Abstract
Background
The COVID-19 pandemic prompted a rapid shift to virtual (video and telephone) delivery of mental health care, disrupting established processes for identifying people at increased risk of suicidal behavior.
Methods
Following the shift to virtual care, Kaiser Permanente Washington implemented a series of workflow changes to administer standard screening and monitoring questionnaires at virtual visits and to complete structured suicide risk assessments for patients reporting frequent suicidal ideation. These new workflows included automated distribution of questionnaires via the electronic health record (EHR) patient portal and automated alerts to clinicians regarding indicators of high risk.
Results
In March 2020, in-person mental health visits were rapidly and completely replaced by video and telephone visits. The proportion of mental health visits with completed screening and monitoring questionnaires fell from approximately 80% in early 2020 to approximately 30% in late March, then gradually recovered to approximately 60% by the end of 2020. Among patients reporting frequent suicidal ideation on monitoring questionnaires, the proportion with a recorded suicide risk assessment fell from over 90% in early 2020 to approximately 40% in late March, then gradually recovered to nearly 100% by the end of 2020.
Conclusion
Use of EHR patient portal messaging capabilities can facilitate systematic identification and assessment of suicide risk for patients receiving mental health care by telephone or video visit.
Outpatient mental health visits are an important opportunity to identify and address risk of suicidal behavior. Half of people who die by suicide and two thirds of people who survive suicide attempts received some outpatient mental health diagnosis or treatment in the prior year.1 , 2 Recognizing those potential opportunities for prevention, The Joint Commission recommends systematic screening for suicide risk among patients receiving treatment for mental health conditions.3 Many large health systems have implemented systematic screening programs, often relying on brief self-report questionnaires.4
The COVID-19 pandemic prompted a dramatic change in delivery of outpatient mental health care. To reduce risk of infection for patients and clinicians and preserve supplies of personal protective equipment, outpatient mental health clinics dramatically reduced face-to-face visits and rapidly increased telehealth, including both video visits and telephone visits.5., 6., 7., 8., 9., 10. This shift was facilitated by temporary relaxation of regulatory and payment restrictions on the use of telehealth care.9 , 11
This rapid shift to telehealth, however, disrupted visit-based processes to screen for risk of suicidal behavior. We describe here the adaptation of an existing suicide risk screening program to accommodate that rapid replacement of face-to-face care with video and telephone visits.
Methods
Setting
Kaiser Permanente Washington (KPWA) is an integrated health system serving approximately 700,000 members in Washington State, with approximately 500,000 served by KPWA–operated clinics and the remainder by external community providers. KPWA members are generally representative of the service area population and are enrolled through a mixture of employer-sponsored insurance, individually purchased insurance (including subsidized insurance exchange plans), Medicare, and Medicaid. KPWA's Mental Health and Wellness (MHW) department provides outpatient specialty mental health care through seven clinics staffed by a mixture of psychiatrists, psychologists, nurses, advanced practice nurses, and masters-prepared psychotherapists.
Pre-Pandemic Screening Process
Since 2010, all patients aged 13 years and older attending outpatient MHW visits are asked to complete a standard monitoring questionnaire, including the Public Health Questionnaire (PHQ)-9 depression scale,12 the generalized anxiety disorder (GAD)-2 anxiety scale,12 and additional questions regarding alcohol,13 cannabis, and other drug use. Monitoring questionnaires were typically completed on paper in the waiting area prior to a visit, presented to clinicians at the start of the visit, and entered by the clinician into the electronic health record (EHR). Beginning in 2017, clinicians could also send the monitoring questionnaire to patients online through the EHR patient portal, but this functionality was rarely used prior to 2020. Beginning in 2014, KPWA added a standard process for MHW providers to identify and address risk of suicidal behavior. For any response to the ninth item of the PHQ-914 indicating thoughts of self-harm or suicide “more than half the days” or “nearly every day,” the treating clinician is expected to conduct and record a structured assessment of suicide risk using the Columbia–Suicide Severity Rating Scale (C-SSRS).15 If the C-SSRS indicates recent suicidal ideation with planning (that is, a score of 3 or higher), the treating clinician is expected to collaborate with the patient to create or update a safety plan,16 including reducing access to lethal means.
Video visits were offered at all MHW clinics beginning in 2018 but rarely used until 2020. Scheduled telephone visits were sometimes offered for patients unable to attend in person or use video visit technology, but this option was also rarely used. Prior to 2020, no systematic processes were in place for completion of monitoring questionnaires prior to or during video or telephone visits.
Transition to Virtual Care
In response to rapid increases in COVID-19 cases, KPWA MHW clinics rapidly shifted to telehealth between March 13 and March 16 of 2020. Previously scheduled appointments were converted to video or telephone visits, and patients requesting appointments were encouraged to schedule video visits when feasible and telephone visits when video visits were not feasible. Face-to-face visits were allowed only when clinically essential, most often for patients in crisis or those unable to communicate effectively via telephone or video. Signage in waiting rooms still asked patients attending in person to complete monitoring questionnaires, but check-in occurred at the building entrance, and receptionists were no longer present in waiting areas to request completion of questionnaires. Limits on face-to-face visits were relaxed somewhat in July, with telehealth still recommended but face-to-face visits allowed in case of patient or clinician preference.
Adaptation of Screening to Virtual Care
Following the initial shift to telehealth in March, clinicians were advised to send monitoring questionnaires via the EHR patient portal in advance of visits. Each clinician was expected to manually send questionnaires to each patient at least one day prior to a scheduled visit, but no automated process was in place to prompt sending those messages. Clinicians were expected to administer questionnaires during visits for patients unable or unwilling to complete questionnaires online. No systematic process was in place to monitor or ensure questionnaire completion. Clinicians were still expected to complete C-SSRS assessments when response to PHQ-9, item 9—either prior to or during the visit—indicated frequent suicidal ideation. The EHR patient portal questionnaire, however, did not automatically prompt clinicians to complete a risk assessment based on the response to item 9 of the PHQ-9.
A more robust process for completion of monitoring questionnaires was implemented in April. Online monitoring questionnaires were sent automatically via the EHR patient portal prior to all scheduled video visits. Questionnaire responses were automatically entered into the record for the associated visit. Clinicians were still expected to administer questionnaires during video visits for patients unwilling or unable to complete questionnaires in advance. Questionnaires were not sent automatically prior to telephone visits, and clinicians were still expected to complete indicated risk assessments without any automated prompting.
Additional process improvements were implemented in November. Online monitoring questionnaires were sent automatically prior to scheduled telephone visits as well as video visits. Also beginning in November, the online monitoring questionnaire automatically presented C-SSRS questions if response to item 9 of the PHQ-9 indicated frequent suicidal ideation (that is, a score of 2 or 3). If responses to the online C-SSRS indicated recent suicidal ideation with planning (a score of 3 or higher), follow-up alerts were routed to MHW clinic staff (during operating hours) or to KPWA's 24-hour consulting nurse service (outside of operating hours). Clinic staff were expected to initiate immediate telephone outreach for a clinical assessment of risk and, as appropriate, creation of a personal safety plan.
Analysis
Data were extracted from KPWA EHR databases regarding numbers of visits of each type completed, numbers of monitoring questionnaires completed, and numbers of C-SSRS risk assessments completed each week from January through December of 2020. Confidence limits for proportions were calculated using the normal approximation to the binomial distribution.17 This Kaiser Permanente Washington Institutional Review Board approved a waiver of consent to use de-identified records data for this evaluation.
Results
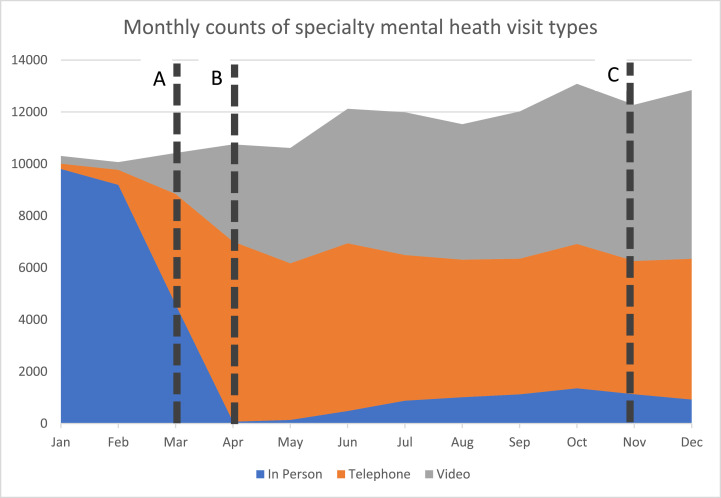
Figure 1 illustrates the rapid transition to telehealth in March and slower changes in visit patterns over the remainder of the year. The total number of mental health specialty visits dropped slightly in March, returned to previous levels by May, and continued to gradually increase over the next several months. In-person visits accounted for nearly all encounters in January and February, rapidly dropping nearly to zero in April and slowly increasing back to approximately 10% of all encounters by October. Video and telephone encounters increased rapidly in mid-March and then continued to gradually increase, accounting for approximately 47% and 42% of all encounters, respectively, by October.
Figure 1.
The graph shows the distribution of mental health specialty visit types during 2020. A, shift to video and telephone visits in March 2020; B, online monitoring questionnaires sent automatically prior to video visits beginning in April 2020; C, online monitoring questionnaires sent automatically prior to telephone visits, and suicide risk questions presented automatically within online questionnaires beginning in November 2020.
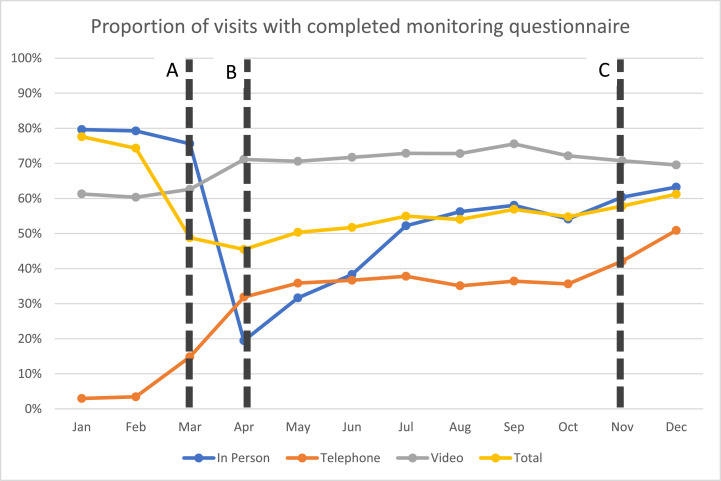
Figure 2 illustrates changes in completion of monitoring questionnaires following the shift to telehealth, and detailed results are shown in Table 1 . The proportion of all encounters with a completed questionnaire was approximately 74% in February and decreased to approximately 45% in April following the shift to video and telephone visits. Monitoring questionnaire completion rates for in-person visits followed that same pattern, decreasing sharply from approximately 79% in February to approximately 19% in April before gradually recovering to approximately 58% in September. Completion rates for video visits were approximately 60% in February, increasing to approximately 71% in April and remaining at approximately that level for the remainder of the year. Completion rates for telephone visits were very low prior to the pandemic, but this rate is based on a very small sample. Those rates remained below 40% from April to October, increasing to approximately 51% by December.
Figure 2.
This graph shows completion of monitoring questionnaires for different mental health specialty visit types during 2020. A, shift to video and telephone visits in March 2020; B, online monitoring questionnaires sent automatically prior to video visits beginning in April 2020; C, online monitoring questionnaires sent automatically prior to telephone visits, and suicide risk questions presented automatically within online questionnaires beginning in November 2020.
Table 1.
Counts, Rates, and Confidence Limits for Completion of Monitoring Questionnaires by Month
| In Person |
Phone |
Video |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| # Visits | # with Quest. | Rate (%) | 95% CI (%) | # Visits | # with Quest | Rate (%) | 95% CI (%) | # Visits | # with Quest | Rate (%) | 95% CI (%) | |
| Jan | 9,806 | 7,809 | 79.6 | 79–81 | 202 | 6 | 3.0 | 1–5 | 297 | 182 | 61.3 | 56–67 |
| Feb | 9,191 | 7,284 | 79.3 | 78–80 | 580 | 20 | 3.4 | 2–5 | 295 | 178 | 60.3 | 55–66 |
| Mar | 4,583 | 3,465 | 75.6 | 74–77 | 4,257 | 631 | 14.8 | 14–16 | 1,578 | 988 | 62.6 | 60–65 |
| Apr | 72 | 14 | 19.4 | 10–29 | 6,936 | 2,211 | 31.9 | 31–33 | 3,742 | 2,662 | 71.1 | 70–73 |
| May | 139 | 44 | 31.7 | 24–39 | 6,030 | 2,162 | 35.9 | 35–37 | 4,444 | 3,137 | 70.6 | 69–72 |
| Jun | 483 | 185 | 38.3 | 34–43 | 6,459 | 2,369 | 36.7 | 36–38 | 5,181 | 3,716 | 71.7 | 70–73 |
| Jul | 879 | 459 | 52.2 | 49–56 | 5,612 | 2,122 | 37.8 | 37–39 | 5,496 | 4,005 | 72.9 | 72–74 |
| Aug | 1,012 | 569 | 56.2 | 53–59 | 5,298 | 1,859 | 35.1 | 34–36 | 5,217 | 3,798 | 72.8 | 72–74 |
| Sep | 1,125 | 653 | 58.0 | 55–61 | 5,224 | 1,903 | 36.4 | 35–38 | 5,668 | 4,282 | 75.5 | 74–77 |
| Oct | 1,356 | 734 | 54.1 | 51–57 | 5,561 | 1,981 | 35.6 | 34–37 | 6,165 | 4,449 | 72.2 | 71–73 |
| Nov | 1,128 | 681 | 60.4 | 58–63 | 5,131 | 2,161 | 42.1 | 41–43 | 6,019 | 4,258 | 70.7 | 70–72 |
| Dec | 922 | 583 | 63.2 | 60–66 | 5,424 | 2,760 | 50.9 | 50–52 | 6,495 | 4,518 | 69.6 | 68–71 |
CI, confidence interval.
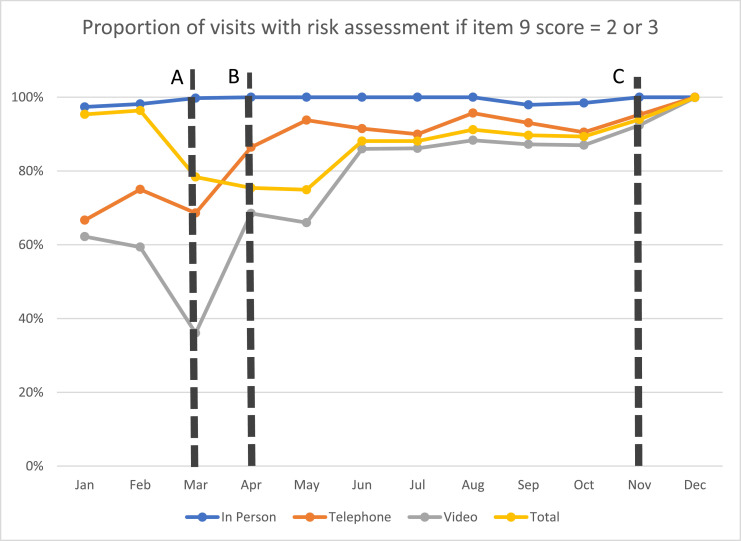
Figure 3 illustrates changes in rates of C-SSRS completion when indicated by response to PHQ-9, item 9. Rates of C-SSRS completion dropped in March for all visit types and then rapidly recovered to relatively high levels for the remainder of the year for all visit types. Rates of C-SSRS completion reached 100% during the last several weeks of the year, reflecting automatic presentation of C-SSRS questions during online completion of monitoring questionnaires (Table 2 ).
Figure 3.
Shown here is the proportion of visits with documented risk assessment if the score on item 9 of the Public Health Questionnaire (PHQ)-9 was 2 or 3. A, shift to video and telephone visits in March 2020; B, online monitoring questionnaires sent automatically prior to video visits beginning in April 2020; C, online monitoring questionnaires sent automatically prior to telephone visits, and suicide risk questions presented automatically within online questionnaires beginning in November 2020.
Table 2.
Counts, Rates, and Confidence Limits for Completion of Risk Assessments by Month
| In Person |
Phone |
Video |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| # Visits Needing Assess. | # with Assess. | Rate (%) | 95% CI (%) | # Visits Needing Assess. | # with Assess. | Rate (%) | 95% CI (%) | # Visits Needing Assess. | # with Assess. | Rate (%) | 95% CI (%) | |
| Jan | 832 | 810 | 97.4 | 96–98 | 6 | 4 | 66.7 | 29–100 | 45 | 28 | 62.2 | 48–76 |
| Feb | 815 | 800 | 98.2 | 97–99 | 12 | 9 | 75.0 | 51–100 | 32 | 19 | 59.4 | 42–76 |
| Mar | 401 | 400 | 99.8 | 99–100 | 86 | 59 | 68.6 | 59–78 | 183 | 66 | 36.1 | 29–43 |
| Apr | 2 | 2 | 100 | 100–100 | 258 | 223 | 86.4 | 82–91 | 419 | 287 | 68.5 | 64–73 |
| May | 12 | 12 | 100 | 100–100 | 241 | 226 | 93.8 | 91–97 | 544 | 359 | 66.0 | 62–70 |
| Jun | 40 | 40 | 100 | 100–100 | 235 | 215 | 91.5 | 88–95 | 607 | 522 | 86.0 | 83–89 |
| Jul | 65 | 65 | 100 | 100–100 | 239 | 215 | 90.0 | 86–94 | 620 | 534 | 86.1 | 83–89 |
| Aug | 72 | 72 | 100 | 100–100 | 209 | 200 | 95.7 | 93–98 | 548 | 484 | 88.3 | 86–91 |
| Sep | 96 | 94 | 97.9 | 95–100 | 230 | 214 | 93.0 | 90–96 | 642 | 560 | 87.2 | 85–90 |
| Oct | 128 | 126 | 98.4 | 96–101 | 221 | 200 | 90.5 | 87–94 | 607 | 528 | 87.0 | 84–90 |
| Nov | 122 | 122 | 100 | 100–100 | 275 | 262 | 95.3 | 93–98 | 696 | 643 | 92.4 | 90–94 |
| Dec | 121 | 121 | 100 | 100–100 | 400 | 400 | 100 | 100–100 | 749 | 748 | 99.9 | 100–100 |
CI, confidence interval.
Discussion
The COVID-19 pandemic prompted a rapid and unexpected shift to telehealth, disrupting established clinic processes for identifying and assessing risk of suicidal behavior. We describe a stepwise effort to implement new processes appropriate for telehealth visits. Although the rapid shift to telehealth did disrupt established processes for screening and risk assessment, adaptations of those processes led to gradual return to approaching or even exceeding previous levels of performance.
Online administration of monitoring questionnaires did raise some concerns regarding identification of suicide risk without the possibility of an immediate clinical response. Similar concerns have been raised regarding remote identification of suicide risk in both outpatient mental health18 , 19 and school health settings.20 These concerns increased with online administration of the C-SSRS, prompting use of immediate automated alerts to clinic staff and the consulting nurse service. We should emphasize, however, that this is more of an institutional liability concern than a true quality or safety concern. We are not aware of any evidence that online assessment of suicidal ideation can create or increase risk of suicidal behavior. Instead, assessment simply reveals risk that might otherwise not be addressed. The National Action Alliance for Suicide Prevention has recently addressed this issue in a recommendation to continue systematic identification of suicide risk following the shift to telehealth visits.21
We should point out specific limitations on the interpretation of our results. Absent any control or comparison group, we cannot determine which specific process improvements led to specific changes in screening or risk assessment rates. In addition, we cannot be certain how our findings regarding the shift to virtual visits or related disruptions in screening processes would apply to other health care settings or systems. Nor can we be certain how the specific improvement strategies implemented in this health care system would or would not succeed in others. We present these findings as one example of how systematic, automated processes can support systematic identification of suicide risk even during unprecedented changes in mental health care delivery.
Conclusion
We anticipate that in-person mental health visits will increase as the COVID-19 pandemic subsides, but we expect that telehealth visits will continue at a much higher level than prior to the pandemic. Consequently, it is essential to develop new care processes to identify increased risk of suicidal behavior for visits conducted by telephone or videoconferencing. Key elements of those new care processes include the use of messaging and online questionnaires through the EHR patient portal, automated alerts to prompt appropriate follow-up regarding questionnaire responses, and well-defined responsibilities for mental health and consulting nurse clinicians.
Acknowledgments
Funding
Supported in part by National Institute of Mental Health (NIMH) cooperative agreements U19MH121738 and U01MH114087.
Conflicts of Interest
All authors report no conflicts of interest.
References
- 1.Ahmedani BK, et al. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29:870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmedani BK, et al. Racial/ethnic differences in health care visits made before suicide attempt across the United States. Med Care. 2015;53:430–435. doi: 10.1097/MLR.0000000000000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Joint Commission. Suicide Prevention. Accessed Apr 25, 2021. https://www.jointcommission.org/resourSces/patient-safety-topics/suicide-prevention/.
- 4.Rossom RC, et al. Facilitating action for suicide prevention by learning health care systems. Psychiatr Serv. 2016 Aug 1;67:830–832. doi: 10.1176/appi.ps.201600068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connolly SL, et al. Rapid increase in telemental health within the Department of Veterans Affairs during the COVID-19 pandemic. Telemed J E Health. 2021;27:454–458. doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- 6.Yellowlees P, et al. Rapid conversion of an outpatient psychiatric clinic to a 100% virtual telepsychiatry clinic in response to COVID-19. Psychiatr Serv. 2020 Jul 1;71:749–752. doi: 10.1176/appi.ps.202000230. [DOI] [PubMed] [Google Scholar]
- 7.Rosen CS, et al. Virtual mental health care in the Veterans Health Administration's immediate response to coronavirus disease-19. Am Psychol. 2021;76:26–38. doi: 10.1037/amp0000751. [DOI] [PubMed] [Google Scholar]
- 8.Gentry MT, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E Health. Epub. 2021 Feb 19 doi: 10.1089/tmj.2020.0575. [DOI] [PubMed] [Google Scholar]
- 9.Haque SN. Telehealth beyond COVID-19. Psychiatr Serv. 2021 Jan 1;72:100–103. doi: 10.1176/appi.ps.202000368. [DOI] [PubMed] [Google Scholar]
- 10.Uscher-Pines L, et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. 2021 Mar 16;325:1106–1107. doi: 10.1001/jama.2021.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moran M. CMS lifts restrictions on telehealth for psychiatry, other services to meet COVID-19 challenge. Psychiatr News. Epub. 2020 Mar 25 [Google Scholar]
- 12.Kroenke K, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Bush K, et al. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998 Sep 14;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 14.Simon GE, et al. Risk of suicide attempt and suicide death following completion of the Patient Health Questionnaire depression module in community practice. J Clin Psychiatry. 2016;77:221–227. doi: 10.4088/JCP.15m09776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Posner K, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stanley B, et al. Brief intervention and follow-up for suicidal patients with repeat emergency department visits enhances treatment engagement. Am J Public Health. 2015;105:1570–1572. doi: 10.2105/AJPH.2015.302656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998 Apr 30;17:857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 18.McGinn MM, et al. Recommendations for using clinical video telehealth with patients at high risk for suicide. Psychiatr Clin North Am. 2019;42:587–595. doi: 10.1016/j.psc.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Luxton DD, et al. Suicide risk management during clinical telepractice. Int J Psychiatry Med. 2014;48:19–31. doi: 10.2190/PM.48.1.c. [DOI] [PubMed] [Google Scholar]
- 20.Brock SE, et al. Conducting school suicide risk assessment in distance learning environments. Contemp Sch Psychol. Epub. 2021 Jan 4 doi: 10.1007/s40688-020-00333-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Action Alliance for Suicide Prevention. COVID Guidance: Screening for Suicide Risk During Telehalth Visits. 2020. Accessed Apr 25, 2021. https://theactionalliance.org/sites/default/files/covid-suicidescreentelehealth_3.pdf.