Abstract
Background:
Propofol is commonly used for providing procedural sedation during pediatric colonoscopy. Intravenous (i.v.) lidocaine can mitigate visceral pain and reduce propofol requirements during surgery. The aim of this study is to investigate the effect of i.v. lidocaine on perioperative propofol and sufentanil dose, pulse oxygen saturation, postoperative pain score, and recovery time during pediatric colonoscopy.
Methods:
We designed a randomized, double-blind, placebo-controlled study and enrolled 40 children aged from 3 to 10 years who underwent colonoscopy. After titration of propofol to achieve unconsciousness, the patients were given i.v. lidocaine (1.5 mg/kg later 2 mg/kg/ hour) or the same volume of saline. Sedation was standardized and combined propofol with sufentanil. The primary outcome variables were intraoperative propofol and sufentanil requirements, and the number of oxygen desaturation episodes. Secondary outcome variables were recovery time after colonoscopy and post-colonoscopy pain.
Results:
Lidocaine infusion resulted in a significant reduction in propofol requirements: (median (quartile) 1.8 (1.5-2.0) vs. 3.0 (2.8-3.3) mg/kg respectively; P < 0.001) and sufentanil requirements: (median (quartile) 0.06 (0.05-0.08) vs. 0.1 (0.1-0.1) μg/kg respectively; P < 0.001). The number of subjects who experienced oxygen desaturation below 95% in the lidocaine group was also significantly less than that in the control group: 1 vs. 6 (P = 0.04). The mean (SD) recovery time was significantly shorter in the lidocaine group: (19.2 (2.6) vs. 13.3 (2.6) min respectively; P < 0.001). There was no significant difference in post-colonoscopy pain.
Conclusion:
Continuous infusion of lidocaine resulted in reduction of propofol and sufentanil requirements, recovery time, and risk of hypoxemia during pediatric colonoscopy.
Keywords: Lidocaine, pediatric colonoscopy, propofol, sufentanil
INTRODUCTION
Colonoscopy is commonly conducted in infants and children for the diagnosis and treatment of abdominal pain, diarrhea, weight loss, unexplained iron deficiency anemia, or unexplained hematochezia.[1,2] Colonoscopy has been developed as a diagnostic and therapeutic tool for pediatric patients.[3] Anesthesiologists are increasingly involved in providing procedural sedation and analgesia for pediatric colonoscopy due to the visceral discomfort associated with colonoscopy. Midazolam, propofol, and opioids are the most commonly used anesthetics for procedural sedation and analgesia during pediatric colonoscopy.[4,5] However, each of these anesthetics cause respiratory depression, and combining midazolam or propofol with opioids may further increase the risk for hypoxemia and apnea during pediatric colonoscopy.[6] In order to decrease the incidence and frequency of complications during pediatric endoscopy, different methods have been tried previously. Propofol–ketamine combinations are associated with fewer cardiopulmonary adverse effects than with propofol alone, according to previous reports.[7,8,9] Lidocaine is an amide local anesthetic. I.V. lidocaine has peripheral and central actions, and involves several mechanisms.[10,11] Previous studies have shown that it can alleviate visceral pain, reduce central or peripheral sensitization of pain, and inflammatory response through the reduction of cytokine secretion.[12,13,14] Thus, i.v. lidocaine may be another potential adjunct to propofol anesthesia, and some researchers have indicated that i.v. lidocaine can alleviate abdominal pain in patients.[15,16] During colonoscopy, colonic distention and traction may cause abdominal discomfort and visceral pain, potentially amenable to i.v. lidocaine. C. Forster et al.[17] have reported that i.v. lidocaine can be another adjunct to propofol sedation during adult colonoscopy and concluded that i.v. lidocaine resulted in a 50% reduction of propofol dose requirements. However, the application of lidocaine in pediatric colonoscopy has not been reported. We therefore conducted a clinical study to investigate whether i.v. lidocaine reduces propofol requirements and improves post-colonoscopy recovery during pediatric colonoscopy.
METHODS
We designed and implemented a randomized placebo-controlled double-blind trial in the operating room of Guangdong Women and Children Hospital, China. This study was approved by the Ethics Committee of Guangdong Women and Children Hospital on December 30, 2019 (identifier number 201901164) and registered with the Chinese Clinical Trials Registry (www.chictr.org.cn, identifier number ChiCTR2000028927, January 8, 2020, prospectively registered). After written informed consent was obtained from the American Society of Anesthesiologists (ASA) grades 1-2, 40 children aged from 3 to 10 years undergoing colonoscopy under sedation were included in our study, from February 15, 2020 to March 15, 2020 (see Figure 1 for CONsolidated Standards Of Reporting Trials (CONSORT) trial profile). Inclusion criteria were children aged from 3 to 10 years with normal electrocardiogram (ECG) results. Exclusion criteria were age >10 years or <3 years, liver insufficiency, major cardiac arrhythmia, and allergy to lidocaine.
Figure 1.
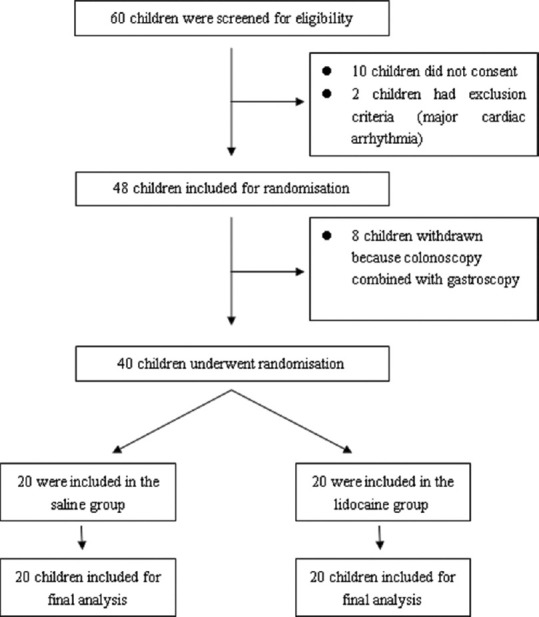
CONSORT 2010 Flow Diagram of this study. A total of 60 children were screened and evaluated from February 15, 2020 to March 15, 2020, in the operating room at Guangdong Women and Children Hospital. Among which, 10 of them did not consent, two of them had exclusion criteria (major cardiac arrhythmia), and eight withdrew because of colonoscopy combined with gastroscopy. In total, 40 children underwent randomization.
Study design and intervention
Once the participants entered the operating room, their ECG and oxygen saturation (SpO2) were routinely monitored. All the children were randomly and double blindly assigned to saline group (group S) and lidocaine group (group L) using sealed envelopes. All the children were sedated with an i.v. bolus injection of propofol (Lipofen, B. Braun Melsungen AG, specifications: 20 ml: 100 mg, batch number: 17515033) 2.5 mg/kg by the same anesthesiologist (C.Y.) who was blinded to patient allocation groups. A dose of sufentanil (Sufentanil citrate injection, EuroCept BV, specifications: 1 ml: 75 ug, batch number: 180262) 0.05 ug/kg was administered via i.v. after loss of consciousness. Group L was given an i.v. bolus of 1.5 mg/kg of lidocaine followed by a continuous infusion of 2 mg/kg/hour of it, whereas group S was given the same volume of saline.[18] Study medications were prepared by the same anesthesiologist (J.W.) involved neither in patient sedation nor in collecting study data. In order to avoid interference with blinding, study medications were infused after loss of consciousness in both groups, as the initial bolus of lidocaine may result in a specific reaction (if lidocaine had been injected first and then propofol, a sting at the injection site might disappear, which would let the researchers know that lidocaine was given instead of a placebo). An i.v. bolus of 1 mg/kg of propofol was administered by the anesthesiologist who was blinded to grouping information in response to abdominal discomfort expressed by the children or body movements or evidenced by irritability or hemodynamic changes (increase in heart rate ≥20 beats/min) during colonoscopy. About 0.05 μg/kg of sufentanil was added if the propofol was insufficiently effective. During colonoscopy, all children breathed spontaneously and received 4 L/min of oxygen through a nasal catheter in order to maintain oxygen saturation >90% during colonoscopy. Assisted ventilation via a mask or endotracheal intubation was given if the children developed respiratory depression (defined as SpO2<90%) or arrest (defined as 10-second apnea). Specifically, the anesthesiologist would lift the child's jaw when the SpO2was lower than 90%, if the SpO2was still lower than 90%, or continued to decrease, the anesthesiologist would use assisted ventilation at this time.
Outcome variables
The primary outcome variables were intraoperative propofol and sufentanil requirements and the number of oxygen desaturation episodes (defined as peripheral capillary oxygen desaturation (SpO2) less than 95% and 90%). The secondary outcome variables were recovery time (time between end of colonoscopy and ability for the children to blink) in the post-anesthesia care unit (PACU) and post-colonoscopy pain. The pain scores were recorded using the Wong-Baker FACES Pain Rating Scale after recovery in the PACU, 15 and 30 min later. The scale contains six cartoon faces showing pain ratings of 0–10, which are, from left to right, no pain (0), a little pain (2), mild pain (4), average pain (6), severe pain (8), and excruciating pain (10). Researchers involved in the assessment of these variables were blinded to patient allocation groups.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows (version 23.0, IBM Corp, Chicago, IL, USA). Quantitative variables were presented as mean ± standard deviation (SD) or median with interquartile range. Categorical data were reported as frequencies. Enumeration data and categorical variables were analyzed using the Chi-square test or Fisher's exact tests as appropriate. Continuous variables were tested with Student's t test or the Mann–Whitney U test depending on the distribution of the data, which was examined by the Shapiro–Wilk normality test. Mixed model analysis of variance (ANOVA) was used to compare postoperative pain scores. A value of P < 0.05 was considered statistically significant.
RESULTS
The sample size was calculated on the basis of a local pilot study. The mean propofol requirement during pediatric colonoscopy was 120 ± 33 mg. To detect a 30% decrease in propofol needs between groups, a power estimation analysis suggested that 18 patients per group will be required to achieve a power of 90%, when considering a bilateral type I error of 0.05. In view of a dropout rate of 10%, the sample size is estimated to be 20 per group. A total of 60 children were screened and evaluated from February 15, 2020 to March 15, 2020 in the operating room at Guangdong Women and Children Hospital. Among which, 10 of them did not consent, two of them had exclusion criteria (major cardiac arrhythmia), and eight withdrew due to a combination with gastroscopy. Finally, after consent from ASA grades 1-2, 40 children aged from 3 to 10 years undergoing colonoscopy under sedation were included in this randomized placebo-controlled double-blind study [Figure 1]. There was no significant difference in age, gender, weight, height, body mass index (BMI), ASA physical status, hemoglobin (Hb), iron, high sensitivity C-reactive protein (hs- CRP), reasons for colonoscopy, and duration of colonoscopy between the two groups [Table 1]. Therefore, the data sets of the two groups were comparable.
Table 1.
Characteristic data and duration of colonoscopy. Data are mean (standard deviation), median (interquartile range), or number
| Group S (n=20) | Group L (n=20) | P | |
|---|---|---|---|
| Age (years) | 6 (5,8) | 7 (5,9) | 0.53 |
| Gender (M/F) | 11/8 | 8/12 | 0.34 |
| Weight (kg) | 24.80±5.68 | 25.20±7.36 | 0.85 |
| Height (cm) | 1.16±0.14 | 1.15±0.14 | 0.82 |
| BMI (kg/m) | 21.25±3.06 | 21.59±4.27 | 0.77 |
| hs-CRP (mg/L) | 3.49±1.80 | 3.75±1.77 | 0.99 |
| Hb (g/L) | 125.0±11.6 | 123.5±11.7 | 0.86 |
| Fe2+ (mumol/L) | 12.26±5.72 | 12.68±5.13 | 0.97 |
| Reason for colonoscopy: | |||
| Hematochezia | 8 | 10 | 0.75 |
| Intestinal polyps | 7 | 6 | 0.99 |
| Inflammatory bowel disease | 5 | 4 | 0.99 |
| ASA physical status (1/2) | 11/9 | 8/12 | 0.34 |
| Duration of colonoscopy (min) | 12.40±1.67 | 12.35±1.81 | 0.93 |
BMI, body mass index; hs-CRP, high-sensitivity C-reactive protein; Hb, hemoglobin; ASA, American Society of Anesthesiologists
The propofol and sufentanil consumption in group L showed a significant reduction compared with group S (P < 0.001; Table 2). The recovery time of group L was shorter than that of group S (P < 0.001; Table 2). The number of subjects who experienced oxygen desaturation below 95% in the lidocaine group was also significantly less than that in the control group: 1 versus 6 (P = 0.04; Table 2). The number of children who experienced oxygen desaturation below 90% (1 vs. 2 subjects in the groups L and S, respectively) was similar in the two groups (P = 0.55; Table 2). There was no significant difference regarding respiratory frequency between the two groups (19 (18-21) vs 20 (19-21) byte/min, P = 0.26; Table 2). No endotracheal intubation or apnea occurred in both groups. In group L, a total of 1.58 (1.56-1.61) mg/kg of lidocaine was administered and the dose of lidocaine was rather low compared to other studies;[19,20,21] one child reported dizziness and vomiting after recovery, however, the incidence of adverse effects (dizziness, vomiting) was self-limited, and did not require any medical intervention. Table 2. The pain scores after colonoscopy were also similar in the two groups [ANOVA: drug effect (df = 1, F = 3.7): P =0.06; time effect (df = 1, F = 74.4): P <0.001; interaction (df = 1, F = 3.3): P =0.071] [Figure 2]. As shown in Figure 2, there was no statistical difference in the pain scores between the two groups of children at 15 and 30 min after recovery in the PACU.
Table 2.
Result variables. Data are mean (standard deviation), median (interquartile range), or number
| Group S (n=20) | Group L (n=20) | P | |
|---|---|---|---|
| Propofol: total dose (mg/kg) | 5.5 (5.3-5.8) | 4.3 (4.0-4.5) | <0.001 |
| Propofol: induction of sedation (mg/kg) | 2.5 (2.5-2.5) | 2.5 (2.5-2.5) | 0.999 |
| Propofol: during infusion of study medications (mg/kg) | 3.0 (2.8-3.3) | 1.8 (1.5-2.0) | <0.001 |
| Sufentanil (µg/kg) | 0.1 (0.1-0.1) | 0.06 (0.05-0.08) | <0.001 |
| Lidocaine (mg/kg) | - | 1.58 (1.56-1.61) | - |
| Recovery time (min) | 19.2±2.6 | 13.3±2.6 | <0.001 |
| SpO2 <95% (n) | 6 | 1 | 0.04 |
| SpO2 <90% (n) | 2 | 1 | 0.55 |
| Respiratory rate (byte/min) | 19 (18-21) | 20 (19-21) | 0.26 |
| Dizziness and vomiting (n) | - | 1 | - |
SpO2, oxygen saturation
Figure 2.
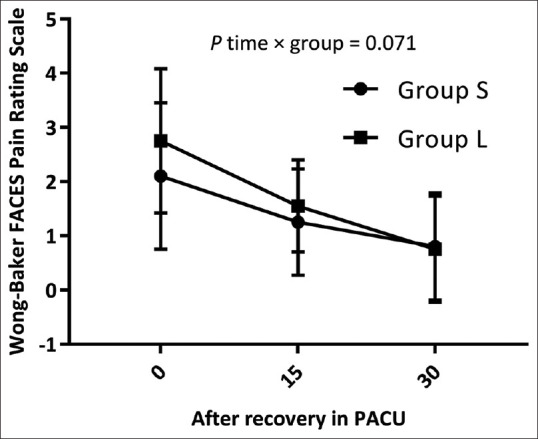
Pain score after colonoscopy. Data are mean (SD). Pain was recorded using the Wong-Baker FACES Pain Rating Scale, after recovery in the PACU 15 and 30 min later. Pain scores after colonoscopy were similar in the two groups (analysis of variance:P=0.071).
DISCUSSION
In the present study, we conducted a randomized, double-blind, placebo-controlled clinical trial to investigate whether i.v. lidocaine as an adjuvant drug reduces propofol requirements and improves postcolonoscopy recovery during pediatric colonoscopy. Our study demonstrated that adding i.v. lidocaine as an adjuvant drug could significantly reduce the propofol and sufentanil requirements for pediatric colonoscopy and at the same time, shorten the recovery time.
In our study, despite the fact that the propofol and sufentanil requirements in the lidocaine group was significantly less, all the children successfully underwent the colonoscopy. In addition, postoperative pain after colorectal surgery was similar in both groups, and no tracheal intubation and apnea occurred in both groups. Hypoxia and apnea secondary to respiratory depression and airway obstruction are the most frequent cardiopulmonary complications of propofol sedation for pediatric colonoscopy. An adjunct is administered to propofol and sufentanil partly to reduce their needs and consequently the incidence of their adverse effects. In our study, the number of subjects who experienced oxygen desaturation below 95% in the lidocaine group was significantly less than that in the control group, and there was no significant difference in age, gender, weight, height, BMI, ASA physical status Hb, iron, hs-CRP, reasons for colonoscopy, and duration of colonoscopy between the two groups. Thus, we believed that continuous infusion of lidocaine could reduce the risk of hypoxemia by reducing the use of propofol and sufentanil. Although the duration of colonoscopy in the two groups was similar, the recovery time was also shortened when adding i.v. lidocaine, which may also be related to reducing the dose of propofol and sufentanil. As the intravenous injection of lidocaine alone did not cause sedation, it just served as an adjunct drug for propofol sedation; thus, the shortening in recovery time might be due to the propofol and sufentanil-sparing effect.
As an amide local anesthetic, lidocaine has peripheral and central actions and involves several mechanisms. One of the possible mechanisms is the lidocaine's blockade of sodium channels. Moreover, blockade of nicotinic, muscarinic, and dopaminergic receptors, strengthening of gamma-aminobutyric acid (GABA) signal pathways, inhibition of opioid receptors, and modulation of proinflammatory signal pathways have also been reported.[22,23,24] Pediatric use of lidocaine has mainly concentrated on perioperative analgesia and preventing postoperative nausea and vomiting.[20,25,26]
Several studies have demonstrated that lidocaine administration as an analgesic could reduce opioids consumption[27,28] and benefit patients with earlier airway activity, the return of bowel function, and a shorter hospital stay after an operation.[29,30] Our study also demonstrated that adding i.v. lidocaine could significantly reduce the propofol and sufentanil comsumption in pediatric colonoscopy. However, lidocaine does have some adverse effects, as with all other medications, such as dizziness, nausea and vomiting, transient slurred speech, perioral numbness, dry mouth and so on.[13,31] The toxicity symptoms are transient and rapidly reversible due to its short half-life. In this study, the calculated total amount of administered lidocaine was 1.58 (1.56-1.61) mg/kg, which was lower than 2.9 (0.38) mg/kg reported by Echevarría et al.[20] However, even in Echevarría's research, the measured lidocaine plasma concentration was 0.87 to 4.88 μg/ml, which was below the toxicity threshold of 5 μg/ml, and no systemic toxic effects of lidocaine, including arrhythmia, were seen in any of the children participating in the clinical trial.[32] Although we did not monitor the lidocaine plasma concentration, it could be speculated that the lidocaine plasma concentration in our study was far from the toxicity threshold. In the present study, we observed lidocaine side-effects, however, the incidence of adverse effects (dizziness, vomiting) was mild, self-limited, and did not require any medical intervention.
In summary, lidocaine can be safely used as an adjunct to propofol sedation in children. However, due to age-related changes that arise in drug absorption, distribution, metabolism, and elimination, close observation and monitoring must be followed in pediatric patients. Of note, the therapeutic serum range for lidocaine is relatively narrow, which is 1.2–4.5 μg/mL. Toxicity can happen when plasma concentrations are >5 μg/mL. Therefore, we recommend consideration of plasma lidocaine concentration measurements, once laboratory conditions permit.
Several limitations of this study should be addressed. For example, recording the blood pressure might further help in detecting differences of adverse events associated with propofol. The endoscopists' working conditions were not quantified in this study. In the future, for better comparison, they can be quantified using visual analog scores. In additon, lidocaine plasma levels were not measured. Finally, this study was a single-center clinical trial. A multi-center clinical study should be carried out for further confirmation.
In conclusion, adding i.v. lidocaine can significantly reduce the propofol and sufentanil consumption and risk of hypoxemia for pediatric colonoscopy, while simultaneously, shortening the recovery time. The potential side-effects of lidocaine i.v. administration should also be considered.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Friedt M, Welsch S. An update on pediatric endoscopy. Eur J Med Res. 2013;18:24. doi: 10.1186/2047-783X-18-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schreiber-Dietrich DG, Hocke M, Gottschalk U, Meier P, Dietrich CF. [Update in pediatric endoscopy] Z Gastroenterol. 2017;55:490–500. doi: 10.1055/s-0042-118715. [DOI] [PubMed] [Google Scholar]
- 3.Lightdale JR, Acosta R, Shergill AK, Chandrasekhara V, Chathadi K, Early D, et al. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2014;79:699–710. doi: 10.1016/j.gie.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Cohen S, Glatstein MM, Scolnik D, Rom L, Yaron A, Otremski S, et al. Propofol for pediatric colonoscopy: The experience of a large, tertiary care pediatric hospital. Am J Ther. 2014;21:509–11. doi: 10.1097/MJT.0b013e31826a94e9. [DOI] [PubMed] [Google Scholar]
- 5.Amornyotin S, Aanpreung P, Prakarnrattana U, Chalayonnavin W, Chatchawankitkul S, Srikureja W. Experience of intravenous sedation for pediatric gastrointestinal endoscopy in a large tertiary referral center in a developing country. Paediatr Anaesth. 2009;19:784–91. doi: 10.1111/j.1460-9592.2009.03063.x. [DOI] [PubMed] [Google Scholar]
- 6.Nieuwenhuijs DJ, Olofsen E, Romberg RR, Sarton E, Ward D, Engbers F, et al. Response surface modeling of remifentanil-propofol interaction on cardiorespiratory control and bispectral index. Anesthesiology. 2003;98:312–22. doi: 10.1097/00000542-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Jalili M, Bahreini M, Doosti-Irani A, Masoomi R, Arbab M, Mirfazaelian H. Ketamine-propofol combination (ketofol) vs propofol for procedural sedation and analgesia: Systematic review and meta-analysis. Am J Emerg Med. 2016;34:558–69. doi: 10.1016/j.ajem.2015.12.074. [DOI] [PubMed] [Google Scholar]
- 8.Hu Y, Xu W, Cao F. A meta-analysis of randomized controlled trials: Combination of ketamine and propofol versus ketamine alone for procedural sedation and analgesia in children. Intern Emerg Med. 2019;14:1159–65. doi: 10.1007/s11739-019-02173-6. [DOI] [PubMed] [Google Scholar]
- 9.Yan JW, McLeod SL, Iansavitchene A. Ketamine-propofol versus propofol alone for procedural sedation in the Emergency Department: A systematic review and meta-analysis. Acad Emerg Med. 2015;22:1003–13. doi: 10.1111/acem.12737. [DOI] [PubMed] [Google Scholar]
- 10.Lauretti GR. Mechanisms of analgesia of intravenous lidocaine. Rev Brasil Anestesiol. 2008;58:280–6. doi: 10.1590/s0034-70942008000300011. [DOI] [PubMed] [Google Scholar]
- 11.Yang X, Wei X, Mu Y, Li Q, Liu J. A review of the mechanism of the central analgesic effect of lidocaine. Medicine. 2020;99:e19898. doi: 10.1097/MD.0000000000019898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weibel S, Jelting Y, Pace NL, Helf A, Eberhart LH, Hahnenkamp K, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst Rev. 2018;6:Cd009642. doi: 10.1002/14651858.CD009642.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, et al. Perioperative intravenous lidocaine infusion for postoperative pain control: A meta-analysis of randomized controlled trials. Can J Anaesth. 2011;58:22–37. doi: 10.1007/s12630-010-9407-0. [DOI] [PubMed] [Google Scholar]
- 14.Oliveira CM, Sakata RK, Slullitel A, Salomão R, Lanchote VL, Issy AM. [Effect of intraoperative intravenous lidocaine on pain and plasma interleukin-6 in patients undergoing hysterectomy] Rev Brasil Anestesiol. 2015;65:92–8. doi: 10.1016/j.bjan.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Firouzian A, Alipour A, Rashidian Dezfouli H, Zamani Kiasari A, Gholipour Baradari A, Emami Zeydi A, et al. Does lidocaine as an adjuvant to morphine improve pain relief in patients presenting to the ED with acute renal colic? A double-blind, randomized controlled trial. Am J Emerg Med. 2016;34:443–8. doi: 10.1016/j.ajem.2015.11.062. [DOI] [PubMed] [Google Scholar]
- 16.Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, et al. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology. 2007;106:11. doi: 10.1097/00000542-200701000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Forster C, Vanhaudenhuyse A, Gast P, Louis E, Hick G, Brichant JF, et al. Intravenous infusion of lidocaine significantly reduces propofol dose for colonoscopy: A randomised placebo-controlled study. Br J Anaesth. 2018;121:1059–64. doi: 10.1016/j.bja.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Hans GA, Lauwick SM, Kaba A, Bonhomme V, Struys MM, Hans PC, et al. Intravenous lidocaine infusion reduces bispectral index-guided requirements of propofol only during surgical stimulation. Br J Anaesth. 2010;105:471–9. doi: 10.1093/bja/aeq189. [DOI] [PubMed] [Google Scholar]
- 19.Kranke P, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015:CD009642. doi: 10.1002/14651858.CD009642.pub2. doi: 10.1002/14651858.CD009642.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Echevarría GC, Altermatt FR, Paredes S, Puga V, Auad H, Veloso AM, et al. Intra-operative lidocaine in the prevention of vomiting after elective tonsillectomy in children: A randomised controlled trial. Eur J Anaesthesiol. 2018;35:343–8. doi: 10.1097/EJA.0000000000000807. [DOI] [PubMed] [Google Scholar]
- 21.Both CP, Thomas J, Bühler PK, Schmitz A, Weiss M, Piegeler T. Factors associated with intravenous lidocaine in pediatric patients undergoing laparoscopic appendectomy-A retrospective, single-centre experience. BMC Anesthesiol. 2018;18:88. doi: 10.1186/s12871-018-0545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cummins TR. Setting up for the block: The mechanism underlying lidocaine's use-dependent inhibition of sodium channels. J Physiol. 2007;582:11. doi: 10.1113/jphysiol.2007.136671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weibel S, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: A systematic review with trial sequential analysis. Br J Anaesth. 2016;116:770–83. doi: 10.1093/bja/aew101. [DOI] [PubMed] [Google Scholar]
- 24.Dunn LK, Durieux ME. Perioperative use of intravenous lidocaine. Anesthesiology. 2017;126:729–37. doi: 10.1097/ALN.0000000000001527. [DOI] [PubMed] [Google Scholar]
- 25.Lemming K, Fang G, Buck ML. Safety and tolerability of lidocaine infusions as a component of multimodal postoperative analgesia in children. J Pediatr Pharmacol Ther. 2019;24:34–8. doi: 10.5863/1551-6776-24.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakajima D, Kawakami H, Mihara T, Sato H, Goto T. Effectiveness of intravenous lidocaine in preventing postoperative nausea and vomiting in pediatric patients: A systematic review and meta-analysis. PLoS One. 2020;15:e0227904. doi: 10.1371/journal.pone.0227904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vahidi E, Shakoor D, Aghaie Meybodi M, Saeedi M. Comparison of intravenous lidocaine versus morphine in alleviating pain in patients with critical limb ischaemia. Emerg Med J. 2015;32:516–9. doi: 10.1136/emermed-2014-203944. [DOI] [PubMed] [Google Scholar]
- 28.Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, et al. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004;98:1050–5, table of contents. doi: 10.1213/01.ANE.0000104582.71710.EE. [DOI] [PubMed] [Google Scholar]
- 29.Beilin B, Shavit Y, Trabekin E, Mordashev B, Mayburd E, Zeidel A, et al. The effects of postoperative pain management on immune response to surgery. Anesth Analg. 2003;97:822–7. doi: 10.1213/01.ANE.0000078586.82810.3B. [DOI] [PubMed] [Google Scholar]
- 30.Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95:1331–8. doi: 10.1002/bjs.6375. [DOI] [PubMed] [Google Scholar]
- 31.Golzari SE, Soleimanpour H, Mahmoodpoor A, Safari S, Ala A. Lidocaine and pain management in the emergency department: A review article. Anesthesiol Pain Med. 2014;4:e15444. doi: 10.5812/aapm.15444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Becker DE, Reed KL. Local anesthetics: Review of pharmacological considerations. Anesth Prog. 2012;59:90–101. doi: 10.2344/0003-3006-59.2.90. quiz 2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


