Abstract
Approximately half of adults are living with a chronic illness, many of whom may feel stigmatized by their chronic illness in different contexts. We explored the impact of internalized, experienced, and anticipated stigma within healthcare settings on the quality of life of 184 participants living with chronic illnesses (e.g. diabetes, inflammatory bowel disease, asthma). Results of a path analysis demonstrate that participants who internalized stigma and experienced stigma from healthcare workers anticipated greater stigma from healthcare workers. Participants who anticipated greater stigma from healthcare workers, in turn, accessed healthcare less and experienced a decreased quality of life.
Keywords: chronic illnesses, discrimination, healthcare, quality of life, stigma
Chronic illnesses are a growing concern internationally. Although global morbidity rates for most chronic illnesses are unavailable, global mortality rates suggest that a substantial number of adults are suffering from chronic illnesses (World Health Organization, 2010). In 2008, an estimated 63 percent of deaths were attributable to chronic illnesses. This number is expected to grow by 15 percent by 2020. Where morbidity rates are available, statistics suggest that over 50 percent of adults are living with at least one chronic illness, 25 percent of whom report significant limitations in their daily activities due to their illness (Anderson, 2004; Wu and Green, 2000). In addition to these physical challenges, people living with chronic illnesses may internalize, experience, and anticipate stigma – social devaluation or discrediting due to their illness (Goffman, 1963). Although people living with chronic illnesses may encounter these forms of stigma in a variety of social contexts, they may be particularly harmful within healthcare settings to the extent that they act as barriers to the regular healthcare access that can be critical to controlling chronic illness symptoms. This decreased healthcare access may, in turn, undermine the overall well-being of people living with chronic illnesses. A stronger understanding of internalized, experienced, and anticipated stigma within healthcare contexts among people living with chronic illnesses may inform strategies to enhance their quality of life.
In the current study we explore how internalized, experienced, and anticipated stigma have an impact upon healthcare access and quality of life (i.e. subjective well-being) among people living with chronic illnesses. Therefore, this work examines the process whereby stigma that is brought into healthcare settings (i.e. internalized stigma) and stigma that arises within interactions with healthcare workers (i.e. experienced stigma) impacts on the subjective well-being of people living with chronic illnesses. We review relevant research before presenting our hypothesized model and an empirical evaluation of that model. Although we focus on research on people living with chronic illnesses, we also include research on the experiences of people living with other stigmatized identities (e.g. HIV/AIDS, mental illness) with the understanding that the process by which internalized, experienced, and anticipated stigma impact the subjective well-being of people living with other stigmatized identities may be similar for people living with chronic illnesses.
People living with chronic illnesses may experience internalized, experienced, and anticipated stigma within healthcare settings. Internalized stigma is the extent to which people endorse negative beliefs and feelings associated with their stigmatized attribute and apply them to the self (Link, 1987). People living with chronic illnesses report feeling shame, guilt, and diminished self-worth (Person et al., 2009); embarrassed and odd (Kilinc and Campbell, 2009); responsibility for their illness (Mak et al., 2007); and even dirty and diseased (Conrad et al., 2006). Exemplifying these feelings of internalized devaluation, a person living with epilepsy reported feeling that ‘basically, I’m one of nature’s rejects’ (Kilinc and Campbell, 2009: 669). Notably, internalized stigma is an intrapersonal phenomenon. It is embodied by people living with chronic illnesses and therefore may be brought into a variety of social contexts, including healthcare settings.
Experienced stigma, also referred to as ‘enacted stigma’ (Earnshaw and Chaudoir, 2009) and ‘perceived discrimination’ (Kinsler et al., 2007), is the extent to which people perceive that they have experienced stereotyping, prejudice, and discrimination directed at them from others (Quinn and Earnshaw, in press; Scambler and Hopkins, 1986). People living with chronic illnesses report a variety of forms of experienced stigma in their daily lives (Hamilton-West and Quine, 2009; McManus et al., 2006), including within healthcare settings. People living with HIV/AIDS (PLWHA), for example, report receiving poor care, being denied care, and being blamed for their illness by healthcare workers (Sayles et al., 2007). People living with other illness-related stigmas report that healthcare workers feel frustrated with them, complaining of their ‘noncompliance’ (Rogge et al., 2004), and treat them differently or unfairly (Conrad et al., 2006). In contrast to internalized stigma, experienced stigma is perceived by people living with chronic illnesses within their interpersonal interactions, including those that occur with healthcare workers.
Anticipated stigma is the extent to which people expect to experience stereotyping, prejudice, and discrimination directed at them from others in the future (Markowitz, 1998). Previous research with a variety of concealable stigmatized identities, including illnesses, has found that greater anticipated stigma is related to increased psychological distress (Quinn and Chaudoir, 2009). These expectations of stigma may originate from stigma that has been internalized and experienced, and therefore may be partly an intrapersonal phenomenon and partly an interpersonal phenomenon. People who have internalized negative beliefs about the self may anticipate that others will treat them negatively because of their stigmatized attribute. Therefore, greater levels of internalized stigma likely predict more anticipated stigma. In support of this hypothesis, PLWHA who have internalized stigma are more likely to avoid disclosing their HIV status to others (Steward et al., 2008). This avoidance may be due to anticipated stigma: PLWHA may avoid disclosing because they expect that others will treat them in negative ways due to their HIV status. Further, people who perceive that they have experienced stigma in the past may come to anticipate stigma in the future. PLWHA who perceive that they have experienced stigma also avoid disclosing their HIV status to others (Steward et al., 2008), again possibly due to anticipated stigma. In short, people living with chronic illnesses who have internalized stigma and experienced stigma in healthcare may anticipate stigma in healthcare in the future.
Internalized, experienced, and anticipated stigma within healthcare settings likely act as barriers to care access. In the current work care access refers to the extent to which people living with chronic illnesses choose to seek healthcare for their chronic illness, rather than the extent to which healthcare resources are available to them. The majority of chronic illnesses are characterized by quiet, asymptomatic phases followed by sometimes severe flare ups of symptoms (Leventhal et al., 2004). Although chronic illnesses cannot be cured, they can often be controlled through medical treatment. Therefore, it can be critical for people living with chronic illnesses to access care regularly to prevent flare ups of symptoms and prolong asymptomatic phases. Regular care access, in turn, might enhance the quality of life of people living with chronic illnesses.
People living with chronic illnesses who have internalized stigma may be less likely to access care because they feel that they do not deserve care or that care may not work for them. Although there has been no direct research on internalized stigma with chronic illness, research on people living with mental illness who have internalized stigma shows that they have poorer attitudes toward mental health treatment (Conner et al., 2009). Similarly, people who perceive that they have experienced stigma in healthcare settings may be less likely to access care because they do not want to face additional negative treatment. Importantly, both internalized and experienced stigma may be related to lower care access through the mediating variable of anticipated stigma. That is, people who have internalized negative beliefs about the self and have experienced prejudice, stereotyping, and discrimination in healthcare settings may come to anticipate that they will encounter similar experiences in the future. They may, in turn, not access care to avoid these negative experiences. Indeed, in a longitudinal study of PLWHA, perceived discrimination in healthcare settings was associated with low levels of care access at a six-month follow-up (Kinsler et al., 2007).
Internalized, experienced, and anticipated stigma, as well as decreased care access, may undermine the quality of life of people living with chronic illnesses. Quality of life is defined by the World Health Organization (1998) as an individual’s subjective evaluation of their life as it relates to their own values and goals. Quality of life is a multidimensional construct, including physical, psychological, social, and environmental domains. Both internalized and experienced stigma are associated with decreased quality of life among PLWHA (Holzemer et al., 2007, 2009). Anticipated stigma has also been negatively linked to several domains of quality of life among people living with HIV and chronic illnesses, including psychological well-being (Berger et al., 2001; Conrad et al., 2006; Conradt et al., 2008; Sayles et al., 2008; Visser et al., 2008) and social integration (Berger et al., 2001; Conradt et al., 2008). Furthermore, anticipated stigma in healthcare settings specifically has been linked to poor health-related outcomes (Chesney and Smith, 1999). It is possible that care access mediates the relationship between stigma in healthcare settings and quality of life. That is, people living with chronic illnesses who internalize, experience, and anticipate stigma within healthcare contexts may avoid accessing care and, in turn, experience decreased quality of life.
In the current study, we evaluate the hypothesized model presented in Fig. 1. We hypothesize that: (1) internalized stigma and experienced stigma in healthcare settings predict increased anticipated stigma in healthcare settings; (2) internalized, experienced, and anticipated stigma predict decreased care access and decreased quality of life; (3) care access predicts increased quality of life. Taken together, this model suggests a process whereby stigma within healthcare settings impacts upon the subjective well-being of people living with chronic illnesses.
Figure 1.
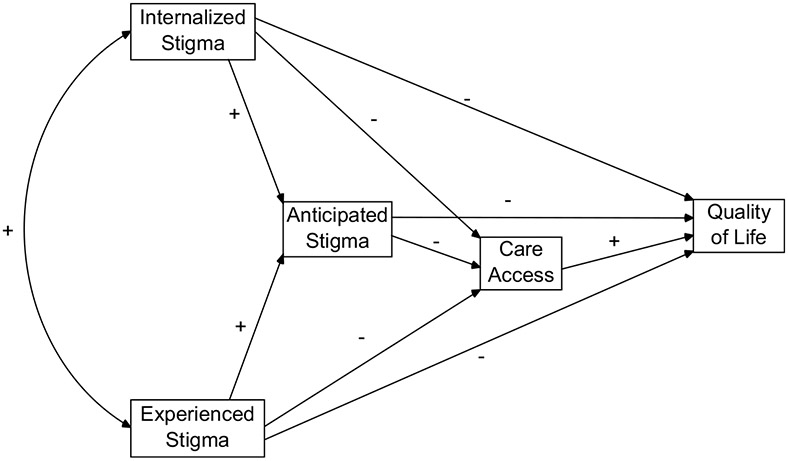
Hypothesized model of the impact of internalized, experienced, and anticipated stigma on healthcare access and quality of life.
Methods
Procedure and participants
The current study was titled ‘Body–Mind Connections’ and was administered online. Approval for the study was obtained from the University of Connecticut Institutional Review Board. Participants were students (undergraduate and graduate) from the University of Connecticut recruited through the psychology department participant pool and the university student listserv. Participants recruited through the participant pool received partial course credit for their participation, and participants recruited through the student listserv were entered into a raffle to win one of several prizes. Students were eligible to participate in the study if they had a medical condition for which they had to see a doctor two or more times in the past year. Upon accessing the study website, participants were asked if they had a chronic illness for which they had to see a doctor in the last year. If participants answered ‘yes’, they completed a series of measures both related and unrelated to their chronic illness. If participants answered ‘no’, they completed a series of measures unrelated to chronic illness.
A total of 447 students responded to the online study. Of these, 184 reported living with a chronic illness and therefore were retained in the analyses. Participant demographic information is presented in Table 1. Participants were primarily in their early 20s, female, and White or European-American. Participants reported living with between one and seven chronic illnesses in total. Participants were asked to indicate the illness that impacts their lives the most. Forty-eight illnesses were indicated, 22 of which were shared by two or more participants. The most common illnesses included asthma, inflammatory bowel disease, diabetes, irritable bowel syndrome, and pain disorders. Participants were further asked to think about the illness that impacts their lives the most when responding to the remainder of the study.
Table 1.
Participant Demographics (N = 184).
| Variable | Participants |
|||
|---|---|---|---|---|
| N | % | M | SD | |
| Age | 21.74 | 5.94 | ||
| Gender | ||||
| Female | 134 | 72.8 | ||
| Male | 50 | 27.2 | ||
| Race/ethnicity | ||||
| White/European-American | 152 | 82.6 | ||
| Asian/Asian-American | 12 | 6.5 | ||
| Multi-racial | 8 | 4.3 | ||
| Black/African-American | 5 | 2.7 | ||
| Latino(a)/Hispanic-American | 3 | 1.6 | ||
| Other | 3 | 1.6 | ||
| Native American | 1 | 0.5 | ||
| Total chronic illnesses | 1.39 | 0.87 | ||
| Most common chronic illnesses | ||||
| Asthma | 53 | 28.8 | ||
| Inflammatory Bowel Disease (Crohn’s and Ulcerative Colitis) | 17 | 9.2 | ||
| Diabetes | 11 | 6.0 | ||
| Irritable Bowel Syndrome | 8 | 4.3 | ||
| Pain Disorder | 8 | 4.3 | ||
Materials
Although scales have been developed to measure stigma and related constructs among people living with specific stigmas such as HIV (e.g. Berger et al., 2001) and mental illness (e.g. Link, 1987), none have been developed to measure these constructs among people living with a variety of chronic illnesses. Therefore, we developed several measures for the current study. These measures are largely modeled after validated scales and include items that are tailored for people living with chronic illnesses. Items created for the current study are based on literature reviews focused on the experiences of people living with a variety of chronic illnesses. These items are included below along with the Cronbach’s alpha for each measure, included as an indicator of reliability.
Internalized stigma.
The internalized stigma measure included five items adapted from the Negative Self-Image subscale of the HIV Stigma Scale (Berger et al., 2001; e.g. ‘I feel I’m not as good as others because I have a health condition’) as well as six items developed for the current study. Items that were developed for the current study included: ‘It is my fault that I have a health condition’; ‘I can’t do a lot of things because I have a health condition’; ‘Because I have a health condition, I’m not a good employee’; ‘I can’t fulfill many of my responsibilities because I have a health condition’; ‘I am as capable as people who do not have a health condition’ (reverse coded); and ‘People who do not have health conditions are not better than me’ (reverse coded). Participants responded to all items on a scale from 1 (strongly disagree) to 5 (strongly disagree). An internalized stigma score was created by averaging the 11 scale items (α = .75).
Experienced stigma.
The experienced stigma measure was modeled after the measure of perceived discrimination employed by Kessler et al. (1999). Participants were provided with a list of 17 examples of experienced stigma in healthcare settings, including ‘A healthcare worker has thought that your illness is your fault’, and were asked to check a box if they perceived that the event described had happened to them.1 An experienced stigma score was created by summing the number of boxes checked by participants.
Anticipated stigma.
The anticipated stigma measure was from the healthcare subscale of the Chronic Illness Anticipated Stigma Scale (Earnshaw and Quinn, 2010). Participants responded to four items gauging anticipated stigma in healthcare settings, including: ‘A healthcare worker will give you poor care’; ‘A healthcare worker will blame you for not getting better’; ‘A healthcare worker will be frustrated with you’; and: ‘A healthcare worker will think that you are a bad patient.’ Participants responded to all items on a scale from 1 (very unlikely) to 5 (very likely). An anticipated stigma score was created by averaging the scale items (α = .89).
Care access.
The care access measure was developed for the current study. Participants were asked to indicate how often they see their doctor and whether they see their doctor when they feel sick. Participants responded to six items, including: ‘I don’t always go to the doctor’s when I should’ (reverse coded); ‘I should have started seeing a doctor for my illness earlier’ (reverse coded); ‘Sometimes I feel sick for awhile before I go to the doctor’s’ (reverse coded); ‘I see my doctor regularly’; ‘I should see my doctor more frequently’ (reverse coded); and: ‘I always go to the doctor’s when I feel sick’, all using a scale from 1 (strongly disagree) to 5 (strongly agree). A care access score was created by averaging the scale items (α = .79).
Quality of life.
The quality of life measure was the brief version of the World Health Organization’s Quality of Life Scale. The scale evaluates quality of life in four domains: physical; psychological; social relationships; and environment. Participants responded to 26 items, including: ‘Do you have enough energy for everyday life?’ on five-point Likert-type scales with anchors tailored for each question. Higher scores indicate higher quality of life. A quality of life score was created by averaging scale items (α = .92).
Results
Given that there were substantially more females than males in the sample, gender differences were examined first. These preliminary analyses demonstrated that there were no statistically significant gender differences on any of the variables included in the study. Consequently, the data were collapsed across gender. Descriptive statistics, including means and correlations between variables, are included in Table 2. Participants reported low levels of internalized, experienced, and anticipated stigma, with average scores toward the lower end of the scales. They reported higher care access and quality of life, with average scores toward the middle of the scales. All variables were correlated except experienced stigma and quality of life.
Table 2.
Means (standard deviations) and correlations between all variables.
| Mean (SD) | Internalized stigma |
Experienced stigma |
Anticipated stigma |
Care access | |
|---|---|---|---|---|---|
| Internalized stigma | 1.96 (.63) | – | |||
| Experienced stigma | 0.92 (2.14) | .27** | – | ||
| Anticipated stigma | 1.55 (.88) | .39** | .77** | – | |
| Care access | 3.29 (.86) | −.22** | −.26** | −.31** | – |
| Quality of life | 3.71 (.74) | −.60** | −.12 | −.24** | .27** |
Note:
p < .01. All variables are means derived from items measured on five-point scales with the exception of experienced stigma which is a sum of up to 17 items.
The data were analyzed using path analysis in AMOS 17.0. Internalized stigma and experienced stigma were included in the model as exogenous variables and anticipated stigma, care access, and quality of life were endogenous variables. First, the saturated model was examined. The paths from experienced stigma to care access, experienced stigma to quality of life, and anticipated stigma to quality of life were non-statistically significant (all ps > .10). As recommended by Kline (2005), these paths were trimmed.
Figure 2 presents the final path model with dashed lines representing trimmed paths. The figure includes the correlation statistic for the exogenous variables, the standardized regression weights for all non-trimmed paths, and the squared multiple correlation statistics for all endogenous variables. Model fit indices reveal that the model is a good fit for the data, χ2 (3) = 7.14, p = .07; RMSEA = .03 (CI = .00−.05); CFI = .99; SRMR = .01. First, the model demonstrates that internalized stigma and experienced stigma were correlated, indicating that participants who perceived that they had experienced more stigma also internalized stigma more. Second, both internalized stigma and experienced stigma were related to greater anticipated stigma. Experienced stigma had a stronger relationship with anticipated stigma than internalized stigma, suggesting that participants’ anticipation of stigma may be more strongly influenced by their perceptions of past experiences of stigma than their internalization of stigma. Third, internalized stigma was further related to care access and quality of life. Participants who internalized stigma more accessed care less and had a lower quality of life. Fourth, anticipated stigma was related to care access. Participants who anticipated greater stigma accessed less care. Interestingly, the relationship between anticipated stigma and care access was stronger than the relationship between internalized stigma and care access, suggesting that participants’ care access may be more influenced by their anticipation of stigma than internalization of stigma. Finally, care access was related to quality of life. Participants who accessed more care had a higher quality of life. The model explains 38.1 percent of the variance in the quality of life of participants.
Figure 2.
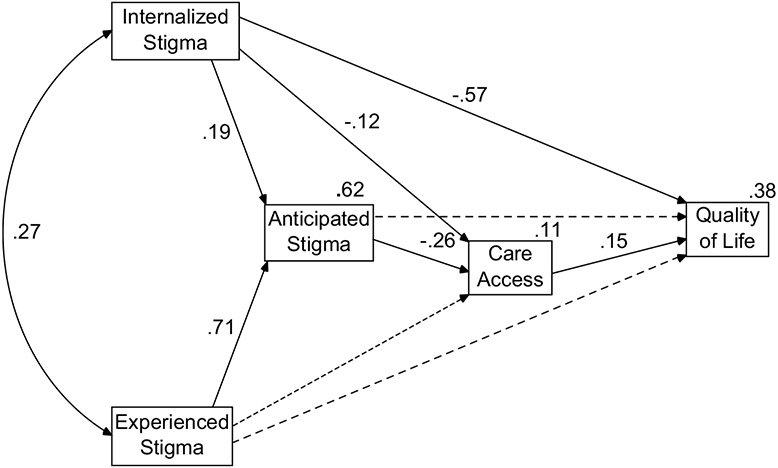
Path analysis of the impact of internalized, experienced, and anticipated stigma on healthcare access and quality of life. Model includes dashed lines representing trimmed paths, standardized regression weights for all non-trimmed paths, and the correlation between internalized and experienced stigma.
The direct and indirect effects were examined next to evaluate potential mediation within the model (Kline, 2005). We performed boot-strapping when conducting the path analysis to acquire tests of statistical significance of the direct and indirect effects. Experienced stigma had an indirect effect on care access of −.19 (p < .001) but no direct effect, suggesting that anticipated stigma mediated the relationship between experienced stigma and care access. Experienced stigma also had an indirect effect on quality of life of −.03 (p < .001) but no direct effect, suggesting that anticipated stigma and care access mediated the relationship between experienced stigma and quality of life. Furthermore, internalized stigma had an indirect effect on care access of −.05 (p < .001) and a direct effect of −.12 (p < .001), suggesting that anticipated stigma partially mediated the relationship between internalized stigma and care access. Internalized stigma also had an indirect effect on quality of life of −.03 (p < .001) and a direct effect of −.57 (p < .001), suggesting that anticipated stigma and care access partially mediated the relationship between internalized stigma and quality of life. Despite this evidence of partial mediation, the direct effects of internalized stigma on care access and quality of life were stronger than the indirect effects, suggesting that internalized stigma has the bulk of its impact on care access and quality of life directly rather than indirectly through other variables in the model. Finally, anticipated stigma had an indirect effect on quality of life of −.04 (p < .001) but no direct effect, suggesting that care access mediated the relationship between anticipated stigma and quality of life.
Because these data are correlational in nature, we cannot form firm conclusions regarding any potential causal relationships between the variables. We therefore evaluated several alternative models to see if a different configuration of the variables would provide a better fit for the data. None of these alternative models offered a better fit for the data.2
Discussion
We explored the process whereby internalized, experienced, and anticipated stigma within healthcare settings impact upon the quality of life of people living with chronic illnesses. The results of the path analysis supported our hypotheses. Notably, internalized stigma was directly related to anticipated stigma, care access, and quality of life, whereas experienced stigma was directly related to anticipated stigma but indirectly related to care access and quality of life. This suggests that the process whereby internalized stigma impacts upon the well-being of people living with chronic illnesses works differently than that of experienced stigma. The impact of experienced stigma on quality of life is mediated by anticipated stigma and care access, whereas the impact of internalized stigma is more direct.
The current work highlights the harmful role of stigma in healthcare settings on the quality of life of people living with chronic illnesses. Participants living with chronic illnesses who internalized, experienced, and anticipated stigma in healthcare settings were less likely to access care and, in turn, had a decreased quality of life. Therefore, stigma impacted more than the physical health of people living with chronic illnesses – it impacted upon their overall sense of satisfaction with life. Although these findings might raise concern for the well-being of people living with chronic illnesses, they might also offer hope for future work designed to improve their well-being. By exploring stigma in healthcare settings and the process by which stigma impacts quality of life, the current work suggests several targets of intervention to alleviate the impact of stigma on people living with chronic illnesses.
First, the study highlights the importance of targeting internalized stigma within interventions given its direct relationship to all of the outcomes of interest within this work. People living with chronic illnesses who endorse stereotypes and prejudice associated with their chronic illness also think that healthcare workers will treat them with stereotyping, prejudice, and discrimination, are less likely to access healthcare, and have a lower quality of life. Internalized stigma may be particularly detrimental to the quality of life of people living with chronic illnesses because it is an intrapersonal phenomenon and can therefore be brought into a variety of social contexts. Indeed, the direct path between internalized stigma and quality of life within the evaluated path model suggests that internalized stigma impacts quality of life regardless of the psychosocial processes occurring within the healthcare context (i.e. anticipated stigma within healthcare contexts and care access). Therefore, interventions designed to reduce internalized stigma among people living with chronic illnesses may improve their well-being in a variety of social contexts. Corrigan and Wassel (2008; Rüschet al., 2005) have made recommendations on how to reduce internalized stigma related to mental illness, many of which might be adapted for people living with chronic illnesses. For example, developing more positive group identities, undermining the legitimacy of stigma, and encouraging empowerment among people living with chronic illnesses may help to reduce internalized stigma and improve the outcomes of people living with chronic illnesses.
Second, the study underscores the importance of targeting experienced stigma to reduce anticipated stigma. Experienced stigma was the strongest predictor of anticipated stigma, which, in turn, was the strongest predictor of decreased healthcare access. Therefore, people living with chronic illnesses who perceive that they have experienced stereotyping, prejudice, and discrimination from healthcare workers in the past expect to encounter similar treatment from healthcare workers in the future and, in turn, are less likely to access healthcare. Interventions designed to reduce stereotyping, prejudice, and discrimination among healthcare workers may decrease the amount of experienced stigma that is perceived by people living with chronic illnesses in healthcare settings and, in turn, decrease their anticipated stigma. Such interventions have been employed with some success among healthcare workers who work with PLWHA (for reviews, see Brown et al., 2003; Pulerwitz et al., 2010), and might be adapted for healthcare workers who work with people living with other types of chronic illnesses.
Third, the process by which stigma impacts quality of life might be targeted. The current study suggests that the relationships between internalized, experienced, and anticipated stigma with quality of life are all at least partially mediated by care access. That is, people living with chronic illnesses who internalize, experience, and anticipate stigma in healthcare may be less likely to go to the doctor and, in turn, may have a decreased quality of life. Interventions designed to disrupt this relationship by increasing care access may also increase the quality of life of people living with chronic illnesses. Recent recommendations for increasing treatment adherence might be adapted for care access by educating people living with chronic illnesses about the importance of care access, and by encouraging self-efficacy regarding setting goals around, and self-monitoring of, care access (Dunbar-Jacob, 2007). Successfully encouraging people living with chronic illnesses to access care despite their concerns of stigma may help to improve their quality of life.
It is important to note several limitations of the study in terms of its methodology and sample. Owing to the cross-sectional nature of our data, firm conclusions regarding any potential causal relationships between the constructs are impossible to make. However, because our hypotheses were formed using previous theory and evidence, our model is one likely candidate for accurately representing the relationships between the constructs. Future research might continue to explore the potential causal relationships between the constructs using longitudinal and experimental research designs.
The study is further limited in terms of its sample. Because our sample is comprised of university students, the generalizability of our findings to non-university student populations is uncertain. The general population may be more likely to be diagnosed after their early 20s, suffer more severe illnesses and symptoms, and experience more stigma than university students. For example, the most prevalent chronic illnesses in the current sample included inflammatory bowel disease, diabetes, and asthma. Underrepresented within this sample were several chronic illnesses that are highly prevalent among older adult populations, including heart disease, cancer, and chronic respiratory diseases such as chronic obstructive pulmonary disease. Future research might explore the extent to which these findings are generalizable by replicating them within other populations of people living with a more diverse range of chronic illnesses.
Conclusions
In sum, this study highlights the harmful effect of stigma in healthcare settings on the quality of life of people living with chronic illnesses. A multipronged approach designed to intervene with healthcare workers to reduce stereotyping, prejudice, and discrimination, as well as with people living with chronic illnesses to reduce internalized stigma and increase care access, may be the best way to decrease anticipated stigma, increase care access, and improve the quality of life of people living with chronic illnesses. Given the growing numbers of people living with chronic illnesses (World Health Organization, 2010; Wu and Green, 2000), better understanding of chronic illness stigma in healthcare will be increasingly important to improve the quality of life of this expanding population.
Acknowledgements
Preparation of this manuscript was supported by a training fellowship (T32MH074387) awarded to the first author from the National Institute of Mental Health. We thank Amy Huntington, Kimberly McClure, Nicole Overstreet, and Eileen Pitpitan for their helpful comments on this work.
Footnotes
Competing Interests
None declared.
The full experienced stigma scale is available from the first author.
First, we evaluated a model representing the alternative hypothesis that quality of life predicts increased care access which, in turn, predicts decreased anticipated, internalized, and experienced stigma. To evaluate this model, we reversed the paths of all of the arrows within the original model. This first alternative model represented a poorer fit for the data than the original model, χ2 (2) = 34.56, p < .001; RMSEA = .09 (CI = .07−.12); CFI = .99; SRMR = .02. Additionally, the AIC for the first alternative model was higher than the original model (70.56 vs 41.14), indicating poorer fit. Second, we evaluated a model representing the alternative hypothesis that there is no mediation between the variables. To evaluate this model, we included internalized stigma, experienced stigma, anticipated stigma, and care access as exogenous variables and quality of life as an endogenous variable. This model was therefore saturated. This second alternative model also represented a poorer fit for the data than the original model, χ2 (0) = 0.00, p = N/A; RMSEA = .40 (CI = .39−.42); CFI = 1.00; SRMR = .00, however the AIC was comparable (40.00). Neither alternative model offered a better fit for the data than the original model.
References
- Anderson G (2004) Chronic Conditions: Making the Case for Ongoing Care. Baltimore, MD: Johns Hopkins University. [Google Scholar]
- Berger BE, Ferrans CE and Lashley FR (2001) Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing & Health 24(6): 518–529. [DOI] [PubMed] [Google Scholar]
- Brown L, Macintyre K and Trujillo L (2003) Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention 15(1): 49–69. [DOI] [PubMed] [Google Scholar]
- Chesney MA and Smith AW (1999) Critical delays in HIV testing and care: The potential role of stigma. American Behavioral Scientist 42(7): 1158–1170. [Google Scholar]
- Conner KO, Koeske G and Brown C (2009) Racial differences in attitudes toward professional mental health treatment: The mediating effect of stigma. Journal of Gerontological Social Work 52(7): 695–712. [DOI] [PubMed] [Google Scholar]
- Conrad S, Garrett LE, Cooksley WGE, MacDonald GA and Dunne MP (2006) Living with chronic hepatitis C means ‘you just haven’t got a normal life any more’. Chronic Illness 2(2): 121–131. [DOI] [PubMed] [Google Scholar]
- Conradt M, Dierk J, Schlumberger P, Hebebrand J, Rief W and Rauh E (2008) Who copes well? Obesity-related coping and its associations with shame, guilt, and weight loss. Journal of Clinical Psychology 64(10): 1129–1144. [DOI] [PubMed] [Google Scholar]
- Corrigan PW and Wassel A (2008) Understanding and influencing the stigma of mental illness. Journal of Psychosocial Nursing & Mental Health Services 46(1): 42–48. [DOI] [PubMed] [Google Scholar]
- Dunbar-Jacob J (2007) Models for changing patient behavior. American Journal of Nursing 107(6): 20–25. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA and Chaudoir SR (2009) From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS & Behavior 13(6): 1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA and Quinn DM (2010) Development and evaluation of the Chronic Illness Anticipated Stigma Scale. Poster presented at the 22nd annual convention of the Association for Psychological Science, Boston, MA, May. [Google Scholar]
- Goffman E (1963) Stigma: Notes on the Management of Spoiled Identity. New York: Simon & Schuster. [Google Scholar]
- Hamilton-West KE and Quine L (2009) Living with ankylosing spondylitis: The patient’s perspective. Journal of Health Psychology 14(6): 820–830. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Human S, Arudo J, et al. (2009) Exploring HIV stigma and quality of life for persons living with HIV infection. Journal of the Association of Nurses in AIDS Care 20(3): 161–168. [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Uys LR, Chirwa ML, et al. (2007) Validation of the HIV/AIDS stigma instrument–PLWA (HASI-P). AIDS Care 19(8): 1002–1012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD and Williams DR (1999) The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior 40(3): 208–230. [PubMed] [Google Scholar]
- Kilinc S and Campbell C (2009) ‘It shouldn’t be something that’s evil, it should be talked about’: A phenomenological approach to epilepsy and stigma. Seizure 18(10): 665–671. [DOI] [PubMed] [Google Scholar]
- Kinsler JJ, Wong MD, Sayles JN, Davis C and Cunningham WE (2007) The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care and STDs 21(8): 584–592. [DOI] [PubMed] [Google Scholar]
- Kline RB (2005) Principles and Practice of Structural Equation Modeling. New York: The Guilford Press. [Google Scholar]
- Leventhal H, Ethan H, Horowitz C, Leventhal E and Ozakinci G (2004) Living with chronic illness: A contextualized, self-regulation approach. In: Sutton S, Baum A and Johnston M (eds) The SAGE Handbook of Health Psychology. London: SAGE; 197–240. [Google Scholar]
- Link BG (1987) Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review 52(1): 96–112. [Google Scholar]
- Mak WW, Cheung RY, Law RW, Woo J, Li PC and Cheung RW (2007) Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Social Science & Medicine 64(8): 1549–1559. [DOI] [PubMed] [Google Scholar]
- Markowitz FE (1998) The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. Journal of Health and Social Behavior 39(4): 335–347. [PubMed] [Google Scholar]
- McManus IC, Stubbings GF and Martin N (2006) Stigmatization, physical illness and mental health in primary ciliary dyskinesia. Journal of Health Psychology 11(3): 467–482. [DOI] [PubMed] [Google Scholar]
- Person B, Bartholomew LK, Gyapong M, Addiss DG and Van Den Borne B (2009) Health-related stigma among women with lymphatic filariasis from the Dominican Republic and Ghana. Social Science & Medicine 68(1): 30–38. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Michaelis A, Weiss E, Brown L and Mahendra V (2010) Reducing HIV-related stigma: Lessons learned from Horizons research and programs. Public Health Reports 125(2): 272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM, Chaudoir SR (2009) Living with a concealable stigmatized identity: The impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. Journal of Personality and Social Psychology 97(4): 634–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM and Earnshaw VA (in press) Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes. Social Issues and Policy Review. [Google Scholar]
- Rogge MM, Greenwald M and Golden A (2004) Obesity, stigma, and civilized oppression. Advances in Nursing Science 27(4): 301–315. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC and Corrigan PW (2005) Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry 20(8): 529–539. [DOI] [PubMed] [Google Scholar]
- Sayles JN, Hays RD, Sarkisian CA, Spritzer KL, Cunningham WE and Mahajan AP (2008) Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS and Behavior 12(5): 748–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayles JN, Ryan GW, Silver JS, Sarkisian CA and Cunningham WE (2007) Experiences of social stigma and implications for healthcare among a diverse population of HIV positive adults. Journal of Urban Health 84(6): 814–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scambler G and Hopkins A (1986) Being epileptic: Coming to terms with stigma. Sociology of Health and Illness 8(1): 26–43. [Google Scholar]
- Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J and Ekstrand ML (2008) HIV-related stigma: Adapting a theoretical framework for use in India. Social Science & Medicine 67(8): 1225–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser MJ, Kershaw T, Makin JD and Forsyth BWC (2008) Development of parallel scales to measure HIV-related stigma. AIDS and Behavior 12(5): 759–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (1998) WHO-QOL User Manual. Geneva, Switzerland: World Health Organization. [Google Scholar]
- World Health Organization (WHO) (2010) Global Status Report on Noncommunicable Diseases 2010. Geneva, Switzerland: WHO Press. [Google Scholar]
- Wu SY and Green A (2000) Projection of Chronic Illness Prevalence and Cost Inflation. Santa Monica, CA: RAND Health. [Google Scholar]


