Abstract
Environmental disasters, pandemics, and other major traumatic events such as the Covid-19 pandemic or war contribute to psychosocial stress which manifests in a wide range of mental and physical consequences. The increasing frequency and severity of such events suggest that the adverse effects of toxic stress are likely to become more widespread and pervasive in the future. The allostatic load (AL) model has important elements that lend themselves well for identifying adverse health effects of disasters. Here we examine several articulations of AL from the standpoint of using AL to gauge short- and long-term health effects of disasters and to provide predictive capacity that would enable mitigation or prevention of some disaster-related health consequences. We developed a transdisciplinary framework combining indices of psychosocial AL and physiological AL to produce a robust estimate of overall AL in people affected by disasters and other traumatic events. In conclusion, we urge researchers to consider the potential of using AL as a component in a proposed disaster-oriented human health observing system.
Keywords: Allostatic load, Disasters, Pandemic, Health observing system, COVID-19, Cohort studies
1. Introduction
Occurrences of natural and climate-related environmental disasters have risen markedly since the mid-20th century, with devastating costs to both human well-being and economic functioning (Learning and Guha-Sapir, 2013, EMDAT, 2020). In 2020, the United States (US) experienced the highest recorded number of billion-dollar environmental disasters with a total of 22 events, and 20 occurred in 2021 (NOAA, 2022). This continues a 7-year trend of > 10 such occurrences per year following previous records of 16 in 2011 and 2017. Overall, since 1980, the US has experienced 310 weather- or climate-related disasters which caused > $1 B in CPI-adjusted damage costs. Years with > 10 such events include 1998, 2008, 2011–2013, and 2015–2021 (NOAA, 2022).
Both the US and Europe experienced major storms, floods, and wildfires in 2021 (CRED (Centre for Research on the Epidemiology of Distasters), 2021, Kaplan and Tran, 2021). Globally, the occurrence of natural disasters, especially associated with climate change, have increased 1.7-fold in the decade 2000–2019 compared to the previous decade (rising from 4212 to 7348). This increase was associated with 1.23 million deaths, over 4.0 billion people affected – sometimes by more than one disaster event – and estimated economic losses of $US 3 trillion (CRED Centre for Research on the Epidemiology of Distasters, 2020). However, global disaster-associated mortality rates have declined markedly over time, likely in part due to enhanced pre-disaster warnings and preparedness efforts.
Regardless of scale, disasters result in high levels of stress, which is perhaps the most pervasive, pernicious, and persistent adverse health impact of disasters. This distress negatively affects the mental and physical health of individuals and the well-being of entire communities (Sandifer and Walker, 2018; Sandifer et al., 2017; Chandra et al., 2018; Saxbe et al., 2019). The concept of stress permeates our culture at multiple levels and is viewed as consequential to disasters of all varieties. In normal parlance, stress indicates a demanding, sometimes overwhelming, state, accompanied by negative emotions and feelings of inability to cope (McEwen, 2006). However, most disaster preparedness and response plans, policies, and programs in the US and elsewhere do not include a central focus on stress and its numerous negative health consequences (Sandifer and Walker, 2018).
Another widespread concern is the lack of sufficient baseline health information against which to compare short- and especially long- term health outcomes and allostatic load following environmental disasters (Goldstein et al., 2011, Colwell and Machlis, 2019; Parker et. al., 2020; Sandifer et al., 2020a). Among others, these include major storms, floods, wildfires, earthquakes, industrial accidents, climate change, along with environmental exposures to large blooms of harmful algae, floodwaters containing infectious organisms and toxic pollutants, mold in previously flooded structures, and the COVID-19 pandemic. Recognition of this critical information gap in the disaster-prone US Gulf of Mexico region led to development of a framework for a comprehensive Community Health Observing System for that region which could also serve as a model for other health observing systems elsewhere (Sandifer et al., 2020a, Sandifer et al., 2020b).
The Community Health Observing System framework builds on national-level cross-sectional and longitudinal studies in the US. If implemented, this health observing system would add disaster-focused longitudinal cohort studies in the vulnerable coastal areas of the Gulf of Mexico states. Key components of the proposed cohort studies are the collection of biomarkers and other indicators of cumulative stress and health outcomes. While this framework was initiated in response to the massive Deepwater Horizon (DWH) oil spill of 2010, the intent is that the design could be adapted readily to many different types of disasters, including economic catastrophes and pandemics (Sandifer, 2022). A core intent from initiation of the Community Health Observing System framework development was inclusion of allostatic load (AL) as a key metric of disaster-associated health consequences, and we suggest that AL be considered for any health surveillance system implemented for disasters.
2. Characterizing allostatic load
2.1. Value of allostatic load model
The AL model connects cumulative stress with morbidity and mortality (McEwen and Stellar, 1993, Seeman et al., 1997, McEwen, 1998, McEwen, 2000). The value of AL is its use to unravel some of the complex mechanisms by which psychological stress impacts physical health and mental well-being. This utility has been demonstrated many times over the last ~25 years (e.g., see reviews by Juster et al., 2010, Juster et al., 2011; Beckie, 2012; Chandra et al., 2018; Koob and Schulkin, 2019; Guidi et al., 2020). More recently, the AL framework was used to identify effects of stress caused by the COVID-19 pandemic (Peng et al., 2021).
2.2. Assessing allostatic load
Cross-sectional scoring schemes designed to measure multi-system dysregulation as an index of AL have been widely utilized since their initial specification by Seeman et al. (1997) (see reviews by Juster et al., 2010, Juster et al., 2011; Lupien et al., 2015; and others). Typically, AL is assessed via calculation of an index based on a suite of biomarkers. A wide variety of biomarkers has been used for this purpose (Beckie, 2012, Juster et al., 2011, Johnson et al., 2017). Typically, a much smaller subset is selected based primarily on availability in an existing database or ongoing study and/or as perceived or expected utility in identifying negative health outcomes. This approach has led to some controversy regarding the heterogeneity of approaches that deviate from the original concept of AL and relate to inconsistencies in choice and use of biomarkers, determination of biomarker thresholds, and calculation of indices with and without weighting (Beckie, 2012, Gallo et al., 2014, Johnson et al., 2017). Gallo et al. (2014) and Epel et al. (2018) highlighted the lack of a clearly defined and widely accepted “gold standard” for determining AL and standardizing it for comparison across settings and studies.
2.3. Alternative operationalizations of allostatic load
Despite the intuitive nature of cumulative physiological dysregulation over time as a central component of AL, it has rarely been operationalized beyond the count-based approach first developed by Seeman et al. (1997). A notable exception has been the work of Yashin and colleagues which has not been adopted widely (Yashin et al., 2012, Arbeev et al., 2016). In addition, and while not referred to as AL, the considerable literature on frailty indices and their dynamics in elderly populations (Rockwood and Mitnitski, 2007, Farrell et al., 2016, Taneja et al., 2016) may be interpretable as an approach to operationalization of AL beyond strict use of biomarkers. Extension of the frailty literature to younger ages is an important research topic that could enhance the AL discussion and time-course of physiological dysregulations.
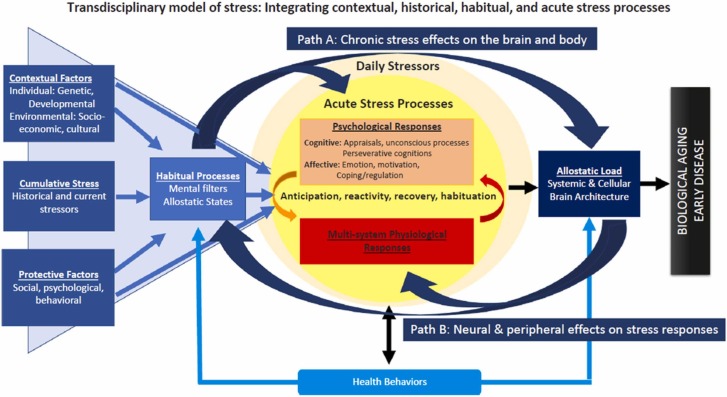
Epel et al. (2018) recommend adoption of a stress effects model that “incorporates epidemiological, affective, and psychophysiological perspectives.” They propose a comprehensive life course model that includes contextual factors (e.g., genetics; development; environmental, cultural, and social factors; past stress exposures and illness; current and cumulative stress exposures) and protective factors (e.g., supportive family, social, psychological, and behavioral characteristics; habitual processes of pessimism or optimism; and psychological and physiological processes and responses) ( Fig. 1). An accompanying stress typology encompasses stressor exposure characteristics, such as timescale (e.g., acute, daily hassles, major life events, chronic); life period of occurrence (in utero, childhood, adulthood); when, where, duration, and target of event (individual, family, community); how effects are assessed; and psychological, behavioral, and physiological responses and measurements. Although Epel et al. (2018) do not present a quantitative formulation of their model, much if not all the information they recommend be considered could be included in AL assessments as described later in this paper.
Fig. 1.
Transdisciplinary model that describes “stress” as a set of interactive and emergent processes. The figure illustrates that stressors are experienced within the context of a person’s life, represented by the contextual factors in the blue triangle. These contextual factors include individual-level characteristics such as personality and demographic factors, the environment in which one lives, current and past stressor exposures, and protective factors. Collectively, all factors combine to determine the baseline allostatic state of physiological regulation, and the lens through which stressors are perceived and assigned meaning. Contextual factors and habitual processes together influence psychological and physiological responses to acute and daily stressors. These responses, if dysregulated, are thought to lead to allostatic load and ultimately biological aging and early disease (from Epel et al., 2018, used with permission).
2.4. Incorporating psychosocial measures of allostatic load
While most of the extant AL reports are based on physiological biomarkers, a particularly salient point is the need to better integrate psychosocial measures with physiological indicators of stress, and with consideration of individual, community, and environmental factors, such as those listed by Epel et al. (2018) as co-variants, moderators, and/or mediators. Specific tools developed to screen for psychosocial AL are the Psychosocial Index presented by Piolanti et al. (2016) and the Diagnostic Criteria for Psychosomatic Research offered by Fava et al. (2019) and Guidi et al. (2020). The Psychosocial Index is based on self-ranked responses to a 55-element questionnaire that can be applied in a clinical situation to assess psychosocial AL. While possible to use in a disaster setting, it may be somewhat difficult to incorporate with collection of biophysical data due to its length. The Diagnostic Criteria for Psychosomatic Research is a shorter and more targeted index that is based on the Psychosocial Index (Fava et al., 2019) and that focuses specifically on a causative stressor event(s), e.g., an environmental disaster or other definable trauma. The psychosocial AL index derived from the Diagnostic Criteria for Psychosomatic Research is determined by responses to a two-part questionnaire, with Criterion A focusing on precipitating events and traumas (the primary recent stressor or stressors of note) and Criteria B targeting psychosocial impacts on individuals and their lives. Answers affirming significant effects related to both sets of Criteria would result in a diagnosis of psychosocial AL ( Table 1, Table 2).
Table 1.
Diagnostic interview for determination of psychosocial allostatic load (PsyAL) (modified slightly from Table 2 in Fava et al., 2019) with minor wording changes and explicit inclusion of disasters).
| Psychosocial Allostatic Load | |||
|---|---|---|---|
| Criteria | Questions | Response | |
| Criterion A. The presence of at least 1 current identifiable source of distress in the form of recent life events and/or chronic stress. Considering the full nature and circumstances of the stressor(s), do you judge it/them to have taxed or exceeded your ability to cope? | A.1 In the last 12 months | Yes | No |
| |||
| A.2. Have you felt that life is asking too much of you? | |||
| Criterion B. The stressor is associated with 1 or more of the following features, which have occurred within 6 months of onset of the stressor: at least 2 of the following symptoms: difficulty falling asleep, restless sleep, early morning awakening, lack of energy, dizziness, generalized anxiety, irritability, sadness, demoralization | B.1. Within 6 months of onset of (NAME OF THE STRESSOR) | ||
| |||
| Significant impairment in social/occupational functioning | B.2. Did you have problems or difficulties at work, at home, or in relationships with other people? | ||
| Significant impairment in environmental mastery (feeling overwhelmed by the demands of everyday life) | B.3. Did you feel overwhelmed by the demands of everyday life? |
Diagnosis of Psychosocial Allostatic Load (PsyAL): A1 = Yes + A2 = Yes + B1 and/or B2 and/or B3 = Yes = PsyAL.
Table 2.
Clinical criteria for allostatic overload (A through B are required) (from Fava et al., 2019).
| Criterion A The presence of a current identifiable source of distress in the form of recent life events and/or chronic stress; the stressor is judged to tax or exceed the individual coping skills when its full nature and circumstances are evaluated |
| Criterion B The stressor is associated with one or more of the following features, which have occurred within 6 months after the onset of the stressor: |
|
3. Predisposing, mediating, and compounding factors
The long history of socioeconomic and racial disparities in health care, along with globally-impactful, slow-moving disasters such as climate change and now the COVID-19 pandemic, as well as more acute and periodic catastrophic events such as hurricanes, floods, wildfires, and others, will continue to lead to negative health outcomes in society at large and especially among marginalized groups. High AL is regularly correlated with all-cause mortality (Seeman et al., 2001, Gruenewald et al., 2006, Borrell et al., 2010, Howard and Sparks, 2016, Robertson et al., 2017, Castagne et al., 2018), individual disorders such as cardiovascular disease (Cohen et al., 2007, Cadar et al., 2018), and in relation to socioeconomic position (Johnson et al., 2017). It is now also associated with global climate change (Crews et al., 2019). Higher AL scores are often encountered among minorities and in low-wealth communities (Johnson et al., 2017, Borrell et al., 2020). These communities frequently bear the brunt of catastrophic events including the COVID-19 pandemic (Lopez et al., 2021) and climate change (USGCRP, 2018, Dietz et al., 2020). People in such communities who already experience higher AL levels “can reasonably be expected to have an impaired immune response to novel pathogens such as SARS-CoV-2″ (Dasco et al., 2020). Increased exposures to harmful algal blooms and their toxins, oil spills, and other injurious substances and circumstances can be expected to add to individuals’ stress levels and hence to AL, particularly in coastal communities (Sandifer, 2022). Substantial evidence shows that a variety of influencing factors may be associated with AL (see in particular, Epel et al., 2018 and Table 3), but much remains to be done to understand the interactions between and among these factors, and how they may exacerbate or mitigate AL and its consequent mental and physical disorders.
Table 3.
A partial list of preexisting influencing factors and challenges that may affect the development and manifestations of psychosocial and physiological allostatic load (informed by Beckie, 2012; Johnson et al., 2017; Sandifer et al., 2020b; Epel et al., 2018; Christensen et al., 2019; Fava et al., 2019; Milad and Bogg, 2020; White et al., 2020; Obeng-Gyasi et al., 2021). This list is intended to be illustrative and is not exhaustive.
| Behavioral Factors | Genetics |
|---|---|
| Diet | Family disease history |
| Smoking | Known genetic issues (e.g., BRCA gene for breast cancer |
| Alcohol/drug use | Personality Traits |
| Physical exercise | Type A vs Type B personality |
| Sleep Habits | Agreeableness |
| Biographical/Demographic Factors | Conscientiousness |
| Age | Extraversion |
| Sex/Gender/Preference | Neuroticism |
| Marital/partner status | Openness |
| Children | Psychosocial Factors |
| Socioeconomic & Educational status (SEES) | Anxiety, including illness anxiety |
| Employment status | Depression |
| Occupation | Optimism |
| Work environment | Pessimism |
| Income | Anger/hostility |
| Childhood Experiences | Coping |
| Adverse childhood experiences (ACES) | Self-mastery |
| Economic, social, or other deprivation | Sense of control |
| Clinical Factors | Resilience |
| Chronic disease (e.g., CVD, diabetes, cancer) | Loneliness/isolation |
| Treatment | Feelings of security/insecurity |
| Medications | Quality of life |
| Medical Procedures | |
| Environmental Factors | Stress/Trauma History |
| Neighborhood characteristics (including “green” and “blue” spaces) | Previous highly stressful events, times of occurrence, duration, time course |
| Social and familial support | Current major stressors |
| Cultural and/or religious aspects | Chronic stress (e.g., from care giving, job) |
| Health care | |
| Housing status | |
| Exposure to toxic or disease-causing substances or organisms |
4. Allostatic load in the context of disasters, traumas, and pandemics
4.1. Using AL for disaster-health impact studies
While a fully developed theoretical foundation remains to be formulated for AL, we know enough to use AL to predict the likelihood of negative stress-associated health outcomes and begin to assess effects of disasters on the trajectory of AL and its health implications for individuals, groups, and communities. Here, we take a pragmatic approach, one focused on potentially useful diagnostic/predictive methods for harmful stress responses in the context of disasters and other traumatic events, including the present COVID-19 pandemic and its social and economic disrupting effects.
Notwithstanding the widely recognized association of stress with disasters, relatively little work has been done to incorporate objective measures of physiological stress such as AL in disaster-related health studies. McEwen (2005) noted “[I]f the additional load of unpredictable events in the environment (e.g., storms, natural disasters), disease outbreaks [emphasis added], disturbances caused by humans and antagonistic social interactions is superimposed, then AL can increase dramatically to become allostatic overload. Allostatic overload serves no useful purpose and predisposes the individual to disease.” McEwen and Tucker, 2011a, McEwen and Tucker, 2011b suggested that AL could be useful in evaluating risks associated with exposure to toxic chemicals, particularly chronic exposure via contaminated sites, and termed such situations technological disasters.
There are other interjections of AL into disaster discussions, but usually these follow a particular event and are related to a specific health outcome such as heart attacks (Kario et al., 2003). Recent recommendations include incorporating AL in evaluating disaster-related human health effects associated with degradation of ecosystem services and making stress and AL a key focus of future disaster-related health research (Sandifer and Walker, 2018). The COVID-19 pandemic provides a heretofore unprecedented opportunity to assess the impact of similar stressful experiences on populations all over the world, which are operating under diverse political, social, and economic conditions. Stress impacts are perhaps most apparent in the psychosocial effects of the pandemic. Some researchers are now forecasting widespread mental and behavioral disorders associated with the COVID-19 pandemic and its stress, with estimates as high as 10% of the global population being affected (Galea et al., 2020, Soloveva et al., 2020, Breslau et al., 2021).
4.2. Harnessing allostatic load for disaster response
Although some AL studies have involved longitudinal cohorts, many have not. This is surprising in light of the numerous times that the need for dedicated prospective longitudinal studies to advance AL has been identified (Beckie, 2012, Buckwalter et al., 2015, Castagne et al., 2018, Epel et al., 2018, Fernandez et al., 2015, Gallo et al., 2014, Howard and Sparks, 2016, Juster et al., 2011, Mauss et al., 2016, Piazza et al., 2010, Picard and McEwen, 2018a, Picard and McEwen, 2018b, Seeman et al., 2001, Solis et al., 2016). Also, most AL research to date does not include psychosocial data in calculation of an AL index or as a complement to physiological AL formulations.
The potential to operationalize AL for use in disaster-health studies was discussed extensively at an expert workshop convened for the express purpose of evaluating options for operationalizing AL (see Sandifer et al., 2020b and acknowledgments for details). Some of the discussion revolved around the possibility of developing a short form of AL or “AL light” for use in disaster contexts. Since a comprehensive measure of multiple neuroendocrine, immune/inflammatory, metabolic, and cardiovascular parameters is costly, a simplified “AL light” could lend itself well to field research. Ideas for an abbreviated formula for AL have been circulating for years, with examples provided by Kanel et al. (2003), Evans et al. (2007), Gersten (2008), Evans and Schamberg (2009), and Seeman (AL Expert Workshop presentation, Feb. 2019), among others.
Researchers have used various numbers of biomarkers based on convenience or other considerations. For example, while Mauss et al. (2015) initially used a total of 15 biomarkers, Mauss et al. (2016) found that a streamlined AL index based on just five – diastolic blood pressure, waist circumference, glycosylated hemoglobin, low density lipoprotein, and heart rate variability – worked well to demonstrate association between high levels of industrial work-related stress and AL in male workers. They concluded that “[a] short form index seems to be a promising approach for occupational health practitioners,” and suggested further validation in longitudinal studies and development of a standardized suite of indicators. While this approach is interesting, there is no agreement on what parameters to definitely include when calculating AL. At a minimum, a determination of which biomarkers should be included in an abbreviated AL, particularly a formulation that could be used in multiple contexts is needed. Without an expert consensus, it is doubtful that one can be developed easily. In particular, a principal concern is the failure to include neuroendocrine mediators of AL in all abbreviated formulations or the inclusion of immune mediators as well as the downstream secondary outcomes reflected in metabolic and cardiovascular biomarkers.
4.3. What is needed to apply AL in disaster contexts?
In order to be of broad use in high-stress contexts such as disasters, a practical construct of AL needs to: (1) be as comprehensive as possible, including assessment of predisposing or influencing factors and psychosocial as well as physiological indicators that capture both the original causative experiences and resulting psychological and physiological responses; (2) have high fidelity in correspondence to the original concept as defined by McEwen, Seeman and others and include primary mediators; (3) incorporate biomarkers from multiple systems (neuroendocrine, immune/inflammatory, cardiovascular, respiratory, metabolic, anthropomorphic) to provide a robust index; (4) incorporate application and tracking within long-term longitudinal cohorts; and (5) have capacity to integrate new metrics as knowledge and technology advance.
5. Potential way forward to apply allostatic load in disaster contexts
5.1. Proposal to include both psychological and physical allostatic load
We propose combining simultaneous calculation of indices for psychosocial AL and physiological AL where requisite data are available. While we do not think it would be appropriate to attempt to calculate a single index score that would include both forms of AL at present, having both scores for the same people and following their evolution over time among participants within cohorts will provide robust indications of cumulative health effects and interactions of stress from psychosocial and physiological standpoints.
5.2. Using the community health observing system to test the concept
The Community Health Observing System recently proposed by Sandifer et al., 2020a, Sandifer et al., 2020b for the disaster-prone Gulf of Mexico region in the US could provide an excellent platform from which to test this concept (Suppl. Fig. 1). While the initial motivation for development of this observing system framework was recurrent environmental disasters in the Gulf of Mexico region, the basic health observing system plan could be adapted for use in many other geographic areas and other kinds of traumatic events including the COVID-19 pandemic. The framework relies on existing national (and mostly cross-sectional) health surveys conducted by the Centers for Disease Control and Prevention (CDC) and the National Institute of Health’s (NIH) new All of Us longitudinal study for comparative information at the national scale as well as community condition indicators such as the American Community Survey. However, the central and unique features of the proposed system are three new, nested longitudinal cohort studies: a Large Cohort that would provide a representative sampling of populations in the study region, a Small Cohort that would encompass a subset of the Large Cohort the members of which agree to provide more clinical data as well as biological specimens, and Disaster-Specific Cohorts that would be established rapidly following a disaster and built as much as possible upon the Large and Small Cohorts. (Suppl. Fig. 1).
Disaster-specific cohorts could be defined based on the geographic footprint of a specific disaster (e.g., hurricane), the type of event (e.g., economic disruption, pandemic), or even a particularly vulnerable community or population. Health data collected in the Large Cohort would comprise participant personally provided information obtained using questionnaires similar to those employed in the national cross-sectional studies along with a considerable amount of clinically-derived data. Much more clinical data including biological specimens would be collected in the Small and Disaster-Specific Cohorts ( Table 4), and supplementary data would be gathered from a variety of additional means including syndromic surveillance, electronic health records, wearable health monitors, remote sensing, social media, telemedicine assessments, and others to name a few examples (Suppl. Fig. 1). As noted in the Discussion, trained teams, consent and data collection protocols, supplies and materials, and institutional review board (IRB) approvals could be prepared and put in place on a region-by-region basis prior to disaster events. Like other disaster response plans, these should be updated regularly.
Table 4.
Types of data proposed for collection in the Gulf of Mexico Community Health Observing System cohort studies. All but personally provided information will be obtained in clinical settings. Modified slightly from Sandifer et al., 2020a, Sandifer et al., 2020b.
| Personally Provided Information From Questionnaires | Physical Health Measures |
|---|---|
| Demographic information, including ethnicity, sex/gender identity, marital/partner status, children | Systolic & diastolic BP |
| Socio-economic information, including ability to deal with minor financial emergencies | Pulse (heart) rate |
| General health status | Height & Weight |
| Personal health history, including chronic and major diseases | Waist-hip ratio |
| Family health history, including chronic and major diseases | Body mass index (BMI) |
| Life history and behavioral factors, including alcohol, tobacco, and illicit drug use, nutrition, exercise, sleep | Lung function (FEV1/FEVC) |
| Health care access and services utilization | Cardiovascular fitness |
| Prescribed medications | Gum health |
| Previous disaster/trauma experiences including in childhood | Balance |
| Residence and adequacy of housing | Ambulatory fitness (ability to rise, stand, walk) |
| Known or suspected exposure to toxic or infectious substances or organisms | Biospecimens |
| Social, religious, tribal, community attachments and memberships | Blood |
| Marginalization and discrimination (political, racism, ethnic, ageism, economic) | Plasma |
| Feeling of security or insecurity in home and neighborhood | Serum |
| Level of trust in government/societal structures | Saliva |
| Mental health measures | Urine |
| Anxiety: GAD-7 | Hair |
| Depression: PHQ-8 or 9 | DNA, mt DNA, telomere length (buccal swab) |
| PTSD/PTSS: PTSD Civilian | Nails (finger and toe) |
| Resilience: CD-RISC-10 (Connor-Davidson Scale) | Stool |
| Breath | |
| Alcohol abuse: AUDIT-C | Umbilical cord blood (when available) |
| Religiosity: RQ-12 | |
| General self-efficacy scale (GSES) | |
| Social capital (adapted from loneliness scale (ULS-8) | |
| Sense of control scale | |
| Cognitive function (IQ or other) |
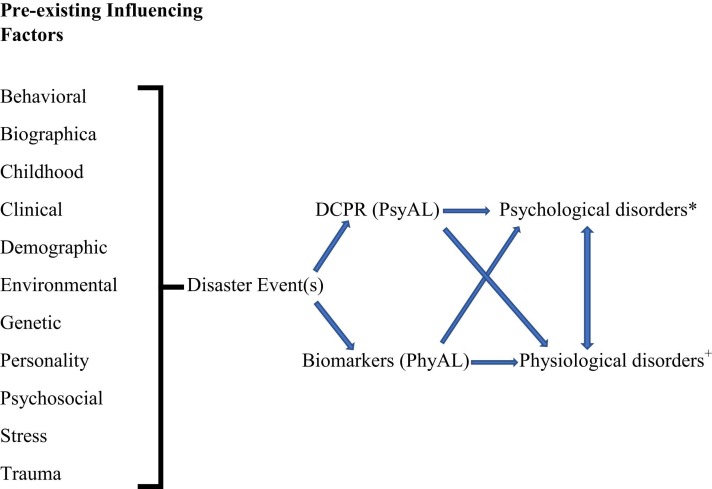
The Diagnostic Criteria for Psychosomatic Research or longer form Psychosocial Index could be included in the participant questionnaire, which already includes several psychosocial indicators as well as information on numerous potentially predisposing, mediating and/or moderating factors (Table 3). Factor analytic approaches to reduce multiple variables into key components or the use of indices that combine multiple variables into similar constructions could be useful in this endeavor. All health observing system Cohort participants would complete the participant questionnaire thereby providing the data to calculate the psychosocial AL index for all. In addition, physiological AL could be assessed for participants in the Small and Disaster-Specific Cohorts, based on the wide range of biomarkers expected to be collected (Suppl. Table 1). Having both psychosocial AL and physiological AL calculations for individuals would provide stronger predictive tools for potential negative health outcomes and allow assessment of interactions between psychosocial and physiological factors and the pre-existing conditions that affect both ( Fig. 2).
Fig. 2.
Simple graphical representation of inclusion of pre-existing influencing factors in calculations of both psychosocial allostatic load (PsyAL) and physiological AL (PsyAL) and some of their associated health outcomes. Arrows also indicate likely interactions whereby PsyAL may produce or exacerbate physiological as well as psychological disorders and vice versa as well as interactions between the disorders (e.g., impacts of chronic anxiety on cardiovascular diseases). Calculating both PsyAL and PhyAL for the same individuals in long-term cohort studies would allow consideration and assessment of such interactions over the life course and multiple traumatic events. (*Includes but not limited to anxiety, depression, PTSS, eating disorders, substance abuse, interpersonal conflict, difficulty concentrating, malaise, mood issues. + Includes but not limited to cardiovascular disease, respiratory and digestive complaints, headaches, and others).
While establishing a standard set of biomarkers should improve reproducibility and comparability of results across studies (Johnson et al., 2017), suggesting such is beyond the scope of this paper. However, at minimum, we recommend that researchers consider the original 10 indicators used by Seeman et al. (1997) (neuroendocrine system/HPA axis: cortisol, dehydroepiandrosterone sulfate, epinephrine, and norepinephrine; cardiovascular system: systolic and diastolic blood pressure; metabolic system: total cholesterol, high density lipoprotein; glycosylated hemoglobin; anthropomorphic: waist-hip ratio) and attempt to balance neuroendocrine, immune, metabolic, and cardiovascular parameters. Many physiological biomarkers previously used or recommended for use in calculating physiological AL are listed by Juster et al., 2010, Juster et al., 2011 and Sandifer et al., 2020a, Sandifer et al., 2020b and others (Suppl. Table 1). Note that while some research has focused on the primary mediators of AL (Gersten, 2008), it may not be sufficient to focus on these without consideration of secondary outcomes (Loucks et al., 2008). With the rapid advance of measurement technologies (e.g., multiplex, mass spectrometry), ambulatory assessments of many biomarkers (e.g., diastolic and systolic blood pressure, heart rate variability, glucose, cortisol, and others), as well as environmental exposures will become routine in the future. These and other indicators could be added to ongoing cohort studies as measurement technologies mature.
6. Discussion
McEwen and Stellar (1993) put forth an elegant concept they termed AL to link adverse physical health effects to cumulative psychosocial stress. In the decades since their initial description and its first operationalizations by Seeman et al. (1997), AL has been described in multiple contexts using varying physiological biomarkers and more recently psychological metrics. Although a complete theoretical underpinning for AL has yet to be developed, AL is well established as a composite diagnostic tool for assessing toxic stress in contexts such as disasters. It is this utility we review here and recommend for further application for disaster-associated health impacts in a world increasingly fraught with environmental and other catastrophes.
Despite nearly three decades of AL-related research and many papers on the topic, there is no fundamental understanding of how AL works. AL was originally described in people, which is undoubtedly the most complex organic system in which to try to understand mechanisms of action. AL also has been employed to assess health status and predict disease risk in captive non-human primates, including gorillas (Edes et al., 2018, Edes et al., 2020) and lemurs (Seeley et al., 2021) and may have potential for much broader application in animal husbandry. However, mechanistic underpinnings for AL have yet to be comprehensively described. The lack of new conceptual formulations of AL combined with empirical studies on simpler animal systems is a major bottleneck to further progress. We strongly recommend that younger scientists with fresh ideas and the latest technologies attack this problem in a comprehensive fashion, starting with new hypotheses and working with non-primate animal models, perhaps beginning with something like C. elegans and then moving up the taxonomic tree to higher animals such as small fish and mice.
Harmful levels of acute, chronic, and cumulative stress, and their psychological, physiological, and social impacts, are hallmarks of disaster events and other traumas. However, there is much yet to be learned about AL and the time course of physiological dysregulations in different contexts. While prospective longitudinal cohort studies provide the best mechanism for identifying AL and beginning to unravel how it works mechanistically, most existing cohort studies were not established with assessment of stress impacts on health in mind. As a result, it has been difficult to obtain sufficient biomarkers and psychosocial indicators post-hoc in such studies. This has contributed to the frequent differences in biomarker use and difficulties in comparing results across studies identified by numerous researchers.
Here, we offer the recently proposed Gulf of Mexico Community Health Observing System to comprehensively address and assess AL. If implemented, a broad range of AL metrics as noted above would be built into the system from the beginning. The health observing system would also include a plan for incorporation of other metrics as they become available or are identified as having particular salience. A pilot human health observing system project, perhaps located in the central Gulf of Mexico region, could be used to demonstrate the usefulness of the approach and fine-tune its design for broader implementation (Sandifer et al., 2021). The ultimate goal will be to build a linked network of regional health observing systems across the US (Sandifer 2022).
Regional health observing systems could include a quick response or “strike team” capacity “to rapidly identify participants, collect data, and provide treatment or referrals immediately following a disaster” (Sandifer et al., 2020b). Building such a capability would require the development of a trained cadre of rapid health responders supported by pre-approved data collection protocols and response plans, stockpiles of equipment and supplies, pre-identification of clinical, laboratory, and analytical capabilities, establishment of IRBs specifically designed and empowered to conduct rapid reviews, integration of the health responders into local and regional emergency response strategies, and the resources to maintain these capacities over time.
While we know of no fully operational and comprehensive health strike teams that could be mobilized rapidly in times of disaster, important progress has been made by the National Institute of Environmental Health Sciences (NIEHS) and its parent agency NIH in its Disaster Response Research (DR2) program that was born out of needs identified following the DWH oil spill (Miller et al., 2016; https://www.niehs.nih.gov/research/programs/disaster/index.cfm). Although the need for rapid IRB approvals apparently remains a concern, the OneFlorida Clinical Research Consortium provides an example of a large entity that has established a single IRB to support work of multiple institutions (https://www.ctsi.ufl.edu/ctsa-consortium-projects/oneflorida/, Shenkman et al., 2018). Rapid response capabilities, including a multi-institutional IRB with ability to conduct reviews and make decisions rapidly, could become an integral part of regional health observing systems. Other parts of the world could consider similar platforms in anticipation of potential disasters.
Regardless of whether a health observing system is implemented in the near term, efforts should be undertaken to establish prospective cohort studies for the specific purpose of assessing, validating, and understanding AL and its utility in predicting and thereby enabling mitigation of unnecessary morbidity and mortality related to stress, whether associated with disaster events, pandemics, climate change, or other factors. Although most reports of AL scores in the literature are based on physiological assessments, including the psychosocial AL questionnaire in one form or another in a health surveillance system, along with physiological AL based on biomarkers, would provide the most comprehensive assessment of AL and its utility in predicting and following disaster-associated health outcomes. Peng et al. (2021) demonstrated the utility of Fava’s (2019) clinimetric approach to assess AL associated with the COVID-19 pandemic among medical nonmedical workers, using the 55-item Psychosocial Index. Their study was conducted online in China about 6 months into the pandemic and involved approximately 3600 participants. The investigators reported AL in 15.8% of medical and 17.8% of nonmedical workers with no significant differences in these levels. However, factors associated with AL differed between the groups, with medical workers more stressed by work dissatisfaction and conflicts and nonmedical workers more by loss of jobs and difficult family issues. They also found that “anxiety, depression, somatization, hostility, and abnormal illness behavior were positively associated with allostatic load, while objective support, subjective support, utilization of support, social support, and global well-being were negatively associated.” Adding physiological AL metrics would have given a much more nuanced and complete assessment as would following of AL over the long term in longitudinal cohorts.
Peters et al. (2021) note that, while stress is typically considered to cause adverse psychological and physiological problems, some acute stress responses can also have positive effects, including the promotion of effective immune responses to viral diseases. They suggest the use of health questionnaires such as the Short Form Health Survey (SF-12) to help identify those whose pre-exposure psychosocial stress levels or positive quality of life may either increase or reduce their susceptibility to infectious disease. The comprehensive assessments of AL that would be a major component of the type of health observing system proposed here would make possible early identification of people who may need interventions to reduce their vulnerability.
As is often the case with environmental disasters, individuals and communities already disadvantaged by socioeconomic conditions, racism, health disparities, limited access to health care, low income and wealth, poor quality housing, and disproportionate exposure to pollutants and other environmental stressors are suffering higher impacts from COVID-19 (Lopez et al., 2021, Terrell and James, 2020) and global climate change (Islam and Winkel, 2017, Ebi et al., 2018; EPA, 2021; Romanello et al., 2021). COVID-19 has significantly reduced overall life expectancy in the U.S., with the impact for Black and Hispanic people 2–3 times greater than for others (Woolf et al., 2021). Further, minorities and people with poorer health often tend to be less well represented in health studies than non-minority and healthier individuals (Signorello et al., 2005, Enzenbach et al., 2019), so less is known about their prior and ongoing health issues. Many low-wealth, predominantly minority communities are located in proximity to ongoing or legacy industrial sites, highways, and other operations that produce significant environmental exposures (Solomon et al., 2016). Communities in such areas frequently suffer limited health care access, poor housing, low incomes, lack of green space, exposure to violence, racism, and ongoing health disparities and are often referred to as environmental justice (EJ) communities. Previous studies have reported that black and African American persons frequently had higher AL scores and mortality than others (Duru et al., 2012, Borrell et al., 2020, Geronimus et al., 2006, Howard and Sparks, 2016). Similarly, lower education and income levels are associated with higher AL and biological risk, independent of race/ethnicity or other factors (Seeman et al., 2004, Seeman et al., 2008; Beckie, 2012;, Borrell et al., 2020). Thus, it is not surprising that populations of EJ and other disadvantaged communities may have increased AL and/or weakened immune responses (Cave et al., 2020, Dasco et al., 2020).
Wakefield and Baxter (2010) used the term “compounded disadvantage” to describe the “multiple, overlapping health challenges faced by marginalized communities.” This concept takes into account social standing and identity, as influenced by environmental and social injustices that are associated with degraded physical and social environments and poorer health and well-being. Environmental justice and climate justice are linked, and both should focus on local impacts, lived experience, vulnerabilities associated with systemic inequalities, and community voices (Schlosberg and Collins, 2014). These are among the basic principles of community based participatory research.
Palinkas et al. (2021) described the vital roles that nongovernmental community organizations have played in COVID-19 responses in building, supporting and sustaining resilience in underserved Louisiana communities and their potential for continuing and expanded roles related to climate change impacts. One such organization is the Community Resilience Learning Collaborative and Research Network (C-LEARN) (https://www.c-learn.org) established in 2017 in Southeast Louisiana as a community-academic partnership “to enhance community and individual resilience in communities threatened by climate change and related disasters” (Springgate et al., 2021). Another excellent example is the Lowcountry Alliance for Model Communities (LAMC) and its associated research and analytic arm, the Charleston Community Research to Action Board (https://lamcnc.org/). This is a well-established and accomplished community based organization founded in 2005 that encompasses a group of eight EJ communities in Charleston, South Carolina, with outreach to others. Partnering with such community-based organizations and community leaders requires commitment to a community based participatory research approach that values input and participation equally from community and academic partners. It effectively ensures that community voices are not only heard but incorporated into projects. The community based participatory approach was built into the Community Health Observing System framework from the beginning (Sandifer et al., 2020a). Additionally, the proposed observing system includes disaster-specific cohorts that would be established to follow effects of individual disasters as well as their additive and synergistic impacts for areas or groups that suffer repeated calamities. Such cohorts could be created in environmental justice communities to assess psychosocial and physiological AL periodically over time for people who not only experienced one or more disasters but also significant pre-disaster and ongoing environmental, socioeconomic, and health stress. Regular measurement of AL in individuals from environmental justice and similar communities could provide ongoing individual and community health assessments and data for comparison with people living in more advantaged circumstances, uncover new information about how AL works and how stress causes specific health issues, and help identify where health care and social interventions might be most efficacious in reducing stress-associated disease burden. Building new partnerships involving biomedical and public health researchers, community leaders, and community based organizations could be an effective way to launch and manage longitudinal cohort studies in EJ and other communities.
As designed, the Community Health Observing System would provide long-running (hopefully continuous) cohorts, with data collection set at regular intervals, so that AL could be followed over the life course. This combined approach would open possibilities of (1) reporting both psychosocial and physiological AL indices for a more robust composite index, (2) using the psychosocial data to help explain physiological results obtained from biomarkers, (3) exploring interactions between psychosocial and physiological factors and outcomes, and (4) ensuring inclusion of substantial representation from marginalized communities. Most importantly, the evolution of individual AL scores could be followed over time for individuals and within groups and across multiple disasters/traumas and inter-disaster recovery periods, addressing crucial gaps in the AL literature and in our understanding of cumulative stress impacts.
7. Conclusions
A decade ago, Beckie (2012) described the need we address, stating: “Priorities for future research include conducting prospective longitudinal studies, examining a broad range of antecedent allostatic challenges, and collecting reliable measures of multisystem dysregulation explicitly designed to assess AL, at multiple time points, in large population-representative samples. Longitudinal data will facilitate the test of selection effects and allow for estimates of within-cohort age trajectories that represent true developmental changes with age, thus distinguishing aging and cohort effects (Yang and Kozloski, 2011).”
Additional priorities now include the pressing need to address not only health effects of environmental disasters but also long-term mental and physical health impacts of the COVID-19 pandemic and acute and more slowly developing consequences of global climate and environmental change. These will require a much more comprehensive and equitable approach to health management, recognition of the pervasive influences of stress on health and well-being, and the necessity for full inclusion of previously marginalized and disadvantaged groups and communities. Essential components of such assessments will be enhanced health surveillance employing linked longitudinal cohort studies that are fully representative of populations along with measurements of psychosocial and physiological AL as predictors of health outcomes. Stress is a nearly universal response to traumatic events, and individuals in disadvantaged communities are likely to experience higher levels of chronic stress. Working with health professionals, community leaders and community-based organizations could seize upon AL as a means of identifying people likely to be more affected by stress, circumstances prone to engender additional stress in their communities (e.g., chronic flooding, gentrification), and how to target interventions to reduce stress and thereby decrease health issues. These and mechanistic studies employing a variety of animal models are important areas for future study and action.
Funding support
Partial support for work that resulted in this paper was provided by contract # C-231826 between the Gulf of Mexico Alliance (GoMA), on behalf of the GoMRI, and the College of Charleston, by the NIEHS under award number P01ES028942 to the University of South Carolina (USC) and through a subaward from USC to the College of Charleston, and by the NIA under awards P30AG017265 and R24AG054365 to the University of California at Los Angeles (UCLA). The content of this paper is solely the responsibility of the authors and does not necessarily reflect the official views of the GoMA, GoMRI, the NIEHS, the NIA, the College of Charleston, UCLA, the University of Pittsburgh, or the University of Florida. Mention of private companies, trade names, or products does not imply endorsement of any kind.
Conflict of interest statement
The authors declare no competing interests.
Acknowledgments
Some of the ideas presented here were informed by a special workshop focused on the potential to operationalize allostatic load for application in a human health observing system. This workshop was supported by the Gulf of Mexico Research Initiative (GoMRI) and held in New Orleans, LA, Feb. 4–5, 2019. Details of the workshop and participant list are included as Appendix 2 in Sandifer et al. (2020b). We are grateful to all the participants for their engagement in the workshop discussions.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.psyneuen.2022.105725.
Appendix A. Supplementary material
Supplementary material
.
References
- Arbeev K.G., Ukraintseva S.V., Yashin A.I. Dynamics of biomarkers in relation to aging and mortality. Mech. Ageing Dev. 2016;156:42–54. doi: 10.1016/j.mad.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckie T.M. A systematic review of allostatic load, health, and health disparities. Biol. Res. Nurs. 2012;14(4):311–346. doi: 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- Borrell L.N., Dallo F.J., Nguyen N. Racial/ethnic disparities in all-cause mortality in U.S. adults: the effect of allostatic load. Public Health Rep. 2010;125:810–816. doi: 10.1177/003335491012500608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell L.N., Rodríguez-Álvarez E., Dallo F.J. Racial/ethnic inequities in the associations of allostatic load with all-cause and cardiovascular-specific mortality risk in US adults. PLoS One. 2020;15 doi: 10.1371/journal.pone.0228336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J., Finucane M.L., Locker M.D., Roth E.A., Collins R.L. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev. Med. 2021 doi: 10.1016/j.ypmed.2020.106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckwalter J.G., Castellani B., McEwen B., Karlamangla A.S., Rizzo A.A., John B., O’Donnell K., Seeman T. Allostatic load as a complex clinical construct: a case-based computational modeling approach. Complexity. 2015;21:291–306. doi: 10.1002/cplx.27143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadar D., Abell J., Hackett R.A., Steptoe A. Allostatic load is associated with coronary heart disease, but not with dementia: evidence from a 12-year follow-up in the English Longitudinal Study of Ageing. J. Epidemiol. Commun. Health. 2018 doi: 10.1136/jech-SSMabstracts22. [DOI] [Google Scholar]
- Castagne R., Gares V., Karimi M., Chadeau-Hyam M., Vineis P., Delpierre C., Kelly-Irving M. Allostatic load and subsequent all-cause mortality: which biological markers drive the relationship? Findings from a UK birth cohort. Eur. J. Epidemiol. 2018;33:441–448. doi: 10.1007/s10654-018-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cave L., Cooper M.N., Zubrick S.R., Shepherd C.C.J. Racial discrimination and allostatic load among First Nations Australians: a nationally representative cross-sectional study. BMC Public Health. 2020;20:1881. doi: 10.1186/s12889-020-009978-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A., Cahill M., Yeung D., Ross R. RAND Corporation; Santa Monica, CA: 2018. Toward an Initial Conceptual Framework to Assess Community Allostatic Load: Early Themes From Literature Review and Community Analyses on the Role of Cumulative Community Stress.〈https://www.rand.org/pubs/research_reports/RR2559.html〉 [Google Scholar]
- Christensen D.S., Flensborg-Madsen T., Garde E., Hansen A.M., Mortensen E.L. Big five personality traits and allostatic load in midlife. Psychol. Health. 2019;34(8):1011–1028. doi: 10.1080/08870446.2019.1585851. [DOI] [PubMed] [Google Scholar]
- Cohen S., Janicki-Deverts D., Miller G.E. Psychological distress and disease. J. Am. Med. Assoc. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Colwell R.R., Machlis G.E. American Academy of Arts and Sciences; Cambridge, MA: 2019. Science During Crisis: Best Practices, Research Needs, and Policy Priorities; p. 32. [Google Scholar]
- CRED (Centre for Research on the Epidemiology of Distasters) Human Cost of Disasters (2000-2019) Cred Crunch,; 2020. p. 3. [Google Scholar]
- CRED (Centre for Research on the Epidemiology of Distasters) Extreme Weather Events in Europe. Cred Crunch; 2021. p. 3. [Google Scholar]
- Crews D.E., Kawa N.C., Cohen J.H., Ulmer G.L., Edes A.N. Climate change, uncertainty and allostatic load. Ann. Hum. Biol. 2019;46(1):3–16. doi: 10.1080/03014460.2019.1584243. [DOI] [PubMed] [Google Scholar]
- Dasco, M., McArthur, K., Dasco, C., 2020. The coronavirus is exposing the underlying biological dangers of being a minority in the US. The Scientist July/August 2020. July 13, 2020. 3 pp.
- Dietz T., Shwom R.L., Whitley C.T. Climate change and society. Annu. Rev. Sociol. 2020;46(1):135–158. doi: 10.1146/annurev-soc-121919-054614. [DOI] [Google Scholar]
- Duru O.K., Harawa N.T., Kermah D., Norris K.C. Allostatic load burden and racial disparities in mortality. Natl. Med. Assoc. 2012;104(1–2):89–95. doi: 10.1016/s0027-9684(15)30120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebi K.L., Balbus J.M., Luber G., Bole A., Crimmins A., Glass G., Saha S., Shimamoto M.M., Trtanj J., White-Newsome J.L. In: Reidmiller D.R., Avery C.W., Easterling D.R., Kunkel K.E., Lewis K.L.M., Maycock T.K., Stewart B.C., editors. Volume II. U.S. Global Change Research Program; Washington, DC, USA: 2018. Human Health. In Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment; pp. 539–571. [DOI] [Google Scholar]
- Edes A.N., Wolfe B.A., Crews D.E. Evaluating allostatic load: a new approach to measuring long-term stress in wildlife. J. Zoo. Wildl. Med. 2018;49(2):272–282. doi: 10.1638/2016-0070.1. [DOI] [PubMed] [Google Scholar]
- Edes A.N., Edwards K.L., Wolfe B.A., Brown J.L., Crews D.E. Allostatic load indices with cholesterol and triglycerides predict disease and mortality risk in zoo-housed western lowland gorillas (Gorilla gorilla gorilla) Biomark. Insights. 2020;15:1–13. doi: 10.1177/117271920914585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMDAT . Universite catholique de Louvain; Brussels, Belgium: 2020. OFDA/CRED International Disaster Database.〈https://ourworldindata.org/grapher/number-of-natural-diaster-events〉 [Google Scholar]
- Enzenbach C., Wicklein B., Wirkner K., Loeffler M. Evaluating selection bias in a population-based cohort study with low baseline participation: the LIFE-Adult_Study. BMC Med. Res. Method. 2019;19:135. doi: 10.1186/s12874-019-0779-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel E.S., Crosswell A.D., Mayer S.E., Prather A.A., Slavich G.M., Puterman E., Mendes W.B. More than a feeling: a unified view of stress measure for population science. Front Neuroendocrinol. 2018;49:146–149. doi: 10.1016/j.yfrne.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G.W., Schamberg M.A. Childhood poverty, chronic stress, and adult working memory. Proc. Natl. Acad. Sci. USA. 2009;106(16):6545–6549. doi: 10.1073/pnas.0811910106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G.W., Kim P., Ting A.H., Tesher H.B., Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev. Psychol. 2007;43(2):341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- Farrell S.G., Mitnitski A.B., Rockwood K., Rutenberg A.D. Network model of human aging: frailty limits and information measures. Phys. Rev. E. 2016;94(5) doi: 10.1103/PhysRevE.94.052409. [DOI] [PubMed] [Google Scholar]
- Fava G.A., McEwen B.S., Guidi J., Gostoli S., Offidani E., Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- Fernandez C.A., Loucks E.B., Arheart K.L., Hickson D.A., Buka S.L., Gjelsvik A. Evaluating the effects of coping style on allostatic load, by sex: the Jackson Heart Study, 2000-2004. Prev. Chronic Dis. 2015;12 doi: 10.5888/pcd12.150166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental consequences of COVID-19 and physical distancing. the need for prevention and early intervention. J. Am. Med. Assoc. Intern. Med. 2020;(April 10, 2020):E1–E2. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gallo L.C., Fortmann A.L., Mattei J. Allostatic load and the assessment of cumulative biological risk in biobehavioral medicine: challenges and opportunities. Psychosom. Med. 2014;76(7):478–480. doi: 10.1097/PSY0000000000000095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T., Hicken M., Keene D., Bound P. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gersten O. Neuroendocrine biomarkers, social relations, and the cumulative costs of stress in Taiwan. Soc. Sci. Med. 2008;66(3):507–519. doi: 10.1016/j.socscimed.2007.09.004. ; discussion 520–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein B.D., Osofsky H.J., Lichtveld M.Y. The Gulf oil spill. New Engl. J. Med. 2011;364(14):1334–1348. doi: 10.1056/NEJMra1007197. [DOI] [PubMed] [Google Scholar]
- Gruenewald T.L., Seeman T.E., Ryff C.D., Karlamangla A.S., Singer B.H. Combinations of biomarkers predictive of later life mortality. Proc. Natl. Acad. Sci. USA. 2006;103(38):14158–14163. doi: 10.1073/pnas.0606215103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidi J., Lucente M., Sonino N., Fava G.A. Allostatic load and its impact on health: a systematic review. Psychother. Psychosom. 2020 doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- Howard J.T., Sparks P.J. The effect of allostatic load on racial/ethnic mortality differences in the United States. Popul. Res. Policy Rev. 2016:421–443. doi: 10.1007/s11113-016-9382-4. [DOI] [Google Scholar]
- Islam, S.N., Winkel, J. 2017. Climate change and social inequality. United Nations, Department of Economic and Social Affairs. DESA Working Paper No.152, ST/ESA/2017/DWP/152. 〈https://www.un.org/development/desa/publications/working-paper〉.
- Johnson S.C., Cavallaro F.L., Leon D.A. A systematic review of allostatic load in relation to socioeconomic position: poor fidelity and major inconsistencies in biomarkers employed. Soc. Sci. Med. 2017;192:66–73. doi: 10.1016/j.socscimed.2017.09.025. [DOI] [PubMed] [Google Scholar]
- Juster R.-P., McEwen B.S., Lupien S.J. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci. Biobehav. Rev. 2010;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Juster R.-P., Bizik G., Picard M., Arsenault-Lapierre G., Sindi S., Trepanier L., Marin M.F., Wan N., Sekerovic Z., Lord C., Fiocco A.J., Plusquellec O., McEwen B.S., Lupien S.J. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Dev. Psychopathol. 2011;23:725–776. doi: 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- Kanel R. v, Dimsdale J.E., Patterson T.L., Grant I. Acute procoagulant stress response as a dynamic measure of allostatic load in Alzheimer caregivers. Ann. Behav. Med. 2003;26(1):42–48. doi: 10.1207/S15324796ABM2601_06. [DOI] [PubMed] [Google Scholar]
- Kaplan, S., Tran, A.B., 2021. Nearly 1 in 3 Americans experienced a weather disaster this summer. The Washington Post. Washingtonpost.com/climate-environment/2021/09/04/climate-disaster-hurricane-ida/. Last accessed 10 Oct 2021.
- Kario K., McEwen B.S., Pickering T.G. Disasters and the heart: a review of the effects of earthquake-induced stress on cardiovascular disease. Hypertens. Res. 2003;26(5):355–367. doi: 10.1291/hypres.26.355. [DOI] [PubMed] [Google Scholar]
- Koob G.F., Schulkin J. Addiction and stress: an allostatic view. Neurosci. Biobehav. Rev. 2019;106:245–263. doi: 10.1016/j.neubiorev.2018.09.008. [DOI] [PubMed] [Google Scholar]
- Learning J., Guha-Sapir D. Natural disasters, armed conflict, and public health. NEJM. 2013;69:836–1842. doi: 10.1056/NEJMra1109877. [DOI] [PubMed] [Google Scholar]
- Lopez L., III, Hart L.H., III, Katz M.H. Racial and ethnic health disparities related to COVID-19. J. Am. Med. Assoc. 2021;325(8):719–720. doi: 10.1001/jama.2020.26443. [DOI] [PubMed] [Google Scholar]
- Loucks E.B., Juster R.P., Pruessner J.C. Neuroendocrine biomarkers, allostatic load, and the challenge of measurement: a commentary on Gersten. Soc. Sci. Med. 2008;66:525–530. [Google Scholar]
- Lupien S.J., Ouellet-Morin I., Hupbach A., Tu M.T., Buss C., Walker D., Preussner J., McEwen B.S. In: Developmental psychopathology, vol.2, Developmental neuroscience. Cicchetti D., Cohen D.J., editors. John Wiley & Sons, Inc; Hoboken, NJ, USA: 2015. Beyond the stress concept: allostatic load- a developmental, biological and cognitive perspective; pp. 578–628. [DOI] [Google Scholar]
- Mauss D., Jarczok M.N., Fischer E. A streamlined approach for assessing the allostatic load index in industrial employees. Stress. 2015;18(4):475–483. doi: 10.3109/10253890.2015.1040987. [DOI] [PubMed] [Google Scholar]
- Mauss D., Jarczok M.N., Fishcer J.E. The streamlined allostatic load index: a replication of study results. Stress. 2016;19(6):553–558. doi: 10.1080/10253890.2016.1219718. [DOI] [PubMed] [Google Scholar]
- McEwen B.S. Protective and damaging effects of stress mediators. New Engl. J. Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen B.S. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22(2):108–124. doi: 10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- McEwen B.S. Stressed or stressed out: what is the difference? J Psychiatr Neurosci 30(5), 315–318. Mcewen, B.S. 2006. Protective and damaging effects of stress mediators: central role of the brain. Dialog Clin. Neurosci. 2005;8(4):367–381. doi: 10.31887/DCNS.2006.8.4/bmcewen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S., Stellar E. Stress and the individual: mechanisms leading to disease. Arch. Intern Med. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- McEwen B.S., Tucker P. Critical biological pathways for chronic psychosocial stress and research opportunities to advance the consideration of stress in chemical risk assessment. Am. J. Public Health. 2011;101(S1):S131–S139. doi: 10.2105/AJPH.2011.300270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S., Tucker P. Critical biological pathways for chronic psychosocial stress and research opportunities to advance the consideration of stress in chemical risk assessment. Am. J. Public Health. 2011;101(S1):S131–S139. doi: 10.2105/AJPH.2011.300270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad E., Bogg T. Personality traits, coping, health-related behaviors, and cumulative psychological health in a national sample: 10 year prospective effects of conscientiouness via perceptions of activity on allostatic load. Ann. Behav. Med. 2020;54:880–892. doi: 10.1093/abm/kaaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller A., Yeskey K., Garantziotis S., Arnesen S., Bennett A., O-Fallon L., Thompson C., Reinlib L., Masten S., Remington J., Love C., Ramsey S., Rosselli R., Galluzzo B., Kowk R., Huges J. Integrating health research into disaster response: the new NIH disaster research response program. Int. J. Environ. Res. Public Health. 2016;13:676. doi: 10.3390/ijerph13070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NOAA National Centers for Environmental Information (NCEI) U.S. Billion-Dollar Weather and Climate Disasters, 2022. 〈https://www.ncdc.noaa.gov/billions/〉, DOI: 10.25921/stkw-7w73 (last accessed 10 Feb. 2022).
- Obeng-Gyasi E., Ferguson A.C., Stamatakis K.A., Province M.A. Combined effect of lead exposure and allostatic load on cardiovascular disease mortality – a preliminary study. Int. J. Environ. Res. Public Health. 2021;18:6879. doi: 10.3390/ijerph18136879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas L.A., Springgate B.F., Hancock J., Sugarman O.K., Pesson C.L., Stallard C.N., Haywood C., Meyers D., Johnson A., Polk M., Seay J.E., Stallard, Wells K.B. Impact of the COVID-19 pandemic on resilience to climate change in underserved communities. Sustain. Clim. Change. 2021;14(5) doi: 10.1089/sccc.2021.0022. [DOI] [Google Scholar]
- Parker A.M., Edelman A.F., Carman K.G., Finucane M.L. On the need for prospective disaster survey panels. Disaster Med. Public Prep. 2020;14(3):299–301. doi: 10.1017/dmp.2019.94. [DOI] [PubMed] [Google Scholar]
- Peng M., Wang L., Xue Q., Yin L., Zhu B.-h, Wang K., Shangguan F.-f, Zhang P.-r, Niu Y.-y, Zhang W.-r, Zhao W.-f, Wang H., Lv J., Song H.-q, Min B.-q, Leng H.-x, Jia Y., Chang H., Yu Z.-p, Tian Q., Yand Y., Zhu S., Li W., Gao X.-l, Liu X.-l, Yang M., Wang P., Wei P.-h, Wang C.-x, Li J.-n, Jia L.-b, Huang X.-m, Li D.-n, Xu D.-j, Deng Y.-l, Si T.-m, Dong H.-q, Wang U.-p, Cosci F., Wang H.,-x. Post-COVID-19 epidemic: allostatic load among medical and nonmedical workers in China. Psychother. Psychosom. 2021;190:127–136. doi: 10.1159/000511823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters E.M.J., Schedlowski M., Watzl C., Gimsa U. To stress or not to stress: brain-behavior-immune interaction may weaken or promote the immune response to SARS-CoV-2. Neurobiol. Stress. 2021;14 doi: 10.1016/j.ynstr.2021.100296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza J.R., Almeida D.M., Dmitrieva N.O., Klein L.C. Frontiers in the use of biomarkers of health in research on stress and aging. J. Gerontol. Psychol. Sci. 2010;65B(5):513–525. doi: 10.1093/geronb/gbq09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picard M., McEwen B.S. Psychological stress and mitochondria: a conceptual framework. Psychosom. Med. 2018;80:126–140. doi: 10.1097/PSY.0000000000000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picard M., McEwen B.S. Psychological stress and mitochondria: a systematic review. Psychosom. Med. 2018;80(2):141–153. doi: 10.1097/PSY.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piolanti A., Offidani E., Guidi J., Gostoli S., Fava G., Sonino N. Use of the psychosocial index: a sensitive tool in research and practice. Psychother. Psychosom. 2016;85:337–345. doi: 10.1159/000447760. [DOI] [PubMed] [Google Scholar]
- Robertson T., Beveridge B., Bromley C. Allostatic load as a predictor or all-cause and cause-specific mortality inn the general population: evidence from the Scottish Health Survey. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0183297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockwood K., Mitnitski A. Frailty in relation to the accumulation of deficits. J. Gerontol. Med. Sci. 2007;62A(7):722–727. doi: 10.1093/gerona/62.7.722. [DOI] [PubMed] [Google Scholar]
- Romanello M., McGushin A., Di Napoli C., Drummond P., Hughes N., Jamart L., et al. The 2021 report of the Lancet countdown on health and climate change: code red for a healthy future. Lancet. 2021;398:1619–1662. doi: 10.1017/S0140-6736(21)10787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer, P., Knapp, L., Lichtveld, M., Manley, R., Abramson, D., Caffey, R., Cochran, D., Collier, T., Eb,i K., Engel, L., Farrington, J., Finucane, M., Hale, C., Halpern, D., Harville, E., Hart, L., Hswen, Y., Kirkpatrick, B., McEwen, B., Morris, G., Orbach, R., Palinkas, L., Partyka, M., Porter, D., Prather, A., Rowles, T., Scott, G., Seeman, T., Solo-Gabriel, H., Svendsen, E., Tincher, T., Trtanj, J., Walker, A.H., Yehuda, R., Yip, F., Yoskowitz, D., Singer, B., 2020b. A Conceptual Framework for a Community Health Observing System for the Gulf of Mexico Region,” Mississippi-Alabama Sea Grant Consortium Technical Report MASGR-20–026 (2020). National Sea Grant Library No. GOMSG-20–001. p. 101.
- Sandifer P., Knapp L., Lichtveld M., Manley R., Abramson D., Caffey R., Cochran D., Collier T., Eb i K., Engel L., Farrington J., Finucane M., Hale C., Halpern D., Harville E., Hart L., Hswen Y., Kirkpatrick B., McEwen, B., Morris, G., Orbach R., Palinkas L., Partyka M., Porter D., Prather A., Rowles T., Scott G., Seeman T., Solo-Gabriel H., Svendsen E., Tincher T., Trtanj J., Walker A.H., Yehuda R., Yip F., Yoskowitz D., Singer B. Framework for a community health observing system for the Gulf of Mexico region: preparing for future disasters. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.578463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer Paul. Disasters, the COVID-19 pandemic, and a human health observing system. Environment: Science and Policy for Sustainable Development. 2022;64(1):4–18. doi: 10.1080/00139157.2022.1997324. [DOI] [Google Scholar]
- Sandifer P.A., Knapp L.C., Collier T.K., Jones A.L., Juster R.-P., Kelble C.R., Kwok R.K., Miglarese J.V., Palinkas L.A., Porter D.E., Scott G.I., Smith L.M., Sullivan W.C., Sutton-Grier A.E. A conceptual model to assess stress-associated health effects of multiple ecosystem services degraded by disaster events in the Gulf of Mexico and elsewhere. GeoHealth. 2017;1:S17–S36. doi: 10.1002/2016GH000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer P.A., Singer B.H., Colwell R.R. The U.S. needs a national human health observing system. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.705597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandifer P.A., Walker A.H. Enhancing disaster resilience by reducing stress-associated health impacts. Front. Pub. Health. 2018;6 doi: 10.3389/fpubh.2018.00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxbe D.E., Beckes L., Stoycos S.A., Coan J.A. Social allostasis and social allostatic load: a new model for research in social dynamics, stress, and health. Perspect. Psychol. Sci. 2019:1–14. doi: 10.1177/174569161987652. [DOI] [PubMed] [Google Scholar]
- Schlosberg D., Collins L.B. From environmental to climate justice: climate change and the discourse of environmental justice. WIREs Clim. Change. 2014;5(3):359–374. doi: 10.1002/wcc.275. [DOI] [Google Scholar]
- Seeley K.E., Proudfoot K.L., Wolfe B., Crews D.E. Assessing allostatic load in ring-tailed Lemurs (Lemur catta. Animals. 2021;11:3074. doi: 10.3390/ani11113074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T., Merkin S.S., Crimmins E., Koretz B., Charette S., Karlamangla K. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988-1994) Soc. Sci. Med. 2008;66(1):72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T.E., Singer B.H., Rowe J.H., Horwitz R.I., McEwen B.S. Price of adaptation\p=m-\allostatic load and its health consequences. Arch. Int. Med. 1997;157:2259–2268. [PubMed] [Google Scholar]
- Seeman T.E., McEwen B.S., Rowe J.W., Singer B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Nat. Acad. Sci. USA. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman T.E., Crimmins E., Huang M.H., Singer B., Bucur A., Gruenewald T., Berkman L.F., Reuben D.B. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc. Sci. Med. 2004;58(10):1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Shenkman E., Hurt M., Hogan W., Carrasquillo O., Smith S., Brickman A., et al. OneFlorida clinical research consortium: Linking a clinical and translational science institute with a community-based distributive medical education model. Acad. Med. 2018;93(3):451–455. doi: 10.1097/ACM.0000000000002029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorello L.B., Hargreaves M., Seinwandel M.D., Zheng W., Cai Q., Schlundt D.G., Buchowski M., Arnold C.W., McLauglin J.K., Blot W.J. Sourthern community cohort study: establishing a cohort to investigate health disparities. J. Nat. Med. Assoc. 2005;97(7):972–979. [PMC free article] [PubMed] [Google Scholar]
- Solis C.B., Fantin R., Kelly-Irving M., Delpierre C. Physiological wear-and-tear and later subjective health in mid-life: findings from the 1958 British birth cohort. Psychoneuroendocrinology. 2016;74:24–33. doi: 10.1016/j.psyneuen.2016.08.018. [DOI] [PubMed] [Google Scholar]
- Solomon G.M., Morello-Frosch R., Zeise L., Faust J.B. Cumulative environmental impacts: science and policy to protect communities. Ann. Rev. Public Health. 2016;37:83–97. doi: 10.1146/annurev-pubhealth-032315-021807. [DOI] [PubMed] [Google Scholar]
- Soloveva N.V., Makarova E.V., Kichuk I.V. Coronavirus syndrome: COVID-19 psychotrauma. Eur. J. Transl. Myol. 2020;30(4):9302. doi: 10.4081/ejem.2020.9302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springgate B.F., Sugarman O., Wells K.B., Palinkas L.A., Meyers D., Wennerstrom A., Johnson A., Haywood C., Sarpong D., Culbertson R. Community partnered participatory research in Southeast Louisiana communities threatened by climate change: the C_LEARN experience. Am. J. Bioeth. 2021 doi: 10.1010/15265161.2021.1965248. [DOI] [PubMed] [Google Scholar]
- Taneja S., Mitnitski A.B., Rockwood K., Rutenberg A.D. Dynamical network model for age-related health deficits and mortality. Phys. Rev. E. 2016;93(2) doi: 10.1103/PhysRevE.93.022309. [DOI] [PubMed] [Google Scholar]
- Terrell K.A., James W. Racial disparities in air pollution burden and COVID—19 deaths in Louisiana, USA, in the context of long-term changes in fine particulate pollution. Environ. Justice. 2020 doi: 10.1089/env.2020.0021.S. [DOI] [Google Scholar]
- USGCRP . Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment. US Global Change Research Program; Washington, DC: 2018. [Google Scholar]
- Wakefield S., Baxter J. Linking Health Inequality and Environmental Justice: Articulating a Precautionary Framework for Research and Action. Geography Publications; 2010. 〈https://ir.lib.uwo.ca/geographypub/272〉 [Google Scholar]
- White M.P., Elliott L.R., Gascon M., Roberts B., Fleming L.E. Blue space, health and well-being: a narrative overview and synthesis of potential effects. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110169. [DOI] [PubMed] [Google Scholar]
- Woolf S.H., Masters R.K., Aron L.Y. Effect of the covid-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: simulations of provisional mortality data. BNJ. 2021;373:n1343. doi: 10.1135/bmj.n1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Kozloski M. Sex differences in age trajectories of physiological dysregulation: Inflammation, metabolic syndrome, and allostatic load. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011;66:493–500. doi: 10.1093/gerona/glr003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yashin A.I., Arbeev K.G., Akushevich I., Kulminski A., Ukraintseva S.V., Stallard E., Land K.C. The quadratic hazard model for analyzing longitudinal data on aging, health, and the life span. Phys. Life Rev. 2012;9(2):177–188. doi: 10.1016/j.plrev.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material