Abstract
Inflammatory myofibroblastic tumor (IMT) of the urinary bladder is a rare soft tissue tumor characterized by spindle cell proliferation with inflammatory cell infiltration. We present a case of bladder IMT occurring in a 6-year-old boy. Pretreatment CT images depicted a polypoid and broad-based mass measuring 18 mm in the superior to the front wall of the bladder, and the mass showed isodensity on precontrast image and ring enhancement of the mass after the intravenous administration of contrast material. Pelvic MRI demonstrated the 18 × 17 × 16 mm broad-based mass, suggesting submucosal tumor in the dome of the bladder. The mass showed low-to-moderate signal intensity on T1-weighted images and slight high signal intensity on T2-weighted images and restricted diffusion with low signal intensity on ADC map and abnormal high signal intensity on DWI. Transurethral resection of the bladder tumor and partial cystectomy were undertaken, and the pathology revealed IMT of the bladder. We suggest its inclusion in the differential diagnosis of cases of a polypoid and broad-based mass on the superior wall or the front wall of the bladder with ring enhancement on contrast-enhanced CT and MRI.
Keywords: Inflammatory myofibroblastic tumor, Bladder, Computed tomography, Magnetic resonance imaging
Introduction
Inflammatory myofibroblastic tumor (IMT) is a rare intermediate soft tissue tumor characterized by spindle cell proliferation with inflammatory cell infiltration. IMT has been termed as plasma cell granuloma, inflammatory pseudotumor, pseudomalignant spindle cell proliferation, or pseudosarcomatous myofibroblastic tumor [1]. IMT arises from any organs, such as the lung, retroperitoneum, omentum, abdominal cavity, and retroperitoneum. IMT of the bladder was first described by Roth [2] in 1980. Although rare, comprising less than 1% of all bladder tumors, the bladder is the most common site involved in the genitourinary tract. Because clinical symptoms and laboratory test results lack specificity for the diagnosis of urinary system IMTs, preoperative imaging-based examination is very important for identifying such IMTs and choosing the appropriate way to manage them. We report computed tomography (CT) and magnetic resonance imaging (MRI) findings.
Case Report
A 6-year-old boy was referred to our hospital for further examination of a bladder tumor. The chief complaint was abdominal pain and had a medical history of Kawasaki disease and herpes. He had negative history of urinary tract infections, surgical procedures, and urethral instrumentation. Systemic review and physical examination were unremarkable. The hematological and biochemical data and urine cytology showed no abnormal findings.
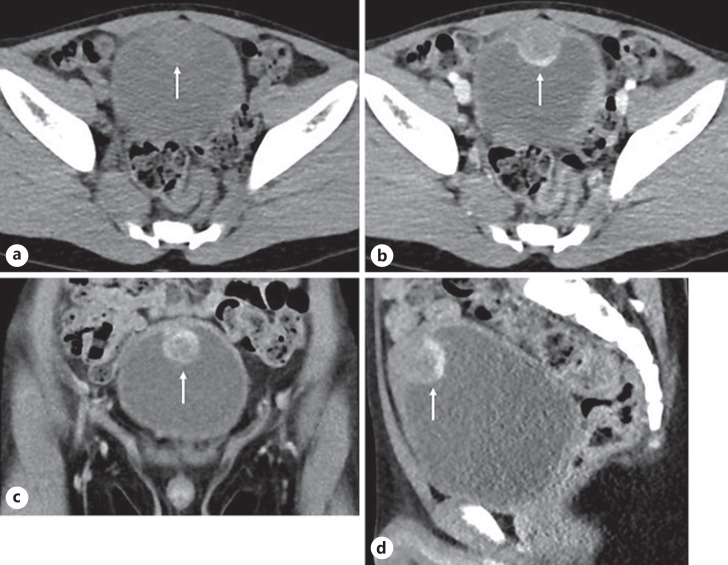
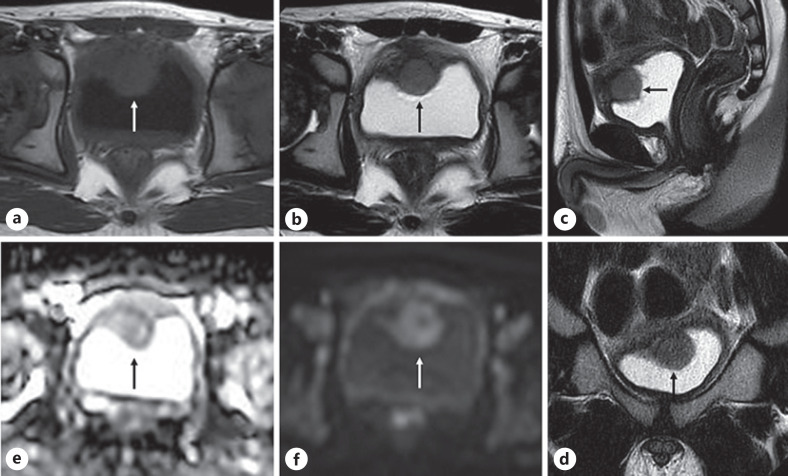
Urinary tract ultrasound showed an immobile 2-cm lesion, seen at the front wall of the bladder with evidence of internal vascularity on Doppler ultrasound. CT demonstrated the polypoid and broad-based mass measuring 18 mm in the superior to the front wall of the bladder. The mass showed isodensity on precontrast image and ring enhancement of the mass after the intravenous administration of contrast material (Fig. 1). No lymph node swelling or distant metastasis was observed. Pelvic MRI demonstrated the 18 × 17 × 16 mm broad-based mass, suggesting submucosal tumor in the dome of the bladder. The mass showed low-to-moderate signal intensity on T1-weighted images and slight high signal intensity on T2-weighted images and restricted diffusion with low signal intensity on apparent diffusion coefficient (ADC) map and abnormal high signal intensity on diffusion-weighed imaging (DWI) (Fig. 2).
Fig. 1.
CT demonstrated the polypoid and broad-based mass (arrow) measuring 18 mm in the superior to the front wall of the bladder. The mass showed isodensity on precontrast image (a) and ring enhancement of the mass after the intravenous administration of contrast material (b–d).
Fig. 2.
Pelvic MRI demonstrated the 18 × 17 × 16 mm broad-based mass (arrow), suggesting submucosal tumor in the dome of the bladder. The mass showed low-to-moderate signal intensity on T1-weighted images (a) and slight high signal intensity on T2-weighted images (b–d) and restricted diffusion with low signal intensity on apparent diffusion coefficient map (e) and abnormal high signal intensity on diffusion-weighed imaging (f).
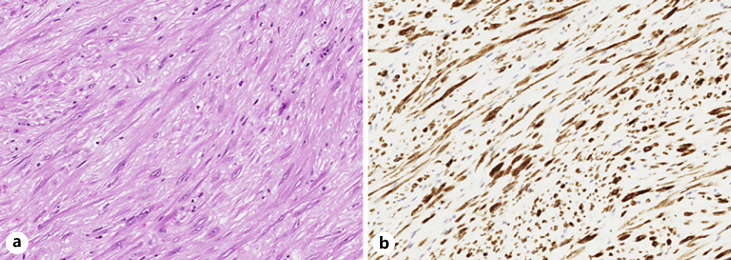
He underwent cystoscopy and transurethral resection of the bladder tumor (TURBT). Cystoscopy revealed a broad-based tumor in the superior wall of the bladder. Urothelium cell presents the varus nature, an alveolar growth pattern; however, all the possibility of reactive lesion, benign, low malignant lesion was suspected, and no definitive diagnosis was determined. He received partial cystectomy, and the pathology revealed inflammatory myofibroblastic tumor of the urinary bladder. Microscopic examination of the lesion showed submucosal spindle cells proliferation arranged in a fascicular and storiform pattern (Fig. 3). The spindle tumor cells had no obvious pleomorphism and mitoses. The lesion abuts on adjacent muscularis propria. Immunohistochemically, the spindle tumor cells were strongly positive for anaplastic lymphoma kinase (ALK) and smooth-muscle actin and desmin (focal). Ki-67 labeling index was low (1%).
Fig. 3.
a Microscopic examination of the lesion showed submucosal spindle cells proliferation arranged in a fascicular and storiform pattern. b Immunohistochemically, the spindle tumor cells were strongly positive for anaplastic lymphoma kinase.
Discussion
IMT rarely involves the urinary bladder. A systematic review by Teoh et al. [3] in 2014 evaluated 182 cases of IMT of the urinary bladder in the literature. Another literature review by Song et al. [1] in 2019 revealed 16 more patients, for a total of 198 cases of IMT of the urinary bladder to date. The most frequently reported symptom is gross hematuria followed by urinary pain, dysuria, and increased urination frequency. The tumor has been observed in a wide range of ages, from around 30 to 50 years, with an equal balance of genders. Although the causes of this tumor have long been believed to be urinary tract infection, surgical invasion, diabetes mellitus, and immune disorders, a number of idiopathic cases have also been reported [1]. Reported IMTs were around 2–5 cm in most cases, but 1 case showed 37.5 cm.
IMT in the urinary system commonly occur in the superior wall or the front wall of the bladder. The observation that polypoid nodules on the bladder walls show ring enhancement on contrast-enhanced CT may be valuable in the diagnostic imaging of IMTs of the urinary system [4]. Liang et al. [4] also reported CT manifestations of IMT in the urinary system in 8 patients, and that their shape was either round-like (n = 7) or round (n = 1), and their size ranged from 1.5 × 2.0 cm2 to 3.7 × 5.2 cm2, tumor margins were smooth (n = 5) or lobulated (n = 3), boundaries were clear (n = 5) or ill defined (n = 3), unenhanced CT scans showed a low density (n = 4), isodensity (n = 3), or a slightly high density (n = 1), the density noted on the unenhanced CT scans was homogeneous (n = 7) or heterogeneous (n = 1), the contrast-enhanced scans showed ring enhancement (n = 3) or significantly heterogeneous enhancement (n = 4), and the type of dynamic enhancement was persistent (n = 6) or washout (n = 1). On MRI, bladder IMTs have diverse manifestations. They may show low-to-moderate signal intensity on T1-weighted images, and they may show low-to-high signal intensity or mixed signal intensity with variable contrast-enhanced manifestations [5].
TURBT is often performed for pathological examination, and additional TURBT or a partial cystectomy option is chosen according to the histopathological result. Due to the risk of local recurrence, complete resection is recommended. On the other hand, some tumors were treated by steroids or anti-inflammatory drugs without radical treatment [6]. IMT has a relatively good prognosis and is considered to be a tumor with intermediate biologic potential because of its low risk of distant metastases [7]. IMTs of the bladder have a local tumor recurrence rate after surgery of only 4%, and no patients with distant metastases have been reported [3].
Histologically, IMT is characterized by proliferation of myofibroblastic spindle cells and inflammatory cell infiltration. Recently, ALK protein expression in IMT has been reported [8]. The most important entities in differential diagnosis are sarcomatoid urothelial carcinoma, leiomyosarcoma, and rhabdomyosarcoma because of the similarity of histological findings. Finding cytological atypia and atypical mitotic figures and immunostaining with ALK are useful to differentiate IMT from other malignant spindle cell tumors.
Conclusion
We present a case of inflammatory myofibroblastic tumor of the bladder dome with ring enhancement and suggest its inclusion in the differential diagnosis of cases of a polypoid and broad-based mass on the superior wall or the front wall of the bladder with ring enhancement on contrast-enhanced CT and MRI.
Statement of Ethics
This report complies with the guidelines for human studies and includes evidence that the research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The authors have no ethical conflicts to disclose. Written informed consent was obtained from the patient and from the parents of the patient for publication of this case report and any accompanying images. The paper is exempt from ethical committee approval because the Institutional Review Board of Hyogo Medical College of Medicine admits case report without ethical committee approval.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors did not receive any funding for this study.
Author Contributions
Concept and design: K.K.; acquisition of data: Y.F., H.K., M.Z., T.O., H.Y., Y.I., T.Y., and S.H.; drafting of the manuscript: K.K.; critical revision of the manuscript for important intellectual content: K.Y. All authors approved the final version of the manuscript.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
- 1.Song D, Jiao W, Gao Z, Liu N, Zhang S, Zong Y, et al. Inflammatory myofibroblastic tumor of urinary bladder with severe hematuria: a case report and literature review. Medicine. 2019 Jan;98((1)):e13987. doi: 10.1097/MD.0000000000013987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth JA. Reactive pseudosarcomatous response in urinary bladder. Urology. 1980 Dec;16((6)):635–637. doi: 10.1016/0090-4295(80)90578-6. [DOI] [PubMed] [Google Scholar]
- 3.Teoh JY, Chan NH, Cheung HY, Hou SS, Ng CF. Inflammatory myofibroblastic tumors of the urinary bladder: a systematic review. Urology. 2014 Sep;84((3)):503–508. doi: 10.1016/j.urology.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 4.Liang W, Zhou X, Xu S, Lin S. CT Manifestations of inflammatory myofibroblastic tumors (inflammatory pseudotumors) of the urinary system. AJR Am J Roentgenol. 2016 Jun;206((6)):1149–1155. doi: 10.2214/AJR.15.14494. [DOI] [PubMed] [Google Scholar]
- 5.Fujiwara T, Sugimura K, Imaoka I, Igawa M. Inflammatory pseudotumor of the bladder: MR findings. J Comput Assist Tomogr. 1999 Jul–Aug;23((4)):558–561. doi: 10.1097/00004728-199907000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Berger A, Kim C, Hagstrom N, Ferrer F. Successful preoperative treatment of pediatric bladder inflammatory myofibroblastic tumor with anti-inflammatory therapy. Urology. 2007 Aug;70((2)):372–375. doi: 10.1016/j.urology.2007.04.047. [DOI] [PubMed] [Google Scholar]
- 7.Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now? J Clin Pathol. 2008;61((4)):428–437. doi: 10.1136/jcp.2007.049387. [DOI] [PubMed] [Google Scholar]
- 8.Tsuzuki T, Magi-Galluzzi C, Epstein JI. ALK-1 expression in inflammatory myofibroblastic tumor of the urinary bladder. Am J Surg Pathol. 2004 Dec;28((12)):1609–1614. doi: 10.1097/00000478-200412000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.