ABSTRACT
The proper development and patterning of organs rely on concerted signaling events emanating from intracellular and extracellular molecular and biophysical cues. The ability to model and understand how these microenvironmental factors contribute to cell fate decisions and physiological processes is crucial for uncovering the biology and mechanisms of life. Recent advances in microfluidic systems have provided novel tools and strategies for studying aspects of human tissue and organ development in ways that have previously been challenging to explore ex vivo. Here, we discuss how microfluidic systems and organs-on-chips provide new ways to understand how extracellular signals affect cell differentiation, how cells interact with each other, and how different tissues and organs are formed for specialized functions. We also highlight key advancements in the field that are contributing to a broad understanding of human embryogenesis, organogenesis and physiology. We conclude by summarizing the key advantages of using dynamic microfluidic or microphysiological platforms to study intricate developmental processes that cannot be accurately modeled by using traditional tissue culture vessels. We also suggest some exciting prospects and potential future applications of these emerging technologies.
KEY WORDS: Biophysics, Microfluidics, Microphysiological systems, Organs-on-chips, Tissue engineering, In vitro models
Summary: This Primer provides an overview of the fabrication and use of microfluidic systems for studying cellular development and differentiation, highlighting the advantages of using these systems over traditional culture techniques.
Introduction
Human development involves multiple concerted and coordinated events that enable the formation of tissues and organs. The ability to model and understand the contributions of different microenvironmental factors to various physiological processes – including cell fate decisions, embryonic development and organogenesis – is crucial for uncovering biological mechanisms and therapies. Many established methods for studying developmental processes have been limited to static ex vivo cell cultures in two-dimensional (2D) substrates, multicellular spheroids and organoids, or in vivo animal models. Each of these methodologies has unique advantages, as well as some limitations. For example, although traditional multiwell plate and biopsy cultures have provided simple and inexpensive means to study cellular behavior, their physiological relevance is limited by the lack of tissue-like structures and the inability to modulate mechanical properties and fluid dynamics. In addition, cell culture systems require frequent media changes to limit cellular exposure to toxic agents and debris. Traditionally, animal models have been used to assess the deleterious effects of gene mutations or drug exposure on developing organs and tissues. However, some developmental and biological pathways are not conserved in humans, and hence animal models often only partially represent physiology and disease phenotypes (Ingber, 2020). Organoids have garnered interest for their ability to model some of the early stages of organ development. However, current methodologies for generating organoids usually result in models with fetal-like characteristics, thus lacking the appropriate cell differentiation states and patterning observed in postnatal and adult tissues and organs. Additionally, organoids are usually not perfusable owing to the lack of microvascular structures with accessible lumina (Hofer and Lutolf, 2021). In contrast, microfluidic systems (µFs) can closely mimic the developing in vivo environment by utilizing substrates with tunable mechanical properties and variable three-dimensional (3D) architectures, while continuously providing nutrients and oxygen to cells through media perfusion (Hofer and Lutolf, 2021).
µFs are small-scale devices (approximately the size of a computer memory stick), which contain channels with micrometer-scale dimensions (Whitesides, 2006). These devices are engineered using various technologies and the channels within the device can be micropatterned to achieve the desired dimensions, geometry, forces and gradients of molecular signals. µFs offer the advantages of being more physiologically relevant and species specific, equipping researchers with tools to address questions related to tissue development and disease, while potentially being more cost-effective than in vivo animal studies. However, μFs do have some limitations (Table 1).
Table 1.
Limitations and potential solutions of using microfluidic devices for biological applications
In this Primer, we introduce µFs as an emerging tool for modeling development. We discuss how different types of µFs have been designed and engineered, how these systems help to recapitulate human organ function, and how they overcome the limitations of traditional tissue culture systems and organoids. We then dive into how human embryonic development and organs have been studied and modeled by µFs. Finally, we suggest some prospects and potential future applications of these emerging µF technologies.
Microfabrication of microfluidic devices for modeling tissue development and function
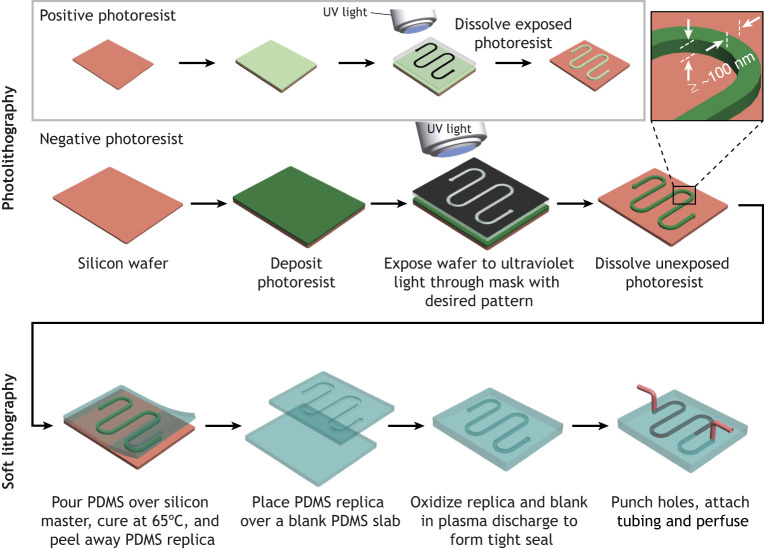
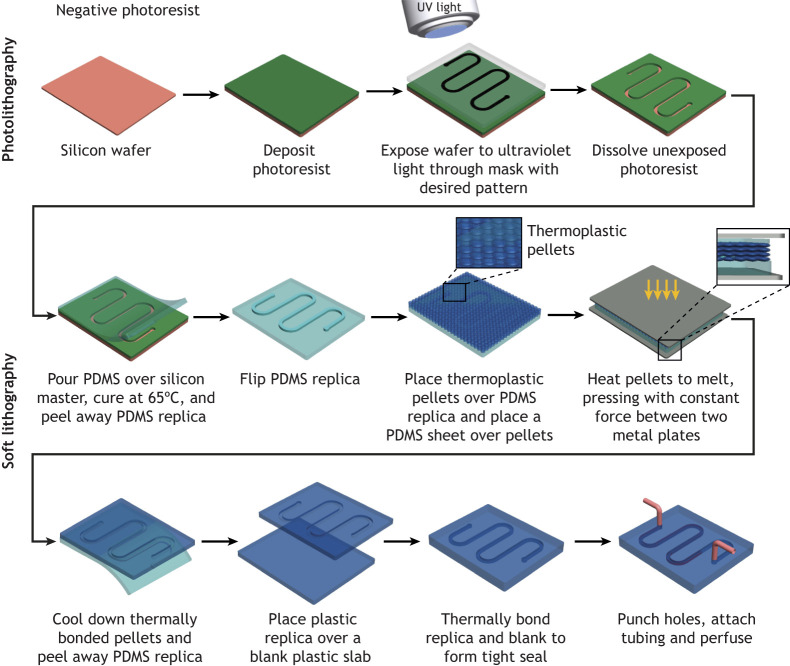
µFs are engineered using photolithography and soft lithography techniques (Fig. 1). In photolithography manufacturing, microscale structures of a light-sensitive polymer or photoresist are transferred onto a silicon wafer (Weibel et al., 2007) by coating it with photoresist material and then projecting ultraviolet (UV) light through a mask onto the wafer. The mask consists of transparent glass coated with opaque chrome at specific regions, which enables selective transmission or blocking of UV light onto the wafer. Two types of photoresist (positive and negative) are commonly used. Upon exposure to UV light, positive photoresist becomes soluble in an aqueous developer solution, whereas negative photoresist becomes insoluble. Hence, the exposed positive photoresist or unexposed negative photoresist is subsequently removed by dissolution with the developer. The resulting wafer provides a mold to produce inverse copies of the structures or microscale channels within polymerized polydimethylsiloxane (PDMS). These engineered PDMS copies are combined with blank PDMS slabs to assemble the µFs for final use (Duffy et al., 1998). If desired, PDMS copies with microscale structures can be used as molds to produce µFs from other materials, including biodegradable synthetic polymers, such as poly(dl-lactide-co-glycolide) (PLGA) (Fig. 2) (King et al., 2004).
Fig. 1.
Microfabrication of a PDMS microfluidic device with photolithography and soft lithography manufacturing processes. Microstructures of a negative photoresist are transferred onto a silicon wafer during photolithography. Similarly, microstructures of positive photoresist can be transferred onto wafers, as shown in the inset (gray box). The width and height (z-dimension) of the microstructure is ≥100 nm. The wafer is used as a mold to produce a PDMS replica during soft lithography. The replica is used to assemble a microfluidic device. Re-drawn based on studies by Duffy et al. (1998).
Fig. 2.
Microfabrication of a biodegradable synthetic polymer-based (thermoplastic) microfluidic device using photolithography and soft lithography manufacturing processes. Microstructures of a negative photoresist are transferred onto a silicon wafer during photolithography. The wafer is used as a mold to produce a PDMS replica during soft lithography. The PDMS replica is then used as a mold to produce a thermoplastic replica. The thermoplastic replica is used to assemble a microfluidic device. Re-drawn based on studies by King et al. (2004).
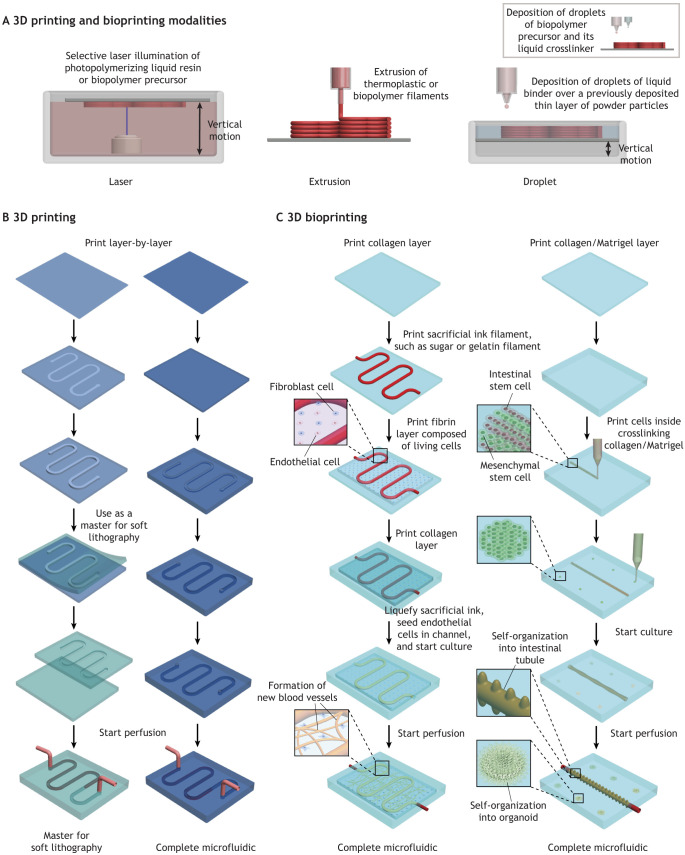
In addition to photolithography, printing technology can simplify the fabrication of µFs. For example, laser printers can print opaque inks onto transparent sheets to replace the more expensive chrome masks (Xia and Whitesides, 1998). 3D printing technology (Fig. 3A) is a potential alternative to photolithography and silicon wafers for the production of PDMS-based µFs (Fig. 3B) (Ozbolat et al., 2018). Furthermore, 3D printing has expanded the use of biodegradable polymers, such as PLGA, poly-L-lactic acid (PLLA) and polycaprolactone (PCL) (Vozzi et al., 2003, 2002), that can be easily molded to form the desired patterns or channels for microfluidic devices. In addition, 3D printing has enhanced the level of complexity with which µFs can be designed and built to achieve specific structures and affect cellular responses (Wu et al., 2011). Bioprinting or 3D bioprinting, which involves precise deposition of living cells, physiological signaling molecules and/or polymeric scaffolds, has improved our ability to recapitulate tissue structure and biological responses within µFs. For example, interconnected microvascular networks have been recapitulated in a bioprinted collagen/fibrin µF through angiogenic sprouting induced by bioprinted endothelial cells (Fig. 3C) (Lee et al., 2014b). Similarly, Lutolf and colleagues have modeled a perfusable intestinal tube through multicellular self-organization of bioprinted multipotent stem cells, such as intestinal stem cells and mesenchymal stem cells (MSCs), within a collagen/Matrigel µF (Fig. 3D) (Brassard et al., 2021).
Fig. 3.
Microfabrication of microfluidic devices using 3D printing and bioprinting technologies. (A) Modalities of 3D printing and bioprinting technology for layer-by-layer microfabrication, including laser-initiated photopolymerization of a synthetic resin or biopolymer precursor, extrusion of a thermoplastic or biopolymer filament, and deposition of droplets of a liquid binder over metals, sand or ceramics, which are available in granular form. Inset (grey box) shows droplet-based bioprinting. (B) 3D printing of synthetic polymers for microfabrication of molds and complete microfluidic devices. (C) 3D bioprinting of biopolymers, living cells and physiological signaling molecules for microfabrication of a microfluidic device consisting of an interconnected vascular network (left) and a microfluidic device consisting of a perfusable intestinal tube (right). Re-drawn based on published studies (Brassard et al., 2021; Lee et al., 2014b; Miller et al., 2012).
Molecular and biophysical regulation of tissue formation and function
Molecular gradients
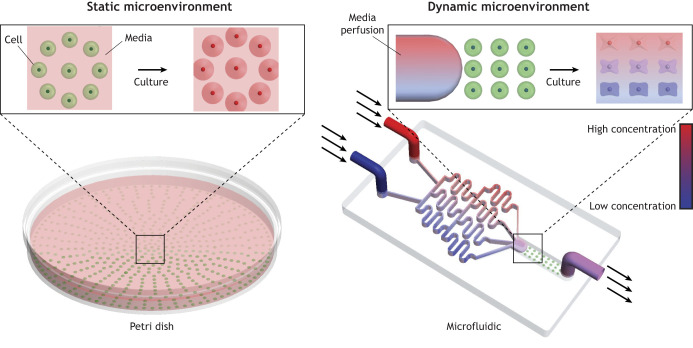
During embryonic development, concentration gradients of morphogens are crucial for the lineage specification and proper patterning of cells, tissues and organs. For example, Wnt signaling orchestrates the development of the primary body axis during the development of multicellular organisms by polarizing primary cells and directing the spatial organization and fates of daughter cells (Loh et al., 2016). µFs can generate Wnt3 gradients and a graded Wnt signaling response in human embryoid bodies (Cimetta et al., 2013). Subsequently, user-controlled systems have been developed for the modulation of cells, such as human pluripotent stem cells (hPSCs). For example, tunable morphogen gradients (Fig. 4) have enabled the formation of dynamic spatial patterning of ectoderm, trophectoderm and mesendoderm cell fates from hPSCs (Manfrin et al., 2019; Regier et al., 2019). In addition, static and fluid flow-based µFs can generate molecular gradients to induce primitive streak formation (Cui et al., 2020). Molecular gradients are also important for regulating the sprouting and branching of blood vessels during angiogenesis (Costa et al., 2020). A high-throughput µF can recapitulate angiogenic sprouting (van Duinen et al., 2019), revealing that prolonged gradient exposure promotes the formation of sprouts that are capable of connecting to other outgrowths within parallel perfusion channels, and leads to pruning and modulation of the capillary structure. Another study has revealed that vascular endothelial cell migration and proliferation can be modulated by oxygen concentration gradients within µFs (Shih et al., 2019), with endothelial cells migrating towards low-oxygen areas. Together, these results indicate that µFs can be used to study the effects of molecular gradients on tissue development and patterning.
Fig. 4.
Schematic of molecular gradient and mechanical or biophysical cues presented by microfluidic systems. A microfluidic device (right) that provides molecular gradients as well as media (fluid) flow compared with static culture conditions lacking both features (left). The use of molecular gradients can reveal the concentration-dependent effects of molecules on cell phenotype and tissue patterning.
Future investigations into the mechanisms of primitive streak formation using µFs could further enhance our understanding of how deleterious genetic mutations occur and influence disease progression, potentially enabling the development of targeted therapies for developmental defects.
Regulation of mechanotransduction
Mechanotransduction is the process by which cells sense mechanical stimuli (Fig. 4) in their microenvironment or intracellularly and convert these signals into biochemical cues to affect gene regulation (Hayward et al., 2021).
Fluid forces (fluid shear stress)
The ability of µFs to control fluid flow dynamically makes them suitable for investigating how fluid forces, such as pressure, strain and shear stress, influence cellular processes (Huber et al., 2018). For example, fluid shear stress can be manipulated in µFs by changing the flow rate of the tissue culture medium or by altering the dimensions and geometry of the fluidic microchannels (Fig. 4). Fluid shear stress plays key roles in regulating endothelial cell migration and thus angiogenesis and neovascularization. Indeed, the impact of fluid shear stress on vascularization has been extensively studied using μFs (reviewed by Akbari et al., 2017). Hsu and colleagues have utilized µFs to investigate the role of luminal shear stress on neovascularization, which is important in angiogenesis because fluid shear stress plays key roles in regulating endothelial cell migration (Li et al., 2005). High levels of shear stress inhibit endothelial sprouting, whereas reduced luminal shear stress promotes neovascularization. Fluid shear stress also facilitates vascularization and differentiation of kidney organoids by enhancing vascular outgrowths and the cellular phenotype to mimic early stages of kidney development (Homan et al., 2019). Furthermore, fluid shear stress influences the differentiation of MSCs into osteocytes (Yourek et al., 2010). Jiang and colleagues have engineered µFs with an objective lens that allows live-cell imaging of the MSCs in the device (Zheng et al., 2012), and the authors have shown that the cells initially undergo contraction, followed by re-spreading after an hour of fluid shear stress stimulation. Mechanistic studies have revealed the involvement of key mechanotransduction pathways as cells respond to fluid shear stress.
Substrate stiffness and mechanical strain
In addition to fluid shear stress, µFs have provided insights into the role of other mechanical stimuli, such as substrate stiffness and compressive forces, on cell fate determination and organ development. Naderi-Manesh and colleagues have investigated the role of substrate elasticity on human amniotic MSC differentiation in µFs using a substrate containing fibrin hydrogel and gold nanowires (Hashemzadeh et al., 2020). By modulating hydrogel elasticity, soft substrates with low fibrin content preferentially guide chondrocyte differentiation of the MSCs, whereas the stiff substrate with high fibrin content promotes osteocyte differentiation. Additionally, mechanical strain plays a crucial role in the development of various organs, including the kidneys, gut and lungs (Huh et al., 2010; Kim et al., 2012; Musah et al., 2018, 2017). For example, applying physiological cyclic strain to a µF containing human alveolar epithelial cells and microvascular endothelial cells results in the alignment of the endothelial cells, resembling observations in vivo (Huh et al., 2010). Studies aiming to reconstitute human kidney functions in vitro have applied mechanical strain (stretch and relaxation motions) in vascularized µFs lined by hPSC-derived podocytes, which significantly improves the development of multicellular structures that more closely mimic the tissue-tissue interface and function of an intact human kidney glomerular capillary wall (Musah et al., 2018, 2017; Roye et al., 2021; Uccelli et al., 2008).
Together, these studies illustrate that µFs possess unique biophysical properties that enable stimulation of mechanotransduction pathways to influence tissue development and structural organization.
Embryogenesis
Embryogenesis is an intricate process characterized by cell division and differentiation in the early stages of development to form an embryo. The early stages of this process consist of key events, such as fertilization, germinal stages, implantation, placenta formation, and neurulation. However, human embryogenesis is difficult to study in vivo because of ethical concerns and the availability of early-stage embryos. µFs provide physiologically relevant platforms with controllable and reproducible features for modeling and understanding the cellular and molecular mechanisms of development in humans and other species.
Fertilization, germinal stages and pre-implantation development
Fertilization, the first step of embryogenesis, has been modeled in a variety of µFs using murine, bovine or porcine cells and tissues (Weng, 2019). After fertilization, the zygote enters the germinal stage and undergoes cleavage divisions leading to the development of blastomeres. Recent work has employed µFs that combine cell isolation, imaging, single-cell immunoblotting and isolation of nuclei for RT-qPCR to investigate protein heterogeneity profiles in two- and four-cell murine embryos (Rosas-Canyelles et al., 2020). Specifically, sister blastomeres from four-cell embryos display higher heterogeneity for the DNA damage repair protein GADD45a than two-cell embryos, validating prior single-cell RNA-sequencing studies. This µF could enhance current understanding of gene and proteome expression profiles at the single-cell level. Mammalian embryos cultured in smaller groups using traditional in vitro methods tend to display lower viability. To overcome these limitations, µFs using an isolated microdrop embryo-culture system supplemented with epidermal growth factor have been used to successfully culture single, isolated embryos up to the blastocyst stage in vitro (Paria and Dey, 1990; reviewed by Krisher and Wheeler, 2010). Additionally, µFs have been used to sort embryonic cell populations in order to dissect gene expression programs in a variety of species (Briggs et al., 2018; Klein et al., 2015).
These studies have revealed that the environment provided by µFs can support in vitro culture of individual embryos up to the blastocyst stage and allow selection of high-quality embryos for subsequent applications (Hashimoto et al., 2012; Kieslinger et al., 2015).
Implantation
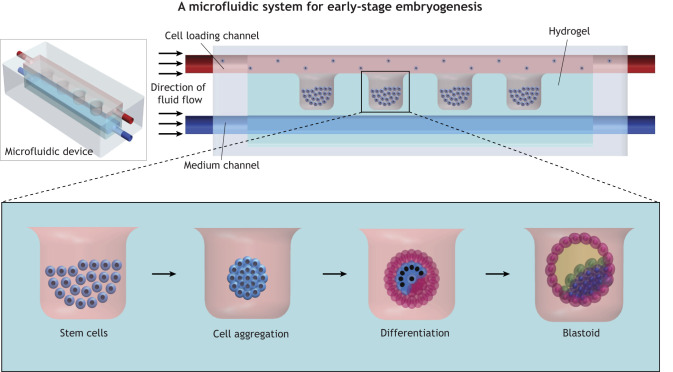
At the blastocyst stage, the human embryo would typically implant in the uterus and the inner cell mass reorganizes into the epiblast and hypoblast layers. To model post-implantation tissue organization, a µF device consisting of three-parallel channels has been developed: one microchannel is used for cell loading, another for supplying cell culture medium and morphogens, and the third, centrally located microchannel contains the extracellular matrix (Zheng et al., 2019). Human embryonic stem cells (hESCs) injected into the cell-loading channel form clusters or aggregates and subsequently differentiate within these microwells. This approach produces epiblast-like cyst structures that resemble the pro-amniotic cavity. By altering the morphogens perfused into the µFs, the authors can anteriorize or posteriorize the resulting sacs. Additional analysis of posteriorized sacs has revealed stratified epiblast epithelium preluding human gastrulation and consisting of the primitive streak, induced mesoderm-like cells and primordial germ cell-like cells. However, these sacs lack a trophoblast layer and primitive endoderm, both of which are required for proper development of the placenta and linings of the digestive tract and respiratory structures in vivo. Still, this study highlights the potential of using hESCs for modeling embryogenesis within the limits of the previously established 14-day embryo culture guidelines (Daley et al., 2016). These studies could be extended in the future to produce constructs with secondary fluidic channels for medium perfusion and incorporation of heterogenous cell populations to generate and simultaneously pattern early embryonic tissues (Fig. 5).
Fig. 5.
Schematic of a microfluidic device for modeling early stages of embryogenesis through the generation of blastoid- or gastruloid-like structures. Seeding of hPSCs or ESCs into a construct with microwells promotes cell aggregation and self-organization. Perfusing the media channels with morphogens (such as FGF2) could direct the cell aggregates to acquire cell fates and pattern into blastocyst-like tissue structures. Varied morphogen perfusion in the respective channels could also direct the aggregates to form specific organoids, such as cardioids. Re-drawn based on studies by Zheng et al. (2019).
Placenta development
During fetal development, the placenta facilitates the transport of nutrients and oxygen from the mother and the removal of waste from fetal circulation. The placenta consists of two cell layers (trophoblast and capillary endothelium) separated by a thin interstitial layer. Together, these components make up the placental barrier, which protects the fetus from harmful particles or toxins circulating in the maternal blood. Several µFs (Fig. 6A) model the placental barrier by culturing human trophoblasts and umbilical vein endothelial cells, separated by an extracellular matrix (Lee et al., 2016). These systems produce more mature cellular phenotypes than those previously developed using traditional in vitro culture methods because media perfusion in µFs results in higher densities of trophoblast microvilli, which are important for molecular transport across the placental barrier (Blundell et al., 2016). µFs can also be used to study mother-fetus molecular crosstalk of nutrients, such as glucose, drugs and potential toxins (Blundell et al., 2016; Fry et al., 2019; Lee et al., 2016). For example, the placental barrier is permeable to carcinogenic TiO2 nanoparticles, commonly found in sunscreens (Fry et al., 2019). Thus, µF placenta models hold great potential for evaluating drug toxicities in the developing fetus and assessing how maternal nutrient and hormonal profiles may affect fetal development.
Fig. 6.
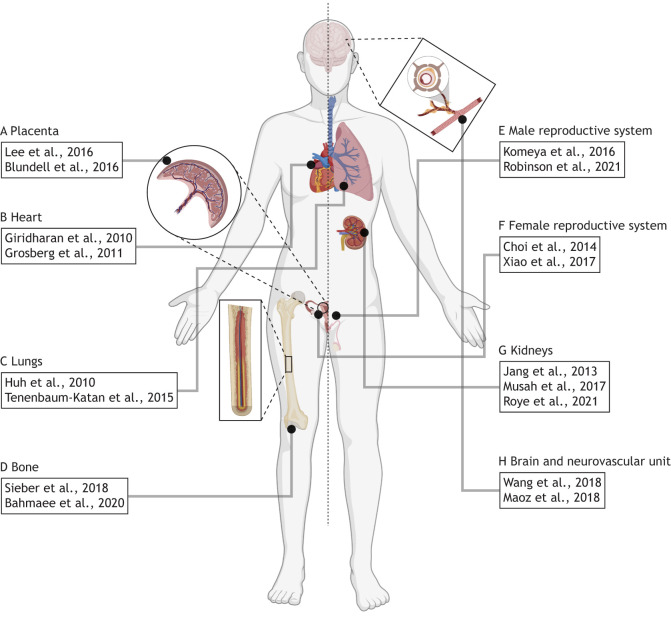
Microfluidic devices for modeling the development and function of various tissues and organs. (A) Microfluidic devices have been used to model the placental barrier (Lee et al., 2016) and have been used to recapitulate maternal-fetal crosstalk (Blundell et al., 2016). (B) Contractile myocytes are commonly used to produce cardiac microfluidic devices (Grosberg et al., 2011) and these systems can subsequently be used to model pharmacological responses (Giridharan et al., 2010). (C) The lungs were one of the first organs modeled using microfluidic devices (Huh et al., 2010), and processes involved in fetal lung development have also been observed (Tenenbaum-Katan et al., 2015). (D) Cells cultured in a microfluidic device mimicking the bone marrow niche are capable of differentiating into specialized types (Sieber et al., 2018), including osteoblasts which facilitate osteogenesis (Bahmaee et al., 2020). (E) Testicular tissue explants cultured in microfluidic devices can generate functional spermatozoa (Komeya et al., 2016), and bioprinted testicular cells organize into their native cytoarchitecture while maintaining their functionality (Robinson et al., 2021 preprint). (F) The role of mechanical heterogeneity in the ovulation of ovarian follicle explants has been studied using microfluidic devices (Choi et al., 2014), and the relationship between the female reproductive tract and the endocrine system has also been studied using connected microfluidic modules (Xiao et al., 2017). (G) The absorption and filtration functions of the kidney proximal tubules (Jang et al., 2013) and glomerulus (Musah et al., 2017; Roye et al., 2021), respectively, have been modeled using microfluidic devices. (H) Microfluidic devices facilitate the differentiation and organization of brain organoids for studying developmental diseases or pharmacological toxicity (Wang et al., 2018). Similarly, multiple microfluidic devices can be coupled to model the blood-brain barrier for observing cell crosstalk and barrier function (Maoz et al., 2018). Anatomical diagram was created with BioRender.com.
Neurulation
Neurulation begins around the fourth week of gestation and gives rise to the neural tube, which later becomes the central nervous system (reviewed by O'Rahilly and Muller, 1994). As mentioned above, µFs with a molecular gradient can model neural tube development from hESCs (Rifes et al., 2020). By exposing hESCs to a gradient of a GSK3 inhibitor (a canonical WNT activator), the WNT gradient necessary for specifying rostral-to-caudal neural axis can be mimicked, with the resulting tissue expressing the caudal marker GBX2 and rostral marker OTX2 in the expected regions. Further differentiation results in the development of neural subregions, such as the midbrain and hindbrain, although these regions lack the characteristic OTX2 caudal borders typically observed in vivo (Broccoli et al., 1999). This limitation of the engineered model could arise from the absence of exogenous WNT agonists and retinoic acid; WNT agonists, such as DKK1, play crucial roles in anterior neural tissue formation and retinoic acid can further posteriorize neural tissues by regulating the expression of Hox genes in the hindbrain (Kiecker and Lumsden, 2005). Thus, appropriate regulation of these molecular targets and pathways could promote delineation of neural tissues, such as the midbrain-hindbrain boundary. Additionally, the ability to propagate the engineered model over prolonged periods could enhance the development of more specialized tissue structures, such as the neural crest and somites. In fact, somitogenesis has recently been achieved using µFs that oscillate WNT, FGF and retinoic acid signaling (van Oostrom et al., 2021).
Microfluidic models of human organs and physiology
During human embryonic development, gastrulation leads to the formation of three germ layers: ectoderm, mesoderm and endoderm (Sadler, 2018). µFs have been used to model the structures and functions of many organs (Rennert et al., 2015; Sriram et al., 2018; Wang et al., 2019); we discuss below some of the models that also recapitulate the process of tissue formation or organ development, including some specific examples representing organs or tissues derived from each of the three germ layers (Fig. 6A-H).
Heart
Heart development begins, at approximately 18-19 days post-fertilization in humans, with factors (such as GATA4) from the underlying endoderm directing the mesoderm towards a cardiac fate (reviewed by Tan and Lewandowski, 2020). Once cardiomyocytes (contractile cardiac cells that perform the rhythmic beating of the heart) have differentiated, they respond to mechanical stimulation, as well as changes in organ size. µFs can be used to apply mechanical stimuli or stress to facilitate the differentiation of hESCs into cardiomyocytes and, in some cases, µFs produce higher yields of cardiomyocytes compared with those generated using embryoid-body methods (Wan et al., 2011). Studies have modeled the effects of mechanical forces on cardiomyocytes observed during organogenesis (Fig. 6B) (Giridharan et al., 2010; Rogers et al., 2016), collectively resulting in the development of µFs capable of modeling the mechanical stretch and atrioventricular pressure seen in the heart, showing that gradual introduction of these biophysical forces, together with a continuous supply of nutrients, leads to greater cell viability and proper tissue alignment, which is crucial for the formation of other cardiac tissue structures, such as the endocardial cushions that later form cardiac valves. Some initial studies have suggested that human endothelial cells in traditional 2D culture systems are unable to undergo the endothelial-to-mesenchymal transition (EMT) required for endocardial cushion formation (Hunter et al., 2018). In contrast, endothelial cells cultured under fluid flow align themselves in the direction of the flow, which might make them more susceptible to EMT in the presence of signaling factors, such as TGFβ (Ma et al., 2020). Compartmentalization of the heart into four different chambers with valves presents some of the greatest challenges of modeling cardiogenesis in vitro. Recently, human hPSC-derived cardiac organoids (or ‘cardioids’), which undergo morphogenesis and self-organization in response to WNT and VEGF signaling to form a cavity that mimics a heart chamber, have been developed (Hofbauer et al., 2021). Using these organoids in combination with mechanical stress in a perfusable system could enable the development of µFs that are capable of modeling events such as a cardiac tube or pericardium formation.
Lungs
Lung organogenesis begins with the formation of the lung bud, which develops from the endoderm-derived foregut. As embryonic development progresses, the lung bud extends to eventually form laryngotracheal and bronchial buds, which subsequently leads to branching morphogenesis and formation of the complex lung architecture (reviewed by Schittny, 2017). The lungs were one of the first organs to be modeled in µFs (Huh et al., 2007, 2010). More recently, µFs have been used to demonstrate that branching morphogenesis, smooth muscle contraction and the rate of tissue maturation of the lungs are influenced by pressure differences between the airway lumen and pleural cavity (Nelson et al., 2017). However, murine embryonic lung explants were used in this study, which are physiologically different from human lungs (Pan et al., 2019). Future work modeling these effects on human embryonic lungs could use branching lung organoids (Vazquez-Armendariz and Herold, 2021) in µFs to examine the contribution of mechanical cues, such as pressure and fluid flow rate, as well as tissue expansion and relaxation to mimic breathing. Another key process in lung development is the formation and maturation of the alveoli, which provide the optimal surface area for gas exchange and form the air-blood interface of the alveolar wall. Sznitman and colleagues have used a human alveolar cell line seeded in the µF (Fig. 6C) to investigate the effects of fluid flow on the formation and maturation of alveolar structures (Tenenbaum-Katan et al., 2015). Using this system, the authors modeled fluid flow dynamics at different developmental stages and calculated the level of wall shear stress at various points within the µF-based alveolar structures. Although this biomimetic model only includes one cell type, the resulting cell monolayers are reminiscent of alveolar epithelium typically seen in fetal lung tissue. More recent studies have designed lung chips that include several types of epithelial cells interfaced with endothelial cells. Although these µFs have been used to model more mature physiology (rather than early developmental processes), they could be useful for studying the etiology of pulmonary diseases and for the discovery of therapeutics (Gkatzis et al., 2018; Jain et al., 2018). Overall, µFs provide an attractive platform for studying the embryonic, fetal and postnatal development and maturation of human lungs.
Bone
The formation of bone (known as ossification or osteogenesis) begins in humans between the sixth and seventh weeks of embryogenesis, and continues until approximately 25 years of age (Breeland et al., 2020). Bone undergoes constant remodeling throughout life and is capable of regeneration after injury (Dimitriou et al., 2011; Einhorn, 1998; Ramachandran, 2018). µFs are useful for studying bone formation and development because they provide 3D environments that can mimic the in vivo bone tissue structure. Incorporation of fluid flow provides fluid shear stress, which facilitates bone formation. For example, Basu and colleagues have developed a µF that contains ultra-high molecular weight polyethylene reinforced with multiwalled carbon nanotubes and/or nanohydroxyapatite (Naskar et al., 2018). By seeding the system with human MSCs to study osteogenesis under shear stress, the authors have characterized three different stages of osteogenesis. Claeyssens and colleagues have developed a 3D µF to study bone formation from human embryonic stem cell-derived mesenchymal progenitor cells (Fig. 6D) (Bahmaee et al., 2020). Here, the cells show enhanced osteogenic differentiation and matrix mineralization when exposed to cyclic fluid flow with intermittent rest periods. Given the role of mechanics in osteogenic differentiation and the dynamic culture environments provided by µFs, it would be intriguing to examine the role of substrate stiffness or mechanical properties on bone formation using µFs (Lee et al., 2014a).
Blood
The ability to study hematopoiesis in vitro could improve the understanding of blood development and related diseases, such as anemia and leukemia (Jagannathan-Bogdan and Zon, 2013). µFs focusing on bone marrow and hematopoiesis have been engineered. For example, Ingber and colleagues have created a mouse ‘bone marrow-on-a-chip’ system by exposing ex vivo cultures of primary bone marrow to fluid flow, bone-inducing growth factors and materials embedded in a PDMS-based µF (Torisawa et al., 2016, 2014). The resulting bone marrow µFs contain cells that express hematopoietic genes and key hematopoietic niche cells. Additionally, the population of blood cells increases gradually for up to 10 days of in vitro culture, suggesting that the bone-marrow chip is capable of hematopoiesis. Recently, work using hPSCs to generate hemogenic endothelium has enabled the generation of a µF model of the human dorsal aorta, from which hematopoietic stem cells are first produced (Lundin et al., 2020). Under fluid shear stress and cyclic strain, the cells increase expression of the hematopoietic marker RUNX1. The dynamic tissue culture conditions within this µF provide a great example of how fluid shear stress and cyclic mechanical strain can regulate distinct cellular responses to affect tissue development and function.
The reproductive system
Spermatogenesis
Reproduction is the process by which precise patterning and coordination between cells, tissues and organs produce viable offspring. In males, the reproductive organs function to produce viable sperm in a process known as spermatogenesis (reviewed by Griswold, 2016). Early attempts to model rat and human spermatogenesis involved 3D ex vivo culture of testicular tissues on a suspension system that was partially immersed in a medium to facilitate nutrient delivery and gas exchange (Steinberger, 1967). However, maintenance of such ex vivo cultures is limited by the lack of a microvascular system, which is crucial for tissue homeostasis. To overcome this challenge, neonatal mouse testis tissues cultured in a µF consisting of a tissue chamber and a fluidic channel for medium perfusion (Fig. 6E) allows tissue maturation and sustained spermatogenesis for up to 6 months (Komeya et al., 2016). The resulting sperm can fertilize an egg (through micro-insemination) and produce offspring. Recently, 3D bioprinted µFs consisting of human testicular cells have been used to create a biomimetic spermatogenic niche (Robinson et al., 2021 preprint). Although this system does not produce spermatozoa within the examined culture period, there is a significant expression of genes involved in self-renewal, differentiation and spermiogenesis. This system successfully mimicked the in vivo cytoarchitecture of testicular cells, but it lacked the in vivo complexity of peritubular and interstitial cell placements. This could be improved in the future by introducing additional printing nozzles to facilitate compartmental printing and interfacing the bioprinted tissues with a perfusable µF channel(s) to deliver morphogens and further pattern the printed structures. Together, these studies indicate that µFs can extend the capabilities of in vitro tissue culture platforms to study the biology of male reproductive tissues.
Oogenesis and the menstrual cycle
Immature eggs are produced in the ovarian follicle where they are stored and matured through hormonal stimulation, followed by release into the fallopian tubes for fertilization or removal from the body (reviewed by Richards et al., 1998). The development of the ovarian follicle (folliculogenesis) has been modeled in µFs using non-planar fluid flow to encapsulate early murine follicles in a soft collagen gel core surrounded by a hard alginate shell to mimic the in vivo tissue environment (Choi et al., 2014). Once the cultured follicles mature to the antral stage (characterized by a fluid-filled cavity), they undergo ovulation in vitro without additional exogenous hormonal stimulation. During ovulation, the oocyte is released from the ovary and then passes into the fallopian tube where it is exposed to biochemical and biophysical stimuli that impact the early stages of embryogenesis. To model the fallopian tube environment in vitro, a µF has been developed that consists of primary bovine oviduct epithelial cells cultured under fluid flow (Ferraz et al., 2018). This system is responsive to cycling hormones (e.g. progesterone and estrogen), exhibits enhanced cell differentiation under fluid flow, and is capable of facilitating fertilization in vitro. After oocytes leave the fallopian tubes, they reach the uterus where they either implant into the endometrium or are shed with the endometrial lining during menstruation. These processes have also been modeled in µFs using human and murine tissues (Gnecco et al., 2017; Xiao et al., 2017). Modeling of the female reproductive tract and hormonal profile of a 28-day human menstrual cycle has been achieved by linking together several organ-on-chip modules, including µFs of the ovaries, fallopian tubes, uterus and cervix (Fig. 6F) (Xiao et al., 2017). By controlling the levels of follicle-stimulating hormone and human chorionic gonadotropin (hCG), hormonal profiles that resemble those observed during a 28-day menstrual cycle are reproduced. Intriguingly, interconnecting the different µFs in sequence increases cell viability, ciliary activity, proliferation and secretory function over prolonged culture in vitro. Additionally, the engineered in vitro model of the fallopian tube mimics pregnancy-like progesterone secretion when stimulated with exogenous hCG and can sustain the corpus luteum for 14 days after ovulation. Taken together, these studies provide compelling evidence for the utility of µFs in understanding the development and functions of the female reproductive organs, providing opportunities to investigate reproductive health and disorders ex vivo.
Kidneys
The functional kidneys develop from the primary ureteric bud, which is a derivative of the Wolffian duct (Michos, 2009). By 36 weeks of gestation in humans, most nephrons (functional unit of the kidneys) are formed (Faa et al., 2012). Several µFs have been established to model the development and functions of nephron components, such as the glomerulus and proximal tubule. For example, µFs have been used to induce the differentiation of hPSCs into podocytes (glomerular epithelial cells) to reconstitute the structure and molecular filtration function of the kidney's glomerulus (Fig. 6G) (Musah et al., 2017, 2018). Intriguingly, modeling the stretch and relaxation motions observed in glomerular capillaries in vivo has revealed a role for mechanical strain on the development and maturation of kidney cells, which is not possible to model in traditional tissue culture systems. This earlier work inspired the generation of a personalized µF of the human kidney glomerulus for which the epithelial (podocyte) and endothelial (vascular) layers are engineered from a specific patient's hPSCs, which also recapitulate drug-induced nephropathy in vitro (Roye et al., 2021). The establishment of personalized models of µFs could help advance mechanistic studies of disease and facilitate precision medicine applications. A layer of basement membrane proteins separates the podocyte and endothelial tissues of the glomerular filtration barrier; therefore, µFs that recapitulate the selective filtration of molecules from the vascular to the urinary compartments of the kidneys employ engineered membranes to separate the fluidic channels representing each of these compartments. Some of these engineered membranes are thicker than the glomerular basement membrane in vivo; thus, future studies that employ thinner and biodegradable materials could be useful for kidney tissue engineering. Although this is yet to be accomplished, a µF of the glomerulus lacking an engineered filtration barrier has been established (Petrosyan et al., 2019); however, the lack of dedicated fluidic compartments limits its utility for studying the selective filtration of molecules from the blood and the analysis of urinary filtrate. A µF of proximal tubules (Fig. 6G) has demonstrated the importance of fluid shear stress in mimicking physiological functions of the kidney's proximal tubule epithelium (Jang et al., 2013). The transport function (or receptor-mediated endocytosis) of these cells is enhanced by fluid flow or shear stress compared with cells propagated under static culture conditions. Although kidney organoids typically exhibit immature, fetal-like characteristics, modulation of fluid shear stress in a 3D-printed µF can improve the vascularization of stem cell-derived kidney organoids (Homan et al., 2019). However, recapitulation of complete nephron structure and function using µFs is yet to be demonstrated. In the future, stem cell-derived kidney cells and organoids could enable the generation of complex tissues with multiple interconnected functional units, thus improving the utility of current organoids and µFs for modeling organ-level functionalities.
Nervous system
Brain
Development of the brain is a prolonged process that begins with neurulation around 2 weeks after conception and continues into adulthood (Tierney and Nelson, 2009). Brain development has been extensively studied by applying brain organoid techniques with μFs. Sur and colleagues have engineered a microfluidic bioreactor coupled with an imaging chamber for culturing and in situ monitoring of brain organoids (Khan et al., 2021). The system allows for long-term tracking of brain organoid growth, self-organization and changes in cell morphology. hPSC-derived embryoid bodies have also been induced into brain organoids using μFs (Fig. 6H) with continuous fluid flow, and the resulting brain organoids exhibit in vivo-like developmental processes (Wang et al., 2018). The development of brain organoids in μFs has been further enhanced by the incorporation of hydrogel containing native human brain extracellular matrix (BEM) components; the BEM provides the hPSC-derived embryoid bodies with environmental cues that mimics the in vivo environment, thus facilitating neurogenesis and formation of brain organoids with improved structural and functional features (Cho et al., 2021). Despite these significant advancements, brain organoids are limited by their size, shape, tissue organization and lack of vascularization. Future optimizations of the μF design and differentiation protocols to provide the cells with more physiologically relevant mechanical and molecular cues will further advance the development of brain organoids to help study human brain development and diseases (Yu et al., 2019).
The neurovascular unit and blood-brain barrier
The neurovascular unit (NVU) represents the structural and functional relationship between the brain and blood vessels at the cellular level. The blood-brain barrier (BBB) forms an interface between the blood and brain tissue and it functions by regulating the transport of ions, molecules and cells between these compartments, thereby protecting the brain from potential toxins and pathogens in circulation (Daneman and Prat, 2015; Rhea and Banks, 2019). Sophisticated µFs that closely recapitulate the structure of the NVU have provided more insight into how the cellular interface affects its development and function. For example, Brewer and colleagues have engineered a µF containing two chambers separated by a thin, porous membrane representing the blood and the brain compartments (Brown et al., 2015). The device mimics BBB barrier structure and function as demonstrated by the presence of tight junctions, as well as time-dependent active transport of ascorbate to the brain compartment of the µF. Mannix and colleagues have engineered a µF that contains three types of individual chips to model different flow compartments of the BBB, and the chips were connected in accordance with the direction of fluid flow in vivo (Fig. 6H) (Maoz et al., 2018). The authors show that fluidic coupling of the µFs results in significant phenotypic and functional change of cells in the system, providing insight into pathways that are involved in metabolic coupling and crosstalk between the BBB and neurons. Despite significant advancement in the understanding of the NVU in adult brains, much remains unknown regarding its development (Bell et al., 2020). A 3D µF that supports the differentiation of neural stem cells into neurons has been developed by Sudo and colleagues (Uwamori et al., 2017), which successfully models neurogenesis and angiogenesis. By co-culturing neural stem cells, human brain microvascular endothelial cells and MSCs in the µF, they generate 3D neurovascular tissue. However, in this study, the authors use genetically heterogeneous cells derived and pooled from multiple sources. Given the capacity of induced pluripotent stem cells to differentiate into almost any cell type, it would be interesting to use cells from a single source in future, which could better recapitulate developmental mechanisms of the NVU at the patient-specific level.
Conclusions
The establishment of in vitro models has greatly enhanced the ability of scientists and engineers to recapitulate and illuminate the mechanisms of human tissue development. However, traditional tissue culture methods often lack physiologically relevant features, such as fluid or blood flow, mechanical strain, and matrix elasticities, necessary for recapitulating organ development and function (Daems et al., 2020). Although current µF technologies do not produce biomimetic models of whole organs, they can provide insight into the development and function of specific tissues and functional subunits of human organs (Ingber, 2020). µFs come in a variety of forms equipped with multiple capabilities and provide opportunities to study the effects of multiple stimuli on tissue development. µFs also offer a more accessible and reproducible format for studying human cellular and tissue organization in vitro. Recent advancements in µF manufacturing methods will enhance the accessibility and utility of this platform for modeling developmental and physiological processes (Box 1). Combining µFs with other tissue culture techniques (e.g. organoids) could enable the derivation of developmentally specialized and functional tissues (Park et al., 2019). For example, co-culturing gastruloids with ectodermal progenitor cells could yield a more holistic embryo-like model and culturing these gastruloids in perfusable µFs could provide adequate oxygen and nutrients needed to induce vascularization (Rossi et al., 2021). µFs can also be interconnected or fluidically linked to create large-scale models of body systems or human body-on-a-chip (Novak et al., 2020; Xiao et al., 2017; Zhang et al., 2009). Such complex µFs could be useful for studying developmentally regulated events in inter-organ communication, disease pathogenesis and co-morbidities. For example, linking a liver and brain chip could facilitate the investigation of how liver cirrhosis and failure can lead to intracranial swelling (Schwendimann and Minagar, 2017). In summary, µFs represent an emerging and powerful technology that is transforming the studies of human development ex vivo and advancing our current understanding of cellular, molecular and physiological processes.
Box 1. Methodological improvements to µFs for biological application.
The technical expertise required for the design, manufacturing and handling of µFs limits the level of complexity researchers can build into the system. However, recent advancements in manufacturing processes have provided viable options for improving µFs for the study of development. For example, light-based 3D-printed hydrogels provide a transparent platform capable of producing intertwined perfusion channels with integrated fluid mixing (Benjamin et al., 2019; Grigoryan et al., 2019). Additionally, the incorporation of biomimetic materials, such as electrospun extracellular matrices, can provide physiologically relevant membranes and substrates as opposed to the traditionally used PDMS membranes (Barlian et al., 2020; Wang et al., 2016). For µFs that utilize bioprinting, the development of bioinks with minimal toxicity to cells and coupled with coaxial extrusion nozzles can facilitate the production of multiple constructs that can be crosslinked during printing to engineer multiple subunits of tissues and organs for advanced tissue modeling (Davoodi et al., 2020; Kjar et al., 2021). The inclusion of biosensors within µFs can provide real-time data acquisition and monitoring to help address a variety of questions related to tissue development and function. For example, incorporating oxygen-sensing microprobes within µFs has provided metabolic readouts for the onset of cell damage or shifts in energy production (Cohen et al., 2021; Ehrlich et al., 2018; Lee et al., 2020). Additionally, these biosensors can be printed or integrated into the µFs, which can help minimize invasiveness or tissue destruction often observed in platforms that require the use of external probes for live-cell readouts (Jeong et al., 2015; Loo et al., 2019). Beyond humans, µFs are amenable to culturing embryos of other species to study their development (reviewed by Hwang and Lu, 2013; Sonnen and Merten, 2019). These applications provide powerful opportunities for parallel and high-throughput studies of phenotypic and genetic changes during the development of different organisms, providing insights into conserved and divergent processes across species.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Funding
The authors were supported by the Whitehead Foundation, the National Institutes of Health (T32GM800555) and the International Foundation for Ethical Research. Deposited in PMC for release after 12 months.
References
- Akbari, E., Spychalski, G. B. and Song, J. W. (2017). Microfluidic approaches to the study of angiogenesis and the microcirculation. Microcirculation 24, 1-8. 10.1111/micc.12363 [DOI] [PubMed] [Google Scholar]
- Bahmaee, H., Owen, R., Boyle, L., Perrault, C. M., Garcia-Granada, A. A., Reilly, G. C. and Claeyssens, F. (2020). Design and evaluation of an osteogenesis-on-a-chip microfluidic device incorporating 3D cell culture. Front. Bioeng. Biotechnol. 8, 1042. 10.3389/fbioe.2020.557111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlian, A., Judawisastra, H., Ridwan, A., Wahyuni, A. R. and Lingga, M. E. (2020). Chondrogenic differentiation of Wharton's Jelly mesenchymal stem cells on silk spidroin-fibroin mix scaffold supplemented with L-ascorbic acid and platelet rich plasma. Sci. Rep. 10, 19449. 10.1038/s41598-020-76466-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, A. H., Miller, S. L., Castillo-Melendez, M. and Malhotra, A. (2020). The neurovascular unit: effects of brain insults during the perinatal period. Front. Neurosci. 13, 1452. 10.3389/fnins.2019.01452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin, A. D., Abbasi, R., Owens, M., Olsen, R. J., Walsh, D. J., LeFevre, T. B. and Wilking, J. N. (2019). Light-based 3D printing of hydrogels with high-resolution channels. Biomed. Phys. Eng. Exp. 5, 025035. 10.1088/2057-1976/aad667 [DOI] [Google Scholar]
- Bhattacharjee, N., Urrios, A., Kang, S. and Folch, A. (2016). The upcoming 3D-printing revolution in microfluidics. Lab. Chip 16, 1720-1742. 10.1039/C6LC00163G [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blundell, C., Tess, E. R., Schanzer, A. S., Coutifaris, C., Su, E. J., Parry, S. and Huh, D. (2016). A microphysiological model of the human placental barrier. Lab. Chip 16, 3065-3073. 10.1039/C6LC00259E [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brassard, J. A., Nikolaev, M., Hubscher, T., Hofer, M. and Lutolf, M. P. (2021). Recapitulating macro-scale tissue self-organization through organoid bioprinting. Nat. Mater. 20, 22-29. 10.1038/s41563-020-00803-5 [DOI] [PubMed] [Google Scholar]
- Breeland, G., Sinkler, M. A. and Menezes, R. G. (2020). Embryology, bone ossification. StatPearls [Internet]. StatPearls Publishing. [PubMed] [Google Scholar]
- Briggs, J. A., Weinreb, C., Wagner, D. E., Megason, S., Peshkin, L., Kirschner, M. W. and Klein, A. M. (2018). The dynamics of gene expression in vertebrate embryogenesis at single-cell resolution. Science 360, eaar5780. 10.1126/science.aar5780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broccoli, V., Boncinelli, E. and Wurst, W. (1999). The caudal limit of Otx2 expression positions the isthmic organizer. Nature 401, 164-168. 10.1038/43670 [DOI] [PubMed] [Google Scholar]
- Brown, J. A., Pensabene, V., Markov, D. A., Allwardt, V., Neely, M. D., Shi, M., Britt, C. M., Hoilett, O. S., Yang, Q. and Brewer, B. M. (2015). Recreating blood-brain barrier physiology and structure on chip: a novel neurovascular microfluidic bioreactor. Biomicrofluidics 9, 054124. 10.1063/1.4934713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho, A. N., Jin, Y., An, Y., Kim, J., Choi, Y. S., Lee, J. S., Kim, J., Choi, W. Y., Koo, D. J., Yu, W.et al. (2021). Microfluidic device with brain extracellular matrix promotes structural and functional maturation of human brain organoids. Nat. Commun. 12, 4730. 10.1038/s41467-021-24775-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, J. K., Agarwal, P., Huang, H., Zhao, S. and He, X. (2014). The crucial role of mechanical heterogeneity in regulating follicle development and ovulation with engineered ovarian microtissue. Biomaterials 35, 5122-5128. 10.1016/j.biomaterials.2014.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuchuy, J., Rogal, J., Ngo, T., Stadelmann, K., Antkowiak, L., Achberger, K., Liebau, S., Schenke-Layland, K. and Loskill, P. (2021). Integration of electrospun membranes into low-absorption thermoplastic organ-on-chip. ACS Biomater. Sci. Eng. 7, 3006-3017. 10.1021/acsbiomaterials.0c01062 [DOI] [PubMed] [Google Scholar]
- Cimetta, E., Sirabella, D., Yeager, K., Davidson, K., Simon, J., Moon, R. T. and Vunjak-Novakovic, G. (2013). Microfluidic bioreactor for dynamic regulation of early mesodermal commitment in human pluripotent stem cells. Lab. Chip 13, 355-364. 10.1039/C2LC40836H [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, A., Ioannidis, K., Ehrlich, A., Regenbaum, S., Cohen, M., Ayyash, M., Tikva, S. S. and Nahmias, Y. (2021). Mechanism and reversal of drug-induced nephrotoxicity on a chip. Sci. Transl. Med. 13, eabd6299. 10.1126/scitranslmed.abd6299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa, L., Reis, R. L., Silva-Correia, J. and Oliveira, J. M. (2020). Microfluidics for angiogenesis research. Adv. Exp. Med. Biol. 1230, 97-119. 10.1007/978-3-030-36588-2_7 [DOI] [PubMed] [Google Scholar]
- Cui, K. W., Engel, L., Dundes, C. E., Nguyen, T. C., Loh, K. M. and Dunn, A. R. (2020). Spatially controlled stem cell differentiation via morphogen gradients: a comparison of static and dynamic microfluidic platforms. J. Vac. Sci. Technol. A 38, 033205. 10.1116/1.5142012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daems, M., Peacock, H. M. and Jones, E. A. V. (2020). Fluid flow as a driver of embryonic morphogenesis. Development 147, dev185579. [DOI] [PubMed] [Google Scholar]
- Daley, G. Q., Hyun, I., Apperley, J. F., Barker, R. A., Benvenisty, N., Bredenoord, A. L., Breuer, C. K., Caulfield, T., Cedars, M. I., Frey-Vasconcells, J.et al. (2016). Setting global standards for stem cell research and clinical translation: the 2016 ISSCR Guidelines. Stem Cell Reports 6, 787-797. 10.1016/j.stemcr.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daneman, R. and Prat, A. (2015). The blood–brain barrier. Cold Spring Harbor Perspect. Biol. 7, a020412. 10.1101/cshperspect.a020412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davoodi, E., Sarikhani, E., Montazerian, H., Ahadian, S., Costantini, M., Swieszkowski, W., Willerth, S., Walus, K., Mofidfar, M., Toyserkani, E.et al. (2020). Extrusion and microfluidic-based bioprinting to fabricate biomimetic tissues and organs. Adv. Mater. Technol. 5, 1901044. 10.1002/admt.201901044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimitriou, R., Jones, E., McGonagle, D. and Giannoudis, P. V. (2011). Bone regeneration: current concepts and future directions. BMC Med. 9, 1-10. 10.1186/1741-7015-9-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy, D. C., McDonald, J. C., Schueller, O. J. and Whitesides, G. M. (1998). Rapid prototyping of microfluidic systems in poly(dimethylsiloxane). Anal. Chem. 70, 4974-4984. 10.1021/ac980656z [DOI] [PubMed] [Google Scholar]
- Ehrlich, A., Tsytkin-Kirschenzweig, S., Ioannidis, K., Ayyash, M., Riu, A., Note, R., Ouedraogo, G., Vanfleteren, J., Cohen, M. and Nahmias, Y. (2018). Microphysiological flux balance platform unravels the dynamics of drug induced steatosis. Lab. Chip 18, 2510-2522. 10.1039/C8LC00357B [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einhorn, T. A. (1998). The cell and molecular biology of fracture healing. Clin. Orthop. Relat. Res. 355, S7-S21. 10.1097/00003086-199810001-00003 [DOI] [PubMed] [Google Scholar]
- Faa, G., Gerosa, C., Fanni, D., Monga, G., Zaffanello, M., Van Eyken, P. and Fanos, V. (2012). Morphogenesis and molecular mechanisms involved in human kidney development. J. Cell. Physiol. 227, 1257-1268. 10.1002/jcp.22985 [DOI] [PubMed] [Google Scholar]
- Ferraz, M., Rho, H. S., Hemerich, D., Henning, H. H. W., van Tol, H. T. A., Holker, M., Besenfelder, U., Mokry, M., Vos, P., Stout, T. A. E.et al. (2018). An oviduct-on-a-chip provides an enhanced in vitro environment for zygote genome reprogramming. Nat. Commun. 9, 4934. 10.1038/s41467-018-07119-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry, R. C., Bangma, J., Szilagyi, J. and Rager, J. E. (2019). Developing novel in vitro methods for the risk assessment of developmental and placental toxicants in the environment. Toxicol. Appl. Pharmacol. 378, 114635. 10.1016/j.taap.2019.114635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giridharan, G. A., Nguyen, M. D., Estrada, R., Parichehreh, V., Hamid, T., Ismahil, M. A., Prabhu, S. D. and Sethu, P. (2010). Microfluidic cardiac cell culture model (muCCCM). Anal. Chem. 82, 7581-7587. 10.1021/ac1012893 [DOI] [PubMed] [Google Scholar]
- Gkatzis, K., Taghizadeh, S., Huh, D., Stainier, D. Y. R. and Bellusci, S. (2018). Use of three-dimensional organoids and lung-on-a-chip methods to study lung development, regeneration and disease. Eur. Respir. J. 52, 1800876. 10.1183/13993003.00876-2018 [DOI] [PubMed] [Google Scholar]
- Gnecco, J. S., Pensabene, V., Li, D. J., Ding, T., Hui, E. E., Bruner-Tran, K. L. and Osteen, K. G. (2017). Compartmentalized culture of perivascular stroma and endothelial cells in a microfluidic model of the human endometrium. Ann. Biomed. Eng. 45, 1758-1769. 10.1007/s10439-017-1797-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoryan, B., Paulsen, S. J., Corbett, D. C., Sazer, D. W., Fortin, C. L., Zaita, A. J., Greenfield, P. T., Calafat, N. J., Gounley, J. P., Ta, A. H.et al. (2019). Multivascular networks and functional intravascular topologies within biocompatible hydrogels. Science 364, 458-464. 10.1126/science.aav9750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griswold, M. D. (2016). Spermatogenesis: the commitment to meiosis. Physiol. Rev. 96, 1-17. 10.1152/physrev.00013.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosberg, A., Alford, P. W., McCain, M. L. and Parker, K. K. (2011). Ensembles of engineered cardiac tissues for physiological and pharmacological study: heart on a chip. Lab. Chip 11, 4165-4173. 10.1039/c1lc20557a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashemzadeh, H., Allahverdi, A., Ghorbani, M., Soleymani, H., Kocsis, Á., Fischer, M. B., Ertl, P. and Naderi-Manesh, H. (2020). Gold nanowires/fibrin nanostructure as microfluidics platforms for enhancing stem cell differentiation: Bio-AFM study. Micromachines 11, 50. 10.3390/mi11010050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashimoto, S., Kato, N., Saeki, K. and Morimoto, Y. (2012). Selection of high-potential embryos by culture in poly(dimethylsiloxane) microwells and time-lapse imaging. Fertil. Steril. 97, 332-337. 10.1016/j.fertnstert.2011.11.042 [DOI] [PubMed] [Google Scholar]
- Hayward, M.-K., Muncie, J. M. and Weaver, V. M. (2021). Tissue mechanics in stem cell fate, development, and cancer. Dev. Cell 56, 1833-1847. 10.1016/j.devcel.2021.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, C. M., Ng, S. H., Li, K. H. and Yoon, Y. J. (2015). 3D printed microfluidics for biological applications. Lab. Chip 15, 3627-3637. 10.1039/C5LC00685F [DOI] [PubMed] [Google Scholar]
- Hofbauer, P., Jahnel, S. M., Papai, N., Giesshammer, M., Deyett, A., Schmidt, C., Penc, M., Tavernini, K., Grdseloff, N., Meledeth, C.et al. (2021). Cardioids reveal self-organizing principles of human cardiogenesis. Cell 184, 3299-3317. 10.1016/j.cell.2021.04.034 [DOI] [PubMed] [Google Scholar]
- Hofer, M. and Lutolf, M. P. (2021). Engineering organoids. Nat. Rev. Mater. 6, 402-420. 10.1038/s41578-021-00279-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan, K. A., Gupta, N., Kroll, K. T., Kolesky, D. B., Skylar-Scott, M., Miyoshi, T., Mau, D., Valerius, M. T., Ferrante, T., Bonventre, J. V.et al. (2019). Flow-enhanced vascularization and maturation of kidney organoids in vitro. Nat. Methods 16, 255-262. 10.1038/s41592-019-0325-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber, D., Oskooei, A., Casadevall, I. S. X.Andrew, d. and Kaigala, G. V. (2018). Hydrodynamics in cell studies. Chem. Rev. 118, 2042-2079. 10.1021/acs.chemrev.7b00317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh, D., Fujioka, H., Tung, Y. C., Futai, N., Paine, R., III, Grotberg, J. B. and Takayama, S. (2007). Acoustically detectable cellular-level lung injury induced by fluid mechanical stresses in microfluidic airway systems. Proc. Natl. Acad. Sci. USA 104, 18886-18891. 10.1073/pnas.0610868104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh, D., Matthews, B. D., Mammoto, A., Montoya-Zavala, M., Hsin, H. Y. and Ingber, D. E. (2010). Reconstituting organ-level lung functions on a chip. Science 328, 1662-1668. 10.1126/science.1188302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter, S., Grode, K., Schwab, A. and Knudsen, T. (2018). Recapitulating human endocardial cushion morphogenesis with organotypic culture models and microfluidics. Birth Defects Res. 110, 715-743. [Google Scholar]
- Hwang, H. and Lu, H. (2013). Microfluidic tools for developmental studies of small model organisms--nematodes, fruit flies, and zebrafish. Biotechnol. J. 8, 192-205. 10.1002/biot.201200129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingber, D. E. (2020). Is it time for reviewer 3 to request human organ chip experiments instead of animal validation studies? Adv. Sci. (Weinh) 7, 2002030. 10.1002/advs.202002030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagannathan-Bogdan, M. and Zon, L. I. (2013). Hematopoiesis. Development 140, 2463-2467. 10.1242/dev.083147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain, A., Barrile, R., van der Meer, A. D., Mammoto, A., Mammoto, T., De Ceunynck, K., Aisiku, O., Otieno, M. A., Louden, C. S., Hamilton, G. A.et al. (2018). Primary human lung alveolus-on-a-chip model of intravascular thrombosis for assessment of therapeutics. Clin. Pharmacol. Ther. 103, 332-340. 10.1002/cpt.742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang, K. J., Mehr, A. P., Hamilton, G. A., McPartlin, L. A., Chung, S., Suh, K. Y. and Ingber, D. E. (2013). Human kidney proximal tubule-on-a-chip for drug transport and nephrotoxicity assessment. Integr. Biol. (Camb) 5, 1119-1129. 10.1039/c3ib40049b [DOI] [PubMed] [Google Scholar]
- Jeong, J. W., McCall, J. G., Shin, G., Zhang, Y., Al-Hasani, R., Kim, M., Li, S., Sim, J. Y., Jang, K. I., Shi, Y.et al. (2015). Wireless optofluidic systems for programmable in vivo pharmacology and optogenetics. Cell 162, 662-674. 10.1016/j.cell.2015.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan, I., Prabhakar, A., Delepine, C., Tsang, H., Pham, V. and Sur, M. (2021). A low-cost 3D printed microfluidic bioreactor and imaging chamber for live-organoid imaging. Biomicrofluidics 15, 024105. 10.1063/5.0041027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecker, C. and Lumsden, A. (2005). Compartments and their boundaries in vertebrate brain development. Nat. Rev. Neurosci. 6, 553-564. 10.1038/nrn1702 [DOI] [PubMed] [Google Scholar]
- Kieslinger, D. C., Hao, Z., Vergouw, C. G., Kostelijk, E. H., Lambalk, C. B. and Le Gac, S. (2015). In vitro development of donated frozen-thawed human embryos in a prototype static microfluidic device: a randomized controlled trial. Fertil. Steril. 103, 680-686. 10.1016/j.fertnstert.2014.12.089 [DOI] [PubMed] [Google Scholar]
- Kim, H. J., Huh, D., Hamilton, G. and Ingber, D. E. (2012). Human gut-on-a-chip inhabited by microbial flora that experiences intestinal peristalsis-like motions and flow. Lab. Chip 12, 2165-2174. 10.1039/c2lc40074j [DOI] [PubMed] [Google Scholar]
- King, K. R., Wang, C. C. J., Kaazempur-Mofrad, M. R., Vacanti, J. P. and Borenstein, J. T. (2004). Biodegradable Microfluidics. Adv. Mater. 16, 2007-2012. 10.1002/adma.200306522 [DOI] [Google Scholar]
- Kjar, A., McFarland, B., Mecham, K., Harward, N. and Huang, Y. (2021). Engineering of tissue constructs using coaxial bioprinting. Bioact. Mater. 6, 460-471. 10.1016/j.bioactmat.2020.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, A. M., Mazutis, L., Akartuna, I., Tallapragada, N., Veres, A., Li, V., Peshkin, L., Weitz, D. A. and Kirschner, M. W. (2015). Droplet barcoding for single-cell transcriptomics applied to embryonic stem cells. Cell 161, 1187-1201. 10.1016/j.cell.2015.04.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komeya, M., Kimura, H., Nakamura, H., Yokonishi, T., Sato, T., Kojima, K., Hayashi, K., Katagiri, K., Yamanaka, H., Sanjo, H.et al. (2016). Long-term ex vivo maintenance of testis tissues producing fertile sperm in a microfluidic device. Sci. Rep. 6, 21472. 10.1038/srep21472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krisher, R. L. and Wheeler, M. B. (2010). Towards the use of microfluidics for individual embryo culture. Reprod. Fertil. Dev. 22, 32-39. 10.1071/RD09219 [DOI] [PubMed] [Google Scholar]
- Lee, J., Abdeen, A. A., Huang, T. H. and Kilian, K. A. (2014a). Controlling cell geometry on substrates of variable stiffness can tune the degree of osteogenesis in human mesenchymal stem cells. J. Mech. Behav. Biomed. Mater. 38, 209-218. 10.1016/j.jmbbm.2014.01.009 [DOI] [PubMed] [Google Scholar]
- Lee, V. K., Lanzi, A. M., Haygan, N., Yoo, S. S., Vincent, P. A. and Dai, G. (2014b). Generation of multi-scale vascular network system within 3d hydrogel using 3D bio-printing technology. Cell Mol. Bioeng. 7, 460-472. 10.1007/s12195-014-0340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. S., Romero, R., Han, Y. M., Kim, H. C., Kim, C. J., Hong, J. S. and Huh, D. (2016). Placenta-on-a-chip: a novel platform to study the biology of the human placenta. J. Matern. Fetal. Neonatal. Med. 29, 1046-1054. 10.3109/14767058.2015.1038518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, M. S., Hsu, W., Huang, H. Y., Tseng, H. Y., Lee, C. T., Hsu, C. Y., Shieh, Y. C., Wang, S. H., Yao, D. J. and Liu, C. H. (2020). Simultaneous detection of two growth factors from human single-embryo culture medium by a bead-based digital microfluidic chip. Biosens. Bioelectron. 150, 111851. 10.1016/j.bios.2019.111851 [DOI] [PubMed] [Google Scholar]
- Li, S., Huang, N. F. and Hsu, S. (2005). Mechanotransduction in endothelial cell migration. J. Cell. Biochem. 96, 1110-1126. 10.1002/jcb.20614 [DOI] [PubMed] [Google Scholar]
- Loh, K. M., van Amerongen, R. and Nusse, R. (2016). Generating cellular diversity and spatial form: Wnt signaling and the evolution of multicellular animals. Dev. Cell 38, 643-655. 10.1016/j.devcel.2016.08.011 [DOI] [PubMed] [Google Scholar]
- Lohasz, C., Frey, O., Bonanini, F., Renggli, K. and Hierlemann, A. (2019). Tubing-free microfluidic microtissue culture system featuring gradual, in vivo-like substance exposure profiles. Fron.t Bioeng. Biotechnol. 7, 72. 10.3389/fbioe.2019.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo, J. F. C., Ho, A. H. P., Turner, A. P. F. and Mak, W. C. (2019). Integrated printed microfluidic biosensors. Trends Biotechnol. 37, 1104-1120. 10.1016/j.tibtech.2019.03.009 [DOI] [PubMed] [Google Scholar]
- Low, L. A. and Tagle, D. A. (2017). Organs-on-chips: progress, challenges, and future directions. Exp. Biol. Med. (Maywood) 242, 1573-1578. 10.1177/1535370217700523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundin, V., Sugden, W. W., Theodore, L. N., Sousa, P. M., Han, A., Chou, S., Wrighton, P. J., Cox, A. G., Ingber, D. E. and Goessling, W. (2020). YAP regulates hematopoietic stem cell formation in response to the biomechanical forces of blood flow. Dev. Cell 52, 446-460. 10.1016/j.devcel.2020.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma, J., Sanchez-Duffhues, G., Goumans, M. J. and Ten Dijke, P. (2020). TGF-beta-induced endothelial to mesenchymal transition in disease and tissue engineering. Front. Cell Dev. Biol. 8, 260. 10.3389/fcell.2020.00260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfrin, A., Tabata, Y., Paquet, E. R., Vuaridel, A. R., Rivest, F. R., Naef, F. and Lutolf, M. P. (2019). Engineered signaling centers for the spatially controlled patterning of human pluripotent stem cells. Nat. Methods 16, 640-648. 10.1038/s41592-019-0455-2 [DOI] [PubMed] [Google Scholar]
- Maoz, B. M., Herland, A., FitzGerald, E. A., Grevesse, T., Vidoudez, C., Pacheco, A. R., Sheehy, S. P., Park, T.-E., Dauth, S. and Mannix, R. (2018). A linked organ-on-chip model of the human neurovascular unit reveals the metabolic coupling of endothelial and neuronal cells. Nat. Biotechnol. 36, 865-874. 10.1038/nbt.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michos, O. (2009). Kidney development: from ureteric bud formation to branching morphogenesis. Curr. Opin. Genet. Dev. 19, 484-490. 10.1016/j.gde.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, J. S., Stevens, K. R., Yang, M. T., Baker, B. M., Nguyen, D. H., Cohen, D. M., Toro, E., Chen, A. A., Galie, P. A., Yu, X.et al. (2012). Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat. Mater. 11, 768-774. 10.1038/nmat3357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musah, S., Mammoto, A., Ferrante, T. C., Jeanty, S. S. F., Hirano-Kobayashi, M., Mammoto, T., Roberts, K., Chung, S., Novak, R., Ingram, M.et al. (2017). Mature induced-pluripotent-stem-cell-derived human podocytes reconstitute kidney glomerular-capillary-wall function on a chip. Nat. Biomed. Eng. 1, 0069. 10.1038/s41551-017-0069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musah, S., Dimitrakakis, N., Camacho, D. M., Church, G. M. and Ingber, D. E. (2018). Directed differentiation of human induced pluripotent stem cells into mature kidney podocytes and establishment of a Glomerulus Chip. Nat. Protoc. 13, 1662-1685. 10.1038/s41596-018-0007-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naskar, S., Panda, A. K., Kumaran, V., Mehta, B. and Basu, B. (2018). Controlled shear flow directs osteogenesis on UHMWPE-based hybrid nanobiocomposites in a custom-designed PMMA microfluidic device. ACS Applied Bio Materials 1, 414-435. 10.1021/acsabm.8b00147 [DOI] [PubMed] [Google Scholar]
- Nelson, C. M., Gleghorn, J. P., Pang, M. F., Jaslove, J. M., Goodwin, K., Varner, V. D., Miller, E., Radisky, D. C. and Stone, H. A. (2017). Microfluidic chest cavities reveal that transmural pressure controls the rate of lung development. Development 144, 4328-4335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak, R., Ingram, M., Marquez, S., Das, D., Delahanty, A., Herland, A., Maoz, B. M., Jeanty, S. S. F., Somayaji, M. R., Burt, M.et al. (2020). Robotic fluidic coupling and interrogation of multiple vascularized organ chips. Nat. Biomed. Eng. 4, 407-420. 10.1038/s41551-019-0497-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Rahilly, R. and Muller, F. (1994). Neurulation in the normal human embryo. Ciba Found. Symp. 181, 70-82; discussion 82-79. 10.1002/9780470514559.ch5 [DOI] [PubMed] [Google Scholar]
- Ozbolat, V., Dey, M., Ayan, B., Povilianskas, A., Demirel, M. C. and Ozbolat, I. T. (2018). 3D printing of PDMS improves its mechanical and cell adhesion properties. ACS Biomater. Sci. Eng. 4, 682-693. 10.1021/acsbiomaterials.7b00646 [DOI] [PubMed] [Google Scholar]
- Pan, H., Deutsch, G. H. and Wert, S. E., Ontology Subcommittee and NHLBI Molecular Atlas of Lung Development Program Consortium (2019). Comprehensive anatomic ontologies for lung development: a comparison of alveolar formation and maturation within mouse and human lung. J. Biomed. Semantics 10, 18. 10.1186/s13326-019-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paria, B. C. and Dey, S. K. (1990). Preimplantation embryo development in vitro: cooperative interactions among embryos and role of growth factors. Proc. Natl. Acad. Sci. USA 87, 4756-4760. 10.1073/pnas.87.12.4756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, S. E., Georgescu, A. and Huh, D. (2019). Organoids-on-a-chip. Science 364, 960-965. 10.1126/science.aaw7894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrosyan, A., Cravedi, P., Villani, V., Angeletti, A., Manrique, J., Renieri, A., De Filippo, R. E., Perin, L. and Da Sacco, S. (2019). A glomerulus-on-a-chip to recapitulate the human glomerular filtration barrier. Nat. Commun. 10, 3656. 10.1038/s41467-019-11577-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran, M. (2018). Basic Orthopaedic Sciences, 2nd edn. CRC Press. [Google Scholar]
- Regehr, K. J., Domenech, M., Koepsel, J. T., Carver, K. C., Ellison-Zelski, S. J., Murphy, W. L., Schuler, L. A., Alarid, E. T. and Beebe, D. J. (2009). Biological implications of polydimethylsiloxane-based microfluidic cell culture. Lab. Chip 9, 2132-2139. 10.1039/b903043c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regier, M. C., Tokar, J. J., Warrick, J. W., Pabon, L., Berthier, E., Beebe, D. J. and Stevens, K. R. (2019). User-defined morphogen patterning for directing human cell fate stratification. Sci. Rep. 9, 6433. 10.1038/s41598-019-42874-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennert, K., Steinborn, S., Gröger, M., Ungerböck, B., Jank, A.-M., Ehgartner, J., Nietzsche, S., Dinger, J., Kiehntopf, M. and Funke, H. (2015). A microfluidically perfused three dimensional human liver model. Biomaterials 71, 119-131. 10.1016/j.biomaterials.2015.08.043 [DOI] [PubMed] [Google Scholar]
- Rhea, E. M. and Banks, W. A. (2019). Role of the blood-brain barrier in central nervous system insulin resistance. Front Neurosci. 13, 521. 10.3389/fnins.2019.00521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards, J. S., Russell, D. L., Robker, R. L., Dajee, M. and Alliston, T. N. (1998). Molecular mechanisms of ovulation and luteinization. Mol. Cell. Endocrinol. 145, 47-54. 10.1016/S0303-7207(98)00168-3 [DOI] [PubMed] [Google Scholar]
- Rifes, P., Isaksson, M., Rathore, G. S., Aldrin-Kirk, P., Moller, O. K., Barzaghi, G., Lee, J., Egerod, K. L., Rausch, D. M., Parmar, M.et al. (2020). Modeling neural tube development by differentiation of human embryonic stem cells in a microfluidic WNT gradient. Nat. Biotechnol. 38, 1265-1273. 10.1038/s41587-020-0525-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, M., Bedford, E., Witherspoon, L., Willerth, S. M. and Flannigan, R. (2021). Microfluidic bioprinting for the in vitro generation of novel biomimetic human testicular tissues. bioRxiv 2021.2006.2004.447126. [Google Scholar]
- Rogers, A. J., Fast, V. G. and Sethu, P. (2016). Biomimetic cardiac tissue model enables the adaption of human induced pluripotent stem cell cardiomyocytes to physiological hemodynamic loads. Anal. Chem. 88, 9862-9868. 10.1021/acs.analchem.6b03105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosas-Canyelles, E., Modzelewski, A. J., Geldert, A., He, L. and Herr, A. E. (2020). Assessing heterogeneity among single embryos and single blastomeres using open microfluidic design. Sci. Adv. 6, eaay1751. 10.1126/sciadv.aay1751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi, G., Broguiere, N., Miyamoto, M., Boni, A., Guiet, R., Girgin, M., Kelly, R. G., Kwon, C. and Lutolf, M. P. (2021). Capturing cardiogenesis in gastruloids. Cell Stem Cell 28, 230-240. 10.1016/j.stem.2020.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roye, Y., Bhattacharya, R., Mou, X., Zhou, Y., Burt, M. A. and Musah, S. (2021). A personalized glomerulus chip engineered from stem cell-derived epithelium and vascular endothelium. Micromachines (Basel) 12, 967. 10.3390/mi12080967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadler, T. W. (2018). Langman's Medical Embryology, 14th edn. Lippincott Williams & Wilkins. [Google Scholar]
- Schittny, J. C. (2017). Development of the lung. Cell Tissue Res. 367, 427-444. 10.1007/s00441-016-2545-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwendimann, R. N. and Minagar, A. (2017). Liver disease and neurology. Continuum (Minneap Minn) 23, 762-777. 10.1212/CON.0000000000000486 [DOI] [PubMed] [Google Scholar]
- Shih, H. C., Lee, T. A., Wu, H. M., Ko, P. L., Liao, W. H. and Tung, Y. C. (2019). Microfluidic collective cell migration assay for study of endothelial cell proliferation and migration under combinations of oxygen gradients, tensions, and drug treatments. Sci. Rep. 9, 8234. 10.1038/s41598-019-44594-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieber, S., Wirth, L., Cavak, N., Koenigsmark, M., Marx, U., Lauster, R. and Rosowski, M. (2018). Bone marrow-on-a-chip: Long-term culture of human haematopoietic stem cells in a three-dimensional microfluidic environment. J. Tissue Eng. Regen. Med. 12, 479-489. 10.1002/term.2507 [DOI] [PubMed] [Google Scholar]
- Sonnen, K. F. and Merten, C. A. (2019). Microfluidics as an emerging precision tool in developmental biology. Dev. Cell 48, 293-311. 10.1016/j.devcel.2019.01.015 [DOI] [PubMed] [Google Scholar]
- Sriram, G., Alberti, M., Dancik, Y., Wu, B., Wu, R., Feng, Z., Ramasamy, S., Bigliardi, P. L., Bigliardi-Qi, M. and Wang, Z. (2018). Full-thickness human skin-on-chip with enhanced epidermal morphogenesis and barrier function. Mater. Today 21, 326-340. 10.1016/j.mattod.2017.11.002 [DOI] [Google Scholar]
- Steinberger, E. (1967). Maintenance of adult human testicular tissue in culture. In Anatomical Record, pp. 327. Wiley. [Google Scholar]
- Tan, C. M. J. and Lewandowski, A. J. (2020). The transitional heart: from early embryonic and fetal development to neonatal life. Fetal Diagn. Ther. 47, 373-386. 10.1159/000501906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenenbaum-Katan, J., Fishler, R., Rothen-Rutishauser, B. and Sznitman, J. (2015). Biomimetics of fetal alveolar flow phenomena using microfluidics. Biomicrofluidics 9, 014120. 10.1063/1.4908269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tierney, A. L. and Nelson, C. A.III (2009). Brain development and the role of experience in the early years. Zero Three 30, 9-13. [PMC free article] [PubMed] [Google Scholar]
- Torisawa, Y.-S., Spina, C. S., Mammoto, T., Mammoto, A., Weaver, J. C., Tat, T., Collins, J. J. and Ingber, D. E. (2014). Bone marrow–on–a–chip replicates hematopoietic niche physiology in vitro. Nat. Methods 11, 663-669. 10.1038/nmeth.2938 [DOI] [PubMed] [Google Scholar]
- Torisawa, Y.-S., Mammoto, T., Jiang, E., Jiang, A., Mammoto, A., Watters, A. L., Bahinski, A. and Ingber, D. E. (2016). Modeling hematopoiesis and responses to radiation countermeasures in a bone marrow-on-a-chip. Tissue Eng. C Methods 22, 509-515. 10.1089/ten.tec.2015.0507 [DOI] [PubMed] [Google Scholar]
- Uccelli, A., Moretta, L. and Pistoia, V. (2008). Mesenchymal stem cells in health and disease. Nat. Rev. Immunol. 8, 726-736. 10.1038/nri2395 [DOI] [PubMed] [Google Scholar]
- Uwamori, H., Higuchi, T., Arai, K. and Sudo, R. (2017). Integration of neurogenesis and angiogenesis models for constructing a neurovascular tissue. Sci. Rep. 7, 1-11. 10.1038/s41598-017-17411-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Duinen, V., Zhu, D., Ramakers, C., van Zonneveld, A. J., Vulto, P. and Hankemeier, T. (2019). Perfused 3D angiogenic sprouting in a high-throughput in vitro platform. Angiogenesis 22, 157-165. 10.1007/s10456-018-9647-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oostrom, M. J., Meijer, W. H. M. and Sonnen, K. F. (2021). A microfluidics approach for the functional investigation of signaling oscillations governing somitogenesis. J. Vis. Exp. 169, e62318. 10.3791/62318 [DOI] [PubMed] [Google Scholar]
- Vazquez-Armendariz, A. I. and Herold, S. (2021). From clones to buds and branches: the use of lung organoids to model branching morphogenesis Ex Vivo. Front. Cell Dev. Biol. 9, 631579. 10.3389/fcell.2021.631579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vozzi, G., Previti, A., De Rossi, D. and Ahluwalia, A. (2002). Microsyringe-based deposition of two-dimensional and three-dimensional polymer scaffolds with a well-defined geometry for application to tissue engineering. Tissue Eng. 8, 1089-1098. 10.1089/107632702320934182 [DOI] [PubMed] [Google Scholar]
- Vozzi, G., Flaim, C., Ahluwalia, A. and Bhatia, S. (2003). Fabrication of PLGA scaffolds using soft lithography and microsyringe deposition. Biomaterials 24, 2533-2540. 10.1016/S0142-9612(03)00052-8 [DOI] [PubMed] [Google Scholar]
- Wan, C.-r., Chung, S. and Kamm, R. D. (2011). Differentiation of embryonic stem cells into cardiomyocytes in a compliant microfluidic system. Ann. Biomed. Eng. 39, 1840-1847. 10.1007/s10439-011-0275-8 [DOI] [PubMed] [Google Scholar]
- Wang, Y., Wang, X., Shi, J., Zhu, R., Zhang, J., Zhang, Z., Ma, D., Hou, Y., Lin, F., Yang, J.et al. (2016). A biomimetic silk fibroin/sodium alginate composite scaffold for soft tissue engineering. Sci. Rep. 6, 39477. 10.1038/srep39477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y., Wang, L., Zhu, Y. and Qin, J. (2018). Human brain organoid-on-a-chip to model prenatal nicotine exposure. Lab. Chip 18, 851-860. 10.1039/C7LC01084B [DOI] [PubMed] [Google Scholar]
- Wang, Y., Shao, Z., Zheng, W., Xie, Y., Luo, G., Ding, M. and Liang, Q. (2019). A 3D construct of the intestinal canal with wrinkle morphology on a centrifugation configuring microfluidic chip. Biofabrication 11, 045001. 10.1088/1758-5090/ab21b0 [DOI] [PubMed] [Google Scholar]
- Weibel, D. B., Diluzio, W. R. and Whitesides, G. M. (2007). Microfabrication meets microbiology. Nat. Rev. Microbiol. 5, 209-218. 10.1038/nrmicro1616 [DOI] [PubMed] [Google Scholar]
- Weng, L. (2019). IVF-on-a-chip: recent advances in microfluidics technology for in vitro fertilization. SLAS Technol 24, 373-385. [DOI] [PubMed] [Google Scholar]
- Whitesides, G. M. (2006). The origins and the future of microfluidics. Nature 442, 368-373. 10.1038/nature05058 [DOI] [PubMed] [Google Scholar]
- Wu, W., DeConinck, A. and Lewis, J. A. (2011). Omnidirectional printing of 3D microvascular networks. Adv. Mater. 23, H178-H183. 10.1002/adma.201004625 [DOI] [PubMed] [Google Scholar]
- Xia, Y. and Whitesides, G. M. (1998). Soft lithography. Angew. Chem. Int. Ed. Engl. 37, 550-575. [DOI] [PubMed] [Google Scholar]
- Xiao, S., Coppeta, J. R., Rogers, H. B., Isenberg, B. C., Zhu, J., Olalekan, S. A., McKinnon, K. E., Dokic, D., Rashedi, A. S., Haisenleder, D. J.et al. (2017). A microfluidic culture model of the human reproductive tract and 28-day menstrual cycle. Nat. Commun. 8, 14584. 10.1038/ncomms14584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yourek, G., McCormick, S. M., Mao, J. J. and Reilly, G. C. (2010). Shear stress induces osteogenic differentiation of human mesenchymal stem cells. Regen. Med. 5, 713-724. 10.2217/rme.10.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, F., Hunziker, W. and Choudhury, D. (2019). Engineering microfluidic organoid-on-a-chip platforms. Micromachines (Basel) 10, 165. 10.3390/mi10030165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, C., Zhao, Z., Abdul Rahim, N. A., van Noort, D. and Yu, H. (2009). Towards a human-on-chip: culturing multiple cell types on a chip with compartmentalized microenvironments. Lab. Chip 9, 3185-3192. 10.1039/b915147h [DOI] [PubMed] [Google Scholar]
- Zheng, W., Xie, Y., Zhang, W., Wang, D., Ma, W., Wang, Z. and Jiang, X. (2012). Fluid flow stress induced contraction and re-spread of mesenchymal stem cells: a microfluidic study. Integr. Biol. 4, 1102-1111. 10.1039/c2ib20094e [DOI] [PubMed] [Google Scholar]
- Zheng, Y., Xue, X., Shao, Y., Wang, S., Esfahani, S. N., Li, Z., Muncie, J. M., Lakins, J. N., Weaver, V. M., Gumucio, D. L.et al. (2019). Controlled modelling of human epiblast and amnion development using stem cells. Nature 573, 421-425. 10.1038/s41586-019-1535-2 [DOI] [PMC free article] [PubMed] [Google Scholar]