Abstract
Background:
Emergency department (ED) physicians often need to quickly assess patients and determine vital signs to prioritize them by the severity of their condition and make optimal treatment decisions. Effective triage requires optimal scoring systems to accelerate and positively influence the treatment of trauma cases. To this end, a variety of scoring systems have been developed to enable rapid assessment of ED patients. The present systematic review and meta-analysis aimed to investigate the accuracy of the rapid emergency medicine score (REMS) system in predicting the mortality rate in non-surgical ED patients.
Methods:
A systematic search of articles published between 1990 and 2020 was conducted using various scientific databases (Medline, Embase, Scopus, Web of Science, ProQuest, Cochrane Library, IranDOC, Magiran, and Scientific Information Database). Both cross-sectional and cohort studies assessing the REMS system to predict mortality in ED settings were considered. Two reviewers appraised the selected articles independently using the National Institutes of Health (NIH) quality assessment tool. The random-effects model was used for meta-analysis. I2 index and Q statistic were used to examine heterogeneity between the articles.
Results:
The search resulted in 1,310 hits from which, 29 articles were eventually selected. Out of these, for 25 articles, the area under the curve value of REMS ranged from 0.52 to 0.986. The predictive power of REMS for the in-hospital mortality rate was high in 19 articles (67.85%) and low in nine articles (32.15%).
Conclusion:
The results showed that the REMS system is an effective tool to predict mortality in non-surgical patients presented to the ED. However, further evidence using high-quality design studies is required to substantiate our findings.
Keywords: Emergency medicine, Mortality, Emergencies, Systematic review, Meta-analysis
What’s Known
Previous studies have shown that the rapid emergency medicine score (REMS) system could be a valuable predictor of long-term mortality in non-surgical emergency department (ED) patients.
REMS is reported to have good prognostic potential (AUC=0.815) to predict hospital mortality in severely injured patients.
What’s New
Results of our systematic review showed that most of the included studies confirmed the REMS system as an effective tool to predict mortality in ED patients.
REMS is recommended as a valuable tool to predict in-hospital mortality in non-surgical patients admitted to the ED.
Introduction
The emergency department (ED) plays a pivotal role in managing complex and acute patients. 1 Triage in ED focuses on effective patient flow management, providing appropriate care, and preventing unnecessary interventions to improve medical outcome. 2 Emergency physicians often need to quickly assess patients, determine vital signs for prioritization, and make optimal decisions. Effective triage requires optimal scoring systems to accelerate treatment and positively influence treatment outcomes.
During the past decades, a variety of scoring systems have been developed to assess patients upon admission. The core element in these systems is an objective assessment of disease severity based on deviations in various physiological variables. More recently, researchers such as Nguyen 3 and Hyzy 4 have developed new scoring systems for critically ill trauma patients. However, none of these systems are dedicated to non-surgical ED patients. 3 The Acute Physiology and Chronic Health Evaluation II (APACHE II) system has been developed based on 12 physiological variables for use in the intensive care unit (ICU). However, APACHE II cannot be applied to ED patients due to the use of biochemical parameters. 5 The Rapid Acute Physiology Score (RAPS), a shortened version of APACHE II, 6 is one of the most appropriate scoring systems used in ED. It evaluates physiological parameters such as blood pressure, respiratory rate, pulse rate, and Glasgow coma scale (GCS). RAPS is further improved by including oxygen saturation and patient age, introducing a new system known as rapid emergency medicine score (REMS). 7 The benefit of these additions is that oxygen saturation can be easily measured in the ED, and age is an independent risk factor for severe diseases and mortality. A previous study showed that REMS is a powerful predictor of patient outcomes in the ED versus other scoring systems. 8 Another study reported that REMS could be a valuable predictor of long-term mortality in non-surgical ED patients. 9 In contrast, Söyüncü and Bektaş indicated that other scoring systems are more reliable than REMS. 10 Due to the lack of comprehensive data on the prognostic value of scoring systems, we performed a systematic review of the literature and meta-analysis to investigate the accuracy of REMS in predicting the mortality rate in non-surgical ED patients.
Materials and Methods
The study was approved by the Local Ethics Committee (code: IR.TBZMED.VCR.REC.1399.003). We conducted a systematic search from 1990 to 2020 using Medline (Ovid, PubMed), Embase, Scopus, Web of Science, ProQuest, and Cochrane Library. We also searched Iranian databases such as IranDOC, Magiran, and Scientific Information Database (SID). The search strategy included a combination of MeSH terms and free-text such as REMS, rapid emergency medicine score, rapid emergency medical score, and mortality (appendix 1-3). PICO (population, interventions, comparisons, outcomes) components were respectively non-surgical patients referred to ED, rapid emergency medicine score, other scoring systems, and mortality.
All identified citations were collated and uploaded into EndNote X9 (Clarivate Analytics, USA) followed by the exclusion of duplicate citations. Then, titles and abstracts were independently screened by two reviewers. The full texts of the screened articles were retrieved and assessed in detail. Inclusion criteria were using REMS as a predictive tool for mortality, studies conducted in ED, cross-sectional and cohort studies, non-surgical patients, and articles in English or Persian. Exclusion criteria were articles published before 1990, the use of languages other than English or Persian, and studies with patients discharged from ED or admitted to ED with cardiac arrest. The assessment was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA). 11 The quality of eligible articles was determined using the National Institutes of Health (NIH) quality assessment tool for observational cohort and cross-sectional studies. 12 Disagreements between reviewers were resolved through discussion until consensus was reached.
Eligible articles were appraised independently by two reviewers for methodological quality using standard critical appraisal tools. Disagreements between reviewers were resolved through mutual discussion. Following a critical appraisal, based on the degree of study bias, articles not fulfilling the quality threshold (i.e., meeting at least two items from the checklist) were excluded. The extracted data from the selected articles were the name of first author, publication year, country, setting, type of study, sample size, age, sex, admission reasons, study period (months), length of hospital stay (days), number of deceased patients, REMS score for survivors and non-survivors, the area under the curve (AUC) value of REMS, and the predictive power of REMS.
Statistical Analysis
The data were analyzed using Comprehensive Meta-Analysis software, version 3.0 (BioStat Inc., USA). The random-effects model was used for meta-analysis. I2 index and Q statistic were used to examine heterogeneity between the articles. Subgroup analysis was conducted based on the age of patients. P values less than 0.05 were considered statistically significant.
Results
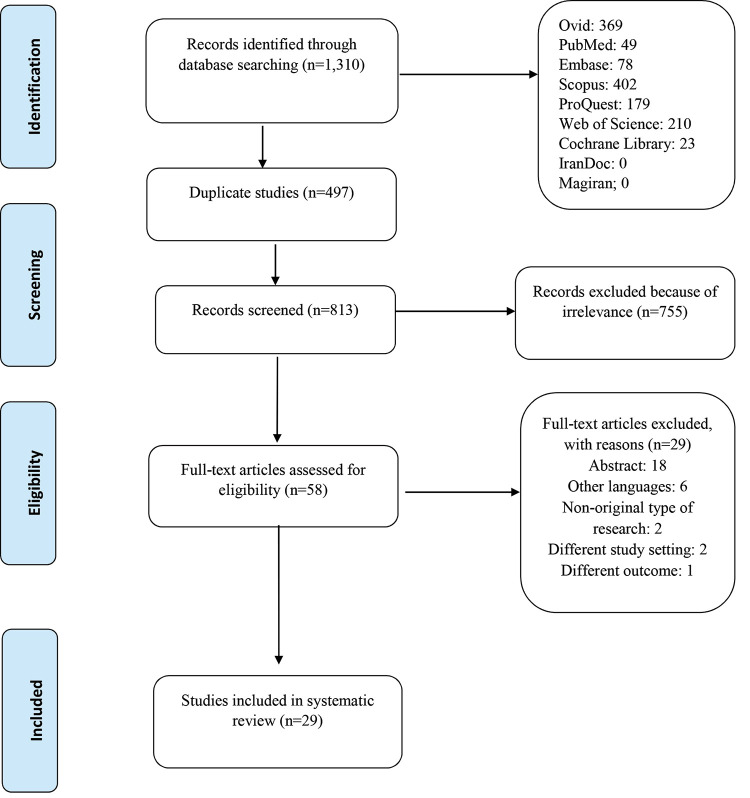
The search resulted in 1,310 hits, of which 497 duplicate articles were removed. From the remaining 813 articles, those that did not meet the inclusion criteria (n=755) were removed. The full texts of the remaining 58 were assessed for eligibility, resulting in the exclusion of a further 29 articles because of non-original type of research, different study settings, or using REMS for assessing patients for procedures other than non-surgical approaches. Subsequently, a total of 29 studies were included in our systematic review. As depicted in figure 1, the selection process was in accordance with the PRISMA checklist. Of the 29 included articles, eight were cross-sectional 13 - 20 and 21 were cohort 1 , 7 , 9 , 21 - 38 studies. A total of 550,966 patients were included in this study of which 324775 (58.95%), 226,191 (41.05%) were men and women, respectively. The mean age of the patients was 49.13 years (range: 6.2-90.8 years). The reported setting was ED and the patients were admitted because of sepsis, injuries, vibrio vulnificus infection, splenic abscess, hepatic portal venous gas; severe fever with thrombocytopenia syndrome, trauma, S. aureus bacteremia or other suspected infections, febrile; non-surgical, acute coronary syndrome, or internal diseases. The average study duration was 27.04±1.0 months (range: 5-183 months). More than 50% of the studies reported an average hospital stay of about six days. Most studies reported the number of deceased patients with an average mortality rate of 7.95% (table 1).
Figure 1.
The search strategy for the systematic review is illustrated according to the PRISMA guidelines.
Table 1.
Detailed characteristics of included articles retrieved from the data extraction form
| Author | Publication year | Country | Setting | Type of study | Sample size (n) | Average age | Admission reasons | Study period (month) | Length of hospital stay (day) | Number of deceased patients | REMS score for survivors | REMS score for non-survivors | AUC of REMS | Predictive power of REMS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||||||||
| Alter 21 | 2017 | USA | A county-based advanced life support EMS agency | Cohort | 28,035 | 33,311 | 51.9 | 12 | 4.3 | High | |||||
| Brabrand 22 | 2017 | Denmark | Hospital | Cohort | 2,917 | 2,867 | 67 | 5 | 1 (median) | 193 | 0.77 | Low | |||
| Bulut 23 | 2014 | Turkey | Hospital | Cohort | 1,039 | 961 | 61.41±18.92 | 6 | 153 | 5 | 7 | 0.589 | High | ||
| Cardenete-Reyes 13 | 2017 | Spain | Hospital | Cross-sectional | 67 | 37 | 60.25±11.06 | Acute coronary syndrome | 12 | High | |||||
| Carugati 24 | 2018 | Tanzania | Hospital | Cohort | Febrile | 11 | 44 | 0.52 | Low | ||||||
| Cattermole 14 | 2009 | Hong Kong | Hospital | Cross-sectional | 195 | 135 | 61.3±20.6 | 12 | 0.771 | Low | |||||
| Crowe 25 | 2010 | USA | Hospital | Cohort | 108 | 108 | Severe sepsis or septic shock | 13 | 1-45 | 10 | 11 | 0.62 | Low | ||
| Dundar 15 | 2015 | Turkey | Hospital | Cross-sectional | 507 | 432 | 71 (median) | Geriatric patients | 12 | 73 | 1 | 5 | 0.833 | High | |
| Ghanem-Zoubi 26 | 2011 | Israel | Community based hospital | Cohort | 582 | 490 | 74.7±16.1 | Sepsis | 15 | 8.77 | 387 | 8.4 | 11.9 | 0.77 | High |
| Gok 16 | 2018 | Turkey | Hospital | Cross-sectional | 144 | 106 | 57.60±20.82 | Internal diseases, surgery, and trauma | 24 | 0.703 | Low | ||||
| Goodacre 27 | 2006 | UK | Hospital | Cohort | 3,222 | 2,361 | 63.4 | 55 | 744 | 8.4 | 0.74 | High | |||
| Ha 17 | 2015 | Vietnam | Hospital | Cross-sectional | 806 | 940 | 7 (median) | 172 | 6 | 9 | 0.712 | High | |||
| Hilderink 28 | 2015 | Netherlands | Hospital | Cohort | 296 | 304 | 64.6 | Sepsis | 12 | 75 | 0.78 | Low | |||
| Howell 29 | 2007 | Israel | Tertiary care hospital | Cohort | 1,020 | 1,112 | 61 | Suspected infection | 10 | 83 | 5 | 10 | 0.80 | High | |
| Hung 1 | 2017 | Taiwan | Hospital | Cohort | 77 | 37 | 56.33±16.12 | Splenic abscess | 183 | 0.10 | 0.16 | 0.67 | Low | ||
| Imhoff 30 | 2014 | USA | Level one trauma center | Cohort | 2,718 | 962 | 36.5 | Trauma | 48 | 7.6 | 191 | 3.4 | 11.8 | 0.91 | High |
| Kuo 31 | 2013 | Taiwan | Hospital | Cohort | 96 | 75 | 63.1±12.3 | Vibrio vulnificus infection | 16.8±14.6 (mean±SD) | 43 | 5.4±2.3 | 9.7±2.6 | 0.895 | High | |
| Miller 32 | 2017 | USA | Level one trauma center | Cohort | 263,957 | 165,656 | Blunt and/or penetrating injuries | 5.2 (mean) | 3,382 | 2.9 | 17.7 | 0.967 | High | ||
| Nakhjavan-Shahraki 18 | 2017 | Iran | Hospital | Cross-sectional | 1,623 | 525 | 39.50±17.27 | Trauma | 123 | 0.92 | High | ||||
| Nakhjavan-Shahraki 19 | 2017 | Iran | Hospital | Cross-sectional | 605 | 209 | 11.65±5.36 | Trauma | 6 | 26 | 0.986 | High | |||
| Olsson 33 | 2003 | Sweden | Hospital | Cohort | 513 | 513 | 70±18.1 | 5 | 116 | 0.911 | High | ||||
| Olsson 9 | 2004 | Sweden | Hospital | Cohort | 5,663 | 6,087 | 61.9±20.7 | Non-surgical disorders | 12 | 3.2 | Predictor of long-term mortality | ||||
| Olsson 7 | 2004 | Sweden | Hospital | Cohort | 5,663 | 6,087 | 61.9±20.7 | Non-surgical disorders | 12 | 3.2 | 285 | 5.5 | 10.5 | 0.852 | High |
| Park 34 | 2017 | South Korea | Hospital | Cohort | 4,298 | 2,607 | 57.42±18.51 | Trauma | 60 | 24.95 | 212 | 4.31 | 9.71 | 0.9 | High |
| Polita 35 | 2014 | Brazil | Hospital | Cohort | 131 | 32 | 38±18 | Trauma | 5 | 17 | 4.9 | 0.761 | Low | ||
| Seak 36 | 2017 | Taiwan | Hospital | Cohort | 36 | 30 | 69.23±16.64 | Hepatic portal venous gas | 38 | 6.86 | 14.21 | 0.9286 | High | ||
| Sharma 37 | 2013 | USA | Tertiary care community hospital | Cohort | 241 | 56.95±17.62 | S. aureus bacteremia | 17 | 55 | 5.24 | 9.58 | 0.806 | High | ||
| Yang 38 | 2017 | China | Hospital | Cohort | 62 | 61 | 59±12 | Severe fever with thrombocytopenia syndrome | 38 | 31 | 8.55 | 12.45 | 0.746 | Low | |
| Ala 20 | 2020 | Iran | Hospital | Cross-sectional | 154 | 146 | 59.21±19.86 | Non-surgical disorders | 30 | 40 | High | ||||
REMS: Rapid emergency medicine score; AUC: Area under the curve
Methodological Quality Assessment
The quality of the included articles was assessed by two reviewers independently using the NIH quality assessment tool for observational cohort and cross-sectional studies. 12 All articles were judged to be fair or good (table 2). Since most of the articles used secondary data and were retrospective studies, three questions in the Critical Appraisal Skills Programme (CASP) checklist (numbers 8, 10, and 12) were deemed not applicable and therefore omitted (table 3).
Table 2.
The quality rating of included articles using the National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies
| No. | Author | Publication year | Quality rating (reviewer 1) | Quality rating (reviewer 2) |
|---|---|---|---|---|
| 1 | Alter 21 | 2017 | Good | Good |
| 2 | Brabrand 22 | 2017 | Fair | Fair |
| 3 | Bulut 23 | 2014 | Fair | Fair |
| 4 | Cattermole 14 | 2009 | Fair | Fair |
| 5 | Carugati24 | 2018 | Good | Good |
| 6 | Crowe 25 | 2010 | Good | Good |
| 7 | Dundar 15 | 2015 | Fair | Fair |
| 8 | Ghanem-Zoubi 26 | 2011 | Fair | Fair |
| 9 | Gok 16 | 2018 | Fair | Fair |
| 10 | Goodacre 27 | 2006 | Fair | Fair |
| 11 | Ha 17 | 2015 | Fair | Fair |
| 12 | Hilderink 28 | 2015 | Fair | Fair |
| 13 | Howell 29 | 2007 | Fair | Fair |
| 14 | Hung1 | 2017 | Fair | Fair |
| 15 | Imhoff 30 | 2014 | Fair | Fair |
| 16 | Kuo 31 | 2013 | Good | Good |
| 17 | Miller 32 | 2017 | Fair | Fair |
| 18 | Nakhjavan-Shahraki 18 | 2017 | Fair | Fair |
| 19 | Nakhjavan-Shahraki 19 | 2017 | Fair | Fair |
| 20 | Olsson 33 | 2003 | Fair | Fair |
| 21 | Olsson 9 | 2004 | Fair | Fair |
| 22 | Olsson 7 | 2004 | Fair | Fair |
| 23 | Park 34 | 2017 | Fair | Fair |
| 24 | Polita 35 | 2014 | Fair | Fair |
| 25 | Cardenete-Reyes 13 | 2017 | Fair | Fair |
| 26 | Seak 36 | 2017 | Fair | Fair |
| 27 | Sharma 37 | 2013 | Good | Good |
| 28 | Yang 38 | 2017 | Good | Good |
| 29 | Ala 20 | 2020 | Good | Good |
Table 3.
Methodological quality assessment of included articles using the Critical Appraisal Skills Programme (CASP) checklist
| Author | 1: Objective | 2: Population definition | 3: Participation rate | 4: Selection criteria | 5: Sample size | 6: Exposure assessment | 7: Timeframe | 9: Exposure measures | 11: Outcome measures | 13: Loss to follow up | 14: Statistical analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alter 21 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Brabrand 22 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Bulut 23 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Cattermole 14 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Carugati 24 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Crowe 25 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Dundar 15 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Ghanem-Zoubi 26 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Gok 16 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Goodacre 27 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Ha 17 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Hilderink 28 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Howell 29 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Hung 1 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Imhoff 30 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Kuo 31 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Miller 32 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Nakhjavan-Shahraki 18 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Nakhjavan-Shahraki 19 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Olsson, et al 33 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Olsson 9 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Olsson 7 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Park 34 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Polita 35 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Cardenete-Reyes 13 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Seak 36 | Yes | Yes | CD | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Sharma 37 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Yang 38 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes |
| Ala 20 | Yes | Yes | CD | Yes | No | Yes | yes | No | No | CD | Yes |
CD: Could not be determined
Predictive Power of REMS
Almost all articles reported the average REMS score for survivors (5.10) and non-survivors (9.88). Except for four articles, average AUC values (0.79; range: 0.52-0.986) were reported. In these articles, REMS was considered independently or in comparison with other scoring systems. The predictive power of REMS for in-hospital mortality rate was high in 19 articles (67.85%) 7 , 9 , 13 , 15 , 17 - 19 , 21 , 23 , 26 , 27 , 29 - 34 , 36 , 37 and low in nine articles (32.15%). 1 , 14 , 16 , 22 , 24 , 25 , 28 , 35 , 38 Only one study reported that REMS was a good predictor of long-term mortality (4.7 years). 9
Meta-analysis
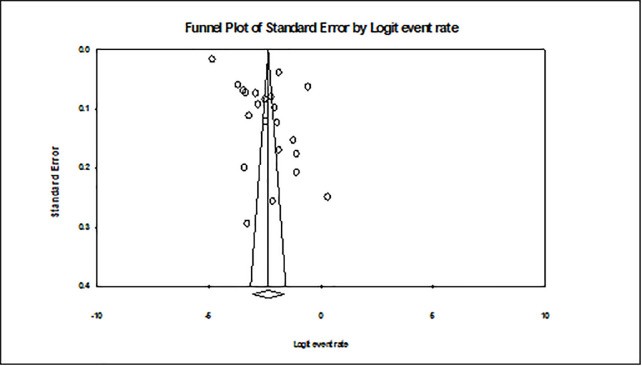
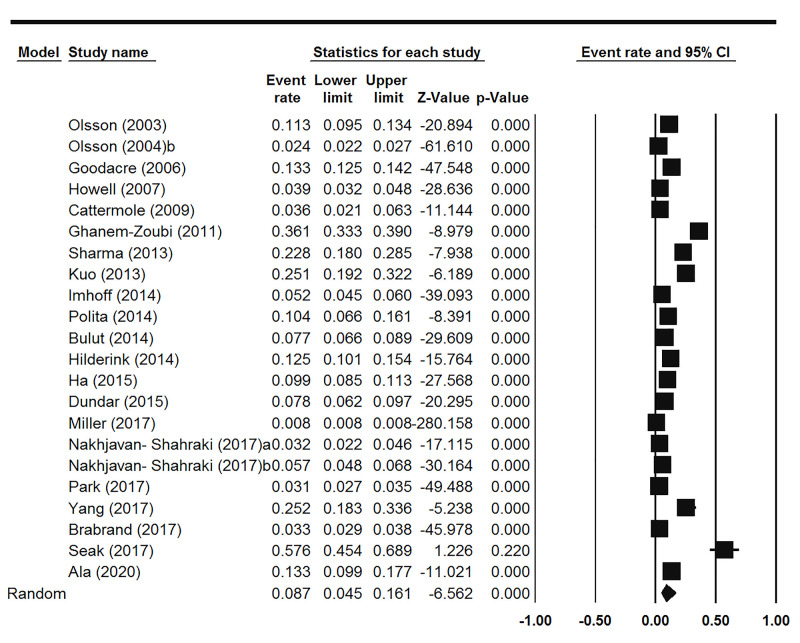
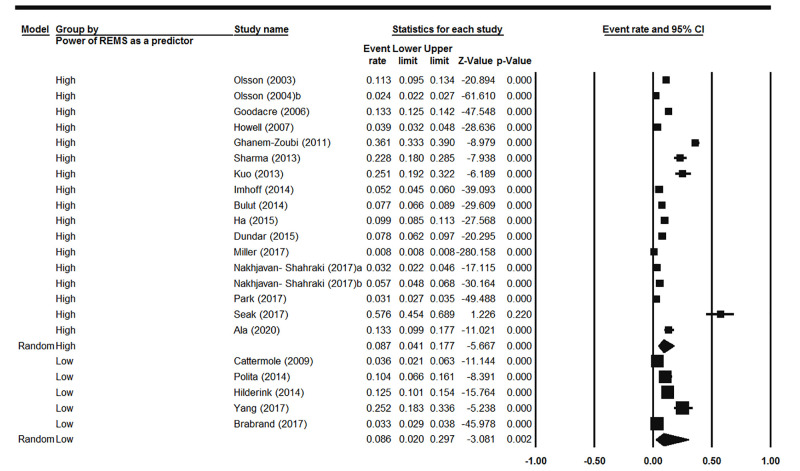
Twenty-two articles reported the percentage of mortality by surveying 477,186 ED cases. Publication bias was assessed using the funnel plot and Egger’s regression test. The results showed that diffusion between the articles was not statistically significant (t=0.59, df=20, P=0.281). Furthermore, the funnel plot showed symmetry between the articles (figure 2). Heterogeneity between the articles was significant (Q=11,340.14, df=21, I2=99.81, P<0.001), and the percentage of mortality was 8.69% (pooled death=0.0869, 95% CI: 4.50-16.11, P<0.001). The forest plot of the result of our meta-analysis is shown in figure 3.
Figure 2.
Funnel plot illustrates bias in the results of the meta-analysis.
Figure 3.
Forest plot depicted the mortality rates, which is extracted from the reviewed articles.
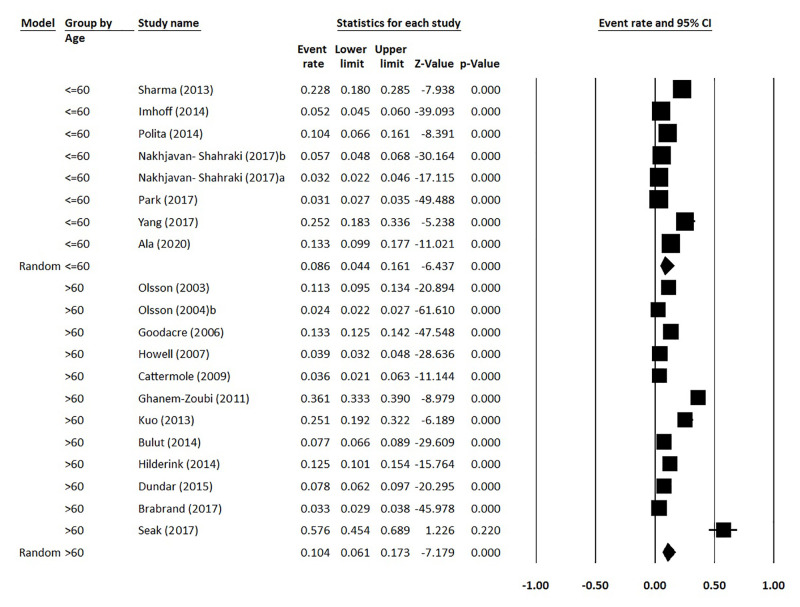
Subgroups Analysis
Subgroup analysis was conducted based on the age of the patients and the predictive power of REMS (table 4, figures 4 and 5). The results showed that the mortality rate in patients under versus above 60 years was 8.5% and 10.44%, respectively. Moreover, studies that evaluated the predictive power of REMS reported high and low levels of mortality rates at 8.72% and 8.59%, respectively.
Table 4.
Tabular presentation of the results of subgroups analysis
| Subgroup | Effect size and 95% interval | Null hypothesis | Heterogeneity | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number Studies | Proportion of patient deaths | Lower limit | Upper limit | Z-value | P value | Q-value | df | P value | I2 | ||
| Predictive power of REMS | High | 17 | 0.0872 | 0.0407 | 0.1771 | -5.67 | <0.001 | 10,881.68 | 16 | <0.001 | 99.85 |
| Low | 5 | 0.0859 | 0.0204 | 0.2973 | -3.08 | 0.002 | 184.62 | 4 | <0.001 | 97.83 | |
| Age | ≤60 | 8 | 0.0857 | 0.0398 | 0.1749 | -5.69 | <0.001 | 308.67 | 7 | <0.001 | 97.73 |
| >60 | 12 | 0.1044 | 0.0566 | 0.1847 | -6.34 | <0.001 | 1,856.35 | 11 | <0.001 | 99.41 | |
Figure 4.
Forest plot depicted the reported mortality rates in patients aged below and above 60 years.
Figure 5.
Forest plot indicated the reported mortality rates in terms of the high and low predictive power of REMS.
Discussion
The results of the present systematic review showed that the AUC value of REMS was 0.79. The majority of the included studies (67.85%) reported that the REMS system has a high or good predictive value for mortality. In contrast, a previous study reported the lack of sufficient evidence to conclude on the accuracy of prognostic models in patients with suspected infection admitted to the ED. 39 The results of another systematic review aimed at validating 10 different scoring systems, including REMS, reported that none of the systems could accurately predict the risk of in-hospital mortality and admission to the ICU. However, they found that REMS had an acceptable discriminatory power but poor calibration. 40
In the present study, we mainly focused on the ED setting, whereas some other review studies focused on other healthcare settings. Nonetheless, their findings on the predictive power of REMS were in line with our study. El-Sarnagawy and Hafez assessed different scoring systems, including REMS, in predicting the need for mechanical ventilation in patients with a drug overdose. They reported that REMS had a 100% positive predictive value and recommended this scoring system as an appropriate tool. 41 In contrast with our study, Yu and colleagues compared REMS with other scoring systems in terms of its predictive ability to detect clinical deterioration in non-ICU patients diagnosed with an infection. They measured each score serially to characterize how these scores changed with time. They reported that REMS had an AUC value of 0.70 and lacked adequate predictive value that other systems. 42 Ji and colleagues conducted a study in the ED and coronary care unit (CCU) of a hospital and showed that REMS did not have adequate predictive value for short-term risk of death in patients with acute myocardial infarction (AMI). After comparing REMS with Global Registry of Acute Coronary Events (GRACE) and APACHE II risk scores, they reported that the AUC value of REMS for predicting mortality in AMI patients within 30 days was 0.615. 43 In the present study, the average AUC value of REMS for non-surgical patients was 0.79, which is an acceptable predictive value.
We also compared the findings of the studies included in our systematic review with the results of other studies. One of the included articles reported that REMS was a good predictor of long-term in-hospital mortality (4.7 years). 9 Similarly, Olsson and colleagues showed that while REMS can be a predictor of long-term mortality, it cannot independently predict short-term (three-day, seven-day) mortality in non-surgical ED patients. 44 Seven studies in our systematic review were conducted in traumatic patients, five of which reported that REMS could accurately predict in-hospital mortality. 18 , 19 , 30 , 32 , 34 Lee and colleagues also reported that REMS had a good prognostic ability (AUC=0.815) to predict hospital mortality in severely injured patients. 45 Although most of the studies in our systematic review assessed patients with infectious diseases, the reported overall AUC>0.70 was in line with other studies conducted on traumatic patients. Furthermore, three studies were conducted on ED patients diagnosed with sepsis in the ED setting. Among these, one study reported the high predictive power of REMS for in-hospital mortality. 26 In line with our findings, another study reported that REMS had a good prognostic ability (AUC=0.72) to predict mortality in adult ED patients diagnosed with sepsis. 46
In the present systematic review, we selected studies that specifically focused on non-surgical patients. It is recommended that future studies include other categories of patients to further confirm the high prognostic ability of REMS to predict mortality. The main limitation of our systematic review was related to poor quality or lack of access to the full text of some of the selected articles, as well as the exclusion of studies published in languages other than English and Persian.
Conclusion
The results of the present systematic review and meta-analysis showed that the REMS system is an effective tool to predict hospital mortality in non-surgical patients admitted to ED. The use of the REMS system is recommended in ED to predict mortality and serve as a basis for developing an efficient care plan. However, further evidence using high-quality design studies is required to substantiate our findings.
Acknowledgement
The authors would like to express their gratitude for the financial support from the Vice-Chancellor for Research of Tabriz University of Medical Sciences, Tabriz, Iran.
Authors’ Contribution
A.Gh: Acquisition and analysis of data, Drafting and critical revision of the manuscript for important intellectual content; N.V: Systematic search, analysis of data, Drafting and critical revision of the manuscript for important intellectual content; S.Sh.V: Study design, Critical reviews, Drafting of the manuscript; A.A: Study concept and design, Drafting and critical revision of the manuscript for important intellectual content; M.J: Study concept and design, Critical reviews, Acquisition of Data, Drafting and critical revision of the manuscript for important intellectual content; All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest: None declared.
References
- 1.Hung SK, Ng CJ, Kuo CF, Goh ZNL, Huang LH, Li CH, et al. Comparison of the Mortality in Emergency Department Sepsis Score, Modified Early Warning Score, Rapid Emergency Medicine Score and Rapid Acute Physiology Score for predicting the outcomes of adult splenic abscess patients in the emergency department. PLoS One. 2017;12:e0187495. doi: 10.1371/journal.pone.0187495. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson R, Goodacre SW, Klingbajl M, Kelly AM, Rainer T, Coats T, et al. Evaluation of the DAVROS (Development And Validation of Risk-adjusted Outcomes for Systems of emergency care) risk-adjustment model as a quality indicator for healthcare. Emerg Med J. 2014;31:471–5. doi: 10.1136/emermed-2013-202359. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen HB, Rivers EP, Havstad S, Knoblich B, Ressler JA, Muzzin AM, et al. Critical care in the emergency department a physiologic assessment and outcome evaluation. Academic Emergency Medicine. 2000;7:1354–61. doi: 10.1111/j.1553-2712.2000.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 4.Hyzy RC. ICU scoring and clinical decision making. Chest. 1995;107:1482–3. doi: 10.1378/chest.107.6.1482. [DOI] [PubMed] [Google Scholar]
- 5.Bhagwanjee S, Paruk F, Moodley J, Muckart DJ. Intensive care unit morbidity and mortality from eclampsia: an evaluation of the Acute Physiology and Chronic Health Evaluation II score and the Glasgow Coma Scale score. Crit Care Med. 2000;28:120–4. doi: 10.1097/00003246-200001000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Rhee KJ, Fisher CJ, Willitis NH. The Rapid Acute Physiology Score. Am J Emerg Med. 1987;5:278–82. doi: 10.1016/0735-6757(87)90350-0. [DOI] [PubMed] [Google Scholar]
- 7.Olsson T, Terent A, Lind L. Rapid Emergency Medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J Intern Med. 2004;255:579–87. doi: 10.1111/j.1365-2796.2004.01321.x. [DOI] [PubMed] [Google Scholar]
- 8.Wei X, Ma H, Liu R, Zhao Y. Comparing the effectiveness of three scoring systems in predicting adult patient outcomes in the emergency department. Medicine (Baltimore) 2019;98:e14289. doi: 10.1097/MD.0000000000014289. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olsson T, Terent A, Lind L. Rapid Emergency Medicine Score can predict long-term mortality in nonsurgical emergency department patients. Acad Emerg Med. 2004;11:1008–13. doi: 10.1197/j.aem.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 10.Söyüncü S, Bektaş F. Comparison of the scoring systems for predicting mortality in intoxicated patients hospitalized to the ICU: a prospective observational study. Erciyes Medical Journal. 2011;33:29–34. [Google Scholar]
- 11.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Health, Lung, and Blood Institutes [Internet] . Study Quality Assessment Tools. [update July 2021] . Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools .
- 13.Cardenete-Reyes C, Gonzalez-Pascual JL, Tellez-Galan G, Velarde-Garcia JF, Polo-Portes CE, Palacios-Cena D. Mortality risk and complications relating to interhospital transfers of patients with acute coronary syndrome receiving primary coronary angioplasty performed by the Medical Emergency Service of Madrid 112: a group comparison study. Hong Kong Journal of Emergency Medicine. 2017;24:177–85. [Google Scholar]
- 14.Cattermole GN, Mak SK, Liow CH, Ho MF, Hung KY, Keung KM, et al. Derivation of a prognostic score for identifying critically ill patients in an emergency department resuscitation room. Resuscitation. 2009;80:1000–5. doi: 10.1016/j.resuscitation.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Dundar ZD, Karamercan MA, Ergin M, Colak T, Tuncar A, Ayrancı K, et al. Rapid emergency medicine score and HOTEL score in geriatric patients admitted to the emergency department. International Journal of Gerontology. 2015;9:87–92. doi: 10.1016/j.ijge.2015.02.003. [DOI] [Google Scholar]
- 16.Gok RGY, Gok A, Bulut M. Assessing prognosis with modified early warning score, rapid emergency medicine score and worthing physiological scoring system in patients admitted to intensive care unit from emergency department. Int Emerg Nurs. 2019;43:9–14. doi: 10.1016/j.ienj.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Ha DT, Dang TQ, Tran NV, Vo NY, Nguyen ND, Nguyen TV. Prognostic performance of the Rapid Emergency Medicine Score (REMS) and Worthing Physiological Scoring system (WPS) in emergency department. Int J Emerg Med. 2015;8:18. doi: 10.1186/s12245-015-0066-3. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakhjavan-Shahraki B, Baikpour M, Yousefifard M, Nikseresht ZS, Abiri S, Mirzay Razaz J, et al. Rapid Acute Physiology Score versus Rapid Emergency Medicine Score in Trauma Outcome Prediction; a Comparative Study. Emerg (Tehran) 2017;5:e30. [ PMC Free Article ] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakhjavan-Shahraki B, Yousefifard M, Faridaalaee G, Shahsavari K, Oraii A, Hajighanbari MJ, et al. Performance of physiology scoring systems in prediction of in-hospital mortality of traumatic children: A prospective observational study. J Clin Orthop Trauma. 2017;8:S43–S8. doi: 10.1016/j.jcot.2017.08.001. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ala A, Vahdati SS, Jalali M, Parsay S. Rapid Emergency Medicine Score as a Predictive Value for 30-day Outcome of Nonsurgical Patients Referred to the Emergency Department. Indian J Crit Care Med. 2020;24:418–22. doi: 10.5005/jp-journals-10071-23456. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alter SM, Infinger A, Swanson D, Studnek JR. Evaluating clinical care in the prehospital setting: Is Rapid Emergency Medicine Score the missing metric of EMS? Am J Emerg Med. 2017;35:218–21. doi: 10.1016/j.ajem.2016.10.047. [DOI] [PubMed] [Google Scholar]
- 22.Brabrand M, Hallas P, Hansen SN, Jensen KM, Madsen JLB, Posth S. Using scores to identify patients at risk of short term mortality at arrival to the acute medical unit: A validation study of six existing scores. Eur J Intern Med. 2017;45:32–6. doi: 10.1016/j.ejim.2017.09.042. [DOI] [PubMed] [Google Scholar]
- 23.Bulut M, Cebicci H, Sigirli D, Sak A, Durmus O, Top AA, et al. The comparison of modified early warning score with rapid emergency medicine score: a prospective multicentre observational cohort study on medical and surgical patients presenting to emergency department. Emerg Med J. 2014;31:476–81. doi: 10.1136/emermed-2013-202444. [DOI] [PubMed] [Google Scholar]
- 24.Carugati M, Zhang HL, Kilonzo KG, Maze MJ, Maro VP, Rubach MP, et al. Predicting Mortality for Adolescent and Adult Patients with Fever in Resource-Limited Settings. Am J Trop Med Hyg. 2018;99:1246–54. doi: 10.4269/ajtmh.17-0682. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crowe CA, Kulstad EB, Mistry CD, Kulstad CE. Comparison of severity of illness scoring systems in the prediction of hospital mortality in severe sepsis and septic shock. J Emerg Trauma Shock. 2010;3:342–7. doi: 10.4103/0974-2700.70761. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghanem-Zoubi NO, Vardi M, Laor A, Weber G, Bitterman H. Assessment of disease-severity scoring systems for patients with sepsis in general internal medicine departments. Crit Care. 2011;15:R95. doi: 10.1186/cc10102. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodacre S, Turner J, Nicholl J. Prediction of mortality among emergency medical admissions. Emerg Med J. 2006;23:372–5. doi: 10.1136/emj.2005.028522. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hilderink MJ, Roest AA, Hermans M, Keulemans YC, Stehouwer CD, Stassen PM. Predictive accuracy and feasibility of risk stratification scores for 28-day mortality of patients with sepsis in an emergency department. Eur J Emerg Med. 2015;22:331–7. doi: 10.1097/MEJ.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 29.Howell MD, Donnino MW, Talmor D, Clardy P, Ngo L, Shapiro NI. Performance of severity of illness scoring systems in emergency department patients with infection. Acad Emerg Med. 2007;14:709–14. doi: 10.1197/j.aem.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 30.Imhoff BF, Thompson NJ, Hastings MA, Nazir N, Moncure M, Cannon CM. Rapid Emergency Medicine Score (REMS) in the trauma population: a retrospective study. BMJ Open. 2014;4:e004738. doi: 10.1136/bmjopen-2013-004738. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuo SH, Tsai CF, Li CR, Tsai SJ, Chao WN, Chan KS, et al. Rapid Emergency Medicine Score as a main predictor of mortality in Vibrio vulnificus-related patients. Am J Emerg Med. 2013;31:1037–41. doi: 10.1016/j.ajem.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 32.Miller RT, Nazir N, McDonald T, Cannon CM. The modified rapid emergency medicine score: A novel trauma triage tool to predict in-hospital mortality. Injury. 2017;48:1870–7. doi: 10.1016/j.injury.2017.04.048. [DOI] [PubMed] [Google Scholar]
- 33.Olsson T, Lind L. Comparison of the rapid emergency medicine score and APACHE II in nonsurgical emergency department patients. Acad Emerg Med. 2003;10:1040–8. doi: 10.1111/j.1553-2712.2003.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 34.Park HO, Kim JW, Kim SH, Moon SH, Byun JH, Kim KN, et al. Usability verification of the Emergency Trauma Score (EMTRAS) and Rapid Emergency Medicine Score (REMS) in patients with trauma: A retrospective cohort study. Medicine (Baltimore) 2017;96:e8449. doi: 10.1097/MD.0000000000008449. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polita JR, Gomez J, Friedman G, Ribeiro SP. Comparison of APACHE II and three abbreviated APACHE II scores for predicting outcome among emergency trauma patients. Rev Assoc Med Bras (1992) 2014;60:381–6. doi: 10.1590/1806-9282.60.04.018. [DOI] [PubMed] [Google Scholar]
- 36.Seak CJ, Yen DH, Ng CJ, Wong YC, Hsu KH, Seak JC, et al. Rapid Emergency Medicine Score: A novel prognostic tool for predicting the outcomes of adult patients with hepatic portal venous gas in the emergency department. PLoS One. 2017;12:e0184813. doi: 10.1371/journal.pone.0184813. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma M, Szpunar S, Khatib R. Validating severity of illness scoring systems in the prediction of outcomes in Staphylococcus aureus bacteremia. Am J Med Sci. 2013;346:87–91. doi: 10.1097/MAJ.0b013e31826767f0. [DOI] [PubMed] [Google Scholar]
- 38.Yang B, Wang X, Li Y, Wu A, Liu Q, Lu Y, et al. A Newly Established Severity Scoring System in Predicting the Prognosis of Patients with Severe Fever with Thrombocytopenia Syndrome. Tohoku J Exp Med. 2017;242:19–25. doi: 10.1620/tjem.242.19. [DOI] [PubMed] [Google Scholar]
- 39.Calle P, Cerro L, Valencia J, Jaimes F. Usefulness of severity scores in patients with suspected infection in the emergency department: a systematic review. J Emerg Med. 2012;42:379–91. doi: 10.1016/j.jemermed.2011.03.033. [DOI] [PubMed] [Google Scholar]
- 40.Brabrand M, Folkestad L, Clausen NG, Knudsen T, Hallas J. Risk scoring systems for adults admitted to the emergency department: a systematic review. Scand J Trauma Resusc Emerg Med. 2010;18:8. doi: 10.1186/1757-7241-18-8. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.El-Sarnagawy GN, Hafez AS. Comparison of different scores as predictors of mechanical ventilation in drug overdose patients. Hum Exp Toxicol. 2017;36:539–46. doi: 10.1177/0960327116655389. [DOI] [PubMed] [Google Scholar]
- 42.Yu S, Leung S, Heo M, Soto GJ, Shah RT, Gunda S, et al. Comparison of risk prediction scoring systems for ward patients: a retrospective nested case-control study. Crit Care. 2014;18:R132. doi: 10.1186/cc13947. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ji CL, Zhou HR, Peng CH, Yang XL, Zhang Q. [Comparison of value of GRACE, APACHEII and REMS for early prognosis of death in patients with acute myocardial infarction] Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2013;25:660–3. doi: 10.3760/cma.j.issn.2095-4352.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 44.Olsson T, Terent A, Lind L. Charlson Comorbidity Index can add prognostic information to Rapid Emergency Medicine Score as a predictor of long-term mortality. Eur J Emerg Med. 2005;12:220–4. doi: 10.1097/00063110-200510000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Lee SH, Park JM, Park JS, Kim KH, Shin DW, Jeon WC, et al. Utility of the Rapid Emergency Medicine Score (REMS) for predicting hospital mortality in severely injured patients. Journal of the Korean Society of Emergency Medicine. 2016;27:199–205. [Google Scholar]
- 46.Taylor RA, Pare JR, Venkatesh AK, Mowafi H, Melnick ER, Fleischman W, et al. Prediction of In-hospital Mortality in Emergency Department Patients With Sepsis: A Local Big Data-Driven, Machine Learning Approach. Acad Emerg Med. 2016;23:269–78. doi: 10.1111/acem.12876. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]