Abstract
Background:
Health care workers (HCWs) are exposed to high risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection due to close contact with infected patients in hospital. The objective of this study was to estimate the seroprevalence and to identify the exposure risk of various subgroups among HCWs to prioritize them for early vaccination.
Methods:
This was a multicentre cross-sectional study conducted between 15 and 29 June 2020. A total of 987 HCWs were recruited randomly from two major tertiary-care hospitals of Peshawar city, Pakistan. The HCWs included doctors, nurses, paramedics and hospital support staff. The US Food and Drug Administration (FDA)–approved kit was used for the detection of SARS-CoV-2 antibodies.
Results:
Overall, 310 (31.4%) HCWs were seropositive for SARS-CoV-2 antibodies (95% confidence interval, CI: 28.5–34.4). Seroprevalence was higher in males (33.5%) and in age group 51–60 years (40.9%). Seropositivity increased with increasing age from 8.3% in age group ⩽20 to 40.9% in 51–60 years of age group (p < 0.05). The highest seroprevalence was identified in paramedical staff (42·5%, 95% CI: 36.6–48.6) followed by nursing staff (38·8%, 95% CI: 32.1–45.7). In logistic regression, being a male HCW led to higher risk of seropositivity (odds ratio, OR: 1.50, 95% CI: 1·06–2.13. p < 0.05) compared with female staff members. The odds of seropositivity was higher in nurses (OR: 3·47, 95% CI: 1.99–6.05. p < 0.01), paramedical staff (OR: 3·19, 95% CI: 1.93–5.28. p < 0.01) and hospital support staff (OR: 2·47, 95% CI: 1.29–4.7. p < 0.01) compared with consultants.
Conclusion:
Overall, our results concluded that nursing and paramedical staff are at higher risk and should be vaccinated on priority.
Keywords: COVID-19, health care workers, priority, subgroups, vaccination
Introduction
Frontline health care workers (HCWs) are exposed to and at higher risk of acquiring infection in hospitals while dealing with patients suffering from highly infectious diseases. 1 During coronavirus disease 2019 (COVID-19) pandemic, HCWs have been facing a significant higher risk of contracting infection and death due to excessive COVID-19 exposure. 2 HCWs accounted for 11% of all COVID-19 cases reported in the United States according to the Centers for Disease Control and Prevention (CDC). 3 As of December 2020, there have been 154 deaths among HCWs in Pakistan, including 128 doctors and 26 paramedical staff/nurses. 4
Reverse transcription polymerase chain reaction (RT-PCR) screening may be negative even in acute phase in certain cases. 5 Antibodies tests [anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies] may be useful in diagnosing PCR negative cases and also provide information about past infection.5,6
HCWs have been globally identified as priority group for vaccination because of the occupational exposure risk of severity of disease transferred to patients and critical situation of the health sector.7 –9 The CDC 10 recommended that HCWs should be the first to receive vaccination against COVID-19 since their well-being and availability play a critical role in caring and treating others; hence, their protection remains a national priority.
Since the benefits of an effective vaccine for individuals and communities can result in high and widespread demand, it is important that vaccine distribution are made in ethical, transparent and scientific manner. 11 It is expected that there will be a limited initial supply of COVID-19 vaccine. Under this scenario, it is necessary to investigate how to prioritize the first available doses in order to achieve the greatest impact. The purpose of this study was to estimate the seroprevalence and to identify the exposure risk of various subgroups among HCWs that would enable the concerned authorities to prioritize them for earlier vaccination.
Materials and methods
This was a multicentre cross-sectional study conducted in two major tertiary-care hospitals (Prime Foundation group of hospitals: Mercy Teaching Hospital and Kuwait Teaching Hospital), Peshawar city Pakistan. Participants of the study were selected from a list of HCWs through simple random sampling technique. A total number of 1000 HCWs were invited to participate (500 from Mercy Teaching Hospital and 500 from Kuwait Teaching Hospital). The sampling period was from 15 to 29 June 2020. The HCWs included doctors, nurses, paramedics and hospital support staff.
Informed consent was obtained from all HCWs. The study has been approved by Institutional Review Board (IRB) of Prime Foundation, Pakistan (IRB approval no. Prime/IRB/2020-394). Data on sociodemographic characteristics were collected on a semi-structured proforma. From each study participant, 5 ml of peripheral venous blood was collected in lithium heparin tubes. Serum was separated using 2500 r/min centrifuge and stored in labelled serum cup for analysis using 20 µl serum volume while the rest was subsequently stored at –80°C temperature. COBAS e411 system was used for immunoassay.
The US Food and Drug Administration (FDA) approved kit was used for detection of SARS-CoV-2 antibodies with specificity: 100% and sensitivity: >98·8% according to the manufacturers. 12 Results were interpreted against a cut-off value of 1 AU/ml, where less than 1 AU/ml was considered negative and more than or equal to 1 AU/ml as positive.
Statistical analyses were performed using SPSS, version 24. Chi-square test was used to compare between categorical variables like gender, age groups, professional categories and seropositivity. Age was categorized into ⩽20, 21–30, 31–40, 41–50 and 51–60 years. Professional category of the HCWs was categorized as consultants, junior doctors, nursing staff, paramedical staff and hospital support staff. The logistic regression analysis was run to predict the odds of seropositivity among different professional categories. Variables with p values <0.05 in the univariable analysis were further used for a multivariable logistic regression analysis to adjust for confounder covariates like age and gender. The threshold for statistical significance was established at a p value ⩽0.05.
Results
A total number of 987 HCWs agreed to participate in this study. More than half (52.5%, n = 519) were younger than or equal to 30 years of age. The participants included 68% (n = 672) males and 32% (n = 315) females with a mean age of 33.2 years (standard deviation, SD: ±9.4). The professional categories of HCWs comprised 13.5% (n = 133) consultants, 29.9% (n = 295) junior doctors (trainee doctors, medical officers and house officers), 21.2% (n = 209) nursing staff, 27.7% (n = 275) paramedical staff and 7.6% (n = 75) hospital support staff (Table 1).
Table 1.
Sociodemographic characteristics and seroprevalence..
| Number of participants N |
Seropositive N (%) |
Seronegative N (%) |
Seroprevalence (95% CI) binomial exact | p value | |
|---|---|---|---|---|---|
| Overall | 987 | 310 (31.4%) | 677 (68.6%) | 31.4% (28.5–34.4) | |
| Gender | |||||
| Male | 672 | 225 (33.5%) | 447 (66.5%) | 33.5% (29.9–37.1) | <0.05 a |
| Female | 315 | 85 (27.0%) | 230 (73.0%) | 27.0% (22.1–32.2) | |
| Age groups | |||||
| ⩽20 | 12 | 1 (8.3%) | 11 (91.7%) | 8.3% (2.1%–38.4%) | <0.05 a |
| 21–30 | 507 | 143 (28.2%) | 364 (71.8%) | 28.2% (24.2%–32.1%) | |
| 31–40 | 266 | 90 (33.8%) | 176 (66.2%) | 33.8% (28.1%–39.8%) | |
| 41–50 | 136 | 49 (36.0%) | 87 (64.0%) | 36.0% (27.9%–44.7%) | |
| 51–60 | 66 | 27 (40.9%) | 39 (59.1%) | 40.9% (28.9%–53.7%) | |
| Professional category | |||||
| Consultant | 133 | 28 (21.1%) | 105 (78.9%) | 21.1% (14.4–28.9) | <0.05 a |
| Junior doctors | 295 | 57 (19.3%) | 238 (80.7%) | 19.3% (14.9–24.3) | |
| Nursing staff | 209 | 81 (38.8%) | 128 (61.2%) | 38.8% (32.1–45.7) | |
| Paramedical staff | 275 | 117 (42.5%) | 158 (57.5%) | 42.5% (36.6–48.6) | |
| Hospital support staff | 75 | 27 (36.0%) | 48 (64.0%) | 36.0% (25.2–47.9) | |
CI, confidence interval.
Chi-square test.
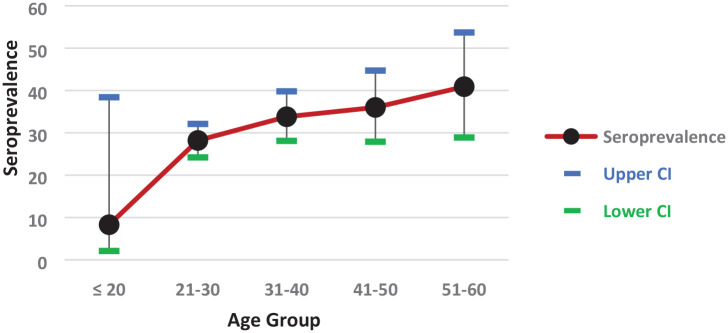
Overall, 310 (31.4%) HCWs were seropositive for SARS-CoV-2 antibodies (95% confidence interval, CI: 28.5–34.4). Seroprevalence was higher in males (33.5%) compared with females (27.0%) with statistical significant difference (p < 0.05; Table 1). Seroprevalence increased with increasing age from 8.3% in age group ⩽20 to 40.9% in 51–60 years of age group (p < 0.05) (Graph 1).
Graph 1.
Seroprevalence of SARS-CoV-2 by age group.
Seroprevalence in different professional category ranged from 19.3% (95% CI: 14.9–24.3) in juniors doctors to 42.5% (95% CI: 36.6–48.6) in paramedical staff. The highest seroprevalence was identified in paramedical staff (42.5%, 95% CI: 36.6–48.6) followed by nursing staff (38.8%, 95% CI: 32.1–45.7) and hospital support staff (36.0%, 95% CI: 25.2–47.9) while consultant and junior doctors had seroprevalence of 21.1% (95% CI: 14.4–28.9) and 19.3% (95% CI: 14.9–24.3), respectively (Table 1). The logistic regression model shows good calibration with Hosmer–Lemeshow test (p = 0.299).
In logistic regression, being a male HCW led to higher risk of seropositivity (odds ratio, OR: 1.50, 95% CI: 1.06–2.13, p < 0.05) compared with female staff members. The odds of seropositivity was higher in nurses (OR: 3.47, 95% CI: 1.99–6.05, p < 0.01), paramedical staff (OR: 3.19, 95% CI: 1.93–5.28, p < 0.01) and hospital support staff (OR: 2.47, 95% CI: 1.29–4.7, p < 0.01) compared with consultants (Table 2).
Table 2.
Univariable and multivariable analysis of professional category with seropositivity.
| Relative variable | Univariable analysis | Multivariable analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Age | 1.01 | 1.01–1.03 | 0.02 a | |||
| Gender | ||||||
| Female (reference) | ||||||
| Male | 1.32 | 1.01–1.83 | 0.04 a | 1.50 | 1·06–2.13 | 0.02 a |
| Professional category | ||||||
| Consultant (reference) | ||||||
| Junior doctor | 0.89 | 0.54–1.49 | 0.67 | 1.25 | 0.71–2.20 | 0.42 |
| Nursing staff | 2.37 | 1.43–3.91 | 0.00 a | 3.47 | 1.99–6.05 | 0.00 a |
| Paramedical staff | 2.77 | 1.71–4.49 | 0.00 a | 3.19 | 1.93–5.28 | 0.00 a |
| Hospital support staff | 2.10 | 1.12–3.95 | 0.02 a | 2.47 | 1.29–4.71 | 0.00 a |
CI, confidence interval; OR, odds ratio.
Refers to p value with statistically significant association.
Discussion
Our study demonstrated a high seroprevalence rate (31.4%) of SARS-CoV-2 antibodies in HCWs. The seroprevalence was higher in age group 51–60 years (40.9%) and in male HCWs (33.5%). The risk of seropositivity was significantly higher (OR: 3·47) in nursing staff compared with other hospital staff.
The seroprevalence of 31.4% revealed a comparatively higher infection rate among HCWs in this country than some others. Several studies from the United States, Spain and Germany have reported lower seroprevalence rate in HCWs,2,13,14 but higher rates have also been reported among those high-risk HCWs serving in COVID-19 isolation unit/wards.15,16
In this study, the investigators observed variation in infection rates by professional category and their job role. The seropositivity was significantly higher in paramedical (42.5%) and nursing staff (38.8%) compared with junior (19.3%) and senior doctors (21.1%) which is consistent with the findings observed in a New Jersey hospital study of 546 HCWs of whom majority of infected HCWs (62.5%) were staff nurses. 17 These findings are suggesting the likelihood of frequent exposure by the nurses and paramedical staff to infection by spending more time in patients’ room. In a recent published review, the significance of heating, ventilation and air conditioning (HVAC) in the SARS outbreak was indirectly proven in six of the seven studies either by the spatial and temporal pattern of cases or using airflow-dynamics models. 18 Apart from higher exposure and longer duration of contact, it may also be due to inadequate use of personal protective equipment (PPE) and their awareness levels.19,20 A recent meta-analysis published in The Lancet journal concluded that physical distancing, use of mask and goggles significantly decrease the risk of infection. 21
This study revealed that the order of priority based on higher risk is given as nurses, paramedics, hospital support staff, young doctors and consultants. The early vaccination of HCWs is critical to ensuring safety and well-being of the frontline workforce that constitutes around 21 million individuals world over apart from those who daily come in contact with them.10,22
Our study also revealed significant difference in seropositivity rate between genders (male: 33.5% and female: 27%, p < 0.05). Some studies observed no significant difference in seroprevalence rate, 23 while several others have reported males are more susceptible to SARS-CoV-2 viral infection. 24 The high infection rate among male HCWs may be due to increased social interaction, ignoring social distancing and inadequate use of PPE. 25
We also observed that seropositivity rate increased with increasing age with highest seroprevalence of 40.9% (95% CI: 28.9%–53.7%) in age group 51–60 years. Similar findings were observed in a study conducted on a larger sample of 35,883 in which highest seroprevalence was identified in age group 45 years and above. 26 The same was concluded in a mathematical model of epidemic data from six countries, and a positive correlation was found with increasing age and the susceptibility of young was almost half to that of adults. 27
Despite the huge supply, COVID-19 vaccines are still far less than the global demand including in developed countries like the United States, Germany and Canada.28 –31
The success of the COVID-19 vaccination plan among HCWs also depends on the uptake rate. 32 Efforts aimed at increasing employee awareness of vaccination efficacy should be encouraged among them in order to increase its acceptability.
The limited supply of COVID-19 vaccine may also affect vaccinating the HCWs especially in low- and middle-income countries. The sub-grouping of HCWs with higher and lower risks will enable health authorities to prioritize them for vaccination against COVID-19. It will ensure fair play in the distribution and administration of vaccines among the various cadres of health staff. Such studies in various other professions may also benefit in analogical terms from the same principle. It will allow queuing the people in wait for vaccines in a transparent way due to its limited supply even in the developed countries.
Strengths and limitations
The key strength of this study is a high participation rate of HCWs from two major teaching hospitals. The participants were not selected based on the presence of symptoms, which gives a unique picture of seroprevalence in different categories of HCWs. Our study has certain limitations. First, this was a cross-sectional study. Second, the participants of the study belong to same group of hospitals and the results might be under-representative.
Conclusion
All HCWs should be vaccinated to reduce their risk of acquiring COVID-19. However, due to higher risk in subgroups among the HCWs, the nursing and paramedical staff should be vaccinated on priority. No study has been done on the same topic in the country; these results will add up to the workforce that is critically required in the current situation for ensuring a functional health care system. The analogy can be extended for equitable distribution of limited supplies of vaccines among other professions, also.
Acknowledgments
The authors would like to thank all study participants from Peshawar Medical College group of hospitals (Mercy teaching hospital and Kuwait teaching hospital).
Footnotes
Author contributions: Mohsina Haq: Conceptualization; Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing.
Asif Rehman: Data curation; Formal analysis; Methodology; Software; Validation; Writing – original draft; Writing – review & editing.
Momina Haq: Investigation; Methodology; Writing – original draft.
Hala Haq: Methodology; Supervision; Writing – original draft.
Hala Rajab: Methodology; Supervision; Writing – original draft.
Junaid Ahmad: Formal analysis; Writing – original draft; Writing – review & editing.
Jawad Ahmed: Conceptualization; Methodology; Writing – original draft.
Saeed Anwar: Formal analysis; Writing – original draft; Writing – review & editing.
Sajjad Ahmad: Conceptualization; Writing – review & editing.
Najib Ul Haq: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Writing – original draft; Writing – review & editing.
Availability of data and material: Study data are available from the corresponding author on reasonable request.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by Prime Foundation (Grant no: PF-PFS-002-201504), while severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody kits were donated by ROCHE.
ORCID iD: Asif Rehman  https://orcid.org/0000-0002-6133-3349
https://orcid.org/0000-0002-6133-3349
Contributor Information
Mohsina Haq, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Asif Rehman, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Momina Haq, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Hala Haq, Fazaia Medical College, Islamabad, Pakistan.
Hala Rajab, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Junaid Ahmad, Prime Institute of Public Health, Riphah International University, Islamabad, Pakistan.
Jawad Ahmed, Institute of Basic Medical Sciences, Khyber Medical University, Peshawar, Pakistan.
Saeed Anwar, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Sajjad Ahmad, Peshawar Medical College, Riphah International University, Islamabad, Pakistan.
Najib Ul Haq, Peshawar Medical College, Riphah International University, Warsak Road Peshawar, Islamabad, Pakistan.
References
- 1. Shaukat N, Ali D, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 2020; 13: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wilkins J, Gray E, Wallia A, et al. Seroprevalence and correlates of SARS-CoV-2 antibodies in health care workers in Chicago. Open Forum Infect Dis 2020; 8: ofaa582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC COVID-19 Response Team. Characteristics of health care personnel with COVID-19 – United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Are authorities under-reporting deaths of healthcare providers due to COVID-19 in Pakistan? Thenews.com.pk, 4 December 2021, https://www.thenews.com.pk/print/753237-are-authorities-under-reporting-deaths-of-healthcare-providers-due-to-covid-19-in-pakistan (accessed 8 March, 2021).
- 5. WHO. Advice on the use of point-of-care immunodiagnostic tests for COVID-19, 2021, https://www.who.int/news-room/commentaries/detail/advice-on-the-use-of-point-of-care-immunodiagnostic-tests-for-covid-19 (accessed 5 March 2021).
- 6. Zhao J, Yuan Q, Wang H, et al. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Clin Infect Dis 2020; 71: 2027–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ministry of Health. COVID-19: guidance for prioritizing health care workers for COVID-19 vaccination, 2021, http://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/Guidance_for_Prioritizing_HCW_covid19_vaccination_2020-01-08.pdf (accessed 3 March 2021).
- 8. Wise J. COVID-19: health and care workers will be ‘highest priority’ for vaccination, says JCVI. BMJ 2020; 369: m2477, https://www.bmj.com/content/369/bmj.m2477 (accessed 6 February 2021). [DOI] [PubMed] [Google Scholar]
- 9. Mantovani C. Health workers should be top priority for vaccines – nurses’ group. Reuters, 27 July 2020, https://www.reuters.com/article/us-health-coronavirus-who-healthworkers-idUSKCN24S1UD (accessed 6 February 2021).
- 10. Centers for Disease Control and Prevention. The importance of COVID-19 vaccination for healthcare personnel, 2020, https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/hcp.html (accessed 6 February 2021).
- 11. COVID-19 immunization strategy: priority population, 2021, https://www.isglobal.org/documents/10179/7860911/REPORT+Priority+populations+for+covid+vaccine.pdf/ffae9d74-e3dc-47b9-8b70-49b82d7478f5 (accessed 8 March 2021).
- 12. Roche’s COVID-19 antibody test receives FDA Emergency Use Authorization and is available in markets accepting the CE mark. Roche.com, 2021, http://www.roche.com/media/releases/med-cor-2020-05-03.html (accessed 8 January 2021).
- 13. Garcia-Basteiro A, Moncunill G, Tortajada M, et al. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun 2020; 11: 3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Korth J, Wilde B, Dolff S, et al. SARS-CoV-2-specific antibody detection in healthcare workers in Germany with direct contact to COVID-19 patients. J Clin Virol 2020; 128: 104437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Contejean A, Leporrier J, Canouï E, et al. Comparing dynamics and determinants of severe acute respiratory syndrome coronavirus 2 transmissions among healthcare workers of adult and pediatric settings in central Paris. Clin Infect Dis 2020; 72: 257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mansour M, Leven E, Muellers K, et al. Prevalence of SARS-CoV-2 antibodies among healthcare workers at a tertiary academic hospital in New York City. J Gen Intern Med 2020; 35: 2485–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Barrett E, Horton D, Roy J, et al. Prevalence of SARS-CoV-2 infection in previously undiagnosed health care workers in New Jersey, at the onset of the U.S. COVID-19 pandemic. BMC Infect Dis 2020; 20: 853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chirico F, Sacco A, Bragazzi N, et al. Can air-conditioning systems contribute to the spread of SARS/MERS/COVID-19 infection? Insights from a rapid review of the literature. Int J Environ Res Public Health 2020; 17: 6052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen Y, Tong X, Wang J, et al. High SARS-CoV-2 antibody prevalence among healthcare workers exposed to COVID-19 patients. J Infect 2020; 81: 420–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Magnavita N, Soave P, Ricciardi W, et al. Occupational stress and mental health among anesthetists during the COVID-19 pandemic. Int J Environ Res Public Health 2020; 17: 8245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chu D, Akl E, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020; 395: 1973–1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Coppeta L, Balbi O, Grattagliano Z, et al. First dose of the BNT162b2 mRNA COVID-19 vaccine reduces symptom duration and viral clearance in healthcare workers. Vaccines 2021; 9: 659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Xu X, Sun J, Nie S, et al. Seroprevalence of immunoglobulin M and G antibodies against SARS-CoV-2 in China. Nat Med 2020; 26: 1193–1195. [DOI] [PubMed] [Google Scholar]
- 24. Ortolan A, Lorenzin M, Felicetti M, et al. Does gender influence clinical expression and disease outcomes in COVID-19? A systematic review and meta-analysis. Int J Infect Dis 2020; 99: 496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tian C, Lovrics O, Vaisman A, et al. Risk factors and protective measures for healthcare worker infection during highly infectious viral respiratory epidemics: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. Epub ahead of print January 2021. DOI: 10.1017/ice.2021.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pollan M, Perez-Gomez B, Pastor-Barriuso R, et al. A population-based seroepidemiological study of SARS-CoV-2 in Spain. Preprints with The Lancet 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Davies N, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med 2020; 26: 1205–1211. [DOI] [PubMed] [Google Scholar]
- 28. Coronavirus: German states say vaccinations delayed due to shortage. DW, 30 December 2020, https://www.dw.com/en/coronavirus-german-states-say-vaccinations-delayed-due-to-shortage/a-56097728 (accessed 8 March 2021).
- 29. Lexchin J. The roots of Canada’s COVID-19 vaccine shortage go back decades. The Conversation, 8 February 2021, https://theconversation.com/the-roots-of-canadas-covid-19-vaccine-shortage-go-back-decades-154792 (accessed 8 March 2021).
- 30. VIRUS TODAY: US states report COVID-19 vaccine shortage. ABC News, 21 January 2021, https://abcnews.go.com/Health/wireStory/virus-today-us-states-report-covid-19-vaccine-75384066 (accessed 8 March 2021).
- 31. Centers for Disease Control and Prevention. COVID data tracker, 2021, https://covid.cdc.gov/covid-data-tracker/#vaccinations (accessed 8 March 2021).
- 32. Trabucco Aurilio M, Mennini F, Gazzillo S, et al. Intention to be vaccinated for COVID-19 among Italian nurses during the pandemic. Vaccines 2021; 9: 500. [DOI] [PMC free article] [PubMed] [Google Scholar]