ABSTRACT
Vaccine hesitancy is a threat to global health, but it is not ubiquitous; depending on the country, the proportion that have confidence in vaccines ranges from a small minority to a huge majority. Little is known about what explains this dramatic variation in vaccine confidence. We hypothesize that variation in religiosity may play a role because traditional religious teachings are likely to be incompatible with the specific magical/spiritual health beliefs that often undergird anti-vaccination sentiments. In analyses of publicly available data in 147 countries, we find that a country measure of religiosity is strongly positively correlated with country measures of confidence in the safety, importance, and effectiveness of vaccines, and these associations are robust to controlling for measures of human development (education, economic development, and health). The underlying mechanism needs to be examined in future research.
KEYWORDS: Vaccine confidence, vaccine hesitancy, religion, religiosity, health beliefs
Vaccine hesitancy is a global threat to public health.1 Surveys show that there are countries in which only a small minority of the population have confidence in the safety, importance, and effectiveness of vaccines, but there are other countries where a huge majority of the population report vaccine confidence.2 To address the problem of vaccine hesitancy it is crucial to understand its roots.3 In this short note we address the roots of the dramatic variation across countries. Determinants of vaccine hesitancy are known to include a range of different factors, such as issues that are directly related to the vaccine or the vaccination process, individual and group influences, and contextual influences such as socio-cultural, environmental, health system/institutional, and economic factors.4 Our focus here will be on religion, which has long been recognized as an important factor for public health.5
In vaccine hesitancy research, religion has been identified as a factor that may contribute to vaccine refusal.6 However, religion does not generally seem to be anti-vaccine; there are several examples of how religious leaders and religious organizations promote vaccines.7 A review of religious teachings and vaccination found essentially no official religious texts that explicitly reject vaccines.8 A survey in 67 countries found religious objections to vaccines to be quite rare across the globe, and religious affiliation was not a strong predictor of vaccine confidence.9
In the present paper we focus on religiosity (i.e., whether religion is important to people) instead of religious affiliation. Our argument is that religiosity could serve to impede the spread of vaccine hesitancy. Anti-vaccination ideas are often grounded in specific magical/spiritual health beliefs (e.g., “healing energies”).10–13 Such beliefs have been termed “spiritual, not religious”,14 and are unlikely to fit with traditional religious teachings. The influence of traditional religious authorities on religious people may therefore serve as inoculation against beliefs that undermine vaccine confidence. If this theory is correct, vaccine confidence should be higher in more religious countries. Here, we test this prediction using available country-level data on vaccine confidence and religiosity.
It is important to consider confounders. According to modernization theorists, traditional religious beliefs tend to decline as societies shift from agrarian to industrial economies.15 Growing prosperity and increased life expectancy may help push people away from religion, and this global trend has been particularly fast in the last decade.16 Consistent with this process, country-levels of religiosity are strongly negatively correlated with the human development index, which measures development in terms of economic prosperity, education, and health.17 Importantly, country indicators of education and health were negatively associated with vaccine confidence in the aforementioned 67-country study.9 When examining the effect of religiosity on vaccine confidence we will therefore control for human development indicators.
We compiled data from different sources. From a recent study of vaccine confidence in 1491 countries, we obtained the percentages in each country that strongly agreed with the statements “I think vaccines are safe”, “I think vaccines are important for children to have”, and “I think vaccines are effective”.2 These measures were available both for 2015 and 2019. Measures of religiosity in 147 countries were obtained from a study based on data collected by Gallup World Poll using the question “Is religion important in your daily life?”.17 From the United Nations Development Programme (http://hdr.undp.org/en/data) we obtained data for 1462 countries on the Human Development Index and its three component measures: health (life expectancy at birth), education (mean of years of schooling for adults aged 25 years and more and expected years of schooling for children of school entering age), and standard of living (gross national income per capita, logarithmized). The compiled dataset is publicly available at github (https://github.com/irinavrt/vaccineconf-by-religiosity).
The 2015 and 2019 measures of vaccine confidence are very strongly correlated (safe: r =.82; important: r =.75; effective: r =.83). We use the average measures for these two years in our analyses. Separate analyses for 2015 and 2019 yield similar results to those we present here.
As a first step we correlated Pearson correlations between vaccine confidence measures and the predictor variables, see Table 1. Every dimension of vaccine confidence was strongly positively associated with religiosity. Figure 1 illustrates the associations between religiosity and confidence in vaccine safety, importance, and effectiveness.
Table 1.
Pearson correlations between vaccine confidence measures and other country variables
| Variable | N | Vaccines are safe | Vaccines are important | Vaccines are effective |
|---|---|---|---|---|
| Religiosity | 147 | 0.66 [0.56, 0.74] | 0.62 [0.51, 0.71] | 0.62 [0.51, 0.71] |
| HDI | 146 | −0.59 [−0.69, −0.47] | −0.54 [−0.65, −0.42] | −0.56 [−0.66, −0.43] |
| HDI:Health | 146 | −0.52 [−0.63, −0.39] | −0.48 [−0.60, −0.35] | −0.51 [−0.62, −0.38] |
| HDI:Education | 146 | −0.59 [−0.69, −0.48] | −0.57 [−0.67, −0.44] | −0.56 [−0.66, −0.43] |
| HDI:Income | 146 | −0.55 [−0.65, −0.42] | −0.48 [−0.60, −0.35] | −0.51 [−0.62, −0.38] |
N is the number of countries for which data were available. 95% confidence intervals in brackets.
Figure 1.
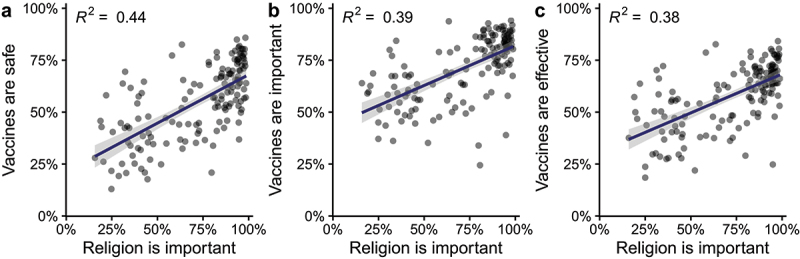
Percentage of people strongly agreeing that vaccines are (A) safe, (B) important for children, (C) effective, plotted against the percentage that think religion is important in 147 countries. Regression lines with 95% confidence intervals.
Table 1 reveals that vaccine confidence was negatively associated with all human development indicators, which potentially confounds results. To establish that religiosity has additional explanatory power we performed hierarchical regression analyses. We first predicted vaccine confidence using HDI3 and then added religiosity in a second step. The results are reported in Table 2, showing that religiosity explains country variation in vaccine confidence above and beyond human development. Note that results were highly similar across all three dimensions of vaccine confidence.
Table 2.
Results from hierarchical regression analyses of three dimensions for vaccine confidence
| Vaccines are safe | Vaccines are important | Vaccines are effective | ||||
|---|---|---|---|---|---|---|
| HDI | −0.59 [−0.72, −0.46] |
−0.22 [−0.40, −0.04] |
−0.54 [−0.68, −0.40] |
−0.18 [−0.37, 0.01] |
−0.56 [−0.70, −0.42] |
−0.22 [−0.41, −0.03] |
| Religiosity | 0.50 [0.33, 0.68] |
0.49 [0.30, 0.68] |
0.46 [0.27, 0.65] |
|||
| R2 | 0.35 | 0.46 | 0.29 | 0.40 | 0.31 | 0.41 |
| R2 change | 0.11 | 0.11 | 0.10 | |||
| BIC | 367 | 343 | 378 | 358 | 375 | 358 |
Standardized regression coefficients, with 95% confidence intervals, based on analyses of N = 146 countries.
By compiling data from different sources, we here examined the relation between religiosity and vaccine confidence. The main finding was that more religious countries tend to have higher confidence in the safety, importance, and effectiveness of vaccines. Religiosity explained country variation in vaccine confidence above and beyond measures of human development, in support of the hypothesis that something about religiosity itself may serve to protect against vaccine hesitancy. Due to the importance to public health of maintaining high confidence in vaccines, the finding that religiosity is so strongly associated with vaccine confidence is remarkable and merits further research. At the country level, religiosity could be confounded by some variable that we have not accounted for. In additional analyses not reported here we have checked that the effect of religiosity remains when controlling for other socio-economic country measures, such as government effectiveness and economic inequality. We have also checked that the effect can be replicated using measures of religiosity from the World Values Survey instead of Gallup, and that the effect of religiosity remains when controlling for a range of other cultural values measured in the World Values Survey. We are not aware of any other likely confounding country variable.
Our proposed explanation for the role of religiosity involves a psychological mechanism at the individual level: the magical/spiritual beliefs that vaccine hesitancy is often grounded in may be incompatible with traditional religious teachings. Thus, even when religions do not speak directly to the issue of vaccines, religiosity may tend to crowd out the philosophical underpinnings of anti-vaccine sentiments. Based on this theory we predict that more religious individuals will be less prone to vaccine hesitancy. This prediction, and the proposed mechanism, could be tested in future studies of vaccine confidence that also measure participants’ religiosity and health beliefs. Conducting such studies in multiple countries would also allow examination of whether the within-country effect of religiosity is moderated by other country variables, thus furthering our understanding of the complexity of vaccine hesitancy.
Funding Statement
This work was supported by the Knut och Alice Wallenbergs Stiftelse [2015.0005]; Knut och Alice Wallenbergs Stiftelse [2017.0257].
Notes
Hong Kong, Taiwan, and Northern Cyprus were treated as separate countries.
For Hong Kong and Taiwan, we used sub-national HDI from https://globaldatalab.org/shdi/.
The three HDI components are so strongly intercorrelated, r >.83, that estimates of their independent effects will be unreliable. The estimated effect of religiosity is very similar whether HDI or its components are used as covariates.
Contribution
All authors attest they meet the ICMJE criteria for authorship.
References
- 1.Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML.. Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. Plos One. 2017;12:e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. The Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. The Lancet. 2011;378(9790):526–35. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 4.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 5.Chatters LM. Religion and health: public health research and practice. Annu Rev Public Health. 2000;21(1):335–67. doi: 10.1146/annurev.publhealth.21.1.335. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed QA, Nishtar S, Memish ZA. Poliomyelitis in Pakistan: time for the Muslim world to step in. The Lancet. 2013;381(9877):1521–23. doi: 10.1016/S0140-6736(13)60764-3. [DOI] [PubMed] [Google Scholar]
- 7.Tomkins A, Duff J, Fitzgibbon A, Karam A, Mills EJ, Munnings K, Smith S, Seshadri SR, Steinberg A, Vitillo R. Controversies in faith and health care. The Lancet. 2015;386(10005):1776–85. doi: 10.1016/S0140-6736(15)60252-5. [DOI] [PubMed] [Google Scholar]
- 8.Grabenstein JD. What the world’s religions teach, applied to vaccines and immune globulins. Vaccine. 2013;31(16):2011–23. doi: 10.1016/j.vaccine.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Larson HJ, De Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolfe RM, Sharp LK. Anti-vaccinationists past and present. BMJ. 2002;325(7361):430–32. doi: 10.1136/bmj.325.7361.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Browne M, Thomson P, Rockloff MJ, Pennycook G. Going against the herd: psychological and cultural factors underlying the ‘vaccination confidence gap’. Plos One. 2015;10(9):e0132562. doi: 10.1371/journal.pone.0132562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bryden GM, Browne M, Rockloff M, Unsworth C. Anti-vaccination and pro-CAM attitudes both reflect magical beliefs about health. Vaccine. 2018;36(9):1227–34. doi: 10.1016/j.vaccine.2017.12.068. [DOI] [PubMed] [Google Scholar]
- 13.Lu J, Luo M, Yee AZH, Sheldenkar A, Lau J, Lwin MO. Do superstitious beliefs affect influenza vaccine uptake through shaping health beliefs? Vaccine. 2019;37(8):1046–52. doi: 10.1016/j.vaccine.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 14.Fuller RC. Spiritual, but not religious: understanding unchurched America. New York (NY): Oxford University Press; 2001. [Google Scholar]
- 15.Inglehart R, Baker WE. Modernization, cultural change, and the persistence of traditional values. Am Sociol Rev. 2000;65:19–51. doi: 10.2307/2657288. [DOI] [Google Scholar]
- 16.Inglehart RF. Giving up on god: the global decline of religion. Foreign Aff. 2020;99:110–18. [Google Scholar]
- 17.Joshanloo M, Gebauer JE. Religiosity’s nomological network and temporal change: introducing an extensive country-level religiosity index based on Gallup World Poll data. Eur Psychol. 2019;25(1):26–40. doi: 10.1027/1016-9040/a000382. [DOI] [Google Scholar]


