Abstract
Few clinical datasets exist in dentistry to conduct secondary research. Hence, a novel dental data repository called BigMouth was developed, which has grown to include 11 academic institutions contributing Electronic Health Record data on over 4.5 million patients. The primary purpose for BigMouth is to serve as a high-quality resource for rapidly conducting oral health-related research. BigMouth allows for assessing the oral health status of a diverse US patient population; provides rationale and evidence for new oral health care delivery modes; and embraces the specific oral health research education mission. A data governance framework that encouraged data sharing while controlling contributed data was initially developed. This transformed over time into a mature framework, including a fee schedule for data requests and allowing access to researchers from noncontributing institutions. Adoption of BigMouth helps to foster new collaborations between clinical, epidemiological, statistical, and informatics experts and provides an additional venue for professional development.
Keywords: dentistry, Research Patient Data Repositories, learning healthcare system, data governance
INTRODUCTION
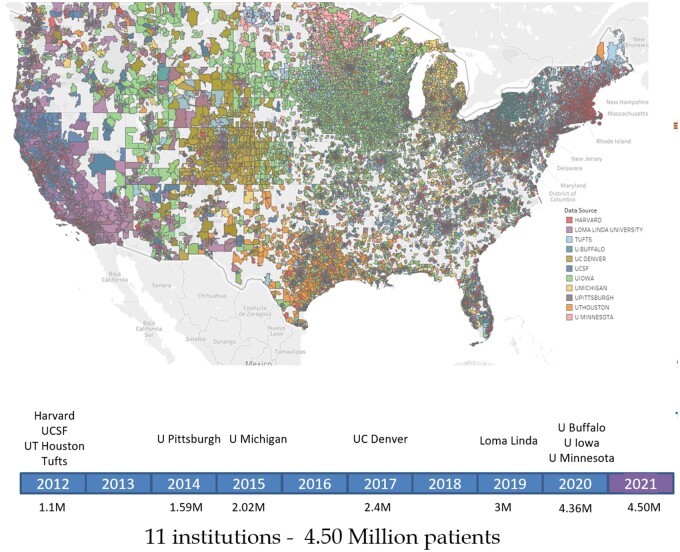
Each year in the United States, over 195 000 dental practitioners provide care to more than 127 million patients.1,2 Despite significant advances over time, researchers have had limited access to oral health datasets. While different Research Patient Data Repositories (RPDRs) exist, they rarely contain information on oral health that is associated with chronic conditions.3 To answer critical oral health-related research questions, investigators often rely on small local datasets, which are difficult to generalize. Alternatively, data are sometimes obtained from third-party payers (eg, dental insurance companies). The usefulness of these data may be limited as they are focused primarily on billed services, and many patients self-pay for dental care without involving a third party. The National Health and Nutritional Examination Survey4 and Behavioral Risk Factor Surveillance System5 are large oral health datasets, providing a view of the population’s dental status but contain limited information on dental diagnoses and actual treatments received. Linked datasets from medical and dental Electronic Health Records (EHRs) are also sorely lacking, impairing the ability to investigate relationships between oral health and general health.6,7 Recognizing this conundrum, we developed a centralized dental data repository using the i2b2 platform,8 called BigMouth.9 BigMouth was successfully launched in August 2012 with data on 1.1 million patients derived from dental EHRs of 4 dental schools—all members of the Consortium of Oral Health Research and Informatics (COHRI).10 Less than a decade later, BigMouth has grown into a formidable dental RPDR with 11 academic dental institutions contributing data on over 4.507 million patients (see Table 1) with diverse geographic coverage (see Figure 1).
Table 1.
BigMouth data elements by contributing institutions/site
| Data | Demographics | Diagnoses | Forms | Insurance | Odontogram | Periodontal Charts | Practice | Medications | Procedures |
|---|---|---|---|---|---|---|---|---|---|
| Site | |||||||||
| UT Houston | 430 189 | 106 723 | 160 211 | 59 992 | 397 847 | 53 500 | 239 172 | 50 626 | 234 482 |
| UCSF | 993 959 | 261 980 | 121 888 | 126 537 | 844 575 | 79 931 | 571 218 | 42 558 | 635 216 |
| HSDM | 97 838 | 28 440 | 43 687 | 26 544 | 88 675 | 21 403 | 53 441 | 15 297 | 55 824 |
| Tufts | 425 100 | 0 | 127 228 | 122 673 | 379 490 | 83 898 | 241 787 | 56 502 | 245 925 |
| U Pitt | 291 648 | 0 | 103 591 | 71 319 | 256 299 | 30 856 | 115 668 | 36 328 | 117 202 |
| U Michigan | 484 781 | 33 780 | 133 216 | 227 235 | 420 802 | 61 358 | 307 904 | 46 009 | 308 348 |
| UC Denver | 167 180 | 14 714 | 48 986 | 44 644 | 142 594 | 34 117 | 99 143 | 41 096 | 105 688 |
| Loma Linda | 482 526 | 22 961 | 195 839 | 115 082 | 393 961 | 67 686 | 207 089 | 32 584 | 210 171 |
| U Buffalo | 231 398 | 22 741 | 21 317 | 9903 | 217 777 | 9822 | 23 812 | 12 021 | 25 065 |
| U Iowa | 801 739 | 898 | 464 412 | 325 697 | 665 953 | 53 844 | 518 717 | 142 689 | 512 259 |
| U Minnesota | 101 274 | 3689 | 101 274 | 77 535 | 101 274 | 46 393 | 95 410 | 49 836 | 97 019 |
| Total patients | 4 507 632 | 495 926 | 1 478 902 | 1 207 161 | 3 909 247 | 542 808 | 2 473 361 | 525 546 | 2 547 199 |
Figure 1.
Timeline showing the year institutions began contributing to BigMouth, and current geographic coverage of patients (by zip code).
MAIN PURPOSE OF BigMouth
The objectives of BigMouth include informing the feasibility of research studies, executing informatic, population health, and observational studies, supporting quality improvement efforts, participation in data-driven research networks, and identifying clinical trial cohorts for recruitment. However, as a dental RPDR, BigMouth also fulfills several other purposes.
Assessment of oral health status quo
BigMouth’s data on 4.5 million patients distributed throughout the United States provide a remarkable window into the oral health status of a diverse patient population. BigMouth has been used to support, or refute, hypotheses of research proposals by generating preliminary data for funding applications and has therefore influenced the direction of oral health research. Moreover, BigMouth has been used to assess the quality of health intervention for specific patient populations, for example, providing dental care to women while pregnant,11 patients with diabetes,12 or children receiving sealants.13,14 Importantly, to date, the 11 participating BigMouth institutions are all academic—but vary in clinic size and resources for conducting research, and the results generated by BigMouth studies have started to illustrate that dental treatments in these educational settings are safe, effective, and cost-efficient.15,16
Research education mission
BigMouth provides a secure environment in which oral health researchers at all levels (faculty, dental students, specialty trainees, master-level students, and doctoral-level students) have rapid access to a large dataset for analysis. Crucially, BigMouth serves as a “sandbox” to learn how to conduct clinical research using “real-world data,” appreciating all their limitations, including data availability, data quality, and challenges of electronic phenotyping.17
Research priorities
By pooling datasets, BigMouth presents a more complete picture of types of patients. More specifically, BigMouth facilitates the study of oral manifestations of rare diseases that can lead to better understanding of the factors that affect more common diseases. Such rare diseases have a prevalence of fewer than 5 cases per 10 000 population18 with a 15% manifestation with oral-facial symptoms. As it takes on average 7 years to diagnose a rare disease, dentists can significantly influence identifying a rare disease by its oral symptomatology and help manage oral and overall quality of life.19 Infrequent diseases with oral health syndromes20 may be easier to locate in dental EHRs; however, individual institutions may not have enough patients with the disease for meaningful research. Another critical priority of BigMouth is the connection of oral health with general health. Information exchange between medical and dental EHRs is sorely limited because of ongoing interoperability issues, lack of consensus of what key components should be recorded in a patient’s record, and lack of documentation standards for dental EHRs.21,22 BigMouth includes medical history data and data on medications, as such allowing for investigation of the oral health-overall health relationship.23 Importantly, BigMouth will also allow for the building of a sustainable dental learning health system focused on providing patients with safe and effective oral health care.
GOVERNANCE
As part of the formation of BigMouth, a data governance framework was developed that encouraged data sharing while allowing control of contributed data.9 BigMouth was originally conceived and remains as a single central repository, where all sites deposit their data. While there have been discussions about moving to a federated model, the complexity of requiring contributing sites to host their own i2b2 instances was a major barrier. Over time, changes were made to encourage site participation, access of data, execution of research studies, and sustainability. Specifically, data from beyond the original dental EHR (axiUm, Vancouver, Canada) were accepted by BigMouth, allowing for more sites to participate. This is important as several institutions are moving to Epic (Epic, Verona, WI). The Governance Committee permits noncontributing sites to receive data from BigMouth as long as those queries are for noncommercial purposes. The decision to limit access to data in BigMouth to nonprofits was based on advice from institutional legal representatives to ensure there was no perception that patient data were being monetized. As our institutions are gaining experience and developing formal policies for collaborating with for-profit entities for discovery using EHR data, we expect to revisit our restrictions on limiting access.
A 3-year National Library of Medicine resource development grant (G08LM010075) originally supported the formation of BigMouth and sharing of data from the 4 founding institutions. Supporting sustainability, a one-time setup fee of $10 000 has been implemented for new sites, and all sites pay an annual fee of $2500 which supports updating the repository on a quarterly basis. Although there is no cost for participating sites to query summary data using i2b2 web interface, there is now a fee schedule, based on complexity, for requests that require extracting data with costs for noncontributing members being higher than for contributors.
OPERATIONS
Conducting research using BigMouth: approaches and lessons learned
Researchers aspiring to use BigMouth data submit a proposal using a predefined template. Each contributing site has a representative who will first independently review the proposal based on scientific merit, potential overlap with other approved BigMouth projects, and if the institution agrees to share data for the proposed research. To date, the BigMouth committee has formally reviewed and approved 18 research proposals. In order to minimize the back and forth, researchers are now invited to join the committee discussion which has led to a robust process with faster approvals.
BigMouth has been used for a variety of scientific purposes, including:
Clinical Research: For example, assessing the use of opioid and antibiotics medications in academic dental settings.
Quality Improvement: As BigMouth contains structured data, it is particularly amenable for quality measurement.11,12,24
Operations: For example, enhancement of the Odontosearch tool to help identify human remains.25
Educational Research: For example, assessing the value of a generalist versus specialist teaching model for periodontics.26
BigMouth is emerging as an indispensable tool that has served as a data source for our learners27 and faculty.9,28–30
Challenges of using BigMouth match those reported for the use of EHR data for research. EHR data are primarily collected for clinical purposes, and are not entirely representative of the population, contain missing data, may imperfectly characterize outcomes, have uncalibrated clinicians input data, and are likely to contain various levels of accuracy.31 Through COHRI, the contributing sites are encouraged to use standardized data collection tools such as a dental diagnostic terminology (SNODDS) and medical and dental history data collection forms. These standardized terminologies have formed the basis for allowing users to query BigMouth. Each user logging into BigMouth can view 2 folders in the ontology (a) site-level terminology and (b) COHRI terminology. A site-level terminology contains terms from the local EHR as is without many transformations. This hierarchy provides users an opportunity to browse through terms that they are familiar with and run queries to get patient counts at their local institution. The BigMouth common data model or “COHRI” terminology combines concepts from all institutions and allows users to run queries across the entire database.
Data accuracy is often difficult to determine, as there are no external data sources for validation purposes, and is often ascertained by assessing if these data are within expected boundaries. Patients also do not always report medical comorbidities such as diabetes and hypertension status to dentists, leading to possible underreporting in the dental EHR.32 Assessing the consistency of the data is even more challenging as the data come from various institutions with a mix of learners and faculty providers.
The BigMouth technical team and researchers work together during the data extraction phase to identify data quality issues. Data quality is checked after data are extracted from sites, and after the load process. Quality checks after data extraction are conducted through an automated script which compares data received from all institutions with the previous extract received from the same site to flag any possible issues. Quality checks are also performed after data are loaded though a system sanity checklist that is used as a guideline to test both data and the functionality of the BigMouth querying interface. There is also often a virtuous cycle where any data quality issues can be communicated to the contributing sites, who can make changes to their EHR to mitigate concerns for the future. We have also found that clinical users, who are often reticent in having to collect structured data in the EHR while treating patients, become more understanding of the importance of secondary data use.
Lastly, we have found the need to provide training sessions that cover the use of the i2b2 web interface in order to explore the type and amount of data available, appropriate observational study designs that can be used, how to formulate research questions, and how to submit a full project proposal.
Ongoing adoption of BigMouth
Contributing institutions value their inclusion in BigMouth as they gain access to a large national dental dataset which directly or indirectly has fostered new research collaborations, provided diverse clinical, epidemiological, statistical, and informatics expertise, and provided an additional venue for professional development. Barriers for other institutions to become a BigMouth contributor include limited technical personnel supporting the data extraction process, costs, lack of perceived value, and absence of leadership support.
New users who are interested in contributing data must be members of COHRI whose mission is to promote and support collaboration for research and education amongst dental institutions.10 There continues to be excellent communication and overlap between the leadership of COHRI and members of the BigMouth project review committee. While our focus has been on onboarding new sites that use the axiUm EHR, we have recently pivoted to onboarding sites with different EHRs. New sites often join due to advocacy of their faculty who may have heard about BigMouth from other colleagues. We, therefore, anticipate that an institution’s decision to adopt BigMouth is more akin to a “complex contagion” as defined by Centola, where interest and adoption are driven by reinforcement from multiple sources or wide bridges.33
Envisioning the future of BigMouth
We consider the 10-year development horizon for BigMouth to drive strategic developments and enable the broader community of data repository experts and learning health system advocates to forge collaborations that will widen the impact of data to improve health outcomes. Accordingly, we have 3 focus areas:
Connecting with medical data: The FDI World Dental Federation’s (FDI) definition of oral health reads: “Oral health is multifaceted and includes the ability to speak, smile, smell, taste, touch, chew, swallow and convey a range of emotions through facial expressions with confidence and without pain, discomfort and disease of the craniofacial complex.”34 Connecting a dental RPDR to a medical EHR might allow us to find correlations between periodontitis and cardiovascular disease.35,36
Expanding types of data in BigMouth: Our vision is to incorporate dental imaging data (2d and 3d) and mandate the use of standardized diagnostic terminologies by all contributing institutions. Connecting to mobile health apps that collect patient-reported outcomes37–39 as well as patient-reported experience measures40 is also crucial aspiring toward a more holistic definition of oral health.
Using BigMouth to improve oral health care: Dentistry lags behind the medical profession in fostering the uptake of research-informed treatments.41–43 The use of computerized knowledge management, for example, in the form of audit and feedback and clinical decision support has been introduced in the oral health arena44–46 and will undoubtedly facilitate alignment of every day dental practice with evidence-based guidelines.47 Hence, BigMouth is positioned to play an important role in getting dental teams and clinics to adopt and consistently use evidence-based oral health guidelines and will be a catalyst for the transition from payment-focused care48 to culturally sensitive, effective, and high-value oral health care.14
We have many challenges ahead, including the expansion of BigMouth to other contributing institutions. While we have developed a process for rapidly incorporating data from the axiUm, EHR, we will need to develop scalable approaches for incorporating data from other platforms. We also strive to include contributing institutions globally, which will require an understanding of legal and policy issues of sharing patient data across borders. While dental institutions have been willing to share patient data, we expect more challenges for connecting or incorporating data from the patient’s medical record. Returning to the FDI definition, we aspire to embrace this holistic definition and finally help move dentistry from treating disease to treating a person with disease.
CONCLUSION
Visionary leadership, combined with a strong governance approach to data sharing, has made the large-scale dental data repository, BigMouth, a reality. Initial federal funding and ongoing efforts to develop sustainability have supported researchers’ efforts to mine data otherwise not available to advance dental research.
FUNDING
This work was supported initially by the National Library of Medicine (grant number G08LM010075).
AUTHOR CONTRIBUTIONS
MFW, EK, and HS conceptualized the manuscript and wrote an initial draft. All authors expanded, proofread, and substantially edited the manuscript. MFW, EK, and JMW secured funding for the project.
ACKNOWLEDGMENTS
We thank Dean John Valenza at UTHealth School of Dentistry for his ongoing support of and belief in BigMouth. We also thank Joseph Applegate, Susan Guerero, and Dr Elmer Bernstam from the UTHealth School of Biomedical Informatics for their continued contributions to maintaining BigMouth. We also thank Roger Gillie from the University of Michigan School of Dentistry and Dr Charles Sfeir from the University of Pittsburgh School of Dental Medicine for representing their institutions.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
REFERENCES
- 1. Munson B, Vujicic M.. Supply of Dentists in the United States Is Likely to Grow. Health Policy Institute Research Brief. Chicago, IL: American Dental Association; 2014. [Google Scholar]
- 2. Franklin A, Gantela S, Shifarraw S, et al. Dashboard visualizations: supporting real-time throughput decision-making. J Biomed Inform 2017; 71: 211–21. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine and National Research Council. Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Washington, DC: The National Academies Press; 2011: 296. [Google Scholar]
- 4. Zipf G, Chiappa M, Porter K, Ostchega Y, Lewis B, Dostal J.. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat Ser 1 Programs Collect Proced 2013; (56): 1–37. [PubMed] [Google Scholar]
- 5. Remington PL, Smith MY, Williamson DF, Anda RF, Gentry EM, Hogelin GC.. Design, characteristics, and usefulness of state-based behavioral risk factor surveillance: 1981–87. Public Health Rep 1988; 103 (4): 366. [PMC free article] [PubMed] [Google Scholar]
- 6. Boland MR, Hripcsak G, Albers DJ, et al. Discovering medical conditions associated with periodontitis using linked electronic health records. J Clin Periodontol 2013; 40 (5): 474–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kalenderian E, Halamka JD, Spallek H.. An EHR with teeth. Appl Clin Inform 2016; 7 (2): 425–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murphy SN, Weber G, Mendis M, et al. Serving the enterprise and beyond with informatics for integrating biology and the bedside (i2b2). J Am Med Inform Assoc 2010; 17 (2): 124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Walji MF, Kalenderian E, Stark PC, et al. BigMouth: a multi-institutional dental data repository. J Am Med Inform Assoc: JAMIA 2014; 21 (6): 1136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stark PC, Kalenderian E, White JM, et al. ; Consortium for Oral Health-Related Informatics (COHRI). Consortium for oral health-related informatics: improving dental research, education, and treatment. J Dent Educ 2010; 74 (10): 1051–65. [PMC free article] [PubMed] [Google Scholar]
- 11. Neumann A, Obadan-Udoh E, Bangar S, et al. Number of pregnant women at four dental clinics and the care they received: a dental quality eMeasure evaluation. J Dent Educ 2019; 83 (10): 1158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neumann A, Kalenderian E, Ramoni R, et al. Evaluating quality of dental care among patients with diabetes: adaptation and testing of a dental quality measure in electronic health records. J Am Dent Assoc 2017; 148 (9): 634–43.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kumar SV, Bangar S, Neumann A, et al. Assessing the validity of existing dental sealant quality measures. J Am Dent Assoc 2018; 149 (9): 756–64.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yansane A, Listl S, Dawda D, et al. Increasing value, reducing waste: tailoring the application of dental sealants according to individual caries risk. J Public Health Dent 2020; 80 (Suppl 2): S8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tokede O, Ramoni RB, Patton M, Da Silva JD, Kalenderian E.. Clinical documentation of dental care in an era of electronic health record use. J Evid Based Dent Pract 2016; 16 (3): 154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kalenderian E, Obadan-Udoh E, Yansane A, et al. Feasibility of electronic health record-based triggers in detecting dental adverse events. Appl Clin Inform 2018; 9 (3): 646–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rogers JR, Lee J, Zhou Z, Cheung YK, Hripcsak G, Weng C.. Contemporary use of real-world data for clinical trial conduct in the United States: a scoping review. J Am Med Inform Assoc: JAMIA 2021; 28 (1): 144–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Molina-Garcia A, Castellanos-Cosano L, Machuca-Portillo G, Posada-de la Paz M.. Impact of rare diseases in oral health. Med Oral Patol Oral Cir Bucal 2016; 21 (5): e587–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wiemann S, Frenzel Baudisch N, Jordan RA, Kleinheinz J, Hanisch M.. Oral symptoms and oral health-related quality of life in people with rare diseases in Germany: a cross-sectional study. Int J Environ Res Public Health 2018; 15 (7): 1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parker SE, Mai CT, Canfield MA, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol 2010; 88 (12): 1008–16. [DOI] [PubMed] [Google Scholar]
- 21. Simon L, Obadan-Udoh E, Yansane AI, et al. Improving oral-systemic healthcare through the interoperability of electronic medical and dental records: an exploratory study. Appl Clin Inform 2019; 10 (3): 367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schleyer T, Spallek H, Hernandez P.. A qualitative investigation of the content of dental paper-based and computer-based patient record formats. J Am Med Inform Assoc: JAMIA 2007; 14 (4): 515–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Messing M, Souza LC, Cavalla F, et al. Investigating potential correlations between endodontic pathology and cardiovascular diseases using epidemiological and genetic approaches. J Endod 2019; 45 (2): 104–10. [DOI] [PubMed] [Google Scholar]
- 24. Neumann A, Kumar S, Bangar S, et al. Tobacco screening and cessation efforts by dental providers: a quality measure evaluation. J Public Health Dent 2019; 79 (2): 93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Adams BJ. Establishing personal identification based on specific patterns of missing, filled, and unrestored teeth. J Forensic Sci 2003; 48 (3): 487–96. [PubMed] [Google Scholar]
- 26. Sajadi A. Clinical Accuracy of Pre-doctoral Periodontal Education in the US: An Evaluation of the Generalist and Specialist Teaching Models on Periodontal Education. Houston, TX: The University of Texas School of Dentistry at Houston; 2015. [Google Scholar]
- 27. Tran DT, Gay IC, Du XL, et al. Partial-mouth periodontal examination protocol for estimating periodontitis extent and severity in a US population. Clin Exp Dent Res 2016; 2 (1): 73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Walji M, Ramoni R, Simmons K, et al. Using EHRs and big data for measuring oral healthcare quality. J Dent Res 2017; 96 (A): 0553. [Google Scholar]
- 29. Kumar S, Obadan-Udoh E, Yansane A, et al. Monitoring sealant treatment practices using EHR-based quality measures. J Dent Res 2018; 97 (A): 2849700. [Google Scholar]
- 30. Kalenderian E, Obadan-Udoh E, Neumann A, et al. Mining the electronic health record for dental adverse events. J Dent Res 2018; 97 (A): 2853847. [Google Scholar]
- 31. Mc Cord KA, Hemkens LG.. Using electronic health records for clinical trials: where do we stand and where can we go? CMAJ 2019; 191 (5): E128–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Adibi S, Li M, Salazar N, et al. Medical and dental electronic health record reporting discrepancies in integrated patient care. JDR Clin Trans Res 2020; 5 (3): 278–83. [DOI] [PubMed] [Google Scholar]
- 33. Centola D. How Behavior Spreads: The Science of Complex Contagions. Princeton, NJ: Princeton University Press; 2018. [Google Scholar]
- 34.Federation FWD. FDI’s Definition of Oral Health. Geneva, Switzerland: FDI. https://www.fdiworlddental.org/fdis-definition-oral-health. Accessed January 1, 2022.
- 35. Hansen GM, Egeberg A, Holmstrup P, Hansen PR.. Relation of periodontitis to risk of cardiovascular and all-cause mortality (from a Danish nationwide cohort study). Am J Cardiol 2016; 118 (4): 489–93. [DOI] [PubMed] [Google Scholar]
- 36. Jeffcoat MK, Jeffcoat RL, Gladowski PA, Bramson JB, Blum JJ.. Impact of periodontal therapy on general health: evidence from insurance data for five systemic conditions. Am J Prev Med 2014; 47 (2): 166–74. [DOI] [PubMed] [Google Scholar]
- 37. Wagle NW. Implementing patient-reported outcome measures. NEJM Catalyst. http://catalyst.nejm.org/implementing-proms-patient-reported-outcome-measures/. Accessed January 1, 2022.
- 38. Wittneben JG, Wismeijer D, Bragger U, Joda T, Abou-Ayash S.. Patient-reported outcome measures focusing on aesthetics of implant- and tooth-supported fixed dental prostheses: a systematic review and meta-analysis. Clin Oral Implants Res 2018; 29 (Suppl 16): 224–40. [DOI] [PubMed] [Google Scholar]
- 39. Yao CJ, Cao C, Bornstein MM, Mattheos N.. Patient-reported outcome measures of edentulous patients restored with implant-supported removable and fixed prostheses: a systematic review. Clin Oral Implants Res 2018; 29 (Suppl 16): 241–54. [DOI] [PubMed] [Google Scholar]
- 40. Hodson M, Andrew S, Roberts CM.. Towards an understanding of PREMS and PROMS in COPD. Breathe 2013; 9 (5): 358–64. [Google Scholar]
- 41. O'Donnell JA, Modesto A, Oakley M, Polk DE, Valappil B, Spallek H.. Sealants and dental caries: insight into dentists’ behaviors regarding implementation of clinical practice recommendations. J Am Dent Assoc 2013; 144 (4): e24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rindal DB, Rush WA, Boyle RG.. Clinical inertia in dentistry: a review of the phenomenon. J Contemp Dent Pract 2008; 9 (1): 113–21. [PubMed] [Google Scholar]
- 43. Van der Sanden WJ, Nienhuijs ME, Mettes TG.. The role of guidelines and systematic reviews in oral healthcare. Ned Tijdschr Tandheelkd 2007; 114 (4): 179–86. [PubMed] [Google Scholar]
- 44. Loffler C, Bohmer F.. The effect of interventions aiming to optimise the prescription of antibiotics in dental care – a systematic review. PloS One 2017; 12 (11): e0188061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Elouafkaoui P, Young L, Newlands R, et al. An audit and feedback intervention for reducing antibiotic prescribing in general dental practice: the RAPiD cluster randomised controlled trial. PLOS Med 2016; 13 (8): e1002115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tianviwat S, Hintao J, Chongsuvivatwong V, Thitasomakul S.. Improvement of dental nurses awareness of school dental sealant quality following the audit and feedback system: first phase of implementation. Edorium J Dent 2015; 2: 7–14. [Google Scholar]
- 47. Titler MG, Titler P.. The evidence for evidence-based practice implementation. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008: 1-113–1-132. [Google Scholar]
- 48. Voinea-Griffin A, Fellows JL, Rindal DB, Barasch A, Gilbert GH, Safford MM.. Pay for performance: will dentistry follow? BMC Oral Health 2010; 10: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.