In this journal, Miller et al. have recently published an interesting article titled “A systematic review of COVID-19 and obstructive sleep apnoea” [1]. In this paper, the authors descriptively reviewed the potential relationship between obstructive sleep apnoea (OSA) and the risk for mortality among patients with coronavirus disease 2019 (COVID-19), but failed to quantitatively address this association. To our knowledge, some original studies reported that OSA was significantly linked to an elevated risk for fatal COVID-19 [[2], [3], [4]], while some others observed non-significant relationship between OSA and fatal COVID-19 [[5], [6], [7]]. Therefore, there is an urgent need to evaluate the association of OSA with fatal COVID-19 by performing a quantitative meta-analysis. Given that several risk factors have been reported to significantly affect the clinical outcomes of COVID-19 patients [[8], [9], [10]], which might modulate the relationship between OSA and fatal COVID-19, this quantitative meta-analysis was conducted on the basis of risk factors-adjusted effect estimates rather than un-adjusted effect estimates.
We conducted a systematic search in the electronic databases of PubMed, Web of Science, EMBASE and Scopus to identify all relevant published studies as of February 5, 2022, using the following search terms: “coronavirus disease 2019” or “COVID-19” or “severe acute respiratory syndrome coronavirus 2” or “SARS-CoV-2” or “2019 novel coronavirus” or “2019-nCoV” and “mortality” or “fatality” or “death” or “non-survivor” or “deceased” and “obstructive sleep apnea” or “obstructive sleep apnea syndrome” or “apnea, obstructive sleep” or “syndrome, obstructive sleep apnea”. Potential eligible articles were also found in references of the identified articles and related reviews. This meta-analysis strictly abided by the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [11]. Studies that met all of the following criteria were included: (i) Participants were COVID-19 patients diagnosed in the laboratory; (ii) Studies should be in English and peer-reviewed; (iii) Studies reported adjusted effect estimates on the association between OSA and the risk of mortality among COVID-19 patients. Studies with poor outcomes from COVID-19 patients that did not include death (mortality, deceased, fatality, and so on) were excluded. Case reports, review papers, comments, repeated studies, studies only reporting the characteristics of COVID-19 patients with OSA, and studies without available full text were also excluded.
Data extractions were independently performed by two authors (Mengke Hu and Jiahao Ren). Disagreements were resolved by communication with a third author (Xueya Han). Main characteristics included the first author name, country, study design, sample size, percentage of males, age, adjusted effect estimates and corresponding 95% confidence interval (CI), and setting. The study outcome of interest was death. The pooled effect was calculated to measure the risk of death outcome among COVID-19 patients with OSA. Heterogeneity between studies was assessed by using the I 2 statistic. A random-effects model was utilized if there was heterogeneity between studies (I 2 ≥ 50%). If not, a fixed-effects model was chosen. Begg's rank correlation test was performed to assess publication bias. Subgroup analysis and leave-one-out sensitivity analysis were also carried out. The R software (version 4.1.2, The R Foundation) was used to perform all statistical analyses. P < 0.05 was considered statistically significant.
383 articles were identified through a preliminary literature search, 152 articles remained after eliminating duplicates, 107 articles were excluded after reading the titles and abstracts, 45 full-text articles were assessed for eligibility, in the end, 13 articles [[2], [3], [4], [5], [6], [7],[12], [13], [14], [15], [16], [17], [18]] with 31,933 COVID-19 patients were included in this study. Of these thirteen studies, four studies were prospective and nine studies were retrospective. Three of the included studies were from Asia (one was from India, one was from South Korea, and one was from China), five studies were from Europe (one was from UK, one was from France, one was from the Netherlands, and two were from the Switzerland), and five studies were from North America (All were from USA). The primary characteristics of the included studies are shown in Table S1.
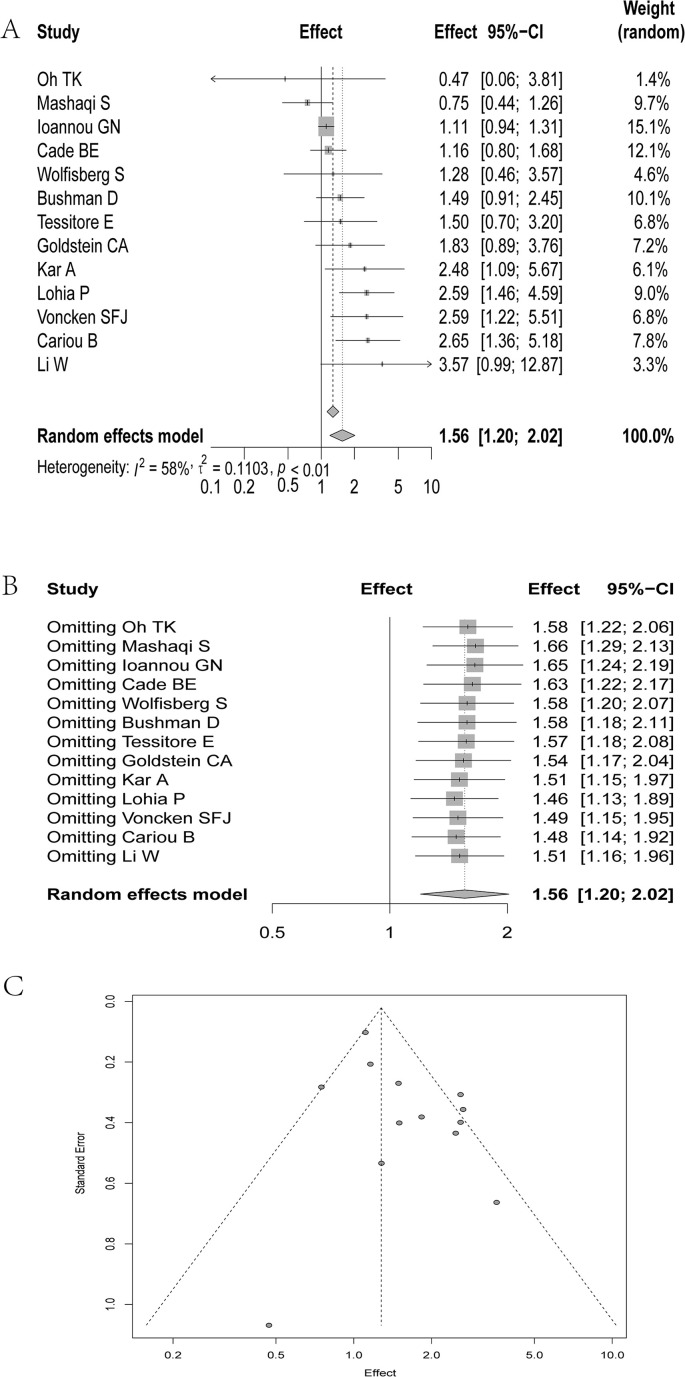
Our quantitative meta-analysis demonstrated that there was a statistically significant relationship between OSA and an elevated risk for fatal COVID-19 based on adjusted effect estimates (pooled effect estimate = 1.56, 95% CI: 1.20–2.02; Fig. 1 A). When the participants were restricted only to the hospitalized COVID-19 patients, this significant relationship still existed (pooled effect estimate = 1.71, 95% CI: 1.38–2.12). We observed consistent results in the subgroup analyses by age (pooled effect estimate = 1.43, 95% CI: 1.09–1.88 for age <60 years old, and pooled effect estimate = 1.82, 95% CI: 1.31–2.53 for age ≥60 years old, respectively) and study design (pooled effect estimate = 1.49, 95% CI: 1.06–2.08 for retrospective study, and pooled effect estimate = 1.73, 95% CI: 1.08–2.79 for prospective study, respectively). Sensitivity analysis showed that our results were stable and robust (Fig. 1B). Begg's test indicated that there was no publication bias in this meta-analysis (P = 0.713, Fig. 1C).
Fig. 1.
(A) The forest plot demonstrated the pooled effect estimate regarding the association between obstructive sleep apnoea (OSA) and the significantly increased risk for death among patients with coronavirus disease 2019 (COVID-19) on the basis of adjusted effect estimates; (B) Leave-one-out sensitivity analysis indicated the robustness of our results; (C) Begg's test showed no potential publication bias.
In conclusion, this quantitative meta-analysis demonstrated that OSA was independently associated with a significantly elevated risk for death among patients with COVID-19. Further well-designed studies with large sample sized prospective studies are warranted to confirm our findings. We hope that the data of this quantitative meta-analysis will contribute to more accurate elaboration and substantiation of the review documented by Miller et al. [1].
Author contributions
Haiyan Yang and Yadong Wang conceptualized the study. Mengke Hu and Jiahao Ren performed literature search and data extraction. Mengke Hu and Xueya Han analyzed the data. Mengke Hu wrote the manuscript. All the authors approved the final manuscript.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 81973105) and Henan Young and Middle-aged Health Science and Technology Innovation Talent Project (No. YXKC2021005). The funders have no role in the data collection, data analysis, preparation of manuscript and decision to submission.
Data availability statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.
Conflicts of interest
The authors do not have any conflicts of interest to disclose.
Acknowledgements
We would like to thank Hongjie Hou, Shuwen Li, Peihua Zhang, Jie Xu, Yang Li, Ruiying Zhang, Jian Wu, Xuan Liang, Ying Wang, Wenwei Xiao and Li Shi (All are from Department of Epidemiology, School of Public Health, Zhengzhou University) for their kind help in searching articles and collecting data, and valuable suggestions for analyzing data.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.smrv.2022.101624.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Miller M.A., Cappuccio F.P. A systematic review of COVID-19 and obstructive sleep apnoea. Sleep Med Rev. 2021;55:101382. doi: 10.1016/j.smrv.2020.101382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kar A., Saxena K., Goyal A., Pakhare A., Khurana A., Saigal S., et al. Assessment of obstructive sleep apnea in association with severity of COVID-19: a prospective observational study. Sleep Vigil. 2021:1–8. doi: 10.1007/s41782-021-00142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lohia P., Sreeram K., Nguyen P., Choudhary A., Khicher S., Yarandi H., et al. Preexisting respiratory diseases and clinical outcomes in COVID-19: a multihospital cohort study on predominantly African American population. Respir Res. 2021;22(1):37. doi: 10.1186/s12931-021-01647-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Voncken S.F.J., Feron T.M.H., Laven S., Karaca U., Beerhorst K., Klarenbeek P., et al. Impact of obstructive sleep apnea on clinical outcomes in patients hospitalized with COVID-19. Sleep Breath. 2021:1–9. doi: 10.1007/s11325-021-02476-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cade B.E., Dashti H.S., Hassan S.M., Redline S., Karlson E.W. Sleep apnea and COVID-19 mortality and hospitalization. Am J Respir Crit Care Med. 2020;202(10):1462–1464. doi: 10.1164/rccm.202006-2252LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bushman D., Davidson A., Pathela P., Greene S.K., Weiss D., Reddy V., et al. Risk factors for death among hospitalized patients aged 21-64 Years diagnosed with COVID-19-New York city, march 13-april 9, 2020. J Racial Ethn Health Disparities. 2021:1–16. [Google Scholar]
- 7.Mashaqi S., Lee-Iannotti J., Rangan P., Celaya M.P., Gozal D., Quan S.F., et al. Obstructive sleep apnea and COVID-19 clinical outcomes during hospitalization: a cohort study. J Clin Sleep Med. 2021;17(11):2197–2204. doi: 10.5664/jcsm.9424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang X., Shi L., Wang Y., Xiao W., Duan G., Yang H., et al. The association of hypertension with the severity and mortality of COVID-19 patients: evidence based on adjusted effect estimates. J Infect. 2020;81(3):e44–e47. doi: 10.1016/j.jinf.2020.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu J., Xiao W., Liang X., Zhang P., Shi L., Wang Y., et al. The association of cerebrovascular disease with adverse outcomes in COVID-19 patients: a meta-analysis based on adjusted effect estimates. J Stroke Cerebrovasc Dis. 2020;29(11):105283. doi: 10.1016/j.jstrokecerebrovasdis.2020.105283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang H., Xu J., Liang X., Shi L., Wang Y. Autoimmune diseases are independently associated with COVID-19 severity: evidence based on adjusted effect estimates. J Infect. 2021;82(4):e23–e26. doi: 10.1016/j.jinf.2020.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cariou B., Hadjadj S., Wargny M., Pichelin M., Al-Salameh A., Allix I., et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020;63(8):1500–1515. doi: 10.1007/s00125-020-05180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldstein C.A., Rizvydeen M., Conroy D.A., O'Brien L.M., Gupta G., Somers E.C., et al. The prevalence and impact of pre-existing sleep disorder diagnoses and objective sleep parameters in patients hospitalized for COVID-19. J Clin Sleep Med. 2021;17(5):1039–1050. doi: 10.5664/jcsm.9132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ioannou G.N., Locke E., Green P., Berry K., O'Hare A.M., Shah J.A., et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US veterans with SARS-CoV-2 infection. JAMA Netw Open. 2020;3(9):e2022310. doi: 10.1001/jamanetworkopen.2020.22310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li W., Xu Z., Xiang H., Zhang C., Guo Y., Xiong J. Risk factors for systemic and venous thromboembolism, mortality and bleeding risks in 1125 patients with COVID-19: relationship with anticoagulation status. Aging (Albany NY) 2021;13(7):9225–9242. doi: 10.18632/aging.202769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh T.K., Song I.A. Impact of coronavirus disease-2019 on chronic respiratory disease in South Korea: an NHIS COVID-19 database cohort study. BMC Pulm Med. 2021;21(1):12. doi: 10.1186/s12890-020-01387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tessitore E., Carballo D., Poncet A., Perrin N., Follonier C., Assouline B., et al. Mortality and high risk of major adverse events in patients with COVID-19 and history of cardiovascular disease. Open Heart. 2021;8(1) doi: 10.1136/openhrt-2020-001526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolfisberg S., Gregoriano C., Struja T., Kutz A., Koch D., Bernasconi L., et al. Comparison of characteristics, predictors and outcomes between the first and second COVID-19 waves in a tertiary care centre in Switzerland: an observational analysis. Swiss Med Wkly. 2021;151:w20569. doi: 10.4414/smw.2021.20569. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.