Circadian Rest-Activity Rhythm (or RAR) disturbances are prospectively associated with major health outcomes including depression [1], dementia [2], and mortality [3]. These findings are from observational studies that cannot determine causality, but nonetheless suggest that certain RAR characteristics may contribute to or signal poor health outcomes. This growing evidence-base has potential for translation into practice, given that RARs can be passively measured with wrist-worn accelerometers, and because RARs can be voluntarily controlled. Routinely surveilling for RAR disturbances could aid risk stratification and early risk detection approaches, and RAR characteristics could serve as targets for modification via intervention. In this brief report, we: (1) propose that future experimental RAR research and related public health/clinical applications will benefit from having a scalable and user-friendly system for real-time RAR assessment/tracking and (2) provide initial “proof of concept” that a consumer wearable-based system can provide the requisite accelerometer data for real-time RARs assessments.
Currently, RAR disturbances are seldomly detected or intervened upon in therapeutic practice. One contributing factor may be the lack of user-friendly systems for RAR assessment. Scientific studies measure RARs using research-grade accelerometer devices that require specialist resources to use and do not provide real-time information. In research, RARs are characterized using statistical software to compute advanced models or other calculations, only after data collection is complete and transferred to a computer via wire. In contrast, commercially available consumer wearable devices (e.g., Apple Watch and FitBit) are widely used, user-friendly, and provide real-time feedback. While existing consumer accelerometer-based devices provide real-time sleep and activity tracking, they do not measure or report on RAR characteristics. Researchers derive various RAR measures from a time series of accelerometer “counts” that are taken continuously every 30 or 60 seconds over several days or weeks. As pointed out previously [4], consumer wearable devices typically do not permit direct access to these data.
One prior study has shown that accelerometer data extracted from the FitBit yields reliable RAR measures [5]. Other studies using the Apple Watch demonstrated separately: accessibility/utility of daytime “step counts” [6]; and that raw accelerometer data from the sleep period is accessible [7]. These studies support the feasibility that accelerometer data from consumer wearables may be comparable to those of research-grade devices. But these prior studies did not show that raw accelerometer data from a consumer wearable can be obtained in real-time over repeated 24-hour periods. If so, this would enable RAR tracking capabilities which could enhance risk monitoring and/or adaptive interventions. Real-time RARs assessments could enhance existing interventions that address rhythm disruption (such as prescribed timing to activities like exercise [8] and bright light exposure [9] as well as Social Rhythm Therapy [10]). Real-time RAR monitoring could be used to precisely and adaptively tailor clinical management strategies for patients. Consumer wearables are already being worn daily by millions of people, and could be leveraged in large-scale and long-term population studies that characterize potential contributions of RARs to health.
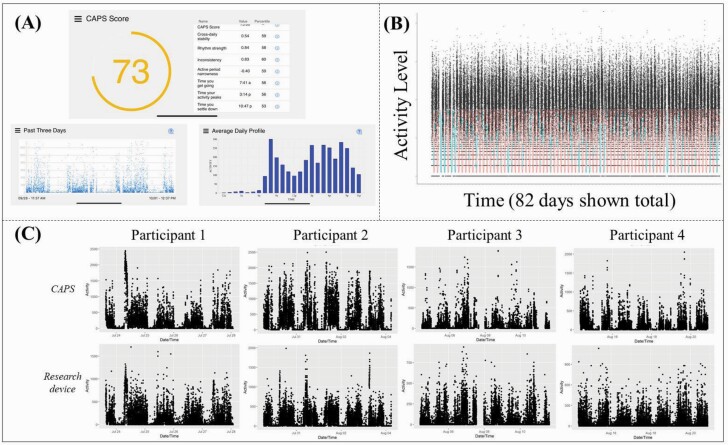
We therefore aimed to evaluate whether real-time RAR tracking is possible with a consumer wearable. In 2017, we began developing a real-time RAR tracking system, which we call the Circadian Activity Profiling System (CAPS). Here the term “circadian” simply refers to activity following a 24-hour pattern and is not intended to imply that such rhythms are necessarily endogenous. The CAPS sends accelerometer data from an Apple Watch to an iPhone, and then a web-based system (Amazon Web Services) for computations, storage, and remote retrieval of RAR data. This prototype graphs an individual’s RARs in terms of average hourly activity levels and epoch-by-epoch data (Figure 1A). It displays values for common RAR measures used in research including those from the extended cosine approach [11]. The system also has a place to display a main summary score, which incorporates elements of various RAR parameters. Such summary scores can be developed by investigators to provide relevant feedback suited to particular use cases.
Figure 1.
Epoch-by-epoch data from the Apple Watch-based Circadian Activity Profiling System (CAPS).
(A) The prototype display featuring a place for an aggregate score, epoch-by-epoch plots, and hourly plots. (B) 82 days of epoch-by-epoch data accelerometer count data obtained from the Apple Watch using the CAPS. Missing data are indicated by blue lines, whereas red portions of the line indicate available data. (C) Comparisons of epoch-by-epoch plots from four participants who wore both the Apple Watch system and the Philips Spectrum device.
This automated (passive) system collecting epoch-by-epoch level data worked over long periods for the initial tester/inventor (SFS, see Figure 1B). We then evaluated if the Apple Watch-based CAPS generated similar data when compared with a popular research-grade device (the Philips Spectrum Pro) in terms of: (1) the percentage of epochs recorded by the Philips device that were also captured by the CAPS; and (2) whether comparable RAR timing measures were produced when applying an extended cosine model. We recruited a convenience sample of 10 participants who wore both devices for 1 week. Watches were worn on separate wrists because device buttons were often inadvertently pressed if wearing both devices on one wrist. Wrist assignment was alternated across participants.
The application ran successfully for 4/10 participants (see next paragraph for why failures occurred). In the participants for whom the CAPS ran successfully, the program effectively synced ≥80% of the data collected by the Philips device, and RAR timing measures were similar across devices (Table 1). Note that procedures for calculating activity counts, and the resulting activity count scales (vertical axis, Figure 1C) differ across devices.
Table 1.
Rest-activity rhythm (RAR) timing measures and epochs synced comparing the two devices
| Up-mesor | Acrophase | Down-mesor | |||||
|---|---|---|---|---|---|---|---|
| CAPS | Philips | CAPS | Philips | CAPS | Philips | CAPS epochs captured as a percentage of those captured by the Philips device (%) | |
| Participant 1 | 7.9 | 7.7 | 15.9 | 15.8 | 24.0 | 23.9 | 92 |
| Participant 2 | 6.0 | 6.0 | 13.7 | 13.7 | 21.4 | 21.3 | 95 |
| Participant 3 | 8.0 | 8.4 | 15.7 | 16.0 | 23.5 | 23.5 | 85 |
| Participant 4 | 7.2 | 7.8 | 16.4 | 15.6 | 23.6 | 23.4 | 85 |
CAPS, Circadian Activity Profiling System.
These timing parameters were estimated with an anti-logistic transformed cosine curve using the R package “RAR” (https://github.com/JessLGraves/RAR). Up-mesor (estimated time participant “gets going”) and down-mesor (estimated time participants “settles down”) come from extended cosine model estimates. Times are expressed in 24-hour decimal format, e.g., 6.5 = 6:30 AM.
Although the success rate was low in this initial feasibility test, we identified specific challenges that can be resolved with further development. Our prototype was developed on an Apple Watch 6 and iPhone 8. We did not have the resources in this initial development work to make the CAPS compatible with other software/hardware platforms. This resulted in the application failing to run on many user’s platforms, e.g., an iPhone 7 with an older operating system. The current prototype was also not optimized for ease-of-use and requires some technical aptitude. Users needed to maintain charged batteries on two devices, maintain Bluetooth connection between the Apple Watch and iPhone and monitor data syncing. The Philips device is a simpler hardware unit equipped with a longer battery life that does not require daily charging. In this study, some users reported forgetting to charge the devices or leaving the watch on the charger for too long. We expect that battery life on consumer wearables will continue to improve in the future. In the near term, these issues can be partially mitigated by programming reminders to help users maintain data collection. Finally, the scales of the activity counts produced by these devices varies, and this prevents direct comparisons of activity-level dependent RAR metrics. Note that this issue was recently addressed by John and colleagues [12] who proposed a device-independent movement intensity count [10] which can be implemented moving forward.
This work provides proof of concept that passively obtaining raw accelerometer data, over repeated 24-hour periods, is possible on the Apple Watch platform. By extension, research and clinical applications of real-time RAR assessments are possible on this platform. Real-time RAR assessments on a consumer wearable could have a positive public health impact, i.e., by helping scale-up observational risk factor studies and supporting novel clinical trials. Despite the potential for such applications, we found that the process of getting data from the Apple platform was not straightforward. Additional development work will be needed before determining the true scalability of using such data for larger trials. This development work requires establishing partnerships that are not typical for academic research (e.g., with software developers/architects/designers). Nonetheless, further efforts are warranted to enable trials evaluating if real-time RAR monitoring improves the efficacy of existing interventions to detect and mitigate related health risks.
Funding
This work was supported by the National Institute of Health via K01MH112683 and R01GM113243. This development and evaluation of the Circadian Activity Profiling System (CAPS) reported here took place at the University of Pittsburgh. An initial version was supported by awards from Philips Advanced Innovation, the University of Pittsburgh Chancellor’s Early Stage Commercialization Fund, and the National Science Foundation Innovation Corps (IIP 1449702 and IIP 0057282). Subsequently, the prototype was developed with additional support from IIP 0057282 and an award from the National Institute on Aging (R41AG069596) to a small business owned by SFS (Activity Rhythm Solutions Corporation). This company, where SFS serves as CEO, recently licensed CAPS IP from the University of Pittsburgh and is pursuing further development of the technology.
Disclosure Statement
The authors have no other interests that could be perceived as conflicts to declare.
References
- 1. Smagula SF, et al. ; Osteoporotic Fractures in Men (MrOS) Research Group. Circadian rest-activity rhythms predict future increases in depressive symptoms among community-dwelling older men. Am J Geriatr Psychiatry. 2015;23(5):495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tranah GJ, et al. ; SOF Research Group. Circadian activity rhythms and risk of incident dementia and mild cognitive impairment in older women. Ann Neurol. 2011;70(5):722–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zuurbier LA, et al. Fragmentation and stability of circadian activity rhythms predict mortality: the Rotterdam study. Am J Epidemiol. 2015;181(1):54–63. [DOI] [PubMed] [Google Scholar]
- 4. Depner CM, et al. Wearable technologies for developing sleep and circadian biomarkers: a summary of workshop discussions. Sleep. 2020;43(2). doi: 10.1093/sleep/zsz254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee HA, et al. Comparison of wearable activity tracker with actigraphy for sleep evaluation and circadian rest-activity rhythm measurement in healthy young adults. Psychiatry Investig. 2017;14(2):179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang Y, et al. Predicting circadian phase across populations: a comparison of mathematical models and wearable devices. Sleep. 2021;44(10). doi: 10.1093/sleep/zsab126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Walch O, et al. Sleep stage prediction with raw acceleration and photoplethysmography heart rate data derived from a consumer wearable device. Sleep. 2019;42(12). doi: 10.1093/sleep/zsz180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chtourou H, et al. The effect of training at a specific time of day: a review. J Strength Cond Res. 2012;26:1984–2005. [DOI] [PubMed] [Google Scholar]
- 9. Ancoli-Israel S, et al. Increased light exposure consolidates sleep and strengthens circadian rhythms in severe Alzheimer’s disease patients. Behav Sleep Med. 2003;1(1):22–36. [DOI] [PubMed] [Google Scholar]
- 10. Frank E. Interpersonal and social rhythm therapy: a means of improving depression and preventing relapse in bipolar disorder. J Clin Psychol. 2007;63(5):463–473. [DOI] [PubMed] [Google Scholar]
- 11. Marler MR, et al. The sigmoidally transformed cosine curve: a mathematical model for circadian rhythms with symmetric non-sinusoidal shapes. Stat Med. 2006;25(22):3893–3904. [DOI] [PubMed] [Google Scholar]
- 12. John D, et al. An open-source monitor-independent movement summary for accelerometer data processing. J Meas Phys Behav. 2019;2(4):268–281. [DOI] [PMC free article] [PubMed] [Google Scholar]