ABSTRACT
Vaccination has had tremendous impact on human health. The tendency to hesitate or delay vaccination has been increasing, which has contributed to outbreaks of vaccine-preventable diseases. This cross-sectional study aimed to investigate the prevalence of childhood vaccine hesitancy and social media misconceptions in vaccine refusal among randomly selected parents from October 2019 through March 2020 in the outpatient clinics of King Khalid University Hospital, Riyadh, Saudi Arabia. The data were collected using a three-part questionnaire: the socio-demographic and economic questions, the Parents’ Attitudes about Childhood Vaccines (PACV) survey, and questions concerning social media use. Based on the PACV survey tool, 37 parents (11%) scored a value > 50 and were suggested as hesitant (8% hesitant and 3% very hesitant). Overall, 288 parents (89%) scored < 50, hence deemed to not be hesitant about childhood vaccination. There was no significant association between high educational level or social media exposure with vaccine hesitancy. The most commonly used social media platform was Twitter (40%). In conclusion, we report a low prevalence of vaccine hesitancy about childhood vaccination among parents, with no significant impact of education level or social media on vaccine hesitancy. Further studies are required to replicate these findings in other regions and cities to generalize these observations for Saudi Arabia.
KEYWORDS: Vaccine Hesitancy, Social Media, Childhood Vaccination, PACV, Saudi Arabia
Introduction
The history of vaccination goes back to the ancient Chinese, who practiced vaccination against smallpox by blowing powdered material from smallpox lesions or rubbing fluid from the pustule of an infected individual onto a scratch in the skin of a healthy individual.1 Later, around 1672, the Ottomans administered similar vaccinations to children in Turkey. In 1796, Edward Jenner became the first English physician to administer vaccinations and to demonstrate resulting immunity to smallpox. Today, the number of deaths due to vaccine-preventable diseases has been reduced, and many childhood diseases have been controlled by vaccination. Vaccines are therefore considered one of the most significant medical discoveries in the world.2,3
However, recent outbreaks of vaccine-preventable diseases have threatened the achievements of vaccination. The World Health Organization (WHO) has listed vaccine refusal among the top ten global threats to health, along with climate change, influenza pandemics, and antimicrobial resistance.4 According to the WHO Strategic Advisory Group of Experts (SAGE) on Immunization, “Vaccine hesitancy refers to a delay in acceptance or refusal of vaccination despite the availability of vaccination services. Vaccine hesitancy is complex and context-specific, varying across time and place. It is influenced by factors such as complacency, convenience, and confidence”.5,6 Vaccine hesitancy has been reported in developing and developed countries and is governed by many factors. Recent measles outbreaks in the United States have been associated with a lack of community vaccine compliance due to non-medical reasons such as religion, culture, and philosophy.7 In Pakistan, the main causes of vaccine hesitancy and refusal are religious conflicts with vaccination, security concerns, and lack of trust in the government.8 In Nigeria’s Kano State, rumors of an association between infertility and the polio vaccine adversely affected the Global Polio Eradication Initiative.9
Social media networks are internet-based applications that enable users to interact and share ideas; social media users can reach a large audience in a short period of time. People’s attitudes toward vaccination are changing with increased access to the internet and social media networks, especially during outbreaks of diseases.10,11 Although healthcare professionals are the primary source of information on health-related issues, many parents consider the internet an easily accessible source of health-related information, including information about vaccinations.12 Vaccine-hesitant groups are very active on social media, and most information about vaccines on social media is anti-vaccination. Such content may influence public opinion and increase vaccine hesitancy.13 Access to social media websites and blogs that are critical of vaccines has been shown to negatively impact attitudes toward vaccines and to increase vaccine hesitancy.14 One study found that viewing vaccine-critical websites for five to ten minutes decreased intention to vaccinate.15
In Saudi Arabia, a complete immunization history is compulsory for every six-year-old entering school. Neonatal tetanus and polio have been eradicated in Saudi Arabia, and measles, mumps, and rubella (MMR) are expected to be eliminated by 2020.16 In 2018, the Ministry of Health reported that 96% of the Saudi population had received the MMR vaccine and the Infanrix hexa vaccine (which protects against diphtheria, pertussis, tetanus, Hib, hepatitis B, and polio).17 Although vaccination rates are high in Saudi Arabia, some parents still seem to be concerned. Vaccine hesitancy rates of 13% to 23% have been reported among parents in different regions; vaccine hesitancy is particularly common in Riyadh, Saudi Arabia. A wide range of issues, such as delayed appointments, concerns about vaccine safety, and vaccine-related side effects requiring doctor’s appointments, are associated with vaccine hesitancy.18–21 Therefore, the present study explores the prevalence of vaccine hesitancy in Riyadh, Saudi Arabia, as well as factors affecting vaccine hesitancy.
The Parent Attitudes about Childhood Vaccines survey (PACV) is a very reliable and valid measure of vaccine hesitancy among parents and can be used to measure the attitudes of geographically and demographically diverse groups of parents.22,23 Thus, the objective of this cross-sectional study was to investigate the prevalence of childhood vaccine hesitancy and the impact of social media use and level of education on vaccine refusal among parents in Riyadh, Saudi Arabia. The PACV survey was used to measure vaccine hesitancy.
Methods
Study setting and sample
This cross-sectional study was conducted from October 2019 through March 2020 in the outpatient clinics of King Khalid University Hospital, Riyadh, Saudi Arabia. The sample size was calculated using the formula n = Zα2 P(1-P)/d2, where Zα = 1.96 (95% confidence level), d = 0.05, P = .15 (characteristics of the population, 15% prevalence of vaccine hesitancy), [(1.96)2(0.15)(1–015)/(0.05)2 = 196]. The calculated sample size was 236 after the sample was increased by 20% to cover the expected non-response rate. However, the final total number of participants in the study was 325. Systematic random sampling was used to select participants. All parents who came to the King Khalid University Hospital outpatient clinics during the study period were eligible to participate, regardless of their children’s ages. Included participants were parents over the age of 21; parents who came to the clinic to vaccinate their children were excluded to minimize selection bias as it was assumed that these parents were not vaccine hesitant.
Pilot study
The PACV is used to measure parental barriers to immunization acceptance. It contains 15 items organized into three domains (behavior, safety and efficacy, and general attitudes). Prior to the present study, the PACV survey had not been translated into Arabic. Therefore, a pilot study was conducted with 20 subjects to validate the tool and test the clarity of the translation. Participants in the pilot study were not included in the final study sample. The pilot study was conducted through a link to a Google form; participants provided consent via electronic signatures.
Data collection
The data were collected in the clinic waiting room using an iPad. The questionnaire was organized into three parts. The first part consisted of eight questions about socio-demographic and economic factors (age, gender, occupation, nationality, monthly income, level of education, place of residence, and number of children). These questions were designed to detect any association between education or socioeconomic status and parents’ childhood vaccination hesitancy. The second part of the questionnaire measured vaccine hesitancy using a validated PACV survey. The third part comprised four questions addressing social media use and the influence of social media on parents’ decisions about vaccinating their children. The questionnaire was delivered through a link to a Google form. The survey was self-administered and took approximately five minutes to complete. The respondents were eligible participants chosen via systematic random sampling. Participating parents confirmed their interest in participation and electronically signed the consent form. Ethical approval was granted by the College of Medicine Institutional Review Board of King Saud University (Ref No. 19/0199/IRB). Participation in the study was voluntary; no incentives or rewards were offered in exchange for participation. All data were kept confidential.
Parents’ attitudes toward childhood vaccines survey tool
Our questionnaire consisted of three parts. The first part collected demographic information about the participants, the second part measured vaccine hesitancy using the established PACV tool, and the third part measured social media use. The PACV tool is an instrument explicitly designed to identify parents’ vaccine hesitancy. It contains 15 questions organized into three domains: behavior, safety and efficacy, and general attitudes. To score the PACV, each of the 15 questions is assigned some points: 0 points are given for answers that do not indicate hesitancy, 1 for neutral answers, and 2 for answers indicating hesitancy. The points are then added to obtain a total raw score out of 30. This score is then converted to a scale from 0 to 100; using to the formula , where is the participant’s score. Parents are then assigned to categories based on this final score. A parent with a score below 50 is categorized as not hesitant, a score of 50 to 69 indicates vaccine hesitancy, and a parent with a score of 70 to 100 is categorized as very hesitant. We asked about the basic vaccinations on the vaccination certificate that children should receive before their first year of school. The vaccines involved are BCG, hepatitis B, hepatitis A, IPV, DTaP, Hib, pneumococcal conjugate (PCV), rotavirus, OPV, measles, meningococcal conjugate quadrivalent (MCV4), MMR, varicella, and DTaP (Td).24 Participants with only a primary, intermediate, or secondary school education were placed in the lower educational level group, and participants with diplomas, baccalaureates, masters, or PhDs were placed in the higher educational level group.
Statistical analysis
The data were analyzed using the statistical software SPSS, version 21.0. Descriptive statistics were calculated using frequencies and percentages, a bivariate statistical analysis was conducted using a chi-squared test, and a p-value of < 0.05 and a 95% confidence interval were used to measure the statistical significance and precision of the results. Frequencies and simple percentages were used to measure prevalence, socio-demographic factors, and the role of social media use in childhood vaccination hesitancy. The PACV scoring system was used to measure vaccine hesitancy, and a chi-squared test was used to determine the association between vaccine hesitancy and socio-demographic characteristics, educational level, and social media use.
Results
Socio-demographic characteristics of the participants
The largest cohort of participants was those aged 31 to 40 years (38.5%), followed by the age range of 41 to 50 (30.15%); most participants were female (69.8%). Most were Saudi nationals (95.4%) with a high level of education (77.5%), and most were employed (64.6%). The largest cohort had a monthly income of 7,501 to 15,000 SR (34.769%), followed by an income level of 15,000 SR or more (33.8%). Almost half of the participants (42.15%) lived in the north of Riyadh. A majority (55.4%) had one to three children (Table 1).
Table 1.
Socio-demographic characteristics of the participants
| Characteristic | Frequency | % |
|---|---|---|
|
Age 21–30 |
48 | 14.7 |
| 31–40 | 125 | 38.5 |
| 41–50 | 98 | 30.2 |
| More than 50 | 54 | 16.6 |
| Grand Total | 325 | 100 |
| Gender | ||
| Female | 227 | 69.85 |
| Male | 98 | 30.15 |
| Grand Total | 325 | 100 |
| Job | ||
| Employed | 210 | 64.6 |
| Unemployed | 115 | 35.4 |
| Grand Total | 325 | 100 |
| Nationality | ||
| Not Saudi | 15 | 4.6 |
| Saudi | 310 | 95.4 |
| Grand Total | 325 | 100 |
| Monthly Income | ||
| 5000 Riyals and less | 59 | 18.2 |
| 5501–7500 Riyals | 43 | 13.2 |
| 7501–15,000 Riyals | 113 | 34.8 |
| 15,000 Riyals and more | 110 | 33.8 |
| Total | 325 | 100 |
| Education | ||
| Higher level of education degree | 252 | 77.5 |
| Lower level of education | 73 | 22.5 |
| Total | 325 | 100 |
| Residency in Riyadh | ||
| North | 137 | 42.2 |
| South | 25 | 7.7 |
| East | 67 | 20.6 |
| West | 37 | 11.4 |
| Center | 14 | 4.3 |
| I do not live in Riyadh | 45 | 13.8 |
| Total | 325 | 100 |
| Number of children | ||
| 1 to 3 | 180 | 55.4 |
| 4 to 6 | 119 | 36.6 |
| 7 to 8 | 18 | 5.5 |
| More than 8 | 8 | 2.5 |
| Grand Total | 325 | 100 |
Socio-demographic characteristics and vaccine hesitancy
Vaccine hesitancy was more common among younger, non-Saudi parents (females aged 21–30 years), as well as among those with more than eight children and a lower level of education. Participants who lived in the west of Riyadh, were employed, and had a monthly income of 5,501 to 7,500 SR were more vaccine hesitant. However, none of the associations between any of the socio-demographic characteristics and vaccine hesitancy were significant (Table 2).
Table 2.
Associations of socio-demographic characteristics and vaccine hesitancy
| Demographic Data | Interpretation of Vaccine Hesitancy |
Count (Total %) | P-Value | |
|---|---|---|---|---|
| Hesitant Group count (% within each category) | Non Hesitant Group count (% within each category) | |||
| Age | ||||
| 21–30 | 9 (18.8) | 39 (81.3) | 48 (100) | 0.163 |
| 31–40 | 16 (12.8) | 109 (87.2) | 125 (100) | |
| 41–50 | 9 (9.2) | 89 (90.8) | 98 (100) | |
| > 50 | 3 (5.6) | 51 (94.4) | 54 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Gender | ||||
| Female | 28 (12.3) | 199 (87.7) | 227 (100) | 0.412 |
| Male | 9 (9.2) | 89 (90.8) | 98 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Job | ||||
| Employed | 28 (13.3) | 182 (86.7) | 210 (100) | 0.135 |
| Unemployed | 9 (7.8) | 106 (92.2) | 115 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Nationality | ||||
| Not Saudi | 3 (20.0) | 12 (80) | 15 (100) | 0.282 |
| Saudi | 34 (11.0) | 276 (89) | 310 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Monthly Income (SR) | ||||
| 5000 and less | 7 (11.9) | 52 (88.1) | 59 (100) | 0.750 |
| 5501–7500 | 6 (14.0) | 37 (86) | 43 (100) | |
| 7501–15,000 | 10 (8.8) | 103 (91.2) | 113 (100) | |
| 15,000 and more | 14 (12.7) | 96 (87.3) | 110 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Education | ||||
| Higher level of education degree | 27 (10.7) | 225 (89.3) | 252 (100) | 0.480 |
| Lower level of education | 10 (13.7) | 63 (86.3) | 73 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Residency | ||||
| North | 19 (13.9) | 118 (86.1) | 137 (100) | 0.310 |
| South | 3 (12) | 22 (88) | 25 (100) | |
| East | 6 (9) | 61 (91) | 67 (100) | |
| West | 6 (16.2) | 31 (83.8) | 37 (100) | |
| Center | 2 (14.3) | 12 (85.7) | 14 (100) | |
| I do not live in Riyadh | 1 (2.2) | 44 (97.8) | 45 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
| Number of Children | ||||
| 1 to 3 | 23 (12.8) | 157 (87.2) | 180 (100) | 0.397 |
| 4 to 6 | 11 (9.2) | 108 (90.8) | 119 (100) | |
| 7 to 8 | 1 (5.6) | 17 (94.4) | 18 (100) | |
| More than 8 | 2 (25) | 6 (75) | 8 (100) | |
| Total | 37 (11.4) | 288 (88.6) | 325 (100) | |
Vaccine acceptance and hesitancy
According to the PACV survey tool, 89% of participating parents were not hesitant; 8% were hesitant, and 3% were very hesitant. The overall prevalence of vaccine hesitancy was 11%. Various factors were associated with high acceptance of childhood vaccinations. In our survey, 87.7% of participating parents indicated that following the recommended vaccine schedule was good for their child, and 92.3% of parents said they would obtain all recommended vaccinations for their child if they had another infant. Most participants (71.4%) expressed confidence that childhood vaccination would prevent the indicated diseases, and 68.6% were not concerned at all about the side effects of vaccinations. Moreover, 74.5% of parents said they trusted the information they received about vaccination schedules and were quite open to discussing childhood vaccinations with their doctor (79%).
Some participants (24%) had delayed vaccinating their children for reasons other than illness or allergies, and 9.2% of participants had decided not to vaccinate their child(ren) for reasons other than illness or allergies. A few (16.3%) parents believed that giving more vaccinations were good for children. However, 22.8% of participants said that they would rather let their child get sick and develop immunity than vaccinate them, and 32.3% said that children should receive fewer vaccines at one time than the recommended schedule suggests (Table 3).
Table 3.
Analysis of parents’ response to PACV queries
| PACV questions | Frequency | % |
|---|---|---|
| 1- Have you ever delayed having your child get a shot for reasons other than illness or allergy? | ||
| Yes | 78 | 24 |
| No | 236 | 72.6 |
| I do not know | 11 | 3.4 |
| Total | 325 | 100 |
| 2- Have you ever decided not to have your child get a shot for reasons other than illness or allergy? | ||
| Yes | 30 | 9.2 |
| No | 278 | 85.6 |
| I do not know | 17 | 5.2 |
| Total | 325 | 100 |
| 3- If you had another infant today, would you want him/her to get all the recommended shots? | ||
| Yes | 300 | 92.3 |
| No | 16 | 4.9 |
| I do not know | 9 | 2.8 |
| Total | 325 | 100 |
| 4- How sure are you that following the recommended shot schedule is a good idea for your child? From 1 to 10 | ||
| 1 to 4 | 23 | 7.1 |
| 5 to 6 | 17 | 5.2 |
| 7 to 10 | 284 | 87.7 |
| Total | 324 | 100 |
| 5-Children get more shots than are good for them. | ||
| Agree | 53 | 16.3 |
| Neither agree nor disagree | 56 | 17.2 |
| Disagree | 216 | 66.5 |
| Total | 325 | 100 |
| 6- I believe that many of the illnesses that shots prevent are severe. | ||
| Agree | 232 | 71.4 |
| Neither agree nor disagree | 42 | 12.9 |
| Disagree | 51 | 15.7 |
| Total | 325 | 100 |
| 7- It is better for my child to develop immunity by getting sick than to get a shot. | ||
| Agree | 74 | 22.8 |
| Neither agree nor disagree | 50 | 15.4 |
| Disagree | 201 | 61.8 |
| Total | 325 | 100 |
| 8-It is better for children to get fewer vaccines at the same time. | ||
| Agree | 105 | 32.3 |
| Neither agree nor disagree | 108 | 33.3 |
| Disagree | 112 | 34.4 |
| Total | 325 | 100 |
| 9-How concerned are you that your child might have a serious side effect from a shot? | ||
| Very concerned | 102 | 31.4 |
| Not at all concerned | 223 | 68.6 |
| Total | 325 | 100 |
| 10- How concerned are you that any one of the childhood shots might not be safe? | ||
| Very concerned | 74 | 22.8 |
| Not at all concerned | 251 | 77.2 |
| Total | 325 | 100 |
| 11- How concerned are you that a shot might not prevent the disease? | ||
| Very concerned | 68 | 21 |
| Not at all concerned | 257 | 79 |
| Total | 325 | 100 |
| 12- Overall, how hesitant about childhood shots would you consider yourself to be? | ||
| Hesitant | 23 | 7 |
| Neutral | 32 | 10 |
| Not hesitant | 270 | 83 |
| Total | 325 | 100 |
| 13 – I trust the information I receive about shots. | ||
| Agree | 242 | 74.5 |
| Neither agree nor disagree | 48 | 14.8 |
| Disagree | 35 | 10.7 |
| Total | 325 | 100 |
| 14 – I am able to openly discuss my concerns about shots with my child’s doctor | ||
| Agree | 257 | 79 |
| Neither agree nor disagree | 46 | 14.2 |
| Disagree | 22 | 6.8 |
| Total | 325 | 100 |
| 15- All things considered; how much do you trust your child’s doctor? From 1 to 10 | ||
| 1 to 4 | 36 | 11.1 |
| 5 to 6 | 43 | 13.2 |
| 7 to 10 | 245 | 75.5 |
| Total | 324 | 100 |
| Vaccine Hesitancy based on PACV score | ||
| Very Hesitant | 10 | 3 |
| Hesitant | 27 | 8 |
| Not Hesitant | 288 | 89 |
| Total | 325 | 100 |
Educational level and vaccine hesitancy
To measure the association of educational level and vaccine hesitancy, participants were assigned to one of two groups: lower level of education (primary, intermediate, and secondary school) and higher level of education (diploma, bachelor, masters, and PhD). A chi-squared test of association showed no significant association between a high level of education and vaccine hesitancy (P = .480, 95% CI = 0.347–1.645). An odds ratio of 0.756 indicated that people with higher levels of education were approximately 24% less likely to be vaccine hesitant (Table 4).
Table 4.
Association between educational level, social media exposure and vaccine hesitancy
| Vaccine hesitant N = 37, n (%) | Non vaccine hesitant N = 37, n (%) | OR | P- value | 95% CI | |
|---|---|---|---|---|---|
| Educational level: | |||||
| Higher level of education | 27 (10.7) | 225 (89.3) | 0.756 | 0.480 | 0.347–1.645 |
| Lower level of education | 10 (13.7) | 63 (86.3) | |||
| Received information regarding vaccination on social media: | |||||
| YES | 20 (11.7) | 151 (88.3) | 1.272 | 0.556 | 0.353–1.752 |
| NO | 10 (9.4) | 96 (90.6) |
Social media use and vaccine hesitancy
A chi-squared test showed no significant association between social media use and vaccine hesitancy (P = .556, 95% CI = 0.353–1.752). An odds ratio of 1.272 showed that people who had received information about vaccines via social media were 1.272 times more likely to be vaccine hesitant. The 48 participants who responded “maybe” to the question about social media use were excluded from the analysis (Table 4). Participants were asked about the role of social media in disseminating information on childhood vaccination; 61.7% said that they had received information via social media, and 65.2% indicated that information on social media would not affect their attitudes toward childhood immunization. On the topic of participants’ preferred social media websites, 40% said they had used Twitter to obtain information about childhood vaccinations (Figure 1).
Figure 1.
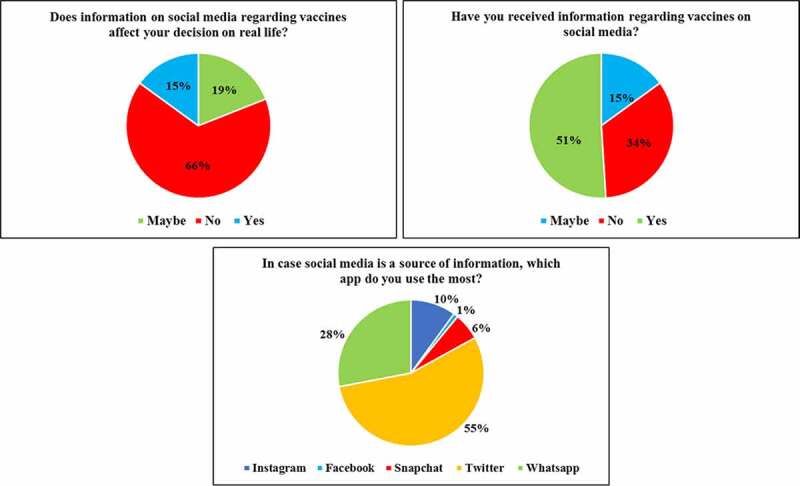
Analysis of role of social media in childhood vaccination.
Discussion
This is the first Arabic-language study of childhood-vaccine hesitancy using a validated survey tool, such as the PACV, in Saudi Arabia. In this survey, 11% of parents had a PACV score over 50, indicating childhood-vaccine hesitancy. A majority of parents (89%) had a PACV score under 50, which suggests high levels of acceptance of childhood vaccination among parents in Riyadh. Another study in Malaysia in which the PACV questionnaire was translated into Malay reported overall vaccine hesitancy of 11.6%; that study found that younger and unemployed parents were more vaccine hesitant.25 This consistency with our study demonstrates the reliability of the PACV questionnaire in different languages. In our study, a small percentage of employed younger parents were more vaccine hesitant. They might have little knowledge about the benefits of childhood vaccination or be unaware of the risks associated with not vaccinating their children. Misleading information from social media may also contribute to vaccine hesitancy. This highlights the need for healthcare professionals to educate younger parents about the importance of childhood vaccinations.
Previous studies in Riyadh have reported that 15% to 20% of wealthy, highly educated parents are childhood-vaccine hesitant. According to these studies, the main reasons for vaccine delay were the unavailability of vaccines and concerns about the safety and effectiveness of vaccines.18–20 However, our study found no association between parents’ level of education and vaccine hesitancy. An earlier study in the Hail region of Saudi Arabia also found high acceptance of childhood immunization (86.2%). Parents’ level of education and Ministry of Health remainders were the main factors that contributed to acceptance of childhood immunization in that study.21
Studies in other countries have reported higher rates of childhood-vaccine hesitance among parents. These different findings may be related to different recruitment methods and different measurements of vaccine hesitancy. In an Italian study that used the PACV survey, 34.7% of participants were vaccine hesitant due to a lack of recommendations from their pediatricians.26 In our study, 79% of parents said they were quite open to discussing childhood vaccinations with their doctor, and 75.5% said they trusted their child’s physician. This indicates a high level of trust in physicians regarding childhood vaccinations.
Recently, an increase in vaccine rejection and hesitation has been reported in Turkey. In that study, individuals with high incomes and high levels of education who lived in developed regions were more hesitant and more likely to refuse vaccines.18,27 Similarly, high income and high education levels have been identified as primary reasons for vaccine hesitancy in many other developed countries.28–30 However, our study found no significant association between level of education and vaccine hesitancy. Parents in our study with lower education levels were more likely to be vaccine hesitant, but this difference was non-significant. A recent study has found that low education levels for both parents is a valid predictor of vaccine refusal.31 These findings describe the multifaceted explanations of vaccine hesitancy in different populations. There may be a relationship between socioeconomic status and vaccine hesitancy, and parents with higher levels of education may trust their own critical thinking skills more and therefore play a more active role in decisions about vaccinations.
The internet and social media have revolutionized the modern world by connecting people and widely disseminating information. People can search for all sorts of information on social media, including information about health-related issues. Although social media plays an important role in disseminating information about the benefits of childhood vaccination, misinformation about vaccination is also receiving attention.32 Many people are now refusing childhood vaccinations due to negative information about vaccinations on social media; this has recently been identified as the second most common cause of vaccine refusal.27,33 In our study, no significant association between social media exposure and vaccine hesitancy was observed; however, vaccine hesitancy was more prevalent among people who obtained more information about vaccinations from social media. Among our participants, the most commonly used social media platform was Twitter (Figure 1). Thus, although the internet and social media platforms provide useful information, they can also disseminate incorrect information, generating distrust and confusion. This highlights the need for health organizations and ministries of health to deliver accurate information about vaccinations via social media platforms.
The participants in this study were all Muslims, and we hope that our findings will help build confidence in vaccination in other Muslim-majority regions and countries where anti-vaccination sentiments are prevalent on religious grounds. Our findings regarding awareness of the importance of vaccines are also encouraging in light of the current COVID-19 pandemic. Our findings indicate that, once an effective COVID-19 vaccine is available, most of the Riyadh community would not hesitate to receive the vaccination. This would help not only save human lives and arrest the virus but also alleviate the socioeconomic burden of the pandemic on individuals and nations.
Study limitations
The survey was conducted in Riyadh. Since most of the participants live in the north of the city, the findings may not be generalizable to other regions of the city. Most of the participants were also highly educated, but vaccine hesitancy was higher among people with lower levels of education, so the estimated prevalence of vaccine hesitancy might be lower than the actual prevalence. It is also assumed that the effect of social media on parents’ views is underestimated in this study due to selection bias. Therefore, future studies should collect data via social media platforms instead of at a hospital. Furthermore, even if both parents were involved in vaccination decisions, another limitation of our study is that mothers represented 69.8% of our sample, since parents may not fully share each other’s views on mandatory vaccinations for school admission. Future studies should include participants from other regions of Riyadh and other cities in Saudi Arabia as well.
Conclusion
Our study revealed a low prevalence of vaccine hesitancy in Riyadh. We investigated parent’s levels of education and socioeconomic status and the role of social media use in vaccine hesitancy in one setting. The participants expressed confidence in and acceptance of childhood vaccinations; we found that vaccine hesitancy was not influenced by level of education or social media use.
Acknowledgments
We would like to thank the participants of the study for their cooperation and assistance.
The authors extend their appreciation to the Deputyship for Research & Innovation, Ministry of Education, Saudi Arabia, for funding this research work through project no. IFKSURG-303.
Disclosure of potential conflicts of interest
The authors declare no potential conflict of interest.
References
- 1.Edward RS. Jenner and the history of smallpox and vaccination. Proc (Bayl Univ Med Cent). 2005;18(1):21–8. doi: 10.1080/08998280.2005.11928028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitney CG, Zhou F, Singleton J, Schuchat A.. Benefits from immunization during the vaccines for children program Era — United States, 1994–2013. MMWR Morb Mortal Wkly Rep. 2014;63:352–55. [PMC free article] [PubMed] [Google Scholar]
- 3.Orenstein WA, Ahmed R. Simply put: Vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114(16):4031–33. doi: 10.1073/pnas.1704507114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larson H, Schulz W. Reverse global vaccine dissent. Science. 2019;364:105. doi: 10.1126/science.aax6172. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald NE. SAGE working group on vaccine hesitancy. vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R. SAGE working group on vaccine hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine. 2015;33(34):4165–75. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 7.Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: A review of Measles and Pertussis. JAMA. 2016;315(11):1149–58. doi: 10.1001/jama.2016.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah SFA, Ginossar T, Weiss D. “This is a Pakhtun disease”: Pakhtun health journalists’ perceptions of the barriers and facilitators to polio vaccine acceptance among the high-risk Pakhtun community in Pakistan. Vaccine. 2019;37(28):3694–703. doi: 10.1016/j.vaccine.2019.05.029. [DOI] [PubMed] [Google Scholar]
- 9.Ghinai I, Willott C, Dadari I, Larson HJ. Listening to the rumours: what the northern Nigeria polio vaccine boycott can tell us ten years on. Glob Public Health. 2013. Dec;8(10):1138–50. doi: 10.1080/17441692.2013.859720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiyeh AB, Cooper S, Jaca A, Mavundza E, Ndwandwe D, Wiysonge CS. Social media and HPV vaccination: Unsolicited public comments on a facebook post by the western cape department of health provide insights into determinants of vaccine hesitancy in South Africa. Vaccine. 2019;37(43):6317–23. doi: 10.1016/j.vaccine.2019.09.019. [DOI] [PubMed] [Google Scholar]
- 11.Loft LH, Pedersen EA, Jacobsen SU, Soborg B, Bigaard J. Using facebook to increase coverage of HPV vaccination among danish girls: An assessment of a danish social media campaign. Vaccine. 2020;31:4901–08. S0264–410X (20)30512–0. doi: 10.1016/j.vaccine.2020.04.032. [DOI] [PubMed] [Google Scholar]
- 12.Bean SJ. Emerging and continuing trends in vaccine opposition website content. Vaccine. 2011;29(10):1874–80. doi: 10.1016/j.vaccine.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Ashkenazi S, Livni G, Klein A, Kremer N, Havlin A, Berkowitz O. The relationship between parental source of information and knowledge about measles/measles vaccine and vaccine hesitancy. Vaccine. 2020. Oct 27;38(46):7292–98. doi: 10.1016/j.vaccine.2020.09.044. [DOI] [PubMed] [Google Scholar]
- 14.Nan X, Madden K. HPV vaccine information in the blogosphere: how positive and negative blogs influence vaccine-related risk perceptions, attitudes, and behavioral intentions. Health Commun. 2012;27(8):829–36. doi: 10.1080/10410236.2012.661348. [DOI] [PubMed] [Google Scholar]
- 15.Betsch C, Renkewitz F, Betsch T, Ulshöfer C. The influence of vaccine-criticalwebsites on perceiving vaccination risks. J Health Psychol. 2010;15(3):446–55. doi: 10.1177/1359105309353647. [DOI] [PubMed] [Google Scholar]
- 16.Alsubaie SS, Gosadi IM, Alsaadi BM, Albacker NB, Bawazir MA, Bin-Daud N, Almanie WB, Alsaadi MM, Alzamil FA. Vaccine hesitancy among Saudi parents and its determinants. Result from the WHO SAGE working group on vaccine hesitancy survey tool. Saudi Med J. 2019;40(12):1242–50. doi: 10.15537/smj.2019.12.24653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.[Accessed November 7, 2020] https://www.moh.gov.sa/Ministry/Statistics/book/Documents/book-Statistics-2018.pdf [Google Scholar]
- 18.Al-Saeed G, Rizk T, Mudawi K, Al-Ramadina BA, Al-Saeed I. Vaccine hesitancy prevalence and correlates in Riyadh, Saudi Arabia. Acta Scientific Paediatrics. 2018;1:5–10. [Google Scholar]
- 19.Alabbad AA, Alsaad AK, Al Shaalan MA, Alola S, Albanyan EA. Prevalence of influenza vaccine hesitancy at a tertiary care hospital in Riyadh, Saudi Arabia. J Infect Public Health. 2018. Jul-Aug;11(4):491–99. doi: 10.1016/j.jiph.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Alrowaili GZ, Dar UF, Bandy AH. May we improve vaccine timeliness among children? A cross sectional survey in northern Saudi Arabia. J Fam Community Med. 2019;26:113‑117. doi: 10.4103/jfcm.JFCM_153_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alshammari TM, Subaiea GM, Hussain T, Moin A, Yusuff KB. Parental perceptions, attitudes and acceptance of childhood immunization in Saudi Arabia: A cross sectional study. Vaccine. 2018;36(1):23–28. doi: 10.1016/j.vaccine.2017.11.050. [DOI] [PubMed] [Google Scholar]
- 22.Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 23.Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: A validation study. JAMA Pediatr. 2013;167(11):1065–71. doi: 10.1001/jamapediatrics.2013.2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.[accessed 2019 Sep 20]. http://www.moh.gov.sa/en/HealthAwareness/EducationalContent/HealthTips/Document/Immunization-Schdule.pdf
- 25.Azizi FSM, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–61. doi: 10.1016/j.vaccine.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Napolitano F, D’Alessandro A, Angelillo IF. Investigating Italian parents‘ vaccine hesitancy: A cross-sectional survey. Hum Vaccin Immunother. 2020;38(31):4901–08. doi: 10.1016/j.vaccine.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Özceylan G, Toprak D, Esen ES. Vaccine rejection and hesitation in Turkey. Hum Vaccin Immunother. 2020;16(5):1034–39. doi: 10.1080/21645515.2020.1717182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rey D, Fressard L, Cortaredona S, Bocquier A, Gautier A, Peretti-Watel P, Verger P. on behalf of the Baromètre santé 2016 group. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Euro Surveill. 2018;23(17):17–00816. doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bocquier A, Ward J, Raude J, Peretti-Watel P, Verger P. Socioeconomic differences in childhood vaccination in developed countries: A systematic review of quantitative studies. Expert Rev Vaccines. 2017;16(11):1107–18. doi: 10.1080/14760584.2017.1381020. [DOI] [PubMed] [Google Scholar]
- 30.McKee C, Bohannon K. Exploring the reasons behind parental refusal of vaccines. J Pediatr Pharmacol Ther. 2016;21(2):104–09. doi: 10.5863/1551-6776-21.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bertoncello C, Ferro A, Fonzo M, Zanovello S, Napoletano G, Russo F, Baldo V, Cocchio S. Socioeconomic determinants in vaccine hesitancy and vaccine Refusal in Italy. Vaccines. 2020;8(2):276. doi: 10.3390/vaccines8020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoffman BL, Felter EM, Chu KH, Shensa A, Hermann C, Wolynn T, Williams D, Primack BA. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on facebook. Vaccine. 2019;37(16):2216–23. doi: 10.1016/j.vaccine.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Tran BX, Boggiano VL, Nguyen LH, Latkin CA, Nguyen HLT, Tran TT, Le HT, Vu TTM, Ho CS, Ho RC. Media representation of vaccine side effects and its impact on utilization of vaccination services in Vietnam. Patient Prefer Adherence. 2018;12:1717–28. doi: 10.2147/PPA.S171362. [DOI] [PMC free article] [PubMed] [Google Scholar]


