Abstract
Background
Thousands of school systems have struggled with the decisions about how to deliver education safely and effectively amid the COVID19 pandemic. This study evaluates the public health impact of various school reopening scenarios (when, and how to return to in-person instruction) on the spread of COVID19.
Methods
An agent-based simulation model was adapted and used to project the impact of various school reopening strategies on the number of infections, hospitalizations, and deaths in the state of Georgia during the study period, i.e., February 18th-November 24th, 2020. The tested strategies include (i) schools closed, i.e., all students receive online instruction, (ii) alternating school day, i.e., half of the students receive in-person instruction on Mondays and Wednesdays and the other half on Tuesdays and Thursdays, (iii) alternating school day for children, i.e., half of the children (ages 0-9) receive in-person instruction on Mondays and Wednesdays and the other half on Tuesdays and Thursdays, (iv) children only, i.e., only children receive in-person instruction, (v) regular, i.e., all students return to in-person instruction. We also tested the impact of universal masking in schools.
Results
Across all scenarios, the number of COVID19-related deaths ranged from approximately 8.8 to 9.9 thousand, the number of cumulative infections ranged from 1.76 to 1.96 million for adults and 625 to 771 thousand for children and youth, and the number of COVID19-related hospitalizations ranged from approximately 71 to 80 thousand during the study period. Compared to schools reopening August 10 with a regular reopening strategy, the percentage of the population infected reduced by 13%, 11%, 9%, and 6% in the schools closed, alternating school day for children, children only, and alternating school day reopening strategies, respectively. Universal masking in schools for all students further reduced outcome measures.
Conclusions
Reopening schools following a regular reopening strategy would lead to higher deaths, hospitalizations, and infections. Hybrid in-person and online reopening strategies, especially if offered as an option to families and teachers who prefer to opt-in, provide a good balance in reducing the infection spread compared to the regular reopening strategy, while ensuring access to in-person education.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-022-12910-w.
Keywords: COVID19, Pandemic, Public health, School reopening, Non-pharmaceutical interventions, Agent-based disease modeling
Background
School systems have developed plans for safely reopening during the fall semester of 2020 while considering the potential impact of in-person interactions on students, staff, families, and public health during the COVID19 pandemic [1–3]. Studies have shown the potential benefits of non-pharmaceutical interventions, such as school and workplace closures [4–7], in slowing down infection spread and reducing the severe health outcomes, but also highlighted their negative impact on the economy, unemployment, mobility, mental health, education, caregiving, etc. [8–10]. Widespread school closures during spring 2020 not only impacted the education of students but also had social and economic consequences, e.g., due to increased childcare responsibilities of working parents [11–19]. In addition, increased childcare responsibilities may also lead to worker absenteeism in healthcare and further exacerbate the already stressed healthcare system [20].
Agent-based models capture complex interactions and processes, such as interventions, adaptive behaviors, and contextual effects across subpopulations [21]. They are particularly helpful in forecasting the spread of emerging infectious diseases by coalescing disease dynamics, pharmaceutical and non-pharmaceutical interventions, and social behaviors, potentially leading to a better understanding of the disease spread and corresponding actions [22]. In this study, we adapted an agent-based simulation model to predict public health outcomes (e.g., number of community-wide infections, hospitalizations, and deaths) under various school reopening scenarios. School reopening scenarios considered different in-person versus online participation options and interventions, such as symptom-based self-isolation and universal masking in schools.
We considered school reopening scenarios for the fall semester of 2020 in the state of Georgia. At this time, COVID19 infections were on the rise due to social unrest and increased mobility [23–27]. Further, vaccines were not widely available [28] and data on levels of compliance with social distancing measures was unreliable [29, 30]. While we use fall 2020 as a template for our study, the methods and insights are applicable to future pandemic situations when cases are on the rise and information is limited. The insights of our study would also be helpful if a major variant of the SARS-CoV-2 virus emerges and significantly reduces the effectiveness of existing vaccines.
The objective of this study is to quantify the public health outcomes (deaths, hospitalizations, and infections) of various school reopening scenarios to measure their impact on the spread of a pandemic in an effort to provide much-needed insights for school system decision-makers amid an ongoing pandemic.
Methods
Model description
The results were obtained by adapting and utilizing an agent-based simulation model to predict the spread of COVID19 geographically and over time [31–34]. An agent-based simulation model is a computational model that simulates a number of autonomous “agents”, where each agent represents an individual in the population, and the model mimics the dynamics and outcomes of a real system under certain assumptions. The study population represented in the model consisted of children (ages 0-9), youth (ages 10-19), adults (ages 20-64), and elderly (ages 65+), mimicking the population characteristics in the state of Georgia. The state of Georgia has a total population of approximately 10.8 million where 1.3 million are children and 1.4 million are youth [35]. The simulation consisted of one million agents (i.e., approximately one agent per ten individuals with similar characteristics in the population), to capture the population dynamics while keeping the run times reasonable. The model captured the progression of the disease in an individual and interactions within households, workplaces, schools, and communities. All children and youth ages 0-19 in Georgia were assumed to be in a peer group of similar age (e.g., school, daycare, etc.). School-based peer interactions occur between individuals within their assigned age groups. Peer groups were chosen on average as 14, 20, and 30 students for age groups 0-4, 5-9, and 10-19, respectively, following average class sizes reported in Georgia [36]. Interactions between different age groups occur within household and community settings. The model enabled the testing of scenarios incorporating various types and durations of physical distancing interventions, namely school closures, shelter-in-place, voluntary quarantine of households (i.e., the entire household remains home if there is a person in the household with cold/flu-like symptoms), and masking. These interventions are defined as follows:
Shelter-in-place: Staying home and refraining from interactions outside of the household.
Voluntary quarantine: Members of a household stay home if there is a person in the household with cold/flu-like symptoms, until the entire household is symptom-free.
Voluntary shelter-in-place: An entire household chooses to remain home, even if there is no shelter-in-place order, and regardless of symptoms.
Voluntary masking: Wearing a face covering/mask while interacting outside of the household.
Additionally, we considered the following school-based interventions:
Symptom-based self-isolation: Students who present with COVID19 symptoms do not engage in school-based peer interactions.
Universal masking in schools: All students are required to wear a face covering/mask while attending in-person instruction. Masks are assumed to reduce the infectivity and susceptibility of individuals by 50%.
The model captures the public’s varying level of compliance with these interventions [37–39] using the demographic and workflow information at the census tract level in Georgia. The initial infections “seeds” follow the distribution of the total number of confirmed COVID19 cases in Georgia (as of May 15, 2020) [29, 40]. Additional information about the model and the data sources can be found in Supplementary Section A and Supplementary Fig. 1, Additional File 1, and in [31, 32]. The study period is from February 18 to November 24, 2020.
School reopening strategies
Schools closed: All students receive online instruction.
Alternating school day: Half of the students receive in-person instruction on Mondays and Wednesdays and the other half on Tuesdays and Thursdays.
Alternating school day for children: Half of the children (ages 0-9) receive in-person instruction on Mondays and Wednesdays and the other half on Tuesdays and Thursdays.
Children only: Only children receive in-person instruction.
Regular: All students return to in-person instruction.
On each day, the school status (“attending in-person" or “attending online”) of children (0-9) and youth (10-19) was tracked and updated in the simulation depending on the chosen school reopening strategy (see Fig. 1 for the description of school reopening strategies). Students “attending online” did not engage in school-based peer interactions and are assumed to stay at home while still interacting in the community.
Fig. 1.
Description of school reopening strategies
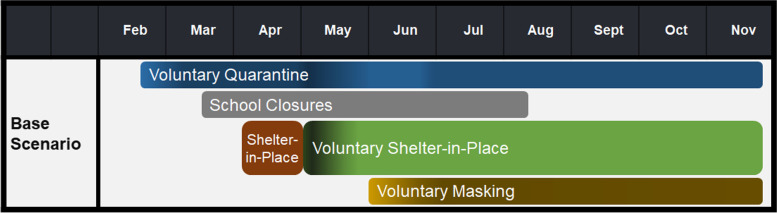
Scenario descriptions
To model the spread of COVID19 in the state of Georgia prior to the start of the fall semester of 2020, the simulation incorporated school closures during March 16- August 10 [41] and physical distancing practices for the entire population with varying levels of compliance (see Fig. 2). In Georgia, the shelter-in-place order was in place during April 3-30, 2020. Shelter-in-place compliance of 80% was assumed for that time period [31]. Voluntary quarantine compliance was 30% in mid-February, increased by 10% weekly until mid-March, and remained at 60% until the end of April. After the end of shelter-in-place, voluntary quarantine compliance was 70% and decreased by 10% weekly until stabilizing at 50% with 40% during the weeks of social unrest (from May 29th to June 23rd, 2020) [23–26]. During the week after the end of shelter-in-place, voluntary shelter-in-place compliance was 60% and decreased to 40%, 20%, and 5%, in consecutive weeks, until stabilizing at 5%. We assume that masks reduce the infectivity and susceptibility of individuals by 50% [42]. In the first two weeks of June, mask compliance in peer groups and the community is assumed to be 20%, later increasing 10% weekly until reaching 60% compliance [43, 44]. Voluntary shelter-in-place and voluntary quarantine compliance levels in the model were chosen to be in line with social mobility indicators [27]. A validation of our model results can be found in Supplementary Section B and Supplementary Fig. 2, Additional File 1.
Fig. 2.
Base Scenario. All scenarios considered are built upon the base scenario along with the corresponding school reopening date. Compliance with shelter-in-place, voluntary quarantine, and voluntary shelter-in-place varies over time
The first set of scenarios considered in this study were each school reopening strategy with different reopening dates. Kindergarten through 12th grade (K-12) schools typically open during the first or second week of August in Georgia; hence, the following reopening dates were considered; August 10, August 17, August 24, August 31, September 7, and September 14 (represented with numbers 1 through 6, respectively, in scenario labeling). In the tables and figures that follow, these scenarios were labeled by their names, as well as numbers 1 through 6. For example, Alternating School Day 3 refers to the scenario in which schools are reopened on August 24 and students adhere to an alternating school day reopening strategy.
In the next set of scenarios, we fixed the reopening date to August 10 and considered each school reopening strategy, along with universal masking in schools. In the tables and figures that follow, these scenarios are labeled by their names, followed by M to denote the inclusion of universal masking in schools (e.g., Children Only M).
All scenarios tested were built upon the base scenario described in Fig. 2 and students adhere to symptom-based self-isolation.
Outcome measures
The infection spread outcome measures during the study period included:
New daily infections: Number of people infected with COVID19 on a given day.
Cumulative infections: Cumulative number of people infected (including asymptomatic infections).
Infection attack rate (IAR): Cumulative percentage of the population infected.
Peak day: The day when the number of new infections was highest.
Peak infection: The number of the population infected on the peak day.
Cumulative deaths: Cumulative number of people who died due to COVID19.
Cumulative hospitalizations: Cumulative number of people hospitalized due to COVID19.
Results
Depending on the school reopening date and strategy, school-based and other interventions, and the public’s compliance with physical distancing, the number of COVID19-related deaths during the study period could range from approximately 8.8 to 9.9 thousand in the state of Georgia and the number of cumulative infections could range from 1.76 to 1.96 million for adults and 625 to 771 thousand for children and youth. The number of COVID19-related hospitalizations could range from approximately 71 to 80 thousand. Compared to all other scenarios, under the regular reopening strategy with a reopening date of August 10, on average, the peak infection in children and youth is 21% higher and the peak day is August 22 (almost one month later than that of other scenarios). Tables 1 and 2 provide results for outcome measures under all scenarios considered.
Table 1.
Outcome measures across scenarios without universal masking in schools
| Reopening Date | Reopening Strategy | Cumulative Deaths | Cumulative Hosp. | Cumulative Infections | IAR % | Peak Infections | Peak Day | ||
|---|---|---|---|---|---|---|---|---|---|
| Children & Youth | Adult | Children & Youth | Adult | ||||||
| - | Schools Closed | 8894 | 71658 | 625238 | 1757331 | 22.06 | 4685 | 13553 | 21-Jul |
| 1 | Alternating School Day for Children | 9032 | 73148 | 646753 | 1794362 | 22.61 | 4785 | 13699 | 24-Jul |
| 2 | 9147 | 73281 | 643065 | 1789006 | 22.52 | 4682 | 13778 | 20-Jul | |
| 3 | 8976 | 72799 | 640933 | 1782047 | 22.44 | 4763 | 13725 | 27-Jul | |
| 4 | 8884 | 72243 | 636193 | 1773745 | 22.32 | 4633 | 13436 | 28-Jul | |
| 5 | 8983 | 72780 | 636659 | 1780587 | 22.39 | 4764 | 13728 | 23-Jul | |
| 6 | 9146 | 73085 | 638953 | 1787263 | 22.47 | 4775 | 13669 | 24-Jul | |
| 1 | Alternating School Day | 9458 | 76563 | 699242 | 1870620 | 23.80 | 4834 | 13861 | 24-Jul |
| 2 | 9381 | 75569 | 685670 | 1850710 | 23.49 | 4731 | 13742 | 24-Jul | |
| 3 | 9255 | 75041 | 676364 | 1831377 | 23.22 | 4642 | 13627 | 26-Jul | |
| 4 | 9154 | 74134 | 667963 | 1818019 | 23.02 | 4681 | 13526 | 22-Jul | |
| 5 | 9211 | 74077 | 664232 | 1814629 | 22.96 | 4819 | 13773 | 24-Jul | |
| 6 | 9149 | 73483 | 656232 | 1800472 | 22.75 | 4650 | 13606 | 23-Jul | |
| 1 | Children Only | 9272 | 74227 | 668797 | 1818029 | 23.03 | 4718 | 13634 | 24-Jul |
| 2 | 9226 | 74282 | 663668 | 1814065 | 22.95 | 4789 | 13726 | 24-Jul | |
| 3 | 9068 | 73680 | 656247 | 1797326 | 22.72 | 4749 | 13684 | 24-Jul | |
| 4 | 9195 | 73555 | 656817 | 1806753 | 22.81 | 4755 | 13819 | 24-Jul | |
| 5 | 8911 | 72094 | 639715 | 1762858 | 22.25 | 4587 | 13405 | 23-Jul | |
| 6 | 9149 | 73270 | 645458 | 1791968 | 22.57 | 4691 | 13814 | 21-Jul | |
| 1 | Regular | 9744 | 80263 | 778272 | 1962672 | 25.38 | 5721 | 12728 | 22-Aug |
| 2 | 9799 | 79422 | 760373 | 1941517 | 25.02 | 4677 | 13731 | 26-Jul | |
| 3 | 9642 | 78414 | 745511 | 1924197 | 24.72 | 4713 | 13683 | 23-Jul | |
| 4 | 9531 | 77770 | 730702 | 1903714 | 24.40 | 4748 | 13994 | 22-Jul | |
| 5 | 9351 | 76124 | 711876 | 1871483 | 23.92 | 4838 | 13948 | 24-Jul | |
| 6 | 9296 | 74954 | 691499 | 1837665 | 23.42 | 4698 | 13704 | 23-Jul | |
Summary comparison of school reopening scenarios without universal masking in schools with respect to cumulative deaths and hospitalizations in the total population, cumulative infections in adults and children/youth, infection attack rate (IAR) in the total population, peak infections in adults and children/youth, and peak day in the total population. Numbers 1-6 correspond to dates Aug 10, Aug 17, Aug 24, Aug 31, Sept 7, and Sept 14, respectively
Table 2.
Outcome measures across scenarios with universal masking in schools
| Reopening Strategy | Cumulative Deaths | Cumulative Hosp. | Cumulative Infections | IAR % | Peak Infections | Peak Day | ||
|---|---|---|---|---|---|---|---|---|
| Children & Youth | Adult | Children & Youth | Adult | |||||
| Schools Closed | 8894 | 71658 | 625238 | 1757331 | 22.06 | 4685 | 13553 | 21-Jul |
| Alternating School Day for Children | 9113 | 73329 | 645689 | 1793551 | 22.59 | 4854 | 14018 | 26-Jul |
| Alternating School Day | 9390 | 75805 | 689727 | 1855026 | 23.57 | 4728 | 13805 | 27-Jul |
| Children Only | 9240 | 73847 | 669356 | 1811767 | 22.98 | 4687 | 13679 | 24-Jul |
| Regular | 9883 | 79734 | 771052 | 1950509 | 25.20 | 4660 | 13463 | 27-Jul |
Summary comparison of school reopening strategies with universal masking during in-person education with respect to cumulative deaths and hospitalizations in the total population, cumulative infections in adults and children/youth, infection attack rate (IAR) in the total population, peak infections in adults and children/youth, and peak day in the total population
Impact of school reopening date
Delaying the school reopening date provided the greatest benefit when implementing a regular reopening strategy. Under the regular reopening strategy, delaying the reopening date by one week reduced the cumulative infections in children and youth by at most 3% and reduced all other outcome measures (cumulative deaths, hospitalizations, and cumulative infections in adults) by at most 2%. Delaying the school reopening date by 5 weeks reduced the cumulative deaths by 5%, cumulative hospitalizations by 7%, cumulative infections in children and youth by 11%, and cumulative infections in adults by 6%. In all other reopening strategies considered, delaying the school reopening date didn’t provide as much benefit compared to the regular reopening strategy. On average, across all school reopening strategies, delaying the reopening date by one week provided a 0.39% reduction in cumulative deaths, a 0.61% reduction in hospitalizations, a 1.13% reduction in cumulative infections in children and youth, and a 0.61% reduction in cumulative infections in adults. Fig. 3 presents a comparison of daily new infections under different reopening dates for a given school reopening strategy.
Fig. 3.
Impact of reopening date given a reopening strategy. Daily new COVID19 infections with different reopening dates under the regular, children only, alternating school day, and alternating school day for children reopening strategies
Impact of school reopening strategies
Compared to schools reopening on August 10 with a regular reopening strategy, the percentage of the population infected reduced by 13%, 11%, 9%, and 6% in the schools closed, alternating school day for children, children only, and alternating school day reopening strategies, respectively.
For the reopening date of August 10, compared to the schools closed reopening strategy:
Deaths increased by 138, 379, 564, and 851 in the alternating school day for children only, children only, alternating school day, and regular reopening strategies, respectively.
Hospitalizations increased by 1,490; 2,569; 4,905; and 8,605 in the alternating school day for children only, children only, alternating school day, and regular reopening strategies, respectively.
Cumulative infections in children and youth increased by 21,514; 43,558; 74,000; and 153,033 in the alternating school day for children only, children only, alternating school day, and regular reopening strategies, respectively.
Cumulative infections in adults increased by 37,031; 60,698; 113,289; and 205,341 in the alternating school day for children only, children only, alternating school day, and regular reopening strategies, respectively.
Results for other reopening dates are similar to those presented above. Fig. 4 shows a comparison of the daily new infections under different school reopening strategies while fixing the reopening dates to August 10, August 17, August 24, and August 31.
Fig. 4.
Impact of reopening strategy given a reopening date. Daily new COVID19 infections with different reopening strategies under the reopening dates of Aug 10, Aug 17, Aug 24, Aug 31
Impact of universal masking in schools
Figure 5 presents a comparison of the daily new infections under different school reopening strategies with and without universal masking in schools. For the reopening date of August 10, universal masking in schools decreased deaths by at most 0.72%, hospitalizations by at most 0.99%, cumulative infections in children and youth by at most 1.36%, and cumulative infections in adults by at most 0.83%. On average, universal masking in schools reduced the cumulative infections in children and youth and in adults by 0.59% and 0.46%, respectively. The addition of universal masking in schools to school reopening strategies reduced outcome measures; however, compared to the schools closed reopening strategy, deaths, hospitalizations, and cumulative infections were higher by 2-3%, 3-7%, 6-10%, and 11-23% in the alternating school day for children, children only, alternating school day, and regular school reopening strategies, respectively.
Fig. 5.
Impact of universal masking in school. Daily new COVID19 infections with different reopening strategies with or without universal masking in schools under the reopening date of Aug 10
Discussion
Governments and school systems have grappled with the decisions of how to prepare students for academic success while also trying to minimize the spread of COVID19. While individuals younger than 20 seemed to be less affected by COVID19 than adults, they could be transmitters of COVID19, potentially increasing community infection spread if schools were to return to in-person instruction [6, 19, 45], particularly considering the challenges in the implementation of social distancing measures and recommendations for some schools (e.g., poor ventilation in buildings, short supply of disinfectant products, state budget shortfalls, etc.) [1, 10].
The negative impact of school closures has been disproportionately high on some students, e.g., those who do not have access to technology in the household, lack proper childcare, face an unsafe home environment, or have traditionally relied on the school system for meals, special education, counseling, and other forms of social or emotional support [10, 46]. School closures could lead to numerous unintended negative consequences as well, such as increased worker absenteeism among parents; higher worker absenteeism within the healthcare system could increase case-fatality risk and the overall mortality rate due to the pandemic [12].
Prior to the start of the fall semester in 2020, guidelines in the state of Georgia recommended for districts with high case numbers to reopen schools with online instruction. However, online instruction poses numerous challenges. Several rural counties have limited internet connectivity; for example, Hancock County ranked number six for COVID19 cases per capita yet only 2% of the county has access to broadband internet [47]. Two-thirds of students in Georgia are not able to read proficiently by the end of third grade; limited or no access to in-person instruction in the fall could further increase this educational gap, with significant long-term consequences [10, 48]. Further, in Georgia, over half of the students are eligible for free and reduced fee school lunches and many families depend on these services [49].
There has been considerable debate about the benefits and risks of when and how to return to in-person instruction in schools during fall 2020. The American Academy of Pediatrics “strongly advocates that all policy considerations for the coming school year should start with a goal of having students physically present in school [50].” Some school systems delayed their opening dates or announced fully online instruction for the fall semester, while others considered hybrid models such as “groups of students to attend on alternating days or weeks, as well as allowing only younger students to attend while older students learn at home [51].”
This study compared the impact of various school reopening strategies, in the presence of a combination of other non-pharmaceutical interventions such as shelter-in-place, voluntary quarantine of households, and masking, with varying levels of compliance, along with universal masking and symptom-based isolation in schools. According to our study results, delaying the reopening date would have a minimal impact on the peak day and peak number of new infections under the alternating school day, the children only, and the alternating school day for children reopening strategies. However, under the regular reopening strategy, delaying the reopening date from August 10 to September 17 could avoid the second peak and reduce the peak number of new children and youth infections by 22%.
Compared to the schools closed reopening strategy, the alternating school day for children reopening strategy increased deaths, hospitalizations, and cumulative infections the least, followed by the children only and then the alternating school day reopening strategies. Hybrid reopening strategies such as the alternating school day for children, children only, and alternating school day significantly reduced the percentage of the population infected when compared to the regular reopening strategy (by 6-13%). Hence, implementing a hybrid reopening strategy or limiting interactions between student cohorts during the in-person instruction could have a significant impact on slowing down the disease spread. A population study focused on Washington and Michigan found that overall, online instruction or providing hybrid instruction led to fewer infections compared to in-person instruction, supporting the findings in this study [52]. The addition of universal masking to in-person instruction further reduced infections, hospitalizations, and deaths.
Conclusions
COVID19 has had a significant impact on society both in terms of public health and social and economic interactions. The health and well-being of the population are of the utmost importance, but there is also a growing desire to return to in-person instruction to support the educational development of students.
As school systems develop plans for modes of instruction during an epidemic or pandemic, it is critical to understand the impact of various scenarios on public health as well as students’ development and the economy. Our results suggest that opening schools following a regular reopening strategy, i.e., all students returning to school without strict public health measures, would significantly increase the number of infections, hospitalizations, and deaths. Hybrid in-person and online reopening strategies, especially if offered as an option to families and teachers who prefer to opt-in, provide a good balance in reducing the infection spread compared to the regular reopening strategy, while ensuring access to in-person education.
The impact of other non-pharmaceutical public health measures, including workplace closings, voluntary quarantine compliance, shelter-in-place, and masking mandates have been considered and compared in prior work [7, 9, 20, 31, 53–56]. Some studies found that the public health effects of school closures are similar to that of workplace closures [20, 53, 54]. Our study focused on the impact of various school reopening scenarios to provide policy suggestions to decision-makers amid an ongoing pandemic or epidemic, in the presence of other non-pharmaceutical interventions. Regardless of how school instruction is formatted during a pandemic, it is important to promote physical distancing measures, vaccination, and the usage of face masks as well as establishing testing and tracing practices to ensure prevention or early detection of outbreaks in schools.
Supplementary Information
Acknowledgements
The authors are thankful to state of Georgia representatives, including Garry McGiboney from Georgia Department of Education, Laura Edison from Georgia Department of Public Health, and Susan Miller and Natalie Lee from Georgia Geospatial Information Office for their support, guidance, or sharing data sources. The authors are also thankful to current and former Georgia Tech students and colleagues, including Ethan Channel, Pravara Harati, Zihao Li, Hannah Lin, Melody Shellman, Gabriel Siewert, Christopher Stone, Julie Swann, and April Zhuoting Yu for their contributions and support. We are grateful to the reviewers and editors for their constructive feedback which helped improve the manuscript.
Abbreviations
- M
Universal masking in schools
- K-12
Kindergarten through 12th grade
- IAR
Infection Attack Rate
Authors’ contributions
BO, AB, PK, JA, and NS contributed to the conception and the design of the study and the models, and the interpretation of the data and model outputs. BO, AB, and JA contributed to data acquisition, simulation model development, model runs, and analysis of the data and model outputs. BO, AB, PK, JA, and NS contributed to the writing of the manuscript and have read and approved the final manuscript. The author(s) read and approved the final manuscript.
Funding
The research was supported by the William W. George and by the Virginia C. and Joseph C. Mello endowments at Georgia Tech. This research was supported in part by Cooperative Agreement number NU38OT000297 from The Centers for Disease Control and Prevention (CDC) and CSTE, NSF Graduate Research Fellowship DGE-1650044, NSF grant MRI 1828187, and research cyberinfrastructure resources and services provided by the Partnership for an Advanced Computing Environment (PACE) at the Georgia Institute of Technology. The funders played no role in the study design, data collection, analysis, interpretation, or in writing the manuscript.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. All data used was publicly available.
Declarations
Ethics approval and consent to participate
No administrative permissions were required to access any raw data used in this study. All data used in this study was taken from the US Census Bureau, which is anonymized.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.When It Comes To Reopening Schools, 'The Devil's In The Details,' Educators Say [https://www.npr.org/2020/07/09/888878030/when-it-comes-to-reopening-schools-the-devil-s-in-the-details-educators-say?utm_medium=social&utm_campaign=npr&utm_term=nprnews&utm_source=twitter.com].
- 2.Reopening Schools While Mitigating COVID-19’s Spread: How Many Days Should Students Attend? [https://ies.ed.gov/ncee/edlabs/regions/midatlantic/app/Blog/Post/1035].
- 3.Kamenetz A. New Report Says Schools Should Try To Reopen In Person For Elementary Students. In.: NPR; 2020.
- 4.Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, Whittaker C, Zhu H, Berah T, Eaton JW et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020. [DOI] [PubMed]
- 5.Hsiang S, Allen D, Annan-Phan S, Bell K, Bolliger I, Chong T, Druckenmiller H, Huang LY, Hultgren A, Krasovich E et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020. [DOI] [PubMed]
- 6.Auger KA, Shah SS, Richardson T, Hartley D, Hall M, Warniment A, Timmons K, Bosse D, Ferris SA, Brady PW et al. Association Between Statewide School Closure and COVID-19 Incidence and Mortality in the US. JAMA. 2020;324(9):859–70. [DOI] [PMC free article] [PubMed]
- 7.Wong MCS, Huang J, Teoh J, Wong SH. Evaluation on different non-pharmaceutical interventions during COVID-19 pandemic: An analysis of 139 countries. Journal of Infection. 2020;81(3):e70–e71. doi: 10.1016/j.jinf.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. New England J Med. 2020;383:510–2. [DOI] [PubMed]
- 9.Oruc BE, Baxter A, Keskinocak P, Asplund J, Serban N. Homebound by COVID19: the benefits and consequences of non-pharmaceutical intervention strategies. BMC Public Health. 2021;21(1):655. doi: 10.1186/s12889-021-10725-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dibner KA, Schweingruber HA, Christakis DA. Reopening K-12 Schools During the COVID-19 Pandemic: A Report From the National Academies of Sciences, Engineering, and Medicine. JAMA. 2020;324(9):833–4. [DOI] [PubMed]
- 11.Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, Mytton O, Bonell C, Booy R. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. The Lancet Child & Adolescent Health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bayham J, Fenichel EP. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. The Lancet Public Health. 2020;5(5):e271–e278. doi: 10.1016/S2468-2667(20)30082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharfstein JM, Morphew CC. The Urgency and Challenge of Opening K-12 Schools in the Fall of 2020. JAMA. 2020;324(2):133–3. [DOI] [PubMed]
- 14.Esposito S, Principi N. School closure during the coronavirus disease 2019 (COVID-19) pandemic: an effective intervention at the global level? JAMA Pediatrics. 2020;174(10):921–2. [DOI] [PubMed]
- 15.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adverse consequences of school closures. [https://en.unesco.org/covid19/educationresponse/consequences].
- 17.Hobbs TD, Hawkins L. The Results Are In for Remote Learning: It Didn’t Work. In: The Wall Street Journal. Online; 2020.
- 18.Burzynska K, Contreras G. Gendered effects of school closures during the COVID-19 pandemic. The Lancet. 2020;395(10242):1968. doi: 10.1016/S0140-6736(20)31377-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubin R. School Superintendents Confront COVID-19—“There Are No Good Options for Next Year”. JAMA. 2020;324(6):534–6. [DOI] [PubMed]
- 20.Wu JT, Mei S, Luo S, Leung K, Liu D, Lv Q, Liu J, Li Y, Prem K, Jit M, et al. A global assessment of the impact of school closure in reducing COVID-19 spread. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences. 2022;380(2214):20210124. doi: 10.1098/rsta.2021.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Y, Lawley MA, Siscovick DS, Zhang D, Pagán JA: Peer reviewed: agent-based modeling of chronic diseases: a narrative review and future research directions. Preventing chronic disease 2016, 13. [DOI] [PMC free article] [PubMed]
- 22.Venkatramanan S, Lewis B, Chen J, Higdon D, Vullikanti A, Marathe M. Using data-driven agent-based models for forecasting emerging infectious diseases. Epidemics. 2018;22:43–49. doi: 10.1016/j.epidem.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fausset R, Levenson M. Atlanta Protesters Clash With Police as Mayor Warns 'You are Disgracing Our City'. In: The New York Times. 2020.
- 24.Nirappil FS, Maria: Mourners recall Rayshard Brooks, say his death 'much bigger than him. In: The Washington Post. 2020.
- 25.Wickert DB, Greg; Stevens, Alexis: Thousands of demonstrators at Georgia Capitol as Legislature reconvenes. In: The Atlanta Journal-Constitution. 2020.
- 26.TIMELINE: Follow daily highlights on local and national civil unrest. [https://georgiastatesignal.com/live-protests-erupt-in-downtown-atlanta-in-response-to-the-death-of-george-floyd/].
- 27.Understand the impact of COVID-19 on traffic, travel patterns, toll revenues and more [https://www.streetlightdata.com/covid-transportation-metrics/].
- 28.Covid-19 Vaccine Dashboard. [https://experience.arcgis.com/experience/3d8eea39f5c1443db1743a4cb8948a9c].
- 29.The New York Times: Coronavirus (Covid-19) Data in the United States. In.: The New York Times; 2020.
- 30.The New York Times: Six Months of Coronavirus: Here’s Some of What We’ve Learned. In: The New York Times. Online; 2020.
- 31.Keskinocak P, Oruc BE, Baxter A, Asplund J, Serban N. The impact of social distancing on COVID19 spread State of Georgia case study. PLoS One. 2020;15(10):e0239798. doi: 10.1371/journal.pone.0239798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ekici A, Keskinocak P, Swann JL. Modeling Influenza Pandemic and Planning Food Distribution. Manufacturing & Service Operations Management. 2014;16(1):11–27. doi: 10.1287/msom.2013.0460. [DOI] [Google Scholar]
- 33.Li Z, Swann JL, Keskinocak P. Value of inventory information in allocating a limited supply of influenza vaccine during a pandemic. PLoS One. 2018;13(10):e0206293. doi: 10.1371/journal.pone.0206293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shi P, Keskinocak P, Swann JL, Lee BY. The impact of mass gatherings and holiday traveling on the course of an influenza pandemic: a computational model. BMC Public Health. 2010;10(1):778. doi: 10.1186/1471-2458-10-778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau: American Community Survey, 2018 American Community Survey 1-year Estimates. In.: U.S. Census Bureau; 2018.
- 36.GAC Standards [http://gac.coe.uga.edu/gac-standards/].
- 37.U.S. Census Bureau: Census Transportation Planning Products, 5-year data. In.: U.S. Census Bureau; 2016.
- 38.U.S. Census Bureau: American Community Survey, 2017 American Community Survey 5-year Estimates. In.; 2017.
- 39.U.S. Census Bureau: Census Summary File 1. In.: U.S. Census Bureau; 2010.
- 40.Methods of Apportionment. [https://www.census.gov/history/www/reference/apportionment/methods_of_apportionment.html].
- 41.Kemp orders schools closed through end of school year [https://www.ajc.com/news/state--regional-education/schools-closed-until-fall/r7QgK2idaQ0681UafbW3XP/].
- 42.Fischer EP, Fischer MC, Grass D, Henrion I, Warren WS, Westman E. Low-cost measurement of face mask efficacy for filtering expelled droplets during speech. Science Advances. 2020;6(36):eabd3083. doi: 10.1126/sciadv.abd3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Biggest Retail Chains Keeping Mask Mandates [https://www.aarp.org/health/healthy-living/info-2020/retailers-require-face-masks-coronavirus.html].
- 44.FULL LIST: What cities and counties are requiring face masks? [https://www.wsbtv.com/news/local/full-list-what-counties-cities-are-requiring-face-masks/VJQ3BQH2TBEMZICWXZQ5DIM5XE/].
- 45.Zhang Y, Johnson K, Yu Z, Fujimoto AB, Lich KH, Ivy J, Keskinocak P, Mayorga M, Swann JL: COVID-19 Projections for K12 Schools in Fall 2021: Significant Transmission without Interventions. medRxiv 2021:2021.2008.2010.21261726.
- 46.The Importance of Reopening America’s Schools this Fall [https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/reopening-schools.html].
- 47.Williams R. Rural Georgia's Back-To-School Blues: COVID-19 Spreads Fast, Internet's Slow. In: Georgia Public Broadcasting. NPR; 2020.
- 48.Framework Overview [https://getgeorgiareading.org/framework-overview/].
- 49.DeGeurin M: One in 5 children live below the poverty line: Here are the states with the highest number of kids dependent on free lunches. In: Insider. Insider Inc.; 2020.
- 50.COVID-19 Planning Considerations: Guidance for School Re-entry [https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-planning-considerations-return-to-in-person-education-in-schools/].
- 51.Tagami T. New Georgia COVID-19 guidelines suggest how schools will look different this fall. In.: The Atlanta Journal-Constitution; 2020.
- 52.Goldhaber D, Imberman SA, Strunk KO, Hopkins B, Brown N, Harbatkin E, Kilbride T. To What Extent Does In-Person Schooling Contribute to the Spread of COVID-19? Evidence from Michigan and Washington. National Bureau of Economic Research Working Paper Series 2021, No. 28455.
- 53.Pozo-Martin F, Weishaar H, Cristea F, Hanefeld J, Bahr T, Schaade L, El Bcheraoui C. The impact of non-pharmaceutical interventions on COVID-19 epidemic growth in the 37 OECD member states. European Journal of Epidemiology. 2021;36(6):629–640. doi: 10.1007/s10654-021-00766-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wibbens PD, Koo WWY, McGahan AM. Which COVID policies are most effective A Bayesian analysis of COVID-19 by jurisdiction. PLoS One. 2021;15(12):e0244177. doi: 10.1371/journal.pone.0244177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patel MD, Rosenstrom E, Ivy JS, Mayorga ME, Keskinocak P, Boyce RM, Hassmiller Lich K, Smith RL, III, Johnson KT, Delamater PL et al. Association of simulated COVID-19 vaccination and nonpharmaceutical interventions with infections, hospitalizations, and mortality. JAMA Network Open. 2021;4(6):e2110782–e2110782. [DOI] [PMC free article] [PubMed]
- 56.Rosenstrom E, Ivy J, Mayorga M, Swann J, Oruc BE, Keskinocak P, Hupert N. High-quality masks reduce covid-19 infections and death in the US. In: 2021 Winter Simulation Conference (WSC). 2021;2021:1–11.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. All data used was publicly available.