Abstract
A 62 years old woman was diagnosed with multinodular toxic goiter and primary hyperparathyroidism/left parathyroid adenoma by hormonal assessment, ultrasound and nuclear thyroid/parathyroid scans. Cervical ultrasound illustrated a multinodular aspect of the thyroid with solid nodules and cystic-component nodules; the larger one represented a multinodular complex with necrosis areas in the left thyroid lobe, ACR TI-RADS score 4 (moderately suspicious). Functional nuclear imaging was performed for accurate differential diagnosis between thyroid vs. parathyroid localization, between cold vs. hot nodules, and eventually, for guiding the choice of a subsequent Fine-Needle Aspiration Biopsy (FNAB). Scans described an early intense 99mTc-sestaMIBI uptake with no 99mTc-pertechnetate uptake in the left thyroid lobe larger nodule. Due to the suspicion of malignancy for this nodule, we performed an additional scan (1 hour before the classical 2 hours parathyroid delayed scan). The intense uptake persists in both delayed scans suggesting no malignant phenotype and which was confirmed after surgery by benign histology. In conclusion, using a 99mTc-sestaMIBI personalized protocol, related to the radiotracer cellular uptake mechanisms: 1 hour scan (supplementary image, corresponding to the maximum uptake pattern of 99mTc-sestaMIBI for cancer cells) and 2 hours scan (for parathyroid washout evaluation) may avoid unnecessary extensive thyroid surgery.
Keywords: 99mTc-sestaMIBI, personalized protocol, uptake mechanisms, thyroid/parathyroid nodules
Introduction
Personalised nuclear diagnosis imaging is, undoubtedly, part of precision medicine approach, and based on concrete data, representing a clear example of evidenced based medicine, by understanding the cellular uptake mechanisms. Establishing an appropriate acquisition protocol is mandatory for making the correct differential diagnosis between thyroid vs. parathyroid nodules and could be useful for determining the differential diagnosis between malignant vs. benign images. Using Technetium-99mmethoxyisobutylisonitrile (99mTc-sestaMIBI) for the diagnosis of parathyroid adenoma could be an easy and standard technique, with early and 2 hours delayed images (1, 2). However, usually, studies do not take into consideration, in intricate thyroid/parathyroid nodular pathology, the possibility of standard protocol personalization, in two delay points: 1 hour scan (supplementary image, corresponding to the maximum uptake pattern of 99mTc-sestaMIBI for cancer cells, in case of such a suspicion) and 2 hours scan (for parathyroid washout evaluation), how this case aims to demonstrate.
Case presentation
A 62 years old woman with a personal history of recurrent renal lithiasis was admitted in the Endocrinology Department, for investigations of cervical antero-lateral multiple nodules, with the complaint of mild dysphagia. Physical examination of the cervical region revealed multiple painless thyroid nodules with different degrees of softness and a dominant one of 2 cm in size, located in the left thyroid lobe region. No cervical lymph nodes were palpable. Hormonal tests study showed subclinical hyperthyroidism (low TSH - 0.137 mIU/L, normal free T4 - 1.03ng/dL, FT4 - 1.03 ng/dL) and primary hyperparathyroidism (PTH - 323.1 pg/mL). Haematology and biochemistry tests were normal (phosphate - 2.71 mg/dL) apart from a hypercalcemia (serum calcium - 11.74 mg/dL) and a hypercalciuria - 423 mg/24h. Bone Mineral Density (BMD) documented osteoporosis (lumbar spine T score = - 4.1 SD, hip-neck T score = -2.4 SD, forearm T score = -3.8 SD).
Imaging investigations
Cervical Ultrasound (US) illustrated a multinodular-cystic aspect of the thyroid, with alternating echogenic foci, as follows: 3 cysts and 2 solid nodules in the right thyroid lobe, 2 other solid nodules and a cyst in the thyroid isthmus and finally, a big polycyclic nodule with multiple small cysts and necrosis areas inside, in the left thyroid lobe. Thyroid Imaging Reporting and Data System (TI-RADS) Committee of the American College of Radiology (ACR) was ACR TI-RADS score 4 (moderately suspicious). The diagnosis of multinodular toxic goiter with primary hyperparathyroidism was established and the patient was referred to further functional nuclear imaging investigations, to help, due to the multinodular aspect, differential diagnosis of nodules origins and, eventually, guide the choice of a nodule for a subsequent FNAB.
A combined 2 days’ protocol, with the 99mTc-pertechnetate (99mTcO4-) Thyroid scintigraphy on the first day (at 20 minutes after 111 MBq intravenous (iv) dose administration), followed by early (20 minutes) and late (1 and 2 hours) parathyroid images on the second day, after 444 MBq 99mTc-sestaMIBI iv dose administration, was performed.
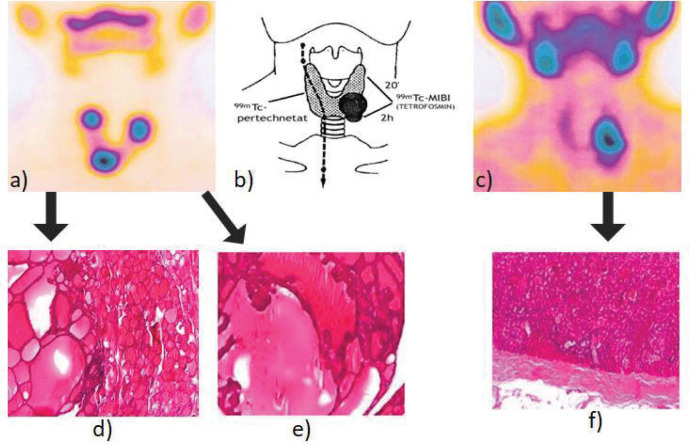
99mTcO4- thyroid images showed that a part of nodules structurally described on US images correspond, as seen in the Figure 1-a, to intense tracer uptakes, in the 1/3 upper region of the right lobe, in the lower area between this lobe and isthmus, and finally, in the 1/3 upper region of the left lobe.
Figure 1.
Thyroid/parathyroid images with two radiotracers, 99mTcO4- (a) and 99mTc sestaMIBI (early scan - at 20 minutes after iv administration) (c), showed comparatively, in addition to the parathyroid scintigraphy principle (b). The nodular formation described in ultrasounds in the left lobe area has an intense 99mTc-sestaMIBI uptake, discordant to the correspondent 99mTcO4-uptake, that presents a totally different nodular uptake pattern. Histopathology confirmed the image findings: colloidal goiter with macrofollicular adenomatous areas and lymphocytic thyroiditis, HE, x4 (d), alternated with macrofollicular adenomatous area with hyperfunctional pseudopapilla, HE, x4 (e) and parathyroid adenoma with oxyphil cells, trabecular and acinar architecture, HE, x4 (f).
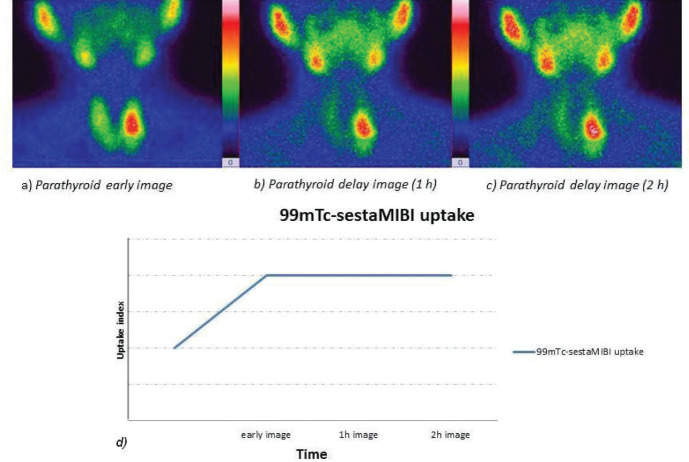
Early 99mTc-sestaMIBI parathyroid scan (Fig. 1-c) revealed an intense uptake in the projection area of the left thyroid lobe, with discordant pattern related to the 99mTcO4- uptake. As it was a high suspicion that this nodule could have a malignant substrate, it was decided to perform a 1 hour delayed scan before the classical 2 hours delayed image. The intense uptake persists in the same region in both delayed scans (quantified by the uptake index - Figure 2 - the graph is obtained by the software of the gamma camera, and it is based on the number of pixels in the images).
Figure 2.
The high 99mTc-sestaMIBI uptake in the projection area of the 1/3 region of the left thyroid lobe, in early images, persists with approximately the same intensity in both 1h and 2h delayed images (quantified by the uptake index - higher values for delayed images, in the graph), suggesting a parathyroid adenoma and less probably a malignant substrate.
Treatment
Taking into account the functional image characteristics of the large persistent uptake described on the 99mTc-sestaMIBI scan (which suggested a parathyroid adenoma) and the 99mTcO4- patchy nodular pattern (which also could not exclude the presence of a neoplastic thyroid nodule), the patient was referred to Surgery Department, and underwent a total thyroidectomy and left superior parathyroidectomy. An image guiding system was used for the surgery, using the Surgery Assist visualisation system (an image database transmission system for displaying, in the operating room, all medical images already performed for the patient) and the intraoperative gamma probe guidance (3-6). The implementation of Surgery Assist system in our hospital, through which the images from radiology and nuclear medicine units can be transmitted in the operating room, thus facilitating the visualisation of the lesions intraoperatively, is used in all thyroid-parathyroid surgery, resulting in shorter operative time and easier intraoperative finding of the lesions (7).
The histopathology report of the surgical specimens revealed left parathyroid adenoma and multiple thyroid adenomatous nodules with an iso-follicular aspect (Fig. 1- d, e, f).
Outcome and follow-up
After the uneventful thyroid - parathyroid surgery and with the histopathological confirmation of the exclusion of malignancy, the endocrinologist prescribed thyroid hormonal substitution drugs (Levothyroxine - 100 μg/day) and scheduled follow-ups. The severe osteoporosis was ameliorated, with the use of Bisphosphonate (Risedronate - 75 mg/day, 2 consecutive days/month) and an analogue of vitamin D (Alpha D3 - 0.5 μgx2/day).
Eight months after the surgery, the patient was symptom-free, with normalization of her PTH (40.4 pg/mL) and total calcium blood levels (8.76 mg/dL). The T score was also improved (lumbar spine T score from - 4.1 SD to -3.2 SD, hip-neck T score from -2.4 SD to -2.1 SD, forearm T score from -3.8 SD to -2.1 SD). In addition, calcium and PTH blood levels remained within normal limits (Table 1).
Table 1.
Laboratory test results in relation with parathyroid function, in evolution
| At baseline | 5 days after Surgery | 8 months after Surgery | |
|---|---|---|---|
| PTH concentration (15–65 pg/mL) | 323.1 | 40.4 | 39.47 |
| Total calcium (8.8–10 mg/dL) | 11.74 | 8.76 | 8.27 |
| Phosphate (2.3–4.7 mg/dL) | 2.71 | 3.95 | 3.06 |
Discussion
The principle of 99mTc-sestaMIBI parathyroid dual phase scan is related to the difference between influx and efflux mechanisms of the radiopharmaceutical used (2, 8). In the case of two radiotracers method, early visualization of thyroid tissue can be performed with the use of a tracer with thyroid tropism (99mTcO4- or 123I/131I). Different imaging patterns are related to benign or malignant nodes (1, 9-11), based on the particularities of the radiotracers cellular uptake mechanisms.
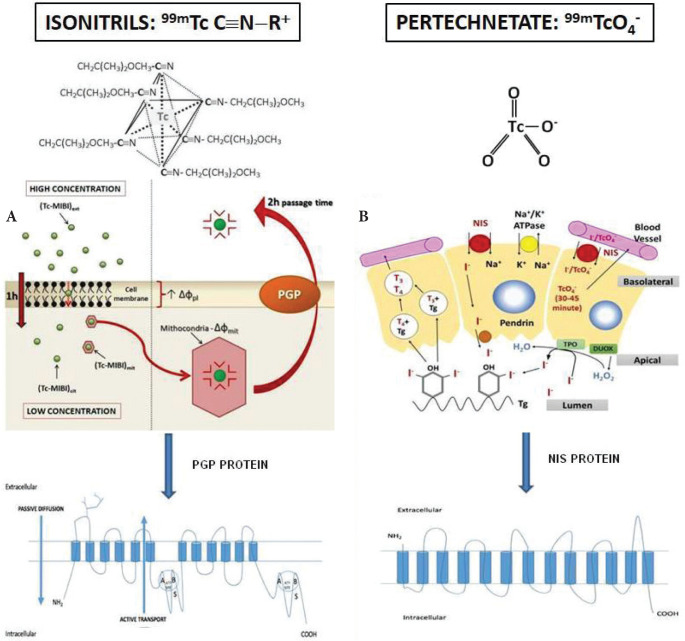
99mTc-pertechnetate uptake mechanism (Fig. 3-B)
Figure 3.
Schematic representation of 99mTc sestaMIBI influx/efflux (A), 99mTcO4- transport through NIS protein in the thyroid cell and of the iodide metabolism (B). Tg: thyroglobulin. T3 and T4: triiodothyronine and thyroxine hormones, respectively.
There is a similarity between the general characteristics of 99mTcO4- uptake and the transport of radioactive iodine, that is why 99mTcO4- represents a substrate for Sodium/Iodide Symporter (NIS), as well as 123I/131I. This analogy is due to its negative electric charge as well as iodine and a molecular weight >100u. However, the difference is that 99mTcO4- can be uptaken but not organified at the level of the thyroid cells; that is why it remains between 30 and 45 minutes after reaching the maximum concentration (at 10-15 minutes after iv administration) followed by its return to the blood through passive transport (12) (Fig. 3-B).
99mTc-isonitrile (99mTc-sestaMIBI) uptake mechanism (Fig. 3-A)
It has been reported that 99mTc-sestaMIBI parathyroid accumulation begins 4-6 minutes after administration. This short time according to the influx, allows acquisition of early images (15-20 minutes). This influx is dependent on several factors. Both the size of the gland and the degree of vascularization positively influences the tracer uptake. In the same way, the influx influences the uptake at the level of oxyphil cells and mitochondria of the parathyroid glands, whose number has been found increased in neoplastic diseases cells (13).
Hyperfunction and active cell growth phase (of the cell cycle) of thyroid and parathyroid cells lead to the uptake of higher amounts of radiopharmaceutical. The Ca2+ plasma level can also influence 99mTc-sestaMIBI kinetics by modifying the membrane potential (14).
Elimination occurs rapidly from normal tissue. Due to the characteristics of tumor cells and hyperplasia in the parathyroid adenoma, the radiotracer is retained in the pathological tissue (15). In the case of neoplasia and proportional to the degree of malignancy, the maximum uptake is described at 60 minutes and not at 120 minutes, like is the case of parathyroid adenoma demonstrated on delayed images (12, 16) (Fig. 3-A).
How 99mTc-sestaMIBI efflux in the cell is mediated by Permeability-GlycoProtein (PGP) and parathyroid adenoma cells have low expression of this protein, this could explain the slow wash-out as a result of a deficient efflux system. There will be no distinct region in which persists the intense radiotracer uptake on late images, if the nodule does not belong to the parathyroid tissue or corresponds only to a normal parathyroid region or even to a parathyroid hyperplasia, and this observation can be verified with radioguided surgery (17-19) (Fig. 3-A).
Consequence of these mechanisms, data confirms the utility of scintigraphy with 99mTc-isonitriles (99mTc-sestaMIBI or 99mTc-Tetrofosmin) in dual phase for the visualization of parathyroid adenomas. This method has up to 90% sensitivity and 98% specificity, which could be increased to 97% and 100%, respectively, by the use of Single Photon Emission Computed Tomography/Computed Tomography (SPECT/CT) (20). However, neck US has a sensitivity of 91% for diagnosing single parathyroid adenomas preoperatively (21), which decreases to 35% in cases with multiple hyperplasia, and even lower in double adenomas (22). The multiphase multidetector 4D CT shows a sensitivity of 81% for left/right localization and 73% for quadrant localization of parathyroid adenomas (23). It was reported that the sensitivity and the specificity of 18F-Fluorocholine Positron Emission Tomography/Computed Tomography (PET/CT), which has been used to image hyperfunctional parathyroid glands, could reach 92% and 100%, respectively (24). Despite its high accuracy, this imaging method is limited by its low availability.
The scintigraphy with two radiopharmaceuticals (99mTcO4- and 99mTc-isonitriles) is described as more useful than the scintigraphy with a single radiotracer - 99mTc-isonitriles for evaluating parathyroid lesions, especially when there are also benign or malignant thyroid related lesions (25-27). In addition, it is justified in such cases to use personalized protocols, based on radiotracers’ different cellular kinetics patterns, with 99mTc-isonitriles (dose 200-740 MBq) early images (at 15-20 minutes) and two points late images (at 60 and 120 minutes), with quantification and even an uptake graph of the radiotracers’ over time, to provide important arguments for the differential diagnosis of benign/malignant, thyroid nodule/parathyroid adenoma.
In conclusion, 99mTc-sestaMIBI and 99mTc-pertechnetate scans are essential tools in the differentiation between thyroid/parathyroid, cold/hot nodules, but a careful approach can improve the radiotracers effectiveness and avoid the passive “reading” of the images. Our conclusion underlines the necessity of personalised image acquisition protocols in completion to the pattern guided protocols, for intricate pathology, based on a mindful understanding of the radiotracer cellular uptake mechanism, to provide a personalized diagnostic approach and to develop new treatment strategies based on their results.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Contributorship
Wael Jalloul and Cipriana Stefanescu were responsible for information gathering, analysis of results and writing. Ruxandra Tibu contributed to linguistic verification and Layout. Teodor Marian Ionescu, Cati Raluca Stolniceanu, Irena Grierosu, Alexandru Tarca, contributed to the design and implementation of the study. Lidia Ionescu, Cristina Ungureanu, Delia Ciobanu, Vlad Ghizdovat provided crucial information about the clinical case.
References
- 1.Kannan S, Milas M, Neumann D, Parikh RT, Siperstein A, Licata A. Parathyroid nuclear scan. A focused review on the technical and biological factors affecting its outcome. Clin Cases Miner Bone Metab. 2014;11(1):25–30. [PMC free article] [PubMed] [Google Scholar]
- 2.Hindié E, Ugur Ö, Fuster D, O’Doherty M, Grassetto G, Ureña P, Kettle A, Gulec S, Pons F, Rubello D. 2009 EANM parathyroid guidelines. Eur J Nucl Med Mol Imaging. 2009;36:1201–1216. doi: 10.1007/s00259-009-1131-z. [DOI] [PubMed] [Google Scholar]
- 3.Kim B, Yousman W, Xiang Wong W, Cheng C, McAninch EA. Less is More: Comparing the 2015 and 2009 American Thyroid Association Guidelines for Thyroid Nodules and Cancer. Thyroid. 2016;26(6):759–764. doi: 10.1089/thy.2016.0068. [DOI] [PubMed] [Google Scholar]
- 4.Dănilă R, Livadariu R, Stefanescu C, Ciobanu D, Ionescu L. Radioguided Mediastinal Parathyroidectomy in a patient with persistent renal hyperparathyroidism. Acta Endocrinol (Buchar). 2017;13(4):514. doi: 10.4183/aeb.2017.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehrabibahar M, Mousavi Z, Sadeghi R, Layegh P, Nouri M, Asadi M. Feasibility and safety of minimally invasive radioguided parathyroidectomy using very low intraoperative dose of Tc-99m MIBI. Int J Surg. 2017;39:229–233. doi: 10.1016/j.ijsu.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Somnay YR, Weinlander E, Alfhefdi A, Schneider D, Sippel RS, Chen H. Radioguided parathyroidectomy for tertiary hyperparathyroidism. J Surg Res. 2015;195(2):406–411. doi: 10.1016/j.jss.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghizdovat V, Nita L, Herghelegiu P, Caraiman S, Capitanu A, Mihai C, Stolniceanu C, Wael J, Ciobanu D, Ionescu L, Grierosu I, Stefanescu C. IEEEXplore - E-Health and Bioengineering Conference 2019 (EHB) Romania: Iasi; 2019. USMED and Surgery Assist: IMAGO MOL Cluster Biomedical Solutions to Improve Patient Imaging Availability and Noninvasive Diagnosis. pp. 1–4. [Google Scholar]
- 8.Greenspan BS, Dillehay G, Intenzo C, Lavely W, O’Doherty M, Palestro CJ. SNM Practice Guideline for Parathyroid Scintigraphy 4.0*. J Nucl Med Technol. 2012;40:111–118. doi: 10.2967/jnmt.112.105122. [DOI] [PubMed] [Google Scholar]
- 9.Kuzminski SJ, Sosa JA, Hoang JK. Update in Parathyroid Imaging. Magn Reson Imaging Clin N Am. 2018;26(1):151–166. doi: 10.1016/j.mric.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, Rejnmark L, Thakker R, D’Amour P, Paul T, Van Uum S, Shrayyef MZ, Goltzman D, Kaiser S, Cusano NE, Bouillon R, Mosekilde L, Kung AW, Rao SD, Bhadada SK, Clarke BL, Liu J, Duh Q, Lewiecki EM, Bandeira F, Eastell R, Marcocci C, Silverberg SJ, Udelsman R, Davison KS, Potts JT, Jr, Brandi ML, Bilezikian JP. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int. 2017;28(1):1–19. doi: 10.1007/s00198-016-3716-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guo R, Wang J, Zhang M, Zhang M, Meng H, Zhang Y, Li B. Value of 99mTc-MIBI SPECT/CT parathyroid imaging and ultrasonography for concomitant thyroid carcinoma. Nucl Med Commun. 2017;38(8):676–682. doi: 10.1097/MNM.0000000000000692. [DOI] [PubMed] [Google Scholar]
- 12.Stefanescu C, Rusu V. Iasi, Romania: Ed. Tehnopress; 2007. From radiopharmaceuticals to functional and molecular imaging. [Google Scholar]
- 13.Carpentier A, Jeannotte S, Verreault J, Lefebvre B, Bisson G, Mongeau CJ, Maheux P. Preoperative localisation of parathyroid lesions in hyperparathyroidism: relationship between technetium-99m-MIBI uptake and oxyphil cell content. J Nucl Med. 1998;39(8):1441–1444. [PubMed] [Google Scholar]
- 14.Mehta NY, Ruda JM, Kapadia S, Boyer PJ, Hollenbeak CS, Stack BC., Jr. Relationship of Technetium Tc 99m Sestamibi Scans to Histopathological Features of Hyperfunctioning Parathyroid Tissue. Arch Otolaryngol Head Neck Surg. 2005;131:493–498. doi: 10.1001/archotol.131.6.493. [DOI] [PubMed] [Google Scholar]
- 15.Kao A, Shiau YC, Tsai SC, Wang JJ, Ho ST. Technetium-99m methoxy isobutyl isonitrile imaging for parathyroid adenoma: relationship to P-glycoprotein or multidrug resistance-related protein expression. Eur J Nucl Med Mol Imaging. 2002;29(8):1012–1015. doi: 10.1007/s00259-002-0817-2. [DOI] [PubMed] [Google Scholar]
- 16.Piwnica-Worms D, Holman BL. Noncardiac applications of hexakis (alkyl isonitril) technetium-99m complexes. J Nucl Med. 1990;31:1166–1167. [PubMed] [Google Scholar]
- 17.Stefanescu C, Ionescu L, Dănilă R, Butcovan D, Tibu R, Bilha S, Timofte D, Vulpoi C. 99mTc MIBI Thymic scintigraphy in diagnosis and therapeutic decision making: what is behind the image ? Acta Endocrinol (Buchar). 2016;12(3):249–256. doi: 10.4183/aeb.2016.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Urkan M, Peker YS, Ozturk E. Minimally invasive parathyroidectomy for primary hyperparathyroidism. Acta Endocrinol (Buchar). 2019;15(2):182–186. doi: 10.4183/aeb.2019.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Somnay YR, Weinlander E, Alfhefdi A, Schneider D, Sippel RS, Chen H. Radioguided parathyroidectomy for tertiary hyperparathyroidism. J Surg Res. 2015;195(2):406–411. doi: 10.1016/j.jss.2015.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Assante R, Zampella E, Nicolai E, Acampa W, Vergara E, Nappi C, Gaudieri V, Fiumara G, Klain M, Petretta M, Cuocolo A. Incremental Value of Sestamibi SPECT/CT Over Dual-Phase Planar Scintigraphy in Patients With Primary Hyperparathyroidism and Inconclusive Ultrasound. Front Med (Lausanne). 2019;6:164. doi: 10.3389/fmed.2019.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho E, Chang JM, Yoon SY, Lee GT, Ku YH, Kim HI, Lee MC, Lee GH, Kim MJ. Preoperative localization and intraoperative parathyroid hormone assay in Korean patients with primary hyperparathyroidism. Endocrinol Metab. 2014;29(4):464–469. doi: 10.3803/EnM.2014.29.4.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chiriac IA, Goldstein AL. Actualities in Endocrinology-Parathyroid Imaging. Acta Endocrinol (Buchar). 2018;14(1):142–144. doi: 10.4183/aeb.2018.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vu TH, Schellingerhout D, Guha-Thakurta N, Sun J, Wei W, Kappadth SC, Perrier N, Kim EE, Rohren E, Chuang HH, Wong FC. Solitary Parathyroid Adenoma Localization in Technetium Tc99m Sestamibi SPECT and Multiphase Multidetector 4D CT. AJNR Am J Neuroradiol. 2019;40(1):142–149. doi: 10.3174/ajnr.A5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taywade SK, Damle NA, Behera A, Devasenathipathy K, Bal C, Tripathi M, Agarwal S, Tandon N, Chumber S, Seenu V. Comparison of 18F-Fluorocholine Positron Emission Tomography/Computed Tomography and Four-dimensional Computed Tomography in the Preoperative Localization of Parathyroid Adenomas-initial Results. Indian J Endocrinol Metab. 2017;21(3):399–403. doi: 10.4103/ijem.IJEM_536_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mehrabibahar M, Mousavi Z, Sadeghi R, Layegh P, Nouri M, Asadi M. Feasibility and safety of minimally invasive radioguided parathyroidectomy using very low intraoperative dose of Tc-99m MIBI. Int J Surg. 2017;39:229–233. doi: 10.1016/j.ijsu.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Fernandes JMP, Paiva C, Correia R, Polónia J, Moreira da Costa A. Parathyroid carcinoma: From a case report to a review of the literature. Int J Surg Case Rep. 2018;42:214–217. doi: 10.1016/j.ijscr.2017.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo R, Wang J, Zhang M, Zhang M, Meng H, Zhang Y, Li B. Value of 99mTc-MIBI SPECT/CT parathyroid imaging and ultrasonography for concomitant thyroid carcinoma. Nucl Med Commun. 2017;38(8):676–682. doi: 10.1097/MNM.0000000000000692. [DOI] [PubMed] [Google Scholar]