Abstract
Background
Data on oral anticoagulant-related (OAC) intracerebral hemorrhage (ICH) incidence are scarce. Most studies on incidence time trends were performed before the introduction of Direct Oral Anticoagulants (DOACs). Between 2008 and 2018, the number of OAC-users in the Netherlands increased by 63%, with the number of DOAC-users almost equaling that of Vitamin K Antagonists (VKA)-users. We aimed to determine the recent total and OAC-related ICH incidence and assess changes over the last decade, including the effect of DOAC introduction.
Methods
All adult non-traumatic ICH patients presenting in any of three hospitals in the enclosed region of South-Limburg, the Netherlands, were retrospectively included, during two 3-year time periods: 2007–2009 and 2017–2019. OAC-related ICH was defined as ICH in patients using VKAs or DOACs. We calculated the incidence rate ratio (IRR) between the two study periods.
Results
In the 2007–2009 period, we registered 652 ICHs of whom 168 (25.8%) were OAC-related (all VKA). In the 2017–2019 period, we registered 522 ICHs, 121 (23.2%) were OAC-related (70 VKA and 51 DOAC). In 2007–2009, the annual incidence of total ICH and OAC-related ICH was 40.9 and 10.5 per 100,000 person-years, respectively, which decreased to 32.4 and 7.5 per 100,000 person-years in 2017–2019. The IRR for total ICH and OAC-related ICH was 0.67 (95%-CI: 0.60–0.75) and 0.58 (0.46–0.73), respectively.
Conclusion
Both total ICH and OAC-related ICH incidence decreased over the past decade in South-Limburg, the Netherlands, despite the aging population and increasing number of OAC-users. The introduction of DOACs, and possibly an improved cardiovascular risk management and change in OAC prescription pattern, could explain these findings.
Keywords: Primary intracerebral hemorrhage, anticoagulants, epidemiology, incidence
Introduction
Intracerebral hemorrhage (ICH) is a feared and devastating complication of the use of oral anticoagulants (OAC) and is associated with high mortality and high morbidity.1,2 Until recently, Vitamin K antagonists (VKAs) were the single and most used OAC; however, since about 2010, Direct Oral Anticoagulants (DOACs) are available, and the number of DOAC users now exceeds that of VKA users in the Netherlands. 3 Furthermore, DOACs reduce the risk of ICH about a half compared to VKAs.4,5
Recent data suggest a declining trend in stroke incidence, especially in ischemic stroke incidence.6,7 However, this remains unclear for the incidence of ICH. A Dutch population study noted a decrease in ICH incidence between 1998 and 2010, especially in patients younger than 75 years. 1 However, the two largest studies to date reporting on ICH incidence outside of the Netherlands found stable ICH incidence rates.8,9 Several other studies on ICH incidence have been performed, and while some recent studies show a decrease in ICH incidence, others show a stable or even increased ICH incidence rate.6,7,10–17 The difference in investigated time-periods, patient selection, and study size, with several studies encompassing single institutional cohorts, could explain these diverse findings.
Data on incidence of OAC-related ICH are limited and mostly dating from before the introduction of DOACs, and generally show increasing OAC-related incidence trends.10,18 We found only two studies on OAC-related ICH incidence in the past decade, including the introduction of DOAC, which both show an increase in OAC-related ICH incidence rate in the past decade.19,20
We previously determined the incidence of OAC-related ICH in South-Limburg, the Netherlands, in 2007–2009. 21 We now re-studied the incidence in the same population area. The aim of this study was to determine the recent annual total and OAC-related ICH incidence and to assess changes in incidence over the past decade, including the effect of the introduction of DOACs in the Netherlands.
Methods
Patient selection
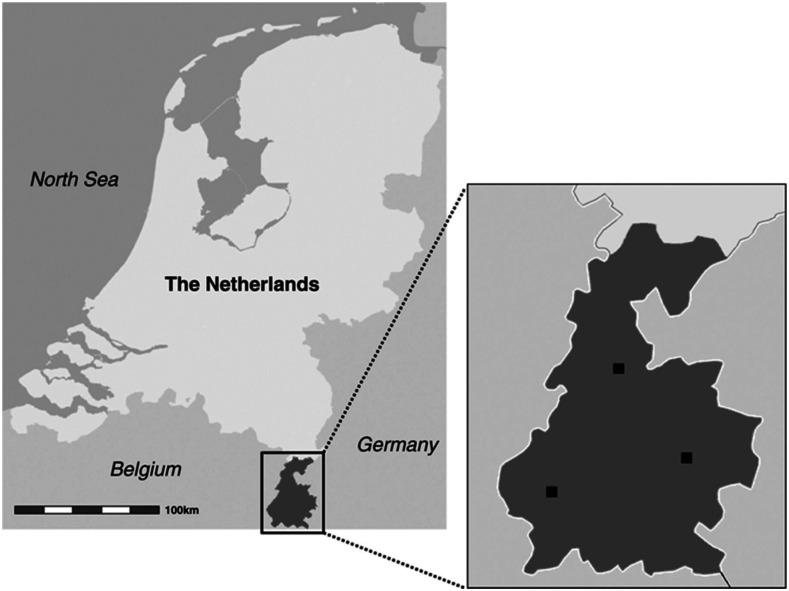
We performed a multicenter, retrospective study over two 3-year time periods. The 2007–2009 cohort has been published before and the same catchment area and in- and exclusion criteria were used for both study periods. 21 We included all consecutive patients ≥ 18 years presenting with a non-traumatic ICH at the emergency department or inpatient clinic in any of the three hospitals in the well-defined and bordered region of South-Limburg, the Netherlands (Figure 1), during two time periods: from January 2007 through December 2009 and from January 2017 through December 2019. We did not include 2020 in the study period because the COVID-19 pandemic might have influenced ICH referral and admittance policies. Recurrent ICHs were included, except for recurrences during the same hospital admission. Exclusion criteria were age < 18 years, patients living outside the postal code area of South-Limburg, traumatic ICH, non-parenchymatous intracranial hematoma (e.g., subdural, epidural, subarachnoidal, or primary intraventricular hemorrhage without visible parenchymatous involvement), ischemic stroke with hemorrhagic transformation as well as ICH associated with a brain tumor or encephalitis.
Figure 1.
The Netherlands with South-Limburg enlarged. The participating hospitals are marked. Figure adjusted from Schols et al. 21
Data collection
For clinical and radiological data, we used the same definitions for both time periods. 21 We recorded age, sex, previous ICH, hypertension (defined as treatment with antihypertensives or hypertension in medical history), diabetes mellitus (defined as treatment with antidiabetics or known diabetes mellitus in medical history), hypercholesterolemia (defined as treatment with a statin, a known medical history of hypercholesterolemia or total serum cholesterol > 6.5 mmol/l in the past 5 years), current smoking (defined as smoking during the last 6 months), Glasgow coma scale (GCS) score at admission, as well as the unadjusted in-hospital mortality. Additionally, we recorded antithrombotic treatment (Antiplatelet therapy, DOACs, VKA, Heparin/Low-Molecular-Weight Heparin (LMWH), or combinations) at the time of admission. Oral anticoagulants-related ICH was defined as an ICH in a patient using VKA or DOAC. Primary brain CT-scans were evaluated. Hematoma location was recorded as lobar, deep, infratentorial, or multifocal. The ICH volume was calculated using the validated ABC/2 formula. 22 Finally, the presence of intraventricular extension was registered.
Data on the number of adult inhabitants in South-Limburg during both study periods were retrieved from the Dutch national statistics institute. 23 Data on the total number of extramural oral anticoagulation-users (both VKAs and DOACs) in the Netherlands in 2008 and 2018 were retrieved from the Dutch Foundation for Pharmaceutical Statistics (SFK).
Data analysis
Differences in patient characteristics between 2007–2009 and 2017–2019 for all ICH and OAC-related ICH were tested using Chi-square test for categorical and ordinal variables. For continuous variables, the Mann–Whitney U test was used. Statistical analyses were performed using SPSS version 25.0.
The crude annual incidence rates of ICH and OAC-related ICH for the study periods 2007–2009 and 2017–2019 were calculated by dividing the number of (OAC-related) ICH by the total person-years at risk for ICH. Person-years at risk in each study period were calculated by adding up the average inhabitant numbers of South-Limburg in the study years. Furthermore, we calculated the crude incidence rates for different age groups, and the total incidence rate age-adjusted to the Dutch and European population of 2008 and 2018, respectively. 24 For all rates, the 95% Poisson confidence intervals (95%-CI) were calculated using Stata version 14.1. Finally, we calculated the age-strata-adjusted incidence rate ratios (IRR) and 95%-CI, by dividing the incidence rate of 2017–2019 for each age group by the incidence rate of 2007–2009 for each age group, for both total and OAC-related ICH, using Open Source Epidemiologic Statistics for Public Health version 3.01. 25
Results
We included a total of 652 ICH cases from 2007–2009 and 522 ICH cases from 2017–2019. Results from 2007–2009 were previously described and were recalculated in this study. 21
Clinical and radiological characteristics for both study periods are described in Table 1. In 2007–2009, 168 (25.8%) patients used OAC (all VKAs). In 2017–2019, 121 (23.2%) patients used OAC, of which 70 (57.9%) used VKAs and 51 (42.1%) used DOACs. Intracerebral hemorrhage patients of the 2007–2009 cohort used significantly more often antiplatelet drugs, were more often smokers, had a worse GCS-score at admission, a larger ICH volume, more often intraventricular extension, as well as a significantly higher in-hospital mortality.
Table 1.
Patient characteristics of all adult ICHs from 2007–2009 and 2017–2019.
| N | All ICHs 2007–2009 | All ICHs 2017–2019 | p value a | |
|---|---|---|---|---|
| N | 1174 | 652 | 522 | |
| Sex, men (%) | 339 (52.0) | 262 (50.2) | .539 | |
| Age, median in y [IQR] | 76.3 (66.6–83.0) | 75.0 (65.9–82.7) | .372 | |
| OAC-related ICH (%) | 168 (25.8) | 121 (23.2) | .307 | |
| VKA-related ICH (%) | 168 (25.8) | 70 (13.4) | <.001 | |
| DOAC-related | 0 | 51 | <.001 | |
| Prior ICH (%) | 1168 | 65 (10.0) | 56 (10.8) | .695 |
| Antiplatelet therapy (%) | 1163 | 228 (35.5) | 146 (28.0) | .007 |
| Hypertension (%) | 1152 | 431 (68.3) | 348 (66.8) | .586 |
| Diabetes mellitus (%) | 1157 | 110 (17.3) | 100 (19.2) | .405 |
| Hypercholesterolemia (%) | 1148 | 260 (41.5) | 234 (44.8) | .262 |
| Current smoking (%) | 835 | 113 (27.4) | 79 (18.7) | .003 |
| GCS-score ≤ 8 (%) | 1173 | 134 (20.6) | 75 (14.4) | .006 |
| ICH location (%) | ||||
| Lobar | 290 (44.5) | 240 (46.0) | ||
| Deep lobar | 272 (41.7) | 222 (42.5) | .027 | |
| Infratentorial | 90 (13.8) | 55 (10.5) | ||
| Multifocal | 0 | 5 (1.0) | ||
| ICH volume, median in cc [IQR] | 1165 | 15.6 [4.3–44.5] | 11.9 [3.5–33.0] | .023 |
| Intraventricular extension (%) | 286 (43.9) | 172 (33.0) | <.001 | |
| Hospital mortality (%) | 256 (39.3) | 160 (30.7) | .002 |
ap value for the difference between All ICHs 2007–2009 and All ICHs 2017–2019.
Abbreviations: ICH - intracerebral hemorrhage; N - number of ICH cases; y - years; IQR - interquartile range; OAC-related ICH - oral anticoagulant-related intracerebral hemorrhage; VKA-related ICH - Vitamin K-related intracerebral hemorrhage; DOAC-related ICH - Direct Oral Anticoagulant-related intracerebral hemorrhage, GCS-score - Glasgow Coma Scale-score; cc - cubic centimeter.
Differences in clinical and radiological characteristics between OAC-related ICH cases of the two cohorts are presented in Table 2. In the 2007–2009 cohort, more patients had a history of prior ICH, patients used significantly more often antiplatelet drugs in addition to OAC, more often had hypertension, had a worse GCS-score at admission, more frequent intraventricular hemorrhagic extension, as well as a significantly higher in-hospital mortality. We also compared characteristics of VKA-related ICH patients from 2007–2009 to VKA-related ICH patients from the 2017–2019 period, as well as the DOAC-related ICH patients to the VKA-related ICH patients from the 2017–2019 period. These results can be found in supplementary Table 1.
Table 2.
Patient characteristics of OAC-related ICHs from 2007–2009 and 2017–2019.
| N | OAC-ICH 2007–2009 | OAC-ICH 2017–2019 | p value | |
|---|---|---|---|---|
| N | 289 | 168 | 121 | |
| Sex, men (%) | 88 (52.4) | 60 (49.6) | .639 | |
| Age, median in y [IQR] | 79.1 [72.6–84.2] | 80.2 [72.7–86.4] | .209 | |
| Prior ICH (%) | 288 | 16 (9.6) | 4 (3.3) | .039 |
| VKA-related ICH (%) | 168 | 70 | <.001 | |
| DOAC-related ICH | 0 | 51 | <.001 | |
| Antiplatelet therapy (%) | 14 (8.3) | 3 (2.5) | .037 | |
| Hypertension (%) | 285 | 148 (90.2) | 91 (75.2) | .001 |
| Diabetes mellitus (%) | 283 | 37 (22.8) | 24 (19.8) | .543 |
| Hypercholesterolemia (%) | 284 | 83 (50.9) | 63 (52.1) | .848 |
| Current smoking (%) | 206 | 21 (19.8) | 18 (18.0) | .740 |
| GCS ≤ 8 (%) | 288 | 46 (27.4) | 17 (14.2) | .007 |
| ICH location (%) | ||||
| Lobar | 70 (41.7) | 45 (37.2) | ||
| Deep lobar | 63 (37.5) | 58 (47.9) | .056 | |
| Infratentorial | 35 (14.3) | 16 (10.7) | ||
| Multifocal | 0 | 2 (1.7) | ||
| ICH volume, median in cc [IQR] | 285 | 17.8 [5.2–62.0] | 13.3 [3.9–32.6] | .106 |
| Intraventricular extension (%) | 91 (54.2) | 45 (37.8) | .004 | |
| Hospital mortality (%) | 92 (54.8) | 47 (38.9) | .008 |
ap value for the difference between All ICHs 2007–2009 and All ICHs 2017–2019.
Abbreviations: ICH - intracerebral hemorrhage; OAC-ICH - oral anticoagulant-related ICH, N - number of OAC-ICH cases; y - years; IQR - interquartile range; VKA-related ICH - Vitamin K-related intracerebral hemorrhage; DOAC-related ICH - Direct Oral Anticoagulant-related intracerebral hemorrhage, GCS-score - Glasgow Coma Scale-score; cc - cubic centimeter.
Incidence of total ICH
For both study periods, the crude ICH incidence as well as the Dutch and European age-adjusted ICH incidence rates is listed in Table 3. In 2007–2009, the crude incidence of total ICH was 40.9 per 100,000 person-years (95%-CI: 37.8–44.1). In 2017–2019, the crude incidence of total ICH was significantly lower, being 32.4 per 100,000 person-years (95%-CI: 29.7–35.3). The IRR for total ICH is 0.67 (95%-CI: 0.60–0.75) (Table 3). The adult population of South-Limburg, the Netherlands, has increased in number and notably aged in the past decade.
Table 3.
Incidence rates per (100,000 person-years) of all adult (OAC-related) ICHs from 2007–2009 and 2017–2019.
| Age groups | 2007–2009 | 2017–2019 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICH | OAC-ICH | ICH | OAC-ICH | |||||||
| N | N | Population at Risk (person-years) | Incidence rate all ICHs (95%-CI) | Incidence rate OAC-ICH (95%-CI) | N | N | Population at Risk (person-years) | Incidence rate all ICHs (95%-CI) | Incidence rate OAC-ICH (95%-CI) | |
| 18–44 years | 20 | 12 | 628,438 | 3.2 (1.9–4.9) | 1.0 (0.5–1.7) | 11 | 11 | 574,475 | 1.9 (1.0–3.4) | 1.0 (0.5–1.7) |
| 45–54 years | 31 | 315,607 | 9.8 (6.7–13.9) | 35 | 270,446 | 12.9 (9.0–18.0) | ||||
| 55–64 years | 96 | 285,791 | 33.6 (27.2–41.0) | 76 | 301,765 | 25.2 (19.8–31.5) | ||||
| 65–74 years | 139 | 40 | 199,670 | 69.6 (58.5–82.2) | 20.0 (14.3–27.3) | 138 | 22 | 257,008 | 53.7 (45.1–63.4) | 8.6 (5.4–13.0) |
| 75–84 years | 260 | 81 | 126,912 | 204.9 (180.7–231.3) | 63.8 (50.7–79.3) | 173 | 51 | 151,083 | 114.5 (98.1–132.9) | 33.8 (25.1–44.4) |
| >85 years | 106 | 35 | 39,384 | 269.1 (220.4–325.5) | 88.9 (61.9–123.6) | 89 | 37 | 57,061 | 156.0 (125.3–191.9) | 64.8 (45.7–89.4) |
| Crude (all ages) | 652 | 168 | 1,595,800 | 40.9 (37.8–44.1) | 10.5 (9.0–12.3) | 522 | 121 | 1,611,838 | 32.4 (29.7–35.3) | 7.5 (6.2–9.0) |
| Age-adjusted rate NL | 34.8 (32.0–37.8) | 8.8 (7.4–10.4) | 27.1 (24.6–29.8) | 6.1 (4.9–7.4) | ||||||
| Age-adjusted rate EU | 37.6 (34.7–40.7) | 9.9 (8.4–11.6) | 28.6 (26.1–31.3) | 6.8 (5.6–8.2) | ||||||
Bold summarize all age categories.
The incidence of OAC-related ICH
The crude ICH incidence as well as the Dutch and European age-adjusted OAC-related ICH incidence rates is listed in Table 3. In 2007–2009, 25.8% of all adult ICHs were OAC-related. The crude incidence of OAC-related ICH was 10.5 per 100,000 person-years (95%-CI: 9.0–12.3). In 2017–2019, 23.2% of all adult ICHs were OAC-related. The crude incidence of OAC-related ICH was significantly lower compared to the 2007–2009 cohort, being 7.5 per 100,000 person-years (95%-CI: 6.2–9.0). The IRR for OAC-related ICH was 0.58 (95%-CI: 0.46–0.73) (Table 4).
Table 4.
Incidence rate ratios (IRR) for (OAC-related) ICH in the 2017–2019 cohort, with the 2007–2009 cohort serving as reference.
| Age groups | IRR all ICHs (95%-CI) | IRR OAC-ICH (95%-CI) | IRR Non-OAC-ICH (95%-CI) |
|---|---|---|---|
| 18–44 years | 0.60 (0.29–1.26) | 0.98 (0.43–2.22) | 0.88 (0.69–1.13) |
| 45–54 years | 1.32 (0.81–2.14) | ||
| 55–64 years | 0.75 (0.56–1.01) | ||
| 65–74 years | 0.77 (0.61–0.98) | 0.43 (0.25–0.72) | 0.91 (0.70–1.19) |
| 75–84 years | 0.56 (0.46–0.68) | 0.53 (0.37–0.75) | 0.57 (0.46–0.72) |
| >85 years | 0.58 (0.44–0.77) | 0.73 (0.46–1.16) | 0.51 (0.35–0.72) |
| Total (age-adjusted) | 0.67 (0.60–0.75) | 0.58 (0.46–0.73) | 0.71 (0.62–0.81) |
Anticoagulation users
The total number of OAC-users in the Netherlands increased from 352,001 in 2008 to 573,073 in 2018. In 2008 only VKAs were used as OAC, in 2018 there were 312,012 (54.5%) VKA-users and 277,077 (48.4%) DOAC-users. 26
Discussion
This study shows a significant decrease in both total ICH incidence and OAC-related ICH incidence in South-Limburg, the Netherlands, in the past decade. At the same time, the number of OAC-users has notably increased by approximately 63% in the Netherlands in recent years, with a shift from VKAs to DOACs.
The Dutch population age-adjusted total ICH incidence in our study is higher when compared to the ICH incidence of 20.7 per 100,000 person-years as reported in the Dutch population study of Jolink et al. 1 in 2015. In other studies, ICH incidence rates range from 10.0 to 46.0 per 100,000 person-years.6,8–12,14,16,27–29 However, we determined the adult incidence rate, while some studies report life-time incidence, which leads to lower incidence rates; yet other studies report incidence in an elderly population, which will result in higher incidence rates. Furthermore, the region South-Limburg is known for its lower socioeconomic and health status compared to other regions in the Netherlands, which may result in a higher incidence. 30
The total ICH incidence decreased in the past decade by approximately 33%. This reduction is mainly seen in older age groups. Some studies show similar results,11,27 though most studies report a stable or even increased incidence rate in the older population.8–10,14,16 A possible explanation for a decreased ICH incidence in our study is the further improvement of cardiovascular risk management, in particular antihypertensive management, and less smoking. Favorably, ICHs were smaller and had lower in-hospital mortality in the 2017–2019 cohort compared to the 2007–2009 cohort.
The proportion of approximately 25% OAC-related ICHs in both study periods is relatively high compared to some other studies, which show proportions ranging from 5% to 25%.9,14,17,19,31,32 Furthermore, previous studies show that the proportion of OAC-related ICH seems to have risen in recent years, yet it remained stable in our study.10,18–20
In the Netherlands, the number of OAC-users has increased by approximately 63% in the past decade. 26 Since DOACs are available, their use has risen exponentially and now exceeds that of VKAs. 3 Nevertheless, the OAC-related ICH incidence in our study shows an overall reduction of approximately 42% in the past decade (Table 3). Moreover, VKA-related ICH incidence in our study shows an overall reduction of about 67% (supplemental Table 2), even though the number of VKA-users remained relatively stable. Possible explanations for the decrease in OAC-related ICH incidence might be the increased proportional use of DOACs (carrying a lower ICH risk) and further improvement of cardiovascular risk management (especially antihypertensive management). Additionally, those VKA users having labile international normalized ratio (INR) and thereby an increased risk of major bleeding events including ICH 33 have likely been switched from VKA to DOAC. This is supported by our finding that INR values of VKA-related ICH patients from the 2007–2009 period were significantly higher on admission and more often supratherapeutic, when compared to VKA-related ICH patients from the 2017–2019 period. Lastly, the number of OAC-related ICH patients with a prior ICH was significantly higher in the 2007–2009 cohort when compared to the 2017–2019 cohort, as were the number of patients who simultaneously used OAC and antiplatelet drugs. Both the resumption of OAC after ICH and the concurrent use of OAC and antiplatelet agents might increase the risk for recurrent ICH,34,35 and these prescription pattern of clinicians could have changed over time.
In contrast to our findings, a recent Spanish study showed a threefold increase in OAC-related ICH incidence from 2008 to 2015. 19 However, their first study period was only 4 months, which was extrapolated to yearly incidence. Also, their study population varied between the different time periods, and whether anticoagulation prescription rates changed is not known. A single other recent study, performed in Denmark between 2010 and 2017, showed an increased number and proportion of OAC-ICH events as well as increase of OAC use over time, despite a stable total number of ICH events. 20 These findings are in contrast to our findings. The discrepancy in the proportion of OAC-ICH patients at the study start, being 25.8% in our study and 12% in the Danish study, likely reflects a differing study population or baseline prescription rate of OAC, which could explain these conflicting findings.
Our study has limitations. First, this study is hospital-based. Patients who were hospitalized outside the inclusion region or who were not seen in the hospital may have been missed. Still, our study region is well-demarcated, hospital care is nearby and easily accessible, and referral from general practitioners is immediate, in compliance with regional guidelines. Hence, we expect the number of missing patients to be limited. Due to the retrospective design of the study, we were unable to verify OAC compliance of the included patients. Direct Oral Anticoagulant plasma concentrations were not routinely obtained, which precludes the assessment of compliance and therapeutic range of DOAC-users. Oral anticoagulant prescription rates were only available on national basis, and therefore not specified for the catchment area. Finally, our study region is known for its poorer socioeconomic and health status, possibly leading to an overestimation of ICH incidence when extrapolating to national level.21,30
In conclusion, the total ICH and OAC-related ICH incidence decreased over the past decade in South-Limburg, the Netherlands, despite the aging population and increasing number of OAC-users. The introduction of DOACs, and possibly an improved cardiovascular risk management and change in OAC prescription pattern, could explain these findings.
Acknowledgment
None
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the medical ethical committee of the Maastricht University Medical Center (METC number 12-4–067 and 14-4-209) and Zuyderland Medical Center (METC number 13-N-44).
Informed consent: Not applicable.
Guarantor: MP
Contributorship: JS and MP conceived the study idea. All authors participated in study design. FV and MP gathered the data and performed the analysis. All authors co-wrote and revised the article for intellectual contend as well as provided approval for article submission. All authors agree to be accountable for all aspects of the work.
ORCID iDs
Michaël TJ Peeters https://orcid.org/0000-0002-6375-2264
Tobien AHCML Schreuder https://orcid.org/0000-0003-1284-7922
Julie Staals https://orcid.org/0000-0002-9502-6937
References
- 1.Jolink WMT, Klijn CJM, Brouwers PJAM, et al. Time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology 2015; 85(15): 1318–1324. [DOI] [PubMed] [Google Scholar]
- 2.Poon MTC, Fonville AF, Al-Shahi Salman R. Long-term prognosis after intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2014; 85(6): 660–667. [DOI] [PubMed] [Google Scholar]
- 3.Kengetallen SF. Anticoagulantia: DOAC blijft terrein winnen op VKA. Pharmaceutisch Weekblad 2019; 154(37): 8. [Google Scholar]
- 4.Caldeira D, Barra M, Pinto FJ, et al. Intracranial hemorrhage risk with the new oral anticoagulants: a systematic review and meta-analysis. J Neurol 2015; 262(3): 516–522. [DOI] [PubMed] [Google Scholar]
- 5.Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet 2014; 383(9921): 955–962. [DOI] [PubMed] [Google Scholar]
- 6.Madsen TE, Khoury JC, Leppert M, et al. Temporal trends in stroke incidence over time by sex and age in the GCNKSS. Stroke 2020; 51(4): 1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li L, Scott CA, Rothwell PM. Trends in stroke incidence in high-income ccountries in the 21st century: population-based study and systematic review. Stroke 2020; 51(5): 1372–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Asch CJ, Luitse MJ, Rinkel GJ, et al. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 2010; 9(2): 167–176. [DOI] [PubMed] [Google Scholar]
- 9.Fernando SM, Qureshi D, Talarico R, et al. Intracerebral hemorrhage incidence, mortality, and association with oral anticoagulation use: a population study. Stroke 2021; 52(5): 1673–1681. [DOI] [PubMed] [Google Scholar]
- 10.Lovelock CE, Molyneux A, Rothwell P. Change in incidence and aetiology of intracerebral haemorrhage in Oxfordshire, UK, between 1981 and 2006: a population-based study. Lancet Neurol 2007; 6(6): 487–493. [DOI] [PubMed] [Google Scholar]
- 11.Sacco S, Ornello R, Degan D, et al. Declining incidence of intracerebral hemorrhage over two decades in a population-based study. Eur J Neurol 2016; 23(11): 1627–1634. [DOI] [PubMed] [Google Scholar]
- 12.Gattellari M, Goumas C, Worthington J. Declining rates of fatal and nonfatal intracerebral hemorrhage: epidemiological trends in Australia. J Am Heart Assoc 2014; 3(6): e001161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schellen C, Posekany A, Ferrari J, et al. Temporal trends in intracerebral hemorrhage: evidence from the Austrian stroke unit registry. PLoS One 2019; 14(11): e0225378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lioutas VA, Beiser AS, Aparicio HJ, et al. Assessment of incidence and risk factors of intracerebral hemorrhage among participants in the Framingham heart study between 1948 and 2016. JAMA Neurol 2020; 77(10): 1252–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charidimou A, Morotti A, Valenti R, et al. Journal club: time trends in incidence, case fatality, and mortality of intracerebral hemorrhage. Neurology 2016; 86(20): e206–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Béjot Y, Cordonnier C, Durier J, et al. Intracerebral haemorrhage profiles are changing: results from the Dijon population-based study. Brain 2013; 136(Pt 2): 658–664. [DOI] [PubMed] [Google Scholar]
- 17.Carlsson M, Wilsgaard T, Johnsen SH, et al. The impact of risk factor trends on intracerebral hemorrhage incidence over the last two decades-the tromso study. Int J Stroke 2019; 14(1): 61–68. [DOI] [PubMed] [Google Scholar]
- 18.Flaherty ML, Kissela B, Woo D, et al. The increasing incidence of anticoagulant-associated intracerebral hemorrhage. Neurology 2007; 68(2): 116–121. [DOI] [PubMed] [Google Scholar]
- 19.Quintas S, Zapata-Wainberg G, Arias-Rivas S, et al. Time trends in intracerebral hemorrhage associated with oral anticoagulation and its risks factors in Spain from 2008 to 2015. Eur Neurol 2020; 84(1): 16–21. [DOI] [PubMed] [Google Scholar]
- 20.Grundtvig J, Ovesen C, Havsteen I, et al. Trends in incidence of oral anticoagulant-related intracerebral hemorrhage and sales of oral anticoagulants in capital region of Denmark 2010-2017. Eur Stroke J 2021; 6(2): 143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schols AMR, Schreuder FHBM, van Raak EPM, et al. Incidence of oral anticoagulant-associated intracerebral hemorrhage in the Netherlands. Stroke 2014; 45(1): 268–270. [DOI] [PubMed] [Google Scholar]
- 22.Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke 1996; 27(8): 1304–1305. [DOI] [PubMed] [Google Scholar]
- 23.Centraal Bureau voor de Statistiek, S . Bevolking op 1 januari en gemiddeld; geslacht, leeftijd en regio, 2020. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/03759ned/table?fromstatweb. [Google Scholar]
- 24.Eurostat . Population on 1 January by age and sex. 2020. Available from: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_pjan&lang=en. [Google Scholar]
- 25.Sullivan KM, Dean AG. Open source statistics for public health: compare two rates. Consulted on the 07th of January 2021 from: https://www.openepi.com/PersonTime2/PersonTime2.htm. [Google Scholar]
- 26.Stichting Farmaceutische Kengetallen (SFK) , 2020.
- 27.Zahuranec DB, Lisabeth LD, Sanchez BN, et al. Intracerebral hemorrhage mortality is not changing despite declining incidence. Neurology 2014; 82(24): 2180–2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan NA, McAlister FA, Pilote L, et al. Temporal trends in stroke incidence in South Asian, Chinese and white patients: a population based analysis. PLoS One 2017; 12(5): e0175556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giroud M, Delpont B, Daubail B, et al. Temporal trends in sex differences with regard to stroke incidence: the dijon stroke registry (1987-2012). Stroke 2017; 48(4): 846–849. [DOI] [PubMed] [Google Scholar]
- 30.Jansen MK. E, Op zoek naar de Limburg-factor. De gezondheidssituatie in Limburg onderzocht en verklaard. Provincie Limburg/GGD Zuid Limburg, 2015. [Google Scholar]
- 31.Cervera Á, Amaro S., Chamorro Á. Oral anticoagulant-associated intracerebral hemorrhage. J Neurol 2012; 259(2): 212–224. [DOI] [PubMed] [Google Scholar]
- 32.Liotta EM, Prabhakaran S. Warfarin-associated intracerebral hemorrhage is increasing in prevalence in the United States. J Stroke Cerebrovasc Dis 2013; 22(7): 1151–1155. [DOI] [PubMed] [Google Scholar]
- 33.Rohla M, Weiss TW, Pecen L, et al. Risk factors for thromboembolic and bleeding events in anticoagulated patients with atrial fibrillation: the prospective, multicentre observational PREvention oF thromboembolic events - European registry in atrial fibrillation (PREFER in AF). BMJ Open 2019; 9(3): e022478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poli D, Antonucci E, Vignini E, et al. Anticoagulation resumption after intracranial hemorrhage in patients treated with VKA and DOACs. Eur J Intern Med 2020; 80: 73–77. [DOI] [PubMed] [Google Scholar]
- 35.Barnes GD. Combining antiplatelet and anticoagulant therapy in cardiovascular disease. Hematol Am Soc Hematol Educ Program 2020; 2020(1): 642–648. [DOI] [PMC free article] [PubMed] [Google Scholar]