Abstract
The decision on which technique to use to perform a total knee arthroplasty has become much more complicated over the last decade. The shortfalls of mechanical alignment and kinematic alignment has led to the development of a new alignment philosophy, functional alignment. Functional alignment uses preoperative radiographic measurements, computer-aided surgery, and intraoperative assessment of balance, to leave the patient with the most “normal” knee kinematics achievable with minimal soft-tissue release. The purpose of this surgical technique article is to describe in detail the particular technique needed to achieve these alignment objectives.
Keywords: Total knee arthroplasty, Alignment, Kinematics, Functional alignment
Introduction
Which technique to use to perform a total knee arthroplasty (TKA) has become much more complicated. Contemporary TKA surgical techniques are typically derived from one of two alignment philosophies: mechanical alignment (MA) or the kinematic alignment (KA). Despite advances in TKA perioperative care, surgical technique, implant, and instrumentation, patient dissatisfaction remains high [1]. RCT data have not clearly shown superiority of KA over MA [2]. Owing to an increased understanding of the potential shortfalls of MA and KA and the recognition of some patients experiencing suboptimal results after TKA, a new alignment philosophy has been developed; functional alignment (FA) [3,4].
FA is a computer-aided surgery (CAS) technique (navigated or robotic), compatible with all standard TKA approaches [5]. FA protects the soft-tissue envelope and achieves a balanced knee with the “most normal” kinematics possible, minimizing tissue releases, relying principally on bony resections. FA is a hybrid technique that starts with a KA-style implant plan, replicating constitutional coronal extension alignment, before using ligament stress values throughout the operative process to further optimize implant position to achieve precisely and reproducibly obtain ideal kinematics. Our described technique takes into consideration variations in native trochlea anatomy and allows the femoral component to be manipulated into a nonanatomic position to achieve an individualized, best-fit compromise. Recent authors have reported promising reports in FA’s ability to achieve soft-tissue balance [4,5].
Surgical technique
Preoperative planning
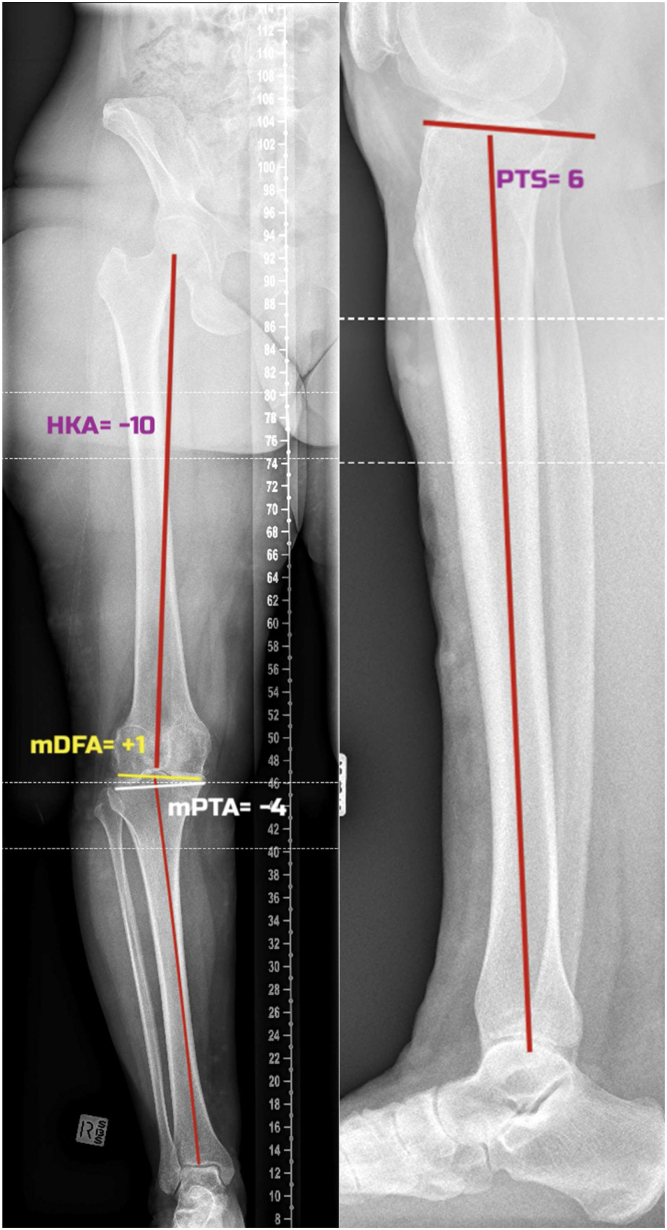
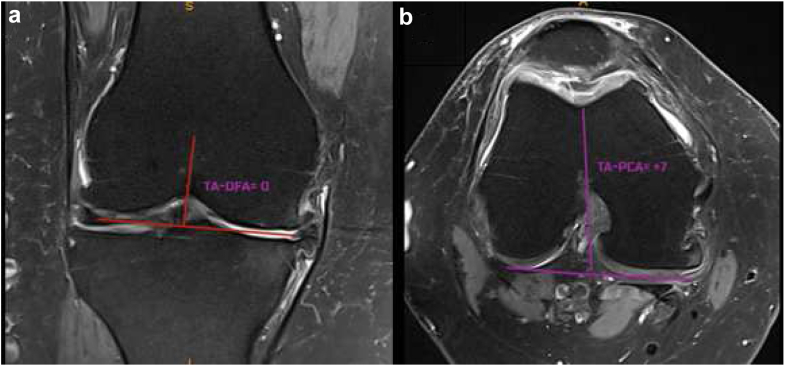
When performing FA, preoperative radiographic alignment should be available for reference within the operating room. Preoperative long-limb radiographs, CT, or EOS scans are necessary to evaluate arthritic weight-bearing alignment. Essential parameters include hip-knee-ankle (HKA), mechanical lateral-distal-femoral angle (mLDFA), mechanical proximal-tibial angle (mPTA), and posterior tibial slope (PTS) measures (Fig. 1). The measurement of trochlear angle to distal femoral angle (TA-DFA), trochlear angle to posterior condylar axis, and lateral/medial tibial slope can be calculated from 3D scans such as CT and MRI (Fig. 2) [6]. FA is compatible with the new knee phenotyping classifications, Coronal Plane Alignment of the Knee, and these data can similarly be recorded [7].
Figure 1.
Long-limb radiographs and alignment measurements. Essential parameters include hip-knee-ankle (HKA), mechanical lateral-distal-femoral angle (mLDFA), mechanical proximal-tibial angle (mPTA), and posterior tibial slope (PTS) measures.
Figure 2.
MRI scan to obtain trochlea angle measurements. (a) Trochlear angle-distal femoral angle (TA-DFA). (b) Trochlear Angle-posterior condylar axis (TA-PCA). These measures add additional explanatory data for optimizing component position when combined with intraoperative CAS data.
Approach, registration, and virtual planning
After incision and exposure of the knee joint, the surgeon should ensure removal of all osteophytes and insert the femoral and tibial navigation trackers before completing navigation point registration.
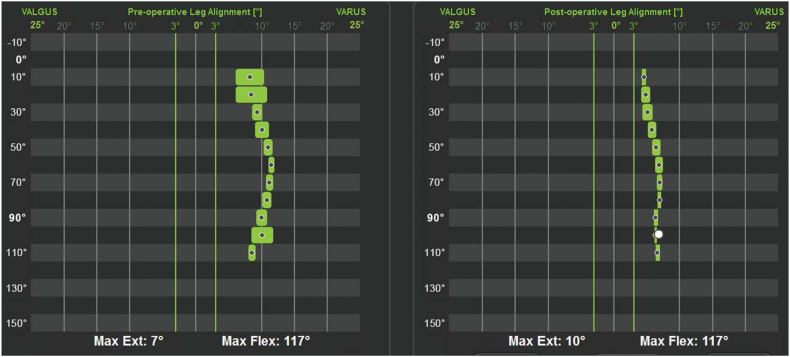
After computer registration, alignment is assessed in extension (0°-10°) and, importantly, at 90° flexion to determine the “neutral”/nonstressed alignment. In addition, an opposing stress to the neutral alignment, varus in a valgus knee or valgus in a varus knee, is applied to the knee in extension and 90° flexion to evaluate ligamentous function or “stress alignment” and approximate the alignment kinematics of the “prearthritic” knee and the prearthritic alignment curve; via determining the extension and flexion alignment of the knee (Fig. 3) [8].
Figure 3.
Computer-aided surgery (CAS) kinematic results tracking alignment and gaps in preoperative curves. The surgeon should record the stress parameters as “preoperative curve.”
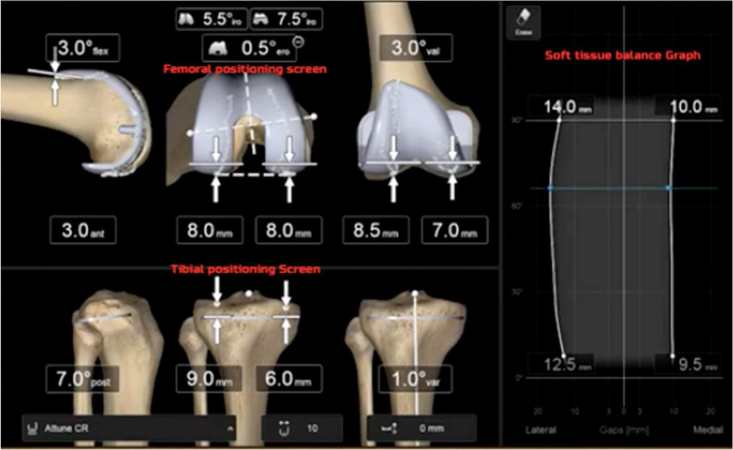
Next, a virtual prosthesis positioning plan is created using the implant planning screen (Fig. 4). The femoral and tibial prostheses are provisionally positioned on the digital planning screen according to the preoperatively measured mLDFA and mPTA. It is worth noting that if there is extensive bone loss in the articulating surfaces, the preoperative measurements may need to be adjusted to reflect the respective value as if there was no bone loss. To address the issue of bone loss, consider the formula “Extension Stress Alignment (Extension Stress HKA) = mLDFA + mMPTA” (varus = negative value) [7]. The extension stress HKA can be determined by applying a valgus force against the extended knee (0°-10°) and reading the HKA off the CAS system. If 2 variables are known, the third can be calculated. Usually, the bone loss will be on either the femoral or the tibial surface; however, in severe deformity, the surgeon may need to approximate and adjust the position after checking predicted kinematics. Resections that approximate the native mLDFA and mMPTA will recreate a joint line obliquity angle (JLOA) similar to the prearthritic state.
Figure 4.
CAS virtual implant planning screen and graphical representation of the soft-tissue gaps.
Once the planned stress extension HKA has been determined, the medial and lateral extension gaps should be checked. An excessive/insufficient gap can be corrected by adjusting the virtual femoral/tibial/both prostheses distally or proximally. Once the extension stress HKA, JLOA, and extension stress gaps have been achieved, the surgeon can consider that there is a plan for a “balanced knee” in extension.
The same concept is used with knee at 90° flexion. The femoral component is repositioned to achieve similar gaps as extension. The authors advocate a tighter medial gap in extension and flexion (1-2 mm laxity) than the lateral, which can be as much as 5 mm in flexion, creating a trapezoidal-kinematic-gap driven by a medial pivot [9]. This laxity can be determined by noting the change in gaps when applying stress in the previous step. If the preoperative analysis has shown a posterior slope difference of greater than 5° between the medial and lateral sides, the femoral rotation may need to be adjusted during the intraoperative phase.
The aim is to have the virtual implants achieve the desired gaps in both flexion and extension, thereby balancing the soft tissue through a full range of motion (Fig. 4).
If there is a large difference between the native (TA-DFA) and prosthetic trochlea angle (>3°) [6], to avoid patellofemoral maltracking, this can be reduced by altering the femoral component position. If altered, the tibia should be adjusted to maintain the desired medial and lateral tibiofemoral gaps. This may have a consequence of variation in JLOA from the native joint line but may be a necessary compromise given the mismatch between the native patellofemoral morphology and implants.
First bony resection—tibia
The tibia or femur can be addressed first. The lead author uses a tibia-first workflow. Femur-first surgeons are encouraged to reverse the order described.
Once the virtual prosthesis positioning has achieved the desired gaps and kinematic curve, the tibia should be resected (Fig. 5). The authors advocate an unrestricted mPTA resection so long as the planned resection is not significantly different from the prearthritic tibia and would advise double-checking the plan for resections greater than 6°.
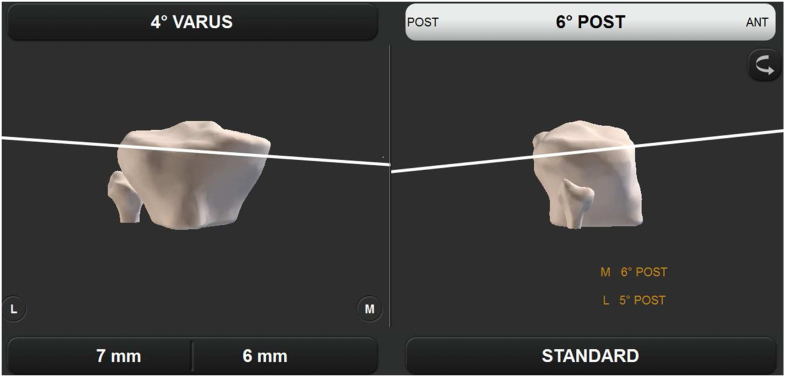
Figure 5.
The tibia should be resected according to the virtually planned mPTA and PTS. CAS tibial mMPTA resection screen and differential slope (PTS) measurements.
Approximate the prearthritic alignment in the coronal and sagittal planes as indicated by the preoperative radiology.
Sagittal tibial alignment makes the concession that differential PTS, which is common in the native knee, is not replicable with a typical symmetric tibial implant. The authors recommend resecting the PTS to a maximum of −9°. The maximum of −9° PTS is based on manufacturer recommendations, and there is support in the literature for limiting PTS because of increased failure risk as well as trying to limit disruption to constitutional sagittal slope that can adversely affect PFJ kinematics [10,11]. The slope of reference is whichever plateau (medial or lateral) is closest to −9°. Some KA literature suggests a more conservative −7° PTS based on different manufacturer specifications and did not note any issues with tibial subsidence [9,12,13]. With more significant degrees of tibial resection, the posterior cruciate ligament origin is at risk and requires protection (Fig. 6).
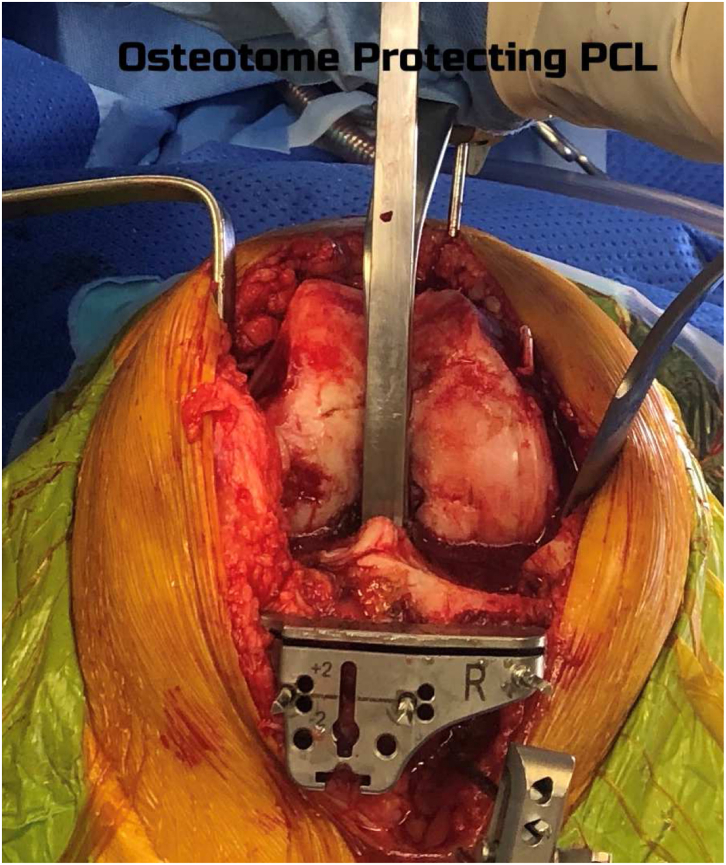
Figure 6.
To address the risk to the PCL, the senior author routinely carves a PCL box with 1.5-cm osteotome and retains the osteotome in place in the coronal plane while resecting the tibia to protect the PCL. A photograph demonstrating the use of an osteotome to protect the PCL insertion at the time of tibial cut using jig and sagittal saw.
Second bony resection—distal femur
After tibial resection, a tibial-only extension gap block is inserted, and the coronal alignment and ligament tension is checked on navigation (Fig. 7). Should this vary from the expected, the femoral component coronal virtual plan can be adjusted (Table 1). The distal femoral resection is then performed to match the tibial resection.
Figure 7.
CAS femoral implant virtual planning/adjustment screen.
Table 1.
Algorithm to correct isolated malalignment and asymmetric medial and lateral gaps.
| Isolated asymmetric mediolateral tightness/laxity |
||||
|---|---|---|---|---|
| Extension |
Flexion |
|||
| Medial | Lateral | Medial | Lateral | |
| CAS data readout & clinical assessment | Tight medial extension gap: relative valgus to predicted stress HKA. <1 mm stress gap medially. Difficulty inserting poly/spacer block due to medial tightness | Tight lateral extension gap: relative varus to predicted stress HKA. <1 mm stress gap laterally. Difficulty inserting poly/spacer block due to lateral tightness | Tight medial flexion gap: relative valgus to predicted stress HKA. <1 mm stress gap medially. Poly spits out medially in flexion/difficulty inserting spacer block | Tight lateral flexion gap: relative varus to predicted stress HKA. <1 mm stress gap laterally |
| Loose medial extension gap: relative varus to predicted stress HKA. >2 mm medial stress gap. Alignment corrected with valgus stress force | Loose lateral extension gap: relative valgus to predicted stress HKA. >3 mm lateral stress gap. Alignment corrected with varus stress force | Loose medial flexion gap: relative varus to predicted stress HKA. >2 mm medial stress gap. Alignment corrected with varus stress force | Loose lateral flexion gap: relative valgus to predicted stress HKA. >5 mm lateral stress gap. Alignment corrected with valgus stress force | |
| Surgical solution | Tight medial extension gap: resect additional 1° = 1 mm resection off the medial femoral condyle | Tight lateral extension gap: resect additional 1° = 1 mm resection off the lateral femoral condyle | Tight isolated medial flexion gap: externally rotate the femur pivoting off the lateral condyle—resect more bone off the medial posterior condyle | Tight isolated lateral flexion gap: internally rotate the femur pivoting off the medial condyle—resect more bone off the lateral posterior condyle |
| Loose medial extension gap: underresect by 1° = 1 mm less resection off the medial femoral condyle | Loose isolated lateral extension gap: underresect by 1° = 1 mm less resection of the lateral femoral condyle | Loose isolated medial flexion gap: internally rotate (IR) the femur pivoting off the lateral femoral condyle, ie, resect 1 mm less bone off the medial posterior condyle but keep lateral condylar resection unchanged | Loose isolated lateral flexion gap: externally rotate (ER) the femur pivoting off the medial femoral condyle, ie, resect 1 mm less bone off the lateral femoral condyle but keep medial condylar resection unchanged | |
Preoperative TA-DFA angle assists in assessing the valgising effect of the prosthetic trochlea during the early virtual planning. Should the constitutional alignment of the coronal femur result in a gross mismatch of >3° between the native and prosthetic trochlea, the femoral component is tilted varus/valgus in the coronal plane to produce the desired net change in TA-DFA [14,15].
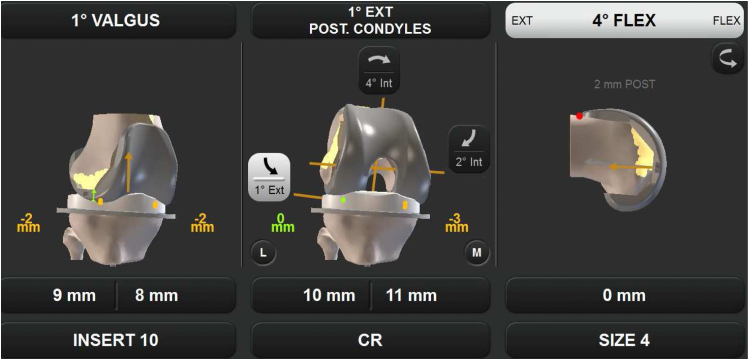
Third bony resection—multiplane femoral resection
Adjusting the femoral prosthesis will have implications for the PFJ. Determining the most appropriate course will depend on any existing mismatch between medial and lateral flexion gaps, the potential impact on the PFJ and, the overall flexion gap.
FA can address mismatches between the lateral and medial tibial slopes, known as differential PTS. If there is differential PTS >5°, then matching the global slope to the greater side will cause a flexion gap mismatch between the medial and lateral compartments. This can be addressed by varying the femoral position in the axial plane. To balance the flexion gap in a differential PTS situation, the femoral component is rotated away from the side with greater tibial slope and toward the side with the lesser slope depending on which slope was matched with the tibial resection. The femoral position should be fixed and pivoted from the opposite femoral condyle rather than the center of the knee such that only one tibiofemoral gap changes as the rotation is performed.
Consideration of the PFJ may occur concurrent to adjusting the flexion gap or in isolation once the extension and flexion gaps are virtually balanced. The same concept applies to the trochlear angle to posterior condylar axis, but in this case, the femoral component is rotated axially. It is important to note that in KA, the femoral rotation is set according to the wear pattern, typically underresecting the worn condyle by 2 mm relative to the contralateral condyle. FA takes into consideration the PFJ, the potential impact of differential PTS, and will derotate or prorotate the femur to achieve the desired kinematics and best fit with implant morphology. The goal is to approximate the planned constitutional alignment and achieve the kinematic targets, producing a balanced knee. This is a nonnative compromise driven by nonanatomic prostheses with a goal of restoring the most normal overall kinematics.
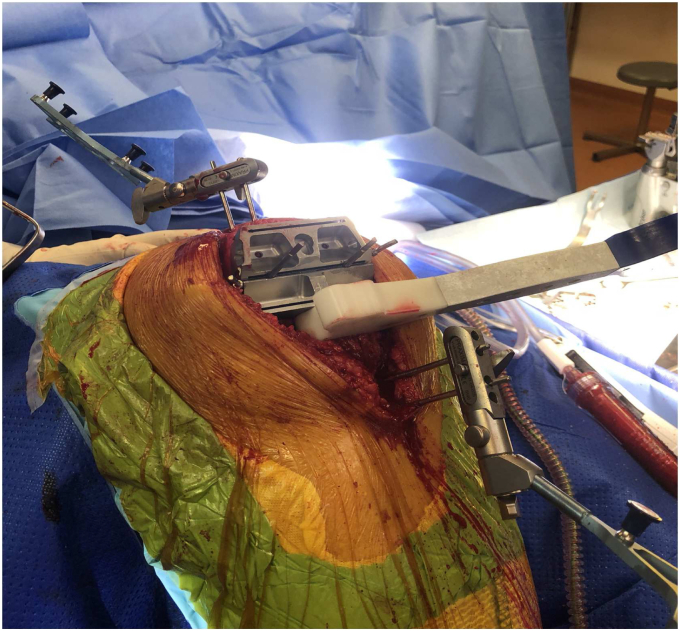
Next, the multiplane cutting block is positioned using CAS. A flexion gap block is seated against the cut surface of the tibia and the pinned multiplane femoral cutting block as seen in Figure 8. A final confirmation of flexion gaps and flexion alignment on the CAS screen is performed with the flexion gap block in place against the cutting block. Recreating the knee’s prearthritic extension and flexion coronal plane alignment sets the optimal knee alignment curve for the soft-tissue envelope to rotate in. While trying to recreate the native knee trapezoidal flexion gap driven by a medial pivot, it is acceptable to keep the lateral side loose and the medial side tight. Should any symmetric flexion gap issues arise, they can be corrected as per the algorithm in Table 1 before the final resection is made. Any unsatisfactory asymmetric mediolateral gaps should be addressed at this point as per Table 2.
Figure 8.
Clinical photograph demonstrating assessment of the flexion gap at 90° with the multiplane cutting block and the implant’s designated flexion gap block.
Table 2.
Algorithm for symmetric and asymmetric flexion-extension gap balance issues where no mediolateral balance issues exist.
| Symmetric tightness/laxity in flexion-extension gaps | Asymmetric tightness/laxity in flexion-extension gaps | |
|---|---|---|
| CAS data readout | Tight: FFD > 5° or <1 mm stress gaps in extension/flexion | Tight extension gap: FFD > 5° but appropriate flexion stress gap |
| Loose: Hyperextension > 5° of native with >1 + mm stress gaps outside of the desired range | Tight flexion gap: appropriate extension but tight flexion stress gap | |
| Loose extension gap: hyperextension > 5° of native but appropriate flexion gap | ||
| Loose flexion gap: appropriate extension but loose flexion gap | ||
| Clinical assessment | Tight: Unable to fully extend and poly squeaks and/or spits out in flexion | Tight extension gap: unable to fully extend but good flexion balance |
| Loose: Hyperextending knee with excessive medial and lateral gaps/laxity | Tight flexion gap: can fully extend but poly squeaks and/or spits out in flexion | |
| Loose extension gap: hyperextending knee with excessive extension medial and lateral gaps but good flexion balance | ||
| Loose flexion gap: can fully extend but flexion gaps are excessive | ||
| Response/Solution | Tight: Resect more of tibia | Tight extension gap: recut femur migrating proximally OR recut tibia more distally with less posterior slope |
| Loose: Increase polyethylene thickness | Tight flexion gap: recut tibia with more posterior slope | |
| Loose extension gap: recut tibia with more posterior slope AND increase poly size | ||
| Loose flexion gap: recut tibia with less posterior slope AND increase poly size |
Current navigation systems do not present the flexion coronal plane alignment at the preresection planning stage in the workflow. This assessment is only available once the multiplanar cutting block has been positioned and the virtual posterior condylar resection has been determined. Once this value is available, minor adjustments to femoral rotation are carried out to align the knee within the predicted stress value in flexion.
After any necessary femoral position adjustments, the resection is made. The trial prosthesis is inserted, and kinematics retested, including PFJ tracking. Once well balanced, the knee surfaces are prepared, and the definitive prosthesis is inserted.
Discussion
The key differences of FA over KA and other non-MA philosophies is that FA not only attempts to realign the knee in the coronal plane in extension but also aims to do the same in flexion while also considering overall joint line height, obliquity, and PFJ morphology. FA achieves this objective using CAS to continually perform intraoperative assessment of soft-tissue balance throughout the range to optimize implant position and avoid soft-tissue releases. In addition, FA accepts that a compromise on implant alignment or position may be required to restore suitable kinematics. Predicting and realigning the knee through its range of motion curve allows the soft tissues to maintain appropriate tension and restore normal kinematic features such as medial pivot. It can be difficult to measure flexion alignment preoperatively or postoperatively, which is why CAS is so crucial. Restoring soft-tissue tension throughout the range is potentially more important than static knee coronal plane alignment in extension and should serve as a guiding principle for surgeons applying FA to their surgical technique [[3], [4], [5]]. It is critical to measure stress gaps in extension and flexion to check knee kinematics [16].
KA studies, which also use a wide variety of implant positions, have not shown increased rates of revision for implant loosening or component migration despite implants being positioned outside of historical “safe zones” [17,18]. Aside from the PTS restrictions, the lead author currently uses an unrestricted approach to FA implant position, asserting the primacy of knee kinematics. Existing KA authors have recommended some degree of constraint in PTS because of concerns regarding subsidence and manufacturer recommendations and have not listed any failure for implant loosening within this range [5,9,12,13].
Summary
FA is an emerging TKA technique that uses CAS to realign and balance the knee in a way that optimizes implant position to a near-native alignment, restoring the most normal kinematics possible without resorting to soft-tissue releases.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: K. Hazratwala receives fellowship funding from DePuy and Stryker.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.01.029.
Appendix A. Supplementary data
References
- 1.Nam D., Nunley R.M., Barrack R.L. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014;96-b:96. doi: 10.1302/0301-620X.96B11.34152. [DOI] [PubMed] [Google Scholar]
- 2.Steer R., Tippett B., Khan R.N., et al. A prospective randomised control trial comparing functional with mechanical axis alignment in total knee arthroplasty: study protocol for an investigator initiated trial. Trials. 2021;22:523. doi: 10.1186/s13063-021-05433-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kayani B., Konan S., Tahmassebi J., et al. A prospective double-blinded randomised control trial comparing robotic arm-assisted functionally aligned total knee arthroplasty versus robotic arm-assisted mechanically aligned total knee arthroplasty. Trials. 2020;21:194. doi: 10.1186/s13063-020-4123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang J.S., Kayani B., Wallace C., et al. Functional alignment achieves soft-tissue balance in total knee arthroplasty as measured with quantitative sensor-guided technology. Bone Joint J. 2021;103-b:507. doi: 10.1302/0301-620X.103B.BJJ-2020-0940.R1. [DOI] [PubMed] [Google Scholar]
- 5.Oussedik S., Abdel M.P., Victor J., et al. Alignment in total knee arthroplasty. Bone Joint J. 2020;102-b:276. doi: 10.1302/0301-620X.102B3.BJJ-2019-1729. [DOI] [PubMed] [Google Scholar]
- 6.Hazratwala K., O’Callaghan W.B., Dhariwal S., et al. Wide variation in tibial slopes and trochlear angles in the arthritic knee: a CT evaluation of 4116 pre-operative knees. Knee Surg Sports Traumatol Arthrosc. 2021 doi: 10.1007/s00167-021-06725-2. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.MacDessi S.J., Griffiths-Jones W., Harris I.A., et al. Coronal plane alignment of the knee (CPAK) classification. Bone Joint J. 2021;103-b:329. doi: 10.1302/0301-620X.103B2.BJJ-2020-1050.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grant A.L., Doma K.D., Hazratwala K. Determination of the accuracy of navigated kinematic unicompartmental knee arthroplasty: a 2-year follow-up. J Arthroplasty. 2017;32:1443. doi: 10.1016/j.arth.2016.11.036. [DOI] [PubMed] [Google Scholar]
- 9.McEwen P., Balendra G., Doma K. Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J. 2019;101-b:331. doi: 10.1302/0301-620X.101B3.BJJ-2018-0544.R1. [DOI] [PubMed] [Google Scholar]
- 10.Kim Y.H., Park J.W., Kim J.S., et al. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38:379. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keshmiri A., Springorum H.R., Baier C., et al. Changes in sagittal component alignment alters patellar kinematics in TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2016;24:823. doi: 10.1007/s00167-016-4004-6. [DOI] [PubMed] [Google Scholar]
- 12.Matsumoto T., Takayama K., Ishida K., et al. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J. 2017;99-b:640. doi: 10.1302/0301-620X.99B5.BJJ-2016-0688.R2. [DOI] [PubMed] [Google Scholar]
- 13.McEwen P.J., Dlaska C.E., Jovanovic I.A., et al. Computer-assisted kinematic and mechanical axis total knee arthroplasty: a prospective randomized controlled trial of bilateral simultaneous surgery. J Arthroplasty. 2020;35:443. doi: 10.1016/j.arth.2019.08.064. [DOI] [PubMed] [Google Scholar]
- 14.Du Z., Chen S., Yan M., et al. Do size, shape, and alignment parameters of the femoral condyle affect the trochlear groove tracking? A morphometric study based on 3D- computed tomography models in Chinese people. BMC Musculoskelet Disord. 2017;18:4. doi: 10.1186/s12891-016-1374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lozano R., Campanelli V., Howell S., et al. Kinematic alignment more closely restores the groove location and the sulcus angle of the native trochlea than mechanical alignment: implications for prosthetic design. Knee Surg Sports Traumatol Arthrosc. 2019;27:1504. doi: 10.1007/s00167-018-5220-z. [DOI] [PubMed] [Google Scholar]
- 16.McEwen P.J. 1 ed. Elsevier; New York, NY: 2021. Calipered kinematically aligned total knee arthroplasty. [Google Scholar]
- 17.Klasan A., de Steiger R., Holland S., et al. Similar risk of revision after kinematically aligned, patient-specific instrumented total knee arthroplasty, and all other total knee arthroplasty: combined results from the Australian and New Zealand joint replacement registries. J Arthroplasty. 2020;35:2872. doi: 10.1016/j.arth.2020.05.065. [DOI] [PubMed] [Google Scholar]
- 18.Laende E.K., Richardson C.G., Dunbar M.J. A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Bone Joint J. 2019;101-b:929. doi: 10.1302/0301-620X.101B8.BJJ-2018-0755.R3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.