Abstract
The COVID-19 pandemic is a major stressor that has negatively impacted global mental health. Many U.S. college students faced an abrupt transition to remote learning in March 2020 that significantly disrupted their routines, likely causing changes in mental health. The current study examined changes in anxiety and depressive symptoms among 990 college students, from before COVID-19 had reached U.S. community spread to 5 months into the pandemic. Results indicate overall increases in anxiety and depressive symptoms; this effect was amplified as more COVID-related challenges with academic impact and loneliness were reported. Increases in anxiety and depression were buffered as a function of greater perceived positive changes attributed to COVID-19; the differences in anxiety and depressive symptoms over time were also lessened when greater perceived stress prior to COVID-19 was reported. Findings reveal an unexpected effect involving pre-pandemic stress, and highlight potential targets to promote resilience, which should be examined long-term.
Keywords: COVID-19, mental health, anxiety, college, depression, moderation, resilience
Introduction
The outbreak of the novel coronavirus disease 2019 (COVID-19, caused by SARS-CoV-2) has resulted in a worldwide public health crisis, earning it the title of pandemic by the World Health Organization (2020). The direct costs of this disease are clear, having infected nearly 90 million and killed close to 2 million in the year since documentation of the first cases (Dong et al., 2020). To reduce disease spread and save lives, countries worldwide enacted public health measures that promoted social distancing, such as closing businesses and schools. As a result, the pandemic has also taken a toll on mental health, as individuals face difficult emotions related to the threat of COVID-19 to themselves, their loved ones, and their routines and activities. For many college students in the United States, March 2020 marked an abrupt transition from in-person learning to remote learning. The present study sought to examine college students’ changes in anxiety and depressive symptoms over time, from before COVID-19 was declared a national emergency and impacted their academic experience to after the completion of their Spring 2020 semester.
COVID-19 is a recognized threat to mental health (Cao et al., 2020; Gruber et al., 2020; Qiu et al., 2020; van der Velden et al., 2020; X. Wang, Pan, Wan, 2020). Over half of adults reporting on their COVID-19 experience in China rated the pandemic as having at least a moderate negative impact on their mental health (Wang, Hegde, Son, 2020). In one of the few published longitudinal analyses of mental health symptoms during COVID-19, Pierce and colleagues (2020) found an overall increase in mental health symptoms among adults from pre-COVID-19 (data collected 2017–2019) to during the COVID-19 pandemic (April 2020). Increases in these symptoms were greatest among the college-aged participants in the sample (18–24 years). Most work in this area has been cross-sectional, capturing important snapshots of the prevalence of mental health symptoms and their associations with COVID-19 related variables, such as virus exposure and economic impact. By utilizing a prospective study, with data collected prior to the onset of remote learning, the present study can go beyond this important cross-sectional work to understand factors that may relate to changes in mental health symptoms over time.
A question remains about whose mental health may be most affected by the COVID-19 pandemic. It has been posited that those with preexisting mental health problems or stressors may be vulnerable to exacerbation of those problems (Ghebreyesus, 2020). Alonzi and colleagues (Alonzi et al., 2020) found that those with preexisting mental health conditions reported worse anxiety and depressive symptoms during the COVID-19 pandemic. The idea that some individuals may have a predisposed vulnerability to psychopathology that is activated by stress is the underlying tenet of the diathesis-stress model. Consistent with this model, exposure to more stressful life events is related to greater psychopathology (Colodro-Conde et al., 2018; Faravelli et al., 2012). Thus, it is likely that preexisting stress may combine with the stressors of COVID-19 to produce greater anxiety and depressive symptoms. However, some work points to an opposing pattern. Hamza and colleagues (2021) found that declines in mental health were more pronounced among those without preexisting mental health conditions and those who had preexisting mental health conditions demonstrated similar or improving symptoms from May 2019 to May 2020. This contrasting finding is consistent with Pearlin’s stress process framework, which suggests that voluntary or involuntary life transitions are uplifting for some and stressful for others, depending on the “quality of experience within the lost role” (Pearlin, 2010). Drawing from this theory, it is possible that the onset of social distancing may have had a smaller negative impact on those higher in stress than those who were at ease in the life roles that they held prior to March 2020.
Among college students, the disruption to the academic experience has been a salient feature of the COVID-19 pandemic. As many universities transitioned to remote learning, students faced new barriers to learning (Besser et al., 2020). For example, students needed to maintain concentration on academics, despite a remote format with less external structure. Remote learning also involved unique challenges, including abrupt moves as campuses closed and a lack of resources needed for remote learning (e.g., stable internet connection, privacy). When asked about their COVID-19-related concerns, Canadian adolescents reported being most worried about the impact on their schooling (Ellis et al., 2020). In a U.S. sample of college students, the over 70% who reported increases in stress/anxiety during the pandemic identified academics as the most common contributor (Wang et al., 2020). Most college students also report barriers related to remote learning during the pandemic (Gillis & Krull, 2020). As such, we expect that experiencing a greater number of COVID-19-related challenges with a perceived negative academic impact would represent a more significant stressor and result in a greater decline in mental health during the pandemic.
Another outcome of the pandemic has been a disruption to social connections. This disruption to social connections may have directly or indirectly affected loneliness, defined as an absence of social contact, belongingness, or a sense of isolation. In a recent manuscript by Palgi and colleagues’ (Palgi et al., 2020), loneliness was identified as a central risk factor for depression and anxiety during COVID-19. Loneliness is especially relevant for college students because it has been linked to the transition to remote learning; loneliness was more common among those who participated in online (synchronous) learning, as compared to face-to-face learning, during COVID-19 (Besser et al., 2020). Elmer, Mepham, and Stadtfeld (2021) also found initial evidence that Swiss college students isolated due to their living situation were more likely to report an increase in depressive symptoms during COVID-19. Loneliness may serve as a risk factor that can exacerbate the increase in anxiety and depressive symptoms during COVID-19.
In addition to factors that may worsen the impact of life stressors, such as COVID-19, there are also factors that contribute to resilience. There is a robust literature linking engagement in active coping behaviors, such as positive reframing, connecting with social support, and engaging in physical activity, to resilience (Booth & Neill, 2017; Chen & Bonanno, 2020; Madsen et al., 2019). Positive reframing is the process of identifying positive elements of a situation, particularly one that is challenging or stressful (Lambert et al., 2009). Therefore, in response to stressors, those who are able to engage in more positive activities, or view the situation in a more positive light, are more psychologically resilient (Armstrong, Galligan, & Critchley, 2011). Biber and colleagues (2020) examined college student data during COVID-19 cross-sectionally and found that greater optimism and gratitude, two factors closely linked to identifying positive elements of a life stressor, were related to lower anxiety. Positive reframing during COVID-19 is also related to greater life satisfaction (Zacher & Rudolph, 2020). Across individuals, there are differences in the experience of positive changes to life during COVID-19, in part due to actual differences in circumstances, and in part due to the interpretation of those circumstances. Perceiving more positive changes is likely to relate to fewer mental health symptoms.
Present Study
The current study examined changes in anxiety and depressive symptoms among college students, from prior to the onset of remote learning during the COVID-19 pandemic (T1) to the completion of the Spring 2020 semester (T2). This work examined whether changes in anxiety or depressive symptoms varied by pre-remote learning perceived stress, the number of experienced challenges to remote learning, loneliness during remote learning, or perception of positive changes as a result of COVID-19. Given recent literature indicates that women have endorsed more pronounced mental health symptoms during COVID-19 (Elmer et al., 2020; Prowse et al., 2021), this work also accounted for the potential role of binary gender as a moderator of the changes in anxiety and depressive symptoms.
It was hypothesized that there would be increases in anxiety (1a) and depressive (1b) symptom endorsement from T1 to T2. It was also hypothesized that changes in T1 and T2 anxiety or depressive symptom endorsement would be moderated, such that identifying as a woman (vs. man; Hypotheses 2a, 2b), greater stress endorsed pre-pandemic (Hypotheses 3a, 3b), COVID-19-related challenges negatively impacting academics (Hypotheses 4a, 4b), and loneliness (Hypotheses 5a, 5b) would relate to greater increases in anxiety and depressive symptoms. Alternatively, we posited that having a perception that COVID-19 related to positive changes in one’s life would buffer the increases in anxiety and depressive symptoms (Hypotheses 6a, 6b) from T1 to T2.
Method
Participants and Procedures
Study participants were members of the junior class of a mid-sized, private university in the northeast who participated as part of a larger longitudinal study examining social networks and alcohol use. All members of the junior class were invited to participate in the T1 survey via email, and a number of in-person recruitment events targeting juniors were conducted on campus to increase participation. Only those students already enrolled in T1 were eligible to participate at T2. These students were invited to participate via email and announcements on the research project’s social media pages. The T2 survey was an addition to the originally planned data collection timeline within the larger study, to assess outcomes following the first semester of remote learning. Only those who completed assessments of anxiety and depression at both timepoints were included in the present sample. The sample consisted of 990 participants. At the first timepoint, the average age was 21.0 (SD = .54) and 61% identified as women. Participants identified as 58.3% White, 8.4% Black, 34.2% Asian, and 6.2% other. In addition, 12.5% percent of participants identified as Hispanic/Latino. About one-sixth of the sample (16.5%) identified as a first-generation college student. During remote learning, 75.1% of students lived with parents and/or other family, 15.3% lived with friends, alone, or on campus housing, 8.2% lived with both parents or family and lived with friends, alone, or on campus, and 1.5% lived with “other” (e.g., reported studying abroad). During remote learning, 11.5% of the sample reported that they did not have access to adequate and reliable internet.
Participation for this study consisted of completing online surveys prior to campus shut-down and the transition to remote learning (T1 survey open February 19 to March 14, 2020) and 5 months later, in the summer following the end of Spring semester (open July 13 to July 27, 2020). At T1, stress, anxiety and depressive symptoms were assessed. At T2, anxiety and depressive symptoms were assessed again along with COVID-19 specific constructs of interest, including COVID-19-related challenges negatively impacting academics, loneliness, and perception of positive changes related to COVID-19. Participants were compensated with a $55 Amazon E-gift card for completing the T1 survey and a $25 Amazon E-gift card for completing the T2 survey. All procedures were approved by the University’s Institutional Review Board.
Measures
Anxiety and Depression
The PHQ-4 (Kroenke et al., 2009) was used to assess anxiety and depressive symptoms experienced over the past 30 days when assessed at T1 and since campus closed when assessed at T2. The four-item measure is commonly used, well-validated and reliable in college populations (Khubchandani et al., 2016). It consists of two items specific to anxiety symptoms (“Feeling nervous, anxious, or on edge” and “Not being able to stop or control worrying”) and two items specific to depressive symptoms (“Feeling down, depressed or hopeless” and “Little interest or pleasure in doing things”). Response options range from not at all (0) to “nearly every day (3)”. Scores are calculated cumulatively for the entire measure and on each separate subscale by summing item responses. The present analysis computed sum scores for the anxiety and depression subscales at each timepoint. Higher scores are indicative of more anxiety and depressive symptom endorsement (α = .85–.88). The anxiety and depressive subscales each use a clinical cut point sum score of 3 to indicate heightened likelihood of clinically significant anxiety or depression; in clinical settings this would serve as a flag for further mental health evaluation.
Perceived Stress Scale
Four items from the widely used 14-item Perceived Stress Scale (Cohen et al., 1983) were administered to assess self-reported stress levels over the past month. The researchers selected items that were most relevant to college student experiences at the time of the assessment to reduce the total items and corresponding participant burden. Items included, how often students felt: “stressed,” “that (they) were effectively coping with important changes (reverse scored),” “found themselves thinking about things (they) have to accomplish,” and “felt difficulties were piling up so high that (they) could not overcome them.” Participant responses ranged from never (0) to very often (4). Mean scores were computed for the present analysis (α = .59). Higher scores indicate more perceived stress prior to March 2020.
COVID-19-Related Challenges with Negative Academic Impact
For the purposes of this project, 13 items were generated by the research team to assess whether students perceived a negative academic impact of various potential challenges unique to COVID-19 and the transition to remote learning. These items were formed in consultation with faculty and undergraduate student members of the research team who were actively teaching or taking courses and hearing first-hand from students about the circumstances impacting their academic experience. Participants were asked “In what ways has the COVID-19 pandemic had a negative impact on your academic experience?” and asked to select all that applied from a list of 13 COVID-19 related challenges. Two items were removed from the composite score due to being endorsed by fewer than 10% of participants and having a minimal impact on reliability. Final items included: remote learning was challenging, concerns about personal health, concerns about friend/family health, moving, lack of access to necessary resources, loss of campus life, loss of involvement in clubs/activities, lack of routine/structure, reduced motivation, uncertainty about the future, and difficulty communicating with faculty/academic advisors. Internal consistency was computed for the final 11 items (α = .75). Responses were coded 0 = no, 1 = yes for each item and summed for the present analysis. Higher scores indicate more experiences of COVID-19-related challenges that participants believed resulted in contributed to academic difficulties.
Loneliness
The 20-item UCLA loneliness scale (Russell et al., 1980) was used to assess subjective feelings of loneliness. This widely used measure has demonstrated internal consistency, concurrent and discriminant validity, and had its factor structure confirmed across different populations (Durak & Senol-Durak, 2010; Hartshorne, 1993). Example items are “I have nobody to talk to” and “I feel isolated from others.” Participant responses ranged from never (0) to often (3). Mean scores were computed for the present analysis (α = .96). Higher scores indicate greater endorsement of loneliness.
Perception of Positive Changes Related to COVID-19
A single item asked, “Has the COVID-19 situation led to any positive changes in your life?” Response options ranged from 1 (not at all) to 7 (several positive changes). Higher scores indicate more positive changes that participants attributed to COVID-19.
Data Analyses
Analyses were conducted using IBM SPSS version 26. Two paired samples t-tests using a 99% confidence interval were conducted to determine whether levels of anxiety and depression scores significantly changed between the time prior to pandemic-related remote learning (T1) and Summer 2020, following the completion of the first semester of remote learning (T2; Hypotheses 1a-1b). Potential moderators of the change in anxiety or depression scores from T1 to T2 were examined using Model 2 of the MEMORE macro (Amanda K. Montoya & Hayes, 2017; Amanda Kay Montoya, 2019; Hypotheses 2-4); with one model being fit to predict change in anxiety and another model to predict change in depression. This model was the most appropriate for the study hypotheses and allowed for examination of each moderator of interest, controlling for the effects of the others. This macro was developed specifically for two-instance repeated measures designs with multiple moderator variables; the procedure computes a pre-post difference score and determines whether the moderator of interest predicts that difference (Judd et al., 2001). The difference was constructed by subtracting T1 anxiety or depression scores from T2 anxiety or depression scores, thus higher scores are reflective of greater endorsement of symptoms during the COVID-19 induced period of remote learning than pre-remote learning. This approach does not require the computation of interaction terms to examine moderating effects. Binary gender was coded such that men represented the reference group (men = 0; women = 1). Non-dichotomous moderator variables (i.e., pre-pandemic stress, COVID-19-related challenges, loneliness, and perception of positive changes in personal life related to pandemic) were mean centered to facilitate interpretation (Aiken et al., 1991). Results reported reflect unit increases on the original metric of the scale. Moderation analyses excluded participants with missing data on any predictor variable, including 19 participants who did not identify with a binary gender and 14 participants with incomplete data on the loneliness measure and 1 participant who did not complete the perception of positive changes, resulting in a sample of 956 for those analyses.
Results
Preliminary Analyses
Descriptive statistics of study variables are shown in Table 1. On average, students reported experiencing over 6 challenges to academic learning (SD = 2.59). Table 2 presents the percentage of participants who endorsed the various COVID-19-related challenges assessed. Correlations between study variables are presented in Table 3.
Table 1.
Descriptive Statistics of Study Variables.
| N | Range | M | SD | Skew | Kurtosis | ||
|---|---|---|---|---|---|---|---|
| PHQ-4 anxiety | |||||||
| T1 | 990 | 0–6 | 2.07 | 1.64 | .88 | .16 | |
| T2 | 990 | 0–6 | 2.64 | 1.82 | .44 | -.74 | |
| PHQ-4 depression | |||||||
| T1 | 990 | 0–6 | 1.38 | 1.50 | 1.34 | 1.72 | |
| T2 | 990 | 0–6 | 2.20 | 1.68 | .72 | −.11 | |
| T1 perceived stress | 990 | 0–4 | 2.26 | .65 | .04 | −.16 | |
| T2 COVID-19 challenges | 990 | 0–11 | 6.34 | 2.59 | −.36 | −.33 | |
| T2 loneliness | 976 | 0–3 | 1.10 | .74 | .34 | −.67 | |
| T2 perception of positive changes | 989 | 1–7 | 4.16 | 1.8 | −.02 | −1.03 | |
Note. T1 data was collected in February-March 2020, prior to the onset of COVID-19 related remote learning. T2 data was collected in July 2020, following the completion of the first semester of COVID-19 related remote learning. COVID-19-related challenges assessed those that participants reported had a negative academic impact.
Table 2.
COVID-19-Related Challenges with Academic Impact Endorsed.
| In what ways has the COVID-19 pandemic had a negative impact on your academic experience? | % Endorsed (N = 990) |
|---|---|
| 1. Lack of routine/structure/schedule | 82.3 |
| 2. Loss of campus life | 80.1 |
| 3. Uncertainty about the future | 75.9 |
| 4. I became less motivated in my academics | 73.7 |
| 5. Loss of involvement in clubs and other activities | 71.7 |
| 6. Remote learning was challenging | 71.4 |
| 7. Moving in the middle of the semester presented challenges that impacted my academics | 44.7 |
| 8. Concerns about the health of my family and friends made it difficult to focus on academics | 41.9 |
| 9. Difficulty communicating with faculty/academic advisors | 41.5 |
| 10. Concerns about my health made it difficult to focus on academics | 25.1 |
| 11. I did not have access to the resources I needed to be successful academically | 24.4 |
Table 3.
Correlations Between Study Variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1.T1 anxiety | - | |||||||
| 2.T2 anxiety | .45** | - | ||||||
| 3.T1 depression | .55** | .33** | - | |||||
| 4.T2 depression | .32** | .65** | .46** | - | ||||
| 5. Gender | .13** | .22** | .02 | .12** | - | |||
| 6. T1 perceived stress | .65** | .40** | .50** | .37** | .17** | - | ||
| 7. T2 COVID-19 challenges | .18** | .42** | .16** | .37** | .19** | .24** | - | |
| 8. T2 loneliness | .28** | .37** | .38** | .50** | −.004 | 26** | .29** | - |
| 9. T2 positive changes | −.03 | −.22** | −.04 | −.26** | −.02 | −.24** | .16** | .04 |
*p<.05, **p<.001.
Changes in Mental Health Symptoms from T1 to T2
Anxiety
Consistent with Hypothesis 1a, there was a significant increase in anxiety symptom scores from T1 (M = 2.07, SD = 1.64) to T2 (M = 2.64, SD = 1.82; t(1, 989) = 9.88, p < 0.001, d = 0.31). Prior to COVID-19-related remote learning, 27.1% of participants scored at least a 3 on the two PHQ items specific to anxiety, the recommended clinical cut point. At T2, 43.5% of the sample met this cut point for anxiety symptoms (a 60.5% increase from the percentage of those scoring at least 3 at T1).
Depression
Consistent with Hypothesis 1b, there was a significant increase in depressive symptoms reported across the two time points (T1 M = 1.38, SD = 1.50; T2 M = 2.20, SD = 1.68; t(1, 989) = 15.49, p < 0.001, d = 0.50). Prior to COVID-19-related remote learning (T1), 13.8% of participants scored at least a 3 on the two PHQ items specific to depression, the recommended clinical cut point. At T2, 30.4% of the sample met this cut point (a 120.3% increase from the percentage scoring at least 3 at T1).
Model Predicting Change in Anxiety Symptoms
Summary statistics for the moderation model including all five moderators of interest are displayed in Table 4. The estimate of the intercept indicates that when all other variables are held constant at zero (i.e., among men, at the mean for all other variables), anxiety scores were expected to be .28 points greater during T2 than T1 (prior to remote learning).
Table 4.
Estimates from Moderation Models Predicting Change in Anxiety and Depression from Pre- to During COVID-19.
| Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|
| F(5, 950) = 39.96, p <.001, R2 = .17 | F(5, 950) = 27.67, p <.001, R2 = .13 | ||||||
| Predictors | B | T | p | B | t | P | |
| Intercept | .28 | 3.17 | <.01 | .59 | 7.08 | <.001 | |
| Gender | .43 | 3.76 | <.001 | .35 | 3.33 | <.001 | |
| COVID-19 challenges | .18 | 7.81 | <.001 | .12 | 5.68 | <.001 | |
| Loneliness | .33 | 4.30 | <.001 | .34 | 4.72 | <.001 | |
| Positive changes | −.14 | −4.30 | <.001 | −.16 | −5.17 | <.001 | |
| Perceived stress | −.86 | −9.70 | <.001 | −.47 | −5.66 | <.001 | |
Note. Degrees of freedom for all regression coefficient estimates is 950.
Gender
Gender was a significant moderator as hypothesized (2a), such that women showed larger increases in anxiety symptoms over time than men. With all other moderators at their mean, women’s anxiety scores were on average .71 points higher at T2, compared to T1.
Perceived Stress
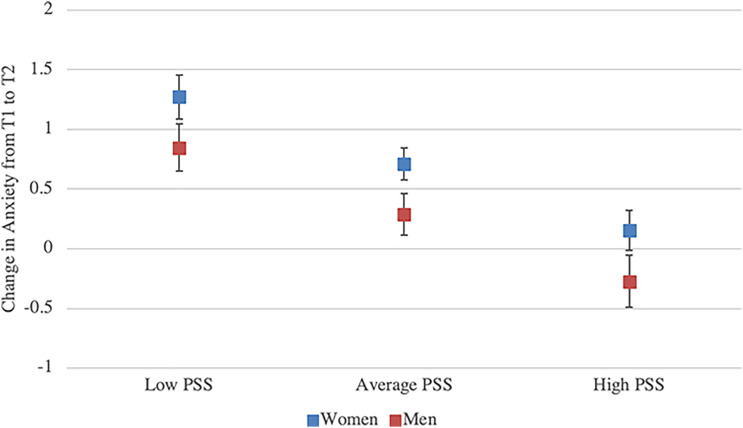
Perceived stress was a significant moderator of changes in anxiety over time. However, the direction of this effect was contrary to Hypothesis 3a. For each unit increase in perceived stress reported at T1, there was a .86 unit decrease in the change in anxiety. With all other predictors held constant, the overall documented increases in anxiety symptoms was blunted among those who were undergoing more perceived stress prior to COVID-19. Figure 1 illustrates the varying impact of perceived stress on the difference in anxiety from T1 to T2, at average perceived stress, and +/−1 SD above and below the average.
Figure 1.
Change in Anxiety from T1 to T2 by Level of Pre-Pandemic Perceived Stress and Gender. Note. This figure represents the predicted change in PHQ-4 anxiety scores from T1 (pre-) to T2 (during-COVID-19) resulting from the analyzed moderation model (see Table 4). Data points represent the estimated change in anxiety at low, average, and high levels of T1 perceived stress (PSS) accounting for academic problems, loneliness, and positive perceptions at their means. At the PSS average, the estimated increase is represented by the constant (.28). Women’s scores reflect greater change from T1 to T2 due to the main effect of gender (.43). Low and high PSS scores represent one standard deviation from the mean. 95% confidence intervals are indicated with error bars.
COVID-19-Related Challenges with Negative Academic Impact
For each unit increase in challenges with a negative academic impact, there was a .18 unit increase in the difference in anxiety from T1 to T2. With all other predictors held constant, individuals with a greater number of challenges with a negative academic impact experienced significantly greater increases in anxiety symptoms over time. For example, at one standard deviation above the mean (8.93 challenges endorsed) this corresponded to a .75 unit increase in anxiety from T1 to T2, while at one standard deviation below the mean (3.75 challenges endorsed) there was a .19 unit decrease in anxiety over this period. This finding is consistent with Hypothesis 4a.
Loneliness
For each unit increase in loneliness, there was a .33 unit increase in the difference in anxiety. With all other predictors held constant, those who reported more loneliness also experienced greater increases in anxiety symptoms over time. At one standard deviation above the mean of loneliness, this corresponded to a .52 unit increase in anxiety over time, as opposed to a .04 unit increase at one standard deviation below the mean of loneliness. This effect is consistent with Hypothesis 5a.
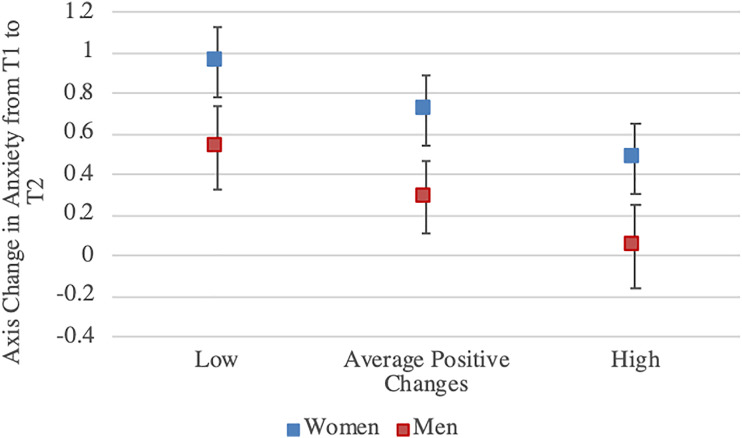
Positive Changes Attributed to COVID-19
For each unit increase in endorsement of positive changes attributed to COVID-19, there was a .14 unit decrease in the change in anxiety. Holding all else constant, the increase in anxiety reported over time was buffered among those who reported more positive changes related to COVID-19. At one standard deviation above the mean of positive changes attributed to COVID-19, the change in anxiety from T1 to T2 was .03. At one standard deviation below the mean, there was a .53 unit increase in anxiety over that time period. Results were consistent with Hypothesis 6a and are illustrated in Figure 2.
Figure 2.
Change in Anxiety from T1 to T2 by Level of Perceived Positive Changes Related to COVID-19 and Gender. Note. This figure represents the predicted change in PHQ-4 anxiety scores from T1 (pre-) to T2 (during-COVID-19) resulting from the analyzed moderation model (see Table 4). Lines representing low, average, and high levels of positive changes related to COVID-19 represent estimated change in anxiety when all other variables in the model are zero (perceived stress, academic problems, and loneliness are at their means). Women’s scores reflect greater change from T1 to T2 due to the main effect of gender (.43). Low and high scores represent one standard deviation from the mean of positive changes attributed to COVID-19. 95% confidence intervals are indicated with error bars.
Model Predicting Change in Depressive Symptoms
Summary statistics for the moderation model including all five moderators of interest are displayed in Table 4. The estimate of the intercept indicates that when all other variables are held constant at zero (i.e., among men, at the mean for all other variables), depressive symptom scores were expected to be greater at T2 by .59 units than at T1 (prior to remote learning).
Gender
Consistent with hypothesis 2b, gender was a significant moderator. Women showed an increase in depressive symptoms over time that was .35 units higher than men.
Perceived Stress
For each unit increase in perceived stress, there was a .47 unit decrease in the difference in depression. This directionality of this finding is opposite of Hypothesis 3b. With all other predictors held constant, the overall increase in depressive symptoms was buffered among those who reported more perceived stress prior to COVID-19.
COVID-19-Related Challenges with Negative Academic Impact
Consistent with Hypothesis 4b, for each unit increase in COVID-19-related challenges experienced, there was a .12 unit increase in the difference in depression. With all other predictors held constant, increases in depressive symptoms over time were exacerbated among those who experienced a greater number of COVID-19-related challenges.
Loneliness
Consistent with Hypothesis 5b, there was evidence of an effect of loneliness, such that for each unit increase in loneliness, there was a .34 unit increase in the difference in depression. With all other predictors held constant, those who reported more loneliness also experienced greater increases in depressive symptoms over time.
Positive Changes Attributed to COVID-19
Consistent with Hypothesis 6b, for each unit increase in endorsement of positive changes attributed to COVID-19, there was a .16 unit decrease in the difference in depression. Holding all else constant, the increase in depressive symptoms reported over time was buffered as reported positive changes increased.
Discussion
The current study offers a prospective analysis of changes in anxiety and depressive symptoms among college students, across the period of time from February-March 2020, before COVID-19 related remote learning was imposed, to July 2020, after the completion of the semester. Potential moderators of change in anxiety or depressive symptoms were also investigated including gender, COVID-19-related challenges with academic impact, loneliness, perceived stress, and perception of positive changes. Consistent with prior work and the study hypotheses, there was a dramatic increase in anxiety and depressive symptoms over the period of time examined and an increase in the proportion of participants meeting the clinical cut-score, with an apparent greater increase in those meeting the cutoff score for depression noted. Women demonstrated larger increases in anxiety and depression symptoms over time than men. COVID-19-related challenges with academic impact and loneliness moderated the effect of time, such that greater challenges and loneliness experienced during remote learning corresponded to greater increases in anxiety and depressive symptoms over time. Also as hypothesized, greater positive changes attributed to COVID-19 buffered against increases in anxiety and depression between T1 and T2. Specifically, the increases in anxiety and depression from T1 to T2 were smaller among those who reported greater positive changes that they attributed to COVID-19.
Unexpectedly, greater perceived stress prior to COVID-19 related to reduced differences in anxiety and depression over time. That is, as T1 perceived stress increased, the expected increase in anxiety and depressive symptoms diminished. Originally, the opposite effect was hypothesized because it was thought that those with greater perceived stress prior to COVID-19 would be vulnerable to the stress of the pandemic. It is possible that those with the highest levels of stress prior to COVID-19 may have experienced some benefit from reductions in the typical demands of daily life as remote learning and social distancing became the norm, consistent with Pearlin’s stress process framework (Pearlin, 2010). If this is the case, these individuals may experience increased difficulty as in-person learning resumes and they are forced to face stressors that social distancing may have allowed them to avoid (Maner & Schmidt, 2006). It is also possible that some type of ceiling effect or regression to the mean may be a factor. While some researchers have suggested abandoning the use of difference scores because of issues such as regression to the mean (Bonate, 2000; Cronbach & Furby, 1970; Twisk & Proper, 2004), others have argued that they have utility (Rogosa, 1995; Thomas & Zumbo, 2012). Ceiling effects refer to a reduced capacity of scores close to the maximum on a given scale to change in comparison to lower values on that scale (Ho & Yu, 2015). Those higher in such symptomatology prior to COVID-19 may have not had as much room for exacerbation in scores. Regression to the mean is a documented phenomenon in which, over time, extreme values have a tendency to be change to be more consistent with average scores (Barnett et al., 2005). Given these statistical phenomena, reductions in anxiety and depression scores among those at high levels of perceived stress, which is highly correlated with psychopathology, should be interpreted with caution. The need for caution when interpreting findings specific to perceived stress is also highlighted by results indicating that the included scale had poor reliability within the present sample.
These findings expand on prior research and identify how changes in mental health symptoms—specifically anxiety and depression—during COVID-19 may vary by other COVID-19 related factors among college students. Students reported experiencing an average of about six challenges to academics and the standard deviation of close to three challenges highlights that the remote learning experience is not homogeneous among college students. Variations in factors that impair academic success during remote learning have the potential to exacerbate increases in mental health problems. Colleges continuing to employ remote learning as a necessary measure for public health should carefully consider how to minimize the potential impact of COVID-19-related challenges on academic performance.
The impact of loneliness on mental health symptoms during COVID-19 in this study is consistent with prior research (Palgi et al., 2020; Ye et al., 2020). Loneliness during the COVID-19 pandemic may be largely attributed to or exacerbated by social distancing measures and associated reductions in personal connection with others (DiGiovanni et al., 2004; Hoffart et al., 2020). To buffer the negative impact of loneliness, college campuses could offer opportunities for safe social connection among college students. Small changes to remote learning, such as professors reserving time during each virtual class for students to connect with one another, may also be effective at enhancing connectedness among students. Relatedly, college students are likely to benefit from guidance on how to build upon and utilize social supports within one’s network, whether in-person or virtually.
The ability to identify positive outcomes associated with the COVID-19 pandemic is an adaptive coping skill and indicative of resilience, and study results indicate it may be protective for mental health. Indeed, a positive outlook or optimism is associated with better mental health (e.g., Kleiman et al., 2017; Rand et al., 2020). Offering training and resources to promote healthy coping skills, such as mindfulness or cognitive restructuring, may be one such avenue to promote positivity during times of stress and challenge, including beyond the COVID-19 pandemic. Admittedly, the specific types of positive changes students experienced were not assessed by this study. It is important to note that some students likely experienced more adversity during the pandemic than others, regardless of their personal outlook and coping skills, and future research should account for these experiences.
Limitations
Results should be examined in the context of study limitations. Though changes in mental health symptoms were measured across the period of time when COVID-19 emerged as a pandemic, no changes can be specifically attributed to the effects of COVID-19 as it was a naturalistic factor faced by all participants. The present work focused on moderating effects to understand if changes in mental health symptoms vary based on other variables that are related to COVID-19. However, predictors do not meet ideal conditions for moderation. Specifically, COVID-19 related potential moderators in the present models (i.e., challenges impacting academics, loneliness, and positive changes) were measured at T2 to assess experiences during remote learning and are correlated with mental health variables. Though these factors were examined as moderators in the present work in order to examine the hypotheses of interest, future work should consider whether these factors may be involved in indirect effects of mental health over time (i.e., mediation).
The present work’s longitudinal design is a benefit over cross-sectional designs; however, the use of only two timepoints does not allow for examination of trajectories. Following a serious stressor, many individuals experience an increase in psychopathology, some experience a delayed increase in psychopathology, and some are resilient following exposure. Of those who experience an increase, some experience short-term distress while others’ are impacted more chronically (Chen & Bonanno, 2020). Future research should examine trajectories of symptoms and resilience with three or more timepoints and other analytic techniques, such as latent class analysis.
Self-report was an ideal methodology for the present work due to the interest in understanding participants’ perceptions and experiences. However, given the novelty of COVID-19, at the time of data collection there were not validated measures of some of the constructs of interest. As a result, the research team developed items for COVID-19 related challenges with academic impact and positive changes related to COVID-19. The perceived stress items included in this work were selected from the validated PSS (Cohen et al., 1983), but no published work has examined this subset psychometrically. Simple evaluation of Cronbach’s alpha indicated that selected items have low internal consistency, though quantitative experts recognize that this metric can demonstrate a low value if there are few items in the scale and heterogeneity across items (Tavakol & Dennick, 2011). Future work should examine changes in mental health symptoms over time using a more valid measure of stress.
T1 data was collected when COVID-19 cases were present in the United States, but just prior to the first community-level mitigation recommendations on March 15, when the CDC released guidance to cancel events with 50 or more people, and on March 16, when the White House announced voluntary guidance for social distancing and gatherings no larger than 10 people. On March 16, the study university canceled classes and transitioned to remote learning. Though the lives of our participants were not disrupted directly by COVID-19-related community-level mitigation recommendations such as social distancing and remote learning until after the T1 data collection period, it is possible that concern about COVID-19 during the T1 data collection period led to differences in endorsement of anxiety and depressive symptoms from participants’ true baseline.
The present sample consists of college students attending a private institution in the northeast, predominantly comprised of White and Asian individuals. Findings resulting from this group may not generalize to other groups. For example, COVID-19 has led to disproportionate hospitalization and death among Black individuals in the United States (Selden & Berdahl, 2020), which may contribute to unique mental health needs (Novacek et al., 2020). Non-college young adults have faced distinct stressors and not experienced concern about academic impact. Further, different colleges and regions of the United States varied widely in their COVID-19 response, which could result in distinct mental health trajectories.
Conclusions
The present findings expand upon the literature by identifying moderators that exacerbate and buffer against the overall increases in anxiety and depression that have been documented since the introduction of COVID-19. Results suggest that COVID-19-related challenges with academic impact and loneliness relate to a worsened decline in mental health among college students. These factors should be targeted by mental health workers and educators serving college students during this time. Alternatively, stronger endorsement of positive changes in one’s life due to COVID-19 was protective. Though the degree of adversity experienced during COVID-19 likely impacts one’s ability to endorse positive changes, being able to identify positive factors within difficult situations is a cognitive skill that can be strengthened to promote resilience (Clark, 2013). Unexpectedly, perceived stress prior to COVID-19 served a buffering effect on the difference in anxiety and depression over time. Though those with the highest levels of stress prior to COVID-19 may have experienced some relief in the short term, it is unknown what will happen to these individuals when pre-remote learning activities resume. Additional longitudinal research is needed to understand the long-term consequences of the pandemic on college students’ mental health, and to understand the adjustment back to more in-person learning and social experiences as vaccines are distributed.
Author’s Contribution: Haikalis, M: contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.Doucette, H; contributed to interpretation; drafted manuscript; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.Meisel, M; contributed to design; contributed to acquisition and analysis; drafted manuscript; critically revised manuscript; agrees to be accountable for all aspects of work ensuring integrity and accuracy.Birch, K; contributed to acquisition; drafted manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.Barnett, N; contributed to conception and design; contributed to interpretation; critically revised manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (2R01AA023522, PI: Barnett; T32AA007459, PI: Monti).
Open Practices: The raw, de-identified data, analysis code, and materials used in this study are not openly available but are available upon request to the corresponding author. This study did not include a pre-registration plan for data collection and analysis.
ORCID iDs
Michelle Haikalis https://orcid.org/0000-0003-1062-5314
Matthew K. Meisel https://orcid.org/0000-0003-2035-9291
References
- Aiken L., West S., Reno R. (1991). Multiple regression: Testing and interpreting interactions. SAGE Publications. [Google Scholar]
- Alonzi S., Torre A. L., Silverstein M. W. (2020). The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(1), 236–238. 10.1037/tra0000840 [DOI] [PubMed] [Google Scholar]
- Barnett A. G., van der Pols J. C., Dobson A. J. (2005). Regression to the mean: What it is and how to deal with it. International Journal of Epidemiology, 34(1), 215–220. 10.1093/ije/dyh299 [DOI] [PubMed] [Google Scholar]
- Besser A., Flett G. L., Zeigler-Hill V. (2020). Adaptability to a sudden transition to online learning during the COVID-19 pandemic: Understanding the challenges for students. In Scholarship of Teaching and Learning in Psychology. American Psychological Association, undefined(undefined), undefined. 10.1037/stl0000198 [DOI] [Google Scholar]
- Bonate P. L. (2000). Analysis of pretest-posttest designs (1st ed.). New York: Chapman and Hall/CRC. [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S., Bonanno G. A. (2020). Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S51. 10.1037/tra0000685 [DOI] [PubMed] [Google Scholar]
- Clark D. A. (2013). Cognitive restructuring. In The Wiley Handbook of Cognitive Behavioral Therapy (pp. 1–22). John Wiley & Sons, Ltd. 10.1002/9781118528563.wbcbt02 [DOI] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Colodro-Conde L., Couvy-Duchesne B., Zhu G., Coventry W. L., Byrne E. M., Gordon S., Wright M. J., Montgomery G. W., Madden P. A. F., Ripke S., Eaves L. J., Heath A. C., Wray N. R., Medland S. E., Martin N. G. (2018). A direct test of the diathesis–stress model for depression. Molecular Psychiatry, 23(7), 1590–1596. 10.1038/mp.2017.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronbach L. J., Furby L. (1970). How we should measure“ change”: Or should we? Psychological Bulletin, 74(1), 68-80. 10.1037/h0029382 [DOI] [Google Scholar]
- DiGiovanni C., Conley J., Chiu D., Zaborski J. (2004). Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecurity and Bioterrorism : Biodefense Strategy, Practice, and Science, 2(4), 265–272. 10.1089/bsp.2004.2.265 [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases, 20(5), 533–534. 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durak M., Senol-Durak E. (2010). Psychometric qualities of the UCLA loneliness scale-version 3 as applied in a Turkish culture. Gerontology, 36(10-11), 988-1007. 10.1080/03601271003756628 [DOI] [Google Scholar]
- Ellis W. E., Dumas T. M., Forbes L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science, 52(3), 177–187. 10.1037/cbs0000215 [DOI] [Google Scholar]
- Elmer T., Mepham K., Stadtfeld C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One, 15(7), e0236337. 10.31234/OSF.IO/UA6TQ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faravelli C., Lo Sauro C., Lorenzo L., Francesco P., Lazzeretti L., Godini L., Benni L., Fioravanti G., Talamba G. A., Castellini G., Ricca V. (2012). The role of life events and hpa axis in anxiety disorders: a review. Current Pharmaceutical Design, 18(35), 5663–5674. 10.2174/138161212803530907 [DOI] [PubMed] [Google Scholar]
- Ghebreyesus T. A. (2020). Addressing mental health needs: an integral part of COVID-19 response. World psychiatry, 19(Issue 2), 129–130. 10.1002/wps.20768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillis A., Krull L. M. (2020). COVID-19 remote learning transition in spring 2020: Class structures, student perceptions, and inequality in college courses. Teaching Sociology, 48(4), 283–299. 10.1177/0092055X20954263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J., Prinstein M., Abramowitz J., Albano A. M., Aldao A., Borelli J., Clark L. A., Davila J., Forbes E., Gee D., Hall G. N., Hallion L., Hinshaw S., Hofmann S., Hollon S., Joormann J., Kazdin A., Klein D., Levenson R., Weinstock L. M. (2020). Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist, 76(3), 409–426. 10.31234/osf.io/desg9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza C. A., Ewing L., Heath N. L., Goldstein A. L. (2021). When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Canadian Psychology/Psychologie Canadienne, 62(1), 20–30. 10.1037/cap0000255 [DOI] [Google Scholar]
- Hartshorne T. S. (1993). Psychometric properties and confirmatory factor analysis of the UCLA Loneliness Scale. Journal of Personality Assessment, 61(1), 182-195. 10.1207/s15327752jpa6101_14 [DOI] [PubMed] [Google Scholar]
- Hoffart A., Johnson S. U., Ebrahimi O. V. (2020). Loneliness and social distancing during the COVID-19 pandemic: Risk factors and associations with psychopathology. Frontiers in Psychiatry, 11, 589127. 10.3389/fpsyt.2020.589127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho A. D., Yu C. C. (2015). Descriptive statistics for modern test score distributions: Skewness, kurtosis, discreteness, and ceiling effects. Educational and Psychological Measurement, 75(3), 365–388. 10.1177/0013164414548576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd C. M., Kenny D. A., McClelland G. H. (2001). Estimating and testing mediation and moderation in within-subject designs. Psychological Methods, 6(2), 115–134. 10.1037/1082-989X.6.2.115 [DOI] [PubMed] [Google Scholar]
- Khubchandani J., Brey R., Kotecki J., Kleinfelder J., Anderson J. (2016). The psychometric properties of PHQ-4 depression and anxiety screening scale among college students. Archives of Psychiatric Nursing, 30(4), 457-462. 10.1016/j.apnu.2016.01.014 [DOI] [PubMed] [Google Scholar]
- Kleiman E. M., Chiara A. M., Liu R. T., Jager-Hyman S. G., Choi J. Y., Alloy L. B. (2017). Optimism and well-being: a prospective multi-method and multi-dimensional examination of optimism as a resilience factor following the occurrence of stressful life events. Cognition and Emotion, 31(2), 269–283. 10.1080/02699931.2015.1108284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., Williams J. B. W., Löwe B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics, 50(6), 613–621. 10.1016/s0033-3182(09)70864-3 [DOI] [PubMed] [Google Scholar]
- Maner J. K., Schmidt N. B. (2006). The role of risk avoidance in anxiety. Behavior Therapy, 37(2), 181–189. 10.1016/j.beth.2005.11.003 [DOI] [PubMed] [Google Scholar]
- Montoya A. K. (2019). Moderation analysis in two-instance repeated measures designs: Probing methods and multiple moderator models. Behavior Research Methods, 51(1), 61–82. 10.3758/s13428-018-1088-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montoya A. K., Hayes A. F. (2017). Two-condition within-participant statistical mediation analysis: A path-analytic framework. Psychological Methods, 22(1), 6–27. 10.1037/met0000086 [DOI] [PubMed] [Google Scholar]
- Novacek D. M., Hampton-Anderson J. N., Ebor M. T., Loeb T. B., Wyatt G. E. (2020). Mental health ramifications of the COVID-19 pandemic for black Americans: Clinical and research recommendations. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 449. 10.1037/tra0000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. (2020). The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. Journal of Affective Disorders, 275, 109–111). 10.1016/j.jad.2020.06.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L. I. (2010). The life course and the stress process: Some conceptual comparisons. Journals of Gerontology - Series B Psychological Sciences and Social Sciences, 65 B(2), 207–215. 10.1093/geronb/gbp106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K. M. (2020). Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prowse R., Sherratt F., Abizaid A., Gabrys R. L., Hellmans K. G., Patterson Z. R., McQuaid R. J. (2021). Coping With the COVID-19 Pandemic: Examining Gender Differences in Stress and Mental Health Among University Students. Frontiers in Psychiatry, 12. 10.3389/fpsyt.2021.650759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General PsychiatryBMJ Publishing Group, 33(Issue 2), 100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand K., Kurth M., Fleming C. H., Linkov I. (2020). A resilience matrix approach for measuring and mitigating disaster-induced population displacement. International Journal of Disaster Risk Reduction, 42, 101310. 10.1016/j.ijdrr.2019.101310 [DOI] [Google Scholar]
- Rogosa D. (1995). Myths and methods: “Myths about longitudinal research” plus supplemental questions. In The analysis of change. Lawrence Erlbaum Associates, Publishers. [Google Scholar]
- Russell D., Peplau L. A., Cutrona C. E. (1980). The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Selden T. M., Berdahl T. A. (2020). COVID-19 And Racial/Ethnic Disparities In Health Risk, Employment, And Household Composition: Study examines potential explanations for racial-ethnic disparities in COVID-19 hospitalizations and mortality. Health Affairs, 39(9), 1624-1632. 10.1377/hlthaff.2020.00897 [DOI] [PubMed] [Google Scholar]
- Tavakol M., Dennick R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas D. R., Zumbo B. D. (2012). Difference scores from the point of view of reliability and repeated-measures ANOVA: In defense of difference scores for data analysis. Educational and Psychological Peasurement, 72(1), 37-43. 10.1177/0013164411409929 [DOI] [Google Scholar]
- Twisk J., Proper K. (2004). Evaluation of the results of a randomized controlled trial: how to define changes between baseline and follow-up. Journal of Clinical Epidemiology, 57(3), 223-228. 10.1016/j.jclinepi.2003.07.009 [DOI] [PubMed] [Google Scholar]
- van der Velden P. G., Contino C., Das M., van Loon P., Bosmans M. W. G. (2020). Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. Journal of Affective Disorders, 277, 540–548. 10.1016/j.jad.2020.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C. S., Ho R. C. (2020. a). Immediate Psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Hegde S., Son C., Keller B., Smith A., Sasangohar F. (2020. b). Investigating mental health of US college students during the COVID-19 pandemic: Cross-sectional survey study. Journal of Medical Internet Research, 22(9), e22817. 10.2196/22817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye Z., Yang X., Zeng C., Wang Y., Shen Z., Li X., Lin D. (2020). Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Applied psychology: Health and well-being. aphw.12211. Advance online publication. 10.1111/aphw.12211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zacher H., Rudolph C. W. (2020). Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. American Psychologist, 76(1), 50–62. 10.1037/amp0000702 [DOI] [PubMed] [Google Scholar]