Abstract
The activities of ampicillin-sulbactam and amoxicillin-clavulanate were studied with 100 selected clinical Escherichia coli isolates with different β-lactam susceptibility phenotypes by standard agar dilution and disk diffusion techniques and with a commercial microdilution system (PASCO). A fixed ratio (2:1) and a fixed concentration (clavulanate, 2 and 4 μg/ml; sulbactam, 8 μg/ml) were used in the agar dilution technique. The resistance frequencies for amoxicillin-clavulanate with different techniques were as follows: fixed ratio agar dilution, 12%; fixed concentration 4-μg/ml agar dilution, 17%; fixed ratio microdilution, 9%; and disk diffusion, 9%. Marked discrepancies were found when these results were compared with those obtained with ampicillin-sulbactam (26 to 52% resistance), showing that susceptibility to amoxicillin-clavulanic acid cannot be predicted by testing the isolate against ampicillin-sulbactam. Interestingly, the discrimination between susceptible and intermediate isolates was better achieved with 4 μg of clavulanate per ml than with the fixed ratio. In contrast, amoxicillin susceptibility was not sufficiently restored when 2 μg of clavulanate per ml was used, particularly in moderate (mean β-lactamase activity, 50.8 mU/mg of protein) and high-level (215 mU/mg) TEM-1 β-lactamase producer isolates. Four micrograms of clavulanate per milliliter could be a reasonable alternative to the 2:1 fixed ratio, because most high-level β-lactamase-hyperproducing isolates would be categorized as nonsusceptible, and low- and moderate-level β-lactamase-producing isolates would be categorized as nonresistant. This approach cannot be applied to sulbactam, either with the fixed 2:1 ratio or with the 8-μg/ml fixed concentration, because many low-level β-lactamase-producing isolates would be classified in the resistant category. These findings call for a review of breakpoints for β-lactam–β-lactamase inhibitor combinations.
Resistance to β-lactam–β-lactamase inhibitor combinations in Escherichia coli isolates has been widely reported to be mainly due to TEM-1 β-lactamase hyperproduction, usually encoded by small multicopy plasmids (14, 31, 38). Moreover, susceptibility to these combinations in this organism is also affected by modified outer membrane permeability (24), inhibitor-resistant TEM (IRT) and OXA-type plasmid-mediated enzyme production (3, 10, 31, 40), and/or chromosomal AmpC β-lactamase hyperproduction (13, 35). It is also known that not all β-lactam–β-lactamase inhibitor combinations are equally affected by these mechanisms (1, 3, 10, 24).
A high variability in resistance frequencies to β-lactam–β-lactam inhibitor combinations has been reported, depending not only on the inhibitor but also on the susceptibility testing method and inoculum size used (1, 20, 24, 36). On the other hand, β-lactamase inhibitor stability may also decline during storage in microdilution panels used by automatic susceptibility testing systems, thus resulting in false resistance (34). In addition, there are significant differences in breakpoint categorization between different committees (2, 4, 15), and the use of a fixed inhibitor concentration or a fixed β-lactam/inhibitor concentration ratio is still the subject of debate (6, 33).
We introduced a commercial microdilution panel in our clinical laboratory for routine antimicrobial susceptibility testing. This panel contains ampicillin-sulbactam as the only β-lactam–β-lactamase inhibitor combination. Initially, the ampicillin-sulbactam susceptibility result was tentatively used as a predictor for susceptibility to other aminopenicillin–β-lactamase inhibitor combinations (mainly amoxicillin-clavulanate). During the first 2 months this system was used, more than 90% of E. coli ampicillin-resistant isolates were also apparently resistant to ampicillin-sulbactam. Because ampicillin-sulbactam resistance frequencies were higher than those previously published for amoxicillin-clavulanate (20, 25, 30, 31), we decided to compare them with those obtained for the amoxicillin-clavulanate combination by using a commercial microdilution panel from the same manufacturer with a selected collection of E. coli clinical isolates. Results from conventional disk diffusion and agar dilution methods performed at the fixed β-lactam–β-lactamase inhibitor ratio of 2:1 and at fixed concentrations of sulbactam of 8 μg/ml and clavulanic acid of 2 and 4 μg/ml were also compared.
(Part of this work was presented at the 38th Interscience Conference on Antimicrobial Agents and Chemotherapy, San Diego, Calif, 24 to 27 September 1998 [19].)
MATERIALS AND METHODS
Bacterial isolates.
A total of 100 E. coli clinical isolates, each from a separate patient and each with a different ampicillin-sulbactam susceptibility MIC by the microdilution PASCO susceptibility testing system (Difco, Detroit, Mich.), were collected during late 1997. Sixty-two ampicillin- and ampicillin-sulbactam-resistant (>16 and >16/8 μg/ml, respectively) E. coli clinical isolates were selected. In addition, 17 ampicillin-resistant, ampicillin-sulbactam-intermediate (16 and >16/8 μg/ml, respectively) and 5 ampicillin-resistant, ampicillin-sulbactam-susceptible isolates (>16 and ≤4/2 μg/ml, respectively) were included as representatives of the scarce population for which these MICs were applicable. No ampicillin-resistant isolates were found for which the ampicillin-sulbactam MICs were ≤4/2 μg/ml. Finally, the collection was completed with 16 ampicillin-susceptible isolates (ampicillin-sulbactam, ≤4/2 μg/ml) for comparative purposes. After susceptibility testing by agar dilution, PASCO microdilution, and disk diffusion for ampicillin-sulbactam, amoxicillin-clavulanate, and other antibiotics, the strains were grouped into six different phenotypes. The identification to the species level of the E. coli isolates was also performed with the microdilution PASCO system.
Susceptibility testing and antibiotics.
Susceptibility profiles obtained by the standard disk diffusion (16) and agar dilution (15) techniques and with the microdilution PASCO system were used to define different β-lactam phenotypes. For this purpose, ampicillin, amoxicillin, amoxicillin-clavulanate, cefazolin, ticarcillin, piperacillin-tazobactam, cefuroxime, cefoxitin, cefotaxime, ceftazidime, cefepime, ampicillin-sulbactam, aztreonam, imipenem, and meropenem inhibition zones and/or MICs were used. MICs of amoxicillin-clavulanate and ampicillin-sulbactam were obtained at the fixed ratio of 2:1 both with the PASCO system and by the agar dilution method. Moreover, a fixed inhibitor concentration was also used in the agar dilution method (amoxicillin-clavulanate, 2 and 4 μg/ml, respectively; and ampicillin-sulbactam, 8 μg/ml).
Antimicrobial agents for agar dilution susceptibility testing were provided by SmithKline Beecham Pharmaceuticals, Madrid, Spain (ampicillin, amoxicillin, and clavulanate) and Pfizer S. A., Madrid, Spain (sulbactam).
Phenotype definition.
E. coli isolates were classified into six different phenotypes according to the following criteria (i) S phenotype isolates were susceptible to all β-lactams tested. (ii) TL phenotype isolates were resistant to aminopenicillins and ticarcillin, susceptible to amoxicillin-clavulanate, and susceptible or intermediate to ampicillin-sulbactam (may correspond to the low-level production of TEM-1 β-lactamase). (iii) TI phenotype isolates were resistant to aminopenicillins and ticarcillin, susceptible to amoxicillin-clavulanate, and resistant to ampicillin-sulbactam (may correspond to intermediate-level production of TEM-1 β-lactamase). (iv) TH-IRT phenotype isolates were resistant to aminopenicillins and ticarcillin, intermediate or resistant to amoxicillin-clavulanate, and resistant to ampicillin-sulbactam (may correspond to high-level production of TEM-1 β-lactamase or the presence of IRT enzymes). (v) ESβL phenotype isolates were resistant to aminopenicillins, ticarcillin, and cefazolin and gave a positive result in the double disk diffusion test (8) (and therefore were expected to produce an extended-spectrum β-lactamase). (vi) CP phenotype isolates were resistant to aminopenicillins, β-lactam–β-lactamase inhibitor combinations, narrow-spectrum cephalosporins, and cephamycins (may correspond to high-level production of chromosomal cephalosporinase and/or TEM-1 β-lactamase in permeability-modified isolates).
Susceptible, intermediate, and resistant categories in β-lactam–β-lactamase inhibitor combinations were established according to the results obtained by the three different techniques (agar dilution fixed ratio, microdilution, and disk diffusion). Nevertheless, because discrepancies may exist between them (21), the possibility of a one-step discrepancy with one of these three techniques was allowed for.
Breakpoints.
The breakpoints defined by the National Committee for Clinical Laboratory Standards (NCCLS) (15, 16) were used with the results obtained by disk diffusion and with the dilution used in the fixed ratio techniques. In addition, susceptibility criteria recommended by Mesa Española de Normalización de la Sensibilidad y Resistencia a los Antimicrobianos (MENSURA) (2) were used with results for amoxicillin-clavulanate and ampicillin-sulbactam obtained at the fixed inhibitor concentrations of 2 and 8 μg/ml, respectively. The concentrations ≤4/4 μg/ml and >16/4 μg/ml were taken as susceptibility and resistance criteria, respectively, for amoxicillin-clavulanate at the fixed inhibitor concentration of 4 μg/ml.
Isoelectric focusing and β-lactamase detection.
Analytical isoelectric focusing was performed by applying crude sonic extract to Phast gels (pH gradients of 3 to 9 and 4 to 6.5) in a Phast system (Pharmacia AB, Uppsala, Sweden) (7). β-Lactamases with known pIs were focused in parallel with the extracts, by using nitrocefin (Oxoid, Ltd., Basingstoke, Hampshire, England) for detection. Specific β-lactamase activity was determined by measuring the decrease in A482 for 50 μM nitrocefin in crude sonic extracts. Enzyme activity was standardized against the total protein concentration in the enzyme preparation, as estimated by Lowry et al. (12). One unit of enzymatic activity was defined as the amount of enzyme that hydrolyzes 1 μmol of nitrocefin in 1 min at 25°C in 0.1 M sodium potasium buffer (pH 7.2).
RESULTS
According to the criteria established above, the 100 E. coli isolates were classified as susceptible, intermediate, or resistant to β-lactam–β-lactamase inhibitor combinations. Results for amoxicillin-clavulanate and ampicillin-sulbactam by disk diffusion, commercial broth microdilution, and agar dilution techniques are shown in Table 1. Isolates investigated by commercial microdilution, agar dilution (fixed ratio and 4-μg/ml clavulanate fixed concentration), and disk diffusion techniques, in contrast with the initial 62% resistance to ampicillin-sulbactam, showed similar frequencies of resistance (9 to 12%) to amoxicillin-clavulanate. On the other hand, a high rate of resistance to amoxicillin-clavulanate was observed with 2 μg of clavulanate per ml (48%) by the agar dilution method. This value was similar to that obtained by the agar dilution method with 8 μg of sulbactam per ml (49%). Remarkable discrepancies were observed regarding resistance frequencies for ampicillin-sulbactam by commercial microdilution (62%) and disk diffusion (26%) techniques. In contrast, the discrepancy was lower when results obtained by ampicillin-sulbactam disk diffusion and amoxicillin-clavulanate disk diffusion, commercial broth microdilution, and agar dilution (fixed ratio and 4 μg of clavulanate per ml) techniques were compared (Table 1).
TABLE 1.
Comparative analysis of ampicillin-sulbactam and amoxicillin-clavulanate susceptibility testing results
| Combination | Method | Amt of inhibitor | %
of isolates
|
||
|---|---|---|---|---|---|
| Susceptible | Intermediate | Resistant | |||
| Ampicillin-sulbactam | Agar dilution | 2:1 | 20 | 28 | 52 |
| Agar dilution | 8 μg/ml | 27 | 24 | 49 | |
| Microdilution | 2:1 | 21 | 17 | 62 | |
| Disk diffusion | 10 μg | 47 | 27 | 26 | |
| Amoxicillin-clavulanate | Agar dilution | 2:1 | 61 | 27 | 12 |
| Agar dilution | 2 μg/ml | 38 | 14 | 48 | |
| Agar dilution | 4 μg/ml | 63 | 20 | 17 | |
| Microdilution | 2:1 | 78 | 13 | 9 | |
| Disk diffusion | 10 μg | 74 | 17 | 9 | |
E. coli isolates were grouped by phenotypes according to the criteria stated in Materials and Methods. Phenotypes ESβL, S, TL, TI, TH-IRT, and CP included 1, 16, 31, 28, 18, and 6 isolates, respectively. Table 2 summarizes the MIC range, MIC at which 50% of the isolates are inhibited (MIC50), MIC90, and geometric mean MICs for amoxicillin-clavulanate and ampicillin-sulbactam obtained by dilution methods for each phenotype. Inhibition diameter ranges and inhibition diameter geometric means for the disk diffusion method are also shown in Table 2. Note that the MIC50 of amoxicillin-clavulanate for the TL and TI phenotypes by microdilution and agar dilution (2:1 ratio) remained just twofold above the MIC50 corresponding to the S phenotype, whereas those of ampicillin-sulbactam were four- and eightfold above the MIC50 for each phenotype, respectively (Table 2).
TABLE 2.
MICs and inhibition zones of ampicillin-sulbactam and amoxicillin-clavulanate for E. coli isolates with different β-lactam susceptibility phenotypes
| Method (amt of inhibitor) | β-Lactam phenotype (no. of
isolates)a
|
|||||
|---|---|---|---|---|---|---|
| S (16) | TL (31) | TI (28) | TH-IRT (18) | CP (6) | ESβL (1) | |
| Ampicillin-sulbactam | ||||||
| Agar dilution (2:1) | ||||||
| Range (μg/ml)b | 2–8 | 4–32 | 16–128 | 16–>256 | 32–>256 | 32 |
| MIC50 (μg/ml) | 4 | 16 | 32 | 32 | 128 | |
| MIC90 (μg/ml) | 8 | 32 | 32 | 256 | >256 | |
| Geometric mean (μg/ml) | 4.7 | 17.4 | 28.3 | 54.8 | 181.0 | |
| Agar dilution (8 μg/ml) | ||||||
| Range (μg/ml)b | 2–8 | 1–128 | 8–>256 | 16–>256 | 128–>256 | 256 |
| MIC50 (μg/ml) | 4 | 16 | 128 | >256 | >256 | |
| MIC90 (μg/ml) | 8 | 32 | >256 | >256 | >256 | |
| Geometric mean (μg/ml) | 4.3 | 15.4 | 68.9 | 181.0 | 406.3 | |
| Microdilution (2:1) | ||||||
| Range (μg/ml)b | 4 | 8–>16 | 16–>16 | >16 | >16 | >16 |
| MIC50 (μg/ml) | 4 | 16 | >16 | >16 | >16 | |
| MIC90 (μg/ml) | 4 | >16 | >16 | >16 | >16 | |
| Geometric mean (μg/ml) | 4 | 18.3 | 31.2 | >16 | >16 | |
| Disk diffusion (10 μg) | ||||||
| Range (mm)b | 18–25 | 13–20 | 6–15 | 6–18 | 6–8 | 12 |
| Geometric mean (mm) | 20.8 | 16.3 | 12.1 | 9.2 | 6.4 | |
| Amoxicillin/clavulanate | ||||||
| Agar dilution (2:1) | ||||||
| Range (μg/ml)b | 2–8 | 2–16 | 4–16 | 8–128 | 32–128 | 8 |
| MIC50 (μg/ml) | 4 | 8 | 8 | 16 | 128 | |
| MIC90 (μg/ml) | 8 | 8 | 16 | 32 | 128 | |
| Geometric mean (μg/ml) | 5.4 | 8 | 9.5 | 21.7 | 80.6 | |
| Agar dilution (4 μg/ml) | ||||||
| Range (μg/ml)b | 2–4 | 2–16 | 2–16 | 8–>256 | 128–512 | 8 |
| MIC50 (μg/ml) | 2 | 8 | 8 | 32 | 256 | |
| MIC90 (μg/ml) | 4 | 8 | 16 | 256 | >256 | |
| Geometric mean (μg/ml) | 2.6 | 7.1 | 7.4 | 40.3 | 256 | |
| Agar dilution (2 μg/ml) | ||||||
| Range (μg/ml)b | 2–8 | 8–256 | 4–128 | 16–512 | >256 | 16 |
| MIC50 (μg/ml) | 4 | 8 | 32 | 128 | >256 | |
| MIC90 (μg/ml) | 8 | 32 | 64 | >256 | >256 | |
| Geometric mean (μg/ml) | 5.4 | 15.1 | 29.9 | 128 | >256 | |
| Microdilution | ||||||
| Range (μg/ml)b | 4 | 4–8 | 4–8 | 8–>16 | 16–>16 | 8 |
| MIC50 (μg/ml) | 4 | 8 | 8 | 16 | >16 | |
| MIC90 (μg/ml) | 4 | 8 | 8 | >16 | >16 | |
| Geometric mean (μg/ml) | 4 | 7.0 | 7.0 | 17.3 | 28.5 | |
| Disk diffusion (10 μg) | ||||||
| Range (mm)b | 21–28 | 13–28 | 16–28 | 6–21 | 6–12 | 20 |
| Geometric mean (mm) | 23.4 | 20.4 | 20.8 | 15.3 | 7.8 | |
See phenotype definitions in Materials and Methods.
Expressed as ampicillin or amoxicillin values.
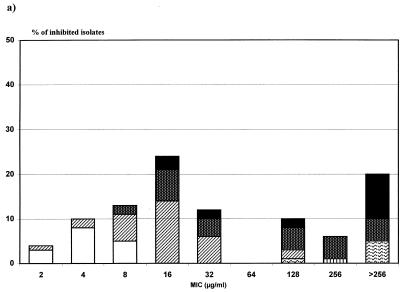
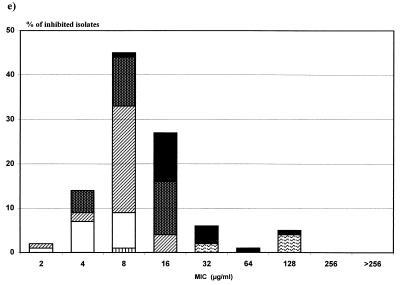
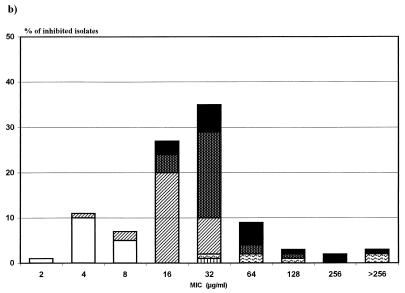
As expected, a poor correlation between amoxicillin-clavulanate and ampicillin-sulbactam MIC distributions was found, the latter being notoriously displaced to the right (Fig. 1). TL and TI phenotypes tended to be on the susceptible side of the diagram (left), while TH-IRT and CP phenotypes tended to be on the intermediate-resistant side (right).
FIG. 1.
Comparative distributions of ampicillin-sulbactam (a and
b) and amoxicillin-clavulanate (c, d, and e) MICs for E.
coli isolates with different β-lactam susceptibility phenotypes.
□, S; ▨, TL; ▩, TI; █, TH-IRT; ▥, ESβL;
 , CP. (a) Ampicillin-sulbactam
agar dilution (fixed concentration, 8 μg/ml). (b)
Ampicillin-sulbactam agar dilution (fixed ratio, 2:1). (c)
Amoxicillin-clavulanate agar dilution (fixed concentration, 2 μg/ml).
(d) Amoxicillin-clavulanate agar dilution (fixed concentration, 4
μg/ml). (e) Amoxicillin-clavulanate agar dilution (fixed ratio,
2:1).
, CP. (a) Ampicillin-sulbactam
agar dilution (fixed concentration, 8 μg/ml). (b)
Ampicillin-sulbactam agar dilution (fixed ratio, 2:1). (c)
Amoxicillin-clavulanate agar dilution (fixed concentration, 2 μg/ml).
(d) Amoxicillin-clavulanate agar dilution (fixed concentration, 4
μg/ml). (e) Amoxicillin-clavulanate agar dilution (fixed ratio,
2:1).
β-Lactamase isoelectric focusing studies were performed with five isolates each of the S, TL, and TI phenotypes and with all isolates corresponding to the TH-IRT, ESβL, and CP phenotypes. As expected, no β-lactamase bands were found for isolates with the S phenotype, and a band with a pI of 5.4 suggestive of a TEM-1 β-lactamase was detected in all isolates with TL and TI phenotypes. This pI 5.4 band was also observed in all but two isolates with the TH-IRT phenotype. One of them had a pI 7.4 band resembling an OXA-1 β-lactamase, and the other had a pI 7.6 band resembling an SHV-type β-lactamase. Four of six isolates with the CP phenotype showed a band with a pI of >8, suggesting an AmpC β-lactamase, whereas in the remaining two isolates, only the pI 5.4 band was detected. For the putative ESβL isolate, a band with a pI of between 7.8 and 8.0 was observed.
A β-lactamase specific activity was determined for five isolates each of the TL, TI, and TH-IRT phenotypes. The range and mean values, respectively, for these phenotypes were as follows: TL, 9.5 to 26.2 and 14.9 mU/mg; TI, 41.9 to 57.4 and 50.8 mU/mg; and TH, 58.5 to 543.8 and 215.4 mU/mg.
DISCUSSION
As in other members of the family Enterobacteriaceae, resistance to β-lactam antibiotics in E. coli is mainly due to the production of β-lactamases (9, 11). Nevertheless, other mechanisms affecting the activity of these antibiotics have been found. Porin-deficient mutants have been described either alone or in association with β-lactamase production (24, 28). They confer resistance to narrow-spectrum cephalosporins as well as cephamycins. This resistance phenotype is usually associated with resistance to other non-β-lactam antibiotics. Modifications in penicillin binding proteins have also been described to affect β-lactam activities (17), although this mechanism remains uncommon. Chromosomal AmpC β-lactamase hyperproduction is found in 2 to 3% of all E. coli isolates (18, 22, 28). Phenotypically, it is recognized by resistance to aminopenicillins, β-lactam–β-lactamase inhibitor combinations, narrow-spectrum cephalosporins, and cephamycins, as well as, to a lesser extent, resistance to carboxy- and ureidopenicillins and extended-spectrum cephalosporins (11). Plasmid-mediated β-lactamases account for more than 90% of aminopenicillin-resistant E. coli isolates and even 60% of all E. coli isolates in many hospitals (26, 27, 37).
Resistance to β-lactam inhibitor combinations may be caused by AmpC hyperproduction as described above, this phenotype being easy to recognize by its particular resistance mechanism. More difficult to recognize is the β-lactam–β-lactamase inhibitor combination resistance due to plasmid-mediated β-lactamases, which could represent a threat to therapeutic success. TEM-1 hyperproduction (14, 31, 39, 40) and its inhibitor-resistant variant (IRT enzymes) (31, 40) are the main factors responsible for such resistance. Moreover, β-lactamase inhibitor combination resistance might be due to the presence of other plasmid-mediated enzymes, i.e., of the OXA type (40), that may be represented in our series by the strain producing a β-lactamase with a pI of 7.4. The TEM-1 β-lactamase production level depends upon the number of plasmid copies, number of gene copies per plasmid, and promoter efficiency (10, 24). Various investigators have already pointed out the correlation between the level of resistance to inhibitor combinations and the amount of enzyme produced (35). This correlation was also observed in our study, because the TI, TL, and TH-IRT phenotypes, defined according the β-lactam–β-lactamase inhibitor combination resistance level, were shown to be dependent on the amount of enzyme produced as well. The level of β-lactamase production affects susceptibility to amoxicillin-clavulanate as well as ampicillin-sulbactam, although to a lesser extent, with organisms remaining susceptible to the first combination when small and moderate amounts of enzyme are produced.
Clavulanate has been previously described to be a better inhibitor of broad-spectrum plasmid-mediated β-lactamases than sulbactam (20, 21). This can certainly be elucidated from our results as well. Note that only 9, 9, and 12 isolates of the 52 isolates resistant to ampicillin-sulbactam by agar dilution were resistant to amoxicillin-clavulanate by disk diffusion, PASCO microdilution, and agar dilution at a fixed inhibitor ratio, respectively. In general, distributions of the MICs of both β-lactam–β-lactamase inhibitor combinations were similar, but were 1 to 2 dilutions higher for ampicillin-sulbactam (Fig. 1). The TL and TI phenotypes were essentially susceptible to amoxicillin-clavulanate, whereas TH-IRT was intermediate or resistant. For ampicillin-sulbactam, even the TL phenotype was not fully susceptible. With the NCCLS criteria, discrepancies between both combinations were noted in our series, and thus ampicillin-sulbactam is a bad predictor for amoxicillin-clavulanate susceptibility; therefore, both antibiotics or, specifically, the one that is intended to be used as a therapeutic option must be tested.
Susceptibility testing of β-lactam–β-lactamase inhibitor combinations at a fixed ratio or at a fixed concentration is still controversial (6, 22, 33). The peak clavulanate concentration in serum after oral administration is not much higher than 2 μg/ml, whereas the concentration of sulbactam in serum reaches 16 μg/ml (5, 32). If breakpoints and criteria established by French and Spanish committees for the antibiogram (2, 4) are used, the results are dramatically different for amoxicillin-clavulanate. Overall, nonsusceptibility (intermediate plus resistant) increases up to 62%, thus showing that 2 μg of clavulanate per ml is not enough to restore amoxicillin susceptibility on many occasions. By using either the Spanish or French criteria (8-μg/ml sulbactam fixed concentration), ampicillin-sulbactam resistance remains at about the same level as with NCCLS criteria, but this is not surprising, because both breakpoints are quite similar (8/8 versus 8/4 μg/ml, respectively). Clinical data support the susceptibility 8- and 4-μg/ml breakpoint for amoxicillin-clavulanate, although the concentration of 4 μg of clavulanate per ml is hardly attainable in serum (32). Moreover, a dynamic interaction of β-lactamase inhibitors with newly synthesized enzyme is expected to occur. Multiple doses over a 24-h period are administered to patients, whereas a single inhibitor concentration is used for susceptibility testing. This rationale may justify an initial inhibitor concentration in susceptibility testing higher than that reached in serum.
Some investigators have suggested the possibility of using amoxicillin with 4 μg of clavulanate per ml (32, 33), keeping 8/4 μg/ml as the breakpoints for susceptibility. This approach could displace the intermediate isolates to a slightly higher MIC and help separate truly susceptible isolates from intermediate-resistant isolates (Fig. 1d). Such criteria could be a reasonable alternative to the 2:1 ratio combination. In the present study, we found similar results with the susceptibility frequencies of the 2:1 ratio and 4-μg/ml concentration of clavulanate being quite similar. Intermediate and resistant frequencies were lower and higher, respectively, with 4 μg of clavulanate per ml than the corresponding values for the 2:1 ratio (Table 1). This finding is consistently observed with the analysis of MIC50s and MIC90s (Table 2).
For ampicillin-sulbactam, based on the attainable concentration in serum and the discrepancies from disk diffusion results, a 1:1 fixed ampicillin-sulbactam ratio or even a 16-μg/ml fixed sulbactam concentration (breakpoints of 8/8 and 8/16 μg/ml, respectively) could be considered, as some investigators have pointed out (32). This change would reduce the discrepancies from the disk diffusion method and the amoxicillin-clavulanate results; moreover, it probably would correlate with the difference in levels reached by both antibiotics in serum.
In conclusion, discrepancies found between amoxicillin-clavulanate and ampicillin-sulbactam resistance levels are high in E. coli, at least when the NCCLS breakpoint criteria are used. The susceptibility of the former is difficult to predict when the susceptibility results from the latter are used. These discrepancies seem to be related in part to the amount of enzyme produced and therefore could be useful to phenotypically detect β-lactamase hyperproduction. Four micrograms of clavulanate per milliliter could be a reasonable alternative to the 2:1 fixed ratio, because most high-level β-lactamase-hyperproducing isolates would be categorized as nonsusceptible and low- and moderate-level β-lactamase-producing isolates would be categorized as nonresistant. This approach cannot be applied to sulbactam, either with a fixed 2:1 ratio or with an 8-μg/ml fixed concentration, because many low-level β-lactamase-producing isolates would be classified in the resistant category. These findings call for a review of breakpoints for β-lactam–β-lactamase inhibitor combinations.
REFERENCES
- 1.Aldridge K E, Sanders C V, Marier R L. Variation in the potentiation of β-lactam antibiotic activity by clavulanic acid and sulbactam against multiply antibiotic-resistant bacteria. J Antimicrob Chemother. 1986;17:463–469. doi: 10.1093/jac/17.4.463. [DOI] [PubMed] [Google Scholar]
- 2.Baquero F, Martínez-Beltrán J, Cantón R los Restantes Miembros del Grupo MENSURA. Criterios del Grupo MENSURA para la definición de los puntos críticos de sensibilidad a los antibióticos. Rev Esp Quimioter. 1997;10:303–313. [Google Scholar]
- 3.Blázquez J, Baquero M-R, Cantón R, Alos I, Baquero F. Characterization of a new TEM-type beta-lactamase resistant to clavulanate, sulbactam, and tazobactam in a clinical isolate of Escherichia coli. Antimicrob Agents Chemother. 1993;37:2059–2063. doi: 10.1128/aac.37.10.2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comité de ĺ Antibiograme de la Société Française de Microbiologie. Statement 1996. CA-SFM. Zone sizes and MIC breakpoints for non-fastidious organisms. Clin Microbiol Infect. 1996;2(Suppl. 1):S46–S49. [PubMed] [Google Scholar]
- 5.Foulds G. Pharmacokinetics of sulbactam/ampicillin in humans: a review. Rev Infect Dis. 1986;8:S503–S511. doi: 10.1093/clinids/8.supplement_5.503. [DOI] [PubMed] [Google Scholar]
- 6.Greenwood D. Fixed or variable concentrations of beta-lactamase inhibitors in in-vitro tests? J Antimicrob Chemother. 1996;38:17–20. doi: 10.1093/jac/38.1.17. [DOI] [PubMed] [Google Scholar]
- 7.Huovinen S. Rapid isoelectric focusing of plasmid-mediated β-lactamases with Pharmacia PhastSystem. Antimicrob Agents Chemother. 1988;32:1730–1732. doi: 10.1128/aac.32.11.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jarlier V, Nicolas M H, Fournier G, Philippon A. Extended spectrum β-lactamases conferring transferable resistance to newer β-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis. 1988;10:867–878. doi: 10.1093/clinids/10.4.867. [DOI] [PubMed] [Google Scholar]
- 9.Liu P Y, Gur D, Hall L-M, Livermore D M. Survey of the prevalence of beta-lactamases amongst 1000 gram-negative bacilli isolated consecutively at the Royal London Hospital. J Antimicrob Chemother. 1997;39:1–3. doi: 10.1093/jac/30.4.429. [DOI] [PubMed] [Google Scholar]
- 10.Livermore D M. Determinants of the activity of betalactamase inhibitor combinations. J Antimicrob Chemother. 1993;31:9–21. doi: 10.1093/jac/31.suppl_a.9. [DOI] [PubMed] [Google Scholar]
- 11.Livermore D M. β-Lactamases in laboratory and clinical resistance. Clin Microbiol Rev. 1995;8:557–584. doi: 10.1128/cmr.8.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowry O H, Rosebrough N J, Farr A L, Randall R J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265–275. [PubMed] [Google Scholar]
- 13.Marre R, Aleksic S. Beta-lactamase types and beta-lactam resistance of Escherichia colistrains with chromosomally mediated ampicillin resistance. Eur J Clin Microbiol Infect Dis. 1990;9:44–46. doi: 10.1007/BF01969534. [DOI] [PubMed] [Google Scholar]
- 14.Martinez J L, Cercenado E, Rodríguez-Creixems M, Vicente-Pérez M F, Delgado-Iribarren A, Baquero F. Resistance to beta-lactam/clavulanate. Lancet. 1987;ii:1473. doi: 10.1016/s0140-6736(87)91180-9. [DOI] [PubMed] [Google Scholar]
- 15.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A4. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 16.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial disk susceptibility tests. Approved standard M2-A6. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 17.Neu H C. Penicillin-binding proteins and beta-lactamases: their effects on the use of cephalosporins and other new beta-lactams. Curr Clin Top Infect Dis. 1987;8:37–61. [PubMed] [Google Scholar]
- 18.Normark S, Lindquist S, Lindberg F. Chromosomal beta-lactam resistance in enterobacteria. Scand J Infect Dis. 1986;49:38–45. [PubMed] [Google Scholar]
- 19.Oliver, A., M. Pérez-Vázquez, M. Martínez-Ferrer, F. Baquero, S. Valdezate, and R. Cantón. Ampicillin-sulbactam and co-amoxiclav susceptibility testing on Escherichia coli: fixed ratio or fixed concentration?, abstr. D-46, p. 142. In Program and abstracts of the 38th Interscience Conference on Antimicrobial Agents and Chemotherapy. American Society for Microbiology, Washington, D.C.
- 20.O’Shaughnessy E M, Fahle G A, Witebsky F G. Correlation of in vitro susceptibility results for amoxicillin-clavulanate and ampicillin-sulbactam tested against Escherichia coli. J Clin Microbiol. 1997;35:1902–1903. doi: 10.1128/jcm.35.7.1902-1903.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Payne D J, Cramp R, Winstanley D J, Knowles D J C. Comparative activities of clavulanic acid, sulbactam, and tazobactam against clinically important β-lactamases. Antimicrob Agents Chemother. 1994;38:767–772. doi: 10.1128/aac.38.4.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pfaller M A, Barry L, Fuchs P C, Gerlach E H, Hardy D J, McLaughlin J C. Comparison of fixed concentration and fixed ratio options for dilution susceptibility testing of gram-negative bacilli to ampicillin and ampicillin/sulbactam. Eur J Clin Microbiol Infect Dis. 1993;12:356–362. doi: 10.1007/BF01964434. [DOI] [PubMed] [Google Scholar]
- 23.Piddock L J, Walters R N, Jin Y F, Turner H L, Gascoyne-Binzi D M, Hawkey P M. Prevalence and mechanism of resistance to ’third-generation’ cephalosporins in clinically relevant isolates of Enterobacteriaceaefrom 43 hospitals in the UK, 1990–1991. J Antimicrob Chemother. 1997;39:177–187. doi: 10.1093/jac/39.2.177. [DOI] [PubMed] [Google Scholar]
- 24.Reguera J A, Baquero F, Pérez-Díaz J C, Martínez J L. Factors determining resistance to beta-lactam combined with beta-lactamase inhibitors in Escherichia coli. J Antimicrob Chemother. 1991;27:569–575. doi: 10.1093/jac/27.5.569. [DOI] [PubMed] [Google Scholar]
- 25.Roy C, Segura C, Torrellas A, Reig R, Teruel D, Hermida M. Activity of amoxycillin/clavulanate against beta-lactamase-producing Escherichia coli and Klebsiella spp. J Antimicrob Chemother. 1989;24:41–47. doi: 10.1093/jac/24.suppl_b.41. [DOI] [PubMed] [Google Scholar]
- 26.Roy C, Segura C, Tirado M, Reig R, Hermida M, Teruel D, Foz A. Frequency of plasmid-determined beta-lactamases in 680 consecutively isolated strains of Enterobacteriaceae. Eur J Clin Microbiol. 1985;4:146–147. doi: 10.1007/BF02013586. [DOI] [PubMed] [Google Scholar]
- 27.Sanders C C, Sanders W E. Beta-lactam resistance in gram-negative bacteria: global trends and clinical impact. Clin Infect Dis. 1992;15:824–839. doi: 10.1093/clind/15.5.824. [DOI] [PubMed] [Google Scholar]
- 28.Sawai T, Yamaguchi A, Hiruma R. Effect of interaction between outer membrane permeability and beta-lactamase production on resistance to beta-lactam agents in gram-negative bacteria. Rev Infect Dis. 1988;10:761–764. doi: 10.1093/clinids/10.4.761. [DOI] [PubMed] [Google Scholar]
- 29.Schumacher H, Skibsted U, Skov R, Scheibel J. Cefuroxime resistance in Escherichia coli. Resistance mechanisms and prevalence. APMIS. 1996;104:531–538. doi: 10.1111/j.1699-0463.1996.tb04908.x. [DOI] [PubMed] [Google Scholar]
- 30.Seetulsingh P S, Hall L M, Livermore D M. Activity of clavulanate combinations against TEM-1 beta-lactamase-producing Escherichia coliisolates obtained in 1982 and 1989. J Antimicrob Chemother. 1991;27:749–759. doi: 10.1093/jac/27.6.749. [DOI] [PubMed] [Google Scholar]
- 31.Stapleton P, Wu P-J, King A, Shannon K, French G, Phillips I. Incidence and mechanisms of resistance to the combination of amoxicillin and clavulanic acid in Escherichia coli. Antimicrob Agents Chemother. 1995;39:2478–2483. doi: 10.1128/aac.39.11.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stephen G, Jenkins P D. Antimicrobial susceptibility tests for β-lactam–β-lactamase inhibitor: predictors of clinical efficacy? Clin Microbiol Newsl. 1992;14:89–91. [Google Scholar]
- 33.Thomson C J, Miles R S, Amyes S G. Susceptibility testing with clavulanic acid: fixed concentration versus fixed ratio. Antimicrob Agents Chemother. 1995;39:2591–2592. doi: 10.1128/aac.39.11.2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valdezate S, Martínez-Beltrán J, de-Rafael L, Baquero F, Cantón R. Beta-lactam stability in frozen microdilution PASCO MIC panels using strains with known resistance mechanisms as biosensors. Diagn Microbiol Infect Dis. 1996;26:53–61. doi: 10.1016/s0732-8893(96)00178-2. [DOI] [PubMed] [Google Scholar]
- 35.Vanjak D, Mulleys C, Picard B, Bergogne-Berezin E, Lambert-Zechovsky N. Activity of beta-lactamase inhibitor combinations on Escherichia coliisolates exhibiting various patterns of resistance to beta-lactam agents. Eur J Clin Microbiol Infect Dis. 1995;14:972–978. doi: 10.1007/BF01691379. [DOI] [PubMed] [Google Scholar]
- 36.Villar H E, Jugo M B, Fernández-Lausi A, Farinati A E. Errores del método de difusión en agar para predecir la susceptibilidad de Escherichia coli frente a ampicilina-sulbactam y amoxicilina-ácido clavulánico. Enferm Infecc Microbiol Clin. 1996;14:308–310. [PubMed] [Google Scholar]
- 37.Wiedemann B, Kliebe C, Kresken M. Epidemiology of beta-lactamases. J Antimicrob Chemother. 1989;24:1–22. doi: 10.1093/jac/24.suppl_b.1. [DOI] [PubMed] [Google Scholar]
- 38.Wu P J, Shannon K, Phillips I. Mechanisms of hyperproduction of TEM-1 β-lactamase by clinical isolates of Escherichia coli. J Antimicrob Chemother. 1995;36:927–939. doi: 10.1093/jac/36.6.927. [DOI] [PubMed] [Google Scholar]
- 39.Wu P-J, Shannon K, Phillips I. Effect of hyperproduction of TEM-1 β-lactamase on in vitro susceptibility of Escherichia colito β-lactam antibiotics. Antimicrob Agents Chemother. 1994;38:494–498. doi: 10.1128/aac.38.3.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou X Y, Bordon F, Sirot D, Kitzis M-D, Gutmann L. Emergence of clinical isolates of Escherichia coliproducing TEM-1 derivatives or an OXA-1 β-lactamase conferring resistance to β-lactamase inhibitors. Antimicrob Agents Chemother. 1994;38:1085–1089. doi: 10.1128/aac.38.5.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]