Abstract
Background
Fatigue, pain, and anxiety, symptoms commonly experienced by children with cancer, may predict pediatric symptom suffering profile membership that is amenable to treatment.
Methods
Three latent profiles (Low, Medium, and High symptom suffering) from 436 pediatric patients undergoing cancer care were assessed for association with three single-item symptoms and socio-demographic variables.
Results
Pediatric-PRO-CTCAE fatigue, pain, and anxiety severity scores at baseline were highly and significantly associated with the Medium and High Suffering profiles comprised of PROMIS pediatric symptom and function measures. The likelihood of membership in the Medium Suffering group was 11.37 times higher for patients who experienced fatigue severity than those with did not, while experience of pain severity increased the likelihood of the child’s membership in the Medium Suffering profile by 2.59 times and anxiety by 3.67 times. The severity of fatigue increased the likelihood of presence in the High Suffering group by 2.99 times while pain severity increased the likelihood of the child’s membership in the High Suffering profile by 6.36 times and anxiety by 16.75 times. Controlling for experience of symptom severity, older patients were more likely to be in the Higher or Medium Suffering profile than in the Low Suffering profile; no other socio-demographic or clinical variables had a significant effect on the latent profile classification.
Conclusion
Clinician knowledge of the strong association between fatigue, pain, and anxiety severity and suffering profiles may help focus supportive care to improve the cancer experience for children most at risk from time of diagnosis through treatment.
Keywords: Patient-reported outcomes, Pediatric oncology, Fatigue, Anxiety, Pain, Supportive care, Pediatric cancer
Introduction
Fatigue, pain, and anxiety are recognized as highly prevalent symptoms experienced by children with cancer. Fatigue has been reported by upwards of 80 [1] to 90% of pediatric oncology patients [2, 3]. Despite increased attentiveness towards pain management [4], children with cancer regularly identify pain as the most prevalent symptom due to underlying disease, medical procedures, and treatment side effects [5]. Snapshot pain profiles for children with cancer reveal at least half of children reporting active pain [6, 7]. Anxiety has been recognized as one of the most severe and long-lasting symptoms for children with cancer [8, 9].
The frequency of these symptoms and the lack of novel pharmaceutical therapeutics targeting these common symptoms risk their normalization as “part of” pediatric cancer [10]. These symptoms negatively impact function, quality of life, and even family strain [11–13]. The potential of the severity of these symptoms then predicts overall adverse event and suffering trajectories across time have been under-explored in pediatric oncology.
Prior latent class and latent profile investigations have revealed that distinct groups of children and adolescents exist regarding their experience with prevalence of subjective adverse events (AEs) during cancer treatment [14–16]. For each of the cross-sectional studies of symptoms and function utilizing the Pediatric Patient Reported Outcomes Measurement System (PROMIS) metrics, there has emerged a high symptom burden (High Suffering) and low-functioning cohort [15, 17, 18]. Our study team gave consideration to whether clinicians could utilize screening clinical assessment queries such as fatigue, pain, and anxiety severity metrics from the Ped-PRO-CTCAE (Pediatric version of the Patient-Reported Outcomes version of the Common Terminology Criteria For Adverse Events) to quickly achieve a verifiable impression of profile membership [19–21]. Clinician awareness of profile membership based on three symptom snapshots could translate into awareness of patients who may need additional symptom intervention or earlier attention to supportive care measures.
This paper explores whether the severity of fatigue, pain, and anxiety as self-reported by children with cancer at baseline may serve as predictors of pediatric patient presence in the Low, Medium, or High Suffering profile. Clinician knowledge of the strong association between the severity of these symptoms and membership in the High Suffering profile may help focus supportive care to improve the cancer experience for children most at risk from time of diagnosis through treatment.
Methods
Nine geographically distinct pediatric oncology centers served as the study sites with Institutional Review Board approval obtained at each site. Data collection occurred from October 2016 to October 2018. As previously described [22], participants completed PROMIS pediatric measures: four PROMIS pediatric symptoms (anxiety, depression, fatigue, pain), and one PROMIS pediatric function measure (mobility) at T1 (within 72 h preceding chemotherapy). The T1 survey was administered to patients and caregivers via tablets or paper surveys in-clinic. Data collection at T2 occurred 7 to 17 days later for those patients receiving chemotherapy, and 4 weeks later for patients receiving radiation.
Patients also completed the Ped-PRO-CTCAE at these time points, a validated set of items to determine the presence, severity, and interference with daily activities of subjective cancer treatment adverse events (AEs) as reported by children 7–17 years [19–21, 23]. Clinicians select AEs from the Ped-PRO-CTCAE library for inclusion in a clinical trial or for assessing clinical concerns. For this study, patients completed items for the three most frequently occurring AEs: fatigue, pain interference, and anxiety. The clinical measures of interest included the severity of fatigue, pain, and anxiety as reported by the child using Pediatric-PRO-CTCAE (PED-PRO-CTCAE) severity metrics. Measured attributes of fatigue on the PRO-CTCAE instrument include severity and interference while attributes for pain and anxiety both also additionally include frequency. Severity of AE was coded as a dichotomous measure for fatigue, pain, and anxiety: 1, if the severity score > 1; 0, otherwise. Items use a 7-day reference period with 4 response options per item consistent with CTCAE grading.
We first conducted descriptive analyses to examine the arithmetic average score (mean) and variation or dispersion (standard deviation) of each patient-reported PROMIS pediatric measures under study. Then, the longitudinal latent profile analysis (LLPA) [24, 25] was conducted. While LTA identifies potential latent profiles of children and adolescents at each specific time and then models profile changes across consecutive time points [16], LLPA, also referred to as repeated measures latent profile analysis, characterizes both within-person variation and between-person variation and identifies potential latent profiles based on groupings of similar patterns of outcome growth trajectory across time with no assumption about the form of outcome change, in a manner similar to spline or piece-wise models [26].
To determine the optimal number of latent profiles, models with different numbers of profiles were compared. Information criterion indices, such as Akaike’s information criterion (AIC), Schwarz’s Bayesian information criterion (BIC), and the sample size-adjusted BIC, as well as the Lo-Mendell-Rubin (LMR) test, the adjusted Lo-Mendell-Rubin (ALMR) test, and bootstrapped likelihood ratio (BLRT), were used for model comparison. The entropy statistic was used to assess the quality of profile classification. The values of entropy range from 0 to 1, and a value closer to 1 indicates better classification.
Once the latent profiles of growth trajectories of the PROMIS measures over time were identified, we tested the associations of the profile membership with socio-demographic (e.g., age, gender, race/ethnicity, and parental education) as well as clinical measures (e.g., time since diagnosis; hemoglobin; baseline pediatric psychological stress; cancer type; and severity of fatigue, pain, and anxiety). In testing such associations, a multinomial logit model was estimated using the newly developed 3-step approach [27, 28] so that the measurement errors in the latent profile membership estimate that are inevitable in mixture models including LLPA were taken into account in model estimation.
Conceptually speaking, in the first step of the three-step approach, an unconditional LPA model without any covariate was estimated. In step 2, the measurement errors in the latent profile estimation were calculated based on the results of step 1. And finally, the measurement errors calculated in step 2 were incorporated in the estimation of the multinomial logit model in step 3. The three-step model estimation was conducted simultaneously using Mplus 8.4 (Muthén & Muthén, 1998–2017). Data manipulation and descriptive statistics were conducted using SAS 9.4 (SAS Institute Inc., 2013).
Results
Our team approached a total of 580 child-caregiver dyads for study participation; however, 88 declined, and 10 withdrew before completing the T1 survey. A total of 436 children inclusive of 235 males and 195 females with cancer, mean age 13 (SD 3.4) years, reported baseline symptom burden. Children were approximately 5.6 (SD 7.3) months from cancer diagnoses and were surveyed on symptom severity within 72 h of beginning their next cycle of disease-directed treatment (T1) and again 7 to 17 days (or 4 + weeks later) following T1. Demographic summary is provided in Table 1.
Table 1.
Sample demographic and PED-PRO-CTCAE symptom severity descriptive findings (N = 436)
| Variable | Statistics |
|---|---|
| Child age (years) | |
| Mean (SD) | 13.03 (3.40) |
| Duration (month) since diagnosis | |
| Mean (SD) | 5.59 (7.34) |
| Hemoglobin (HGB) | |
| Mean (SD) | 10.47 (1.54) |
| n (%) | |
| Gender | |
| Male | 235 (54.65) |
| Female | 195 (45.35) |
| Race/ethnicity | |
| White | 242 (56.54) |
| Black | 73 (17.06) |
| Hispanic | 67 (15.65) |
| Others | 46 (10.75) |
| Parent education | |
| Elementary/primary school | 7 (1.64) |
| Secondary/high school | 88 (20.56) |
| Some college/university | 113 (26.40) |
| College/university | 155 (36.21) |
| Postgraduate degree | 65 (15.19) |
| Anxiety severity1 | |
| No | 258 (59.58) |
| Yes | 175 (40.42) |
| Fatigue severity2 | |
| No | 132 (30.34) |
| Yes | 303 (69.66) |
| Pain severity3 | |
| No | 216 (50.00) |
| Yes | 216 (50.00) |
| Cancer type | |
| Leukemia/lymphoma | 258 (59.17) |
| Solid tumor | 124 (28.44) |
| Neuro-oncology | 54 (12.39) |
Note. Frequencies of some variable may not sum up to N = 436 due to missing values
T1 PEDS-PRO_CTCAE anxiety severity score = > 1
T1 PEDS-PRO_CTCAE fatigue severity score = > 1
T1 PEDS-PRO_CTCAE pain severity score = > 1
Symptom severity as measured by the Ped-PRO-CTCAE items included fatigue severity in 69.7% of the children, pain severity in 50%, and anxiety severity in 40.4% at T1. The means and standard deviations of the symptoms reported by the PROMIS pediatric symptom measures at T1 and T2 are shown in Table 2.
Table 2.
PROMIS pediatric symptom measure mean scores by time
| PROMIS measure | Time 1 (N = 436) Mean (SD) | Time 2 (N = 382) Mean (SD) |
|---|---|---|
| Anxiety | 43.31 (9.98) | 41.33 (10.11) |
| Depression | 45.38 (10.60) | 43.40 (10.48) |
| Pain | 43.28 (8.93) | 43.14 (9.25) |
| Fatigue | 44.66 (11.91) | 43.67 (12.70) |
| Mobility | 44.30 (9.95) | 44.88 (10.78) |
| Stress | 47.98 (9.52) | 46.13 (9.66) |
Our LPA model results rejected the single-profile solution, indicating the patient population is not homogeneous but heterogeneous with respect to growth trajectory of all PROMIS measures from T1 to T2. By comparison of models with more than one profile, either the 3-profile or 4-profile model fits data well. While information criterion indices (e.g., AIC, BIC, ABIC) favored the 4-profile solution, LR tests (Lo-LMR, ALMR) favored the 3-profile solution. On the balance of goodness of fit, model parsimony, profile size, and clinical interpretability of the profiles, we preferred the 3-profile model. The three-profile LPA model achieved high-quality latent profile classification: the entropy statistic was 0.87, and the average latent profile probabilities for most likely latent profile membership were 0.95, 0.93, and 0.93, respectively.
The LLPA profile pattern is shown in Fig. 1. Those profiles represent an a priori unknown pattern of growth trajectories of the PROMIS measures over time. We defined Profile 1 as the Low Suffering Trajectory profile, Profile 2 as the Medium Suffering Trajectory profile, and Profile 3 as the High Suffering Trajectory profile. About 43.0% of the patients were classified into Profile 1, and 40.3% and 16.7% in Profiles 2 and 3, respectively.
Fig. 1.
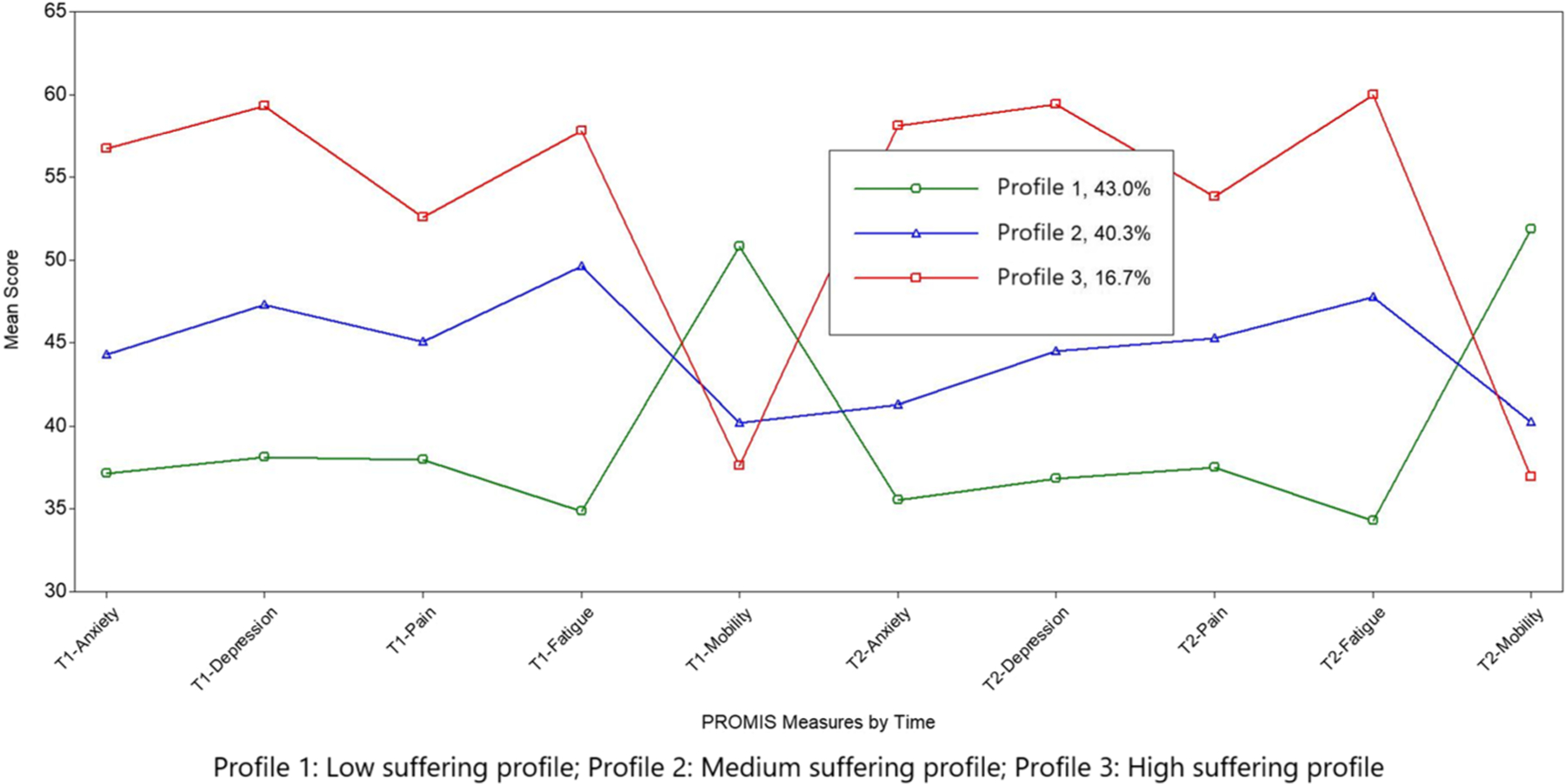
The LLPA profile pattern
The mean scores of four PROMIS pediatric symptom measures were lower (better) at T1 in Profile 1 and higher in Profiles 2 and 3. Such pattern remained unchanged at T2. The scores of the PROMIS function measure (mobility), which notably work in the opposite direction from the symptom scores in the PROMIS system, were higher (better) at both T1 and T2 in Profiles 1 and 2, and lower (worse) in Profile 3.
The effects of socio-demographic and clinical variables on latent profile membership are shown in Table 3. The presence of fatigue severity increased the likelihood of the child’s presence in the Medium Suffering group by 11.37 times (OR = 11.37, 95%C.I.: 4.53, 28.58), while pain severity increased the likelihood of the child’s presence in the Medium Suffering group profile by 2.59 times (OR = 2.59, 95% C.I.: 1.30, 5.15), and anxiety severity by 3.67 times (OR = 3.67, 95%C.I.: 1.76, 7.68). The presence of fatigue severity increased the likelihood of the child’s presence in the High Suffering group by 2.99 times (OR = 2.99, 95%C.I.: 1.08, 8.31), while pain severity increased the likelihood of the child’s presence in the High Suffering group profile by 6.36 times (OR = 6.36, 95%C.I.: 2.64, 15.34) and anxiety severity by 16.75 times (OR = 16.75, 95%C.I.: 6.36, 44.15). The effect of clinical variables such as hemoglobin, time since diagnoses, and cancer type was not statistically significant. Controlling for experience of the symptom severity, older patients were more likely to be in the Higher or Medium Suffering profile than in the Low Suffering profile; all other socio-demographic had no significant effect on the latent profile classification.
Table 3.
Effects of demographic and clinical variables on latent profile classification: selected results of multinomial logit model1
| Covariate | Latent Profile | ||
|---|---|---|---|
| High Symptom SufferingOR (95% C.I.) | Medium Symptom SufferingOR (95% C.I.) | Low Symptom SufferingOR (95% C.I.) | |
| Age | 1.22 (1.05, 1.41) * | 1.14 (1.03, 1.26)* | - |
| Gender | |||
| Female | - | - | - |
| Male | 0.80 (0.34, 1.91) | 0.89 (0.45, 1.76) | |
| Parent Education | 0.79 (0.35, 1.81) | 0.73 (0.37, 1.46) | - |
| <College | - | - | |
| College+ | 0.79 (0.35, 1.81) | 0.73 (0.37, 1.46) | - |
| Race | |||
| Others | - | - | |
| White | 0.48 (0.19, 1.25) | 0.83 (0.35, 1.97) | - |
| Black | 0.57 (0.17, 1.99) | 0.64 (0.23, 1.75) | |
| Time since diagnosis | |||
| ≤ Median | - | - | |
| > Median | 1.03 (0.98, 1.08) | 1.03 (0.99, 1.06) | |
| Hemoglobin | 1.00 (0.77, 1.30) | 0.80 (0.64, 1.00) | - |
| Fatigue Severity2 | |||
| No | - | - | |
| Yes | 2.99 (1.08, 8.31) * | 11.37 (4.53, 28.58)* | - |
| Pain Severity2 | |||
| No | - | - | |
| Yes | 6.36 (2.64, 15.34) * | 2.59 (1.30, 5.15)* | - |
| Anxiety Severity2 | |||
| No | - | - | |
| Yes | 16.75 (6.36, 44.15) * | 3.67 (1.76, 7.68)* | - |
| Cancer Type | |||
| Neuro-oncology | - | - | |
| Leukemia/Lymphoma | 2.56 (0.56, 11.79) | 1.66 (0.64, 4.34) | |
| Solid tumor | 3.00 (0.62, 14.61) | 1.74 (0.62, 4.89) | |
Notes:
-Reference group
Statistically significant as α < 0.05
Estimated using 3-step method in Mplus 8.4
Ped-PRO-CTCAE severity experience at baseline (T1)
Discussion
This study revealed that the severity of fatigue, pain, and anxiety as measured by the Ped-PRO-CTCAE single items at baseline inquiry were strongly associated with the phenotype of symptom suffering profiles in regard to longitudinal measures of four PROMIS measures (depression, anxiety, pain, and fatigue) and one PROMIS function measure (mobility) [14]. For busy clinicians, inquiring consistently and compassionately about this trifecta of symptoms (their severity, frequency, burdensomeness) from the perspective of the pediatric oncology patient would be high yield in prognostication regarding likely membership in a symptom suffering profile, and creates an opportunity for interventions to address these symptoms and potentially lessen suffering.
Of utmost importance in this work was that the reporting of symptom burden was directly obtained from child self-report via the Ped-PRO-CTCAE single severity items. Fatigue, pain, and anxiety are notably at risk of being under-reported by a pediatric patient’s caregiver [29, 30] and so clinician familiarity with pediatric patient report tools (Table 4) would further foster symptom recognition and reporting [31]. Patient-reported outcomes are increasingly recognized as the gold standard in pediatric oncology symptom tracking [21, 32].
While this study analyzed the individual presence of fatigue, pain, and anxiety, symptoms are rarely singular and are instead experienced simultaneously [33, 34]. Symptoms are experienced synergistically with exponential interactive effect [35–37]. A study of 67 childhood cancer patients receiving chemotherapy revealed those patients with fatigue experienced more behavior changes and depressive symptoms [38]. Physical discomfort, mood disturbance, cognitive wellness, and psychological discomfort notably cluster into symptom patterns for children receiving cancer-directed treatment [39–41]. This study was unique in offering a pediatric patient-centered analytic approach by utilizing the symptom severity to predict the child’s presence in a latent class symptom profile.
Treatments, treatment side effects, and comorbidities such as anemia collectively impact the child’s symptom burden. Furthermore, psychological concerns such as stress and loneliness contribute to the child’s collective cancer experience [42]. The presence of fatigue, pain, and anxiety significantly impacts total burden of symptoms experienced by the child [43] and decreases health-related quality of life [44]. Fatigue and sleep problems [45], pain, and anxiety may each and may together be expressed as lack of energy or decreased activity, sleepiness, mood changes, change in appetite, decreased concentration, and decreased interest in socialization or play. These symptoms combine to impact mental, emotional, relational, existential, and physical components of the pediatric cancer experience [46].
Recent development of family web pages for symptom reports and care encourages recommendations for symptom management based on clinical practice guidelines [47]. Using the case example of fatigue, few pharmaceutical options exist. Creativity has been a necessary component of fatigue innovations in pediatric oncology, such as task-oriented cognitive rehabilitation [48]; humor entertainment [49]; therapeutic videogames and mobile medical applications [50]; sleep-hygiene education, relaxation techniques, and progressive muscle relaxation [51]; and carnitine replacement [52] and even beetroot juice has been studied for reduction of exercise-induced fatigue [53]. Clearly, additional scientific inquiry is warranted to further understand the neurotransmitter, oxidative stress, and pathways which may contribute to cancer-related fatigue in order to advance symptom targets [54].
Despite the prevalence of pain in children treated for cancer and multiple available pharmacologic interventions, pediatric cancer-related pain remains under-treated, and many families and providers are wary of opioid pain medications [55]. Clinical practice guidelines specific to pain in pediatric cancer are needed, as is incorporation of evidenced-based non-pharmacologic interventions. Anxiety is similarly prevalent, particularly surrounding procedures and treatments [56]. Novel non-pharmacologic interventions to address pain and anxiety during pediatric cancer treatment have been used with some success throughout the cancer experience including creative arts therapy and massage [57], drawing and story-telling [58], and technologic interventions such as robots and virtual reality [59], and mHealth applications [60–62].
Recent efforts to feedback PROs to clinicians and families through formal reports or integration into the electronic health record may prove a promising strategy for early recognition of symptoms such as fatigue, pain, and anxiety [63–65], which could lead to earlier initiation of symptom-specific supportive care. Some patient subgroups experienced improvement in symptoms with PRO feedback to clinicians and families [66], presumably due to PRO adding new insight. Providers in the same study reported learning new information about psychosocial concerns from PROs, and many initiated consultations with specialists in pain management, psychosocial care, and palliative care as a result [66]. New strategies of simultaneous symptom capture linked with supportive care clinical practice guideline advice to families may be one avenue to simultaneously recognize and manage symptom burden [47].
A representative sample of the US pediatric population revealed that 47.5% of children experience fatigue, 48.5% pain behavior, and 52% anxiety using PROMIS pediatric symptom measures [67]. Of interest, our study’s PROMIS measures showed higher prevalence of fatigue at time point 1 with 69.7% of participants experiencing fatigue, similar pain prevalence of 50%, and lower prevalence of anxiety at 40.4% compared to representative sample from prior study.29 Pain interference and fatigue were higher (worse) in this sample than in a national sample, and anxiety and depressive symptoms were approximately the same as the national sample [67]. The mean score for psychological stress was lower than in the national sample [67].
Strengths of this particular study include prioritization of patient-reported outcomes and inclusion of multiple study sites. As this methodology relied on a single item at a time to predict profile membership, the findings may appeal to busy clinicians who may readily incorporate single or multiple symptom inquiry into patient care. Limitations of this study include current cohort including only children who understood English. The analyses did not separate participants according to treatment protocol or chemotherapy exposure dose, which is a recognized limitation since a longer time since diagnoses impacted likelihood of profile group assignment. As some children participated in the study during their first versus tenth cycle of chemotherapy, symptoms could notably differ as physiology and disease response changes with time. Future latent class analyses would benefit from longitudinal disease- and treatment-specific assessments. Use of conceptually similar/related single items was used to predict profile membership.
Conclusion
Direct reports from children on the presence and severity of fatigue, pain, and anxiety as individual symptoms can predict patterns of patient experiences based on the phenotypic probability of symptom burden. Conscientiousness about potential groups of children with cancer experiencing fatigue, pain, and anxiety during the treatment course could lead to earlier anticipation of suffering, preventative approach to functional impairment risks, and proactive mediations and integrative therapies to benefit the child’s quality of life [15].
While the prevalence of individual symptoms of pain, fatigue, and anxiety has been previously described in children with cancer, in this study, we found that the presence of each of these symptoms was strongly associated with greater suffering. The insight obtained from the profile analyses urges for interventions to improve suffering of children with cancer through earlier recognition of children at greatest risk of experiencing high symptom burden, and thereby earlier initiation of treatment to mitigate symptoms. In busy clinical practice, providers may struggle to prioritize the time required to inquire about an entire, extensive panel of potential symptoms. This study suggests that by asking children about pain, fatigue, and anxiety severity, or by soliciting their answers through PROs that are fed forward to clinicians, care teams may gain considerable insight into the experiences and needs of their patients.
Understanding the fatigue, pain, and anxiety experiences of children receiving cancer treatment from the perspective of the child is critical to refine supportive care interventions to minimize the symptom burden of disease-directed therapies and improve the quality of life for children with cancer.
Supplementary Material
Funding
This study was supported by the National Cancer Institute (R01CA175759) and the National Institute of Arthritis and Musculo-skeletal and Skin Diseases (U19AR069522).
Role of funding/support
Dr Weaver contributed to this paper in a private capacity. No official support or endorsement by the U.S. Department of Veterans Affairs is intended, nor should be inferred.
Appendix
Table 4.
Patient-reported outcome vocabulary and validated tools
| Symptom | Child-friendly words used | Instrument (and age appropriateness)* |
|---|---|---|
| Anxiety | Worried, nervous, scared | PROMIS pediatric anxiety (ages 8–17) |
| Fatigue | Tired, feeling tired, worn out | PROMIS pediatric fatigue (ages 8–17) Fatigue scale–children (ages 7–12) Fatigue scale—adolescents (ages 13–18) |
| Pain | Pain, hurt | Pain Squad app (ages 8–18) |
Ped-PRO-CTCAE (ages 7–17), Memorial Symptom Assessment Scale (MSAS) (versions for ages 7–12 and 10–18), and Symptom Screening in Pediatrics (SSPedi) (ages 8–18) are measures that assess all three symptoms listed above and have been validated in children with cancer
Footnotes
Ethics approval This study was approved by the Institutional Review Board Approval.
Consent to participate Freely given, informed consent to participate in the study was obtained from participants (or their parent or legal guardian in the case of children under legal age of majority). Assent was additionally obtained from pediatric-age patients.
Consent for publication Not applicable. Data de-identified.
Conflicts of interest The authors declare no competing interests.
Data availability
Data are available upon request from senior author.
References
- 1.Dupuis LL et al. (2010) Symptom assessment in children receiving cancer therapy: the parents’ perspective. Support Care Cancer 18(3):281–299 [DOI] [PubMed] [Google Scholar]
- 2.Enskar K, von Essen L (2007) Prevalence of aspects of distress, coping, support and care among adolescents and young adults undergoing and being off cancer treatment. Eur J Oncol Nurs 11(5):400–408 [DOI] [PubMed] [Google Scholar]
- 3.Ye ZJ et al. (2019) Symptoms and management of children with incurable cancer in mainland China. Eur J Oncol Nurs 38:42–49 [DOI] [PubMed] [Google Scholar]
- 4.Friedrichsdorf SJ, Postier AC (2019) Recent advances in pain treatment for children with serious illness. Pain Manag 9(6):583–596 [DOI] [PubMed] [Google Scholar]
- 5.Twycross A et al. (2015) Cancer-related pain and pain management: sources, prevalence, and the experiences of children and parents. J Pediatr Oncol Nurs 32(6):369–384 [DOI] [PubMed] [Google Scholar]
- 6.Miser AW et al. (1987) The prevalence of pain in a pediatric and young adult cancer population. Pain 29(1):73–83 [DOI] [PubMed] [Google Scholar]
- 7.Nunes MDR et al. (2019) Pain, sleep patterns and health-related quality of life in paediatric patients with cancer. Eur J Cancer Care (Engl) 28(4):e13029. [DOI] [PubMed] [Google Scholar]
- 8.Schlegelmilch M, et al. (2019) Observational study of pediatric inpatient pain, nausea/vomiting and anxiety. Children (Basel) 6(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng L et al. (2018) Perspectives of children, family caregivers, and health professionals about pediatric oncology symptoms: a systematic review. Support Care Cancer 26(9):2957–2971 [DOI] [PubMed] [Google Scholar]
- 10.Leahy AB, Feudtner C, Basch E (2018) Symptom monitoring in pediatric oncology using patient-reported outcomes: why, how, and where next. Patient 11(2):147–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang IC et al. (2018) Child symptoms, parent behaviors, and family strain in long-term survivors of childhood acute lymphoblastic leukemia. Psychooncology 27(8):2031–2038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baggott C et al. (2009) Multiple symptoms in pediatric oncology patients: a systematic review. J Pediatr Oncol Nurs 26(6):325–339 [DOI] [PubMed] [Google Scholar]
- 13.Walsh D, Rybicki L (2006) Symptom clustering in advanced cancer. Support Care Cancer 14(8):831–836 [DOI] [PubMed] [Google Scholar]
- 14.Hinds PS, et al. (2020) Subjective toxicity profiles of children in treatment for cancer: a new guide to supportive care? J Pain Symptom Manage [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buckner TW et al. (2014) Patterns of symptoms and functional impairments in children with cancer. Pediatr Blood Cancer 61(7):1282–1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J et al. (2018) A longitudinal study of PROMIS Pediatric Symptom clusters in children undergoing chemotherapy. J Pain Symptom Manage 55(2):359–367 [DOI] [PubMed] [Google Scholar]
- 17.Hinds PS et al. (2019) PROMIS pediatric measures validated in a longitudinal study design in pediatric oncology. Pediatr Blood Cancer 66(5):e27606. [DOI] [PubMed] [Google Scholar]
- 18.Yeh CH et al. (2008) Symptom clustering in older Taiwanese children with cancer. Oncol Nurs Forum 35(2):273–281 [DOI] [PubMed] [Google Scholar]
- 19.Reeve BB et al. (2020) Validity and reliability of the pediatric patient-reported outcomes version of the common terminology criteria for adverse events. J Natl Cancer Inst 112(11):1143–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McFatrich M et al. (2020) Mapping child and adolescent self-reported symptom data to clinician-reported adverse event grading to improve pediatric oncology care and research. Cancer 126(1):140–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reeve BB, et al. (2017) Eliciting the child’s voice in adverse event reporting in oncology trials: cognitive interview findings from the Pediatric Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events initiative. Pediatr Blood Cancer 64(3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hinds PS et al. (2021) Subjective toxicity profiles of children in treatment for cancer: a new guide to supportive care? J Pain Symptom Manage 61(6):1188–1195 e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Withycombe JS et al. (2019) The association of age, literacy, and race on completing patient-reported outcome measures in pediatric oncology. Qual Life Res 28(7):1793–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feldman BJ, Masyn KE, Conger RD (2009) New approaches to studying problem behaviors: a comparison of methods for modeling longitudinal, categorical adolescent drinking data. Dev Psychol 45(3):652–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lanza ST, Collins LM (2006) A mixture model of discontinuous development in heavy drinking from ages 18 to 30: the role of college enrollment. J Stud Alcohol 67(4):552–561 [DOI] [PubMed] [Google Scholar]
- 26.McArdle J (2004) Latent growth curve analyses using structural equation modeling techniques. In: Teti D (ed) Handbook of research methods in developmental science. Blackwell, Malden, MA, pp 340–366 [Google Scholar]
- 27.Vermunt J (2010) Latent class modeling with covariates: two improved three-step approaches. Polit Anal 18:450–469 [Google Scholar]
- 28.Asparouhov T, Muthén B (2014) Auxiliary variables in mixture modeling. Struct Equ Model A Multidiscip J 21:329–341 [Google Scholar]
- 29.Montgomery KE et al. (2020) Comparison of child self-report and parent proxy-report of symptoms: results from a longitudinal symptom assessment study of children with advanced cancer. J Spec Pediatr Nurs e12316. [DOI] [PubMed] [Google Scholar]
- 30.Mack JW et al. (2020) Agreement between child self-report and caregiver-proxy report for symptoms and functioning of children undergoing cancer treatment. JAMA Pediatr 174(11):e202861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pinheiro LC et al. (2018) Child and adolescent self-report symptom measurement in pediatric oncology research: a systematic literature review. Qual Life Res 27(2):291–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leahy AB, Steineck A (2020) Patient-reported outcomes in pediatric oncology: the patient voice as a gold standard. JAMA Pediatr 174(11):e202868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weaver MS et al. (2016) Concept-elicitation phase for the development of the pediatric patient-reported outcome version of the Common Terminology Criteria for Adverse Events. Cancer 122(1):141–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams PD et al. (2012) A symptom checklist for children with cancer: the therapy-related symptom checklist-children. Cancer Nurs 35(2):89–98 [DOI] [PubMed] [Google Scholar]
- 35.Dodd MJ, Miaskowski C, Lee KA (2004) Occurrence of symptom clusters. J Natl Cancer Inst Monogr 32:76–78 [DOI] [PubMed] [Google Scholar]
- 36.Docherty SL (2003) Symptom experiences of children and adolescents with cancer. Annu Rev Nurs Res 21:123–149 [PubMed] [Google Scholar]
- 37.Madden K et al. (2019) Systematic symptom reporting by pediatric palliative care patients with cancer: a preliminary report. J Palliat Med 22(8):894–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hockenberry MJ et al. (2011) Sickness behavior clustering in children with cancer. J Pediatr Oncol Nurs 28(5):263–272 [DOI] [PubMed] [Google Scholar]
- 39.Baggott C et al. (2012) Symptom cluster analyses based on symptom occurrence and severity ratings among pediatric oncology patients during myelosuppressive chemotherapy. Cancer Nurs 35(1):19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Atay S, Conk Z, Bahar Z (2012) Identifying symptom clusters in paediatric cancer patients using the Memorial Symptom Assessment Scale. Eur J Cancer Care (Engl) 21(4):460–468 [DOI] [PubMed] [Google Scholar]
- 41.Hooke MC et al. (2018) Physical activity, the childhood cancer symptom cluster-leukemia, and cognitive function: a longitudinal mediation analysis. Cancer Nurs 41(6):434–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rostagno E et al. (2020) Italian nurses knowledge and attitudes towards fatigue in pediatric onco-hematology: a cross-sectional nationwide survey. Int J Pediatr Adolesc Med 7(4):161–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miller E, Jacob E, Hockenberry MJ (2011) Nausea, pain, fatigue, and multiple symptoms in hospitalized children with cancer. Oncol Nurs Forum 38(5):E382–E393 [DOI] [PubMed] [Google Scholar]
- 44.Eche IJ, Eche IM, Aronowitz T (2020) An integrative review of factors associated with symptom burden at the end of life in children with cancer. J Pediatr Oncol Nurs 37(4):284–295 [DOI] [PubMed] [Google Scholar]
- 45.Castelli L, et al. (2021) Sleep problems and their interaction with physical activity and fatigue in hematological cancer patients during onset of high dose chemotherapy. Support Care Cancer [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hooke MC, Garwick AW, Gross CR (2011) Fatigue and physical performance in children and adolescents receiving chemotherapy. Oncol Nurs Forum 38(6):649–657 [DOI] [PubMed] [Google Scholar]
- 47.Watling CZ et al. (2020) Development of the SPARK family member web pages to improve symptom management for pediatric patients receiving cancer treatments. BMC Cancer 20(1):923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akel BS et al. (2019) Cognitive rehabilitation is advantageous in terms of fatigue and independence in pediatric cancer treatment: a randomized-controlled study. Int J Rehabil Res 42(2):145–151 [DOI] [PubMed] [Google Scholar]
- 49.Lopes-Junior LC et al. (2020) Clown intervention on psychological stress and fatigue in pediatric patients with cancer undergoing chemotherapy. Cancer Nurs 43(4):290–299 [DOI] [PubMed] [Google Scholar]
- 50.Govender M et al. (2015) Clinical and neurobiological perspectives of empowering pediatric cancer patients using videogames. Games Health J 4(5):362–374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zupanec S et al. (2017) A sleep hygiene and relaxation intervention for children with acute lymphoblastic leukemia: a pilot randomized controlled trial. Cancer Nurs 40(6):488–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lai JS et al. (2016) A cross-sectional study of carnitine deficiency and fatigue in pediatric cancer patients. Childs Nerv Syst 32(3):475–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Swartz MC, et al. (2019) A narrative review on the potential of red beetroot as an adjuvant strategy to counter fatigue in children with cancer. Nutrients 11(12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown AL et al. (2021) Cerebrospinal fluid metabolomic profiles associated with fatigue during treatment for pediatric acute lymphoblastic leukemia. J Pain Symptom Manage 61(3):464–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fortier MA et al. (2020) Children’s cancer pain in a world of the opioid epidemic: challenges and opportunities. Pediatr Blood Cancer 67(4):e28124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dupuis LL et al. (2016) Anxiety, pain, and nausea during the treatment of standard-risk childhood acute lymphoblastic leukemia: a prospective, longitudinal study from the Children’s Oncology Group. Cancer 122(7):1116–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thrane S (2013) Effectiveness of integrative modalities for pain and anxiety in children and adolescents with cancer: a systematic review. J Pediatr Oncol Nurs 30(6):320–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Altay N, Kilicarslan-Toruner E, Sari C (2017) The effect of drawing and writing technique on the anxiety level of children undergoing cancer treatment. Eur J Oncol Nurs 28:1–6 [DOI] [PubMed] [Google Scholar]
- 59.Lopez-Rodriguez MM, et al. (2020) New technologies to improve pain, anxiety and depression in children and adolescents with cancer: a systematic review. Int J Environ Res Public Health 17(10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hunter JF et al. (2020) A pilot study of the preliminary efficacy of Pain Buddy: a novel intervention for the management of children’s cancer-related pain. Pediatr Blood Cancer 67(10):e28278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jibb LA, et al. (2017) Implementation and preliminary effectiveness of a real-time pain management smartphone app for adolescents with cancer: a multicenter pilot clinical study. Pediatr Blood Cancer 64(10) [DOI] [PubMed] [Google Scholar]
- 62.Ander M et al. (2017) Guided internet-administered self-help to reduce symptoms of anxiety and depression among adolescents and young adults diagnosed with cancer during adolescence (U-CARE: YoungCan): a study protocol for a feasibility trial. BMJ Open 7(1):e013906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Snaman J et al. (2020) Pediatric Palliative Care in Oncology. J Clin Oncol 38(9):954–962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sung L, Miller TP, Phillips R (2020) Improving symptom control and reducing toxicities for pediatric patients with hematological malignancies. Hematology Am Soc Hematol Educ Program 2020(1):280–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cook S et al. (2020) Feasibility of a randomized controlled trial of symptom screening and feedback to healthcare providers compared with standard of care using the SPARK platform. Support Care Cancer 28(6):2729–2734 [DOI] [PubMed] [Google Scholar]
- 66.Wolfe J et al. (2014) Improving the care of children with advanced cancer by using an electronic patient-reported feedback intervention: results from the PediQUEST randomized controlled trial. J Clin Oncol 32(11):1119–1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Carle AC et al. (2021) Using nationally representative percentiles to interpret PROMIS pediatric measures. Qual Life Res 30(4):997–1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon request from senior author.


