Summary
Background
Brazil has been severely impacted by COVID-19 pandemics that is aggravated by the absence of a scientifically-driven coordinated informative campaign and the interference in public health management, which ultimately affected health measures to avoid SARS-CoV2 spread. The decentralization and resultant conflicts in disease control activities produced different protection behaviours and local government measures. In the present study, we investigated how political partisanship and socio-economic factors determined the outcome of COVID-19 at the local level in Brazil.
Methods
A retrospective study of COVID-19 deaths was carried out using mortality databases between Feb 2020, and Jun 2021 for the 5570 Brazilian municipalities. Socio-economic parameters including city categories, income and inequality indexes, health service quality and partisanship, assessed by the result of the second round of the 2018 Brazilian presidential elections, were included. Regression tree analysis was carried out to identify the statistical significance and conditioning relationships of variables.
Findings
Municipalities that supported then-candidate Jair Bolsonaro in the 2018 elections were those that had the worst COVID-19 mortality rates, mainly during the second epidemic wave of 2021. This pattern was observed even considering structural inequalities among cities.
Interpretation
In general, the first phase of the pandemic hit large and central cities hardest, while the second wave mostly impacted Bolsonarian municipalities, where scientific denialism among the population was stronger. Negative effects of partisanship towards the right-wing on COVID-19 outcomes counterbalances favourable socioeconomic indexes in affluent Brazilian cities. Our results underscore the fragility of public health policies which were undermined by the scientific denialism of right-wing supporters in Brazil.
Funding
International joint laboratories of Institute de Recherche pour le Développement, a partnership between the University of Brasília and the Oswaldo Cruz Foundation (LMI-Sentinela - UnB - Fiocruz - IRD), Coordination for the Improvement of Higher Education Personnel (CAPES), National Council for Scientific and Technological Development (CNPq).
Keywords: COVID-19, Pandemic, Politics, Social inequalities, Data mining, Brazil
Research in context.
Evidence before this study
The influence of political affiliation, citizen partisanships, government ideological orientation and the role of media (and social media) in the response to COVID-19 pandemic is an increasing concern in Global Health. We searched PubMed on September 21st, 2021, with the terms “COVID-19”, “partisan*”, “ideolog*” and “Bolsonaro”. A total of 204 articles were listed, with a predominant emphasis in the analysis of public discourse, ideologic affiliation and the role of media, mostly studying events that occurred in the US during the Trump administration. We found 15 articles analysing the role of Bolsonaro in the responses to the pandemic. They focused on denialism, conspiracy theories, access to information, public health policies, federalism, and legal conflicts. Few studies applied quantitative approaches and we did not find multivariate models or big data being used to analyse relations among epidemiologic indicators, socio-economic and political determinants, which is the main proposal of this article.
Added value of this study
This study contributes to expanding the scientific evidence on the factors that influenced the distribution of COVID-19 mortality rate in Brazil and demonstrates, using data mining methods, that among the explanatory variables that make up the established modeling (city hierarchy, income, inequality, vote in the 2018 presidential elections, and mortality from preventable causes), local political affiliation – here represented by the vote for Bolsonaro – affected COVID-19 mortality rate, after considering socioeconomic variables. This was particularly important along the second wave of the COVID-19 in Brazil, supporting the influence of the negationist discourse on the disease outcome.
Implications of all the available evidence
The dynamics of the pandemic has been influenced by previous conditions, such as the position of cities in the national urban network, mean income and socio-economic inequalities. However, it cannot be ignored the role of political orientation and ideology that drives both the response of the health sector, the protective behaviour of the population, affecting mainly small and peripheral cities. National leaders and influencers had an important role in shaping defensive social behaviours to mitigate COVID-19 through the distribution of information to citizens. The dissemination of correct up to date scientific recommendations, as well as preparing the health system to deal with the impacts of COVID-19 has been critical for the management of the pandemic. The weight of anti-scientific ideologies and partisanship cannot be ignored when proposing the control strategies of epidemics.
Alt-text: Unlabelled box
Introduction
Owing to the increase in the human population, misuse of natural resources, extensive animal production, deforestation, and global warming, a series of emerging and re-emerging diseases have been reported in recent decades.1 They include, among others, several respiratory diseases caused by viruses from the Coronaviridae family, such as the Middle East Respiratory Syndrome Coronavirus (MERS-CoV) and the Severe Acute Respiratory Distress Syndrome Coronavirus (SARS-CoV).2 The most recent and devastating disease caused by a coronavirus was identified for the first time in 2019 (COVID-19) in Wuhan, China, and this has been responsible for more than 5.3 million deaths worldwide to date.3 COVID-19 was declared a pandemic by the World Health Organization (WHO) on March 11th 20204 and the Severe Acute Respiratory Distress Syndrome Coronavirus – 2 (SARS-CoV-2) was identified as its causative agent.
COVID-19 is a complex disease, and the large spectrum of its clinical presentations and severities span from asymptomatic mild flu-like symptoms to severe complications such as pneumonia, septic shock, acute respiratory distress syndrome, and death. The global average cases-to-fatalities ratio is close to 2%, which is mainly, but not only, associated with advanced age or the presence of comorbidities including obesity, diabetes, and hypertension.5 Since the beginning of the outbreak, respiratory droplets and fomites from infected subjects have been recognised as the main source of transmission. Without an effective treatment or vaccine during the first year of the pandemic, the only preventive action to control the spread of COVID-19 comprised social distancing, imposed by governments as a series of unpopular lockdowns, hand hygiene, and the use of face masks.6 These strategies were openly advertised by the WHO as the only effective way to prevent infection, limit the spread of COVID-19, and avoid the collapse of healthcare systems when vaccines were not available.
The large spectrum of COVID-19 symptoms has fuelled misperceptions about the disease setting, development, and outcome. Considering that the COVID-19 cases-to-fatalities ratio is relatively low compared with the Ebola virus (40% during the 2013–2016 outbreak),7 some governments quickly relaxed lockdowns to allow the reopening of businesses and services to avoid the collapse of their economies. In some cases, this permissiveness promoted massive infection to achieve herd immunity before vaccination. However, the consequences of unmitigated SARS-CoV-2 infection are tragic, as observed in the outbreak in Manaus, Brazil.8 The Amazon state was hit hardest by COVID-19 in Brazil as a consequence of multiple factors including the resistance of local and federal government to impose non-pharmacological mitigation measures, such as social distancing and masks use, allowing virus circulation among the population which fuelled the emergence of a highly transmissible new variant (gamma). Altogether, the combination of these factors boosted infirmary and ICU hospitalizations, culminating in the collapse of oxygen supply and massive deaths in Manaus.
While the global COVID-19 catastrophe continues to develop, Brazil has emerged as an example of how the lack of a robust national public health policy and implementation of an active anti-science campaign can aggravate the outcomes of the pandemic. Despite Brazil accounting for approximately 2.7% of the world's population, its contribution to COVID-19 cases and deaths is unevenly high, reaching around 8.15% and 11.55% of the global share, respectively.3 Indeed, Brazil ranked just behind the United States in total deaths (617,121 deaths) as of 15 December 2021.3
Several factors may explain the unexpected severity of COVID-19 outcomes in Brazil. First, historical socioeconomic inequalities have directly contributed to the disproportionate burden of COVID-19 in vulnerable populations.9 Second, the widespread surge of a novel and more transmissible SARS-CoV-2 variant of concern (P.1) in Manaus led to the collapse of healthcare systems in many localities.10 Third, the disinterest of the federal administration in implementing a coordinated and aggressive national response to tackle COVID-19, focusing on the promotion of non-pharmaceutical interventions such as local lockdown measures, social distancing, the mandatory use of masks, vigorous testing, and contact tracing of the population, has been a factor.11 Fourth, the delay in implementing a robust vaccination campaign has played a role.12 Lastly, a well-organised campaign of scientific denialism and misinformation led by the Brazilian federal administration, endorsed by the right-wing-oriented Brazilian medical associations, which have promoted self-medication with chloroquine and ivermectin, has amplified the severity of COVID-19, mainly among the elderly population.13
The practices implemented by the federal government were essentially through ‘medical demagogy’ and included: (i) the propagation of conspiracy theories about the origins of SARS-CoV-2; (ii) the consistent (since March 2020) defiance about the severity of pandemics, with the president declaring on TV that ‘it's just the flu’14; (iii) the ‘repositioning’ of pre-existent drugs such as chloroquine, hydroxychloroquine, azithromycin, and ivermectin for the treatment of COVID-19 patients through the so-called ‘kit-covid’15,16; (iv) the frequent changes in the Ministry of Health (four in total) in less than a year resulting from disagreements between the current administration and Ministers of Health, especially on the push to implement ineffective drugs for COVID-19 treatment; and (v) the delay in acquisition and denial about the effectiveness of vaccines for controlling COVID-19. As a result of the disastrous management of COVID-19 by the Brazilian Ministry of Health, a parliamentary committee of inquiry established by the Senate has confirmed the hypothesis that President Jair Bolsonaro deliberately spread COVID-19 among the population, allegedly to accelerate herd immunity.13
In contrast to the US case, the Brazilian anti-science movement has not been organised but has quickly risen in the three years since the present administration took office. Nevertheless, the top-down implementation of an anti-science agenda permeated Brazilian society.16 Indeed, adherence to social distancing and mask use is lower than that in other countries.17
Denial is a defence mechanism for individuals against an unbearable reality, not just death.18 Denialism, on the contrary, is a mass phenomenon based on the trivialisation of death, adoption of distractions from reality, production of imaginary enemies (usually associated with conspiracy theories), the disempowerment of institutions, and displacement to personal and symbolic authority.19 Specifically, scientific denialism questions scientific knowledge and replaces it with beliefs. Unsurprisingly, the Bolsonarian narrative is based on the supremacy of individual freedom, above any other Enlightenment value such as equality, the defence of life, justice, and solidarity.20 In this case, freedom, frequently evoked by Bolsonarians, delegates to each individual the care of their health and introduces the idea of death as a fortuitous event, for no apparent rational reason.
The role of leaders in demonstrating adequate practices to handle COVID-19 through their own examples has critical positive effects on the population.21,22 Indeed, Brazil has experienced extreme political polarisation and hostility since 2015, with a recrudescence since 2018, with potentially negative consequences for the public's perception of COVID-19.17 Although recent observations indicate a clear relationship between partisanship and COVID-19 prognosis,22,23 there is no clear evidence that partisanship defines COVID-19 outcomes relative to key socioeconomic variables. In this context, we postulate that partisanship plays an important role in defining the outcomes of COVID-19 as well as population income, human development, and preventable diseases at the local level in Brazil.
Methods
The present work is an ecological study to examine why Brazilian municipalities with the same inequality, income, and healthcare service characteristics had different COVID-19 mortality behaviours, we used contextual indicators that allowed us to observe the categorisation, development, and quality of healthcare services of cities and their political choices. A regression tree with conditional inference was built to classify the outcome variable according to the different levels of response of the contextual variables, and thus verify the effect of these contextual variables on COVID-19 death rates in Brazilian municipalities. In Brazil, a municipality is the total territorial area administered by a mayor's office, which has administrative autonomy and is made up of certain political and administrative bodies. There are currently 5570 municipalities in Brazil, while the city is the most urbanised part of the municipality. The databases and details of this method are described below.
Data sources
COVID-19 mortality data
A retrospective study was carried out on COVID-19 deaths registered in the Influenza Epidemiological Surveillance Information System (SIVEP-Gripe), a system used by local, state, and federal governments to monitor severe acute respiratory infections in Brazil, which indicated the epidemic process of COVID-19 as early as epidemiological week 12 of 2020.24 As requested by the Ministry of Health, SARS deaths should be reported in SIVEP-Gripe regardless of hospitalisation. This data source contains information about hospitalisation and deaths and consequently deals with the most severe cases. Because COVID-19 is a disease that requires mandatory notification, the database includes information from public and private health systems.25
We separated the two main waves of the pandemic in Brazil using the cut-off date of November 1st, 2020, when there was a large reduction in the number of deaths. We, therefore, analysed the data according to the two periods, from February to October 2020 and from November 2020 to June 2021. We analysed 472,634 COVID-19 deaths confirmed by laboratory tests with positive results from the quantitative RT-PCR test for SARS-CoV-2, from February 16th 2020 to June 17th 2021. The unit of analysis for this study was the municipality and the age-standardised mortality rate (SMR) was used to control for differences in demographic age structures. The SMR was calculated by the direct method using death data from COVID-19 from SIVEP Influenza.25 The direct method was used to standardise the mortality rate in the municipalities in which the rates of the age groups (0–4, 5–10, 11–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80 and over) of a locality were obtained based on the distribution of the standard population and then aggregated to generate the standardised values. We used the population of Brazil as the standard population for 2020 (preliminary estimates prepared by the Ministry of Health/SVS/DASNT/CGIAE) made available by the Brazilian Ministry of Health.26
Data on city categories
We classified the cities hierarchically using the Regions of Influence of Cities structure produced by the Brazilian Institute of Geography and Statistics (IBGE),27 which defines the hierarchy of Brazilian urban centres and delimits the regions of influence associated with them. This identifies, for example, the Brazilian metropolises and regional capitals as well as the spatial scope of their influence. The urban hierarchy and areas of influence were identified by classifying urban centres that have certain equipment and services that attract populations from other locations. The differentiated offer of goods and services among cities causes populations to travel to well-equipped urban centres to acquire health and education services or access an airport. Knowing the relationships among Brazilian cities based on the flows of goods, services, and management is an important tool for making locational choices, such as deciding the location of a university, hospital, or company branch. The hierarchical categories were local centres, zonal centres, sub-regional centres, regional capitals, and metropolises (ranked 1–5, respectively).
Data on the human development index (HDI) and Gini index
The municipal-level HDI was calculated from municipal data on education, income, and longevity in the same way as the HDI. The data on the HDI, provided by Atlas Brasil,28 was collected from the 2010 Demographic Census, which is the most recent source that includes the indices from all Brazilian municipalities. We used the HDI proportion of income component (HDI-Income) in our estimations. This choice met two conditions: The first was related to the characteristics of the country, which is heterogeneous and has an unequal distribution of wealth, and the second was related to the use of the Gini index, which captures part of this inequality, helping to explain how this context is shaped and if this amplified the effect of COVID-19 in Brazil, especially on deaths. In general, municipalities with higher income have lower inequality, as measured by the high Gini index, with important exceptions in some rural areas where economic development has been more equitable.
Healthcare service quality data
The infant mortality rate from preventable causes in children under 5 years was used to demonstrate the quality of local health before the COVID-19 pandemic. The rate was composed of data on infant deaths from preventable causes in 2019 obtained from the Mortality Information System and data on live births in 2019 from the Live Births Information System, both organised by the Ministry of Health and made available through the Department of Health Information.26
Data on the 2018 presidential election
The electronic ballot box data of the second round of the presidential election on October 7th 2018 were obtained from the Electoral Data Repository of the Superior Electoral Court (TSE).29 Only two candidates participated in this runoff, namely, Fernando Haddad (Workers’ Party) and the current Brazilian president, Jair Bolsonaro (Liberal Social Party, at the time). These data were converted into percentages, where the numerator referred to the number of votes received by the presidential candidate and the denominator was the number of voters able to participate in the election in the municipality at the time.
Statistical analyses
In contrast to traditional statistical analysis, we employed Knowledge Discovery in Databases (KDD) and data mining which allows discovery using large datasets with no previous hypothesis. In this sense, regression trees were employed in this study to ensure an unbiased classification of municipalities that better explain the distribution of the COVID-19 impact, here expressed by the SMR. These classifications were based on independent variables without any previous categorisation because cut-off points are established throughout the model.30 This approach can identify complex interactions between contextual variables without the a priori specification of interaction terms. In addition, it supports a large number of contextual variables relative to the number of observations.
The choice for this method consists in evaluating the effects of contextual variables without prior classification of the partisanship effect. This has been a common behaviour in analyses presented in the context of COVID-19 that consider the importance of government decisions without assessing basic problems and sometimes compare homogeneous areas, but which in Brazil, due to their size and heterogeneity, demands strategic of different analyses and conditional inference trees can shed light on the problem.
The regression tree with conditional inference uses the partitioning criterion based on statistical significance and evaluates the conditional relationships between the contextual variables in search of homogeneous groups that describe the behaviour of the outcome variable. The first step of the algorithm considers the global null hypothesis of independence between the contextual variables and outcome variable; if this hypothesis cannot be rejected, the partitioning stops. If the global null hypothesis is rejected, the most significant contextual variable in the conditional model relative to the other contextual variables is selected. When the selected variable is dichotomous, the choice of the best binary partition is trivial; for non-dichotomous variables, the algorithm identifies the best binary partition of all possible partitions.31 Because conditional trees are based on statistical inference, pruning is not necessary, and nor is the approach used in the recursive partitioning algorithms as previously proposed.32
The statistics for the partitioning are based on the asymptotic theory of permutation statistics proposed by Strasser and Weber.32 Initially, the possible partitions based on all contextual variables are created and the analysis units are classified; then, a statistical test is applied to select the groups that will compose the tree. In this study, the Monte Carlo test was used to evaluate independence as well as compare the p-values and select the nodes. A significance level of 0.05 was adopted as a reference for the p-value to include the partitioning of the contextual variables. Based on these results, the groups were created and the predicted values of the terminal nodes were determined. Finally, the ctree function from the R package (or library), called partykit, version 3.4.0, was used.33
A regression tree with conditional inference was built to classify the outcome variable according to the different levels of response of the contextual variables to verify their effect on the occurrence of COVID-19 in Brazilian municipalities. This regression with conditional inference allowed us to estimate the occurrence of deaths from the disease by groups of municipalities considering the partisan issue that influenced the behaviour of the disease in the country. Finally, estimates and errors with 95% confidence intervals (CIs) for each created group were presented. The results predicted by the model were processed in a geographic information system (GIS) environment to construct the final maps, and graphs of the rates by the groups of municipalities were prepared to evaluate the behaviour of the disease throughout the pandemic.
This method may have limitations due to the inherent quality of the data. Municipalities with very small populations can influence the variable by inflating the indicator. Another limitation concerns the lack of information for context variables in municipalities created after the year 2010 (Census demographic), which was when the census data were made available. These municipalities (5 in total) were excluded and may influence the results.
Role of the funding source
The funder of the study had no role in study design, data analysis, data interpretation, or writing of the manuscript.
Results
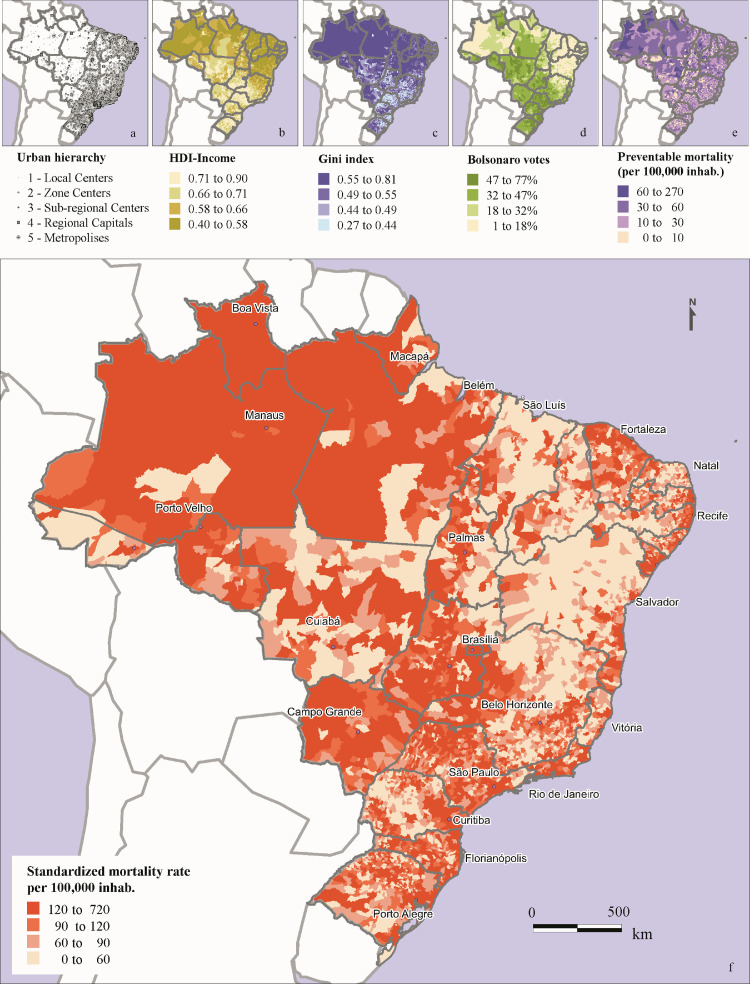
Figure 1 shows the spatial distribution of the explanatory variables used in the model. The HDI-Income highlights the dichotomy that exists in the country, where the northern and northeastern regions contain municipalities with lower income than that in the southern, southeastern, and coastal regions of the northeast. In addition, municipalities with high income have significant inequality, as measured by the high Gini index and compared with the HDI-Income map. The preventable causes present a more random distribution concerning the other explanatory variables, and some municipalities in the northern region are facing the worst access to healthcare than those in other regions. The partisanship indicator that describes the result of the Brazilian presidential election in 2018 shows a clear pattern of income inversion.
Figure 1.
Main determinants and COVID-19 standardised mortality rate (SMR) in Brazilian municipalities. (a) Urban hierarchy of cities according to the classification of the IBGE.27 (ib) Human development index proportion of income (HDI-Income). (c) Gini index of income inequality. (d) Proportion of votes for Bolsonaro in the second round of the 2018 presidential election in %. (e) Mortality rate due to preventable causes. (f) COVID-19 SMR from February 16th, 2020 to June 17th, 2021.
The first contextual variable, which defined the subsequent groups, was the hierarchical level of cities, demonstrating the importance of city function and connectivity in the regional impact of COVID-19 incidence and mortality. Urban hierarchy is not directly related to city size but to its role in the regional economy and the national urban network, which may reflect both the capacity of cities health services to treat disease cases as well as their role in the propagation of the virus to their influenced surrounding areas. Higher hierarchical cities attract investments and are better equipped, including health facilities, while lower hierarchical cities play a minor role in human mobility and market of goods. São Paulo, Brasilia and Rio de Janeiro are national metropolises and influence great extension of Brazil. Other state capitals and large conurbated urban areas are also considered metropolises, while medium and less connected cities are classified as regional centres. Finally, small and remote cities are classified as zonal centres and comprise the majority (82.4%) of Brazilian cities. Small and remote cities (local and zonal centres) were less affected by COVID-19 than central and large cities (sub-regional and regional centres and metropolises). In small cities, income (HDI-Income) was the main differential and wealthier cities presented higher mortality rates than poorer cities. For large and central cities, income distribution (expressed by the Gini index) separated more equal cities presenting higher COVID-19 mortality from unequal cities with lower mortality rates. Votes for Bolsonaro was a subsequent variable in the classification tree, which indicates the importance of political partisanship in COVID-19 outcomes, after taking into account the underlying socioeconomic conditions in the composition of Brazilian municipalities.
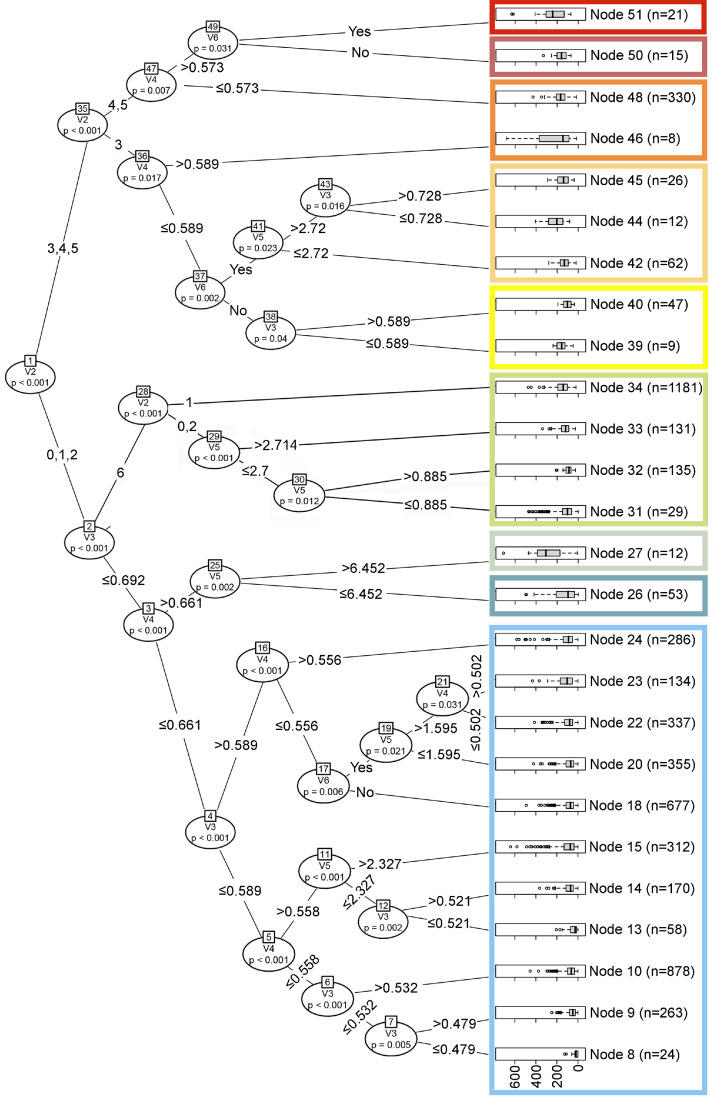
Figure 2 shows a regression tree with 25 internal nodes and 26 end nodes. The main contextual variable among the input variables in the model was the hierarchy of cities, with an emphasis on regional capitals and metropolises. The group with 21 cities (node 51) was the set of analysis units that presented the second highest COVID-19 SMR, 255 (95% CI: 189–321) deaths per 100,000 inhabitants. This occurred in regional capitals and metropolises with high inequality and in which the current president won the election. Municipalities with the same characteristics, presenting only a difference in low electoral enthusiasm for Bolsonaro, showed much lower rates, with a mean of 161 (95% CI: 125–197). Internal node 37 also highlights the importance of the political position manifested through the election results variable. Our analyses identified that in places with lower inequality, represented by the Gini index (V4), the COVID-19 SMR increased. Places with higher mortality rates from preventable causes (V5) also presented a higher COVID-19 SMR, even in localities with high incomes (HDI-Income, V3).
Figure 2.
Classification of Brazilian municipalities according to the conditional regression tree for COVID-19 and the independent variables. Groups are aggregations of nodes and are presented in different colours.
Even considering these structural variables, in places in which the current president won the election, the COVID-19 SMR was higher. This was observed in node 45, which had a rate of 148 (95% CI: 123–173). In smaller cities classified as groups 1 (local centres), 2 (zonal centres), and 3 (sub-regional centres), the HDI-income (V3) behaved contrary to our expectations; that is, the higher income, the greater was the COVID-19 SMR. In zonal centres, mortality from preventable causes grew proportionally with the COVID-19 SMR (node 33, 154 (95% CI: 140–167)). Node 34 had the largest number of municipalities (1,181) and high income, with a COVID-19 SMR of 113 (95% CI: 120–149). Interestingly, in most of these municipalities (92.4%), the highest shares of votes were for then-candidate Bolsonaro.
The municipalities with a low HDI-Income (Gini indices between 0.452 and 0.591) with different mortality rates from preventable causes were 8 (25, 95% CI: 12–38), 9 (58, 95% CI: 52–63), 10 (72, 95% CI: 68–70), 13 (44, 95% CI: 33–56), 14 (82, 95% CI: 74–91), 15 (100, 95% CI: 89–111), and 18 (83, 95% CI: 79–88), which presented the lowest COVID-19 SMR. These groups accounted for 2387 municipalities, but Bolsonaro won the presidential election in 2018 in only 24 of them.
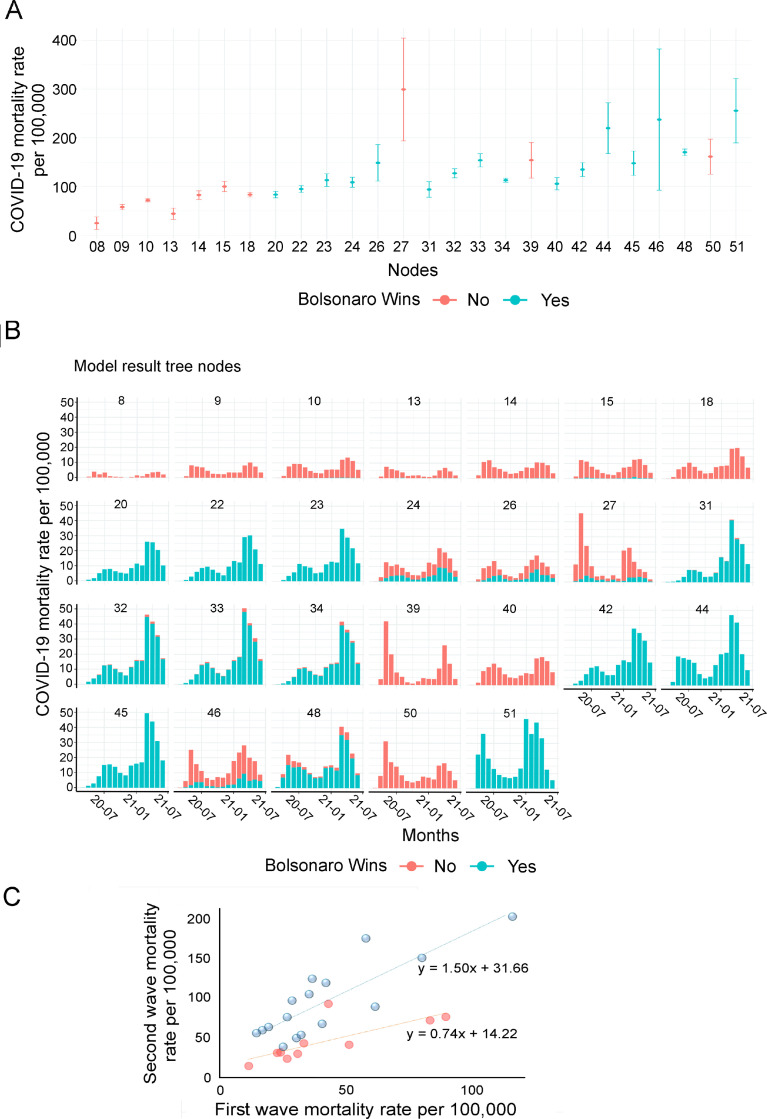
In Figure 3A, the mean SMR and its standard deviation among the nodes were obtained from the regression tree model. Brazil's municipalities differed markedly by their demographic composition and small populations caused the outcome indicator to fluctuate. Even so, the figure shows that there was only a large CI of municipal rates in node 27 with 12 municipalities (22,214 inhabitants) and in node 46 with eight municipalities (78,842 inhabitants).
Figure 3.
(A) Mean and standard deviation of the standardised mortality rate (SMR) (deaths per 100,000 inhabitants) from COVID-19 according to the municipalities’ classification nodes obtained from the regression tree. (B) Time series of the SMR (deaths per 100,000 inhabitants) from COVID-19 over time according to the municipalities’ classification nodes obtained from the regression tree. (C) Correlation between COVID-19 mortality rates during the first and second waves (March to October 2020 and November 2020 to July 2021, respectively) according to nodes of municipality vote preferences.
During the pandemic, Brazil presented different phases with distinct transmission intensities, spatial distributions, and impacts on healthcare services. The first wave, from March to October 2020, was characterised by low transmission rates and the disease diffusion from metropolitan areas to smaller and inner cities. After a peak of high incidence and mortality rates, between June and August 2020, a more uniform and synchronous pattern involving all cities nationally was observed. From November 2020 to June 2021, there was a new surge in the disease, hitting the entire Brazilian territory, with peak levels in April 2021 (second wave), namely, higher incidence and mortality rates and the collapse of the healthcare system. During the first wave, some measures to restrict mobility and economic activities were implemented, while during the second wave, these measures were more flexible and decentralised, except for certain metropolitan regions and small cities that adopted new restrictions in March 2021.
Figure 3B shows the difference in the evolution of mortality according to groups of municipalities and Figure 3C shows the difference in the increase of SMR between the first and second wave among municipalities according to political preferences (voting for Bolsonaro). There was a significant increase in mortality in nodes identified as Bolsonaro voters, compared to those city nodes that voted in the other presidential candidate.
Owing to this dynamic of the pandemic, small cities (nodes 8 to 34) (Figure 3B) had lower COVID-19 mortality rates in the first phase (i.e., expansion) than Brazilian metropolises and other hard-hit countries in Europe and the United States. Larger cities (nodes 39 to 51), on the contrary, had higher COVID-19 mortality rates in the first months of the pandemic (May and June 2020), such as those cities belonging to node 39 (medium-sized cities with low income, mainly in the northern and northeastern regions), node 50 (medium-sized and large cities, with higher income, spread nationally), and node 51 (medium-sized and large cities, with lower income and located mainly in metropolitan areas in the northeastern region). However, the largest distinction between cities emerged in the second wave, when many small cities, which had escaped the impact of the first wave, were seriously hit, mainly those belonging to nodes 20, 22, 23 (Group 1), 31, 32, 33, and 34 (Group 2). All these cities shared a preference for Bolsonaro in the second round of the 2018 election.
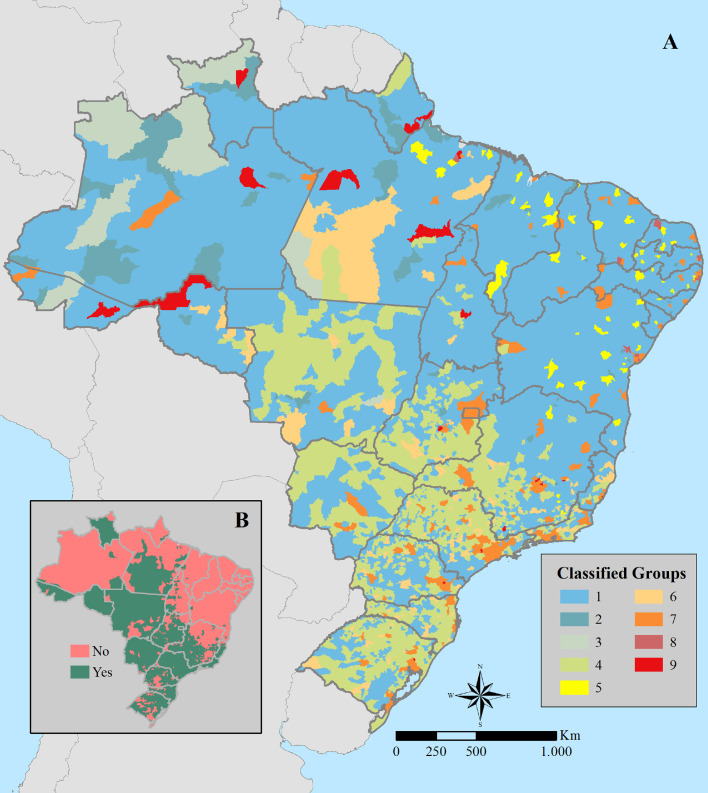
To better illustrate the results, the municipalities were mapped using the last hierarchical node of the tree by group (1–9), as shown in Figure 4. Table 1 summarizes the characteristics of the groups by presenting the mean and standard deviation of the selected variables. Group 1 comprises 3,499 small municipalities (average population of 15,000 inhabitants), which together correspond to 51 million people (24% of the Brazilian population). This group presented a lower SMR (mean 85 deaths per 100,000 inhabitants) than the other groups; however, there were important internal differences. Nodes were differentiated by combinations of the HDI-Income, the Gini index, and mortality from preventable causes. Nodes 8, 9, 10, 13, 14, and 15 of the classification trees had low income (HDI-Income) and few municipalities had Bolsonaro's victory in the second round. On the contrary, nodes 20, 22, and 23 had higher average income (HDI-Income) within Group 1 and all municipalities supported Bolsonaro in the 2018 presidential election. In the first group, the SMR was 72 deaths per 100,000 inhabitants, while it was 103 deaths per 100,000 inhabitants in the second group. Considering that the other independent variables showed no significant variability among groups, being a wealthier and right wing-oriented municipality increased the risk of COVID-19 death by 44%.
Figure 4.
Spatial distribution of the groups of municipalities obtained by the conditional regression tree (A), and municipalities where Bolsonaro won 2018 presidential elections (B).
Table 1.
Mean and standard deviation of COVID-19 SMR and socio-political covariates and total population according to the classified node of municipalities.
| Node | Group | Number of municipalities | Total population | COVID-19 SMR | Urban hierarchy | HDI- Income | Gini Index | Mortality preventable causes | Proportion of votes for Bolsonaro |
|---|---|---|---|---|---|---|---|---|---|
| 8 | 1 | 24 | 339121 | 24 ± 32 | 1.04 ± 0.04 | 0.46 ± 0.01 | 0.58 ± 0.03 | 31.1 ± 23.6 | 9.9 ± 3.3 |
| 9 | 1 | 268 | 3911433 | 57 ± 45 | 1.00 ± 0.01 | 0.51 ± 0.01 | 0.53 ± 0.04 | 27.4 ± 21.4 | 11.8 ± 4.4 |
| 10 | 1 | 877 | 13248058 | 71 ± 52 | 1.06 ± 0.01 | 0.56 ± 0.01 | 0.50 ± 0.04 | 27.3 ± 23.4 | 16.2 ± 6.2 |
| 13 | 1 | 58 | 815826 | 44 ± 45 | 1.01 ± 0.01 | 0.49 ± 0.02 | 0.55 ± 0.04 | 10.3 ± 8.9 | 10.9 ± 3.9 |
| 14 | 1 | 170 | 2595887 | 82 ± 58 | 1.05 ± 0.01 | 0.55 ± 0.01 | 0.52 ± 0.04 | 11.5 ± 8.7 | 15.8 ± 6.4 |
| 15 | 1 | 311 | 6613637 | 99 ± 96 | 1.07 ± 0.01 | 0.54 ± 0.03 | 0.54 ± 0.05 | 43.1 ± 20.9 | 15.6 ± 7.5 |
| 18 | 1 | 676 | 9316131 | 83 ± 61 | 1.12 ± 0.01 | 0.63 ± 0.02 | 0.49 ± 0.05 | 25.7 ± 25.6 | 25.4 ± 7.1 |
| 20 | 1 | 355 | 2842579 | 83 ± 62 | 1.01 ± 0.00 | 0.66 ± 0.05 | 0.44 ± 0.06 | 1.8 ± 4.5 | 42.9 ± 6.7 |
| 22 | 1 | 337 | 4044135 | 94 ± 65 | 1.08 ± 0.01 | 0.66 ± 0.02 | 0.45 ± 0.05 | 42.5 ± 28.2 | 42.2 ± 6.0 |
| 23 | 1 | 135 | 1916393 | 113 ± 76 | 1.08 ± 0.02 | 0.65 ± 0.06 | 0.47 ± 0.06 | 41.3 ± 22.7 | 42.3 ± 6.8 |
| 24 | 1 | 288 | 5388036 | 108 ± 89 | 1.11 ± 0.02 | 0.63 ± 0.06 | 0.51 ± 0.08 | 28.1 ± 24.4 | 32.8 ± 11.6 |
| 26 | 2 | 53 | 1067252 | 148 ± 140 | 1.05 ± 0.03 | 0.56 ± 0.06 | 0.57 ± 0.10 | 29.2 ± 18.1 | 23.0 ± 13.3 |
| 27 | 3 | 12 | 267416 | 299 ± 194 | 1.08 ± 0.08 | 0.55 ± 0.06 | 0.70 ± 0.08 | 101.5 ± 50.2 | 27.1 ± 12.7 |
| 31 | 4 | 29 | 605000 | 93 ± 46 | 2.00 ± 0.01 | 0.73 ± 0.02 | 0.48 ± 0.06 | 0.2 ± 0.3 | 50.5 ± 9.3 |
| 32 | 4 | 142 | 7098344 | 127 ± 54 | 1.98 ± 0.01 | 0.73 ± 0.02 | 0.48 ± 0.04 | 19.9 ± 5.4 | 49.0 ± 7.8 |
| 33 | 4 | 124 | 5831905 | 154 ± 81 | 2.02 ± 0.01 | 0.73 ± 0.02 | 0.49 ± 0.04 | 37.8 ± 9.2 | 47.4 ± 8.8 |
| 34 | 4 | 1181 | 15570549 | 113 ± 71 | 1.00 ± 0.02 | 0.72 ± 0.02 | 0.46 ± 0.06 | 24.5 ± 29.6 | 49.0 ± 9.6 |
| 39 | 5 | 9 | 936685 | 154 ± 59 | 3.03 ± 0.02 | 0.56 ± 0.02 | 0.55 ± 0.04 | 32.7 ± 12.2 | 18.6 ± 3.2 |
| 40 | 5 | 47 | 3937531 | 105 ± 44 | 3.00 ± 0.00 | 0.65 ± 0.03 | 0.55 ± 0.02 | 33.1 ± 9.2 | 23.1 ± 5.7 |
| 42 | 6 | 62 | 8091979 | 134 ± 57 | 3.00 ± 0.01 | 0.75 ± 0.02 | 0.49 ± 0.03 | 20.8 ± 4.1 | 51.1 ± 8.4 |
| 44 | 6 | 12 | 1239748 | 219 ± 95 | 3.00 ± 0.00 | 0.69 ± 0.02 | 0.53 ± 0.03 | 37 ± 11.6 | 44.5 ± 7.1 |
| 45 | 6 | 26 | 3285806 | 147 ± 66 | 3.00 ± 0.00 | 0.75 ± 0.02 | 0.5 ± 0.02 | 33.6 ± 8.5 | 50.7 ± 7.4 |
| 46 | 7 | 8 | 630746 | 237 ± 223 | 3.00 ± 0.00 | 0.64 ± 0.05 | 0.57 ± 0.04 | 33.9 ± 8.3 | 26.7 ± 17.5 |
| 48 | 7 | 330 | 100918831 | 170 ± 61 | 4.48 ± 0.02 | 0.71 ± 0.06 | 0.48 ± 0.06 | 26.1 ± 12.4 | 44.2 ± 11 |
| 50 | 8 | 15 | 3063593 | 161 ± 73 | 4.46 ± 0.13 | 0.64 ± 0.05 | 0.52 ± 0.05 | 30.3 ± 9.0 | 25.6 ± 7.1 |
| 51 | 9 | 21 | 8179071 | 255 ± 158 | 4.42 ± 0.11 | 0.71 ± 0.04 | 0.51 ± 0.07 | 30.9 ± 12.3 | 47.9 ± 6.4 |
Group 2, categorised at node 26 of the regression tree, consisted of 53 municipalities and accounted for 0.50% of the country's population. Among the dimensions analysed, it presented very low income (0.56), a median mortality rate of preventable causes (31.0), vast income inequality (0.69), and a median COVID-19 mortality rate (151). In the 2018 election, 22.6% of municipalities (12) elected Bolsonaro.
Group 3, which belonged to node 27, had only 12 municipalities and 0.13% of the Brazilian population. Despite this, it registered the highest COVID-19 SMR (299). It was characterised by having low income (0.55), a high mortality rate from preventable causes (101), and income inequality (0.72). In the 2018 election, 41.6% of municipalities (5) elected Bolsonaro.
Group 4 was composed of 1476 small municipalities, with an average population of 32,000 inhabitants, comprising 30 million people (approximately 14% of the Brazilian population), located in the southern, southeastern, and central-western regions of the country. Group 4 was categorised at nodes 31, 32, 33, and 34 of the regression tree, with relatively low income/wealth inequality (0.47–0.48) and high income. Another similarity between all these nodes was the right-wing orientation, with around 95% of municipalities choosing Bolsonaro. The SMR of COVID-19 deaths per 100,000 inhabitants among these nodes was 123, a median rate compared with other Brazilian municipalities, but with important internal differences. Node 31 was composed of relatively rich municipalities located predominantly in the south of the country. Although presenting a low preventable mortality rate (0.7 per 100,000 inhabitants compared with 31.5 in the rest of Group 4) and good access to healthcare services, node 31 did not avoid COVID-19 deaths at the same efficiency, presenting an SMR of 93 deaths per 100,000 inhabitants compared with 132.7 in nodes 32, 33, and 34.
Group 5 consisted of 56 median income municipalities located in northeastern states distributed at nodes 39 and 40, representing about 2.3% of the Brazilian population. None of these municipalities voted for Bolsonaro. Municipalities clustered in node 39 presented less favourable socioeconomic indicators than node 40, as reflected in their SMR of COVID-19 deaths per 100,000 inhabitants (154 in node 39 and 106 in node 40).
Group 6 comprised about 100 small and medium-sized municipalities (up to 300,000 inhabitants), where about 6% of the Brazilian population lives; their Gini and income rates were better than the Brazilian average and rates of preventable causes lower than the national average (i.e., these municipalities had above-average socioeconomic indicators). Despite this, their COVID-19 mortality rates were well above the national average and a high percentage of the electorate voted for Bolsonaro in the second round. They were mainly located in the southeastern and southern regions of the country. This group exemplified that municipalities that supported Bolsonaro in 2018, even with indicators that demonstrate their greater capacities to deal with COVID-19, had high death rates from the disease.
Group 7, inserted at nodes 46 and 48, covered approximately 48% of the Brazilian population, with 330 municipalities. They were characterised by being capital cities or cities of regional importance (i.e., metropolitan regions). They were represented in all Brazilian regions, presenting better socioeconomic conditions than the country's average, with low rates of preventable causes (26.5); that is, good access to healthcare services. Nonetheless, this group—even cities with a highly diverse population—had COVID-19 rates (170 deaths per 100,000 inhabitants) above the national average and presented a high percentage of voting for Bolsonaro (79.7%), underscoring the impact of party choices on COVID-19.
Group 8, categorised at node 50 of the regression tree, consisted of only 15 municipalities, mostly from the northeastern region (14 of 15, or 93.3%), with a single municipality (Barcarena, PA) in the northern region. Together, Group 8 municipalities represented only 1.45% of the Brazilian population and exhibited income rates (HDI-Income = 0.649) and preventable death rates (30.3) close to the country's average. However, the COVID-19 SMR was slightly above the national average (161 deaths per 100,000 inhabitants). In contrast to this observation, the share of Bolsonaro's votes was remarkably low (only 25.7%), and he did not win in any Group 8 municipalities. This indicates that despite the socioeconomic indices being close to the national average, the slightly poor COVID-19 performance of Group 8 municipalities was not associated with strong support for the right-wing movement.
Group 9, categorised at node 51 of the regression tree, consisted of 21 municipalities that represented approximately 3.9% of the Brazilian population. Interestingly, 80% of the Group 9 population was from 10 municipalities comprising all capitals and cities with more than 100,000 inhabitants from northern states. The remaining 11 municipalities were from the southeastern, southern, and central-western regions. The key features of Group 9 included their relatively high income (HDI-Income = 0.718), while preventable deaths (31.0) were close to the national average. By contrast, the SMR of COVID-19 deaths was well above the country's average (approximately 255 deaths per 100,000 inhabitants). Predictably, Bolsonaro won in all 21 municipalities of this group in the 2018 presidential election. These data strongly indicated that in cities in the richer northern region, partisanship towards the right-wing movement was a strong driver of the poor COVID-19 outcome independent of the relatively high socioeconomic indices.
The municipalities in Groups 4 (with strong Bolsonaro support) and 5 (no Bolsonaro support) presented similar death rates from COVID-19. However, the social indices of the municipalities that comprise Groups 4 and 5 differed: municipalities in Group 4 were richer than those in Group 5, which had a worse income distribution (Gini) and lower-income (HDI-Income). Another aspect that distinguishes them was the rate of voting for Bolsonaro, which was 90% in municipalities that comprise Group 4 in contrast to Group 5, formed by poorer municipalities, in which none of the 56 municipalities supported Bolsonaro.
Group 3 (node 27), which registered the highest mortality rate (299.2), was composed of municipalities located in remote areas of Brazil, nine of them in the borderland strip of the northern region. They presented great vulnerabilities according to the HDIs. Moreover, their capacity to respond to emergencies was insufficient because they also had the highest mortality rate from preventable causes (101 per 100,000 inhabitants), which showed the shortcomings of the structure of healthcare services (promotion, surveillance, and healthcare) for routine actions. The municipalities that comprised Group 5 had an average preventable death rate of 33 per 100,000 inhabitants compared with 24 per 100,000 inhabitants in the municipalities clustered in Group 4. Further, all the nodes comprising Group 4 (nodes 31–34) showed a more intense second wave of COVID-19 deaths than the first one. The opposite was observed in nodes 39 and 40, clustered in Group 5, where Bolsonaro was not supported.
Group 7, composed of municipalities in Brazilian metropolitan regions, had municipal HDIs at the national average and low mortality rates from preventable causes, indicating more structured healthcare services than the national average. However, it showed a high COVID SMR (170–237 per 100,000 inhabitants), strongly affected by the second wave. Bolsonaro won in most municipalities in the second round.
Discussion
Public health problems occur in a multifactorial manner, and the COVID-19 pandemic has shown that behavioural factors, among the various conditioning factors affecting the occurrence of a health problem, were preponderant for the occurrence of the disease. Countries that ignored the problem had to backtrack on certain policies and faced problems during the pandemic that those countries that organised and followed the scientific knowledge about a new disease did not face.
In this sense, structural inequalities interplay with political positions, ideologies, and normative acts. In this study, party choices appearing in the lowest nodes of the tree may indicate that Brazil is marked by regional differences such as socioeconomic inequality, which are structural issues in the country. In this sense, our study contributes by shedding light on the more complex interaction between socioeconomic and political divides in the country than Catholic/Pentecostal, left-/right-wing, traditional/recently developed regions, and rural/urban, which are usually employed to explain election results and economic performance.34
However, given this general context, there is still a political party factor. Municipalities with similar socioeconomic profiles may have been differently affected by the pandemic depending on the local administration and ideological profile of the population that is reflected in its choice of party. Our analysis points out that as the first decision variable, the size and centrality of the municipality, which demonstrates the combination of contextual variables with the denial behaviour of an uninformed population, highly affected the outcome and translated into deaths. The opposite is also proven, as municipalities, even those with more deficient health conditions, lower-income, and greater inequality managed to go through the pandemic with less damage.
Denial discourse reinforces the initiatives of small groups—increasingly connected at a distance through digital platforms—that seek to protect themselves against a common, and sometimes imaginary, enemy. This discourse and practices are never oriented towards the virus itself, but rather its symbolic embodiment in institutions and public figures, therapeutic medicines, laws, socioeconomic activities, and minority groups that are adopted as enemies or allies. Adopting one or another enemy, which is marked by group identity, can influence the behaviour of people in their communities. More conscious or rational people, unlike extroverts, tend to adopt protective measures such as social isolation.35 A recent study demonstrated the unequal impact of the pandemic among US counties with different lifestyles,36 which is influenced by their socioeconomic status, place in the global economy, and consumption habits.
Not all behavioural changes recommended by institutions and legal frameworks are immediately incorporated by people, but are evaluated according to their source (i.e., the credibility of the institutions proposing these changes); the social context, including knowledge about the pandemic and virus transmission; and the subject to whom the message is addressed (potential vulnerability to illness, sensitivity, and beliefs).37 Faced with the profusion of news, standards, and technical information, people tend to assimilate knowledge and attitudes from political and community leaders, selected according to their beliefs, proposals, and power, to synthesise complex situations.38
In this sense, not only national leaders and media, but also local power groups, city halls, economic forces, and religious leaders in each community and municipality can influence the behaviour and beliefs of people affected by the pandemic. The (false) purpose of the Bolsonaro government to decentralise decisions on measures to control the pandemic, such as the adoption of ineffective medicines, the lack of encouragement of vaccines, and risk communication campaigns, strengthened local authorities (not only mayors but also groups with economic or symbolic power). This decision was contradicted by the attitude of President Bolsonaro, who openly criticised some measures to restrict mobility, including judicial actions by the Brazilian Supreme Court against governors' decrees.13
Since this is an ecological study and all variables were aggregated in municipalities as spatial units of analysis, we cannot assert that individuals identified with a certain ideology are prone to behave differently, are more exposed and have a higher risk of death. What this study design allows us to point out is that the impact of the pandemic is dependent on a combination of previous social and political conditions. In this sense, a municipality that could have better conditions to deal with pandemic management (better HDI, better health services and lower-income inequalities) may have higher mortality because of its political positioning. Other ecological studies carried out in Brazil have been showing that poverty, inequality and environmental contextual factors affect disease distribution and severity.39,40
The lack of integrated policies and national unity made each local manager adopt measures that met their local political and economic needs. The decentralization of policies to municipal governments also affected the health care emergence infrastructure. It was estimated that approximately one-quarter of COVID‐19 deaths in hospitals could be reduced with the correct management of hospital resources, as carried out in Belo Horizonte.41 In the municipalities of metropolitan areas, characterised by the intensity of people's movement and dependence on the same healthcare services and equipment, we observed the worst effects of the collapse of healthcare services and the failure of the pandemic's contingency, mainly during the first pandemic wave. On the other hand, an extreme decentralization of pandemic management measures was a characteristic of the second wave. Politically, the two waves were marked by the performance of different ministers of health: LH Madetta and N Teich from March 2019 to May 2020, and E Pazuello and M Queiroga from September 2020 onwards. The transition between ministers was also marked by increasing obedience to president Bolsonaro, and failures of national coordination when faced with problems such as the indiscriminate use of the “COVID kit”, the shortage of medical oxygen supply in Manaus, faltering in the purchase of vaccine, among other problems of pandemic management. These omissions by the Ministry of Health led to greater decentralisation and autonomy of municipalities to adopt control measures or strengthen the health system. This explains the main differences in the impact of the first and second waves in municipalities with a Bolsonaro orientation (see Figure 3C).
A practical example of the misinformation and denial of the problem, especially in these municipalities in metropolitan areas, was the question of population density. Even in mid-2020, some articles were pointing out the importance of this condition for the occurrence of COVID-19.42 In this period, calculations circulated on social networks that considered a population density of 280 people per km² similar to Italy; however, Rio de Janeiro's population density is 5.2 inhabitants per km², about 20 times that of Italy.43
The first phases of the pandemic were determined by the spatial arrangement and sociodemographic composition of cities; by contrast, in subsequent phases, particularly during the second wave, ideology and political orientation determined each city's ability to protect itself from infection and the subsequent effects on mortality. The decentralisation of decisions throughout 2021, insistence on the use of non-scientifically proven therapies such as chloroquine and hydroxychloroquine (part of “COVID kit”), and the free spread of erroneous or fake information about the disease may explain these differences in the dynamics of the pandemic.
Conclusions
In general, vulnerabilities related to income inequalities and health infrastructure shaped the dynamics of the first wave of COVID-19 in Brazil the most. Meanwhile, the second wave of COVID-19 was explicitly shaped by the partisan choice of municipalities. That is, municipalities that chose Bolsonaro as the country's president showed intensified COVID-19 mortality rates in the second wave. This behaviour can be explained by the fact that almost a year after the pandemic, the federal government still refused to support recommendations of social distancing and face mask-wearing or promoted early treatment using drugs proved to be ineffective months before. This boosted the risk behaviour of people aligned to the thinking of President Bolsonaro, exposing them to COVID-19 and resulting in a higher mortality rate. Thus, our analysis demonstrates that partisan choice was one of the factors explaining why Brazilian municipalities with the same inequality, income, and healthcare service characteristics behaved differently in the first and second waves of the COVID-19 pandemic.
As the pandemic is still unfolding, it remains to be seen how it can call critical attention to leaders’ political styles, tilt future elections, and exact accountability from those who failed to act properly. Overall, however, the illustrative examples in this paper suggest that world leaders mobilise familiar patterns of action and rhetoric when confronted with health crises: patterns that can be anticipated for pandemic planning at local, national, and global levels.19 Exactly which kinds of leaders mobilise such styles, under which circumstances, and to which outcomes, remain germane questions in studying the politics and governance of health crises.
Contributors
DRX: conceptualisation, writing original draft, writing review and editing, investigation; all authors contributed to the subsequent drafts and the final manuscript. ELS: writing original draft, editing, investigation. FAL: Conceptualisation, writing original draft, writing review, MFO: Conceptualisation, writing original draft, writing review, investigation; GRRS: Obtaining and organising the data and writing review and editing; HG: Conceptualisation, writing original draft, writing review and editing, investigation and mapping; CB: Conceptualisation, writing review, statistical analysis and mapping. All authors had access to all estimates presented in the paper and had final responsibility for the decision to submit for publication. HG and CB accessed and verified the underlying data.
Data sharing statement
All data used in this study are publicly available.
Editorial disclaimer
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
None.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2022.100221.
Appendix. Supplementary materials
References
- 1.Hofmeister A.M., Seckler J.M., Criss G.M. Possible roles of permafrost melting, atmospheric transport, and solar irradiance in the development of major coronavirus and influenza pandemics. Int J Environ Res Public Health. 2021;18(6):3055. doi: 10.3390/ijerph18063055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Payne S. Family coronaviridae. Viruses. 2017:149–158. doi: 10.1016/B978-0-12-803109-4.00017-9. (From Understanding to Investigation) [DOI] [Google Scholar]
- 3.Worldometer - real time world statistics. https://www.worldometers.info/coronavirus/.
- 4.World Health Organization . World Health Organization; 2020. WHO Announces COVID-19 Outbreak a Pandemic.http://www.euro.who.int/en/health-topics/health-emergencies/coronaviruscovid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic [Google Scholar]
- 5.Coronavirus Death Rate (COVID-19) Worldometer. Coronavirus update (Live): reported cases and deaths by country or territory - coronavirus death rate (COVID-19). Available: https://worldometers.info.
- 6.World Health Organization . World Health Organization; 2020. Advice on the Use of Masks in the Context of COVID-19: Interim Guidance.https://apps.who.int/iris/handle/10665/331693 [Google Scholar]
- 7.Shultz J.M., Espinel Z., Espinola M., Rechkemmer A. Distinguishing epidemiological features of the 2013–2016 West Africa Ebola virus disease outbreak. Disaster Health. 2016;3(3):78–88. doi: 10.1080/21665044.2016.1228326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buss L.F., Prete C.A., Abrahim C.M.M., et al. Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science. 2021;371(6526):288–292. doi: 10.1126/science.abe9728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rocha R., Atun R., Massuda A., et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9(6):e782–e792. doi: 10.1016/S2214-109X(21)00081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naveca F.G., Nascimento V., Souza V.C., et al. COVID-19 in Amazonas, Brazil, was driven by the persistence of endemic lineages and P.1 emergence. Nat Med. 2021;27(7):1230–1238. doi: 10.1038/s41591-021-01378-7. [DOI] [PubMed] [Google Scholar]
- 11.Malta M., Vettore M.V., Silva C., et al. Political neglect of COVID-19 and the public health consequences in Brazil: The high costs of science denial. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathieu E., Ritchie H., Ortiz-Ospina E., et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- 13.Ferrante L., Duczmal L., Steinmetz W.A., et al. How Brazil's President turned the country into a global epicenter of COVID-19. J Public Health Pol. 2021;42:439–451. doi: 10.1057/s41271-021-00302-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Machado Silva H. The Brazilian scientific denialism through the American Journal of Medicine. Am J Med. 2021;134(4):415–416. doi: 10.1016/j.amjmed.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavalcanti A.B., Zampieri F.G., Rosa R.G., et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate COVID-19. N Engl J Med. 2020;19(383(21)):2041–2052. doi: 10.1056/NEJMoa2019014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor L. We are being ignored': Brazil's researchers blame anti-science government for devastating COVID surge. Nature. 2021;593(7857):15–16. doi: 10.1038/d41586-021-01031-w. PMID: 33907333. [DOI] [PubMed] [Google Scholar]
- 17.Souza Santos A.A., Candido D.D.S., de Souza W.M., et al. Dataset on SARS-CoV-2 non-pharmaceutical interventions in Brazilian municipalities. Sci Data. 2021;8(1):73. doi: 10.1038/s41597-021-00859-1. Mar 4PMID: 33664243; PMCID: PMC7933188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baumeister R.F., Dale K., Sommer K.L. Freudian defense mechanisms and empirical findings in modern social psychology: reaction formation, projection, displacement, undoing, isolation, sublimation, and denial. J Personal. 1998;66:1081–1124. doi: 10.1111/1467-6494.00043. [DOI] [Google Scholar]
- 19.Lasco G. Medical populism and the COVID-19 pandemic. Glob Public Health. 2020;15(10):1417–1429. doi: 10.1080/17441692.2020.1807581. [DOI] [PubMed] [Google Scholar]
- 20.Lancet COVID-19 in Brazil: “so what”? (Editorial) Lancet. 2020;395(10235):1461. doi: 10.1016/S0140-6736(20)31095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Druckman J.N., Klar S., Krupnikov Y., Levendusky M., Ryan J.B. Affective polarization, local contexts and public opinion in America. Nat Hum Behav. 2021;5(1):28–38. doi: 10.1038/s41562-020-01012-5. [DOI] [PubMed] [Google Scholar]
- 22.Clinton J., Cohen J., Lapinski J., Trussler M. Partisan pandemic: how partisanship and public health concerns affect individuals' social mobility during COVID-19. Sci Adv. 2021;6(7(2)):eabd7204. doi: 10.1126/sciadv.abd7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.[preprint] Cabral, Ito, Pongeluppe L. The disastrous effects of leaders in denial: evidence from the COVID-19 Crisis in Brazil. SSRN: https://ssrn.com/abstract=3836147.
- 24.Niquini R.P., Lana R.M., Pacheco A.G., et al. Description and comparison of demographic characteristics and comorbidities in SARI from COVID-19, SARI from influenza, and the Brazilian general population. Cad Saude Publica. 2020;36(7) doi: 10.1590/0102-311x00149420. [DOI] [PubMed] [Google Scholar]
- 25.DATASUS. Ministry of Health. SRAG 2020 - severe acute respiratory syndrome database—including data from COVID-19. Surveillance of severe acute respiratory syndrome (SARS). 2021. https://opendatasus.saude.gov.br/dataset/bd-srag-2021. Date accessed: Jun 17, 2021.
- 26.Brazilian Ministry of Health. Datasus. Population estimates. http://tabnet.datasus.gov.br/cgi/deftohtm.exe?popsvs/cnv/popbr.def. Date accessed: Jun 17, 2021.
- 27.Brazilian Institute of Geography and Statistics (IBGE). REGIC. Regions of influence of cities. https://www.ibge.gov.br/geociencias/cartas-e-mapas/redes-geograficas/15798-regioes-de-influencia-das-cidades.html?=&t=o-que-e]. Date accessed: Jun 10, 2021.
- 28.Applied Economy Research Institute (IPEA) Atlas of human development in Brazil. http://www.atlasbrasil.org.br/. Date accessed: May 6, 2021.
- 29.Superior Electoral Court (2018). Boletim de Urna - Segundo Turno. Retrivied from https://www.tse.jus.br/hotsites/pesquisas-eleitorais/resultados_anos/boletim_urna/2018/boletim_urna_2_turno.html.
- 30.Maimon O., Rokach L. In: Data Mining and Knowledge Discovery Handbook. Maimon O., Rokach L., editors. Springer; Boston: 2005. Decomposition methodology for knowledge discovery and data mining. [DOI] [Google Scholar]
- 31.Strobl C., Malley J., Tutz G. An introduction to recursive partitioning: rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol Methods. 2009;14:323–348. doi: 10.1037/a0016973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strasser H., Weber C. On the asymptotic theory of permutation statistics. Math Methods Stat. 1999;8:220–250. [Google Scholar]
- 33.Zeileis A., Hornik K. Unbiased recursive partitioning: a conditional inference framework. J Comput Graph Stat. 2006;15:651–674. [Google Scholar]
- 34.Terry H. Quels sont les facteurs associés à la propagation de l’épidémie de Covid-19 au Brésil? Diploweb.com (la revue géopolitique), 5 juillet 2020.
- 35.Carvalho L.F., Pianowski G., Gonçalves A.P. Personality differences and COVID-19: are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends Psychiatry Psychother. 2020;42(2):179–184. doi: 10.1590/2237-6089-2020-0029. [DOI] [PubMed] [Google Scholar]
- 36.Ozdenerol E., Seboly J. Lifestyle effects on the risk of transmission of COVID-19 in the United States: evaluation of market segmentation systems. Int J Environ Res Public Health. 2021;30(18(9)):4826. doi: 10.3390/ijerph18094826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fazio R.H., Ruisch B.C., Moore C.A., Granados Samayoa J.A., Boggs S.T., Ladanyi J.T. Who is (not) complying with the U. S. social distancing directive and why? Testing a general framework of compliance with virtual measures of social distancing. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0247520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gramacho W., Turgeon M., Kennedy J., Stabile M., Mundim P.S. Political preferences, knowledge, and misinformation about COVID-19: the case of Brazil. Front Political Sci. 2021 doi: 10.3389/fpos.2021.646430. [DOI] [Google Scholar]
- 39.San Pedro A., Oliveira R.M. Tuberculosis and socioeconomic indicators: systematic review of the literature. Rev Panam Salud Publica. 2013;33(4):294–301. doi: 10.1590/s1020-49892013000400009. [DOI] [PubMed] [Google Scholar]
- 40.Silva C.L.M., Fonseca S.C., Kawa H., Palmer D.O.Q. Spatial distribution of leprosy in Brazil: a literature review. Rev Soc Bras Med Trop. 2017;50(4):439–449. doi: 10.1590/0037-8682-0170-2016. [DOI] [PubMed] [Google Scholar]
- 41.Brizzi A., Whittaker C., Servo L.M.S., et al. Imperial College London; 2021. Factors Driving Extensive Spatial and Temporal Fluctuations in COVID-19 Fatality Rates in Brazilian Hospitals. [DOI] [Google Scholar]
- 42.Carozzi F. London School of Economics & Political Science (LSE); 2020. Urban Density and Covid-19.https://www.iza.org/publications/dp/13440/urban-density-and-covid-19 IZA, Discussion Paper No. 13440. [Google Scholar]
- 43.Brazilian Institute of Geography and Statistics (IBGE). Cidades. Brazilian Institute of Geography and Statistics (IBGE) https://cidades.ibge.gov.br/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.