ABSTRACT
Background
Addressing COVID-19 vaccine hesitancy is key to ending the COVID-19 pandemic. Communication and media environments are potential drivers of vaccine hesitancy. It is worthwhile to examine the relationship between social media use and COVID-19 vaccine hesitancy.
Objective
This study aims to understand the prevalence and determinants of COVID-19 vaccine hesitancy.
Methods
Questionnaires were administered to 463 participants in mainland China. Factor analysis, correlation analysis, and linear regression models were utilized to examine the prevalence and influencing factors of COVID-19 vaccine hesitancy in China, as well as the relationship between social media use, media trust, health information literacy, and COVID-19 vaccine hesitancy.
Results
Lack of confidence and risk were identified as factors of COVID-19 vaccine hesitancy. Age, occupation status and income levels were significantly associated with COVID-19 vaccine hesitancy. In addition, we observed that frequency of social media use, diversity of social media use, media trust and health information literacy were significantly correlated with COVID-19 vaccine hesitancy.
Conclusion
Increased frequency and diversity of social media use, media trust and health information literacy can mitigate COVID-19 vaccine hesitancy and promote COVID-19 vaccination.
KEYWORDS: COVID-19, vaccine hesitancy, social media use, media trust, health information literacy
1. Introduction
To date, the outbreak of coronavirus disease (COVID-19) has posed a serious threat to the health of people worldwide. Countries worldwide have instituted containment strategies, such as physical distancing and lockdown suppression, to mitigate the spread of the epidemic. These non-pharmaceutical interventions (NPIs) have caused considerable disruption to societies and economies, even though they have proven successful. As such, a safe and effective COVID-19 vaccine is critical for fighting against COVID-19. Thus far, 2 billion cumulative doses of the COVID-19 vaccine have been administered worldwide, with China having the highest cumulative number of vaccine doses, followed by the United States. Timely vaccination and a high vaccination rate are required to control diseases effectively1. Epidemics will only cease once vaccination coverage reaches about 70% to 80%,2 but the COVID-19 vaccination rate remains low, the vaccination rate in China being less than 40% by 15 June 2021.3
Vaccine hesitancy, one of the top 10 global health threats,4 may be responsible for the low COVID-19 vaccination rate. The Strategic Advisory Group of Experts (SAGE) defined vaccine hesitancy as “delay in acceptance or refusal of vaccines despite availability of vaccination services.”5 Previous studies have indicated that outbreaks of invasive diseases, such as chickenpox and pertussis, tend to occur in communities with high vaccine hesitancy1. Therefore, it is worthwhile to understand the prevalence of COVID-19 vaccine hesitancy and related influencing factors.
Communication and media environments are potential drivers of vaccine hesitancy.6(pp2007–2012) Social media connects people while at the same time rapidly transferring, sharing, and accessing knowledge about COVID-19 on a large scale. This knowledge is likely to increase awareness of the COVID-19 vaccine, clarify its efficacy and safety, and alleviate vaccine hesitancy. However, social media has created an “infodemic,” an information overload both online and offline,7 where too much information (some correct and some wrong) makes it difficult for people to discover trustworthy sources of information. Misinformation and rumors about COVID-19 vaccination appear on social media, and people have no way to distinguish between the truth and falsity of the information, which leads to vaccine hesitancy.
Previous studies (see Table 1) have concluded that vaccine-related knowledge on social media promote vaccination intentions,8 while vaccine misinformation reduce vaccination intentions.9,10 A few scholars have explored the relationship between social media use and vaccine hesitancy.11 Wilson and Wiysonge12 assessed globally whether social media and online disinformation campaigns increase vaccine hesitancy in populations. While most existing studies have recognized social media use as a prevalent driver, very few studies have specifically explored the relationship and influencing mechanisms of social media use and vaccine hesitancy. Therefore, this study is novel and could guide the advancement of vaccine hesitancy theory.
Table 1.
Previous studies involving the relationship between social media and vaccination intentions
| Author | Years | Article | Research questions |
|---|---|---|---|
| Lama et al. | 2020 | Social media use and human papillomavirus awareness and knowledge among adults with children in the household: examining the role of race, ethnicity, and gender | Investigate the association between social media use and HPV-related awareness. |
| Featherstone and Zhang | 2020 | Feeling angry: the effects of vaccine misinformation and reputational messages on negative emotions and vaccination attitude | Investigate the association between vaccine misinformation and vaccination attitude. |
| Pan, Zhang, and Zhang | 2020 | Caught in the Crossfire: How Contradictory Information and Norms on Social Media Influence Young Women’s Intentions to Receive HPV Vaccination in the United States and China | Investigate the association between contradictory information regarding HPV vaccines obtained through social media and HPV vaccination attitudes. |
| Puri et al. | 2020 | Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases | Investigate how social media may be used to foster public trust in vaccination. |
| Wilson and Wiysonge | 2020 | Social media and vaccine hesitancy | Investigate the effect of social media on vaccination rates and attitudes toward vaccine safety. |
To address this research gap, this study aims to understand the prevalence and determinants of COVID-19 vaccine hesitancy and explore the mechanisms by which social media use influences COVID-19 vaccine hesitancy. Specially, we investigate how social media use, media trust and health information literacy jointly influence COVID-19 vaccine hesitancy. This study can help guide the advancement of the theory and practice of COVID-19 vaccination.
2. Data and method
2.1. Participants and measures
This study conducted a questionnaire survey on an online survey platform (Credamo) in mainland China from April 10 to April 14, 2020. Considering that the willingness of minors to be vaccinated may be largely influenced by their parents, the target population of this study was adults who had not received COVID-19 vaccine. Questionnaires were distributed to the target population, 566 respondents were recruited and 463 valid samples were returned. This study is a non-interventional research study, only investigating people’s COVID-19 vaccine hesitancy and other actual conditions, strictly abide by the Declaration of Helsinki. All the participants voluntarily completed the questionnaire on the platform, and the questionnaire instructions informed that this survey was for research use. In addition, the survey data were processed and did not involve information that could identify any participant. Therefore, all the participants in this study gave their informed consent and their privacy was kept strictly confidential.
Key constructs were measured as follows, and all constructs were measured by five-point Likert scales.
2.1.1. Vaccine hesitancy
A 13-item scale was used to measure COVID-19 vaccine hesitancy. Ten of these items used the vaccine hesitancy Likert Scale Questions developed by SAGE.13 Shapiro et al.14 tested the structure and internal consistency, structural validity, and standard validity of the above Likert Scale Questions, and concluded that the scale was good. We followed the five-point Likert scale used in the scale developed by SAGE, with 1–5 representing strongly disagree, disagree, neutral, agree and strongly agree respectively. A pilot study was conducted using a scale containing only ten items. After data analysis we found that the scale had good reliability and construct validity (Cronbach’ α > 0.6, KMO > 0.7, Bartlett’s Test of Sphericity P < .05) and could be factor analyzed and roughly divided into two dimensions. Because one of the dimensions contained only three variables, we added three items related to perceived risk that were summarized from previous studies, listed as questions 11 to 13 in Table 2.
Table 2.
Factor analysis of the COVID-19 vaccine hesitancy scale
| Items | F1 | F2 |
|---|---|---|
| 1. The COVID-19 vaccine is important to my health. | −0.08 | 0.75 |
| 2. The COVID-19 vaccine is effective. | −0.40 | 0.56 |
| 3. My COVID-19 vaccination helps maintain the health of others in my community. | −0.05 | 0.70 |
| 4. All types of COVID-19 vaccines offered by community health centers are beneficial. | −0.35 | 0.52 |
| 5. The COVID-19 vaccine is associated with greater risk compared to other established vaccines. | 0.77 | −0.18 |
| 6. The information about the vaccine provided in the COVID-19 vaccination policy is trustworthy. | −0.26 | 0.62 |
| 7. Vaccination against COVID-19 is a good way to prevent infection with COVID-19. | −0.19 | 0.61 |
| 8. I will decide whether to get the COVID-19 vaccine based on the recommendations of my health care provider. | −0.14 | 0.57 |
| 9. I am concerned that the COVID-19 vaccine may cause serious adverse reactions. | 0.84 | −0.12 |
| 10. I no longer need the COVID-19 vaccine because the COVID-19 outbreak has been effectively controlled in my country. | 0.33 | −0.57 |
| 11. I feel uncomfortable about receiving the COVID-19 vaccine that has been rushed into production. | 0.82 | −0.21 |
| 12. I feel uncomfortable about receiving the COVID-19 vaccine. | 0.79 | −0.27 |
| 13. The COVID-19 vaccine can cause disease. | 0.60 | −0.24 |
2.1.2. Social media usage
Inspired by the Health Information National Trends Survey,15 we used multiple choice questions to ask respondents if they engaged in the following four types of social media use behaviors over the past six months: a) visited social networking sites (such as WeChat, QQ, Weibo, and Douban) to exchange information about the vaccine with others; b) shared information about the vaccine on social networking sites; c) joined online forums or discussion groups about the vaccine; d) used the Internet on video sites (e.g., Tik Tok, iQiYi, Bilibili) to watch or post videos related to the COVID-19 vaccine. Besides, we measured the time and frequency of social media use by measurement scales adapted from Shensa et al.16 Respondents were asked about the frequency to get COVID-19 vaccine information using four typical social media platforms. The scale used was a 3-point Likert scale, with 1–3 representing never, occasionally and almost daily use respectively. We examined social media usage from two aspects: (1) diversity of social media use, which refers to the number of different types of social media usage. We considered higher number as higher diversity.; and (2) frequency of social media use, which refers to the average frequency of using each social media platforms, the higher the average frequency, the more frequently they accessed COVID-19 vaccine information on social media.
2.1.3. Media trust
Media trust was measured using a five-point Likert scale designed by Turcotte et al.17 where 1–5 represents strongly disagree, disagree, neutral, agree and strongly agree respectively. After conducting the pilot study we found that the scale had good reliability (Cronbach’ α > 0.7) and was suitable for use in the follow-up formal survey. In the formal survey, respondents were asked how much they trusted the Chinese media and the reported news related to the COVID-19 vaccine (Cronbach’s alpha = 0.78).
2.1.4. Health information literacy
Health information literacy scale was adapted from Eriksson-Backa et al.18 and initially followed the original scale using a five-point Likert scale containing eight questions to measure, with 1–5 indicating strongly disagree, disagree, neutral, agree and strongly agree respectively. A pilot study of the original scale revealed poor reliability (Cronbach’s α = 0.58) and internal consistency of the items. The results of the pilot study data analysis showed that the removal of three items resulted in a significant increase in the reliability of the scale (Cronbach’s α = 0.73). Therefore, three items were removed and a scale with five items was used to measure health information literacy. The sample items in the final measurement scale included: “I can easily know when I need health information,” and “I understand the main sources for obtaining health information” (Cronbach’s alpha = 0.78).
2.1.5. Demographic characteristics
Demographic variables include age, gender, education, income, residency, occupation, and living area. It is worth noting that occupation was classified into three categories according to COVID-19 vaccination priority: non-priority groups, priority groups, and unemployed groups. Priority groups refer to 9 types of COVID-19 vaccination priority groups, such as imported cold chain food-related personnel, staff involved in the prevention, control and treatment of the outbreak, transportation workers. Based on the number of COVID-19 confirmed cases in residential areas, we identified the provinces as three types of areas with more than 5,000, 1,000–5,000, and less than 1,000 confirmed COVID-19 cases.
2.2. Data analysis
Common factors of COVID-19 vaccine hesitancy items were first extracted using factor analysis. Subsequently, we summarized the demographic characteristics of the respondents and reported the correlations between all independent variables and vaccine hesitancy. Finally, demographic variables that were significantly correlated with vaccine hesitancy were used as control variables. Social media use frequency, social media use diversity, media trust, and health information literacy were used as independent variables. Regression models were then performed to explore the relationship between each variable and COVID-19 vaccine hesitancy. Data were analyzed using SPSS 26.0.
3. Results
3.1. Dimensions and prevalence of vaccine hesitancy
Before conducting a factor analysis of the vaccine hesitancy scale, the scale was demonstrated to be sustainable for factor analysis by correlation-matrix (> 0.3), KMO (0.9) and Bartlett’s test (p = .000). According to scree plot (shown in Figure 1), eigenvalues of greater than 1, and total variance explained, two factors were obtained after rotation. The results of the factor analysis are shown in Table 2, where two factors were extracted from 13 question items, containing seven and six items respectively. Two factors that represented “lack of confidence” and “risk” were identified, respectively according to previous studies.19 Thus, we considered these two factors as constructs and examined their reliability. The Cronbach’s alpha coefficients for the lack of confidence and risk were 0.78 and 0.85, respectively, indicating that the internal consistency was satisfactory. We recoded the first factor and ensured the high scores represent high levels of COVID-19 vaccine hesitancy. Vaccine hesitancy was characterized more by concerns about risk (Mean = 2.73, SD = 0.72) than lack of confidence (Mean = 1.85, SD = 0.43).
Figure 1.
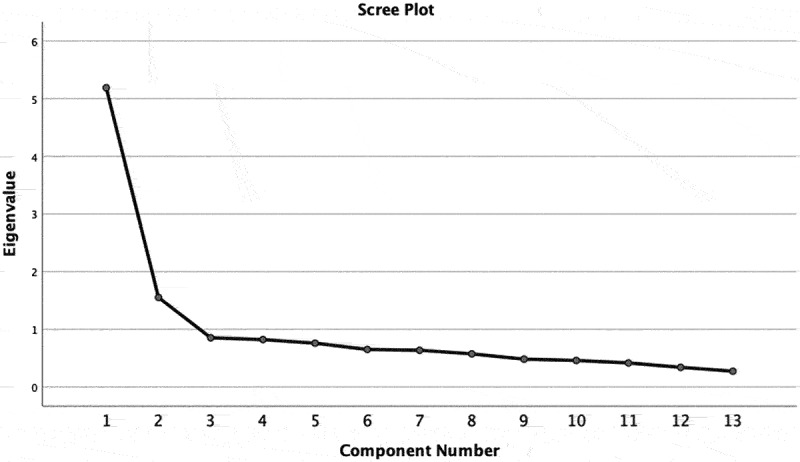
Scree plot authenticating factorability of the scale based on Eigenvalues of.
3.2. Descriptive statistics
Table 3 summarized the demographic characteristics of the sample and the prevalence of vaccine hesitancy. Notably, 48.16% of the respondents were located in provinces where the cumulative number of confirmed COVID-19 cases ranged from 1000 to 5000, and only 3.24% of the respondents were located in those where the cumulative number of confirmed cases exceeded 5000. Non-priority groups accounted for 80.99%, followed by the unemployed groups (17.1) and COVID-19 vaccination priority groups (1.94%). Only about one-tenth of the respondents were living alone. One-way ANOVA indicated that age, occupations, and income levels showed significant correlations with perceived risk for COVID-19 vaccine hesitancy.
Table 3.
Sample characteristics and prevalence of vaccine hesitancy (n = 463)
| Vaccine hesitancy |
||||
|---|---|---|---|---|
| N (%) | Mean (SD) | Lack of confidence | Risk | |
| Gender | 0.90a | 0.12a | ||
| Male | 199 (43.0) | |||
| Female | 264 (57.0) | |||
| Age | 28.88 (7.76) | 0.10*b | −0.02b | |
| Area | 0.56a | 0.67a | ||
| 5001 and above | 15 (3.2) | |||
| 1000–5000 | 223 (48.2) | |||
| Less than 1000 | 225 (48.6) | |||
| Occupation | 0.18a | 0.01*a | ||
| Priority groups | 9 (1.9) | |||
| Non-priority groups | 375 (80.99) | |||
| Unemployed groups | 79 (17.1) | |||
| Residence patterns | 0.29a | 0.08a | ||
| Living with others | 413 (89.2) | |||
| Living alone | 50 (10.8) | |||
| Education | 0.64a | 0.05a | ||
| Junior college and below | 77 (16.6) | |||
| Undergraduate | 347 (75.0) | |||
| Postgraduate and above | 39 (8.4) | |||
| Income | 0.37a | 0.02*a | ||
| Less than 3000 CNY | 116 (25.1) | |||
| 3000–8000 CNY | 207 (44.7) | |||
| 8001 CNY or more | 140 (30.2) | |||
| Residency | 0.35a | 0.90a | ||
| Rural | 31 (6.7) | |||
| Urban | 432 (93.3) | |||
| Diversity of social media use | 2.20 (0.86) | −0.14**b | −0.06b | |
| Frequency of social media use | 2.20 (0.42) | −0.14** b | −0.17*** b | |
| Media Trust | 3.86 (0.52) | −0.62*** b | −0.56*** b | |
| Health Information Literacy | 3.90 (0.53) | −0.43*** b | −0.35*** b | |
*p < .05, **p < .01, *** p < .001.
a: p-value of one-way ANOVA.
b: p-value of Pearson’s correlation analysis.
Respondents reported high levels of social media use (Mean = 2.20, SD = 0.42), media trust (Mean = 3.86, SD = 0.52), and health information literacy (Mean = 3.90, SD = 0.53). According to the Pearson’s correlation analysis, we observed frequency of social media use (for lack of confidence r = −0.14, p < .01; for risk r = −0.17, p < .001), diverse use of social media (for lack of confidence r = −0.14 p < .01), media trust (for lack of confidence r = −0.62 p < .001; for risk r = −0.56, p < .001) and health information literacy (for lack of confidence r = −0.43, p < .001; for risk r = −0.35, p < .001) were significantly correlated with COVID-19 vaccine hesitancy.
3.3. Regression results
Table 4 shows the associations of social media use frequency, social media use diversity, media trust, and health information literacy with lack of confidence (model 1) and risk (model 2) for vaccine hesitancy, controlling for age, income level and occupation status. We found that diversity of social media use (β = −0.10, SE = 0.02), media trust (β = −0.54, SE = 0.03) and health information literacy (β = −0.20, SE = 0.03) were significantly associated with a decline in the lack of confidence for vaccine hesitancy. In Model 2, media trust showed a significant negative association with risk for vaccine hesitancy (β = −0.50, SE = 0.06), while frequency of social media use, diversity of social media use and health information literacy as independent variables did not significantly correlate with risk for vaccine hesitancy.
Table 4.
Associations between two dimensions of vaccine hesitancy and occupation, education, income, frequency of social media use, diversity of media use, media trust, and health information literacy
| Variable | Model 1: Vaccine hesitancy (lack of confidence) β(SE) |
Model 2: Vaccine hesitancy (risks) β(SE) |
|---|---|---|
| Age | 0.05 (0.00) | 0.01 (0.00) |
| Occupation (reference: Non-priority groups) | ||
| Priority groups | 0.00 (0.11) | −0.09* (0.20) |
| Unemployed groups | −0.09 (0.05) | −0.02 (0.09) |
| Income (reference: Less than 3000 CNY) | ||
| 3000–8000 CNY | 0.07 (0.05) | −0.04 (0.09) |
| 8001 CNY or more | 0.14** (0.05) | −0.08 (0.10) |
| Frequency of social media use | 0.02 (0.04) | −0.07 (0.08) |
| Diversity of social media use | −0.10* (0.02) | 0.05 (0.04) |
| Media Trust | −0.54*** (0.03) | −0.50*** (0.06) |
| Health Information Literacy | −0.20*** (0.03) | −0.08 (0.06) |
| Observation | 463 | 463 |
| R2 | 0.45 | 0.34 |
| Adjusted R2 | 0.43 | 0.32 |
*p < .05, **p < .01, *** p < .001.
In addition, respondents with an income of 8001 CNY or more were more likely to lack confidence for COVID-19 vaccines (β = 0.14, SE = 0.05). The COVID-19 vaccine priority group was less likely to perceive the risk of COVID-19 vaccines.
4. Discussion
4.1. Key findings
This study reveals an overall low level of COVID-19 vaccine hesitancy in mainland China. The reasons may include that people are willing to achieve herd immunity since the COVID-19 pandemic is still spreading globally. Furthermore, free COVID-19 vaccines provided to all people20 increases their willingness to get vaccinated. Most publicly available information emphasizes the safety and efficacy of the vaccine, allowing people to receive it with confidence. Our study obtained several main findings as discussed below.
First, occupation status and income levels were associated with risk for COVID-19 vaccine hesitancy, and age was positively associated with lack of confidence. A possible explanation is that older people have less opportunity to receive information about the effectiveness of the COVID-19 vaccine on media outlets, or they cannot distinguish between rumors and reliable information. This observation suggests that the digital divide may cause vaccine hesitancy.
Second, social media use was negatively correlated with COVID-19 vaccine hesitancy. We assume that people can obtain more knowledge about COVID-19 vaccine (both right and wrong perceptions) when they use social media more frequently and use various social media channels. Previous studies showed that using social media can help increase HPV vaccine awareness among adults with children in the household.8 Therefore, it can be assumed that the more frequently information about the COVID-19 vaccine is obtained through social media, awareness of the COVID-19 vaccine will increase, and vaccine hesitancy will subsequently decrease. In contrast, many studies have found a negative association between the use of social media and the intention to accept vaccines.21,22 Therefore, it is likely that messages encouraging vaccination are circulating on Chinese social media, which facilitates the intention to vaccination. In addition, in terms of exaggerated information, previous studies have shown that exaggerated information about COVID-19 is mainly exaggerated pandemic estimates, exaggerated case fatality rate and other information that exaggerates the severity of the virus.23 Based on this, we speculate that exaggerated information about the COVID-19 vaccine on social media is likely to be primarily information that exaggerates the negative effects of the vaccine. In contrast, information that exaggerates the negative effects of the vaccine could lead to increased vaccine hesitancy due to fear of the vaccine. Since our results show that social media use is negatively associated with COVID-19 vaccine hesitancy, we speculate that because the Chinese government is more stringent in controlling false information on social media, the amount of exaggerated information in social media is less likely to influence people’s vaccination intentions.
Third, media trust toward the domestic media was negatively associated with vaccine hesitancy. Because media trust can influence public opinion on important policies,17 it is worthwhile to examine the impact of media trust on COVID-19 vaccine hesitancy. Taha, Matheson, and Anisman24 showed that as people’s trust in the media decreased, their willingness to get vaccinated decreased. Thus, the low level of vaccine hesitancy may contribute to the high level of media trust in mainland China.
Finally, health information literacy was negatively associated with vaccine hesitancy. This result is consistent with Jarrett et al,25 who pointed out that improving vaccination knowledge and awareness is an effective measure to address vaccine hesitancy. People with higher levels of health information literacy are more likely to distinguish factual information from false information, and consequently have more confidence in the effectiveness of the vaccine and perceive less risk, making them less hesitant about the vaccine.
4.2. Implications
This study has several implications for policy makers and social media companies. First, our findings suggest that social media currently plays a positive role in reducing vaccination hesitancy, but we cannot ignore the influence of the large number of falsehoods, misinformation, and anti-vaccination groups that still exist in social media. Many studies have shown that misinformation, rumors, and statements from anti-vaccine groups in social media are likely to exacerbate vaccine hesitancy.11,26,27 Therefore, we suggest government and social media companies make a great effort to regulate misinformation in social media. Policy makers should be aware of the dangers of misinformation in social media and limit false and unconfirmed COVID-19 vaccine-related information by punishing users who maliciously spread false information and disinformation accordingly.21 At the same time, policy makers should strive to leverage the role of social media in mitigating vaccine hesitancy by creating appropriate incentives to encourage relevant professional bodies or personnel to promote COVID-19 vaccine information and science on social media. Alternatively, the government can also establish official government accounts on social media to push correct and confirmed COVID-19 vaccine information, pay attention to the needs and preferences of the target audience in the COVID-19 propaganda and science information, and make the information content more user-friendly.8,27 On the part of social media companies, social media sites can purge anti-COVID-19 vaccine information by tagging false and misleading information in a timely manner, while proactively pushing correct COVID-19 vaccine information to users.11
Second, measures can be taken to enhance media trust to mitigate COVID-19 vaccine hesitancy. Many studies have identified health care providers as one of the most trusted sources of information, so encouraging health care providers to play a role in social networks is one possible way to enhance media trust.8,11,24,28 Specifically, healthcare professionals can be encouraged to create dedicated social media accounts to use social media platforms for science outreach; and to actively respond to questions about the COVID-19 vaccine and clarify misconceptions about it. This will take more extra time of healthcare providers and therefore relevant departments need to give healthcare providers corresponding incentives. In addition, influential leaders and celebrities can also have an impact on vaccine hesitancy,6,11 so we suggest influential leaders promote the COVID-19 vaccine on social media, making full use of the influence of leaders and the rapid, widespread dissemination of information on social media to mitigate vaccine hesitation. Another way could be to increase trust in information about the COVID-19 vaccine by indicating authoritative sources, real data, or scientific support for the information, thereby increasing trust in the relevant media.11
Third, we need to take action to improve people’s health information literacy to reduce people’s COVID-19 vaccine hesitancy, and this requires the joint efforts of many parties. The government can teach people how to distinguish the authenticity of COVID-19 vaccine-related information through various social media or other channels, and provide authoritative access to relevant information. Social media companies can set up accuracy alerts on social media to remind users of the need to be aware of the accuracy of the content they are viewing when viewing posts on social media.11 Citizens can take the initiative to learn about COVID-19 vaccine, obtain relevant health information, and improve their own information screening ability.
4.3. Strengths, limitations & future research
This study measured vaccine hesitancy and provided valuable information about the prevalence of COVID-19 vaccine hesitancy in mainland China. In addition, the relationship between social media use, media trust, health information literacy, and COVID-19 vaccine hesitancy were also explored empirically. The limitations of this study consist mainly of the following points. Firstly, the sample for this study may not be representative enough and there is selection bias since the study draws its sample from the Credamo platform, where the established sample is similar in terms of educational attainment, age and other characteristics; at the same time, this survey is subject to the Hawthorne Effect, and study participants may change their behavioral tendencies while taking the survey due to, for example, awareness that they are being studied, leading to a degree of reporting bias, so our findings may not fully reflect the true picture. Secondly, this study ignored the effect of confounding factors and did not treat them accordingly. Further research could reveal other potentially important influences. In addition, as mentioned above, this study contradicts some previous findings regarding the correlation between frequency of social media use and vaccine hesitancy, so further research in this area could be pursued.
5. Conclusion
Addressing COVID-19 vaccine hesitancy is key to ending the COVID-19 pandemic. This study suggests that social media use, media trust and health information literacy were negatively associated with COVID-19 vaccine hesitancy. Therefore, joint efforts by the government, social media companies, and individuals are needed to alleviate COVID-19 vaccine hesitancy and increase the public’s willingness to get vaccinated.
Acknowledgments
The authors are grateful to Ms. Aruhan Mu and Ms. Feiyang Zheng at School of Medicine and Health Management, Huazhong University of Science & Technology, who gave valuable advices on this paper.
Authors’ contributions and Authorship
Hui Ouyang (HO), Xiaohan Ma (XM) and Dr. Xiang Wu (XW) designed the study. HO organized the data, conducted the statistical analysis, and drafted the first version of the manuscript. XW and XM revised the manuscript. All authors attest they meet the ICMJE criteria for authorship.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical approval
This study is a survey study and is non-interventional, so ethical approval was not required. The study was conducted using the Credamo platform, and participants voluntarily completed the questionnaire on the platform. All participants were informed of the reason for conducting the study through the questionnaire instructions before the start of the survey, and were assured that the questionnaire was for research use only and strictly confidential. Therefore, all participants who participated in this questionnaire agreed to participate in this study.
References
- 1.Salmon DA, Dudley MZ, Glanz JM, Omer SB.. Vaccine hesitancy causes, consequences, and a call to action. Vaccine. 2015;33(4):D66–7. doi: 10.1016/j.vaccine.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 2.Episode #1 - Herd immunity. [accessed 2021 Jun 21]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-1.
- 3.Coronavirus (COVID-19) Vaccinations - Statistics and Research . Our world in data. [accessed 2021 Jun 24]. https://ourworldindata.org/covid-vaccinations.
- 4.Ten threats to global health in 2019. [accessed 2021 Jul 25]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 5.Dudley MZ, Privor-Dumm L, Dube E, MacDonald NE. Words matter: vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine. 2020;38(4):709–11. doi: 10.1016/j.vaccine.2019.11.056. [DOI] [PubMed] [Google Scholar]
- 6.Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 7.Managing the COVID-19 infodemic: promoting healthy behaviours and mitigating the harm from misinformation and disinformation. [accessed 2021 Jun 24]. https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation.
- 8.Lama Y, Quinn SC, Nan X, Cruz-Cano R. Social media use and human papillomavirus awareness and knowledge among adults with children in the household: examining the role of race, ethnicity, and gender. Hum Vaccin Immunother. 2020;1–11. doi: 10.1080/21645515.2020.1824498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Featherstone JD, Zhang J. Feeling angry: the effects of vaccine misinformation and refutational messages on negative emotions and vaccination attitude. J Health Commun. 2020;25(9):692–702. doi: 10.1080/10810730.2020.1838671. [DOI] [PubMed] [Google Scholar]
- 10.Pan S, Zhang D, Zhang J. Caught in the crossfire: how contradictory information and norms on social media influence young women’s intentions to receive HPV vaccination in the United States and China. Front Psychol. 2020;11. doi: 10.3389/fpsyg.2020.548365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–93. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R; Hesitancy SWGV . Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34, SI):4165–75. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 14.Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, Perez S, Rosberger Z. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36(5):660–67. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 15.View HINTS questions | HINTS. [accessed 2021 Jun 24]. https://hints.cancer.gov/view-questions-topics/all-hints-questions.aspx#divtopanchor.
- 16.Shensa A, Escobar-Viera CG, Sidani JE, Bowman ND, Marshal MP, Primack BA. Problematic social media use and depressive symptoms among US young adults: a nationally-representative study. Soc Sci Med. 2017;182:150–57. doi: 10.1016/j.socscimed.2017.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turcotte J, York C, Irving J, Scholl RM, Pingree RJ. News recommendations from social media opinion leaders: effects on media trust and information seeking. J Comput-Mediated Commun. 2015;20(5):520–35. doi: 10.1111/jcc4.12127. [DOI] [Google Scholar]
- 18.Eriksson-Backa K, Ek S, Niemela R, Huotari M-L. Health information literacy in everyday life: a study of Finns aged 65-79 years. Health Informatics J. 2012;18(2,SI):83–94. doi: 10.1177/1460458212445797. [DOI] [PubMed] [Google Scholar]
- 19.Thaker J. The persistence of vaccine hesitancy: COVID-19 vaccination intention in New Zealand. J Health Commun. 2021;26(2):104–11. doi: 10.1080/10810730.2021.1899346. [DOI] [PubMed] [Google Scholar]
- 20.China to offer free COVID-19 vaccination to citizens: official - people’s daily online. [accessed 2021 Nov12]. http://en.people.cn/n3/2021/0110/c90000-9807645.html.
- 21.Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digital Health. 2020;2(10):E504–E505. doi: 10.1016/S2589-7500(20)30227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hwang J, Shah DV. Health information sources, perceived vaccination benefits, and maintenance of childhood vaccination schedules. Health Commun. 2019;34(11):1279–88. doi: 10.1080/10410236.2018.1481707. [DOI] [PubMed] [Google Scholar]
- 23.Ioannidis JPA. Coronavirus disease 2019: the harms of exaggerated information and non‐evidence‐based measures. Eur J Clin Invest. 2020;50(4). doi: 10.1111/eci.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taha SA, Matheson K, Anisman H. The 2009 H1N1 influenza pandemic: the role of threat, coping, and media trust on vaccination intentions in Canada. J Health Commun. 2013;18(3):278–90. doi: 10.1080/10810730.2012.727960. [DOI] [PubMed] [Google Scholar]
- 25.Jarrett C, Wilson R, O’Leary M, Eckersberger E, Larson HJ. Strategies for addressing vaccine hesitancy – a systematic review. Vaccine. 2015. [accessed 2020 Dec 8];33(34):4180–90. (WHO Recommendations Regarding Vaccine Hesitancy). http://www.sciencedirect.com/science/article/pii/S0264410X15005046. [DOI] [PubMed] [Google Scholar]
- 26.Chadwick A, Kaiser J, Vaccari C, Freeman D, Lambe S, Loe BS, Vanderslott S, Lewandowsky S, Conroy M, Ross ARN, et al. Online social endorsement and COVID-19 vaccine hesitancy in the United Kingdom. Social Media + Soc. 2021;7(2). doi: 10.1177/20563051211008817. [DOI] [Google Scholar]
- 27.Pullan S, Dey M. Vaccine hesitancy and anti-vaccination in the time of COVID-19: a Google trends analysis. Vaccine. 2021;39(14):1877–81. doi: 10.1016/j.vaccine.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016. [accessed 2020 Dec 8];34(52):6700–06. (The Changing Face of Vaccines and Vaccination). http://www.sciencedirect.com/science/article/pii/S0264410X1630977X. [DOI] [PubMed] [Google Scholar]


