Highlights
-
•
Vaccine uptake was low among jail residents but increased with repeated offers.
-
•
Concerns around side effects and efficacy were major reasons for vaccine hesitancy.
-
•
Jail residents trusted jail health staff less than their doctor outside jail.
-
•
Trust in medical personnel was associated with greater vaccine acceptance.
-
•
Friends/family were the most trusted source for COVID-19 information.
Keywords: COVID-19, Vaccination, Incarcerated populations, Jails, Vaccine hesitancy, Vaccine acceptance, Medical mistrust
Abstract
Carceral facilities are high-risk settings for COVID-19 transmission. Factors associated with COVID-19 vaccine acceptance and hesitancy among incarcerated individuals are poorly understood, especially among jail residents. Here, we conducted a retrospective review of electronic health record (EHR) data on COVID-19 vaccine uptake in custody and additionally administered a survey to assess reasons for vaccine hesitancy, sources of COVID-19 information, and medical mistrust among residents of four Northern California jails. We performed multivariate logistic regression to determine associations with vaccine acceptance. Of 2,564 jail residents offered a COVID-19 vaccine between March 19, 2021 and June 30, 2021, 1,441 (56.2%) accepted at least one dose. Among vaccinated residents, 497 (34.5%) had initially refused. Vaccine uptake was higher among older individuals, women, those with recent flu vaccination, and those living in shared housing. Among 509 survey respondents, leading reasons for vaccine hesitancy were concerns around side effects and suboptimal efficacy, with cost and the need for an annual booster being other hypothetical deterrents to vaccination. Vaccine hesitancy was also associated with mistrust of medical personnel in and out of jail, although this association varied by race/ethnicity. Television and friends/family were the most common and most trusted sources of COVID-19 information, respectively. Overall, vaccine acceptance was much lower among jail residents than the local and national general population. Interventions to increase vaccination rates in this setting should utilize accessible and trusted sources of information to address concerns about side effects and efficacy, while working to mitigate medical and institutional mistrust among residents.
1. Introduction
Prisons, jails, and detention centers have been dangerous settings for COVID-19 transmission (Toblin and Hagan, 2021, Marquez et al., 2020), with some of the largest outbreaks in the US to-date (Burkhalter et al., 2021). Moreover, policing and incarceration disproportionately affect individuals and communities that already experience increased risk of COVID-19 infection and death due to systemic inequities, medical comorbidities, substance use disorders, mental health illnesses, and housing insecurity (Nowotny et al., 2021, Adhikari et al., 2020, Couloute, 2018, Jones and Wendy, 2019Jones and Wendy, 2019, Wang et al., 2021).
High vaccine coverage is needed to mitigate COVID-19 transmission in congregate, high-density settings such as prisons and jails, especially amidst viral variants (Ryckman et al., 2021, Chin et al., 2021). Studies in US prisons have identified differences in COVID-19 vaccine uptake across demographic groups (Chin et al., 2021, Hagan et al., 2021). However, less is known about COVID-19 vaccination in jails, which house people who have not been convicted of a crime or who are serving shorter sentences (Sawyer, 2020). Specific evidence from jails is needed given the unique conditions and population characteristics that may affect vaccine acceptance. For instance, jails have higher population turnover than prisons; such dynamicity may hinder vaccine operationalization and acceptance while simultaneously posing increased risk for infection spillover into outside communities (Kajeepeta et al., 2021, Reinhart and Chen, 2021). Jail residents are also younger on average and may experience differential risk of COVID-19 mortality than prison residents (James, 2002, Minton et al., 2020, Covid, 2021). Indeed, surveys conducted prior to vaccine availability have suggested lower willingness to get a COVID-19 vaccine among jail residents than prison residents (Khorasani et al., 2021, Stern et al., 2020), but data on actual COVID-19 vaccine uptake in jails is scarce (Berk et al., 2021, Komarla, 2021). Furthermore, while there have been studies on reasons for vaccine hesitancy in non-incarcerated populations (Aw et al., 2021, Thompson et al., 2021, Kreps et al., 2020, Ruiz and Bell, 2021), there are scant data on this topic among incarcerated individuals, even when considering the broader literature on vaccines for other communicable diseases (Madeddu et al., 2019). One reason for vaccine hesitancy may be mistrust of medical, custodial, or governmental personnel or institutions (Thompson et al., 2021, Vandergrift and Christopher, 2021); however, little research has directly examined its association with vaccine acceptance among incarcerated individuals. Such knowledge gaps preclude evidence-based efforts to improve vaccination rates for COVID-19 and other vaccine-preventable diseases in this high-risk setting.
In this study, we examine factors underlying COVID-19 vaccine acceptance and hesitancy, including medical mistrust, among residents of four jails in Santa Clara County and San Mateo County, California. COVID-19 vaccines became available to older and medically vulnerable residents in these jails on January 29, 2021 and to all jail residents on March 19, 2021. Beginning January 19, 2021, jail residents were screened periodically for interest in COVID-19 vaccination; anyone who expressed interest during screening was scheduled, upon becoming eligible, for an upcoming on-site vaccination clinic. We utilized electronic health record (EHR) data to examine COVID-19 vaccination uptake in these jails and changes in vaccine acceptance over time. We additionally conducted a survey among incarcerated individuals to understand vaccine hesitancy and its association with medical mistrust and sources of COVID-19 information. We hypothesized that vaccine acceptance would be associated with increased medical trust and with different trusted sources of COVID-19 information.
2. Methods
2.1. Retrospective chart review of vaccine uptake in jail
Data and study population. In Santa Clara County, all data related to COVID-19 vaccination in custody were entered in the jail EHR, which uses the same Epic software as the County of Santa Clara Health and Hospital System. These data included responses to screenings for interest in vaccination and records of vaccine uptake or refusal during biweekly vaccination clinics. We searched the EHR for individuals screened and/or vaccinated in custody between March 19, 2021 and June 30, 2021. We excluded individuals who were incarcerated for less than 26 days (the longest time between vaccine clinics) during the study period or who were only screened during the booking process. We extracted EHR data on age, gender, race/ethnicity, recent flu vaccination (within the last two years), and housing type (single cell, shared/double cell, or open dorm) at the time of vaccination or the most recent screening. S2 Text contains detailed information on race/ethnicity categorizations from EHR and survey data (see below). Open dorms are defined as units housing at least three, typically between 40 and 80, individuals. We did not have access to data on history of residence in other housing types. We report the chart review using the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines (S3 Checklists).
Changes in decision to get a vaccine. In an attempt to increase vaccination rates, custody health providers repeatedly screened for vaccine interest among residents who had previously declined. Individuals who declined interest could subsequently express interest and get vaccinated (i.e. change their decision from “No” to “Yes”). Conversely, individuals who expressed interest during screening could subsequently decline vaccination at the upcoming clinic for which they were scheduled (i.e. change their decision from “Yes” to “No”). For this analysis, we included screenings beginning January 19, 2021.
2.2. Survey on vaccine attitudes, sources of COVID-19 information, and medical trust
Survey development and administration. We conducted a cross-sectional survey between December 15, 2020 and April 30, 2021 to assess attitudes toward vaccination among jail residents in both counties (S1 Survey). Questions on vaccine acceptance were adapted from national surveys conducted by the Pew research group (Tyson et al., 2020). Questions on medical trust and general trust were adapted from research on the effect of physician race and medical mistrust on patients’ demand for preventive care (Alsan et al., 2018). Participants were recruited through flyers and announcements in their housing unit; in single-cell units, recruitment was done door-to-door. We excluded COVID-19 isolation units, units deemed by custody staff to be “high security risk,” and units designated for people with severe mental illnesses. Research assistants (RAs) obtained written informed consent and administered surveys via an electronic tablet; participants could choose to read and respond to questions themselves or respond orally to questions read aloud. Study procedures were conducted in a separate multi-purpose room within the housing unit whenever possible to increase privacy. Spanish-translated documents and Spanish-speaking RAs were available. Survey data were recorded in a HIPAA-secure REDCap database (Harris et al., 2009, Harris et al., 2019). Additional methodological details are provided in S2 Text. We report the survey using the Checklist for Reporting of Survey Studies (CROSS) (S3 Checklists) (Sharma et al., 2021).
Definition of vaccine acceptance and hesitancy. While most respondents had not yet been offered a vaccine at the time of taking the survey, a fraction (N = 115) had already been vaccinated or had already refused. We defined vaccine acceptance as uptake or intent, depending on whether a respondent had already been offered a vaccine at the time of survey completion. We defined vaccine hesitancy as vaccine refusal or intent to not get a vaccine when offered. These definitions are consistent with widely used definitions of vaccine acceptance and hesitancy in the literature, including those determined by the Strategic Advisory Group of Experts (SAGE) on Immunization (Aw et al., 2021, Kreps et al., 2020, Solís Arce et al., 2021, Sallam, 2021, MacDonald, 2015).
Linkage of survey responses with vaccination data. For respondents who had not yet been offered a vaccine, we linked their survey responses with records of their subsequent vaccine uptake or refusal through June 30, 2021 (S2 Text). For 90 respondents, data were missing or insufficient to determine vaccine refusal or uptake, likely due to release from jail prior to vaccine eligibility.
2.3. Statistical analysis
We performed multivariable logistic regression (a generalized linear model with a logit link function) to determine the association between COVID-19 vaccine uptake (response variable) and the following explanatory variables: age, gender, race/ethnicity, recent flu vaccination, and housing type. We also used multivariable logistic regression to investigate the effect of medical trust on vaccine acceptance (response variable) among survey respondents. We adjusted for age group, gender, race/ethnicity (self-reported), general trust, and medical trust, with the interaction between race/ethnicity and medical trust as the main explanatory variable of interest. General trust and medical trust were dichotomized as trust or neutral/do not trust. We computed adjusted odds ratios for the change in vaccine acceptance among those within each racial/ethnic group who reported medical trust. Separate regressions were fit using either trust in jail health staff or trust in one’s doctor outside of jail. Using a rule-of-thumb of at least ten events per variable (Peduzzi et al., 1996), we expect stable estimates for regression coefficients with at least 60 events.
We performed chi-square tests of independence to determine whether differences in vaccine acceptance among subgroups were statistically significant. Respondents who selected “Prefer not to answer” for a given question were excluded from analysis of that question. Analyses were conducted using Stata version 17.0 and R version 4.0.5. This work was approved by the institutional review boards of Stanford University (#56169) and Valley Medical Center (#20–022 and #21–018).
3. Results
3.1. Factors associated with COVID-19 vaccine uptake
Of 2,564 jail residents who were offered a COVID-19 vaccine between March 19, 2021 and June 30, 2021, 1,441 (56.2%) accepted at least one dose. Results of a multivariable logistic regression showed that uptake increased with age and was higher among women than men and lower among Black individuals than other racial/ethnic groups (Table 1). COVID-19 vaccine uptake was also significantly higher among those with recent flu vaccination than those without, and among those housed in shared cells or open dorms than those in single cells.
Table 1.
Vaccination and adjusted odds ratios for vaccine uptake by demographic characteristics, recent flu vaccination, and housing type.
| Group | Number Offered Vaccine (% of total) | Number Receiving Any Dose (% of subgroup) | Adjusted Odds Ratio (95% CI) |
|---|---|---|---|
| Age | |||
| 18–29 | 781 (30.5) | 319 (40.8) | Ref |
| 30–49 | 1,433 (55.9) | 869 (60.6) | 2.2 (1.9–2.7)*** |
| 50+ | 350 (13.7) | 253 (72.3) | 3.7 (2.8–4.9)*** |
| Gender | |||
| Female | 256 (10.0) | 164 (64.1) | Ref |
| Male | 2,308 (90.0) | 1,277 (55.3) | 0.6 (0.4-0.8)*** |
| Race/ethnicity | |||
| White | 474 (18.5) | 271 (57.2) | Ref |
| Hispanic/Latinx | 1,374 (53.6) | 784 (57.1) | 1.1 (0.9–1.4) |
| Black | 303 (11.8) | 145 (47.9) | 0.8 (0.6–1.0) |
| Asian | 213 (8.3) | 128 (60.1) | 1.1 (0.8–1.6) |
| Other/Unknown | 200 (7.8) | 113 (56.5) | 1.2 (0.8–1.7) |
| Recent Flu Vaccination | |||
| No / Unknown | 2,019 (78.7) | 1,034 (51.2) | Ref |
| Yes | 545 (21.3) | 407 (74.7) | 2.8 (2.3–3.5)*** |
| Housing Type | |||
| Single Cell | 146 (5.7) | 61 (41.8) | Ref |
| Shared Cell | 1,121 (43.7) | 595 (53.1) | 1.8 (1.3–2.6)*** |
| Open Dorm | 1,297 (50.6) | 785 (60.5) | 2.3 (1.6–3.3)*** |
| Total | 2,564 | 1,441 (56.2) | |
***, p ≤ 0.001. Recent flu vaccination was defined as documentation within the last two years in the EHR and state vaccination repository.
3.2. Changes in decision to get a vaccine
Of the 1,441 vaccinated individuals, 497 (34.5%) had declined during at least one previous screening. Those who were ultimately vaccinated despite previous refusal (i.e. who changed their decision from “No” to “Yes”), were more likely to be younger, women, and residing in shared housing (Fig S1A). Conversely, of the 1,1123 individuals who remained vaccinated, 148 (13.2%) had expressed interest in vaccination during a previous screening. Among those who remained unvaccinated, the percentage who had previously expressed interest (“Yes to No”) ranged from 10% to 16% across demographic groups (Fig S1B).
3.3. Reasons for COVID-19 vaccine hesitancy
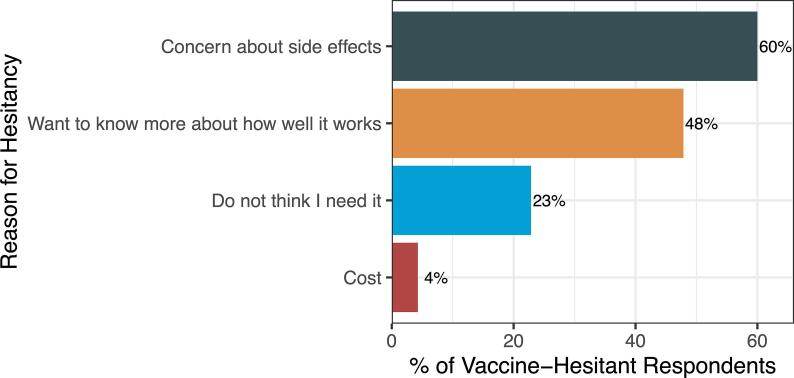
Between December 15, 2020 and April 30, 2021 we surveyed 509 jail residents about attitudes towarrd vaccination, trust in medical personnel, and sources of COVID-19 information (Table S1). This sample represented approximately one-fifth of the average daily jail population. Among survey respondents who did not intend to get a COVID-19 vaccine or who had already refused the vaccine (N = 140), leading reasons for hesitancy were concern about side effects (60%) and wanting more information about efficacy (48%), followed by not thinking they need it (23%) and cost (4%) (Fig. 1).
Fig. 1.
Reasons for vaccine hesitancy among survey respondents who did not intend to get a COVID-19 vaccine or who already refused the vaccine. Percentage of vaccine-hesitant participants (N = 140) who cite each reason.
We next assessed potential deterrents to vaccination among respondents who had not yet been offered a vaccine at the time of taking the survey, but who had a record of subsequent uptake or refusal through June 30, 2021 (N = 281). Among respondents who did not intend to get a vaccine, those who remained unvaccinated (“Consistent No”) cited side effects as a leading deterrent (52%), followed by suboptimal efficacy (31%) and the hypothetical need for an annual booster (31%). In comparison, those who ultimately got vaccinated (“No to Yes”) were more likely to cite suboptimal efficacy (43%) and cost (19%) as deterrents (Fig S2A). Among respondents who intended to get vaccinated, cost was also a leading potential deterrent (49%), but those who remained unvaccinated (“Yes to No”) were more likely than vaccinated individuals (“Consistent Yes”) to select all factors as potential deterrents (Fig S2B).
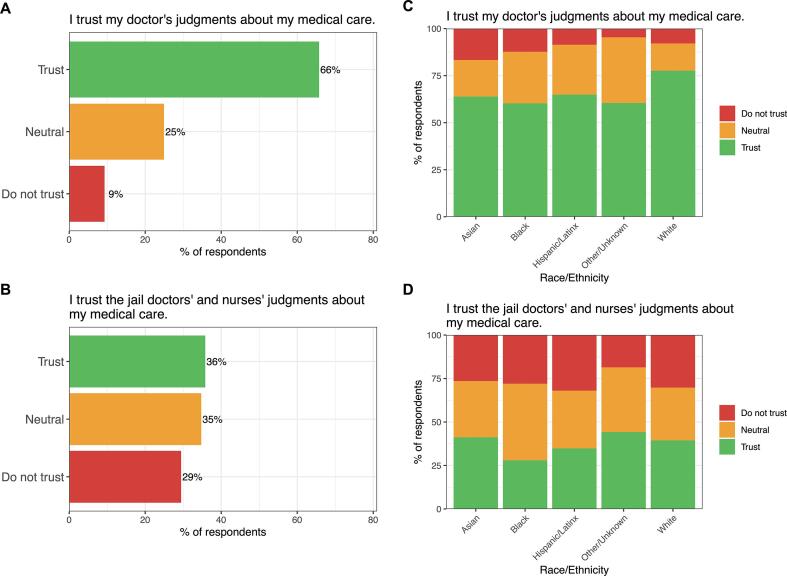
3.4. Medical mistrust
When considering their doctor outside of jail, 66% of survey participants reported trusting their doctor’s judgments about their medical care, whereas 25% and 9% reported feeling neutral or mistrustful, respectively (Fig. 2A). Trust in jail health staff was much lower, with 36%, 35%, and 29% of respondents who felt trustful, neutral, or mistrustful, respectively, toward jail health staff (Fig. 2B). Trust in medical personnel was highest among white respondents compared to Latinx or Black respondents (Fig. 2C-D).
Fig. 2.
Trust in one’s outside doctor and in jail health staff among survey respondents. Percentage of A) all respondents or C) respondents stratified by race/ethnicity who said they felt trustful, neutral, or distrustful toward their doctor outside of jail. Percentage of B) all respondents or D) respondents stratified by race/ethnicity who said they felt trustful, neutral, or distrustful toward jail health staff. Respondents who selected “Prefer not to answer” (N = 36 and 37 for trust in outside doctor and trust in jail health staff, respectively) were excluded from this analysis.
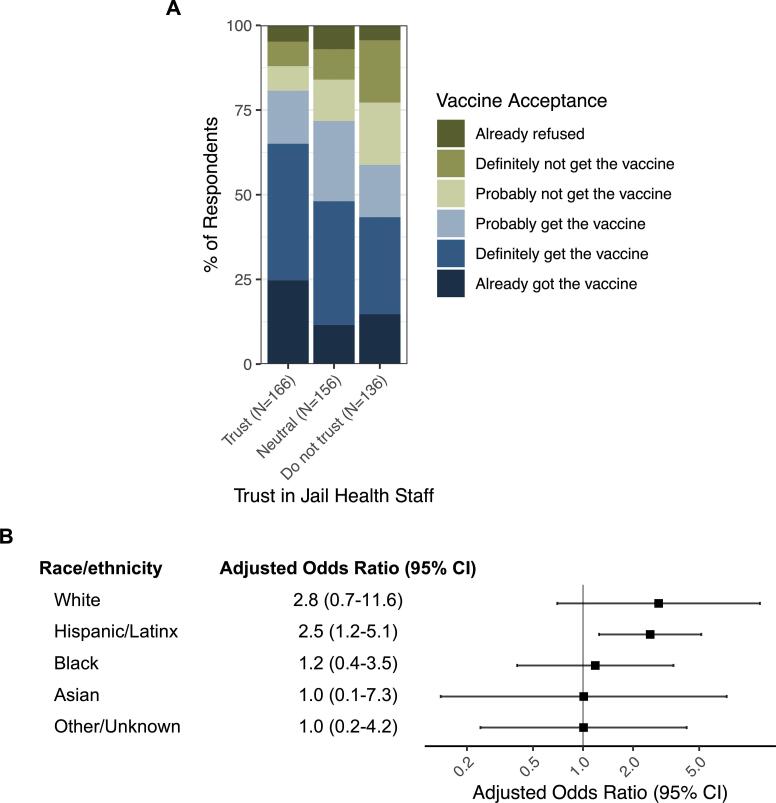
Trust in jail health staff was significantly associated with COVID-19 vaccine acceptance (p < 0.001), with 81%, 72%, and 59% acceptance among respondents who reported feeling trustful, neutral, or distrustful, respectively, toward jail health staff (Fig. 3A). However, this association was not generalizable across racial/ethnic groups. After adjusting for age, gender, and general trust, trust in jail health staff was associated with 2.8 (95% CI, 0.7–11.6) and 2.5 (95% CI, 1.2–5.1) times greater vaccine acceptance among white and Latinx participants, respectively, but had no effect on vaccine acceptance among participants of other races (Fig. 3B). Similar trends were found with trust in one’s outside doctor (Fig S3).
Fig. 3.
Association between trust in jail health staff and COVID-19 vaccine acceptance among survey respondents. A) Percentage of respondents, stratified by trust in jail health staff, who indicated vaccine acceptance (shades of blue) or hesitancy (shades of green). The difference in vaccine acceptance/hesitancy among different trust strata was statistically significant by the chi-square test of independence, with p-value < 0.001. B) Results of a multivariate logistic regression adjusted for age, gender, and general trust. The adjusted odds ratio reflects the increase in likelihood of vaccine acceptance among respondents in each racial/ethnic group who trust jail health staff. Respondents who selected “Prefer not to answer” for the vaccine and/or trust question (N = 51) were excluded from this analysis. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
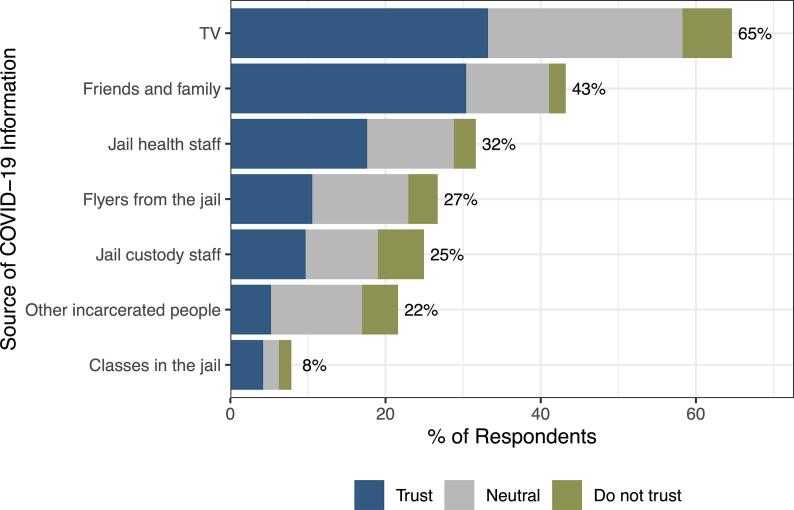
3.5. Vaccine acceptance and sources of COVID-19 information
Television was the leading source of COVID-19 information cited by 65% of survey respondents, followed by friends and family (43%) (Fig. 4). Vaccine-hesitant respondents were less likely to trust most sources of information but cited friends and family as the most trusted source (Fig S4).
Fig. 4.
Sources of information about COVID-19 and trust in each source among survey respondents. Percentage of respondents who report receiving information about COVID-19 from each source and who trust, do not trust, or are neutral toward each source.
4. Discussion
In this study, we found relatively low COVID-19 vaccine uptake among jail residents, despite many initially hesitant individuals who ultimately got vaccinated. Leading reasons for hesitancy, including among those who remained unvaccinated, were concerns about side effects and suboptimal efficacy. Vaccine hesitancy was also associated with medical mistrust, although this association varied substantially by race/ethnicity. Television and friends and family were leading sources of COVID-19 information, with friends and family being the most trusted source among vaccine-hesitant individuals. Collectively, our findings illuminate the factors underlying vaccine hesitancy among jail residents and reveal potential focus areas for future efforts to increase vaccine acceptance in this high-risk setting.
The vaccination trends by demographic characteristics in this study largely mirror those found in incarcerated and non-incarcerated populations in the US (Chin et al., 2021, Hagan et al., 2021, Mayo, 2021, Demographic Trends of People Receiving COVID-19, 2022). However, the 57% vaccine uptake rate among jail residents in this study is much lower than that observed among individuals 18 or older in the US (67%) and in the two counties studied (84–86%) as of June 30, 2021 (Centers for Disease Control and Prevention, 2021, Centers for Disease Control and Prevention CDC, 2021), demonstrating substantial vaccine hesitancy in this population that cannot be attributed solely to lack of access. Of note, we found even lower initial uptake that increased over time as some hesitant individuals decided to get vaccinated, although this trend was partly offset by others who had expressed interest during a prior screening but subsequently declined. These findings underscore the importance of continued vaccine offers and suggest that uptake may increase if vaccines were readily available at the time of screening. Not surprisingly, individuals with a history of recent flu vaccination were more likely to get vaccinated for COVID-19, confirming prior surveys (Aw et al., 2021, Ruiz and Bell, 2021, Funk, 2021) and suggesting that flu vaccination campaigns may indirectly affect COVID-19 vaccine acceptance.
Concerns surrounding side effects and efficacy were major reasons for hesitancy, reflecting findings from other studies in the US and abroad (Stern et al., 2020, Aw et al., 2021, Tyson et al., 2020, Solís Arce et al., 2021, Di Giuseppe et al., 2022). Although guidance for booster shots had not yet emerged during the study period, many respondents--especially vaccine hesitant respondents--indicated that needing an annual booster would be a deterrent to vaccination. Furthermore, although COVID-19 vaccines are currently free of charge in and out of custody, cost was cited as a reason for hesitancy among 4% of vaccine-hesitant respondents and was the leading hypothetical deterrent among vaccine-accepting respondents. These results highlight the need for the continuation of, and clearer information about, free access to vaccines. They also show that costs may be a significant barrier to seeking other medical and preventive care in custody (Awofeso, 2005, Hatton et al., 2006), and they provide support for policies eliminating medical co-payments in carceral facilities during COVID-19 and beyond (CDC. Interim Guidance on Management of Coronavirus Disease, 2019, Herring, 2022). Of note, California ended co-pays in custody in 2019; however, until such policies are permanent and universal across all states, clear communication of temporary changes is vital and should occur through accessible, varied, and trusted sources as identified by justice-involved populations. Whereas surveys among non-incarcerated individuals in the US and other countries identified health care workers or government websites as the most trusted sources of COVID-19 information (Solís Arce et al., 2021, Ali et al., 2020), participants of the present study, especially vaccine-hesitant individuals, cited family and friends as the most trusted source of COVID-19 information. This finding was notwithstanding declines in contact with loved ones due to pandemic restrictions on in-person visitation, suggesting that vaccine information campaigns outside of jail may reach and influence vaccine attitudes among incarcerated individuals.
Although it is often hypothesized that incarcerated individuals harbor mistrust of medical personnel and institutions, little research has directly assessed this mistrust or its association with vaccine acceptance (Stern et al., 2020, Vandergrift and Christopher, 2021, Peterson et al., 2019, Valera et al., 2018, Junewicz et al., 2017). In this study, trust in jail health staff was much lower than trust in one’s doctor outside of jail, although both were associated with higher vaccine acceptance. Notably, this association was absent among Black respondents, a surprising result given the frequently evoked link between lower COVID-19 vaccination rates and medical mistrust among Black Americans (Bajaj and Stanford, 2021, Thompson et al., 2021, Collaborative, 2020). However, our sample size of Black respondents was small (N = 77), and additional research is needed to validate this finding. Future research should also focus on identifying root causes of medical mistrust and evaluating interventions (individual, relational, and structural) to improve trust in this population, which may in turn improve vaccine uptake and other care-seeking.
To our knowledge, this is one of few studies to assess attitudes towards COVID-19 vaccination among incarcerated individuals, particularly among jail residents who represent a unique, understudied population. Compared to other studies in incarcerated populations that report only demographic characteristics associated with vaccine acceptance, we additionally examined reasons for hesitancy, association with medical trust, and sources of COVID-19 information. Our mixed methods also enabled us to examine deterrents to vaccination among those whose decision to get vaccinated changed over time.
This study has several limitations. First, our retrospective chart review was restricted to data on vaccination in custody and did not include data following release. For the association of housing type and vaccine uptake, we were unable to adjust for history of residence in other housing types due to lack of data access. The chart review also excluded individuals who were in custody for under 26 days; future research should examine vaccine acceptance among those who are frequently admitted and released from custody as they may represent a uniquely vulnerable group and may facilitate COVID-19 transmission between jails and the community (Reinhart and Chen, 2021). Regarding the survey, although we adapted the questions from prior research, we did not pilot them or the Spanish translations in the study population. The survey findings were limited by sample size and may not be representative of the entire jail population, as we were unable to track response rates or estimate potential bias (S2 Text). They are also subject to limitations of self-reported data. Furthermore, although both chart review and survey enrollment occurred across several months, we did not have sufficient power to examine effects of calendar time on vaccine acceptance, as shown elsewhere (Funk, 2021). While we attempted to infer factors underlying hesitancy and acceptance by linking survey responses with vaccination data, our understanding would be enhanced by more open-ended questions and qualitative data. Finally, these findings may have limited generalizability to other incarcerated and non-incarcerated populations in the US and globally, given high observed variation in vaccine acceptance across carceral facilities, regions, and countries (Aw et al., 2021, Berk et al., 2021, Sallam, 2021, Solís Arce et al., 2021, Hagan et al., 2021, Stern et al., 2020, Centers for Disease Control and Prevention CDC, 2021).
5. Conclusion
This study addresses persistent knowledge gaps surrounding COVID-19 vaccination among jail residents and highlights several actionable steps to increase vaccination rates in this population. First, custody health providers should continue regularly screening for interest in vaccination as acceptance may change over time. Vaccine information campaigns should focus on concerns about side effects and efficacy and clarify that the vaccine (and medical care during COVID-19, if applicable) is free of charge. Such information should be disseminated through accessible and trusted sources, including friends and family. Moreover, custody health should work to improve medical trust among residents, although future research is needed to identify the root causes of mistrust and effective interventions. Finally, given the high vaccine coverage needed in congregate settings and amidst new viral variants, efforts to increase vaccination rates should be carried out alongside other protective measures like masking, regular testing, and decarceration (Reinhart and Chen, 2021). Altogether, these measures can mitigate morbidity and mortality from COVID-19 and other vaccine-preventable infectious diseases in this high-risk setting.
6. Funding sources
Supported by the COVID-19 Emergency Response Fund from Stanford University, which was established with a gift from the Horowitz Family Foundation, and by the Clinical and Translational Science Award (#5UL1TR003142) from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS). The funders had no involvement in any aspect of the study.
CRediT authorship contribution statement
Yiran E. Liu: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. Jillian Oto: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. John Will: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. Christopher LeBoa: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. Alexis Doyle: Conceptualization, Methodology, Writing – review & editing. Neil Rens: Conceptualization, Methodology, Writing – review & editing. Shelley Aggarwal: Conceptualization, Supervision, Writing – review & editing. Iryna Kalish: Conceptualization, Data curation, Writing – review & editing. Marcela Rodriguez: Data curation, Project administration, Validation, Writing – review & editing. Beruk Sherif: Investigation, Validation, Writing – review & editing. Chrisele Trinidad: Investigation, Validation, Writing – review & editing. Michael Del Rosario: Investigation, Data curation, Project administration, Writing – review & editing. Sophie Allen: Conceptualization, Writing – review & editing. Robert Spencer: Conceptualization, Writing – review & editing. Carlos Morales: Conceptualization, Supervision, Writing – review & editing. Alexander Chyorny: Conceptualization, Project administration, Supervision, Writing – review & editing. Jason R Andrews: Conceptualization, Project administration, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interests
Jillian Oto, John Will, Shelley Aggarwal, Iryna Kalish, Michael Del Rosario, Robert Spencer, Carlos Morales, and Alexander Chyorny are employees and/or affiliates of Correctional/Custody Health Services in the county jail systems involved in this study.
All other authors declare no competing interests.
Acknowledgements
This work was supported by the COVID-19 Emergency Response Fund from Stanford University, which was established with a gift from the Horowitz Family Foundation, and by the Clinical and Translational Science Award (#5UL1TR003142) from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS). The funders had no involvement in any aspect of the study. We thank the members of our community advisory boards and focus groups for their critical input on how to make the study sensitive to and relevant for stakeholder populations. We thank Lisa Goldman-Rosas, Wei-ting Chen, Hector Romero, and Olivia Tigre for their guidance and support with the community engagement components of the study. We thank Melissa Wagner, Nicole Hayes, and Natalie Saavedra for providing access to data in San Mateo County.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101771.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Toblin R.L., Hagan L.M. COVID-19 case and mortality rates in the federal bureau of prisons. Am. J. Prev. Med. 2021;61(1):120–123. doi: 10.1016/j.amepre.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez N., Ward J.A., Parish K., Saloner B., Dolovich S. COVID-19 Incidence and Mortality in Federal and State Prisons Compared With the US Population, April 5 to April 3, 2021. JAMA. 2020;2021 doi: 10.1001/jama.2021.17575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhalter EC, Izzy; Derr, Brendon; Gamio, Lazaro; Griesbach, Rebecca; Hinga Klein, Ann; Issawi, Danya; Mensah, K.B.; Norman, Derek M.; Redl, Savannah; Reynolds, Chloe; Schwing, Emily; Seline, Libby; Sherman, Rachel; Turcotte, Maura; Williams, Timothy. Incarcerated and Infected: How the Virus Tore Through the U.S. Prison System. New York Times. 2021.
- Nowotny K.M., Bailey Z., Brinkley-Rubinstein L. The Contribution of Prisons and Jails to US Racial Disparities During COVID-19. Am. J. Public Health. 2021;111(2):197–199. doi: 10.2105/AJPH.2020.306040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adhikari S., Pantaleo N.P., Feldman J.M., Ogedegbe O., Thorpe L., Troxel A.B. Assessment of Community-Level Disparities in Coronavirus Disease 2019 (COVID-19) Infections and Deaths in Large US Metropolitan Areas. JAMA Network Open. 2020;3(7):e2016938. doi: 10.1001/jamanetworkopen.2020.16938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couloute L. Nowhere to Go: Homelessness among formerly incarcerated people. Prison Policy Initiative. 2018 [Google Scholar]
- Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L., McLeod L., Delacqua G., Delacqua F., et al. The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.S., Wendy Arrest, Release, Repeat: How police and jails are misused to respond to social problems. Prison Policy Initiative. 2019 [Google Scholar]
- Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol. Psychiatry. 2021;26(1):30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryckman T., Chin E.T., Prince L., Leidner D., Long E., Studdert D.M., Salomon J.A., Alarid-Escudero F., Andrews J.R., Goldhaber-Fiebert J.D. Outbreaks of COVID-19 variants in US prisons: a mathematical modelling analysis of vaccination and reopening policies. Lancet Public Health. 2021;6(10):e760–e770. doi: 10.1016/S2468-2667(21)00162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin E.T., Leidner D., Zhang Y., Long E., Prince L., Li Y., Andrews J.R., Studdert D.M., Goldhaber-Fiebert J.D., Salomon J.A. Effectiveness of the mRNA-1273 Vaccine during a SARS-CoV-2 Delta Outbreak in a Prison. N. Engl. J. Med. 2021;385(24):2300–2301. doi: 10.1056/NEJMc2114089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin E.T., Leidner D., Ryckman T., Liu Y.E., Prince L., Alarid-Escudero F., Andrews J.R., Salomon J.A., Goldhaber-Fiebert J.D., Studdert D.M. Covid-19 Vaccine Acceptance in California State Prisons. N. Engl. J. Med. 2021;385(4):374–376. doi: 10.1056/NEJMc2105282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan, L.M., Dusseau, C., Crockett, M., Rodriguez, T., Long, M.J. COVID-19 vaccination in the Federal Bureau of Prisons, December 2020-April 2021. Vaccine. 2021:S0264-410X(21)01078-1. doi: 10.1016/j.vaccine.2021.08.045. PubMed PMID: 34465473. [DOI] [PMC free article] [PubMed]
- Sawyer WW, Peter. Mass Incarceration: The Whole Pie 2020. Prison Policy Initiative: 2020.
- Kajeepeta S., Mauro P.M., Keyes K.M., El-Sayed A.M., Rutherford C.G., Prins S.J. Association between county jail incarceration and cause-specific county mortality in the USA, 1987–2017: a retrospective, longitudinal study. Lancet Public Health. 2021;6(4):e240–e248. doi: 10.1016/S2468-2667(20)30283-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhart, E., Chen, D.L., 2021. Carceral-community epidemiology, structural racism, and COVID-19 disparities. Proceedings of the National Academy of Sciences. 2021;118(21):e2026577118. doi: 10.1073/pnas.2026577118. [DOI] [PMC free article] [PubMed]
- James DJ. Selected characteristics of jail inmates, by conviction status, 2002 and 1996. In: Statistics BoJ, editor. 2004.
- Minton TDZ, Zhen; Maruschak, Laura M. Impact of COVID-19 on the Local Jail Population, January-June 2020. Bureau of Justice Statistics, 2021.
- COVID Prison Project. In: Lab UHaJR, editor. GitHub2021.
- Khorasani S.B., Koutoujian P.J., Zubiago J., Guardado R., Siddiqi K., Wurcel A.G. COVID-19 Vaccine Interest among Corrections Officers and People Who Are Incarcerated at Middlesex County Jail, Massachusetts. J. Urban Health. 2021;98(4):459–463. doi: 10.1007/s11524-021-00545-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, M.F., Piasecki, A.M., Strick, L.B., Rajeshwar, P., Tyagi, E., Dolovich, S., et al., 2020. Willingness to Receive a COVID-19 Vaccination Among Incarcerated or Detained Persons in Correctional and Detention Facilities - Four States, September-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(13):473-7. Epub 2021/04/02. doi: 10.15585/mmwr.mm7013a3. [DOI] [PMC free article] [PubMed]
- Berk J., Murphy M., Kane K., Chan P., Rich J., Brinkley-Rubinstein L. Initial SARS-CoV-2 Vaccination Uptake in a Correctional Setting: Cross-sectional Study. JMIRx Med. 2021;2(3) doi: 10.2196/30176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komarla ACI-CP. COVID-19 vaccination data in California jails: lessons from an imperfect model 2021.
- Aw J., Seng J.J.B., Seah S.S.Y., Low L.L. COVID-19 Vaccine Hesitancy—A Scoping Review of Literature in High-Income Countries. Vaccines. 2021;9(8):900. doi: 10.3390/vaccines9080900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson H.S., Manning M., Mitchell J., Kim S., Harper F.W.K., Cresswell S., Johns K., Pal S., Dowe B., Tariq M., Sayed N., Saigh L.M., Rutledge L., Lipscomb C., Lilly J.Y., Gustine H., Sanders A., Landry M., Marks B. Factors Associated With Racial/Ethnic Group-Based Medical Mistrust and Perspectives on COVID-19 Vaccine Trial Participation and Vaccine Uptake in the US. JAMA Network Open. 2021;4(5):e2111629. doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., Kriner D.L. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Network Open. 2020;3(10):e2025594. doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz, J.B., Bell, R.A., 2021. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080-6. Epub 2021/01/20. doi: 10.1016/j.vaccine.2021.01.010. PubMed PMID: 33461833; PubMed Central PMCID: PMCPMC7794597. [DOI] [PMC free article] [PubMed]
- Madeddu G., Vroling H., Oordt-Speets A., Babudieri S., O'Moore Éamonn, Noordegraaf M.V., Monarca R., Lopalco P.L., Hedrich D., Tavoschi L. Vaccinations in prison settings: A systematic review to assess the situation in EU/EEA countries and in other high income countries. Vaccine. 2019;37(35):4906–4919. doi: 10.1016/j.vaccine.2019.07.014. [DOI] [PubMed] [Google Scholar]
- Vandergrift L.A., Christopher P.P. Do prisoners trust the healthcare system? Health Justice. 2021;9(1) doi: 10.1186/s40352-021-00141-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention; 2021. COVID-19 Vaccinations in the United States,County. In: (NCIRD).
- Centers for Disease Control and Prevention (CDC), 2021. COVID-19 Vaccinations in the United States, Jurisdiction. In: (NCIRD).
- Tyson AJ, Courtney; Funk, Cary. U.S. Public Now Divided Over Whether To Get COVID-19 Vaccine2020 11/8/21. Available from: https://www.pewresearch.org/science/2020/09/17/u-s-public-now-divided-over-whether-to-get-covid-19-vaccine/.
- Alsan MG, Owen; Graziani, Grant C. Does Diversity Matter for Health? Experimental Evidence from Oakland. National Bureau of Economic Research Working Paper Series. 2018.
- Sharma, A., Minh Duc, N.T., Luu Lam Thang, T., Nam, N.H., Ng, S.J., Abbas, K.S., et al., 2021. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med. 2021;36(10):3179-87. Epub 2021/04/23. doi: 10.1007/s11606-021-06737-1. PubMed PMID: 33886027; PubMed Central PMCID: PMCPMC8481359. [DOI] [PMC free article] [PubMed]
- Solís Arce J.S., Warren S.S., Meriggi Niccolò.F., Scacco A., McMurry N., Voors M., Syunyaev G., Malik A.A., Aboutajdine S., Adeojo O., Anigo D., Armand A., Asad S., Atyera M., Augsburg B., Awasthi M., Ayesiga G.E., Bancalari A., Björkman Nyqvist M., Borisova E., Bosancianu C.M., Cabra García M.R., Cheema A., Collins E., Cuccaro F., Farooqi A.Z., Fatima T., Fracchia M., Galindo Soria M.L., Guariso A., Hasanain A., Jaramillo S., Kallon S., Kamwesigye A., Kharel A., Kreps S., Levine M., Littman R., Malik M., Manirabaruta G., Mfura J.Léodomir.H., Momoh F., Mucauque A., Mussa I., Nsabimana J.A., Obara I., Otálora María.J., Ouédraogo Béchir.W., Pare T.B., Platas M.R., Polanco L., Qureshi J.A., Raheem M., Ramakrishna V., Rendrá I., Shah T., Shaked S.E., Shapiro J.N., Svensson J., Tariq A., Tchibozo A.M., Tiwana H.A., Trivedi B., Vernot C., Vicente P.C., Weissinger L.B., Zafar B., Zhang B., Karlan D., Callen M., Teachout M., Humphreys M., Mobarak A.M., Omer S.B. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021;27(8):1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. PubMed PMID: 33669441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Peduzzi P., Concato J., Kemper E., Holford T.R., Feinstein A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996;49(12):1373–1379. doi: 10.1016/S0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- Mayo Clinic. U.S. COVID-19 vaccine tracker: See your state’s progress2021 11/8/21. Available from: https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker.
- Demographic Trends of People Receiving COVID-19 Vaccinations in the United States. In: (NCIRD) NCfIaRD, editor.: Centers for Disease Control and Prevention; 2022.
- Funk CT, Alec. Growing Share of Americans Say They Plan To Get a COVID-19 Vaccine – or Already Have2021 11/8/21. Available from: https://www.pewresearch.org/science/2021/03/05/growing-share-of-americans-say-they-plan-to-get-a-covid-19-vaccine-or-already-have/.
- Di Giuseppe G., Pelullo C.P., Lanzano R., Napolitano F., Pavia M. Knowledge, attitudes, and behavior of incarcerated people regarding COVID-19 and related vaccination: a survey in Italy. Sci. Rep. 2022;12(1):960. doi: 10.1038/s41598-022-04919-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awofeso N. Prisoner healthcare co-payment policy: a cost-cutting measure that might threaten inmates' health. Appl Health Econ Health Policy. 2005;4(3):159-64. Epub 2005/11/29. doi: 10.2165/00148365-200504030-00004. PubMed PMID: 16309333. [DOI] [PubMed]
- Hatton DC, Kleffel D, Fisher AA. Prisoners' perspectives of health problems and healthcare in a US women's jail. Women Health. 2006;44(1):119-36. Epub 2006/12/22. doi: 10.1300/J013v44n01_07. PubMed PMID: 17182530. [DOI] [PubMed]
- CDC. Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities2021 October 11, 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/correction-detention/guidance-correctional-detention.html.
- Herring T. COVID looks like it may stay. That means prison medical copays must go. Prison Policy Initiative: 2022.
- Ali S.H., Foreman J., Tozan Y., Capasso A., Jones A.M., DiClemente R.J. Trends and Predictors of COVID-19 Information Sources and Their Relationship With Knowledge and Beliefs Related to the Pandemic: Nationwide Cross-Sectional Study. JMIR Public Health Surveill. 2020;6(4) doi: 10.2196/21071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson, M., Nowotny, K., Dauria, E., Arnold, T., Brinkley-Rubinstein, L., 2019. Institutional distrust among gay, bisexual, and other men who have sex with men as a barrier to accessing pre-exposure prophylaxis (PrEP). AIDS Care. 2019;31(3):364-9. Epub 2018/09/20. doi: 10.1080/09540121.2018.1524114. PubMed PMID: 30227719. [DOI] [PMC free article] [PubMed]
- Valera, P., Boyas, J.F., Bernal, C., Chiongbian, V.B., Chang, Y., Shelton, R.C., 2018. A Validation of the Group-Based Medical Mistrust Scale in Formerly Incarcerated Black and Latino Men. Am J Mens Health. 2018;12(4):844-50. Epub 2016/05/19. doi: 10.1177/1557988316645152. PubMed PMID: 27192716; PubMed Central PMCID: PMCPMC6131472. [DOI] [PMC free article] [PubMed]
- Junewicz A., Kleinert K.J., Dubler N.N., Caplan A. Victimization and Vulnerability: A Study of Incarceration, Interpersonal Trauma, and Patient-Physician Trust. Psychiatr. Q. 2017;88(3):459–472. doi: 10.1007/s11126-016-9463-x. [DOI] [PubMed] [Google Scholar]
- Bajaj S.S., Stanford F.C. Beyond Tuskegee — Vaccine Distrust and Everyday Racism. N. Engl. J. Med. 2021;384(5):e12. doi: 10.1056/NEJMpv2035827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID Collaborative LR, ; UnidosUS, ; NAACP, . Coronavirus Vaccine Hesitancy in Black and Latinx Communities. 2020.
- Reinhart E., Chen D.L. Association of Jail Decarceration and Anticontagion Policies With COVID-19 Case Growth Rates in US Counties. JAMA Network Open. 2021;4(9):e2123405. doi: 10.1001/jamanetworkopen.2021.23405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.