Abstract
Introduction
Men who have sex with men (MSM) living with HIV are more likely to be depressed than MSM without HIV. The AIDS epidemic will not end if the needs of people living with HIV and the determinants of health are not being addressed. Compared to HIV individuals without depression, depressed HIV individuals have worse clinical outcomes and higher mortality risk. Depression is caused by a complex combination of social, psychological, and biological variables. This systematic review, thereby motivated by the need to address this gap in the literature, aims to articulate determinants of depression among MSM living with HIV according to the biopsychosocial approach.
Methodology
We systematically searched four databases from 2011 to 2021. We searched for observational studies on determinants of depression among MSM living with HIV. The outcome is depression based on the categorical or numerical outcome. Two reviewers independently extracted data and assessed study risks of bias. Any disagreements are consulted with the third reviewer.
Results
We identified 533 articles, of which only eight studies are included. A total of 3,172 MSMs are included in the studies. We found the determinants of depression and categorized them according to biological, psychological, and social approaches.
Conclusion
The determinants of depression with the strongest evidence across studies were enacted HIV-related stigma, unemployment, sleep disturbance, current smoker, black ethnicity, born overseas, ART initiation, and access to mental health care. Despite weaker evidence, the other relevant determinants to be included were older age, internalized stigma, self-efficacy, and social support. Efforts to improve or prevent depression among MSM living with HIV could benefit from addressing the determinants of depression based on the biopsychosocial approach immediately after HIV diagnosis. Integrating mental health screening and care into HIV treatment settings would strengthen HIV prevention and care outcomes and improve access to mental healthcare.
1. Introduction
Depression is marked by persistent sadness and a lack of interest or enjoyment in previously satisfying or pleasurable behaviors. It may also cause sleep and appetite disturbances, exhaustion, and poor concentration [1]. Based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD–10), depression is diagnosed if the patient has two of the first three symptoms: 1) depressed mood; 2) loss of interest in everyday activities; and 3) reduction in energy, plus at least two of the remaining seven depressive symptoms [2]. An estimated 264 million people worldwide suffer from depression [1]. MSM living with HIV were more likely to be depressed compared to MSM without HIV. The previous extensive systematic reviews show that 40% to 43% of MSM living with HIV had depression [3, 4].
Compared to HIV patients without depression, depressed HIV patients have a worsened immune function, decreased adherence to antiretroviral therapy (ART), slower viral suppression, faster progression to AIDS, and a higher risk of mortality [5]. MSM are vulnerable to mental health problems due to sexual minority stress, society’s homophobia, sexual orientation-based victimization, and stigmatization that hinder healthy behavior [6, 7]. Depression is caused by a variety of complicated interactions or multilevel mechanisms, including the following: 1) social factors such as socioeconomic status and social support; 2) psychological factors such as health beliefs and lifestyle and 3) biological factors such as physiological or genetic predispositions, and hence making the biopsychosocial (BPS) approach valid to investigate depression [1, 8, 9]. Concerning social factors, depression among MSM living with HIV was associated with physical abuse, being HIV positive, HIV risk behaviors [10], poverty and food insecurity [11, 12], and being unemployed [13]. The psychological factors of depression include verbal abuse [10], perceived stigma [14], low social support [15], and substance use [16]. Finally, the biological factors include younger age [17] and opportunistic infections [12]. The BPS model consists of the concept of psychobiological vulnerability, which is determined by risk factors such as biogenetic, psychological, somatic, and societal nature [18]. Therefore, the biopsychosocial approach will provide a holistic approach to finding the determinants of depression among MSM living with HIV.
Depression experienced by MSM living with HIV has physical, educational, social, financial, psychological, and short- and long-term health consequences [11]. The co-occurrence of HIV and depression was associated with poor health outcomes like poor quality of life and worsening disease states [19]. Untreated depression in MSM living with HIV can lead to risky sexual behavior, alcohol and drug misuse and abuse, and suicide [20]. Among MSM with newly diagnosed HIV, depression leads to poor adherence to antiretroviral drugs [21], resulting in poor immunological and virological outcomes [22].
According to the Sustainable Development Goals (SDGs) of the AIDS response, no one should be left behind. The AIDS epidemic will not end if the needs of people living with HIV (PLHIV) and the determinants of health are not being addressed [23]. The SDGs that firmly address mental health include the following: 1) SDG 3: Good Health and Well-being; 2) SDG 5: Gender Equality; 3) SDG 10: Reduced Inequality; and 4) SDG 16: Peace, Justice, and Strong Institutions. The indicators are important because they encourage equity, justice, patient-centered care, community involvement, and mental health awareness [24]. The future of the HIV response is inextricably tied to worldwide efforts to combat non-communicable diseases (NCDs), including mental illness. The worldwide HIV response has increased the chances for gay and bisexual men groups to be recognized as citizens, holders of rights, and beneficiaries of public health programs in their nations, which is a distinct success [25].
Despite the growing HIV epidemic and depression among MSM worldwide and increased research in this population, empirical evidence on depression based on the biopsychosocial approach has not been synthesized. This systematic review, thereby motivated by the need to address this gap in the literature, aims to articulate determinants of depression among MSM living with HIV according to the biopsychosocial approach. It will offer recommendations for future mental and behavioral health interventions to reduce potential adverse outcomes in the HIV care continuum. Identifying determinants of depression will help the health authorities, stakeholders, and policymakers to provide a complete health package for MSM, in general, to support Ending AIDS 2030.
2. Methodology
This systematic review protocol was written following the Preferred Reporting Items for Systematic Review and PRISMA guidelines.
2.1 Eligibility criteria
Articles were included if they fulfill the following: 1) Published in English from 2011 to 2021; 2) used cross-sectional, cohort study, case-control study design; 3) used a standard instrument to assess depression; 4) Population: MSM living with HIV aged 18 and above; 5) Exposure: Factors associated with depression; 6) Comparison: MSM living with HIV without depression; and 7) Outcome: Depression. The review has depression determined by standard or accepted tools or instruments with categorical or numerical outcomes.
In contrast, articles were excluded if they were the following: 1) Review papers, conference abstracts, case reports, and qualitative studies, study protocol, mixed-methods study; 2) No statistical analysis conducted; and 3) If there is more than one study involving the same population, only the most recent published or comprehensive one will be included.
2.2 Information sources
Two reviewers independently searched four databases: 1) Academic Search Complete; 2) CINAHL; 3) Medline; and 4) SCOPUS from 3 May 2021 to 17 May 2021.
2.3 Search strategy
The following search terms were used: depression or depressive disorder or major depressive disorder AND HIV or Human Immunodeficiency Virus AND men who have sex with men or gay or homosexual or bisexual or MSM AND factors or determinants or predictors.
2.4 Study selection
Two reviewers independently screened the papers in two stages: title/abstract screening and full-text screening. The eligibility criteria were then compiled into a checklist. Then, we checked the titles and abstracts against the eligibility criteria. Next, we obtained all possibly eligible articles’ entire texts. The whole text was reviewed by two reviewers who applied inclusion criteria independently. When required, we resolved differences by consensus at both screening stages with the help of a third reviewer. All differences were recorded in Excel spreadsheets, along with the reasons for inclusion or exclusion.
2.5 Data collection process
We developed a data extraction sheet to guide data collection. This sheet directed us to collect the definition and methods for each step of the cascade, the results of estimations, and data sources. Two reviewers independently read each article and extracted the relevant data. In discussions with a third reviewer, any discrepancies in the extracted data were resolved by consensus.
2.6 Data item
The following data were extracted into two tables. The first table is the characteristic of selected articles: The first author/year, timing of data collection, study aim, study design, study location, and sample size. The second table is the determinants of depression according to the BPS approach: Author/year, screening tool, outcome definition (screening instrument cut-off or diagnostic criteria), and significant variables associated with depression and statistical value. When there were multiple estimates over time in the same study sample, the last one was chosen.
2.7 Quality assessment
The selected articles were entered into the quality assessment stage. Two authors independently assessed the quality of studies using the Joanna Briggs Institute (JBI) Appraisal Tools. There are two separate tools addressed specifically for cross-sectional and cohort studies. There are eight questions for the cross-sectional checklist, and 12 questions for the cohort checklist. Each question requires answering yes, no, unsure, or not applicable. Then, the decision was made on overall appraisal whether to include, exclude the studies, or seek further information [26]. The reviewers then met to discuss the results of their critical appraisal for the final appraisal. If the two reviewers disagree on the final critical appraisal and this cannot be resolved through discussion, the third reviewer was consulted. The authors then determined whether a study can be included, excluded, or seek further information.
2.8 Summary measures
The principal summary measures include multivariate analysis. The adjusted odds ratio (AOR) and beta values were taken with a 95% confidence interval. The significant value was chosen at P<0.05.
3. Results
3.1 Study selection
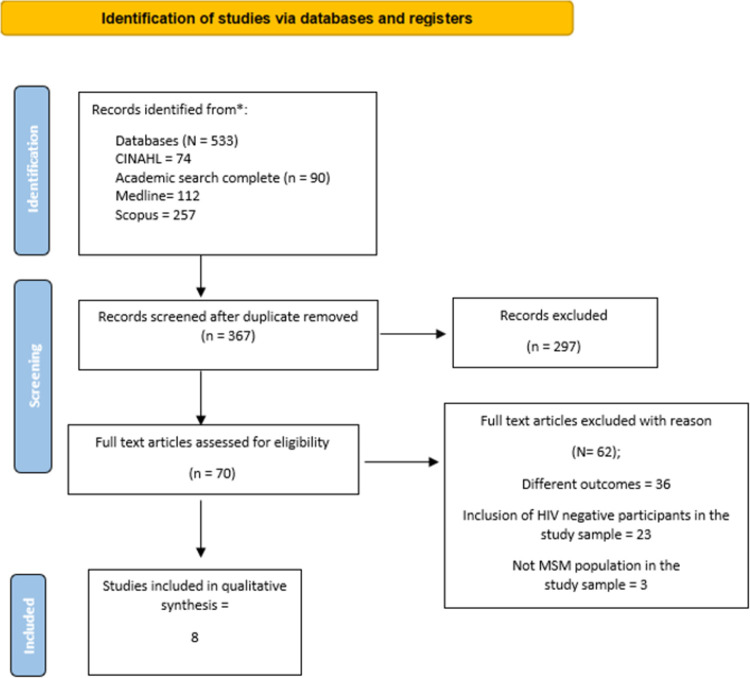
We identified 533 articles through our electronic databases and manual search, reducing them to 367 after removing duplicates. Then, 297 articles were excluded following titles and abstracts screening due to different study designs, not MSM living with HIV populations, and different outcomes. Then, 70 full-text articles were screened, of which 62 were excluded for the following reasons: different outcomes, the inclusion of HIV-negative participants in the study sample, and not MSM population in the study sample. Finally, eight studies were included in this review. Fig 1 shows the PRISMA flowchart.
Fig 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart for selecting studies.
3.2 Studies characteristics
In the eight studies, there were a total of 3,172 MSM living with HIV. Four studies were conducted in China [27–30], two studies in the USA [31, 32], and one in Australia [33]. One study was conducted in two countries, which were the United Kingdom and Ireland [34]. The papers were published between 2015 and 2020. Six studies used a cross-sectional design, and two studies used a cohort design. The results are presented in Table 1.
Table 1. Characteristics of selected articles.
| No | Author/year | Timing of data collection | Study aim | Study design | Study location | Sample size |
|---|---|---|---|---|---|---|
| 1. | Li et al. (2016) [27] | Not mentioned | To investigate the prevalence of depression and anxiety, and the significance of two risk factors (enacted HIV-related stigma and perceived stress) and one protective factor (gratitude) of depression/anxiety. | Cross-sectional | Chengdu, China | 321 |
| 2. | Tao et al. (2017) [28] | Not mentioned | To assess the relationship between HIV-related stigma and depression. | Cross-sectional | Beijing, China | 367 |
| 3. | Wang et al. (2019) [29] | March 2013 to March 2014. | To evaluate the relationship between self-efficacy and depression and anxiety. | Cross-sectional | Beijing, China | 367 |
| 4. | Luo et al. (2020) [30] | March 2013 to August 2014. | To determine the changes in mental health (depression and anxiety) one year after HIV diagnosis and the disparities in mental health trajectories. | Cohort | Changsha, China | 258 |
| 5. | Rood et al. (2015) [31] | Not mentioned | To investigate how different coping combinations may predict depression severity and the utilization of a range of clinically meaningful support services. | Cross-sectional | Massachusetts (USA) | 170 |
| 6. | Irwin et al. (2018) [32] | October 2001 to October 2012. | To determine an association between sleep disturbance and depression. | Cohort | Four sites in the USA: Baltimore, Maryland; Chicago, Illinois; Los Angeles, California; Pittsburgh, Pennsylvania. | 1054 |
| 7. | Heywood & Lyon (2016) [33] | August 2014 to December 2014. | To identify and compare risk and protective factors for depression, anxiety, and generalized stress. | Cross-sectional | Online recruitment in Australia | 357 |
| 8. | Murphy et al. (2018) [34] | May and November 2014 | To investigate the associations between forms of HIV-related optimism, HIV-related stigma, and anxiety and depression. | Cross-sectional | UK and Ireland | 278 |
3.3 Study quality
The appraisal results for the included studies are outlined in Tables 2 and 3. All studies included in the review got over 50% "yes" answers in the critical appraisal checklist. All outcomes in the studies included were measured in a valid and reliable way. One study had 75% “yes” [14], and one study had 83% “yes” [32] and the remaining studies had 100% yes based on the JBI checklist. Tables 2 and 3 show the quality assessment of cross-sectional and cohort studies.
Table 2. Quality assessment of cross-sectional studies.
| Questions | Li et al. (2016) [27] | Tao et al. (2017) [28] | Wang et al. (2019) [29] | Rood et al. (2015) [31] | Heywood & Lyon (2016) [33] | Murphy et al. (2018) [34] |
|---|---|---|---|---|---|---|
| 1. Were the criteria for inclusion in the sample clearly defined? | Y | Y | N | Y | Y | Y |
| 2. Were the study subjects and the setting described in detail? | Y | Y | N | Y | Y | Y |
| 3. Was the exposure measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y |
| 4. Were objective, standard criteria used for measurement of the condition? | Y | Y | Y | Y | Y | Y |
| 5. Were confounding factors identified? | Y | Y | Y | Y | Y | Y |
| 6. Were strategies to deal with confounding factors stated? | Y | Y | Y | Y | Y | Y |
| 7. Were the outcomes measured in a valid and reliable way? | Y | Y | Y | Y | Y | Y |
| 8. Was appropriate statistical analysis used? | Y | Y | Y | Y | Y | Y |
| % Yes | 100 | 100 | 75 | 100 | 100 | 100 |
Abbreviations: Y = Yes; N = No; U = Unclear; NA = Not applicable.
Table 3. Quality assessment of cohort studies.
| Questions | Luo et al. (2020) [30] | Irwin et al. (2018) [32] |
|---|---|---|
| 1. Were the two groups similar and recruited from the same population? | Y | Y |
| 2. Were the exposures measured similarly to assign people to both exposed and unexposed groups? | Y | Y |
| 3. Was the exposure measured in a valid and reliable way? | Y | Y |
| 4.Were confounding factors identified? | Y | Y |
| 5. Were strategies to deal with confounding factors stated? | Y | Y |
| 6. Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)? | Y | Y |
| 7. Were the outcomes measured in a valid and reliable way? | Y | Y |
| 8. Was the follow up time reported and sufficient to be long enough for outcomes to occur? | Y | Y |
| 9. Was follow up complete, and if not, were the reasons to loss to follow up described and explored? | Y | N |
| 10. Were strategies to address incomplete follow up utilized? | Y | U |
| 11. Was appropriate statistical analysis used? | Y | Y |
| % Yes | 100 | 83 |
Abbreviations: Y = Yes; N = No.
3.4 Results of individual studies
Our review identified three domains for determinants of depression among MSM living with HIV: biological, psychological, and social. The results are presented in Table 4.
Table 4. Determinants of depression according to the biopsychosocial approach.
| No | Author/year | Screening tool | Outcome definition of depression | Significant variables associated with depression | Statistical value | |
|---|---|---|---|---|---|---|
| 1. | Li et al. (2016) [27] | 20-item Center for Epidemiological Studies-Depression (CES-D) scale | 16/21/25 for mild, moderate, and severe depression | Psychological | Perceived stress | AOR: 1.17, 95% CI = 1.12, 1.22, P = 0.001 |
| Enacted stigma | AOR: 7.72, 95% CI = 2.27, 26.25, P<0.001 | |||||
| Gratitude | AOR: 0.90, 95% CI = 0.86, 0.94, P<0.001 | |||||
| 2. | Tao et al. (2017) [28] | Hospital Anxiety and Depression Scale (HADS) | A score of 0 to 7 was defined as normal, 8 to 10 as borderline depression, and a score of 11 to 21 as suspected depression. | Psychological | Internalized stigma | AOR: 1.09, 95%CI: 1.07, 1.12, P<0.001. |
| Vicarious stigma from the community/health care | AOR: 1.06, 95%CI: 1.03, 1.10, P<0.001 | |||||
| 3. | Wang et al. (2019) [29] | Hospital Anxiety and Depression Scale (HADS) | A score of 0 to 7 was defined as normal, 8 to 10 as borderline depression, and a score of 11 to 21 as suspected depression. | Psychological | Self-efficacy | AOR: 0.88, 95% CI: 0.85, 0.92, P<0.001 |
| 4. | Luo et al. (2020) [30] | Patient Health Questionnaires Depression Scale (PHQ-9) | A score of 10 the cut-off score for significant depressive symptoms | Biological | Received ART during the first year after diagnosis. | β = −2.14, P = 0.008 |
| Psychological | Participants who had access to mental health care after diagnosis were more likely to improve depression. | β = −3.51, P = 0.003 | ||||
| Increases in social stress scores were associated with increases in depression. | β = 0.43, P<0.001 | |||||
| Social | Increases in support were associated with decreases in PHQ-9 score. | β = −0.37, P<0.001 | ||||
| 5. | Rood et al. (2015) [31] | Center for Epidemiological Studies-Depression (CES-D) scale | A total score ranging from 0 to 60, and a clinical cut-off score of 23, instead of 16, was used to indicate probable depression. | Psychological | High Functional/High Dysfunctional coping strategies | β = 0.36, t = 4.47, P< 0.01 |
| Low Functional/High Dysfunctional coping strategies | β = 0.50, t = 6.34, P< 0.01 | |||||
| 6. | Irwin et al. (2018) [32] | Center for Epidemiological Studies-Depression (CES-D) scale | A score≥ 16 represents a higher risk of depression. | Biological | Older age | OR: 0·98, 95% CI: 0·96, 0·99, P<0.05 |
| Viral load > 10,000 copies/ml | OR: 1·38, 95%CI: 1·04, 1·85, P<0.05 | |||||
| Psychological | Sleep disturbance | OR: 1·52, 95%CI: 1·29, 1·80, P<0.001 | ||||
| Current smoker | OR: 1·61, 95% CI: 1·12, 2·33, P<0.05 | |||||
| Social | Black ethnicity | OR: 1·62, 95% CI: 1·17, 2·24, P<0.05 | ||||
| 7. | Heywood & Lyon. (2016) [33] | The short-form Depression Anxiety Stress Scales (DASS-21) | A higher score represents a greater indication of depression. | Psychological | Experiencing greater internalized stigma | β = 1.14, P<0.001 |
| Social | Unemployment | β = 5.41, P = 0.05 | ||||
| Born overseas | β = − 2.62, P = 0.05 | |||||
| 8. | Murphy et al. (2018) [34] | 14-item Hospital Anxiety and Depression Scale (HADS) | A score of 0 to 7 was defined as normal, 8 to 10 as borderline depression, and a score of 11 to 21 as suspected depression. | Psychological | HIV Health Optimism | β = − 0.15, 95% CI: -0.44, -0.06, P<0.05 |
| Enacted stigma | β = 0.15, 95% CI: 0.02, 0.28, P<0.05 | |||||
| Internalized stigma | β = 0.36, 95% CI: 0.26, 0.09, P<0.001 | |||||
Abbreviations: AOR: Adjusted odds ratio; OR: odds ratio, CI: confidence interval.
3.4.1 Biological
Two studies found a significant association between depression and biological factors [30, 32]. Within the first year of diagnosis, ART initiation was associated with reduced depressive symptoms (β = -2.14) compared to those not placed on ART [30]. The other predictor with increased odds of depression was high viral load >10,000 copies/ml (OR: 1.38); however, the evidence is not strong [32]. Meanwhile, older age was associated with reduced odds of depression (OR: 0.98) [32].
3.4.2 Psychological
Four studies reported a significant association between increased depression and stigma, either internalized HIV-related stigma [28, 33] or enacted HIV-related stigma [27, 34]. In our review, only enacted HIV-related stigma [27] is strongly associated with increased odds of depression (OR: 7.72), while the other three studies show weak evidence [13, 28, 32]. The other risk factors with increased odds of depression include sleep disturbance (OR: 1.52) and current smoker (OR:1.61) [32]. Meanwhile, weak evidence for increased depression has been found for engagement in high functional/high dysfunctional coping strategies and low functional/high dysfunctional coping strategies [31], perceived stress [27], and social stress [30]. With solid evidence, access to mental healthcare was associated with reduced depression (β = -3.51) [30]. The other factors associated with reduced depression were gratitude [27], self-efficacy [29)] and HIV health optimism [34].
3.4.3 Social
One study conducted in Australia found that unemployment was positively associated with increased depression (β = 5.41) [33]. In another study, being born overseas was associated with reduced depression with good evidence (β = -2.62), whereby black ethnicity was associated with increased odds of depression (OR: 1.62) [32]. Increases in social support were associated with decreased depressive symptoms, but the evidence is weak [30].
Regarding outcome measurement of depression, three studies [27, 31, 32] used the Center for Epidemiological Studies-Depression checklist (CES-D). Following the test objectives, the CES-D provides cut-off scores; for example, a score of 16 or higher can aid in identifying persons who are at risk for clinical depression, with good sensitivity and specificity, as well as a high level of internal consistency [35, 36]. Another three studies used the Hospital Anxiety and Depression Scale (HADS) [28, 29, 34]. HADS focuses on non-physical symptoms, so that it can be used to diagnose depression [37]. The remaining study used the Patient Health Questionnaire-9 (PHQ-9) [30] and the Depression Anxiety Stress Scale-21 (DASS-21) [33]. The PHQ-9 can be used for diagnostics as well as a depression severity score [38], while the DASS-21 satisfactorily predicts depression as diagnosed with the Mini International Neuropsychiatric Interview (MINI) [39].
4. Discussion
Our review found that the potential determinants in depression among MSM living with HIV varied across studies. However, the determinants of depression with good evidence are enacted HIV-related stigma, unemployment, sleep disturbance, current smoker, black ethnicity, born overseas, ART initiation, and access to mental health care. The other relevant determinants to be discussed are older age, internalized stigma, self-efficacy, and social support. Although the evidence may be weak or moderate for some, they are relevant to be considered and analyzed for theoretical or practical reasons.
4.1 Biological factors
4.1.1 Age
One study shows older age was a protective factor for depression (OR:0.98) [32]. The age factor should be highlighted due to the increased prevalence of young MSM living with HIV [40] and the association of depression among MSM with young age [41]. Depression was prevalent among adolescents and young adults with illnesses such as HIV, underscoring the importance of improved psychological examination and monitoring, particularly on young patients [42].
4.1.2 Antiretroviral therapy (ART)
Initiation of ART in the first year after HIV diagnosis was associated with reducing depressive symptoms in one study [30]. The finding is in line with other studies, whereby PLHIV placed on ART had reduced depression and higher quality of life (QOL) for physical, psychological, and environmental domains [43–45]. Accelerated commencement of ART has been shown to improve clinical results, and follows the WHO recommendation in supporting accelerated ART initiation, including same-day ART initiation [46]. During acute HIV infection, ART limits the viral reservoir, preserves immune function, and decreases systemic inflammation [47]. The introduction of ART has reduced morbidity, mortality and increased the quality of PLHIV [48]. Furthermore, Treatment as prevention (TasP) which uses ART among HIV-positive persons to decrease the chances of HIV transmission will benefit all serodiscordant couples [49]. With all the shreds of evidence of ART benefits, early initiation of ART could give MSM reassurance towards achieving a good quality of life that could reduce their risk of having depression or improve the state of depression.
4.2 Psychological factors
4.2.1 Enacted HIV-related stigma
Enacted HIV-related stigma refers to the experience of being discriminated, stigmatized, and treated in an unfriendly manner due to their HIV status, and it is often influenced by the perception of others’ attitudes towards PLHIV [27, 28]. Sixty-nine countries, nearly half of which are in Africa, have laws criminalizing homosexuality [50]. In addition, MSM could see themselves as doubly stigmatized due to their sexual identity and HIV status [51, 52]. Three studies in this review [27, 28, 34] show enacted HIV-related stigma as the determinant of depression among HIV MSM. The strongest evidence came from an adjusted odds ratio of 7.72, in which participants judged the degree of enacted HIV-related stigma based on personal experiences of discrimination, stigmatization, or unfriendly treatment because of their HIV diagnosis [27]. Previous systematic reviews and studies were consistent with the enacted HIV-related stigma associated with poor mental health and depression among PLHIV [53–55].
Previous studies show that MSM living with HIV face discriminatory treatment from the general public, MSM community, and the healthcare system [56–58]. Stigma and social pressure for MSM also come from their families who urge them to marry and have children to protect their family reputation and lineage [59]. In general, minority stress explains that stigma, prejudice, and discrimination create a hostile and stressful social environment that causes mental health problems [60]. Therefore, health care providers need to address stigma in their facilities and educate patients’ family members or their circle of confidentiality.
4.2.2 Internalized HIV-related stigma
Internalized HIV-related stigma refers to endorsing negative beliefs and feelings about oneself because of one’s HIV-positive status [28]. Although evidence is not strong, three studies mentioned it as a risk factor for increased depression [28, 33, 34]. Internalized HIV-related stigma was positively associated with depression, which, combined with enacted HIV-related stigma, increased the likelihood of suicide [61]. In another study, internalized HIV-related stigma partly mediated the relationship between enacted HIV-related stigma and depression symptoms [62]. When combined with enacted HIV-related stigma by health care practitioners, stigma can impede MSM utilization of health services; thus, stigma should be addressed at individual and institutional levels [63].
4.2.3 Self-efficacy
Self-efficacy is the belief in one’s ability to plan and carry out the actions necessary to manage potential scenarios [64]. Self-efficacy is a protective factor for depression in one study (OR:0.88) [29]. Lack of coping self-efficacy among HIV individuals may increase the likelihood of non-disclosure and depression [65]. In addition, self-efficacy for HIV disclosure decisions is the novel stressor for newly diagnosed individuals [66]. Therefore, interventions that enhance self-efficacy may help manage the demands of daily life with HIV, increase disclosure, and reduce depression [63].
4.2.4 Sleep disturbance
Sleep disturbance is associated with increased depression among MSM living with HIV [32]. The finding was consistent with the previous study among PLHIV, whereby those with more sleep problems were significantly more likely to have worse depression over time than those with fewer sleep problems [67]. Poor sleep quality was observed in 47% to 73% of PLHIV [68, 69]. Sleep disturbances can occur early in the course of HIV infection and suggest that the observed changes in sleep physiology could result from central nervous system involvement or immune defense mobilization in the early phases of HIV infection [70]. In addition, factors that influence sleep include psychosocial factors such as stigma and social isolation [66]. Therefore, it is imperative to identify and treat sleep disturbances in MSM living with HIV to improve mental health and quality-of-life outcomes.
4.2.5 Current smoker
One study found an association between current smokers and depression among MSM living with HIV [32]. The finding was observed in another study where HIV-infected smokers reported higher symptoms of depression than non-smokers [71]. In Canada, a study among the lesbian, bisexual, gay, transgender, and questioning (LBGTQ) population who smoke regularly showed that 62% suffer from depression symptoms, and 38% had a major depressive disorder [72]. On the other hand, they are more likely to smoke and use drugs to cope with stress, illness, social disadvantages, and sexual orientation concerns, all of which can be barriers to quitting smoking [72]. Apart from non-communicable diseases, PLHIV who smoke cigarettes are more likely to get an opportunistic infection like oral candidiasis, Pneumocystis pneumonia, and gastrointestinal infection [73, 74]. Smoking was linked to more than 60% of fatalities in PLHIV, whereby they lose more life-years due to smoking, with 12.3 years lost to smoking than 5.1 years lost to HIV [75]. All the physical impacts of smoking may indirectly contribute to depression among MSM. Therefore, health care providers must recognize smoking behavior among MSM and make smoking cessation a priority for them.
4.2.6. Access to mental health care
One study conducted in China shows that participants who had access to mental health services were more likely to experience reduced depression [30]. Among Chinese MSM, minority stress is a significant predictor of psychological distress. Nonetheless, mental health treatments and interventions concentrating on MSM are lacking in China [76]. Previous systematic reviews and meta-analyses demonstrate that PLHIV can benefit from various mental and behavioral health interventions [77, 78]. MSM are more likely than other men to have tried to commit suicide and have succeeded in suicide [79]. As MSM suffer double discrimination for being gay and living with HIV, it could prevent them from accessing mental health services. Therefore, early and routine screening is mandatory to provide them with early mental health support and treatment intervention.
4.3 Social factors
4.3.1 Social support
Social support is a significant factor for improvement in depression in one study in this review [30]. Social support has been linked to coping with life stressors such as HIV/AIDS and other chronic health issues [80]. Evidence suggests that improved social support may reduce depressive symptoms among MSM living with HIV [81]. Another study found that the negative association between social isolation and depression was stronger for sexual minority male youths than non-minority youths and sexual minority females [82]. MSM with more social support networks also perceived lower levels of stigma [27]. MSM are prone to inadequate social support and severe depression symptoms, emphasizing the importance of developing psychological interventions specifically for them [83].
4.3.2 Unemployment
Depression scores increased among MSM living with HIV in unemployed men [33], as supported by another study [84]. PLHIV may encounter challenges to employment and retention due to HIV-related stigma, disclosure and confidentiality difficulties at work, the impact of poor health on their capacity to work, and the requirement for medical leave and healthcare appointments [85]. Additionally, unemployed PLHIV are less likely to have a sufficient income, a meaningful life, a daily routine, social support, and a sufficient income and participation in intellectually engaging activities [86, 87]. Therefore, psychosocial treatment combined with early ART could serve MSM living with HIV mentally and physically fit in sustaining their job and avoiding unemployment.
4.3.3 Born overseas
Lower depression scores were found among migrants in one study conducted in Australia [33]. Many studies have observed a “healthy migrant effect” (HME) among PLHIV, for example, in North America, Denmark, Germany, Spain, and Norway [88]. Based on HME, migrants often have a better health status than the remaining population in the native country, compared with the majority in the host country, especially during the first five to ten years after immigration [88]. In contrast, stigma and lack of access to care appear to be the main factors influencing poor HIV outcomes among migrants in high-income countries [89]. With regards to mental health among migrants, the two widely accepted theories were the following: (1) Loneliness theory: to escape loneliness, migrants frequently reside with other migrants, particularly those from the same country of origin [90]; and (2) Acculturation theory: owing to their experiences with discrimination and rejection, migrants feel like they are not part of the community [91]. Therefore, improving migrants’ access to health and HIV care will require a human rights-based approach to the governance of the entire migration process [92].
4.3.4 Black ethnicity
Black ethnicity was the predictor of increased risk of depression in this review [32]. The finding is consistent with the previous studies that depression may affect this group more than the general adult population due to racism, homophobia, and other forms of discrimination; however, it has been less fully explored [93–96]. Likewise, racial disparities in ART initiation for black MSM have been reported in the UK and the USA [97]. Despite rising interest in understanding how social factors contribute to poor health outcomes, many academics and relevant bodies remain wary of naming racism a primary cause of racial health disparities [98]. In keeping with SDG 10, inequalities in health care of any kind based on race, ethnicity, origin, or religion should be addressed by diverse stakeholders’ commitment.
5. Limitations
Inconsistency and limited comparability of results may have been caused by the heterogeneity of outcome assessments using different tools to measure depression and different statistical analyses. Furthermore, our review involved studies from different countries. As a result, patient demographic factors also substantially affected the outcome. It also implies different cultural and legal contexts, with profound variations in accepting gay and bisexual (GB) identities and rights. This influences the levels of social stigma, which is one of the main factors identified in this systematic review. More importantly, some of these countries have laws protecting GB people’s rights, whereas others do not.
Most of the studies were cross-sectional. It has weaknesses like difficulty in making a causal inference. Associations identified might be challenging to interpret and cannot investigate the temporal relationship between outcomes and risk factors. We did not include non-English language articles, which may have introduced bias as most studies come from English-speaking countries, and there is little evidence from other regions.
6. Conclusion
The determinants of depression with the strongest evidence among MSM living with HIV were enacted HIV-related stigma, unemployment, sleep disturbance, current smoker, black ethnicity, born overseas, ART initiation, and access to mental health care. Although the evidence may be weak or moderate, other risk factors worth considering are older age, internalized HIV stigma, self-efficacy, and social support. Efforts to improve and prevent depression among MSM living with HIV could benefit from addressing these determinants based on the biopsychosocial approach as soon as possible after HIV diagnosis. Engagement and retention in care will improve medical outcomes, in line with Ending AIDS 2030 and the SDGs that aim to leave no one behind.
7. Recommendations
Integrating mental health screening and care into HIV treatment settings would strengthen HIV prevention and care outcomes and improve access to mental healthcare. Actions to fight HIV-related stigma, in general, should be prioritized, as it is one of the key determinants of depression among MSM. A structured program on eliminating HIV-related stigma should be planned at multiple levels, including the interpersonal, institutional, community, and judicial levels. Legislations protecting the rights of GB citizens should be enacted immediately; as of present, they are struggling for their civil rights in a forum, in courtrooms, and on the streets. Healthcare services should be designed to acknowledge, affirm, and validate diverse sexual identities. A solid and sustainable support system could prevent depression or aid in managing depression. The other determinants of depression, such as age, unemployment, self-efficacy, sleep disturbance, and smoking behavior, need to be addressed when providing care for MSM. Elimination of disparities for black MSM and migrants needs to address structural barriers or differences in HIV clinical care access and outcomes. More importantly, ART should be provided as soon as possible, aligning with the SDGs to treat all irrespective of immune status. Additional research is needed to better understand depression and minority stress theory among MSM living with HIV and how interventions could be tailored to meet specific needs.
Supporting information
(DOCX)
Data Availability
All relevant data are within the paper.
Funding Statement
We received funding from our institution, which is Universiti Putra Malaysia (UPM). The funders had no role in study design, data collection, and analysis, decision to publish, or manuscript preparation. Authors received no salary from the funders.
References
- 1.WHO. Depression [Internet]. 2021 [cited 2021 Apr 25]. Available from: https://www.who.int/health-topics/depression#tab=tab_1
- 2.(UK) NCC for MH. The classification of depression and depression rating scales/questionnaires. 2010 [cited 2021 Jul 23]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK82926/
- 3.Xiao L, Qi H, Wang Y yuan, Wang D, Wilkinson M, Hall BJ, et al. The prevalence of depression in men who have sex with men (MSM) living with HIV: A meta-analysis of comparative and epidemiological studies. Gen Hosp Psychiatry [Internet]. 2020. Sep 1 [cited 2020 Dec 17];66:112–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0163834320300463 doi: 10.1016/j.genhosppsych.2020.04.001 [DOI] [PubMed] [Google Scholar]
- 4.Fu H, Feng T, Wang T, Wu X, Cai Y, Yang T. Reported prevalence of depression or depressive symptoms among men who have sex with men in China, 2004–2018: A systematic review and meta-analysis [Internet]. Vol. 277, Journal of Affective Disorders. Elsevier B.V.; 2020 [cited 2021 Apr 16]. p. 192–203. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0165032720326070 doi: 10.1016/j.jad.2020.08.011 [DOI] [PubMed] [Google Scholar]
- 5.Levintow SN, Pence BW, Ha TV, Le Minh N, Sripaipan T, Latkin CA, et al. Prevalence and predictors of depressive symptoms among HIV-positive men who inject drugs in Vietnam. Moitra E, editor. PLoS One [Internet]. 2018. Jan 1 [cited 2021 Apr 7];13(1):e0191548. Available from: doi: 10.1371/journal.pone.0191548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Safren SA, Blashill AJ, Conall O’cleirigh M. Promoting the Sexual Health of MSM in the Context of Comorbid Mental Health Problems. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pachankis JE. A Transdiagnostic Minority Stress Treatment Approach for Gay and Bisexual Men’s Syndemic Health Conditions. Arch Sex Behav [Internet]. 2015. Oct 7 [cited 2021 Apr 1];44(7):1843–60. Available from: http://link.springer.com/10.1007/s10508-015-0480-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tripathi A, Das A, Kar SK. Biopsychosocial Model in Contemporary Psychiatry: Current Validity and Future Prospects. Indian J Psychol Med [Internet]. 2019. [cited 2021 Apr 25];41(6):582. Available from: /pmc/articles/PMC6875848/ doi: 10.4103/IJPSYM.IJPSYM_314_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engel GL. THE BIOPSYCHOSOCIAL MODEL AND THE EDUCATION OF HEALTH PROFESSIONALS†. Ann N Y Acad Sci [Internet]. 1978. Jun [cited 2021 Feb 9];310(1):169–81. Available from: http://doi.wiley.com/10.1111/j.1749-6632.1978.tb22070.x [DOI] [PubMed] [Google Scholar]
- 10.Ahaneku H, Ross MW, Nyoni JE, Selwyn B, Troisi C, Mbwambo J, et al. Depression and HIV risk among men who have sex with men in Tanzania. Vol. 28, AIDS Care—Psychological and Socio-Medical Aspects of AIDS/HIV. 2016. p. 140–7. doi: 10.1080/09540121.2016.1146207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulqueeny DM, Nkabini SM, Pokiya MH. Mapping evidence of depression in HIV-seropositive MSM in sub-Saharan Africa: a scoping review protocol. Syst Rev [Internet]. 2021. Dec 1 [cited 2021 Apr 6];10(1):50. Available from: https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01604-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hibbert MP, Brett CE, Porcellato LA, Hope VD. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect [Internet]. 2019. Aug 1 [cited 2021 Jan 19];95(5):342–50. Available from: https://sti.bmj.com/lookup/doi/10.1136/sextrans-2018-053933 [DOI] [PubMed] [Google Scholar]
- 13.Lyons A, Heywood W, Rozbroj T. Psychosocial factors associated with flourishing among Australian HIV-positive gay men. BMC Psychol [Internet]. 2016. Sep 15 [cited 2021 May 2];4(1):46. Available from: http://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-016-0154-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang W, Yang Y, Li S. Association between perceived HIV stigma, social support, resilience, self-esteem, and depressive symptoms among HIV-positive men who have sex with men (MSM) in Nanjing, China. 2019. [cited 2021 Feb 17]; Available from: 10.1080/09540121.2019.1601677 [DOI] [PubMed] [Google Scholar]
- 15.Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: Results from the steps study. AIDS Behav. 2011;15(6):1161–70. doi: 10.1007/s10461-010-9778-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Javanbakht M, Shoptaw S, Ragsdale A, Brookmeyer R, Bolan R, Gorbach PM. Depressive symptoms and substance use: Changes overtime among a cohort of HIV-positive and HIV-negative MSM. Drug Alcohol Depend [Internet]. 2020. Feb 1 [cited 2021 Apr 6];207:107770. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0376871619305472 doi: 10.1016/j.drugalcdep.2019.107770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan BT, Pradeep A, Prasad L, Murugesan V, Chandrasekaran E, Kumarasamy N, et al. Association between internalized stigma and depression among HIV-positive persons entering into care in Southern India. J Glob Health. 2017;7(2). doi: 10.7189/jogh.07.020403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schotte CKW, Van Den Bossche B, De Doncker D, Claes S, Cosyns P. A biopsychosocial model as a guide for psychoeducation and treatment of depression. Vol. 23, Depression and Anxiety. 2006. p. 312–24. doi: 10.1002/da.20177 [DOI] [PubMed] [Google Scholar]
- 19.Tran BX, Ho RCM, Ho CSH, Latkin CA, Phan HT, Ha GH, et al. Depression among patients with HIV/AIDS: Research development and effective interventions (gapresearch). Int J Environ Res Public Health [Internet]. 2019. May 2 [cited 2020 Dec 16];16(10):1772. Available from: https://www.mdpi.com/1660-4601/16/10/1772 doi: 10.3390/ijerph16101772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Willie TC, Overstreet NM, Peasant C, Kershaw T, Sikkema KJ, Hansen NB. Anxiety and Depressive Symptoms Among People Living with HIV and Childhood Sexual Abuse: The Role of Shame and Posttraumatic Growth. AIDS Behav. 2016;20(8):1609–20. doi: 10.1007/s10461-016-1298-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tao J, Vermund SH, Lu H, Ruan Y, Shepherd BE, Kipp AM, et al. Impact of Depression and Anxiety on Initiation of Antiretroviral Therapy among Men Who Have Sex with Men with Newly Diagnosed HIV Infections in China. AIDS Patient Care STDS. 2017;31(2):96–104. doi: 10.1089/apc.2016.0214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ironson G, O’Cleirigh C, Fletcher MA, Laurenceau JP, Balbin E, Klimas N, et al. Psychosocial Factors Predict CD4 and Viral Load Change in Men and Women With Human Immunodeficiency Virus in the Era of Highly Active Antiretroviral Treatment. Psychosom Med [Internet]. 2005. Nov [cited 2021 Apr 25];67(6):1013–21. Available from: http://journals.lww.com/00006842-200511000-00024 doi: 10.1097/01.psy.0000188569.58998.c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.UNAIDS. The AIDS response in the 2030 agenda for sustainable development: joint work, shared gains | UNAIDS [Internet]. [cited 2020 Nov 14]. Available from: https://www.unaids.org/en/AIDS_SDGs
- 24.WHO/Europe | Fact sheets on the Sustainable Development Goals (SDGs): health targets [Internet]. [cited 2021 Dec 6]. Available from: https://www.euro.who.int/en/health-topics/health-policy/sustainable-development-goals/publications/2017/fact-sheets-on-the-sustainable-development-goals-sdgs-health-targets
- 25.Bekker LG, Alleyne G, Baral S, Cepeda J, Daskalakis D, Dowdy D, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society—Lancet Commission. Vol. 392, The Lancet. Lancet Publishing Group; 2018. p. 312–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.critical-appraisal-tools—Critical Appraisal Tools | Joanna Briggs Institute [Internet]. [cited 2021 Jun 3]. Available from: https://jbi.global/critical-appraisal-tools
- 27.Li J, Mo PKH, Kahler CW, Lau JTF, Du M, Dai Y, et al. Prevalence and associated factors of depressive and anxiety symptoms among HIV-infected men who have sex with men in China. AIDS Care—Psychol Socio-Medical Asp AIDS/HIV. 2016;28(4):465–70. doi: 10.1080/09540121.2015.1118430 [DOI] [PubMed] [Google Scholar]
- 28.Tao J, Wang L, Kipp AM, Qian HZ, Yin L, Ruan Y, et al. Relationship of Stigma and Depression Among Newly HIV-Diagnosed Chinese Men Who Have Sex with Men. AIDS Behav. 2017;21(1):292–9. doi: 10.1007/s10461-016-1477-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang N, Wang S, Qian HZ, Ruan Y, Amico KR, Vermund SH, et al. Negative associations between general self-efficacy and anxiety/depression among newly HIV-diagnosed men who have sex with men in Beijing, China. AIDS Care—Psychol Socio-Medical Asp AIDS/HIV. 2019;31(5):629–35. doi: 10.1080/09540121.2018.1549721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luo R, Silenzio VMB, Huang Y, Chen X, Luo D. The Disparities in Mental Health Between Gay and Bisexual Men Following Positive HIV Diagnosis in China: A One-Year Follow-Up Study. Int J Environ Res Public Health [Internet]. 2020. May 2 [cited 2021 Jul 24];17(10). Available from: /pmc/articles/PMC7277388/ doi: 10.3390/ijerph17103414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rood BA, McConnell EA, Pantalone DW. Distinct Coping Combinations are Associated with Depression and Support Service Utilization in Men who have Sex with Men Living with HIV. Psychol Sex Orientat Gend Divers [Internet]. 2015. [cited 2021 Jul 22];2(1):96. Available from: /pmc/articles/PMC4450098/ doi: 10.1037/sgd0000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Irwin MR, Archer G, Olmstead R, Brown TT, Teplin LA, Patel SR, et al. Increased risk of depression in non-depressed HIV infected men with sleep disturbance: Prospective findings from the Multicenter AIDS Cohort Study. EBioMedicine [Internet]. 2018;36:454–60. Available from: doi: 10.1016/j.ebiom.2018.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heywood W, Lyons A. HIV and Elevated Mental Health Problems: Diagnostic, Treatment, and Risk Patterns for Symptoms of Depression, Anxiety, and Stress in a National Community-Based Cohort of Gay Men Living with HIV. AIDS Behav. 2016;20(8):1632–45. doi: 10.1007/s10461-016-1324-y [DOI] [PubMed] [Google Scholar]
- 34.Murphy PJ, Garrido-Hernansaiz H, Mulcahy F, Hevey D. HIV-related stigma and optimism as predictors of anxiety and depression among HIV-positive men who have sex with men in the United Kingdom and Ireland. AIDS Care—Psychol Socio-Medical Asp AIDS/HIV [Internet]. 2018;30(9):1173–9. Available from: doi: 10.1080/09540121.2018.1445827 [DOI] [PubMed] [Google Scholar]
- 35.Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLoS One [Internet]. 2016. May 1 [cited 2021 Dec 6];11(5):e0155431. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0155431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging [Internet]. 1997. [cited 2021 Dec 6];12(2):277–87. Available from: https://pubmed.ncbi.nlm.nih.gov/9189988/ doi: 10.1037//0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- 37.Stern AF. The hospital anxiety and depression scale. Occup Med (Lond) [Internet]. 2014. [cited 2021 Dec 6];64(5):393–4. Available from: https://pubmed.ncbi.nlm.nih.gov/25005549/ doi: 10.1093/occmed/kqu024 [DOI] [PubMed] [Google Scholar]
- 38.PHQ and GAD-7 Instructions INSTRUCTION MANUAL Instructions for Patient Health Questionnaire (PHQ) and GAD-7 Measures.
- 39.Beaufort IN, De Weert-Van Oene GH, Buwalda VAJ, De Leeuw JRJ, Goudriaan AE. The Depression, Anxiety and Stress Scale (DASS-21) as a Screener for Depression in Substance Use Disorder Inpatients: A Pilot Study. Eur Addict Res [Internet]. 2017. Dec 1 [cited 2021 Dec 6];23(5):260–8. Available from: https://pubmed.ncbi.nlm.nih.gov/29224000/ doi: 10.1159/000485182 [DOI] [PubMed] [Google Scholar]
- 40.Mitsch A, Singh S, Li J, Balaji A, Linley L, Selik R. Age-Associated Trends in Diagnosis and Prevalence of Infection with HIV Among Men Who Have Sex with Men—United States, 2008–2016. MMWR Morb Mortal Wkly Rep [Internet]. 2019. Sep 21 [cited 2021 Nov 30];67(37):1025–31. Available from: https://www.cdc.gov/mmwr/volumes/67/wr/mm6737a2.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu Y, Zhong XN, Peng B, Zhang Y, Liang H, Dai JH, et al. Comparison of depression and anxiety between HIV-negative men who have sex with men and women (MSMW) and men who have sex with men only (MSMO): a cross-sectional study in Western China. BMJ Open [Internet]. 2019. Jan 1 [cited 2021 Nov 28];9(1):e023498. Available from: https://bmjopen.bmj.com/content/9/1/e023498 doi: 10.1136/bmjopen-2018-023498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barker MM, Beresford B, Bland M, Fraser LK. Prevalence and Incidence of Anxiety and Depression Among Children, Adolescents, and Young Adults With Life-Limiting Conditions: A Systematic Review and Meta-analysis. JAMA Pediatr [Internet]. 2019. Sep 1 [cited 2021 Dec 2];173(9):835–44. Available from: https://jamanetwork.com/journals/jamapediatrics/fullarticle/2737640 doi: 10.1001/jamapediatrics.2019.1712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.GJ W, B G-D, J G, C K, P M. Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosom Med [Internet]. 2012. [cited 2021 Jul 19];74(9):883–90. Available from: https://pubmed.ncbi.nlm.nih.gov/22923701/ doi: 10.1097/PSY.0b013e31826629db [DOI] [PubMed] [Google Scholar]
- 44.Martins C, Coelho FMDC, Pinheiro RT, Motta JVDS, De Souza LDM, Pinheiro CAT, et al. People living with HIV/AIDS: body image and its important associations with mental health and BMI. Psychol Heal Med. 2020. Sep 13;25(8):1020–8. doi: 10.1080/13548506.2019.1691244 [DOI] [PubMed] [Google Scholar]
- 45.Judd FK, Cockram AM, Komiti A, Mijch AM, Hoy J, Bell R. Depressive Symptoms Reduced in Individuals with HIV/AIDS Treated with Highly Active Antiretroviral Therapy: A Longitudinal Study: http://dx.doi.org/101080/000486700278 [Internet]. 2016. Dec 21 [cited 2021 Jul 14];34(6):1015–21. Available from: https://journals.sagepub.com/doi/abs/10.1080/000486700278 [DOI] [PubMed] [Google Scholar]
- 46.Ford N, Migone C, Calmy A, Kerschberger B, Kanters S, Nsanzimana S, et al. Benefits and risks of rapid initiation of antiretroviral therapy. AIDS [Internet]. 2018. Jan 2 [cited 2020 Nov 5];32(1):17–23. Available from: http://journals.lww.com/00002030-201801020-00003 doi: 10.1097/QAD.0000000000001671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clercq J De, Rutsaert S, Scheerder M-A De, Verhofstede C, Callens S, Vandekerckhove L. Benefits of antiretroviral therapy initiation during acute HIV infection. https://doi.org/101080/1784328620201770413 [Internet]. 2020. May 29 [cited 2021 Jul 14];1–9. Available from: https://www.tandfonline.com/doi/abs/10.1080/17843286.2020.1770413 doi: 10.1080/17843286.2020.1770413 [DOI] [PubMed] [Google Scholar]
- 48.Betancur MN, Lins L, Oliveira IR de, Brites C. Quality of life, anxiety and depression in patients with HIV/AIDS who present poor adherence to antiretroviral therapy: a cross-sectional study in Salvador, Brazil. Brazilian J Infect Dis [Internet]. 2017. Sep 1 [cited 2021 Jul 22];21(5):507–14. Available from: http://www.scielo.br/j/bjid/a/X9F5DjghxK7GTzK3tWrJqtM/?lang=en doi: 10.1016/j.bjid.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yombi JC, Mertes H. Treatment as Prevention for HIV Infection: Current Data, Challenges, and Global Perspectives. AIDS Rev [Internet]. 2018. Jul 1 [cited 2021 Dec 6];20(3):131–40. Available from: https://pubmed.ncbi.nlm.nih.gov/30264827/ doi: 10.24875/AIDSRev.M18000024 [DOI] [PubMed] [Google Scholar]
- 50.Homosexuality: The countries where it is illegal to be gay—BBC News [Internet]. [cited 2021 Jul 22]. Available from: https://www.bbc.com/news/world-43822234
- 51.Garcia R, Ramos DG. P4.012 The Impact of Stigma and Discrimination in MSM HIV-Positive. Sex Transm Infect [Internet]. 2013. Jul 1 [cited 2021 Jul 1];89(Suppl 1):A292.3–A292. Available from: https://sti.bmj.com/content/89/Suppl_1/A292.3 [Google Scholar]
- 52.Wang N, Huang B, Ruan Y, Amico KR, Vermund SH, Zheng S, et al. Association between stigma towards HIV and MSM and intimate partner violence among newly HIV-diagnosed Chinese men who have sex with men. BMC Public Health [Internet]. 2020. Feb 10 [cited 2021 Jun 29];20(1):1–8. Available from: doi: 10.1186/s12889-019-7969-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. https://doi.org/101080/09540120802511877 [Internet]. 2009. Jun [cited 2021 Jul 31];21(6):742–53. Available from: https://www.tandfonline.com/doi/abs/10.1080/09540120802511877 [DOI] [PubMed] [Google Scholar]
- 54.Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016. Jul 13;6(7):e011453. doi: 10.1136/bmjopen-2016-011453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zeng C, Li L, Hong YA, Zhang H, Babbitt AW, Liu C, et al. A structural equation model of perceived and internalized stigma, depression, and suicidal status among people living with HIV/AIDS. BMC Public Health [Internet]. 2018. Jan 15 [cited 2021 Jul 1];18(1):1–11. Available from: https://link.springer.com/articles/10.1186/s12889-018-5053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Courtenay-Quirk C, Wolitski RJ, Parsons JT, Gómez CA. Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Educ Prev [Internet]. 2006. Feb [cited 2021 Jul 1];18(1):56–67. Available from: https://pubmed.ncbi.nlm.nih.gov/16539576/ doi: 10.1521/aeap.2006.18.1.56 [DOI] [PubMed] [Google Scholar]
- 57.Dowshen N, Binns HJ, Garofalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS [Internet]. 2009. May 1 [cited 2021 Jul 1];23(5):371–6. Available from: /pmc/articles/PMC2856436/ doi: 10.1089/apc.2008.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Philbin MM, Hirsch JS, Wilson PA, Ly AT, Giang LM, Parker RG. Structural barriers to HIV prevention among men who have sex with men (MSM) in Vietnam: Diversity, stigma, and healthcare access. PLoS One [Internet]. 2018. Apr 1 [cited 2021 Jul 1];13(4):e0195000. Available from: doi: 10.1371/journal.pone.0195000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fu H, Feng T, Wang T, Wu X, Cai Y, Yang T. Reported prevalence of depression or depressive symptoms among men who have sex with men in China, 2004–2018: A systematic review and meta-analysis. J Affect Disord. 2020. Dec 1;277:192–203. doi: 10.1016/j.jad.2020.08.011 [DOI] [PubMed] [Google Scholar]
- 60.Meyer IH. Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol Bull [Internet]. 2003. Sep [cited 2021 Jul 20];129(5):674. Available from: /pmc/articles/PMC2072932/ doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zeng C, Li L, Hong YA, Zhang H, Babbitt AW, Liu C, et al. A structural equation model of perceived and internalized stigma, depression, and suicidal status among people living with HIV/AIDS. BMC Public Health [Internet]. 2018. Jan 15 [cited 2021 Dec 8];18(1):1–11. Available from: https://link.springer.com/articles/10.1186/s12889-018-5053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li X, Yan H, Wang W, Yang H, Li S. Association between enacted stigma, internalized stigma, resilience, and depressive symptoms among young men who have sex with men in China: a moderated mediation model analysis. Ann Epidemiol. 2021. Apr 1;56:1–8. doi: 10.1016/j.annepidem.2021.01.001 [DOI] [PubMed] [Google Scholar]
- 63.ICRW | PASSION. PROOF. POWER. [Internet]. [cited 2021 Dec 8]. Available from: https://www.icrw.org/publications/a-global-hiv-stigma-reduction-framework-adapted-and-implemented-in-five-settings-in-india/
- 64.Self-Efficacy Theory | Simply Psychology [Internet]. [cited 2021 Dec 6]. Available from: https://www.simplypsychology.org/self-efficacy.html
- 65.Rodkjaer L, Chesney MA, Lomborg K, Ostergaard L, Laursen T, Sodemann M. HIV-infected individuals with high coping self-efficacy are less likely to report depressive symptoms: a cross-sectional study from Denmark. Int J Infect Dis [Internet]. 2014. [cited 2021 Dec 5];22:67–72. Available from: https://pubmed.ncbi.nlm.nih.gov/24657129/ doi: 10.1016/j.ijid.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 66.Cherenack EM, Sikkema KJ, Watt MH, Hansen NB, Wilson PA. Avoidant Coping Mediates the Relationship between Self-Efficacy for HIV Disclosure and Depression Symptoms among Men who have Sex with Men Newly Diagnosed with HIV. AIDS Behav [Internet]. 2018. Oct 1 [cited 2021 Dec 5];22(10):3130. Available from: /pmc/articles/PMC6060017/ doi: 10.1007/s10461-018-2036-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rogers BG, Lee JS, Bainter SA, Bedoya CA, Pinkston M, Safren SA. A multilevel examination of sleep, depression, and quality of life in people living with HIV/AIDS. J Health Psychol. 2020. Sep 1;25(10–11):1556–66. doi: 10.1177/1359105318765632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fekete EM, Williams SL, Skinta MD. Internalised HIV-stigma, loneliness, depressive symptoms and sleep quality in people living with HIV. https://doi.org/101080/0887044620171357816 [Internet]. 2017. Mar 4 [cited 2021 Jul 22];33(3):398–415. Available from: https://www.tandfonline.com/doi/abs/10.1080/08870446.2017.1357816 [DOI] [PubMed] [Google Scholar]
- 69.Rubinstein ML, Selwyn PA. High prevalence of insomnia in an outpatient population with HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol [Internet]. 1998. Nov 1 [cited 2021 Dec 13];19(3):260–5. Available from: https://pubmed.ncbi.nlm.nih.gov/9803968/ doi: 10.1097/00042560-199811010-00008 [DOI] [PubMed] [Google Scholar]
- 70.Norman SE, Chediak AD, Kiel M, Cohn MA. Sleep disturbances in HIV-infected homosexual men. AIDS [Internet]. 1990. [cited 2021 Dec 13];4(8):775–81. Available from: https://pubmed.ncbi.nlm.nih.gov/2261133/ doi: 10.1097/00002030-199008000-00009 [DOI] [PubMed] [Google Scholar]
- 71.Webb MS, Vanable PA, Carey MP, Blair DC. Cigarette Smoking among HIV+ Men and Women: Examining Health, Substance Use, and Psychosocial Correlates across the Smoking Spectrum. J Behav Med 2007. 305 [Internet]. 2007 Jun 15 [cited 2021 Jul 22];30(5):371–83. Available from: https://link.springer.com/article/10.1007/s10865-007-9112-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ma JE, Dworkind M. Tobacco Use and the LBGTQI2 and HIV/AIDS communities in Canada. [Google Scholar]
- 73.Smoking and HIV | Overviews of Diseases/Conditions | Tips From Former Smokers | CDC [Internet]. [cited 2021 Jul 22]. Available from: https://www.cdc.gov/tobacco/campaign/tips/diseases/smoking-and-hiv.html
- 74.Ompad DC, Kingdon M, Kupprat S, Halkitis SN, Storholm ED, Halkitis PN. Smoking and HIV-related Health Issues among Older HIV-positive Gay, Bisexual, and Other Men Who Have Sex with Men. http://dx.doi.org/101080/089642892014889067 [Internet]. 2014. Jul 3 [cited 2021 Jul 22];40(3):99–107. Available from: https://www.tandfonline.com/doi/abs/10.1080/08964289.2014.889067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Helleberg M, May MT, Ingle SM, Dabis F, Reiss P, Fätkenheuer G, et al. Smoking and life expectancy among HIV-infected individuals on antiretroviral therapy in Europe and North America. AIDS [Internet]. 2015. Jan 14 [cited 2021 Dec 13];29(2):221–9. Available from: https://pubmed.ncbi.nlm.nih.gov/25426809/ doi: 10.1097/QAD.0000000000000540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sun S, Pachankis JE, Li X, Operario D. Addressing Minority Stress and Mental Health among Men Who Have Sex with Men (MSM) in China. Curr HIV/AIDS Reports 2020. 171 [Internet]. 2020 Jan 16 [cited 2021 Jul 24];17(1):35–62. Available from: https://link.springer.com/article/10.1007/s11904-019-00479-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.van Luenen S, Garnefski N, Spinhoven P, Spaan P, Dusseldorp E, Kraaij V. The Benefits of Psychosocial Interventions for Mental Health in People Living with HIV: A Systematic Review and Meta-analysis. AIDS Behav [Internet]. 2018. Jan 1 [cited 2021 Dec 13];22(1):9–42. Available from: https://pubmed.ncbi.nlm.nih.gov/28361453/ doi: 10.1007/s10461-017-1757-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sherr L, Clucas C, Harding R, Sibley E, Catalan J. HIV and depression—a systematic review of interventions. Psychol Health Med [Internet]. 2011. Oct [cited 2021 Dec 13];16(5):493–527. Available from: https://pubmed.ncbi.nlm.nih.gov/21809936/ doi: 10.1080/13548506.2011.579990 [DOI] [PubMed] [Google Scholar]
- 79.Mental Health for Gay and Bisexual Men | CDC [Internet]. [cited 2021 Jul 22]. Available from: https://www.cdc.gov/msmhealth/mental-health.htm
- 80.Okonkwo NO, Larkan F, Galligan M. An assessment of the levels of perceived social support among older adults living with HIV and AIDS in Dublin. Springerplus [Internet]. 2016. Dec 1 [cited 2020 Nov 23];5(1). Available from: /pmc/articles/PMC4909667/?report = abstract doi: 10.1186/s40064-016-2302-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yan H, Li X, Li J, Wang W, Yang Y, Yao X, et al. Association between perceived HIV stigma, social support, resilience, self-esteem, and depressive symptoms among HIV-positive men who have sex with men (MSM) in Nanjing, China. https://doi.org/101080/0954012120191601677 [Internet]. 2019. Sep 2 [cited 2021 Dec 7];31(9):1069–76. Available from: https://www.tandfonline.com/doi/abs/10.1080/09540121.2019.1601677 [DOI] [PubMed] [Google Scholar]
- 82.Hatzenbuehler ML, McLaughlin KA, Xuan Z. Social Networks and Risk for Depressive Symptoms in a National Sample of Sexual Minority Youth. Soc Sci Med [Internet]. 2012. Oct [cited 2021 Dec 7];75(7):1184. Available from: /pmc/articles/PMC3407288/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yan H, Wong FY, Zheng T, Ning Z, Ding Y, Nehl EJ, et al. Social support and depressive symptoms among ‘money’ boys and general men who have sex with men in Shanghai, China. Sex Health [Internet]. 2014. Jun 12 [cited 2021 Dec 8];11(3):285–7. Available from: https://www.publish.csiro.au/sh/SH14017 doi: 10.1071/SH14017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zeng C, Guo Y, Hong YA, Gentz S, Zhang J, Zhang H, et al. Differential effects of unemployment on depression in people living with HIV/AIDS: a quantile regression approach. AIDS Care—Psychol Socio-Medical Asp AIDS/HIV. 2019. Nov 2;31(11):1412–9. doi: 10.1080/09540121.2019.1587366 [DOI] [PubMed] [Google Scholar]
- 85.Grierson J, Pitts M, Koelmeyer R. HIV Futures Seven The Health and Wellbeing of HIV Positive People in Australia. 2013. [cited 2021 Dec 7]; Available from: www.ashm.org.au [Google Scholar]
- 86.Vance D, Larsen KI, Eagerton G, Wright MA. Comorbidities and cognitive functioning: implications for nursing research and practice. J Neurosci Nurs [Internet]. 2011. Aug [cited 2021 Dec 5];43(4):215–24. Available from: https://pubmed.ncbi.nlm.nih.gov/21796044/ doi: 10.1097/JNN.0b013e3182212a04 [DOI] [PubMed] [Google Scholar]
- 87.Vance DE, Cody SL, Yoo-Jeong M, Jones GLD, Nicholson WC. The Role of Employment on Neurocognitive Reserve in Adults With HIV: A Review of the Literature. J Assoc Nurses AIDS Care [Internet]. 2015. Jul 1 [cited 2021 Dec 5];26(4):316–29. Available from: https://pubmed.ncbi.nlm.nih.gov/26066688/ doi: 10.1016/j.jana.2015.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Helgesson M, Johansson B, Nordquist T, Vingård E, Svartengren M. Healthy migrant effect in the Swedish context: A register-based, longitudinal cohort study. BMJ Open [Internet]. 2019. Mar 1 [cited 2021 Jun 30];9(3):26972. Available from: http://bmjopen.bmj.com/ doi: 10.1136/bmjopen-2018-026972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ross J, Cunningham CO, Hanna DB. HIV outcomes among migrants from low-income and middle-income countries living in high-income countries: a review of recent evidence. Curr Opin Infect Dis [Internet]. 2018. Feb 1 [cited 2021 Dec 7];31(1):25–32. Available from: https://pubmed.ncbi.nlm.nih.gov/29095720/ doi: 10.1097/QCO.0000000000000415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ponizovsky AM, Ritsner MS. Patterns of loneliness in an immigrant population. Compr Psychiatry [Internet]. 2004. Sep [cited 2021 Dec 7];45(5):408–14. Available from: https://www.researchgate.net/publication/8380550_Patterns_of_loneliness_in_an_immigrant_population doi: 10.1016/j.comppsych.2004.03.011 [DOI] [PubMed] [Google Scholar]
- 91.Berry JW. Immigration, Acculturation, and Adaptation. Appl Psychol [Internet]. 1997. Jan 1 [cited 2021 Dec 7];46(1):5–34. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1464-0597.1997.tb01087.x [Google Scholar]
- 92.Promoting a Rights-basedApproach to Migration, Health,and HIV and AIDS:A Framework for Action. [cited 2021 Dec 8]; Available from: http://www.ilo.org/global/topics/hiv-aids/WCMS_605763/lang—en/index.htm
- 93.Alvy LM, McKirnan DJ, Mansergh G, Koblin B, Colfax GN, Flores SA, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15(6):1171–9. doi: 10.1007/s10461-010-9678-z [DOI] [PubMed] [Google Scholar]
- 94.Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav [Internet]. 2014. Jan [cited 2021 Dec 13];18(1):10–25. Available from: https://pubmed.ncbi.nlm.nih.gov/23620241/ doi: 10.1007/s10461-013-0476-2 [DOI] [PubMed] [Google Scholar]
- 95.Friedman MR, Bukowski L, Eaton LA, Matthews DD, Dyer T V., Siconolfi D, et al. Psychosocial Health Disparities Among Black Bisexual Men in the U.S.: Effects of Sexuality Nondisclosure and Gay Community Support. Arch Sex Behav [Internet]. 2018. Jan 1 [cited 2021 Dec 13];48(1):213–24. Available from: https://www.rand.org/pubs/external_publications/EP67605.html doi: 10.1007/s10508-018-1162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLoS One [Internet]. 2017. Jun 1 [cited 2021 Jul 23];12(6):e0179688. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0179688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries IV WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet (London, England) [Internet]. 2012. [cited 2021 Dec 13];380(9839):341–8. Available from: https://pubmed.ncbi.nlm.nih.gov/22819656/ [DOI] [PubMed] [Google Scholar]
- 98.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet (London, England) [Internet]. 2017. Apr 8 [cited 2021 Dec 13];389(10077):1453–63. Available from: https://pubmed.ncbi.nlm.nih.gov/28402827/ doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]