Abstract
Objectives
Structured reporting (SR) in radiology reporting is suggested to be a promising tool in clinical practice. In order to implement such an emerging innovation, it is necessary to verify that radiology reporting can benefit from SR. Therefore, the purpose of this systematic review is to explore the level of evidence of structured reporting in radiology. Additionally, this review provides an overview on the current status of SR in radiology.
Methods
A narrative systematic review was conducted, searching PubMed, Embase, and the Cochrane Library using the syntax ‘radiol*’ AND ‘structur*’ AND ‘report*’. Structured reporting was divided in SR level 1, structured layout (use of templates and checklists), and SR level 2, structured content (a drop-down menu, point-and-click or clickable decision trees). Two reviewers screened the search results and included all quantitative experimental studies that discussed SR in radiology. A thematic analysis was performed to appraise the evidence level.
Results
The search resulted in 63 relevant full text articles out of a total of 8561 articles. Thematic analysis resulted in 44 SR level 1 and 19 level 2 reports. Only one paper was scored as highest level of evidence, which concerned a double cohort study with randomized trial design.
Conclusion
The level of evidence for implementing SR in radiology is still low and outcomes should be interpreted with caution.
Key Points
• Structured reporting is increasingly being used in radiology, especially in abdominal and neuroradiological CT and MRI reports.
• SR can be subdivided into structured layout (SR level 1) and structured content (SR level 2), in which the first is defined as being a template in which the reporter has to report; the latter is an IT-based manner in which the content of the radiology report can be inserted and displayed into the report.
• Despite the extensive amount of research on the subject of structured reporting, the level of evidence is low.
Keywords: Radiology, Reports, Neoplasm staging, Magnetic resonance imaging, Multidetector computed tomography
Introduction
The area of radiology is an ever innovating field with new applications, such as speech recognition systems and the introduction of Picture Archiving and Communication System (PACS), leading to digitalization and new possibilities in radiology reporting [1, 2]. The recent introduction of different types of structured reporting (SR) further accelerates initiatives in the field of reporting, and many radiology departments use some sort of SR already [3]. The magnitude of this trend and its promotion by large radiological societies, such as the Radiological Society of North America (RSNA) and the European Society of Radiology (ESR), suggests that this way of reporting is promising and that implementation of SR in clinical practice should be seriously considered [4, 5]. Overall, SR has been thought to be the key to improve clinical and radiological workflow.
The main goal of implementing SR seems to be enhancing the content of the radiological report as well as the reporting process itself. Due to increasing imaging possibilities, larger data sets and the availability of more specific treatments, details become ever more important. The radiological report should arrange this huge amount of information into a readable (legible) text containing the most accurate and specific information that is needed to make accurate decisions to treat the patient best. This renders the radiological reporting process more complicated and time consuming.
To accommodate this increasing demand of information, several tools have been proposed to improve the quality of the radiological report. Standardization tools (RECIST (Response Evaluation Criteria in Solid Tumors), Fleischner glossary, the RADS (Reporting And Data System) collection) [6–8], are created to be more accurate on describing pathology and its extension or evolution, to ensure that the content of the report is accurate. On the other hand, reporting tools, such as structured reporting and reporting guidelines, are constructed in order to enhance the reporting process; this concept is in literature generally referred to as “structured reporting.”
However, before implementation of SR, it is necessary to provide evidence to justify its introduction and implementation in the clinical workflow with a systematic review. As there is a plethora of definitions and interpretations of SR present in literature, a clear definition had to be determined for this review. The definition “structured reporting is an IT-based method to import and arrange the medical content into the radiological report,” as coined by Nobel et al. [9], was used. The main purpose of this systematic review is to explore the level of evidence of structured reporting. Additionally, this review provides an overview on the current status of SR in radiology.
Materials and methods
A systematic search was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) criteria [10], and results were further categorized using a thematic analysis approach [11]. Results were analyzed and interpreted consistently with a textual narrative synthesis to visualize the similarities and differences among various methodologies in study design [12]. The next step was to determine the level of evidence of the studies. Because of the heterogeneity in study design, the simplified grading system (level A/B/C) according to Siwek et al. [13] was used to determine the strength of evidence on which outcomes were based. Randomized controlled trials are considered level A. Level B studies consist of all other evidence except for expert opinions or commentaries, which are level C. The groups were ordered on publication year followed by an alphabetical order. In case of discrepancy, consensus was reached between two authors (J.M.N. and K.G.).
Literature review protocol
A literature search was conducted by searching PubMed, Embase, and the Cochrane Library up to 10 August 2020. To include relevant papers, a wide search strategy was applied using the combination of the synonyms of ‘radiology’, ‘structure’ and ‘reporting’ (radiol* AND structur* AND report*).
Eligibility and study selection
All quantitative experimental studies that discussed SR in radiology have been included. After removing duplicates, title and abstract were independently screened on relevance by two authors. The following articles were excluded: articles that did not discuss structured reporting in radiology; comments or expert opinions (level C [13]); articles not in English, German, or Dutch; or those without full text availability. Bibliographies of included studies were searched in order to find additional relevant papers.
Definition of structured reporting (SR)
The definition “structured reporting is an IT-based method to import and arrange the medical content into the radiological report” [9] was used to frame the field of interest. This definition acknowledges a difference between SR and standardized reporting. Standardized reporting refers to the increase of uniformity of the report content with standardization tools (e.g., RECIST, Fleischner glossary, the RADS collection [6–8]). SR refers to the use of specific tools (structured reporting or reporting guidelines) that can be used to properly build, structure, or fill the radiological report itself. This differentiation is necessary to be able to only include the right studies which change the reporting process and not studies that merely change, for instance, the vocabulary used.
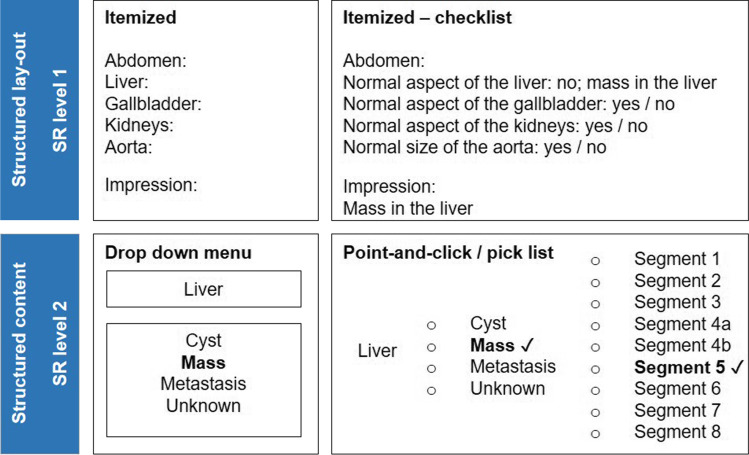
Additionally, SR is subdivided into structured layout (SR level 1) and structured content (SR level 2) [9]. In this stratification model, structured layout (SR level 1) is defined as being a template or blueprint format in which the reporter has to report or has to adjust to. Structured content (SR level 2) is a manner in which the content of the radiology report can be inserted and displayed into the report (Fig. 1). As such, structured layout (e.g., templates and checklists) and structured content (e.g., drop-down menu, point-and-click or clickable decision trees) highlight the level of IT involvement when implementing SR. This subdivision is used to be able to categorize the types of SR found in the included studies.
Fig. 1.
Examples of different levels of structured reporting. SR level 1, structured layout: itemized, itemized-checklist; in these examples, the obligated items or possible options are already stated in the template to ensure its presence. SR level 2, structured content: drop-down menu, point-and-click/pick list; these are examples of IT-based tools to insert specific textual items into the radiological report, for instance with the use of a drop-down menu in which an option can be chosen out of a particular list, or by using a point-and-click/pick list which in turn can open a new point-and-click/pick list option in order to build the report
Results
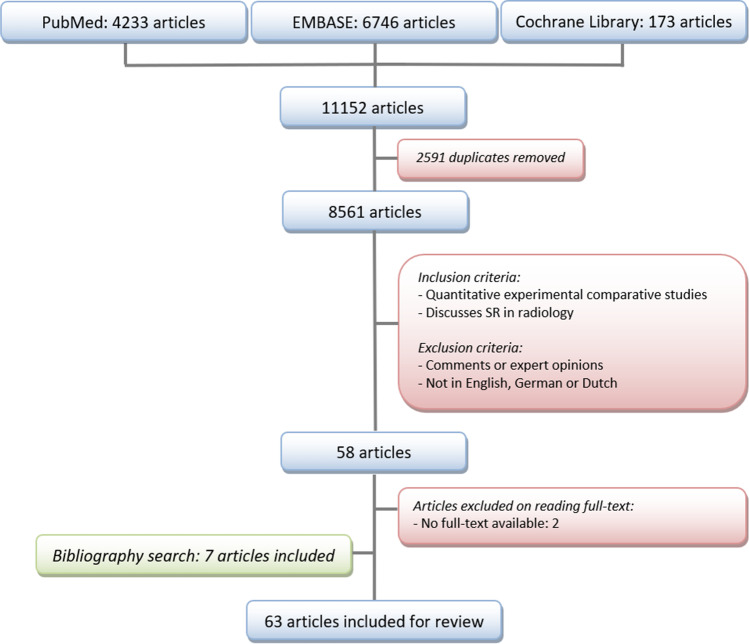
The literature search retrieved 4233, 6746, and 173 articles (total 11,152) from PubMed, Embase, and the Cochrane Library databases respectively. A total of 2591 duplicates were removed. Title and abstract of 8561 articles were assessed by J.M.N. and K.G., which resulted in 58 relevant articles. Full text was available for 56 articles. Bibliography search resulted in 7 additional studies, leading to a total of 63 studies that were included (Fig. 2 and Table 1). No reviews were found. Due to the heterogeneity of included studies, it was neither possible to perform a meta-analysis nor to pool the results.
Fig. 2.
Search flow chart. SR, structured reporting
Table 1.
Study characteristics. Overview of articles with level A and B evidence which studied structured reporting in radiology. Presented is the level of evidence, control group, intervention, subspecialty/field, indication, modality and outcome(s)
| Level of evidence | Control | Intervention | Subspecialty/field | Indication | Modality | Outcome(s) | ||
|---|---|---|---|---|---|---|---|---|
| Structured layout (SR level 1) — one template | ||||||||
| Dimarco et al. (2020) [14] | B | Free text | Structured itemized template with four parts and several key items | Abdomen | Pancreatic ductal adenocarcinoma | CT |
Significant reduction of missing morphological and vascular features Improvement inter-reader agreement |
|
| Gupta et al. (2020) [15] | B | Free text | Added 14 essential parameters | Abdomen | Rectal cancer staging | MRI |
Significant report quality improvement Referring provider satisfaction improved |
|
| McFarland (2020) [16] | B | Free text | Free-form structured itemized templates | Abdomen | Various | CT |
Less reporting errors potentially reducing The report word length did not differ |
|
| Olthof et al. (2020)[17] | B | Free text | Additional template with key items for critical findings | Neurology | CNS metastasis | MRI |
Automated insertion of context-dependent data and required elements is feasible Guideline adherence concerning critical findings improved |
|
| Alessandrino et al. (2019)[18] | B | Free text | Adding key features concerning inherited neuromuscular disorders | Musculoskeletal radiology | Lower limb inherited neuromuscular disorder | MRI | More clinically relevant disease management information | |
| Benson et al. (2019) [19] | B | Free text | Structured template with three options to score CNS metastasis after RT | Neurology | CNS metastasis | MRI |
Decreasing non-specific description Improving discrete characterization Usage of non-specific language usage did not differ |
|
| Gore et al. (2019)[20] | B | Free text | Template with headings according to BT-RADS | Neurology | Brain tumor (BT-RADS) | MRI | Perception improvement among radiologists and referring providers | |
| Liu et al. (2019) [21] | B | Free text | Structured itemized template with key features and standardized entries | Abdomen | Endometrial cancer | MRI | Increasing radiologists’ work efficiency and gynecologists’ satisfaction | |
| Wetterauer et al. (2019) [22] | B | Free text | Structured reports with PI-RADS key features | Abdomen | Prostate cancer (PI-RADS) | MRI |
Urologists’ surgical planning was facilitated by better assessing exact tumor location Improved satisfaction referring physician |
|
| Bink et al. (2018)[23] | B | Free text | Itemized template (17 tumor items) | Neurology | Brain tumor staging | MRI | Template ensured reliable detection of all relevant predefined items and reproducible documentation | |
| Griffin et al. (2018) [24] | B | Free text | Itemized template with TI-RADS and/or management integration | Head and Neck | Thyroid nodules (TI-RADS) | Ultrasound | Better feature description ACR TIRADS usage substantially improved management recommendations | |
| Magnetta et al. (2018)[25] | B | Free text | Itemized template using PI-RADS | Abdomen | Prostate (PI-RADS) | MRI | Improved communication and clinical report impact with referring urologists | |
| Olthof et al. (2018) [26] | B | Free text | Itemized RECIST template | Various | RECIST | CT | Combination of optimized workflow, subspecialization and SR led to significantly better report quality | |
| Poullos et al. (2018) [27] | B | Free text | Itemized template | Abdomen | Hepatocellular carcinoma | CT | Assessment of transplant suitability improved using Milan criteria | |
| Tersteeg et al. (2018)[28] | B | Free text | Itemized template with incorporated guidelines and key features | Abdomen | Rectal cancer staging | MRI | More complete report | |
| Flusberg et al. (2017)[29] | B | Free text | Itemized template incorporating including LI-RADS | Abdomen | Hepatocellular carcinoma (LI-RADS) | MRI/CT | More comprehensive and consistent reporting | |
| Franconeri et al. (2017)[30] | B | Free text | Disease-specific itemized template | Abdomen | Uterine fibroid | MRI |
Fewer key features were missed More helpful for treatment planning and understanding |
|
| Pysarenko et al. (2017)[31] | B | Free text | Template with 8 itemized key-elements | Abdomen | Various | Ultrasound | Improved reimbursement | |
| Wildman-Tobriner et al. (2017) [32] | B | Free text | Itemized template | Abdomen | IBD | CT |
Key feature reporting improved Minimal impact on accuracy SR reports were preferred by referring physicians |
|
| Wildman-Tobriner et al. (2017)[33] | B | Free text | Itemized template with 15 key elements | Abdomen | Pediatric Crohn’s disease | MRI | Significantly increasing on key features mentioning Referring clinicians subjectively preferred SR | |
| Dickerson et al. (2016)[34] | B | Free text | Itemized template with 12 key features | Brain | MS | MRI |
Increased rate relevant findings Standardized reports are preferred by neurologists |
|
| Brook et al. (2015) [35] | B | Free text | Itemized template with 12 key features | Abdomen | Pancreatic cancer | CT |
Superior evaluation Facilitated surgical planning Increased surgeons confidence concerning tumor resectability |
|
| Sahni et al. (2015) [36] | B | Free text | Template with 14 itemized quality measures | Abdomen | Rectal cancer staging | MRI | Report quality improved, 30% of reports remained unsatisfactory | |
| Silveira et al. (2015)[37] | B | Free text | Itemized template and computer-aided diagnosis | Abdomen | Prostate | MRI |
Improving report quality Improving contrast enhancement kinetic curve |
|
| Lin et al. (2014)[38] | B | Free text | Itemized checklist-based template | Neurology/trauma | Cervical spine | CT |
Significant decrease in missed non-fracture findings No change in missed fractures |
|
| Marcovici et al. (2014)[39] | B | Free text | Prepopulated itemized checklist template | Thorax | Various | X-ray | Templates are more complete and more effective | |
| Powell et al. (2014) [40] | B | Free text | Itemized checklist-based template | Neurology/trauma | Maxillofacial | CT |
No improvement on report accuracy of radiology residents Focused training, checklist flexibility, and an adjustment period are important Only mandatory checklists were readily adopted by residents |
|
| Fraser et al. (2013) [41] | B | Free text | Itemized template with different options (paper) | Head and Neck | Cervical lymphadenopathy | Ultrasound | Increased report streamline | |
| Structured layout (SR level 1) — multiple templates | ||||||||
| Chung et al. (2020)[42] | B | Free text | Seven different cross-divisional standardized structured reports | Thorax | Various | X-ray | Improvement of economic gains and projected radiologist time | |
| Hanna et al. (2016) [43] | B | Free text | Seven different itemized templates (4 CTs, 2 X-rays, 1 ultrasound) | Emergency | Various | Various |
Decrease of dictation time Decrease of total word length in some cases Mixed impact on total reporting time |
|
| Hawkins et al. (2014)[44] | B | Free text | 228 different prepopulated templates which may consist a pick list, fill-in-field and/or prose dictation | Various | Various | Various | Carefully constructed structured reports can help reducing errors | |
| Larson et al. (2013)[45] | B | Free text | 228 different prepopulated templates which may consist a pick list, fill-in-field and/or prose dictation | Various | Various | Various | High implementation adaptation rate | |
| Hawkins et al. (2012)[46] | B | Free text | Different prepopulated templates | Various | Various | Various | Prepopulated reports alone do not affect error rate or dictation time of radiology reports | |
| Schwartz et al. (2011) [47] | B | Free text | Different itemized templates | Various | Various | CT | Better content and greater clarity for radiologists and referring clinicians | |
| Liu et al. (2003) [48] | B | Free text | Different menu-based templates | Various | Various | Various |
Faster report turn-around time Less transcription errors and lower transcription costs |
|
| Structured layout (SR level 1) — hypothetical research | ||||||||
| Dabrowiecki et al. (2020) [49] | B | Free text | One negative chest X-ray report compared with one out of four templates | Thorax | Chest | X-ray |
Template use resulted in better comprehension by the public Unnecessary follow-up was less likely |
|
| Camilo et al. (2019) [50] | B | Free text | Four different templates (one free text, two ultrasound and one CT report) | Abdomen | Various | Ultrasound CT | Structured report with final conclusion/comment is preferred by attending and requesting physicians | |
| Heye et al. (2018) [51] | B | Free text | Three different layouts (structured itemized text, tables, images) | Thorax | Chest | CT | The costumer favors structured reporting | |
| Lather et al. (2017) [52] | B | Free text | Structured itemized template | Thorax | Chest | CT | SR is superior | |
| Travis et al. (2014) [53] | B | Free text | Three different layouts with measurement section | Thorax/abdomen | Various oncological | CT | A separate lesion measurement section is preferred over random mentioning | |
| Krupinski et al. (2011) [54] | B | Free text | Itemized and hierarchical template | Abdomen | Renal abnormalities | CT | A “one-size-fits-all” radiology report format does not exist | |
| Grieve et al. (2008) [55] | B | Free text | Four different templates | Abdomen | Negative examination | Ultrasound | Detailed reports and a radiologists’ opinion is preferred by general practitioners | |
| Sistrom et al. (2005) [56] | B | Free text | Itemized structured templates | Abdomen | Renal calcifications | CT | Equally efficient and accurate for transmitting content | |
| Naik et al. (2001) [57] | B | Free text | Three itemized with difference in completeness | Abdomen | Various | Ultrasound |
Improved facilitation of complete documentation Itemized reports are preferred by radiologists and referring clinicians |
|
| Structured content (SR level 2) | ||||||||
| Johnson et al. (2010) [58]a | A | Free text | Point-and-click system used to build a sentence in the structured report | Neurology | Possible stroke | MRI | No improvement in report clarity by attending physicians | |
| Johnson et al. (2009) [59]a | A | Free text | Point-and-click system used to build a sentence in the structured report | Neurology | Possible stroke | MRI | Report accuracy and completeness did not improve | |
| Aase et al. (2020) [60] | B | Free text | Template checklist with six pick list options concerning incidental pulmonary nodule description | Thorax | Pulmonary nodule | CT |
Increased documentation compliance Better follow-up process Low utilization rates |
|
| Alper et al. (2020) [61] | B | Free text | Template with pick list options with preferred terms for abdominal organs normal finding mentioning | Abdomen | Various | CT/MRI |
Better use of preferred/acceptable phrases Decreased use of equivocal terms |
|
| Kim et al. (2020) [62] | B | Free text | Template-based structured reports with point-and-click menus including standard elements used in a densitometry report | Nuclear radiology | Osteoporosis | DXA |
Shorter reporting times Increased report quality |
|
| Tuncyurek et al. (2019) [63] | B | Free text | Template with pick list options to describe 12 key features of pelvic MRI for perianal fistulizing disease | Abdomen | Perianal fistulizing disease | MRI |
Fewer key features were missed More complete, clear and helpful for treatment planning |
|
| Armbruster et al. (2018) [64] | B | Free text | Clickable decision trees that function as a checklist and to use for building automatically semantic sentences | Head and neck | Petrous bone | MRI |
Increases completeness and quality Satisfaction of referring physicians improved |
|
| Sabel et al. (2018) [65] | B | Free text | Clickable decision trees on several items with several subitems concerning vascular status | Vascular | Lower extremities | CTA | Superior clarity, completeness, clinical relevance, and usefulness rated by referring clinicians | |
| Schoeppe et al. (2018) [66] | B | Free text | Clickable decision trees in which outcomes were used to create semantic sentences and were displayed in the report | Abdomen | Swallowing disorders | Swallowing studies |
Increases detailed information and facilitation of information extraction Better assisting clinical decision-making |
|
| Schöppe et al. (2018) [67] | B | Free text | Clickable decision trees for specific items concerning (degenerative) osteoarthritis of the glenohumoral joint used to create semantic sentences used in the report | Musculoskeletal radiology | Shoulder | X-ray | May be a useful tool in clinical decision-making | |
| Shaish et al. (2018) [68] | B | Layout template | Drop-down menus which were used as template to describe individual lesion characteristics concerning PI-RADS | Abdomen | Prostate | MRI |
PI-RADS adherence improved May increase diagnostic performance |
|
| Gassenmaier et al. (2017) [69] | B | Free text | Template with findings and impression section with clickable decision trees with several levels | Musculoskeletal radiology | Shoulder | MRI |
Improved readability Improved linguistic quality |
|
| Norenberg et al. (2017) [70] | B | Free text | Clickable decision trees used to describe 13 key features | Abdomen | Rectal cancer | MRI |
Facilitates surgical planning Higher satisfaction level of referring surgeons about report correctness and clinical decision making |
|
| Sabel et al. (2017) [71] | B | Free text | Clickable decision trees containing observations with standardized subheadings in a consistent order | Thorax | Pulmonary embolism | CTA | Superior in clarity, better content and clinical utility | |
| Walter et al. (2015) [72] | B | Free text | Pick list about coronary calcifications added to a structured report with normal and abnormal default standard terminology which auto-populates the report | Cardio | Coronary calcifications | CT | Improved accuracy of coronary calcification mentions | |
| Schweitzer et al. (2014) [73] | B | Free text | Template with 108 obligated items with drop-down menus and free text option. The report contains highlighted parts when stated as abnormal | Forensics | Whole body | CT | Can act as guideline | |
| Karim et al. (2013) [74] | B | Free text | Different IT-based options were used and included standardized point-and-click menus, including anatomy, measures and additional diagnostic findings listed by organ and dedicated pathology in three different sections with a free text option for personal judgment | Vascular | Abdominal aortic aneurysm | CTA |
Decrease in average reporting time Ease of use may lead to more accurate decision support |
|
| Barbosa et al. (2010) [75] | B | Free text | Pick list reporting system on 8 descriptive items necessary for thyroid nodule characterization | Head and neck | Thyroid | Ultrasound | Information transmission improved for radiologists and referring clinicians | |
| Hasegawa et al. (2010) [76] | B | Free text | Pick list items and particular modifiers for different categories can be entered in templates that link those together | Thorax | Chest | X-ray | Report production time decreased | |
aIdentical study population or cohort
SR, structured reporting; SR level 1, structured layout; SR level 2, structured content; CNS, central nervous system; BT-RADS, Brain Tumor-Reporting And Data System; PI-RADS, Prostate Imaging-Reporting And Data System; TI-RADS, Thyroid Imaging-Reporting And Data System; RECIST, Response Evaluation Criteria in Solid Tumours; LI-RADS, Liver Imaging-Reporting And Data System; RT, radiotherapy; IBD, irritable bowel disease; MS, multiple sclerosis
Thematic data analysis
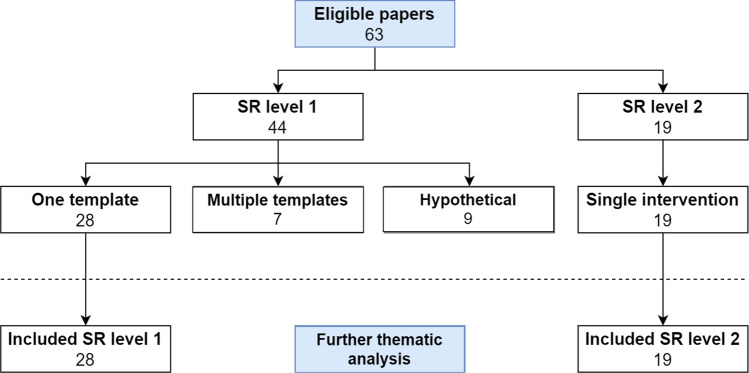
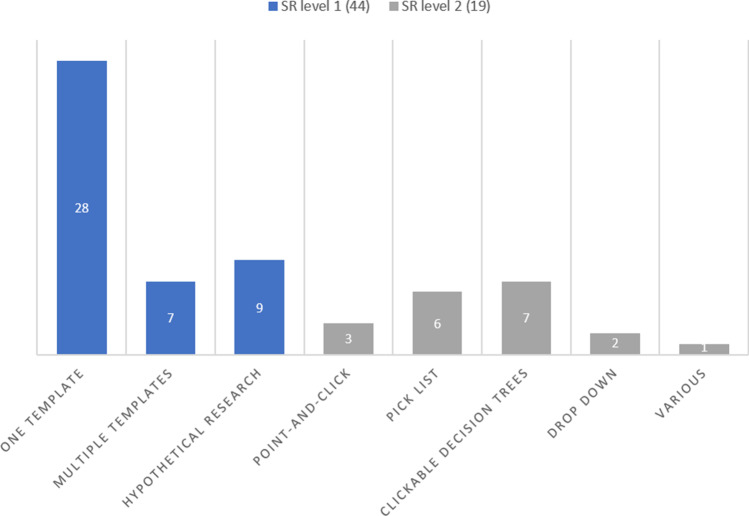
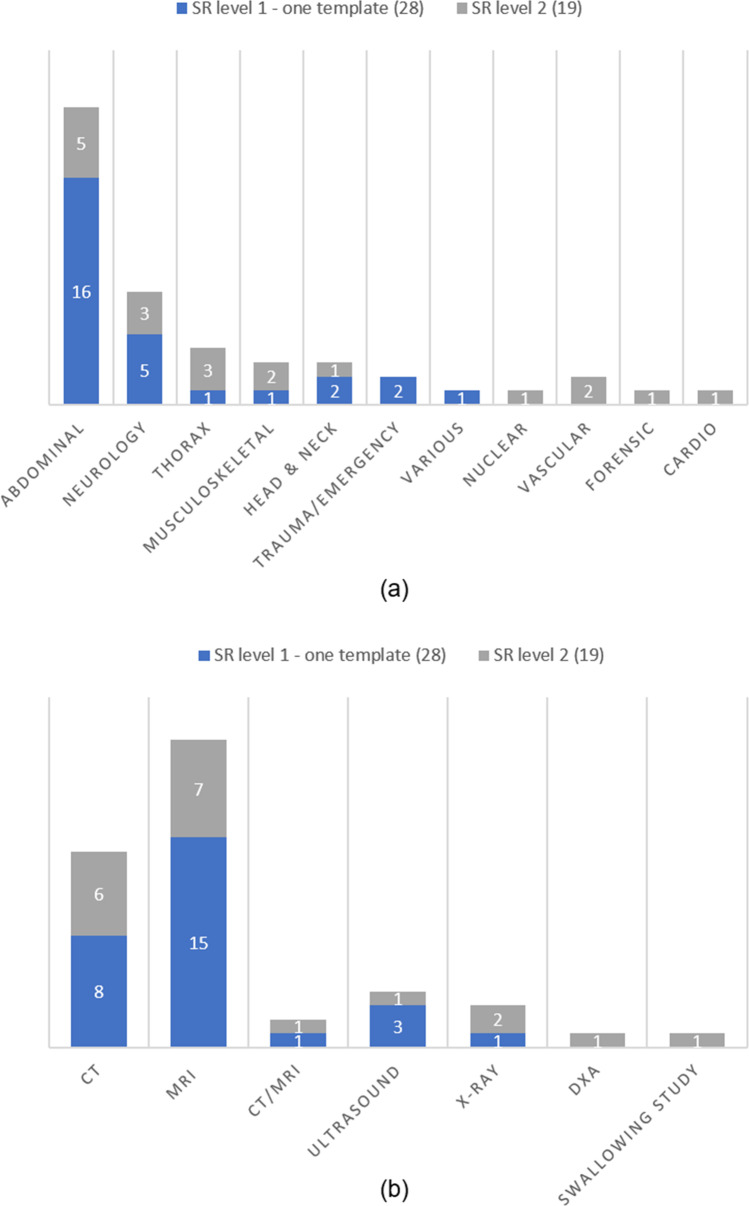
After inclusion, the 63 studies were grouped into structured layout (SR level 1) and structured content (SR level 2) groups (Fig. 3). Control group, intervention, subspecialty/field, indication, modality, and outcome of each study were assigned. Because of heterogeneity in the structured layout group (SR level 1), this group of 44 studies was subdivided into three subcategories: (1) one template (n = 28), (2) multiple templates (n = 7), and (3) hypothetical research (n = 9) (Table 1, Fig. 3 and Fig. 4).
Fig. 3.
Characteristics of included studies based on SR level. SR level 1, structured layout; SR level 2, structured content
Fig. 4.
Intervention based on SR level. SR level 1, structured layout; SR level 2, structured content
The first subcategory “one template” consists of studies that implement and compare only one template with a free text report comparison. An example can be an itemized template to report a specific clinical question, such as a magnetic resonance imaging (MRI) for brain tumor staging. The second subcategory “multiple templates” implemented several templates at once in their study before the comparison with free text reports was made. An example can be the implementation of several different templates for different clinical questions, such as implementing templates for computed tomography (CT), ultrasound, and X-ray concerning kidney stones, appendicitis, and heart failure. The third subcategory “hypothetical research” concerned studies that did not actually implement SR in clinical workflow, but assessed clinical or referring preferences on how to present the radiological information in the radiological report.
All 19 structured content (SR level 2) studies were interventional studies using an IT-based method to create the radiological report in the subcategories point-and-click system, pick list, clickable decision trees, drop-down and various (Table 1, Fig. 3 and Fig. 4).
As it is only possible, in an evidence-based manner, to accurately compare one structured reporting tool in one clinical interventional setting at once, only the studies implementing one template from the structured layout group and non-hypothetical studies have been used for further analysis. When not taking into account the hypothetical studies, nor the studies of the multiple template category, 28 studies remain on the structured layout level (SR level 1). All 19 structured content (SR level 2) studies were interventional studies using one IT-based method to create the radiological report and were all suitable for further analysis (Table 1, Fig. 3 and Fig. 4). The remaining subcategories (one template SR level 1 and all SR level 2 studies) resulted in 47 studies (Fig. 3).
Further analysis of these 47 studies resulted in additional characteristics about subspecialty field and used modalities (Fig. 5a and b). Overall, CT and MRI modalities are mostly used on the subspecialties abdomen and neurology.
Fig. 5.
a Subspecialty based on SR level and (b) modality used based on SR level. All included single intervention studies according to the field of specialty and modality used. SR level 1, structured layout; SR level 2, structured content; DXA, dual-energy X-ray absorptiometry (DXA)
Level of evidence
Two papers (one single study) were scored as level A in the structured content group. All other studies in the structured layout and structured content group were scored as level B evidence (Fig. 6).
Fig. 6.
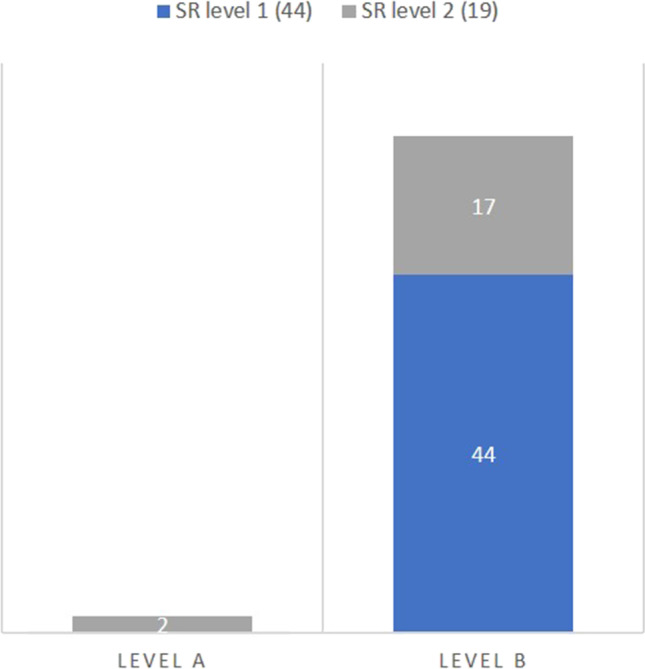
Level of evidence based on SR level. Level A, level A evidence according to Siwek et al. [13]; SR level 1, structured layout; SR level 2, structured content
Outcome
The value of outcomes of the studies on structured reporting depends heavily on the level of evidence of these studies. Therefore, the main focus of this study was to determine the level of evidence. However, to create an overview of research done on SR in radiology, main outcomes of included SR studies have been summarized in Table 1.
Discussion
The main goal of this narrative systematic literature review was to explore the level of evidence of all studies that try to enhance the radiological reporting process by using SR. This also resulted in an overview on the current status of SR in radiology and a summary of its outcomes. To our knowledge, this is the first paper to provide a systematic review of SR in radiology.
Level of evidence
A double-blinded, randomized controlled trial is considered the highest level of original research (not including systematic reviews or meta-analysis). In our literature search, the only study that approximates this level was the double cohort study with randomized trial design conducted by Johnson et al. [58, 59] and was therefore scored as level A evidence. They compared a point-and-click reporting system (SR level 2) with free text reporting in brain MRI in stroke patients in two papers. This study states that only the way of reporting varied in order to exclude all other interfering factors, thereby only investigating the effect of the change in reporting method. The remaining 61 studies were considered level B evidence, showing an overall low level of evidence.
The hypothetical subcategory studies (n = 7) are not implementational but only exploratory of nature. The multiple template studies (n = 9) are considered low-level evidence, because it is virtually impossible to confidentially match outcomes to a particular way of reporting, when (a) introducing several templates or reports simultaneously, (b) using different levels of SR, for (c) trying to answer different clinical questions.
However, also the other subcategory studies (one template SR level 1 and all SR level 2 studies), except both level A studies, changed several factors during the implementation of SR, which again can result in some sort of confounding. For instance, many papers describe an expert meeting among radiologists and/or clinicians, or conducted a literature review in order to create a template or pick-list with adequate vocabulary, before implementing SR. This introduced an additional standardizing step next to the implementation of SR in the reporting routine. As a result, both the report content and the reporting manner differed, and outcomes of these studies reflect the effect of the combined interventions. The effects of any individual intervention, however, remain unclear.
Additionally, an expert meeting or literature review before implementing the new reporting manner will likely result in an increase in report quality or accuracy, because the reporter will be guided in stating the correct (newly stated) items necessary for diagnosing when using SR, and thereby enhancing the report content. In this way, confirmation bias can occur, especially when report content quality or accuracy was the main goal of the study, and when outcomes were scored by the same experts that participated in the initial expert meeting.
The aforementioned shows that the study design of the included studies was hampered, resulting in low level of evidence studies. However, despite the fact that most studies are of low evidence, the total amount of published papers show the magnitude of the trend towards structured reporting in radiology.
One of the issues in chosen study design is probably based on the willingness to improve the radiological report as final clinical outcome, rather than searching for the true (single) vehicle that facilitates this.
Furthermore, a reason for the lack of high-level evidence papers can be the fact that proper implementation of SR might be highly case-specific. In radiology, multiple modalities as well as multiple clinical questions coexist and therefore it is possible that a SR tool or a specific SR level is not beneficial for all clinical settings or that it is depending on for instance difficulty level. A point-and-click or clickable decision tree method (SR level 2) may be better for a simple task with only few options, such as describing a thyroid nodule on an ultrasound examination. Likewise, a difficult, extensive clinical question which needs highly specific information or an extensive description, such as the description of a brain tumor on MRI, may suit a template or checklist (SR level 1) better than a point-and-click/pick list. In combination with several vendor-dependent structuring methods on different SR levels, this makes it difficult to choose a specific topic to set up a well-designed study. Also the fact that there are no studies found that compare two different SR methods, but only comparing free text with some sort of SR, shows that research on SR in radiological reporting is still at an exploratory level.
Current standing and future perspectives
Looking at the levels of SR, in total, 28 studies were performed at the level of structured layout implementing one template and 19 on the structured content level implementing a more IT-based type of SR, which shows that both SR level 1 and 2 are used in clinical studies. It is interesting to see that both levels are being investigated, because it is important to realize that in most cases it is easier, due to its lower IT-demand, to implement a template (SR level 1) in the reporting process than, for instance, implement a drop-down-menu-based report (SR level 2).
When looking at modality and subspecialty, most efforts are made with reports of CT and MRI examinations in the field of abdominal radiology and neuroradiology. An explanation might be the fact that the most important (staging) procedures use CT and MRI as a modality. Perhaps, the abdominal and neuroradiology fields are more suitable for using templates or it can be triggered by the fact that good classification systems or standardization systems already exist in these fields. If this is the case, this highlights the fact that SR is used for standardization by making sure that specific items or classification systems are described or used.
Table 1 shows that SR level 1 (templates) are mainly used to describe key features necessary to stage a particular disease or tumor with a predefined sentence with or without a particular standardization tool. Used standardization tools or classification systems can be found in Table 1, and examples are for instance PI-RADS, LI-RADS and RECIST, but also key elements concerning Crohn’s disease, rectal cancer staging, multiple sclerosis (MS), trauma or head and neck lymphadenopathy are used. Hence, also SR level 2 studies use key feature description or standardization tools (e.g., PI-RADS) to describe specific disease or tumors, such as stroke, pulmonary nodules, rectal cancer, thyroid nodules, or prostatic cancer (Table 1). However, SR level 2 studies use an IT-based system that supports constructing (semantic) sentences, according to the chosen option from the drop-down menu or point-and-click system, in which standardization is almost automatically linked to structured reporting.
When looking at the study outcomes in Table 1, the main goals, incentives, used SR method, and outcomes of each study vary widely, and therefore, pooling of outcomes is difficult. Despite this heterogeneity, this table of outcomes provides a panoramic overview of the present status of SR in radiology.
It shows that most of the included papers show an improvement in outcome when implementing SR. However, when looking at the evidence level, the only level A study [58, 59] did not improve the report clarity, accuracy, and completeness of the report using their point-and-click method. This is an interesting finding and can show that this particular point-and-click system was not beneficial in radiological reporting in this specific setting and concerning this specific outcome. However, the outcome of this study alone is insufficient to state that SR level 2 is not beneficial in radiology reporting, because outcomes seem to be highly case-specific. However, it is also hard to state that SR is beneficial in reporting in radiology when looking at the low level of evidence of all other included studies.
Overall, the level of evidence for SR is low and especially the link between structured reporting and standardization and its different effects on the radiological report is currently overlooked, but is of utmost importance. It seems that improving radiology reporting is more than just implementing SR and that standardization is necessary next to SR, and that both are highly entangled when implementing SR. This is likely caused by the fact that SR is based on a rather strict format in which several (mandatory) items or key features should be reported. Perhaps the question should be whether SR is not just a means to facilitate standardization, rather than that SR is improving the radiological report itself.
As such, high-quality research is necessary to separately investigate the value of all individual factors that are involved in standardization and SR to determine the best type of SR for a specific clinical problem. Investigating the effect of standardization should be prioritized, because it may make sense that improving the content of the report, hence making a complete report with all items referring clinicians are asking for, will likely improve reporting quality. Then, the next question should be how this standardized information should be placed in the radiological report and how we can assure it is inserted correctly. For instance, this can be done with a simple template or checklist (SR level 1), or with a more sophisticated point-and-click system (SR level 2). Finally, it is important to know whether the efforts are beneficial for the patient (e.g., better staging), the referring clinician (e.g., reduced reading time), the reporter (e.g., faster reporting), or for all. Nevertheless, it is possible that this supposed reporting improvement is mainly caused by standardization rather than SR.
Limitations
First of all, it was difficult to find all relevant implementational studies published on the subject of SR due to ambiguous use of the terms “standardized reporting” and “structured reporting.” To be as complete as possible, as well as to answer the research question best, a prior set definition for SR and its categorization system was used. In addition, a bibliography search was used to search for missed studies after conducting the main search. Because of heterogeneity of the included studies, it was hard to pool the data on a more specific level and therefore a thematic analysis was used. The outcome analysis performed in this paper was limited by the large heterogeneity of outcomes and study design. A more thorough analysis should be done to explore outcome measurements better and to see who (the referring clinician, radiologist or patient) will benefit from SR most, as well as which specific efforts resulted in this outcome.
Conclusion
Structured reporting is thought to have great potential to improve reporting in radiology. However, due to difficulties in study design there is a lack of high-quality research on this topic resulting in low overall evidence. Future research is needed to explore the individual effects of standardization and SR, as it is questionable whether SR is the solution for improving reporting in radiology or only a means in facilitating standardization.
Abbreviations
- ESR
European Society of Radiology
- PACS
Picture Archiving and Communication System
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- RSNA
Radiological Society of North America
- SR
Structured reporting
Funding
The authors state that this work has not received any funding.
Declarations
Guarantor
The scientific guarantor of this publication is Simon G.F. Robben, MD, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Not applicable.
Ethical approval
Institutional Review Board approval was not required because the nature of the submitted article.
Methodology
• Systemic literature review
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liu D, Zucherman M, Tulloss WB., Jr Six characteristics of effective structured reporting and the inevitable integration with speech recognition. J Digit Imaging. 2006;19:98–104. doi: 10.1007/s10278-005-8734-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reiner BI. The challenges, opportunities, and imperative of structured reporting in medical imaging. J Digit Imaging. 2009;22:562–568. doi: 10.1007/s10278-009-9239-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Powell DK, Silberzweig JE. state of structured reporting in radiology, a survey. Acad Radiol. 2015;22:226–33. doi: 10.1016/j.acra.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Radiological Society of North America (2020) RadReport template library. Radiological Society of North America, Oak Brook (IL), USA. Available via https://radreport.org. Accessed 15 Dec 2020.
- 5.European Society of Radiology (ESR) ESR paper on structured reporting in radiology. Insights Imaging. 2018;9:1–7. doi: 10.1007/s13244-017-0588-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwartz LH, Seymour L, Litière S, et al. RECIST 1.1 – standardisation and disease-specific adaptations: perspectives from the RECIST Working Group. Eur J Cancer. 2016;62:138–145. doi: 10.1016/j.ejca.2016.03.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
- 8.An JY, Unsdorfer KML, Weinreb JC. BI-RADS, C-RADS, CAD-RADS, LI-RADS, Lung-RADS, NI-RADS, O-RADS, PI-RADS, TI-RADS: reporting and data systems. Radiographics. 2019;39:1435–1436. doi: 10.1148/rg.2019190087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nobel JM, Kok EM, Robben SGF. Redefining the structure of structured reporting in radiology. Insights Imaging. 2020;11:10. doi: 10.1186/s13244-019-0831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535 [PMC free article] [PubMed]
- 11.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10(Suppl 1):6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 12.Lucas PJ, Baird J, Arai L, Law C, Roberts HM (2007) Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol 7:4 [DOI] [PMC free article] [PubMed]
- 13.Siwek J, Gourlay ML, Slawson DC, Shaughnessy AF. How to write an evidence-based clinical review article. Am Fam Physician. 2002;65:251–258. [PubMed] [Google Scholar]
- 14.Dimarco M, Cannella R, Pellegrino S, et al. Impact of structured report on the quality of preoperative CT staging of pancreatic ductal adenocarcinoma: assessment of intra- and inter-reader variability. Abdom Radiol (NY) 2020;45:437–448. doi: 10.1007/s00261-019-02287-7. [DOI] [PubMed] [Google Scholar]
- 15.Gupta NA, Mahajan S, Sumankumar A, Saklani A, Engineer R, Baheti AD. Impact of a standardized reporting format on the quality of MRI reports for rectal cancer staging. Indian J Radiol Imaging. 2020;30:7–12. doi: 10.4103/ijri.IJRI_308_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McFarland JA, Elkassem AMA, Casals L, Smith GD, Smith AD, Gunn AJ. Objective comparison of errors and report length between structured and freeform abdominopelvic computed tomography reports. Abdom Radiol (NY) 2021;46:387–393. doi: 10.1007/s00261-020-02646-9. [DOI] [PubMed] [Google Scholar]
- 17.Olthof AW, Leusveld ALM, de Groot JC, Callenbach PMC, van Ooijen PMA (2020) Contextual structured reporting in radiology: implementation and long-term evaluation in improving the communication of critical findings. J Med Syst 44(9):148 [DOI] [PMC free article] [PubMed]
- 18.Alessandrino F, Cristiano L, Cinnante CM, et al. Value of structured reporting in neuromuscular disorders. Radiol Med (Torino) 2019;124:628–635. doi: 10.1007/s11547-019-01012-0. [DOI] [PubMed] [Google Scholar]
- 19.Benson J, Burgstahler M, Zhang L, Rischall M. The value of structured radiology reports to categorize intracranial metastases following radiation therapy. Neuroradiol J. 2019;32:267–272. doi: 10.1177/1971400919845365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gore A, Hoch MJ, Shu H-KG, Olson JJ, Voloschin AD, Weinberg BD. Institutional implementation of a structured reporting system: our experience with the brain tumor reporting and data system. Acad Radiol. 2019;26:974–980. doi: 10.1016/j.acra.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 21.Liu Y, Feng Z, Qin S, Yang J, Han C, Wang X (2019) Structured reports of pelvic magnetic resonance imaging in primary endometrial cancer: potential benefits for clinical decision-making. PLoS One 14(3):e0213928 [DOI] [PMC free article] [PubMed]
- 22.Wetterauer C, Winkel DJ, Federer-Gsponer JR et al (2019) Structured reporting of prostate magnetic resonance imaging has the potential to improve interdisciplinary communication. PLoS One 14(2):e0212444 [DOI] [PMC free article] [PubMed]
- 23.Bink A, Benner J, Reinhardt J et al (2018) Structured reporting in neuroradiology: Intracranial tumors. Front Neurol 9:32 [DOI] [PMC free article] [PubMed]
- 24.Griffin AS, Mitsky J, Rawal U, Bronner AJ, Tessler FN, Hoang JK. Improved quality of thyroid ultrasound reports after implementation of the ACR thyroid imaging reporting and data system nodule lexicon and risk stratification System. J Am Coll Radiol. 2018;15:743–748. doi: 10.1016/j.jacr.2018.01.024. [DOI] [PubMed] [Google Scholar]
- 25.Magnetta MJ, Donovan AL, Jacobs BL, Davies BJ, Furlan A. Evidence-based reporting: a method to optimize prostate MRI communications with referring physicians. AJR Am J Roentgenol. 2018;210:108–112. doi: 10.2214/AJR.17.18260. [DOI] [PubMed] [Google Scholar]
- 26.Olthof AW, Borstlap J, Roeloffzen WW, Callenbach PMC, van Ooijen PMA. Improvement of radiology reporting in a clinical cancer network: impact of an optimised multidisciplinary workflow. Eur Radiol. 2018;28:4274–4280. doi: 10.1007/s00330-018-5427-x. [DOI] [PubMed] [Google Scholar]
- 27.Poullos PD, Tseng JJ, Melcher ML, et al. Structured reporting of multiphasic CT for hepatocellular carcinoma: effect on staging and suitability for transplant. AJR Am J Roentgenol. 2018;210:766–774. doi: 10.2214/AJR.17.18725. [DOI] [PubMed] [Google Scholar]
- 28.Tersteeg JJC, Gobardhan PD, Crolla RMPH, et al. Improving the quality of MRI reports of preoperative patients with rectal cancer: effect of national guidelines and structured reporting. AJR Am J Roentgenol. 2018;210:1240–1244. doi: 10.2214/AJR.17.19054. [DOI] [PubMed] [Google Scholar]
- 29.Flusberg M, Ganeles J, Ekinci T, et al. Impact of a structured report template on the quality of CT and MRI reports for hepatocellular carcinoma diagnosis. J Am Coll Radiol. 2017;14:1206–1211. doi: 10.1016/j.jacr.2017.02.050. [DOI] [PubMed] [Google Scholar]
- 30.Franconeri A, Fang J, Carney B, et al. Structured vs narrative reporting of pelvic MRI for fibroids: clarity and impact on treatment planning. Eur Radiol. 2018;28:3009–3017. doi: 10.1007/s00330-017-5161-9. [DOI] [PubMed] [Google Scholar]
- 31.Pysarenko K, Recht M, Kim D. Structured reporting: a tool to improve reimbursement. J Am Coll Radiol. 2017;14:662–664. doi: 10.1016/j.jacr.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 32.Wildman-Tobriner B, Allen BC, Bashir MR, et al. Structured reporting of CT enterography for inflammatory bowel disease: effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians. Abdom Radiol (NY) 2017;42:2243–2250. doi: 10.1007/s00261-017-1136-1. [DOI] [PubMed] [Google Scholar]
- 33.Wildman-Tobriner B, Allen BC, Davis JT, et al. Structured reporting of magnetic resonance enterography for pediatric Crohn’s disease: effect on key feature reporting and subjective assessment of disease by referring physicians. Curr Probl Diagn Radiol. 2017;46:110–114. doi: 10.1067/j.cpradiol.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Dickerson E, Davenport MS, Syed F et al; Michigan Radiology Quality Collaborative (2017) Effect of template reporting of brain MRIs for multiple sclerosis on report thoroughness and neurologist-rated quality: results of a prospective quality improvement project. J Am Coll Radiol 14(3):371–379.e1 [DOI] [PubMed]
- 35.Brook OR, Brook A, Vollmer CM, Kent TS, Sanchez N, Pedrosa I. Structured reporting of multiphasic CT for pancreatic cancer: potential effect on staging and surgical planning. Radiology. 2015;274:464–472. doi: 10.1148/radiol.14140206. [DOI] [PubMed] [Google Scholar]
- 36.Sahni VA, Silveira PC, Sainani NI, Khorasani R. Impact of a structured report template on the quality of MRI reports for rectal cancer staging. AJR Am J Roentgenol. 2015;205:584–588. doi: 10.2214/AJR.14.14053. [DOI] [PubMed] [Google Scholar]
- 37.Silveira PC, Dunne R, Sainani NI, et al. Impact of an information technology-enabled initiative on the quality of prostate multiparametric MRI reports. Acad Radiol. 2015;22:827–833. doi: 10.1016/j.acra.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin E, Powell DK, Kagetsu NJ. Efficacy of a checklist-style structured radiology reporting template in reducing resident misses on cervical spine computed tomography examinations. J Digit Imaging. 2014;27:588–593. doi: 10.1007/s10278-014-9703-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marcovici PA, Taylor GA. Journal Club: structured radiology reports are more complete and more effective than unstructured reports. AJR Am J Roentgenol. 2014;203:1265–1271. doi: 10.2214/AJR.14.12636. [DOI] [PubMed] [Google Scholar]
- 40.Powell DK, Lin E, Silberzweig JE, Kagetsu NJ. Introducing radiology report checklists among residents: adherence rates when suggesting versus requiring their use and early experience in improving accuracy. Acad Radiol. 2014;21:415–423. doi: 10.1016/j.acra.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Fraser L, O’Neill K, Locke R, et al. Standardising reporting of cervical lymphadenopathy in paediatric neck ultrasound: a pilot study using an evidence-based reporting protocol. Int J Pediatr Otorhinolaryngol. 2013;77:1248–1251. doi: 10.1016/j.ijporl.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 42.Chung CY, Makeeva V, Yan J, et al. Improving billing accuracy through enterprise-wide standardized structured reporting with cross-divisional shared templates. J Am Coll Radiol. 2020;17:157–164. doi: 10.1016/j.jacr.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 43.Hanna TN, Shekhani H, Maddu K, Zhang C, Chen Z, Johnson J-O. Structured report compliance: effect on audio dictation time, report length, and total radiologist study time. Emerg Radiol. 2016;23:449–453. doi: 10.1007/s10140-016-1418-x. [DOI] [PubMed] [Google Scholar]
- 44.Hawkins CM, Hall S, Zhang B, Towbin AJ. Creation and implementation of department-wide structured reports: an analysis of the impact on error rate in radiology reports. J Digit Imaging. 2014;27:581–587. doi: 10.1007/s10278-014-9699-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Larson DB, Towbin AJ, Pryor RM, Donnelly LF. Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology. 2013;267:240–250. doi: 10.1148/radiol.12121502. [DOI] [PubMed] [Google Scholar]
- 46.Hawkins CM, Hall S, Hardin J, Salisbury S, Towbin AJ. Prepopulated radiology report templates: a prospective analysis of error rate and turnaround time. J Digit Imaging. 2012;25:504–511. doi: 10.1007/s10278-012-9455-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H. Improving communication of diagnostic radiology findings through structured reporting. Radiology. 2011;260:174–181. doi: 10.1148/radiol.11101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu D, Berman GD, Gray RN. The use of structured radiology reporting at a community hospital: a 4-year case study of more than 200,000 reports. Appl Radiol. 2003;32:23–26. [Google Scholar]
- 49.Dabrowiecki A, Sadigh G, Duszak R. Chest radiograph reporting: public preferences and perceptions. J Am Coll Radiol. 2020;17:1259–1268. doi: 10.1016/j.jacr.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Camilo DMR, Tibana TK, Adôrno IF, et al. Radiology report format preferred by requesting physicians: prospective analysis in a population of physicians at a university hospital. Radiol Bras. 2019;52:97–103. doi: 10.1590/0100-3984.2018.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heye T, Gysin V, Boll DT, Merkle EM. Journal Club: structured reporting: the voice of the customer in an ongoing debate about the future of radiology reporting. AJR Am J Roentgenol. 2018;211:964–970. doi: 10.2214/AJR.18.19714. [DOI] [PubMed] [Google Scholar]
- 52.Lather JD, Che Z, Saltzman B, Bieszczad J. Structured reporting in the academic setting: what the referring clinician wants. J Am Coll Radiol. 2018;15:772–775. doi: 10.1016/j.jacr.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 53.Travis AR, Sevenster M, Ganesh R, Peters JF, Chang PJ. Preferences for structured reporting of measurement data. An institutional survey of medical oncologists, oncology registrars, and radiologists. Acad Radiol. 2014;21:785–796. doi: 10.1016/j.acra.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 54.Krupinski EA, Hall ET, Jaw S, Reiner B, Siegel E. Influence of radiology report format on reading time and comprehension. J Digit Imaging. 2012;25:63–69. doi: 10.1007/s10278-011-9424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grieve FM, Plumb AA, Khan SH. Radiology reporting: a general practitioner’s perspective. Br J Radiol. 2010;83:17–22. doi: 10.1259/bjr/16360063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sistrom CL, Honeyman-Buck J. Free text versus structured format: information transfer efficiency of radiology reports. AJR Am J Roentgenol. 2005;185:804–812. doi: 10.2214/ajr.185.3.01850804. [DOI] [PubMed] [Google Scholar]
- 57.Naik SS, Hanbidge A, Wilson SR. Radiology reports: examining radiologist and clinician preferences regarding style and content. AJR Am J Roentgenol. 2001;176:591–598. doi: 10.2214/ajr.176.3.1760591. [DOI] [PubMed] [Google Scholar]
- 58.Johnson AJ, Chen MYM, Zapadka ME, Lyders EM, Littenberg B. Radiology report clarity: a cohort study of structured reporting compared with conventional dictation. J Am Coll Radiol. 2010;7:501–506. doi: 10.1016/j.jacr.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 59.Johnson AJ, Chen MYM, Shannon Swan J, Applegate KE, Littenberg B. Cohort study of structured reporting compared with conventional dictation. Radiology. 2009;253:74–80. doi: 10.1148/radiol.2531090138. [DOI] [PubMed] [Google Scholar]
- 60.Aase A, Fabbrini AE, White KM, Averill S, Gravely A, Melzer AC. Implementation of a standardized template for reporting of incidental pulmonary nodules: feasibility, acceptability, and outcomes. J Am Coll Radiol. 2020;17:216–223. doi: 10.1016/j.jacr.2019.11.013. [DOI] [PubMed] [Google Scholar]
- 61.Alper DP, Shinagare AB, Hashemi SR, et al. Effect of a report template-enabled quality improvement initiative on use of preferred phrases for communicating normal findings in structured abdominal CT and MRI reports. AJR Am J Roentgenol. 2020;214:835–842. doi: 10.2214/AJR.19.21735. [DOI] [PubMed] [Google Scholar]
- 62.Kim SH, Sobez LM, Spiro JE et al (2020) Structured reporting has the potential to reduce reporting times of dual-energy x-ray absorptiometry exams. BMC Musculoskelet Disord 21(1):248 [DOI] [PMC free article] [PubMed]
- 63.Tuncyurek O, Garces-Descovich A, Jaramillo-Cardoso A, et al. Structured versus narrative reporting of pelvic MRI in perianal fistulizing disease: impact on clarity, completeness, and surgical planning. Abdom Radiol (NY) 2019;44:811–820. doi: 10.1007/s00261-018-1858-8. [DOI] [PubMed] [Google Scholar]
- 64.Armbruster M, Gassenmaier S, Haack M, et al. Structured reporting in petrous bone MRI examinations: impact on report completeness and quality. Int J Comput Assist Radiol Surg. 2018;13:1971–1980. doi: 10.1007/s11548-018-1828-1. [DOI] [PubMed] [Google Scholar]
- 65.Sabel BO, Plum JL, Czihal M, et al. Structured reporting of CT angiography runoff examinations of the lower extremities. Eur J Vasc Endovasc Surg. 2018;55:679–687. doi: 10.1016/j.ejvs.2018.01.026. [DOI] [PubMed] [Google Scholar]
- 66.Schoeppe F, Sommer WH, Haack M, et al. Structured reports of videofluoroscopic swallowing studies have the potential to improve overall report quality compared to free text reports. Eur Radiol. 2018;28:308–315. doi: 10.1007/s00330-017-4971-0. [DOI] [PubMed] [Google Scholar]
- 67.Schöppe F, Sommer WH, Schmidutz F et al (2018) Structured reporting of x-rays for atraumatic shoulder pain: advantages over free text? BMC Med Imaging 18(1):20 [DOI] [PMC free article] [PubMed]
- 68.Shaish H, Feltus W, Steinman J, Hecht E, Wenske S, Ahmed F. Impact of a structured reporting template on adherence to prostate imaging reporting and data system version 2 and on the diagnostic performance of prostate MRI for clinically significant prostate cancer. J Am Coll Radiol. 2018;15:749–754. doi: 10.1016/j.jacr.2018.01.034. [DOI] [PubMed] [Google Scholar]
- 69.Gassenmaier S, Armbruster M, Haasters F, et al. Structured reporting of MRI of the shoulder - improvement of report quality? Eur Radiol. 2017;27:4110–4119. doi: 10.1007/s00330-017-4778-z. [DOI] [PubMed] [Google Scholar]
- 70.Norenberg D, Sommer WH, Thasler W, et al. Structured reporting of rectal magnetic resonance imaging in suspected primary rectal cancer: potential benefits for surgical planning and interdisciplinary communication. Invest Radiol. 2017;52:232–239. doi: 10.1097/RLI.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 71.Sabel BO, Plum JL, Kneidinger N, et al. Structured reporting of CT examinations in acute pulmonary embolism. J Cardiovasc Comput Tomogr. 2017;11:188–195. doi: 10.1016/j.jcct.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 72.Walter WR, Goldberg-Stein S, Levsky JM, Cohen HW, Scheinfeld MH. A default normal chest CT structured reporting field for coronary calcifications does not cause excessive false-negative reporting. J Am Coll Radiol. 2015;12:783–787. doi: 10.1016/j.jacr.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schweitzer W, Bartsch C, Ruder TD, Thali MJ. Virtopsy approach: structured reporting versus free reporting for PMCT findings. J Forensic Radiol Imaging. 2014;2:28–33. [Google Scholar]
- 74.Karim S, Fegeler C, Boeckler D, Schwartz LH, Kauczor H-U, von Tengg-Kobligk H (2013) Development, implementation, and evaluation of a structured reporting web tool for abdominal aortic aneurysms. JMIR Res Protoc 2(2):e30 [DOI] [PMC free article] [PubMed]
- 75.Barbosa F, Maciel LMZ, Vieira EM, Azevedo Marques PM, de, Elias J, Muglia VF, Radiological reports: a comparison between the transmission efficiency of information in free text and in structured reports. Clinics (Sao Paulo) 2010;65:15–21. doi: 10.1590/S1807-59322010000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hasegawa Y, Matsumura Y, Mihara N, et al. Development of a system that generates structured reports for chest x-ray radiography. Methods Inf Med. 2010;49:360–370. doi: 10.3414/ME09-01-0014. [DOI] [PubMed] [Google Scholar]