Abstract
Introduction
Childhood exposure to neighborhood firearm violence adversely affects mental and physical health across the life course. Study objectives were to (1) quantify racial disparities in these exposures across the U.S. and (2) assess changes during the COVID-19 pandemic, when firearm violence increased.
Methods
The study used counts of children aged 5–17 years, disaggregated by U.S. Census racial category, for every census tract (N=73,056). Neighborhood firearm violence was the number of fatal shootings per census tract, based on 2015–2021 Gun Violence Archive data. Quasi-Poisson regressions were used to estimate baseline disparities and COVID-19‒related changes and examined differences across geographic regions.
Results
Prepandemic exposure was lowest among White children and highest among Black children, who experienced 4.44 times more neighborhood firearm violence exposure (95% CI=4.33, 4.56, p<0.001) than White children. The pandemic increased exposure by 27% in the lowest risk group (i.e., White children; 95% CI=20%, 34%, p<0.001), but pandemic effects were even greater for children in nearly all non-White categories. Baseline violence levels and racial disparities varied considerably by region, with the highest levels in the South and the largest magnitude disparities observed in the Northeast and Midwest.
Conclusions
Large-scale racial disparities exist in child exposure to neighborhood firearm violence, and these disparities grew during the pandemic. Equitable access to trauma-informed programs, community-based prevention, and structural reforms are urgently needed.
INTRODUCTION
Firearm violence persists in the U.S. as a public health crisis. Tragically, firearm injury is now the leading cause of death among children and teens.1 The epidemic of firearm violence affects children through multiple pathways. These pathways include direct exposure (i.e., being killed, injured, or threatened with a firearm) and indirect exposure (e.g., witnessing firearm violence, hearing gunshots, living in a community where violence is common, losing a friend or family member to firearm injury).2
Each type of firearm violence exposure can contribute to adverse child outcomes. Children exposed to firearm violence, whether directly or indirectly, may experience adverse short-term and long-term psychological effects,3 including post-traumatic stress disorder.2 These effects of trauma carry over into student learning outcomes, physical health, and emotional well-being.4 Children exposed to firearm violence in their neighborhood experience greater difficulty with concentration, experience overall reduced performance in school,5 and spend less time playing and being physically active owing to neighborhood safety concerns.6 In addition, exposure to community violence can manifest as collective feelings of hopelessness, disorganized social networks, and altered social norms that can promote further violence.7
The rates of childhood firearm violence exposure vary by exposure type and across racial groups. More than 17,000 children are shot every year.2 A total of 41% of children in a nationally representative sample reported having recently seen or heard firearm violence occur, and 8% had a friend or family member who died by firearm homicide.8 These exposures disproportionately burden children of color, especially Black children.9 , 10 A study of fifth graders in 3 U.S. cities found that the rate of witnessing a threat of injury with a firearm in the past year was 20% for Black youth, 11% for Latinx youth, and 5% for White youth.11 These racial disparities in exposure further reinforce the disparities in other adverse child outcomes.7 , 9
Understanding racial disparities in childhood exposure to neighborhood firearm violence—and thus children's opportunities for healthy development—is critical to informed policy responses, particularly amid the coronavirus disease 2019 (COVID-19) pandemic. Firearm violence has spiked since the beginning of the pandemic.12, 13, 14, 15 However, few researchers have documented the impacts of this spike specifically on childhood violence exposures and racial disparities.16 Moreover, the extent to which these outcomes vary across U.S. regions is poorly understood, posing a barrier to informed policy-making.
This study examines the racial disparities in childhood exposure to firearm violence before and during the COVID-19 pandemic, leveraging timely, national data on firearm violence incidence to generate analyses for every census tract in the U.S. To inform programming, policy making, and data collection, analyses estimate (1) the magnitude of racial disparities in how many firearm homicides occurred within each child's neighborhood of residence, (2) changes in racial disparities during the COVID-19 pandemic, and (3) the extent to which these disparities varied between geographic regions.
METHODS
Exposure to firearm violence was measured on the basis of the number of firearm homicide incidents that occurred in a child's census tract of residence. In this study, this outcome is referred to as neighborhood exposure to firearm violence. Although some exposure to violence occurs outside a child's home neighborhood, a majority occurs within the home neighborhood,17 and home neighborhood exposures are associated with childhood outcomes.3 , 5 This neighborhood effects approach treats monitoring of neighborhood firearm violence as akin to monitoring the presence of other neighborhood-level determinants of health, such as air and water quality and healthy food access, for example. From this social ecologic standpoint, racial health disparities emerge from the differences in social context that U.S. society allocates inequitably according to racial status.18
Study Sample
The study team obtained firearm injury data from March 2015 through March 2021 from the Gun Violence Archive (GVA), a nonprofit organization that tracks shootings across the U.S. using media reports and other public sources.19 GVA staff manually verify each record and extract basic characteristics, including the date, location, and the number of persons injured or killed. GVA data were used rather than government sources because there is currently no government source that provides firearm violence data at the spatial granularity required (i.e., neighborhood level) on a national scale.20 GVA, by comparison, provides the street block location of each incident. An additional advantage of GVA data is timeliness, compared with that of government data sources with lags that approach 1 year.20 For similar reasons, previous studies have used GVA data to study neighborhood effects10 , 21 , 22 and COVID-19 effects12 on firearm violence.
Measures
Only GVA data on fatal shootings were used, even though GVA data contain both fatal and nonfatal shootings. GVA captures fatal shootings with good accuracy: 83% of fatal shootings from 3 cities were accurately represented in GVA data on date, location, and victim age and gender23; in 2018, GVA under-reported fatal shootings by just 2%, compared with government counts.13 By contrast, GVA only matched 43% of nonfatal shooting incidents in the 3-city study, and no government source exists for nonfatal shootings, leaving important questions about GVA accuracy for nonfatal shootings.
Population data were obtained from the 2015–2019 American Community Survey of the U.S. Census, specifically the estimated count of children aged 5–17 years for 8 racial categories: Black, American Indian and Alaska Native (referred to as Native American in the remaining part of this paper), Asian, Native Hawaiian/Pacific Islander, Hispanic, White, ≥2 races, and some other race, a category assigned when a respondent manually enters a different category. These categories were mutually exclusive, meaning that any individual identified to be of Hispanic ethnicity was counted as Hispanic. Asian and Native Hawaiian and Other Pacific Islander categories were combined as Asian Pacific Islander, generating 7 categories for analysis. Census data on children aged <5 years were omitted because including this category would have added infants and very young children whose experiences of neighborhood violence would likely differ from those of older children. Sensitivity analyses including this age group produced similar results.
Statistical Analysis
The research team geocoded each incident using the GVA-supplied location (e.g., 1,000 Block of Main Street, Boston, MA) and matched locations to the full set of U.S. census tracts (N=73,056). Census tracts were used as proxies for neighborhoods to measure children's exposure to neighborhood firearm homicide, consistent with previous studies of neighborhood effects on firearm violence,21 , 24 , 25 including the finding by Sharkey (2010)5 that homicide occurrence in a child's census tract measurably diminishes academic test performance.
For each census tract and time period, outcomes were the number of incidents involving ≥1 firearm fatalities. This outcome variable was constructed to incorporate the cumulative effects of multiple exposures to violence,4 while assuming that effects on children would not necessarily increase along with the number of victims in a particular incident.
Time periods were pandemic years beginning on March 15 of each calendar year and ending on March 14 of the following calendar year. These time periods were devised to facilitate comparisons with the first 365 days in which the COVID-19 pandemic altered daily life in the U.S. Analyses using smartphone mobility data have shown that daily activity patterns changed starkly in mid-March 2020.26 This pandemic-year approach enabled comparisons of the first 12 months of the COVID-19 pandemic with earlier time periods, without separate adjustments for seasonal trends in firearm violence. There were 6 time periods (pandemic years 2015–2020), including the first year of COVID-19 in the U.S. The analytical data set was constructed to include 1 row per year, tract, and racial group. To describe the magnitude of exposure to neighborhood firearm violence in absolute terms, mean yearly counts of fatal shootings per census tract were calculated, weighted by the number of children from each racial category, for the prepandemic and pandemic periods.
All subsequent analyses were focused on estimating and explaining the racial disparities in neighborhood firearm violence exposure rates. Study models analyzed fatal shootings as a function of child racial composition. Quasi-Poisson regression was used because of moderate overdispersion in the firearm violence outcomes. These models were weighted by race-specific population count for each census tract to estimate disparities at the U.S. population level.27 On the basis of published work, the lowest exposure rates were expected among White children,4 , 11 and this category was used as the reference group. Fixed effects were included for each racial category (except White, the reference group) and an interaction term with the COVID-19 pandemic-year indicator to estimate the effects of the pandemic and any changes in racial disparities associated with the pandemic. For interaction terms, this approach estimates a multiplicative effect—the interpretation of this effect is explained further in Results.
Standard errors were clustered by pandemic year and census tract to address possible intraclass correlation across each unit of analysis.28 In subsequent models, the main model was stratified by geographic region to determine whether the national trends were consistent across spatial contexts. Race-specific exposures and disparities by state were mapped for additional granularity.
All analyses were performed in R, version 3.6.1, using the sf package for spatial analyses and the fixest package for regression models. The Boston University Medical IRB waived review as nonhuman subjects research because all data were publicly available and deidentified.
RESULTS
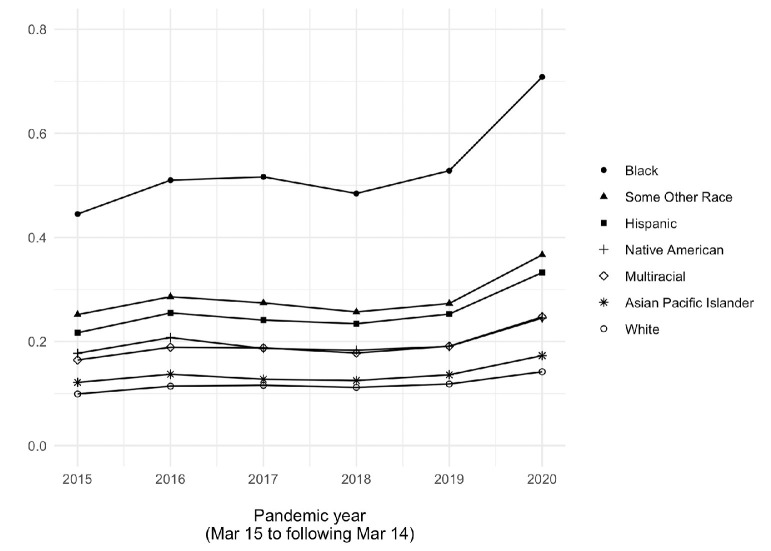
The population sample comprised approximately 58,350,000 children aged 5–17 years. Non-Hispanic White (referred to as White in the remaining part of the paper) children represented the single largest population group (46.9%), followed by Hispanic (22.9%) and Black (12.9%) children (Table 1 ). In an average prepandemic year, 9,063,000 children were exposed to ≥1 firearm fatality. In the first pandemic year, 11,121,000 children were exposed (difference=2,058,000) (Table 1). Before the pandemic, White children experienced the lowest exposure to neighborhood firearm violence (mean=0.11 incidents/year), whereas Black children averaged the highest exposure (mean=0.50 incidents/year) (Table 1). Rates of exposure and between-group differences in exposure were relatively stable from 2015 to 2019 (Figure 1 ). During the pandemic year 2020, mean exposure rates increased for every racial group, including for Black children, whose mean exposure increased to 0.71 incidents/year (Table 1).
Table 1.
Sample Characteristics
| Variables | Total population (thousands) | Share of total (%) | By census tract |
N exposed to 1 or more incidents (thousands) |
Exposures per year |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean |
Disparity versus White (rate ratio) |
||||||||||
| Mean | SD | 2015‒2019 (mean) | 2020 | 2015‒2019 | 2020 | 2015‒2019 | 2020 | Change (%) | |||
| Asian Pacific Islander | 2,708 | 4.6 | 37 | 99 | 289 | 363 | 0.13 | 0.17 | 1.18 | 1.21 | 2.8 |
| Black | 7,545 | 12.9 | 103 | 194 | 2,378 | 2,902 | 0.50 | 0.71 | 4.55 | 5.07 | 11.6 |
| Hispanic | 13,350 | 22.9 | 183 | 303 | 2,476 | 3,083 | 0.24 | 0.33 | 2.18 | 2.36 | 8.0 |
| Native American | 549 | 0.9 | 8 | 47 | 82 | 94 | 0.19 | 0.25 | 1.73 | 1.79 | 3.4 |
| 2 or more races | 3,358 | 5.8 | 46 | 66 | 483 | 600 | 0.18 | 0.25 | 1.64 | 1.79 | 9.1 |
| Some other race | 3,471 | 6.0 | 48 | 112 | 703 | 854 | 0.27 | 0.37 | 2.45 | 2.64 | 7.7 |
| White | 27,369 | 46.9 | 375 | 371 | 2,653 | 3,226 | 0.11 | 0.14 | — | — | — |
| Total | 58,350 | 100.0 | 114 | 237 | 9,063 | 11,121 | 0.21 | 0.28 | — | — | — |
Note: Mean exposures per year is the population-weighted mean count of firearm violence incidents involving at least 1 fatality. Time periods are not calendar years but rather years starting on March 15 and ending on March 14 to correspond with the first 365 days of major societal disruption associated with the COVID-19 pandemic. Demographic data are based on the 2015‒2019 American Community Survey. Some other race is a U.S. Census‒designated category for individuals who provide a response not otherwise listed on the Census form.
Figure 1.
Mean annual firearm homicide incidents in home census tract, by child's race.
Note: Outcomes are incidents involving at least 1 firearm homicide. Time periods are pandemic years, starting on March 15 of the year listed and ending on March 14 of the following calendar year. These time periods correspond to the first 12 months during which the COVID-19 pandemic disrupted most routine activities in most U.S. geographies.27 Racial categories are mutually exclusive, using U.S. Census-designated racial categories, except for Asian Pacific Islander, which combines Asian and Native Hawaiian and Pacific Islander categories.
In the national model, every other racial category experienced greater prepandemic exposure than White children (Table 2 ). The incident rate ratio for Black children was largest (4.44, 95% CI=4.33, 4.56, p<0.001) than that for White children, followed by those of some other race (2.40, 95% CI=2.29, 2.51, p<0.001) and Hispanic (2.15, 95% CI=2.08, 2.22, p<0.001). Disparities for Asian Pacific Islander children were the lowest but nontrivial and statistically significant in this model (1.16, 95% CI=1.10, 1.22, p<0.001).
Table 2.
Results of Quasi-Poisson Regression Estimating the Comparative Risk of Exposure to Neighborhood Firearm Violence
| Variables | Incident rate ratio (95% CI) |
||||
|---|---|---|---|---|---|
| Entire U.S. | Northeast | Midwest | South | West | |
| Asian Pacific Islander | 1.16***(1.10, 1.22) | 1.36***(1.19, 1.55) | 1.55*** (1.39, 1.73) | 1.08(0.98, 1.19) | 1.18***(1.12, 1.23) |
| Black | 4.44*** (4.33, 4.56) | 7.03*** (6.36, 7.78) | 7.69*** (7.17, 8.24) | 3.12*** (3.00, 3.23) | 2.61*** (2.41, 2.82) |
| Hispanic | 2.15*** (2.08, 2.22) | 3.95*** (3.60, 4.34) | 3.02*** (2.77, 3.29) | 1.56*** (1.48, 1.65) | 2.13*** (2.03, 2.24) |
| Native American | 1.69*** (1.56, 1.83) | 3.07*** (2.58, 3.66) | 1.60*** (1.42, 1.81) | 1.50*** (1.30, 1.73) | 1.61*** (1.40, 1.84) |
| Two or more races | 1.63*** (1.59, 1.66) | 2.55*** (2.37, 2.74) | 2.23*** (2.12, 2.35) | 1.41*** (1.37, 1.45) | 1.40*** (1.33, 1.47) |
| Some other race | 2.40*** (2.29, 2.51) | 4.57*** (4.07, 5.14) | 3.83*** (3.43, 4.28) | 1.79*** (1.71, 1.88) | 2.35*** (2.19, 2.53) |
| COVID-19 | 1.27***a(1.20, 1.34) | 1.19*** (1.12, 1.27) | 1.32*** (1.25, 1.40) | 1.25*** (1.16, 1.34) | 1.30*** (1.23, 1.37) |
| Asian Pacific Islander* COVID-19 | 1.05*** (1.02, 1.09) | 1.22*** (1.11, 1.34) | 1.18*** (1.10, 1.26) | 1.06** (1.02, 1.11) | 0.96*** (0.93, 0.98) |
| Black* COVID-19 | 1.12*** (1.12, 1.13) | 1.32*** (1.24, 1.42) | 1.10*** (1.06, 1.13) | 1.11*** (1.09, 1.13) | 1.12*** (1.06, 1.17) |
| Hispanic* COVID-19 | 1.09*** (1.07, 1.11) | 1.15*** (1.10, 1.20) | 1.08*** (1.03, 1.13) | 1.12*** (1.07, 1.17) | 1.05*** (1.02, 1.08) |
| Native American* COVID-19 | 1.02(0.99, 1.06) | 1.25*** (1.21, 1.28) | 1.10** (1.02, 1.19) | 0.98(0.89, 1.07) | 1.00(0.96, 1.05) |
| 2 or more races* COVID-19 | 1.07***(1.06, 1.08) | 1.23*** (1.19, 1.28) | 1.11*** (1.08, 1.14) | 1.09*** (1.08, 1.10) | 0.96* (0.93, 0.99) |
| Some other race* COVID-19 | 1.08*** (1.04, 1.11) | 1.14*** (1.07, 1.21) | 1.12*** (1.08, 1.17) | 1.12*** (1.09, 1.16) | 1.01(0.96, 1.06) |
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001).
Model is a Quasi-Poisson regression with SEs clustered by time step and census tract. Some other race is a U.S. Census‒designated category for individuals who provide a response not otherwise listed on the Census form.
The COVID-19 pandemic was associated with 1.27 times greater exposure in the reference group (i.e., White children; 95% CI=1.20, 1.34, p<0.001, Model 2) (Table 2). For every racial category except 1 (Native American children), COVID-19 was associated with a larger magnitude increase in exposure. In other words, the pandemic increased the estimated disparity between non-White and White children. The largest estimated pandemic-related increase was for Black children, for whom the estimated COVID-19 effect was 1.12 times greater than for White children (95% CI=1.12, 1.13, p<0.001). This effect was multiplicative, meaning that Black children's exposure rates during COVID-19 were the product of the higher baseline rate observed in Model 1, multiplied by a COVID-19 effect that was 1.12 times larger than the COVID-19 effect applied to White children (i.e., approximately 1.42 times Black children's baseline rates).
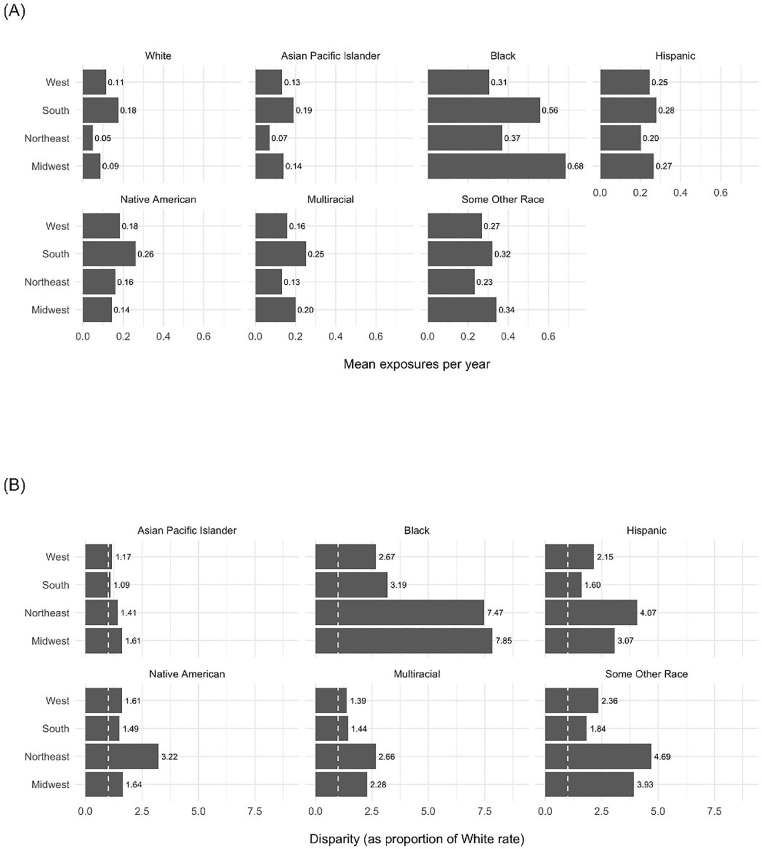
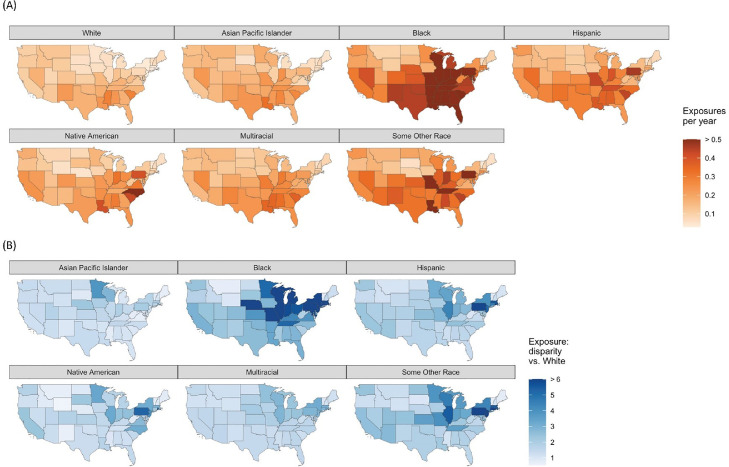
These national trends contained substantial regional variation. The South displayed the highest overall rates of exposure, but the Northeast and Midwest displayed the largest racial disparities (Figure 2 ). Virtually every non-White group exhibited prepandemic disparities in every region, but wide variation was observed: for example, Black–White disparities ranged from 2.61 (95% CI=2.41, 2.82, p<0.001) in the West to 7.69 (95% CI=7.17, 8.24, p<0.001) in the Midwest (Table 2). Overall COVID-19‒related changes were similar across all regions, but race-specific effects varied: for example, for Asian children, COVID-19 was associated with 1.22 times (95% CI=1.11, 1.34, p<0.001) increased disparity in the Northeast but slightly reduced disparity in the West (incidence rate ratio=0.96, 95% CI=0.93, 0.98, p<0.001). Maps of state-level exposures and disparities highlight more granular trends, such as an East–West band of high Black–White disparities coinciding approximately with the Rust Belt (Figure 3 ).
Figure 2.
Regional differences in (A) rates of exposure; (B) racial disparities compared with the White group.
Note: Data includes a full study time period (March 15, 2015‒March 14, 2021). The dashed line in Panel B is set to 1, interpreted as subgroup rate=White rate.
Figure 3.
State-level differences in (A) rates of exposure; (B) racial disparities compared with the White group.
Note: Data includes a full study time period (March 15, 2015‒March 14, 2021). Top values on each color scale correspond to approximate 95th percentile.
DISCUSSION
Children of all non-White racial groups experienced higher levels of exposure to neighborhood firearm violence than White children, and these disparities grew during the COVID-19 pandemic. Black children experienced the highest prepandemic levels of exposure and the largest increase in exposure to firearm violence during the pandemic. The analysis also identified important differences between regions. These findings are consistent with those of previous work showing that children of color experience higher rates of violence exposure than White children.9 , 11
This study is the first to estimate racial disparities in child firearm violence exposure using data from every U.S. neighborhood and one of the few studies to document the sharp increase in firearm violence during the COVID-19 pandemic.12 , 14 The analysis quantifies the disparities affecting children under-represented in previous studies, including Asian Pacific Islander, Native American, and multiracial children. The finding of large disparities affecting children identified to be of some other race by the U.S. Census highlights the social marginalization of these individuals and the need for data collection that properly disambiguates among the racial identities that tend to occupy this category, including Arab and other Middle Eastern and North African identities as well as Hispanic subgroups who identify with specific countries of ancestry.29 Even aggregation by Asian race may mask the disparities affecting children within subgroups (e.g., those of Hmong, Filipino, and Vietnamese descent30) and across geographies—these should be disaggregated in future work.
A sizable increase in firearm violence exposure during the pandemic has the potential to reverberate across health and educational outcomes over the life course. Researchers studying the health disparities that arise from natural disasters have noted that long-term access to integrated social services is key.31 Schools have been the most common sites for identification of children affected by violence and—with sufficient resources and support—can provide opportunities for establishing sustainable interventions.32 Access to evidence-based after-school programming also shows promise.33 Other approaches include psychological first aid, a strategy used in the immediate aftermath of a traumatic event to mitigate the impact of exposure to gun violence through healthy coping mechanisms and increased resiliency.34
Moreover, racially disparate exposure to firearm violence requires structural solutions focused on preventing violence. Person-focused strategies include community violence intervention, an approach in which credible messengers mediate disputes and connect individuals with social services.35 Place-based strategies, such as greening vacant lots36 and demolishing abandoned buildings,37 , 38 can address the impacts of physical deterioration and disinvestment that have disproportionately affected communities of color.
Little previous work39 has documented the considerable variation in racial disparities in childhood violence exposure found across U.S. regions. Although overall rates of neighborhood firearm violence exposure are highest in the South, racial disparities are substantially larger in the Northeast and Midwest. Residential racial segregation is one possible explanation. Institutional discrimination against Black Americans moving from the South during the 20th century contributed to high levels of segregation in Midwestern and Northeastern cities,40 including the Rust Belt, where the largest disparities were found. Distinctive exposure patterns by race and geography suggest a need for focused and culturally appropriate intervention as well as reversing disinvestment in the most segregated contexts.
Limitations
Some limitations of this work should be considered when interpreting these findings. Census tract–level counts of children by race were based on U.S. Census estimates that include nontrivial margins of error. Because 5-year counts were used, children moving neighborhoods or larger-scale shifts in demographics were not observed.
Unlike many previous studies in this area, children's experiences of violence (e.g., hearing gunshots or witnessing assaults) were not measured. Instead, the incidence of firearm homicide in a child's home neighborhood was measured. This measure is potentially overinclusive of direct experiences because it includes events that a given child might be unaware of and underinclusive because it omits experiences of violence that occur outside the home neighborhood. This methodologic choice limits the ability to draw conclusions about the mental and physical health implications of the measured exposures. This limitation points toward the importance of large-scale surveillance of these experiences using surveys and other methods.
However, direct measures are not necessary to anticipate serious adverse consequences from neighborhood violence exposure. Children are often highly sensitive to neighborhood safety threats, even at young ages,6 , 41 and researchers have found adverse effects on children only on the basis of information about where violence occurred, without directly observing whether children were aware of it.5 , 42 Moreover, firearm violence can affect children's lives without their directly experiencing it: for example, caregivers may curtail children's time outside the home to protect them from threats perceived by adults.41 Firearm violence also hinders economic development and is often met with aggressive policing,24 with important implications for the social and physical environment where children develop.
Finally, GVA is not a government data source, and previous work has identified gaps in the incidents that appear in GVA.23 Therefore, GVA data on nonfatal shootings, the type that displayed large gaps, were omitted. As a consequence, this study only measured a subset of exposures to firearm violence. In previous work, fatal shootings matched government records at higher rates (83%)23 and closely aligned with aggregated government data.13 It is unknown whether GVA data on fatal shootings display systematic bias (e.g., by victim's race), but if they did, this study would likely underestimate the disparities. Moreover, although this study's results align with estimates from other sources that homicides increased by approximately 30% during the COVID-19 pandemic,43 it is possible that GVA data collection procedures have improved over time, in which case using these data to assess longitudinal trends could overestimate the COVID-19‒related increase in firearm injuries. Improving access to government data on firearm injuries is critically important for future work.44
CONCLUSIONS
Nationally, children of color, especially Black children, experience greater exposure to neighborhood firearm violence than White children. The COVID-19 pandemic only exacerbated these racial disparities. These findings highlight the importance of firearm violence exposure as a source of racial inequity starting in childhood, the importance of surveillance to track child exposure to firearm violence, and the need for substantial investments in specific policies and programs that prevent violence and mitigate the consequences of exposure to firearm violence.
CRediT authorship contribution statement
Rachel Martin: Writing – original draft. Sonali Rajan: Conceptualization, Writing – review & editing. Faizah Shareef: Writing – original draft. Kristal C. Xie: Writing – original draft. Kalice A. Allen: Project administration, Writing – original draft. Marc Zimmerman: Conceptualization, Writing – review & editing. Jonathan Jay: Conceptualization, Formal analysis, Methodology, Supervision, Writing – original draft.
ACKNOWLEDGMENTS
The authors thank Arezoo Sadeghi and Jeff Simeon at the Software & Application Innovation Laboratory at Boston University for their help in obtaining the Gun Violence Archive data.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agency.
This work has been supported by the Boston University Clinical & Translational Science Institute (NCATS 1UL1TR001430), by the Boston University Undergraduate Research Opportunities Program, and by the Firearm-safety Among Children and Teens Consortium (NICHD 1R24HD087149-01A1). No honoraria, grants, or other forms of payment were received for producing this manuscript.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.CDC Wonder. Centers for Disease Control and Prevention. https://wonder.cdc.gov/. Updated April 1, 2022. Accessed April 7, 2022.
- 2.Rajan S, Branas CC, Myers D, Agrawal N. Youth exposure to violence involving a gun: evidence for adverse childhood experience classification. J Behav Med. 2019;42(4):646–657. doi: 10.1007/s10865-019-00053-0. [DOI] [PubMed] [Google Scholar]
- 3.Vasan A, Mitchell HK, Fein JA, Buckler DG, Wiebe DJ, South EC. Association of neighborhood gun violence with mental health-related pediatric emergency department utilization. JAMA Pediatr. 2021;175(12):1244–1251. doi: 10.1001/jamapediatrics.2021.3512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turner HA, Mitchell KJ, Jones LM, Hamby S, Wade R, Beseler CL. Gun violence exposure and posttraumatic symptoms among children and youth. J Trauma Stress. 2019;32(6):881–889. doi: 10.1002/jts.22466. [DOI] [PubMed] [Google Scholar]
- 5.Sharkey P. The acute effect of local homicides on children's cognitive performance. Proc Natl Acad Sci U S A. 2010;107(26):11733–11738. doi: 10.1073/pnas.1000690107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molnar BE, Gortmaker SL, Bull FC, Buka SL. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. Am J Health Promot. 2004;18(5):378–386. doi: 10.4278/0890-1171-18.5.378. [DOI] [PubMed] [Google Scholar]
- 7.Opara I, Lardier DT, Jr, Metzger I, et al. Bullets have no names”: a qualitative exploration of community trauma among Black and Latinx youth. J Child Fam Stud. 2020;29(8):2117–2129. doi: 10.1007/s10826-020-01764-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turner HA, Finkelhor D, Henly M. Exposure to family and friend homicide in a nationally representative sample of youth. J Interpers Violence. 2021;36(7–8):NP4413–NP4442. doi: 10.1177/0886260518787200. [DOI] [PubMed] [Google Scholar]
- 9.Sheats KJ, Irving SM, Mercy JA, et al. Violence-related disparities experienced by Black youth and young adults: opportunities for prevention. Am J Prev Med. 2018;55(4):462–469. doi: 10.1016/j.amepre.2018.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James S, Gold S, Rouhani S, McLanahan S, Brooks-Gunn J. Adolescent exposure to deadly gun violence within 500 meters of home or school: ethnoracial and income disparities. Health Aff (Millwood) 2021;40(6):961–969. doi: 10.1377/hlthaff.2020.02295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schuster MA, Elliott MN, Kanouse DE, et al. Racial and ethnic health disparities among fifth-graders in three cities. N Engl J Med. 2012;367(8):735–745. doi: 10.1056/NEJMsa1114353. [DOI] [PubMed] [Google Scholar]
- 12.Cohen JS, Donnelly K, Patel SJ, et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148(1) doi: 10.1542/peds.2020-042697. [DOI] [PubMed] [Google Scholar]
- 13.Rochford HI, Brooks K, Berg M, Peek-Asa C. COVID-19-related violence trend data challenges & a resource for injury researchers. Inj Epidemiol. 2021;8(1):45. doi: 10.1186/s40621-021-00338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdallah HO, Zhao C, Kaufman E, et al. Increased firearm injury during the COVID-19 pandemic: a hidden urban burden. J Am Coll Surg. 2021;232(2):159–168. doi: 10.1016/j.jamcollsurg.2020.09.028. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schleimer JP, McCort CD, Tomsich EA, et al. Physical distancing, violence, and crime in U.S. cities during the coronavirus pandemic. J Urban Health. 2021;98(6):772–776. doi: 10.1007/s11524-021-00593-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schleimer JP, Buggs SA, McCort CD, et al. Neighborhood racial and economic segregation and disparities in violence during the COVID-19 pandemic. Am J Public Health. 2022;112(1):144–153. doi: 10.2105/AJPH.2021.306540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Browning CR, Calder CA, Ford JL, Boettner B, Smith AL, Haynie D. Understanding racial differences in exposure to violent areas: integrating survey, smartphone, and administrative data resources. Ann Am Acad Pol Soc Sci. 2017;669(1):41–62. doi: 10.1177/0002716216678167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sampson RJ, Morenoff JD, Raudenbush S. Social anatomy of racial and ethnic disparities in violence [published correction appears in Am J Public Health. 2006;96(4):591] Am J Public Health. 2005;95(2):224–232. doi: 10.2105/AJPH.2004.037705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gun violence archive. https://www.gunviolencearchive.org/. Accessed July 7, 2021.
- 20.Roman JK. NORC at the University of Chicago; Bethesda, MD: 2022. A blueprint for a U.S. firearms data infrastructure.https://www.norc.org/PDFs/FirearmDataInfrastructureExpertPanel/ABlueprintforaU.S.FirearmsDataInfrastructure_NORCExpertPanelFinalReport_October2020.pdf Published October 2020. [Google Scholar]
- 21.Kim D. Social determinants of health in relation to firearm-related homicides in the United States: a nationwide multilevel cross-sectional study. PLoS Med. 2019;16(12) doi: 10.1371/journal.pmed.1002978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson BT, Sisti A, Bernstein M, et al. Community-level factors and incidence of gun violence in the United States, 2014-2017. Soc Sci Med. 2021;280 doi: 10.1016/j.socscimed.2021.113969. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman EJ, Passman JE, Jacoby SF, et al. Making the news: victim characteristics associated with media reporting on firearm injury. Prev Med. 2020;141 doi: 10.1016/j.ypmed.2020.106275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krieger N, Feldman JM, Waterman PD, Chen JT, Coull BA, Hemenway D. Local residential segregation matters: stronger association of census tract compared to conventional city-level measures with fatal and non-fatal assaults (total and firearm related), using the Index of Concentration at the Extremes (ICE) for racial, economic, and racialized economic segregation, Massachusetts (US), 1995-2010. J Urban Health. 2017;94(2):244–258. doi: 10.1007/s11524-016-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siegel M, Poulson M, Sangar R, Jay J. The interaction of race and place: predictors of fatal police shootings of Black victims at the incident, census tract, city, and state levels, 2013‒2018. Race Soc Probl. 2021;13(3):245–265. doi: 10.1007/s12552-020-09307-y. [DOI] [Google Scholar]
- 26.Jay J, Bor J, Nsoesie EO, et al. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat Hum Behav. 2020;4(12):1294–1302. doi: 10.1038/s41562-020-00998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keppel K, Pamuk E, Lynch J, et al. Methodological issues in measuring health disparities. Vital Health Stat. 2005;2(141):1–16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681823/ Accessed July 7, 2021. [PMC free article] [PubMed] [Google Scholar]
- 28.Cameron AC, Gelbach JB, Miller DL. Robust inference with multiway clustering. J Bus Econ Stat. 2011;29(2):238–249. doi: 10.1198/jbes.2010.07136. [DOI] [Google Scholar]
- 29.Read JG. Measuring ethnicity with U.S. Census data: implications for Mexicans and Arabs. Popul Res Policy Rev. 2013;32(4):611–631. doi: 10.1007/s11113-013-9286-5. [DOI] [Google Scholar]
- 30.Adia AC, Nazareno J, Operario D, Ponce NA. Health conditions, outcomes, and service access among Filipino, Vietnamese, Chinese, Japanese, and Korean Adults in California, 2011-2017. Am J Public Health. 2020;110(4):520–526. doi: 10.2105/AJPH.2019.305523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raker EJ, Arcaya MC, Lowe SR, Zacher M, Rhodes J, Waters MC. Mitigating health disparities after natural disasters: lessons from the risk project. Health Aff (Millwood) 2020;39(12):2128–2135. doi: 10.1377/hlthaff.2020.01161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garbarino J, Bradshaw CP, Vorrasi JA. Mitigating the effects of gun violence on children and youth. Future Child. 2002;12(2):72–85. doi: 10.2307/1602739. [DOI] [PubMed] [Google Scholar]
- 33.The impact of gun violence on children and teens. Everytown Research & Policy. https://everytownresearch.org/report/the-impact-of-gun-violence-on-children-and-teens/#recommendations. Updated December 28, 2021. Accessed April 7, 2022.
- 34.Saltzman WR, Pynoos RS, Layne CM, Steinberg AM, Aisenberg E. Trauma- and grief-focused intervention for adolescents exposed to community violence: results of a school-based screening and group treatment protocol. Group Dyn. 2001;5(4):291–303. doi: 10.1037/1089-2699.5.4.291. [DOI] [Google Scholar]
- 35.Buggs SA, Webster DW, Crifasi CK. Using synthetic control methodology to estimate effects of a Cure Violence intervention in Baltimore, Maryland. Inj Prev. 2022;28(1):61–67. doi: 10.1136/injuryprev-2020-044056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heinze JE, Krusky-Morey A, Vagi KJ, et al. Busy streets theory: the effects of community-engaged greening on violence. Am J Community Psychol. 2018;62(1–2):101–109. doi: 10.1002/ajcp.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jay J, Miratrix LW, Branas CC, Zimmerman MA, Hemenway D. Urban building demolitions, firearm violence and drug crime. J Behav Med. 2019;42(4):626–634. doi: 10.1007/s10865-019-00031-6. [DOI] [PubMed] [Google Scholar]
- 38.Jay J, de Jong J, Jimenez MP, Nguyen Q, Goldstick J. Effects of demolishing abandoned buildings on firearm violence: a moderation analysis using aerial imagery and deep learning. Inj Prev. 2021 doi: 10.1136/injuryprev-2021-044412. In press. Online December 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wong B, Bernstein S, Jay J, Siegel M. Differences in racial disparities in firearm homicide across cities: the role of racial residential segregation and gaps in structural disadvantage. J Natl Med Assoc. 2020;112(5):518–530. doi: 10.1016/j.jnma.2020.05.014. [DOI] [PubMed] [Google Scholar]
- 40.Farley R, Frey WH. Changes in the segregation of whites from blacks during the 1980s: small steps toward a more integrated society. Am Sociol Rev. 1994;59(1):23–45. doi: 10.2307/2096131. [DOI] [Google Scholar]
- 41.Teitelman A, McDonald CC, Wiebe DJ, et al. Youth's strategies for staying safe and coping with the stress of living in violent communities. J Community Psychol. 2010;38(7):874–885. doi: 10.1002/jcop.20402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burdick-Will J, Stein ML, Grigg J. Danger on the way to school: exposure to violent crime, public transportation, and absenteeism. Sociol Sci. 2019;6:118–142. doi: 10.15195/v6.a5. [DOI] [Google Scholar]
- 43.Rosenfeld R, Lopez E. Council on Criminal Justice; Washington, DC: 2020. Pandemic, social unrest, and crime in U.S cities.https://ncvc.dspacedirect.org/handle/20.500.11990/1918 [Google Scholar]
- 44.Goldstick JE, Kaufman EJ, Delgado MK, Jay J, Carter PM. Commentary: reducing youth firearm violence and the associated health disparities requires enhanced surveillance and modern behavioral intervention strategies - a commentary on Bottiani et al. (2021) J Child Psychol Psychiatry. 2021;62(5):580–583. doi: 10.1111/jcpp.13421. [DOI] [PMC free article] [PubMed] [Google Scholar]