Abstract
Objective:
To evaluate the treatment and posttreatment dentoskeletal effects induced by the Mandibular Advancement Repositioning Appliance (MARA) in the treatment of Class II malocclusion.
Materials and Methods:
The treated sample consisted of 23 consecutively treated patients at prepubertal or pubertal stages, as assessed by the cervical vertebral maturation method. A control group of untreated Class II subjects was generated from published normative growth data. Lateral cephalograms were digitized and superimposed via cephalometric software at three different times: T1, pretreatment; T2, post-MARA treatment; and T3, at least 1 year after T2. The T1–T2, T2–T3, and T1–T3 changes in the treated group were compared to those in the control group with independent-sample Student's t-tests.
Results:
Skeletal and dentoalveolar effects of MARA were assessed after the active phase of the treatment (T1–T2). Mandibular elongation in length (Co-Gn, +2.2 mm) was evident together with lower incisor proclination (IMPA, +5.8 mm). A relapse tendency for IMPA was noticed after removing the appliance (IMPA, −2.1° during T2–T3). Significant skeletal effects (Co-Gn, +2.0 mm) and headgear effects on the maxilla (SNA, −1.2°) were significant in the long term (T1–T3).
Conclusions:
The MARA appliance provides an effective correction of Class II malocclusion, which is maintained at a posttreatment observation with a moderate skeletal effect.
Keywords: Fixed functional appliances, Class II malocclusion, Cephalometrics
INTRODUCTION
The Mandibular Advancement Repositioning Appliance (MARA), a noncompliance device for Class II treatment, was first proposed by Eckhart and Toll in 1998.1 Since then it has received scarce attention in the literature2–5 in spite of the increasing interest in Class II noncompliance treatment options6–11 such as the Herbst, the Forsus, and the Jasper Jumper.
When cooperation may be a problem12 or in late-adolescence treatment, a recommendable choice can include noncompliance appliances.13 Bulkiness and complications represent a problem in the clinical management of the Herbst appliance in 60% of patients.14 The MARA is an alternative to the Herbst, with the major advantage being that it treats a Class II malocclusion in combination with comprehensive fixed appliances. This may represent a favorable clinical feature in shortening treatment duration. The MARA differs from other noncompliance Class II devices such as the Forsus8,9 or Jasper Jumper7,9,10 because it is rigid and has no continuous upper arch–lower arch connection.
Gonner et al.2 evaluated the clinical effectiveness of the appliance in the posttreatment period with no controls, while Pangrazio-Kulbersh et al.3 used a matched untreated Class II control group for comparisons with the treated group, with no follow-up. Only recently Siara-Olds et al.4 evaluated the posttreatment effects of MARA with respect to untreated controls. In this study the authors annualized the treatment outcomes in order to compare their findings with those of other treatment modalities. According to the present literature, the MARA is able to produce effective Class II correction by reducing overjet, Wits, and ANB angle. Gonner et al.2 showed a few dental side effects (lower incisor proclination adversely related to age of treatment). Pangrazio-Kulbersh et al.3 reported similar findings together with a distalizing effect on the upper first molar with a smaller “headgear effect” (growth restriction of the maxilla), as compared to the Herbst appliance. Mandibular first molars and incisors experienced significant sagittal advancement. Siara-Olds et al.4 reported long-term stability of dentoalveolar changes of comprehensive MARA and fixed appliance therapy, while no significant annualized changes of skeletal growth were reported. Unfortunately, the annualization used in studies on growing patients is questionable.
The aim of this controlled clinical study was to evaluate the treatment and posttreatment dentoskeletal effects induced by MARA in the treatment of Class II malocclusion.
MATERIALS AND METHODS
Subjects
Approval for this study was received from the Ethical Committee at the University of Florence, Italy. From a parent sample of 62 Class II division 1 subjects treated consecutively with the MARA appliance, 23 subjects were selected according to the following inclusion criteria: ANB greater than or equal to 4°, full Class II or end-to-end molar relationships, and follow-up observation at least 1 year after the end of comprehensive treatment with MARA and fixed appliances. All patients received active treatment with MARA before (15 subjects) or during (8 subjects) their pubertal growth spurt, as assessed by the cervical vertebral maturation (CVM) method.15 The assessment of the cervical vertebral stages for each subject was performed by one investigator and verified by a second one (T.B.). Any disagreements were resolved to the satisfaction of both observers.
The mean age of the treated group at time 1 (T1, maximum 6 months before the start of treatment) was 10.2 ± 1.5 years; at time 2 (T2, immediately after MARA treatment) it was 12.3 ± 1.5 years; and at time 3 (T3, at least 1 year after comprehensive treatment) it was 14.8 ± 2.3 years. Mean T1–T2 interval was 2.1 ± 1.0 years, mean T2–T3 interval was 2.4 ± 1.7 years, and mean T1–T3 interval was 4.6 ± 2.0 years. The median value for the CVM stages at T1 was 2 (range, 1–3); it was 3 (range, 2–5) at T2; and it was 5 (range, 3–6) at T3.
The control “group” comprised data calculated on longitudinal series of 17 untreated Class II subjects selected from the University of Michigan and Denver Child Growth Studies.16 The longitudinal series consisted of Class II subjects who matched the treated subjects for Class II dentoskeletal features at T1, sex distribution, age, and skeletal maturation (CVM stages) at T1, T2, and T3. The use of historical controls was due to the lack of ethical reasons to leave Class II patients untreated at the developmental period (puberty), which is known to represent the optimal time for orthopedic modifications.6,15
Treatment Protocol
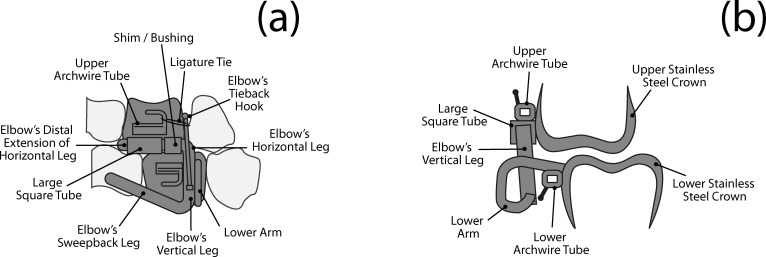
All patients were consecutively treated by the same operator with MARA (AOA, Sturtevant, Wis) and fixed appliances followed by removable retention in a private practice setting. No subjects underwent extraction of teeth as part of the treatment protocol, nor did any undergo maxillary expansion concurrent with the use of the MARA appliance. The MARA inclined plane (elbow's sweepback leg; Figure 1) works as an obstacle to be avoided during closure, inducing the lower jaw to move forward. This is supposed to favor a neuromuscular reeducation during correction of the Class II dentoskeletal relationship. During treatment with the MARA it is also possible to use other appliances (like fixed appliances or rapid palatal expander) to better address specific patient needs and to shorten treatment duration. The developers1 of the appliance recommend a 12-month treatment time to achieve a bite-jumping or orthopedic effect. Stabilization of the lower molars is assisted by the fitting of a lingual arch, which is constructed at a 2-mm to 3-mm distance from the lingual surface of the lower incisors in order to prevent proclination of these teeth. This appliance does not require the placement of attachments on teeth other than the first molars.
Figure 1.
The Mandibular Advancement Repositioning Appliance (MARA) and its components: (a) sagittal view, (b) frontal section.
A stepwise advancement protocol with 2–3-mm enhancement steps17–19 was used up until the point that a slight overcorrection of the Class II dental relationship was achieved. Fixed appliances were initiated together with the MARA or after a few months of active treatment. The T1–T2 interval provided information about the active treatment with the MARA appliance. The T2–T3 interval gave data about posttreatment changes that included a phase of finishing treatment with fixed appliances. The T1–T3 interval provided information about the overall effects induced by MARA during treatment and posttreatment intervals.
Cephalometric Analysis
Lateral cephalograms were traced and measured using a digitizing software (Viewbox, ver. 3.0; DHAL software, Kifissia, Greece).20 There was no difference in cephalometric magnification between the cephalograms of the two groups (8%).
A customized analysis required the digitization of 65 landmarks and four fiducial markers.14 The analysis contained measurements from the analyses of Steiner,21 Jacobson,22 Ricketts,23 and McNamara.24 It generated 34 variables (12 angular and 22 linear) for each tracing. Tracing involved anatomic stable structures such as the inner contour of the symphysis, the alveolar nerve canal, and the inner contour of the palatal bone. A preliminary tracing was made on T1 cephalograms for each patient and fiducial points were placed (two in the maxilla and two in the mandible). Fiducial markers were then transferred to the T2 and T3 tracings based on superimposition, via software, over anatomical stable structures,25 as described by Stahl et al.16 This superimposition allowed for the description of the movement of the maxillary dentition relative to the maxilla and of mandibular dentition relative to the mandible.
Method Error
All cephalograms were traced and superimposed by the same operator and were checked by a second operator to verify anatomic outlines, landmark placement, and tracing superimpositions. Any disagreements were resolved to the satisfaction of both observers.
Ten randomly selected cephalograms were re-digitized by the same operator, and the variables were recalculated to determine the method error with the Intraclass Correlation Coefficient (ICC). The ICCs ranged from 0.90 to 0.99 for linear measurements and from 0.92 to 0.98 for angular measurements. All recalculated measures were within 1 mm/1 d° from the original, and the average discrepancy was 0.4 mm/0.4°.
Statistical Analysis
Descriptive statistics were calculated for each cephalometric variable. Craniofacial changes in the treated group were compared with the growth changes occurring in the corresponding control group. T1–T2 (active MARA treatment), T2–T3 (posttreatment modifications), and T1–T3 (long-term effects) changes were analyzed.
A preliminary Shapiro-Wilks test was performed to assess whether or not data had a normal distribution. All statistical comparisons were performed by an independent-sample Student's t-test. The significance level was set at P < .05. Considering mandibular elongation (Co-Gn) a sensitive variable for Class II correction, the power of the statistics was calculated as 0.82 with reference to the literature.6 The tests were carried out using a commercial statistical package (SPSS for Windows, release 12.0, SPSS Inc, Chicago, Ill).
RESULTS
In the present study the mean duration of the MARA treatment was 1.2 ± 0.5 years. Results of the statistical comparisons between MARA patients and Class II control subjects on the changes for all cephalometric variables during the T1–T2 observation interval are reported in Table 1. All cephalometric variables contributing to Class II correction showed significantly favorable changes (ANB angle, −1.4°; Wits, −2.1 mm; overjet, −2.8 mm). A “headgear effect” was observed in the maxilla (A to Nasion perpendicular, −0.8 mm), while total mandibular length (Co-Gn) and ramus height (Co-Go) increased significantly more in cases than in controls (+2.2 mm and +2.3 mm, respectively), thus enhancing a favorable differential growth pattern (Max/Mand differential, +2.8 mm). The lower incisors exhibited sagittal advancement and proclination (+5.8°) relative to the mandibular plane. The lower molars were also significantly advanced (+1.0 mm) and showed some extrusion (+0.9 mm). There were no adverse effects on the vertical dimension with any significant change on vertical measures.
Table 1.
Statistical Comparison of Pretreatment T1–T2 Changes: Mandibular Advancement Repositioning Appliance (MARA) Active Phasea
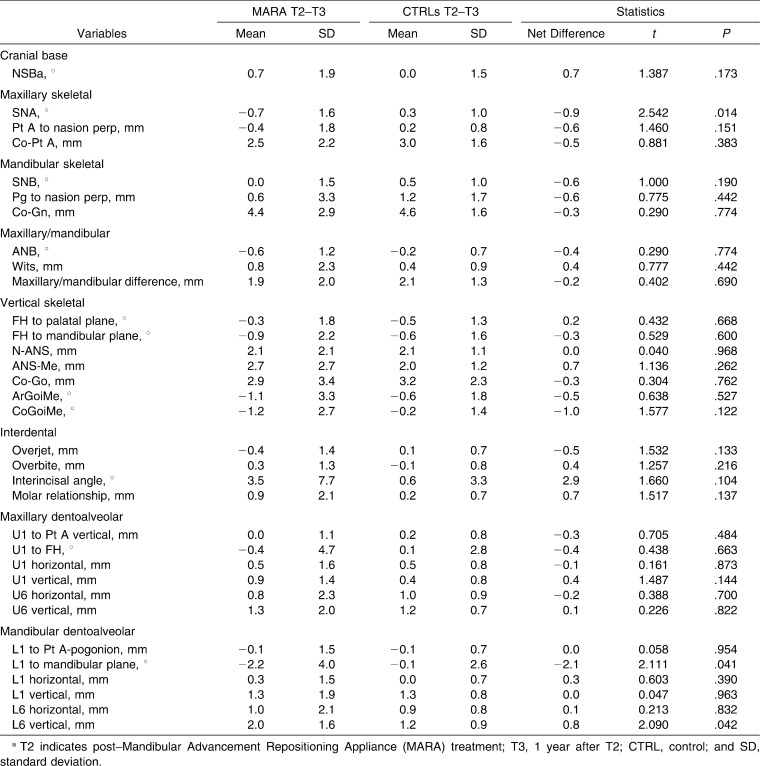
T2–T3 interval changes and statistical comparison are reported in Table 2. Only minor posttreatment changes were noted as a slight, but significant, relapse (−2.2°) in the excessive proclination of the lower incisors. The “headgear effect” on the maxilla (SNA, −0.9°) continued during this phase.
Table 2.
Statistical Comparison of T2–T3 Changes: Fixed Appliance Finishing and Recovery Phasea
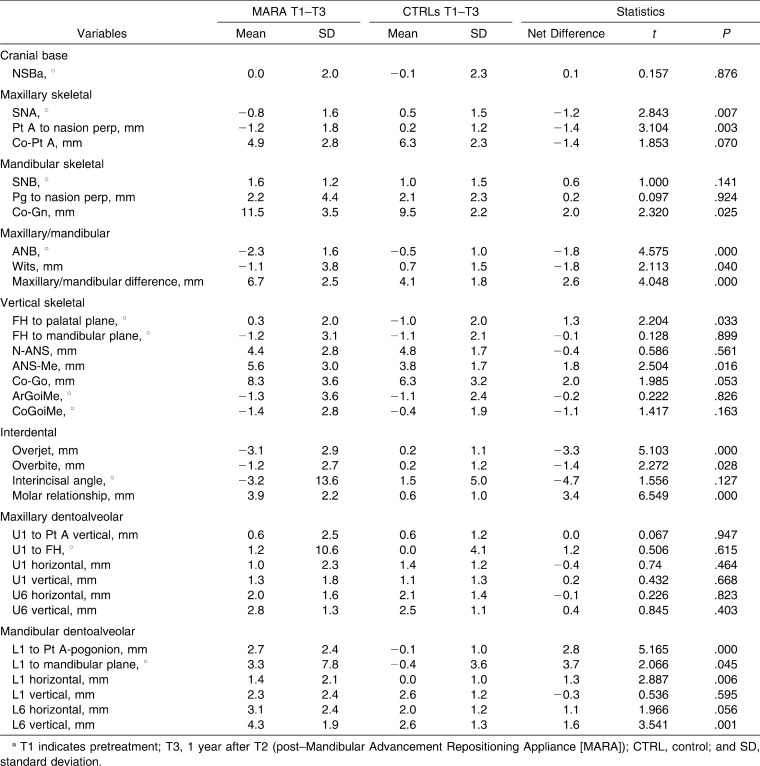
T1–T3 changes describe overall treatment effects of comprehensive MARA and fixed appliance treatment and are shown in Table 3. The headgear effect (SNA, −1.2°; A to Nasion per, −1.4 mm) on the maxilla was associated with mandibular supplemental elongation (Co-Gn, +2.0 mm). ANB angle (−1.8°), Wits (−1.8 mm), overjet (−3.3 mm), and overbite (−1.4 mm) showed significantly greater decreases in MARA patients when compared to Class II controls. A vertical effect was present, with a slight opening of the Frankfurt to palatal plane angle (+1.3°) and an increase of the lower third of the face (ANS-Me, + 1.8 mm) in the MARA group. The lower incisors were proclined (+3.7°), with a tendency for the mandibular first molar to extrude (+1.6 mm) in the MARA group vs controls.
Table 3.
Statistical Comparison of T1–T3 Changes: Long-Term Changesa
DISCUSSION
The present controlled clinical study evaluated the effectiveness of MARA in Class II patients treated at circumpubertal ages compared with the use of untreated Class II controls and the inclusion of a posttreatment observation period.
Gonner et al.2 followed a protocol similar to the one used in the present study, but without untreated Class II controls or evaluation of skeletal maturity. They reported only a few cephalometric variables (ANB, IMPA, incisor position change, and overjet) that showed changes that were similar to those shown in the present study. The study by the group at the University of Detroit3,4 compared MARA patients vs Herbst, Twin Block, and bionator patients and Class II untreated controls using a larger number of cephalometric variables. However, comparisons shown in these studies were possible only after annualization of measurements. No skeletal effect was evident for any of the appliances, apart from a maxillary growth restriction potential of the acrylic splint Herbst. Thus, Class II correction was mainly attributed to dentoalveolar effects. Since concurrent treatment with Class II devices and fixed appliances is rare, the ability to compare the effect of the combination of MARA and fixed appliances with the effects of other similar treatment alternatives is very limited.
The presence of tubes on the upper and lower molar bands of the MARA offers the rare opportunity for a one-stage treatment that combines an effective Class II treatment device and comprehensive fixed appliances. Comparisons are possible with Forsus,8,9 Jasper Jumper7,9,10 (concurrent treatment), and Herbst (consecutive treatment)6,11 appliances. No significant differences can be found with regard to the effectiveness of different Class II noncompliance treatment protocols. A general trend can be described according to the values of the different variables: Forsus and Jasper Jumper appliances present with a Class II correction potential that is mainly dentoalveolar, while the Herbst appliance has a defined, although moderate, skeletal effect both in the mandible and the maxilla. The MARA is similar to the Herbst in that it offers mild but significant skeletal effects (on the mandible Co-Gn, +2.0 mm, and on the maxilla A to Na perp, −1.4 mm after follow-up) with a reduced lower incisor proclination.
During the finishing and recovery phase (T2–T3) no relapse tendency was assessed with the exception of the lower incisors that tended to lose torque. Remodeling at point A went on during this phase, giving a continued slight headgear effect on the maxilla, as reported also by Siara-Olds et al.4 The MARA treatment of most of the patients was active during or slightly before the pubertal peak. Thus, the T2–T3 period was mainly postpubertal, and this may have resulted in the stability of the outcomes. During this period the growth rate of the treated subjects was similar to that of the Class II controls, and it has been reported15 that physiological postpubertal mandibular growth in untreated Class II subjects is similar to that of untreated Class I subjects.
The vertical dentoskeletal changes were generally not pronounced (within 2.0 mm or degrees when compared to those of the controls). A significant amount of lower first molar extrusion (1.6 mm) did not lead to skeletal bite opening because of the concurrent supplementary elongation of the mandibular ramus (Co-Go, 2.0 mm).
The overall T1–T3 change in the inclination of the lower incisor to the mandibular plane in the treated sample was +3.3°. This value is limited with respect to the range of average proclination (3–7°) reported in the literature.6,9,26,27 This favorable effect may be attributed to the particular design of the MARA, which allows for concurrent treatment with fixed appliances. Furthermore, the use of full-size wires on the lower incisor may help in maintaining incisor inclination with respect to the mandibular plane.
CONCLUSIONS
When compared to matched untreated Class II controls, the MARA produces favorable skeletal changes (mandibular elongation, maxillary growth restriction, ANB decrease), although modest in entity, and dentoalveolar changes (overjet and overbite decrease, molar relationship correction) are maintained at an average 1-year posttreatment observation.
Lower incisor proclination is limited, probably as a result of fixed appliance treatment used concurrently with MARA.
REFERENCES
- 1.Eckhart J. E, Toll D. E, inventors; Ormco Corporation, assignee Appliance and method for assisting a patient in maintaining a forward-moving force on the patient's mandibular jaw. US patent 5848891. December 15, 1998. [Google Scholar]
- 2.Gonner U, Ozkan V, Jahn E, Toll D. E. Effect of the MARA appliance on the position of the lower anteriors in children, adolescents and adults with Class II malocclusion. J Orofac Orthop. 2007;68:397–412. doi: 10.1007/s00056-007-0656-7. [DOI] [PubMed] [Google Scholar]
- 3.Pangrazio-Kulbersh V, Berger J. L, Chermak D. S, Kaczynski R, Simon E. S, Haerian A. Treatment effects of the mandibular anterior repositioning appliance on patients with Class II malocclusion. Am J Orthod Dentofacial Orthop. 2003;123:286–295. doi: 10.1067/mod.2003.8. [DOI] [PubMed] [Google Scholar]
- 4.Siara-Olds N. J, Pangrazio-Kulbersh V, Berger J, Bayirli B. Long-term dentoskeletal changes with the bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010;80:18–29. doi: 10.2319/020109-11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toll D. E, Popovic N, Andjelic J, Drinkuth N. Modified camouflage therapy in an adult Class I patient with TMJ complaints. A case report. J Orofac Orthop. 2010;71:152–162. doi: 10.1007/s00056-010-9948-4. [DOI] [PubMed] [Google Scholar]
- 6.Baccetti T, Franchi L, Stahl F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. Am J Orthod Dentofacial Orthop. 2009;135:698e1–698e10, 98–99. doi: 10.1016/j.ajodo.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 7.de Oliveira J. N, Jr, Rodrigues de Almeida R, Rodrigues de Almeida M, de Oliveira J. N. Dentoskeletal changes induced by the Jasper Jumper and cervical headgear appliances followed by fixed orthodontic treatment. Am J Orthod Dentofacial Orthop. 2007;132:54–62. doi: 10.1016/j.ajodo.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 8.Jones G, Buschang P. H, Kim K. B, Oliver D. R. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 9.Karacay S, Akin E, Olmez H, Gurton A. U, Sagdic D. Forsus Nitinol Flat Spring and Jasper Jumper corrections of Class II division 1 malocclusions. Angle Orthod. 2006;76:666–672. doi: 10.1043/0003-3219(2006)076[0666:FNFSAJ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Kucukkeles N, Ilhan I, Orgun I. A. Treatment efficiency in skeletal Class II patients treated with the Jasper Jumper. Angle Orthod. 2007;77:449–456. doi: 10.2319/0003-3219(2007)077[0449:TEISCI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Ruf S, Pancherz H. Herbst/multibracket appliance treatment of Class II division 1 malocclusions in early and late adulthood. A prospective cephalometric study of consecutively treated subjects. Eur J Orthod. 2006;28:352–360. doi: 10.1093/ejo/cji116. [DOI] [PubMed] [Google Scholar]
- 12.O'Brien K, Wright J, Conboy F, et al. Effectiveness of treatment for Class II malocclusion with the Herbst or twin-block appliances: a randomized, controlled trial. Am J Orthod Dentofacial Orthop. 2003;124:128–137. doi: 10.1016/s0889-5406(03)00345-7. [DOI] [PubMed] [Google Scholar]
- 13.McSherry P. F, Bradley H. Class II correction—reducing patient compliance: a review of the available techniques. J Orthod. 2000;27:219–225. doi: 10.1179/ortho.27.3.219. [DOI] [PubMed] [Google Scholar]
- 14.Schioth T, von Bremen J, Pancherz H, Ruf S. Complications during Herbst appliance treatment with reduced mandibular cast splints: a prospective, clinical multicenter study. J Orofac Orthop. 2007;68:321–327. doi: 10.1007/s00056-007-0703-4. [DOI] [PubMed] [Google Scholar]
- 15.Baccetti T, Franchi L, McNamara J. A., Jr The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 16.Stahl F, Baccetti T, Franchi L, McNamara J. A., Jr Longitudinal growth changes in untreated subjects with Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:125–137. doi: 10.1016/j.ajodo.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 17.Du X, Hagg U, Rabie A. B. Effects of headgear Herbst and mandibular step-by-step advancement versus conventional Herbst appliance and maximal jumping of the mandible. Eur J Orthod. 2002;24:167–174. doi: 10.1093/ejo/24.2.167. [DOI] [PubMed] [Google Scholar]
- 18.Hägg U, Rabie A. B, Bendeus M, et al. Condylar growth and mandibular positioning with stepwise vs maximum advancement. Am J Orthod Dentofacial Orthop. 2008;134:525–536. doi: 10.1016/j.ajodo.2006.09.064. [DOI] [PubMed] [Google Scholar]
- 19.Purkayastha S. K, Rabie A. B, Wong R. Treatment of skeletal Class II malocclusion in adults: stepwise vs single-step advancement with the Herbst appliance. World J Orthod. 2008;9:233–243. [PubMed] [Google Scholar]
- 20.Halazonetis D. J. Computer-assisted cephalometric analysis. Am J Orthod Dentofacial Orthop. 1994;105:517–521. doi: 10.1016/S0889-5406(06)80049-1. [DOI] [PubMed] [Google Scholar]
- 21.Steiner C. C. Cephalometrics for you and me. Am J Orthod. 1953;39:729–755. [Google Scholar]
- 22.Jacobson A. The “Wits” appraisal of jaw disharmony. Am J Orthod. 1975;67:125–138. doi: 10.1016/0002-9416(75)90065-2. [DOI] [PubMed] [Google Scholar]
- 23.Ricketts R. M. Perspectives in the clinical application of cephalometrics. The first fifty years. Angle Orthod. 1981;51:115–150. doi: 10.1043/0003-3219(1981)051<0115:PITCAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.McNamara J. A., Jr A method of cephalometric evaluation. Am J Orthod. 1984;86:449–469. doi: 10.1016/s0002-9416(84)90352-x. [DOI] [PubMed] [Google Scholar]
- 25.Bjork A, Skieller V. Facial development and tooth eruption. An implant study at the age of puberty. Am J Orthod. 1972;62:339–383. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 26.Hansen K, Koutsonas T. G, Pancherz H. Long-term effects of Herbst treatment on the mandibular incisor segment: a cephalometric and biometric investigation. Am J Orthod Dentofacial Orthop. 1997;112:92–103. doi: 10.1016/s0889-5406(97)70279-8. [DOI] [PubMed] [Google Scholar]
- 27.Ruf S, Pancherz H. Dentoskeletal effects and facial profile changes in young adults treated with the Herbst appliance. Angle Orthod. 1999;69:239–246. doi: 10.1043/0003-3219(1999)069<0239:DEAFPC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]