Abstract
The 15th European Bifurcation Club (EBC) meeting was held in Barcelona in October 2019. It facilitated a renewed consensus on coronary bifurcation lesions (CBL) and unprotected left main (LM) percutaneous interventions. Bifurcation stenting techniques continue to be refined, developed and tested. It remains evident that a provisional approach with optional side branch treatment utilising T, T and small protrusion (TAP) or culotte continues to provide flexible options for the majority of CBL patients. Debate persists regarding the optimal treatment of side branches, including assessment of clinical significance and thresholds for bail-out treatment. In more complex CBL, especially those involving the LM, adoption of dedicated two-stent techniques should be considered. Operators using such techniques have to be fully familiar with their procedural steps and should acknowledge associated limitations and challenges. When using two-stent techniques, failure to perform a final kissing inflation is regarded as a technical failure, since it may jeopardise clinical outcome. The development of novel technical tools and drug regimens deserves attention. In particular, intracoronary imaging, bifurcation simulation, drug-eluting balloon technology and tailored antiplatelet therapy have been identified as promising tools to enhance clinical outcomes. In conclusion, the evolution of a broad spectrum of bifurcation PCI components has resulted from studies extending from bench testing to randomised controlled trials. However, further advances are still needed to achieve the ambitious goal of optimising the clinical outcomes for every patient undergoing PCI on a CBL.
Introduction
Since 2004, the European Bifurcation Club (EBC) has continuously promoted the improvement and standardisation of percutaneous coronary intervention (PCI) for coronary bifurcation lesions (CBL) and left main (LM). The annual meeting constitutes a unique opportunity for a comprehensive overview of the available data and incorporates “pro et con” debates (that are followed by electronic voting sessions involving all attendees) to facilitate generation of consensus statements. The 15th EBC meeting was held in Barcelona on 18-19 October 2019 and all presentations are freely accessible on the EBC website (https://bifurc.eu/). The present document reports the updated EBC consensus. Table 1 summarises the recommendations (established and new as compared with the previous documents1,2,3).
Table 1. Overview on EBC recommendations.
| Topic | Previously established (and confirmed) recommendations | New recommendations |
| Bifurcation lesion definition | – A bifurcation lesion is ‘‘a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant SB’’ – A significant SB is a branch that the operator does not want to lose in the global context of a particular patient |
|
| Bifurcation anatomy description | – Coronary bifurcation anatomy should be regarded as a complex vessel/function structure composed of 3 different vessel segments (proximal MV, distal MV and SB) – Mathematical relationships regulate the size and flow at the level of three bifurcation segments – The flow-divider (also called bifurcation carina) is a very important anatomic-functional structure |
|
| In vivo, in vitro and computational simulations General issues. Details regarding biomechanical modelling and bench tests in bifurcations reported in specific consensus papers13,14. |
– Bench tests have pivotal importance in the understanding of device performance in bifurcated lesions – Due to improvement in computational modelling, biomechanical and fluid-dynamic studies have started providing novel insights |
– In vitro (bench testing), ex vivo (Visible Heart™ methodologies) and computational simulations have an increasingly recognised relevance to improve the knowledge in the field of bifurcation interventions and to facilitate education and training on bifurcation techniques. – Patient-specific stenting simulations have the potential to facilitate preprocedural planning, optimise stenting techniques, guide device refinement, and provide the foundation for virtual (in silico) clinical trials in bifurcations. |
| Defining complexity in bifurcation PCI | – The complexity of PCI on bifurcation lesion in clinical practice is a multifactorial phenomenon including clinical, angiographic and procedural aspects. | |
| General approach to bifurcation stenting | – PCI on bifurcation stenting should adhere to a KISS (keep it simple and safe) principle – Systematically wire both branches – Try to limit the number of stents – Aim for well apposed and well expanded stents with limited overlaps – Stenting technique reporting may be appropriately described and reported according to the updated MADS system21 |
|
| One-stent strategy General issues. Details regarding one-stent strategy reported in a specific techniques consensus paper21. |
– One-stent strategy is recommended for the vast majority of bifurcated lesions and is based on a “provisional SB stenting philosophy” (stent implantation in the MV eventually followed by SB intervention and stenting if needed) – MV predilation should be liberally performed – Stent implantation in the MV (selected 1:1 according to the distal MV size) followed by systematic POT (post-dilation of the stent at the level of proximal MV with a balloon diameter sized 1:1 according to the proximal MV) is the recommended way to perform one-stent strategy – When SB intervention is required, the following steps are advised: 1. pullback rewiring technique to aim at “distal re-wiring” 2. kissing balloon inflation using short balloons (and MV balloon sized 1:1 according to the distal MV diameter, consider non-compliant balloons). 3. final POT (also called repeat POT or re-POT). – When SB stenting is needed, T/TAP and culotte are valuable options – In selected anatomic conditions, the provisional 1-stent technique may be practised according to the “inverted provisional” approach (stent implanted in SB-proximal MV, across distal MV). |
– When treating complex bifurcations with tight SB ostial stenosis, SB dilation may be considered before MV stenting. – POT efficacy is dependent on correct balloon placement (best position: just proximal to the carina and reaching up to the proximal edge of the MV stent) – Kissing balloon effect is highly dependent on SB wire re-cross site and balloon selection (distal re-cross and short balloon overlaps are strongly recommended). – POT-side-POT may simplify the procedure (no need to advance 2 balloons together) but its efficacy is strongly dependent on optimal positioning of POT balloon during each step. – The definition of optimal SB result has yet to be established |
| Two-stent strategy General issues. Details regarding two-stent strategy reported in a specific techniques consensus paper21. |
– An intentional (up-front) two-stent approach represents optimal practice in selected patients with complex lesions involving large and diseased SB (especially in LM location) – Meticulous lesion preparation is recommended – When there is no concern about SB occlusion/re-access, techniques based on MV stenting first can be used (T, TAP and culotte stenting) – When there is major concern regarding SB occlusion/re-access, SB stenting first techniques have to be selected. Among these, best options are inverted T/TAP, inverted culotte or DK-crush. – Final kissing inflation (sequential high-pressure inflation followed by simultaneous inflation) is mandatory – Repeat POT recommended (being careful not to reach neocarina in the case of TAP) |
– The use of a 2-stent technique should be selected according to bifurcation anatomy and the operator’s experience. – Extensive understanding of the 2-stent technical steps is pivotal since adherence to best practice (sequences of ballooning, etc.) impacts on the efficacy of all 2-stent techniques. – The use of POT (one, two or even three times) is part of an optimal 2-stent technique. – In 2-stent techniques, final kissing might be regarded as a measure of procedural quality since failure in its performance continues to be strongly associated with adverse late clinical outcome. |
| Drug-eluting balloon | – Studies exploring DEB efficacy in de novo bifurcation lesions had major limitations and to date have provided no conclusive evidence. – DEB in bifurcation restenosis (especially after 2-stent techniques) is feasible and may minimise metal within the bifurcation. |
|
| Quantitative coronary analysis General issues. Details on QCA use in bifurcations reported in a specific consensus paper12. |
– QCA is an important standard analysis in scientific reporting and for regulatory assessment – Contemporary 3D QCA systems further provide the optimal projection angle in bifurcations and in some systems form the backbone for co-registration with OCT and IVUS |
|
| Intracoronary imaging General issues. Details regarding IVUS use and OCT use in bifurcations reported in specific consensus papers16,17. |
– Intracoronary imaging is a valuable tool in PCI on bifurcation lesion and LM since it facilitates technical planning and optimisation of the final result. – Selection of a preferred imaging modality should reflect operator experience and the primary objective of assessment – IVUS is gold standard for LM – OCT is feasible for distal LM lesions – OCT provides superior evaluation of stent and wire positions – Pullback in both MV & SB is recommended for 2-stent procedures |
– OCT combined with angio co-registration and sophisticated real-time analysis software provides real advantages for a stepwise bifurcation approach, especially 3D reconstruction to facilitate guidewire re-crossing towards the SB – Intracoronary imaging should be available in the cath lab and it is recommended that it is used when faced with procedural complications or unexpected technical challenges. |
| Fractional flow reserve | – FFR should be used in MV before treatment when ischaemia was not confirmed – SB FFR reflects proximal main vessel and SB disease/plaque burden – Pressure wires should not be routinely jailed in SB – After MV stenting, FFR in the SB is feasible (but some risk of SB dissection during wiring does exist) and more accurate than angiographic stenosis to establish SB ostial lesion severity |
|
| PCI for unprotected left main General issues. Details regarding the LM PCI consensus15. |
– Registries, trials and meta-analyses suggest that PCI (performed in experienced centres) represents a valuable option for myocardial revascularisation in selected patients with unprotected LM disease. – PCI results are influenced by LM disease pattern (bifurcation involvement) and overall coronary atherosclerotic burden (other diseased vessels, SYNTAX score) – Non-emergent PCI in patients with LM should be performed by an experienced and appropriately equipped PCI team. – DES should be selected and post-dilated (POT) in order to reach adequate matching with the individual patient’s anatomy. – Provisional strategy preferred for majority of patients – Intracoronary imaging and functional assessment may improve the decision-making process in the course of LM PCI – The use of intracoronary imaging during LM PCI is recommended whenever unexpected difficulties are encountered or the achievement of an optimal result is uncertain. |
– LM PCI efficacy and limitations have been highlighted in the recent extended follow-up of randomised trials. Thus, patient-tailored, collegial (Heart Team) decisions for revascularisation strategy (CABG or PCI) in stable or stabilised patients with LM disease are strongly advised. |
| Antiplatelet therapy General issues. Details regarding DAPT issues reported in a dedicated review paper42. |
– Contemporary studies highlight bifurcation lesions, especially when treated by 2-stent techniques, as risk factors for thrombotic events. – Trials on antiplatelet drug regimens focused on patients treated by PCI for bifurcation lesions are lacking. |
|
| DEB: drug-eluting balloon; FFR: fractional flow reserve; LM: unprotected left main; MV: main vessel (or main branch); POT: proximal optimisation technique; QCA: quantitative coronary analysis; SB: side branch | ||
IMAGING IN BIFURCATIONS: LATEST EFFORTS ARE GOING TO PROVIDE NOVEL INSIGHTS
Intracoronary imaging use represents an important and promising aspect of CBL PCI. The EBC recently released documents on the specific issues related to intravascular ultrasound (IVUS)4 and optical coherence tomography (OCT)5.
Selection of a preferred imaging modality should reflect operator experience and the primary objective of the assessment. It is acknowledged that many operators have greater IVUS experience, and IVUS is favoured for ostial LM and large-vessel evaluation. However, the superior resolution of OCT provides potential advantages for specific steps of bifurcation interventions, including visualisation of the site of guidewire crossing and stent optimisation tools. Finally, the recently released high-definition IVUS is an attractive evolution of IVUS technology that combines high-resolution imaging with image depth; its utility in bifurcation stenting has still to be established.
Calcium, a key determinant of stent optimisation, is easily recognised by IVUS and OCT. Novel OCT criteria predicting stent underexpansion have been recognised: circumferential calcium (>180°), longitudinal extension >5 mm and calcium thickness >0.5 mm6. Algorithms to guide the selection of calcium modification tools have started to be developed7 but deserve clinical validation. Of note, data regarding best management of calcification in the setting of CBL are lacking, so that calcium recognition and lesion preparation should not differ from non-CB and may include debulking techniques such as rotablation and balloon lithotripsy.
Advances in OCT imaging processing now facilitate real-time analysis of stent-vessel interactions and precise location of guidewire crossing through stent side cells into the side branch (SB). In particular, a recent study documented that the position of “link” struts across SB ostia, a phenomenon that cannot be controlled by the operator during stent implantation, is associated with incomplete stent apposition after kissing8. After stenting, the assessment of adequate stent expansion and “landing”, together with the recognition of edge dissections, may guide further PCI optimisation5.
Two independent trials are assessing the impact of OCT guidance in bifurcation PCI. The ongoing OCT optimised bifurcation event reduction (OCTOBER) study is a large randomised trial aimed at assessing clinical superiority (two-year major adverse cardiac events) of OCT-guided stent implantation compared to standard angiography-guided implantation in bifurcation lesions9. The online three-dimensional optical frequency domain imaging to optimise bifurcation stenting using Ultimaster stent (OPTIMUM) study is a proof-of-concept randomised trial (endpoint: malapposed struts) comparing online three-dimensional OCT-guided PCI to angiography-guided PCI in bifurcation lesions treated by provisional stenting with kissing inflation10.
IN VITRO, EX VIVO AND COMPUTATIONAL SIMULATIONS
The last EBC meeting placed special emphasis on bifurcation stenting simulations and the use of advanced technologies, including artificial intelligence, machine and deep learning, and extended reality (virtual, augmented and mixed), to facilitate precision and planning of bifurcation interventions11,12.
Three types of stent simulation were discussed - in vitro (bench), ex vivo (Visible Heart™ methodologies) and computational.
In vitro simulations represent bench testing of bifurcation stenting using patient-specific silicone-based bifurcation anatomies coupled with experimental flow dynamics and imaging (micro CT)13. There is potential to explore how flow changes in different coronary anatomies, and to explore how stent designs and deployment techniques may optimise flow.
Ex vivo simulations represent experimental stenting of porcine or cadaveric human donor hearts14 in a sophisticated perfusion circuit (Visible Heart™ methodologies; http://www.vhlab.umn.edu/) eventually combined with invasive (OCT) or non-invasive (micro CT) imaging.
Computational simulations involve computational (virtual) stenting using patient-specific bifurcation anatomies, and realistic plaque, stent and balloon geometries and material properties coupled with computational fluid dynamics and solid mechanics15 (Figure 1). Computational simulations run in computer clusters. They are feasible, widely applicable, accurate, time-effective, and potentially cost-effective. Accordingly, patient-specific stenting simulations are anticipated to shift the future evolution of coronary bifurcation interventions and to offer valuable tools for education and training.
Figure 1.
Example of in vitro and computational stenting simulations using a patient-specific coronary bifurcation anatomy. A) In vitro stenting of a patient-specific coronary artery bifurcation (TAP with a long neocarina denoted by the white arrow in panel C)). B) Computational simulation of the same stenting technique in the same bifurcation anatomy. C) Virtual fly-through view of the neocarina. D) Computational fluid dynamics of the stented bifurcation. E) Von-Mises stress distribution.
WHAT DEFINES A COMPLEX BIFURCATION LESION?
To date, no unique definition for a “complex” CBL exists within the literature. The historical “Medina” bifurcation classification, endorsed by the EBC, allows easy description of the angiographic plaque distribution and is known to influence the occurrence of procedural complications and adverse clinical events16. Medina 1,1,1 and Medina 0,1,1 have been regarded as complex CBL subsets in some studies. However, SB lesion length17, SB take-off angle and plaque composition (calcification, thrombus) are important modulators of CBL PCI complexity. In keeping with such a perspective, the definitions and impact of complex bifurcation lesions on clinical outcomes after PCI using drug-eluting stents (DEFINITION) registry18 generated a multi-parametric system where major criteria and minor criteria have been combined to categorise simple and complex CBL. This classification has recently been used for patient selection in the two-stent vs. provisional stenting techniques for patients with complex coronary bifurcation lesions (DEFINITION II) trial19.
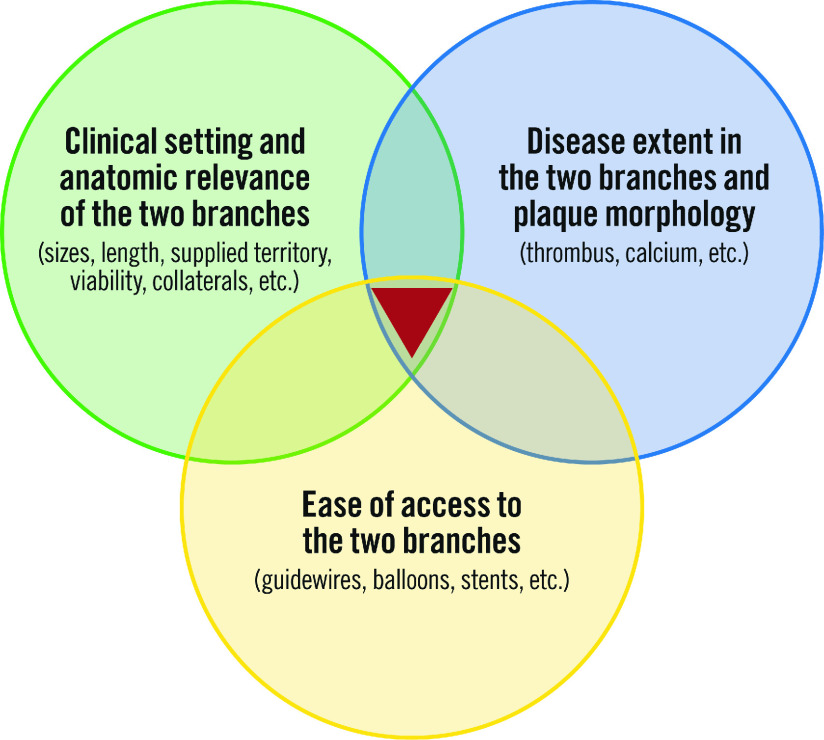
Overall, a series of clinical, anatomic and procedural factors might combine to determine the technical difficulties and complication risk in an individual patient (Figure 2).
Figure 2.
Main determinants of bifurcation PCI complexity.
MAJOR CONTROVERSIES REGARDING DECISION MAKING IN THE CONTEXT OF A ONE-STENT STRATEGY
Implantation of a main vessel (MV) stent (sized according to the distal MV diameter) across the SB ostium (“crossover” stenting) followed by the proximal optimisation technique (POT) is the minimal recommendation for a one-stent strategy in CBL. Of note, bench tests demonstrated that superior results from POT are obtained when the balloon is positioned immediately proximal to the carina20. Incorrect placement of the POT balloon too proximal or distal is associated with suboptimal results, as shown in Figure 3. Details regarding the technical aspects of the one-stent technique have been provided elsewhere21. During the last EBC meeting, the following key issues regarding a one-stent strategy were debated.
Figure 3.
Possible consequences of incorrect balloon position during POT.
WHAT ABOUT DISEASED SIDE BRANCH PREDILATION?
When applying a provisional approach to CBL with extensive atherosclerosis involving both the MV and SB take-off, the question of optimal lesion preparation represents a major issue since the SB may occlude after MV stenting. A prospective randomised study on “true” CBL by Pan et al documented that SB predilation results in improved flow after MB stenting and less need to treat the SB subsequently22.
The standard practice for CBL dilation in complex lesions is sequential dilation of the MV and SB. However, simultaneous dilation (“pre-kissing” technique) has the potential to avoid bifurcation carina displacement during predilation at the risk of proximal MV overstretch and dissection. The pre-kissing technique with undersized balloons (to limit dissections) was recently reported to be associated with a lower incidence of SB-associated complications in a small observational study23. However, these findings are regarded as inconclusive.
WHAT IS THE BEST TREATMENT OF OSTIAL LEFT ANTERIOR DESCENDING OR CIRCUMFLEX ARTERY LESIONS?
The optimal management of ostial left anterior descending (LAD) or ostial left circumflex artery (LCX) lesions (also called Medina 0,1,0 and 0,0,1 LM bifurcations) is an unresolved issue. Of note, angiography is known to underestimate LM bifurcation atherosclerosis extension4,5, so that IVUS or OCT confirmation of isolated LAD/LCX stenosis is advisable before ostial stenting is considered.
A recent study compared treatment with one stent positioned precisely at the LAD ostium with crossover stenting, showing the feasibility of ostial stenting24. However, higher restenosis as compared with crossover stenting24 was documented. Thus, ostial stenting might be considered in order to avoid LM stenting when the anatomy is particularly favourable (rectangular angle between LAD-LCX, perfect visualisation of SB take-off, non-diseased LM). In all other situations, crossover stenting (covering the involved ostial LAD or ostial LCX and the diseased segment of LM) followed by POT and eventual kissing (according to either provisional or “inverted” provisional21) represents a preferable option.
WHEN TO PERFORM SIDE BRANCH DILATION DURING ONE-STENT STRATEGY FOR DISTAL LEFT MAIN?
Whether to perform SB dilation after crossover stenting in an unprotected LM is a challenge in daily practice. According to the “provisional” strategy, SB intervention is recommended whenever the result in the SB is considered suboptimal. However, defining a “suboptimal” result for the LCX ostium is difficult and not standardised (Supplementary Table 1 for overview of suboptimal SB result criteria adopted in recent studies).
Even in the absence of a suboptimal SB result, the need to clear stent struts from the SB ostium, facilitating access to the LCX, continues to be debated. Indeed, “floating” struts across the ostium may support the development of an LCX ostial “fenestrated” restenosis (Figure 4). Contrary to this concern, a large registry of patients treated with crossover stenting from the left main coronary artery (LMCA) to the LAD has demonstrated that the cumulative five-year incidence of target lesion revascularisation was not significantly different between the kissing and non-kissing balloon groups25.
Figure 4.
“Fenestrated” restenosis after crossover stenting. A) Pre-PCI angiography. B) Result after stent implantation into the LM-LAD followed by POT. C) 36-month follow-up with short restenosis at LCX ostium. D) Three-dimensional OCT assessment showing neointima growth over the stent struts splitting the LCX ostium in three different, small orifices. E) Fractional flow reserve assessment documenting the haemodynamic significance of the multi-hole restenosis. (Case presented at EBC 2019 by Dr Rony Mathew Kadavil).
HOW AND WHY TO PERFORM KISSING
Over the years, it has clearly emerged that the efficacy of strut clearance from the SB by kissing balloon inflation is dependent on the location of the wire re-cross and that kissing balloon inflation may induce a major oval distortion in the proximal MV. Thus, POT, distal SB rewiring followed by kissing balloon inflation (eventually conducted with short non-compliant balloons) and repeat POT are recommended21 in order to minimise proximal MV distortion and to restore an ideal bifurcation anatomy (Figure 5). To date, clinical data do not support the use of routine kissing balloon inflation26. However, the results of a recent multicentre registry on CBL, treated by ultra-thin stents, suggested that kissing inflation performed with short balloon overlap may reduce target lesion revascularisations27.
Figure 5.
Efficacy of provisional technique in modifying the stent platform allowing the achievement of a good result in a patient with a complex bifurcation lesion. A) Pre-PCI angiography. B) Result after LAD stent implantation followed by POT, distal rewiring, kissing balloon inflation with short balloon overlap and re-POT. C) & D) Three-dimensional OCT reconstructions of the final result achieved.
WHAT ABOUT THE POT-SIDE-POT STRATEGY?
The sequential application of single balloon dilation in the proximal MV, SB and proximal MV (POT-side-POT) is appealing due to its simplicity and efficacy in bench tests. Of note, recent data documented that this technique is probably less simple than theorised. In particular, SB ballooning induces a distortion in the MV stent deserving appropriate correction and it is able to clear SB stent struts only when performed after distal rewiring (similar to kissing). Furthermore, the position of the final (re-)POT balloon (a factor that can be challenging to control in clinical practice) impacts significantly on final SB obstruction28.
NOVELTIES IN AN ELECTIVE TWO-STENT STRATEGY
CBL with extensive atherosclerosis involving a large and significantly diseased SB may benefit from an elective two-stent bifurcation technique. Different technical options are available and should be selected according to the specific lesion anatomy and the operator’s experience. T, T and small protrusion (TAP), culotte and double-kissing (DK) crush represent the most popular two-stent techniques. Their recommended steps have been summarised previously21. In all two-stent techniques, repeated POT manoeuvres21 before any branch rewiring are pivotal since malapposed stent struts in the proximal MV or around the carina may easily be displaced during device (balloon/stent) advancement, causing metallic strut accumulation. Observational data on patients treated by two-stent techniques are continuing to report better clinical outcomes with final kissing balloon inflation27, so that its performance can be regarded as a measure of procedural success.
The culotte technique represents a very “flexible” technique, offering the opportunity for liberal selection of the first treated branch between the distal MV and SB. Among possible technical improvements, the minimisation of stent overlap in the MV and the addition of a further kissing balloon inflation after first stent implantation are notable. These modifications add technical complexity during the practice, but the resulting “DK-mini-culotte” has the potential for outstanding stent configuration29.
Regarding the DK-crush technique, a further increase in its popularity is expected after the outstanding results recently reported in the DK-CRUSH V trial30 and the DEFINITION II trial18. However, the complexity of the technique continues to pose specific challenges, and high-volume DK-crush operators continue to develop technical refinements with the potential addition of further steps. Among these, the immediate high-pressure post-dilation of the SB stent (“proximal SB optimisation”) proposed by Lavarra31 has been recognised by the EBC as useful21. Other operators are suggesting that the selection of ultra-thin strut biodegradable polymer-coated stents may minimise stent overlap thickness and enhance healing after stent crushing32.
DRUG-ELUTING BALLOON FOR BIFURCATION: WHERE ARE WE?
Drug-eluting balloon (DEB) technology incorporates devices with known heterogeneity (no class effect) and potential interest in the setting of bifurcation PCI.
In de novo CBL, DEB use in the SB is an attractive approach. The PEPCAD BIF trial showed that SB lesions without both major dissections and significant early vessel recoil have a very acceptable late lumen loss33. A meta-analysis including 349 patients compared the SB result using standard balloon versus DEB angioplasty34. At nine months, DEB use was associated with lower SB late lumen loss compared with balloon angioplasty; however, SB binary restenosis was not reduced significantly. Overall, the data are inconclusive, with many unanswered questions including the appropriate SB selection, technique (DEB with or without final kissing ballooning or repeat POT) and actual impact on meaningful clinical endpoints.
DEB usage in restenosis has been more extensively tested and clearly provides an advantage of minimising multiple stent layers in patients presenting with CBL restenosis, especially where the index PCI involved two-stent techniques35.
CERTAINTIES AND EMERGING DOUBTS ON UNPROTECTED LM PCI EFFICACY
Within the last year, long-term clinical follow-up results have been published from important landmark studies comparing PCI and coronary artery bypass grafting (CABG) for patients with unprotected LM disease.
In the extended 10-year follow-up of mortality within the SYNTAX trial36, all-cause death was not significantly different between PCI and CABG. Of note, CABG provided a significant survival benefit in patients with three-vessel disease, but not in those with LM disease.
The recently published five-year results from the EXCEL and NOBLE trials37,38 have generated vigorous debate regarding contemporary PCI versus CABG in the treatment of LM disease. Repeat revascularisation was higher in the PCI arm in both trials. Total mortality differed significantly in EXCEL but not in the NOBLE trial.
A very recent meta-analysis39 of five randomised trials (including NOBLE and EXCEL) on a total of 4,612 unprotected LM patients with a weighted mean follow-up duration of 67 months allowed derivation of the data summarised in Supplementary Table 2.
These novel data reinforce the need for tailored patient selection and PCI improvements. The role of a multidisciplinary Heart Team in the treatment decision for stable or stabilised patients with unprotected LM disease is emphasised. The key issues (anatomical assessment, team organisation) that might be critical for successful LM PCI programmes were extensively reviewed in the previous EBC consensus documents2,3.
DUAL ANTIPLATELET THERAPY IN BIFURCATION LESION PCI PATIENTS
The ESC guidelines highlight coronary bifurcation as a risk factor for coronary ischaemic events, suggesting that a longer duration (≥12 months) of dual antiplatelet therapy (DAPT) may be considered40. This recommendation is based mainly on a meta-analysis41 comprising 9,577 patients, showing that two-stent bifurcation stenting was the strongest risk factor for adverse events.
In the recent EBC registry41 including 5,036 patients undergoing bifurcation PCI, the risk of adverse events was significantly increased among patients who discontinued DAPT prematurely (<6 months in stable CAD, <12 months in ACS). Also, as compared with one-stent techniques, two-stent techniques were associated with significantly increased major adverse events.
Given the trade-off between ischaemic and bleeding risks for any DAPT duration, a careful patient risk stratification seems of utmost relevance. An EBC-promoted study group has recently revised available DAPT selection options42.
Conclusions
Devices, techniques and imaging modalities are evolving at an incredible pace and their use in bifurcated lesions and unprotected left main needs to be updated. Bifurcation stenting techniques, intracoronary imaging, bifurcation simulation, drug-eluting balloon technology and tailored antiplatelet therapy are identified as pivotal to enhance clinical outcomes.
Supplementary data
Definitions of suboptimal side branch result during provisional stenting approach in recent study protocols.
Adverse events comparison at the longest available follow-up in trials comparing PCI and CABG in patients with unprotected left main disease.
Visual summary.
15th consensus document from the European Bifurcation Club.
Acknowledgments
Conflict of interest statement
F. Burzotta has received speaker fees from Medtronic, Abiomed, and Abbott. J.F. Lassen has received speaker fees from Medtronic, Boston Scientific, Biotronik, Abbott and Biosensors. A.P. Banning has received institutional funding of a fellowship from Boston Scientific and speaker fees from Boston, Abbott, Medtronic, Philips/Volcano and Miracor. T.W. Johnson has received speaker fees from Abbott, Boston Scientific, Medtronic, and Terumo, and institutional funding for fellowships from Boston Scientific and Terumo. D. Hildick-Smith has received advisory board/consultancy/research funding from Terumo, Medtronic, Abbott, and Boston Scientific. R. Albiero has received speaker fees from Medtronic and Abbott. M. Pan has received speaker fees from Abbott, Terumo and Volcano. A. Chieffo has received speaker fees from Abiomed and GADA. O. Darremont has received speaker fees from Edwards. Y.S. Chatzizisis has received speaker fees, consultation fees and research grant from Boston Scientific, and research support from Medtronic. T. Lefèvre has received speaker fees from Abbott, Medtronic and Terumo. The other authors have no conflicts of interest to declare.
Abbreviations
- CABG
coronary artery bypass graft
- CBL
coronary bifurcation lesion(s)
- DAPT
dual antiplatelet therapy
- DEB
drug-eluting balloon
- DK-crush
double-kissing crush
- EBC
European Bifurcation Club
- IVUS
intravascular ultrasound
- LAD
left anterior descending artery
- LCX
left circumflex artery
- LM
left main
- MV
main vessel
- OCT
optical coherence tomography
- PCI
percutaneous coronary intervention
- POT
proximal optimisation technique
- SB
side branch
- TAP
T and small protrusion
Contributor Information
Francesco Burzotta, Insitute of Cardiology, Fondazione Policlinico Universitario A. Gemelli IRCCS, Università Cattolica del Sacro Cuore, Rome, Italy.
Jens Lassen, Department of Cardiology B, Odense Universitets hospital & University of Southern Denmark, Odense C, Denmark.
Thierry Lefèvre, Ramsay Générale de Santé - Institut cardiovasculaire Paris Sud, Hopital Privé Jacques Cartier, Massy, France.
Adrian P. Banning, Cardiovascular Medicine Division, Radcliffe Department of Medicine, John Radcliffe Hospital, Oxford, United Kingdom.
Yiannis Chatzizisis, Cardiovascular Division, University of Nebraska Medical Center, Omaha, NE, USA.
Thomas W. Johnson, Department of Cardiology, Bristol Heart Institute, University Hospitals Bristol NHSFT & University of Bristol, Bristol, United Kingdom.
Miroslaw Ferenc, Division of Cardiology and Angiology II, University Heart Center Freiburg-Bad Krozingen, Bad Krozingen, Germany.
Sudhir Rathore, Frimley Health NHS Foundation Trust, Camberley, Surrey, United Kingdom.
Remo Albiero, Interventional Cardiology Unit, Ospedale Civile, Sondrio, Italy.
Manuel Pan, Department of Cardiology, Reina Sofía Hospital, University of Córdoba (IMIBIC), Córdoba, Spain.
Olivier Darremont, Clinique St Augustin, Bordeaux, France.
David Hildick-Smith, Sussex Cardiac Centre, Brighton and Sussex University Hospitals, Brighton, United Kingdom.
Alaide Chieffo, Interventional Cardiology Unit, San Raffaele Scientific Institute, Milan, Italy.
Marco Zimarino, Cath Lab SS. Annunziata Hospital and Institute of Cardiology, University of Chieti, Chieti, Italy.
Yves Louvard, Ramsay Générale de Santé - Institut cardiovasculaire Paris Sud, Hopital Privé Jacques Cartier, Massy, France.
Goran Stankovic, Department of Cardiology, Clinical Center of Serbia, and Medical faculty, University of Belgrade, Belgrade, Serbia.
References
- Lassen JF, Burzotta F, Banning AP, Lefevre T, Darremont O, Hildick-Smith D, Chieffo A, Pan M, Holm NR, Louvard Y, Stankovic G. Percutaneous coronary intervention for the left main stem and other bifurcation lesions:12th consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:1540–53. doi: 10.4244/EIJ-D-17-00622. [DOI] [PubMed] [Google Scholar]
- Banning AP, Lassen JF, Burzotta F, Lefevre T, Darremont O, Hildick-Smith D, Louvard Y, Stankovic G. Percutaneous coronary intervention for obstructive bifurcation lesions: the 14th consensus document from the European Bifurcation Club. EuroIntervention. 2019;15:90–8. doi: 10.4244/EIJ-D-19-00144. [DOI] [PubMed] [Google Scholar]
- Burzotta F, Lassen JF, Banning AP, Lefevre T, Hildick-Smith D, Chieffo A, Darremont O, Pan M, Chatzizisis YS, Albiero R, Louvard Y, Stankovic G. Percutaneous coronary intervention in left main coronary artery disease: the 13th consensus document from the European Bifurcation Club. EuroIntervention. 2018;14:112–20. doi: 10.4244/EIJ-D-18-00357. [DOI] [PubMed] [Google Scholar]
- Mintz GS, Lefevre T, Lassen JF, Testa L, Pan M, Singh J, Stankovic G, Banning AP. Intravascular ultrasound in the evaluation and treatment of left main coronary artery disease: a consensus statement from the European Bifurcation Club. EuroIntervention. 2018;14:e467–74. doi: 10.4244/EIJ-D-18-00194. [DOI] [PubMed] [Google Scholar]
- Onuma Y, Katagiri Y, Burzotta F, Ramsing Holm N, Amabile N, Okamura T, Mintz GS, Darremont O, Lassen JF, Lefevre T, Louvard Y, Stankovic G, Serruys PW. Joint consensus on the use of OCT in coronary bifurcation lesions by the European and Japanese bifurcation clubs. EuroIntervention. 2019;14:1568–77. doi: 10.4244/EIJ-D-18-00391. [DOI] [PubMed] [Google Scholar]
- Fujino A, Mintz GS, Matsumura M, Lee T, Kim SY, Hoshino M, Usui E, Yonetsu T, Haag E, Shlofmitz RA, Kakuta T, Maehara A. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018;13:e2182–9. doi: 10.4244/EIJ-D-17-00962. [DOI] [PubMed] [Google Scholar]
- Perfetti M, Fulgenzi F, Radico F, Toro A, Procopio A, Maddestra N, Zimarino M. Calcific lesion preparation for coronary bifurcation stenting. Cardiol J. 2019;26:429–37. doi: 10.5603/CJ.a2019.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murasato Y, Mori T, Okamura T, Nagoshi R, Fujimura T, Yamawaki M, Ono S, Serikawa T, Nakao F, Shite J 3D-OCT Bifurcation Registry Investigators. Efficacy of the proximal optimization technique on crossover stenting in coronary bifurcation lesions in the 3D-OCT bifurcation registry. Int J Cardiovasc Imaging. 2019;35:981–90. doi: 10.1007/s10554-019-01581-1. [DOI] [PubMed] [Google Scholar]
- Holm NR, Andreasen LN, Walsh S, Kajander OA, Witt N, Eek C, Knaapen P, Koltowski L, Gutiérrez-Chico JL, Burzotta F, Kockman J, Ormiston J, Santos-Pardo I, Laanmets P, Mylotte D, Madsen M, Hjort J, Kumsars I, Råmunddal T, Christiansen EH. Rational and design of the European randomized Optical Coherence Tomography Optimized Bifurcation Event Reduction Trial (OCTOBER). Am Heart J. 2018;205:97–109. doi: 10.1016/j.ahj.2018.08.003. [DOI] [PubMed] [Google Scholar]
- Miyazaki Y, Muramatsu T, Asano T, Katagiri Y, Sotomi Y, Nakatani S, Takahashi K, Kogame N, Higuchi Y, Ishikawa M, Kyono H, Yano M, Ozaki Y, Serruys PW, Okamura T, Onuma Y. Online three-dimensional OFDI guided PCI vs. angiography guided in bifurcation lesions: design and rationale of the randomized OPTIMUM trial. EuroIntervention. 2021;16:1333–41. doi: 10.4244/EIJ-D-18-00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzizisis YS. Complex cardiovascular interventions: visualization, planning, outcomes. JACC Case Reports. 2019;1:124–6. doi: 10.1016/j.jaccas.2019.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoniadis AP, Mortier P, Kassab G, Dubini G, Foin N, Murasato Y, Giannopoulos AA, Tu S, Iwasaki K, Hikichi Y, Migliavacca F, Chiastra C, Wentzel JJ, Gijsen F, Reiber JH, Barlis P, Serruys PW, Bhatt DL, Stankovic G, Edelman ER, Giannoglou GD, Louvard Y, Chatzizisis YS. Biomechanical Modeling to Improve Coronary Artery Bifurcation Stenting: Expert Review Document on Techniques and Clinical Implementation. JACC Cardiovasc Interv. 2015;8:1281–96. doi: 10.1016/j.jcin.2015.06.015. [DOI] [PubMed] [Google Scholar]
- Ormiston JA, Kassab G, Finet G, Chatzizisis YS, Foin N, Mickley TJ, Chiastra C, Murasato Y, Hikichi Y, Wentzel JJ, Darremont O, Iwasaki K, Lefevre T, Louvard Y, Beier S, Hojeibane H, Netravali A, Wooton J, Cowan B, Webster MW, Medrano-Gracia P, Stankovic G. Bench testing and coronary artery bifurcations: a consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:e1794–803. doi: 10.4244/EIJ-D-17-00270. [DOI] [PubMed] [Google Scholar]
- Iles TL, Burzotta F, Lassen JF, Iaizzo PA. Stepwise visualisation of a provisional bifurcation stenting procedure - multimodal visualisation within a reanimated human heart utilising Visible Heart methodologies. EuroIntervention. 2020;16:e734–7. doi: 10.4244/EIJ-D-19-00606. [DOI] [PubMed] [Google Scholar]
- Genuardi L, Chatzizisis YS, Chiastra C, Sgueglia G, Samady H, Kassab G, Migliavacca F, Trani C, Burzotta F. Local fluid dynamics in patients with bifurcated coronary lesions undergoing percutaneous coronary interventions. Cardiol J. 2020 Feb 13; doi: 10.5603/CJ.a2020.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park TK, Park YH, Song YB, Oh JH, Chun WJ, Kang GH, Jang WJ, Hahn JY, Yang JH, Choi SH, Choi JH, Lee SH, Jeong MH, Kim HS, Lee JH, Yu CW, Rha SW, Jang Y, Yoon JH, Tahk SJ, Seung KB, Park JS, Gwon HC. Long-Term Clinical Outcomes of True and Non-True Bifurcation Lesions According to Medina Classification- Results From the COBIS (COronary BIfurcation Stent) II Registry. Circ J. 2015;79:1954–62. doi: 10.1253/circj.CJ-15-0264. [DOI] [PubMed] [Google Scholar]
- Zimarino M, Barbato E, Nakamura S, Radico F, Di Nicola M, Briguori C, Gil RJ, Kanic V, Perfetti M, Pellicano M, Mairic K, Stankovic G European Bifurcation Club. The impact of the extent of side branch disease on outcomes following bifurcation stenting. Catheter Cardiovasc Interv. 2020;96:E84–95. doi: 10.1002/ccd.28842. [DOI] [PubMed] [Google Scholar]
- Chen SL, Sheiban I, Xu B, Jepson N, Paiboon C, Zhang JJ, Ye F, Sansoto T, Kwan TW, Lee M, Han YL, Lv SZ, Wen SY, Zhang Q, Wang HC, Jiang TM, Wang Y, Chen LL, Tian NL, Cao F, Qiu CG, Zhang YJ, Leon MB. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and impact of complEx biFurcation lesIons on clinical outcomes after percutaNeous coronary IntervenTIOn using drug-eluting steNts). JACC Cardiovasc Interv. 2014;7:1266–76. doi: 10.1016/j.jcin.2014.04.026. [DOI] [PubMed] [Google Scholar]
- Zhang JJ, Ye F, Xu K, Kan J, Tao L, Santoso T, Munawar M, Tresukosol D, Li L, Sheiban I, Li F, Tian NL, Rodríguez AE, Paiboon C, Lavarra F, Lu S, Vichairuangthum K, Zeng H, Chen L, Zhang R, Ding S, Gao F, Jin Z, Hong L, Ma L, Wen S, Wu X, Yang S, Yin WH, Zhang J, Wang Y, Zheng Y, Zhou L, Zhou L, Zhu Y, Xu T, Wang X, Qu H, Tian Y, Lin S, Liu L, Lu Q, Li Q, Li B, Jiang Q, Han L, Gan G, Yu M, Pan D, Shang Z, Zhao Y, Liu Z, Yuan Y, Chen C, Stone GW, Han Y, Chen SL. Multicentre, randomized comparison of two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: the DEFINITION II trial. Eur Heart J. 2020;41:2523–36. doi: 10.1093/eurheartj/ehaa543. [DOI] [PubMed] [Google Scholar]
- Derimay F, Rioufol G, Nishi T, Kobayashi Y, Fearon WF, Veziers J, Guerin P, Finet G. Optimal balloon positioning for the proximal optimization technique? An experimental bench study. Int J Cardiol. 2019;292:95–7. doi: 10.1016/j.ijcard.2019.05.041. [DOI] [PubMed] [Google Scholar]
- Burzotta F, Lassen JF, Louvard Y, Lefevre T, Banning AP, Daremont O, Pan M, Hildick-Smith D, Chieffo A, Chatzizisis YS, Džavík V, Gwon HC, Hikichi Y, Murasato Y, Koo BK, Chen SL, Serruys P, Stankovic G. European Bifurcation Club white paper on stenting techniques for patients with bifurcated coronary artery lesions. Catheter Cardiovasc Interv. 2020;96:1067–79. doi: 10.1002/ccd.29071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan M, Medina A, Romero M, Ojeda S, Martín P, Suarez de Lezo J, Segura J, Mazuelos F, Novoa J, Suarez de Lezo J. Assessment of side branch predilation before a provisional T-stent strategy for bifurcation lesions. A randomized trial. Am Heart J. 2014;168:374–80. doi: 10.1016/j.ahj.2014.05.014. [DOI] [PubMed] [Google Scholar]
- Burzotta F, Shoeib O, Aurigemma C, Porto I, Leone AM, Niccoli G, Genuardi L, Trani C, Crea F. Procedural Impact of a Kissing-Balloon Predilation (Pre-Kissing) Technique in Patients With Complex Bifurcations Undergoing Drug-Eluting Stenting. J Invasive Cardiol. 2019;31:80–8. doi: 10.25270/jic/18.00298. [DOI] [PubMed] [Google Scholar]
- Rigatelli G, Zuin M, Baracca E, Galasso P, Carraro M, Mazza A, Lanza D, Roncon L, Daggubati R. Long-Term Clinical Outcomes of Isolated Ostial Left Anterior Descending Disease Treatment: Ostial Stenting Versus Left Main Cross-Over Stenting. Cardiovasc Revasc Med. 2019;20:1058–62. doi: 10.1016/j.carrev.2019.01.030. [DOI] [PubMed] [Google Scholar]
- Nishida K, Toyofuku M, Morimoto T, Ohya M, Fuku Y, Higami H, Yamaji K, Muranishi H, Yamaji Y, Furukawa D, Tada T, Ko E, Kadota K, Ando K, Sakamoto H, Tamura T, Kawai K, Kimura T AOI LMCA Stenting Registry Investigators. Prognostic impact of final kissing balloon technique after crossover stenting for the left main coronary artery: from the AOI-LMCA registry. Cardiovasc Interv Ther. 2019;34:197–206. doi: 10.1007/s12928-018-0522-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong M, Tang B, Zhao Q, Cheng J, Jin Q, Fu S. Should kissing balloon inflation after main vessel stenting be routine in the one-stent approach? A systematic review and meta-analysis of randomized trials. PLoS One. 2018;13:e0197580. doi: 10.1371/journal.pone.0197580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaido L, D’Ascenzo F, Imori Y, Wojakowski W, Saglietto A, Figini F, Mattesini A, Trabattoni D, Rognoni A, Tomassini F, Bernardi A, Ryan N, Muscoli S, Helft G, De Filippo O, Parma R, De Luca L, Ugo F, Cerrato E, Montefusco A, Pennacchi M, Wanha W, Smolka G, de Lio G, Bruno F, Huczek Z, Boccuzzi G, Cortese B, Capodanno D, Omede P, Mancone M, Nunez-Gil I, Romeo F, Varbella F, Rinaldi M, Escaned J, Conrotto F, Burzotta F, Chieffo A, Perl L, D’Amico M, Di Mario C, Sheiban I, Gagnor A, Giammaria M, De Ferrari GM. Impact of Kissing Balloon in Patients Treated With Ultrathin Stents for Left Main Lesions and Bifurcations: An Analysis From the RAIN-CARDIOGROUP VII Study. Circ Cardiovasc Interv. 2020;13:e008325. doi: 10.1161/CIRCINTERVENTIONS.119.008325. [DOI] [PubMed] [Google Scholar]
- Andreasen LN, Holm NR, Webber B, Ormiston JA. Critical aspects of balloon position during final proximal optimization technique (POT) in coronary bifurcation stenting. Catheter Cardiovasc Interv. 2020;96:31–9. doi: 10.1002/ccd.28801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth GG, Sasi V, Franco D, Prassl AJ, Di Serafino L, Ng JC, Szanto G, Schneller L, Ang HY, Plank G, Wijns W, Barbato E. Double-kissing culotte technique for coronary bifurcation stenting. EuroIntervention. 2020;16:e724–33. doi: 10.4244/EIJ-D-20-00130. [DOI] [PubMed] [Google Scholar]
- Chen X, Li X, Zhang JJ, Han Y, Kan J, Chen L, Qiu C, Santoso T, Paiboon C, Kwan TW, Sheiban I, Leon MB, Stone GW, Chen SL DKCRUSH-V Investigators. 3-Year Outcomes of the DKCRUSH-V Trial Comparing DK Crush With Provisional Stenting for Left Main Bifurcation Lesions. JACC Cardiovasc Interv. 2019;12:1927–37. doi: 10.1016/j.jcin.2019.04.056. [DOI] [PubMed] [Google Scholar]
- Lavarra F. Proximal side optimization: a modification of the double kissing crush technique. US Cardiology Review. 2020;14:e02. doi: 10.15420/usc.2020.07. [DOI] [Google Scholar]
- Rigatelli G, Zuin M, Dell’avvocata F, Vassilev D, Daggubati R, Nguyen T, Nguyễn MTN, Foin N. Complex coronary bifurcation treatment by a novel stenting technique: Bench test, fluid dynamic study and clinical outcomes. Catheter Cardiovasc Interv. 2018;92:907–14. doi: 10.1002/ccd.27494. [DOI] [PubMed] [Google Scholar]
- Kleber FX, Rittger H, Ludwig J, Schulz A, Mathey DG, Boxberger M, Degenhardt R, Scheller B, Strasser RH. Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016;105:613–21. doi: 10.1007/s00392-015-0957-6. [DOI] [PubMed] [Google Scholar]
- Megaly M, Rofael M, Saad M, Shishehbor M, Brilakis ES. Outcomes With Drug-Coated Balloons for Treating the Side Branch of Coronary Bifurcation Lesions. J Invasive Cardiol. 2018;30:393–9. [PubMed] [Google Scholar]
- Harada Y, Colleran R, Pinieck S, Giacoppo D, Michel J, Kufner S, Cassese S, Joner M, Ibrahim T, Laugwitz KL, Kastrati A, Byrne RA. Angiographic and clinical outcomes of patients treated with drug-coated balloon angioplasty for in-stent restenosis after coronary bifurcation stenting with a two-stent technique. EuroIntervention. 2017;12:2132–9. doi: 10.4244/EIJ-D-16-00226. [DOI] [PubMed] [Google Scholar]
- Thuijs DJFM, Kappetein AP, Serruys PW, Mohr FW, Morice MC, Mack MJ, Holmes DR, Jr, Curzen N, Davierwala P, Noack T, Milojevic M, Dawkins KD, da Costa BR, Jüni P, Head SJ SYNTAX Extended Survival Investigators. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394:1325–34. doi: 10.1016/S0140-6736(19)31997-X. [DOI] [PubMed] [Google Scholar]
- Stone GW, Kappetein AP, Sabik JF, Pocock SJ, Morice MC, Puskas J, Kandzari DE, Karmpaliotis D, Brown WM, 3rd, Lembo NJ, Banning A, Merkely B, Horkay F, Boonstra PW, van Boven AJ, Ungi I, Bogáts G, Mansour S, Noiseux N, Sabate M, Pomar J, Hickey M, Gershlick A, Buszman PE, Bochenek A, Schampaert E, Pagé P, Modolo R, Gregson J, Simonton CA, Mehran R, Kosmidou I, Généreux P, Crowley A, Dressler O, Serruys PW EXCEL Trial Investigators. Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N Engl J Med. 2019;381:1820–30. doi: 10.1056/NEJMoa1909406. [DOI] [PubMed] [Google Scholar]
- Holm NR, Mäkikallio T, Lindsay MM, Spence MS, Erglis A, Menown IBA, Trovik T, Kellerth T, Kalinauskas G, Mogensen LJH, Nielsen PH, Niemelä M, Lassen JF, Oldroyd K, Berg G, Stradins P, Walsh SJ, Graham ANJ, Endresen PC, Fröbert O, Trivedi U, Anttila V, Hildick-Smith D, Thuesen L, Christiansen EH NOBLE investigators. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: updated 5-year outcomes from the randomised, non-inferiority NOBLE trial. Lancet. 2020;395:191–9. doi: 10.1016/S0140-6736(19)32972-1. [DOI] [PubMed] [Google Scholar]
- Ahmad Y, Howard JP, Arnold AD, Cook CM, Prasad M, Ali ZA, Parikh MA, Kosmidou I, Francis DP, Moses JW, Leon MB, Kirtane AJ, Stone GW, Karmpaliotis D. Mortality after drug-eluting stents vs. coronary artery bypass grafting for left main coronary artery disease: a meta-analysis of randomized controlled trials. Eur Heart J. 2020;41:3228–35. doi: 10.1093/eurheartj/ehaa135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, Jüni P, Kastrati A, Kolh P, Mauri L, Montalescot G, Neumann FJ, Petricevic M, Roffi M, Steg PG, Windecker S, Zamorano JL, Levine GN ESC Scientific Document Group; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39:213–60. doi: 10.1093/eurheartj/ehx419. [DOI] [PubMed] [Google Scholar]
- Zimarino M, Briguori C, Amat-Santos IJ, Radico F, Barbato E, Chieffo A, Cirillo P, Costa RA, Erglis A, Gamra H, Gil RJ, Kanic V, Kedev SA, Maddestra N, Nakamura S, Pellicano M, Petrov I, Strozzi M, Tesorio T, Vukcevic V, De Caterina R, Stankovic G EuroBifurcation Club. Mid-term outcomes after percutaneous interventions in coronary bifurcations. Int J Cardiol. 2019;283:78–83. doi: 10.1016/j.ijcard.2018.11.139. [DOI] [PubMed] [Google Scholar]
- Zimarino M, Angiolillo DJ, Dangas G, Capodanno D, Barbato E, Hahn JY, Giustino G, Watanabe H, Costa F, Cuisset T, Rossini R, Sibbing D, Burzotta F, Louvard Y, Shehab A, Renda G, Kimura T, Gwon HC, Chen SL, Costa R, Koo BK, Storey RF, Valgimigli M, Mehran R, Stankovic G. Antithrombotic Therapy after Percutaneous Coronary Intervention of Bifurcation Lesions. EuroIntervention. 2020 Sep 15; doi: 10.4244/EIJ-D-20-00885. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Definitions of suboptimal side branch result during provisional stenting approach in recent study protocols.
Adverse events comparison at the longest available follow-up in trials comparing PCI and CABG in patients with unprotected left main disease.