena Maziarz, Maria Månsson Martinez, Jessica Melin, Zeliha Mestan, Caroline Nilsson, Yohanna Nordh, Kobra Rahmati, Anita Ramelius, Falastin Salami, Anette Sjöberg, Carina Törn, Ulrika Ulvenhag, Terese Wiktorsson, Åsa Wimar, William A. Hagopian, Michael Killian, Claire Cowen Crouch, Jennifer Skidmore, Christian Chamberlain, Brelon Fairman, Arlene Meyer, Jocelyn Meyer, Denise Mulenga, Nole Powell, Jared Radtke, Shreya Roy, Davey Schmitt, Sarah Zink, Dorothy Becker, Margaret Franciscus, MaryEllen Dalmagro-Elias Smith, Ashi Daftary, Mary Beth Klein, Chrystal Yates, Jeffrey P. Krischer, Rajesh Adusumali, Sarah Austin-Gonzalez, Maryouri Avendano, Sandra Baethke, Brant Burkhardt, Martha Butterworth, Nicholas Cadigan, Joanna Clasen, Kevin Counts, Christopher Eberhard, Steven Fiske, Laura Gandolfo, Jennifer Garmeson, Veena Gowda, Belinda Hsiao, Christina Karges, Qian Li, Shu Liu, Xiang Liu, Kristian Lynch, Jamie Malloy, Cristina McCarthy, Jose Moreno, Hemang M. Parikh, Cassandra Remedios, Chris Shaffer, Susan Smith, Noah Sulman, Roy Tamura, Dena Tewey, Michael Toth, Ulla Uusitalo, Kendra Vehik, Ponni Vijayakandipan, Melissa Wroble, Jimin Yang, Kenneth Young, Beena Akolkar, Liping Yu, Dongmei Miao, Kathleen Gillespie, Alistair Williams, Kyla Chandler, Ilana Kelland, Yassin Ben Khoud, Matthew Randell, William Hagopian, Christian Chamberlain, Jared Radtke, Sarah Zink, Stephen S. Rich, Wei-Min Chen, Suna Onengut-Gumuscu, Emily Farber, Rebecca Roche Pickin, Jonathan Davis, Jordan Davis, Dan Gallo, Jessica Bonnie, Paul Campolieto, Sandra Ke, Niveen Mulholland, Thomas Briese, Todd Brusko, Suzanne Bennett Johnson, Eoin McKinney, Tomi Pastinen, and Eric Triplett
References
- 1. International Diabetes Federation . IDF Diabetes Atlas, eighth edition, 2017. Accessed 29 November 2020. Available from https://diabetesatlas.org/upload/resources/previous/files/8/IDF_DA_8e-EN- final.pdf
- 2. Zheng S, Mathews CE. Metabolic abnormalities in the pathogenesis of type 1 diabetes. Vol. 14. Curr Diab Rep 2014;14:519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dabelea D, Rewers A, Stafford JM, et al.; SEARCH for Diabetes in Youth Study Group . Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics 2014;133:e938–e945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Evans-Molina C, Sims EK, DiMeglio LA, et al.; Type 1 Diabetes TrialNet Study Group . β Cell dysfunction exists more than 5 years before type 1 diabetes diagnosis. JCI Insight 2018;3:e120877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sosenko JM, Palmer JP, Rafkin LE, et al.; Diabetes Prevention Trial-Type 1 Study Group . Trends of earlier and later responses of C-peptide to oral glucose challenges with progression to type 1 diabetes in diabetes prevention trial-type 1 participants. Diabetes Care 2010;33:620–625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koskinen MK, Helminen O, Matomäki J, et al. Reduced β-cell function in early preclinical type 1 diabetes. Eur J Endocrinol 2016;174:251–259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sosenko JM, Skyler JS, Herold KC, et al.; Type 1 Diabetes TrialNet Study Group . Slowed metabolic decline after 1 year of oral insulin treatment among individuals at high risk for type 1 diabetes in the diabetes prevention trial–type 1 (DPT-1) and trialnet oral insulin prevention trials. Diabetes 2020;69:1827–1832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schatz D, Cuthbertson D, Atkinson M, et al. Preservation of C-peptide secretion in subjects at high risk of developing type 1 diabetes mellitus—a new surrogate measure of non-progression? Pediatr Diabetes 2004;5:72–79 [DOI] [PubMed] [Google Scholar]
- 9. Skyler JS, Krischer JP, Wolfsdorf J, et al. Effects of oral insulin in relatives of patients with type 1 diabetes: The Diabetes Prevention Trial—Type 1. Diabetes Care 2005;28:1068–1076 [DOI] [PubMed] [Google Scholar]
- 10. Koskinen MK, Lempainen J, Löyttyniemi E, et al. Class II HLA genotype association with first-phase insulin response is explained by islet autoantibodies. J Clin Endocrinol Metab 2018;103:2870–2878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care 2015;38:1964–1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hao W, Gitelman S, DiMeglio LA, Boulware D; Type 1 Diabetes TrialNet Study Group . Fall in C-peptide during first 4 years from diagnosis of type 1 diabetes: variable relation to age, HbA1c, and insulin dose. Diabetes Care 2016;39:1664–1670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hagopian WA, Erlich H, Lernmark A, et al.; TEDDY Study Group . The Environmental Determinants of Diabetes in the Young (TEDDY): genetic criteria and international diabetes risk screening of 421 000 infants. Pediatr Diabetes 2011;12:733–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. TEDDY Study Group . The Environmental Determinants of Diabetes in the Young (TEDDY) Study. Ann N Y Acad Sci 2008;1150:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vehik K, Cuthbertson D, Boulware D, et al.; TEDDY, TRIGR, Diabetes Prevention Trial–Type 1, and Type 1 Diabetes TrialNet Natural History Study Groups . Performance of HbA1c as an early diagnostic indicator of type 1 diabetes in children and youth. Diabetes Care 2012;35:1821–1825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Törn C, Mueller PW, Schlosser M, Bonifacio E; Participating Laboratories . Diabetes Antibody Standardization Program: evaluation of assays for autoantibodies to glutamic acid decarboxylase and islet antigen-2. Diabetologia 2008;51:846–852 [DOI] [PubMed] [Google Scholar]
- 18. Dabelea D, Bell RA, D’Agostino RB Jr, et al.; Writing Group for the SEARCH for Diabetes in Youth Study Group . Incidence of diabetes in youth in the United States. JAMA 2007;297:2716–2724 [DOI] [PubMed] [Google Scholar]
- 19. Patterson CC, Dahlquist G, Soltész G; EURODIAB ACE Study Group . Variation and trends in incidence of childhood diabetes in Europe. Lancet 2000;355:873–876 [PubMed] [Google Scholar]
- 20. Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, LaPorte R, Tuomilehto J. Incidence of childhood type 1 diabetes worldwide. Diabetes Mondiale (DiaMond) Project Group. Diabetes Care 2000;23:1516–1526 [DOI] [PubMed] [Google Scholar]
- 21. Patterson CC, Dahlquist GG, Gyürüs E, Green A; EURODIAB Study Group . Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 2009;373:2027–2033 [DOI] [PubMed] [Google Scholar]
- 22. Greenbaum CJ, Beam CA, Boulware D, et al.; Type 1 Diabetes TrialNet Study Group . Fall in C-peptide during first 2 years from diagnosis: evidence of at least two distinct phases from composite Type 1 Diabetes TrialNet data. Diabetes 2012;61:2066–2073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wolfsdorf JI, Glaser N, Agus M, et al. ISPAD clinical practice consensus guidelines 2018: diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Pediatr Diabetes 2018; 19(Suppl. 27):155–177 [DOI] [PubMed] [Google Scholar]
- 24. Elding Larsson H, Vehik K, Bell R, et al.; TEDDY Study Group; SEARCH Study Group; Swediabkids Study Group; DPV Study Group; Finnish Diabetes Registry Study Group . Reduced prevalence of diabetic ketoacidosis at diagnosis of type 1 diabetes in young children participating in longitudinal follow-up. Diabetes Care 2011;34:2347–2352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hekkala AM, Ilonen J, Toppari J, Knip M, Veijola R. Ketoacidosis at diagnosis of type 1 diabetes: effect of prospective studies with newborn genetic screening and follow up of risk children. Pediatr Diabetes 2018;19:314–319 [DOI] [PubMed] [Google Scholar]
- 26. Steck AK, Rewers MJ. Genetics of type 1 diabetes. Clin Chem 2011;57:176–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harjutsalo V, Reunanen A, Tuomilehto J. Differential transmission of type 1 diabetes from diabetic fathers and mothers to their offspring. Diabetes 2006;55:1517–1524 [DOI] [PubMed] [Google Scholar]
- 28. Turtinen M, Härkönen T, Parkkola A, Ilonen J; Finnish Pediatric Diabetes Register . Characteristics of familial type 1 diabetes: effects of the relationship to the affected family member on phenotype and genotype at diagnosis. Diabetologia 2019;62:2025–2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hippich M, Beyerlein A, Hagopian WA, et al.; TEDDY Study Group; Teddy Study Group . Genetic contribution to the divergence in type 1 diabetes risk between children from the general population and children from affected families. Diabetes 2019;68:847–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Krischer JP, Lynch KF, Lernmark Å, et al.; TEDDY Study Group . Genetic and environmental interactions modify the risk of diabetes-related autoimmunity by 6 years of age: the TEDDY study. Diabetes Care 2017;40:1194–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Steck AK, Johnson K, Barriga KJ, et al. Age of islet autoantibody appearance and mean levels of insulin, but not GAD or IA-2 autoantibodies, predict age of diagnosis of type 1 diabetes: diabetes autoimmunity study in the young. Diabetes Care 2011;34:1397–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bilbao JR, Rica I, Vázquez JA, Busturia MA, Castaño L. Influence of sex and age at onset on autoantibodies against insulin, GAD65 and IA2 in recent onset type 1 diabetic patients. Horm Res 2000;54:181–185 [DOI] [PubMed] [Google Scholar]
- 33. Ferrannini E, Mari A, Nofrate V, Sosenko JM; DPT-1 Study Group . Progression to diabetes in relatives of type 1 diabetic patients: mechanisms and mode of onset. Diabetes 2010;59:679–685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Greenbaum CJ, Prigeon RL, D’Alessio DA. Impaired β-cell function, incretin effect, and glucagon suppression in patients with type 1 diabetes who have normal fasting glucose. Diabetes 2002;51:951–957 [DOI] [PubMed] [Google Scholar]
- 35. Helminen O, Aspholm S, Pokka T, et al. OGTT and random plasma glucose in the prediction of type 1 diabetes and time to diagnosis. Diabetologia 2015;58:1787–1796 [DOI] [PubMed] [Google Scholar]
- 36. Vehik K. HbA1c—is it a good diagnostic predictor of type 1 onset in a pediatric population? Presented at the 80th American Diabetes Association Scientific Sessions, 12–16 June 2020 [Google Scholar]
- 37. Ferrat LA, Vehik K, Sharp SA, et al.; TEDDY Study Group; Committees . A combined risk score enhances prediction of type 1 diabetes among susceptible children. Nat Med 2020;26:1247–1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jacobsen LM, Bocchino L, Evans-Molina C, et al. The risk of progression to type 1 diabetes is highly variable in individuals with multiple autoantibodies following screening. Diabetologia 2020;63:588–596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ziegler AG, Danne T, Dunger DB, et al. Primary prevention of beta-cell autoimmunity and type 1 diabetes - the Global Platform for the Prevention of Autoimmune Diabetes (GPPAD) perspectives. Mol Metab 2016;5:255–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vellanki P, Umpierrez GE. Increasing hospitalizations for DKA: A need for prevention programs. Diabetes Care 2018;41:1839–1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hekkala A, Knip M, Veijola R. Ketoacidosis at diagnosis of type 1 diabetes in children in northern Finland: temporal changes over 20 years. Diabetes Care 2007;30:861–866 [DOI] [PubMed] [Google Scholar]
- 42. Hanas R, Lindgren F, Lindblad B. A 2-yr national population study of pediatric ketoacidosis in Sweden: predisposing conditions and insulin pump use. Pediatr Diabetes 2009;10:33–37 [DOI] [PubMed] [Google Scholar]
- 43. Neu A, Hofer SE, Karges B, Oeverink R, Rosenbauer J; DPV Initiative and the German BMBF Competency Network for Diabetes Mellitus . Ketoacidosis at diabetes onset is still frequent in children and adolescents: a multicenter analysis of 14,664 patients from 106 institutions. Diabetes Care 2009;32:1647–1648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Elding Larsson H, Vehik K, Gesualdo P, et al.; TEDDY Study Group . Children followed in the TEDDY study are diagnosed with type 1 diabetes at an early stage of disease. Pediatr Diabetes 2014;15:118–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Duca LM, Wang B, Rewers M, Rewers A. Diabetic ketoacidosis at diagnosis of type 1 diabetes predicts poor long-term glycemic control. Diabetes Care 2017;40:1249–1255 [DOI] [PubMed] [Google Scholar]
- 46. Fredheim S, Johannesen J, Johansen A, et al.; Danish Society for Diabetes in Childhood and Adolescence . Diabetic ketoacidosis at the onset of type 1 diabetes is associated with future HbA1c levels. Diabetologia 2013;56:995–1003 [DOI] [PubMed] [Google Scholar]
- 47. Johnson SB, Lynch KF, Roth R; TEDDY Study Group . My child is islet autoantibody positive: impact on parental anxiety. Diabetes Care 2017;40:1167–1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Unsworth R, Wallace S, Oliver NS, et al. New-onset type 1 diabetes in children during COVID-19: multicenter regional findings in the U.K. Diabetes Care 2020;43:e170–e171 [DOI] [PubMed] [Google Scholar]
- 49. Tittel SR, Rosenbauer J, Kamrath C, et al.; DPV Initiative . Did the COVID-19 lockdown affect the incidence of pediatric type 1 diabetes in Germany? Diabetes Care 2020;43:e172–e173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rabbone I, Schiaffini R, Cherubini V, Maffeis C; Diabetes Study Group of the Italian Society for Pediatric Endocrinology and Diabetes . Has Covid-19 delayed the diagnosis and worsened the presentation of type 1 diabetes in children? Diabetes Care 2020;43:2870–2872 [DOI] [PubMed] [Google Scholar]
- 51. Kamrath C, Mönkemöller K, Biester T, et al. Ketoacidosis in children and adolescents with newly diagnosed type 1 diabetes during the COVID-19 pandemic in Germany. JAMA 2020;324:801–804 [DOI] [PMC free article] [PubMed] [Google Scholar]