Abstract
Background:
The cancer burden in the United States of America (USA) has decreased gradually. However, China is experiencing a transition in its cancer profiles, with greater incidence of cancers that were previously more common in the USA. This study compared the latest cancer profiles, trends, and determinants between China and USA.
Methods:
This was a comparative study using open-source data. Cancer cases and deaths in 2022 were calculated using cancer estimates from GLOBOCAN 2020 and population estimates from the United Nations. Trends in cancer incidence and mortality rates in the USA used data from the Surveillance, Epidemiology, and End Results program and National Center for Health Statistics. Chinese data were obtained from cancer registry reports. Data from the Global Burden of Disease 2019 and a decomposition method were used to express cancer deaths as the product of four determinant factors.
Results:
In 2022, there will be approximately 4,820,000 and 2,370,000 new cancer cases, and 3,210,000 and 640,000 cancer deaths in China and the USA, respectively. The most common cancers are lung cancer in China and breast cancer in the USA, and lung cancer is the leading cause of cancer death in both. Age-standardized incidence and mortality rates for lung cancer and colorectal cancer in the USA have decreased significantly recently, but rates of liver cancer have increased slightly. Rates of stomach, liver, and esophageal cancer decreased gradually in China, but rates have increased for colorectal cancer in the whole population, prostate cancer in men, and other seven cancer types in women. Increases in adult population size and population aging were major determinants for incremental cancer deaths, and case-fatality rates contributed to reduced cancer deaths in both countries.
Conclusions:
The decreasing cancer burden in liver, stomach, and esophagus, and increasing burden in lung, colorectum, breast, and prostate, mean that cancer profiles in China and the USA are converging. Population aging is a growing determinant of incremental cancer burden. Progress in cancer prevention and care in the USA, and measures to actively respond to population aging, may help China to reduce the cancer burden.
Keywords: Cancer, Incidence, Mortality, Trends, Aging, China, USA
Introduction
Cancer is the leading cause of deaths in China and developed countries.[1,2] GLOBOCAN 2020 estimated that there were 19,292,789 cancer cases and 9,958,133 cancer deaths globally in 2020.[2] The number of cancer cases and deaths, as well as crude incidence and mortality of cancer in China have increased gradually since 2000.[3,4] In the United States of America (USA), however, age-standardized rates of cancer incidence in men and cancer mortality in the whole population have generally decreased since the early 1990s.[5] Long-term trends in cancer burden and rates reflect both patterns in behaviors associated with cancer risk and changes in medical practice, such as the use of cancer screening tests. The relatively successful progress in cancer research, prevention, and care in the USA may provide lessons for other countries.[6]
China is making efforts to confront its rapidly increasing cancer burden.[7] However, rapid population aging and accumulated effects of risk factor exposure mean that it faces many new challenges for cancer prevention. A comparison of cancer profiles, trends, and determinants between China and the USA may inform activities and policy making around cancer prevention in China. We therefore carried out a comparative study to report cancer burden, long-term trends in cancer incidence and mortality rates, and the contributions of four determinant factors to incremental cancer deaths.
Methods
Data sources
We used open-source data from GLOBOCAN 2020 released by the International Agency for Research on Cancer,[8] the 2019 revision of World Population Prospects released by the United Nations (UN),[9] the Surveillance, Epidemiology, and End Results (SEER) program released by the National Cancer Institute,[5] the USA mortality files released by the National Center for Health Statistics,[5] cancer registry data released by the National Cancer Center (NCC) of China,[10] and the Global Burden of Disease (GBD 2019) released by the Institute for Health Metrics and Evaluation.[11] Cancer data from GLOBOCAN 2020 and population estimates from UN were used to estimate the cancer profiles in China and the USA in 2022. Longitudinal cancer data from SEER and China NCC were used in the trend analyses. Data from GBD 2019 were used to analyze the determinant factors of cancer deaths.
From the GLOBOCAN 2020 database, we extracted sex- and age-specific estimates of cancer cases and deaths for 35 cancer types (including all cancers combined) in China and the USA in 2020. The corresponding population estimates for 2020 and projections to 2022 were downloaded from the UN website by sex and age. For the 14 cancer types included in the trend analyses (top 10 cancer types for cancer cases and deaths among men and women in China in 2000),[10] we collected age-standardized cancer incidence rate from 1975 to 2018 and age-standardized cancer mortality rate from 1975 to 2019 in the USA from the SEER interactive website. Age-standardized cancer incidence and mortality in China between 2000 and 2015 were extracted from the previous published cancer registry report.[10] From the GBD 2019 database, we collected year-, sex-, and age-specific estimates of cancer cases and deaths for 29 cancer types in China and the USA between 1990 and 2019, accompanied by the corresponding population estimates.
Statistical analysis
Using the same methodology as GLOBOCAN 2020,[12] we linked cancer cases and deaths to the corresponding population estimates released by the UN. Age-specific cancer incidence and mortality rate in 2020 were calculated for 35 cancer types and by sex. We assumed that the age-specific rate in 2022 would remain constant at the rates estimated in 2020.[13] Cancer cases and deaths in 2022 in China and the USA were calculated by multiplying the age-specific rate by population estimates in 2022, and then aggregated by 35 cancer types (including all cancers combined) and sex. Cancer profiles in China in 2022 were estimated for Chinese mainland, Hong Kong, and Macau. Taiwan province was not included because of lack of data in GLOBOCAN 2020. Cancer profiles in the USA in 2022 were estimated for 50 states and the District of Columbia, but not the dependencies.
Trends in cancer incidence and mortality rates were reported separately by sex. Rates for USA cancer incidence (1975–2018) and mortality (1975–2019) were adjusted by 2000 USA standard population. Rates for cancer incidence and mortality (2000–2015) in China were adjusted by Segi's world standard population. A total of 14 cancer types were included in the trends analysis, including the top 10 cancer types in China in 2000 by incidence (lung, stomach, liver, esophagus, colorectum, bladder, pancreas, brain and central nervous system [CNS], leukemia, and prostate) and mortality (lung, liver, stomach, esophagus, colorectum, pancreas, brain and CNS, leukemia, bladder, and prostate) in males, and by incidence (breast, lung, stomach, colorectal, esophagus, liver, uterus, brain and CNS, thyroid, and cervix) and mortality (lung, stomach, liver, esophagus, colorectum, breast, brain and CNS, uterus, cervix, and thyroid) in females.[4,10]
Using the cancer deaths in 1990 as a reference, we used a decomposition method to express cancer deaths as the product of four determinant factors (ie, population aging, population size, age-specific cancer incidence rate, and case-fatality rate) among men and women aged 25 years and older from 1991 to 2019.[14,15] The four determinants corresponded to the four terms shown in the sum below:[14–16]
where a represents the 5-year age groups of men and women aged 25 years and older (up to 90 years and older), c represents the cancer type, and y represents the year. Cancer deaths attributable to the four determinant factors were calculated for 29 cancer types by sex, and then summed to give the total attributable cancer deaths in that year. The proportions of attributable cancer deaths among total cancer deaths in that year were calculated and the time trends between 1991 and 2019 were assessed.
Results
Profiles of cancer cases and deaths in 2022
The estimated numbers of new cancer cases and deaths in China (Taiwan province were not included) and the USA (excluding dependencies) in 2022 by sex and cancer type are shown in Table 1. In total, it is expected that there will be approximately 4,820,000 and 2,370,000 people newly diagnosed with cancer, and 3,210,000 and 640,000 people dying from cancer in China and the USA, respectively.
Table 1.
Estimated new cancer cases and deaths by sex in China and the United States, 2022.∗
| Estimated new cases | Estimated deaths | ||||||||||||
| China† | USA‡ | China† | USA‡ | ||||||||||
| ICD-10 | Cancer site | Total | Male | Female | Total | Male | Female | Total | Male | Female | Total | Male | Female |
| C00-97 | All sites | 4,820,834 | 2,625,070 | 2,195,764 | 2,372,145 | 1,282,341 | 1,089,804 | 3,208,516 | 1,943,763 | 1,264,753 | 640,724 | 338,601 | 302,123 |
| C00-97, but C44 | All sites excluding nonmelanoma skin | 4,796,996 | 2,612,375 | 2,184,621 | 1,817,871 | 925,496 | 892,375 | 3,193,744 | 1,935,833 | 1,257,911 | 633,795 | 333,898 | 299,897 |
| C00-06 | Lip, oral cavity | 31,733 | 19,484 | 12,249 | 25,210 | 16,914 | 8296 | 15,745 | 9913 | 5832 | 4452 | 2886 | 1566 |
| C07-08 | Salivary glands | 9165 | 5078 | 4087 | 5109 | 3033 | 2076 | 2912 | 1898 | 1014 | 1003 | 667 | 336 |
| C09-10 | Oropharynx | 5875 | 4575 | 1300 | 13,019 | 10,698 | 2321 | 3074 | 2516 | 558 | 3313 | 2601 | 712 |
| C11 | Nasopharynx | 64,165 | 46,570 | 17,595 | 1933 | 1385 | 548 | 36,315 | 26,168 | 10,147 | 945 | 665 | 280 |
| C12-13 | Hypopharynx | 6574 | 6079 | 495 | 2314 | 1892 | 422 | 3569 | 3235 | 334 | 572 | 475 | 97 |
| C15 | Oesophagus | 346,633 | 237,543 | 109,090 | 19,042 | 14,975 | 4067 | 323,600 | 221,524 | 102,076 | 16,916 | 13,617 | 3299 |
| C16 | Stomach | 509,421 | 352,955 | 156,466 | 27,294 | 16,612 | 10,682 | 400,415 | 274,691 | 125,724 | 11,898 | 7160 | 4738 |
| C18-21 | Colorectum | 592,232 | 340,257 | 251,975 | 160,248 | 84,579 | 75,669 | 309,114 | 177,921 | 131,193 | 56,693 | 30,164 | 26,529 |
| C22 | Liver | 431,383 | 316,979 | 114,404 | 43,732 | 30,712 | 13,020 | 412,216 | 302,327 | 109,889 | 32,332 | 21,415 | 10,917 |
| C23 | Gallbladder | 31,114 | 11,876 | 19,238 | 4874 | 1705 | 3169 | 25,143 | 10,086 | 15,057 | 2409 | 795 | 1614 |
| C25 | Pancreas | 134,374 | 75,178 | 59,196 | 59,143 | 31,227 | 27,916 | 131,203 | 72,680 | 58,523 | 49,920 | 26,166 | 23,754 |
| C32 | Larynx | 30,832 | 27,335 | 3497 | 12,954 | 10,295 | 2659 | 16,939 | 14,404 | 2535 | 3995 | 3173 | 822 |
| C33-34 | Lung | 870,982 | 575,302 | 295,680 | 238,032 | 121,953 | 116,079 | 766,898 | 505,618 | 261,280 | 144,913 | 76,828 | 68,085 |
| C43 | Melanoma of skin | 8114 | 4292 | 3822 | 99,935 | 59,435 | 40,500 | 4369 | 2396 | 1973 | 7530 | 4920 | 2610 |
| C44§ | Nonmelanoma skin§ | 23,838 | 12,695 | 11,143 | 554,274 | 356,845 | 197,429 | 11,181 | 6156 | 5025 | 5002 | 3626 | 1376 |
| C45 | Mesothelioma | 3381 | 1904 | 1477 | 3601 | 2677 | 924 | 2942 | 1731 | 1211 | 2695 | 2056 | 639 |
| C46 | Kaposi sarcoma | 282 | 154 | 128 | 1107 | 980 | 127 | 171 | 97 | 74 | 95 | 79 | 16 |
| C50 | Breast | 429,105 | – | 429,105 | 259,827 | – | 259,827 | 124,002 | – | 124,002 | 44,094 | – | 44,094 |
| C51 | Vulva | 3516 | – | 3516 | 6317 | – | 6317 | 1319 | – | 1319 | 1551 | – | 1551 |
| C52 | Vagina | 1711 | – | 1711 | 1496 | – | 1496 | 720 | – | 720 | 431 | – | 431 |
| C53 | Cervix uteri | 111,820 | – | 111,820 | 13,740 | – | 13,740 | 61,579 | – | 61,579 | 5830 | – | 5830 |
| C54 | Corpus uteri | 84,520 | – | 84,520 | 63,246 | – | 63,246 | 17,543 | – | 17,543 | 11,909 | – | 11,909 |
| C56 | Ovary | 57,090 | – | 57,090 | 24,494 | – | 24,494 | 39,306 | – | 39,306 | 14,914 | – | 14,914 |
| C60 | Penis | 4882 | 4882 | – | 1583 | 1583 | – | 1678 | 1678 | – | 435 | 435 | – |
| C61 | Prostate | 125,646 | 125,646 | – | 216,900 | 216,900 | – | 56,239 | 56,239 | – | 34,611 | 34,611 | – |
| C62 | Testis | 4509 | 4509 | – | 9500 | 9500 | – | 884 | 884 | – | 457 | 457 | – |
| C64-65 | Kidney | 77,410 | 50,088 | 27,322 | 71,676 | 45,128 | 26,548 | 46,345 | 31,172 | 15,173 | 15,259 | 9950 | 5309 |
| C67 | Bladder | 91,893 | 71,002 | 20,891 | 84,825 | 65,181 | 19,644 | 42,973 | 32,391 | 10,582 | 19,223 | 13,904 | 5319 |
| C70-72 | Brain, central nervous system | 82,673 | 42,474 | 40,199 | 25,177 | 14,136 | 11,041 | 68,283 | 35,204 | 33,079 | 18,752 | 10,590 | 8162 |
| C73 | Thyroid | 224,023 | 54,252 | 169,771 | 53,815 | 14,674 | 39,141 | 9915 | 3640 | 6275 | 2262 | 1084 | 1178 |
| C81 | Hodgkin lymphoma | 6984 | 4624 | 2360 | 8240 | 4676 | 3564 | 2948 | 1958 | 990 | 984 | 586 | 398 |
| C82-86, C96 | Non-Hodgkin lymphoma | 97,788 | 52,767 | 45,021 | 76,510 | 42,426 | 34,084 | 57,929 | 31,625 | 26,304 | 21,974 | 12,766 | 9208 |
| C88, C90 | Multiple myeloma | 22,450 | 12,989 | 9461 | 33,463 | 18,899 | 14,564 | 17,360 | 10,376 | 6984 | 14,145 | 8024 | 6121 |
| C91-95 | Leukaemia | 88,249 | 50,213 | 38,036 | 63,469 | 37,028 | 26,441 | 64,489 | 37,328 | 27,161 | 25,017 | 14,679 | 10,338 |
Estimates based on data released by the International Agency for Research on Cancer for GLOBOCAN 2020 and the WHO for World Population Prospects (2019 revision).
Including Chinese mainland, Hong Kong, and Macau. Taiwan province was not included because of lack of data in GLOBOCAN 2020.
USA dependencies were not included.
New cases exclude basal cell carcinoma, whereas deaths include all types of nonmelanoma skin cancer.
ICD: International Classification of Diseases.
Estimates suggest that the leading five cancer types diagnosed in 2022 will be cancers of the lung, colorectum, stomach, liver, and breast in China, and cancers of the breast, lung, prostate, colorectum, and melanoma of skin in the USA. The leading five causes of cancer death will be cancers of the lung, liver, stomach, esophagus, and colorectum in China, and cancers of the lung, colorectum, pancreas, breast, and prostate in the USA [Table 1]. The most common cancers diagnosed in males will be lung cancer in China and prostate cancer in the USA. Breast cancer will be the most common cancer in females in both countries. Lung cancer is expected to be the biggest cause of death in 2022 in both males and females, and in both countries [Table 1].
Trends in cancer incidence and mortality
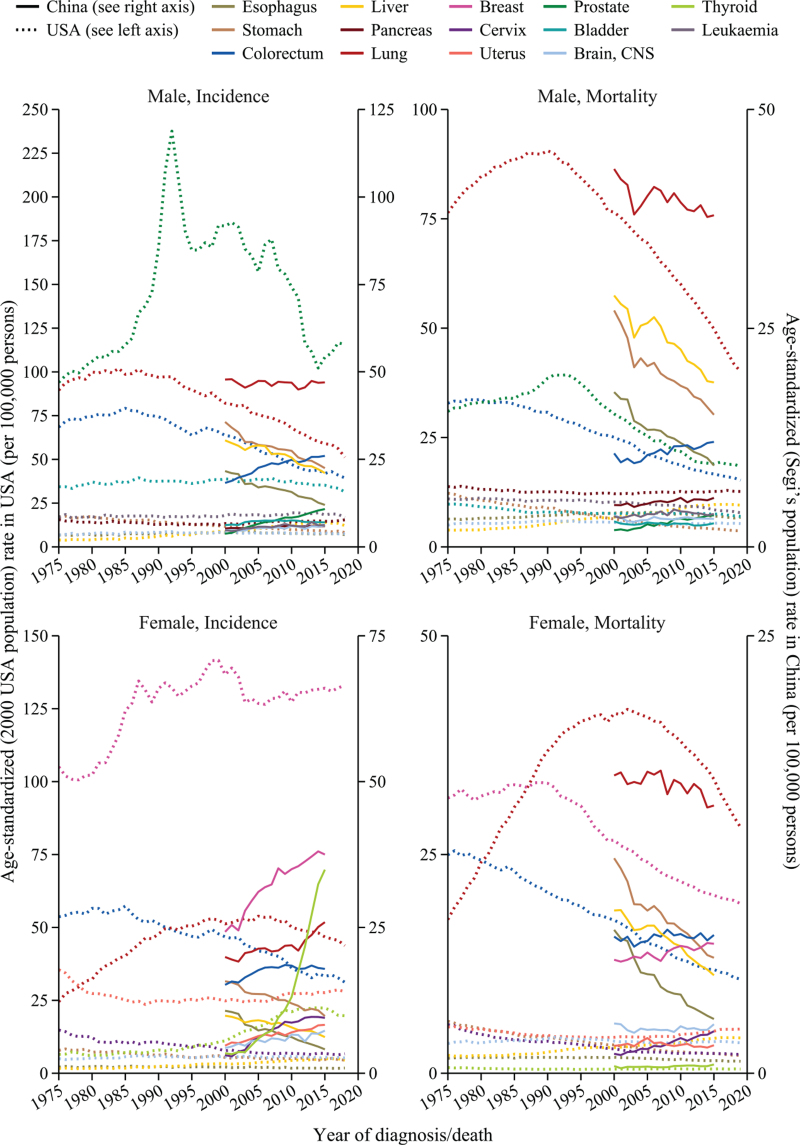
Long-term trends in incidence and mortality rates of 10 major cancer types are shown in Figure 1. Among male population, the incidence and mortality rates of lung and colorectal cancer in the USA, and of stomach, liver, and esophageal cancer in China have decreased gradually in recent years. However, the rates have significantly increased for liver cancer in the USA, and colorectal and prostate cancer in China. There was a spike in incidence of prostate cancer in the USA during the early 1990s because of widespread screening using prostate-specific antigen testing. From 2007 to 2014, the prostate cancer incidence rate decreased rapidly. Mortality rate for prostate cancer in the USA increased slightly during the early 1990s, and has since decreased almost continuously.
Figure 1.
Trends in cancer incidence and mortality rates by sex for China and the United States of America. Analyses were based on data released by the USA Surveillance, Epidemiology, and End Results program and the China National Cancer Center. Rates for USA cancer incidence (1975–2018) and mortality (1975–2019) were standardized by 2000 USA standard population. Rates for cancer incidence and mortality in China (2000–2015) were standardized by Segi's world standard population. CNS: Central nervous system.
Among female population, the incidence and mortality rates of lung and colorectal cancer in the USA, and of stomach, liver, and esophageal cancer in China have decreased gradually in recent years. However, the incidence rates for the other seven most common cancer types in Chinese women have all increased since 2000. Noticeably, the incidence rate of thyroid cancer has sharply increased since 2000 in both China and the USA, although the mortality rates were very stable during the same period [Figure 1].
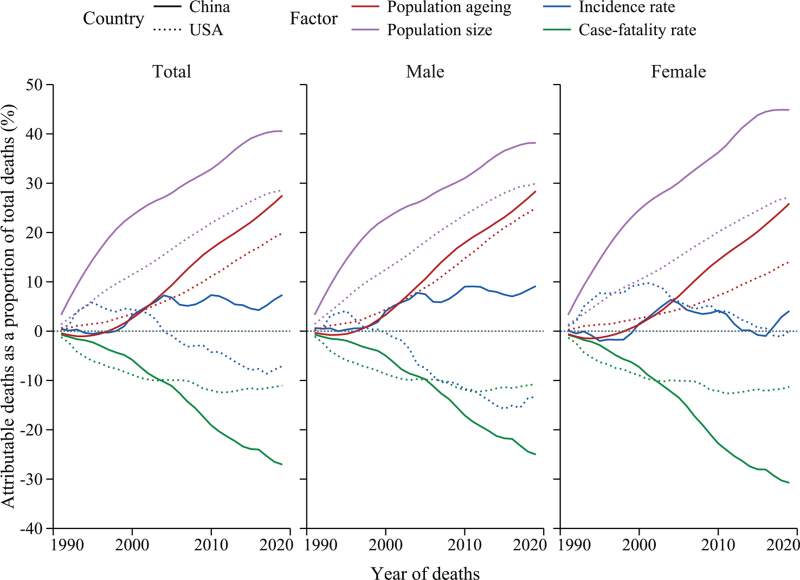
Determinants of cancer deaths
The incremental deaths between 1991 and 2019 were expressed by four determinant factors, using cancer deaths in 1990 as a baseline. The proportions of all cancer deaths attributable to the four determinant factors in each year are shown in Figure 2. The increase in the population size of adults aged 25 years and older was the leading determinant of incremental cancer deaths in both countries. Population aging was the second determinant of incremental cancer deaths since 2005, and in future may overtake population size. Except for males in the USA, age-specific cancer incidence rates contributed to increased cancer deaths. However, the proportion of deaths associated with age-specific incidence rate was much lower than that associated with population size and population aging, and the gaps were rapidly widening. Case-fatality rates contributed to reduced cancer deaths in both countries, with a more dramatic contribution in China in recent years than in the USA.
Figure 2.
Trends in determinant factors influencing cancer deaths by sex in China and the United States of America. Analyses were based on data released by the Institute for Health Metrics and Evaluation for Global Burden of Disease 2019. Cancer deaths were expressed as the product of four factors: (1) population aging, (2) population size, (3) age-specific cancer incidence rate, and (4) cancer case-fatality rate.
Discussion
In this comparative study, we reported estimated cancer statistics and profiles for 2022, long-term trends in cancer incidence and mortality rates, and determinant factors for incremental cancer deaths in China and USA. Lung cancer is expected to be the most common cancer in China and the leading cause of cancer death in both countries, with breast cancer the most common cancer in the USA in 2022. With the decreases in incidence and mortality rates for cancers of the stomach, liver, and esophagus, and increases in rates for cancers of the lung, colorectum, breast, and prostate, China's cancer profile is becoming similar to that of the USA. Increases in adult population size and population aging were major determinants of incremental cancer deaths. Some achievements in cancer prevention in the USA may inform the development of cancer control strategies in China.
The estimated cancer cases and deaths in the USA in our study were higher than projections reported by the American Cancer Society (ACS).[5] Cancer statistics in 2022 published by ACS projected 1,918,030 new cancer cases and 609,360 cancer deaths in the USA,[5] giving a gap of about 454,000 cancer cases and 31,000 cancer deaths between the two estimates. Similar differences were observed in reports of cancer statistics in 2020 and GLOBOCAN 2020, resulting in approximately 475,068 cancer cases and 5870 cancer deaths fewer than estimates in the USA in 2020.[8,17] The gaps between our estimates based on GLOBOCAN 2020 and cancer statistics published by ACS may be explained by the different measurements of non-melanoma cancer of the skin. We included non-melanomas of the skin in total cancer cases and deaths [Table 1], but the ACS did not.[2,5,8,17]
Population aging is likely to be a major social characteristic in China for the foreseeable future. China has one of the fastest growing aging populations in the world.[18] By the end of 2020, the population in China aged 60 years and older was 260 million, with an annual increase of approximately 10 million expected from 2021 to 2025.[19] The total population size in China is expected to reach a peak around 2025, and the proportion of those aged 60 years and older is expected to exceed 30% by 2035.[18,20] If population size remains stable or decreases, but population aging continues to increase, the upward trend in cancer burden is likely to remain unchanged in China. Healthy aging strategies would therefore need to be included in cancer prevention activities and multisectoral collaboration should be enhanced in policy development.[21]
China is undergoing a transition toward the cancer profiles in developed counties, characterized by high incidence of cancers of the lung, colorectum, breast, and prostate.[22] These changes are driving a move toward mass cancer screening and early detection for the eligible population aged 45 to 74 years old.[23] Several screening technologies and strategies have been developed to reduce the cancer burden in the USA, and might be introduced into cancer screening services in China.[5,24] Screening should target the high-risk population and cancers, such as colorectal, breast, lung, cervical, and upper gastrointestinal cancer.[24] Considering the large population, potential benefits and harms from screening, and the capacity of health services, China would probably not provide a “one size fit all” cancer screening service across each province and county.[10] Providing organized screening for high-risk areas and opportunistic screening for non-high-risk areas might be the most feasible solution in the near future.
Approximately 45.2% cancer deaths in China in adults aged 20 years or older were attributable to 23 modifiable risk factors.[25] Primary cancer prevention that is focused on controlling behavioral, dietary, metabolic and environmental factors, and infectious agents has great potential to reduce the burden of cancer in China. Compared with the USA, where smoking prevalence gradually decreased from 25% in 1997 to 15% in 2015, Chinese adults have a higher smoking prevalence (25.2% in 2013) and this is not changing.[26,27] Consequently, approximately 16.8% of all cancer deaths in adults 30 years and older in China were attributable to active and second-hand smoking, and more than 98% of these deaths in men were attributable to active smoking compared with 50% in women.[28] The tobacco epidemic remains at an earlier stage in China than in the USA, and the full impact of tobacco smoking patterns in recent decades on cancer mortality may therefore not yet have been realized.[29] If no tobacco control action is taken to immediately reduce tobacco use with implementation of targeted policies and programs, the burden of cancer will continue to grow dramatically. Comprehensive smoke-free policies should be adopted across China, instead of being largely limited to particular metropolitan areas.[28]
Cervical cancer is expected to be eliminated as a public health problem worldwide for the first time.[30] However, incidence and mortality rates of cervical cancer in China have increased significantly since 2000. Only if China adopts a comprehensive strategy, including human papillomavirus vaccination, cervical screening, and treatment of pre-invasive lesions and invasive cancer, then cervical cancer could be eliminated by the late 2040s, with potential economic benefits.[31]
The 5-year relative survival rate in cancer increased from 30.9% in 2003–2005 to 40.5% in 2012–2015 in China.[32] However, the survival rates for specific cancer types were lower in China than the USA, especially breast and colorectal cancer.[5,32] The data reported in our study also suggest that cancer prognosis in China is poorer than in the USA because the cancer-type-specific mortality to incidence ratios were generally lower in China. More efforts are needed in China to deliver effective cancer care and improve universal health coverage.[33]
Our study had several limitations. First, the estimates of cancer burden in 2022 were subject to biases within the GLOBOCAN 2020 reporting system.[12] Second, we used cancer rates in 2020 as an approximation of rates in 2022, which did not account for any potential changes from 2020 to 2022. Third, the data from GBD 2019 depended on the out-of-sample predictive validity of modeling work, particularly where data were not available.[34] Lastly, we adopted two distinct standard populations in calculating age-standardized incidence and mortality rates because long-term age-specific cancer cases, deaths and populations were not reported.[5,10]
In summary, there was a dramatic increase in incidence and mortality rates in cancers of the colorectum, female breast, and male prostate in China. However, rates of cancers of the stomach, liver, and esophagus decreased gradually. This produced a narrowing disparity between cancer profiles in China and the USA. Given the increasing contributions of population aging on the incremental cancer burden, China may benefit from adopting some of the effective prevention measures from USA, as well as actions to support healthy aging.
Funding
The work was supported by grants from the Chinese Academy of Medical Sciences (No. 2021-I2M-1-033), National Natural Science Foundation of China (No. 81974492), the Jing-jin-ji Special Projects for Basic Research Cooperation (No. J200017) and the Sanming Project of the Medicine in Shenzhen (No. SZSM201911015).
Acknowledgments
The views expressed are those of the authors only and do not represent any official position of the National Cancer Center (NCC) of China, Cancer Hospital, Chinese Academy of Medical Sciences (CHCAMS), Chinese Academy of Medical Sciences (CAMS), or Peking Union Medical College (PUMC).
Conflicts of interest
None.
Footnotes
How to cite this article: Xia C, Dong X, Li H, Cao M, Sun D, He S, Yang F, Yan X, Zhang S, Li N, Chen W. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J 2022;135:584–590. doi: 10.1097/CM9.0000000000002108
References
- 1.Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer 2021; 127:3029–3030. doi: 10.1002/cncr.33587. [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol 2020; 21:e342–e349. doi: 10.1016/s1470-2045(20)30073-5. [DOI] [PubMed] [Google Scholar]
- 4.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016; 66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 5.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin 2022; 72:7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 6.Schilsky RL, Nass S, Le Beau MM, Benz EJ, Jr. Progress in cancer research, prevention, and care. N Engl J Med 2020; 383:897–900. doi: 10.1056/NEJMp2007839. [DOI] [PubMed] [Google Scholar]
- 7. National Health Commission. Healthy China Action: cancer prevention and control implementation plan (2019–2022). Beijing: National Health Commission; 2019. Available from: http://www.nhc.gov.cn/jkj/s5878/201909/2cb5dfb5d4f84f8881897e232b376b60.shtml. [Accessed January 20, 2022] [Google Scholar]
- 8.Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer; 2020. [Google Scholar]
- 9. United Nations Department of Economic and Social Affairs Population Division. World Urbanization Prospects: The 2019 Revision. New York, USA United Nations, 2019; Available from: https://population.un.org/wpp/. [Accessed January 14, 2022] [Google Scholar]
- 10.Zhang S, Sun K, Zheng R, Zeng H, Wang S, Chen R, et al. Cancer incidence and mortality in China, 2015. J Natl Cancer Center 2021; 1:2–11. doi: 10.1016/j.jncc.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle, WA, USA: Institute for Health Metrics and Evaluation (IHME); 2020. [Google Scholar]
- 12.Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, et al. Cancer statistics for the year 2020: an overview. Int J Cancer 2021; 149:778–789. doi: 10.1002/ijc.33588. [DOI] [PubMed] [Google Scholar]
- 13.Ferlay J, Laversanne M, Ervik M, Lam F, Colombet M, Mery L, et al. Global Cancer Observatory: Cancer Tomorrow. Lyon, France: International Agency for Research on Cancer; 2020. [Google Scholar]
- 14.Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public health 2019; 4:e159–e167. doi: 10.1016/s2468-2667(19)30019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xia C, Chen W. Fractions and trends of cancer burden attributable to population ageing in China (in Chinese). Chin J Oncol 2022; 44:79–85. doi: 10.3760/cma.j.cn112152-20211012-00756. [DOI] [PubMed] [Google Scholar]
- 16.Das Gupta P. Standardization and Decomposition of Rates: A User's Manual. Washington, DC, USA: US Department of Commerce Economics and Statistics Administration; 1993. [Google Scholar]
- 17.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020; 70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 18.Vollset SE, Goren E, Yuan CW, Cao J, Smith AE, Hsiao T, et al. Fertility, mortality, migration, and population scenarios for 195 countries and territories from 2017 to 2100: a forecasting analysis for the Global Burden of Disease Study. Lancet 2020; 396:1285–1306. doi: 10.1016/s0140-6736(20)30677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The State Council of the People's Republic of China. The Projects to Actively Respond to Population Aging and Nursery School Constructions During the “14th Five-Year Plan”. Beijing, China: National Development and Reform Commission; 2021. [Google Scholar]
- 20.Institute for Health Metrics and Evaluation (IHME). Global Fertility, Mortality, Migration, and Population Forecasts 2017-2100. Seattle, WA, USA: Institute for Health Metrics and Evaluation (IHME); 2020. [Google Scholar]
- 21.Ye P, Jin Y, Er Y, Duan L, Palagyi A, Fang L, et al. A scoping review of national policies for healthy ageing in mainland China from 2016 to 2020. Lancet Reg Health West Pac 2021; 12:100168.doi: 10.1016/j.lanwpc.2021.100168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J 2021; 134:783–791. doi: 10.1097/cm9.0000000000001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cao M, Li H, Sun D, He S, Yu Y, Li J, et al. Cancer screening in China: the current status, challenges, and suggestions. Cancer Lett 2021; 506:120–127. doi: 10.1016/j.canlet.2021.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Cancer screening in the United States, 2019: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2019; 69:184–210. doi: 10.3322/caac.21557. [DOI] [PubMed] [Google Scholar]
- 25.Chen W, Xia C, Zheng R, Zhou M, Lin C, Zeng H, et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health 2019; 7:e257–e269. doi: 10.1016/s2214-109x(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 26.Wang M, Luo X, Xu S, Liu W, Ding F, Zhang X, et al. Trends in smoking prevalence and implication for chronic diseases in China: serial national cross-sectional surveys from 2003 to 2013. Lancet Respir Med 2019; 7:35–45. doi: 10.1016/s2213-2600(18)30432-6. [DOI] [PubMed] [Google Scholar]
- 27. Ward BW, Clarke TC, Nugent CN, Schiller JS. Early release of selected estimates based on data from the 2015 National Health Interview Survey. National Center for Health Statistics, 2016; Available from: http://www.cdc.gov/nchs/nhis.htm. [Accessed January 21, 2022] [Google Scholar]
- 28.Xia C, Zheng R, Zeng H, Zhou M, Wang L, Zhang S, et al. Provincial-level cancer burden attributable to active and second-hand smoking in China. Tob Control 2019; 28:669–675. doi: 10.1136/tobaccocontrol-2018-054583. [DOI] [PubMed] [Google Scholar]
- 29.Thun M, Peto R, Boreham J, Lopez AD. Stages of the cigarette epidemic on entering its second century. Tob Control 2012; 21:96–101. doi: 10.1136/tobaccocontrol-2011-050294. [DOI] [PubMed] [Google Scholar]
- 30.Xia C, Qiao Y, Zhang Y, Zhao F. WHO's global strategy of cervical cancer elimination and the challenges and initiatives in China (in Chinese). Natl Med J China 2020; 100:3484–3488. doi: 10.3760/cma.j.cn112137-20200909-02606. [DOI] [PubMed] [Google Scholar]
- 31.Xia C, Xu X, Zhao X, Hu S, Qiao Y, Zhang Y, et al. Effectiveness and cost-effectiveness of eliminating cervical cancer through a tailored optimal pathway: a modeling study. BMC Med 2021; 19:62.doi: 10.1186/s12916-021-01930-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, et al. Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob health 2018; 6:e555–e567. doi: 10.1016/s2214-109x(18)30127-x. [DOI] [PubMed] [Google Scholar]
- 33.GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1250–1284. doi: 10.1016/s0140-6736(20)30750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1204–1222. doi: 10.1016/s0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]