Abstract
BACKGROUND
Previous studies have shown that women who experience intimate partner violence have higher rates of unintended pregnancy and abortion—but whether there are differences between the types of abortion care accessed is unknown. Understanding the predictors of self-managed abortion is important for providing risk-mitigating information and resources to those at highest risk for unintended pregnancy and intimate partner violence. With access to information and medication abortion drugs, it is possible that self-managed abortion can be performed safely, increasing reproductive autonomy for women.
OBJECTIVE
The purpose of this study is to evaluate the association between experiencing intimate partner violence and using self-managed abortion.
STUDY DESIGN
This is a cross-sectional analysis of responses of 57,090 married women to the National Family Health Survey-4 conducted across India from 2015 to 2016. The association between the type of intimate partner violence and self-managed abortion was analyzed using multivariable multinomial logistic regression.
RESULTS
Women who have ever experienced physical intimate partner violence were more likely to have any abortion (adjusted relative risk=1.5; 95% confidence interval, 1.2–2.0) and use self-managed abortion (adjusted relative risk=1.7; 95% confidence interval, 1.1–2.6) than women who have not experienced physical intimate partner violence. Women who have ever experienced sexual intimate partner violence may have been more likely to use self-managed abortion, though this association was not statistically significant (adjusted relative risk=2.7; 95% confidence interval, 0.7–10.4).
CONCLUSION
Women who have experienced physical intimate partner violence disproportionately use abortion care, both facility-based and self-managed. Women who have experienced sexual intimate partner violence may also be more likely to use self-managed abortion. Although abortion is legal, self-managed abortion is commonly occurring in India. Self-managed abortion represents an additional choice and enhances reproductive autonomy in settings where abortion is legal. The implementation of risk-mitigation resources and policies regarding self-managed abortion would provide protection and enhanced autonomy to susceptible groups across India.
Key words: autonomy, clinician-managed abortion, gender-based violence, intimate partner violence, National Family Health Survey, physical violence, reproductive, self-use abortion, sexual violence
AJOG Global Reports at a Glance.
Why was this study conducted?
Despite abortion being legal in India since 1971, self-managed abortion (SMA) remains common. Understanding the predictors of SMA is important to providing safe, accessible, and comprehensive reproductive care across India. This study aimed to determine the association between lifetime experience of intimate partner violence (IPV) and SMA in the last 5 years.
Key findings
Women who experienced physical IPV had a higher risk of any abortion (both clinically managed and self-managed) than women who have not experienced IPV. Urban women were more likely to undergo SMA than rural women.
What does this add to what is known?
Women who experience physical IPV are a vulnerable population who disproportionately use abortion services, both within and outside the legal system. The specific needs of this population should be considered when increasing the availability of reproductive care in India.
Introduction
One in 3 Indian women experience intimate partner violence (IPV).1 This abuse may lead to loss of reproductive autonomy or control over reproductive life decisions and is associated with increased odds of unintended pregnancy and abortion.2,3
In India, approximately one-third of pregnancies end in abortion.4 In 2015, an estimated 15.6 million abortions occurred.4 Despite abortion being legal in India since 1971, abortion practices commonly occur outside of the legal healthcare system. Estimates of self-managed abortion (SMA) incidence vary widely; the National Family Health Survey (NFHS) estimates that 26% of abortions in India are self-managed.1 A 2015 Uttar Pradesh study found that only 11% of abortions occurred in facilities, whereas 83% were managed with medication abortion drugs purchased from pharmacies or private vendors outside the formal health system.5 The final 5% were managed with procedures outside the health system.5
SMA is a broad term encompassing many practices, which may provide greater reproductive autonomy but may also have higher risks of complications. Unsafe abortion is a leading cause of maternal mortality worldwide.6 In countries where abortion is legal and accessible, abortion-related complications are rare.7 When abortion is performed safely, as defined by the World Health Organization, abortion complications are less frequent than the complications associated with full-term pregnancy.8 There is a lack of data on the reasons why women in India self-manage abortion and the information and methods used in the process.
One factor that may contribute to self-managing abortion is the lack of reproductive autonomy to safely access reproductive healthcare. We hypothesized that women who experienced IPV are more likely to self-manage abortion because of their compromised reproductive autonomy than women who have not experienced IPV. We performed a retrospective cross-sectional analysis of the fourth round of NFHS (NFHS-4), a nationally representative survey, to assess the association between IPV and SMA among women in India.
Materials and Methods
Study design
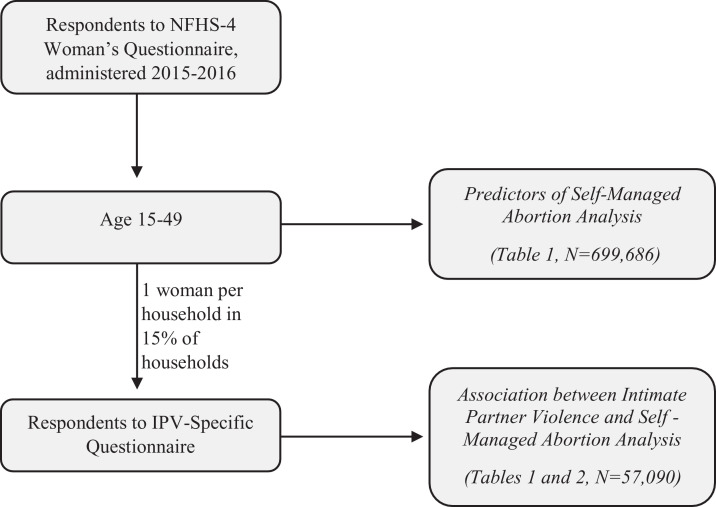
This is a cross-sectional analysis of predictors of SMA among women of reproductive age (15–49 years) in India who participated in the NFHS-4 (2015–2016) (Figure). An analysis of the association between self-reported IPV and SMA was conducted in a subset of ever-married women who were asked about experiences of IPV (1 woman per household in 15% of households); never-married women were thus excluded from the analytical sample.
Figure.
Flowchart of analyzed sample population
IPV, intimate partner violence; NFHS, National Family Health Survey.
Goemans. Intimate partner violence and self-managed abortion in India. Am J Obstet Gynceol Glob Rep 2021.
Data collection
Survey data were collected through the NFHS-4 (2015–2016) under the stewardship of the Ministry of Health and Family Welfare and administered by the International Institute for Population Sciences (IIPS) in Mumbai, India. The interviewer-administered survey was conducted in all 36 states and union territories. Additional information is provided in the final IIPS report.1
Ethics
All participants provided informed consent before completing the NFHS-4 survey. Ethical approval for data collection was provided by the IIPS Institutional Review Board. Ethical approval for analysis of this deidentified, publicly available data were provided by the Human Research Protections Program at the University of California San Diego, La Jolla, California.
Measures
IPV: we defined the occurrence of IPV (none, sexual only, physical only, or both sexual and physical) based on participants’ answers to a series of questions concerning their husbands’ behavior. Sexual IPV was defined by at least 1 affirmative answer to “Does/did your husband ever”: “physically force you to have sexual intercourse with him even when you did not want to?”; “physically force you to perform any other sexual acts you did not want to?”; or “force you with threats or in any other way to perform sexual acts you did not want to?” Physical IPV was defined by at least 1 affirmative answer to “Does/did your husband ever”: “push you, shake you, or throw something at you?”; “twist your arm or pull your hair?”; “slap you?”; “punch you with his fist or something that could hurt?”; “kick you, drag you, or beat you up?”; “try to choke you or burn you on purpose?”; or “threaten or attack you with a knife, gun, or any other weapon?”
Abortion: we defined the occurrence of abortion as an affirmative response to “Have you ever had a pregnancy that miscarried, was aborted, or ended in a still birth?” followed by selecting “abortion” when asked “Did that pregnancy end in a miscarriage, an abortion, or a stillbirth?” SMA was defined as actions taken by a person to end a pregnancy without supervision by a clinician outside of a medical facility.9 We restricted the analysis to recent SMA among women who reported having an abortion between 2011 and 2016, taking into account the recent increased availability of medication abortion regimens, which have the potential to affect the safety and availability of SMA. The occurrence of SMA was defined based on participants’ response to “Who performed your abortion?”, with the potential answers including the woman herself, a family member, a relative, a friend, or a Dai (traditional birth attendant). Women who reported that a trained medical professional (doctor, nurse, or auxiliary nurse midwife) supervised their abortion were considered to have had a clinically managed abortion.
Location of abortion was determined by asking “Where was your abortion performed?” and categorized as: (1) within the legal health system in a public or private facility (hospital, clinic, health center, dispensary, homeopathy clinic, or subcenter) or (2) outside the legal healthcare system (including at home or elsewhere).
Statistical analysis
Estimates of the prevalence of SMA in India vary widely, ranging from 16% to 75%.4,10 We estimated a priori that a 10% difference in SMA is clinically meaningful (30% for those who experience IPV and 20% for those who do not). To detect a 10% difference in SMA with a power of 80% and a 2-sided alpha of 0.05, we estimated that a sample size of at least 672 women (224 who experience IPV and 468 who do not) would be needed, assuming a 33% prevalence of IPV.1
All analyses were conducted using Stata software (version 15.0; StataCorp LLC, College Station, TX). We compared baseline characteristics between groups (those who experienced SMA and those who did not) using descriptive statistics, including: residence (urban or rural), age at first birth (continuous), birth parity (continuous), presence of a living son (yes or no), age at interview (continuous), caste (scheduled caste or scheduled tribe, other backward caste, or other), highest education level completed (no education, primary, secondary, or higher), and household wealth index, which is a composite measure of a household's cumulative living standard based on asset ownership (1st or lowest, 2nd, 3rd, 4th, and 5th or highest), religious affiliation (Muslim, Hindu, or other), and current employment status (employed or unemployed). We analyzed bivariate comparisons using chi-squared tests or Fisher exact tests for categorical variables and t-tests for continuous variables.
We used multivariable multinomial logistic regression to assess the association between IPV (physical, sexual, or both) and abortion type (no abortion, SMA, or clinically managed abortion). To account for the sample weights and multistage cluster survey sampling design, we used the “svy” commands of Stata 15.0 with domestic violence sample weights. Multivariable analyses were adjusted for covariates chosen a priori, including: residence, age at first birth, birth parity, presence of a living son, age at interview, caste, highest education level completed, and household wealth index.
Results
A total of 699,686 women of reproductive age (15–49 years) were interviewed. Of these, 190,898 women (26.4%) reported a pregnancy between 2011 and 2016 and 8878 (1.3%) reported an abortion. Of the abortions, 2486 (26.3%) were reported as self-managed and the remaining 6392 (73.7%) were managed by clinicians. There was high agreement between who performed the abortion (the woman herself or a clinician) and where the abortion occurred (home or health facility). We found that 90.4% of SMAs took place outside of a clinical setting. Of those reported to have been clinically managed, 94.7% were performed in a clinical setting (data not shown).
Among the subset of women who were administered the expanded questionnaire pertaining to IPV, 1026 reported an abortion between 2011 and 2016. A total of 402 women (39.2%) reported having experienced IPV, with 14 (1.4%) reporting only sexual IPV, 299 (29.1%) reporting only physical IPV, and 89 (8.7%) reporting both (Table 1). Among the subset asked about IPV who had an abortion, 332 women (32.4%) reported that their abortion was self-managed. Women who self-managed their abortion were on average younger at their first birth, had higher birth parity, and were more likely to already have a male child (P<.001 for all; Table 1) than women who received care from a clinician. In addition, women who self-managed their abortion had completed less education and had lower wealth indices than those who received clinical care (P<.01 for both; Table 1).
Table 1.
Descriptive analysis of women reporting an abortion in past five years preceding NFHS-4 in India
| Self-managed Abortion | Clinician-managed Abortion | No Reported Abortion | p-value | |
|---|---|---|---|---|
| Total women of reproductive age (15-49) (n=699,686) | 2,486 | 6,392 | 690,808 | |
| Total asked about IPV and Reproductive History (n=57,090) | 332 | 694 | 55,981 | |
| Ever Experience IPV by type N (%) | <0.001 | |||
| None | 189 (55.6) | 435 (62.8) | 39,302 (68.4) | |
| Physical | 95 (28.3) | 204 (28.0) | 13,085 (24.9) | |
| Sexual | 8 (2.7) | 6 (0.7) | 648 (1.2) | |
| Both | 40 (13.4) | 49 (8.5) | 2,946 (5.6) | |
| Reproductive History | ||||
| Age at first birth # [95% CI] | 20.3 [19.9, 20.7] | 21.2 [20.8, 21.6] | 20.5 [20.4, 20.5] | 0.006 |
| Birth parity # [95% CI] | 2.6 [2.3, 2.8] | 2.2 [2.02, 2.4] | 2.7 [2.6, 2.7] | <0.001 |
| Living Son N (%) | ||||
| Yes | 277 (83.4) | 525 (75.7) | 46,373 (81.5) | 0.006 |
| Socio-demographics | ||||
| Age of woman # [95% CI] | 28.6 [27.8, 29.4] | 28.9 [28.1, 29.7] | 33.9 [33.7,34.0] | <0.001 |
| Caste N (%) | 0.03 | |||
| SC/ST | 97 (28.8) | 191 (25.2) | 20,099 (28.3) | |
| OBC | 128 (35.5) | 283 (44.1) | 21,852 (44.8) | |
| Other | 107 (36.0) | 220 (31.0) | 14,030 (26.9) | |
| Completed Education N (%) | <0.001 | |||
| No education | 81 (22.4) | 129 (18.7) | 19,164 (33.6) | |
| Primary | 57 (16.8) | 94 (13.5) | 8,317 (14.5) | |
| Secondary | 170 (53.1) | 371 (51.9) | 23,658 (42.3) | |
| Higher | 24 (7.8) | 100 (16.0) | 4,842 (9.6) | |
| Wealth Index N (%) | 0.009 | |||
| 1st (lowest) | 64 (18.5) | 83 (11.1) | 10,911 (17.1) | |
| 2nd | 82 (20.8) | 145 (21.9) | 11,869 (19.2) | |
| 3rd | 80 (22.6) | 173 (23.5) | 11,582 (20.5) | |
| 4th | 66 (25.1) | 162 (22.5) | 11,174 (21.3) | |
| 5th (highest) | 40 (12.7) | 131 (21.1) | 10,445 (22.0) | |
| Residence N (%) | 0.343 | |||
| Rural | 229 (60.4) | 457 (64.1) | 39,727 (65.7) | |
| Urban | 103 (39.6) | 237 (36.0) | 16,254 (34.3) | |
| Religion N (%) | <0.001 | |||
| Muslim | 50 (15.7) | 126 (20.3) | 7,362 (13.6) | |
| Hindu / Other | 288 (84.3) | 569 (79.7) | 48,619 (86.4) | |
| Working N (%) | 0.234 | |||
| Currently employed | 71 (23.3) | 162 (20.7) | 13,756 (24.7) | |
| Currently unemployed | 267 (76.7) | 533 (79.3) | 42,225 (75.3) |
Goemans. Intimate partner violence and self-managed abortion in India. Am J Obstet Gynceol Glob Rep 2021.
Women who reported physical IPV (compared with no IPV) were more likely to have any abortion, whether self-managed or clinically managed (adjusted relative risk [ARR]=1.7; 95% confidence interval [CI], 1.1–2.6; ARR=1.5; 95% CI, 1.2–2.0, respectively) (Table 2). Women who experienced both physical and sexual IPV were also more likely to have self-managed or clinically managed abortions (ARR=3.0; 95% CI, 1.9–4.8; ARR=2.6; 95% CI, 1.6–4.2, respectively).
Table 2.
Unadjusted and adjusted multivariable multinomial logistic regression to examine the association between type of intimate partner violence and abortion, adjusting for confounders among women in India responding to National Family Health Survey-4
| Variables | Unadjusted relative risk of SMA (95% CI)/no abortion | Adjusted relative risk of SMA (95% CI)/no abortion | Unadjusted relative risk of clinically managed abortion (95% CI)/no abortion | Adjusted relative risk of clinically managed abortion (95% CI)/no abortion |
|---|---|---|---|---|
| Experience of IPV by type | ||||
| None | Ref | Ref | Ref | Ref |
| Sexual | 2.8 (0.8–10.1) | 2.7 (0.7–10.4) | 0.7 (0.3–1.7) | 0.8 (0.3–2.0) |
| Physical | 1.6a (1.1–2.3) | 1.7a (1.1–2.6) | 1.2 (1.0–1.6) | 1.5a (1.2–2.0) |
| Both | 3.0a (1.9–4.7) | 3.0a (1.9–4.8) | 2.0a (1.3–3.3) | 2.6a (1.6–4.2) |
| Reproductive history | ||||
| Age at first birth (y) | 1.0 (1.0–1.0) | 1.1a (1.1–1.2) | 1.0 (1.0–1.0) | 1.1a (1.1–1.1) |
| Birth parity | 1.0 (0.9–1.1) | 1.5a (1.3–1.6) | 0.8a (0.7–0.9) | 1.2a (1.1–1.3) |
| Living son | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 1.2 (0.8–1.8) | 1.6a (1.0–2.4) | 0.7a (0.5–0.9) | 1.1 (0.8–1.4) |
| Socio-demographics | ||||
| Age (y) | 0.9a (0.9–0.9) | 0.9a (0.9–0.9) | 0.9a (0.9–0.9) | 0.9a (0.9–0.9) |
| Caste | ||||
| SC/ST | Ref | Ref | Ref | Ref |
| OBC | 0.8 (0.5–1.1) | 0.8 (0.6–1.1) | 1.0 (0.8–1.4) | 1.0 (0.7–1.3) |
| Others | 1.3 (0.9–2.0) | 1.6a (1.07–2.4) | 1.2 (0.9–1.7) | 1.2 (0.8–1.7) |
| Completed education | ||||
| No education | Ref | Ref | Ref | Ref |
| Primary | 1.9a (1.2–3.0) | 1.9a (1.1–3.0) | 1.5a (1.0–2.3) | 1.2 (0.8–1.9) |
| Secondary | 2.0a (1.4–2.9) | 2.1a (1.3–3.5) | 2.1a (1.6–2.9) | 1.4a (1.0–1.9) |
| Higher | 1.2 (0.6–2.3) | 1.6 (0.7–3.6) | 2.9a (1.9–4.5) | 1.8a (1.2–2.9) |
| Wealth index | ||||
| 1st (lowest) | Ref | Ref | Ref | Ref |
| 2nd | 1.0 (0.7–1.5) | 1.0 (0.6–1.5) | 1.9a (1.2–3.1) | 2.0a (1.2–3.3) |
| 3rd | 1.1 (0.7–1.8) | 1.1 (0.7–1.9) | 2.0a (1.3–3.0) | 2.0a (1.3–3.2) |
| 4th | 1.1 (0.7–1.7) | 1.1 (0.6–1.8) | 1.8a (1.2–2.7) | 1.8a (1.1–2.9) |
| 5th (highest) | 0.5a (0.3–0.9) | 0.5a (0.3–1.0) | 1.7a (1.1–2.6) | 1.7 (1.0–2.9) |
| Residence | ||||
| Rural | Ref | Ref | Ref | Ref |
| Urban | 1.2 (0.8–1.6) | 1.6a (1.1–2.2) | 1.2 (0.9–1.5) | 1.1 (0.9–1.4) |
Total number of women=3223.
CI, confidence interval; IPV, intimate partner violence; OBC, other backward class; Ref, reference; SC/ST, scheduled caste/scheduled tribe; SMA, self managed abortion.
p-value <0.05
Goemans. Intimate partner violence and self-managed abortion in India. Am J Obstet Gynceol Glob Rep 2021.
Women who experienced only sexual IPV had increased risk of SMA compared with women who did not report any IPV, though this association did not meet statistical significance (ARR=2.7; 95% CI, 0.7–10.4). There was no difference between the risk of clinically managed abortion in those who experienced only sexual IPV and those who did not report any IPV (Table 2).
Women residing in urban areas had higher odds of self-managing their abortion than those in rural areas (ARR=1.6; 95% CI, 1.1–2.2) (Table 2).
Comment
Principal findings
In this cross-sectional study, we found that women who experienced physical IPV or both sexual and physical IPV were more likely to have an abortion. In addition, experiencing physical IPV or both sexual and physical IPV were associated with greater odds of SMA. Finally, we observed that urban women in India are more likely to self-manage an abortion than women living in rural areas, contrary to our hypothesis.
Results
In our study, women who experienced physical IPV were more likely to have an abortion. In previous studies, women who experienced physical violence had higher rates of unintended pregnancy.11 Moreover, studies in India show that physical IPV is associated with greater rates of abortion when compared with cases without reported IPV.11 This association between experiencing physical IPV and abortion in India is consistent with our results.
We found that women who experienced physical IPV, in addition to being more likely to have an abortion, were also more likely to self-manage abortion. As far as we are aware, this association has not been previously studied in India. A study in Bangladesh found that physical IPV was associated with SMA among women presenting for postabortion care.12 Factors influencing abortion care in Bangladesh and India differ greatly; notably, abortion is legal in India but largely illegal in Bangladesh, except when occurring in the context of menstrual regulation.
We also observed that women who experienced sexual IPV were more likely to have had a SMA than those who experienced no IPV. However, this association did not meet statistical significance, and we were underpowered to assess the association between SMA and sexual IPV further. The magnitude of the association was notable despite limited power to assess IPV by type. Unlike physical IPV, previous studies in India have shown that sexual IPV is not associated with higher rates of unintended pregnancy.11,13 Similarly, our analysis does not show an increase in abortion, but does demonstrate a higher likelihood of SMA in cases with reported sexual IPV. To our knowledge, this association has not been previously noted in India.
In our study, women living in urban areas were more likely to self-manage an abortion than those living rurally. Little research has been conducted concerning SMA rates in areas where abortion is legal and accessible. It is generally accepted that this practice occurs, but less frequently than in areas where abortion is otherwise inaccessible. This follows from the well-documented disparity in abortion safety across countries; abortion is increasingly safe as laws are less restrictive.7 If the correlation between access to legal, safe abortion and its frequency of use persisted within particular countries, this would conflict with our findings. However, this logic assumes that SMA is inherently unsafe and only used when other abortion options are unavailable. In contrast, SMA is becoming safer with the wider availability of medication abortion regimens.8,9,14 Moreover, previous studies have documented many reasons for choosing to self-manage over seeking clinical care, including safety considerations, autonomy, and privacy.9
Clinical implications
Experiencing physical violence may leave women vulnerable to reproductive coercion, a type of gender-based violence in which partners or families prevent contraceptive method use or otherwise coerce women into pregnancy against their will.15 This leads to a higher rate of unintended pregnancy among women who experience physical IPV.11 To avoid continuing an unintended pregnancy to term, women who experience physical IPV rely on abortion. In addition, they may particularly rely on SMA, a covert method of pregnancy termination, to resist the manipulation of reproductive coercion. Indeed, in India, women who experience physical IPV are more likely to use female-controlled contraceptives (eg, IUDs, pills), suggesting that covert use of family planning may be preferred in this population.16,17 Research from Niger also indicates that physical IPV is associated with greater covert use of contraceptive methods.15 Approximately one-third (over 100 million) of reproductive-age women in India experience physical IPV. With the significant size of this population and their greater use of all abortion methods, including SMA, it is critically important to consider how to best support reproductive autonomy and access to safe abortion in this population.18
Covert methods may be preferred both by women experiencing sexual IPV and those experiencing physical IPV, but contraceptives, even female-controlled ones, are used less frequently when the violence is primarily sexual.13 Other covert methods to gain control over reproductive choices, such as SMA, may be preferred by women experiencing sexual IPV because this makes pregnancy termination seem spontaneous. Overall, the effects of sexual IPV on the reproductive needs of women in India remain vastly unexplored. Further study is warranted to understand the reproductive health needs of this vulnerable population while preventing violence.
We originally hypothesized that women with less access to legal abortion services, such as women in rural areas, would be more dependent on SMA. This hypothesis was based on the traditional view of SMA as a last resort where formal abortion care is unavailable. However, the recent rise in availability of medication abortion regimens for SMA increasingly enables safe, effective, and accessible options.8 Our analysis accounted for this by including recent abortions since medication abortion regimens became widely available in India. This practice of SMA with medication abortion drugs is otherwise known as self-use abortion.19 SMA may be a preference rather than a last resort for some women because of considerations regarding autonomy and privacy.9 In a prospective study conducted across 3 countries, self-use abortion had few complications and was highly effective, making it a comparable option to clinically managed abortion where available.14 Indeed, contrary to our hypothesis, we observed that urban women were more likely to self-manage an abortion than women living in rural areas, suggesting that access to formal systems of care does not correlate with the frequency of clinically managed abortion. Urban women have greater access to clinics and information about self-managed methods but may choose the latter because it provides a few key advantages. Globally, women cite concerns about their emotional and social safety and logistic and financial barriers to legal abortion services.9 Abortion stigma and mistreatment by staff remain significant barriers to formal abortion care. Studies have explicitly cited avoiding the stigma of receiving abortion care or being seen at an abortion clinic as primary reasons for pursuing SMA.9 As the safety and efficacy of medication abortion improves and barriers to formal care persist, SMA may increasingly become a carefully considered choice enhancing reproductive autonomy rather than an act of desperation.18 However, this can only be true where safe and legal facility-based care is available along with SMA.
Research implications
Further prospective data are needed to understand the information acquired on SMA, the methods used in the process, and the reasons for selecting SMA. In addition, further investigation of the relationship between IPV, particularly sexual violence, and SMA is warranted.
Strengths and limitations
This study has several strengths. The dataset includes a large, nationally representative sample which allows the inclusion of many confounding variables owing to the comprehensive questionnaire. Our dataset was limited to recent abortions to reflect the contemporary abortion experience where medication abortion is widely available.
This study also has several limitations, including the cross-sectional nature of the analysis, which prevents conclusions regarding temporality and causality. Similarly, the time frame of lifetime experience of IPV differed from abortion use in the last 5 years, further limiting conclusions regarding temporality. All data are self-reported, making it prone to recall and social desirability biases. Nonetheless, self-reporting is the only method currently available for data collection on SMA because of its covert nature. In addition, only women who reported having an abortion were surveyed about SMA, so women who considered SMA to be menstrual regulation, miscarriage, or stillbirth were excluded. The questionnaire was administered by interview, which often results in underreporting of abortion and IPV, and presumably, even further underreporting of SMA. We observed a lower proportion of pregnancies reported to have ended in abortion (5.5 1.3%) compared with other studies from India which reported as many as 33% of pregnancies having ended in abortion in 2015.4
Conclusion
Legislative and medical bodies have historically viewed SMA as a dangerous act of last resort. With the increased availability of medication abortion drugs and medical information, SMA is becoming increasingly safe.9 SMA represents an additional choice when considering pregnancy termination; safe SMA increases reproductive autonomy, even where legal abortion care is available. For example, we found that women living in urban areas were more likely to have SMAs than women in rural areas, despite greater access to clinical care. SMA overcomes the key obstacles of facility-based abortion care, including stigma and financial and logistic barriers. However, we found that women susceptible to reproductive coercion, such as those who experienced IPV, continue to depend on SMA to covertly deal with unintended pregnancy. Despite the availability of legal abortion in India, multiple factors contribute to the use of SMA. Regardless of individual motivators, SMA is commonly occurring in India and can be safe if appropriate information, methods, and indications for seeking facility-based abortion care and postabortion care are available. The implementation of risk-mitigation policies expanding access to abortion medications through community locations could ensure accessible and safe abortion for more women, particularly those who experience IPV. More research is needed to meet the health and reproductive health needs of women who experience IPV in India.
Footnotes
The authors report no conflict of interest.
This work was supported by the Bill and Melinda Gates Foundation, grant number INV-002967; the National Institutes of Health, grant number 1R01HD084453-01A1; and the Gender Equity and Demographic Research Project, grant number BMGF OPP1179208.
Cite this article as: Goemans SL, Singh A, Yadav AK, et al. The association between intimate partner violence and recent self-managed abortion in India. Am J Obstet Gynecol Glob Rep 2021;1:100029.
References
- 1.Ministry of Health. Wellfare F. International Institute for Population Sciences . 2016. India fact sheet 2015–2016.http://rchiips.org/nfhs/pdf/NFHS4/India.pdf Available at: Accessed September 23, 2021. [Google Scholar]
- 2.Bhat M, Ullman SE. Examining marital violence in India: review and recommendations for future research and practice. Trauma Violence Abuse. 2014;15:57–74. doi: 10.1177/1524838013496331. [DOI] [PubMed] [Google Scholar]
- 3.Pallitto CC, García-Moreno C, Jansen HA, et al. Intimate partner violence, abortion, and unintended pregnancy: results from the WHO multi-country study on Women's Health and Domestic Violence. Int J Gynaecol Obstet. 2013;120:3–9. doi: 10.1016/j.ijgo.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Singh S, Shekhar C, Acharya R, et al. The incidence of abortion and unintended pregnancy in India, 2015. Lancet Glob Health. 2018;6:e111–e120. doi: 10.1016/S2214-109X(17)30453-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shekhar C, Sundaram A, Hussain R et al. Unintended Pregnancy and Post-abortion care in Uttar Pradesh India, 2015, New York: Guttmacher Institute, 2018. Available at:https://www.guttmacher.org/report/unintended-pregnancy-abortion-postabortion-care-uttar-pradesh-india-2015. Accessed September 23, 2021.
- 6.Haddad LB, Nour NM. Unsafe abortion: unnecessary maternal mortality. Rev Obstet Gynecol. 2009;2:122–126. [PMC free article] [PubMed] [Google Scholar]
- 7.Singh S, Remez L, Sedgh G, et al. 2018. The Guttmacher Institute. Abortion worldwide 2017. Uneven progress and unequal access.https://www.guttmacher.org/sites/default/files/report_pdf/abortion-worldwide-2017.pdf Available at: Accessed September 23, 2021. [Google Scholar]
- 8.Harris LH, Grossman D. Complication of unsafe and self-managed abortion. N Engl J Med. 2020;382:1029–1040. doi: 10.1056/NEJMra1908412. [DOI] [PubMed] [Google Scholar]
- 9.Moseson H, Herold S, et al. Self-managed abortion: A systematic scoping review. Best Pract Res Clin Obstet Gynaecol. 2020;63:87–110. doi: 10.1016/j.bpobgyn.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Arcara JL. Abortion and autonomy in urban Uttar Pradesh, India. Available at:https://cdr.lib.unc.edu/concern/dissertations/wh246x91r. Accessed September 23, 2021
- 11.Silverman JG, Boyce SC, Dehingia N, et al. Reproductive coercion in Uttar Pradesh, India: prevalence and associations with partner violence and reproductive health. SSM Popul Health. 2019;9 doi: 10.1016/j.ssmph.2019.100484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crouthamel B, Dixit A, Pearson E, et al. P14 intimate partner violence is associated with self-managed abortion in Bangladesh. Contraception. 2020;102:281. [Google Scholar]
- 13.Raj A, McDougal L. Associations of intimate partner violence with unintended pregnancy and pre-pregnancy contraceptive use in South Asia. Contraception. 2015;91:456–463. doi: 10.1016/j.contraception.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moseson H, Jayaweera R, Raifman S, et al. Self-managed medication abortion outcomes: results from a prospective pilot study. Reprod Health. 2020;17:164. doi: 10.1186/s12978-020-01016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverman JG, Challa S, Boyce SC, Averbach S, Raj A. Associations of reproductive coercion and intimate partner violence with overt and covert family planning use among married adolescent girls in Niger. EClinicalMedicine. 2020;22 doi: 10.1016/j.eclinm.2020.100359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen GL, Silverman JG, Dixit A, et al. A cross-sectional analysis of intimate partner violence and family planning use in rural India. EClinicalMedicine. 2020;21 doi: 10.1016/j.eclinm.2020.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDougal L, Silverman JG, Singh A, Raj A. Exploring the relationship between spousal violence during pregnancy and subsequent postpartum spacing contraception among first-time mothers in India. EClinicalMedicine. 2020;23 doi: 10.1016/j.eclinm.2020.100414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erdman JN, Jelinska K, Yanow S. Understandings of self-managed abortion as health inequity, harm reduction and social change. Reprod Health Matters. 2018;26:13–19. doi: 10.1080/09688080.2018.1511769. [DOI] [PubMed] [Google Scholar]
- 19.Kapp N, Blanchard K, Coast E. Developing a forward-looking agenda and methodologies for research of self-use of medical abortion. Contraception. 2018;97:184–188. doi: 10.1016/j.contraception.2017.09.007. [DOI] [PubMed] [Google Scholar]