Abstract
Alcohol sales and consumption have increased during the coronavirus disease 2019 pandemic, but their downstream effects on alcohol-related liver disease (ALD) are unclear. We analyzed inter-hospital escalation-of-care referrals to our tertiary care inpatient liver unit across 18 months through December 2020. There was a significant rise in severe ALD with recent unhealthy drinking in our regional community during the pandemic.
Short Summary: During the coronavirus disease 2019 pandemic, the most frequent (46.9%) inter-hospital referral to our inpatient liver unit was for severe alcohol-related liver disease with contemporaneous unhealthy drinking. It was the only liver diagnosis that increased significantly during our study period, and patients were generally younger than with other liver disease etiologies.
INTRODUCTION
Declared by the World Health Organization on 11 March 2020 (WHO Director-General, 2020), the coronavirus disease 2019 (COVID-19) pandemic has been a generational calamity. For many individuals, the pandemic shaped a myriad of adverse medical and psychosocial consequences. Alcohol sales and self-reported consumption increased by ~20 and 60%, respectively, after March 2020 (Editor, 2020; Grossman et al., 2020). In comparison, data on their downstream effects on alcohol-related liver disease (ALD) are less well-characterized, though anecdotal reports suggest increased hospitalizations (Cahan, 2021). ALD has been a substantial cause of liver-related mortality and healthcare utilization in the USA for many years (Mellinger et al., 2018; Tapper and Parikh, 2018), so a timely understanding of its developments during the pandemic is of utmost public health importance. The present study’s primary aim was to estimate our regional trend of inter-hospital escalation-of-care referrals for hospitalized patients with severe ALD and recent unhealthy drinking during the first calendar year of the COVID-19 pandemic.
METHODS
Study setting and population
We are a high-volume tertiary referral liver transplant (LT) center experienced in caring for patients with the highest disease acuity, including severe hepatitis from harmful alcohol drinking (Weeks et al., 2018). The full spectrum of inter-hospital referrals that we regularly receive is well-suited for examining COVID-19-related changes in liver disease presentation in our regional community. In July 2019, we established a prospective registry of hospitalized patients referred for inter-hospital care escalation to our adult inpatient liver unit at the Johns Hopkins Hospital in Baltimore, Maryland. To minimize patient privacy incursions, the registry captured only clinical and demographic data immediately relevant to the triage decision. We obtained all information solely from referring healthcare providers and neither interacted with patients nor medical records until they arrived at our hospital. One hepatologist (AG) conducted over 90% of the exchanges with referring providers. Our remaining hepatologists provided coverage when AG was unavailable. Consequently, there have been no time gaps in the registry since its conception.
The present observational analysis excluded requests from outside of Maryland, its four neighboring states or the District of Columbia. These distant referrals were infrequent (∼5%) and unpredictable, without notable temporal patterns. We also excluded previous LT recipients since their inter-hospital referrals frequently involved non-liver-related conditions (e.g. pneumonia and hip fractures). The data underlying our article are available on reasonable request to the corresponding author (PC).
Definitions of liver diagnosis categories
We defined ALD-with-recent-drinking (ALD-RD) as ALD with alcohol use within the preceding 6 months, a predictor of mortality in acute severe ALD (Louvet et al., 2017). Advanced stage ALD can manifest in several conceptually distinct but often clinically overlapping forms: acute alcohol-associated hepatitis, acute-on-chronic liver failure and decompensated cirrhosis (Crabb et al., 2020). ALD-RD encompassed all these forms, provided there was recent alcohol consumption. In contrast, Other ALD described ALD-only cases that had no reported alcohol use during the previous 6 months. We also specified other common liver diagnoses, including non-alcoholic steatohepatitis (NASH), drug-induced liver injury (DILI) and hepatitis C virus (HCV). The other diagnostic category comprised liver diseases that were relatively infrequent at our center; these included hepatitis B virus, primary biliary cholangitis and Wilson’s disease. Finally, the Undiagnosed category indicated referrals that preceded the diagnosis of the underlying liver disease etiology.
Statistical analysis
We performed the nonparametric linear-by-linear test with 10,000 Monte Carlo permutations to assess trends across time for categorical variables. We also used the Kruskal–Wallis H test to compare continuous variables by study period. All statistical tests were two-tailed with α = 0.05, calculated using Stata/MP release 17.0 (StataCorp LLC, College Station, Texas).
Ethical considerations
The Johns Hopkins Institutional Review Boards determined our study as exempt research under the US Department of Health and Human Services regulations (IRB00236315).
RESULTS
Our study comprised 459 inter-hospital escalation-of-care requests from July 2019 through December 2020 (Table 1). The overall median age of referred patients was 53 years (P25–P75, 39–62), which was not significantly different between the study periods (P = 0.68). Men composed 57.5% of the overall cohort. The proportion of male referrals increased from 49.1 and 51.4% in the third (Q3) and fourth (Q4) quarters of 2019, respectively, to 61.2 and 54.8% during the same quarters in 2020, though it was not statistically significant (Ptrend = 0.36). As expected, most of the referrals originated from Maryland (70.4%); the next three most common states were Virginia (16.6%), Pennsylvania (5%) and West Virginia (4.1%). The distribution of origin states did not vary substantially during the study (Ptrend = 0.39).
Table 1.
Demographic and clinical information of hospitalized patients referred for inter-hospital transfer to the Johns Hopkins Hospital adult inpatient liver unit, stratified by time period starting in the third quarter (Q3) of 2019
| Overall (n = 459) | 2019 Q3 (n = 55) | 2019 Q4 (n = 70) | 2020 Q1 (n = 78) | 2020 Q2 (n = 65) | 2020 Q3 (n = 98) | 2020 Q4 (n = 93) | P value | |
|---|---|---|---|---|---|---|---|---|
| Age, median (P25–P75), y | 53 (39–62) | 54 (44–61) | 54 (37–59) | 54 (40–65) | 51 (38–60) | 51.5 (39–62) | 50 (40–64) | 0.68 |
| Men, no. (%) | 264 (57.5) | 27 (49.1) | 36 (51.4) | 49 (62.8) | 41 (63.1) | 60 (61.2) | 51 (54.8) | 0.36 |
| State, no. (%) | 0.39 | |||||||
| Maryland | 323 (70.4) | 39 (70.9) | 50 (71.4) | 53 (68.0) | 47 (72.3) | 70 (71.4) | 64 (68.8) | |
| Virginia | 76 (16.6) | 9 (16.4) | 9 (12.9) | 14 (18.0) | 12 (18.5) | 13 (13.3) | 19 (20.4) | |
| Pennsylvania | 23 (5.0) | 0 (0) | 8 (11.4) | 7 (9.0) | 4 (6.2) | 1 (1.0) | 3 (3.2) | |
| West Virginia | 19 (4.1) | 4 (7.3) | 2 (2.9) | 2 (2.6) | 0 (0) | 7 (7.1) | 4 (4.3) | |
| Delaware | 10 (2.2) | 1 (1.8) | 0 (0) | 1 (1.3) | 1 (1.5) | 4 (4.1) | 3 (3.2) | |
| District of Columbia | 8 (1.7) | 2 (3.6) | 1 (1.4) | 1 (1.3) | 1 (1.5) | 3 (3.1) | 0 (0) | |
| Liver disease*, no. (%) | ||||||||
| ALD-RD†† | 191 (41.6) | 18 (37.7) | 22 (31.4) | 31 (39.7) | 27 (41.5) | 50 (51.0) | 43 (46.2) | 0.007 |
| Other ALD** | 69 (15.0) | 10 (18.2) | 11 (15.7) | 12 (15.4) | 9 (13.9) | 15 (15.3) | 12 (12.9) | 0.47 |
| NASH | 55 (12.0) | 6 (10.9) | 5 (7.1) | 8 (10.3) | 7 (10.8) | 14 (14.3) | 15 (16.1) | 0.09 |
| DILI | 33 (7.2) | 3 (5.5) | 6 (8.6) | 4 (5.1) | 1 (1.5) | 7 (7.1) | 12 (12.9) | 0.17 |
| HCV | 27 (5.9) | 5 (9.1) | 1 (1.4) | 7 (9.0) | 3 (4.6) | 6 (6.1) | 5 (5.4) | 0.82 |
| Other | 70 (15.3) | 9 (16.4) | 13 (18.6) | 12 (15.4) | 17 (26.2) | 10 (10.2) | 9 (9.7) | 0.10 |
| Undiagnosed*** | 43 (9.4) | 8 (14.6) | 13 (18.6) | 8 (10.3) | 6 (9.2) | 4 (4.1) | 4 (4.3) | <0.001 |
| COVID-19, no. (%) | 7 (1.5) | NA | NA | 0 (0) | 1 (1.5) | 2 (2.0) | 4 (4.3) | 0.39† |
*A patient may have multiple liver diagnoses.
**ALD with no reported alcohol use during the preceding 6 months.
***Liver disease etiology not yet diagnosed at the time of referral.
†Based on 2020 Q2 through Q4 since 2020 Q1 only minimally overlapped the COVID-19 pandemic.
††Recent drinking (RD) is defined as alcohol use within the previous 6 months.
The inter-hospital referrals predominantly concerned ALD-RD (41.6% of all referrals), followed by Other ALD (15%), NASH (12%) and DILI (7.2%). Two-thirds of DILI referrals were due to acetaminophen toxicity; our registry did not capture information on the nature of toxic exposure (i.e. intentional, accidental or idiosyncratic) as it was not central to the triage decision. ALD-RD was the only liver diagnosis that increased significantly during the COVID-19 pandemic, rising from a baseline 32% of referrals in 2019—and 39.7% of referrals in the first quarter (Q1) of 2020—to 48.7% during the latter half of 2020 (Ptrend = 0.007). By contrast, Other ALD constituted 16.8 and 14.1% of all referrals in the second halves of 2019 and 2020, respectively (Ptrend = 0.47). The frequency of DILI—7.2% in 2019 Q3–Q4 and 9.9% in 2020 Q3–Q4 (Ptrend = 0.17)—was similarly unchanged. Other non-ALD liver diagnoses also largely remained stable over the study period (Table 1 and Fig. 1).
Fig. 1.
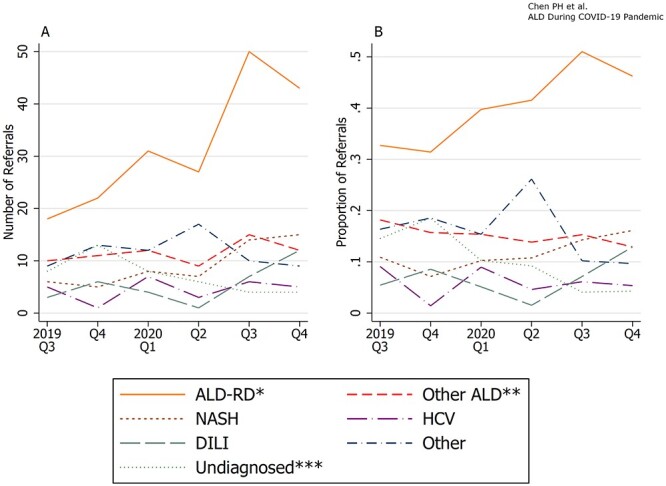
The number (A) and proportion (B) of inter-hospital escalation-of-care referrals to the Johns Hopkins Hospital liver unit from the third quarter of 2019 through the fourth quarter of 2020, stratified by liver disease diagnosis.
*Recent drinking (RD) is defined as alcohol use within the previous 6 months.
* *ALD with no reported alcohol use during the preceding 6 months.
***Liver disease etiology not yet diagnosed at the time of referral.
Among patients with ALD-RD, the median age of 44 years (P25–P75, 35–53) did not change over time (P = 0.88). They were collectively younger than patients with Other ALD (median age 56 years [P25–P75, 49–61]) or non-ALD diagnoses (median age 58 years [P25–P75, 46–66]) (P < 0.001). The proportion of men with ALD-RD changed from 38.9% (2019 Q3) and 50% (2019 Q4) to 60% (2020 Q3) and 55.8% (2020 Q4), though the trend was not statistically significant (Ptrend = 0.46). There was also no gender trend among patients with Other ALD, which remained stable with 76.2% men in 2019 Q3–Q4 and 70.4% in 2020 Q3–Q4 (Ptrend = 0.53). Similarly, non-ALD diagnoses also did not exhibit gender trends over time (Ptrend = 0.41).
DISCUSSION
For many, the COVID-19 pandemic has induced numerous psychosocial stressors—including social isolation, the dissolution of structured endeavors and unemployment—that can trigger or intensify harmful alcohol consumption (Flaudias et al., 2021). Market and survey studies have shown increased alcohol purchases and drinking during the pandemic (Editor, 2020; Grossman et al., 2020; Pollard et al., 2020). Accounting for nearly half of all liver-related deaths in the USA since 2000, ALD was already a devastating liver disease even before the COVID-19 era (Yoon and Chen, 2016). Our analysis now presents an 18-month perspective on the pandemic-associated rise in inter-hospital escalation-of-care referrals for severe ALD with recent unhealthy drinking in Maryland and neighboring states. The report leverages our vantage point from a high-acuity tertiary referral hospital with a specialized clinical and research center that serves patients with severe ALD (Weeks et al., 2018).
The three most common liver diagnoses in our study were, in descending order, ALD, NASH and DILI. A recent analysis of the US national trends among adult LT waitlist registrants saw similar findings after 2016, though the study did not include DILI (Wong and Singal, 2020). Patients with severe ALD and recent unhealthy drinking dominated the inter-hospital transfer referrals to our inpatient liver unit during the COVID-19 pandemic, growing 2.3-times in number or 1.5-times by percentage between corresponding months (July–December) in 2019 and 2020 (Table 1 and Fig. 1). Correspondingly, an internal audit of our program also suggested no slowing of LTs in 2020 for patients with ALD, even while many transplant centers in the country curtailed their practices during the pandemic’s early months (Strauss et al., 2021). Moreover, our program shifted toward a notably higher proportion of new LTs for ALD-RD during 2020 Q2–Q4 relative to our historical norm. We presented these data in greater detail elsewhere as they were generally outside the scope of the current report.
In our cohort, patients with severe ALD and recent unhealthy drinking were generally younger than individuals with other liver diagnoses. It was consistent with previous population-level surveillance data (Yoon and Chen, 2016; Tapper and Parikh, 2018), but we saw no age-related trends during our study period. We also discerned no significant gender trends in either our overall cohort or patients with recent unhealthy drinking. Our findings diverged from a 2020 RAND Corporation survey study during the early months of the pandemic, in which women reported more overall and heavy alcohol drinking days from 2019 to 2020 (Pollard et al., 2020). One possible explanation for our divergence may be gender-dependent decisions when external healthcare providers refer hospitalized patients.
One limitation of our study was its single-center perspective, but the prospective data from numerous referring hospitals created a valuable denominator that helped offset the weakness. Unlike analyses of a single-hospital census, our approach enabled us to identify hospitalized patients with liver disease in our regional community once local providers initiated a referral, irrespective of the success of the actual transfers. Another study limitation was our restricted access to patients’ clinical and demographic information at the time of inter-hospital referral to minimize potential intrusions in patient privacy. Our data relied on the reporting accuracy of the referring healthcare providers; we were unable to confirm the data ourselves via a manual review of individual medical records. Nonetheless, we expected any potential misclassification error to be nondifferential (i.e. random) across time and diagnosis groups. If anything, such scenarios often—albeit not universally—result in underestimating differences between groups (Alexander et al., 2014). A related limitation was our deferral to the referring provider on his/her professional practices for diagnosing unhealthy alcohol use. Local practices often favored history taking alone for self-reported alcohol intake, which is frequently associated with underreporting relative to alcohol biomarkers (Grüner Nielsen et al., 2021). Therefore, our study findings may potentially be a ‘best-case scenario’ regarding the frequency and escalation of decompensations from ALD with active drinking.
In summary, our report represents an early effort to quantify a heightened incidence of severe ALD with unhealthy alcohol drinking during the first calendar year of the COVID-19 pandemic. These timely findings support the early warnings by experts against potential downstream adverse effects from increased hazardous alcohol drinking during the pandemic (Da et al., 2020). ALD has been a leading driver of liver-related mortality in the USA over the past decade, particularly among young individuals (Yoon and Chen, 2016; Tapper and Parikh, 2018). Given population-wide rises in alcohol use during the COVID-19 era, we may continue to see surges of ALD-related complications for the foreseeable future, possibly even post-pandemic. There is a potential for exacerbating the already sizeable burden of ALD-related healthcare utilization (Mellinger et al., 2018).
To stem the unfortunate cascade of unwelcome events following increased drinking during the COVID-19 pandemic, health institutions may consider strengthening the synergy between substance use treatment and medical services from primary care to organ transplantation. There is some evidence that an integrated, co-located clinical model that jointly delivers addiction and medical care may be superior to standard referral practices at promoting and maintaining alcohol abstinence (Khan et al., 2016). Unfortunately, these multidisciplinary practices are currently uncommon, at least in our country. In a survey of primarily hepatologists and gastroenterologists in the USA, fewer than one-third of respondents reported working in an integrated clinic with addiction providers (Im et al., 2020). Further investigation is thus needed to identify best practices for implementing mitigation strategies toward potential causal effects between pandemic-related real-world events, alcohol consumption and ALD occurrence.
Conflict of Interest statement
Nothing to report.
FUNDING
We gratefully acknowledge funding by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award numbers K23AA028297 (Chen), K24AA027483 (Chander) and P50AA027054 (Chander and Cameron) and Gilead Sciences Research Scholars Program in Liver Disease—The Americas (Chen). The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health or other sponsors.
Role of the sponsor(s)
The sponsor(s) had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript and decision to submit the manuscript for publication.
Previous presentation
None.
Contributor Information
Po-Hung Chen, Division of Gastroenterology & Hepatology, Department of Medicine, Johns Hopkins University School of Medicine, 1800 Orleans Street, M2066, Baltimore, MD 21287, USA.
Peng-Sheng Ting, Division of Gastroenterology & Hepatology, Department of Medicine, Johns Hopkins University School of Medicine, 1800 Orleans Street, M2066, Baltimore, MD 21287, USA.
Erik Almazan, Johns Hopkins University School of Medicine, 733 N. Broadway, Baltimore, MD 21205, USA.
Geetanjali Chander, Division of General Internal Medicine, Department of Medicine, Johns Hopkins University School of Medicine, 2024 E. Monument Street, Baltimore, MD 21205, USA.
Andrew M Cameron, Division of Transplantation, Department of Surgery, Johns Hopkins University School of Medicine, 600 N. Wolfe Street, Blalock 424, Baltimore, MD 21287, USA.
Ahmet Gurakar, Division of Gastroenterology & Hepatology, Department of Medicine, Johns Hopkins University School of Medicine, 1800 Orleans Street, M2066, Baltimore, MD 21287, USA.
References
- Alexander LK, Lopes B, Ricchetti-Masterson K et al. (2014) Sources of Systematic Error or Bias: Information Bias. In e-periodical. Chapel Hill, North Carolina: UNC Gillings School of Global Public Health, 1–5. [Google Scholar]
- Cahan E. (2021) Pandemic-Fueled Alcohol Abuse Creates Wave of Hospitalizations for Liver Disease. Washington, DC, Kaiser Health News. https://khn.org/news/article/pandemic-fueled-alcohol-abuse-creates-wave-of-hospitalizations-for-liver-disease/ (17 April 2021, date last accessed). [Google Scholar]
- Crabb DW, Im GY, Szabo G et al. (2020) Diagnosis and treatment of alcohol-associated liver diseases: 2019 practice guidance from the American Association for the Study of Liver Diseases. Hepatology 71:306–33. [DOI] [PubMed] [Google Scholar]
- Da BL, Im GY, Schiano TD. (2020) Coronavirus disease 2019 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology 72:1102–8. [DOI] [PubMed] [Google Scholar]
- Director-General WHO. (2020) WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Editor . (2020) Nielsen COVID-19 Beverage Alcohol Insights. Healdsburg, CA, Wine Industry Advisor. https://wineindustryadvisor.com/2020/11/16/nielsen-covid-beverage-alcohol-insights (17 April 2021, date last accessed). [Google Scholar]
- Flaudias V, Zerhouni O, Pereira B et al. (2021) The early impact of the COVID-19 lockdown on stress and addictive behaviors in an alcohol-consuming student population in France. Front Psych 12:628631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman ER, Benjamin-Neelon SE, Sonnenschein S. (2020) Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int J Environ Res Public Health 17:E9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grüner Nielsen D, Andersen K, Søgaard Nielsen A et al. (2021) Consistency between self-reported alcohol consumption and biological markers among patients with alcohol use disorder – a systematic review. Neurosci Biobehav Rev 124:370–85. [DOI] [PubMed] [Google Scholar]
- Im GY, Mellinger JL, Winters A et al. (2020) Provider attitudes and practices for alcohol screening, treatment, and education in patients with liver disease: A survey from the American Association for the Study of Liver Diseases alcohol-associated liver disease special interest group. Clin Gastroenterol Hepatol. S1542-3565(20)31439-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, Tansel A, White DL, et al. (2016) Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: A systematic review. Clin Gastroenterol Hepatol 14: 191–202.e1-4; quiz e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louvet A, Labreuche J, Artru F et al. (2017) Main drivers of outcome differ between short term and long term in severe alcoholic hepatitis: A prospective study. Hepatology (Baltimore, Md) 66:1464–73. [DOI] [PubMed] [Google Scholar]
- Mellinger JL, Shedden K, Winder GS et al. (2018) The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology (Baltimore, Md) 68:872–82. [DOI] [PubMed] [Google Scholar]
- Pollard MS, Tucker JS, Green HD. (2020) Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open 3:e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss AT, Boyarsky BJ, Garonzik-Wang JM et al. (2021) Liver transplantation in the United States during the COVID-19 pandemic: National and center-level responses. Am J Transplant 21:1838–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapper EB, Parikh ND. (2018) Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: Observational study. BMJ (Clin Res Ed) 362:k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks SR, Sun Z, McCaul ME et al. (2018) Liver transplantation for severe alcoholic hepatitis, updated lessons from the World’s largest series. J Am Coll Surg 226:549–57. [DOI] [PubMed] [Google Scholar]
- Wong RJ, Singal AK. (2020) Trends in liver disease Etiology among adults awaiting liver transplantation in the United States, 2014-2019. JAMA Netw Open 3:e1920294. [DOI] [PubMed] [Google Scholar]
- Yoon Y-H, Chen CM. (2016) Surveillance Report #105: Liver Cirrhosis Mortality in the United States: National, State, and Regional Trends, 2000–2013. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism (NIAAA). [Google Scholar]


