Abstract
Ankylosed teeth in growing patients cause troublesome dentoalveolar problems and require special therapeutic care for accomplishing long-term esthetic and functional results. The various treatment modalities for ankylosed teeth include reconstruction after extraction, surgical extrusive luxation, individual segmental osteotomy or corticotomy, and alveolar distraction osteogenesis. This report describes a case of a 13-year-old boy with anterior open bite complicated by an ankylosed maxillary central incisor that was managed by corticotomy-facilitated orthodontic treatment.
Keywords: Ankylosis, Individual corticotomy, Miniscrew
INTRODUCTION
Tooth ankylosis is caused by the fusion of some portion of the root surface with the surrounding alveolar process. The permanent maxillary incisors frequently become ankylosed after periodontal ligament damage by local trauma.1,2 An ankylosed tooth in a growing child fails to erupt along with the remaining vertical growth of the alveolar process,3 causing functional and esthetic problems. Therefore, a patient with an ankylosed tooth needs several treatments for infraocclusion and alveolar bone deficiency.
Ankylosis is clinically diagnosed by tooth immobility under an applied orthodontic force.4 In the case of open bite with ankylosed teeth, correcting the open bite by orthodontic tooth movement is impossible. This report describes the case of a 13-year-old boy with anterior open bite complicated by an ankylosed maxillary central incisor that was treated by individual corticotomy and subsequent orthodontic traction.
CASE REPORT
Case Summary
The patient's chief complaint was a progressive anterior open bite. His maxillary right central incisor had been extrusively subluxated by trauma 1 year earlier. The tooth had been reconstructed by using a porcelain-fused metal crown after endodontic treatment. However, the patient worried about the continued progression of the open bite since the trauma.
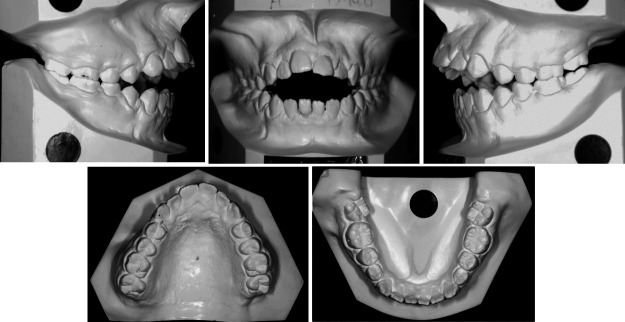
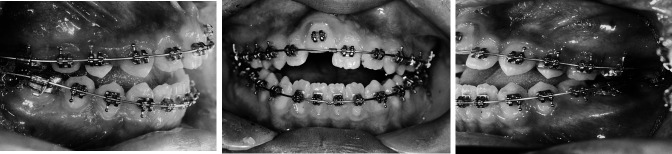
Pretreatment facial photographs showed a convex profile related to the retruded chin, incompetent lips, and mentalis hyperactivity. Maxillary incisal exposure at full smile was insufficient. Intraoral photographs showed generalized gingival swelling because of poor oral hygiene and habitual mouth breathing (Figure 1).
Figure 1.
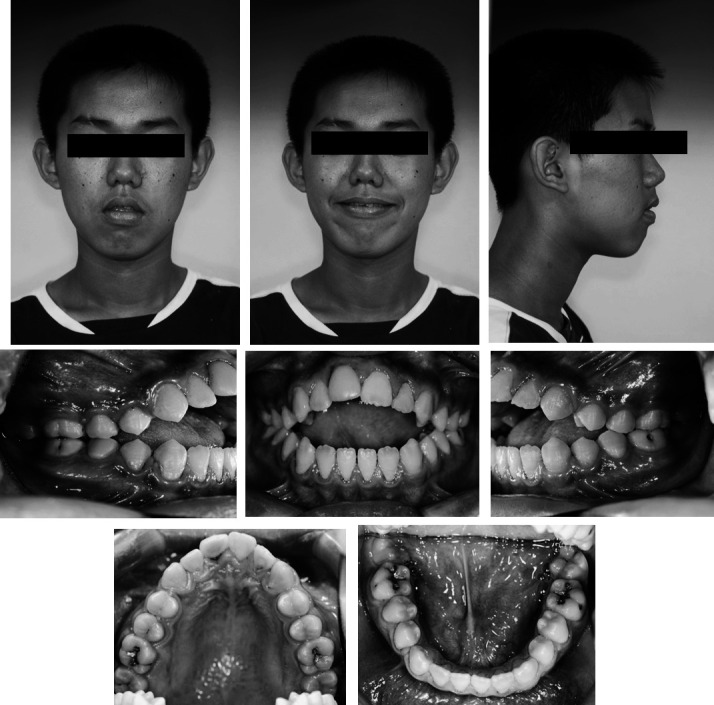
Facial and intraoral photographs at the beginning of treatment.
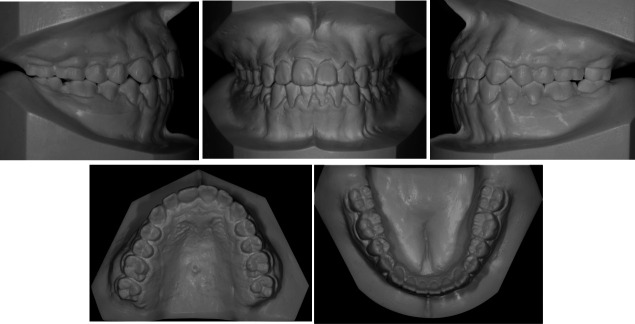
The maxillary dental arch was constricted, whereas the mandibular dental arch was broad. Both canine and molar relationships were Class II. The maxillary dental arch showed a severe curve of Spee. The mandibular dental arch showed a reverse curve of Spee and spaces among the anterior teeth due to tongue thrusting. The overjet and overbite were 9 and −12 mm, respectively (Figure 2).
Figure 2.
Pretreatment dental casts.
In the panoramic radiograph, the alveolar bone of the maxillary anterior region showed insufficient growth (Figure 3). In the standard view, the maxillary right central incisor had external root resorption (Figure 4).
Figure 3.
Pretreatment panoramic radiograph.
Figure 4.

Pretreatment periapical radiograph of the maxillary incisors.
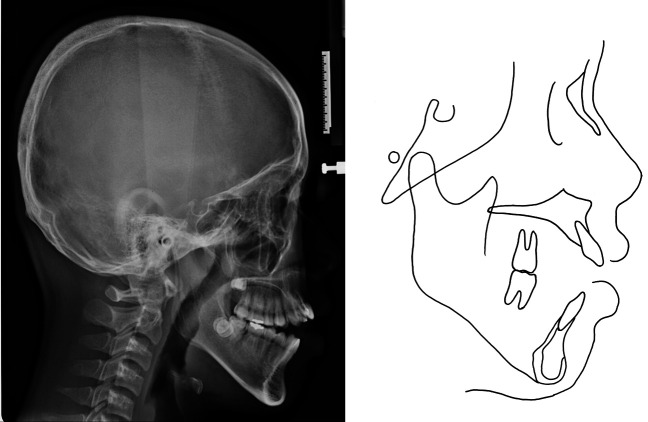
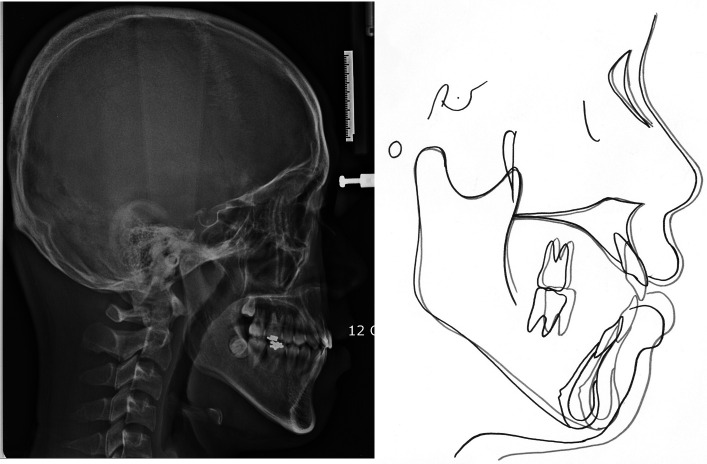
The lateral cephalometric analysis indicated a skeletal Class II jaw relationship with a hyperdivergent facial pattern. Excessive extrusion of the maxillary posterior teeth was evident (Figure 5, Table 1).
Figure 5.
Pretreatment lateral cephalogram and its tracing.
Table 1.
Cephalometric Summary
Diagnosis, Treatment Objective, and Treatment Alternatives
The case was diagnosed as a skeletal Class II malocclusion with open bite, high mandibular plane angle, and vertical maxillary excess. The maxillary right central incisor was diagnosed as potentially ankylosed because of the trauma history, inadequate alveolar bone of the maxillary anterior region, infraocclusion, and external root resorption.
The main treatment objectives were intrusion of the maxillary posterior teeth for bite closure by autorotation of the mandible, extrusion of the maxillary and mandibular anterior teeth and establishment of proper overjet and overbite with the Class I molar relationship.
Although orthognathic surgery was necessary to resolve the patient's skeletal problems, he was too young to undergo surgery. Therefore, a camouflage orthodontic treatment using a miniscrew was planned.
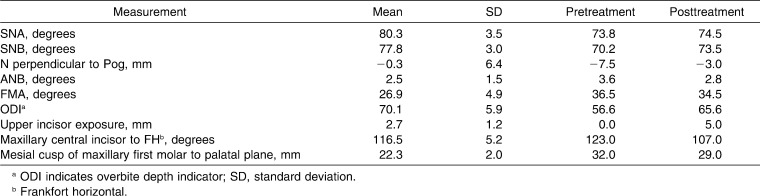
Treatment Progress
Preadjusted edgewise brackets (SmartClip, 3M Unitek, Monrovia, Calif) were placed on both dental arches. To assess the response of the maxillary right central incisor to orthodontic force, a continuous arch wire was applied preferentially on the maxillary dental arch. On the mandibular dental arch, leveling was performed by using another continuous arch wire. For intrusion of the maxillary posterior teeth, a miniscrew (Orlus, Osolution Co, Seoul, Korea) was implanted on the midpalatal suture area. The appliance (constructed of 0.9-mm stainless steel wire) connected all the posterior teeth as one unit. A constant intrusive force was applied by NiTi coil springs (Ni-Ti extension spring, Ormco, Orange, Calif) (Figure 6). The maxillary canines and premolars intruded toward the maxillary right central incisor in 3 months (Figure 7), confirming that this incisor was ankylosed. Leveling progressed without ankylosed tooth (Figure 8).
Figure 6.
Continuous arch wires were placed on both arches and intrusive force was applied palatally on the maxillary posterior teeth.
Figure 7.
The open bite worsened after 3 months of intrusive force applied on the teeth adjacent to the maxillary right central incisor.
Figure 8.
After the ankylosed maxillary right central incisor was bypassed, leveling progressed.
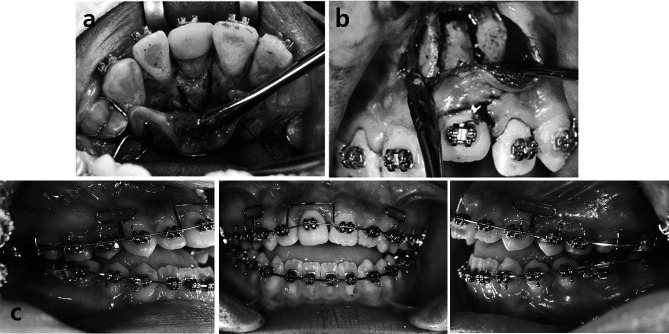
When the distance between the ankylosed tooth and the adjacent teeth was 4 mm, individual corticotomy was performed on the palatal side under local anesthesia (Figure 9a). Three weeks later, when a callus formed at the surgical site, individual corticotomy was repeated on the buccal side (Figure 9b). After a latency period of 2 days, a 0.016-inch superelastic NiTi wire (Sentalloy, Tomy, Tokyo, Japan) was overlaid on the maxillary right central incisor for extrusion while continuously intruding the maxillary posterior teeth. Two weeks later, the ankylosed incisor extruded to the level of the adjacent teeth (Figure 9c). Multiloop edgewise arch wire (MEAW) and anterior elastics were used for extruding the maxillary anterior teeth, and continuous intrusive force was applied on the maxillary posterior teeth (Figure 10). After 5 months, the open bite was corrected, and the intraoral appliance was removed that connected the maxillary posterior teeth (Figure 11).
Figure 9.
Individual corticotomy of the ankylosed maxillary right central incisor was performed twice. Two days after the surgery, a 0.016-inch NiTi wire was overlaid. (a) Individual corticotomy on the palatal side, (b) Individual corticotomy on the buccal side after callus formation (in three weeks), (c) Ankylosed tooth extruded after two weeks.
Figure 10.
MEAW and anterior elastics were used for extruding the maxillary anterior teeth.
Figure 11.
The open bite was corrected 5 months after the corticotomy.
At the finishing and detailing stage, intrusion of the maxillary posterior teeth and extrusion of the mandibular anterior teeth were planned to obtain a deeper overbite. Because the rigid intraoral appliance was removed to avoid decreasing the maxillary dental arch dimension and to avoid root torque on the maxillary posterior teeth, the intrusive forces were applied from both the palatal and the buccal sides. Although placement of additional miniscrews were planned in the maxillary posterior regions, the procedure failed and additional intrusion of the posterior teeth was not achieved. The mandibular anterior teeth were extruded using box elastics anteriorly. When a sufficient deep overbite was achieved, debonding was performed.
Treatment Results
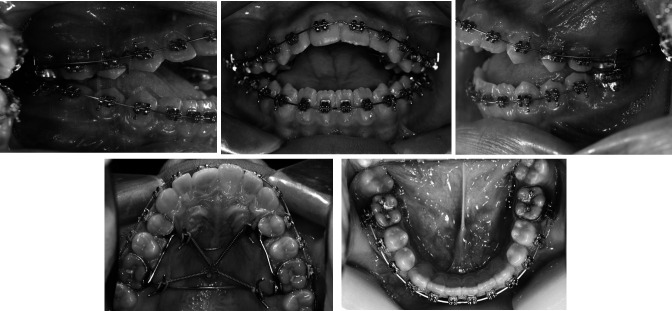
Incisal exposure while smiling increased after extrusion of the maxillary anterior teeth. Further, Class I canine and molar relationships with proper overjet and overbite were achieved (Figures 12 and 13). Good root parallelism was observed on the posttreatment panoramic radiograph, with little root resorption of the intruded molars and extruded incisors (Figure 14). Cephalometric superimposition showed the counterclockwise rotated mandible by intrusion of the maxillary molar teeth. As the mandible moved forward, the sella-nasion-point B (SNB) angle, N perpendicular to Pog, and Frankfort Horizontal to mandibular plane angle (FMA) decreased (Figure 15).
Figure 12.

Posttreatment facial and intraoral photographs. Note the increased incisal exposure.
Figure 13.
Posttreatment dental casts.
Figure 14.
Posttreatment panoramic radiograph.
Figure 15.
Posttreatment lateral cephalogram and its tracing and superimposition.
DISCUSSION
Ankylosis can be diagnosed clinically by the typical metallic sound, lack of normal mobility, radiographic absence of the periodontal space, and dental infraocclusion. However, percussion and radiographs are not reliable because only a third of the reported patients exhibited a metallic sound and only a third of the patients demonstrated loss of the periodontal space radiographically.5 Therefore, accurate diagnosis is possible only through the orthodontic force application. The present patient had a trauma history, infraocclusion, and external resorption of the maxillary right central incisor radiographically. According to these findings, the tooth was potentially diagnosed as an ankylosed tooth. To confirm the diagnosis, an orthodontic force was applied on the tooth for 3 months. The tooth's immobility despite the orthodontic force (Figure 7) confirmed that it was ankylosed.
A decision was made to correct the open bite as early as possible for several reasons. First, the alveolar bone in the maxillary anterior region showed insufficient growth because of the ankylosed tooth despite the remaining growth potential. These circumstances worsen a negative overbite. The patient was only 13 years old at the first visit. With growth, the tooth might become totally embedded in bone. Lim et al.6 reported several interventions for treating an ankylosed mandibular molar over 11 years. Although several interventions are possible, open bite complicated by an ankylosed tooth should be corrected early if the patient's growth potential remains. Second, open bite is detrimental to the temporomandibular joint (TMJ). Birgit et al.7 reported that temporomandibular disorders are associated with anterior open bite. In patients with open bite, the function of the TMJ for mandibular movement is restricted.8 Moreover, without anterior guidance, harmful forces affect the molars, which could result in dental wear and periodontal disease.
Once ankylosis is diagnosed in children and adolescents, immediate extraction is necessary to avoid complications. Lack of sufficient alveolar bone may compromise future prosthetic solutions and necessitate complex regenerative procedures to provide sufficient bone and soft tissue for enabling an esthetic solution with an implant.9 However, extraction should be decided carefully because of its irreversibility. Early extraction of an ankylosed tooth may damage the alveolar bone. Decoronation is an alternative treatment protocol to preserve the surrounding alveolar bone and prevent infraocclusion.10 However, to preserve the ankylosed tooth in the present case, distraction of the tooth by orthodontic treatment was selected.
There are several surgical treatment protocols to extrude an ankylosed tooth, such as single tooth osteotomy, surgical luxation, and distraction osteogenesis (DO). Single tooth osteotomy allows rapid movement of a tooth or teeth in a bony block, and is a feasible procedure for ankylosed maxillary teeth because of favorable vascularity in the maxilla.11 When single tooth osteotomy is undertaken, it is important to keep the soft tissue pedicle attached to the cortices, especially the labial pedicle.12 If the amount of movement of the bony block is large, the surgical procedure must be performed carefully to avoid stretching of the limited soft tissue and subsequent dehiscence. Surgical luxation involves an attempt to break the fusion between the cementum and the bone, leading to the possibility of loss of vitality and root fracture. After this procedure, orthodontic force must be applied immediately because ankylosis reoccurs as the luxation is repaired.
DO reportedly extrudes ankylosed teeth.3,13 As the bony block is gradually distracted, the attached soft tissue can regenerate along with the transported bony segment. Recently, Isaacson et al.14 reported the extrusion of an ankylosed tooth by using a standard orthodontic appliance after osteotomy. Both corticotomy and osteotomy are used to fracture bone for DO. Hu et al.15 reported greater amount of bone formation and earlier mineralization on the corticotomy side than on the osteotomy side. This result can be explained by the fact that corticotomy maintains the integrity of the endosteum, bone marrow, and capillary networks. The ankylosed tooth in the present case was managed by individual corticotomy to induce earlier bone regeneration and better bone remodeling. The corticotomy was performed in two phases because of two possible problems: bony segment fracture and lack of blood supply. If corticotomy was performed on the palatal and buccal cortical plates simultaneously, the bony segment could have fractured or undergone necrosis due to inadequate blood supply. Therefore, corticotomy was first performed on the palatal side, which has a thicker cortical plate than that on the buccal side. The latency period (2 weeks) for callus formation on the palatal side was necessary to obtain sufficient mechanical support and to sustain the bony segment.
There are some biomechanical considerations for molar intrusion with a miniscrew. The implantation area is determined depending on the safety and efficiency of tooth movement. Miniscrews implanted on the buccal side might have failed because of the patient's young age and poor oral hygiene. The midpalatal area is composed of good-quality cortical bone16 and overlaid by thin keratinized soft tissue17; therefore, a miniscrew was implanted in this area. However, when intrusive forces are applied through a miniscrew on the midpalatal suture, the transverse dimension of the posterior teeth diminishes and buccal root torque develops on these teeth (Figure 16). To avoid these complications, the rigid intraoral appliance constructed of 0.9-mm stainless steel wire was inserted. At the final stage of treatment, when the intraoral appliance was removed, miniscrews were implanted on the buccal side to apply intrusive forces on both sides and avoid the possible problems, but in vain.
Figure 16.
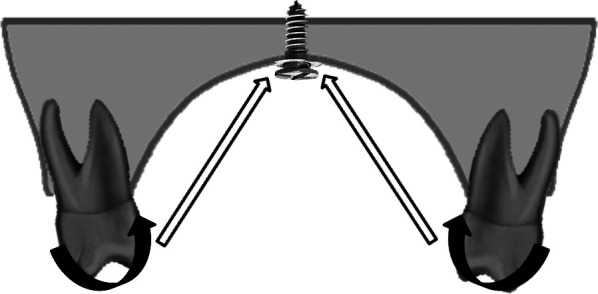
Intrusive forces from the midpalatal suture cause root buccal torque and decrease in the transverse dimension.
This case has a high possibility of relapse. To correct the patient's open bite, the maxillary posterior teeth were intruded. However, intruded molars tend to rebound. Sugawara et al.18 reported the average relapse rate of maxillary intruded molars as 30.3%. After the correction of open bite, the patient's overbite was carefully monitored for 6 months without any intrusive force. Infraocclusion of the treated tooth will recur because of the remaining growth potential. Therefore, the prognosis should be monitored until the patient grows up. If the relapse occurs, additional orthodontic or prosthodontic treatment may be necessary.
CONCLUSIONS
The present patient had open bite induced by complex etiologies such as a hyperdivergent skeletal pattern, an ankylosed tooth, and abnormal habits (tongue thrusting and mouth breathing). Therefore, various factors had to be considered while treating the patient.
Both tooth ankylosis and skeletal open bite are difficult to treat and the results are uncertain.
Individual corticotomy and miniscrew application enhance the efficiency of treatment for open bite and tooth ankylosis.
REFERENCES
- 1.Andreasen J. O, Andreasen F. M. Essentials of Traumatic Injuries to the Teeth. Copenhagen, Denmark: Munksgaard; 1991. pp. 103–131. [Google Scholar]
- 2.Andreasen J. O, Andreasen F. M. Textbook and Color Atlas of Traumatic Injuries to the Tooth 3rd ed. Copenhagen, Denmark: Munksgaard; 1994. pp. 587–633. [Google Scholar]
- 3.Kofod T, Würtz V, Melsen B. Treatment of an ankylosed central incisor by using tooth dento-osseous osteotomy and a simple distraction device. Am J Orthod Dentofacial Orthop. 2005;127:72–80. doi: 10.1016/j.ajodo.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Vanarsdall R. L. Complications of orthodontic treatment. Curr Opin Dent. 1991;1:622–633. [PubMed] [Google Scholar]
- 5.Raghoebar G. M, Boering A, Jansen H. W, Vissink A. Secondary retention of permanent molars: a histologic study. J Oral Pathol Med. 1989;18:427–431. doi: 10.1111/j.1600-0714.1989.tb01338.x. [DOI] [PubMed] [Google Scholar]
- 6.Lim W. H, Kim H. J, Chun Y. S. Treatment of ankylosed mandibular first permanent molar. Am J Orthod Dentofacial Orthop. 2008;133:95–101. doi: 10.1016/j.ajodo.2006.03.032. [DOI] [PubMed] [Google Scholar]
- 7.Birgit T, Guillermo R, Lucia P, Clara M. Prevalence of temporomandibular dysfunction and its association with malocclusion in children and adolescents: an epidemiologic study related to specified stages of dental development. Angle Orthod. 2002;72:146–154. doi: 10.1043/0003-3219(2002)072<0146:POTDAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Koak J. Y, Kim K. N, Heo S. J. A study on the mandibular movement of anterior openbite patients. J Oral Rehabil. 2000;27:817–822. doi: 10.1046/j.1365-2842.2000.00655.x. [DOI] [PubMed] [Google Scholar]
- 9.Shabtai S, Joseph S. Decoronation for the management of an ankylosed young permanent tooth. Dent Traumatol. 2008;24:131–135. doi: 10.1111/j.1600-9657.2006.00506.x. [DOI] [PubMed] [Google Scholar]
- 10.Malmgren B, Cvek M, Lundberg M, Frykholm A. Surgical treatment of ankylosed and infrapositioned reimplanted incisors in adolescents. Scand J Dent Res. 1984;92:391–399. doi: 10.1111/j.1600-0722.1984.tb00907.x. [DOI] [PubMed] [Google Scholar]
- 11.Im D. H, Nahm D. S, Chang Y. I. The treatment of an ankylosed canine: luxation and forced eruption. Korean J Orthod. 2002;32:395–400. [Google Scholar]
- 12.Bell W. H, Proffit W. R, White R. P, editors. Surgical Correction of Dentofacial Deformities. Philadelphia, Pa: WB Saunders; 1980. pp. 234–441. [Google Scholar]
- 13.Kinzinger G. S. M, Jänicke S, Riediger D, Diedrich P. R. Orthodontic fine adjustment after vertical callus distraction of an ankylosed incisor using the floating bone concept. Am J Orthod Dentofacial Orthop. 2003;124:582–590. doi: 10.1016/s0889-5406(03)00569-9. [DOI] [PubMed] [Google Scholar]
- 14.Isaacson R. J, Strauss R. A, Bridges-Poquis A, Peluso A. R, Lindauer S. J. Moving an ankylosed central incisor using orthodontics, surgery and distraction osteogenesis. Angle Orthod. 2001;71:411–418. doi: 10.1043/0003-3219(2001)071<0411:MAACIU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Hu J, Li J, Wang D, Buckley M. J, Agarwal S. Differences in mandibular distraction osteogenesis after corticotomy and osteotomy. Int J Oral Maxillofac Surg. 2002;31:185–198. doi: 10.1054/ijom.2001.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee J. S, Kim D. H, Park Y. C, Kyung S. H, Kim T. K. The efficient use of midpalatal miniscrew implants. Angle Orthod. 2004;74:711–714. doi: 10.1043/0003-3219(2004)074<0711:TEUOMM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Kim H. J, Yun H. S, Park H. D, Kim D. H, Park Y. C. Soft-tissue and cortical bone thickness at orthodontic implant sites. Am J Orthod Dentofacial Orthop. 2006;130:177–182. doi: 10.1016/j.ajodo.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Sugawara J, Baek U. B, Umemori M, Takahashi I, Nagasaki H, Kawamura H, Mitani H. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthodon Orthognath Surg. 2002;17:243–253. [PubMed] [Google Scholar]