ABSTRACT
Bronchiolitis represents a heavy burden of disease in children under 2 years of age in our society due to the high infectivity of the Respiratory Syncytial Virus [RSV] and the vulnerability of the youngest children.
The objective of this retrospective epidemiological study was to show the burden of severe bronchiolitis in Spain through population-based estimates of hospitalizations due to bronchiolitis in children up to 24 months old during a 6-year period (2012–2017).
A total of 100,115 cases of bronchiolitis required hospitalization in Spain from 2012 to 2017. Most cases of bronchiolitis that required hospitalization were in infants under 3 months of age. The hospitalization rate for bronchiolitis for children under 1 year of age was 3,838.27 per 100,000 healthy children. During the 6-year study period, a total of 82 deaths due to bronchiolitis were reported among hospitalized infants. Among these deaths, more than 50% were in patients younger than 3 months of age. The annual average cost to the National Health Care System was €58 M, with a mean hospitalization cost of €3,512 per case.
KEYWORDS: Bronchiolitis, respiratory syncytial virus, epidemiology, Spain, vaccine, immunotherapy, children
Introduction
Bronchiolitis is the leading cause of severe lower respiratory tract illness and hospitalization in children under 2 years of age in developed countries. The Respiratory Syncytial Virus (RSV) is the primary cause of respiratory difficulty, in the form of bronchiolitis, bronchitis or pneumonia, in children under 12 months of age. It is important to realize that patients with antecedents such as prematurity, immunodeficiency, and heart or lung disease (such as bronchopulmonary dysplasia) have higher mortality and morbidity rates when affected by bronchiolitis since there is no specific therapy for it.1–6
According to the available data, every year 33% of children under 1 year of age in Spain will suffer from bronchiolitis.7 RSV causes 70–80% of cases, with a maximum incidence at 2–3 months of age. RSV is transmitted through respiratory secretions, as well as through contaminated fomites. Due to its high infectivity, it has been estimated that 75% of all children will suffer from infection by RSV during their first year of age.8 In Spain, RSV infections occurred in annual outbreaks from November until February.8 Approximately 2–3% of children infected by RSV their first year of life will require hospitalization, and 2–6% of them will require Intensive Care. Mortality from RSV in previously healthy children is very low in developed countries (0–1.5%). However, due to the high incidence of bronchiolitis, 66,000–199,000 children around the world die every year due to RSV infections, being the second cause of death after malaria in children 1–12 months of age.1,7–12
Bronchiolitis has been supposed to be a great burden in children these past years, but an RSV vaccine is still under development. The objective of this study was to obtain information on population-based estimates of the burden of hospitalization due to bronchiolitis in children up to 24 months old in Spain during a 6-year period (2012–2017). It may serve as a starting checkpoint for later evaluation of the effectivity and efficiency of different preventive measures such as vaccination or immunotherapy.
Materials and methods
The Spanish national information system for hospital data (Conjunto Mínimo Básico de Datos; CMBD) from the Ministry of Health was accessed to gather all retrospective cases with diagnoses of bronchiolitis in children under 2 years of age hospitalized from 1 January 2012 to 31 December 2017.13–15 Following the definition of bronchiolitis, only first incidence hospitalizations with a diagnosis of bronchiolitis were included in the study.16
All bronchiolitis-related hospitalizations in any diagnostic position with the International Classification of Diseases, 9th revision, Clinical Modification ICD-9-CM codes (ICD 9 CM: 466.1 Acute bronchiolitis: Bronchiolitis (acute), Capillary pneumonia, 466.11 Acute bronchiolitis RSV, 466.19, Acute bronchiolitis other (from 2012 to 2015) and ICD-10-CM codes (“J21.0”, “J21.1”, “J21.8”, and “J21.9” (from 2016 to 2017)), were analyzed.
The annual hospitalization rates were calculated. For the rates, data from population municipal records for children were used as the denominators. In order to calculate rates by months of age, the number of total newborns and perinatal mortality in Spain was also searched through the Spanish Instituto Nacional de Estadística (INE) that collects epidemiological data about the Spanish population every year. For the population denominators by months of age, we assumed a constant birth rate throughout the year in order to associate the precise hospitalization date for the population at risk in any given month. The case-fatality rate (CFR), which reflects the severity of the cases, was calculated by dividing the number of deaths by the total number of hospitalizations due to bronchiolitis (%). The average length of stay at the hospital (ALOS) was calculated. The same age, sex and epidemiological characteristics distributions were assumed for the population and for hospitalizations not covered by CMBD.
The cost to the health care system of these hospitalizations is estimated by the Ministry of Health. The cost was calculated by considering the diagnostic cost group, the total cost and the number of discharges. The diagnostic cost group was based on the Diagnosis Related Groups (DRG) for hospitalized patients depending on discharge ICD classification, age, sex, and resource consumption. Each group has a similar weight in hospital costs and can be applied to each related patient. DRGs calculations were made by 3 M with Core Grouping System Software.17
Statistics:
Student´s t-test was used for comparing continuous variables. The chi-square test was used to assess significant differences in proportions. Poisson regression models were used to assess differences in the hospitalization rates over the study period by age group and sex.
In all tests, the significance level used was p < .05.
Statistical analyses were performed using R Software (version 3.4.3).
The patient information was anonymized and de-identified prior to the analysis. The local ethics committee (Comité de Ética de la Investigación de la Universidad Rey Juan Carlos) ruled that no formal ethics approval was required for this study.
Results
A total of 100,115 hospital discharges due to bronchiolitis, defined as a first incident episode of respiratory difficulty in children <2 years of age, 16 were reported in Spain during the 6-year study period, which accounts for a hospitalization rate of 1981.09 (95% CI = 1968.93–1993.24) hospitalizations per 100,000 children <2 years old. Of those, 93,534 (93.4%) occurred in children up to 12 months old. Their mean age was 3.66 (SD 4.30) months and 57.9% of the patients were male. The average length of hospital stay was 5.46 (SD 7.24) days, and it slightly decreased during the study period from 5.62 (SD 7.09) days to 5.36 (SD 7.62) days (p = .016).
Table 1 shows the hospitalization rate for bronchiolitis at 0 and 1 year old during the period studied. Each year of the study had a similar number of cases, with 17,440 cases of bronchiolitis that required hospitalization in 2012, 14,806 cases in 2013, 16,129 cases in 2014, 17,923 cases in 2015, 17,074 cases in 2016, and 16,743 cases in 2017. The highest incidence of hospitalization is shown in the first year of life with a hospitalization rate per 100,000 children <12 months of 383,827 (CI 95%: 3814.15–3862.39). The hospitalization rate in our study was 251.5 (95% CI: 245.44–257.57) per 100,000 children during the second year of life. These rates showed a slight linear increase of 3.6% per year during the study period (p < .001). Average length of stay also significantly decreased with age, being 5.54 (SD 7.38) days in children up to 12 months of age and 4.28 (SD 4.70) days in children from 12 to 23 months old (p < .001)
Table 1.
Hospitalization rate and case fatality rate of bronchiolitis by age in Spain (2012–2017)
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total | |
|---|---|---|---|---|---|---|---|
| Hospitalization Rates in 0 years old (95% CI) | 3731.34 (3675.04; 3787.64) | 3261.24 (3207.72; 3314.76) | 3772.06 (3712.92; 3831.21) | 4204.67 (4142.4; 4266.93) | 4055.47 (3993.88; 4117.06) | 4058.91 (3996.71; 4121.12) | 3838.27 (3814.15; 3862.39) |
| Hospitalization Rates in 1 year old (95% CI) | 252.69 (238.38; 267) | 219.65 (206.09; 233.2) | 247.04 (232.41; 261.67) | 275.72 (259.75; 291.69) | 262.17 (246.66; 277.69) | 255.21 (239.8; 270.62) | 251.5 (245.44; 257.57) |
| Case-Fatality Rates in 0 years old (95% CI) | 0.105 (0.055; 0.154) | 0.072 (0.028; 0.117) | 0.113 (0.059; 0.167) | 0.072 (0.031; 0.112) | 0.038 (0.008; 0.068) | 0.057 (0.02; 0.095) | 0.076 (0.058; 0.094) |
| Case-Fatality Rates in 1 year old (95% CI) | 0.251 (−0.033; 0.535) | 0.199 (−0.076; 0.474) | 0.091 (−0.088; 0.271) | 0.35 (0.008; 0.693) | 0 (0; 0) | 0.095 (−0.091; 0.282) | 0.167 (0.068; 0.266) |
When studying the hospitalization rate by months of age (Figure 1), most of the cases (n = 56,293, 56.2%) occurred in infants under 3 months old with 16,304 cases in the child’s first month, 24,079 in the child’s second month, and 15,910 cases in the child’s third month of age, reaching 8028.63 (95% CI 7910.44–8146.82), 11857.30 (95% CI 11,716.69–11,997.91), and 7834.61 (95% CI 7717.74–7951.49) cases per 100,000 infants of 0, 1, and 2 months of age, respectively. The HR significantly decreased with age (p < .001).
Figure 1.

Incidence of hospitalization associated with bronchiolitis per 100,000 children by age in month in Spain.
During the 6-year study period, a total of 82 deaths were reported among the bronchiolitis hospitalized children, 40 in boys and 42 in girls. Of all the deaths in the boys, 9 (22.5%) were in patients younger than 1 month, 21 (52.5%) were in patients younger than 3 months, 33 (82.5%) were <1 year old and 7 (17.5%) were in their second year of life. Of all the deaths of the girls, 9 (21.4%) were in patients younger than 1 month, 25 (9.5%) were in patients younger than 3 months, 38 (90.5%) were <1 year old and 4 (9.5%) were in their second year of life. The overall case-fatality rate was: 0.082% (95% CI: 0.064–0.100), ranging from 0.035% (0.007–0.063) in 2016 to 0.115 (0.064–0.165) in 2012 and it showed a significant linear decrease of 14.4% per year (95% CI 2.8%–24.8%, p = .018) over the study period. (Table 1). Fifty-six of the 82 deaths were confirmed to be RSV positive, being acute respiratory failure, cute kidney failure and septic shock the most frequent complications. Table 2 shows the HR and CFR by age in months and sex. The HR was significantly higher in boys (p < .001) and this difference was larger in infants <1 year of age. CFR did not significantly vary neither with sex (p = .10) nor with age (p = .28). Bronchiolitis is a clearly seasonal disease, as can be seen in Figure 2, with almost no cases in summer and peaking in December/January. The annual average cost to the National Health Care System for bronchiolitis requiring hospitalization was €58,6 M with a mean hospitalization cost per case of €3,512.
Table 2.
Hospitalization rate and case fatality rate of bronchiolitis by month of age and sex in Spain (2012–2017)
| Age (in months) | HR in males | HR in females | CFR in males | CFR in females |
|---|---|---|---|---|
| 0 | 8426.8 (8258.3; 8595.2) | 7606.8 (7441.4; 7772.3) | 0.102 (0.035; 0.169) | 0.12 (0.042; 0.198) |
| 1 | 13474.4 (13267.4; 13681.5) | 10144.1 (9955.7; 10332.6) | 0.057 (0.017; 0.096) | 0.13 (0.059; 0.201) |
| 2 | 8900.6 (8728; 9073.3) | 6705.3 (6549.2; 6861.4) | 0.043 (0.001; 0.085) | 0.045 (−0.006; 0.097) |
| 3 | 5256.3 (5121; 5391.7) | 3806 (3686.5; 3925.4) | 0.036 (−0.014; 0.087) | 0.053 (−0.021; 0.127) |
| 4 | 4094.2 (3974; 4214.4) | 2941.9 (2836.5; 3047.4) | 0.07 (−0.009; 0.149) | 0.034 (−0.033; 0.102) |
| 5 | 2937.8 (2835.4; 3040.2) | 2043.4 (1955.1; 2131.7) | 0.098 (−0.013; 0.208) | 0.298 (0.06; 0.536) |
| 6 | 2635.3 (2538.2; 2732.5) | 1755.4 (1673.5; 1837.4) | 0.073 (−0.028; 0.173) | 0.116 (−0.044; 0.276) |
| 7 | 1944.2 (1860.5; 2027.9) | 1422.8 (1348.9; 1496.7) | 0 (0; 0) | 0 (0; 0) |
| 8 | 1515.3 (1441.3; 1589.4) | 1003 (940.8; 1065.1) | 0 (0; 0) | 0.202 (−0.078; 0.482) |
| 9 | 1216.7 (1150.2; 1283.2) | 875.2 (817; 933.3) | 0 (0; 0) | 0 (0; 0) |
| 10 | 933.3 (875; 991.6) | 743.3 (689.7; 797) | 0.103 (−0.098; 0.303) | 0 (0; 0) |
| 11 | 747.6 (695.4; 799.9) | 624.7 (575.5; 673.9) | 0.128 (−0.123; 0.379) | 0 (0; 0) |
| 12 | 518.7 (476.7; 560.7) | 469.5 (428.3; 510.7) | 0.172 (−0.165; 0.508) | 0.402 (−0.154; 0.959) |
| 13 | 432.3 (393.9; 470.6) | 372.2 (335.5; 408.9) | 0.206 (−0.198; 0.61) | 0.254 (−0.243; 0.751) |
| 14 | 353.8 (319.1; 388.6) | 318.4 (284.4; 352.3) | 0 (0; 0) | 0 (0; 0) |
| 15 | 311.9 (279.3; 344.6) | 302.3 (269.2; 335.4) | 0 (0; 0) | 0 (0; 0) |
| 16 | 267.4 (237.2; 297.6) | 250.3 (220.2; 280.4) | 0 (0; 0) | 0 (0; 0) |
| 17 | 247.8 (218.7; 276.9) | 226.7 (198.1; 255.4) | 0.36 (−0.344; 1.063) | 0.417 (−0.398; 1.232) |
| 18 | 239.7 (211.1; 268.4) | 203.1 (176; 230.2) | 0.372 (−0.356; 1.099) | 0 (0; 0) |
| 19 | 173.8 (149.4; 198.2) | 173.8 (148.7; 198.9) | 1.026 (−0.389; 2.44) | 0 (0; 0) |
| 20 | 176.5 (151.9; 201) | 167.2 (142.6; 191.8) | 0 (0; 0) | 0 (0; 0) |
| 21 | 155.1 (132.1; 178.1) | 164.4 (140; 188.8) | 0 (0; 0) | 0 (0; 0) |
| 22 | 138.1 (116.4; 159.9) | 146.4 (123.4; 169.5) | 0.645 (−0.615; 1.906) | 0 (0; 0) |
| 23 | 120.3 (100; 140.6) | 104.9 (85.4; 124.4) | 0 (0; 0) | 0 (0; 0) |
| Total | 2227.9 (2210; 2245.9) | 1719.5 (1703.2; 1735.8) | 0.069 (0.048; 0.09) | 0.1 (0.069; 0.13) |
Figure 2.
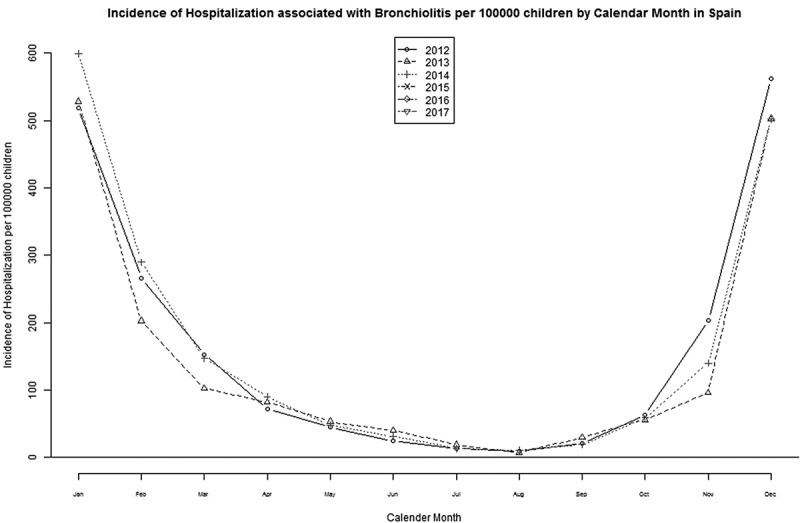
Incidence of hospitalization associated with bronchiolitis per 100,000 children by calendar month in Spain.
Discussion
A total of 101,903 cases of bronchiolitis among children less than 2 years old were hospitalized in Spain from 2012 to 2017. That means that two children out of every 100 up to 24 months of age and four children out of every 100 up to 12 months of age were hospitalized during the study period in our country due to bronchiolitis. The hospitalization rate in our study was 15-fold higher during the first year of life than in the second year of life. This statistically significant difference is also clinically relevant because it shows that bronchiolitis in children over 1 year of age very rarely requires hospitalization. It is also remarkable to see that there were more hospitalizations due to bronchiolitis in the children’s second month than in the first one, since this has also been seen in other series.8,10,18 It seems that the IgG against RSV the fetus receives from its mother through the placenta during the pregnancy offers partial, though incomplete, protection against the most severe cases of bronchiolitis during the first 4–6 weeks of life in term newborns.19
Regarding mortality, there were 85 deaths due to bronchiolitis during this past 6 years in Spain, without finding statistically significant differences in the case-fatality rate between children above or below 1 year of age. However, this lack of statistical significance is probably due to the small sample size.
Previous studies in Spain showed a mean Hospitalization Rate of 2,413 cases per 100,000 susceptible children, with most cases in children below 1 year of age (4,136/100,000).1
Our study showed a significantly lower Hospitalization Rate in this population with 3,838 (3,814–3,862) per 100,000 susceptible children. The clinical criteria to define bronchiolitis are different according to different sources and authors, and this difference could be due to the inclusion in our study of only the first episode of respiratory distress, excluding all further episodes
When comparing with other RSV-related infections in other countries in the 2014–2015 season, we find that UK (England and Scotland) have a mean annual incidence of hospital admissions attributable to RSV of 28.3/100,000 in children below 1 year old and 1.3/100,000 in children from 1 to 4 years old. In Slovenia RSV causes 105.9/100,000 children below 5 years of age to be hospitalized due to lower respiratory tract infections and 54.5/100,000 due to acute bronchiolitis. In France, the incidence rates of RSV-related infection varied between 145 and 485 per 100,000. Sweden had a cumulative incidence of 52.56/100,000.20
Compared to other studies in developed countries, our results are very similar. Consistently, studies find that most hospitalizations occur in the first months of age, and about 45% of hospital admissions and in-hospital deaths due to RSV-related bronchiolitis occur in children younger than 6 months,5 with a substantial RSV disease burden in neonates, with estimates of 40 episodes per 1000 neonates per year (95% CI 2.5–635.7),6 but with low mortality and case-fatality rates.5,6,10,18,21
Consistent with previously published data, we showed that the hospitalization rate was significantly higher in boys.19 Several studies have shown that boys develop respiratory tract infections more frequently than girls, probably due to sex differences in the anatomy and physiology of the pediatric airway, as the peripheral airways are disproportionately narrower during the early years of life in boys, which may predispose them to lower respiratory tract infections.22–26
As for the limitations of this study, it is important to note that despite all cases of hospitalizations due to bronchiolitis being gathered, we were not able to take into account the bronchiolitis cases that are managed in the primary attention care clinics.
Furthermore, although we know that about 70–80% of bronchiolitis cases are caused by RSV, and that they tend to have a higher risk of hospitalization,8 in the patients included in this study we don’t have microbiological confirmation of RSV infection for all of them, so there is an uncertain number of bronchiolitis not caused by RSV in the sample, so the RSV associated hospitalizations results may be overestimated.
However, a strength of this study is that the data were gathered nationwide over 6 years. This will make it easier to calculate the real impact of future vaccination and immunotherapy on hospitalizations due to bronchiolitis in the Spanish population after their implementation.
Studies on the epidemiology and the incidence of bronchiolitis are needed in order to evaluate current and future preventive measures implementation. At the present moment, the burden of hospitalizations in Spain is quite significant, suggesting the necessity of passive protection against RSV infection at birth, either through maternal immunization or the administration of an at-birth dose of extended half-life monoclonal antibodies. Once an effective and safe vaccine against RSV is available, one strategy could be its administration to pregnant women, using their immune system for immunoglobulins transmission to the newborns.27 This strategy has been proven useful before in whooping cough, as its mortality has decreased greatly since the start of vaccination of pregnant women.28,29 Thus, we could also have positive results against RSV bronchiolitis by applying the inactivated vaccine during the pregnancy.30
Vaccination of children at a very young age could be another strategy to evaluate, along with the particular seasonal characteristics of RSV and the complexity of implementing a new vaccine into the current routine vaccination schedules. Some mathematical models predicted that RSV vaccination could prevent 29–48% of in-hospital deaths due to RSV.31 However, at the moment, most efforts to reduce the bronchiolitis disease burden are based on specific indications for monoclonal antibodies. Passive RSV antibody approaches have proven their efficacy in clinical trials, 32–38 but the currently available prophylaxis is limited to the administration of palivizumab to infants at a higher risk of serious RSV sequelae.39 Adding monoclonal antibodies for RSV prevention to all children in their first year of life during the epidemic months of RSV, besides administering inactivated RSV vaccine to pregnant women, could also be considered.5,40–44
The development of more effective preventive strategies (i.e., specific indications of monoclonal antibodies) is needed, especially for high-risk children, but also to prevent RSV infection in all children during their first year of life during the epidemic months of RSV, which may coincide with influenza or, nowadays, COVID-19 epidemics.
Acknowledgments
The authors thank the Subdirección General del Instituto de Información Sanitaria for providing the information on which this study is based.
Funding Statement
This research study is part of the research activities of the “Cathedra in Vaccines Research from Rey Juan Carlos University”, which is sponsored by Sanofi..
Disclosure of potential conflicts of interest
RGP has received travel and research grants and has participated in advisory boards from Sanofi, Merck and Pfizer
AGM has received travel and research grants and has participated in advisory boards from Sanofi, Merck and Pfizer
SW has participated in advisory boards from Sanofi
MHM and FAB have no conflicts of interest.
References
- 1.Gil-Prieto R, Gonzalez-Escalada A, Marín-García P, Gallardo-Pino C, Gil-de-Miguel A.. Respiratory syncytial virus bronchiolitis in children up to 5 years of age in Spain. Medicine (Baltimore) [Internet]. 2015;94(21):e831. Available from http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005792-201505050-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sardón O, Korta J, Pérez-Yarza G. E. Bronquiolitis. An Pediatría Contin [Internet]. Elsevier; 2007. Dec 1;5(6):332–7. [accessed 2018 Jul 14]. http://linkinghub.elsevier.com/retrieve/pii/S1696281807741562. [Google Scholar]
- 3.Thwaites RS, Coates M, Ito K, Ghazaly M, Feather C, Abdulla F, Tunstall T, Jain P, Cass L, Rapeport G, et al. Reduced nasal viral load and IFN responses in infants with respiratory syncytial virus bronchiolitis and respiratory failure. Am J Respir Crit Care Med [Internet]. 2018;198(8):1074–84. http://www.atsjournals.org/doi/ 10.1164/rccm.201712-2567OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higgins D, Trujillo C, Keech C. Advances in RSV vaccine research and development - A global agenda. Vaccine [Internet]. 2016;34(26):2870–75. Elsevier Ltd. doi: 10.1016/j.vaccine.2016.03.109. [DOI] [PubMed] [Google Scholar]
- 5.Shi T, McAllister DA, O’Brien KL, Simoes EAF, Madhi SA, Gessner BD, Polack FP, Balsells E, Acacio S, Aguayo C, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390(10098):946–58. doi: 10.1016/S0140-6736(17)30938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karron RA, Black RE. Determining the burden of respiratory syncytial virus disease: the known and the unknown. Lancet [Internet]. 2017;390(10098):917–18. doi: 10.1016/S0140-6736(17)31476-9. [DOI] [PubMed] [Google Scholar]
- 7.Blecua C, Praena M, Águeda C, Isabel GM, Mora Gandarillas M, Luis Montón Alvarez J, Antonio Castillo Laita J. Diagnóstico Tratamiento en Atención Primaria. Bronquiolitis [Internet]. 2015. https://www.respirar.org/images/pdf/grupovias/bronquiolitis_p_gvr_4_2015.pdf. [Google Scholar]
- 8.Luz García MA, Murua JK. ACC. Bronquiolitis aguda viral. ©asociación Española de Pediatría. Internet]. 2017;1(1):85–102. http://www.aeped.es/sites/default/files/documentos/06_bronquiolitis_aguda_viral_0.pdf. [Google Scholar]
- 9.Muñoz-Quiles C, López-Lacort M, Úbeda-Sansano I, Alemán-Sánchez S, Pérez-Vilar S, Puig-Barberà J, Díez-Domingo J. Population-based analysis of bronchiolitis epidemiology in Valencia, Spain. Pediatr Infect Dis J. 2016;35(3):275–80. doi: 10.1097/INF.0000000000000993. [DOI] [PubMed] [Google Scholar]
- 10.Bont L, Checchia PA, Fauroux B, Figueras-Aloy J, Manzoni P, Paes B, Simões EAF, Carbonell-Estrany X. Defining the epidemiology and burden of severe respiratory syncytial virus infection among infants and children in Western Countries. Infect Dis Ther. 2016;5(3):271–98. doi: 10.1007/s40121-016-0123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meer HC. Viral Bronchiolitis in Children. N Engl J Med. Internet]. 2016;374(1):62–72. http://www.nejm.org/doi/ 10.1056/NEJMra1413456. [DOI] [PubMed] [Google Scholar]
- 12.Weinberg GA. Respiratory syncytial virus mortality among young children. Lancet Glob Heal [Internet]. 2017;5(10):e951–2. doi: 10.1016/S2214-109X(17)30348-0. [DOI] [PubMed] [Google Scholar]
- 13.Ministerio de Sanidad y Consumo . Clasificación internacional de enfermedades 9ª revisión, modificación clínica. 1994.
- 14.Instituto Nacional de la Salud. Subdirección General de Coordinación administrativa . Conjunto Mínimo Básico de Datos. Hospitales de INSALUD 2001. Madrid; 2002. http://www.ingesa.msc.es/. [Google Scholar]
- 15.Rivero Cuadrado A. El conjunto mínimo básico de datos en el SNS: inicios y desarrollo actual. Rev Fuentes Estadísticas. 2000;49:18–19. http://www.ingesa.msc.es/estadEstudios/documPublica/pdf/CMBD-2001.pdf. [Google Scholar]
- 16.Sánchez Martín M, Calvo Rey C. Bronquiolitis Aguda. In: Guerrero-Fdez J, Cartón SA, Barreda BA, Menéndez SJ, Ruiz DJ, editors. Manual de diagnóstico y terapéutica en pediatría. 6ª Edición. Madrid: Editorial Panamericana; 2017. p. 1379–85. [Google Scholar]
- 17.Schreyögg J, Stargardt T, Tiemann O, Busse R. Methods to determine reimbursement rates for diagnosis related groups (DRG): a comparison of nine European countries. Health Care Manag Sci. 2006;9(3):215–23. doi: 10.1007/s10729-006-9040-1. [DOI] [PubMed] [Google Scholar]
- 18.Cattoir L, Vankeerberghen A, Boel A, Van Vaerenbergh K, De Beenhouwer H. Epidemiology of RSV and hMPV in Belgium: a 10-year follow-up. Acta Clin Belgica Int J Clin Lab Med [Internet]. 2019;74(4):229–35. doi: 10.1080/17843286.2018.1492509. [DOI] [PubMed] [Google Scholar]
- 19.James E, Crowe J. Virus Respiratorio Sincitial. En: tratado de Pediatría. Nelson, Kliegman, Stanton, St. Geme, Schor. 20ª Edición. Barcelona: Editorial Elsevier; 2016. Vol. 1. p. 1683–86. [Google Scholar]
- 20.ECDC Expert Consultation Meeting, Stockholm, 23-24 November 2015. Workshop on burden of RSV disease in Europe. https://www.ecdc.europa.eu/sites/portal/files/media/en/press/events/Documents/Meeting%20report%20ECDC%20RSV%20surv%20and%20burden%20of%20disease%20workshop%2023-24%20Nov.pdf
- 21.Buchwald AG, Tamboura B, Tennant SM, Haidara FC, Coulibaly F, Doumbia M. Epidemiology, risk factors, and outcomes of respiratory syncytial virus infections in newborns in Bamako, Mali. Clin Infect Dis. 2019;(April). doi: 10.1093/cid/ciy427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carbonell-Estrany X, Figueras-Aloy J, Law BJ, Infección Respiratoria Infantil por Virus Respiratorio Sincitial Study Group, Pediatric Investigators Collaborative Network on Infections in Canada Study Group . Identifying risk factors for severe respiratory syncytial virus among infants born after 33 through 35 completed weeks of gestation: different methodologies yield consistent findings. Pediatr Infect Dis J. 2004. Nov;23(11 Suppl):S193–201. doi: 10.1097/01.inf.0000144664.31888.53 [DOI] [PubMed] [Google Scholar]
- 23.Liese JG, Grill E, Fischer B, Roeckl-Wiedmann I, Carr D, Belohradsky BH, Munich RSV Study Group . Incidence and risk factors of respiratory syncytial virus-related hospitalizations in premature infants in Germany. Eur J Pediatr. 2003. Apr;162(4):230–36. Epub 2003 Mar 1. doi: 10.1007/s00431-002-1105-7 [DOI] [PubMed] [Google Scholar]
- 24.Gouyon JB, Rozé JC, Guillermet-Fromentin C, Glorieux I, Adamon L, DI Maio M, Miloradovich T, Anghelescu D, Pinquier D, Escande B, Elleau C. Hospitalizations for respiratory syncytial virus bronchiolitis in preterm infants at <33 weeks gestation without bronchopulmonary dysplasia: the CASTOR study. Epidemiol Infect. 2013. Apr;141(4):816–26. doi: 10.1017/S0950268812001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med. 2007. Sep;101(9):1845–63. doi: 10.1016/j.rmed.2007.04.011. Epub 2007 Jun 1. [DOI] [PubMed] [Google Scholar]
- 26.Simoes EA. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr. 2003;143:S118–26. doi: 10.1067/S0022-3476(03)00511-0. [DOI] [PubMed] [Google Scholar]
- 27.Chu HY, Tielsch J, Katz J, Magaret AS, Khatry S, LeClerq SC, Shrestha L, Kuypers J, Steinhoff MC, Englund JA. Transplacental transfer of maternal respiratory syncytial virus (RSV) antibody and protection against RSV disease in infants in rural Nepal. J Clin Virol. 2017;95:90–95. October 2016. doi: 10.1016/j.jcv.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gopal DP, Barber J, Toeg D. Pertussis (whooping cough). BMJ [Internet]. 2019. February;364:4–11. doi: 10.1136/bmj.l401. [DOI] [PubMed] [Google Scholar]
- 29.Murthy S, Godinho MA, Lakiang T, Lewis MGG, Lewis L, Nair NS. Efficacy and safety of pertussis vaccination in pregnancy to prevent whooping cough in early infancy. Cochrane Database Syst Rev. 2018;2018:4. [Google Scholar]
- 30.Modjarrad K, Giersing B, Kaslow DC, Smith PG, Moorthy VS. WHO consultation on respiratory syncytial virus vaccine development report from a World Health Organization Meeting held on 23-24 March 2015. Vaccine. 2016;34(2):190–97. doi: 10.1016/j.vaccine.2015.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scheltema NM, Kavelaars XM, Thorburn K, Hennus MP, van Woensel JB, van der Ent CK, Borghans JAM, Bont LJ, Drylewicz J. Potential impact of maternal vaccination on life-threatening respiratory syncytial virus infection during infancy. Vaccine [Internet]. 2018;36(31):4693–700. doi: 10.1016/j.vaccine.2018.06.021. [DOI] [PubMed] [Google Scholar]
- 32.Groothuis JR, Simoes EA, Levin MJ, Hall CB, Long CE, Rodriguez WJ, Arrobio J, Meer HC, Fulton DR, Welliver RC. Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. N Engl J Med. 1993;329(21):1524–30. doi: 10.1056/NEJM199311183292102. [DOI] [PubMed] [Google Scholar]
- 33.The IMpact-RSV Study Group . Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics. 1998;102(3):531–37. doi: 10.1542/peds.102.3.531. [DOI] [PubMed] [Google Scholar]
- 34.Feltes TF, Cabalka AK, Meer HC, Piazza FM, Carlin DA, Top FH, Connor EM, Sondheimer HM, The Cardiac Synagis Study Group F. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003;143(4):532–40. doi: 10.1067/S0022-3476(03)00454-2. [DOI] [PubMed] [Google Scholar]
- 35.Feltes TF, Sondheimer HM, Tulloh RM, Harris BS, Jensen KM, Losonsky GA, Griffin MP. A randomized controlled trial of motavizumab versus palivizumab for the prophylaxis of serious respiratory syncytial virus disease in children with hemodynamically significant congenital heart disease. Pediatr Res. 2011;70(2):18691. doi: 10.1203/PDR.0b013e318220a553. [DOI] [PubMed] [Google Scholar]
- 36.Carbonell-Estrany X, Simões EA, Dagan R. Motavizumab for prophylaxis of respiratory syncytial virus in high-risk children: a noninferiority trial. Pediatrics. 2010;125(1):e35–e51. doi: 10.1542/peds.2008-1036. [DOI] [PubMed] [Google Scholar]
- 37.O’Brien KL, Chandran A, Weatherholtz R, Jafri HS, Griffin MP, Bellamy T, Millar EV, Jensen KM, Harris BS, Reid R, et al. Efficacy of motavizumab for the prevention of respiratory syncytial virus disease in healthy Native American infants: a phase 3 randomised doubleblind placebo-controlled trial. Lancet Infect Dis. 2015;15:1398–408. doi: 10.1016/S1473-3099(15)00247-9. [DOI] [PubMed] [Google Scholar]
- 38.Pamela Griffin M, Yuan Y, Takas T, Domachowske JB, Madhi SA, Manzoni P, Simões EAF, Esser MT, Khan AA, Dubovsky F, et al., Nirsevimab Study Group . Single-dose nirsevimab for prevention of RSV in preterm infants. N Engl J Med. 2020. Jul 30;383(5):415–25. doi: 10.1056/NEJMoa1913556. [DOI] [PubMed] [Google Scholar]
- 39.Synagis (palivizumab): highlights of prescribing information. Gaithersburg (MD): MedImmune; 2017. [Google Scholar]
- 40.Capizzi A, Silvestri M, Orsi A, Cutrera R, Rossi GA, Sacco O. The impact of the recent AAP changes in palivizumab authorization on RSV-induced bronchiolitis severity and incidence. Ital J Pediatr. 2017;43(1):71. doi: 10.1186/s13052-017-0390-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Acero-Bedoya S, Wozniak PS, Sánchez PJ, Ramilo O, Mejias A. Recent Trends in RSV Immunoprophylaxis: clinical Implications for the Infant. Am J Perinatol [Internet]. 2019;36(S02):S63–7. https://www.thieme-connect.com/products/ejournals/abstract/ 10.1055/s-0039-1691803 [DOI] [PubMed] [Google Scholar]
- 42.Mazur NI, Martinón-Torres F, Baraldi E, Fauroux B, Greenough A, Heikkinen T, Manzoni P, Mejias A, Nair H, Papadopoulos NG, et al. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir Med. 2015;3(11):888–900. doi: 10.1016/S2213-2600(15)00255-6. [DOI] [PubMed] [Google Scholar]
- 43.Mazur NI, Higgins D, Nunes MC, Melero JA, Langedijk AC, Horsley N, Buchholz UJ, Openshaw PJ, McLellan JS, Englund JA, et al. The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect Dis. 2018;18(10):e295–311. doi: 10.1016/S1473-3099(18)30292-5. [DOI] [PubMed] [Google Scholar]
- 44.Mejias A, Garcia-Maurino C, Rodriguez-Fernandez R, Peeples ME, Ramilo O. Development and clinical applications of novel antibodies for prevention and treatment of respiratory syncytial virus infection. Vaccine [Internet]. 2017;35(3):496–502. doi: 10.1016/j.vaccine.2016.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]


