Abstract
Objective:
To evaluate the skeletal and dentoalveolar components in adult subjects with skeletal open bite in the presence or absence of dental compensation.
Materials and Methods:
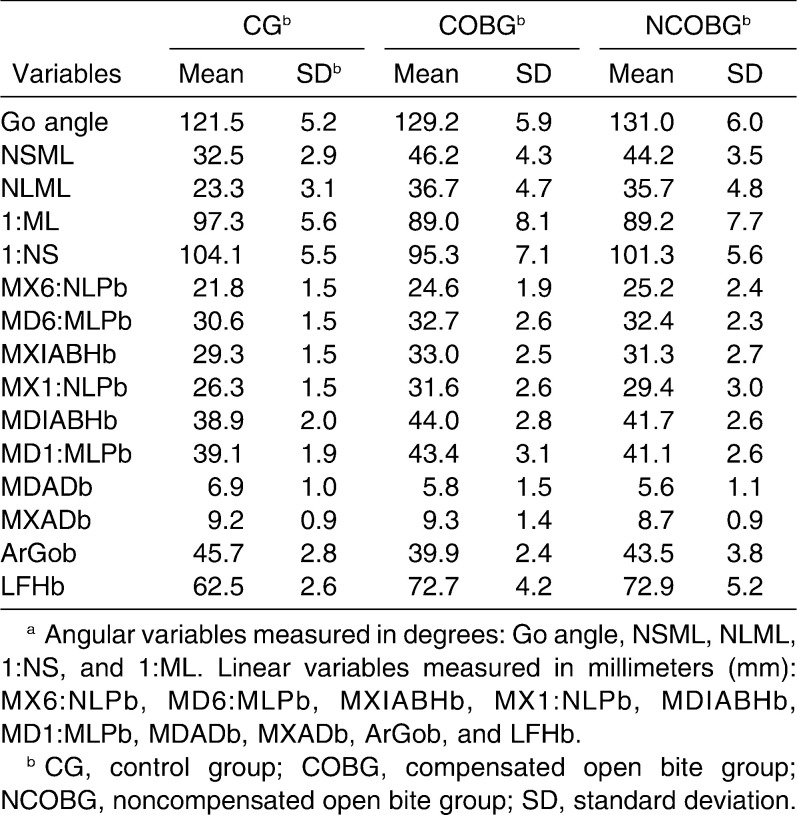
The study sample included 69 adult female subjects who belonged to three groups according to skeletal vertical relationships and overbite. A total of 15 variables (5 angular, 10 linear) were evaluated. Values in the dentally compensated open bite group (COBG), the dentally noncompensated open bite group (NCOBG), and the control group with normal vertical skeletal relationships and overbite (CG) were compared by means of parametric statistics.
Results:
The COBG and the NCOBG showed significantly greater incisor and molar heights in both jaws than the CG. No significant difference in upper or lower molar height was found between COBG and NCOBG. Incisor height was significantly greater in COBG than in NCOBG. Elongation in the incisor region was accompanied by significant narrowing of the lower anterior alveolar process in both skeletal open bite groups. Proclination of the upper incisors was significantly smaller in the COBG than in the other groups.
Conclusions:
Dentoalveolar components consisting of incisor elongation and inclination play a significant role in compensating for skeletal open bite configuration in adult subjects. Increased molar height is a common finding in adults with skeletal open bite.
Keywords: Molar height, Dentoalveolar compensation, Skeletal open bite, Cephalometrics
INTRODUCTION
Skeletal open bite patients present a severe challenge in orthodontic treatment. In growing patients, relative intrusion of the molars is recommended to control for vertical development of the jaws.1 In adult patients, absolute intrusion of posterior occlusal segments can be performed with the aid of temporary anchorage devices,2–10 and surgical treatment can be considered as well. The choice of treatment protocol depends on many factors, including esthetic and occlusal aspects, morphologic characteristics, and the severity of the skeletal anomaly.11–26
The indication for molar intrusion is often based on the assumption that the value of molar height in open bite patients is greater than in the “normal population.”2,6,10,27–29 Many authors state that increased molar height is one of the common features of individuals with dentoskeletal open bite, and they advocate molar intrusion to correct the disharmony.12–21,30,31 However, other authors do not support these claims.15,22–24 In a subpopulation of subjects with skeletal open bite, dental compensation occurring in the frontal region may significantly limit the negative overbite. In fact, these patients present with a normal or even excessive dental overbite (dentally compensated skeletal open bite).11
The aims of the present prospective study were (1) to analyze the dentofacial characteristics of adult subjects with skeletal open bite in comparison with adult subjects with normal vertical skeletal characteristics and ideal occlusion, and (2) to compare the dentoalveolar features of subjects showing compensated vs noncompensated skeletal open bite.
MATERIALS AND METHODS
Our sample included 69 pretreatment cephalograms of adult white female subjects. An informed consent was obtained from each of the subjects enrolled in this prospective study. The minimum age requirement was 17 years, and lateral cephalograms had to be taken after active circumpubertal growth stage CS6 had been completed, according to the cervical vertebral maturation method described by Baccetti et al.32
The study sample comprised three groups categorized according to vertical skeletal relationships and overbite. The control group (CG; n = 23; mean age, 24.6 years) included subjects who met the following criteria: bilateral Class I angle occlusion, NS-ML angle within the range of 33 ± 6 degrees, and overbite measuring 1 to 4 mm; subjects in the dentally compensated open bite group (COBG; n = 20; mean age, 25.5 years) met the following criteria: NS-ML angle greater than 40 degrees and overbite greater than 0.5 mm; and the dentally noncompensated open bite group (NCOBG; n = 20; mean age, 23.7 years) consisted of subjects for whom the following criteria applied: NS-ML angle greater than 40 degrees and negative overbite (ie, less than 0 mm).
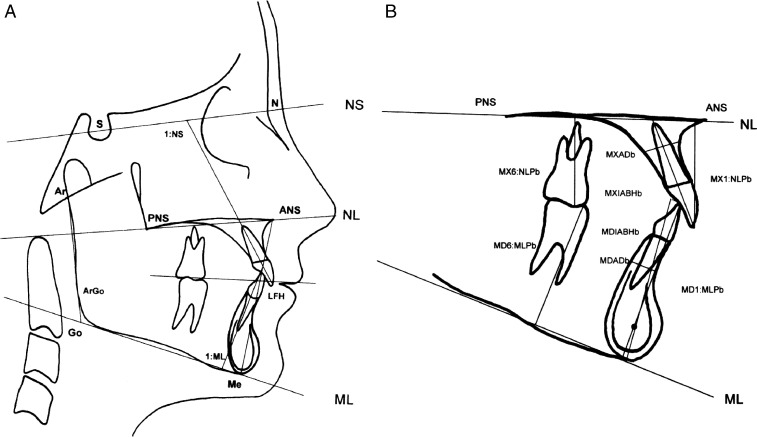
All cephalograms were traced by hand on acetate paper over an illuminated viewbox. The data measured were evaluated within an accuracy of 0.5 mm and 0.5 degrees. All tracings and evaluations were performed by the same operator. A total of 15 parameters were evaluated—5 angular and 10 linear. The list of variables can be derived from Table 1. A graphic representation of the cephalometric parameters is shown in Figures 1A and 1B. Owing to the varying magnification of individual cephalograms, all linear parameters were recalculated, and data are shown at life size.
Table 1.
Descriptive Statistics of Cephalometric Variablesa
Figure 1.
Tracing of cephalometric x-ray (A) and dentoalveolar variables (B). Angular variables (degrees): Go angle—Ar-Go-Me angle; NSML—angle NS-ML; NLML—angle NL-ML; 1:ML—inclination of lower incisors to ML; and 1:NS—inclination of upper incisors to NS. Linear variables (mm): MX6:NLPb—upper molar height, distance between MB cusp of upper first molar on perpendicular line to NL27; MD6:MLPb—lower molar height, distance between MB cusp of lower first molar on perpendicular line to ML27; MXIABHb—upper incisor length in long axis of alveolar process26; MX1:NLPb—upper incisor length on perpendicular to NL27; MDIABHb—lower incisor length in long axis of alveolar process26; MD1:MLPb—lower incisor length on perpendicular to ML27; MDADb—width of lower anterior alveolar process26; MXADb—width of upper anterior alveolar process26; ArGob—mandibular ramus length (Ar-Go); and LFHb—lower facial height (ANS-Me).
Statistical Analysis and Measurement Error
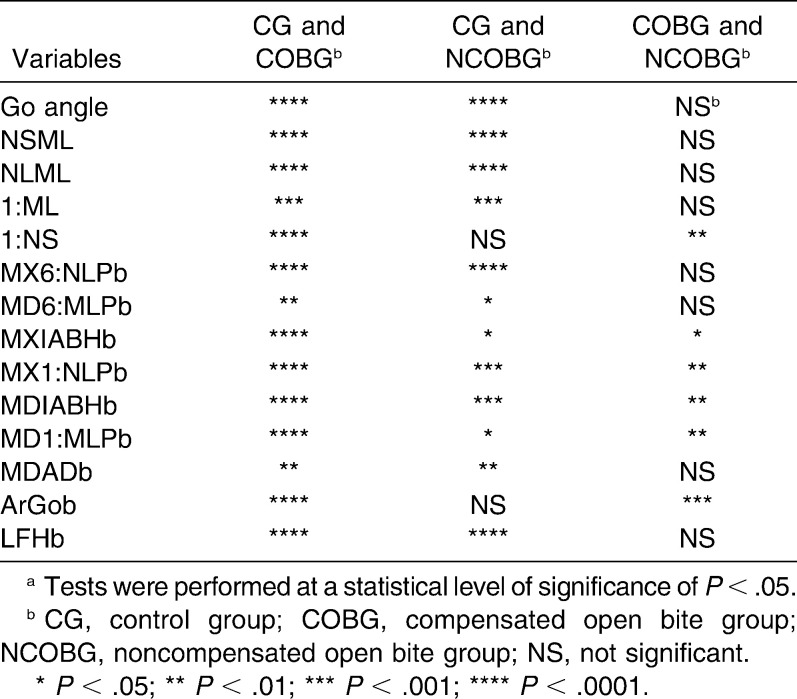
An estimate of the power of the study was performed on the basis of the effect size of a relevant variable (MX6:NLPb) at α = .05, with a sample size of 23 subjects in each group.33 The power of the study in each of the observed groups exceeded 0.90. An exploratory test (Shapiro-Wilks test) revealed normality of the distribution for all variables within each group. Therefore, parametric statistics was used. Between-group comparisons (COBG vs NCOBG vs CG) were performed using analysis of variance (ANOVA). When parameters revealed statistically significant differences, post hoc Bonferroni tests were carried out for multiple comparisons (Table 2). All tests were performed at the level of statistical significance of .05. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software package, version 15 (SPSS Inc., Chicago, Ill).
Table 2.
Significance of Intergroup Differencesa
One month after measurements were taken, the main investigator retraced 20 randomly chosen cephalograms, and the error of measurement was determined using intraclass correlation coefficients (ICCs). Correlations for repeated measurements were statistically significant for all variables at the .01 level. Correlation analysis showed the highest r value of 0.990 for lower face height (LFHb) and the lowest r value of 0.784 for the width of the anterior maxillary alveolar process (MXADb).
RESULTS
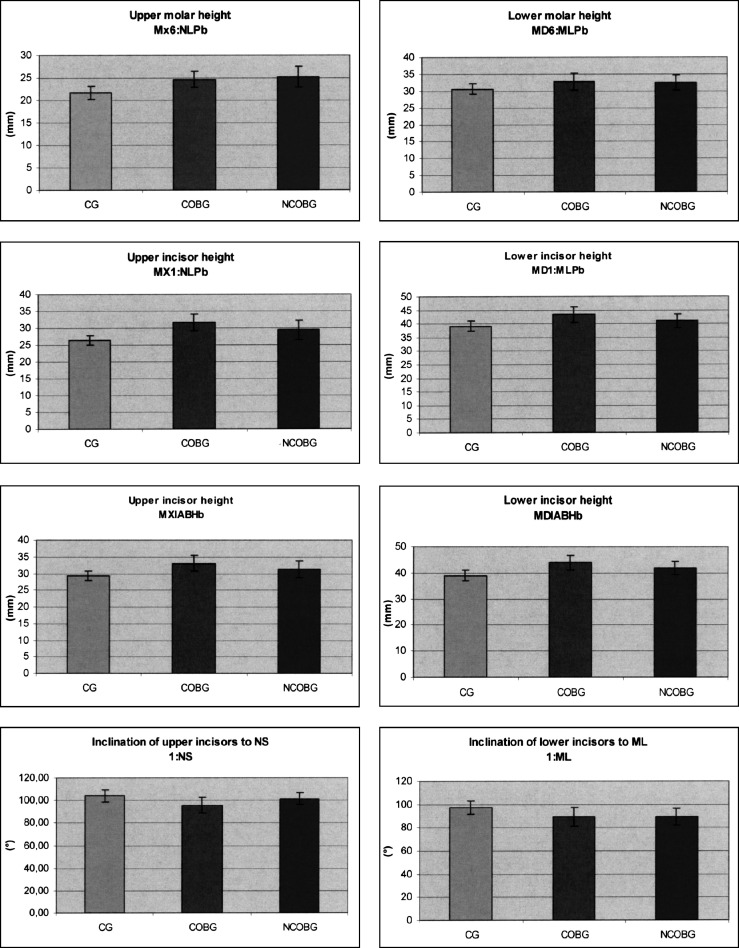
Descriptive statistics for the variables included in this study is provided in Table 1. Table 2 shows the results of between-group comparisons (Bonferroni). Results for selected dentoalveolar variables are shown in Figure 2.
Figure 2.
Graphic representation of results for selected dentoalveolar variables. Error bars represent standard deviations. CG, control group; COBG, compensated open bite group; and NCOBG, noncompensated open bite group.
Upper (MX6:NLPb) and lower (MD6:MLPb) molar heights were significantly greater in COBG and NCOBG than in CG. However, no significant difference in molar height was noted between COBG and NCOBG. Both mandibular and maxillary incisor heights were significantly greater in COBG and NCOBG than in CG. Both upper (MX1:NLPb, MXIABHb) and lower (MD1:MLPb, MDIABHb) incisor heights were significantly smaller in NCOBG than in COBG. Increased incisor height was accompanied by significant narrowing of the alveolar process in the mandibular frontal region (MDADb) in both COBG and NCOBG. The buccal inclination of the lower incisors (1:ML) was significantly smaller in COBG and NCOBG than in CG. The buccal inclination of the upper incisors (1:NS) was significantly smaller in COBG than in NCOBG. No significant difference in the inclination of the upper incisors was observed in NCOBG compared with CG.
DISCUSSION
The purpose of this study was to identify morphologic differences at the dentoalveolar level between subjects in two skeletal open bite groups with or without dental compensation (COBG, NCOBG) and a control group (CG) with normal vertical and sagittal relationships. The study sample included only female subjects in whom growth had been completed. The method of this study, therefore, respected skeletal maturation and sexual dimorphism to avoid potential bias of the results deriving from analysis of different growth phases34 or intersexual differences.27
Both upper and lower molar heights were significantly greater in COBG and NCOBG than in CG. These results confirm previous observations12–21 and demonstrate that both upper and lower molars are significantly more extruded in skeletal open bite subjects than in normal controls. From a clinical point of view, these data suggest that a primary goal of treatment for a skeletal open bite can be represented by intrusion of the upper and/or lower molar regions. Bony anchorage can be extremely useful in this regard.
We also found that in both skeletal open bite groups, the incisor regions were significantly elongated, regardless of the measurement method used. Once again, these results are consistent with those of previous studies,1,12,19–21 but they contradict those reported by Nahoum et al.,22–24 who found smaller values for incisal height in patients with open bite than in control group patients. When we evaluated incisor height along the long axis of the alveolar process, where the results are not biased by the inclination of incisors, dentoalveolar height of the mandibular incisors (MDIABHb) provided the greatest contribution to the dental compensatory process, as published previously by other authors.11,25,26 Therefore, vertical dentoalveolar compensation in skeletal open bite adult patients appears to be caused by significant elongation of both upper and lower incisors, with lower incisors playing a more important role. This confirms that excessive extrusion of incisors in open bite treatment may bring results that are neither stable nor esthetic.1 Also, in open bite patients undergoing orthognathic surgery, extrusion of the incisors is to be avoided in presurgical orthodontics to decrease the risk of dental relapse after surgery.31
Significant differences were found in the buccal inclinations of upper and lower incisors to NS and ML, along with significantly smaller values in COBG and NCOBG than in CG. In the presence of an increased mandibular plane angle, the lower incisors tended to show more pronounced lingual inclination, which is consistent with results reported by Beckmann et al.,11 Björk,15 Björk and Skieller,16 and Frost et al.19 Although NCOBG did not differ significantly from CG, significantly retroclined upper incisors were noted in COBG. This finding corresponds to results reported by Beckmann et al.11 and Kuitert et al.26 Proclination of incisors during poorly managed biomechanics can result in iatrogenic bite opening in compensated open bite patients. Outcomes related to incisor compensation in skeletal open bite subjects were corroborated by analysis of the three groups according to sagittal skeletal relationships. In fact, both COBG and NCOBG presented with a higher prevalence rate of Class II tendencies than was observed in CG. This was due to the effect of vertical skeletal relationships with skeletal open bite in facilitating the establishment of skeletal Class II relationships.13,31
Finally, the present study revealed a significant difference between both COBG and NCOBG vs CG in terms of width of the incisor alveolar process in the mandible (MDADb). Similar findings were reported by Beckmann al.11,25 and Kuitert et al.26 This difference implies that in skeletal open bite patients, the apices of the lower incisors may be located very close to the vestibular bone cortex because of the narrow morphology of the alveolar process. When high angle patients are treated, buccolingual position and inclination of the lower incisors should be altered with caution, to avoid the risk of root resorption or periodontal problems.
CONCLUSIONS
Increased molar height is a common finding in adult skeletal open bite subjects. Orthodontic treatment in these patients should be aimed primarily at limiting or correcting excessive dentoalveolar height in the upper and lower posterior regions.
Incisor height was significantly greater in dentally compensated skeletal open bite vs dentally noncompensated skeletal open bite subjects; upper incisors were significantly more retroclined in dentally compensated subjects.
A significantly narrower alveolar process was found in the incisor region of the mandible in both skeletal open bite groups. Large excursions of the lower incisors during orthodontic movement in skeletal open bite patients should be avoided to prevent the risk of root resorption and bone dehiscence.
Acknowledgments
The authors would like to thank Mgr. Katerina Langova from the Department of Medical Biophysics, Medical Faculty, Palacky University in Olomouc, Czech Republic, for kind help with statistical analysis of the data.
REFERENCES
- 1.Subtelny J. D, Sakuda M. Open-bite: diagnosis and treatment. Am J Orthod. 1964;50:337–358. [Google Scholar]
- 2.Sherwood K. H, Burch J. G, Thompson W. J. Closing anterior open bites by intruding molars with titanium miniplate anchorage. Am J Orthod Dentofacial Orthop. 2002;122:593–600. doi: 10.1067/mod.2002.128641. [DOI] [PubMed] [Google Scholar]
- 3.Sugawara J, Baik U. B, Umemori M, Takahashi I, Nagasaka H, Kawamura H, Mitani H. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthod Orthognath Surg. 2002;17:243–253. [PubMed] [Google Scholar]
- 4.Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999;115:166–174. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- 5.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 6.Park H. S, Kwon O. W, Sung J. H. Nonextraction treatment of an open bite with microscrew implants anchorage. Am J Orthod Dentofacial Orthop. 2006;130:391–402. doi: 10.1016/j.ajodo.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Erverdi N, Usumez S, Solak A. New generation open-bite treatment with zygomatic anchorage. Angle Orthod. 2006;76:519–526. doi: 10.1043/0003-3219(2006)076[0519:NGOTWZ]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74:381–390. doi: 10.1043/0003-3219(2004)074<0381:TUOSAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Kondo E, Aoba T. J. Nonsurgical and nonextraction treatment of skeletal Class III open bite: its long-term stability. Am J Orthod Dentofacial Orthop. 2000;117:267–287. doi: 10.1016/s0889-5406(00)70232-0. [DOI] [PubMed] [Google Scholar]
- 10.Kuroda S, Sugawara Y, Tamamura N, Takano-Yamamoto T. Anterior open bite with temporomandibular disorder treated with titanium screw anchorage: evaluation of morphological and functional improvement. Am J Orthod Dentofacial Orthop. 2007;131:550–560. doi: 10.1016/j.ajodo.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Beckmann S. H, Kuitert R. B, Prahl-Andersen B, Segner D, Tuinzing D. B. Alveolar and skeletal dimensions associated with overbite. Am J Orthod Dentofacial Orthop. 1998;113:443–452. [PubMed] [Google Scholar]
- 12.Schendel S. A, Eisenfeld J, Bell W. H, Epker B. N, Mishelevich D. J. The long face syndrome: vertical maxillary excess. Am J Orthod Dentofacial Orthop. 1976;70:398–408. doi: 10.1016/0002-9416(76)90112-3. [DOI] [PubMed] [Google Scholar]
- 13.Schudy F. F. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964;34:75–93. [Google Scholar]
- 14.Schudy F. F. The rotation of the mandible resulting from growth: its implications in orthodontic treatment. Angle Orthod. 1965;35:36–50. doi: 10.1043/0003-3219(1965)035<0036:TROTMR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Björk A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55:585–599. doi: 10.1016/0002-9416(69)90036-0. [DOI] [PubMed] [Google Scholar]
- 16.Björk A, Skieller V. Facial development and tooth eruption: an implant study at the age of puberty. Am J Orthod. 1972;62:339–383. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 17.Enlow D. H, Kuroda T, Lewis A. B. Intrinsic craniofacial compensations. Angle Orthod. 1971;10:271–285. doi: 10.1043/0003-3219(1971)041<0271:ICC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Cangialosi T. J. Skeletal morphologic features of anterior open bite. Am J Orthod. 1980;85:28–36. doi: 10.1016/0002-9416(84)90120-9. [DOI] [PubMed] [Google Scholar]
- 19.Frost D. E, Fonseca R. J, Turvey T. A, Hall D. J. Cephalometric diagnosis and surgical-orthodontic correction of aperthognatia. Am J Orthod. 1980;78:657–669. doi: 10.1016/0002-9416(80)90205-5. [DOI] [PubMed] [Google Scholar]
- 20.Sassouni V, Nanda S. Analysis of dentofacial vertical proportions. Am J Orthod. 1964;50:801–822. [Google Scholar]
- 21.Isaacson J. R, Isaacson R. J, Speidel M. T, Worms F. W. Extreme variation in vertical growth and associated variation in skeletal and dental relations. Angle Orthod. 1971;41:219–229. doi: 10.1043/0003-3219(1971)041<0219:EVIVFG>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Nahoum H. I. Vertical proportions: a guide for prognosis and treatment in anterior open-bite. Am J Orthod. 1977;72:128–146. doi: 10.1016/0002-9416(77)90055-0. [DOI] [PubMed] [Google Scholar]
- 23.Nahoum H. I, Horowitz S. L, Benedicto E. A. Varieties of anterior open-bite. Am J Orthod. 1972;61:486–492. doi: 10.1016/0002-9416(72)90153-4. [DOI] [PubMed] [Google Scholar]
- 24.Nahoum H. I. Anterior open-bite: a cephalometric analysis and suggested treatment procedures. Am J Orthod. 1975;67:513–520. doi: 10.1016/0002-9416(75)90297-3. [DOI] [PubMed] [Google Scholar]
- 25.Beckmann S. H, Kuitert R. B, Prahl-Andersen B, Segner D, Tuinzing D. B. Alveolar and skeletal dimensions associated with lower face height. Am J Orthod Dentofacial Orthop. 1998;113:498–506. doi: 10.1016/s0889-5406(98)70260-4. [DOI] [PubMed] [Google Scholar]
- 26.Kuitert R, Beckmann S, van Loenen M, Tuinzing B, Zentnere A. Dentoalveolar compensation in subjects with vertical skeletal dysplasia. Am J Orthod Dentofacial Orthop. 2006;129:649–657. doi: 10.1016/j.ajodo.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 27.Burstone C. J, James R. B, Legan H, Murphy G. A, Norton L. A. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269–277. [PubMed] [Google Scholar]
- 28.Sung J. H, Kwon O. H, Kyung H. M, Park K. D. Longitudinal data of craniofacial growth from lateral cephalometrics in Koreans with normal occlusion. Seoul: Jung-Won; 2001. pp. 105–152. [Google Scholar]
- 29.Wada K, Matsushita K, Shimazaki S, Miwa Y, Hasuike Y, Susami R. An evaluation of a new case analysis of a lateral cephalometric roentgenogram. J Kanazawa Med Univ. 1981;6:60–70. [Google Scholar]
- 30.Nanda R. Biomechanics and esthetic strategies in clinical orthodontics. St Louis, Mo: Elsevier; 2005. pp. 156–176. [Google Scholar]
- 31.Proffit W. R, White P. R, Sarver D. M. Contemporary treatment of dentofacial deformity. St Louis, Mo: Mosby Elsevier; 2003. pp. 464–506. [Google Scholar]
- 32.Baccetti T, Franchi L, McNamara J. A. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 33.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 34.Iseri H, Solow B. Continued eruption of maxillary incisors and first molars in girls from 9 to 25 years, studied by the implant method. Eur J Orthod. 1996;18:245–256. doi: 10.1093/ejo/18.3.245. [DOI] [PubMed] [Google Scholar]