Abstract
Background:
With rising unemployment rates brought on by coronavirus disease 2019 pandemic, the rates of underinsured and uninsured consumers are likely to rise. Health information intermediaries play a critical role in assisting consumers with navigating the complexities of the United States health care system and the ever-changing health care policy landscape. Not much is known about the health insurance literacy (HIL) levels of information intermediaries and their ability to assist consumers with making informed decisions about their health insurance.
Objective:
This study aimed to examine the association between information intermediary levels of HIL, sociodemographic factors, and confidence and behaviors in assisting consumers with health insurance needs.
Methods:
We surveyed 118 information intermediaries from various roles to assess objective and subjective HIL, frequency, and confidence in assisting consumers, and confidence in understanding changes in federal health reform policies and state Medicaid waiver programs.
Key Results:
Less than one-half (39%) of information intermediaries had high subjective HIL and much fewer (13%) had high objective HIL. The average frequency of assisting consumers with health insurance scores were somewhat low, and confidence in assisting consumers with health insurance scores and confidence with understanding state and federal policies were modest. Results from our logistic regression model indicated that confidence in assisting consumers was found to be the only significant contributor to high subjective HIL. For every one-point increase on the confidence assisting subscale, there was a 35% increase in the information intermediaries having high subjective HIL.
Conclusions:
Findings from this study, coupled with rising uninsured rates, indicate the need for tailored training programs and resources to equip our information intermediaries to provide timely and appropriate health insurance support for consumers. [HLRP: Health Literacy Research and Practice. 2022;6(1):e30–e36.]
Plain Language Summary:
In a sample of 118 information intermediaries, representing community health workers, navigators, and other people in outreach roles, the majority had low subjective and objective HIL. We also found that as confidence with assisting consumers with health insurance needs increases, HIL increased as well. These findings indicate that tailored training programs and resources are needed to equip information intermediaries to provide health insurance support for consumers.
The coronavirus disease 2019 (COVID-19) pandemic and its economic fallout has had a devastating effect on people in the United States, especially those residing in underserved rural regions. The growth in job losses could potentially have a direct influence on health, especially because health insurance and employment are closely linked for roughly 160 million people (Sonfield et al., 2020). Although current data reveal that insurance coverage rates have remained steady, the potential effect of increasing COVID-19 infection rates and permanent job losses on uninsured rates is yet to be determined (Cox & McDermott, 2020; Keith, 2020). As people experience changes in health insurance coverage, they will need assistance with enrolling in alternate health insurance plans that best fit their needs. However, the low health insurance literacy (HIL) of the average U.S. adult serves as a significant barrier to finding appropriate health insurance coverage.
HIL, defined as an individual's ability to seek, obtain, and use health insurance, plays a critical role in access to coverage and care (Consumers Union, 2012; Paez et al., 2014). More than one-half of the U.S. adult population does not understand basic health insurance terms (American Institutes of Certified Professional Accountants, 2013). In a nationally representative sample of 15,168 adults, Edward et al. (2019) found that the majority (51%) reported having inadequate HIL as measured by knowledge of basic insurance terms, and close to one-half (48%) had low confidence in using their insurance to access health care. These trends indicate the need for tailored programs and resources, such as in-person health insurance assistance and navigation services.
Increasingly recognized resources used by consumers to obtain health insurance information are information intermediaries. As a result of the Affordable Care Act (ACA), formal information intermediary roles such as navigators or certified application counselors/assisters were created and trained to meet state and/or federal training and certification requirements to help consumers enroll in federally or state-facilitated marketplaces (Mittler et al., 2013). As the need for health insurance assistance has grown over the years so has the need for expanded health insurance information intermediary roles, which now includes community health workers (CHWs), nurse navigators, case managers, and other outreach workers, who play key roles in translating and transmitting health information to consumers, especially in underserved rural regions (Hibbard & Peters, 2003). Generally, these informal roles do not have standardized training programs or even supervision, but still play a crucial role in assisting consumers with health insurance to accommodate the growing need.
Studies document that compared to usual care, decision coaching provided by information intermediaries can significantly improve knowledge, participation, and improved satisfaction with the decision-making process among consumers (Brown et al., 2016; Sommers et al., 2015; Stacey et al., 2008). Brown et al. (2016), found evidence to support the effect of an information intermediary-led program on increasing consumer confidence in purchasing health insurance. In another study, Sommers et al. (2015) reported assistance from navigators or application assisters were the strongest predictor of enrolling in health insurance. Although effective, gaps in existing programs include the limited focus on identifying and addressing the HIL levels of information intermediaries themselves and their ability to use decision coaching techniques to guide consumers to select health insurance plans that best fit their needs. To address these gaps, we examined the association between HIL, sociodemographic factors, and confidence and behaviors in assisting consumers understand and navigate health insurance among information intermediaries serving rural and urban communities of Kentucky.
Methods
We used a cross-sectional survey design guided by the SHARE approach, a model for shared decision-making. The SHARE approach is a five-step process that is used to guide health professionals to engage in shared decision-making: (1) seek consumers participation; (2) help consumer explore and compare options; (3) assess consumers values and preferences; (4) reach a decision; and (5) evaluate decision (Agency for Healthcare Research and Quality, 2020).
After obtaining Institutional Review Board approval from the University of Kentucky, we recruited information intermediary participants with the help of three statewide organizations of CHWs, primary care clinics, and extension offices using emails and recruitment flyers, which were distributed via organization membership listservs, conferences, and social media platforms. Inclusion criteria included adults who were age 18 years or older and who identified as working in some type of information intermediary role assisting consumers with any aspect of health insurance in Kentucky. This includes both community- and health system-based information intermediaries. An email providing information about the study and a link to participate in an online survey was sent to all members of all organizations who identified as information intermediaries. All surveys were anonymous, and the only identifiable information obtained were emails so we could keep track of those who completed surveys and help address duplication. Participants received a $25 incentive for completing surveys.
Measures
The following measures were collected in the online survey and assessed the various principles addressed in the SHARE approach. Demographic variables included age, sex, race, educational level, and zip code of participants' primary employment location. Frequency of assisting consumers was assessed with 5-items, including helping compare plans, enroll in plan, assess personal values/preferences with selecting plans, assessing financial circumstances, and following up to evaluate use of the plan. Response options for each item ranged from 0 (never) to 4 (always) and a summary score was calculated to represent overall frequency of assisting consumers, yielding a potential range of 0–20. Cronbach's alpha for this scale was 0.98. Next, confidence in assisting consumers regarding the same items as above were assessed. Response options for confidence ranged from 0 (not at all confident) to 3 (very confident) and a summary score was calculated to represent overall confidence in assisting consumers, yielding a potential range of 0 to 15. Cronbach's alpha for this scale was 0.94. Finally, confidence in understanding changes in federal health reform policies and changes in Kentucky's proposed Medicaid waiver program were assessed. Each of these two items followed the same response option as the other confidence items. Again, a summary score was calculated with a potential range of 0 to 6.
The Health Insurance Literacy Measure (HILM) (Paez et al., 2014), a 21-item self-assessment instrument with two scales that measure confidence levels and behaviors when selecting and using health insurance, was used to measure subjective HIL. A 15-item health insurance literacy knowledge (HILK) questionnaire was used to measure objective HIL by assessing knowledge of key health insurance terms and health insurance related processes and policies (such as questions around Medicaid, Medicare, ACA, and state waiver programs and eligibility). This knowledge questionnaire was developed by the research team with input from subject matter experts to measure objective HIL. For each instrument, participants who scored at or above 80% of the potential maximum scores (i.e., 50 or greater for the HILM, 12 of 15 correct answers on the HILK questionnaire) were coded as having “high” HIL for the respective measure.
Data Analysis
Descriptive statistics, including frequency distributions or means and standard deviations were used to summarize study variables. We used multiple logistic regression to examine associations between demographic variables, frequency of, and confidence in assisting consumers and HILM and HILK scores. Variance inflation factors (VIFs) were used to assess for multicollinearity and the Hosmer-Lemeshow test examined overall model fit. In the original models, confidence in understanding state and federal policies was considered, but due to multicollinearity it was removed in the final adjusted models presented. All data analysis was conducted using SAS version 9.4 with an alpha level of .05 throughout.
Results
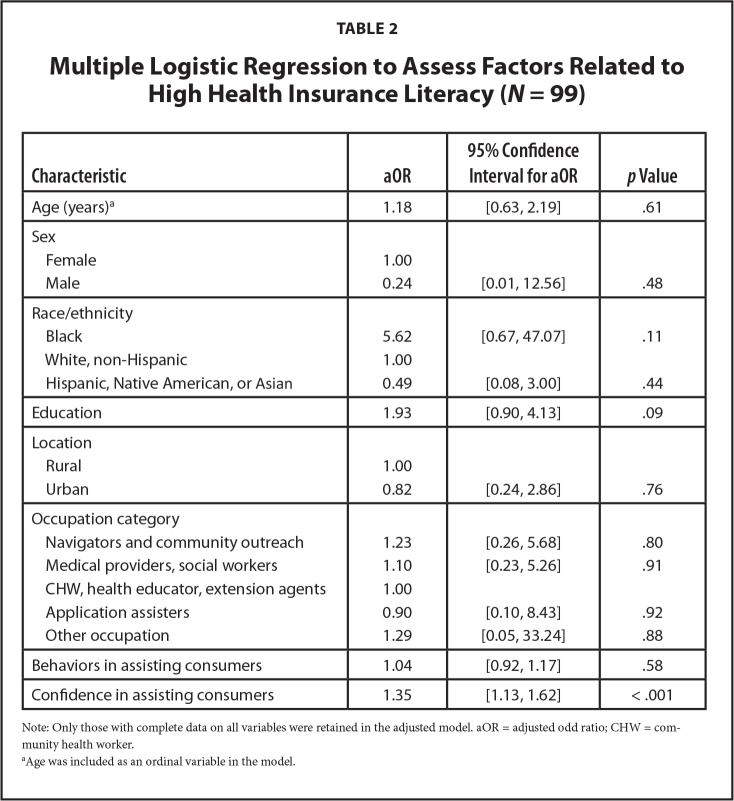
A total of 122 responses were obtained; however, only those with complete data on both HIL tools were retained in this analysis, yielding an effective sample size of 118 respondents. Almost all (89%) respondents were women, and the majority identified as White, non-Hispanic (72%) and served in rural locations (52%) (Table 1). Educational levels were fairly well distributed with less than one-quarter having below a Bachelor's degree (20%), almost one-third (30%) with a Bachelor's, and close to one-half (42%) with a Master's or Doctorate degree. Forty-one percent of respondents were CHWs, health educators, or extension agents.
Table 1.
Descriptive Summary of the Study Sample (N = 118)
| Characteristic | n (%) |
|---|---|
|
| |
| Age (years) | |
| 18–24 | 5 (4.2) |
| 25–34 | 28 (23.7) |
| 35–44 | 29 (24.6) |
| 45+ | 46 (39) |
| Missing data | 10 (8.5) |
|
| |
| Sex | |
| Female | 105 (89) |
| Male | 3 (2.5) |
| Missing data | 10 (8.5) |
|
| |
| Race/ethnicity | |
| White, non-Hispanic | 85 (72) |
| Black/African American | 10 (8.5) |
| Asian | 6 (5.1) |
| Hispanic | 5 (4.2) |
| Native American | 1 (0.85) |
| Missing data | 11 (9.3) |
|
| |
| Education | |
| Less than Bachelor's degree | 24 (20.3) |
| Bachelor's degree | 35 (29.7) |
| Beyond Bachelor's degree | 49 (41.5) |
| Missing data | 10 (8.5) |
|
| |
| Location | |
| Rural | 61 (51.7) |
| Urban | 44 (37.3) |
| Missing data | 13 (11) |
|
| |
| Occupation category | |
| CHW, health educator, extension agents | 48 (40.7) |
| Navigators and community outreach | 22 (18.6) |
| Medical providers, social workers | 18 (15.3) |
| Application assisters | 10 (8.5) |
| Other occupation | 3 (2.5) |
| Missing data | 17 (14.4) |
|
| |
| Health Insurance Literacy Measure | |
| Low | 103 (87.3) |
| Higha | 15 (12.7) |
|
| |
| Health Insurance Literacy Knowledge | |
| Low | 103 (87.3) |
| Highb | 15 (12.7) |
Note. CHW = community health worker.
Score of >80% on the Health Insurance Literacy Measure.
Score of 80% (12 of 15 questions) on Health Insurance Literacy Knowledge.
Less than one-half (39%) of information intermediaries had high subjective HIL and much fewer (13%) had high objective HIL knowledge. Average frequency of assisting consumers with health insurance scores were somewhat low with a mean of 6.9 (standard deviation [SD] = 7.1), from a potential scale range of 0 to 20. Similarly, confidence in assisting consumers with health insurance scores and confidence with understanding state and federal policies were modest (mean [M]= 6.6, SD = 5.2; potential range, 0–15 and M = 6.6, SD = 5.2; potential range, 0–6, respectively). Low consumer HIL (30%) and affordability of health insurance (20%) were identified as the greatest barriers to assisting consumers with health insurance. The greatest needs for consumers were identified as education and instruction around how health insurance works (45%) and the need for affordable insurance options and prescriptions (37%). Participants identified educational programs that promote HIL in multiple languages and literacy levels as the most needed resource (48%) to enable them to better assist consumers.
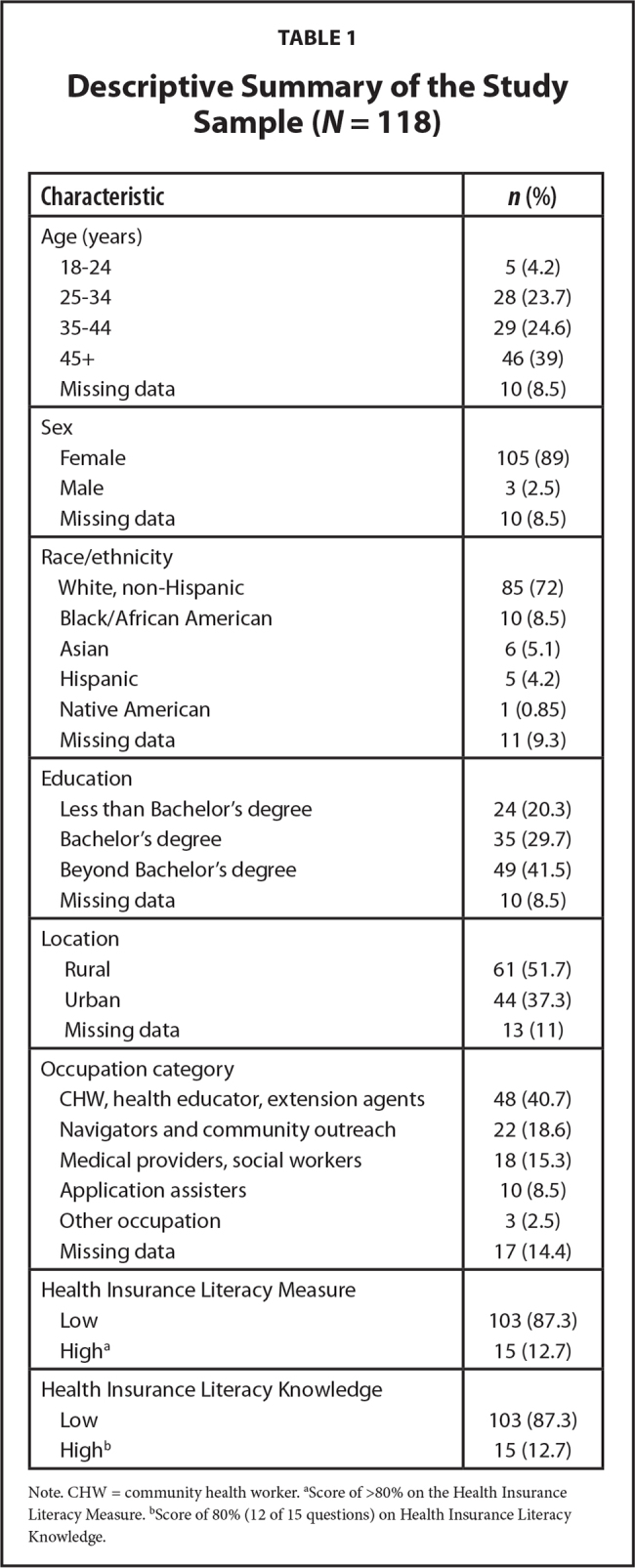
The logistic regression modeling high subjective HIL (HILM) was significant overall (Chi-square = 44.0, p < .001; Table 2). Adjusting for all other variables in the model, confidence in assisting consumers was significantly associated with subjective HIL. For every one-point increase on the confidence assisting subscale, there was a 35% increase in the information intermediaries having high subjective HIL (odds ratio = 1.35, 95% confidence interval = [1.13,1.62]; p < .001). Age, sex, race/ethnicity, education, location, occupation, and frequency of assisting consumers were not related to subjective HIL. The Hosmer-Lemeshow test was nonsignificant (Chi-square = 7.9, p = .44), suggesting the model fit the data. All VIFs were less than 2.7, therefore, multicollinearity was not distorting parameter estimates. For objective HIL (HILK), the overall logistic regression was not significant (Chi-square = 14.5, p = .27), suggesting there were no relationships between any of the sociodemographic variables or behaviors and confidence with assisting subscales and objective HIL.
Table 2.
Multiple Logistic Regression to Assess Factors Related to High Health Insurance Literacy (N = 99)
| Characteristic | aOR | 95% Confidence Interval for aOR | p Value |
|---|---|---|---|
|
| |||
| Age (years)a | 1.18 | [0.63, 2.19] | .61 |
|
| |||
| Sex | |||
| Female | 1.00 | ||
| Male | 0.24 | [0.01, 12.56] | .48 |
|
| |||
| Race/ethnicity | |||
| Black | 5.62 | [0.67, 47.07] | .11 |
| White, non-Hispanic | 1.00 | ||
| Hispanic, Native American, or Asian | 0.49 | [0.08, 3.00] | .44 |
|
| |||
| Education | 1.93 | [0.90, 4.13] | .09 |
|
| |||
| Location | |||
| Rural | 1.00 | ||
| Urban | 0.82 | [0.24, 2.86] | .76 |
|
| |||
| Occupation category | |||
| Navigators and community outreach | 1.23 | [0.26, 5.68] | .80 |
| Medical providers, social workers | 1.10 | [0.23, 5.26] | .91 |
| CHW, health educator, extension agents | 1.00 | ||
| Application assisters | 0.90 | [0.10, 8.43] | .92 |
| Other occupation | 1.29 | [0.05, 33.24] | .88 |
|
| |||
| Behaviors in assisting consumers | 1.04 | [0.92, 1.17] | .58 |
|
| |||
| Confidence in assisting consumers | 1.35 | [1.13, 1.62] | < .001 |
Note: Only those with complete data on all variables were retained in the adjusted model. aOR = adjusted odd ratio; CHW = community health worker.
Age was included as an ordinal variable in the model.
Discussion
In a sample of 118 health information intermediaries serving Kentuckians, with the majority being CHWs, health educators, or extension agents, we found that the majority had low subjective and objective HIL. Participants had a low frequency of assisting consumers with selecting, purchasing, and using health insurance as well as mediocre levels of confidence in helping with these tasks. Confidence in assisting consumers was found to be significant contributor to high subjective HIL, indicating that as confidence with assisting consumers increases, HIL is found to increase as well. These findings have significant implications for information intermediaries who serve in essential roles to educate and empower uninsured and underinsured individuals with the knowledge and understanding of where and how to seek and obtain health insurance to access health care.
The population of uninsured in the U.S. has been increasing in recent years. From 2016 to 2018, the number of people who are uninsured increased from 28.6 million to 30.4 million (Munira & Collins, 2019). The ACA provides access to Medicaid for adults earning less than 138% of the poverty level and subsidized plans through the exchanges for adults earning up to 400% of the poverty level. A 2018 survey indicated that among the uninsured, almost one-half are likely eligible for subsidized insurance options (Munira & Collins, 2019), indicating a lack of consumer awareness around eligibility. Another cross-sectional study of 506 insured U.S. adults conducted in 2016 found lower health information literacy scores to be significantly associated with higher rates of avoiding preventive services and nonpreventive services (Tipirneni et al., 2018). As these studies indicate, the path to accessing health care can be confusing; even when a consumer is already enrolled in a health insurance plan. With the potential effect of the COVID-19 pandemic on rising uninsured rates, information intermediaries and their roles will continue to be crucial to ensuring that consumers get the coverage they need.
Results from our logistic regression analysis indicated that among information intermediaries, confidence in assisting consumers was found to be the only significant predictor of HIL. With increased levels of HIL, information intermediaries will have increased confidence with assisting consumers they serve. Similar results were found in a recent cross-sectional study assessing HIL among a group of 152 community health center staff (Williams et al., 2021). People who reported higher confidence levels (3–4 out of 4) in choosing, comparing, utilizing, and managing their health insurance had higher HIL scores (7.2 average HIL score out of 10) compared to people reporting lower confidence levels of 1 to 2 (5.1 average HIL score) and confidence levels of 2 to 3 (5.8 average HIL score) (p < .05).
In our study, information intermediaries who assisted consumers with health insurance represented various roles and occupations: (1) CHWs, health educators, and extension agents; (2) medical providers and social workers; (3) application assisters; and (4) navigators and community outreach workers. Historically, the role of assisting consumers with health insurance was led by application assisters who became prevalent with the rollout of the ACA. The Department of Health and Human Services (HHS) appropriated funding for states to train and hire this role specifically to support consumer assistance programs (Selwyn & Senter, 2016). Federal legislation also required application assisters, trained to provide enrollment services, to meet state and/or federal training and certification requirements. As a result, we expected but did not find occupation (specifically, application assisters) to be a significant predictor of HIL knowledge in this study indicating potential insufficiencies in training for application assisters in this study.
Currently, no evidence-based programs to support training of information intermediaries targeted at promoting HIL and supporting informed consumer decision-making exist in Kentucky. Additionally, the ever-changing health care and healthcare policy landscape is an additional challenge for those serving in an information intermediary role. In a recent qualitative study conducted with a group of 46 information intermediaries primarily serving rural Kentucky residents, 25% of participants indicated that difficulties in keeping up with the constantly changing policies and procedures related to health insurance were barriers to serving consumers (Edward et al., 2021).
Participants in this study had both low subjective and objective HIL, which reflects the low HIL levels of the general U.S. population (Edward et al., 2019). Subjective HIL was relatively higher in our sample (39%) compared to objective HIL (13%). A discrepancy that is most likely related to consumers overestimating their understanding of health insurance concepts, policies, and processes (Policygenius, 2016). As such, it is important to incorporate objective assessments of HIL within training programs ensure acquisition of the essential skills. Validated tools to measure HIL knowledge are also needed for research and evaluation purposes.
In a 2014 survey conducted by Kaiser Family Foundation, there was an estimated 28,000 full-time staff and volunteers that served in an information intermediary role as health insurance marketplace assisters (Pollitz et al., 2014). Findings from this survey also indicated that training for application assisters could be improved with 92% of assister programs indicating they would like to receive more in-depth training on specific topics including a breakdown of the different plans offered in their Marketplace and how to handle denied claims, disputes with insurers and other problems that arise post-enrollment. The additional training that assisters receive vary considerably by state, with some states supplying more in-depth training than others. For example, between 2013 and 2015, New York experienced high success with implementing the ACA and considers the prioritization of workforce training and development of assisters to be a significant facilitator in that success (Selwyn & Senter, 2016). The 3 day in-person comprehensive training provided to over 1,600 assisters across the state also underwent evaluation via quantitative and qualitative methods, which provided feedback on the quality and effectiveness of the training. In addition to federal training offerings for application assisters and navigators, states will benefit from investing early on in robust training programs for all types of information intermediaries as their roles expand to assisting consumers with accessing health insurance coverage.
Another barrier to the availability of trained information intermediaries is limited funding. The United States Government Accountability Office (2018) report indicated that from 2017 to 2018 funding for advertising open enrollment periods had decreased by 90% from $100 to $10 million dollars. Funding for insurance navigator organizations was also decreased from $63 million to $37 million during that same time frame due to a shift in the Federal Administration's priorities. With this decline in funding, others in contact with consumers such as extension agents, social workers, health educators, and community health workers will be tasked with connecting with the uninsured and underinsured to ensure that they are able to navigate the complex path to healthcare access. Without appropriated funding to formally train and increase availability of this essential resource, it is crucial that training programs are easily accessible, effective, and reflect the most current health care landscape and associated policies. Appropriations from grant funding agencies along with workgroups at the local and state levels that involve a variety of stakeholders from nonprofit organizations to academic researchers invested in health care access are key elements to furthering this initiative.
Study Limitations
Findings from our study should be interpreted cautiously as there were several limitations. Our use of a nonrandomized convenient sample limits generalizability of findings to other information intermediaries. Further, data on length of time in current occupation were not collected; therefore, we are unaware of how experience level predicts HIL knowledge. The HILK questionnaire was developed to assess objective HIL in this study, but the psychometric properties of this tool have not been established. Despite these limitations, this is one of the first studies to establish the HIL and training needs of information intermediaries with varying roles focused on assisting consumers with health insurance. The use of state-wide community and healthcare allowed us to recruit a geographically diverse population to represent information intermediaries serving Kentucky residents in both urban and rural counties. Furthermore, the use of validated tools to measure subjective and objective HIL added to the credibility of our study findings.
Conclusion
Findings from this study indicate that information intermediaries who assist consumers with accessing health insurance coverage in Kentucky serve in numerous community and health system roles. Most participants had low HIL and low confidence in assisting consumers with selecting and using health insurance, indicating the need for tailored training programs and resources to equip our information intermediaries to provide better support for consumers. Evidence gained from this study is crucial to advancing programs promoting HIL and access to care, especially in the current volatile economic and health climate. Additional research is needed to help evaluate training programs to help identify if improvements in HIL can influence consumer's abilities to understand health insurance and increase confidence in enrolling in health insurance plans that best fit their needs.
Acknowledgments
The authors thank the Kentucky Association of Community Health Workers, the Kentucky Primary Care Association, and the University of Kentucky Cooperative Extension Service for support in making this study possible.
References
- Agency for Healthcare Research and Quality . ( 2020. ). The SHARE approach: A model for shared decision making . https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tools/fact-sheet.html [Google Scholar]
- American Institutes of Certified Professional Accountants . ( 2013. ). Half of U.S. adults fail 'health insurance 101,' misidentify common financial terms in plans . https://blog.aicpa.org/2013/09/half-of-usadults-fail-health-insurance-101.html#sthash.CBW3m6AW.dpbs [Google Scholar]
- Brown , V. , Russell , M. , Ginter , A. , Braun , B. , Little , L. , Pippidis , M. , & McCoy , T. ( 2016. ). Smart choice health insurance© . Health Promotion Practice , 17 ( 2 ), 209 – 216 . 10.1177/1524839915620393 PMID: [DOI] [PubMed] [Google Scholar]
- Consumers Union . ( 2012. ). Measuring health insurance literacy: A call to action . https://advocacy.consumerreports.org/wp-content/uploads/2013/03/Health_Insurance_Literacy_Roundtable_rpt.pdf [Google Scholar]
- Cox , C. , & McDermott , D. ( 2020. ). What have pandemic-related job losses meant for health coverage? Kaiser Family Foundation; . https://www.kff.org/policy-watch/what-have-pandemic-related-job-losses-meant-for-health-coverage/ [Google Scholar]
- Edward , J. , Thompson , R. , & Jaramillo , A. ( 2021. ). Availability of health insurance literacy resources fails to meet consumer needs in rural, Appalachian communities: Implications for state Medicaid waivers . The Journal of Rural Health , 37 ( 3 ), 1 – 11 . doi: 10.1111/jrh.12485 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edward , J. , Wiggins , A. , Young , M. H. , & Rayens , M. K. ( 2019. ). significant disparities exist in consumer health insurance literacy: Implications for health care reform . HLRP: Health Literacy Research and Practice , 3 ( 4 ), e250 – e258 . 10.3928/24748307-20190923-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard , J. H. , & Peters , E. ( 2003. ). Supporting informed consumer health care decisions: Data presentation approaches that facilitate the use of information in choice . Annual Review of Public Health , 24 ( 1 ), 413 – 433 . 10.1146/annurev.publ-health.24.100901.141005 PMID: [DOI] [PubMed] [Google Scholar]
- Keith , K. ( 2020. ). CDC 2019 coverage numbers show increase in uninsurance rate, with caveats . Health Affairs Blog; . https://www.healthaf-fairs.org/do/10.1377/hblog20200914.60859/full/ [Google Scholar]
- Mittler , J. N. , Martsolf , G. R. , Telenko , S. J. , & Scanlon , D. P. ( 2013. ). Making sense of “consumer engagement” initiatives to improve health and health care: A conceptual framework to guide policy and practice . The Milbank Quarterly , 91 ( 1 ), 37 – 77 . 10.1111/milq.12002 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munira , Z. G. , & Collins , S. R. ( 2019. ). Who are the remaining uninsured, and why do they lack coverage? Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2018 . Commonwealth Fund; . 10.26099/h0xy-az24 [DOI] [Google Scholar]
- Paez , K. A. , Mallery , C. J. , Noel , H. , Pugliese , C. , McSorley , V. E. , Lucado , J. L. , & Ganachari , D. ( 2014. ). Development of the Health Insurance Literacy Measure (HILM): Conceptualizing and measuring consumer ability to choose and use private health insurance . Journal of Health Communication , 19 ( 2, Suppl. 2 ), 225 – 239 . 10.1080/10810730.2014.936568 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Policygenius . ( 2016. ). Health insurance literacy survey . Radius Global Market Research; . https://www.policygenius.com/health-insurance/health-insurance-literacy-survey/#survey-results [Google Scholar]
- Pollitz , K. , Tolbert , J. , & Ma , R. ( 2014. ). Survey of health insurance marketplace assister programs: A First look at consumer assistance under the affordable care act . Kaiser Family Foundation; . http://files.kff.org/attachment/survey-of-health-insurance-marketplace-assister-programs-report [Google Scholar]
- Selwyn , C. , & Senter , L. ( 2016. ). From policy to practice in the Affordable Care Act: Training center for New York State's health insurance programs . Healthcare (Amsterdam, Netherlands) , 4 ( 3 ), 235 – 239 . 10.1016/j.hjdsi.2015.12.007 PMID: [DOI] [PubMed] [Google Scholar]
- Sommers , B. D. , Maylone , B. , Nguyen , K. H. , Blendon , R. J. , & Epstein , A. M. ( 2015. ). The impact of state policies on ACA applications and enrollment among low-income adults in Arkansas, Kentucky, and Texas . Health Affairs (Project Hope) , 34 , 1010 – 1018 . 10.1377/hlthaff.2015.0215 PMID: [DOI] [PubMed] [Google Scholar]
- Sonfield , A. , Frost , J. J. , Dawson , R. , & Lindberg , L. D. ( 2020. ). COVID-19 job losses threaten insurance coverage and access to reproductive health care for millions . Health Affairs Blog; . 10.1377/hblog20200728.779022 [DOI] [Google Scholar]
- Stacey , D. , Murray , M. A. , Légaré , F. , Sandy , D. , Menard , P. , & O'Connor , A. ( 2008. ). Decision coaching to support shared decision making: A framework, evidence, and implications for nursing practice, education, and policy . Worldviews on Evidence-Based Nursing , 5 ( 1 ), 25 – 35 . 10.1111/j.1741-6787.2007.00108.x PMID: [DOI] [PubMed] [Google Scholar]
- Tipirneni , R. , Politi , M. C. , Kullgren , J. T. , Kieffer , E. C. , Goold , S. D. , & Scherer , A. M. ( 2018. ). Association between health insurance literacy and avoidance of health care services owing to cost . JAMA Network Open , 1 ( 7 ), e184796 10.1001/jamanetworkopen.2018.4796 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams , C. B. , Pensa , M. A. , & Olson , D. P. ( 2021. ). Health insurance literacy in community health center staff . Journal of Public Health , 29 , 1261 – 1265 . 10.1007/s10389-020-01250-x [DOI] [Google Scholar]
- United States Government Accountability Office . ( 2018. ). Health insurance exchanges. HHS should enhance its management of open enrollment performance . GAO Highlights; . https://www.gao.gov/assets/700/693362.pdf [Google Scholar]