Abstract
Acute risk of death by suicide manifests in heightened suicidal ideation in certain contexts and time periods. These increases are thought to emerge from complex and mutually reinforcing relationships between dispositional vulnerability factors and individually suicidogenic short-term stressors. Together, these processes inform clinical safety planning and our therapeutic tools accommodate a reasonable degree of idiosyncrasy when we individualize interventions. Unraveling these multifaceted factors and processes on a quantitative level, however, requires estimation frameworks capable of representing idiosyncrasies relevant to intervention and psychotherapy. Using, data from a 21-day ambulatory assessment protocol that included six random prompts per day, we developed personalized (i.e., idiographic) models of interacting risk factors and suicidal ideation via Group Iterative Multiple Model Estimation (GIMME) in a sample of people diagnosed with borderline personality disorder (N=95) stratified for a history of high lethality suicide attempts. Our models revealed high levels of heterogeneity in state risk factors related to suicidal ideation, with no features shared among the majority of participants or even among relatively homogenous clusters of participants (i.e., empirically derived subgroups). We discuss steps toward clinical implementation of personalized models, which can eventually capture suicidogenic changes in proximal risk factors and inform safety planning and interventions.
Keywords: suicide risk, borderline personality disorder, idiographic models, Ecological Momentary Assessment, Group Iterative Multiple Model Estimation
It is hard to know when a suicide will occur. For one, risk is a dynamic state that dramatically fluctuates over time (Kleiman et al., 2017), and even chronic suicidal thoughts do not necessarily imply a continuous state of crisis. A person who endorses no suicidal thoughts during an assessment may feel substantially different shortly thereafter (Linehan et al., 2012; Rudd et al., 2006). Moreover, the reasons for why a person may decide to take their life are deeply personal (e.g., Stanley et al., 2009). In his book “The Savage God,” motivated by the death of his friend Sylvia Plath, Alvarez (p. 123, Alvarez, 2013) describes how suicidal crises emerge from a variety of possible functional constellations by noting: “A suicide’s excuses are mostly by the way. At best they assuage the guilt of the survivors, soothe the tidy-minded and encourage the sociologists in their endless search for convincing categories and theories. (…) The real motives which impel a man [SIC] to take his [SIC] own life are elsewhere; they belong to the internal world, devious, contradictory, labyrinthine, and mostly out of sight.” These words resonate with the clinical intuition that the processes leading to this most personal of acts vary considerably across individuals (Rudd et al., 2006).
Because of this unpredictability, clinicians often refuse to accept suicidal patients, refer those that become suicidal, or even terminate care with patients who attempt suicide after contractually agreeing not to do so (Linehan et al., 2012; Stanley & Brown, 2012). Many clinicians feel responsible for the lives of their patients and fear liability risks as well as the traumatizing impact of losing a patient to suicide (Linehan et al., 2012; Sandford et al., 2020), and find little comfort in a research on risk factors that oftentimes do not help in clinical decision-making (Burger et al., 2020).
Although many researchers call for a shift toward proximate antecedents of emergent suicide risk (Rudd et al., 2006; Kleiman & Nock, 2018), empirically suicide risk is generally estimated as a weighted sum or multiple of largely dispositional risk factors. To date, few studies examine the hypothesized precipitants of suicide over clinically meaningful time frames (Franklin et al., 2017). Even fewer examine the multifaceted, often mutually reinforcing processes that precede a suicidal crisis via estimation frameworks that can potentially inform intervention and psychotherapy (Millner et al., 2020).
The idiographic (N=1) approach, in which intensive longitudinal data are collected from one individual and then used to develop a personalized statistical network model (Beltz et al., 2016; Fisher at al., 2017; Haynes et al., 2009; Wright & Woods, 2020), may meet these needs. This is because such models capture the dynamic and multidimensional human experience: Information about a person’s thoughts, feelings, behaviors, and the contexts within which they manifest, can be sampled repeatedly in their daily life, enough times that they can be used to build an individual model on the interrelationships between each of those components. Broadly, network models refer to systems of interrelated components (Bringmann, 2021). Thus, by capturing the current level of suicidal ideation and/or intent, along with hypothetical risk factors, a statistical network model may help reveal unique patterns of interconnections (i.e., edges/links) among predictors (i.e., nodes) of suicidal risk (Bringmann, 2021; Molenaar, 2009; Robinaugh et al., 2020; for an overview see Wright & Woods (2020)). Because these associations emerge from the pattern of fluctuations in variables across time and context, they can be used to infer the processes of an individual’s acute risk of death by suicide in a given moment/situation. Clinically, the examination of these interrelationships is key to the generation and articulation of hypotheses about the exacerbation and maintenance of clinically relevant symptomatology (Persons, 2012). As our case examples will illustrate, suicidal intent may closely follow a relational conflict for person A, but for person B it is more likely to occur during episodes of extreme tension and despair.
It is plausible that idiographic models — relative to nomothetic approaches — provide a tighter connection between psychological assessment and intervention as well as psychotherapy (Haynes et al., 2009; Millner et al., 2020). They can generate personalized short-term functional models of suicide risk that fundamentally resemble clinical case formulation. The broad elements of clinical case formulation include assessment to obtain a diagnosis and form etiological hypotheses about the development and maintenance of the underlying symptomatology (Haynes & O’Brien, 2000). At the core of a case formulation lies a hypothetical framework of expected functional relations between symptoms and potentially causal variables. This formalization of intraindividual relations among risk factors is key for the development of an empirically-based yet tailored treatment rationale, addressing the most significant symptoms of an individual (see Persons (2012) for a more detailed overview). Therefore, in suicide prevention research and practice, personalized network models have the potential to aid safety plan construction and reevaluation (Linehan et al., 2012; Stanley et al., 2009).
A small but growing body of research demonstrates how these hypothesized relations can be empirically tested in person-specific analyses of intensive longitudinal data (Mumma & Fluck; 2016; Rath et al., 2019; Wright & Zimmermann, 2019). Traditionally, however, idiographic modeling has been rare in systematic clinical research because it was cumbersome and difficult to integrate across any reasonably large group of subjects. That is, because this approach requires developing a statistical model for each individual, as many models as subjects must be estimated. And, given the potentially high complexity (i.e., many plausible associations), how can each of these be compared and integrated across individuals? This is especially important because any common signal that emerges frequently across participants would be a candidate clinical target. Without effective ways to increase ease and comparability across idigraphic models, the approach seemed unable to produce much in the way of generalizable inferences.
Recently, however, group iterative multiple model estimation (GIMME; Gates & Molenaar, 2012; Lane et al., 2020) was developed to address these concerns. It does so by enslisting algorithms that (a) perform automatic model building for each individual, while (b) searching for commonalities among individuals. The essence of the GIMME procedure is that while it automatically estimates person-specific or idiographic models, it also searches for commonly occurring features (e.g., regression paths among two variables present in the majority of participants) across models within a group of participants. If it identifies common features, it prioritizes those features by building them in to everyone’s model as it iterates through everyone’s personal model again.
This aspect aligns with the the structure of standardized treatments which usually consist of elements that are the same for all patients (e.g., fixed modules in DBT, Linehan, 1993; Collaborative Assessment and Management of Suicide Risk, Jobes et al., 2016; Unified Protocol, Barlow et al., 2017), but also permit reasonable degrees of freedom to accommodate idiosyncrasies in suicide risk (Hofmann & Hayes, 2019).
Thus, GIMME is a promising approach for harnessing within-person variability in states as well as between-person heterogeneity in processes that reflect amplified suicidal risk (Rudd et al., 2006; Wright & Woods, 2020). Of note, there has been long-standing interest in idiographic assessment and modeling in clinical psychology (Shapiro, 1961), and calls for the use of idiographic models in suicide research have existed for more than 15 years (Leenars, 2002; see Kleiman et al., (2019) for an overview). Personalized approaches in suicide research have been introduced in the context of qualitative suicide note analyses which were conducted to gain access to thought content, emotional states, and messages that were regarded important preceding a suicidal act (Handelman & Lester, 2007). Thus, the examination of idiosyncrasy in suicide risk is not new per se, but technological progress has provided us with the ability to collect assessments of suicidal ideation that are adequate for idiographic analyses (e.g., Wright & Woods, 2020).
Therefore, the goal of the present paper is to evaluate whether and how an idiographic approach might help narrow the persistent implementation gap between psychotherapeutic research and crisis intervention practice. For this purpose we illustrate how GIMME might provide a dynamic typology of suicidal risk, thus uncovering potentially idiosyncratic paths to suicidal behavior.
A Heterogeneous Phenomenon
Almost all key theories describe suicide as a multifactorial (Rudd et al., 2006), transitory, or quickly resolving state (Abramson et al., 2000; Klonsky & May, 2015; Rudd et al., 2006; Wenzel & Beck, 2008). At the same time, however, many theories of suicide have prioritized principles that are true of all individuals in a group (i.e., nomothetic principles; see Selby et al. (2014) for an overview of theories), fueling an agenda of clinical research that is dominated by a focus on “the suicidal person” (Brown et al., 2000)1. The abstract nature of broad constructs used in nomothetic research (e.g., negative affect, pain) would seem to allow clinicians to accommodate idiosyncrasy in symptom presentation. That is, most of these theories assume some level of similarity among individuals who are in a state of suicidal ideation, even when the triggers and mutually reinforcing dynamics governing its progression would seem to be barely comparable between two individuals. To illustrate the heterogeneity observed in clinical practice, we provide three case vignettes of individuals who have suffered from severe chronic states of suicidal ideation and engaged in lethal suicide attempts. We share these cases from our own practice to highlight the diversity of suicidal struggles in clinical settings2:
Case Example 1.
Person A was an undocumented refugee in their early twenties. They had served in the army of a middle eastern country during a civil war, where they described having seen “bad things” (e.g., captives being tortured, dismembered corpses). The loss of a comrade they were secretly in love with was the “the straw that broke the camel’s back.” Person A described that ever since their friend’s passing, they experienced recurrent, blurred memories of the traumatic events, felt deep despair and hopelessness. They constantly blamed themselves for the death of their secret love, suffered from severe states of suicidal ideation and engaged in self-harm. They were also very scared of being deported. They explained that since their military service they felt no one could understand them, nor could they recognize themselves anymore. They further reported a persistent state of tension and irritability. Often, they would react with disproportionate intensity, especially during conflicts with their partner or family, but also during seemingly insignificant events. They slept about 2-3 hours a day and were plagued by nightmares during which they reexperienced traumatic war events. They reported intrusions where they found themselves back in the war that were triggered by everyday stimuli, and thus avoided people, places, or activities that brought back memories of this time. The experience of uncontrollable flashbacks, danger, self-alienation, and the grief about the loss of their everyday life in their home country, in combination with the stressors associated with the burden of living as a refugee further contributed to severe episodes of suicidal exacerbation. Person A reported that since their arrival in the new country they had twice attempted suicide, both times in response to a conflict with significant others, and both times they were rescued by their partner.
Case Example 2.
Person B was a 50-year-old divorced person, living alone in small apartment. They were on disability for longstanding psychiatric problems and previously in therapy for depression, though they carried a primary diagnosis of borderline personality disorder. They longed for a return to “feeling joy” in their life, and despite having an engaging and inviting interpersonal style they expressed a desire to foreclose on future romantic relationships by becoming a nun and were actively seeking to join a convent. They also had a significant history of self-harm and prior suicide attempts, reflected in scars she revealed on their wrists. They kept an Exacto knife, a boxcutter, and straight razor blades in their apartment. The initial several sessions of the therapy involved a progression of increasingly severe self-harm each week, culminating in 50-100 deep lacerations that crisscrossed her torso, at which point they agreed to enter the hospital. Following discharge from this hospitalization, B’s progress in the therapy was considerable and sustained, though punctuated by bouts of great despair following interpersonal or professional setbacks. During these periods, they would often feel like they were “going crazy” and contemplate suicide. Indeed, B described their suicidal thoughts as a great comfort, because “I know that no matter how bad it gets, I can always take my own life.”
Case Example 3.
Person C was recently discharged from the hospital following an involuntary commitment due to suicidal ideation with a plan and intent. They too carried a diagnosis of borderline personality disorder. They lived with their parents, attending a large public university in their hometown. Their parents, though supportive of their child’s education and career, were very religious people who insisted on strictly following rules of dress and behavior. C found them overbearing and wanted to live like other college students. They would not placate her parents’ desire for them to adhere to the religious edicts, arguing with them about the logic and perceived hypocrisy of the rules. Their relationship became strained. C often felt socially awkward, alone, and that they did not belong. They also expressed a chronic desire and willingness to take their own life at each session with the therapist. Their desire to end their life at times subsided, but family conflict triggered acute elevations in suicidal intent and behavior. Despite fundamental disagreements about values and her life choices, they revered their parents and the conflict made them feel guilty and that they were a failure. After moving out of their family’s home to live with a family friend in an effort to reduce the conflict, they took about 50 antihistamine pills with no serious consequences. They then purchased 600 of the same pills, and before one of the last sessions before transitioning to a new therapist, they took the majority of these in the clinic bathroom, resulting in a coma and hospitalization. Their extreme and chronic suicidality continued through treatment with two more therapists before they ultimately took a fatal overdose.
Synthesizing Idiosyncratic Symptom Presentation with Theory and Research
Our case examples illustrate that the precipitants of suicide risk are heterogenous, often operate on very brief timeframes, and are governed by diverse functional interrelations, even among those with the same primary diagnosis. For A it was an overwhelming state of agitation, despair, and self-alienation that suddenly and disproportionately exacerbated in interpersonal conflicts with close others and that was maintained by an enduring insecurity about his permanent residency and personal safety in turn. For B suicidal thoughts would grip her during bouts of despairing rumination about feeling stuck in her situation and the perceived futility of making big changes in her life. Whereas, for C. familial conflicts would leave her feeling guilty and alone, which would inflame her chronic suicidal thoughts, and catalyze her to act on them.
Despite their predominant focus on nomothetic principles, all major theories of suicide emphasize brief timescales in more or less obvious ways. Joiner’s interpersonal theory (2005) proposes that suicidal desire develops through interactive effects of perceived burdensomeness, thwarted belongingness, as well as hopelessness about these beliefs. Although the Three-Step Theory (Klonsky & May, 2015) similarly posits that connectedness is a key driving force for the progression of suicidal ideation, it features instances of strong negative affect and hopelessness as major risk factors, which accounts for the heterogeneity of causes for suicidal ideation more clearly. The heterogeneity in causes and functional constellations of suicide risk makes it difficult to establish when and why it will spike in different people.
Conceptualizing suicide risk as a dynamic behavioral system has important implications for suicide intervention or prevention strategies that have traditionally been based on the formalization of suicide risk as a continuum (Cha et al., 2018; Zalsman et al., 2016). These works generally understand suicide risk to range from the presence of suicidal thoughts, nonfatal suicidal behavior, to death by suicide (Siddaway et al., 2021). There are, however, empirical and conceptual reasons to suspect that the within-person progression of a suicidal crisis does not follow a strictly linear or uniform process (Siddaway et al., 2021). Rather, multiple pathways likely underlie superficially similar progressions (Bryan et al., 2020; Dombrovski & Hallquist, 2021; Szanto et al., 2018), and individually functional constellations of risk factors escalate abruptly rather than gradually (e.g., Bryan et al., 2016; Linehan et al., 2012; Millner et al., 2017; Nock et al., 2009). Empirically, various ambulatory assessment studies demonstrated that suicidal ideation is highly transient and dynamic, increasing and decreasing considerably over the course of a few hours (Kleiman et al., 2017; Nock et al., 2009). From a conceptual point of view, so-called “ideation to action” frameworks (Klonsky et al., 2018) explicitly distinguish between suicidal thoughts and suicidal behavior and imply the existence of a “tipping point”, potentially explaining abrupt changes or spikes in suicidality. In a related line of work, suicidal crises are thought to arise in the context of an intricate, multi-componential, self-reinforcing dynamic system (Rudd et al., 2006), as we see from subjective reports of patients who have attempted suicide (e.g., Wyder & DeLeo, 2007).
Synthesizing the complexities of individual symptom presentation with theory and research is key to case conceptualization and facilitates forming and refining working hypotheses about short-term precipitants of imminent suicide risk (Burger et al., 2020; Jobes, 2016; Linehan et al., 2012; Persons, 2012). At this point, an empirical framework that quantitatively systematizes the dynamics of emergent suicidal crises in an ecologically valid, and therefore clinically valuable, manner is needed. Related models may very well hold the key to informing our assessments of when and under what conditions suicidal crises are more or less likely to occur within one specific individual (Coppersmith et al., 2021). By extending this approach to many people, but allowing for heterogeneity, we have the potential to inform both theory and treatment in the long run by revealing scientifically applicable dynamics.
To bring this approach to life, appropriate data are needed. Sometimes referred to as ambulatory assessment, ecological momentary assessment, or experience sampling, intensive longitudinal sampling in naturalistic settings or real-time monitoring techniques are ideal for the study of suicidal progression (David et al., 2018; Haynes et al., 2009; Kaurin et al., 2020; Kleiman et al., 2017; Roche et al., 2014)3. Because of the repeated sampling of an individual, such data return more proximate estimates of relevant processes in a person’s daily life. This provides a data structure that permits personalized analyses via idiographic approaches (Bastiaansen et al., 2020), such as the above mentioned GIMME (Gates & Molenaar, 2012). When applied to momentary assessments of short-term risk factors suicide, GIMME generates multivariate person-specific estimates of the associations among risk factors and suicidal ideation (e.g., Wright & Zimmermann, 2019). At the same time, person-specific effects in GIMME are estimated alongside the identification of nomothetic features that may apply to the majority or at least a subgroup of the sample (Woods et al., 2020).
The Present Study.
Considering functional dynamics of suicide risk in a manner that is reflective of day-to-day clinical routine is vital to understanding the conditions under which suicidal thoughts and behaviors are more or less likely to occur. The present study applied a dynamic perspective on suicide risk and examined the interactive patterning among risk factors of suicide near to acute suicidal ideation in daily life.
Because this is the first study to articulate quantitative idiographic models of suicide risk, our overarching goal is to demonstrate how the GIMME approach may be applied to intensive longitudinal data of suicidal ideation. Thus, in line with previous studies (e.g., Dotterer et al., 2020; Woods et al., 2020; Wright et al., 2019), we view our analyses as exploratory and we did not anticipate specific group-level or subgroup-level effects. However, consistent with theoretical (e.g., Rudd et al., 2006; Klonsky & May, 2015) and empirical work on suicide risk (Kleiman et al., 2017), as well as past experiences using GIMME in several data sets (Beltz et al., 2016; Price et al., 2017) we anticipate a high degree of person-specific heterogeneity.
Our empirical demonstration is based on data from a 21-day ambulatory assessment protocol that features risk factors from the impulsivity, affect, and hostility (i.e., externalizing processes) domains in sample of people diagnosed with borderline personality disorder (BPD) that is enriched for a history of high-lethality suicide attempts. Likewise, this sampling strategy was chosen because serious suicidal thoughts are rare, episodic events, which likely manifest infrequently, even in a high-risk population. Both, BPD (Yen et al., 2021) and a history of suicide attempt are among the most powerful, nomothetic long-term predictors of lethal suicidal behavior (Christiansen & Jensen, 2007; Suominen et al., 2004). Thus, individuals with a history of high-lethality suicide attempts likely share characteristics and processes with those that died by suicide as the lethality of suicide attempts progresses with repeated attempts (Malone et al., 1995), and a history of multiple suicide attempts has been associated with more frequent and longer lasting high risk states (Bryan et al., 2015; Joiner et al., 2000).
Method
Written informed consent was obtained prior to participation. Study procedures were approved by the Institutional Review Board of the University of Pittsburgh (STUDY19050210).
Participants
The sample used in this study was collected as part of a project designed to investigate short-term precipitants of suicidal ideation in daily life among individuals diagnosed with BPD. More detailed information about recruitment, sample characteristics and the sampling strategy for enhanced suicide risk can be found in Kaurin et al. (2020), which used this same sample. Originally, this sample consisted of 153 individuals diagnosed with BPD and 52 healthy control (HC) participants (Mage: 33.62, SD=9.60; 81% female). HCs, however, were excluded for the purpose of the present paper (see below). Of these 153 individuals with BPD, n=105 had a history of suicide attempt (BPD-ATT group) and n=48 reported no past suicide attempts (BPD-NON group) but frequent instances of suicidal ideation. Among all participants, 79% identified as White, 1.3% Asian, 9% Black or African American, and the rest identified as more than one or another race.
In line with recommendations from simulation studies of GIMME’s ability to recover group and individual paths (Lane et al., 2020), only participants with at least 60 completed EMA queries were included in the current analyses (M=126.33; range: 60-171). We further excluded participants with no variance on at least one of the variables of interest (e.g., no variability in suicidal ideation in HCs) because variability is needed to calculate associations at the person level. This resulted in a total sample size of n=95 (nBPD-ATT= 70)4.
Procedure
Participants completed a 21-day EMA protocol within pre-defined time windows. They received 6 random surveys per day via push notifications, which were delivered over a 12-hour period via the MetricWire Version 4.2.8 (2019) smartphone application. Assessments were aligned with participants’ typical waking hours, which they specified prior to enrollment in the study. The random assessments were spaced apart by a minimum of 90 minutes, and participants were given 60 minutes to respond to each prompt.
Participants rated the degree to which they felt internalizing negative affect (i.e., mean of sad, nervous, guilty, ashamed; ωwithin=.80; ωbetween=.94), hostility (i.e., mean of anger, irritability; ωwithin=.78; ωbetween=.93), and positive affect (i.e., mean of happy, content, excited; ωwithin= .74; ωbetween=.84). Items were derived from the Positive and Negative Affect Schedule (Watson et al., 1988), read “How [AFFECTIVE STATE] did you feel right now?”, and ratings were made on a scale from 1 (“Not at All”) to 5 (“A great deal”).
Items from the Comprehensive Assessment of Traits Relevant to Personality Disorder (CAT-PD; Wright & Simms, 2014) were adapted to reflect momentary features of impulsivity. To cover the construct comprehensively, we selected items from key subscales of the disconstraint domain, including irresponsibility (“I said/did things that I wish I hadn’t”), non-planfulness (“I acted without thinking”), and risk taking (“I did something risky”). All three items were rated based on the same 5-point scale as affect and were averaged to form an impulsivity score (ωwithin= .80; ωbetween= .95).
Suicidal ideation was assessed with two dichotomous items (1=yes, 0=no) derived from the suicidal ideation subscale of the Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2008). The two items were used to form an average score of suicidal intent severity, and read as follows: “Have you wished you were dead or wished you could go to sleep and not wake up?”, “Have you actually had any thoughts of killing yourself?” (ωwithin= .83; ωbetween= .67).
Data Analytic Strategy
Personalized models of acute suicide risk (suicidal ideation, hostility, negative and positive affect, impulsivity) were estimated using the “gimmeSEM” function built into to the R package gimme (version 0.7-4; Lane et al., 2020). The GIMME algorithm uses data-driven model searches to estimate unified structural equation models (uSEMs; Gates et al., 2010) among a set of observed variables that are assessed repeatedly within one individual. uSEMs represent combination of traditional SEM and vector autoregressive (VAR) model. VAR models are based on a sequential algorithm, where lagged relations are estimated first, followed by the identification of contemporaneous relations based on the covariance matrix of the residuals (Lütkepohl, 2005). In contrast, uSEMs identify both lagged and contemporaneous relations simultaneously. This has the advantage that results are independent of the order in which the variables were fed into the algorithm (Molenaar & Lo, 2016; for a more detailed comparison of personalized network modelling approaches please see Beltz & Gates, 2017).
GIMME proceeds in an iterative fashion. First, idiographic uSEM models are estimated from each participant’s time series data. Parameters are added to each model (e.g., contemporaneous or lagged regression paths) on the basis of improvement in model fit (i.e., modification indices or Lagrange multiplier tests), such that parameters that lead to the most improvement are added until no parameter significantly improves model fit. Next, based on the results of those individual models, GIMME identifies any paths that are common among the group of individuals (e.g., 75% of individuals by default), and re-estimates each model with these paths freely estimated by default. This is repeated until no further “group-level” paths are identified, and then each idiographic model is finalized. Autoregressive paths are estimated by default (rounded arrows in Figure 1A). It is important to note that GIMME models are estimated separately for each individual, and therefore even the strength of group-level paths are unique to each uSEM. These personalized uSEMs identify the structure of significant associations (i.e., paths) along with their estimated regression weights at both group and individual levels. The GIMME algorithm has been tested with a minimum of 5 to a maximum of 15 variables and shown to perform well in this range of nodes (Lane & Gates, 2017). Thus, the resulting uSEMs from GIMME can be conceptualized as networks of associations for each individual that also identify which paths are common to the group.
Figure 1.
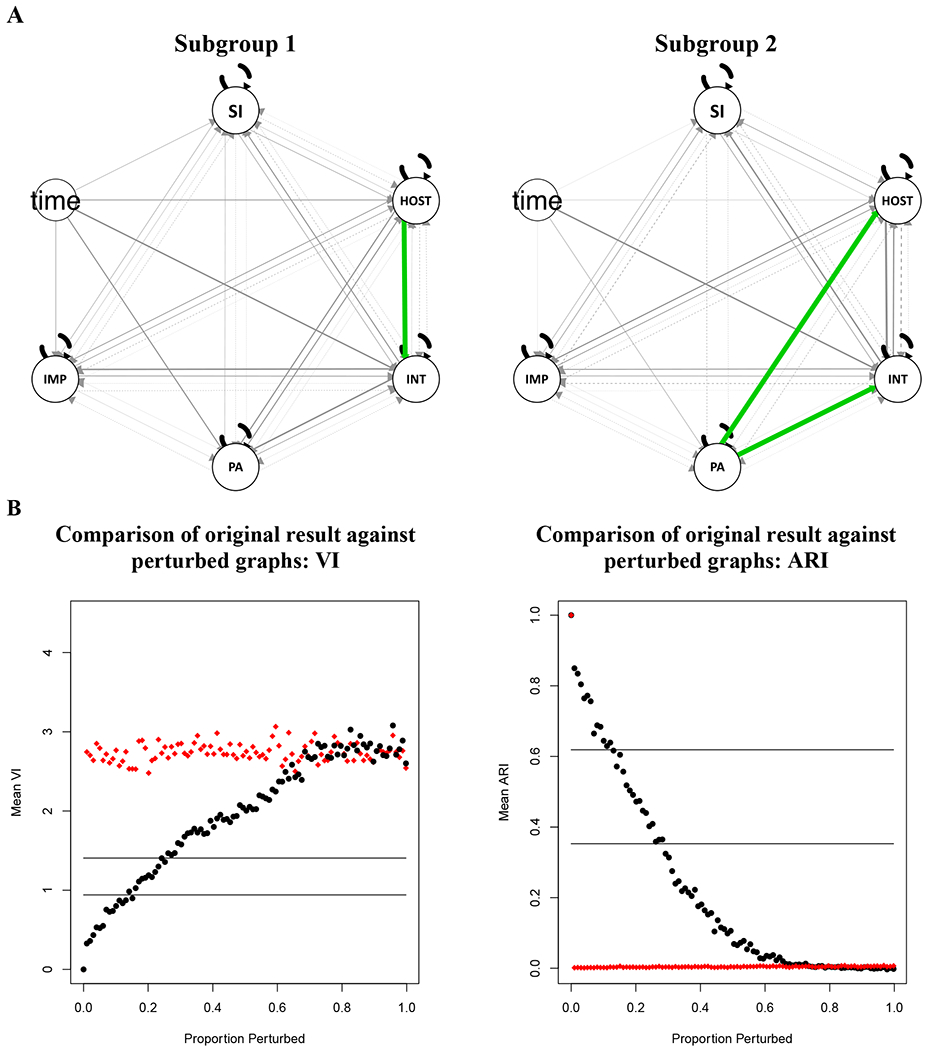
A: Depiction of subgroup- and individual-level paths assessed via GIMME. SI = suicidal ideation; HOST = hostility; INT = internalizing negative affect; PA = positive affect; IMP = impulsivity; Grey paths represent individual-level estimates and green paths subgroup-level estimates. Line thickness corresponds to the number of individuals that share the same path proportionate to the total group size. Contemporaneous effects are represented with solid lines, and lagged effects are represented with dashed lines. B: Subgroup validation results based on VI and ARI. The horizontal lines indicate difference between solutions where 10% (bottom) and 20% (top line) of the nodes are randomly switched to different clusters. Black dots represent the perturbed graph based on the original clustering solution; red rhombi represent a perturbed random graph.
We used an extension of GIMME that identifies subgroups who share similar patterns in their individual networks. To obtain subgroups, a similarity matrix is generated and a community detection algorithm is used (Walktrap; Pons & Latapy, 2005) to place individuals into subgroups based on whether they share similar estimates and patterns of effects. When this feature is invoked, the iterative process proceeds within each subgroup with the potential to identify subgroup-level paths if they exist. As with the group-level paths, if identified, sub-group paths are incorporated in all subgroup members’ models. The default for identifying sub-group paths is 50%, indicating that a path must be significant in 50% or more of the individual models in a subgroup in order for it to be included as a subgroup-level path. In the current study, we estimated GIMME models using the default cutoffs for both group and subgroup-level paths.
To evaluate the robustness of our recovered subgroups, we used the R (R Core Team, 2017) package perturbR (Gates, Fisher, & Arizmendi, 2018). Results obtained from these sensitivity analyses indicate the degree to which the subsets are susceptible to change or solutions are sensitive to minor modifications of the network. The underlying algorithm incrementally adds noise to network edges (i.e., randomly shuffles a specific proportion of edges to rewire the original matrix) while keeping the initial graph’s general features and compares resulting subgroup solutions with the solution for the original network. That way, a distribution of gradually perturbed matrices is achieved, which can be used to plot the degree of similarity for the subgroup solutions found in the original matrix and rewired matrices across all increments of perturbation. A subgroup solution is considered stable if the graph had 20% or more of its edges perturbed before the cluster solution for the rewired graph is as different as when 20% of the nodes are randomly placed into different clusters (Karrer et al., 2008). This criterion is quantified by two complementary indices. Both provide a metric of the degree to which two community solutions differ: Hubert-Arabie Adjusted Rand Index and Variation of Information (see Gates et al. (2019) for details on computational steps common and distinct to both approaches).
The validity of the uSEM and GIMME frameworks rests on several key assumptions, including the assumption of “weak stationarity” of the time series (i.e., a constant mean, variance, and covariance; Beltz et al., 2016). These assumptions may be violated in certain empirical data sets including the dataset reported here. Thus, to guard against the possibility of non-stationarity we used the gimme R package’s (Lane et al., 2020) exogenous variable feature to adjust for the effects of time (i.e., detrend) in our path estimates.
Power for GIMME models involves consideration of the individual-model paths as well as the group-level paths. Power for individual-model paths follow the logic of traditional power analyses, such that the sample of the individual’s time-series is presumed to be a random sample from the population of their behavior. Thus, the power for this effect can be calculated as the power to detect a regression path for a sample the size of the length of the observed time-series (i.e., given that the standard path used in GIMME are regression paths). Given that there are 95 individuals in our study across which the numbers of observations vary, we calculate that we have .80 power to detect an effect of size f2 = .063 for the average time series length (N observations=126), with a range of f2 =.135 for the individual with the fewest observations (N=60) to f2 = .046 for the individual with the largest (AR=171). Here the target population shifts from the observation within a single individual to the observations across individuals. That is, if there is a true effect present in the population from which the individual models are drawn, then each individual model serves as a repeated sampling of that population. So, if one had power of .80 to detect a true effect of a given size in the population, then one would expect it to be present in 80% of the individual models. GIMME’s default of 75% presence (i.e., significant effect) of group-level paths is therefore close to the number of models in which a significant effect would be expected to be found for .80 power, though with a cushion in favor of finding a group-level path. Note that these observed effects can still vary, potentially significantly from each other, and a moderately large proportion (25%) might be non-significant and still the conclusion would be there is a group-level effect. If the threshold is not met, then one can conclude that these effects are likely heterogeneous among individuals, or at least not drawn from one population given a particular effect size and level of power. In the case of subgroups, as Henry et al. (2019) describe, the threshold has been lowered by convention (50%) because often subgroups are small, and a 75% threshold would effectively require all or almost all individuals have an effect.
For readers interested in a more comprehensive introduction into GIMME, we recommend consulting Gates & Molenaar (2012) for a detailed overview of the underlying algorithm, or Lane & Gates (2017), or Wright et al. (2019) for accessible tutorials. All gimme input syntax, individual data files, output files, and diagrams are available at the https://osf.io/t8umy/.
Results
The goal of this presentation is not to interpret every possible parameter in detail, but rather to demonstrate how such models may be used in a clinically intuitive manner. Thus, many more interpretations are possible, but we will limit our elaboration to the purpose of this paper. To provide some context, on average prompts were spaced apart by two hours (i.e., 6 random assessments delivered in a 12-hour frame no less than 90 minutes apart), returning lagged effects of approximately the same length. This schedule sought to balance the burdensomeness of the EMA schedule with the goal of covering the majority of the waking hours, because the design could not be informed by a well-established sense of the actual duration of a suicidal crisis, which is still a matter of ongoing research as we discuss below.
The subgrouping algorithm also suggested that a majority (n=95) of participants could be grouped into 2 groups (n1=59; n2=36). According to the Variation of Information and Adjusted Rand Index the cluster solution attained was stable and valid (Figure 1B). Based on the Variation of Information, approximately 26% edges had to be perturbed before 20% of participants were placed into different clusters than the original solution. This is visualized on the left side of Figure 1B, where the black circles cross the upper horizontal line. Moreover, the examination of the average Adjusted Rand Index at the 20% perturbation point indicated that the solutions at this point of perturbation were, on average, more similar to the original solution (average index=.47) than when 20% of the cluster assignments are randomly swapped (Adjusted Rand Index=.35). A one-sampled t-test returned that this difference was significant (t=5.99, p=<.001). Overall, this pattern provides evidence that our recovered subgroup solution was robust.
Both subgroups were found to have significant contemporaneous associations between affective network nodes, but no exploratory group- or subgroup-level paths emerged that were directly linked to suicidal ideation attesting to the heterogeneity of specific features of suicidal ideation across individuals. For participants in the first subgroup (left side of Figure 1A), we found one shared path, negative affect regressed on hostility. For participants in the second subgroup (right side of Figure 1A) we found two shared paths, hostility and negative affect regressed on positive affect. Thus, for a subset of individuals (e.g., 126, 141) positive affect seemed to serve a protective role in the emergence of negative affective states which were linked to suicidal ideation. Even if not directly linked to suicidal ideation, descriptively, this is important information, because therapeutically, the induction of positive affective states may represent an important mechanism for crisis intervention. To provide a comprehensive overview of estimated paths, Figure 1A depicts individual (grey) and group-level (black) paths (note, the autoregressive paths are estimated a priori as group-level paths). In addition to the visual presentation of results, Table 1 contains two matrices that summarize the number of individual models that included each path, in Table 2 this overview is broken down by subgroup. Summary matrices are informative, as they illustrate that certain paths are much more common than others, even if they do not rise to the level of subgroup or group paths.
Table 1.
Number of individuals with significant contemporaneous and lagged paths.
| Contemporaneous Paths | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| suicidal ideation | hostility | negative affect | positive affect | impulsivity | time | |||||||
|
| ||||||||||||
| suicidal ideation | 0 | 7 | 21 | 4 | 7 | 6 | ||||||
| hostility | 8 | 0 | 11 | 47 | 12 | 11 | ||||||
| negative affect | 10 | 74 | 0 | 43 | 12 | 28 | ||||||
| positive affect | 0 | 13 | 19 | 0 | 3 | 15 | ||||||
| impulsivity | 8 | 16 | 23 | 2 | 0 | 8 | ||||||
|
| ||||||||||||
| Lagged Paths | ||||||||||||
| suicidal ideation | hostility | negative affect | positive affect | impulsivity | ||||||||
|
| ||||||||||||
| suicidal ideation | 95 | 1 | 6 | 4 | 8 | |||||||
| hostility | 6 | 95 | 6 | 5 | 4 | |||||||
| negative affect | 8 | 12 | 95 | 4 | 5 | |||||||
| positive affect | 6 | 4 | 4 | 95 | 2 | |||||||
| impulsivity | 5 | 7 | 6 | 5 | 95 | |||||||
Note. Column variables are predictors of row variables. The diagonal of the lagged paths matrix represent autoregressive effects, which are estimated by default.
Table 2.
Number of individuals with significant contemporaneous and lagged paths within subgroups.
| Subgroup 1 |
Subgroup 2 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contemporaneous Paths | ||||||||||||
| suicidal ideation | hostility | negative affect | positive affect | impulsivity | time | suicidal ideation | hostility | negative affect | positive affect | impulsivity | time | |
|
| ||||||||||||
| SI | 0 | 3 | 11 | 4 | 3 | 5 | 0 | 4 | 10 | 0 | 4 | 1 |
| HOST | 6 | 0 | 2 | 11 | 7 | 9 | 2 | 0 | 9 | 36 | 5 | 2 |
| NA | 6 | 59 | 0 | 7 | 8 | 17 | 4 | 15 | 0 | 36 | 4 | 11 |
| PA | 0 | 13 | 18 | 0 | 2 | 12 | 0 | 0 | 1 | 0 | 1 | 3 |
| IMP | 5 | 8 | 17 | 1 | 0 | 7 | 3 | 8 | 6 | 1 | 0 | 1 |
|
| ||||||||||||
| Lagged Paths | ||||||||||||
| suicidal ideation | hostility | negative affect | positive affect | impulsivity | time | suicidal ideation | hostility | negative affect | positive affect | impulsivity | time | |
|
| ||||||||||||
| SI | 59 | 1 | 3 | 2 | 4 | - | 36 | 0 | 3 | 2 | 4 | - |
| HOST | 4 | 59 | 4 | 2 | 1 | - | 2 | 36 | 2 | 3 | 3 | - |
| NA | 5 | 5 | 59 | 3 | 4 | - | 3 | 7 | 36 | 1 | 1 | - |
| PA | 3 | 2 | 2 | 59 | 0 | - | 3 | 2 | 2 | 36 | 2 | - |
| IMP | 3 | 5 | 2 | 3 | 59 | - | 2 | 2 | 4 | 2 | 36 | - |
Note. Column variables are predictors of row variables. The diagonal of the lagged paths matrix represent autoregressive effects, which are estimated by default. SI = suicidal ideation; HOST = hostility; NA = negative affect; PA = positive affect; IMP = impulsivity;
To ease the interpretation of individual-level paths, Figure 2 provides a small selection of diagrams and illustrates the diversity of dynamic patterns in our data, and is amended by Figure 3 which provides descriptive data using a) kernel density plots, which illustrate average values and dispersion, b) time-series plots, which demonstrate the temporal sequencing of daily experiences, c) correlational heat maps, which convey the carryover from day to day among the various nodes as well as d) their interplay. A full overview of diagrams and path coefficients can be found under https://osf.io/t8umy/. Looking at each of these individual models reveals structural differences in the patterning of associations across their networks. We view these as reflecting each individual’s functional model constellation, that is, the ways in which multiple variables interact within an individual over time, including the clinical target suicidal ideation. This has the potential to uncover mechanistic hypotheses about momentary processes that govern suicide risk, which is similar to working models explored an interrogated with patients throughout therapy. In the following, we will discuss individual network models in a manner that we as clinicians would expect those to be discussed with patients in the consultation room. The goal of such discussions is to uncover plausible perpetuating principles for a person’s problem presentation. We do, however, acknowledge, that such interpretations are different from formal principles of causal inference. Thus, although the language might imply a certain degree of causation (e.g., increase), we would like to emphasize that the data structure is not suitable to validly uncover cause-effect relationships (Bringmann, 2021).
Figure 2.
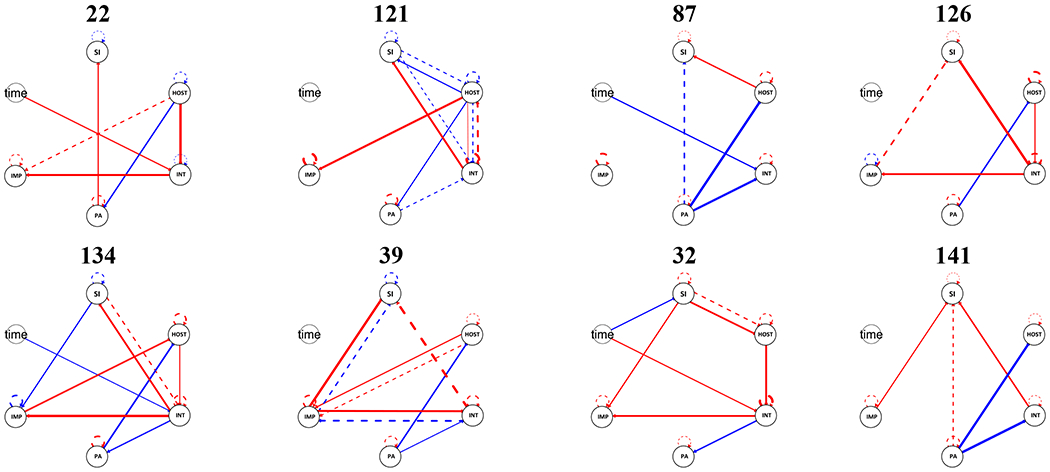
Sample diagrams of individual-level models from GIMME. SI = suicidal ideation; HOST = hostility; INT = internalizing negative affect; POS = positive affect; IMP = impulsivity; Contemporaneous effects are represented with solid lines, and lagged effects are represented with dashed lines. Positive effects are in red, negative effects are in blue. Line thickness denotes strength of effect.
Figure 3.
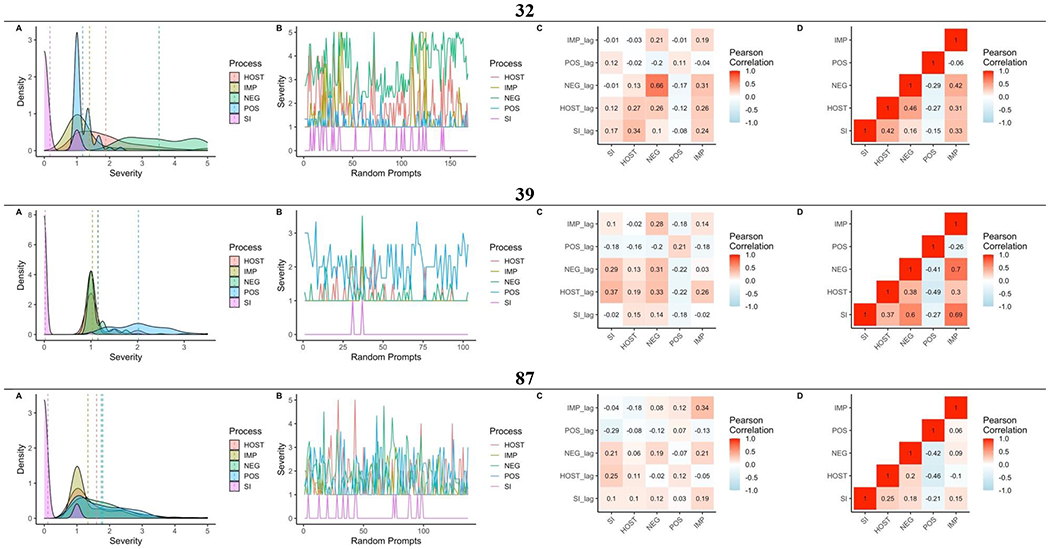
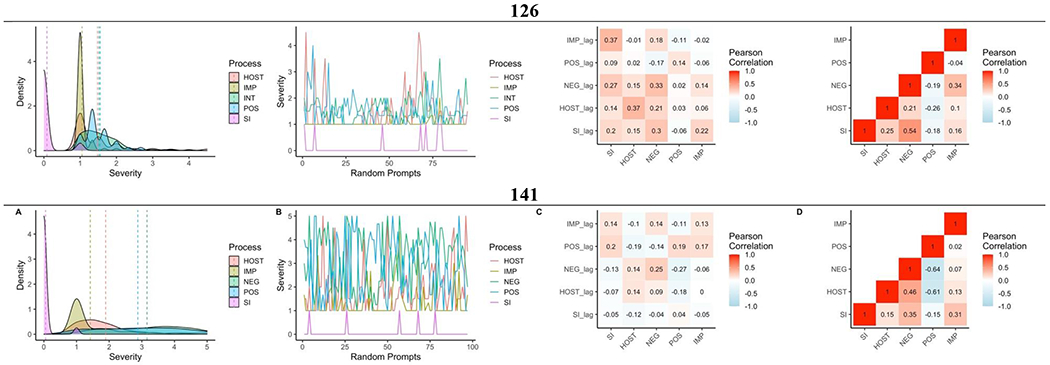
A: Kernel density plots with vertical dashed lines denoting mean values, B: time-series plots, correlation heat maps of C: lagged (diagonal reflects autocorrelation) and D: contemporaneous associations of daily assessed suicidal ideation (SI), hostility (HOST), negative affect (NEG), positive affect (POS), and impulsivity (IMP) for five participants.
One important finding from individual-level analyses was the difference in the strength and direction of autoregressive effects for suicidal ideation. For some individuals, we found positive autoregressive effects of suicidal ideation (e.g., 87 & 126 in Figure 2), indicating that ideation was relatively consistent across assessments after controlling for the influence of other variables in the model. That is, once these individuals started feeling suicidal, they had a tendency to “get stuck” feeling suicidal for some period. Indeed, the exemplary time series plot for participant 87 in Figure 3 is indicative of high-frequency periods of suicidal ideation (i.e., the person seems to be stuck in a suicidal crisis), that alternate with extended periods without any endorsements of ideation. For others, autoregressive effects of suicidal ideation were either smaller, or in the opposite direction (e.g., 134, 39). For those with a negative autoregressive association, this suggests a tendency to regulate away from a particular state from one assessment to another. It may, however, as exemplified for 39 in Figure 3, also be indicative of very few endorsements of suicidal ideation. This overall pattern suggests that there is large variability across participants in how well current assessments of suicidal ideation may be predicted by previous ones on the same schedule.
Another relevant finding emerges from the fact that personalized models generally differed in their density and structure regarding dynamic links among observed variables. For some individuals more significant paths emerged than for others (e.g., participant 126 vs. participant 121 in Figure 2). For example, it appears that for participant 121, affective, hostile and impulsive and suicidal processes are more interwoven, whereas for participant 126 these variables are more separable in their dynamics and dominated by experiences of hostility.
It is also important to note that across our individual-level models, no variable appeared to be of consistent central importance; that is, none had a consistently higher number of links to other variables. A pattern of centrality may allow inferences about risk factors that are more relevant for the unfolding suicide risk sequences, though the exact meaning of centrality in psychological networks is a fraught topic (Bringmann et al., 2019).
As we alluded to above, although some individuals share links between the same two variables, these effects are part of distinct overall patterns of associations. For instance, for participants 126 or 141, experiences of negative affect generally coincided with greater suicidal ideation (see time series in Figure 3 for an illustration of how both processes track together across time), whereas for participant 39 effects of negative affect carried over from assessment to assessment, and for participant 121 these carry-over effects went in the opposite direction. More generally, suicidal ideation in participant 121 seemed to be governed by a reciprocal dynamic between suicidal ideation and negative affect where experiences of negative affect tended to coincide with higher levels of suicidal ideation, but lagged assessments of suicidal ideation would predict lower levels negative affect. This may be indicative of a regulatory circle, within which suicidal contemplation may ease experiences of negative affect (much like Ms. B above). A similar dynamic presents in participant 134, where negative affect coincided with enhanced suicidal ideation. At the same time, however, negative affect was linked to hostility and impulsivity, which could be indicative of an escalating system, where especially impulsive and – to a lesser degree – hostile acts would be associated with negative affective experiences, which would increase levels of suicidal ideation in turn.
In contrast, participant 39 exhibits a regulatory process between hostility and impulsive behaviors, such that increases in anger would be associated with more impulsive behaviors, which in turn predict levels of negative affect and, with some temporal distance, elevated suicide risk. Participants 87 and 32 also exhibit patterns suggestive of a transactional process between hostility and suicidal ideation, however, to different extents. Moreover, for participant 87 hostility seems to function as a way to cope with lowered levels of positive affect, which would coincide with hostility and contribute to suicide risk in a lagged manner.
Beyond functional relationships among the variables, we also observed variability in the estimates for the paths between affect and suicidal ideation (see also Figure 3). Although all individuals depicted in Figure 2 had positive estimates the link between suicidal ideation and negative affect, participant 141 has a notably smaller value (as indicated by thinner lines) compared to participant 134. Other models share several features such as a negative link between positive and negative affect or hostility (126, 134, 39), but also display substantial structural und functional differences.
Discussion
Suicide represents different things for different people at different times in their lives. For A. it was a desperate escape from trauma, loss and insecurity; for B it was solace when it life felt unbearable and overwhelming; for C it was struggles with identity and striving for autonomy punctuated by conflict with those closest to her. This notion of idiosyncrasy in suicide risk is widely discussed in the clinical literature and well-reflected in our data. In our models, within-person dynamics of suicide risk were characterized by a high degree of heterogeneity, as evidenced by the absence of shared paths related to suicidal ideation across individuals or even subgroups of similar patterns (see Figure 2 for a partial illustration of this finding). This is noteworthy, because our data illustrate that even the most frequently reported nomothetic risk factor for suicide, negative affect (Abramson et al., 2000; Joiner, 2005; Linehan, 1993; Shneidman, 1993), is likely not equally relevant for all individuals for suicide risk in the moment.
Our findings add to previous research on real-time assessment of suicidal thoughts and behaviors (see Kleiman & Nock (2018) for an overview) in that we demonstrate that even among those who share a link between affect and suicidal thoughts this nexus is likely governed by different functional constellations (see 143 vs. 39 in Figure 2). Similarly, we also found that the magnitude of autoregressive effects differed across individuals in their strength and direction, which suggests individual differences in the recovery from states of high risk for suicide. The fact that the magnitude of carry-over effects from one episode of suicidal ideation to the next may vary considerably across individuals, has implications for assessment schedules of real-time monitoring protocols of suicide risk (e.g., number and spacing of prompts; choice of event-contingent vs. random assessment schedules).
Although both findings need to be interpreted with caution, they also offer a possible reinterpretation of previous findings that suggest limited predictive validity of well-known, nomothetic risk factors for short-term changes in suicidal ideation (Ben-Zeev et al., 2012; Kleiman et al., 2017). It is likely not that they are not informative, just not informative for all individuals, only some. This shifts the fundamental question we need to be asking from which risk factors are predictive for most individuals, to which are the most predictive risk factors for a given individual. Identifying highly individualized mechanisms across a range of precipitants allows us to accommodate the heterogeneity of risk, and each personalized network invites comprehensive analyses and interpretations, just as is commonly done in therapy. As noted above, we would miss crucial pieces of information about any of our case example protagonists’ precipitants of suicide risk if we applied only what we knew about general risk factors at the population level.
However, the majority of existing interventions for suicide risk are not designed to be delivered at a frequency that matches abrupt changes in suicidal ideation and nor are they tailored to the heterogeneous nature of suicide (Cha et al., 2018; Coppersmith et al., 2021; Zalsman et al., 2016). The ability of network depictions to provide a nuanced overview of functional relationships across risk factors is compelling, and from an empirical point of view, personalized models have been celebrated for their potential clinical utility (Fisher & Boswell, 2016; Kroeze et al., 2017; Piccirillo & Rodebaugh, 2019; Robinaugh, Brown, et al., 2020; van der Krieke et al., 2015; Zimmermann et al., 2019). Because suicide risk is often uncertain and unpredictable, person-specific time series models of suicide risk may offer both the patient and therapist a quantitative tool that is useful to increment safety planning. At the same time, emerging evidence suggests that it is more likely patients that might see value in these models, whereas clinicians express doubts as to whether idiographic models would provide incremental information over and above insights generated in the therapeutic process (Frumkin et al., 2020; Zimmermann et al., 2019). Moreover, because personalized network models provide a quantitative articulation of functional relations between risk factors and suicidal ideation, other assessment data key to therapy such as mean-levels and degree of given behaviors are not provided and need to be supplemented just like we did in Figure 3. It, thus, remains an open empirical question whether the use of idiographic models like the ones we estimated here could be practically useful for improving the effectiveness of our interventions.
In addition to the potential barrier of practitioner skepticism, the quest for tractable idiographic models encounters conceptual and methodological challenges. First, idiographic models are susceptible to error from a variety of sources, including biases in self-report measures, the influence of unmeasured variables, and inadequate timing of assessments (Frumkin et al., 2020; Hopwood et al., 2021), but also the variable timing between prompts, when the lag model assumes equidistant measurement (see below). Moreover, the GIMME models used here contain measurement error in their estimates, which can bias effect estimates and standard errors. GIMME now has the ability to incorporate latent variable measurement models (Gates, Fisher, & Bollen, 2020). However, it has not yet been widely employed in empirical data.
All these aspects also represent pressing issues toward a valid conceptualization and assessment of suicide risk. As discussed by Millner et al. (2020), current measures derived from largely cross-sectional work lack the validity to aid the reliable identification of suicidal thoughts or behaviors (Hom et al., 2015; Plöderl et al., 2011), and often diverse facets of suicidal thoughts are confused into one metric without appropriately evaluating its construct validity (Millner et al., 2020). At the same time, self-report measures of suicidal ideation have numerous threats to validity, including stigma and a fear of loss of autonomy, which can lead to underreporting (Blanchard & Farber, 2020; Richards et al., 2019). At the same time, denial of suicidal ideation may be genuine, because ideation and intent may emerge and peak within minutes or hours preceding suicidal behaviors (Deisenhammer et al., 2008; Simon et al., 2001). Thus, because little research has examined the “true” timescale of an emergent suicidal crisis it is possible that suicidal ideation changes on such a rapid timescale that the sampling of self-reported ideation is unable to match the respective timescale (Ram et al., 2017). The typical timing too may differ across individuals, or within individuals over time.
Moreover, the rarity of suicide attempts complicates any quantitative assessment effort immensely, because it obscures the comparability of estimates across individuals. Even though idiographic models seem perfect for a quantitative articulation of precipitating risk dynamics, the question remains on how to validly interpret individualized models in the absence of meaningful comparison estimates (Wright & Zimmermann, 2019). For instance, knowing that a person’s autocorrelation for suicidal ideation is .4 offers little information on whether this person tends to quickly or slowly recover from high-risk states, or whether this coefficient reflects what can be generally expected for the permanence of suicidal states. More importantly, the coefficient depends on the sampling rate. Therefore, given the current state of knowledge, heterogeneity across individuals and little knowledge about the true timescale of a suicidal crisis, what a lag-1 coefficient reflects in terms of the duration and resolution of a suicidal crisis can be ambiguous. However, as the debate moves forward and as one reviewer pointed out, an important future direction entails research on the interpretation of autoregression coefficients as organizing features of personalized networks of suicide risk. Such analyses would allow to characterize which individuals tend to persevere and which ones tend to quickly recover from states of suicidal ideation or suicide risk more generally.
Relatedly, the heterogeneity in model complexity across individuals raises fundamental questions about the interpretation of non-significant paths within individual models. Simply, statistical power scales with the number of measurements, and with the frequency of suicidal states within the sampling window. Increasing the density of assessments (i.e., more frequent assessment) would increase the number of total observations, thereby increasing power. However, in the case of rare events, like bouts of suicidal ideation, increasing density will not address the issue of infrequency. Rather, one would need to increase the duration of the assessment protocol (e.g., add days). This may erode clinical utility if very long assessment periods are necessitated. Increasing density would increase the precision of estimates for continuously occurring phenomena, like emotions, which may indirectly assist in mitigating suicide risk.
It is also possible that suicidal ideation may be governed by alternative sets of processes that were not assessed in our protocol. Thus, checking how well a node is predicted by all other nodes in the network is important to examine if there is a lot of unexplained variance, indicating that important variables are missing from the network (Halsbeck & Waldorp, 2018). This raises questions about what should be included in future studies that seek to build on this work, as well as which items should be selected for a specific patient. Personalized assessments struggle with the traditional “bandwidth-fidelity tradeoff,” though arguably heighted at N=1 (Wright & Woods, 2020). This tension represents a critical issue in the development and clinical implementation of idiographic models, because it complicates the choice of valid risk factors and raises questions as to whether and how ambulatory assessment items should be personalized or standardized across individuals (Elliott et al., 2016, Haynes et al., 2009, Wright & Zimmermann, 2019). This is important, if the goal is to accommodate idiosyncrasy in nomothetic constructs. One way of addressing this is to go fully idiographic (Wright & Woods, 2020), and work with each individual to develop assessment questionnaires tailored to their specific conceptualization of relevant variables. Early efforts adopted this approach (Shapiro, 1961), and when applied to treatment outcome tracking using bespoke items is associated with stronger observed treatment gains (Lindheim et al., 2016). Thus, although preliminary evidence suggests the possibility to match the complexity and heterogeneity of suicide risk with a diverse set of existing evidence-based interventions, the development of relevant applications is still in the early stages and needs to be amended by research efforts focusing on the measurement and description of suicide risk that allow to more clearly distill short-term risk factors underlying emerging suicide crises.
Another challenge is that the individual variability not accounted for by group-level models may reflect poor internal validity instead of poor generalizability from groups to individuals. The internal validity of a model may be threatened when data is assessed during periods that are not representative for typical daily functioning of the individual, which may be the case when data are collected atypical phases which may not generalize to other periods. This would mean collecting data over a long-enough period to capture a range of periods and control for atypicality. In other words, it is important to observe a system long enough to see sufficient variation in the process of interest, and in parallel, to gain confidence in that the system is weakly stationary. The longer the assessment intervals (e.g., seconds, days, weeks, months), the more tenuous stationarity becomes, but the more likely it is to observe variation in rare processes such as suicidal ideation. At the same time, a longer monitoring period, of course, presents additional logistical challenges for compliance and retention (e.g., Kleiman et al., 2019).
On a more methodological level, it is important to note that GIMME was initially designed for a different type of time-series analyses which has several implications for study design considerations. For instance, as with all statistical models, constant values within timeseries of an individual are not permitted (Lane et al., 2020). That is, if a participant reports no instances of suicidal ideation throughout the monitoring period, their data cannot be used for the analysis. This aspect is of particular relevance for any empirical investigation of suicide risk, as relevant outcomes such as suicidal thoughts and behaviors are well-known to be zero-inflated (Millner et al., 2020). Moreover, GIMME assumes that data are evenly spaced and data from most ambulatory assessment studies are not equidistant due to the randomness of delivered prompts. GIMME was originally designed to be applied to data that are evenly spaced in time, and therefore applying the model to unevenly spaced EMA data may lead to some ambiguity in lagged parameter interpretation, as well as of autocorrelation coefficients (de Haan-Rietdijk et al., 2007). The power of any study design scales with the sample size of a given study. GIMME analyses pose high demands on the quantity of the data such as a minimum of 60 completed EMA queries per participant (Lane et al., 2020). Thus, to avoid the risk of selection bias, studies with a particular focus on shared paths at the subgroup or group level need to be designed in a way that guarantees enough assessments per participant to conduct replicable and generalizable process-oriented research.
With the ultimate goal in mind that our clinical insights into processes of suicide risk will translate to interventions that acknowledge the complexity, idiosyncrasy and ambiguity of suicide risk, systematic research is needed that thoroughly addresses these challenges across a variety of studies and samples.
Despite these limitations, we believe that our study takes an important first step and provides an overview of the potential as well as challenges of integrating idiographic methods into clinical assessments of suicide risk and safety planning considerations, such as lists of idiosyncratic warning signs, coping strategies and sources of support to be used by patients who have been assessed to be at high risk for suicide.
Our study adds to a growing body of evidence suggesting that adequate assessments of suicide risk require a method that acknowledges the complexity, idiosyncrasy and ambiguity of suicidal ideation and that permits to accommodate heterogeneity in the interactive relationships among key short-term risk factors; a feature that mirrors the general logic underlying the individualization of standardized treatment modules such as those implemented in DBT. However, whatever implications future methodological advances may hold for safety planning, they can only aid an improved measurement of dynamic states with the ultimate goal to prevent suicide. The human connection central to the alleviation of such pain is fundamental principle of therapy, and it seems unlikely that any quantitative approach can replace the responsibility and commitment it takes to offer support for someone in crisis, to listen carefully and pay close attention to the unfolding subjective realities.
Highlights.
Acute suicide risk results from volatile, contextualized dynamic processes
Idiographic models depict within-person dynamics of suicide risk
Models reveal high levels of heterogeneity across individuals
More work is needed before personalized models can be applied in clinical settings
Acknowledgements
We are grateful to the participants who took part in this study, as well as the staff and students associated with the present study, who made this work possible. We would also like to thank Aaron J. Fisher and Laura F. Bringmann for valuable reviewer feedback on the initial submission of this manuscript. This research was supported by grants from the National Institute of Mental Health (R01MH048463, R01MH100095, R01MH119399, T32MH018269), the University of Pittsburgh’s Clinical and Translational Science Institute, which is funded by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program (UL1TR001857). The CTSA program is led by the NIH’s National Center for Advancing Translational Sciences. The opinions expressed are solely those of the authors and not those of the funding source.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest
The authors have declared that they have no potential or competing conflicts of interest.
To provide some historic context, Émile Durkheim famously attributed heightened national levels of suicide to particular forms of social interaction practiced in Protestant countries. However, because Durkheim postulated individual effects based on aggregate data at the country level, his work has since been critiqued for committing an ecological fallacy, instances where characteristics of a group are falsely attributed to all members of the group (e.g., Piantadosi, Byar, & Green, 1988). The question of group-to-individual generalizability of nomothetic models of suicide has been to some extent revived in more recent works (e.g., Barlow & Nock, 2009; Fisher et al., 2018; Hamaker, 2012; Molenaar & Campbell, 2009), illustrating that although individuals’ mean-level values correspond to the overall group mean, the variability around that mean is characterized by considerable heterogeneity.
The three case examples are from our own clinical experience and not the present study. The individuals depicted have been anonymized and identifying circumstances were changed.
A handful of studies has applied an idiographic framework when working with attempt survivors (Crockwell & Burford, 1995; Rosen, 1975, 1976). Rosen interviewed attempt survivors who had survived jumps off the Golden Gate or San Francisco Oakland Bay bridges, and primarily focused on how the survivors experienced the jump, and whether they had attempted suicide in the years since their jump. Crockwell and Burford (1995) interviewed adolescent females about their respective suicide attempts, and their work revealed a series of four core conflicts with which all participants identified struggling at some point during their suicide attempt or subsequent treatment.
Most cases were excluded because they had no variance in momentary assessments of suicidal ideation, the main outcome in our analyses. Thus, although only a subgroup of the original sample had sufficient observations to be included in this analysis, this circumstance does not necessarily narrow the representativity of the sample for the purpose of the present analyses.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Gibb BE, Hankin BL, & Comette MM (2000). The hopelessness theory of suicidality. In Suicide Science (pp. 17–32). Springer, Boston, MA. [Google Scholar]
- Alvarez AI (2013). The Savage God: A Study of Suicide (p. 123). Bloomsbury Publishing. [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, Bentley KH, Thompson-Hollands J, Conklin LR, Boswell JF, Ametaj A, Carl JR, Boettcher HT, & Cassiello-Robbins C (2017). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA psychiatry, 74(9), 875–884. 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastiaansen JA, Kunkels YK, Blaauw FJ, Boker SM, Ceulemans E, Chen M, Chow S-M, De Jonge P, Emerencia AC, Epskamp S, Fisher AJ, Hamaker EL, Kuppens P, Lutz W, Meyer MJ, Moulder R, Oravecz Z, Riese H, Rubel J, Ryan O, Servaas MN, Sjobeck G, Snippe E, Trull TJ, Tschacher W, Van Der Veen DC, Wichers M, Wood PK, Woods WC, Wright AGC, Albers CJ, Bringmann LF (2020). Time to get personal? The impact of researchers choices on the selection of treatment targets using the experience sampling methodology. Journal of Psychosomatic Research 137, 110211. doi: 10.1016/j.jpsychores.2020.110211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsher BE, Smolenski DJ, Pruitt LD, Bush NE, Beech EH, Workman DE, Morgan RL, Evatt DP, Tucker J, & Skopp NA (2019). Prediction Models for Suicide Attempts and Deaths: A Systematic Review and Simulation. JAMA psychiatry, 76(6), 642–651. 10.1001/jamapsychiatry.2019.017 [DOI] [PubMed] [Google Scholar]
- Beltz AM, & Gates KM (2017). Network mapping with GIMME. Multivariate Behavioral Research, 52(6), 789–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltz AM, Wright AG, Sprague BN, & Molenaar PC (2016). Bridging the nomothetic and idiographic approaches to the analysis of clinical data. Assessment, 25(4), 447–458. 10.1177/1073191116648209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Young MA, & Depp CA (2012). Real-time predictors of suicidal ideation: mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1-2), 55–59. 10.1016/j.psychres.2011.11.025 [DOI] [PubMed] [Google Scholar]
- Blanchard M, & Farber BA (2020). “It is never okay to talk about suicide”: Patients’ reasons for concealing suicidal ideation in psychotherapy. Psychotherapy Research, 30(1), 124–136. 10.1080/10503307.2018.1543977 [DOI] [PubMed] [Google Scholar]
- Bringmann LF (2021). Person-specific networks in psychopathology: Past, present, and future. Current opinion in psychology, 41, 59–64. Advance online publication. 10.1016/j.copsyc.2021.03.004 [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Elmer T, Epskamp S, Krause RW, Schoch D, Wichers M, Wigman JTW, & Snippe E (2019). What do centrality measures measure in psychological networks? Journal of Abnormal Psychology, 725(8), 892–903. 10.1037/abn0000446 [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, & Grisham JR (2000). Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology, 68(3), 371–377. [PubMed] [Google Scholar]
- Bryan CJ, Butner JE, May AM, Rugo KF, Harris JA, Oakey DN, … & Bryan AO (2020). Nonlinear change processes and the emergence of suicidal behavior: A conceptual model based on the fluid vulnerability theory of suicide. New ideas in psychology, 57, 100758. 10.1016/j.newideapsych.2019.100758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Garland EL, & Rudd MD (2016). From impulse to action among military personnel hospitalized for suicide risk: Alcohol consumption and the reported transition from suicidal thought to behavior. General Hospital Psychiatry, 41, 13–19. 10.1016/j.genhosppsych.2016.05.001 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Clemans TA, Leeson B, & Rudd MD (2015). Acute vs. chronic stressors, multiple suicide attempts, and persistent suicide ideation in US soldiers. The Journal of Nervous and Mental Disease, 205(1), 48–53. 10.1097/NMD.0000000000000236 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, & Rudd MD (2016). The importance of temporal dynamics in the transition from suicidal thought to behavior. Clinical Psychology: Science and Practice, 23(1), 21–25. 10.1111/cpsp.12135 [DOI] [Google Scholar]
- Burger J, Van Der Veen DC, Robinaugh DJ, Quax R, Riese H, Schoevers RA, & Epskamp S (2020). Bridging the gap between complexity science and clinical practice by formalizing idiographic theories: a computational model of functional analysis. BMC Medicine, 18(1). 10.1186/s12916-020-01558-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha CB, Franz PJ, Guzmán EM, Glenn CR, Kleiman EM, & Nock MK (2018). Annual Research Review: Suicide among youth – epidemiology, (potential) etiology, and treatment. Journal of Child Psychology and Psychiatry, 39(4), 460–482. 10.1111/jcpp.12831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen E, & Frank Jensen B (2007). Risk of repetition of suicide attempt, suicide or all deaths after an episode of attempted suicide: a register-based survival analysis. Australian & New Zealand Journal of Psychiatry, 41(3), 257–265. 10.1080/00048670601172749 [DOI] [PubMed] [Google Scholar]
- Coppersmith DD, Dempsey W, Kleiman E, Bentley K, Murphy S, & Nock M (2021). Just-in-Time Adaptive Interventions for Suicide Prevention: Promise, Challenges, and Future Directions. 10.31234/osf.io/eg9fx [DOI] [PMC free article] [PubMed] [Google Scholar]
- David SJ, Marshall AJ, Evanovich EK, & Mumma GH (2018). Intraindividual dynamic network analysis–implications for clinical assessment. Journal of Psychopathology and Behavioral Assessment, 40(2), 235–248. 10.1007/s10862-017-9632-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deisenhammer EA, Ing CM, Strauss R, Kemmler G, Hinterhuber H, & Weiss EM (2008). The duration of the suicidal process: how much time is left for intervention between consideration and accomplishment of a suicide attempt?. The Journal of Clinical Psychiatry, 70(1), 19–24. [PubMed] [Google Scholar]
- de Haan-Rietdijk S, Voelkle MC, Keijsers L, & Hamaker EL (2017). Discrete-vs. continuous-time modeling of unequally spaced experience sampling method data. Frontiers in Psychology, 8, 1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, & Hallquist MN (2021). Search for solutions, learning, simulation, and choice processes in suicidal behavior. Wiley Interdisciplinary Reviews: Cognitive Science, e1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotterer HL, Beltz AM, Foster KT, Simms LJ, & Wright AG (2020). Personalized models of personality disorders: Using a temporal network method to understand symptomatology and daily functioning in a clinical sample. Psychological Medicine, 50(14), 2397–2405. 10.1017/S0033291719002563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott R, Wagner J, Sales CMD, Rodgers B, Alves P, & Café MJ (2016). Psychometrics of the Personal Questionnaire: A client-generated outcome measure. Psychological Assessment, 28(3), 263–278. 10.1037/pas0000174 [DOI] [PubMed] [Google Scholar]
- Epskamp S, Waldorp LJ, Mõttus R, & Borsboom D (2018). The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behavioral Research, 53(4), 453–480. 10.1080/00273171.2018.1454823 [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Reeves JW, Lawyer G, Medaglia JD, Rubel JA (2017). Exploring the idiographic dynamics of mood and anxiety via network analysis. Journal of Abnormal Psychology. 726(8), 1044–1056. 10.1037/abn0000311 [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Medaglia JD, & Jeronimus BF (2018). Lack of group-to-individual generalizability is a threat to human subjects research. Proceedings of the National Academy of Sciences, 115(27), E6106–E6115. 10.1073/pnas.1711978115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher AJ, & Boswell JF (2016). Enhancing the personalization of psychotherapy with dynamic assessment and modeling. Assessment, 23(4), 496–506. 10.1177/1073191116638735 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Frumkin MR, Piccirillo ML, Beck ED, Grossman JT & Rodebaugh TL (2020). Feasibility and utility of idiographic models in the clinic: A pilot study. Psychotherapy Research, 31(4), 520–534. 10.1080/10503307.2020.1805133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, Fisher ZF, & Bollen KA (2020). Latent variable GIMME using model implied instrumental variables (MIIVs). Psychological Methods, 25(2), 227–242. 10.1037/met0000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, Fisher ZF, Arizmendi C, Henry TR, Duffy KA, & Mucha PJ (2019). Assessing the robustness of cluster solutions obtained from sparse count matrices. Psychological Methods, 24(6), 675–689. 10.1037/met0000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, & Molenaar PC (2012). Group search algorithm recovers effective connectivity maps for individuals in homogeneous and heterogeneous samples. Neuroimage, 63(1), 310–319. 10.1016/j.neuroimage.2012.06.026 [DOI] [PubMed] [Google Scholar]
- Gates KM, Molenaar PC, Hillary FG, Ram N, & Rovine MJ (2010). Automatic search for fMRI connectivity mapping: an alternative to Granger causality testing using formal equivalences among SEM path modeling, VAR, and unified SEM. Neuroimage, 50(3), 1118–1125. 10.1016/j.neuroimage.2009.12.117 [DOI] [PubMed] [Google Scholar]
- Haslbeck JM, & Waldorp LJ (2018). How well do network models predict observations? On the importance of predictability in network models. Behavior Research Methods, 50(2), 853–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes SN, Mumma GH, & Pinson C (2009). Idiographic assessment: Conceptual and psychometric foundations of individualized behavioral assessment. Clinical Psychology Review, 29(2), 179–191. 10.1016/j.cpr.2008.12.003 [DOI] [PubMed] [Google Scholar]
- Haynes SN, & O’Brien WO (2000). Principles of behavioral assessment: A functional approach to psychological assessment Plenum/Kluwer Press. [Google Scholar]
- Hofmann SG, & Hayes SC (2019). The future of intervention science: Process-based therapy. Clinical Psychological Science, 7(1), 37–50. 10.1177/2167702618772296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hom MA, Stanley IH, & Joiner TE Jr (2015). Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clinical Psychology Review, 40, 28–39. 10.1016/j.cpr.2015.05.006 [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Bleidom W, & Wright AGC (in press). Getting the timing right in longitudinal research. Perspectives on Psychological Science. [DOI] [PubMed] [Google Scholar]
- Jobes DA (2012). The Collaborative Assessment and Management of Suicidality (CAMS): An evolving evidence-based clinical approach to suicidal risk. Suicide and Life-Threatening Behavior, 42(6), 640–653. 10.1111/j.1943-278X.2012.00119.x [DOI] [PubMed] [Google Scholar]
- Jobes DA, Comtois KA, Brenner LA, Gutierrez PM, & O’Connor SS (2016). Lessons learned from clinical trials of the Collaborative Assessment and Management of Suicidality (CAMS). In O’Connor RC, Pirkis J (eds), The International Handbook of Suicide Prevention (2nd ed., pp. 431–439). John Wiley & Sons. [Google Scholar]
- Joiner TE (2005). Why people die by suicide Harvard University Press. [Google Scholar]
- Joiner TE Jr, Rudd MD, Rouleau MR, & Wagner KD (2000). Parameters of suicidal crises vary as a function of previous suicide attempts in youth inpatients. Journal of the American Academy of Child & Adolescent Psychiatry, 39(7), 876–880. 10.1097/00004583-200007000-00016 [DOI] [PubMed] [Google Scholar]
- Kaurin A, Dombrovski AY, Hallquist MN, & Wright A (2020). Momentary interpersonal processes of suicidal surges in borderline personality disorder. Psychological medicine, 1–11. Advance online publication. 10.1017/S0033291720004791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, & Nock MK (2018). Real-time assessment of suicidal thoughts and behaviors. Current Opinion in Psychology, 22, 33–37. 10.1016/j.copsyc.2017.07.026 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. 10.1037/abn0000273 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Glenn CR, & Liu RT (2019). Real-time monitoring of suicide risk among adolescents: Potential barriers, possible solutions, and future directions. Journal of Clinical Child & Adolescent Psychology, 48(6), 934–946. 10.1080/15374416.2019.1666400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” framework. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Klonsky ED, Saffer BY, & Bryan CJ (2018). Ideation-to-action theories of suicide: a conceptual and empirical update. Current Opinion in Psychology, 22, 38–43. 10.1016/j.copsyc.2017.07.020 [DOI] [PubMed] [Google Scholar]
- Kroeze R, van der Veen DC, Servaas MN, Bastiaansen JA, Voshaar RCOV, Borsboom D, & Riese H (2017). Personalized feedback on symptom dynamics of psychopathology: A proof-of-principle study. Journal for Person-Oriented Research, 3(1), 1–11. 10.17505/jpor.2017.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane S, Fisher Z, Arizmendi C, Molenaar P, Hallquist M, Pike H, Henry T, Duffy K, Luo L, Beltz A, Wright AGC, Park J, Alvarez SC (2020). Group Iterative Multiple Model Estimation. (R package version 0.7-5). In. [Google Scholar]
- Lane ST, & Gates KM (2017). Automated selection of robust individual-level structural equation models for time series data. Structural Equation Modeling: A Multidisciplinary Journal, 24(5), 768–782. 10.1080/10705511.2017.1309978 [DOI] [Google Scholar]
- Lindheim O, Bennett CB, Orimoto TE, & Kolko DJ (2016). A meta-analysis of personalized treatment goals in psychotherapy: A preliminary report and call for more studies. Clinical Psychology: Science and Practice, 23(2), 165–176. 10.1111/cpsp.12153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM (1993). The Skills Training Manual for Treating Borderline Personality Disorder. The Guilford Press. [Google Scholar]
- Linehan MM, Comtois KA, & Ward-Ciesielski EF (2012). Assessing and managing risk with suicidal individuals. Cognitive and Behavioral Practice, 19(2), 218–232. 10.1016/j.cbpra.2010.11.008 [DOI] [Google Scholar]
- Lütkepohl H (2005). New Introduction to Multiple Time Series Analysis. Springer. [Google Scholar]
- Malone KM, Haas GL, Sweeney JA, & Mann JJ (1995). Major depression and the risk of attempted suicide. Journal of Affective Disorders, 34(3), 173–185. 10.1016/0165-0327(95)00015-f [DOI] [PubMed] [Google Scholar]
- McHugh CM, & Large MM (2020). Can machine-learning methods really help predict suicide?. Current Opinion in Psychiatry, 33(4), 369–374. 10.1097/YCO.0000000000000609 [DOI] [PubMed] [Google Scholar]
- MetricWire Inc. (2019). MetricWire (Version 4.2.8) [Mobile application software]. https://metricwire.com/
- Millner AJ, Lee MD, & Nock MK (2017). Describing and measuring the pathway to suicide attempts: A preliminary study. Suicide and Life-Threatening Behavior, 47(3), 353–369. 10.1111/sltb.12284 [DOI] [PubMed] [Google Scholar]
- Millner AJ, Robinaugh DJ, & Nock MK (2020). Advancing the understanding of suicide: the need for formal theory and rigorous descriptive research. Trends in Cognitive Sciences, 24(9), 704–716. 10.1016/j.tics.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molenaar PC, & Lo LL (2016). Alternative forms of Granger causality, heterogeneity, and nonstationarity. Statistics and Causality: Methods for Applied Empirical Research, 205–230. [Google Scholar]
- Mumma GH, & Fluck J (2016). How valid is your case formulation? Empirically testing your cognitive behavioral case formulation for tailored treatment. The Cognitive Behaviour Therapist, 9, 1–25. 10.1017/s1754470x16000088 [DOI] [Google Scholar]
- Nock MK, Prinstein MJ, & Sterba SK (2009). Revealing the form and function of self-injurious thoughts and behaviors: A real-time ecological assessment study among adolescents and young adults. Journal of Abnormal Psychology, 118(4), 816–827. 10.1037/a0016948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachkowski MC, Hewitt PL, & Klonsky ED (2021). Examining suicidal desire through the lens of the Three-Step Theory: A cross-sectional and longitudinal investigation in a community sample. Journal of Consulting and Clinical Psychology, 89, 1–10. 10.1037/ccp0000546 [DOI] [PubMed] [Google Scholar]
- Persons JB (2012). The Case Formulation Approach to Cognitive-Behavior Therapy. The Guilford Press [Google Scholar]
- Piccirillo ML, & Rodebaugh TL (2019). Foundations of idiographic methods in psychology and applications for psychotherapy. Clinical Psychology Review, 71, 90–100. 10.1016/j.cpr.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plöderl M, Kralovec K, Yazdi K, & Fartacek R (2011). A closer look at self-reported suicide attempts: False positives and false negatives. Suicide and Life-Threatening Behavior, 41(1), 1–5. 10.1111/j.1943-278X.2010.00005.x [DOI] [PubMed] [Google Scholar]
- Pons P & Latapy M (2005). Computing Communities in Large Networks Using Random Walks. Computer and Information Sciences - ISCIS 2005, 284–293. 10.1007/11569596_31 [DOI] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, Fisher P, Zelazny J, Burke A, Oquendo M & Mann J (2008). Columbia-Suicide Severity Rating Scale (C-SSRS). Columbia University Medical Center, 2008. [Google Scholar]
- Price RB, Gates K, Kraynak TE, Thase ME, & Siegle GJ (2017). Data-driven subgroups in depression derived from directed functional connectivity paths at rest. Neuropsychopharmacology, 42(13), 2623–2632. 10.1038/npp.2017.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram N, Brinberg M, Pincus AL, & Conroy DE (2017). The questionable ecological validity of ecological momentary assessment: Considerations for design and analysis. Research in Human Development, 14(3), 253–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rath D, De Beurs D, Hallensleben N, Spangenberg L, Glaesmer L, & Forkmann T (2019). Modelling suicide ideation from beep to beep: Application of network analysis to ecological momentary assessment data. Internet Interventions, 18, 100292. 10.1016/j.invent.2019.100292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards JE, Whiteside U, Ludman EJ, Pabiniak C, Kirlin B, Hidalgo R, & Simon G (2019). Understanding why patients may not report suicidal ideation at a health care visit prior to a suicide attempt: a qualitative study. Psychiatric Services, 70(1), 40–45. 10.1176/appi.ps.201800342 [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Hoekstra RH, Toner ER, & Borsboom D (2020). The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychological Medicine, 50(3), 353–366. 10.1017/S0033291719003404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinaugh DJ, Brown ML, Losiewicz OM, Jones PJ, Marques L, & Baker AW (2020). Towards a precision psychiatry approach to anxiety disorders with ecological momentary assessment: the example of panic disorder. General psychiatry, 33(1), e100161. 10.1136/gpsych-2019-100161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche MJ, Pincus AL, Rebar AL, Conroy DE, Ram N. (2014). Enriching psychological assessment using a person-specific analysis of interpersonal processes in daily life. Assessment, 21, 515–28. 10.1177/1073191114540320 [DOI] [PubMed] [Google Scholar]
- Rudd MD, Berman AL, Joiner TE Jr, Nock MK, Silverman MM, Mandrusiak M, Van Orden K, & Witte T (2006). Warning signs for suicide: Theory, research, and clinical applications. Suicide and Life-Threatening Behavior, 36(3), 255–262. 10.1521/suli.2006.36.3.255 [DOI] [PubMed] [Google Scholar]
- Sandford DM, Kirtley OJ, Thwaites R, & O’Connor RC (2020). The impact on mental health practitioners of the death of a patient by suicide: A systematic review. Clinical Psychology & Psychotherapy, 28(2), 261–294. 10.1002/cpp.2515 [DOI] [PubMed] [Google Scholar]
- Schuurman NK, Houtveen JH, & Hamaker EL (2015). Incorporating measurement error in n=1 psychological autoregressive modeling. Frontiers in Psychology, 6, 1038. 10.3389/fpsyg.2015.01038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Joiner TE Jr., & Ribeiro JD (2014). Comprehensive theories of suicidal behaviors. In Nock MK (Ed.), Oxford library of psychology. The Oxford handbook of suicide and self-injury (p. 286–307). Oxford University Press. [Google Scholar]
- Shapiro MB 1961. A method of measuring psychological changes specific to the individual psychiatric patient. British Journal of Medical Psychology, 34(2), 151–155. [Google Scholar]
- Shneidman ES (1993). Suicide as Psychache: A Clinical Approach to Self-Destructive Behavior. Jason Aronson. [Google Scholar]
- Siddaway AP, Holm-Denoma J, Witte TK, & Ruscio J (2021). Reexamining the latent structure of suicidal thoughts using taxometric analysis: Implications for testing ideation to action theoretical models of suicidal thoughts and behavior. Psychological Assessment, 33(3), 243–254. 10.1037/pas0000889 [DOI] [PubMed] [Google Scholar]
- Simon TR, Swann AC, Powell KE, Potter LB, Kresnow MJ, & O’Carroll PW (2001). Characteristics of impulsive suicide attempts and attempters. Suicide and Life-Threatening Behavior, 32(1 Suppl), 49–59. 10.1521/suli.32.1.5.49.24212 [DOI] [PubMed] [Google Scholar]
- Stanley B, & Brown GK (2012). Safety planning intervention: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256–264. 10.1016/j.cbpra.2011.01.001 [DOI] [Google Scholar]
- Stanley B, Brown G, Brent DA, Wells K, Poling K, Curry J, Kennard BD, Wagner A, Cwik MF, Klomek AB, Goldstein T, Vitiello B, Barnett S, Daniel S, & Hughes J (2009). Cognitive-behavioral therapy for suicide prevention (CBT-SP): treatment model, feasibility, and acceptability. Journal of the American Academy of Child & Adolescent Psychiatry, 48(10), 1005–1013. 10.1097/CHI.0b013e3181b5dbfe [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, & Lönnqvist J (2004). Completed suicide after a suicide attempt: a 37-year follow-up study. American Journal of Psychiatry, 161(3), 562–563. 10.1176/appi.ajp.161.3.562 [DOI] [PubMed] [Google Scholar]
- Szanto K, Galfalvy H, Vanyukov PM, Keilp JG, & Dombrovski AY (2018). Pathways to late-life suicidal behavior: cluster analysis and predictive validation of suicidal behavior in a sample of older adults with major depression. The Journal of Clinical Psychiatry, 79(2), 17m11611. 10.4088/JCP.17m11611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Krieke L, Emerencia AC, Bos EH, Rosmalen JG, Riese H, Aiello M, Sytema S & de Jonge P (2015). Ecological momentary assessments and automated time series analysis to promote tailored health care: a proof-of-principle study. JMIR research protocols, 4(3), e100. 10.2196/resprot.4000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Wenzel A, & Beck AT (2008). A cognitive model of suicidal behavior: Theory and treatment. Applied and Preventive Psychology, 12(4), 189–201. 10.1016/j.appsy.2008.05.001 [DOI] [Google Scholar]
- Woods WC, Arizmendi C, Gates KM, Stepp SD, Pilkonis PA, & Wright AGC (2020). Personalized models of psychopathology as contextualized dynamic processes: An example from individuals with borderline personality disorder. Journal of Consulting and Clinical Psychology, 88(3), 240–254. 10.1037/ccp0000472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Simms LJ (2014). On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment, 5(1), 43–54. 10.1037/per0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AG, & Woods WC (2020). Personalized models of psychopathology. Annual Review of Clinical Psychology, 16(1), 49–74. 10.1146/annurev-clinpsy-102419-125032 [DOI] [PubMed] [Google Scholar]
- Wright AGC, Gates KM, Arizmendi C, Lane ST, Woods WC, & Edershile EA (2019). Focusing personality assessment on the person: Modeling general, shared, and person specific processes in personality and psychopathology. Psychological Assessment, 31(4), 502–515. 10.1037/pas0000617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Zimmermann J (2019). Applied ambulatory assessment: Integrating idiographic and nomothetic principles of measurement. Psychological Assessment, 31(12), 1467–1480. 10.1037/pas0000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyder M, & De Leo D (2007). Behind impulsive suicide attempts: Indications from a community study. Journal of Affective Disorders, 104(1-3), 167–173. 10.1016/j.jad.2007.02.015 [DOI] [PubMed] [Google Scholar]
- Yen S, Peters JR, Nishar S, Grilo CM, Sanislow CA, Shea MT, Zanarini MC, McGlashan TH, Morey LC, & Skodol AE (2021). Association of borderline personality disorder criteria with suicide attempts: findings from the Collaborative Longitudinal Study of Personality Disorders over 10 years of follow-up. JAATA Psychiatry, 78(2), 187–194. 10.1001/jamapsychiatry.2020.3598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalsman G, Hawton K, Wasserman D, Heeringen K van, Arensman E, Sarchiapone M, Carli V, Höschl C, Barzilay R, Balazs J, Purebl G, Kahn JP, Sàiz PA, Lipsicas CB, Bobes J, Cozman D, Hegerl U, & Zohar J (2016). Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry, 3(7), 646–659. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- Zimmermann J, Woods WC, Ritter S, Happel M, Masuhr O, Jaeger U, Spitzer C, & Wright AGC (2019). Integrating structure and dynamics in personality assessment: First steps toward the development and validation of a Personality Dynamics Diary. Psychological Assessment, 31(4), 516–531. 10.1037/pas0000625 [DOI] [PubMed] [Google Scholar]
References from Footnotes
- Barlow DH, & Nock MK (2009). Why can’t we be more idiographic in our research?. Perspectives on Psychological Science, 4(1), 19–21. 10.1111/j.1745-6924.2009.01088.x [DOI] [PubMed] [Google Scholar]
- Crockwell L, & Burford G (1995). What makes the difference? Adolescent females’ stories about their suicide attempts. Journal of Child and Youth Care, 10, 1–14. [Google Scholar]
- Hamaker EL (2012). Why researchers should think “within-person”: A paradigmatic rationale. In Mehl MR & Conner TS (Eds.), Handbook of research methods for studying daily life (pp. 43–61). The Guilford Press. [Google Scholar]
- Molenaar PC, & Campbell CG (2009). The new person-specific paradigm in psychology. Current directions in psychological science, 18(2), 112–117. 10.1111/j.1467-8721.2009.01619.x [DOI] [Google Scholar]
- Piantadosi S, Byar DP, & Green SB (1988). The ecological fallacy. American journal of epidemiology, 127(5), 893–904. 10.1093/oxfordjournals.aje.a114892 [DOI] [PubMed] [Google Scholar]
- Rosen DH (1975). Suicide survivors: a follow-up study of persons who survived jumping from the Golden Gate and San Francisco-Oakland Bay Bridges. Western Journal of Medicine, 122(4), 289–294. [PMC free article] [PubMed] [Google Scholar]
- Rosen DH (1976). Suicide survivors: Psychotherapeutic implications of egocide. Suicide and Life-Threatening Behavior, 6(4), 209–215. [PubMed] [Google Scholar]


