Abstract
Background:
Preoperative diagnosis of concomitant meniscal tears in pediatric and adolescent patients with acute anterior cruciate ligament (ACL) deficiency is challenging.
Purpose:
To investigate the diagnostic performance of magnetic resonance imaging (MRI) in detecting meniscal injuries for pediatric and adolescent patients with acute ACL tears.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
The authors retrospectively identified patients aged ≤18 years who underwent acute ACL reconstruction between 2006 and 2018 at 2 tertiary academic hospitals. The primary outcomes were arthroscopically confirmed medial, lateral, or any (defined as medial and/or lateral) meniscal tears. To control for chronically deficient knees, patients must have received their MRI study within 4 weeks of injury and must have undergone surgery no more than 8 weeks after their MRI study. Preoperative MRI reports were compared with the gold standard of arthroscopically confirmed tears to calculate sensitivity, specificity, positive predictive value, and negative predictive value. In a secondary analysis, patients were stratified by age into 2 groups (≤13 or ≥14 years), body mass index-for-age data from the Centers for Disease Control were used to classify patients as obese or nonobese, and differences between sensitivity and specificity proportions were analyzed using chi-square test for homogeneity.
Results:
Overall, 406 patients with a mean age of 15.4 years (range, 10-18 years) were identified. The sensitivity, specificity, positive predictive value, and negative predictive value were as follows: for lateral meniscal (LM) tears, 51.0%, 86.5%, 78.3%, and 65.0%; for medial meniscal tears, 83.2%, 80.6%, 62.3%, and 92.5%; and for any meniscal tear, 75.0%, 72.1%, 81.5%, and 63.8%, respectively. In the stratified analysis, MRI was less specific for the following diagnoses: any meniscal tear in patients aged ≤13 years (P = .048) and LM tears in obese patients (P = .020).
Conclusion:
The diagnostic ability of MRI to predict meniscal injuries present at acute ACL reconstruction was moderate. Performance was poorest at the lateral meniscus, where MRI failed to detect 97 tears that were found arthroscopically. Specificity was significantly lower in younger patients for any meniscal tear and in obese patients for LM tears.
Keywords: pediatric, adolescent, meniscus, MRI, sensitivity, specificity
Magnetic resonance imaging (MRI) is one of the most used imaging modalities in evaluating intra-articular knee injuries. In the pediatric and adolescent population, the ability to detect meniscal tears using MRI varies from poor to excellent. 2,16,27,33,35,40,42 The highest measurements of sensitivity and specificity (ranging from 87.0% to 95.0%) have been reported in studies with small samples of anterior cruciate ligament (ACL)-deficient knees, making them difficult to generalize for the growing number of young patients with ACL injuries. 2,16,27,32,33,42 Further, significant differences in diagnostic accuracy have been observed among younger, immature populations. 27,34,35,40 Limitations that we perceived from published literature were the inclusion of patients with substantial delays between MRI and surgery (in 2 studies, this approached 1 year), as well as no differentiation between acute and chronic ACL-deficient knees. 16,38 As the incidence of ACL injuries has risen in this patient population in the last 20 years, the importance of accurately diagnosing meniscal pathology cannot be understated as ACL injuries are highly associated with concomitant meniscal tears. 11,12,40 In clinical practice, the implications affect informed consent, operative planning, and assigning postoperative rehabilitation protocols.
The purpose of this study was to investigate the diagnostic performance of MRI in detecting meniscal injuries for pediatric and adolescent patients with acute ACL tears. A secondary stratified analysis was conducted to compare sensitivity and specificity measurements between cohorts to determine whether differences existed across age groups or among obese patients.
Methods
The patients in this study were incorporated retrospectively into an ACL registry that was maintained by 2 tertiary academic medical centers between 2006 and 2018. Included were patients undergoing ACL reconstruction (Current Procedural Terminology code 29888) who had no prior ipsilateral knee injury and who were aged ≤18 years at the time of surgery. To control for chronically unstable knees, patients could not have received their diagnostic MRI scan >4 weeks from their reported injury and must have undergone surgery within 8 weeks of their diagnostic MRI scan. Both cutoffs were chosen a priori, following the example of Church and Keating, 4 to limit our analyses to ACL tears without extensive chronicity. Demographic factors gathered for the registry included age, sex, and body mass index (BMI). The date of injury was reported by patients during their first encounter and collected from medical record review. Imaging and operative reports provided precise dates of MRI and surgery. The primary outcomes were any arthroscopically identified medial meniscal (MM) tears, lateral meniscal (LM) tears, and any meniscal tears (defined as a knee with a medial and/or lateral tear). Tears were recorded as positive regardless of whether they underwent any additional surgical intervention.
MRI Protocol
At tertiary hospital A, the standard MRI knee protocol over the course of the study period was proton density (PD)-weighted sequences with and without fat saturation. A T2-weighted fast-spin (FS) sequence was included as a replacement to PD in 1 plane, typically coronal. At tertiary hospital B, the standard MRI knee protocol over the course of the study period was also PD-weighted sequences with and without fat saturation. T2-weighted FS sequences were always taken in the coronal and the axial plane, and a T1-weighted FS coronal sequence was also taken. In composing the ACL registry, we determined the presence of a meniscal tear on MRI scan using the final radiology report.
Statistical Analysis
Data collected included age, sex, BMI, time interval from injury to MRI, and time interval from MRI to ACL reconstruction. For the primary outcomes, baseline characteristics were reported as a mean and SD or frequency and percentage. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated using MRI findings as a diagnostic tool and arthroscopy as the gold standard. Total true positive, true negative, false positive, and false negative results were reported separately for MM, LM, any meniscal tear, and no meniscal tear. Stratified analysis was conducted to compare sensitivity and specificity measurements at the medial, lateral, and any meniscus. Patients were age-stratified into 2 groups, those aged ≤13 years and those aged ≥14 years. BMI-for-age data from the Centers for Disease Control and Prevention were used to classify patients as obese (≥95th percentile) or nonobese. 3 Differences between sensitivity and specificity proportions were tested using the chi-square test for homogeneity. Statistical significance was set at P < .05. All statistics and calculations were conducted using SPSS Version 26.0 (IBM, Armonk, NY).
Results
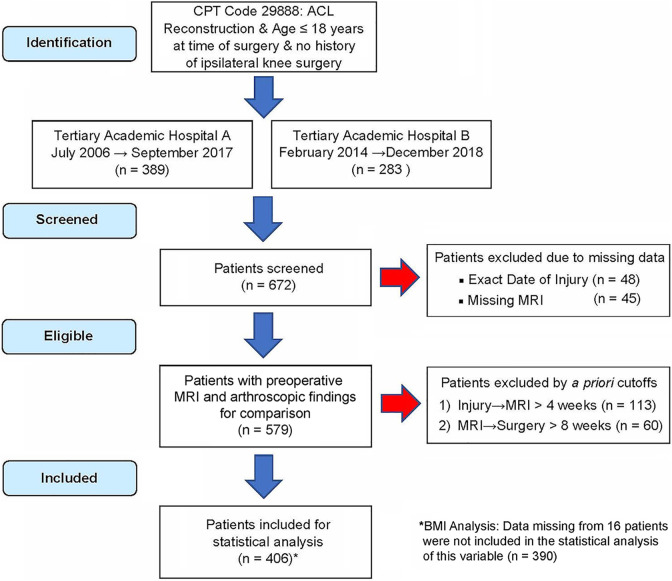
During the study period, 672 patients were identified (Figure 1). A total of 45 patients were missing a preoperative MRI study within their medical record and were excluded. While the date of MRI and surgery were reliable, occasionally patients did not remember their exact date of injury. A total of 48 patients were excluded for this reason. A total of 113 patients were excluded because their delay from reported date of injury until MRI exceeded 4 weeks. In the ensuing step, 60 patients were further excluded because their delay from date of MRI until surgery exceeded 8 weeks. Of note, 16 patients were missing BMI data; when reporting statistics and analyses for this variable, we excluded these patients.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram for patients included in the study. ACL, anterior cruciate ligament; BMI, body mass index; CPT, Current Procedural Terminology; MRI, magnetic resonance imaging.
A total of 406 patients with a mean age of 15.4 ± 1.6 years (range, 10-18 years) were included. Females comprised 53.0% of patients. Of the 390 patients with BMI data, 66 (16.9%) were classified as obese. Hospital A contributed 257 (63.3%) patients, and hospital B contributed 149 (36.7%) patients. On average, patients received their MRI scan 1.3 ± 1.0 weeks after their reported injury (range, 0-4 weeks) and underwent surgery 3.8 ± 1.7 weeks after their MRI scan (range, 0-8 weeks). In total, the average time elapsed between injury and surgery for all patients was 5.0 ± 2.1 weeks (range, 0-12 weeks).
Most patients, 252 (62.1%), had at least 1 meniscal tear present at surgery. Of these tears, 198 were LM, 113 were MM, and 59 occurred bilaterally. Of the 198 LM tears, all but 6 received operative treatment, and, of the 113 MM tears, all but 1 received operative treatment. The age; frequencies of female patients and obese patients are reported for each primary outcome in Table 1. Sensitivity, specificity, PPV, and NPV are reported for each primary outcome.
TABLE 1.
Primary Outcome Descriptive Data and MRI Diagnostic Performance a
| Any Meniscal Tear (n = 252) |
No Meniscal Tear (n = 154) |
Lateral Meniscus Tear (n = 198) |
Medial Meniscal Tear (n = 113) |
|
|---|---|---|---|---|
| Age, y, mean ± SD | 16.1 ± 1.5 | 15.7 ± 1.5 | 16.1 ± 1.4 | 16.1 ± 1.6 |
| Female sex | 117 (46.4) | 98 (63.6) | 82 (41.4) | 64 (56.6) |
| Obese | 41/236 (17.4) | 25/154 (16.2) | 29/187 (15.5) | 21/104 (20.2) |
| Hospital A patients | 113 (44.8) | 144 (93.5) | 95 (48.0) | 33 (29.2) |
| Hospital B patients | 139 (55.2) | 10 (6.5) | 103 (52.0) | 80 (70.8) |
| MRI diagnostic performance | ||||
| True positive, n | 189 | — | 101 | 94 |
| False negative, n | 63 | — | 97 | 19 |
| False positive, n | — | 43 | 28 | 57 |
| True negative, n | — | 111 | 180 | 236 |
| Sensitivity, % | 75.0 | — | 51.0 | 83.2 |
| Specificity, % | 72.1 | — | 86.5 | 80.6 |
| PPV, % | 81.5 | — | 78.3 | 62.3 |
| NPV, % | 63.8 | — | 65.0 | 92.5 |
a Data are reported as n (%) unless otherwise indicated. MRI, magnetic resonance imaging; NPV, negative predictive value; PPV, positive predictive value. Dashes indicate not applicable.
Stratified analyses by age and obesity are presented in Table 2. Of note, 42 patients were aged ≤13 years at surgery, representing 10.3% of the study population. Obese patients comprised 16.9% of the study population (66 of 390 total patients with BMI data). Among age groups, MRI was less specific when used to detect any meniscal tear in patients aged ≤13 years relative to patients aged ≥14 years (54.5% vs 75.0%; P = .048). In obese patients, MRI was less specific when used to detect LM tears relative to nonobese patients (75.7% vs 89.8%; P = .020).
TABLE 2.
Diagnostic Performance of MRI by Injury a
| Age | Body Mass Index | |||||
|---|---|---|---|---|---|---|
| ≤13 y | ≥14 y | P | Obese | Nonobese | P | |
| Sensitivity, % | ||||||
| Any meniscal tear | 80.0 | 74.6 | .590 | 85.4 | 74.9 | .149 |
| Lateral meniscal tear | 64.3 | 50.0 | .303 | 62.1 | 53.1 | .284 |
| Medial meniscal tear | 70.0 | 84.5 | .243 | 85.7 | 84.3 | .876 |
| Specificity, % | ||||||
| Any meniscal tear | 54.5 | 75.0 | .048 | 60.0 | 74.4 | .141 |
| Lateral meniscal tear | 78.6 | 87.8 | .184 | 75.7 | 89.8 | .020 |
| Medial meniscal tear | 81.3 | 80.5 | .915 | 82.2 | 80.1 | .745 |
a Bolding indicates statistically significant difference between groups (P < .05). MRI, magnetic resonance imaging.
Discussion
We reviewed 406 pediatric and adolescent patients undergoing ACL reconstruction to assess the diagnostic performance of MRI. Findings indicated that the sensitivity, specificity, PPV, and NPV, respectively, were as follows: for LM tears, 51.0%, 86.5%, 78.3%, and 65.0%; for MM tears, 83.2%, 80.6%, 62.3%, and 92.5%; and for any meniscal tear, 75.0%, 72.1%, 81.5%, and 63.8%. While this topic has been examined in previous papers, this study represents the largest cohort of pediatric and adolescent patients with acute ACL injuries and concomitant meniscal tears to date. In addition, cutoffs employed for the time elapsed from date of injury to date of MRI (4 weeks) and from date of MRI to date of surgery (8 weeks) prevented the inclusion of patients with chronic ACL deficiency. This is important because of the propensity for new meniscal tears (especially on the medial side) to occur before surgery, a trend that has been described extensively in recent literature. 1,6,21,31,37,38
We found that the diagnostic ability of MRI to predict meniscal injuries present at ACL reconstruction was moderate. False-positive rates were higher for MM tears, while false-negative rates were higher for LM injuries. Perhaps most concerning, MRI failed to detect 97 LM tears that were later found arthroscopically. In patients aged ≤13 years, the ability of MRI to correctly detect no tear in any meniscus was significantly lower than the ability in their older counterparts. Likewise, in obese patients compared with their counterparts, the ability of MRI to correctly detect no LM tear was significantly lower.
MRI is an essential noninvasive test to assess intra-articular knee pathology. 14,41,47 In the pediatric and adolescent population, MRI is extremely reliable at assessing ACL injuries among patients with suspected intra-articular pathology. 27,33,42 Similar encouraging literature has been published documenting the ability of MRI to detect MM and LM injuries. 2,16,27,32 –34,42 However, MRI is seemingly more reliable in detecting meniscal tears when these are in isolation than when associated with an ACL injury. 8,9,35,40 A 2014 study by Nam et al 36 examined traumatic meniscal lesions in adults and adolescents who had either an acute ACL tear or an intact ACL. The sensitivity for detecting LM and MM tears via MRI was significantly lower in the cohort with an acute ACL tear (70.2% MM, 71.4% LM) relative to patients without an acute ACL tear (94.0% MM, 82.1% LM). 36 In 2014, Gans et al 16 examined 178 pediatric and adolescent patients with various knee conditions. Likewise, in patients with >1 intra-articular lesion, meniscal tears were less likely to be diagnosed correctly using MRI. 16 Table 3 presents a comparison of study design parameters and diagnostic measurements across peer-reviewed literature. Studies are sorted in descending order based on the sample size of patients with ACL deficiency.
TABLE 3.
Comparison of Similar Intra-Articular Diagnostic MRI Studies a
| Diagnostic Performance of MRI | ||||||||
|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Sample Size b | Concomitant ACL Tear, n (%) b | Age, y c | Time From Injury to MRI, wk c | Time From MRI to Surgery, wk c | Any Meniscal Tear | Medial Meniscal Tear | Lateral Meniscal Tear |
| Present study | 406 | 406 (100) | 15.9 (10-18) | 1.3 (0.0-4.0) | 3.8 (0.1-8.0) | Sn: 75.0% Sp: 72.1% |
Sn: 83.2% Sp: 80.6% |
Sn: 51.0% Sp: 86.5% |
| Munger (2019) 35 | 107 | 107 (100) | 15 (7-18) | 2.4 (0.1-74.6) | 5.4 (0.4-12.4) | Sn: 62.3% Sp: 68.4% |
NR | NR |
| Samora (2011) 40 | 69 | 69 (100) | 14.1 (12.7-16.1) | NR d | NR d | Sn: 58.7% Sp: 91.3% |
NR | NR |
| Gans (2014) 16 | 178 | 54 (30.3) | 13.9 | NR | 6.4 (0-46.3) | NR | Sn: 87.5% Sp: 91.1% |
Sn: 67.5% Sp: 94.9% |
| Schub (2012) 42 | 119 | 47 (39.5) | 16 (10-19) | NR | 6.6 (0.1-52.3) | NR | Sn: 81.0% Sp: 90.9% |
Sn: 68.8% Sp: 93.0% |
| Luhmann (2005) 32 | 96 | 39 (40.6) | 14.6 (7.3-18.7) | 13 (2 wk-5 y) | NR | NR | Sn: 94.4% Sp: 91.0% |
Sn: 88.9% Sp: 87.0% |
| Kocher (2001) 27 | 118 | 32 (27.1) | 12.6 | NR | NR | NR | Sn: 79.3% Sp: 92.0% |
Sn: 66.7% Sp: 82.8% |
| Major (2003) 33 | 59 | 25 (42.4) | 15 (11-17) | NR | NR | NR | Sn: 92.0% Sp: 87.0% |
Sn: 93.0% Sp: 95.0% |
| Bouju (2011) 2 | 69 | 21 (30.4) | 13.3 (9-16) | 33 | 8.3 | Sn: 70.0% Sp: 81.0% |
Sn: 75.0% Sp: 77.0% |
Sn: 78.0% Sp: 69.0% |
a ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; NR, not reported; Sn, sensitivity; Sp, specificity.
b Presented in descending order by number of patients in study with concomitant ACL tear.
c Mean and range (if reported).
d Inclusion criteria were patients undergoing surgery within 3 months of injury.
Multiple hypotheses have been presented as to why visualizing concomitant meniscal tears in patients with acute ACL injury on MRI scans still poses a diagnostic challenge. The subject of many previous studies has been the LM tear, where false-negative rates are consistently highest. 13,27,34,42 Tear locations, such as the posterior horn of the lateral meniscus, and oblique tear orientation have been the most difficult for imaging planes to visualize adequately. 7 –9,23,30 However, no specific clinical characteristics such as patient age, injury mechanism, delay from injury to imaging, delay from imaging to surgery, or magnetic resonance sequence type are significantly associated with lowering false-negative rates at the lateral meniscus. 9,24,30
Imaging pediatric and adolescent patients also present distinctive challenges, both in capturing and interpreting images. Motion artifact, patient pain tolerance, developmental maturity, and other underlying conditions have been presented as challenges with image acquisition. 20,39,45 In interpreting studies, training background and experience have correlated with higher interpreting reliability among radiologists in 1 study yet yielded no significant difference in another. 25,46 One of the elements cited most often as influencing study interpretation is the underlying anatomical variations among pediatric and adolescent patients. Specifically, the increased vascularity in the preadolescent meniscus and its effect on imaging has been thoroughly described. 5,15,16,26,27,32,41,47 Furthermore, a high signal in the meniscus has been observed in both atraumatic and asymptomatic children and adolescents in additional studies. 28,29,44 Conceivably, higher false-positive rates among patients aged ≤13 years can be a manifestation of falsely interpreting high signal in the menisci as a positive study. However, this conjecture and others presented in literature are mostly speculative.
In the present study, the patients analyzed came from the same geographical area but differed in rural versus metropolitan setting. The patients in hospital A were younger and had a higher proportion of females compared with those in hospital B. In addition, data from 1 institution spanned 11 years, while data from the other spanned 4 years. However, because they represent 2 distinct and diverse patient populations, the study results are more likely to be generalizable.
The strengths of the present study include the largest population of pediatric and adolescent patients presented in literature to date, in addition to meticulous detail as to the timing of interventions, with strict time interval cutoffs. In examining the peer-reviewed literature, we found this practice to be inconsistent. By strictly including only patients with time from MRI to surgery of ≤8 weeks, the current study reduced the risk of false-negative MRI results by minimizing the time in which a new injury could be sustained.
A shorter time interval is also an important consideration for this population in controlling for the inverse outcome (ie, false-positive MRI results representing true tears that healed before surgery). This phenomenon has been the topic of multiple previous studies. 10,19,22,24 Notably, a 2014 investigation by Kijowski et al 24 reported 17 of 18 tears located at the medial meniscus outer rim had healed before surgery. Mean time from MRI to surgery for all patients in this study was 48 days (range, 12-98 days). In another study of 7 longitudinal tears of the posterior horn of the medial meniscus treated conservatively, at repeat arthroscopy 3 months later, 6 of 7 tears were healed. 19
We observed that, in the existing literature, it was common to use longer time intervals to increase the size of the study cohort size. 16,32,35,42 To that end, imposing a strict time frame as we have done between the diagnostic MRI and its confirmatory arthroscopy aimed to control for confounding variables that would overestimate both false-negative and false-positive rates.
We recognize the intrinsic limitations of this study. It was retrospective and thus prone to selection bias as well as differences in institutional record keeping. One flaw was the reliance of radiologist reports rather than independent review with intra- and interrater reliability. Furthermore, multiple radiologists and multiple surgeons provided data. During the 11-year study period, 3.0-T magnets were adopted. Data detailing which MRI studies were gathered using 1.5-T magnets and which were gathered using 3.0-T magnets was not available to the researchers. Nevertheless, since their introduction into clinical practice, the question of whether new scanners, capable of generating twice the magnetic field strength, are indeed more diagnostically accurate has been thoroughly investigated. 17,18,42,43 Specifically, as it pertains to diagnosing meniscal tears, data from multiple studies have shown comparable accuracy but no significant diagnostic superiority in favor of 3.0-T machines. A 2021 study by Hancock et al 18 examined 330 pediatric and adolescent patients (mean age, 13.5 years) with any intra-articular knee pathology, with 125 patients receiving MRI with 3.0-T magnet strength and 205 receiving 1.5-T MRI. Mean time between MRI scan and surgery was 120 days. No significant difference in accuracy (sensitivity or specificity) was reported for any knee pathology (ACL rupture, meniscal tear, osteochondral defects, or chondral lesions) 18 Furthermore, a 2016 meta-analysis by Smith et al 43 examined the efficacy of 3.0-T machines and compared diagnostic measures to a previous meta-analysis with 1.5-T machines.
This study included pediatric, adolescent, and adult patients, with a mean age of 41.9 years. Mean time between MRI and surgery was 47.4 days. At the medial meniscus, no significant difference in sensitivity or specificity was found. At the lateral meniscus, there was no significant difference in sensitivity, but there was a significantly greater specificity for detecting LM tears in favor of the 1.5-T machines (95.7% vs 87.0%). 43
Differences in specialty training (pediatric vs adult specialized and sports fellowship training) were known to exist at each institution. In addition, the use of birth age as a proxy measurement for maturity was used as opposed to bone age or physeal patency. This method has previously been used in published literature. 27,34,35 In agreement, we believe that a study that analyzes MRI as a screening test for the pediatric and adolescent population is justified in using a general measurement such as birth age for a cutoff. Often, surgeons examining a patient at an initial visit after an ACL injury will not have an accurate bone age or physeal patency to reference. Birth age, however, will be a known constant regardless and, thus, an acceptable proxy measurement to gauge potential accuracy of the screening MRI study.
The results of this study suggest that MRI is better at screening patients for MM tears than LM tears. In patients aged ≥14 years, MRI is more specific for any meniscal tear and, in nonobese patients, more specific for the LM tears. MRI also appears to positively predict LM tears more effectively than MM tears. It is worth noting that our study redemonstrates that LM tears are more common than MM tears in patients with acute ACL deficiency, in agreement with previous literature. 1,31,37 The implications of this are worth highlighting, as the prevalence of a disease directly influences pretest probability. In this study, the roughly 2-fold likelihood that a patient would have a true LM tear instead of a MM tear influenced both PPV and NPV. Hence, because LM tears are more prevalent with acute ACL injuries, the PPV of an MRI study was expected to be greater (LM PPV, 78.3% vs MM PPV, 62.3%). Likewise, because MM tears are less common in acute ACL injuries, the NPV was expected to be greater (MM NPV, 92.5% vs LM NPV, 65.0%). We observed both trends in this study.
We recommend that preoperative discussions, including consent, with patients and their guardians should cover the possibility of finding undiagnosed meniscal tears at arthroscopy. Operative planning and postoperative rehabilitation protocols should also include these contingencies. Above all, clinicians should use sound judgment to correlate each patient’s ACL injury chronicity, mechanism, and other clinical factors when anticipating concomitant meniscal pathology in surgery from a positive or negative MRI study.
Conclusion
The diagnostic ability of MRI to predict meniscal injuries present at ACL reconstruction was moderate. Performance was poorest at the lateral meniscus, where MRI failed to detect 97 tears that were found arthroscopically. Among all patients, false-positive rates were higher for MM tears, while false-negative rates were higher for LM injuries. The specificity of MRI as a diagnostic tool for detecting any meniscal tear was significantly lower for patients aged ≤13 years as well as for detecting LM tears for obese patients.
Footnotes
Final revision submitted November 9, 2021; accepted November 29, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.D.F. has received hospitality payments from Medical Device Business Services. A.G. has received education payments from Arthrex. M.S. has received consulting fees and royalties from OrthoPediatrics and hospitality payments from Stryker. R.J.M. has received education payments from Arthrex, consulting fees from Medical Device Business Services and OrthoPediatrics, speaking fees from Philips Electronic North America, and hospitality payments from Globus Medical and Medical Device Business Services. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Geisinger Medical Center (reference No. 2018-0157).
References
- 1. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. doi:10.1177/0363546514559912 [DOI] [PubMed] [Google Scholar]
- 2. Bouju Y, Carpentier E, Bergerault F, de Courtivron B, Bonnard C, Garaud P. The concordance of MRI and arthroscopy in traumatic meniscal lesions in children. Orthop Traumatol Surg Res. 2011;97(7):712–718. doi:10.1016/j.otsr.2011.07.010 [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Clinical Growth Charts. https://www.cdc.gov/growthcharts/clinical_charts.htm
- 4. Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87(12):1639–1642. doi:10.1302/0301-620X.87B12.16916 [DOI] [PubMed] [Google Scholar]
- 5. Clark CR, Ogden JA. Development of the menisci of the human knee joint. J Bone Joint Surg Am. 1983;65(4):538–547. [PubMed] [Google Scholar]
- 6. Cohen M, Ferretti M, Quarteiro M, et al. Transphyseal anterior cruciate ligament reconstruction in patients with open physes. Arthroscopy. 2009;25(8):831–838. doi:10.1016/j.arthro.2009.01.015 [DOI] [PubMed] [Google Scholar]
- 7. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480–486. doi:10.2214/AJR.08.1300 [DOI] [PubMed] [Google Scholar]
- 8. De Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol. 1994;162(4):905–911. [DOI] [PubMed] [Google Scholar]
- 9. De Smet AA, Mukherjee R. Clinical, MRI, and arthroscopic findings associated with failure to diagnose a lateral meniscal tear on knee MRI. AJR Am J Roentgenol. 2008;190(1):22–26. doi:10.2214/AJR.07.2611 [DOI] [PubMed] [Google Scholar]
- 10. De Smet AA, Nathan DH, Graf BK, Haaland BA, Fine JP. Clinical and MRI findings associated with false-positive knee MR diagnoses of medial meniscal tears. AJR Am J Roentgenol. 2008;191(1):93–99. doi:10.2214/AJR.07.3034 [DOI] [PubMed] [Google Scholar]
- 11. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med. 2014;42(3):675–680. doi:10.1177/0363546513518412 [DOI] [PubMed] [Google Scholar]
- 12. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40(9):2128–2133. doi:10.1177/0363546512449994 [DOI] [PubMed] [Google Scholar]
- 13. Engelhardt LV, Schmitz A, Pennekamp PH, Schild HH, Wirtz DC, Falkenhausen F. Diagnostics of degenerative meniscal tears at 3-tesla MRI compared to arthroscopy as reference standard. Arch Orthop Trauma Surg. 2008;128(5):451–456. doi:10.1007/s00402-007-0485-6 [DOI] [PubMed] [Google Scholar]
- 14. Figueiredo S, Sa Castelo L, Pereira AD, Machado L, Silva JA, Sa A. Use of MRI by radiologists and orthopaedic surgeons to detect intra-articular injuries of the knee. Rev Bras Ortop. 2018;53(1):28–32. doi:10.1016/j.rboe.2016.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Francavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatr Radiol. 2014;44(8):910–925. doi:10.1007/s00247-014-3022-0 [DOI] [PubMed] [Google Scholar]
- 16. Gans I, Bedoya MA, Ho-Fung V, Ganley TJ. Diagnostic performance of magnetic resonance imaging and pre-surgical evaluation in the assessment of traumatic intra-articular knee disorders in children and adolescents: what conditions still pose diagnostic challenges? Pediatr Radiol. 2014;45(2):194–202. doi:10.1007/s00247-014-3127-5 [DOI] [PubMed] [Google Scholar]
- 17. Grossman JW, de Smet AA, Shinki K. Comparison of the accuracy rates of 3-T and 1.5-T MRI of the knee in the diagnosis of meniscal tear. AJR Am J Roentgenol. 2009;193(2):509–514. doi:10.2214/AJR.08.2101 [DOI] [PubMed] [Google Scholar]
- 18. Hancock GE, Hampton MJ, Broadley P, Ali FM, Nicolaou N. Accuracy of magnetic resonance imaging of the knee for intra-articular pathology in children: a comparison of 3 T versus 1.5 T imaging. J Arthrosc Joint Surg. 2021;8(2):172–176. doi:10.1016/j.jajs.2021.02.010 [Google Scholar]
- 19. Ihara H, Miwa M, Takayanagi K, Nakayama A. Acute torn meniscus combined with acute cruciate ligament injury: second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res . 1994;307:146–154. http://europepmc.org/abstract/MED/7924027 [PubMed]
- 20. Jaite C, Kappel V, Napp A, et al. A comparison study of anxiety in children undergoing brain MRI vs adults undergoing brain MRI vs children undergoing an electroencephalogram. PLoS One. 2019;14(3):e0211552. doi:10.1371/journal.pone.0211552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. James EW, Dawkins BJ, Schachne JM, et al. Early operative versus delayed operative versus nonoperative treatment of pediatric and adolescent anterior cruciate ligament injuries: a systematic review and meta-analysis. Am J Sports Med. 2021;49(14):4008–4017. doi:10.1177/0363546521990817 [DOI] [PubMed] [Google Scholar]
- 22. Jaremko JL, Guenther ZD, Jans LBO, MacMahon PJ. Spectrum of injuries associated with paediatric ACL tears: an MRI pictorial review. Insights Imaging. 2013;4(3):273–285. doi:10.1007/s13244-013-0250-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jee WH, McCauley TR, Kim JM. Magnetic resonance diagnosis of meniscal tears in patients with acute anterior cruciate ligament tears. J Comput Assist Tomogr. 2004;28(3):402–406. doi:10.1097/00004728-200405000-00017 [DOI] [PubMed] [Google Scholar]
- 24. Kijowski R, Rosas HG, Lee KL, Cheung A, del Rio AM, Graf BK. MRI characteristics of healed and unhealed peripheral vertical meniscal tears. AJR Am J Roentgenol. 2014;202(3):585–592. doi:10.2214/AJR.13.11496 [DOI] [PubMed] [Google Scholar]
- 25. Kim A, Khoury L, Schweitzer M, et al. Effect of specialty and experience on the interpretation of knee MRI scans. Bull NYU Hosp Jt Dis. 2008;66(4):272–275. [PubMed] [Google Scholar]
- 26. King SJ, Carty HM, Brady O. Magnetic resonance imaging of knee injuries in children. Pediatr Radiol. 1996;26(4):287–290. doi:10.1007/BF01372115 [DOI] [PubMed] [Google Scholar]
- 27. Kocher MS, DiCanzio J, Zurakowski D, Micheli LJ. Diagnostic performance of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee disorders in children and adolescents. Am J Sports Med. 2001;29(3):292–296. doi:10.1177/03635465010290030601 [DOI] [PubMed] [Google Scholar]
- 28. Kornick J, Trefelner E, McCarthy S, Lange R, Lynch K, Jokl P. Meniscal abnormalities in the asymptomatic population at MR imaging. Radiology. 1990;177(2):463–465. doi:10.1148/radiology.177.2.2217786 [DOI] [PubMed] [Google Scholar]
- 29. Laprade RF, Burnett QM, Veenstra MA, Hodgman CG. The prevalence of abnormal magnetic resonance imaging findings in asymptomatic knees: with correlation of magnetic resonance imaging to arthroscopic findings in symptomatic knees. Am J Sports Med. 1994;22(6):739–745. doi:10.1177/036354659402200603 [DOI] [PubMed] [Google Scholar]
- 30. Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament injury and the clinical relevance of missed tears. AMR Am J Roentgenol. 2009;193(2):515–523. doi:10.2214/AJR.08.2146 [DOI] [PubMed] [Google Scholar]
- 31. Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. doi:10.1177/0363546511420818 [DOI] [PubMed] [Google Scholar]
- 32. Luhmann SJ, Schootman M, Gordon JE, Wright RW. Magnetic resonance imaging of the knee in children and adolescents: its role in clinical decision-making. J Bone Joint Surg Am. 2005;87(3):497–502. doi:10.2106/00004623-200503000-00003 [DOI] [PubMed] [Google Scholar]
- 33. Major NM, Beard LN, Helms CA. Accuracy of MR imaging of the knee in adolescents. AMR Am J Roentgenol. 2003;180(1):17–19. doi:10.2214/ajr.180.1.1800017 [DOI] [PubMed] [Google Scholar]
- 34. McDermott MJ, Bathgate B, Gillingham BL, Hennrikus WL. Correlation of MRI and arthroscopic diagnosis of knee pathology in children and adolescents. J Pediatr Orthop. 1998;18(5):675–678. doi:10.1097/00004694-199809000-00024 [DOI] [PubMed] [Google Scholar]
- 35. Munger AM, Gonsalves NR, Sarkisova N, Clarke E, Vandenberg CD, Pace JL. Confirming the presence of unrecognized meniscal injuries on magnetic resonance imaging in pediatric and adolescent patients with anterior cruciate ligament tears. J Pediatr Orthop. 2019;39(9):E661–E667. doi:10.1097/BPO.0000000000001331 [DOI] [PubMed] [Google Scholar]
- 36. Nam TS, Kim MK, Ahn JH. Efficacy of magnetic resonance imaging evaluation for meniscal tear in acute anterior cruciate ligament injuries. Arthroscopy. 2014;30(4):475–482. doi:10.1016/j.arthro.2013.12.016 [DOI] [PubMed] [Google Scholar]
- 37. Newman JT, Carry PM, Terhune EB, et al. Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med. 2015;43(2):282–288. doi:10.1177/0363546514562168 [DOI] [PubMed] [Google Scholar]
- 38. Reid D, Leigh W, Wilkins S, Willis R, Twaddle B, Walsh S. A 10-year retrospective review of functional outcomes of adolescent anterior cruciate ligament reconstruction. J Pediatr Orthop. 2017;37(2):133–137. doi:10.1097/BPO.0000000000000594 [DOI] [PubMed] [Google Scholar]
- 39. Rothman S, Gonen A, Vodonos A, Novack V, Shelef I. Does preparation of children before MRI reduce the need for anesthesia? Prospective randomized control trial. Pediatr Radiol. 2016;46(11):1599–1605. doi:10.1007/s00247-016-3651-6 [DOI] [PubMed] [Google Scholar]
- 40. Samora WP, Palmer R, Klingele KE. Meniscal pathology associated with acute anterior cruciate ligament tears in patients with open physes. J Pediatr Orthop. 2011;31(3):272–276. doi:10.1097/BPO.0b013e31820fc6b8 [DOI] [PubMed] [Google Scholar]
- 41. Sanchez TRS, Jadhav SP, Swischuk LE. MR imaging of pediatric trauma. Radiol Clin North Am. 2009;47(6):927–938. doi:10.1016/j.rcl.2009.08.008 [DOI] [PubMed] [Google Scholar]
- 42. Schub DL, Altahawi F, Meisel AF, Winalski C, Parker RD, M. Saluan P. Accuracy of 3-Tesla magnetic resonance imaging for the diagnosis of intra-articular knee injuries in children and teenagers. J Pediatr Orthop. 2012;32(8):765–769. doi:10.1097/BPO.0b013e3182619181 [DOI] [PubMed] [Google Scholar]
- 43. Smith C, McGarvey C, Harb Z, et al. Diagnostic efficacy of 3-T MRI for knee injuries using arthroscopy as a reference standard: a meta-analysis. AMR Am J Roentgenol. 2016;207(2):369–377. doi:10.2214/AJR.15.15795 [DOI] [PubMed] [Google Scholar]
- 44. Takeda Y, Ikata T, Yoshida S, Takai H, Kashiwaguchi S. MRI high-signal intensity in the menisci of asymptomatic children. J Bone Joint Surg Br. 1998;80(3):463–467. doi:10.1302/0301-620X.80B3.8013 [DOI] [PubMed] [Google Scholar]
- 45. Uffman JC, Tumin D, Raman V, Thung A, Adler B, Tobias JD. MRI utilization and the associated use of sedation and anesthesia in a pediatric ACO. J Am Coll Radiol. 2017;14(7):924–930. doi:10.1016/j.jacr.2017.01.025 [DOI] [PubMed] [Google Scholar]
- 46. White LM, Schweitzer ME, Deely DM, Morrison WB. The effect of training and experience on the magnetic resonance imaging interpretation of meniscal tears. Arthroscopy. 1997;13(2):224–228. doi:10.1016/S0749-8063(97)90158-4 [DOI] [PubMed] [Google Scholar]
- 47. Zobel MS, Borrello JA, Siegel MJ, Stewart NR. Pediatric knee MR imaging: pattern of injuries in the immature skeleton. Radiology. 1994;190(2):397–401. doi:10.1148/radiology.190.2.8284387 [DOI] [PubMed] [Google Scholar]