Abstract
Background:
Outcomes following meniscal allograft transplantation (MAT) are an evolving topic.
Purpose:
To review clinical outcomes in younger, previously active patients who underwent an isolated MAT or MAT plus any osteotomy. Concurrent surgeries, complications, and graft survivorship are presented.
Study Design:
Case series; Level of evidence, 4.
Methods:
Inclusion criteria included having undergone MAT with a minimum of 1 year of follow-up with at least 1 of the following patient-reported outcome (PRO) measures collected pre- and postoperatively: visual analog scale for pain, Knee injury and Osteoarthritis Outcome Score (KOOS), the Western Ontario and McMaster Universities Arthritis Index, the 36-Item Short Form Health Survey, and overall satisfaction. From patient records, we recorded descriptive data, side (medial/lateral), previous or concurrent procedures, perioperative complications, revisions, and conversion to arthroplasty. Two-factor analysis of variance (ANOVA) was used to test for differences in age and body mass index (BMI). A 2 × 2 chi-square test was used to determine if the spectrum of procedures performed on our study’s patient group was representative of the entire population. PRO results were analyzed using a multivariate ANOVA.
Results:
From a total of 91 eligible patients, 61 (63 knees) met our inclusion criteria. Mean presurgery age was 25.5 ± 9.2 years, and mean BMI was 26.7 (range, 18.5-38.4). At follow-up (mean, 4.8 years; range, 1.0-13.6 years) overall PROs were statistically and clinically improved at final follow-up (P ≤ .003); effect sizes were moderate and large. KOOS Pain and KOOS Activities of Daily Living showed some main or interaction effects that were trivial or small. Patient satisfaction with the treatment was ≥7 out of 10 in 85% of patients. A minimum of 1 subsequent surgery for various concerns was necessary in 23% of the 93 knees. Graft survival in the included patients was 100%.
Conclusion:
Complications (conditions requiring at least 1 subsequent surgery) affected about one-quarter of the patients who underwent MAT. Nevertheless, MAT seemed to provide our patients with adequate pain relief and improved function.
Keywords: allograft, meniscal allograft transplantation, meniscectomy, postmeniscectomy syndrome, transplantation
Menisci have essential roles in load distribution, joint congruity, shock absorption, lubrication, and proprioception. 19,27,28 Meniscal tears are the most common injuries of the knee, with an incidence of 61 per 100,000 per year, 5 and arthroscopic surgery for meniscal injury is the most common procedure performed by orthopaedic surgeons. 15 There is increasing evidence reporting the detrimental effects of meniscectomy on the knee joint. 43 Baratz and colleagues 6 demonstrated that contact areas and peak local contact stresses increase significantly after either partial or total meniscectomy while surgical removal of a meniscus increases the relative risk (14.0) for tibiofemoral arthritis after 21 years. 43 Improved understanding of the biomechanical importance of the meniscus and the evolution of meniscal-preserving procedures has popularized meniscal repair. 12,36,38
Even with the best meniscal repair techniques, the failure rate (>20%) is still high regardless of surgical technique. 30,37,40,42 Given the failure rate of meniscal repair, meniscal allograft transplantation (MAT) was proposed and first performed as a salvage procedure 14 ; high-demand, competitive sports were discouraged to preserve the graft. 61 Case series and systematic reviews have summarized outcomes and graft survivorship from patients mostly ≥30 years of age who did not detail preoperative activity levels. 8,22,34,39,44,48 Several case reports have been reported in the literature with encouraging outcomes, 44 and the chondroprotective effects of MAT have also been reported in the literature, 1,3,20,24,47 although this remains controversial. 49,57
The primary aim of this study was to evaluate outcomes after MAT performed on a younger population that had been active previously (collegiate athletes)---a group that has been discussed infrequently. Another primary aim was a comparison of outcomes between patients who underwent an isolated transplantation (MAT) and patients who had a concurrent procedure performed at the time of the transplant (MAT+), be it a high tibial osteotomy (HTO) or a distal femoral osteotomy (DFO). The secondary aim was to review concurrent surgeries performed at the time of the index MAT, complications, and survivorship of MAT. We hypothesized that the graft would have a good-to-excellent survival at a medium-term follow-up, with no differences between MAT and MAT+.
Methods
Institutional review board approval (exempt) was obtained before initiation of this study. All cases of MAT performed by the senior surgeon (A.A.) between June 2001 and November 2014 were reviewed (91 patients; 93 knees). Included in this study were patients who had knee pain after a total or subtotal meniscectomy that required MAT. A minimum of 1 year follow-up was necessary for inclusion. Graft survival (defined as a revision procedure related to the initial MAT for complete graft removal or conversion to knee arthroplasty) was determined at this follow-up, from institutional records, or both. Each patient also needed to have completed at least 1 patient-reported outcome (PRO) measure preoperatively and at one’s most recent follow-up. PRO measures included a 10-cm visual analog scale for pain (VAS), the Knee injury and Osteoarthritis Outcome Score (KOOS), the Western Ontario and McMaster Universities Arthritis Index (WOMAC; 100-mm VAS version), and the 36-Item Short Form Health Survey (SF-36).
Patient satisfaction at the time of most recent follow-up was collected (0 = highly dissatisfied, 10 = highly satisfied). Descriptive information, surgical details (including which meniscus was transplanted), and radiographic data were collected from medical records. Radiographic information was obtained from preoperative and most recent reports of full-length weightbearing imaging in the standing position and from standard anteroposterior and lateral knee views. The radiographic information was used to assess lower limb alignment and degenerative changes according to the Kellgren and Lawrence (KL) system. 23 All 91 eligible patients were contacted by telephone or secure email and offered a free-of-charge clinic visit for clinical and radiographic evaluation as well as completing the follow-up PRO questionnaires. From our review of medical records, we recorded the number and type of procedures performed concurrent with the MAT. We also recorded complications and any subsequent procedures performed at our institution. Time to graft failure was used to determine graft survival where failure was defined as a revision procedure related to the initial MAT (for complete graft removal) or as conversion to (total or unilateral) knee arthroplasty.
Surgical Technique
MAT was performed by the senior author (A.A.), a fellowship-trained sports medicine foot and ankle surgeon. Grafts were sized on anteroposterior and lateral radiographs of the knee according to the method described by Pollard et al, 41 and the size was confirmed based on preoperative magnetic resonance imaging scans. Medial MAT was performed using the 2 bone-plug technique with the anterior and posterior horns each attached to a separate bone plug. Lateral MAT was performed using a modified bone-bridge technique in which the graft contained a common bone bridge attached to both anterior and posterior horns. 58 We used fresh-frozen allografts in all cases.
When patients showed a valgus alignment (mechanical tibiofemoral angle >180°), they underwent a varus-producing osteotomy via an opening wedge distal femoral lateral osteotomy. 59 If patients showed a varus alignment (mechanical tibiofemoral angle <180°), they underwent a valgus producing osteotomy via an opening wedge HTO. 9 Concomitant lesions were addressed at the time of MAT surgery. Lesions of the native or previously reconstructed anterior cruciate ligament were addressed via reconstruction. Contralateral meniscal tear (medial meniscus in case of lateral MAT and lateral meniscus in case of medial MAT) was addressed via repair or partial meniscectomy according to the type of lesion. Chondral lesions were addressed according to the following criteria: debridement and lavage (<2 cm; partial thickness), marrow stimulation (<2 cm; full thickness), osteochondral allografts (>2 cm; subchondral bone involvement), and autologous chondrocyte implantation (>2 cm; minimal subchondral bone involvement).
Rehabilitation Protocol
Immediately after surgery while still in the operating room, the patients were placed in a long-leg hinged knee brace that was locked in extension for 2 weeks; weightbearing was allowed as tolerated in extension. From weeks 3 to 6, the brace was locked in extension for ambulation but was removed for passive range of motion (0°-90°) exercises. Brace use was dismissed after 6 weeks of use. From weeks 7 to 12, patients progressed to full range of motion in addition to muscle strengthening and general conditioning. After 12 weeks, patients progressed to jogging and sport-specific training. While patients were allowed to return to sports at 6 months, we recommended against performing strenuous contact sports. Patients were discouraged from participating in competitive-level sports in order to preserve the integrity of the meniscal allograft.
The data were summarized using routine descriptive statistics SPSS (Version 20; IBM SPSS Statistics). Two-factor analysis of variance (sex, MAT/MAT+) was used to test for differences in age and body mass index (BMI). A 2 × 2 chi-square test was used to determine if the spectrum of procedures performed on our study’s patient group was representative of the entire population. PRO results were analyzed using a multivariate analysis of variance with 3 grouping factors (sex, side [medial or lateral meniscus], and surgery [MAT or MAT+]) and 1 repeated factor (time; presurgery and latest follow-up). Significant P values and effect sizes (based on Cohen d and eta squared) are reported.
Results
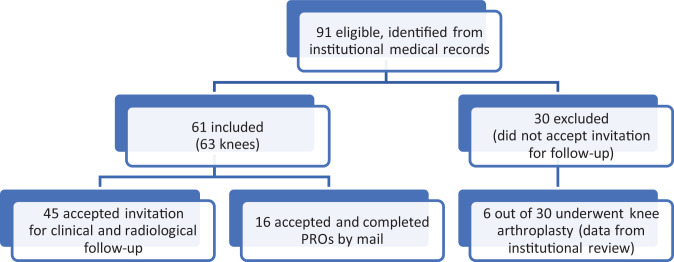
Of the 61 (63 knees) patients who met our inclusion criteria (all of whom had a history of prior intercollegiate athletics), 45 patients (47 knees) were seen in clinic, and 16 patients (16 knees) were unable to return to the clinic but did complete the necessary PRO measures. A total of 30 patients who had not completed at least 1 of the PRO instruments or had not completed both a pre- and postoperative PRO were excluded from the study (Figure 1). Basic characteristics of the patients are presented in Table 1. The mean age was 25.5 ± 9.2 years, which is younger than the mean age (mid-30s) in recent systematic reviews. 13,21,39,57 BMI ranged from 18.5 to 38.4 (male patients, 29.8; female patients, 24.3; P < .0001). BMI differences between levels of the 2 other grouping factors (surgery type, meniscal side) were not significant. Patients in our study were distributed across the 3 common BMI classification categories (Table 1). From the 61 patients who met our inclusion criteria, 43 had undergone an isolated MAT (female, 22), and 18 patients had undergone MAT+ for realignment (female, 9). The mean follow-up time was 4.8 ± 3.5 years (range, 1.0-13.6 years).
Figure 1.
Flow diagram of the patient selection process. PRO, patient-reported outcome.
TABLE 1.
Patient Characteristics by Sex and Surgery a
| MAT | MAT+ | ||||
|---|---|---|---|---|---|
| Variable | Female (n = 22) | Male (n = 21) | Female (n = 9) | Male (n = 9) | Overall (N = 61) |
| Age, y | 24.5 ± 9.5 | 28.2 ± 10.2 | 25.3 ± 7.2 | 21.8 ± 8.1 | 25.5 ± 9.2 |
| BMI bc | 24.3 ± 4.4 | 28.1 ± 3.8 | 24.4 ± 2.7 | 31.4 ± 4.3 | 26.7 ± 4.7 |
| Normal | 14 | 4 | 7 | 1 | 26 |
| Overweight | 7 | 9 | 2 | 2 | 20 |
| Obese | 1 | 9 | 1 | 6 | 17 |
| Follow-up, y | 5.1 ± 3.7 | 4.3 ± 3 | 6.3 ± 3.7 | 3.8 ± 3.6 | 4.8 ± 3.5 |
| Knee | |||||
| Right | 12 | 12 | 6 | 2 | 32 |
| Left | 10 | 10 | 4 | 7 | 31 |
| Meniscus | |||||
| Medial | 8 | 7 | 4 | 2 | 21 |
| Lateral | 14 | 14 | 6 | 7 | 41 |
| Both | 0 | 1 | 0 | 1 | 1 |
a Data are presented as mean ± SD or number. BMI, body mass index; MAT, meniscal allograft transplantation; MAT+, MAT plus any osteotomy.
b Normal = 18.5-24.9; overweight = 25.0-29.9; obese = 30.0-39.9.
c Male BMI > female BMI (P < .0001).
Concurrent procedures were a part of the surgical record, so we can present these data on both the 61 included patients and the 30 excluded patients. Table 2 summarizes the procedures performed concurrently with the index MAT. In the group of included patients, there were a total of 8 HTOs and 11 DFOs for a total of 19 MAT+ procedures in 18 patients, whereas the most common other concurrent procedure was a microfracture. When comparing frequencies between the included and excluded patients, we observed more chondroplasties and revision anterior cruciate ligament reconstructions (ACLRs) were performed on the excluded patients, with little difference among the other procedures.
Table 2.
Concurrent Procedures Performed During the Index MAT a
| Procedure | Included Patients (N = 61) | Excluded Patients (n = 30) | P |
|---|---|---|---|
| HTO | 8 (13) | 5 (17) | .65 |
| DFO | 11 (18) | 5 (17) | .87 |
| ACL reconstruction | 3 (5) | 0 (0) | - b |
| Revision ACL reconstruction | 0 (0) | 3 (10) | - b |
| Osteochondral allograft transplantation | 1 (2) | 2 (7) | .22 |
| Meniscal repair | 1 (2) | 0 (0) | - b |
| Microfracture | 7 (12) | 5 (17) | .49 |
| Chondroplasty | 3 (5) | 9 (30) | .001 |
| Autologous chondrocyte implantation | 0 (0) | 1 (1) | - b |
| Removal of implants | 0 (0) | 1 (1) | - b |
a Data are presented as n (%). Boldface P value indicates statistically significant difference between groups (P < .05). ACL, anterior cruciate ligament; DFO, distal femoral osteotomy; HTO, high tibial osteotomy; MAT, meniscal allograft transplantation.
b Unable to determine chi-square.
As complications and treatments were a part of the surgical record, we can present these data on both the 61 included patients and the full set of 91 patients who underwent surgery. The most common complication (Table 3) was a tear of the graft (11 tears in 43 patients with MAT, 1 tear in 18 patients with MAT+), and the most frequent treatment was debridement (in 8 patients with MAT and 1 patient with MAT+). Subsequent surgery was performed on 21 knees (21/93 knees; 23%). Of these 21 knees, 14 knees underwent 1 subsequent surgery, 4 required 2 subsequent surgeries, 1 required 3 surgeries, and 2 required 4 subsequent surgeries. Each subsequent surgery included 1 or more procedures for a total of 34 subsequent procedures. Debridement of the graft was the most common reason for subsequent surgery. None of the 61 included patients (63 knees) needed complete removal of the graft or went on to partial or total knee arthroplasty.
TABLE 3.
Complications and Related Treatments After MAT by Surgery Type a
| Complication | Study Population (N = 61) |
All Patients (n = 90) |
Related Treatment | Study Population (N = 61) |
All Patients (n = 90) |
||
|---|---|---|---|---|---|---|---|
| MAT | MAT+ | MAT | MAT+ | ||||
| MAT failure | 1 | 1 | 3 | Revision MAT | 2 | 1 | 3 |
| MAT tear | 11 | 1 | 14 | Repair | 3 | 1 | 4 |
| Debridement | 8 | 1 | 10 | ||||
| Chondral damage | 4 | Chondroplasty | 2 | 3 | |||
| Microfracture | 1 | 1 | |||||
| Painful sutures | 1 | 2 | Removal of sutures | 1 | 1 | 2 | |
| Stiffness | 1 | 1 | 3 | MUA | 1 | 1 | |
| Debridement | 1 | 1 | 2 | ||||
| Painful implants | 1 | 3 | 5 | Removal of implants | 2 | 2 | 5 |
| Peroneal nerve palsy | 1 | 1 | Neurolysis | 1 | 1 | ||
| ACL tear | 1 | 1 | ACL reconstruction | 1 | 1 | ||
| Continued pain | 2 | 1 | 9 | HTO | 2 | 1 | 3 |
| TKA | 5 b | ||||||
| UKA | 1 b | ||||||
| Superficial wound infection | 1 | 1 | Oral antibiotics | 1 | 1 | ||
| Deep wound infection | 1 | Removal of MAT | 1 | ||||
a ACL, anterior cruciate ligament; HTO, high tibial osteotomy; MAT, meniscal allograft transplantation; MAT+, MAT plus any osteotomy; MUA, manipulation under anesthesia; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty. Blank cells indicate none.
b Six excluded patients underwent arthroplasty at our institution. Actual total for all excluded patients is unknown.
We were able to obtain the necessary imaging for KL osteoarthritis (OA) grades on the 45 patients who came in for the follow-up visit (Table 4). A total of 44 (94%) of our patients had either grade 0 or 1 OA at the time of the index surgery. At the mean follow-up (4.8 years), there was evidence of radiographic progression of OA in 20 of the 47 knees (45 patients; 43%); 2 knees had progressed to grade 4 OA.
TABLE 4.
KL Progression by Sex, Meniscus, and Surgery Type a
| KL Grade Change | Sex | Meniscus | Surgery | ||||
|---|---|---|---|---|---|---|---|
| Female | Male | Medial b | Lateral | MAT | MAT+ | All | |
| 0 | 13 | 14 | 8 | 19 | 22 | 5 | 27 |
| +1 | 9 | 8 | 7 | 10 | 10 | 7 | 17 |
| +2 | 1 | 1 | 1 | 1 | |||
| +4 | 2 | 1 | 1 | 1 | 1 | 2 | |
a KL, Kellgren-Lawrence; Last, last follow-up; MAT, meniscal allograft transplantation; MAT+, MAT plus osteotomy; Pre, preoperative; SF-36, short form 36.
b There were no patients whose KL grade changed by 3 units (ie, 0 to 3, or 1 to 4).
PROs for the 61 included patients, collected preoperatively and at each patient’s latest follow-up appointment, are presented in Table 5. There were no preoperative differences in PRO scores between those awaiting MAT or MAT+. There were only 3 instances where the main effects were significant: KOOS Symptoms (female > male) and KOOS Activities of Daily Living (ADL) (female > male; lateral > medial). As expected, the main effect of time showed significant improvement on all PRO scales (P ≤ .003) and the PRO effect sizes (Cohen's d) were ‘large’ (ES > 0.8; VAS, KOOS Pain, KOOS Sport, KOOS ADL, WOMAC Function) or ‘medium' (ES = 0.5-0.8; KOOS Symptoms, KOOS QOL; WOMAC Pain, WOMAC Stiffness; SF-36 Physical, SF-36 Function).
TABLE 5.
Means of PRO Subscales by Sex, Surgery Type, Meniscus Transplanted, and Time a
| MAT | MAT+ | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lateral | Medial | Lateral | Medial | ||||||
| Sex | Pre | Last | Pre | Last | Pre | Last | Pre | Last | |
| VAS pain | F | 5.1 | 1.5 | 3.6 | 2.2 | 4.7 | 2.0 | 4.8 | 3.8 |
| M | 4.3 | 1.5 | 2.9 | 1.1 | 4.1 | 2.0 | 4.5 | 4.0 | |
| KOOS | |||||||||
| Pain | F | 54.1 | 72.2 | 61.9 | 81.2 | 61.5 | 82.5 | 69.6 | 85.4 |
| M | 56.6 | 80.6 | 60.2 | 76.2 | 62.2 | 89.0 | 36.0 | 52.7 | |
| Symptoms | F | 49.3 | 67.6 | 53.3 | 66.9 | 60.9 | 67.2 | 65.2 | 72.3 |
| M | 55.1 | 70.2 | 58.7 | 69.2 | 38.9 | 71.8 | 30.6 | 57.1 | |
| ADL | F | 63.0 | 88.0 | 64.6 | 90.0 | 69.6 | 96.1 | 80.7 | 89.3 |
| M | 71.2 | 86.4 | 74.3 | 85.5 | 65.3 | 93.0 | 47.8 | 54.4 | |
| Sport/Rec | F | 36.1 | 57.1 | 27.5 | 62.5 | 41.7 | 56.7 | 40.0 | 68.8 |
| M | 36.6 | 66.1 | 27.9 | 58.6 | 26.2 | 72.1 | 15.0 | 39.6 | |
| QoL | F | 38.2 | 56.9 | 38.1 | 57.8 | 40.8 | 53.5 | 41.2 | 60.3 |
| M | 41.0 | 63.8 | 35.0 | 56.3 | 35.2 | 57.7 | 41.6 | 39.6 | |
| WOMAC | |||||||||
| Pain | F | 58.6 | 79.6 | 76.2 | 86.9 | 64.2 | 95.8 | 61.2 | 87.5 |
| M | 68.1 | 85.4 | 75.7 | 80.7 | 63.6 | 90.0 | 55.0 | 60.0 | |
| Stiffness | F | 54.5 | 75.9 | 78.1 | 76.6 | 56.2 | 93.3 | 51.2 | 81.2 |
| M | 63.8 | 73.2 | 65.1 | 67.9 | 53.6 | 83.9 | 37.5 | 75.0 | |
| Function | F | 59.2 | 88.3 | 75.1 | 89.7 | 64.7 | 97.5 | 57.3 | 88.2 |
| M | 74.3 | 87.5 | 75.5 | 84.6 | 65.0 | 93.9 | 52.9 b | 71.3 | |
| SF-36 | |||||||||
| Physical | F | 33.3 | 46.1 | 32.6 | 45.8 | 45 | 44.8 | 38.7 | 39.2 |
| M | 38.4 | 50.3 | 41.5 | 46.4 | 31.1 | 49.2 | 39.9 | 48.4 | |
| Mental | F | 47.0 | 57.2 | 45.7 | 57.2 | 41.3 | 54.8 | 41.2 | 55.8 |
| M | 50.0 | 56.6 | 39.4 | 55.4 | 55.1 | 58.2 | 55.6 | 50.0 | |
| Satisfaction | F | 8.6 | 8.2 | 8.2 | 7.8 | ||||
| M | 7.8 | 8.6 | 8.8 | 7.0 | |||||
a ADL, Activities of Daily Living; F, female; KOOS, Knee injury and Osteoarthritis Outcome Score; M, male; MAT, meniscal allograft transplantation; MAT+, MAT plus osteotomy; PRO, patient-reported outcome; QoL, Quality of Life; Sport/Rec, Sport and Recreation; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
b Shaded cells indicate the location of sex × surgery type × transplant location × time interactions.
Given the potential for a multitude of interactions, statistical interactions were limited. For example, there was a significant time × surgery type interaction for the WOMAC Stiffness scale that indicated patients who underwent the MAT+ procedure showed greater improvement than did patients who underwent MAT. We expected improvement over time, but the greater improvement for the patients who underwent MAT+ may be because they started off with worse stiffness. One other within-patient interaction was apparent, and it too was due primarily to a time effect (SF-36 Physical; time × sex × surgery). There was a significant side by surgery interaction for WOMAC Pain scale (medial MAT > medial MAT+) and for the WOMAC Function scale (medial MAT > medial MAT+; lateral MAT+ > medial MAT+). Two scales did show the highest level of between-patient interactions: KOOS Pain and KOOS ADL. Male patients with a medial meniscal transplant who underwent the MAT+ procedure had significantly greater pain and poorer KOOS ADL scores than patients in other surgical groupings. Despite the noted instances of some poorer PRO scores (in male patients who underwent MAT+ with a medial meniscal transplant), the satisfaction scores of ≥7 (out of 10) were recorded in 85% of patients indicating that patients seemed to be satisfied with the outcomes of their surgery.
Discussion
The most significant result from this study is that all PROs improved from initial to final follow-up (P ≤ .003), with a graft survivorship of 100% (63/63 knees) at a mean follow-up of 4.8 years (range, 1.0-13.6 years). However, about one-quarter of the patients needed subsequent surgery (22.6%; 21 of 93 knees).
MAT is an attempt to overcome the well-known consequences of meniscectomy or failed meniscal repairs. For the procedure to be considered successful, graft survival is an essential component that contributes to prevention of future OA. Survival rates are, in part, a function of time after surgery. In the initial 5 to 7 years, graft survival hovers around 80% to 90% 10,17,31,45 then begins to decline, reaching about 50% by 20 years 51 and 15% by 24 years. 51 Most of the initial decline seems to be due in part to the graft detaching from the capsule or the graft failing to revascularize secondary to malalignment. 26 The graft survival rate for the 61 patients who met the inclusion criteria was, at an average of 4.8 years of follow-up, 100%---an unusual rate that is higher than that in other reports based on patients of a similar age and length of follow-up. 10,17,45
Other factors that contribute to long-term graft survival include age and knee alignment. Grafts in older patients tend to have poorer survival than grafts in younger patients. For example, at a mean of 6.8 years postoperatively, graft survival in patients aged <35 years (at time of index surgery) was 24% versus 8% in patients who were aged >35 years. 51 If, at the time of the index surgery, a patient has varus or valgus malalignment, it is not unusual for an osteotomy to also be performed in an attempt to increase graft survival. At 10 years after surgery, MAT survival was 70% to 75% in patients not needing an HTO, but inclusion of an HTO raised 10-year survival to 83%. 52 Of our 61 patients, 31% (n = 19) underwent a concomitant HTO or DFO. The literature has reported a wide range of MAT procedures with concurrent osteotomies, ranging from 6% to 62%. 22,56 Most reports have been based on case series that reflect the author’s patient mix and are not a true statement about the population.
In our series, no differences in the associated procedures were found between patients who underwent MAT versus those who underwent MAT+ (Table 2). Malalignment is generally considered a contraindication for MAT, 44 but when the knee is realigned via a previous or a concomitant osteotomy at the time of the MAT, outcomes are comparable with those of patients undergoing MAT without malalignment. Kazi et al 22 reported the outcomes of 86 patients who underwent MAT with or without an osteotomy. At a mean follow-up of 180 months, they found no significant difference in survival for isolated MAT compared with MAT+; overall survival was 71% at a mean of 15 years postoperatively. Van Arkel and de Boer 50 reported on 23 patients who underwent cryopreserved MAT and showed that patients with uncorrected varus or valgus malalignment had poorer Lysholm scores and higher failure rates compared with patients with neutral alignment. The general trend is to correct malalignment either as a concomitant procedure or staged with the osteotomy as a first stage and followed by MAT as a second stage. 4,9,10,16 In contrast to the current trend in the literature, however, Van Der Straeten et al, 51 in their work on 329 MATs, noted that concomitant HTO had a negative effect on long-term graft survival (0% at 24 years).
Most studies have defined failure of MAT to be conversion to a total knee replacement, which has been reported to be as high as 18%. 51,53 Complications were quite varied as can be seen in Table 3. The complication rate in our patients was 22.6% (21 of 93 knees), with allograft tearing requiring debridement being the most common complication. Looking at the available literature, the rate of complication needing subsequent surgeries after the index procedure ranges from 13% to one-third, 35,48 the latter of which is slightly higher than what we found in this retrospective case series. However, with 30 patients being unavailable for follow-up, we were unable to account for those patients who could have undergone subsequent surgeries elsewhere. Regardless, given that our patients were athletes who had returned to their sports, it might be surprising to not have had more concerns given the demands of competitive sports.
The item most likely to be of interest is our success rate. There were no failures among the 61 patients who met the inclusion criteria (we defined failure as revision procedure related to the initial MAT or as conversion to knee arthroplasty). A success rate of 100% is an unusual result. In studies like this, information about patients who did not meet the inclusion criteria is sometimes as important as information about included patients. For example, institutional records showed that 6 excluded patients subsequently underwent arthroplasty. Had they met the inclusion criteria, the success rate would have been 91% (61/67). Further, rates of concurrent procedures of the 30 who did not meet the inclusion criteria were similar to those of the study population except for ACLR (10% vs 0%), osteochondral allograft transplantation (7% vs 2%), and chondroplasty (30% vs 4%). One might expect that patients with more complex issues would have poorer outcomes. If we were to assume that all 30 patients met our inclusion criteria, there would be 14 patients with complex initial procedures (assuming no patient underwent multiple concurrent procedures). If we were to further expect that those 14 patients eventually underwent an arthroplasty (the 14 includes those 6 we already knew had an arthroplasty), our success rate would have been 77/91 or 85%, which is more consistent with data on patients of similar age and follow-up time. 48 This is, however, based on speculation and assumptions.
Preoperatively, there were no statistical or clinically meaningful differences in PROs between our patients who were destined for MAT or for MAT+. The overall improvement from preoperative scores to the latest follow-up across all the subscales was 36.4%. Across the 3 instruments and their subscales, improvement ranged from 19% (SF-36 Mental) to 92% (KOOS Sport and Recreation). For the various patient groups, improvements over time were similar for sex (female, 35%; male, 39%), transplant side (medial, 33%; lateral, 40%), and surgery type (MAT, 34%; MAT+, 40%).
Although it is considered a salvage procedure, MAT with or without osteotomy may be the only option to relieve symptoms and allow patients to return to an active life. VAS for pain was reduced by similarly to previous data 8 whether the patient had a MAT alone on in combination. 8 The results presented in Table 5 show mean values for the KOOS, WOMAC, and SF-36 PRO tools. The mean percentage improvements for all 5 subscales of the KOOS in our patients are similar to those reported elsewhere. 8,11,29,54,55 The literature has reported that relative improvements in KOOS subscales for Pain, Symptoms, and ADL generally range from 20% to 68%. 29,54 Improvements in Sport and Recreation and for Quality of Life (QoL) tend to be greater, such as 144% for Sport and Recreation 54 and 132% for QoL. 8 In addition, in the few instances where the meniscal side location was a factor, our results are consistent with those in a current meta-analysis that indicated that patients who received a medial meniscal transplant did not fare as well as did patients who received a lateral meniscal transplant. 7
When viewed over time, the greatest improvement in PRO data came within the first year and was maintained for up to 7 years consistent with the pattern reported by Bloch et al. 8 The minimum clinically important difference in KOOS scores has been reported to range from about 10% (Pain, Symptoms, ADL) to 15% (Sport and Recreation, QoL), 32 indicating that our patients demonstrated not only statistical improvement but also clinically relevant improvement. Despite the impressive improvement in Sport and Recreation and for QoL, however, the actual mean scores at follow-up (60 and 56, respectively; Table 5) are, at best, just over half of those obtained from patients with healthy knees (95-100 and 100 for healthy patients aged 18-25 years and 26-35 years, respectively). 60 What might be interesting is that male patients who underwent MAT+ for the medial meniscus were the only subgroup that showed no improvement in the KOOS QoL score. While the number of patients (n = 2) is too small for the result to be meaningful, this finding might be worth exploring in the future.
Our patients recorded a 50% reduction in pain via VAS, which is similar to what others have noted. 33,54,55 The WOMAC has not been collected widely from patients undergoing MAT, but the subscales for our patients improved by 28% to 34% (Table 5), which is greater than the 19.6% improvement reported by Marcacci et al. 33 Male patients who underwent MAT+ started out with worse scores in WOMAC Stiffness and KOOS Symptoms; however, they demonstrated a significantly greater improvement than male patients who underwent MAT. These data underline the importance of knee realignment associated with biologic procedures and its synergistic relationship with MAT.
MAT is considered a salvage procedure to delay or prevent cartilage deterioration. In 2006, Verdonk et al 53 reported long-term (minimum 10-year follow-up) clinical and radiological outcomes of a group of 41 patients who underwent MAT with or without HTO. Joint space narrowing and Fairbank changes were assessed on radiographs available from 32 patients. In 41% (13/32) of patients, those parameters remained stable, and, by final follow-up, 18% (7/39) of patients underwent total knee arthroplasty. Lee et al 25 showed that radiographic progression of OA of the lateral compartment of the knee was slowed after MAT. The authors noted that the KL grade worsened from the time of initial meniscectomy to the meniscal transplantation, but there was no further degeneration after MAT at follow-up (mean, 3.8 years). Ha et al 18 showed that KL grade changed at 1 and 4 years post-MAT. The long-term follow-up study by Van Der Straeten and colleagues 51 indicated that OA progresses by 1 KL grade every 1000 days after the index MAT surgery. The current literature has yet to identify risk factors of OA progression other than MAT in the medial compartment. 2 In the 47 knees evaluated in the clinic using radiographs, 94% were KL grades 0 or 1, and we found radiographic progression of OA in 43% of the 47 knees, which is in line with other published data. BMI, sex, and MAT location were not associated with radiographic OA progression.
This study was not without its limitations. Primarily, our data were limited to the 61 patients who accepted our invitation. The reasons why the other 30 chose not to participate are unknown, but we did learn that 6 of the 30 had undergone knee arthroplasty. With one-third of our original patient pool being unavailable for follow-up, the power and generalizability of the study were reduced. In addition, as this is a retrospective study, data from intermediate follow-ups between the preoperative assessment and the last evaluation were lacking, so we were unable to fully assess the ongoing benefits of MAT over time. Our results were also specific only to patients who underwent MAT that used bone plugs (for the medial meniscus) or a bone bridge (for the lateral meniscus). Radiographs were used to evaluate progression of OA although magnetic resonance imaging could have been more accurate in estimating cartilage and meniscal allograft degeneration. As with most case series projects, some data points were missing from several patients (eg, missing pre- or postoperative PRO scores, missing satisfaction scores, missing pre- or postoperative radiographs), and those might have affected our statistical results. We did not measure graft extrusion since it has been demonstrated that extrusion does not correlate well with clinical outcome. 46
Conclusion
Based on this case series, MAT (with or without a concomitant osteotomy) is a reliable procedure that provides good clinical outcomes at midterm follow-up for younger patients with knee pain and disability. MAT in previously active younger patients resulted in acceptable clinical and radiographic improvements with both statistical and clinically relevant improvements in PRO. However, we did see some suggestion that male patients receiving a medial meniscal transplant when undergoing a MAT+ procedure may need close oversight, as they seemed to have issues with pain and functional activities. Graft survivorship at 5 years postoperatively was excellent. For this population, MAT provided good pain relief and improved knee function with a complication rate less than that reported in older patients.
Acknowledgment
The authors greatly appreciate the professional editorial and publication assistance provided by Donald T. Kirkendall, ELS.
Footnotes
Final revision submitted October 24, 2021; accepted November 8, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Y.E.B. has received education payments from Wardlow Enterprises. A.A. has received consulting fees from Arthrex, Bioventus, and Limacorporate SpA; nonconsulting fees from Arthrex; and royalties from Arthrex and has an investment interest in Anika Therapeutics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Iowa (ID No. 201306709).
References
- 1. Abat F, Gelber PE, Erquicia JI, et al. Prospective comparative study between two different fixation techniques in meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1516–1522. doi:10.1007/s00167-012-2032-4 [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Kang HW, Yang TY, Lee JY. Risk factors for radiographic progression of osteoarthritis after meniscus allograft transplantation. Arthroscopy. 2016;32(12):2539–2546. doi:10.1016/j.arthro.2016.04.023 [DOI] [PubMed] [Google Scholar]
- 3. Alhalki MM, Hull ML, Howell SM. Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft: a human cadaveric study. Am J Sports Med. 2000;28(3):370–376. doi:10.1177/03635465000280031501 [DOI] [PubMed] [Google Scholar]
- 4. Amendola A. Knee osteotomy and meniscal transplantation: indications, technical considerations, and results. Sports Med Arthrosc Rev. 2007;15(1):32–38. doi:10.1097/JSA.0b013e31802f997b [DOI] [PubMed] [Google Scholar]
- 5. Baker BE, Peckham AC, Pupparo F, Sanborn JC. Review of meniscal injury and associated sports. Am J Sports Med. 1985;13(1):1–4. doi:10.1177/036354658501300101 [DOI] [PubMed] [Google Scholar]
- 6. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14(4):270–275. doi:10.1177/036354658601400405 [DOI] [PubMed] [Google Scholar]
- 7. Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med. 2018;46(5):1243–1250. doi:10.1177/0363546517709777 [DOI] [PubMed] [Google Scholar]
- 8. Bloch B, Asplin L, Smith N, Thompson P, Spalding T. Higher survivorship following meniscal allograft transplantation in less worn knees justifies earlier referral for symptomatic patients: experience from 240 patients. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1891–1899. doi:10.1007/s00167-019-05459-6. doi:10.1007/s00167-019-05459-6 [DOI] [PubMed] [Google Scholar]
- 9. Bonasia DE, Amendola A. Combined medial meniscal transplantation and high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):870–873. doi:10.1007/s00167-009-0999-2 [DOI] [PubMed] [Google Scholar]
- 10. Cameron JC, Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res. 1997;337:164–171. doi:10.1097/00003086-199704000-00018 [DOI] [PubMed] [Google Scholar]
- 11. De Bruycker M, Verdonk PCM, Verdonk RC. Meniscal allograft transplantation: a meta-analysis. SICOT J. 2017;3:33. doi:10.1051/sicotj/2017016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DeHaven KE, Lohrer WA, Lovelock JE. Long-term results of open meniscal repair. Am J Sports Med. 1995;23(5):524–530. doi:10.1177/036354659502300502 [DOI] [PubMed] [Google Scholar]
- 13. Fanelli D, Mercurio M, Gasparini G, Galasso O. Predictors of meniscal allograft transplantation outcome: a systematic review. J Knee Surg. 2021;34(3):303–321. doi:10.1055/s-0039-1695043 [DOI] [PubMed] [Google Scholar]
- 14. Garrett JC, Steensen RN. Meniscal transplantation in the human knee: a preliminary report. Arthroscopy. 1991;7(1):57–62. doi:10.1016/0749-8063(91)90079-d [DOI] [PubMed] [Google Scholar]
- 15. Garrett WE, Swiontkowski MF, Weinstein JN, et al. American Board of Orthopaedic Surgery practice of the orthopaedic surgeon, part-II: certification examination case mix. J Bone Joint Surg Am. 2006;88:660–667. [DOI] [PubMed] [Google Scholar]
- 16. Gomoll AH, Kang RW, Chen AL, Cole BJ. Triad of cartilage restoration for unicompartmental arthritis treatment in young patients: meniscus allograft transplantation, cartilage repair and osteotomy. J Knee Surg. 2009;22(2):137–141. doi:10.1055/s-0030-1247738 [DOI] [PubMed] [Google Scholar]
- 17. Gonzalez-Lucena G, Gelber PE, Pelfort X, Tey M, Monllau JC. Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy. 2010;26(12):1633–1640. doi:10.1016/j.arthro.2010.05.005 [DOI] [PubMed] [Google Scholar]
- 18. Ha JK, Jang HW, Jung JE, Cho SI, Kim JG. Clinical and radiologic outcomes after meniscus allograft transplantation at 1-year and 4-year follow-up. Arthroscopy. 2014;30(11):1424–1429. doi:10.1016/j.arthro.2014.05.032 [DOI] [PubMed] [Google Scholar]
- 19. Henning CE, Lynch MA. Current concepts of meniscal function and pathology. Clin Sports Med. 1985;4(2):259–265. [PubMed] [Google Scholar]
- 20. Huang A, Hull ML, Howell SM. The level of compressive load affects conclusions from statistical analyses to determine whether a lateral meniscal autograft restores tibial contact pressure to normal: a study in human cadaveric knees. J Orthop Res. 2003;21(3):459–464. doi:10.1016/S0736-0266(02)00201-2 [DOI] [PubMed] [Google Scholar]
- 21. Hurley ET, Davey MS, Jamal MS, et al. High rate of return-to-play following meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3561–3568. doi:10.1007/s00167-020-05956-z [DOI] [PubMed] [Google Scholar]
- 22. Kazi HA, Abdel-Rahman W, Brady PA, Cameron JC. Meniscal allograft with or without osteotomy: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):303–309. doi:10.1007/s00167-014-3291-z [DOI] [PubMed] [Google Scholar]
- 23. Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494. doi:10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kim JM, Bin SI. Meniscal allograft transplantation after total meniscectomy of torn discoid lateral meniscus. Arthroscopy. 2006;22(12):1344–1350.e1341. doi:10.1016/j.arthro.2006.07.048 [DOI] [PubMed] [Google Scholar]
- 25. Lee BS, Bin SI, Kim JM. Articular cartilage degenerates after subtotal/total lateral meniscectomy but radiographic arthrosis progression is reduced after meniscal transplantation. Am J Sports Med. 2016;44(1):159–165. doi:10.1177/0363546515612076 [DOI] [PubMed] [Google Scholar]
- 26. Lee BS, Kim JM, Sohn DW, Bin SI. Review of meniscal allograft transplantation focusing on long-term results and evaluation methods. Knee Surg Relat Res. 2013;25(1):1–6. doi:10.5792/ksrr.2013.25.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Levy IM, Torzilli PA, Gould JD, Warren RF. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71(3):401–406. [PubMed] [Google Scholar]
- 28. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 29. Liu JN, Gowd AK, Redondo ML, et al. Establishing clinically significant outcomes after meniscal allograft transplantation. Orthop J Sports Med. 2019;7(1):2325967118818462. doi:10.1177/2325967118818462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lutz C, Dalmay F, Ehkirch FP, et al. Meniscectomy versus meniscal repair: 10 years radiological and clinical results in vertical lesions in stable knee. Orthop Traumatol Surg Res. 2015;101(8 suppl):S327–S331. doi:10.1016/j.otsr.2015.09.008 [DOI] [PubMed] [Google Scholar]
- 31. Mahmoud A, Young J, Bullock-Saxton J, Myers P. Meniscal allograft transplantation: the effect of cartilage status on survivorship and clinical outcome. Arthroscopy. 2018;34(6):1871–1876.e1871. doi:10.1016/j.arthro.2018.01.010 [DOI] [PubMed] [Google Scholar]
- 32. Maltenfort M, Diaz-Ledezma C. Statistics in brief: minimum clinically important difference-availability of reliable estimates. Clin Orthop Relat Res. 2017;475(4):933–946. doi:10.1007/s11999-016-5204-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Marcacci M, Marcheggiani Muccioli GM, Grassi A, et al. Arthroscopic meniscus allograft transplantation in male professional soccer players: a 36-month follow-up study. Am J Sports Med. 2014;42(2):382–388. doi:10.1177/0363546513508763 [DOI] [PubMed] [Google Scholar]
- 34. Matava MJ. Meniscal allograft transplantation: a systematic review. Clin Orthop Relat Res. 2007;455:142–157. doi:10.1097/BLO.0b013e318030c24e [DOI] [PubMed] [Google Scholar]
- 35. McCormick F, Harris JD, Abrams GD, et al. Survival and reoperation rates after meniscal allograft transplantation: analysis of failures for 172 consecutive transplants at a minimum 2-year follow-up. Am J Sports Med. 2014;42(4):892–897. doi:10.1177/0363546513520115 [DOI] [PubMed] [Google Scholar]
- 36. McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88(12):1549–1556. doi:10.1302/0301-620X.88B12.18140 [DOI] [PubMed] [Google Scholar]
- 37. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94(24):2222–2227. doi:10.2106/JBJS.K.01584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Northmore-Ball MD, Dandy DJ, Jackson RW. Arthroscopic, open partial, and total meniscectomy: a comparative study. J Bone Joint Surg Br. 1983;65(4):400–404. doi:10.1302/0301-620X.65B4.6874710 [DOI] [PubMed] [Google Scholar]
- 39. Novaretti JV, Patel NK, Lian J, et al. Long-term survival analysis and outcomes of meniscal allograft transplantation with minimum 10-year follow-up: a systematic review. Arthroscopy. 2019;35(2):659–667. doi:10.1016/j.arthro.2018.08.031 [DOI] [PubMed] [Google Scholar]
- 40. Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27(9):1275–1288. doi:10.1016/j.arthro.2011.03.088 [DOI] [PubMed] [Google Scholar]
- 41. Pollard ME, Kang Q, Berg EE. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11(6):684–687. doi:10.1016/0749-8063(95)90110-8 [DOI] [PubMed] [Google Scholar]
- 42. Ronnblad E, Barenius B, Engström B, Eriksson K. Predictive factors for failure of meniscal repair: a retrospective dual-center analysis of 918 consecutive cases. Orthop J Sports Med. 2020;8(3):2325967120905529. doi:10.1177/2325967120905529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Roos H, Lauren M, Adalberth T, et al. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4):687–693. doi:10.1002/1529-0131(199804)41:4<687:: AID-ART16>3.0.CO;2-2 [DOI] [PubMed] [Google Scholar]
- 44. Rosso F, Bisicchia S, Bonasia DE, Amendola A. Meniscal allograft transplantation: a systematic review. Am J Sports Med. 2015;43(4):998–1007. doi:10.1177/0363546514536021 [DOI] [PubMed] [Google Scholar]
- 45. Saltzman BM, Bajaj S, Salata M, et al. Prospective long-term evaluation of meniscal allograft transplantation procedure: a minimum of 7-year follow-up. J Knee Surg. 2012;25(2):165–175. doi:10.1055/s-0032-1313738 [DOI] [PubMed] [Google Scholar]
- 46. Samitier G, Alentorn-Geli E, Taylor DC, et al. Meniscal allograft transplantation, part 2: systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):323–333. doi:10.1007/s00167-014-3344-3 [DOI] [PubMed] [Google Scholar]
- 47. Sekiya JK, Giffin JR, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(6):896–906. doi:10.1177/03635465030310062701 [DOI] [PubMed] [Google Scholar]
- 48. Smith NA, MacKay N, Costa M, Spalding T. Meniscal allograft transplantation in a symptomatic meniscal deficient knee: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):270–279. doi:10.1007/s00167-014-3310-0 [DOI] [PubMed] [Google Scholar]
- 49. Smith NA, Parsons N, Wright D, et al. A pilot randomized trial of meniscal allograft transplantation versus personalized physiotherapy for patients with a symptomatic meniscal deficient knee compartment. Bone Joint J. 2018;100-B(1):56–63. doi:10.1302/0301-620x.100b1.Bjj-2017-0918.R1 [DOI] [PubMed] [Google Scholar]
- 50. van Arkel ER, de Boer HH. Human meniscal transplantation: preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br. 1995;77(4):589–595. [PubMed] [Google Scholar]
- 51. Van Der Straeten C, Byttebier P, Eeckhoudt A, Victor J. Meniscal allograft transplantation does not prevent or delay progression of knee osteoarthritis. PLoS One. 2016;11(5):e01561 83. doi:10.1371/journal.pone.0156183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Verdonk PC, Demurie A, Almqvist KF, et al. Transplantation of viable meniscal allograft: survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87(4):715–724. doi:10.2106/jbjs.C.01344 [DOI] [PubMed] [Google Scholar]
- 53. Verdonk PC, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):694–706. doi:10.1007/s00167-005-0033-2 [DOI] [PubMed] [Google Scholar]
- 54. Vundelinckx B, Bellemans J, Vanlauwe J. Arthroscopically assisted meniscal allograft transplantation in the knee: a medium-term subjective, clinical, and radiographical outcome evaluation. Am J Sports Med. 2010;38(11):2240–2247. doi:10.1177/0363546510375399 [DOI] [PubMed] [Google Scholar]
- 55. Vundelinckx B, Vanlauwe J, Bellemans J. Long-term subjective, clinical, and radiographic outcome evaluation of meniscal allograft transplantation in the knee. Am J Sports Med. 2014;42(7):1592–1599. doi:10.1177/0363546514530092 [DOI] [PubMed] [Google Scholar]
- 56. Waterman BR, Rensing N, Cameron KL, Owens BD, Pallis M. Survivorship of meniscal allograft transplantation in an athletic patient population. Am J Sports Med. 2016;44(5):1237–1242. doi:10.1177/0363546515626184 [DOI] [PubMed] [Google Scholar]
- 57. Waugh N, Mistry H, Metcalfe A, et al. Meniscal allograft transplantation after meniscectomy: clinical effectiveness and cost-effectiveness. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1825–1839. doi:10.1007/s00167-019-05504-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wilcox TR, Goble EM. Indications for meniscal allograft reconstruction. Am J Knee Surg. 1996;9(1):35–36. [PubMed] [Google Scholar]
- 59. Willey M, Wolf BR, Kocaglu B, Amendola A. Complications associated with realignment osteotomy of the knee performed simultaneously with additional reconstructive procedures. Iowa Orthop J. 2010;30:55–60. [PMC free article] [PubMed] [Google Scholar]
- 60. Williamson T, Sikka R, Tompkins M, Nelson BJ. Use of the knee injury and osteoarthritis outcome score in a healthy United States population. Am J Sports Med. 2016;44(2):440–446. doi:10.1177/0363546515616812 [DOI] [PubMed] [Google Scholar]
- 61. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Is sport activity possible after arthroscopic meniscal allograft transplantation? Midterm results in active patients. Am J Sports Med. 2016;44(3):625–632. doi:10.1177/0363546515621763 [DOI] [PubMed] [Google Scholar]